User login
Architect of VA Transformation Urges Innovation Amid Uncertainty
Architect of VA Transformation Urges Innovation Amid Uncertainty
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
Architect of VA Transformation Urges Innovation Amid Uncertainty
Architect of VA Transformation Urges Innovation Amid Uncertainty
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
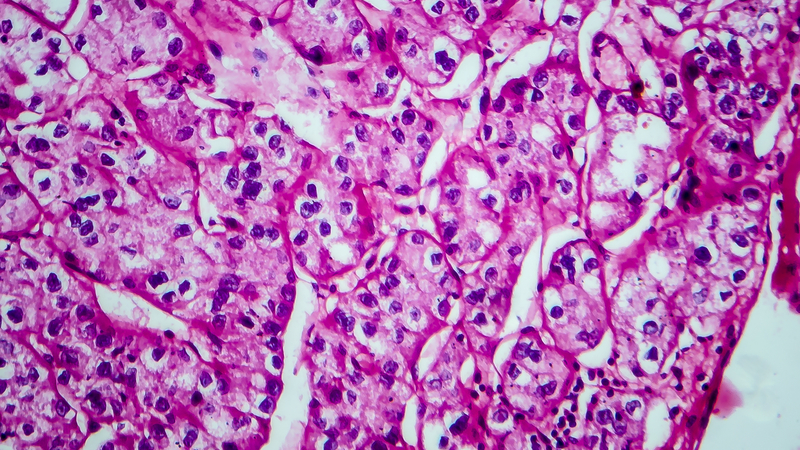
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treatment of metastatic renal cell carcinoma (RCC) is complex and requires careful analysis of risk and treatment options, an oncologist said at the July Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, regarding treating veterans with kidney cancer.
“We’ve come a long way in treating this disease, but individualizing therapy remains critical, especially in complex populations like our veterans,” said Matthew B. Rettig, MD, chief of Hematology-Oncology at the Veterans Affairs Greater Los Angeles Healthcare System and professor of Medicine and Urology at UCLA.
Rettig emphasized 2 critical early questions clinicians should consider when encountering metastatic RCC. First: Can the patient be treated with localized interventions such as metastasectomy, radiation therapy, or nephrectomy? These can be curative, Rettig said.
And second: Does the patient currently need systemic therapy? “[There are] a small subset of patients,” Rettig said, “who go into a durable, complete remission, dare I say ‘cure,’ with immunotherapeutic-based approaches.”
Rettig highlighted the International Metastatic Renal Cell Carcinoma Database Consortium criteria as a guide for clinicians as they determine the best strategy for treatment. The Database Consortium estimates survival in various lines of therapy by incorporating 6 prognostic factors: anemia, hypercalcemia, neutrophilia, thrombocytosis, performance status, and time from diagnosis to treatment.
These criteria classify patients into favorable, intermediate, or poor risk categories that can guide first-line systemic therapy. The criteria also provide estimates of median survival.
Rettig noted a “huge percentage” of veterans mirror the intermediate-risk demographics of clinical trial cohorts but often present with greater comorbidity burdens: “That plays into whether we treat and how we treat,” he said.
Rettig highlighted kidney cancer guidelines from the National Comprehensive Cancer Network and noted that several trials examined first-line use of combinations of vascular endothelial growth factor receptor tyrosine kinase inhibitors (TKIs) and checkpoint inhibitors.
There’s a general theme in the findings, he said: “You have OS (overall survival) and PFS (progression-free survival) benefit in the intermediate/poor risk group, but only PFS benefit in the patients who have favorable-risk disease. And you see higher objective response rates with the combinations.
“If you have a patient who's highly symptomatic or has an organ system threatened by a metastasis, you'd want to use a combination that elicits a higher objective response rate,” Rettig added.
A TKI is going to be the most appropriate second-line therapy for patients who received a prior checkpoint inhibitor, Rettig said.
“Don't change to another checkpoint inhibitor,” he said. “We have enough phase 3 data that indicates checkpoint inhibitors are no longer really adding to benefit once they’ve had a checkpoint inhibitor.”
Rettig said to even consider checkpoint inhibitors for patients who are checkpoint inhibitor-naïve, especially given the potential for durable remissions. As for third-line therapy, he said, “we have both belzutifan and tivozanib, which have been shown to improve PFS. More studies are ongoing.”
There are many adverse events linked to TKIs, Rettig said, including cardiovascular problems, thrombosis, hypertension, heart failure, torsades de pointes, QT prolongation, and gastrointestinal toxicity. TKIs tend to be the major drivers of adverse events in combination therapy.
Rettig emphasized the shorter half-life of the TKI axitinib, which he said allows for easier management of toxicities: “That’s why it’s preferred in the VA RCC clinical pathway.”
Rettig discloses relationships with Ambrx, Amgen, AVEO, Bayer, INmune Bio, Johnson & Johnson Health Care Systems, Lantheus, Merck, Myovant, Novartis, ORIC, and Progenics.
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Treating Metastatic RCC: From Risk Assessment to Therapy Selection
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
The role of hereditary syndromes in renal cell carcinoma (RCC) might be easily missed, a kidney cancer specialist said during a recent Association of VA Hematology and Oncology (AVAHO) seminar in Long Beach, California, though careful clinical evaluation can uncover genetic traits that may affect treatment and familial risk.
“The importance of finding or identifying hereditary forms of kidney cancer really should not be underestimated,” said urologist Brian Shuch, MD, director of the UCLA Kidney Cancer Program, on treating veterans with kidney cancer.
According to Shuch, recent data suggest that about 4.5% of patients with RCC have a hereditary syndrome: “A lot of times, these hide in plain sight. You have to really look deep and try to figure things out and understand that maybe they have a hereditary form of kidney cancer.”
It is important to consider early genetic testing, Shuch said. Red flags for hereditary syndromes include early-onset RCC (age ≤ 45 years), multifocal tumors, bilateral tumors (especially in younger individuals), or a relevant family personal history, he said.
Unusual skin conditions are also potential signs, Shuch said. These can include leiomyomas, fibrofolliculomas, and angiofibromas: “Patients have lots of lumps or bumps.”
“When I look at a patient, I go head to toe and ask if there any issues with your vision, any issues with your hearing, any issues swallowing,” he explained at the meeting. “Do you have any problems with heart issues, adrenal issues? You’ve got to go through each organ, and it can lead you to different things.”
Shuch highlighted Von Hippel-Lindau (VHL) syndrome, which affects 1 in 25,000 people. About 80% to 90% of these patients have a family history, Shuch said.
But the others do not. “Unfortunately, some get diagnosed later in life because they don’t get cascade testing starting at aged 2, which is recommended. These are the patients who might be coming into the ER with a hemangioblastoma or picking up the phone and all of a sudden being deaf in one ear due to an endolymphatic sac tumor.
“We want to limit metastatic spread and preserve the kidneys,” Shuch said. “We don’t want to be doing radical nephrectomies. We want to avoid chronic kidney disease, prevent end-stage renal disease, and maximize quality of life.”
It’s a good idea to avoid surgical removal unless a patient’s tumor grows to be > 3 cm, a line that indicates risk of metastases, he said.
In terms of treatment, Shuch highlighted a 2021 study that showed benefit in VHL from belzutifan (Welireg), an oral HIF-2 α inhibitor approved by the US Food and Drug Administration. The medication significantly reduced the need for surgical intervention.
“Patients go on this drug, and surgeons are putting their scalpels down,” said Shuch, who worked on the 2021 study.
Other hereditary syndromes include the rare hereditary papillary RCC, and Birt-Hogg-Dubé syndrome, believed to affect 1 in 200,000 people but may be more common, he said.
Birt-Hogg-Dubé syndrome is linked to lung cysts, lung collapse, and skin manifestations. The 3 cm surgery rule is appropriate in these cases, Shuch said, and metastases are rare.
Another condition, hereditary leiomyomatosis and RCC, is the most dangerous hereditary form. Originally thought to affect 1 in 200,000 people, hereditary leiomyomatosis and RCC is similar to Birt-Hogg-Dubé syndrome in that it is believed to be more common.
“You will see this,” Shuch predicted.
Shuch advised colleagues to intervene early and take a large margin during surgery.
He also highlighted familial paraganglioma syndrome, which is associated with gastrointestinal stromal tumors, and Cowden syndrome, which is linked to skin manifestations and breast, thyroid, and endometrial cancer.
Shuch reported that he had no disclosures.
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
Renal Cell Carcinoma: What You Need to Know About Hereditary Syndromes
What Hematologists Should Know About Cutaneous Porphyria and Hemochromatosis
One patient, a 39-year-old woman, went to a dermatologist seeking care for fluid-filled blisters over the backs of her hands and arms. Another patient, a 56-year-old man, sought care from his general practitioner owing to fatigue.
Their presentations were quite different, but the two patients shared one thing in common: iron overload. Both ended up in the care of hematologists who diagnosed their conditions as porphyria cutanea tarda (PCT) and hemochromatosis, respectively.
A pair of hematologists discussed the treatment of these disorders at the American Society of Hematology (ASH) 2024 Annual Meeting and in reports in Hematology: American Society of Hematology Education Program. Here’s a look at the guidance they provided.
Porphyria Cutanea Tarda: Skin Trouble
Testing revealed that the female patient had a highly elevated porphyrin levels: Her urine uroporphyrin was 3959 nmol/L (normal, < 30 nmol/L) and plasma uroporphyrin was 2.0 µg/dL (normal, < 1.0 µg/dL). Her serum ferritin level was also high, at 420 ng/mL (normal, < 200 ng/mL).
Rebecca Karp Leaf, MD, of Massachusetts General Hospital and Harvard Medical School, diagnosed her with PCT, a disorder of heme biosynthesis that often presents with skin manifestations.
As co-founder and co-director of the Boston hospital’s Porphyria Center, Karp Leaf is a leading expert in PCT, a rare disease that affects 5-10 people per 100,000. In addition to speaking at the ASH meeting in December, she described PCT in a December 2024 article in Hematology: American Society of Hematology Education Program.
PCT is caused by inhibition of an enzyme in heme biosynthesis and leads to accumulation of porphyrins in the liver and plasma, Karp Leaf said. Through a complex process, excess of iron leads to inhibition of the enzyme, which leads to a buildup of toxic porphyrins, she said. The condition causes painless, blistering lesions on sun-exposed skin, scarring, skin fragility, dark urine, and liver disease.
PCT most commonly occurs in middle age after the age of 40 and affects men more than women. “It’s the only porphyria that can occur absent a genetic variant,” she said, and 75% of cases have no genetic component.
Options for Treatment Include Antivirals and Phlebotomy
Risk factors for PCT include alcohol use, smoking, exogenous estrogen, hepatitis, and HIV mutations.
In regard to treatment, “modification of risk factors can be variably helpful: alcohol and smoking cessation, stopping exogenous estrogen, sun-protective clothing, and steroid-containing creams for lesions,” Karp Leaf said. “Most patients typically require further therapy to reduce liver porphyrins.”
Urine and plasma tests can help with diagnosis, she said. In patients with hepatitis C (HCV), “direct-acting antivirals can actually lead to resolution of PCT without any other therapy. We suspect that with effective antiviral treatment for HCV, the incidence of PCT will really go down.”
Therapeutic phlebotomy — blood removal — is another option. “It’s one of my favorite therapies because you don’t have to give somebody a drug. You can just take out iron,” Karp Leaf said. “Typically, we’ll start with venesection of 450 ccs of whole blood every 2 weeks, We target a ferritin level of 20 [ng/mL] but permit it up to 50 [ng/mL], or a little bit higher.”
The treatment leads to resolution of blisters in about 2-3 months, she said, and normalization of porphyrins by 13 months. Patients typically require about 6-8 treatments, she said.
Another option is iron chelation, iron removal via medicine, “but it’s expensive, has side effects, and is really not recommended if other treatments are available,” she said.
Hydroxychloroquine Can Be Helpful Too
Low-dose hydroxychloroquine can also be effective at 100 mg twice a week, “much lower than what we use in autoimmune disease,” Karp Leaf said. “We suspect that it’s taken up by the hepatic lysosomes and causes release of porphyrins. It causes clinical remission in about 6 months.”
However, higher doses can lead to liver injury, and the drug’s use is limited in end-stage kidney disease since porphyrins are excreted in the urine. These patients are especially difficult to treat, she said.
In the case of the 39-year-old patient, Karp Leaf recommended that the woman reduce her alcohol intake and begin using a copper intrauterine device for contraception instead of a combined oral contraceptive pill, which allowed her to undergo phlebotomy.
“She needed about eight sessions of therapeutic phlebotomy to achieve a ferritin of 30 [ng/mL], and her lesions resolved in 6 months,” Karp Leaf said. “Her plasma porphyrins resolved by 12 months. Her liver biochemistries were a bit elevated, and they subsequently normalized.”
Karp Leaf said she sees the patient about once a year.
Hemochromatosis: It’s (Probably) a Family Affair
In an adjoining presentation at ASH and in a December 2024 article in Hematology: American Society of Hematology Education Program, hematologist Domenico Girelli, MD, PhD, with the University of Verona, Italy, told colleagues about the 56-year-old male patient with fatigue. He also had a mildly enlarged liver, hyperferritinemia (890 µg/L vs normal value < 300 µg/L) and a mildly increased alanine aminotransferase level (46 U/L vs normal value < 40 U/L).
The patient was diagnosed with hemochromatosis, a genetic disorder caused by mutations that leads to increased transferrin saturation, Girelli said.
“By definition, hemochromatosis is characterized by the absence of signs of a primary red blood cell disorder — different from other disorders like transfusion iron overload or iron-loading anemias,” he said.
It’s also important to consider other possible causes of hyperferritinemia, because most cases of the symptom aren’t related to iron overload, he said. “A careful clinical history and a few laboratory parameters including transferrin saturation are generally sufficient for the differential diagnosis.”
As Girelli noted, “hemochromatosis can have a wide clinical spectrum ranging from mild to severe forms, which are strongly influenced by the co-presence of risk factors like alcohol [use], blood transfusion, and genetic factors captured by polygenic risk score.”
In Many Cases, Hemochromatosis Can Be Successfully Treated
According to Girelli, it’s important to understand the disease stage, because this information can predict the probability of advanced liver fibrosis, which can be a sign of a worse prognosis.
“The strongest clinical predictors of advanced liver fibrosis are ferritin higher than 1000 [µg/L] and the presence of arthropathy [joint disease],” he said. “If both are absent and the patient is asymptomatic, there is no need for further investigation. If both are present, further investigation — including cardiac MRI and full endocrine profile — are indicated. Liver biopsy may be indicated only in uncertain cases.”
Fortunately, “most patients are diagnosed in preclinical or early stage, and their prognosis is excellent, with a normal life expectancy,” he said
Phlebotomy remains the standard of care for hemochromatosis in uncomplicated cases. “It is safe, cheap, well-tolerated, and significantly reduces mortality and morbidity, especially when it is started before the development of cirrhosis,” he said.
Family Members Should Be Tested for Genetic Traits
It’s important to advise patients prior to phlebotomy to avoid undercooked seafood and wound contact with sea water because of the risk for sepsis due to the pathogen Vibrio vulnificus, Girelli said.
And it’s a good idea to test family members to see if they share a genetic risk for hemochromatosis, he said. The 56-year-old patient’s brother turned out to also have genetic risk, and his iron levels were very high. He had recently been diagnosed with seronegative arthritis that could be classified as secondary to hemochromatosis.
For management, Girelli said, patients should minimize or avoid alcohol consumption, eat a healthy diet, and avoid vitamin C and iron supplements even in multivitamin compounds. Patients should be encouraged to exercise and maintain an ideal weight.
The 56-year-old patient fared well, reaching a ferritin target of 50 mg/mL after multiple phlebotomy procedures that removed nearly 5 g of iron.
The patient tolerated the treatment and his fatigue resolved, Girelli said. “The maintenance treatment consisted of 3 phlebotomies per year. The patient remained asymptomatic and was eventually enrolled as a regular blood donor.”
Karp Leaf disclosed relationships with Alnylam, Recordati, and Disc Medicine. She is a member of the Porphyrias Consortium, part of the Rare Diseases Clinical Research Network, funded by the National Institutes of Health and led by the National Center for Advancing Translational Sciences (NCATS). The consortium is funded by NCATS and the National Institute of Diabetes and Digestive and Kidney Diseases. Girelli had no disclosures.
A version of this article first appeared on Medscape.com.
One patient, a 39-year-old woman, went to a dermatologist seeking care for fluid-filled blisters over the backs of her hands and arms. Another patient, a 56-year-old man, sought care from his general practitioner owing to fatigue.
Their presentations were quite different, but the two patients shared one thing in common: iron overload. Both ended up in the care of hematologists who diagnosed their conditions as porphyria cutanea tarda (PCT) and hemochromatosis, respectively.
A pair of hematologists discussed the treatment of these disorders at the American Society of Hematology (ASH) 2024 Annual Meeting and in reports in Hematology: American Society of Hematology Education Program. Here’s a look at the guidance they provided.
Porphyria Cutanea Tarda: Skin Trouble
Testing revealed that the female patient had a highly elevated porphyrin levels: Her urine uroporphyrin was 3959 nmol/L (normal, < 30 nmol/L) and plasma uroporphyrin was 2.0 µg/dL (normal, < 1.0 µg/dL). Her serum ferritin level was also high, at 420 ng/mL (normal, < 200 ng/mL).
Rebecca Karp Leaf, MD, of Massachusetts General Hospital and Harvard Medical School, diagnosed her with PCT, a disorder of heme biosynthesis that often presents with skin manifestations.
As co-founder and co-director of the Boston hospital’s Porphyria Center, Karp Leaf is a leading expert in PCT, a rare disease that affects 5-10 people per 100,000. In addition to speaking at the ASH meeting in December, she described PCT in a December 2024 article in Hematology: American Society of Hematology Education Program.
PCT is caused by inhibition of an enzyme in heme biosynthesis and leads to accumulation of porphyrins in the liver and plasma, Karp Leaf said. Through a complex process, excess of iron leads to inhibition of the enzyme, which leads to a buildup of toxic porphyrins, she said. The condition causes painless, blistering lesions on sun-exposed skin, scarring, skin fragility, dark urine, and liver disease.
PCT most commonly occurs in middle age after the age of 40 and affects men more than women. “It’s the only porphyria that can occur absent a genetic variant,” she said, and 75% of cases have no genetic component.
Options for Treatment Include Antivirals and Phlebotomy
Risk factors for PCT include alcohol use, smoking, exogenous estrogen, hepatitis, and HIV mutations.
In regard to treatment, “modification of risk factors can be variably helpful: alcohol and smoking cessation, stopping exogenous estrogen, sun-protective clothing, and steroid-containing creams for lesions,” Karp Leaf said. “Most patients typically require further therapy to reduce liver porphyrins.”
Urine and plasma tests can help with diagnosis, she said. In patients with hepatitis C (HCV), “direct-acting antivirals can actually lead to resolution of PCT without any other therapy. We suspect that with effective antiviral treatment for HCV, the incidence of PCT will really go down.”
Therapeutic phlebotomy — blood removal — is another option. “It’s one of my favorite therapies because you don’t have to give somebody a drug. You can just take out iron,” Karp Leaf said. “Typically, we’ll start with venesection of 450 ccs of whole blood every 2 weeks, We target a ferritin level of 20 [ng/mL] but permit it up to 50 [ng/mL], or a little bit higher.”
The treatment leads to resolution of blisters in about 2-3 months, she said, and normalization of porphyrins by 13 months. Patients typically require about 6-8 treatments, she said.
Another option is iron chelation, iron removal via medicine, “but it’s expensive, has side effects, and is really not recommended if other treatments are available,” she said.
Hydroxychloroquine Can Be Helpful Too
Low-dose hydroxychloroquine can also be effective at 100 mg twice a week, “much lower than what we use in autoimmune disease,” Karp Leaf said. “We suspect that it’s taken up by the hepatic lysosomes and causes release of porphyrins. It causes clinical remission in about 6 months.”
However, higher doses can lead to liver injury, and the drug’s use is limited in end-stage kidney disease since porphyrins are excreted in the urine. These patients are especially difficult to treat, she said.
In the case of the 39-year-old patient, Karp Leaf recommended that the woman reduce her alcohol intake and begin using a copper intrauterine device for contraception instead of a combined oral contraceptive pill, which allowed her to undergo phlebotomy.
“She needed about eight sessions of therapeutic phlebotomy to achieve a ferritin of 30 [ng/mL], and her lesions resolved in 6 months,” Karp Leaf said. “Her plasma porphyrins resolved by 12 months. Her liver biochemistries were a bit elevated, and they subsequently normalized.”
Karp Leaf said she sees the patient about once a year.
Hemochromatosis: It’s (Probably) a Family Affair
In an adjoining presentation at ASH and in a December 2024 article in Hematology: American Society of Hematology Education Program, hematologist Domenico Girelli, MD, PhD, with the University of Verona, Italy, told colleagues about the 56-year-old male patient with fatigue. He also had a mildly enlarged liver, hyperferritinemia (890 µg/L vs normal value < 300 µg/L) and a mildly increased alanine aminotransferase level (46 U/L vs normal value < 40 U/L).
The patient was diagnosed with hemochromatosis, a genetic disorder caused by mutations that leads to increased transferrin saturation, Girelli said.
“By definition, hemochromatosis is characterized by the absence of signs of a primary red blood cell disorder — different from other disorders like transfusion iron overload or iron-loading anemias,” he said.
It’s also important to consider other possible causes of hyperferritinemia, because most cases of the symptom aren’t related to iron overload, he said. “A careful clinical history and a few laboratory parameters including transferrin saturation are generally sufficient for the differential diagnosis.”
As Girelli noted, “hemochromatosis can have a wide clinical spectrum ranging from mild to severe forms, which are strongly influenced by the co-presence of risk factors like alcohol [use], blood transfusion, and genetic factors captured by polygenic risk score.”
In Many Cases, Hemochromatosis Can Be Successfully Treated
According to Girelli, it’s important to understand the disease stage, because this information can predict the probability of advanced liver fibrosis, which can be a sign of a worse prognosis.
“The strongest clinical predictors of advanced liver fibrosis are ferritin higher than 1000 [µg/L] and the presence of arthropathy [joint disease],” he said. “If both are absent and the patient is asymptomatic, there is no need for further investigation. If both are present, further investigation — including cardiac MRI and full endocrine profile — are indicated. Liver biopsy may be indicated only in uncertain cases.”
Fortunately, “most patients are diagnosed in preclinical or early stage, and their prognosis is excellent, with a normal life expectancy,” he said
Phlebotomy remains the standard of care for hemochromatosis in uncomplicated cases. “It is safe, cheap, well-tolerated, and significantly reduces mortality and morbidity, especially when it is started before the development of cirrhosis,” he said.
Family Members Should Be Tested for Genetic Traits
It’s important to advise patients prior to phlebotomy to avoid undercooked seafood and wound contact with sea water because of the risk for sepsis due to the pathogen Vibrio vulnificus, Girelli said.
And it’s a good idea to test family members to see if they share a genetic risk for hemochromatosis, he said. The 56-year-old patient’s brother turned out to also have genetic risk, and his iron levels were very high. He had recently been diagnosed with seronegative arthritis that could be classified as secondary to hemochromatosis.
For management, Girelli said, patients should minimize or avoid alcohol consumption, eat a healthy diet, and avoid vitamin C and iron supplements even in multivitamin compounds. Patients should be encouraged to exercise and maintain an ideal weight.
The 56-year-old patient fared well, reaching a ferritin target of 50 mg/mL after multiple phlebotomy procedures that removed nearly 5 g of iron.
The patient tolerated the treatment and his fatigue resolved, Girelli said. “The maintenance treatment consisted of 3 phlebotomies per year. The patient remained asymptomatic and was eventually enrolled as a regular blood donor.”
Karp Leaf disclosed relationships with Alnylam, Recordati, and Disc Medicine. She is a member of the Porphyrias Consortium, part of the Rare Diseases Clinical Research Network, funded by the National Institutes of Health and led by the National Center for Advancing Translational Sciences (NCATS). The consortium is funded by NCATS and the National Institute of Diabetes and Digestive and Kidney Diseases. Girelli had no disclosures.
A version of this article first appeared on Medscape.com.
One patient, a 39-year-old woman, went to a dermatologist seeking care for fluid-filled blisters over the backs of her hands and arms. Another patient, a 56-year-old man, sought care from his general practitioner owing to fatigue.
Their presentations were quite different, but the two patients shared one thing in common: iron overload. Both ended up in the care of hematologists who diagnosed their conditions as porphyria cutanea tarda (PCT) and hemochromatosis, respectively.
A pair of hematologists discussed the treatment of these disorders at the American Society of Hematology (ASH) 2024 Annual Meeting and in reports in Hematology: American Society of Hematology Education Program. Here’s a look at the guidance they provided.
Porphyria Cutanea Tarda: Skin Trouble
Testing revealed that the female patient had a highly elevated porphyrin levels: Her urine uroporphyrin was 3959 nmol/L (normal, < 30 nmol/L) and plasma uroporphyrin was 2.0 µg/dL (normal, < 1.0 µg/dL). Her serum ferritin level was also high, at 420 ng/mL (normal, < 200 ng/mL).
Rebecca Karp Leaf, MD, of Massachusetts General Hospital and Harvard Medical School, diagnosed her with PCT, a disorder of heme biosynthesis that often presents with skin manifestations.
As co-founder and co-director of the Boston hospital’s Porphyria Center, Karp Leaf is a leading expert in PCT, a rare disease that affects 5-10 people per 100,000. In addition to speaking at the ASH meeting in December, she described PCT in a December 2024 article in Hematology: American Society of Hematology Education Program.
PCT is caused by inhibition of an enzyme in heme biosynthesis and leads to accumulation of porphyrins in the liver and plasma, Karp Leaf said. Through a complex process, excess of iron leads to inhibition of the enzyme, which leads to a buildup of toxic porphyrins, she said. The condition causes painless, blistering lesions on sun-exposed skin, scarring, skin fragility, dark urine, and liver disease.
PCT most commonly occurs in middle age after the age of 40 and affects men more than women. “It’s the only porphyria that can occur absent a genetic variant,” she said, and 75% of cases have no genetic component.
Options for Treatment Include Antivirals and Phlebotomy
Risk factors for PCT include alcohol use, smoking, exogenous estrogen, hepatitis, and HIV mutations.
In regard to treatment, “modification of risk factors can be variably helpful: alcohol and smoking cessation, stopping exogenous estrogen, sun-protective clothing, and steroid-containing creams for lesions,” Karp Leaf said. “Most patients typically require further therapy to reduce liver porphyrins.”
Urine and plasma tests can help with diagnosis, she said. In patients with hepatitis C (HCV), “direct-acting antivirals can actually lead to resolution of PCT without any other therapy. We suspect that with effective antiviral treatment for HCV, the incidence of PCT will really go down.”
Therapeutic phlebotomy — blood removal — is another option. “It’s one of my favorite therapies because you don’t have to give somebody a drug. You can just take out iron,” Karp Leaf said. “Typically, we’ll start with venesection of 450 ccs of whole blood every 2 weeks, We target a ferritin level of 20 [ng/mL] but permit it up to 50 [ng/mL], or a little bit higher.”
The treatment leads to resolution of blisters in about 2-3 months, she said, and normalization of porphyrins by 13 months. Patients typically require about 6-8 treatments, she said.
Another option is iron chelation, iron removal via medicine, “but it’s expensive, has side effects, and is really not recommended if other treatments are available,” she said.
Hydroxychloroquine Can Be Helpful Too
Low-dose hydroxychloroquine can also be effective at 100 mg twice a week, “much lower than what we use in autoimmune disease,” Karp Leaf said. “We suspect that it’s taken up by the hepatic lysosomes and causes release of porphyrins. It causes clinical remission in about 6 months.”
However, higher doses can lead to liver injury, and the drug’s use is limited in end-stage kidney disease since porphyrins are excreted in the urine. These patients are especially difficult to treat, she said.
In the case of the 39-year-old patient, Karp Leaf recommended that the woman reduce her alcohol intake and begin using a copper intrauterine device for contraception instead of a combined oral contraceptive pill, which allowed her to undergo phlebotomy.
“She needed about eight sessions of therapeutic phlebotomy to achieve a ferritin of 30 [ng/mL], and her lesions resolved in 6 months,” Karp Leaf said. “Her plasma porphyrins resolved by 12 months. Her liver biochemistries were a bit elevated, and they subsequently normalized.”
Karp Leaf said she sees the patient about once a year.
Hemochromatosis: It’s (Probably) a Family Affair
In an adjoining presentation at ASH and in a December 2024 article in Hematology: American Society of Hematology Education Program, hematologist Domenico Girelli, MD, PhD, with the University of Verona, Italy, told colleagues about the 56-year-old male patient with fatigue. He also had a mildly enlarged liver, hyperferritinemia (890 µg/L vs normal value < 300 µg/L) and a mildly increased alanine aminotransferase level (46 U/L vs normal value < 40 U/L).
The patient was diagnosed with hemochromatosis, a genetic disorder caused by mutations that leads to increased transferrin saturation, Girelli said.
“By definition, hemochromatosis is characterized by the absence of signs of a primary red blood cell disorder — different from other disorders like transfusion iron overload or iron-loading anemias,” he said.
It’s also important to consider other possible causes of hyperferritinemia, because most cases of the symptom aren’t related to iron overload, he said. “A careful clinical history and a few laboratory parameters including transferrin saturation are generally sufficient for the differential diagnosis.”
As Girelli noted, “hemochromatosis can have a wide clinical spectrum ranging from mild to severe forms, which are strongly influenced by the co-presence of risk factors like alcohol [use], blood transfusion, and genetic factors captured by polygenic risk score.”
In Many Cases, Hemochromatosis Can Be Successfully Treated
According to Girelli, it’s important to understand the disease stage, because this information can predict the probability of advanced liver fibrosis, which can be a sign of a worse prognosis.
“The strongest clinical predictors of advanced liver fibrosis are ferritin higher than 1000 [µg/L] and the presence of arthropathy [joint disease],” he said. “If both are absent and the patient is asymptomatic, there is no need for further investigation. If both are present, further investigation — including cardiac MRI and full endocrine profile — are indicated. Liver biopsy may be indicated only in uncertain cases.”
Fortunately, “most patients are diagnosed in preclinical or early stage, and their prognosis is excellent, with a normal life expectancy,” he said
Phlebotomy remains the standard of care for hemochromatosis in uncomplicated cases. “It is safe, cheap, well-tolerated, and significantly reduces mortality and morbidity, especially when it is started before the development of cirrhosis,” he said.
Family Members Should Be Tested for Genetic Traits
It’s important to advise patients prior to phlebotomy to avoid undercooked seafood and wound contact with sea water because of the risk for sepsis due to the pathogen Vibrio vulnificus, Girelli said.
And it’s a good idea to test family members to see if they share a genetic risk for hemochromatosis, he said. The 56-year-old patient’s brother turned out to also have genetic risk, and his iron levels were very high. He had recently been diagnosed with seronegative arthritis that could be classified as secondary to hemochromatosis.
For management, Girelli said, patients should minimize or avoid alcohol consumption, eat a healthy diet, and avoid vitamin C and iron supplements even in multivitamin compounds. Patients should be encouraged to exercise and maintain an ideal weight.
The 56-year-old patient fared well, reaching a ferritin target of 50 mg/mL after multiple phlebotomy procedures that removed nearly 5 g of iron.
The patient tolerated the treatment and his fatigue resolved, Girelli said. “The maintenance treatment consisted of 3 phlebotomies per year. The patient remained asymptomatic and was eventually enrolled as a regular blood donor.”
Karp Leaf disclosed relationships with Alnylam, Recordati, and Disc Medicine. She is a member of the Porphyrias Consortium, part of the Rare Diseases Clinical Research Network, funded by the National Institutes of Health and led by the National Center for Advancing Translational Sciences (NCATS). The consortium is funded by NCATS and the National Institute of Diabetes and Digestive and Kidney Diseases. Girelli had no disclosures.
A version of this article first appeared on Medscape.com.
Heavy Menstrual Bleeding: How Hematologists Can Help
Heavy menstrual bleeding is more than an inconvenience in adolescents: It often leads to significant medical complications, in addition to disruptions in quality of life. While measuring the true level of bleeding can be a challenge, hematologists say treatments are helpful and can be as simple — and surprising — as doses of aspirin.
About 90% of adolescents with heavy menstrual bleeding will have low ferritin, and 70% will develop anemia, said benign hematologist Juliana Perez Botero, MD, of the Mayo Clinic in Rochester, Minnesota, in a presentation at the American Society of Hematology (ASH) 2024 Annual Meeting. “This is an issue of big magnitude that has public health implications, but it’s also an issue of gender equality and social justice.”
Measuring Menstruation: What Counts as Heavy Bleeding?
According to hematologist Allison Wheeler, MD, of the University of Washington in Seattle, normal menstrual bleeding is defined as lasting for about 5 days with 30-50 mL of blood loss.
“Historically, heavy menstrual bleeding was defined as bleeding as > 7 days or > 80 mL of blood loss,” Wheeler said. “It’s pretty hard to measure those mL. So a more modern definition is increased menstrual blood loss that interferes with a female’s physical, social, emotional, or material quality of life.”
Measuring blood loss during menstruation isn’t simple. The alkaline hematin method, which measures blood in feminine hygiene products, is the “gold standard, but that’s all I’m going to say about that,” Wheeler said.
An alternative is the Pictorial Blood Loss Assessment Chart, a visual tool that patients can use to estimate blood loss, she said, although there have been questions about its accuracy. In addition, it only covers pads and tampons even though other products are now available.
Another option is the Adolescent Menstrual Bleeding Questionnaire. “It captures both how much patients are bleeding and a lot of quality-of-life aspects,” she said.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), Surprisingly, Can Be Effective Treatments
It seems counterintuitive that NSAIDs can be helpful in patients with heavy bleeding. “We don’t think about them because Cox inhibition ends up leading to decreases in thromboxane A2, which is going to increase bleeding,” Wheeler said. However, she said, the drugs also decrease prostaglandin within the endometrium, which can improve menstrual bleeding.
“In a meta-analysis, when NSAIDs were compared to placebo, there was decreased menstrual bleeding,” she said. “It was pretty similar to estrogen-progesterone formulations together. And when compared to antifibrinolytics, there was a little more menstrual bleeding with the NSAID use.”
Wheeler cautioned that “it’s important to optimize NSAID dosage. You really can’t use lower doses, and you can’t use sporadic doses.”
Other Options: Tranexamic Acid, Hormone Management
Tranexamic acid is the most common antifibrinolytic treatment for heavy bleeding, Wheeler said. “This is a lysine analog that’s going to inhibit the conversion from plasminogen to plasmin,” she said. “This is going to strengthen and stabilize blood clots that are already formed.”
Multiple clinical trials have studied the treatment in heavy menstrual bleeding, she said. “There’s no increased risk of venous or arterial thrombosis among participants in these clinical trials, but patients with a history of thrombosis were excluded from the majority of them. So we do need to keep that in mind.”
As for adverse effects, they’re mild and sporadic and include headaches and stomach upset, she said.
Another treatment option is estrogen and progesterone therapy using pill, patch, or vaginal ring, Wheeler said. The treatment leads to a “stable and thin very endometrium,” and typically takes 3-6 months to fully kick in. Studies have suggested the therapy can lead to 35%-80% reduction in menstrual blood loss, she said.
Keep in mind, Wheeler noted, “that there are many contraindications associated with estrogen use. Please take note of this, especially in consideration of discussions with patients shifting over to progesterone-only hormonal therapy” — another option to treat excess bleeding.
In most patients, she added, progesterone-only therapy “is going to result in irregular bleeding when you first start taking it. That irregular bleeding can last from up to 3-6 months. It’s something that’s really important to discuss with patients.”
She also noted that this therapy can be given to patients in forms that do not prevent pregnancy.
Botero had no disclosures. Wheeler reported relationships with Novo Nordisk, Bayer, BioMarin, Bioverativ, CSL Behring, Genentech, HEMA, Octapharma, Pfizer, Sanofi-Aventis, Shire North America, Spark, and Takeda.
A version of this article first appeared on Medscape.com.
Heavy menstrual bleeding is more than an inconvenience in adolescents: It often leads to significant medical complications, in addition to disruptions in quality of life. While measuring the true level of bleeding can be a challenge, hematologists say treatments are helpful and can be as simple — and surprising — as doses of aspirin.
About 90% of adolescents with heavy menstrual bleeding will have low ferritin, and 70% will develop anemia, said benign hematologist Juliana Perez Botero, MD, of the Mayo Clinic in Rochester, Minnesota, in a presentation at the American Society of Hematology (ASH) 2024 Annual Meeting. “This is an issue of big magnitude that has public health implications, but it’s also an issue of gender equality and social justice.”
Measuring Menstruation: What Counts as Heavy Bleeding?
According to hematologist Allison Wheeler, MD, of the University of Washington in Seattle, normal menstrual bleeding is defined as lasting for about 5 days with 30-50 mL of blood loss.
“Historically, heavy menstrual bleeding was defined as bleeding as > 7 days or > 80 mL of blood loss,” Wheeler said. “It’s pretty hard to measure those mL. So a more modern definition is increased menstrual blood loss that interferes with a female’s physical, social, emotional, or material quality of life.”
Measuring blood loss during menstruation isn’t simple. The alkaline hematin method, which measures blood in feminine hygiene products, is the “gold standard, but that’s all I’m going to say about that,” Wheeler said.
An alternative is the Pictorial Blood Loss Assessment Chart, a visual tool that patients can use to estimate blood loss, she said, although there have been questions about its accuracy. In addition, it only covers pads and tampons even though other products are now available.
Another option is the Adolescent Menstrual Bleeding Questionnaire. “It captures both how much patients are bleeding and a lot of quality-of-life aspects,” she said.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), Surprisingly, Can Be Effective Treatments
It seems counterintuitive that NSAIDs can be helpful in patients with heavy bleeding. “We don’t think about them because Cox inhibition ends up leading to decreases in thromboxane A2, which is going to increase bleeding,” Wheeler said. However, she said, the drugs also decrease prostaglandin within the endometrium, which can improve menstrual bleeding.
“In a meta-analysis, when NSAIDs were compared to placebo, there was decreased menstrual bleeding,” she said. “It was pretty similar to estrogen-progesterone formulations together. And when compared to antifibrinolytics, there was a little more menstrual bleeding with the NSAID use.”
Wheeler cautioned that “it’s important to optimize NSAID dosage. You really can’t use lower doses, and you can’t use sporadic doses.”
Other Options: Tranexamic Acid, Hormone Management
Tranexamic acid is the most common antifibrinolytic treatment for heavy bleeding, Wheeler said. “This is a lysine analog that’s going to inhibit the conversion from plasminogen to plasmin,” she said. “This is going to strengthen and stabilize blood clots that are already formed.”
Multiple clinical trials have studied the treatment in heavy menstrual bleeding, she said. “There’s no increased risk of venous or arterial thrombosis among participants in these clinical trials, but patients with a history of thrombosis were excluded from the majority of them. So we do need to keep that in mind.”
As for adverse effects, they’re mild and sporadic and include headaches and stomach upset, she said.
Another treatment option is estrogen and progesterone therapy using pill, patch, or vaginal ring, Wheeler said. The treatment leads to a “stable and thin very endometrium,” and typically takes 3-6 months to fully kick in. Studies have suggested the therapy can lead to 35%-80% reduction in menstrual blood loss, she said.
Keep in mind, Wheeler noted, “that there are many contraindications associated with estrogen use. Please take note of this, especially in consideration of discussions with patients shifting over to progesterone-only hormonal therapy” — another option to treat excess bleeding.
In most patients, she added, progesterone-only therapy “is going to result in irregular bleeding when you first start taking it. That irregular bleeding can last from up to 3-6 months. It’s something that’s really important to discuss with patients.”
She also noted that this therapy can be given to patients in forms that do not prevent pregnancy.
Botero had no disclosures. Wheeler reported relationships with Novo Nordisk, Bayer, BioMarin, Bioverativ, CSL Behring, Genentech, HEMA, Octapharma, Pfizer, Sanofi-Aventis, Shire North America, Spark, and Takeda.
A version of this article first appeared on Medscape.com.
Heavy menstrual bleeding is more than an inconvenience in adolescents: It often leads to significant medical complications, in addition to disruptions in quality of life. While measuring the true level of bleeding can be a challenge, hematologists say treatments are helpful and can be as simple — and surprising — as doses of aspirin.
About 90% of adolescents with heavy menstrual bleeding will have low ferritin, and 70% will develop anemia, said benign hematologist Juliana Perez Botero, MD, of the Mayo Clinic in Rochester, Minnesota, in a presentation at the American Society of Hematology (ASH) 2024 Annual Meeting. “This is an issue of big magnitude that has public health implications, but it’s also an issue of gender equality and social justice.”
Measuring Menstruation: What Counts as Heavy Bleeding?
According to hematologist Allison Wheeler, MD, of the University of Washington in Seattle, normal menstrual bleeding is defined as lasting for about 5 days with 30-50 mL of blood loss.
“Historically, heavy menstrual bleeding was defined as bleeding as > 7 days or > 80 mL of blood loss,” Wheeler said. “It’s pretty hard to measure those mL. So a more modern definition is increased menstrual blood loss that interferes with a female’s physical, social, emotional, or material quality of life.”
Measuring blood loss during menstruation isn’t simple. The alkaline hematin method, which measures blood in feminine hygiene products, is the “gold standard, but that’s all I’m going to say about that,” Wheeler said.
An alternative is the Pictorial Blood Loss Assessment Chart, a visual tool that patients can use to estimate blood loss, she said, although there have been questions about its accuracy. In addition, it only covers pads and tampons even though other products are now available.
Another option is the Adolescent Menstrual Bleeding Questionnaire. “It captures both how much patients are bleeding and a lot of quality-of-life aspects,” she said.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), Surprisingly, Can Be Effective Treatments
It seems counterintuitive that NSAIDs can be helpful in patients with heavy bleeding. “We don’t think about them because Cox inhibition ends up leading to decreases in thromboxane A2, which is going to increase bleeding,” Wheeler said. However, she said, the drugs also decrease prostaglandin within the endometrium, which can improve menstrual bleeding.
“In a meta-analysis, when NSAIDs were compared to placebo, there was decreased menstrual bleeding,” she said. “It was pretty similar to estrogen-progesterone formulations together. And when compared to antifibrinolytics, there was a little more menstrual bleeding with the NSAID use.”
Wheeler cautioned that “it’s important to optimize NSAID dosage. You really can’t use lower doses, and you can’t use sporadic doses.”
Other Options: Tranexamic Acid, Hormone Management
Tranexamic acid is the most common antifibrinolytic treatment for heavy bleeding, Wheeler said. “This is a lysine analog that’s going to inhibit the conversion from plasminogen to plasmin,” she said. “This is going to strengthen and stabilize blood clots that are already formed.”
Multiple clinical trials have studied the treatment in heavy menstrual bleeding, she said. “There’s no increased risk of venous or arterial thrombosis among participants in these clinical trials, but patients with a history of thrombosis were excluded from the majority of them. So we do need to keep that in mind.”
As for adverse effects, they’re mild and sporadic and include headaches and stomach upset, she said.
Another treatment option is estrogen and progesterone therapy using pill, patch, or vaginal ring, Wheeler said. The treatment leads to a “stable and thin very endometrium,” and typically takes 3-6 months to fully kick in. Studies have suggested the therapy can lead to 35%-80% reduction in menstrual blood loss, she said.
Keep in mind, Wheeler noted, “that there are many contraindications associated with estrogen use. Please take note of this, especially in consideration of discussions with patients shifting over to progesterone-only hormonal therapy” — another option to treat excess bleeding.
In most patients, she added, progesterone-only therapy “is going to result in irregular bleeding when you first start taking it. That irregular bleeding can last from up to 3-6 months. It’s something that’s really important to discuss with patients.”
She also noted that this therapy can be given to patients in forms that do not prevent pregnancy.
Botero had no disclosures. Wheeler reported relationships with Novo Nordisk, Bayer, BioMarin, Bioverativ, CSL Behring, Genentech, HEMA, Octapharma, Pfizer, Sanofi-Aventis, Shire North America, Spark, and Takeda.
A version of this article first appeared on Medscape.com.
Hemophilia A: Bleeds Plummet After Experimental Gene Therapy
SAN DIEGO — Promising early results from an ongoing randomized, open-label, single-arm, phase 3 study could pave the way for a Pfizer product to become the second US Food and Drug Administration (FDA)–approved gene therapy for hemophilia A.
In an efficacy population of 50 patients with hemophilia A, the AFFINE trial found that their mean annualized bleeding rate (ABR) fell from 4.73 pre-infusion with giroctocogene fitelparvovec to 1.24 post-infusion (week 12 to 15 or more months, −3.49, −6.06 to −0.91; P = .004), researchers reported earlier this month at American Society of Hematology (ASH) 2024 Annual Meeting. Sixty-four percent had no bleeding events over a median follow-up of 33.6 months (14.5-44.4).
The ABR for treated bleeds fell from 4.08 to 0.07 (−4.01, −5.57 to −2.45; P < .0001), and 88% had no treated bleeds over the same follow-up period.
“The primary endpoint for this trial was a reduction in total bleeds in patients, and that was achieved,” hematologist and first author Andrew D. Leavitt, MD, of the University of California at San Francisco, said in an interview. “More impressive was the reduction in treated bleeds, a kind of a surrogate marker for bleeds of clinical significance to the individual. And as one would expect or hope to see in a gene therapy trial, there was a significant and marked reduction in the use of factor.”
Moving forward, he said, the message to clinicians is that “there’s every reason to believe that they will have yet another option for their patients.”
Gene Therapy on the Rise in Hemophilia
Gene therapy has arisen as an approved therapy for hemophilia over just the last few years. Two gene therapies for hemophilia B have been approved by the FDA since 2022, and one was approved for hemophilia A, the more common type, in 2023.
As Leavitt noted, one-time treatment with gene therapy offers an alternative to treatment with blood factor, long the mainstay of hemophilia therapy.
“One of the real pluses of gene therapy is the potential to remove the burden of hemophilia, which is large and, I suspect, underappreciated even by providers,” he said. “You have to sit down with your patients and really get a real good sense of just how difficult it is for them to manage with many products on the market over the last few decades.”
Why is there a need for multiple gene therapy products? “A patient may have neutralizing antibodies against the proteins on the surface of gene therapy product A that prevents its use, but not on gene therapy B, which allows use of product B,” Leavitt said. “We need a few flavors so that we can offer gene therapy to the maximum number of interested patients.”
High Efficacy and an ‘Acceptable’ Safety Profile
For the study, researchers dosed 75 patients (mean age, 32.3 [19-59]; 100% men, 74.7% White and 18.7% Asian,) with hemophilia A with giroctocogene fitelparvovec, a hepatocyte-directed recombinant adeno-associated virus serotype 6 vector encoding a B-domain–deleted variant of human factor VIII. The efficacy population is 50 patients with at least 6 months of follow-up in the lead-in study.
The annualized infusion rate of exogenous FVIII was 124.39 mean annualized infusion rate prior to the treatment infusion vs 0.21 post-infusion, week 12 through at least 15 months (−124.18, −139.47 to −108.89; P < .0001).
Leavitt said the results are similar to other gene therapies for hemophilia in that “it is difficult to predict how high your factor level will become. There’s a broad range of outcomes for individuals, and the duration of expression remains an unknown.”
The study authors described the treatment as “generally well tolerated” with “an acceptable and manageable safety profile.”
Of the 75 subjects, 98.7% had adverse effects (AEs, 740 events) and 90.7% had treatment-related AEs. Common treatment-related AEs included hepatotoxicity (62.7%) and infusion-related reactions (73.3%). No subjects discontinued therapy due to AEs.
Nearly two thirds — 62.7% — of subjects used corticosteroids for a mean 114.6 days (11-296).
Study Findings ‘Look Really Good’
In an interview, Guy Young, MD, director of the Hemostasis and Thrombosis Program at Children’s Hospital Los Angeles and professor of pediatrics, Keck School of Medicine of University of Southern California, Los Angeles, said that “generally speaking, the new data looks really good.” Young, who didn’t take part in the study, noted that factor levels following treatment were high, and one subject actually had a thrombotic event and needed to be treated with an anticoagulant.
The high factor levels could actually be a sign of lasting benefit vs valoctocogene roxaparvovec (Roctavian), the sole FDA-approved gene therapy for hemophilia A, which is linked to significant drops in factor level after 6 months, he said. “Wouldn’t it be better to start really high?”
Gene therapy for hemophilia is highly expensive, although proponents noted that insurers may save money over the long run if patients don’t require prophylactic treatment or therapy for bleeds.
A Pfizer spokesman declined to comment on the new therapy’s potential cost. In regard to when the therapy may receive FDA approval, he said “Pfizer is discussing this data with regulatory authorities.”
Pfizer funded this study. Leavitt disclosed ties with HEMA, Merck, Catalyst, Genentech, Pfizer, BioMarin, and Sangamo. Other study authors reported relationships with Pfizer. Young disclosed ties with Pfizer and BioMarin.
A version of this article appeared on Medscape.com.
SAN DIEGO — Promising early results from an ongoing randomized, open-label, single-arm, phase 3 study could pave the way for a Pfizer product to become the second US Food and Drug Administration (FDA)–approved gene therapy for hemophilia A.
In an efficacy population of 50 patients with hemophilia A, the AFFINE trial found that their mean annualized bleeding rate (ABR) fell from 4.73 pre-infusion with giroctocogene fitelparvovec to 1.24 post-infusion (week 12 to 15 or more months, −3.49, −6.06 to −0.91; P = .004), researchers reported earlier this month at American Society of Hematology (ASH) 2024 Annual Meeting. Sixty-four percent had no bleeding events over a median follow-up of 33.6 months (14.5-44.4).
The ABR for treated bleeds fell from 4.08 to 0.07 (−4.01, −5.57 to −2.45; P < .0001), and 88% had no treated bleeds over the same follow-up period.
“The primary endpoint for this trial was a reduction in total bleeds in patients, and that was achieved,” hematologist and first author Andrew D. Leavitt, MD, of the University of California at San Francisco, said in an interview. “More impressive was the reduction in treated bleeds, a kind of a surrogate marker for bleeds of clinical significance to the individual. And as one would expect or hope to see in a gene therapy trial, there was a significant and marked reduction in the use of factor.”
Moving forward, he said, the message to clinicians is that “there’s every reason to believe that they will have yet another option for their patients.”
Gene Therapy on the Rise in Hemophilia
Gene therapy has arisen as an approved therapy for hemophilia over just the last few years. Two gene therapies for hemophilia B have been approved by the FDA since 2022, and one was approved for hemophilia A, the more common type, in 2023.
As Leavitt noted, one-time treatment with gene therapy offers an alternative to treatment with blood factor, long the mainstay of hemophilia therapy.
“One of the real pluses of gene therapy is the potential to remove the burden of hemophilia, which is large and, I suspect, underappreciated even by providers,” he said. “You have to sit down with your patients and really get a real good sense of just how difficult it is for them to manage with many products on the market over the last few decades.”
Why is there a need for multiple gene therapy products? “A patient may have neutralizing antibodies against the proteins on the surface of gene therapy product A that prevents its use, but not on gene therapy B, which allows use of product B,” Leavitt said. “We need a few flavors so that we can offer gene therapy to the maximum number of interested patients.”
High Efficacy and an ‘Acceptable’ Safety Profile
For the study, researchers dosed 75 patients (mean age, 32.3 [19-59]; 100% men, 74.7% White and 18.7% Asian,) with hemophilia A with giroctocogene fitelparvovec, a hepatocyte-directed recombinant adeno-associated virus serotype 6 vector encoding a B-domain–deleted variant of human factor VIII. The efficacy population is 50 patients with at least 6 months of follow-up in the lead-in study.
The annualized infusion rate of exogenous FVIII was 124.39 mean annualized infusion rate prior to the treatment infusion vs 0.21 post-infusion, week 12 through at least 15 months (−124.18, −139.47 to −108.89; P < .0001).
Leavitt said the results are similar to other gene therapies for hemophilia in that “it is difficult to predict how high your factor level will become. There’s a broad range of outcomes for individuals, and the duration of expression remains an unknown.”
The study authors described the treatment as “generally well tolerated” with “an acceptable and manageable safety profile.”
Of the 75 subjects, 98.7% had adverse effects (AEs, 740 events) and 90.7% had treatment-related AEs. Common treatment-related AEs included hepatotoxicity (62.7%) and infusion-related reactions (73.3%). No subjects discontinued therapy due to AEs.
Nearly two thirds — 62.7% — of subjects used corticosteroids for a mean 114.6 days (11-296).
Study Findings ‘Look Really Good’
In an interview, Guy Young, MD, director of the Hemostasis and Thrombosis Program at Children’s Hospital Los Angeles and professor of pediatrics, Keck School of Medicine of University of Southern California, Los Angeles, said that “generally speaking, the new data looks really good.” Young, who didn’t take part in the study, noted that factor levels following treatment were high, and one subject actually had a thrombotic event and needed to be treated with an anticoagulant.
The high factor levels could actually be a sign of lasting benefit vs valoctocogene roxaparvovec (Roctavian), the sole FDA-approved gene therapy for hemophilia A, which is linked to significant drops in factor level after 6 months, he said. “Wouldn’t it be better to start really high?”
Gene therapy for hemophilia is highly expensive, although proponents noted that insurers may save money over the long run if patients don’t require prophylactic treatment or therapy for bleeds.
A Pfizer spokesman declined to comment on the new therapy’s potential cost. In regard to when the therapy may receive FDA approval, he said “Pfizer is discussing this data with regulatory authorities.”
Pfizer funded this study. Leavitt disclosed ties with HEMA, Merck, Catalyst, Genentech, Pfizer, BioMarin, and Sangamo. Other study authors reported relationships with Pfizer. Young disclosed ties with Pfizer and BioMarin.
A version of this article appeared on Medscape.com.
SAN DIEGO — Promising early results from an ongoing randomized, open-label, single-arm, phase 3 study could pave the way for a Pfizer product to become the second US Food and Drug Administration (FDA)–approved gene therapy for hemophilia A.
In an efficacy population of 50 patients with hemophilia A, the AFFINE trial found that their mean annualized bleeding rate (ABR) fell from 4.73 pre-infusion with giroctocogene fitelparvovec to 1.24 post-infusion (week 12 to 15 or more months, −3.49, −6.06 to −0.91; P = .004), researchers reported earlier this month at American Society of Hematology (ASH) 2024 Annual Meeting. Sixty-four percent had no bleeding events over a median follow-up of 33.6 months (14.5-44.4).
The ABR for treated bleeds fell from 4.08 to 0.07 (−4.01, −5.57 to −2.45; P < .0001), and 88% had no treated bleeds over the same follow-up period.
“The primary endpoint for this trial was a reduction in total bleeds in patients, and that was achieved,” hematologist and first author Andrew D. Leavitt, MD, of the University of California at San Francisco, said in an interview. “More impressive was the reduction in treated bleeds, a kind of a surrogate marker for bleeds of clinical significance to the individual. And as one would expect or hope to see in a gene therapy trial, there was a significant and marked reduction in the use of factor.”
Moving forward, he said, the message to clinicians is that “there’s every reason to believe that they will have yet another option for their patients.”
Gene Therapy on the Rise in Hemophilia
Gene therapy has arisen as an approved therapy for hemophilia over just the last few years. Two gene therapies for hemophilia B have been approved by the FDA since 2022, and one was approved for hemophilia A, the more common type, in 2023.
As Leavitt noted, one-time treatment with gene therapy offers an alternative to treatment with blood factor, long the mainstay of hemophilia therapy.
“One of the real pluses of gene therapy is the potential to remove the burden of hemophilia, which is large and, I suspect, underappreciated even by providers,” he said. “You have to sit down with your patients and really get a real good sense of just how difficult it is for them to manage with many products on the market over the last few decades.”
Why is there a need for multiple gene therapy products? “A patient may have neutralizing antibodies against the proteins on the surface of gene therapy product A that prevents its use, but not on gene therapy B, which allows use of product B,” Leavitt said. “We need a few flavors so that we can offer gene therapy to the maximum number of interested patients.”
High Efficacy and an ‘Acceptable’ Safety Profile
For the study, researchers dosed 75 patients (mean age, 32.3 [19-59]; 100% men, 74.7% White and 18.7% Asian,) with hemophilia A with giroctocogene fitelparvovec, a hepatocyte-directed recombinant adeno-associated virus serotype 6 vector encoding a B-domain–deleted variant of human factor VIII. The efficacy population is 50 patients with at least 6 months of follow-up in the lead-in study.
The annualized infusion rate of exogenous FVIII was 124.39 mean annualized infusion rate prior to the treatment infusion vs 0.21 post-infusion, week 12 through at least 15 months (−124.18, −139.47 to −108.89; P < .0001).
Leavitt said the results are similar to other gene therapies for hemophilia in that “it is difficult to predict how high your factor level will become. There’s a broad range of outcomes for individuals, and the duration of expression remains an unknown.”
The study authors described the treatment as “generally well tolerated” with “an acceptable and manageable safety profile.”
Of the 75 subjects, 98.7% had adverse effects (AEs, 740 events) and 90.7% had treatment-related AEs. Common treatment-related AEs included hepatotoxicity (62.7%) and infusion-related reactions (73.3%). No subjects discontinued therapy due to AEs.
Nearly two thirds — 62.7% — of subjects used corticosteroids for a mean 114.6 days (11-296).
Study Findings ‘Look Really Good’
In an interview, Guy Young, MD, director of the Hemostasis and Thrombosis Program at Children’s Hospital Los Angeles and professor of pediatrics, Keck School of Medicine of University of Southern California, Los Angeles, said that “generally speaking, the new data looks really good.” Young, who didn’t take part in the study, noted that factor levels following treatment were high, and one subject actually had a thrombotic event and needed to be treated with an anticoagulant.
The high factor levels could actually be a sign of lasting benefit vs valoctocogene roxaparvovec (Roctavian), the sole FDA-approved gene therapy for hemophilia A, which is linked to significant drops in factor level after 6 months, he said. “Wouldn’t it be better to start really high?”
Gene therapy for hemophilia is highly expensive, although proponents noted that insurers may save money over the long run if patients don’t require prophylactic treatment or therapy for bleeds.
A Pfizer spokesman declined to comment on the new therapy’s potential cost. In regard to when the therapy may receive FDA approval, he said “Pfizer is discussing this data with regulatory authorities.”
Pfizer funded this study. Leavitt disclosed ties with HEMA, Merck, Catalyst, Genentech, Pfizer, BioMarin, and Sangamo. Other study authors reported relationships with Pfizer. Young disclosed ties with Pfizer and BioMarin.
A version of this article appeared on Medscape.com.
FROM ASH 2024
Physician Union Drives Skyrocketed in 2023 and 2024, Data Show
While fewer than 10% of US physicians are unionized, the number of official union drives among private-sector doctors have skyrocketed in the last 2 years, compared with 2 decades prior, according to a new study.
Researchers counted 21 union drives in 2023 and 12 in the first 5 months of 2024, compared with 0-6 drives each year between 2000 and 2022.
If the 2023 and 2024 drives succeed, unions will represent 3523 new physicians — nearly equal to the 3541 doctors who sought unionization between 2000 and 2022.
“We were able to document a significant uptick in union petitions and success in certification drives,” said corresponding author Hayden Rooke-Ley, JD, of the Center for Advancing Health Policy Through Research, Brown University School of Public Health, Providence, Rhode Island. “We were surprised to see such a marked shift in 2023.”
About 72,000 physicians, an estimated 8% of all US doctors, are covered by unions, including some in the public sector. Physicians who are self-employed, now comprising less than a fifth of all doctors, are not eligible to join labor unions.
The study authors launched their research to better understand trends in physician unionization in light of high-profile union drives, especially among residents. Rooke-Ley said: “We suspected that declining morale and increased corporate employment for physicians were leading them to consider unionization.”
The researchers gathered data from the National Labor Relations Board about union drives by potential bargaining units that included physicians. From 2000 to 2022, 44 union petitions were filed. The number jumped to 33 from 2023-2024.
“Tip of the Iceberg”
“This is the tip of the iceberg,” said ethicist Joseph F. Kras, MD, DDS, MA, an associate professor of anesthesiology at Washington University in St. Louis, Missouri, and corresponding author of a recent Anesthesia & Analgesia report about physician unionization.
“We are independent by nature,” Kras said. “But when you put us in an employed environment and start treating us as widgets, then we will act like employees of Amazon, Starbucks, and other companies and join together to push back against the increasing emphasis on profit over all at the expense of our independent judgment on what’s best for the patient.”
Of the 66 unionization efforts between 2000 and 2024 that were decided, 62% were certified, according to the JAMA study. The drives targeted hospitals (49%), community health centers (38%), and nonhospital corporate owners (13%).
The researchers only analyzed private-sector unionization and did not include physicians who are unionized at public institutions.
What’s Behind Union Drives?
Alyssa Burgart, MD, MA, an ethicist and clinical associate professor of anesthesiology and pediatrics at Stanford University in California, told this news organization that physician unionization “is a big topic with a lot of really strong opinions.”
Many doctors wrongly assume they can’t unionize because they’re physicians, said Burgart, a coauthor of the Anesthesia & Analgesia report.
Supporters of unionization believe it’s a strategy to be “recognized not as simply as a single physician with a concern,” she said. “When you’re among clinicians who can speak as a more unified group, organizations are more likely to take that seriously.”
A union may also be able to hold employers to account in areas such as the gender wage gap, sexual harassment, and bias in hiring and firing, Burgart said. And union supporters believe they’ll make more money if they collectively bargain.
Other factors driving interest in unions include “increasing physician burnout, increasing physician exhaustion, and immense frustration with the ways that private equity is influencing how physicians need to work in order to practice,” she said.
Earlier in 2024, physicians in Delaware’s ChristianaCare health system voted 288-130 to be represented by Doctors Council/Service Employees International, according to the union.
“We have still not been able to staff up enough to where us physicians can get back to just focusing on taking care of patients,” a unionization leader told WHYY.
The JAMA study examined news reports regarding most of the 2023-2024 union drives and found that supporters claimed they were motivated by working conditions (85%), lack of voice in management (81%), patient care concerns (54%), and pay (4%).
Critics Worry They’ll Lose Pay Because of Unions
Skeptics of unionization worry about whether “I’m going to be required to stand by some union stance that is actually out of alignment with my values as a physician,” Burgart said. And, she said, critics such as highly paid surgeons fear that adjustments to salaries because of union contracts could cause them to lose income.
In regard to compensation, a 2024 study surveyed unionized residents — along with faculty and staff — at general surgery programs and found evidence that unionization didn’t improve resident well-being or benefits, although it “provided a mechanism for resident voice and agency.”
“It is critical to study the outcomes of those who unionized to ensure that the reasons for unionizing were realized over time,” said that study’s coauthor Karl Bilimoria, MD, MS, chair of surgery at Indiana University School of Medicine, Indianapolis. “The unintended consequences of unionization must be examined along with the potential improvements.”
Rooke-Ley discloses consulting fees from the American Economic Liberties Project, National Academy of State Health Policy, and 32BJ Funds. Kras and Burgart disclose previous union membership. Bilimoria has no disclosures.
A version of this article first appeared on Medscape.com.
While fewer than 10% of US physicians are unionized, the number of official union drives among private-sector doctors have skyrocketed in the last 2 years, compared with 2 decades prior, according to a new study.
Researchers counted 21 union drives in 2023 and 12 in the first 5 months of 2024, compared with 0-6 drives each year between 2000 and 2022.
If the 2023 and 2024 drives succeed, unions will represent 3523 new physicians — nearly equal to the 3541 doctors who sought unionization between 2000 and 2022.
“We were able to document a significant uptick in union petitions and success in certification drives,” said corresponding author Hayden Rooke-Ley, JD, of the Center for Advancing Health Policy Through Research, Brown University School of Public Health, Providence, Rhode Island. “We were surprised to see such a marked shift in 2023.”
About 72,000 physicians, an estimated 8% of all US doctors, are covered by unions, including some in the public sector. Physicians who are self-employed, now comprising less than a fifth of all doctors, are not eligible to join labor unions.
The study authors launched their research to better understand trends in physician unionization in light of high-profile union drives, especially among residents. Rooke-Ley said: “We suspected that declining morale and increased corporate employment for physicians were leading them to consider unionization.”
The researchers gathered data from the National Labor Relations Board about union drives by potential bargaining units that included physicians. From 2000 to 2022, 44 union petitions were filed. The number jumped to 33 from 2023-2024.
“Tip of the Iceberg”
“This is the tip of the iceberg,” said ethicist Joseph F. Kras, MD, DDS, MA, an associate professor of anesthesiology at Washington University in St. Louis, Missouri, and corresponding author of a recent Anesthesia & Analgesia report about physician unionization.
“We are independent by nature,” Kras said. “But when you put us in an employed environment and start treating us as widgets, then we will act like employees of Amazon, Starbucks, and other companies and join together to push back against the increasing emphasis on profit over all at the expense of our independent judgment on what’s best for the patient.”
Of the 66 unionization efforts between 2000 and 2024 that were decided, 62% were certified, according to the JAMA study. The drives targeted hospitals (49%), community health centers (38%), and nonhospital corporate owners (13%).
The researchers only analyzed private-sector unionization and did not include physicians who are unionized at public institutions.
What’s Behind Union Drives?
Alyssa Burgart, MD, MA, an ethicist and clinical associate professor of anesthesiology and pediatrics at Stanford University in California, told this news organization that physician unionization “is a big topic with a lot of really strong opinions.”
Many doctors wrongly assume they can’t unionize because they’re physicians, said Burgart, a coauthor of the Anesthesia & Analgesia report.
Supporters of unionization believe it’s a strategy to be “recognized not as simply as a single physician with a concern,” she said. “When you’re among clinicians who can speak as a more unified group, organizations are more likely to take that seriously.”
A union may also be able to hold employers to account in areas such as the gender wage gap, sexual harassment, and bias in hiring and firing, Burgart said. And union supporters believe they’ll make more money if they collectively bargain.
Other factors driving interest in unions include “increasing physician burnout, increasing physician exhaustion, and immense frustration with the ways that private equity is influencing how physicians need to work in order to practice,” she said.
Earlier in 2024, physicians in Delaware’s ChristianaCare health system voted 288-130 to be represented by Doctors Council/Service Employees International, according to the union.
“We have still not been able to staff up enough to where us physicians can get back to just focusing on taking care of patients,” a unionization leader told WHYY.
The JAMA study examined news reports regarding most of the 2023-2024 union drives and found that supporters claimed they were motivated by working conditions (85%), lack of voice in management (81%), patient care concerns (54%), and pay (4%).
Critics Worry They’ll Lose Pay Because of Unions
Skeptics of unionization worry about whether “I’m going to be required to stand by some union stance that is actually out of alignment with my values as a physician,” Burgart said. And, she said, critics such as highly paid surgeons fear that adjustments to salaries because of union contracts could cause them to lose income.
In regard to compensation, a 2024 study surveyed unionized residents — along with faculty and staff — at general surgery programs and found evidence that unionization didn’t improve resident well-being or benefits, although it “provided a mechanism for resident voice and agency.”
“It is critical to study the outcomes of those who unionized to ensure that the reasons for unionizing were realized over time,” said that study’s coauthor Karl Bilimoria, MD, MS, chair of surgery at Indiana University School of Medicine, Indianapolis. “The unintended consequences of unionization must be examined along with the potential improvements.”
Rooke-Ley discloses consulting fees from the American Economic Liberties Project, National Academy of State Health Policy, and 32BJ Funds. Kras and Burgart disclose previous union membership. Bilimoria has no disclosures.
A version of this article first appeared on Medscape.com.
While fewer than 10% of US physicians are unionized, the number of official union drives among private-sector doctors have skyrocketed in the last 2 years, compared with 2 decades prior, according to a new study.
Researchers counted 21 union drives in 2023 and 12 in the first 5 months of 2024, compared with 0-6 drives each year between 2000 and 2022.
If the 2023 and 2024 drives succeed, unions will represent 3523 new physicians — nearly equal to the 3541 doctors who sought unionization between 2000 and 2022.
“We were able to document a significant uptick in union petitions and success in certification drives,” said corresponding author Hayden Rooke-Ley, JD, of the Center for Advancing Health Policy Through Research, Brown University School of Public Health, Providence, Rhode Island. “We were surprised to see such a marked shift in 2023.”
About 72,000 physicians, an estimated 8% of all US doctors, are covered by unions, including some in the public sector. Physicians who are self-employed, now comprising less than a fifth of all doctors, are not eligible to join labor unions.
The study authors launched their research to better understand trends in physician unionization in light of high-profile union drives, especially among residents. Rooke-Ley said: “We suspected that declining morale and increased corporate employment for physicians were leading them to consider unionization.”
The researchers gathered data from the National Labor Relations Board about union drives by potential bargaining units that included physicians. From 2000 to 2022, 44 union petitions were filed. The number jumped to 33 from 2023-2024.
“Tip of the Iceberg”
“This is the tip of the iceberg,” said ethicist Joseph F. Kras, MD, DDS, MA, an associate professor of anesthesiology at Washington University in St. Louis, Missouri, and corresponding author of a recent Anesthesia & Analgesia report about physician unionization.
“We are independent by nature,” Kras said. “But when you put us in an employed environment and start treating us as widgets, then we will act like employees of Amazon, Starbucks, and other companies and join together to push back against the increasing emphasis on profit over all at the expense of our independent judgment on what’s best for the patient.”
Of the 66 unionization efforts between 2000 and 2024 that were decided, 62% were certified, according to the JAMA study. The drives targeted hospitals (49%), community health centers (38%), and nonhospital corporate owners (13%).
The researchers only analyzed private-sector unionization and did not include physicians who are unionized at public institutions.
What’s Behind Union Drives?
Alyssa Burgart, MD, MA, an ethicist and clinical associate professor of anesthesiology and pediatrics at Stanford University in California, told this news organization that physician unionization “is a big topic with a lot of really strong opinions.”
Many doctors wrongly assume they can’t unionize because they’re physicians, said Burgart, a coauthor of the Anesthesia & Analgesia report.
Supporters of unionization believe it’s a strategy to be “recognized not as simply as a single physician with a concern,” she said. “When you’re among clinicians who can speak as a more unified group, organizations are more likely to take that seriously.”
A union may also be able to hold employers to account in areas such as the gender wage gap, sexual harassment, and bias in hiring and firing, Burgart said. And union supporters believe they’ll make more money if they collectively bargain.
Other factors driving interest in unions include “increasing physician burnout, increasing physician exhaustion, and immense frustration with the ways that private equity is influencing how physicians need to work in order to practice,” she said.
Earlier in 2024, physicians in Delaware’s ChristianaCare health system voted 288-130 to be represented by Doctors Council/Service Employees International, according to the union.
“We have still not been able to staff up enough to where us physicians can get back to just focusing on taking care of patients,” a unionization leader told WHYY.
The JAMA study examined news reports regarding most of the 2023-2024 union drives and found that supporters claimed they were motivated by working conditions (85%), lack of voice in management (81%), patient care concerns (54%), and pay (4%).
Critics Worry They’ll Lose Pay Because of Unions
Skeptics of unionization worry about whether “I’m going to be required to stand by some union stance that is actually out of alignment with my values as a physician,” Burgart said. And, she said, critics such as highly paid surgeons fear that adjustments to salaries because of union contracts could cause them to lose income.
In regard to compensation, a 2024 study surveyed unionized residents — along with faculty and staff — at general surgery programs and found evidence that unionization didn’t improve resident well-being or benefits, although it “provided a mechanism for resident voice and agency.”
“It is critical to study the outcomes of those who unionized to ensure that the reasons for unionizing were realized over time,” said that study’s coauthor Karl Bilimoria, MD, MS, chair of surgery at Indiana University School of Medicine, Indianapolis. “The unintended consequences of unionization must be examined along with the potential improvements.”
Rooke-Ley discloses consulting fees from the American Economic Liberties Project, National Academy of State Health Policy, and 32BJ Funds. Kras and Burgart disclose previous union membership. Bilimoria has no disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA
Smoldering MM: Big Prevention Benefits With Daratumumab?
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Among 390 patients with SMM (194 assigned to daratumumab and 196 to active monitoring), progression to active MM or death over a follow-up of 65.2 (0-76.6) months was 51% lower in the daratumumab group vs active monitoring (34.5% vs 50.5%, hazard ratio [HR], 0.49; 95% CI, 0.36-0.67; P < .0001), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting and in a simultaneous publication in the New England Journal of Medicine.
Rahul Banerjee, MD, an assistant professor with the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, who wasn’t involved with the research, said the study “is a big deal, and I suspect this will ultimately lead to an FDA [Food and Drug Administration] approval for daratumumab in this setting. If using daratumumab up-front can prevent further myeloma and therefore make patients live longer, this would be immediately adopted at many practices.”
As study first author Meletios Athanasios Dimopoulos, MD, of National and Kapodistrian University of Athens and Alexandra General Hospital in Greece, noted at a news briefing, SMM is common, affecting 0.5% of the population aged over 40, per a 2023 Iceland study.
“Standard practice is close follow-up without immediate intervention. However, this oftentimes ends in organ tissue damage, and hypercalcemia, bone lesions, renal impairment, and anemia,” Dimopoulos said.
According to him, researchers launched the AQUILA study in light of indications that daratumumab may benefit patients with intermediate- and high-risk SMM.
For the study, researchers recruited patients from 2017 to 2019 in 23 countries with confirmed high-risk SMM for ≤ 5 years (median age, 64 [31-86] years; 47%-49% men; 83% White).
In the daratumumab group, the drug was administered in 28-day cycles until cycle 39, 36 months, or disease progression, whichever came first (median treatment duration, 38 months [35 months]).
At 5 years, progression-free survival (PFS) — the primary endpoint — was 63.1% (daratumumab) and 40.8% (active monitoring). Researchers estimated 60-month PFS rates at 63.1% and 40.8%, respectively, and overall response rates were 63.4% vs 2.0% (P < .0001), respectively.
The 60-month overall survival rates were 93.0% and 86.9% (HR, 0.52; 95% CI, 0.27-0.98) with 15 deaths in the daratumumab and 26 in the active monitoring group.
“During the follow-up period, there was continuous improvement in favor of the daratumumab arm,” Dimopoulos said. “Even after treatment was discontinued at 3 years, or even at 5 or 6 years, there was a continuous benefit from treatment with daratumumab.”
By clinical cutoff in May 2024, 65% of patients taking daratumumab had finished 39 cycles/3 years of treatment vs 40.8% in the active monitoring group. Progressive disease was the most common reason that patients stopped treatment (21.8% and 41.8% of patients in the groups, respectively).
Grade 3/4 treatment-emergent adverse events (TEAEs) occurred in 40.4% (daratumumab) and 30.1% (active monitoring) of patients. The most common was hypertension (5.7% and 4.6%, respectively).
In the daratumumab group, 5.7% discontinued therapy because of TEAEs, which the researchers described as a “low” number, and fatal TEAEs were similar in both groups (1.0% and 2.0%, respectively).
Banerjee said that “one theoretical risk of using daratumumab monotherapy to treat perceived high-risk SMM is that if the patient actually has active multiple myeloma, you are undertreating them. For anyone with HR-SMM, active multiple myeloma must be completely ruled out. I always insist on both a PET-CT and a whole-body MRI to evaluate the bone marrow comprehensively.”
For now, Banerjee said, clinicians should wait for the US Food and Drug Administration approval before prescribing daratumumab for high-risk SMM.
Are there alternatives to reduce the risk for SMM turning into MM? “Generally, I advise close observation in most cases, but we do have clinical trials in this space,” Banerjee said. “Technically, it is possible to consider lenalidomide monotherapy in SMM based on the results of a large phase 3 study. But lenalidomide is expensive and has many side effects. Insurance companies often won’t cover it fully, and patients almost always have at least one side effect.”
Also, he added, “only half of patients saw their high-risk SMM disease burden drop. Lenalidomide also has a clear link to rare, delayed toxicities such as second primary malignancies, which makes us nervous.”
Janssen Pharmaceuticals, the maker of daratumumab, funded the study. Dimopoulos disclosed ties with Sanofi, Regeneron, Menarini, Takeda, GSK, BMS, Janssen Pharmaceuticals, BeiGene, Swixx, AstraZeneca, and Amgen. Banerjee disclosed ties with AbbVie, Adaptive, BMS, Caribou, Genentech/Roche, GSK, Karyopharm Therapeutics, Legend, Johnson & Johnson, Novartis, Pack, Pfizer, Prothena, Sanofi Pasteur, and SparkCures. Some other authors reported various and multiple disclosures, including ties with Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM ASH 2024
Smoking Linked to More Genetic Havoc in MDS
The prospective National MDS Natural History Study evaluated 1898 patients with recently diagnosed or suspected MDS. An adjusted analysis linked higher number of pack-years to more mutations (P = .006), with those at the 90th percentile with 3.5 times the number of mutations as nonsmokers, researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
The findings “suggest that smoking potentially contributes to the multistep molecular genetic pathogenesis that ultimately results in diagnosis of the cancer,” said corresponding author Mikkael A. Sekeres, MD, of the Sylvester Comprehensive Cancer Center, University of Miami Health System in Florida, at a news briefing. “The more you smoke, the more likely you are to acquire more mutations and even develop a higher risk of myelodysplastic syndromes. [More smoking] was also associated with progression and survival.”
While numbers are uncertain, an estimated 10,000 or more people in the United States each year are diagnosed with MDS, also known as preleukemia, according to the American Cancer Society. Median survival ranges from 1 to 10.6 years based on risk group, although the cancer society says the statistics are dated and mainly from Europe.
Multiple studies have linked smoking to MDS. The new study aims to understand the possible effects of smoking on genetic mutations.
The research analyzed 1898 patients enrolled from 2016 to 2023 (52% who had ever smoked; 18% current smokers; mean smoking years, 29.8 ± 16.9 years). The patients had diagnoses of MDSs, MDS/myeloproliferative neoplasm overlap, or precursor conditions such as clonal cytopenia of undetermined significance (CCUS).
Smokers were more likely than nonsmokers to be men (68% vs 54%; P < .001) and aged 70-79 years (45% vs 34%; P < .001).
After adjustment for confounders, smokers had more average mutations linked to MDS than nonsmokers (2.0 vs 1.4; P = .04). Those at the 75th percentile of pack-years had 1.8 times as many MDS-linked mutations as nonsmokers.
The 5-year cumulative incidence of disease progression was higher in long-term smokers than in nonsmokers and those with shorter smoking history (mean proportion progressed, 20+ years vs < 20 years smoking/nonsmoking, 27% [19%-36%] vs 18% [13%-24%]; P < .05, respectively).
Also, overall survival was lower in smokers than in nonsmokers for patients with CCUS (hazard ratio [HR], 1.91; 95% CI, 1.03-3.55; P = .04) but not for those with MDS (HR, 1.21; 95% CI, 0.53-1.30; P = .41).
“The data suggests that a patient with a new diagnosis of MDS who also smokes should be counseled to stop smoking,” Sekeres said.
This may seem counterintuitive to patients, he acknowledged. When Sekeres was a medical student, he counseled a female patient with advanced lung cancer to quit smoking. “The patient looked at me like I had three heads and she said: ‘Why should I stop smoking? The cats are already out of the bag. I have lung cancer.’ ”
But the new study points to a possible benefit from quitting smoking while sick. “It appears that smoking contributes to the acquisition of new genetic mutations that can lead to worsening of the myelodysplastic syndromes and even evolution of the cancer into acute myeloid leukemia,” Sekeres said.
He added: “One thing to understand about these cancers of the bone marrow is they can take years or decades to develop. They’re not one-hit wonders. Smoking caused very specific genetic mutations. The cool part of this is that they’re the same genetic mutations smoking has been shown to cause in cancers like lung cancer, so we’re seeing consistency across cancers.”
Sekeres said he himself will counsel patients with MDS or acute myeloid leukemia to stop smoking. “If there’s anything we can do to intervene to prevent myelodysplastic syndrome from evolving into acute leukemia, my word, I sure I’m going to try it.”
In an interview, Peter Greenberg, MD, professor of medicine at Stanford Cancer Center in California, who’s familiar with the study but didn’t take part in the research, said the study suggests that smoking in MDS isn’t just related to exposure to fumes “but appears to be a much more widespread problem” related to its impact on generating hematologic stem cell mutations.
Most clinicians don’t warn patients with MDS about the dangers of smoking because they’re not aware of tobacco’s connection to the disease, Greenberg said. But there’s another reason to bring up smoking, he said: It boosts the risk for cardiovascular disease, which may be partially responsible for decreased survival in smokers.
Sekeres disclosed ties with Kurome, Schrödinger, and Bristol-Myers Squibb. Other authors reported multiple and various relationships with industry. Greenberg had no disclosures.
A version of this article appeared on Medscape.com.
The prospective National MDS Natural History Study evaluated 1898 patients with recently diagnosed or suspected MDS. An adjusted analysis linked higher number of pack-years to more mutations (P = .006), with those at the 90th percentile with 3.5 times the number of mutations as nonsmokers, researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
The findings “suggest that smoking potentially contributes to the multistep molecular genetic pathogenesis that ultimately results in diagnosis of the cancer,” said corresponding author Mikkael A. Sekeres, MD, of the Sylvester Comprehensive Cancer Center, University of Miami Health System in Florida, at a news briefing. “The more you smoke, the more likely you are to acquire more mutations and even develop a higher risk of myelodysplastic syndromes. [More smoking] was also associated with progression and survival.”
While numbers are uncertain, an estimated 10,000 or more people in the United States each year are diagnosed with MDS, also known as preleukemia, according to the American Cancer Society. Median survival ranges from 1 to 10.6 years based on risk group, although the cancer society says the statistics are dated and mainly from Europe.
Multiple studies have linked smoking to MDS. The new study aims to understand the possible effects of smoking on genetic mutations.
The research analyzed 1898 patients enrolled from 2016 to 2023 (52% who had ever smoked; 18% current smokers; mean smoking years, 29.8 ± 16.9 years). The patients had diagnoses of MDSs, MDS/myeloproliferative neoplasm overlap, or precursor conditions such as clonal cytopenia of undetermined significance (CCUS).
Smokers were more likely than nonsmokers to be men (68% vs 54%; P < .001) and aged 70-79 years (45% vs 34%; P < .001).
After adjustment for confounders, smokers had more average mutations linked to MDS than nonsmokers (2.0 vs 1.4; P = .04). Those at the 75th percentile of pack-years had 1.8 times as many MDS-linked mutations as nonsmokers.
The 5-year cumulative incidence of disease progression was higher in long-term smokers than in nonsmokers and those with shorter smoking history (mean proportion progressed, 20+ years vs < 20 years smoking/nonsmoking, 27% [19%-36%] vs 18% [13%-24%]; P < .05, respectively).
Also, overall survival was lower in smokers than in nonsmokers for patients with CCUS (hazard ratio [HR], 1.91; 95% CI, 1.03-3.55; P = .04) but not for those with MDS (HR, 1.21; 95% CI, 0.53-1.30; P = .41).
“The data suggests that a patient with a new diagnosis of MDS who also smokes should be counseled to stop smoking,” Sekeres said.
This may seem counterintuitive to patients, he acknowledged. When Sekeres was a medical student, he counseled a female patient with advanced lung cancer to quit smoking. “The patient looked at me like I had three heads and she said: ‘Why should I stop smoking? The cats are already out of the bag. I have lung cancer.’ ”
But the new study points to a possible benefit from quitting smoking while sick. “It appears that smoking contributes to the acquisition of new genetic mutations that can lead to worsening of the myelodysplastic syndromes and even evolution of the cancer into acute myeloid leukemia,” Sekeres said.
He added: “One thing to understand about these cancers of the bone marrow is they can take years or decades to develop. They’re not one-hit wonders. Smoking caused very specific genetic mutations. The cool part of this is that they’re the same genetic mutations smoking has been shown to cause in cancers like lung cancer, so we’re seeing consistency across cancers.”
Sekeres said he himself will counsel patients with MDS or acute myeloid leukemia to stop smoking. “If there’s anything we can do to intervene to prevent myelodysplastic syndrome from evolving into acute leukemia, my word, I sure I’m going to try it.”
In an interview, Peter Greenberg, MD, professor of medicine at Stanford Cancer Center in California, who’s familiar with the study but didn’t take part in the research, said the study suggests that smoking in MDS isn’t just related to exposure to fumes “but appears to be a much more widespread problem” related to its impact on generating hematologic stem cell mutations.
Most clinicians don’t warn patients with MDS about the dangers of smoking because they’re not aware of tobacco’s connection to the disease, Greenberg said. But there’s another reason to bring up smoking, he said: It boosts the risk for cardiovascular disease, which may be partially responsible for decreased survival in smokers.
Sekeres disclosed ties with Kurome, Schrödinger, and Bristol-Myers Squibb. Other authors reported multiple and various relationships with industry. Greenberg had no disclosures.
A version of this article appeared on Medscape.com.
The prospective National MDS Natural History Study evaluated 1898 patients with recently diagnosed or suspected MDS. An adjusted analysis linked higher number of pack-years to more mutations (P = .006), with those at the 90th percentile with 3.5 times the number of mutations as nonsmokers, researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
The findings “suggest that smoking potentially contributes to the multistep molecular genetic pathogenesis that ultimately results in diagnosis of the cancer,” said corresponding author Mikkael A. Sekeres, MD, of the Sylvester Comprehensive Cancer Center, University of Miami Health System in Florida, at a news briefing. “The more you smoke, the more likely you are to acquire more mutations and even develop a higher risk of myelodysplastic syndromes. [More smoking] was also associated with progression and survival.”
While numbers are uncertain, an estimated 10,000 or more people in the United States each year are diagnosed with MDS, also known as preleukemia, according to the American Cancer Society. Median survival ranges from 1 to 10.6 years based on risk group, although the cancer society says the statistics are dated and mainly from Europe.
Multiple studies have linked smoking to MDS. The new study aims to understand the possible effects of smoking on genetic mutations.
The research analyzed 1898 patients enrolled from 2016 to 2023 (52% who had ever smoked; 18% current smokers; mean smoking years, 29.8 ± 16.9 years). The patients had diagnoses of MDSs, MDS/myeloproliferative neoplasm overlap, or precursor conditions such as clonal cytopenia of undetermined significance (CCUS).
Smokers were more likely than nonsmokers to be men (68% vs 54%; P < .001) and aged 70-79 years (45% vs 34%; P < .001).
After adjustment for confounders, smokers had more average mutations linked to MDS than nonsmokers (2.0 vs 1.4; P = .04). Those at the 75th percentile of pack-years had 1.8 times as many MDS-linked mutations as nonsmokers.
The 5-year cumulative incidence of disease progression was higher in long-term smokers than in nonsmokers and those with shorter smoking history (mean proportion progressed, 20+ years vs < 20 years smoking/nonsmoking, 27% [19%-36%] vs 18% [13%-24%]; P < .05, respectively).
Also, overall survival was lower in smokers than in nonsmokers for patients with CCUS (hazard ratio [HR], 1.91; 95% CI, 1.03-3.55; P = .04) but not for those with MDS (HR, 1.21; 95% CI, 0.53-1.30; P = .41).
“The data suggests that a patient with a new diagnosis of MDS who also smokes should be counseled to stop smoking,” Sekeres said.
This may seem counterintuitive to patients, he acknowledged. When Sekeres was a medical student, he counseled a female patient with advanced lung cancer to quit smoking. “The patient looked at me like I had three heads and she said: ‘Why should I stop smoking? The cats are already out of the bag. I have lung cancer.’ ”
But the new study points to a possible benefit from quitting smoking while sick. “It appears that smoking contributes to the acquisition of new genetic mutations that can lead to worsening of the myelodysplastic syndromes and even evolution of the cancer into acute myeloid leukemia,” Sekeres said.
He added: “One thing to understand about these cancers of the bone marrow is they can take years or decades to develop. They’re not one-hit wonders. Smoking caused very specific genetic mutations. The cool part of this is that they’re the same genetic mutations smoking has been shown to cause in cancers like lung cancer, so we’re seeing consistency across cancers.”
Sekeres said he himself will counsel patients with MDS or acute myeloid leukemia to stop smoking. “If there’s anything we can do to intervene to prevent myelodysplastic syndrome from evolving into acute leukemia, my word, I sure I’m going to try it.”
In an interview, Peter Greenberg, MD, professor of medicine at Stanford Cancer Center in California, who’s familiar with the study but didn’t take part in the research, said the study suggests that smoking in MDS isn’t just related to exposure to fumes “but appears to be a much more widespread problem” related to its impact on generating hematologic stem cell mutations.
Most clinicians don’t warn patients with MDS about the dangers of smoking because they’re not aware of tobacco’s connection to the disease, Greenberg said. But there’s another reason to bring up smoking, he said: It boosts the risk for cardiovascular disease, which may be partially responsible for decreased survival in smokers.
Sekeres disclosed ties with Kurome, Schrödinger, and Bristol-Myers Squibb. Other authors reported multiple and various relationships with industry. Greenberg had no disclosures.
A version of this article appeared on Medscape.com.
FROM ASH 2024
Fertility Preservation in SCD: Women Have More Complications
Of 46 patients with SCD, complications occurred in 25 of 55 controlled ovarian hyperstimulation cycles, including 29 vaso-occlusive episodes (VOEs), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
Of 21 post-retrieval VOEs, 19 required emergency department care or hospitalization.
“Baseline sickle cell disease severity is most likely associated with a patient’s risk of complications from an egg retrieval cycle,” study co-author Sarah Cromack, MD, a reproductive endocrinology and infertility fellow at Northwestern University, Chicago, said in an interview.
“Both hematologists and reproductive endocrinologists can use this information to plan ahead and anticipate possible issues, check blood counts prior to and after egg retrieval to see if transfusion is needed, and plan close follow-up during stimulation and immediately after egg retrieval to evaluate and treat pain.”
SCD Accelerates Decline in Ovarian Reserve
Pediatric hematologist Lydia H. Pecker, MD, MS, of Johns Hopkins University School of Medicine, Baltimore, the study’s corresponding author, said in an interview that SCD is “a disease of accelerated aging” that leads to accelerated decline in ovarian reserve. “The common indication for fertility preservation in SCD is before bone marrow transplant or gene therapy,” she said, although FP can also be offered to other patients with SCD.
According to Cromack, researchers launched the study to expand information about SCD and FP in light of sparse data about outcomes.
All the 46 patients had hemoglobin SS (HbSS, 93%) and HbSβ0-thalassemia (7%) and a median age of 23.7 (18-28) years. Almost all (44 patients) underwent FP prior to curative treatments, and all had at least one SCD-related complication, mainly cerebrovascular disease (16), acute chest syndrome (23), and more than two VOEs per year (31).
Median anti-Mullerian hormone (AMH) level (2.1 ng/mL), a measurement of ovarian reserve, was lower than the expected level of 2.8-3.4 ng/mL among women in the age range of the patients, the researchers reported. “This is consistent with previous studies showing lower AMH for age in women with sickle cell disease,” Pecker said.
Complications in 45% of Retrieval Cycles
“In terms of success of oocyte cryopreservation, the median number of mature eggs frozen was 11,” said co-author and reproductive endocrinologist Jessica Walter, MD, of Northwestern University, in an interview. “Given the average age of 24 years in the cohort, this would give each patient about a 70% estimated probability of at least one live birth from their cohort of frozen eggs. Thus, patients hoping for more than one child may want to consider more than one cycle of egg freezing.”
The rate of complications was “fairly high” at 45% of all cycles, Walter said. “These were mostly complications from underlying sickle cell disease, including unplanned transfusions and admissions for vaso-occlusive crises. Surprisingly, there were very few cases of ovarian hyperstimulation syndrome in this young patient group, which may be due to a combination of underlying vascular disease, lower peak estradiol levels, and slightly less eggs retrieved then would be expected compared to an age-matched healthy controls.”
Any FP complication was associated with more than three VOEs in the year before controlled ovarian hyperstimulation (mean of three VOEs per patient without complications vs six per patient with complications; P = .036).
Higher Than Normal Need for Multiple Cycles
Reproductive endocrinologist H. Irene Su, MD, professor and co-director of the Center for OB/GYN Research Innovations at Moores Cancer Center, University of California San Diego, praised the study as “an important report” in an interview.
Su, who wasn’t involved in the research, said the percentage of patients requiring more than one cycle due to cancellation or low oocyte yield — 13% — is “higher than expected, given the young age of this cohort.”
This could reflect the hypothesis that “sickle cell crises and hypoxia adversely affect the finite number of oocytes in the ovary,” she said.
As for the study findings regarding complications, she said the rate “is very high compared to the general infertility or fertility preservation population. It would be good to learn predictors of these outcomes so that fertility and hematology clinicians can work together to stratify risk and supportive services around FP cycles. It would also be good to know if the post-retrieval VOE were unexpected given the patient’s disease activity prior to FP.”
Message: FP in SCD Is Feasible, Acceptable
A.D. Mishkin, MD, MPH, associate professor of psychiatry and liaison to the Blood and Marrow Transplantation Program at NewYork–Presbyterian/Columbia University Irving Medical Center, New York City, said in an interview that the study “establishes the feasibility and acceptability of oocyte harvest and preservation in a population of patients with active ongoing symptoms from SCD. It also indicates their interest in pursuing fertility preservation in the setting of frequent crises and the potential for management of ensuing complications.”
Mishkin, who didn’t take part in the research, highlighted the finding that half the patients got access to FP via public insurance or research funding. “Even in this population where most women had multiple complications in the year prior to FP, and even among patients who needed multiple retrievals, these patients wanted to go through that risk to preserve their fertility,” Mishkin said. “This is an important finding given the very limited access many individuals have to FP due to its high cost and limited insurance coverage, which is also largely state-dependent.”
There’s another factor to consider regarding SCD and FP: The potential danger of pregnancy.
Corresponding author Pecker noted that “pregnancy is high risk for people with sickle cell disease. There are very high rates of severe maternal mortality and morbidity even in high-income countries. However, some of this is modifiable with routine use of chronic transfusions during pregnancy and with high-quality and integrated expert SCD and expert maternal fetal medicine care during pregnancy.”
The National Institutes of Health supported the research. Pecker reported receiving research funding from Alexion, Novartis, and Aummune and consulting for Novo Nordisk. Other authors reported no disclosures. Su and Mishkin reported no disclosures.
A version of this article appeared on Medscape.com.
Of 46 patients with SCD, complications occurred in 25 of 55 controlled ovarian hyperstimulation cycles, including 29 vaso-occlusive episodes (VOEs), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
Of 21 post-retrieval VOEs, 19 required emergency department care or hospitalization.
“Baseline sickle cell disease severity is most likely associated with a patient’s risk of complications from an egg retrieval cycle,” study co-author Sarah Cromack, MD, a reproductive endocrinology and infertility fellow at Northwestern University, Chicago, said in an interview.
“Both hematologists and reproductive endocrinologists can use this information to plan ahead and anticipate possible issues, check blood counts prior to and after egg retrieval to see if transfusion is needed, and plan close follow-up during stimulation and immediately after egg retrieval to evaluate and treat pain.”
SCD Accelerates Decline in Ovarian Reserve
Pediatric hematologist Lydia H. Pecker, MD, MS, of Johns Hopkins University School of Medicine, Baltimore, the study’s corresponding author, said in an interview that SCD is “a disease of accelerated aging” that leads to accelerated decline in ovarian reserve. “The common indication for fertility preservation in SCD is before bone marrow transplant or gene therapy,” she said, although FP can also be offered to other patients with SCD.
According to Cromack, researchers launched the study to expand information about SCD and FP in light of sparse data about outcomes.
All the 46 patients had hemoglobin SS (HbSS, 93%) and HbSβ0-thalassemia (7%) and a median age of 23.7 (18-28) years. Almost all (44 patients) underwent FP prior to curative treatments, and all had at least one SCD-related complication, mainly cerebrovascular disease (16), acute chest syndrome (23), and more than two VOEs per year (31).
Median anti-Mullerian hormone (AMH) level (2.1 ng/mL), a measurement of ovarian reserve, was lower than the expected level of 2.8-3.4 ng/mL among women in the age range of the patients, the researchers reported. “This is consistent with previous studies showing lower AMH for age in women with sickle cell disease,” Pecker said.
Complications in 45% of Retrieval Cycles
“In terms of success of oocyte cryopreservation, the median number of mature eggs frozen was 11,” said co-author and reproductive endocrinologist Jessica Walter, MD, of Northwestern University, in an interview. “Given the average age of 24 years in the cohort, this would give each patient about a 70% estimated probability of at least one live birth from their cohort of frozen eggs. Thus, patients hoping for more than one child may want to consider more than one cycle of egg freezing.”
The rate of complications was “fairly high” at 45% of all cycles, Walter said. “These were mostly complications from underlying sickle cell disease, including unplanned transfusions and admissions for vaso-occlusive crises. Surprisingly, there were very few cases of ovarian hyperstimulation syndrome in this young patient group, which may be due to a combination of underlying vascular disease, lower peak estradiol levels, and slightly less eggs retrieved then would be expected compared to an age-matched healthy controls.”
Any FP complication was associated with more than three VOEs in the year before controlled ovarian hyperstimulation (mean of three VOEs per patient without complications vs six per patient with complications; P = .036).
Higher Than Normal Need for Multiple Cycles
Reproductive endocrinologist H. Irene Su, MD, professor and co-director of the Center for OB/GYN Research Innovations at Moores Cancer Center, University of California San Diego, praised the study as “an important report” in an interview.
Su, who wasn’t involved in the research, said the percentage of patients requiring more than one cycle due to cancellation or low oocyte yield — 13% — is “higher than expected, given the young age of this cohort.”
This could reflect the hypothesis that “sickle cell crises and hypoxia adversely affect the finite number of oocytes in the ovary,” she said.
As for the study findings regarding complications, she said the rate “is very high compared to the general infertility or fertility preservation population. It would be good to learn predictors of these outcomes so that fertility and hematology clinicians can work together to stratify risk and supportive services around FP cycles. It would also be good to know if the post-retrieval VOE were unexpected given the patient’s disease activity prior to FP.”
Message: FP in SCD Is Feasible, Acceptable
A.D. Mishkin, MD, MPH, associate professor of psychiatry and liaison to the Blood and Marrow Transplantation Program at NewYork–Presbyterian/Columbia University Irving Medical Center, New York City, said in an interview that the study “establishes the feasibility and acceptability of oocyte harvest and preservation in a population of patients with active ongoing symptoms from SCD. It also indicates their interest in pursuing fertility preservation in the setting of frequent crises and the potential for management of ensuing complications.”
Mishkin, who didn’t take part in the research, highlighted the finding that half the patients got access to FP via public insurance or research funding. “Even in this population where most women had multiple complications in the year prior to FP, and even among patients who needed multiple retrievals, these patients wanted to go through that risk to preserve their fertility,” Mishkin said. “This is an important finding given the very limited access many individuals have to FP due to its high cost and limited insurance coverage, which is also largely state-dependent.”
There’s another factor to consider regarding SCD and FP: The potential danger of pregnancy.
Corresponding author Pecker noted that “pregnancy is high risk for people with sickle cell disease. There are very high rates of severe maternal mortality and morbidity even in high-income countries. However, some of this is modifiable with routine use of chronic transfusions during pregnancy and with high-quality and integrated expert SCD and expert maternal fetal medicine care during pregnancy.”
The National Institutes of Health supported the research. Pecker reported receiving research funding from Alexion, Novartis, and Aummune and consulting for Novo Nordisk. Other authors reported no disclosures. Su and Mishkin reported no disclosures.
A version of this article appeared on Medscape.com.
Of 46 patients with SCD, complications occurred in 25 of 55 controlled ovarian hyperstimulation cycles, including 29 vaso-occlusive episodes (VOEs), researchers reported at the American Society of Hematology (ASH) 2024 Annual Meeting.
Of 21 post-retrieval VOEs, 19 required emergency department care or hospitalization.
“Baseline sickle cell disease severity is most likely associated with a patient’s risk of complications from an egg retrieval cycle,” study co-author Sarah Cromack, MD, a reproductive endocrinology and infertility fellow at Northwestern University, Chicago, said in an interview.
“Both hematologists and reproductive endocrinologists can use this information to plan ahead and anticipate possible issues, check blood counts prior to and after egg retrieval to see if transfusion is needed, and plan close follow-up during stimulation and immediately after egg retrieval to evaluate and treat pain.”
SCD Accelerates Decline in Ovarian Reserve
Pediatric hematologist Lydia H. Pecker, MD, MS, of Johns Hopkins University School of Medicine, Baltimore, the study’s corresponding author, said in an interview that SCD is “a disease of accelerated aging” that leads to accelerated decline in ovarian reserve. “The common indication for fertility preservation in SCD is before bone marrow transplant or gene therapy,” she said, although FP can also be offered to other patients with SCD.
According to Cromack, researchers launched the study to expand information about SCD and FP in light of sparse data about outcomes.
All the 46 patients had hemoglobin SS (HbSS, 93%) and HbSβ0-thalassemia (7%) and a median age of 23.7 (18-28) years. Almost all (44 patients) underwent FP prior to curative treatments, and all had at least one SCD-related complication, mainly cerebrovascular disease (16), acute chest syndrome (23), and more than two VOEs per year (31).
Median anti-Mullerian hormone (AMH) level (2.1 ng/mL), a measurement of ovarian reserve, was lower than the expected level of 2.8-3.4 ng/mL among women in the age range of the patients, the researchers reported. “This is consistent with previous studies showing lower AMH for age in women with sickle cell disease,” Pecker said.
Complications in 45% of Retrieval Cycles
“In terms of success of oocyte cryopreservation, the median number of mature eggs frozen was 11,” said co-author and reproductive endocrinologist Jessica Walter, MD, of Northwestern University, in an interview. “Given the average age of 24 years in the cohort, this would give each patient about a 70% estimated probability of at least one live birth from their cohort of frozen eggs. Thus, patients hoping for more than one child may want to consider more than one cycle of egg freezing.”
The rate of complications was “fairly high” at 45% of all cycles, Walter said. “These were mostly complications from underlying sickle cell disease, including unplanned transfusions and admissions for vaso-occlusive crises. Surprisingly, there were very few cases of ovarian hyperstimulation syndrome in this young patient group, which may be due to a combination of underlying vascular disease, lower peak estradiol levels, and slightly less eggs retrieved then would be expected compared to an age-matched healthy controls.”
Any FP complication was associated with more than three VOEs in the year before controlled ovarian hyperstimulation (mean of three VOEs per patient without complications vs six per patient with complications; P = .036).
Higher Than Normal Need for Multiple Cycles
Reproductive endocrinologist H. Irene Su, MD, professor and co-director of the Center for OB/GYN Research Innovations at Moores Cancer Center, University of California San Diego, praised the study as “an important report” in an interview.
Su, who wasn’t involved in the research, said the percentage of patients requiring more than one cycle due to cancellation or low oocyte yield — 13% — is “higher than expected, given the young age of this cohort.”
This could reflect the hypothesis that “sickle cell crises and hypoxia adversely affect the finite number of oocytes in the ovary,” she said.
As for the study findings regarding complications, she said the rate “is very high compared to the general infertility or fertility preservation population. It would be good to learn predictors of these outcomes so that fertility and hematology clinicians can work together to stratify risk and supportive services around FP cycles. It would also be good to know if the post-retrieval VOE were unexpected given the patient’s disease activity prior to FP.”
Message: FP in SCD Is Feasible, Acceptable
A.D. Mishkin, MD, MPH, associate professor of psychiatry and liaison to the Blood and Marrow Transplantation Program at NewYork–Presbyterian/Columbia University Irving Medical Center, New York City, said in an interview that the study “establishes the feasibility and acceptability of oocyte harvest and preservation in a population of patients with active ongoing symptoms from SCD. It also indicates their interest in pursuing fertility preservation in the setting of frequent crises and the potential for management of ensuing complications.”
Mishkin, who didn’t take part in the research, highlighted the finding that half the patients got access to FP via public insurance or research funding. “Even in this population where most women had multiple complications in the year prior to FP, and even among patients who needed multiple retrievals, these patients wanted to go through that risk to preserve their fertility,” Mishkin said. “This is an important finding given the very limited access many individuals have to FP due to its high cost and limited insurance coverage, which is also largely state-dependent.”
There’s another factor to consider regarding SCD and FP: The potential danger of pregnancy.
Corresponding author Pecker noted that “pregnancy is high risk for people with sickle cell disease. There are very high rates of severe maternal mortality and morbidity even in high-income countries. However, some of this is modifiable with routine use of chronic transfusions during pregnancy and with high-quality and integrated expert SCD and expert maternal fetal medicine care during pregnancy.”
The National Institutes of Health supported the research. Pecker reported receiving research funding from Alexion, Novartis, and Aummune and consulting for Novo Nordisk. Other authors reported no disclosures. Su and Mishkin reported no disclosures.
A version of this article appeared on Medscape.com.
FROM ASH 2024