User login
Smoking impairs biologic response in axial spondyloarthritis
Patients with axial spondyloarthritis who smoke and have elevated C-reactive protein levels respond less well to anti–tumor necrosis factor treatment than do nonsmokers, Swiss researchers reported.
The influence of smoking on treatment response is well known in rheumatoid arthritis, but the impact of tobacco use on patients with axial spondyloarthritis is only beginning to emerge.
In this study of 698 patients with confirmed axial spondyloarthritis who were taking a first anti–tumor necrosis factor (TNF) agent, the effect of smoking on treatment response was measured at 1 year using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Ankylosing Spondylitis Disease Activity Score (ASDAS) after adjustment for potential confounders, such as sex, amount of exercise, age, and disease duration (Ann. Rheum. Dis. 2015 Feb. 9 [doi:10.1136/annrheumdis-2013-205133]).
Dr. Adrian Ciurea of the University Hospital Zurich and associates found that patients with elevated C-reactive protein (CRP) levels who smoked achieved significantly smaller reductions in BASDAI and ASDAS scores after initiation of TNF inhibitors, compared with nonsmokers (0.75 BASDAI and 0.69 ASDAS units less, P = .005 and P = .001, respectively).
The odds of reaching a 50% improvement in BASDAI score or meeting ASAS criteria for 40% improvement after 1 year was significantly lower in current smokers than in nonsmokers (odds ratio, 0.54; P = .03; and OR, 0.43; P = .004, respectively).
Past smoking had no significant effect on response to treatment, the researchers said.
The underlying mechanisms on the influence of smoking are unclear, but could be related to an interference with the pharmacokinetics of anti-TNFs or smoking may increase pain levels or starve tissues of oxygen, the researchers suggested.
“Whether quitting smoking might ameliorate the course of disease during treatment with TNFi remains to be confirmed in prospective studies,” they concluded.
Patients in the study were part of the Swiss Clinical Quality Management Cohort during 2005-2014. Almost two-thirds (62%) were smokers; 38% were nonsmokers.
Dr. Ciurea and two coauthors have received consulting and/or speaking fees from a variety of companies marketing biologic drugs for rheumatic diseases. The study was funded by grants from the Foundation for Arthritis Research and the Swiss Spondylitis Foundation.
Patients with axial spondyloarthritis who smoke and have elevated C-reactive protein levels respond less well to anti–tumor necrosis factor treatment than do nonsmokers, Swiss researchers reported.
The influence of smoking on treatment response is well known in rheumatoid arthritis, but the impact of tobacco use on patients with axial spondyloarthritis is only beginning to emerge.
In this study of 698 patients with confirmed axial spondyloarthritis who were taking a first anti–tumor necrosis factor (TNF) agent, the effect of smoking on treatment response was measured at 1 year using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Ankylosing Spondylitis Disease Activity Score (ASDAS) after adjustment for potential confounders, such as sex, amount of exercise, age, and disease duration (Ann. Rheum. Dis. 2015 Feb. 9 [doi:10.1136/annrheumdis-2013-205133]).
Dr. Adrian Ciurea of the University Hospital Zurich and associates found that patients with elevated C-reactive protein (CRP) levels who smoked achieved significantly smaller reductions in BASDAI and ASDAS scores after initiation of TNF inhibitors, compared with nonsmokers (0.75 BASDAI and 0.69 ASDAS units less, P = .005 and P = .001, respectively).
The odds of reaching a 50% improvement in BASDAI score or meeting ASAS criteria for 40% improvement after 1 year was significantly lower in current smokers than in nonsmokers (odds ratio, 0.54; P = .03; and OR, 0.43; P = .004, respectively).
Past smoking had no significant effect on response to treatment, the researchers said.
The underlying mechanisms on the influence of smoking are unclear, but could be related to an interference with the pharmacokinetics of anti-TNFs or smoking may increase pain levels or starve tissues of oxygen, the researchers suggested.
“Whether quitting smoking might ameliorate the course of disease during treatment with TNFi remains to be confirmed in prospective studies,” they concluded.
Patients in the study were part of the Swiss Clinical Quality Management Cohort during 2005-2014. Almost two-thirds (62%) were smokers; 38% were nonsmokers.
Dr. Ciurea and two coauthors have received consulting and/or speaking fees from a variety of companies marketing biologic drugs for rheumatic diseases. The study was funded by grants from the Foundation for Arthritis Research and the Swiss Spondylitis Foundation.
Patients with axial spondyloarthritis who smoke and have elevated C-reactive protein levels respond less well to anti–tumor necrosis factor treatment than do nonsmokers, Swiss researchers reported.
The influence of smoking on treatment response is well known in rheumatoid arthritis, but the impact of tobacco use on patients with axial spondyloarthritis is only beginning to emerge.
In this study of 698 patients with confirmed axial spondyloarthritis who were taking a first anti–tumor necrosis factor (TNF) agent, the effect of smoking on treatment response was measured at 1 year using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Ankylosing Spondylitis Disease Activity Score (ASDAS) after adjustment for potential confounders, such as sex, amount of exercise, age, and disease duration (Ann. Rheum. Dis. 2015 Feb. 9 [doi:10.1136/annrheumdis-2013-205133]).
Dr. Adrian Ciurea of the University Hospital Zurich and associates found that patients with elevated C-reactive protein (CRP) levels who smoked achieved significantly smaller reductions in BASDAI and ASDAS scores after initiation of TNF inhibitors, compared with nonsmokers (0.75 BASDAI and 0.69 ASDAS units less, P = .005 and P = .001, respectively).
The odds of reaching a 50% improvement in BASDAI score or meeting ASAS criteria for 40% improvement after 1 year was significantly lower in current smokers than in nonsmokers (odds ratio, 0.54; P = .03; and OR, 0.43; P = .004, respectively).
Past smoking had no significant effect on response to treatment, the researchers said.
The underlying mechanisms on the influence of smoking are unclear, but could be related to an interference with the pharmacokinetics of anti-TNFs or smoking may increase pain levels or starve tissues of oxygen, the researchers suggested.
“Whether quitting smoking might ameliorate the course of disease during treatment with TNFi remains to be confirmed in prospective studies,” they concluded.
Patients in the study were part of the Swiss Clinical Quality Management Cohort during 2005-2014. Almost two-thirds (62%) were smokers; 38% were nonsmokers.
Dr. Ciurea and two coauthors have received consulting and/or speaking fees from a variety of companies marketing biologic drugs for rheumatic diseases. The study was funded by grants from the Foundation for Arthritis Research and the Swiss Spondylitis Foundation.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Current smoking impairs treatment response to anti-TNFs in patients with axial spondyloarthritis who had elevated C-reactive protein levels.
Major finding: People with axial spondyloarthritis who smoked and had elevated C-reactive protein levels achieved significantly smaller reductions in BASDAI and ASDAS scores, compared with nonsmokers.
Source: A longitudinal study of 698 patients with axial spondyloarthritis who were taking a first anti-TNF agent and were part of the Swiss Clinical Quality Management Cohort between 2005 and 2014.
Disclosures: Dr. Ciurea and two coauthors have received consulting and/or speaking fees from a variety of companies marketing biologic drugs for rheumatic diseases. The study was funded by grants from the Foundation for Arthritis Research and the Swiss Spondylitis Foundation.
Unnecessary Stress Tests in ED Leading to Overdiagnosis
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing. “When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing. “When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing. “When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
Consider Chikungunya virus in new-onset polyarthritis
Rheumatologists should consider the possibility of Chikungunya virus in patients who present with new symmetric polyarthritis, especially if they have just returned from an endemic region such as the Caribbean, according to researchers.
In their paper, first authors Dr. Jonathan J. Miner and Dr. Han-Xian Aw-Yeang and colleagues at Washington University, St. Louis, describe a cohort of 10 Americans who traveled to Haiti within a 20-day period in June 2014 and became infected with Chikungunya virus (CHIKV), an arthritogenic, mosquito-transmitted alphavirus (Arthritis Rheumatol. 2015 Jan. 20 [doi:10.1002/art.39027]).
The virus spread to the Caribbean in 2013 and the United States in 2014. Its acute phase of infection includes symptoms such as fever, headache, rash, arthralgia, arthritis, and myalgia.
The virus is likely to become a unique diagnostic challenge for rheumatologists as the arthritis symptoms mimic seronegative arthritis, the researchers said.
“Eight out of these patients would have met the 2010 ACR/EULAR criteria for RA [rheumatoid arthritis] if the initial fever, rash, and travel to the Caribbean had not been revealed,” they noted.
Most of the patients had joint pain and morning stiffness at least 8 weeks after initial infection, although some reported gradual improvement of their symptoms, the investigators reported.
One of the patients developed fever; diffuse arthritis; an erythematous, maculopapular rash; and severe symmetric polyarthritis that persisted more than 5 months post infection. She was treated with prednisolone but it exacerbated her joint pain and treatment was stopped.
The other patient detailed in the report presented with similar symptoms. His fever and rash resolved within 2 days but his arthritis symptoms persisted. He was treated with NSAIDs that provided only minimal relief.
To understand more about the immunologic parameters of the virus, the researchers used cytometry by time of flight to compare the peripheral mononuclear cells from CHIKV-infected patients with those of healthy controls and untreated patients with RA.
They discovered that naive, activated, and effector T killer– and T helper–cell populations occurred in similar percentages in the virus-infected patients and RA patients but not in the healthy controls.
The RA patients, however, had a higher expression of L-selectin expression in CD4+ T cells than did either virus-infected patients or healthy controls.
“These data suggest that lymphocyte phenotypes in patients with Chikungunya infection are similar to each other, with subtle but distinct trends that could potentially distinguish these two groups from healthy controls and from each other,” Dr. Miner and Dr. Aw-Yeang and their associates wrote.
Whether treatment with disease-modifying antirheumatic drugs or biologics used in RA is appropriate or effective is controversial in the absence of randomized controlled trials for CHIKV-related arthritis, they said.
“Immunosuppression in CHIKV-infected patients could be deleterious because viral RNA and antigens can be found in target tissues in the chronic phase in humans and experimental animals,” the authors wrote.
“Rheumatologists, even in non-CHIKV-endemic regions, need to consider CHIKV in their evaluation of symmetric polyarthritis lasting more than 6 weeks by obtaining a history of travel to CHIKV-endemic regions, which are likely to expand in the near future,” the investigators advised.
Patients who may have been exposed to the virus may need serologic testing before initiating immunosuppression, they said.
“Unfortunately, access to CHIKV testing is highly constrained at the current time as it is only available from the [Centers for Disease Control and Prevention] and research laboratories,” they added.
The study was supported by the Barnes-Jewish Hospital Foundation and the Howard Hughes Medical Institute. The authors reported no conflicts of interest.
Rheumatologists should consider the possibility of Chikungunya virus in patients who present with new symmetric polyarthritis, especially if they have just returned from an endemic region such as the Caribbean, according to researchers.
In their paper, first authors Dr. Jonathan J. Miner and Dr. Han-Xian Aw-Yeang and colleagues at Washington University, St. Louis, describe a cohort of 10 Americans who traveled to Haiti within a 20-day period in June 2014 and became infected with Chikungunya virus (CHIKV), an arthritogenic, mosquito-transmitted alphavirus (Arthritis Rheumatol. 2015 Jan. 20 [doi:10.1002/art.39027]).
The virus spread to the Caribbean in 2013 and the United States in 2014. Its acute phase of infection includes symptoms such as fever, headache, rash, arthralgia, arthritis, and myalgia.
The virus is likely to become a unique diagnostic challenge for rheumatologists as the arthritis symptoms mimic seronegative arthritis, the researchers said.
“Eight out of these patients would have met the 2010 ACR/EULAR criteria for RA [rheumatoid arthritis] if the initial fever, rash, and travel to the Caribbean had not been revealed,” they noted.
Most of the patients had joint pain and morning stiffness at least 8 weeks after initial infection, although some reported gradual improvement of their symptoms, the investigators reported.
One of the patients developed fever; diffuse arthritis; an erythematous, maculopapular rash; and severe symmetric polyarthritis that persisted more than 5 months post infection. She was treated with prednisolone but it exacerbated her joint pain and treatment was stopped.
The other patient detailed in the report presented with similar symptoms. His fever and rash resolved within 2 days but his arthritis symptoms persisted. He was treated with NSAIDs that provided only minimal relief.
To understand more about the immunologic parameters of the virus, the researchers used cytometry by time of flight to compare the peripheral mononuclear cells from CHIKV-infected patients with those of healthy controls and untreated patients with RA.
They discovered that naive, activated, and effector T killer– and T helper–cell populations occurred in similar percentages in the virus-infected patients and RA patients but not in the healthy controls.
The RA patients, however, had a higher expression of L-selectin expression in CD4+ T cells than did either virus-infected patients or healthy controls.
“These data suggest that lymphocyte phenotypes in patients with Chikungunya infection are similar to each other, with subtle but distinct trends that could potentially distinguish these two groups from healthy controls and from each other,” Dr. Miner and Dr. Aw-Yeang and their associates wrote.
Whether treatment with disease-modifying antirheumatic drugs or biologics used in RA is appropriate or effective is controversial in the absence of randomized controlled trials for CHIKV-related arthritis, they said.
“Immunosuppression in CHIKV-infected patients could be deleterious because viral RNA and antigens can be found in target tissues in the chronic phase in humans and experimental animals,” the authors wrote.
“Rheumatologists, even in non-CHIKV-endemic regions, need to consider CHIKV in their evaluation of symmetric polyarthritis lasting more than 6 weeks by obtaining a history of travel to CHIKV-endemic regions, which are likely to expand in the near future,” the investigators advised.
Patients who may have been exposed to the virus may need serologic testing before initiating immunosuppression, they said.
“Unfortunately, access to CHIKV testing is highly constrained at the current time as it is only available from the [Centers for Disease Control and Prevention] and research laboratories,” they added.
The study was supported by the Barnes-Jewish Hospital Foundation and the Howard Hughes Medical Institute. The authors reported no conflicts of interest.
Rheumatologists should consider the possibility of Chikungunya virus in patients who present with new symmetric polyarthritis, especially if they have just returned from an endemic region such as the Caribbean, according to researchers.
In their paper, first authors Dr. Jonathan J. Miner and Dr. Han-Xian Aw-Yeang and colleagues at Washington University, St. Louis, describe a cohort of 10 Americans who traveled to Haiti within a 20-day period in June 2014 and became infected with Chikungunya virus (CHIKV), an arthritogenic, mosquito-transmitted alphavirus (Arthritis Rheumatol. 2015 Jan. 20 [doi:10.1002/art.39027]).
The virus spread to the Caribbean in 2013 and the United States in 2014. Its acute phase of infection includes symptoms such as fever, headache, rash, arthralgia, arthritis, and myalgia.
The virus is likely to become a unique diagnostic challenge for rheumatologists as the arthritis symptoms mimic seronegative arthritis, the researchers said.
“Eight out of these patients would have met the 2010 ACR/EULAR criteria for RA [rheumatoid arthritis] if the initial fever, rash, and travel to the Caribbean had not been revealed,” they noted.
Most of the patients had joint pain and morning stiffness at least 8 weeks after initial infection, although some reported gradual improvement of their symptoms, the investigators reported.
One of the patients developed fever; diffuse arthritis; an erythematous, maculopapular rash; and severe symmetric polyarthritis that persisted more than 5 months post infection. She was treated with prednisolone but it exacerbated her joint pain and treatment was stopped.
The other patient detailed in the report presented with similar symptoms. His fever and rash resolved within 2 days but his arthritis symptoms persisted. He was treated with NSAIDs that provided only minimal relief.
To understand more about the immunologic parameters of the virus, the researchers used cytometry by time of flight to compare the peripheral mononuclear cells from CHIKV-infected patients with those of healthy controls and untreated patients with RA.
They discovered that naive, activated, and effector T killer– and T helper–cell populations occurred in similar percentages in the virus-infected patients and RA patients but not in the healthy controls.
The RA patients, however, had a higher expression of L-selectin expression in CD4+ T cells than did either virus-infected patients or healthy controls.
“These data suggest that lymphocyte phenotypes in patients with Chikungunya infection are similar to each other, with subtle but distinct trends that could potentially distinguish these two groups from healthy controls and from each other,” Dr. Miner and Dr. Aw-Yeang and their associates wrote.
Whether treatment with disease-modifying antirheumatic drugs or biologics used in RA is appropriate or effective is controversial in the absence of randomized controlled trials for CHIKV-related arthritis, they said.
“Immunosuppression in CHIKV-infected patients could be deleterious because viral RNA and antigens can be found in target tissues in the chronic phase in humans and experimental animals,” the authors wrote.
“Rheumatologists, even in non-CHIKV-endemic regions, need to consider CHIKV in their evaluation of symmetric polyarthritis lasting more than 6 weeks by obtaining a history of travel to CHIKV-endemic regions, which are likely to expand in the near future,” the investigators advised.
Patients who may have been exposed to the virus may need serologic testing before initiating immunosuppression, they said.
“Unfortunately, access to CHIKV testing is highly constrained at the current time as it is only available from the [Centers for Disease Control and Prevention] and research laboratories,” they added.
The study was supported by the Barnes-Jewish Hospital Foundation and the Howard Hughes Medical Institute. The authors reported no conflicts of interest.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: The mosquito-spread Chikungunya virus mimics seronegative rheumatoid arthritis. Rheumatologists should consider this diagnosis in patients who present with arthritis symptoms after visiting an endemic area.
Major finding: Eight out of the 10 people confirmed to be infected with the CHIKV virus met the 2010 ACR/EULAR criteria for RA.
Source: An observational study of a group of 10 Americans who traveled to Haiti within a 20-day period in June 2014 and became infected with CHIKV.
Disclosures: The study was supported by the Barnes-Jewish Hospital Foundation and the Howard Hughes Medical Institute. The authors reported no conflicts of interest.
Unnecessary stress tests in ED leading to overdiagnosis
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing.“When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
The findings suggest that the current practice of performing a stress test on low-risk patients in the emergency department is unnecessary, prolonging stays and exposing patients to medical imaging that comes with significant associated radiation risk. It may be time to change guidelines for the treatment of chest pain in low-risk patients. Such patients should be given a close follow-up appointment with a primary care physician who can determine, based on the patient’s condition, whether further evaluation was necessary.
Dr. Rita F. Redberg is the chief editor of JAMA Internal Medicine and professor of medicine at the University of California, San Francisco. She made her comments in an editor’s note that accompanied the article (doi:10.1001/jamainternmed.2014.7698).
The findings suggest that the current practice of performing a stress test on low-risk patients in the emergency department is unnecessary, prolonging stays and exposing patients to medical imaging that comes with significant associated radiation risk. It may be time to change guidelines for the treatment of chest pain in low-risk patients. Such patients should be given a close follow-up appointment with a primary care physician who can determine, based on the patient’s condition, whether further evaluation was necessary.
Dr. Rita F. Redberg is the chief editor of JAMA Internal Medicine and professor of medicine at the University of California, San Francisco. She made her comments in an editor’s note that accompanied the article (doi:10.1001/jamainternmed.2014.7698).
The findings suggest that the current practice of performing a stress test on low-risk patients in the emergency department is unnecessary, prolonging stays and exposing patients to medical imaging that comes with significant associated radiation risk. It may be time to change guidelines for the treatment of chest pain in low-risk patients. Such patients should be given a close follow-up appointment with a primary care physician who can determine, based on the patient’s condition, whether further evaluation was necessary.
Dr. Rita F. Redberg is the chief editor of JAMA Internal Medicine and professor of medicine at the University of California, San Francisco. She made her comments in an editor’s note that accompanied the article (doi:10.1001/jamainternmed.2014.7698).
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing.“When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
Noninvasive testing in the emergency department of patients who have chest pain and have not had a myocardial infarction can result in overdiagnosis and unnecessary interventions, based on the results of a retrospective analysis.
After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to the emergency department (ED) with chest pain were hospitalized with an MI. There was no difference in the rate of MIs in patients who did and did not undergo exercise and stress electrocardiography, myocardial perfusion scintigraphy (MPS), or coronary CT angiography, Dr. Andrew. J. Foy of Penn State Milton S. Hershey Medical Center in Hershey, Pa., and his colleagues reported in an article published online in JAMA Internal Medicine (2015 Jan. 26 [doi:10.1001/jamainternmed.2014.7657]).
However, interventions were increased in patients who underwent tests without a concomitant reduction in MI in patients who underwent tests in the ED. “Overdiagnosis is a legitimate concern in this patient population,” the study authors wrote.
Using data from the analysis, the researchers estimated that an unnecessary catheterization is performed in 1 of every 27 patients who undergo MPS instead of an initial strategy of no testing.“When viewed in the broader context of the approximately 6 million ED visits for a chief symptom of chest pain, for every 100,000 patients who undergo MPS instead of an initial strategy of no testing, approximately 3,700 patients will undergo an unnecessary catheterization,” they wrote.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Guidelines for treatment of chest pain in low-risk patients in the emergency department may need revision, as noninvasive testing of these patients may be leading to unneeded interventions.
Major finding: After 6 months of follow-up, 0.33% of 421,774 privately insured patients who presented to an ED with chest pain were hospitalized with a myocardial infarction.
Data source: A retrospective analysis of health insurance claims data.
Disclosures: The researchers reported having no conflicts of interest.
ACOG outlines new treatment options for hypertensive emergencies in pregnancy
The American College of Obstetricians and Gynecologists has added nifedipine as a first-line treatment for acute-onset severe hypertension during pregnancy and the postpartum period in an updated opinion from its Committee on Obstetric Practice.
The update, released on Jan. 22, points to studies showing that women who received oral nifedipine had their blood pressure lowered more quickly than with either intravenous labetalol or hydralazine – the traditional first-line treatments – and had a significant increase in urine output. Concerns about neuromuscular blockade and severe hypotension with the use of nifedipine and magnesium sulphate were not borne out in a large review, the committee members wrote, but they advised careful monitoring since both drugs are calcium antagonists.
The committee opinion includes model order sets for the use of labetalol, hydralazine, and nifedipine for the initial management of acute onset severe hypertension in women who are pregnant or post partum with preeclampsia or eclampsia (Obstet. Gynecol. 2015;125:521-5).
While all three medications are appropriate in treating hypertensive emergencies during pregnancy, each drug has adverse effects.
For instance, parenteral hydralazine can increase the risk of maternal hypotension. Parenteral labetalol may cause neonatal bradycardia and should be avoided in women with asthma, heart disease, or heart failure. Nifedipine has been associated with increased maternal heart rate and overshoot hypotension.
“Patients may respond to one drug and not another,” the committee noted.
The ACOG committee also called for standardized clinical guidelines for the management of patients with preeclampsia and eclampsia.
“With the advent of pregnancy hypertension guidelines in the United Kingdom, care of maternity patients with preeclampsia or eclampsia improved significantly and maternal mortality rates decreased because of a reduction in cerebral and respiratory complications,” they wrote. “Individuals and institutions should have mechanisms in place to initiate the prompt administration of medication when a patient presents with a hypertensive emergency.”
The committee recommended checklists as one tool to help standardize the use of guidelines.
The American College of Obstetricians and Gynecologists has added nifedipine as a first-line treatment for acute-onset severe hypertension during pregnancy and the postpartum period in an updated opinion from its Committee on Obstetric Practice.
The update, released on Jan. 22, points to studies showing that women who received oral nifedipine had their blood pressure lowered more quickly than with either intravenous labetalol or hydralazine – the traditional first-line treatments – and had a significant increase in urine output. Concerns about neuromuscular blockade and severe hypotension with the use of nifedipine and magnesium sulphate were not borne out in a large review, the committee members wrote, but they advised careful monitoring since both drugs are calcium antagonists.
The committee opinion includes model order sets for the use of labetalol, hydralazine, and nifedipine for the initial management of acute onset severe hypertension in women who are pregnant or post partum with preeclampsia or eclampsia (Obstet. Gynecol. 2015;125:521-5).
While all three medications are appropriate in treating hypertensive emergencies during pregnancy, each drug has adverse effects.
For instance, parenteral hydralazine can increase the risk of maternal hypotension. Parenteral labetalol may cause neonatal bradycardia and should be avoided in women with asthma, heart disease, or heart failure. Nifedipine has been associated with increased maternal heart rate and overshoot hypotension.
“Patients may respond to one drug and not another,” the committee noted.
The ACOG committee also called for standardized clinical guidelines for the management of patients with preeclampsia and eclampsia.
“With the advent of pregnancy hypertension guidelines in the United Kingdom, care of maternity patients with preeclampsia or eclampsia improved significantly and maternal mortality rates decreased because of a reduction in cerebral and respiratory complications,” they wrote. “Individuals and institutions should have mechanisms in place to initiate the prompt administration of medication when a patient presents with a hypertensive emergency.”
The committee recommended checklists as one tool to help standardize the use of guidelines.
The American College of Obstetricians and Gynecologists has added nifedipine as a first-line treatment for acute-onset severe hypertension during pregnancy and the postpartum period in an updated opinion from its Committee on Obstetric Practice.
The update, released on Jan. 22, points to studies showing that women who received oral nifedipine had their blood pressure lowered more quickly than with either intravenous labetalol or hydralazine – the traditional first-line treatments – and had a significant increase in urine output. Concerns about neuromuscular blockade and severe hypotension with the use of nifedipine and magnesium sulphate were not borne out in a large review, the committee members wrote, but they advised careful monitoring since both drugs are calcium antagonists.
The committee opinion includes model order sets for the use of labetalol, hydralazine, and nifedipine for the initial management of acute onset severe hypertension in women who are pregnant or post partum with preeclampsia or eclampsia (Obstet. Gynecol. 2015;125:521-5).
While all three medications are appropriate in treating hypertensive emergencies during pregnancy, each drug has adverse effects.
For instance, parenteral hydralazine can increase the risk of maternal hypotension. Parenteral labetalol may cause neonatal bradycardia and should be avoided in women with asthma, heart disease, or heart failure. Nifedipine has been associated with increased maternal heart rate and overshoot hypotension.
“Patients may respond to one drug and not another,” the committee noted.
The ACOG committee also called for standardized clinical guidelines for the management of patients with preeclampsia and eclampsia.
“With the advent of pregnancy hypertension guidelines in the United Kingdom, care of maternity patients with preeclampsia or eclampsia improved significantly and maternal mortality rates decreased because of a reduction in cerebral and respiratory complications,” they wrote. “Individuals and institutions should have mechanisms in place to initiate the prompt administration of medication when a patient presents with a hypertensive emergency.”
The committee recommended checklists as one tool to help standardize the use of guidelines.
FROM OBSTETRICS AND GYNECOLOGY
Antibody hallmark for lupus challenged by study
The findings of a new study challenge the importance of anti–double stranded DNA antibodies as a diagnostic hallmark for lupus.
The assessment of different anti–double stranded DNA (dsDNA) antibody specificities using different techniques in patients testing either positive or negative for antinuclear antibodies (ANA) resulted in a “considerable discrepancy of outcomes and correlations to clinical and biochemical manifestations,” said an international team of researchers led by Dr. Michele Compagno of Lund University in Sweden.
Although anti-dsDNA antibodies are regarded as fairly specific for systemic lupus erythematosus (SLE), the pathogenic and diagnostic roles they play are still debated. It’s also unclear whether SLE represents one disease entity or is a continuous overlap of etiologically unrelated organ manifestations, making it particularly challenging to determine biomarkers for the disease, the researchers wrote (Lupus Sci. Med. 2014;1:e000007 [doi:10.1136/lupus-2013-000007]).
Dr. Compagno and her associates therefore aimed to correlate the presence of anti-dsDNA antibodies with individual clinical manifestations and laboratory variables in patients with recent-onset rheumatic symptoms, regardless of their diagnosis.
“By this approach, we aimed to reproduce the usual clinical setting, where the physician, at an early stage, is challenged to formulate a diagnosis and predict the outcome, based on clinical manifestations and suitable diagnostic tools available locally,” they wrote.
For the multicenter observational study, 292 ANA-positive and 292 sex- and age-matched ANA-negative patients were tested for different anti-dsDNA antibody specificities with assays commonly used in laboratories.
The discrepancies between outcomes and correlations to clinical phenotypes and biochemical profiles included, for example, anti-dsDNA antibodies that were associated with the presence of proteinuria, regardless of clinical diagnosis, outcome of ANA screening, and assay and technique used.
Also, in distinct subgroups of patients, the antibodies were variously associated with hematuria, leukopenia, pleuritis, and alopecia. The study results provided clinical support for Crithidia Luciliae Immunofluorescence Test (CLIFT)–determined anti-dsDNA antibodies, but only in a limited number of key SLE manifestations.
The findings also challenged the broad role of enzyme-linked immunosorbent assay–based anti-dsDNA antibody testing in diagnosis and classification of SLE, according to the investigators.
“The data support the notion that various anti-dsDNA antibodies impact differently on the classification of SLE,” they said.
“These observations raise the discussion about the performance of the various anti-dsDNA detection techniques, the general pathogenic role of the various anti-dsDNA antibodies identified, their clinical associations, and how the syndrome of SLE is currently delineated,” they concluded.
The study was supported by a variety of patient-advocacy organizations and research foundations. The study authors declared having no competing interests.
The findings of a new study challenge the importance of anti–double stranded DNA antibodies as a diagnostic hallmark for lupus.
The assessment of different anti–double stranded DNA (dsDNA) antibody specificities using different techniques in patients testing either positive or negative for antinuclear antibodies (ANA) resulted in a “considerable discrepancy of outcomes and correlations to clinical and biochemical manifestations,” said an international team of researchers led by Dr. Michele Compagno of Lund University in Sweden.
Although anti-dsDNA antibodies are regarded as fairly specific for systemic lupus erythematosus (SLE), the pathogenic and diagnostic roles they play are still debated. It’s also unclear whether SLE represents one disease entity or is a continuous overlap of etiologically unrelated organ manifestations, making it particularly challenging to determine biomarkers for the disease, the researchers wrote (Lupus Sci. Med. 2014;1:e000007 [doi:10.1136/lupus-2013-000007]).
Dr. Compagno and her associates therefore aimed to correlate the presence of anti-dsDNA antibodies with individual clinical manifestations and laboratory variables in patients with recent-onset rheumatic symptoms, regardless of their diagnosis.
“By this approach, we aimed to reproduce the usual clinical setting, where the physician, at an early stage, is challenged to formulate a diagnosis and predict the outcome, based on clinical manifestations and suitable diagnostic tools available locally,” they wrote.
For the multicenter observational study, 292 ANA-positive and 292 sex- and age-matched ANA-negative patients were tested for different anti-dsDNA antibody specificities with assays commonly used in laboratories.
The discrepancies between outcomes and correlations to clinical phenotypes and biochemical profiles included, for example, anti-dsDNA antibodies that were associated with the presence of proteinuria, regardless of clinical diagnosis, outcome of ANA screening, and assay and technique used.
Also, in distinct subgroups of patients, the antibodies were variously associated with hematuria, leukopenia, pleuritis, and alopecia. The study results provided clinical support for Crithidia Luciliae Immunofluorescence Test (CLIFT)–determined anti-dsDNA antibodies, but only in a limited number of key SLE manifestations.
The findings also challenged the broad role of enzyme-linked immunosorbent assay–based anti-dsDNA antibody testing in diagnosis and classification of SLE, according to the investigators.
“The data support the notion that various anti-dsDNA antibodies impact differently on the classification of SLE,” they said.
“These observations raise the discussion about the performance of the various anti-dsDNA detection techniques, the general pathogenic role of the various anti-dsDNA antibodies identified, their clinical associations, and how the syndrome of SLE is currently delineated,” they concluded.
The study was supported by a variety of patient-advocacy organizations and research foundations. The study authors declared having no competing interests.
The findings of a new study challenge the importance of anti–double stranded DNA antibodies as a diagnostic hallmark for lupus.
The assessment of different anti–double stranded DNA (dsDNA) antibody specificities using different techniques in patients testing either positive or negative for antinuclear antibodies (ANA) resulted in a “considerable discrepancy of outcomes and correlations to clinical and biochemical manifestations,” said an international team of researchers led by Dr. Michele Compagno of Lund University in Sweden.
Although anti-dsDNA antibodies are regarded as fairly specific for systemic lupus erythematosus (SLE), the pathogenic and diagnostic roles they play are still debated. It’s also unclear whether SLE represents one disease entity or is a continuous overlap of etiologically unrelated organ manifestations, making it particularly challenging to determine biomarkers for the disease, the researchers wrote (Lupus Sci. Med. 2014;1:e000007 [doi:10.1136/lupus-2013-000007]).
Dr. Compagno and her associates therefore aimed to correlate the presence of anti-dsDNA antibodies with individual clinical manifestations and laboratory variables in patients with recent-onset rheumatic symptoms, regardless of their diagnosis.
“By this approach, we aimed to reproduce the usual clinical setting, where the physician, at an early stage, is challenged to formulate a diagnosis and predict the outcome, based on clinical manifestations and suitable diagnostic tools available locally,” they wrote.
For the multicenter observational study, 292 ANA-positive and 292 sex- and age-matched ANA-negative patients were tested for different anti-dsDNA antibody specificities with assays commonly used in laboratories.
The discrepancies between outcomes and correlations to clinical phenotypes and biochemical profiles included, for example, anti-dsDNA antibodies that were associated with the presence of proteinuria, regardless of clinical diagnosis, outcome of ANA screening, and assay and technique used.
Also, in distinct subgroups of patients, the antibodies were variously associated with hematuria, leukopenia, pleuritis, and alopecia. The study results provided clinical support for Crithidia Luciliae Immunofluorescence Test (CLIFT)–determined anti-dsDNA antibodies, but only in a limited number of key SLE manifestations.
The findings also challenged the broad role of enzyme-linked immunosorbent assay–based anti-dsDNA antibody testing in diagnosis and classification of SLE, according to the investigators.
“The data support the notion that various anti-dsDNA antibodies impact differently on the classification of SLE,” they said.
“These observations raise the discussion about the performance of the various anti-dsDNA detection techniques, the general pathogenic role of the various anti-dsDNA antibodies identified, their clinical associations, and how the syndrome of SLE is currently delineated,” they concluded.
The study was supported by a variety of patient-advocacy organizations and research foundations. The study authors declared having no competing interests.
FROM LUPUS SCIENCE & MEDICINE
Key clinical point: Various anti-dsDNA antibodies have different effects on the classification of SLE, challenging the biomarkers role as a diagnostic hallmark for lupus.
Major finding: The assessment of anti-dsDNA antibodies using different techniques resulted in a “considerable discrepancy” in terms of outcomes and correlations to clinical and biochemical manifestations.
Data source: A multicenter observational study tested 292 ANA-positive and 292 matching ANA-negative patients for different anti-dsDNA antibody specificities with assays commonly used in laboratories.
Disclosures: The study was supported by a variety of patient-advocacy organizations and research foundations. The study authors declared having no competing interests.
Early psoriatic arthritis treatment with etanercept gives better outcomes
Patients with psoriatic arthritis and psoriasis report having a better response to etanercept the earlier they are treated, according to a post hoc analysis of the PRESTA trial.
Patients with shorter psoriatic arthritis (PsA) duration had greater improvements in arthritis scores and several patient-reported outcomes at 24 weeks of treatment with etanercept 50 mg a week, compared with patients with longer disease duration.
The researchers, led by Dr. Bruce Kirkham from Guy’s and St. Thomas’ NHS Foundation Trust, London, said the results showed “clinicians should consider treating their PsA patients with therapies effective in PsA early rather than late.”
The industry-sponsored PRESTA (Psoriasis Randomized Etanercept Study in Patients with Psoriatic Arthritis) trial was a randomized, blinded, 24-week, multicenter study enrolling adults with active but stable plaque psoriasis involving at least 10% body surface area and active PsA defined as 2 or more swollen joints, 2 or more tender joints, joint pain for 3 months or longer, and a negative serum rheumatoid factor within 6 months prior to baseline.
Overall, 372 patients who received etanercept 50 mg once a week for 24 weeks were included in the current post hoc analysis (Clin. Exp. Rheumatol. 2014 Dec. 22).
Baseline and after treatment changes were compared between patients with PsA disease duration of 2 years or less (n = 103) and those with disease more than 2 years (n = 269).
Baseline efficacy measures were similar between the shorter duration and longer duration groups, with the exception of Physicians Global Assessment (PGA) arthritis score, which was significantly lower in the group with 2 years or less duration (44.9 vs. 51.8; P = .006), the authors reported.
At week 24, joint disease improved, based on the PGA arthritis score, by a significantly greater amount in the shorter duration group (–39.8 vs. –35.7; P = .03).
Clinically meaningful improvements in patient-reported outcomes with etanercept treatment occurred in both groups, the study authors said, but changes in scores from baseline to week 24 were significantly higher in the shorter duration group for visual analog scale reports of joint pain (P = .007) and arthritis activity (P = .01) as well as quality of life on EuroQol 5D utility (P = .046) and EuroQol 5D visual analog scale (P = .04) responses.
The mean number of swollen joints that had improved from baseline to week 24 was not significantly different between the groups, and no significant between-group differences were seen in the percentages of patients achieving the ACR20, ACR50, and ACR70 responses.
While all patients responded to treatment irrespective of disease duration, patients with shorter disease duration had greater improvements on some measures, the authors concluded.
However, the study was limited by the fact that it was a post hoc analysis and the original trial was not designed to explore the effect of early treatment versus later treatment in patients with PsA and moderate-to-severe psoriasis, they noted.
The study was sponsored by Wyeth, which was acquired by Pfizer, the manufacturer of etanercept, in October 2009. Several of the authors declared receiving honoraria from several pharmaceutical companies. Two authors were employees of Pfizer during the PRESTA study and development of the current manuscript, and two other authors are current employees of Pfizer.
Patients with psoriatic arthritis and psoriasis report having a better response to etanercept the earlier they are treated, according to a post hoc analysis of the PRESTA trial.
Patients with shorter psoriatic arthritis (PsA) duration had greater improvements in arthritis scores and several patient-reported outcomes at 24 weeks of treatment with etanercept 50 mg a week, compared with patients with longer disease duration.
The researchers, led by Dr. Bruce Kirkham from Guy’s and St. Thomas’ NHS Foundation Trust, London, said the results showed “clinicians should consider treating their PsA patients with therapies effective in PsA early rather than late.”
The industry-sponsored PRESTA (Psoriasis Randomized Etanercept Study in Patients with Psoriatic Arthritis) trial was a randomized, blinded, 24-week, multicenter study enrolling adults with active but stable plaque psoriasis involving at least 10% body surface area and active PsA defined as 2 or more swollen joints, 2 or more tender joints, joint pain for 3 months or longer, and a negative serum rheumatoid factor within 6 months prior to baseline.
Overall, 372 patients who received etanercept 50 mg once a week for 24 weeks were included in the current post hoc analysis (Clin. Exp. Rheumatol. 2014 Dec. 22).
Baseline and after treatment changes were compared between patients with PsA disease duration of 2 years or less (n = 103) and those with disease more than 2 years (n = 269).
Baseline efficacy measures were similar between the shorter duration and longer duration groups, with the exception of Physicians Global Assessment (PGA) arthritis score, which was significantly lower in the group with 2 years or less duration (44.9 vs. 51.8; P = .006), the authors reported.
At week 24, joint disease improved, based on the PGA arthritis score, by a significantly greater amount in the shorter duration group (–39.8 vs. –35.7; P = .03).
Clinically meaningful improvements in patient-reported outcomes with etanercept treatment occurred in both groups, the study authors said, but changes in scores from baseline to week 24 were significantly higher in the shorter duration group for visual analog scale reports of joint pain (P = .007) and arthritis activity (P = .01) as well as quality of life on EuroQol 5D utility (P = .046) and EuroQol 5D visual analog scale (P = .04) responses.
The mean number of swollen joints that had improved from baseline to week 24 was not significantly different between the groups, and no significant between-group differences were seen in the percentages of patients achieving the ACR20, ACR50, and ACR70 responses.
While all patients responded to treatment irrespective of disease duration, patients with shorter disease duration had greater improvements on some measures, the authors concluded.
However, the study was limited by the fact that it was a post hoc analysis and the original trial was not designed to explore the effect of early treatment versus later treatment in patients with PsA and moderate-to-severe psoriasis, they noted.
The study was sponsored by Wyeth, which was acquired by Pfizer, the manufacturer of etanercept, in October 2009. Several of the authors declared receiving honoraria from several pharmaceutical companies. Two authors were employees of Pfizer during the PRESTA study and development of the current manuscript, and two other authors are current employees of Pfizer.
Patients with psoriatic arthritis and psoriasis report having a better response to etanercept the earlier they are treated, according to a post hoc analysis of the PRESTA trial.
Patients with shorter psoriatic arthritis (PsA) duration had greater improvements in arthritis scores and several patient-reported outcomes at 24 weeks of treatment with etanercept 50 mg a week, compared with patients with longer disease duration.
The researchers, led by Dr. Bruce Kirkham from Guy’s and St. Thomas’ NHS Foundation Trust, London, said the results showed “clinicians should consider treating their PsA patients with therapies effective in PsA early rather than late.”
The industry-sponsored PRESTA (Psoriasis Randomized Etanercept Study in Patients with Psoriatic Arthritis) trial was a randomized, blinded, 24-week, multicenter study enrolling adults with active but stable plaque psoriasis involving at least 10% body surface area and active PsA defined as 2 or more swollen joints, 2 or more tender joints, joint pain for 3 months or longer, and a negative serum rheumatoid factor within 6 months prior to baseline.
Overall, 372 patients who received etanercept 50 mg once a week for 24 weeks were included in the current post hoc analysis (Clin. Exp. Rheumatol. 2014 Dec. 22).
Baseline and after treatment changes were compared between patients with PsA disease duration of 2 years or less (n = 103) and those with disease more than 2 years (n = 269).
Baseline efficacy measures were similar between the shorter duration and longer duration groups, with the exception of Physicians Global Assessment (PGA) arthritis score, which was significantly lower in the group with 2 years or less duration (44.9 vs. 51.8; P = .006), the authors reported.
At week 24, joint disease improved, based on the PGA arthritis score, by a significantly greater amount in the shorter duration group (–39.8 vs. –35.7; P = .03).
Clinically meaningful improvements in patient-reported outcomes with etanercept treatment occurred in both groups, the study authors said, but changes in scores from baseline to week 24 were significantly higher in the shorter duration group for visual analog scale reports of joint pain (P = .007) and arthritis activity (P = .01) as well as quality of life on EuroQol 5D utility (P = .046) and EuroQol 5D visual analog scale (P = .04) responses.
The mean number of swollen joints that had improved from baseline to week 24 was not significantly different between the groups, and no significant between-group differences were seen in the percentages of patients achieving the ACR20, ACR50, and ACR70 responses.
While all patients responded to treatment irrespective of disease duration, patients with shorter disease duration had greater improvements on some measures, the authors concluded.
However, the study was limited by the fact that it was a post hoc analysis and the original trial was not designed to explore the effect of early treatment versus later treatment in patients with PsA and moderate-to-severe psoriasis, they noted.
The study was sponsored by Wyeth, which was acquired by Pfizer, the manufacturer of etanercept, in October 2009. Several of the authors declared receiving honoraria from several pharmaceutical companies. Two authors were employees of Pfizer during the PRESTA study and development of the current manuscript, and two other authors are current employees of Pfizer.
FROM CLINICAL AND EXPERIMENTAL RHEUMATOLOGY
Key clinical point: PsA treatment with etanercept within 2 years of diagnosis may lead to better patient-reported quality of life outcomes than does treatment starting more than 2 years after diagnosis.
Major finding: After 24 weeks of etanercept 50 mg per week, joint disease improved, based on the PGA arthritis score, by a significantly greater amount in patients with PsA for 2 years or less vs. those with the disease for more than 2 years (–39.8 vs. –35.7, respectively; P = .03) .
Data source: A post hoc analysis of 372 patients with PsA and psoriasis who were enrolled in the PRESTA trial.
Disclosures: The study was sponsored by Wyeth, which was acquired by Pfizer, the manufacturer of etanercept, in October 2009. Several of the authors declared receiving honoraria from several pharmaceutical companies. Two authors were employees of Pfizer during the PRESTA study and development of the current manuscript, and two other authors are current employees of Pfizer.
RA clinical remission possible with half etanercept dose
Maintaining clinical remission with half-dose etanercept is possible for many rheumatoid arthritis patients, according to a single-center, prospective cohort study.
Over 80% of rheumatoid arthritis (RA) patients in remission who were randomized to a half dose treatment of 25 mg of etanercept per week were still in remission after an average follow-up period of 3.6 years, Dr. Bernd Raffeiner and his colleagues at the University of Padova (Italy) reported (Clin. Exp. Rheumatol. 2014 Dec. 22).
The study randomized 323 RA patients to etanercept 25 mg weekly (group A, n = 159) or etanercept 25 mg bi-weekly (group B, n = 164). The patients had a mean age of 56 years and about 82% were female. had failed traditional synthetic disease-modifying antirheumatic drugs and then achieved remission on etanercept 25 mg bi-weekly (50 mg per week). The investigators defined remission as a 28-joint disease activity score using erythrocyte sedimentation rate of less than 2.6 for at least 12 months.
At the end of follow-up, 81.8% of the patients in group A maintained remission for a mean of 3.6 years.
These patients were slightly younger than those who failed dose reduction and were taking fewer nonsteroidal anti-inflammatory drugs. Disease activity prior to biologic therapy did not influence response to half-dose etanercept.
The data showed that half-dose etanercept halted radiographic damage as effectively as standard dose, the researchers said. About 80% of patients reached radiographic remission, and almost 20% showed minor radiographic changes. Just 1.5% of patients experienced a relevant progression among all groups.
Patients who flared during dose reduction and returned to full dose did not show a greater radiographic progression.
“Low dose etanercept seems to prevent radiographic damage even if full clinical response is not achieved,” they wrote.
Furthermore, most (75.9%) of the patients who went back onto full-dose treatment regained remission.
Etanercept has unique pharmacokinetics and pharmacodynamics that are different from other TNF-α inhibitors, which could make it more suitable for dose adjustment, the study authors suggested.
The findings have important economic implications, they said. In Italy, low-dose etanercept is the lowest priced biologic treatment protocol available that meets the present standards in RA therapy.
“The resources gained could be invested for candidate patients for TNF-α inhibitor or other biologic therapy, especially in situations where policy maker intervention sets limitations to contain ever more increasing healthcare costs,” they wrote.
There were no conflicts of interest declared.
Maintaining clinical remission with half-dose etanercept is possible for many rheumatoid arthritis patients, according to a single-center, prospective cohort study.
Over 80% of rheumatoid arthritis (RA) patients in remission who were randomized to a half dose treatment of 25 mg of etanercept per week were still in remission after an average follow-up period of 3.6 years, Dr. Bernd Raffeiner and his colleagues at the University of Padova (Italy) reported (Clin. Exp. Rheumatol. 2014 Dec. 22).
The study randomized 323 RA patients to etanercept 25 mg weekly (group A, n = 159) or etanercept 25 mg bi-weekly (group B, n = 164). The patients had a mean age of 56 years and about 82% were female. had failed traditional synthetic disease-modifying antirheumatic drugs and then achieved remission on etanercept 25 mg bi-weekly (50 mg per week). The investigators defined remission as a 28-joint disease activity score using erythrocyte sedimentation rate of less than 2.6 for at least 12 months.
At the end of follow-up, 81.8% of the patients in group A maintained remission for a mean of 3.6 years.
These patients were slightly younger than those who failed dose reduction and were taking fewer nonsteroidal anti-inflammatory drugs. Disease activity prior to biologic therapy did not influence response to half-dose etanercept.
The data showed that half-dose etanercept halted radiographic damage as effectively as standard dose, the researchers said. About 80% of patients reached radiographic remission, and almost 20% showed minor radiographic changes. Just 1.5% of patients experienced a relevant progression among all groups.
Patients who flared during dose reduction and returned to full dose did not show a greater radiographic progression.
“Low dose etanercept seems to prevent radiographic damage even if full clinical response is not achieved,” they wrote.
Furthermore, most (75.9%) of the patients who went back onto full-dose treatment regained remission.
Etanercept has unique pharmacokinetics and pharmacodynamics that are different from other TNF-α inhibitors, which could make it more suitable for dose adjustment, the study authors suggested.
The findings have important economic implications, they said. In Italy, low-dose etanercept is the lowest priced biologic treatment protocol available that meets the present standards in RA therapy.
“The resources gained could be invested for candidate patients for TNF-α inhibitor or other biologic therapy, especially in situations where policy maker intervention sets limitations to contain ever more increasing healthcare costs,” they wrote.
There were no conflicts of interest declared.
Maintaining clinical remission with half-dose etanercept is possible for many rheumatoid arthritis patients, according to a single-center, prospective cohort study.
Over 80% of rheumatoid arthritis (RA) patients in remission who were randomized to a half dose treatment of 25 mg of etanercept per week were still in remission after an average follow-up period of 3.6 years, Dr. Bernd Raffeiner and his colleagues at the University of Padova (Italy) reported (Clin. Exp. Rheumatol. 2014 Dec. 22).
The study randomized 323 RA patients to etanercept 25 mg weekly (group A, n = 159) or etanercept 25 mg bi-weekly (group B, n = 164). The patients had a mean age of 56 years and about 82% were female. had failed traditional synthetic disease-modifying antirheumatic drugs and then achieved remission on etanercept 25 mg bi-weekly (50 mg per week). The investigators defined remission as a 28-joint disease activity score using erythrocyte sedimentation rate of less than 2.6 for at least 12 months.
At the end of follow-up, 81.8% of the patients in group A maintained remission for a mean of 3.6 years.
These patients were slightly younger than those who failed dose reduction and were taking fewer nonsteroidal anti-inflammatory drugs. Disease activity prior to biologic therapy did not influence response to half-dose etanercept.
The data showed that half-dose etanercept halted radiographic damage as effectively as standard dose, the researchers said. About 80% of patients reached radiographic remission, and almost 20% showed minor radiographic changes. Just 1.5% of patients experienced a relevant progression among all groups.
Patients who flared during dose reduction and returned to full dose did not show a greater radiographic progression.
“Low dose etanercept seems to prevent radiographic damage even if full clinical response is not achieved,” they wrote.
Furthermore, most (75.9%) of the patients who went back onto full-dose treatment regained remission.
Etanercept has unique pharmacokinetics and pharmacodynamics that are different from other TNF-α inhibitors, which could make it more suitable for dose adjustment, the study authors suggested.
The findings have important economic implications, they said. In Italy, low-dose etanercept is the lowest priced biologic treatment protocol available that meets the present standards in RA therapy.
“The resources gained could be invested for candidate patients for TNF-α inhibitor or other biologic therapy, especially in situations where policy maker intervention sets limitations to contain ever more increasing healthcare costs,” they wrote.
There were no conflicts of interest declared.
FROM CLINICAL AND EXPERIMENTAL RHEUMATOLOGY
Key clinical point: Half dose etanercept halts radiographic damage in RA as effectively as standard dose.
Major finding: A large majority (81.8%) of RA patients stayed in remission on half-dose etanercept (25 mg weekly).
Data source: A single-center, prospective, long-term follow-up study of 524 biologic-naïve RA patients who were randomized to half-dose etanercept (25 mg weekly) or 25 mg bi-weekly.
Disclosures: None declared.
Microbiota Organization Influences Colorectal Cancers
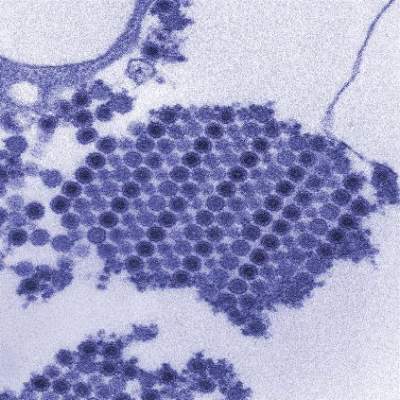
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Microbiota organization influences colorectal cancers
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
The way in which microbial communities are organized in the mucosa of the colon could be a critical factor in the development of some colorectal cancers, researchers said.
The presence of bacterial biofilms – collections of microbial communities encased in a polymeric matrix – was associated with a fivefold higher risk of developing colorectal cancer, compared with individuals without biofilms, the international team of researchers reported in the Proceedings of the National Academy of Sciences.
Writing in background information to their paper, Christine M. Dejea of the departments of microbiology and immunology at the Johns Hopkins Medical Institutions, Baltimore, and associates noted that biofilms characterize many chronic mucosal diseases like inflammatory bowel disease, otitis media, and rhinosinusitus. Until now, however, they haven’t been associated with colorectal cancer (Proc. Natl. Acad. Sci. U. S. A. 2015;111:18321-26).
The researchers systematically studied healthy and cancerous tissue biopsies from 118 people who were undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
They identified invasive polymicrobial bacterial biofilms structures on 89% of right-side tumors (13 of 15 CRCs, 4 of 4 adenomas) and 12% of left-side tumors (2 of 15 CRCs, 0 of 2 adenomas).
Patients with biofilm-positive tumors, whether they were CRCs or adenomas, all had biofilms on their tumor-free mucosa far distant from their tumors. None of the normal mucosa from patients with biofilm-negative CRCs possessed a biofilm, the investigators said.
Biofilm formation in both the colon cancer host and healthy subjects was associated with a reduced or redistributed colonic epithelial cell E-cadherin, consistent with increased epithelial permeability.
The inflammatory marker IL-6 also was enhanced with biofilm formation, even in healthy patients without CRC, suggesting that early biofilm formation can initiate procarcinogenic tissue inflammation, the researchers said.
“Our data support a model whereby biofilm formation enhances epithelial permeability that increases direct access of bacterial antigens/mutagens to an unshielded epithelial surface and promotes procarcinogenic tissue inflammation,” they wrote.
The findings also introduce the concept that the organization, as opposed to the composition per se, of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon, they said.
The authors speculated “that colorectal cancers develop in two different settings: individuals with biofilms and individuals without them.”
“Based on the data described here, the risk of developing CRC is more than fivefold higher in the patients with biofilms compared with those without biofilms,” they wrote.
The study authors suggest that the new findings could be used to develop a noninvasive test that detects these biofilms.
Probiotic therapies also could potentially eliminate them, they said.
The National Institutes of Health supported the study. The authors declared no conflicts of interest.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Key clinical point: The organization of the mucosa-associated microbial community is an important factor in CRC pathogenesis, particularly in the proximal colon.
Major finding: The risk of developing CRC is more than fivefold higher in patients with biofilms, compared with those without biofilms.
Data source: Systematic study of the biopsies of 118 people undergoing surgery or colonoscopy at the Johns Hopkins Hospital or the University of Malaya Medical Centre in Kuala Lumpur, Malaysia.
Disclosures: The National Institutes of Health supported the study. The authors declared no conflicts of interest.