User login
Prostate Cancer More Likely to Recur, Kill Men Who Smoke at Diagnosis
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
FROM JAMA
Major Finding: Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Data Source: A prospective, observational study of 5,366 men diagnosed with prostate cancer in the Health Professionals Follow-Up Study,
Disclosures: The authors reported they had no conflicts of interest.
Prostate Cancer More Likely to Recur, Kill Men Who Smoke at Diagnosis
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
FROM JAMA
Major Finding: Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Data Source: A prospective, observational study of 5,366 men diagnosed with prostate cancer in the Health Professionals Follow-Up Study,
Disclosures: The authors reported they had no conflicts of interest.
Prostate Cancer More Likely to Recur, Kill Men Who Smoke at Diagnosis
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
Men who smoke at the time of prostate cancer diagnosis have substantially increased rates of overall mortality and prostate cancer mortality and biochemical recurrence compared with men who had never smoked, according to a prospective, observational study of a large database.
Early quitting was associated with better outcomes, however, as the analysis shows that men who stopped smoking more than 10 years before diagnosis had prostate cancer mortality and recurrence risks similar to those in men who had never smoked.
"These results provide further support that smoking may increase risk of death from prostate cancer," the authors concluded in a report of their findings in JAMA.
Analysis of data on 5,366 men diagnosed with prostate cancer between 1986 and 2006 shows a 61% increase in prostate cancer mortality and biochemical recurrence in current smokers compared with those who had never smoked. Current smokers also had more than a twofold increase in total mortality risk and risk of mortality from cardiovascular disease (CVD).
"We weren’t surprised," said Stacey Kenfield, Sc.D., lead author of the study; previous but much smaller studies had shown the association.
"What was interesting was that the association between smoking and prostate cancer death and recurrence was exactly the same. These data taken together provide further support that smoking may lead to prostate cancer progression," Dr. Kenfield, a research associate in the department of epidemiology at Harvard School of Public Health, Boston, said in an interview.
Asked to comment, Dr. Judd W. Moul, chief of the division of urologic surgery at Duke University Medical Center, Durham, N.C., called the findings "very interesting."
"From a practical standpoint, it’s more of the same, that smoking is bad for your health. Here’s another study that smoking leads to adverse outcomes when a man is diagnosed with prostate cancer," he said.
"We see younger and younger men diagnosed with prostate cancer as a result of screening," added Dr. Moul. "If we run across a younger man, this study shows that they should quit immediately. We also need to take a more active role in men’s health issues, and help them with smoking cessation."
The researchers analyzed data from the Health Professionals Follow-Up Study, a prospective cohort study of 51,529 male health professionals in the United States who completed a questionnaire when enrolled in 1986. The participants were assessed every 2 years for 22 years until January 2008.
For the study, 5,366 men diagnosed with prostate cancer were included in the analysis based on the fact that they were free of a cancer diagnosis (except nonmelanoma skin cancer) in 1986, and that they had provided information on their smoking status before prostate cancer diagnosis.
The primary outcomes for the analysis were prostate cancer mortality and biochemical recurrence, according to the study. Secondary outcomes were total and CVD mortality. Median follow-up was 8.1 years in the mortality analysis and 3.8% in the recurrence analysis, which did not include men with metastatic disease at diagnosis.
In all, 32% (524) died due to prostate cancer and 26% (416) due to CVD. There were 878 biochemical recurrences. Other cancer was the most common other cause of death, occurring in 19.5%.
Using current smokers as the reference group, researchers found that former smokers overall did not have an increased risk of prostate cancer death and recurrence when compared to never smokers. The study then divided the participants by years since they had quit smoking and by dose as expressed in pack years (multiplying years of smoking by average number of packs smoked per day).
The analysis showed that former smokers who had quit at least 10 years prior to the diagnosis had risks similar to never-smokers – as did former smokers who had quit less than 10 years prior and had smoked less than 20 pack years. But in men who had quit less than 10 years prior to diagnosis, and had 20 or more pack years, the risks of prostate cancer mortality and recurrence were similar to these risks in current smokers.
"It makes total sense. If you smoked a lot, you should quit as soon as possible. If you smoked a lot, you won’t see a benefit for 10 years after quitting," said Dr. Kenfield.
The results also showed that compared with never-smokers, current smokers had a higher stage and grade of prostate cancer. Nearly 15% of current smokers had stage T3 or higher at the time of diagnosis, vs. 8.3% of never smokers. And 16% of current smokers had a Gleason score of 7 or more vs. 10.7% of never smokers.
The analysis also shows that current smokers made unhealthier lifestyle choices: They exercised less, drank more coffee, and had a higher intake of saturated fat and lower intake of calcium than never or former smokers. Smokers – both former and current – consumed more alcohol, but their body mass index was similar to the BMI of never smokers.
The mortality data showed a "statistically significant difference in overall survival across smoking status," at 5 and 10 years after diagnosis, the authors wrote (JAMA 2011;305:2548-2555).
Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were slightly lower at 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Although some studies have suggested that smokers tend to have less PSA testing and may be diagnosed at a more advanced stage, the "differential PSA screening across strata of smoking status was unlikely to fully account for our results," wrote the authors, because the percentage of men who had at least one PSA test before their diagnosis varied little among the three groups.
The authors added that direct effect of smoking on prostate cancer progression "is biologically plausible." They proposed four hypotheses: tumor promotion through carcinogens from tobacco smoke, increased plasma levels of total and free testosterone, epigenetic effects such as aberrant methylation profiles, and "nicotine-induced angiogenesis, capillary growth, and tumor growth and proliferation."
"There are very few factors that are known to increase or decrease risk of progression of prostate cancer. My goal is to find out what’s related to the rate of prostate cancer progression and what men can do to improve their chances of survival with prostate cancer," said Dr. Kenfield.
The authors reported they had nothing to disclose.
FROM JAMA
Major Finding: Among never smokers, 89.7% were alive 5 years after diagnosis and 74.8% at 10 years; among former smokers, survival rates were 86.2% and 68.2%, respectively. Among current smokers they fell to 78.8% and 54.8%, respectively.
Data Source: A prospective, observational study of 5,366 men diagnosed with prostate cancer in the Health Professionals Follow-Up Study,
Disclosures: The authors reported they had no conflicts of interest.
Obesity May Affect Levonorgestrel Intrauterine System Efficacy in Treating Menorrhagia
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Data Source: A retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009.
Disclosures: Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
Obesity May Affect Levonorgestrel Intrauterine System Efficacy in Treating Menorrhagia
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
WASHINGTON – In very obese women, treatment of menorrhagia with levonorgestrel intrauterine system may be slightly less effective, but the treatment’s success rate justifies its use, according to a study conducted by researchers at the University of Michigan.
In addition, levonorgestrel intrauterine system (LNG-IUS) "may be an especially important treatment choice for women at high surgical risk," the authors reported.
Although studies have shown the effectiveness of LNG-IUS in treatment of menorrhagia, most have not considered the role of body mass index (BMI), said Ms. Paige C. Fairchild, a medical student at the university who presented the study at the annual meeting of the American College of Obstetricians and Gynecologists.
The team conducted a retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009 within the University of Michigan Health System, Ann Arbor. Nearly 50% had BMI of 30 kg/m2 or greater; 25% had BMI of 35 or greater. Treatment failure was defined as removal of LNG-IUS for continued menorrhagia, need for additional treatment, or expulsion. Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Also, removal of LNG-IUS because of continued menorrhagia was more common among women who had BMI greater than 34, compared with those in all BMI groups (6.9% vs. 4.1%).
The odds of surgery within 2 years of LNG-IUS removal also was higher in obese patients (2.6 times), compared with other groups.
Some factors that might contribute to the reduced effectiveness of LNG-IUS in obese women are larger uterus, persistent unopposed estrogen endometrial stimulation, or poor placement/difficulty in achieving fundal placement, Dr. Vanessa Dalton of the department of obstetrics and gynecology at the university and one of the study authors said in an interview.
Despite the findings, the authors concluded that the high continuation rates of LNG-IUS and low surgery rates indicate that the treatment is still a good option for women with a high BMI.
One of the limitations of the study was that it was observational and "that cannot assess details about decision-making. It is possible that providers are more likely to recommend surgical treatment for obese women than [for] normal weight women," Dr. Dalton said.
"Additional analysis is ongoing to further characterize predictors of treatment failure," she added.
Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Continued menorrhagia was uncommon in all BMI groups, but it was most common in women with BMI greater than 34 kg/m2, compared with those in all BMI groups (6.9% vs. 3.3%).
Data Source: A retrospective chart review of 398 women with menorrhagia who were treated with LNG-IUS between 1999 and 2009.
Disclosures: Ms. Fairchild and Dr. Dalton said that they had no relevant financial disclosures.
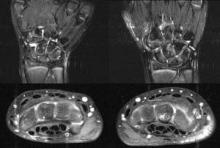
Unguided Intra-Articular Injections of Betamethasone Safe, Effective
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Unguided Intra-Articular Injections of Betamethasone Safe, Effective
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
Unguided intra-articular injection of betamethasone in small and large peripheral joints in patients with early rheumatoid arthritis results in rapid, effective, and long-lasting inflammatory control when used in combination with systemic medication, according to findings from a 2-year "treat to target" study.
Dr. Merete Lund Hetland, an associate professor at the University of Copenhagen and consultant in rheumatology, said in an interview that "unguided intra-articular injections should be used much more in routine care of early RA, not only in the large joints, but also in smaller joints such as proximal interphalangeal and metacarpophalangeal joints.
"The study was a ‘treat-to-target’ study, aiming at complete inflammatory control [that is, no swollen joints] using conventional DMARDs [disease-modifying antirheumatic drugs] together with intra-articular injections with betamethasone," she added.
The results are part of the CIMESTRA (Cyclosporine, Methotrexate, Steroid in RA) trial, which showed that "continuous methotrexate and intra-articular corticosteroid treatment resulted in excellent clinical response and disease control at 2 years, and the radiographic erosive progression was minimal" (Ann. Rheum. Dis. 2008;67:815-22; Arthritis Rheum. 2006;54:1401-9
The study investigated the short- and long-term efficacy of unguided intra-articular injections with betamethasone. Investigators determined the effect of repeated injections on pathology visible on MRI, anti–cyclic citrullinated peptide (anti-CCP) antibodies, and IgM-rheumatoid factor status.
For the study, 160 patients with early RA (duration less than 6 months) received intra-articular betamethasone in a maximum of four swollen joints at each visit. They received the injections at 2-week intervals for 8 weeks, then every 4 weeks in combination with step-up DMARDs during 2 years.
In all, 1,373 unique joints, including wrists, knees, shoulders, ankles, elbows, metacarpophalangeal (MCP) joints, and proximal interphalangeal (PIP) joints, were injected; 531 joints were injected a second time, and 262 a third time.
The patients were treated with methotrexate as monotherapy or in combination with cyclosporine.
Short-term efficacy was assessed by EULAR good-response criteria. Long-term efficacy was assessed by Kaplan-Meier plots of joint-injection survival.
After the first year, 62.3% of the joints that were injected at baseline had not relapsed. After 2 years, 55.5% of the injected joints had not relapsed. All joint areas had good 2-year joint injection survival, which was highest for the PIP joints (73.7%). The 2-year joint response was higher for first injections (56.6%) than for second (43.4%) and third injections (31.3%).
The average total dosage of betamethasone injected after 2 years was 11 mL.
Adverse events were mild and transient, with injections being well tolerated.
A high MRI synovitis score for MCP joints and anti-CCP negativity were associated with poorer joint-injection survival, whereas C-reactive protein and IgM-RF were not, according to the study.
Limitations of the study included the fact that "patients also were treated with DMARDs. Thus, after 6-8 weeks, the effect of DMARD treatment intermingled with the effect of steroids. However, this also reflects real-life practice," said Dr. Hetland.
A new study is underway in which they will investigate "the efficacy of joint injections in patients with early RA receiving TNF [tumor necrosis factor] inhibitor treatment," she added.
"We expect to present 1-year data at the ACR [in Chicago in 2011]."
The study was funded by the Danish Arthritis Foundation. Novartis, Pfizer, and MSD Pharmaceuticals provided study drugs and an independent Good Clinical Practice monitor. Dr. Hetland has received grants and/or honoraria from the Danish Arthritis Association, Abbott, Pfizer, Bristol-Myers Squibb, MSD, UCB, and Roche.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Policy & Practice : Want more health reform news? Subscribe to our podcast – search 'Policy & Practice' in the iTunes store
ADA Offers Research Grants
The American Diabetes Association and device maker Medtronic are offering grants for research into online diabetes-management tools, including the company's CoreLink database. Researcher will have access to CoreLink – which contains anonymous data from more 200,000 people with diabetes – to examine the impact of management technology on clinical outcomes, compliance, and various factors that affect glycemic control in patients taking insulin. “In the long run, this research can help influence future diabetes technology and shape how we educate people with diabetes,” said Dr. Robert R. Henry, president for medicine and science at the association.
Thyroid Group Urges More Free KI
Following the catastrophe at Japan's Fukushima Nuclear Plant, the American Thyroid Association has reissued its call for free potassium iodide for states and local governments to distribute to residents living within 20 miles of nuclear plants, not just 10 miles. The association asserted that the Bioterrorism Preparedness and Response Act of 2002 directed the president to implement the wider distribution but that neither President Bush nor President Obama had done so. “The 1986 Chernobyl accident illustrated how Poland (about 200 miles from Chernobyl) was the only country to distribute [potassium iodide] to its population and was the only radiation exposed country that did not have an increase in the subsequent development of thyroid nodules and thyroid cancer,” according to an association statement. Rep. Edward Markey (D-Mass.) has also sent a letter to the White House, urging the president to implement the program.
You Too Can Fight Obesity
The nonprofit group National Initiative for Children's Healthcare Quality has begun recruiting community teams to its Healthy Weight Collaborative to fight obesity. The program is funded by $5 million from the Affordable Care Act's prevention fund. In the first phase of the collaborative, the group is recruiting 10 teams that can be made up of physicians and public health leaders. The second phase of the program will launch in December and will include about 40 more teams. Teams are to help “develop practical approaches that link primary care, public health, and communities to prevent and treat obesity for children and families, according to the initiative's website. For more information, visit
www.collaborateforhealthyweight.org
McDonald's: Ronald is Golden
McDonald's Corp. will continue to use mascot Ronald McDonald to advertise Happy Meals to children despite calls for the fast food giant to cut the clown to help reduce childhood obesity, company CEO Jim Skinner told a shareholders' meeting. Mr. Skinner spoke in answer to a challenge by Donald Zeigler, Ph.D., the American Medical Association's director of prevention and healthy lifestyles, in a statement presented at the meeting. “Changing course now and ending marketing to kids … would have a profound impact on McDonald's reputation and the health and well-being of generations to come throughout the world,” Dr. Zeigler said. Mr. Skinner countered that the marketing strategy has yielded profits. “This is about the personal and individual right to choose,” he said.
CME-Funding Dilemma Persists
Although physicians and other medical professionals say they're concerned that commercial funding of continuing medical education may bias the information provided, most are not willing to pay more to offset or eliminate such funding, a study in Archives of Internal Medicine shows. Researchers surveyed 770 physicians, nurses, nurse practitioners, and physician assistants at CME sessions and found that the vast majority (88%) said that commercial support of CME introduces bias. However, only 15% would eliminate commercial support from CME activities and only 42% said they were willing to pay more in an effort to cut industry financial involvement. Most CME participants also significantly underestimated the amount of commercial funding for their courses, the authors wrote, adding that “the dilemma remains of how to provide quality CME either with [alternative funding] or at reduced cost.”
ADA Offers Research Grants
The American Diabetes Association and device maker Medtronic are offering grants for research into online diabetes-management tools, including the company's CoreLink database. Researcher will have access to CoreLink – which contains anonymous data from more 200,000 people with diabetes – to examine the impact of management technology on clinical outcomes, compliance, and various factors that affect glycemic control in patients taking insulin. “In the long run, this research can help influence future diabetes technology and shape how we educate people with diabetes,” said Dr. Robert R. Henry, president for medicine and science at the association.
Thyroid Group Urges More Free KI
Following the catastrophe at Japan's Fukushima Nuclear Plant, the American Thyroid Association has reissued its call for free potassium iodide for states and local governments to distribute to residents living within 20 miles of nuclear plants, not just 10 miles. The association asserted that the Bioterrorism Preparedness and Response Act of 2002 directed the president to implement the wider distribution but that neither President Bush nor President Obama had done so. “The 1986 Chernobyl accident illustrated how Poland (about 200 miles from Chernobyl) was the only country to distribute [potassium iodide] to its population and was the only radiation exposed country that did not have an increase in the subsequent development of thyroid nodules and thyroid cancer,” according to an association statement. Rep. Edward Markey (D-Mass.) has also sent a letter to the White House, urging the president to implement the program.
You Too Can Fight Obesity
The nonprofit group National Initiative for Children's Healthcare Quality has begun recruiting community teams to its Healthy Weight Collaborative to fight obesity. The program is funded by $5 million from the Affordable Care Act's prevention fund. In the first phase of the collaborative, the group is recruiting 10 teams that can be made up of physicians and public health leaders. The second phase of the program will launch in December and will include about 40 more teams. Teams are to help “develop practical approaches that link primary care, public health, and communities to prevent and treat obesity for children and families, according to the initiative's website. For more information, visit
www.collaborateforhealthyweight.org
McDonald's: Ronald is Golden
McDonald's Corp. will continue to use mascot Ronald McDonald to advertise Happy Meals to children despite calls for the fast food giant to cut the clown to help reduce childhood obesity, company CEO Jim Skinner told a shareholders' meeting. Mr. Skinner spoke in answer to a challenge by Donald Zeigler, Ph.D., the American Medical Association's director of prevention and healthy lifestyles, in a statement presented at the meeting. “Changing course now and ending marketing to kids … would have a profound impact on McDonald's reputation and the health and well-being of generations to come throughout the world,” Dr. Zeigler said. Mr. Skinner countered that the marketing strategy has yielded profits. “This is about the personal and individual right to choose,” he said.
CME-Funding Dilemma Persists
Although physicians and other medical professionals say they're concerned that commercial funding of continuing medical education may bias the information provided, most are not willing to pay more to offset or eliminate such funding, a study in Archives of Internal Medicine shows. Researchers surveyed 770 physicians, nurses, nurse practitioners, and physician assistants at CME sessions and found that the vast majority (88%) said that commercial support of CME introduces bias. However, only 15% would eliminate commercial support from CME activities and only 42% said they were willing to pay more in an effort to cut industry financial involvement. Most CME participants also significantly underestimated the amount of commercial funding for their courses, the authors wrote, adding that “the dilemma remains of how to provide quality CME either with [alternative funding] or at reduced cost.”
ADA Offers Research Grants
The American Diabetes Association and device maker Medtronic are offering grants for research into online diabetes-management tools, including the company's CoreLink database. Researcher will have access to CoreLink – which contains anonymous data from more 200,000 people with diabetes – to examine the impact of management technology on clinical outcomes, compliance, and various factors that affect glycemic control in patients taking insulin. “In the long run, this research can help influence future diabetes technology and shape how we educate people with diabetes,” said Dr. Robert R. Henry, president for medicine and science at the association.
Thyroid Group Urges More Free KI
Following the catastrophe at Japan's Fukushima Nuclear Plant, the American Thyroid Association has reissued its call for free potassium iodide for states and local governments to distribute to residents living within 20 miles of nuclear plants, not just 10 miles. The association asserted that the Bioterrorism Preparedness and Response Act of 2002 directed the president to implement the wider distribution but that neither President Bush nor President Obama had done so. “The 1986 Chernobyl accident illustrated how Poland (about 200 miles from Chernobyl) was the only country to distribute [potassium iodide] to its population and was the only radiation exposed country that did not have an increase in the subsequent development of thyroid nodules and thyroid cancer,” according to an association statement. Rep. Edward Markey (D-Mass.) has also sent a letter to the White House, urging the president to implement the program.
You Too Can Fight Obesity
The nonprofit group National Initiative for Children's Healthcare Quality has begun recruiting community teams to its Healthy Weight Collaborative to fight obesity. The program is funded by $5 million from the Affordable Care Act's prevention fund. In the first phase of the collaborative, the group is recruiting 10 teams that can be made up of physicians and public health leaders. The second phase of the program will launch in December and will include about 40 more teams. Teams are to help “develop practical approaches that link primary care, public health, and communities to prevent and treat obesity for children and families, according to the initiative's website. For more information, visit
www.collaborateforhealthyweight.org
McDonald's: Ronald is Golden
McDonald's Corp. will continue to use mascot Ronald McDonald to advertise Happy Meals to children despite calls for the fast food giant to cut the clown to help reduce childhood obesity, company CEO Jim Skinner told a shareholders' meeting. Mr. Skinner spoke in answer to a challenge by Donald Zeigler, Ph.D., the American Medical Association's director of prevention and healthy lifestyles, in a statement presented at the meeting. “Changing course now and ending marketing to kids … would have a profound impact on McDonald's reputation and the health and well-being of generations to come throughout the world,” Dr. Zeigler said. Mr. Skinner countered that the marketing strategy has yielded profits. “This is about the personal and individual right to choose,” he said.
CME-Funding Dilemma Persists
Although physicians and other medical professionals say they're concerned that commercial funding of continuing medical education may bias the information provided, most are not willing to pay more to offset or eliminate such funding, a study in Archives of Internal Medicine shows. Researchers surveyed 770 physicians, nurses, nurse practitioners, and physician assistants at CME sessions and found that the vast majority (88%) said that commercial support of CME introduces bias. However, only 15% would eliminate commercial support from CME activities and only 42% said they were willing to pay more in an effort to cut industry financial involvement. Most CME participants also significantly underestimated the amount of commercial funding for their courses, the authors wrote, adding that “the dilemma remains of how to provide quality CME either with [alternative funding] or at reduced cost.”
Policy & Practice : Want more health reform news? Subscribe to our podcast – search 'Policy & Practice' in the iTunes store
Headaches Take a Toll …
Headaches were the main cause of 3 million emergency department visits and 81,000 hospital stays in the United States, according to an analysis of 2008 data by the Agency for Healthcare Research and Quality. Those figures represented 2.4% of ED visits and 0.2% of hospitalizations, respectively. Migraines made up one-third of the headache emergencies and two-thirds of the hospital stays for headaches. The ED visits increased during the summer months, peaked in September, and were lowest during February and December. Three-fourths of the headache sufferers were women, who also were four times more likely to have migraines than were men. People in low-income and rural communities were more likely than their counterparts to visit EDs for headaches.
… While They're Under-Diagnosed
Headaches are under-recognized, under-diagnosed, and under-treated worldwide, according to the World Health Organization. “Health-care providers need better knowledge of how to diagnose and treat the small number of headache disorders that contribute substantially to public ill-health,” according to the “Atlas of Headache Disorders and Resources in the World 2011” compiled by the WHO and the group Lifting the Burden. Only about 40% of patients with migraines or tension-type headaches are professionally diagnosed, according to the report. About half of the people with headaches treat themselves without contacting a health care professional. Regardless of national wealth, many countries cited the unavailability of appropriate headache drugs as a barrier to care. The researchers studied epidemiologic data and answers on questionnaires completed by neurologists, general practitioners, and patients in 101 countries.
Group Decries Alzheimer's Test
The watchdog group Public Citizen has challenged a recent JAMA report of success with a radioactive dye for detecting beta-amyloid plaques by positron-emission tomography (PET). The dye maker's study in January concluded that PET with florbetapir F 18 can indicate the presence and density of the plaques associated with Alzheimer's disease. In a letter to the journal, Public Citizen claimed that the authors withheld “critically important data,” and it urged the Food and Drug Administration not to approve the dye. “In their JAMA article, the researchers presented only the median score of the three physician readers for the amount of beta-amyloid seen on each florbetapir-PET scan, but withheld critical data on the scores for each individual physician reader,” the group said in a statement. Also in January, the FDA withheld approval of the dye pending additional data on reliability between florbetapir-PET scan readers.
A $212 Million Botox Verdict
A Virginia jury voted to award $212 million to a man who said he sustained permanent brain damage after receiving injections of Botox for tremors in his hand. Douglas M. Ray alleged that Allergan Inc. had failed to properly warn of all of Botox's inherent dangers, including the autoimmune disorder he developed after the injections. In a statement, a company spokeswoman said that “the facts, data and qualified expert testimony in this case established that there is no evidence to suggest Allergan failed to make available adequate information to Mr. Ray's treating physician about the potential risks associated with Botox. Nor was there any proof that Botox caused the symptoms suffered by Mr. Ray.” Although the jury said Mr. Ray should get $212 million, $200 million of that – the punitive damages portion – will be capped at $350,000 under Virginia law. Allergan is “currently evaluating the basis for an appeal,” a spokeswoman said.
Headaches Take a Toll …
Headaches were the main cause of 3 million emergency department visits and 81,000 hospital stays in the United States, according to an analysis of 2008 data by the Agency for Healthcare Research and Quality. Those figures represented 2.4% of ED visits and 0.2% of hospitalizations, respectively. Migraines made up one-third of the headache emergencies and two-thirds of the hospital stays for headaches. The ED visits increased during the summer months, peaked in September, and were lowest during February and December. Three-fourths of the headache sufferers were women, who also were four times more likely to have migraines than were men. People in low-income and rural communities were more likely than their counterparts to visit EDs for headaches.
… While They're Under-Diagnosed
Headaches are under-recognized, under-diagnosed, and under-treated worldwide, according to the World Health Organization. “Health-care providers need better knowledge of how to diagnose and treat the small number of headache disorders that contribute substantially to public ill-health,” according to the “Atlas of Headache Disorders and Resources in the World 2011” compiled by the WHO and the group Lifting the Burden. Only about 40% of patients with migraines or tension-type headaches are professionally diagnosed, according to the report. About half of the people with headaches treat themselves without contacting a health care professional. Regardless of national wealth, many countries cited the unavailability of appropriate headache drugs as a barrier to care. The researchers studied epidemiologic data and answers on questionnaires completed by neurologists, general practitioners, and patients in 101 countries.
Group Decries Alzheimer's Test
The watchdog group Public Citizen has challenged a recent JAMA report of success with a radioactive dye for detecting beta-amyloid plaques by positron-emission tomography (PET). The dye maker's study in January concluded that PET with florbetapir F 18 can indicate the presence and density of the plaques associated with Alzheimer's disease. In a letter to the journal, Public Citizen claimed that the authors withheld “critically important data,” and it urged the Food and Drug Administration not to approve the dye. “In their JAMA article, the researchers presented only the median score of the three physician readers for the amount of beta-amyloid seen on each florbetapir-PET scan, but withheld critical data on the scores for each individual physician reader,” the group said in a statement. Also in January, the FDA withheld approval of the dye pending additional data on reliability between florbetapir-PET scan readers.
A $212 Million Botox Verdict
A Virginia jury voted to award $212 million to a man who said he sustained permanent brain damage after receiving injections of Botox for tremors in his hand. Douglas M. Ray alleged that Allergan Inc. had failed to properly warn of all of Botox's inherent dangers, including the autoimmune disorder he developed after the injections. In a statement, a company spokeswoman said that “the facts, data and qualified expert testimony in this case established that there is no evidence to suggest Allergan failed to make available adequate information to Mr. Ray's treating physician about the potential risks associated with Botox. Nor was there any proof that Botox caused the symptoms suffered by Mr. Ray.” Although the jury said Mr. Ray should get $212 million, $200 million of that – the punitive damages portion – will be capped at $350,000 under Virginia law. Allergan is “currently evaluating the basis for an appeal,” a spokeswoman said.
Headaches Take a Toll …
Headaches were the main cause of 3 million emergency department visits and 81,000 hospital stays in the United States, according to an analysis of 2008 data by the Agency for Healthcare Research and Quality. Those figures represented 2.4% of ED visits and 0.2% of hospitalizations, respectively. Migraines made up one-third of the headache emergencies and two-thirds of the hospital stays for headaches. The ED visits increased during the summer months, peaked in September, and were lowest during February and December. Three-fourths of the headache sufferers were women, who also were four times more likely to have migraines than were men. People in low-income and rural communities were more likely than their counterparts to visit EDs for headaches.
… While They're Under-Diagnosed
Headaches are under-recognized, under-diagnosed, and under-treated worldwide, according to the World Health Organization. “Health-care providers need better knowledge of how to diagnose and treat the small number of headache disorders that contribute substantially to public ill-health,” according to the “Atlas of Headache Disorders and Resources in the World 2011” compiled by the WHO and the group Lifting the Burden. Only about 40% of patients with migraines or tension-type headaches are professionally diagnosed, according to the report. About half of the people with headaches treat themselves without contacting a health care professional. Regardless of national wealth, many countries cited the unavailability of appropriate headache drugs as a barrier to care. The researchers studied epidemiologic data and answers on questionnaires completed by neurologists, general practitioners, and patients in 101 countries.
Group Decries Alzheimer's Test
The watchdog group Public Citizen has challenged a recent JAMA report of success with a radioactive dye for detecting beta-amyloid plaques by positron-emission tomography (PET). The dye maker's study in January concluded that PET with florbetapir F 18 can indicate the presence and density of the plaques associated with Alzheimer's disease. In a letter to the journal, Public Citizen claimed that the authors withheld “critically important data,” and it urged the Food and Drug Administration not to approve the dye. “In their JAMA article, the researchers presented only the median score of the three physician readers for the amount of beta-amyloid seen on each florbetapir-PET scan, but withheld critical data on the scores for each individual physician reader,” the group said in a statement. Also in January, the FDA withheld approval of the dye pending additional data on reliability between florbetapir-PET scan readers.
A $212 Million Botox Verdict
A Virginia jury voted to award $212 million to a man who said he sustained permanent brain damage after receiving injections of Botox for tremors in his hand. Douglas M. Ray alleged that Allergan Inc. had failed to properly warn of all of Botox's inherent dangers, including the autoimmune disorder he developed after the injections. In a statement, a company spokeswoman said that “the facts, data and qualified expert testimony in this case established that there is no evidence to suggest Allergan failed to make available adequate information to Mr. Ray's treating physician about the potential risks associated with Botox. Nor was there any proof that Botox caused the symptoms suffered by Mr. Ray.” Although the jury said Mr. Ray should get $212 million, $200 million of that – the punitive damages portion – will be capped at $350,000 under Virginia law. Allergan is “currently evaluating the basis for an appeal,” a spokeswoman said.
MRI Is an Important Tool in Identifying Silent JIA
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: All of the patients with clinically defined persistent oligoarticular
juvenile idiopathic arthritis (JIA) were found to have polyarticular
disease on MRI.
Data Source: A study of 21 patients with JIA (median age, 10.2 years at
enrollment), who were on medications including NSAIDs, methotrexate,
and/or tumor necrosis factor antagonists
Disclosures: Dr. Tzaribachev has received a research grant from Pfizer on
temporomandibular joint arthritis in patients with JIA. His coauthors
reported no disclosures.