User login
Hospital employment or physician-led ACO?
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
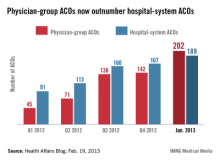
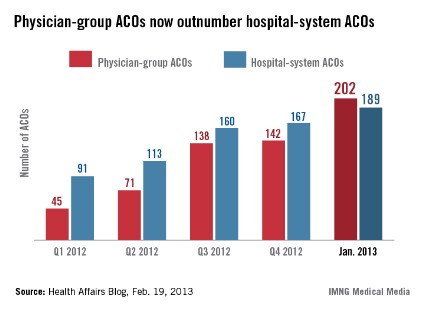
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
Primary care physicians around the country are facing the largest decision of their lives: Do I stay independent and maybe form an accountable care organization with other independent physicians, or do I become an employee of a hospital or health system?
As accountable care is taking hold, new data may alter historic thinking on this "bet-the-practice" question.
Tired of being overworked, undersatisfied, and overwhelmed with growing regulatory requirements, many primary care physicians have sought the security and strength of hospital employment. They say the pressures to invest in technology, billing, coding, and continued reimbursement pressures are just too great.
Yet, the majority of these physicians miss their days of self-employed autonomy, are on average less productive, and worry that the clocks on their compensation guarantees are ticking down.
Most of the moves by your colleagues, and perhaps you, to hospital employment have been defensive. It was just no longer feasible to stay afloat in the current fee-for-service system. You cannot work any harder, faster, or cheaper. You can no longer spend satisfactory time with your patients.
On the other hand, some of you may have joined a hospital or health system to be proactive and gain a solid platform to prepare for the new value-based payment era.
You may have envisioned being integrated with a critical mass of like-minded physicians and facilities, aided by advanced population management tools and a strong balance sheet, and all linked together on the hospital’s health information technology platform. You read that primary care should be in a leadership position and financially incentivized in any accountable care organization – including a hospital’s. Independent physicians could theoretically form ACOs, too, but lack the up-front capital, know-how, and any spare intellectual bandwidth to do so.
So, from a strategic perspective, becoming employed with other physicians by a health system seemed the way to go.
The pace has quickened of health care’s movement away from fee for service or "pay for volume" to payment for better outcomes at lower overall costs, or "pay for value." The factors that applied to the decision to become employed in the fee-for-service era may be yielding to those in the accountable care era sooner than anticipated.
Independent physician-led ACOs appear to be adapting better than hospitals to this change. Although much better prepared fiscally, hospitals are conflicted, or at least hesitant, to make this switch, because much of the savings comes from avoidable admissions and readmissions. On the other hand, emerging data and experience are showing that physician-led ACOs can be very successful.
There are some very integrated and successful hospital-led ACOs or other value-delivery hospital/physician models. In fact, I believe that if the hospital is willing to right-size and truly commit to value, it can be the most successful model.
However, many physicians signed volume-only physician work relative value unit (wRVU) compensation formulas in their hospital employment agreements, with no incentive payments for value. They have not been involved as partners, much less leaders, in any ACO planning. Even though the fee-for-service days are waning and strains are showing for many hospitals that are not adapting, for many employed physicians, the pace of preparedness for the accountable care era has been disappointing.
New data show that while most of the early ACOs in the Medicare Shared Savings Program were hospital led, there are now more physician-led ACOs than any other. At the same time, early results of some modest primary care–only ACOs have been exciting. The rural primary care physician ACO previously reported on in this column, Rio Grande Valley Health Alliance in McAllen, Tex., is preliminarily looking at 90th-percentile quality results and more than $500,000 in (unofficial) savings per physician in their first year under the Medicare Shared Savings Program.
In fact, in a May 14, 2014, article in JAMA, its authors stated: "Even though most adult primary care physicians may not realize it, they each can be seen as a chief executive officer (CEO) in charge of approximately $10 million in annual revenue" (JAMA 2014;311:1855-6). They noted that primary care receives only 5% of that spending, but can control much of the average of $5,000 in annual spending of their 2,000 or so patients. The independent physician-led Palm Beach ACO is cited as an example, with $22 million in savings their first year. The authors recommend physician-led ACOs as the best way to leverage that "CEO" power.
These new success lessons are being learned and need to be shared. Primary care physicians need to understand that the risk of change is now much less than the risk of maintaining the status quo. You need transparency regarding the realities of all your choices, including hospital employment and physician ACOs.
As readers of this column know, I heartily endorse the trend recognized in the JAMA article: "[A]n increasing number of primary care physicians see physician-led ACOs as a powerful opportunity to retain their autonomy and make a positive difference for their patient – as well as their practices’ bottom lines."
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
Anatomy of an independent primary care ACO, part 2
In our last column, we highlighted the Rio Grande Valley Health Alliance, an accountable care organization in McAllen, Tex., composed of 14 independent primary care physicians in 11 practices. As primary care physicians, the RGVHA providers realized the potential for a primary care ACO to generate savings from value-based care.
Because RGVHA is a network model ACO – the physicians stay in their separate independent practices but participate in the ACO through contracts – RGVHA needed a way to manage the ACO data collection, sorting, and reporting requirements in an efficient and effective manner.
Fortunately, Dr. Gretchen Hoyle of MD Online Solutions was able to tailor a data management solution for RGVHA. In addition, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Through Dr. Hoyle’s data collection and interpretation work with RGVHA, the ACO now has concrete data showing utilization trends and patterns. The most positive result has been the demonstrated benefit of nurse care coordinators, who work with patients in the post–acute care settings between their office visits.
In fact, care coordinators have proved to be RGVHA’s secret weapon, because their work has been invaluable in managing patients with chronic conditions between provider appointments.
Conversely, the data have revealed a pattern of overuse of home health care services, which helps contribute to higher care costs overall, making home health the biggest disappointment.
The secret weapon
As Dr. Hoyle so aptly said, "To become a fully functioning ACO, an organization must be able to address both sides of the ACO ‘coin’: quality improvement and cost control." Care coordinators have the capacity to address both concerns.
Within RGVHA, care coordinators have performed chart reviews that identify the ACO’s current performance according to the Centers for Medicare and Medicaid Services’ quality standards. This is the first secret weapon for a small primary care ACO.
This data collection helps RGVHA fill in knowledge gaps as it works toward having a fully integrated electronic health records system. In turn, it helps the care coordinators identify the strengths and weaknesses of each of the participating ACO providers. This ensures that weaknesses can be addressed in a timely fashion. In addition, the chart reviews help identify documentation issues. Documentation is critical to meeting CMS benchmarks, which ultimately helps determine the amount of shared savings for an ACO.
In addition, the data have proved crucial to being able to rank patients by cost. That has allowed RGVHA to identify the top 10% of patients whose care accounts for 50% of the total care costs in the ACO. This information allows providers to understand which patients and types of patients are more expensive, and who can benefit most from intense care coordination and/or longer visits with RGVHA’s primary care doctors.
Claims data show that even a small amount of additional time and care coordination outside of the clinic setting curbs utilization for the most complex patients and saves money. Most important, care coordinators help providers focus their time and energy where it can have the most impact.
The biggest disappointment
Shortly after RGVHA began reviewing patient claims data, home health care costs per patient emerged as one of the greatest cost outliers. The data revealed that providers outside of the ACO were prescribing home health at much higher rates than providers within the ACO. A subsequent gap analysis showed that home health was a prime opportunity target for RGVHA.
As RGVHA developed a strategy to address the overutilization and extremely high home health costs for their patient population, the providers faced their biggest disappointment to date: The Medicare Shared Savings Program regulations only permit ACOs to "ask" that providers outside the ACO coordinate patient care with doctors inside the ACO, not "tell" the providers that they must collaborate in delivering evidence-based, high-value care.
So, RGVHA decided to use those data as the starting point to reach out to those providers.
Dr. Hoyle helped RGVHA identify the amount of home health care generated by each specific agency and ordering physician. That information was used to craft a targeted letter to each provider outside the ACO requesting and encouraging their collaboration and cooperation in the development of a care plan for each home health patient.
Now, several months later, home health care overutilization and costs are beginning to decline, as patient care is monitored by RGVHA and appropriately coordinated among each ACO patient’s team of care providers.
RGVHA’s biggest concern has now become one of its biggest assets. The ACO doctors finally feel empowered in their ability to impact the quality and costs of patient care. Furthermore, they are excited they are getting paid for doing what they are trained to do: provide high-value care to their patients.
The good news is that, when properly informed and invited to help shape high-value patient care, providers want to and will do the right thing.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. Mr. Bobbitt is grateful for the excellent lead research and drafting of this article by Ms. Poe. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
In our last column, we highlighted the Rio Grande Valley Health Alliance, an accountable care organization in McAllen, Tex., composed of 14 independent primary care physicians in 11 practices. As primary care physicians, the RGVHA providers realized the potential for a primary care ACO to generate savings from value-based care.
Because RGVHA is a network model ACO – the physicians stay in their separate independent practices but participate in the ACO through contracts – RGVHA needed a way to manage the ACO data collection, sorting, and reporting requirements in an efficient and effective manner.
Fortunately, Dr. Gretchen Hoyle of MD Online Solutions was able to tailor a data management solution for RGVHA. In addition, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Through Dr. Hoyle’s data collection and interpretation work with RGVHA, the ACO now has concrete data showing utilization trends and patterns. The most positive result has been the demonstrated benefit of nurse care coordinators, who work with patients in the post–acute care settings between their office visits.
In fact, care coordinators have proved to be RGVHA’s secret weapon, because their work has been invaluable in managing patients with chronic conditions between provider appointments.
Conversely, the data have revealed a pattern of overuse of home health care services, which helps contribute to higher care costs overall, making home health the biggest disappointment.
The secret weapon
As Dr. Hoyle so aptly said, "To become a fully functioning ACO, an organization must be able to address both sides of the ACO ‘coin’: quality improvement and cost control." Care coordinators have the capacity to address both concerns.
Within RGVHA, care coordinators have performed chart reviews that identify the ACO’s current performance according to the Centers for Medicare and Medicaid Services’ quality standards. This is the first secret weapon for a small primary care ACO.
This data collection helps RGVHA fill in knowledge gaps as it works toward having a fully integrated electronic health records system. In turn, it helps the care coordinators identify the strengths and weaknesses of each of the participating ACO providers. This ensures that weaknesses can be addressed in a timely fashion. In addition, the chart reviews help identify documentation issues. Documentation is critical to meeting CMS benchmarks, which ultimately helps determine the amount of shared savings for an ACO.
In addition, the data have proved crucial to being able to rank patients by cost. That has allowed RGVHA to identify the top 10% of patients whose care accounts for 50% of the total care costs in the ACO. This information allows providers to understand which patients and types of patients are more expensive, and who can benefit most from intense care coordination and/or longer visits with RGVHA’s primary care doctors.
Claims data show that even a small amount of additional time and care coordination outside of the clinic setting curbs utilization for the most complex patients and saves money. Most important, care coordinators help providers focus their time and energy where it can have the most impact.
The biggest disappointment
Shortly after RGVHA began reviewing patient claims data, home health care costs per patient emerged as one of the greatest cost outliers. The data revealed that providers outside of the ACO were prescribing home health at much higher rates than providers within the ACO. A subsequent gap analysis showed that home health was a prime opportunity target for RGVHA.
As RGVHA developed a strategy to address the overutilization and extremely high home health costs for their patient population, the providers faced their biggest disappointment to date: The Medicare Shared Savings Program regulations only permit ACOs to "ask" that providers outside the ACO coordinate patient care with doctors inside the ACO, not "tell" the providers that they must collaborate in delivering evidence-based, high-value care.
So, RGVHA decided to use those data as the starting point to reach out to those providers.
Dr. Hoyle helped RGVHA identify the amount of home health care generated by each specific agency and ordering physician. That information was used to craft a targeted letter to each provider outside the ACO requesting and encouraging their collaboration and cooperation in the development of a care plan for each home health patient.
Now, several months later, home health care overutilization and costs are beginning to decline, as patient care is monitored by RGVHA and appropriately coordinated among each ACO patient’s team of care providers.
RGVHA’s biggest concern has now become one of its biggest assets. The ACO doctors finally feel empowered in their ability to impact the quality and costs of patient care. Furthermore, they are excited they are getting paid for doing what they are trained to do: provide high-value care to their patients.
The good news is that, when properly informed and invited to help shape high-value patient care, providers want to and will do the right thing.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. Mr. Bobbitt is grateful for the excellent lead research and drafting of this article by Ms. Poe. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
In our last column, we highlighted the Rio Grande Valley Health Alliance, an accountable care organization in McAllen, Tex., composed of 14 independent primary care physicians in 11 practices. As primary care physicians, the RGVHA providers realized the potential for a primary care ACO to generate savings from value-based care.
Because RGVHA is a network model ACO – the physicians stay in their separate independent practices but participate in the ACO through contracts – RGVHA needed a way to manage the ACO data collection, sorting, and reporting requirements in an efficient and effective manner.
Fortunately, Dr. Gretchen Hoyle of MD Online Solutions was able to tailor a data management solution for RGVHA. In addition, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Through Dr. Hoyle’s data collection and interpretation work with RGVHA, the ACO now has concrete data showing utilization trends and patterns. The most positive result has been the demonstrated benefit of nurse care coordinators, who work with patients in the post–acute care settings between their office visits.
In fact, care coordinators have proved to be RGVHA’s secret weapon, because their work has been invaluable in managing patients with chronic conditions between provider appointments.
Conversely, the data have revealed a pattern of overuse of home health care services, which helps contribute to higher care costs overall, making home health the biggest disappointment.
The secret weapon
As Dr. Hoyle so aptly said, "To become a fully functioning ACO, an organization must be able to address both sides of the ACO ‘coin’: quality improvement and cost control." Care coordinators have the capacity to address both concerns.
Within RGVHA, care coordinators have performed chart reviews that identify the ACO’s current performance according to the Centers for Medicare and Medicaid Services’ quality standards. This is the first secret weapon for a small primary care ACO.
This data collection helps RGVHA fill in knowledge gaps as it works toward having a fully integrated electronic health records system. In turn, it helps the care coordinators identify the strengths and weaknesses of each of the participating ACO providers. This ensures that weaknesses can be addressed in a timely fashion. In addition, the chart reviews help identify documentation issues. Documentation is critical to meeting CMS benchmarks, which ultimately helps determine the amount of shared savings for an ACO.
In addition, the data have proved crucial to being able to rank patients by cost. That has allowed RGVHA to identify the top 10% of patients whose care accounts for 50% of the total care costs in the ACO. This information allows providers to understand which patients and types of patients are more expensive, and who can benefit most from intense care coordination and/or longer visits with RGVHA’s primary care doctors.
Claims data show that even a small amount of additional time and care coordination outside of the clinic setting curbs utilization for the most complex patients and saves money. Most important, care coordinators help providers focus their time and energy where it can have the most impact.
The biggest disappointment
Shortly after RGVHA began reviewing patient claims data, home health care costs per patient emerged as one of the greatest cost outliers. The data revealed that providers outside of the ACO were prescribing home health at much higher rates than providers within the ACO. A subsequent gap analysis showed that home health was a prime opportunity target for RGVHA.
As RGVHA developed a strategy to address the overutilization and extremely high home health costs for their patient population, the providers faced their biggest disappointment to date: The Medicare Shared Savings Program regulations only permit ACOs to "ask" that providers outside the ACO coordinate patient care with doctors inside the ACO, not "tell" the providers that they must collaborate in delivering evidence-based, high-value care.
So, RGVHA decided to use those data as the starting point to reach out to those providers.
Dr. Hoyle helped RGVHA identify the amount of home health care generated by each specific agency and ordering physician. That information was used to craft a targeted letter to each provider outside the ACO requesting and encouraging their collaboration and cooperation in the development of a care plan for each home health patient.
Now, several months later, home health care overutilization and costs are beginning to decline, as patient care is monitored by RGVHA and appropriately coordinated among each ACO patient’s team of care providers.
RGVHA’s biggest concern has now become one of its biggest assets. The ACO doctors finally feel empowered in their ability to impact the quality and costs of patient care. Furthermore, they are excited they are getting paid for doing what they are trained to do: provide high-value care to their patients.
The good news is that, when properly informed and invited to help shape high-value patient care, providers want to and will do the right thing.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. Mr. Bobbitt is grateful for the excellent lead research and drafting of this article by Ms. Poe. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
ACO Insider: Anatomy of an independent primary care ACO, part 1
While concepts and theories can go a long way, sometimes the best way to understand something is through a concrete example.
So, from time to time, ACO Insider will check in on a new accountable care organization composed of 14 independent physicians in 11 practices in McAllen, Tex.
We chose them because they share many of the same questions and concerns as quite a few of you readers: Will this work? Where do I begin? How can we do this, since we have no free time or money? How much will this cost? Will there be any shared savings? Do we have to affiliate with a hospital or a large practice? Are we too small? How do we apply for the Medicare Shared Savings Program (MSSP)? What will change in my practice?
The name of the ACO is Rio Grande Valley Health Alliance (RGVHA). It was formed in January 2012 as a "network-model" ACO, meaning that the physicians stay in their separate independent practices but participate in the ACO through contract. Its first – and as of this writing, only – ACO payer contract is with Medicare, the MSSP.
So far, there have been a number of unexpected highs and a number of unexpected lows. The primary care physicians of RGVHA hope that by sharing their story, they can help you better navigate your own ACO course.
Opportunity for primary care
Dr. Luis Delgado became intrigued by the possibility under accountable care of rewarding primary care physicians for the savings they generate while maintaining or improving quality. Instead of resisting change, he saw opportunity.
He also saw a chance to do something about McAllen’s reputation, gained through Dr. Atul Gawande’s 2009 article in the New Yorker entitled, "The Cost Conundrum." That article focused on McAllen’s Medicare health costs, which were almost twice those of its Rio Grande River neighbor, El Paso.
However, beyond having a vision, he had no know-how and no budget.
Fortunately, as readers of this column know, there is so much documented "low-hanging fruit" for primary care to generate savings through value-based care that the strategic time and expertise expenditures proved not to be significant. The legal structure and backroom business logistics for a small network-model primary care physician ACO are also relatively straightforward. RGVHA has two full-time administrative staffers, one part-time president (Dr. Delgado), and one part-time medical director (Dr. Roger Heredia).
However, the new ACO data collection, sorting, and reporting requirements were somewhat daunting – that is, until they met Dr. Gretchen Hoyle of MD Online Solutions (MDOS). Dr. Hoyle is a practicing pediatrician who spearheaded the design of a physician-friendly care management data system for her practice and found it ideal for the accountable care era. Her company targets small- to medium-sized physician-led ACOs.
MDOS was able to tailor a nimble ACO solution scaled to RGVHA’s needs, thus allowing RGVHA to supply its last missing piece in a cost-effective manner. Because she is a practicing physician, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Approved for the Medicare ACO
Despite initial fears, RGVHA found that the MSSP application process was not intimidating at all. It turned out to be a reflection of its business structure and primary care physician ACO strategy.
"If you get your game plan together ahead of time, independent primary care physicians should be successful in applying for the Medicare Shared Savings Program," stated Dr. Delgado. "We found that Medicare is supportive of this type of ACO, I guess because it sees their potential to improve health care," he said.
The Centers for Medicare & Medicaid Services does indeed support these types of ACOs, as RGVHA qualified for one of the last Advanced Payment Program grants. The CMS is so confident that these physician-led, nonmetropolitan ACOs will work, that the agency actually fronted the infrastructure and operational money to them. RGVHA was one of the last grantees of this one-time appropriation.
They began the MSSP program Jan. 1, 2013, opting not to take risk and to receive 50% of the savings they generated for the 5,000 patients attributed to them, if quality and patient satisfaction metrics are met.
‘I haven’t had this much fun practicing medicine in 10 years!’
To decide what type of initiatives to undertake, the physicians read the Physician’s Accountable Care Toolkit (profiled in an earlier column) and convened a weekend workshop. They were pleasantly surprised when they realized that so many savings and quality improvement opportunities are available to primary care physicians under accountable care – and control over the physician-patient relationship was being returned to them.
They targeted diabetes management, patient engagement, best practices for enhanced prevention and wellness, and home health management.
One physician summed up the mood when she exclaimed, "I haven’t had this much fun practicing medicine in 10 years."
As they celebrate their first year under the MSSP, how are they doing? Check in next month for part 2: Our secret weapon, and our biggest disappointment.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
While concepts and theories can go a long way, sometimes the best way to understand something is through a concrete example.
So, from time to time, ACO Insider will check in on a new accountable care organization composed of 14 independent physicians in 11 practices in McAllen, Tex.
We chose them because they share many of the same questions and concerns as quite a few of you readers: Will this work? Where do I begin? How can we do this, since we have no free time or money? How much will this cost? Will there be any shared savings? Do we have to affiliate with a hospital or a large practice? Are we too small? How do we apply for the Medicare Shared Savings Program (MSSP)? What will change in my practice?
The name of the ACO is Rio Grande Valley Health Alliance (RGVHA). It was formed in January 2012 as a "network-model" ACO, meaning that the physicians stay in their separate independent practices but participate in the ACO through contract. Its first – and as of this writing, only – ACO payer contract is with Medicare, the MSSP.
So far, there have been a number of unexpected highs and a number of unexpected lows. The primary care physicians of RGVHA hope that by sharing their story, they can help you better navigate your own ACO course.
Opportunity for primary care
Dr. Luis Delgado became intrigued by the possibility under accountable care of rewarding primary care physicians for the savings they generate while maintaining or improving quality. Instead of resisting change, he saw opportunity.
He also saw a chance to do something about McAllen’s reputation, gained through Dr. Atul Gawande’s 2009 article in the New Yorker entitled, "The Cost Conundrum." That article focused on McAllen’s Medicare health costs, which were almost twice those of its Rio Grande River neighbor, El Paso.
However, beyond having a vision, he had no know-how and no budget.
Fortunately, as readers of this column know, there is so much documented "low-hanging fruit" for primary care to generate savings through value-based care that the strategic time and expertise expenditures proved not to be significant. The legal structure and backroom business logistics for a small network-model primary care physician ACO are also relatively straightforward. RGVHA has two full-time administrative staffers, one part-time president (Dr. Delgado), and one part-time medical director (Dr. Roger Heredia).
However, the new ACO data collection, sorting, and reporting requirements were somewhat daunting – that is, until they met Dr. Gretchen Hoyle of MD Online Solutions (MDOS). Dr. Hoyle is a practicing pediatrician who spearheaded the design of a physician-friendly care management data system for her practice and found it ideal for the accountable care era. Her company targets small- to medium-sized physician-led ACOs.
MDOS was able to tailor a nimble ACO solution scaled to RGVHA’s needs, thus allowing RGVHA to supply its last missing piece in a cost-effective manner. Because she is a practicing physician, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Approved for the Medicare ACO
Despite initial fears, RGVHA found that the MSSP application process was not intimidating at all. It turned out to be a reflection of its business structure and primary care physician ACO strategy.
"If you get your game plan together ahead of time, independent primary care physicians should be successful in applying for the Medicare Shared Savings Program," stated Dr. Delgado. "We found that Medicare is supportive of this type of ACO, I guess because it sees their potential to improve health care," he said.
The Centers for Medicare & Medicaid Services does indeed support these types of ACOs, as RGVHA qualified for one of the last Advanced Payment Program grants. The CMS is so confident that these physician-led, nonmetropolitan ACOs will work, that the agency actually fronted the infrastructure and operational money to them. RGVHA was one of the last grantees of this one-time appropriation.
They began the MSSP program Jan. 1, 2013, opting not to take risk and to receive 50% of the savings they generated for the 5,000 patients attributed to them, if quality and patient satisfaction metrics are met.
‘I haven’t had this much fun practicing medicine in 10 years!’
To decide what type of initiatives to undertake, the physicians read the Physician’s Accountable Care Toolkit (profiled in an earlier column) and convened a weekend workshop. They were pleasantly surprised when they realized that so many savings and quality improvement opportunities are available to primary care physicians under accountable care – and control over the physician-patient relationship was being returned to them.
They targeted diabetes management, patient engagement, best practices for enhanced prevention and wellness, and home health management.
One physician summed up the mood when she exclaimed, "I haven’t had this much fun practicing medicine in 10 years."
As they celebrate their first year under the MSSP, how are they doing? Check in next month for part 2: Our secret weapon, and our biggest disappointment.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
While concepts and theories can go a long way, sometimes the best way to understand something is through a concrete example.
So, from time to time, ACO Insider will check in on a new accountable care organization composed of 14 independent physicians in 11 practices in McAllen, Tex.
We chose them because they share many of the same questions and concerns as quite a few of you readers: Will this work? Where do I begin? How can we do this, since we have no free time or money? How much will this cost? Will there be any shared savings? Do we have to affiliate with a hospital or a large practice? Are we too small? How do we apply for the Medicare Shared Savings Program (MSSP)? What will change in my practice?
The name of the ACO is Rio Grande Valley Health Alliance (RGVHA). It was formed in January 2012 as a "network-model" ACO, meaning that the physicians stay in their separate independent practices but participate in the ACO through contract. Its first – and as of this writing, only – ACO payer contract is with Medicare, the MSSP.
So far, there have been a number of unexpected highs and a number of unexpected lows. The primary care physicians of RGVHA hope that by sharing their story, they can help you better navigate your own ACO course.
Opportunity for primary care
Dr. Luis Delgado became intrigued by the possibility under accountable care of rewarding primary care physicians for the savings they generate while maintaining or improving quality. Instead of resisting change, he saw opportunity.
He also saw a chance to do something about McAllen’s reputation, gained through Dr. Atul Gawande’s 2009 article in the New Yorker entitled, "The Cost Conundrum." That article focused on McAllen’s Medicare health costs, which were almost twice those of its Rio Grande River neighbor, El Paso.
However, beyond having a vision, he had no know-how and no budget.
Fortunately, as readers of this column know, there is so much documented "low-hanging fruit" for primary care to generate savings through value-based care that the strategic time and expertise expenditures proved not to be significant. The legal structure and backroom business logistics for a small network-model primary care physician ACO are also relatively straightforward. RGVHA has two full-time administrative staffers, one part-time president (Dr. Delgado), and one part-time medical director (Dr. Roger Heredia).
However, the new ACO data collection, sorting, and reporting requirements were somewhat daunting – that is, until they met Dr. Gretchen Hoyle of MD Online Solutions (MDOS). Dr. Hoyle is a practicing pediatrician who spearheaded the design of a physician-friendly care management data system for her practice and found it ideal for the accountable care era. Her company targets small- to medium-sized physician-led ACOs.
MDOS was able to tailor a nimble ACO solution scaled to RGVHA’s needs, thus allowing RGVHA to supply its last missing piece in a cost-effective manner. Because she is a practicing physician, Dr. Hoyle helps interpret the data and leads a weekly data-driven staff conference call with the ACO’s nurse care coordinators.
Approved for the Medicare ACO
Despite initial fears, RGVHA found that the MSSP application process was not intimidating at all. It turned out to be a reflection of its business structure and primary care physician ACO strategy.
"If you get your game plan together ahead of time, independent primary care physicians should be successful in applying for the Medicare Shared Savings Program," stated Dr. Delgado. "We found that Medicare is supportive of this type of ACO, I guess because it sees their potential to improve health care," he said.
The Centers for Medicare & Medicaid Services does indeed support these types of ACOs, as RGVHA qualified for one of the last Advanced Payment Program grants. The CMS is so confident that these physician-led, nonmetropolitan ACOs will work, that the agency actually fronted the infrastructure and operational money to them. RGVHA was one of the last grantees of this one-time appropriation.
They began the MSSP program Jan. 1, 2013, opting not to take risk and to receive 50% of the savings they generated for the 5,000 patients attributed to them, if quality and patient satisfaction metrics are met.
‘I haven’t had this much fun practicing medicine in 10 years!’
To decide what type of initiatives to undertake, the physicians read the Physician’s Accountable Care Toolkit (profiled in an earlier column) and convened a weekend workshop. They were pleasantly surprised when they realized that so many savings and quality improvement opportunities are available to primary care physicians under accountable care – and control over the physician-patient relationship was being returned to them.
They targeted diabetes management, patient engagement, best practices for enhanced prevention and wellness, and home health management.
One physician summed up the mood when she exclaimed, "I haven’t had this much fun practicing medicine in 10 years."
As they celebrate their first year under the MSSP, how are they doing? Check in next month for part 2: Our secret weapon, and our biggest disappointment.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or at 919-821-6612.
Distribution based on contribution: The merit-based ACO shared savings distribution model
Our nation is in the midst of an inexorable shift in health care delivery from "pay for volume" to "pay for value." It is well documented that our current largely fee-for-service system is unsustainable and a dramatic incentive shift must occur. Every provider needs to be committed to providing the highest quality at the lowest cost. This is the fundamental goal of the pay-for-value system.
If quality and patient satisfaction criteria are met and providers working together in an accountable care organization or similar entity create savings for a defined patient population, then the ACO usually gets a portion of the savings, commonly 50%. Unlike capitated arrangements, shared savings arrangements can avoid or limit downside financial risk and therefore can serve as stepping-stones toward fuller accountability and incentives. They are quite appropriate for start-up and smaller ACOs.
The ACO gets the savings, if there are any. But what the ACO does with them is crucial to the success and sustainability of the organization. "ACOs must offer a realistic and achievable opportunity for providers to share in the savings created from delivering higher-value care. The incentive system must reward providers for delivering efficient care as opposed to the current volume-driven system" (The ACO Toolkit; the Dartmouth Institute, p. 9, Jan. 2011).
If providers or hospital stakeholders feel that their efforts to drive value are not being fairly recognized, they will no longer participate meaningfully, the goals of value-based medicine will be thwarted, and savings will not occur in the long-run. Before signing a participation contract, physicians should scrutinize how each ACO plans to distribute the savings it receives.
The Centers for Medicare and Medicaid Services administers the Medicare Shared Savings Program (MSSP). The fact that CMS’s regulations concerning MSSP are not prescriptive about a given savings distribution formula gives ACOs flexibility in this area. But the regulations are specific about the ultimate purpose of distributions: "As part of its application, an ACO must describe the following: (1) how it plans to use shared savings payments, including the criteria it plans to employ for distributing shared savings among its ACO participants and ACO providers/suppliers, ... and (3) how the proposed plan will achieve the general aims of better care for individuals, better health for populations, and lower growth in expenditures" (42 CFR 425.204(d), 76 Fed. Reg. 6798 [Nov. 2, 2011]).
Fatal flaw?
Some ACOs, however, have lost sight of the fact that failure to have a fair shared savings distribution formula (linking relative distributions to relative contributions) will be fatal to its sustainability. Some view them as "profits" to go to the owners or shareholders. Some simply lock in a fixed allocation similar to fee-for-service payment ratios, without regard to who generated the savings. Some employers of physicians have contracted to compensate only on a work production basis with zero performance incentive payments at all. Other ACOs are putting off the issue because it is sensitive culturally. As health care moves more and more to value-based compensation, the distribution of savings must be viewed primarily as the providers’ professional remuneration and not corporate "profit." Payments for administrative services and debt service must, of course, come out of the savings distribution to "keep the pump primed," but they should be carefully managed. The bulk must be distributed in proportion to contribution toward quality and cost-effective care.
One physician stated, "No physician is going to join an ACO when someone else is telling them what they are worth unless they know that the savings distribution formula is impeccably fair." To those putting off design of a fair merit-based compensation system until there is more physician buy-in, we respectfully submit that you cannot get buy-in without one.
A need for honed metrics
Yes, this concept is pretty basic when you think about it. But though it may be easy to understand, it can be complex to implement, especially when multiple specialists and facilities are involved in an ACO’s care coordination. One not only needs to determine the relative potential and actual value contribution for each provider, but also the clinically valid metrics by which to measure them. Under fee for service, metrics for success were usually transactional and objective (in other words, volume of procedure times rate). An ACO’s success metrics may be neither. Success may come from things not happening (that is, fewer ED visits, avoidable admissions, and reduced readmissions). At the same time, the distribution model needs to be clear, practical, and capable of being understood by all.
But there can be a replicable framework for any ACO to use to create a fair and sustainable shared savings distribution model. There are necessary subjective judgments – at this time, many metrics are imprecise or nonexistent – and the sophistication of the distribution process must parallel the sophistication of the ACO’s infrastructure. But, if the right people are involved and apply the ACO’s guiding principles on savings allocation, participants will be appropriately incentivized. The precision of distribution application will grow over time. Don’t let the perfect be the enemy of the good.
The six guiding principles for shared savings distribution
Though application will vary widely because of differing circumstances and types of initiatives, chances for success will increase if every activity can be judged by whether it is consistent with a set of guiding principles viewed as fair by the ACO members. You may want to consider a savings distribution formula with the following principles:
• Eyes on the prize: Triple Aim. It offers incentives for the delivery of high-quality and cost-effective care to achieve the Triple Aim – better care for individuals, better health for populations, and lower per capita costs.
• Broad provider input. It is the result of input from a diverse spectrum of knowledgeable providers who understand what drives patient population value.
• Fairness. It is fair to all in that it links relative distribution to relative contribution to the organization’s total savings and quality performance, and adheres to measurable clinically valid metrics.
• Transparency. It is clear, transparent, practical to implement and replicable.
• Constant evolution. It adapts and improves as the capabilities and experience as the ACO grows.
• Maximized incentive to drive value by all participants. After prudently meeting overhead costs, it allows gradual transition as well as commercially reasonable return on capital investment or debt service. It makes the most of ongoing incentive programs for all to deliver value by distributing as much of the savings surplus as possible to those who generate them.
Weighting: How to assign relative percentage among providers
As mentioned, it is important that design of a fair distribution formula be the product of collaboration among informed and committed clinicians who understand patient population management. Like virtually all organization compensation formulas, the determination of relative contributions of the different providers in a given ACO, or care initiative within the ACO, will involve a certain amount of inherent subjectivity but will be guided by weighted criteria applied in good faith.
• Step 1: Break down each initiative into its value-adding elements and assign provider responsibility for each. The ACO will have a number of different care management initiatives. Some, like outpatient diabetes management, may be completely the responsibility of one provider specialty, (that is, primary care). Others may involve coordination across multiple settings for patients with multiple conditions involving multiple specialties. Each initiative was chosen for a reason – to drive value. In setting relative potential distribution percentages, envision the perfect implementation of each initiative. Next, look at what tasks or best practices are needed to drive success, and then who is assigned responsibility for each.
• Step 2: Assign relative percentages to each specialty relative to its potential to realize savings. For a pure primary care prevention initiative, they would get 100% in all categories. For multispecialty initiatives, the percentage is tied to the proportion of those savings predicted to flow from that provider class.
N.B.: Historically, cost centers are not necessarily the cost savers. A mature ACO will be able to allocate savings to each initiative and the relative savings distribution within each. But for a start-up ACO, because it is so apparently logical and fits the traditional fee-for-service mindset, it is tempting to look at claims differences in the various service categories, such as inpatient, outpatient, primary care, specialists, drugs, and ancillaries, and attribute savings to the provider historically billing for same (that is, hospitals get "credit" for reduced hospital costs). However, a successful wellness, prevention, or lifestyle counseling program in a medical home may be the reason those patients never go to the hospital. The radiologist embedded in the medical home diagnostic team may have helped make an informed image analysis confirming a negative result and avoided those admissions. But, do use those service categories to set cost targets.
• Step 3: Individual attribution. We now know every provider group’s potential savings, but how do we determine the actual distribution based on actual results? Select metrics that are accurately associated with the desired individual and collective conduct of that provider class. They should cover both quality and efficiency. In the value-based reimbursement world, even if the performance is superb, if it is not measured appropriately, it will not be rewarded.
Once the proper metrics are selected, each provider’s performance is measured.
Keep it simple and open
Pick a few of the very best quality and efficiency metrics and have them and the data collection process thoroughly vetted by the providers. Following the guiding principles, the distribution model will be a success if: (1) everyone understands that this is the best practical approach, (2) the process has been open, and (3) everyone is acting in good faith to have as fair a shared savings distribution process as the current sophistication level of the ACO’s infrastructure allows. It cannot be viewed as coming from a "black box." For a young ACO, it will be crude, at best, in the beginning.
Conclusion
Even at this dawning of the movement to value-based reimbursement in health care, a framework for a fair merit-based shared savings distribution is available to all ACOs. As ACOs gain actual performance data, their health information technology capabilities improve, and refined quality and efficiency metrics emerge, the process will evolve from an open and good-faith application of the guiding principles with limited tools, to more and more refined determinations of the sources of the ACO’s quality and savings results. The path will get easier over time, but the destination is always clear – distribution in proportion to contribution.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
Our nation is in the midst of an inexorable shift in health care delivery from "pay for volume" to "pay for value." It is well documented that our current largely fee-for-service system is unsustainable and a dramatic incentive shift must occur. Every provider needs to be committed to providing the highest quality at the lowest cost. This is the fundamental goal of the pay-for-value system.
If quality and patient satisfaction criteria are met and providers working together in an accountable care organization or similar entity create savings for a defined patient population, then the ACO usually gets a portion of the savings, commonly 50%. Unlike capitated arrangements, shared savings arrangements can avoid or limit downside financial risk and therefore can serve as stepping-stones toward fuller accountability and incentives. They are quite appropriate for start-up and smaller ACOs.
The ACO gets the savings, if there are any. But what the ACO does with them is crucial to the success and sustainability of the organization. "ACOs must offer a realistic and achievable opportunity for providers to share in the savings created from delivering higher-value care. The incentive system must reward providers for delivering efficient care as opposed to the current volume-driven system" (The ACO Toolkit; the Dartmouth Institute, p. 9, Jan. 2011).
If providers or hospital stakeholders feel that their efforts to drive value are not being fairly recognized, they will no longer participate meaningfully, the goals of value-based medicine will be thwarted, and savings will not occur in the long-run. Before signing a participation contract, physicians should scrutinize how each ACO plans to distribute the savings it receives.
The Centers for Medicare and Medicaid Services administers the Medicare Shared Savings Program (MSSP). The fact that CMS’s regulations concerning MSSP are not prescriptive about a given savings distribution formula gives ACOs flexibility in this area. But the regulations are specific about the ultimate purpose of distributions: "As part of its application, an ACO must describe the following: (1) how it plans to use shared savings payments, including the criteria it plans to employ for distributing shared savings among its ACO participants and ACO providers/suppliers, ... and (3) how the proposed plan will achieve the general aims of better care for individuals, better health for populations, and lower growth in expenditures" (42 CFR 425.204(d), 76 Fed. Reg. 6798 [Nov. 2, 2011]).
Fatal flaw?
Some ACOs, however, have lost sight of the fact that failure to have a fair shared savings distribution formula (linking relative distributions to relative contributions) will be fatal to its sustainability. Some view them as "profits" to go to the owners or shareholders. Some simply lock in a fixed allocation similar to fee-for-service payment ratios, without regard to who generated the savings. Some employers of physicians have contracted to compensate only on a work production basis with zero performance incentive payments at all. Other ACOs are putting off the issue because it is sensitive culturally. As health care moves more and more to value-based compensation, the distribution of savings must be viewed primarily as the providers’ professional remuneration and not corporate "profit." Payments for administrative services and debt service must, of course, come out of the savings distribution to "keep the pump primed," but they should be carefully managed. The bulk must be distributed in proportion to contribution toward quality and cost-effective care.
One physician stated, "No physician is going to join an ACO when someone else is telling them what they are worth unless they know that the savings distribution formula is impeccably fair." To those putting off design of a fair merit-based compensation system until there is more physician buy-in, we respectfully submit that you cannot get buy-in without one.
A need for honed metrics
Yes, this concept is pretty basic when you think about it. But though it may be easy to understand, it can be complex to implement, especially when multiple specialists and facilities are involved in an ACO’s care coordination. One not only needs to determine the relative potential and actual value contribution for each provider, but also the clinically valid metrics by which to measure them. Under fee for service, metrics for success were usually transactional and objective (in other words, volume of procedure times rate). An ACO’s success metrics may be neither. Success may come from things not happening (that is, fewer ED visits, avoidable admissions, and reduced readmissions). At the same time, the distribution model needs to be clear, practical, and capable of being understood by all.
But there can be a replicable framework for any ACO to use to create a fair and sustainable shared savings distribution model. There are necessary subjective judgments – at this time, many metrics are imprecise or nonexistent – and the sophistication of the distribution process must parallel the sophistication of the ACO’s infrastructure. But, if the right people are involved and apply the ACO’s guiding principles on savings allocation, participants will be appropriately incentivized. The precision of distribution application will grow over time. Don’t let the perfect be the enemy of the good.
The six guiding principles for shared savings distribution
Though application will vary widely because of differing circumstances and types of initiatives, chances for success will increase if every activity can be judged by whether it is consistent with a set of guiding principles viewed as fair by the ACO members. You may want to consider a savings distribution formula with the following principles:
• Eyes on the prize: Triple Aim. It offers incentives for the delivery of high-quality and cost-effective care to achieve the Triple Aim – better care for individuals, better health for populations, and lower per capita costs.
• Broad provider input. It is the result of input from a diverse spectrum of knowledgeable providers who understand what drives patient population value.
• Fairness. It is fair to all in that it links relative distribution to relative contribution to the organization’s total savings and quality performance, and adheres to measurable clinically valid metrics.
• Transparency. It is clear, transparent, practical to implement and replicable.
• Constant evolution. It adapts and improves as the capabilities and experience as the ACO grows.
• Maximized incentive to drive value by all participants. After prudently meeting overhead costs, it allows gradual transition as well as commercially reasonable return on capital investment or debt service. It makes the most of ongoing incentive programs for all to deliver value by distributing as much of the savings surplus as possible to those who generate them.
Weighting: How to assign relative percentage among providers
As mentioned, it is important that design of a fair distribution formula be the product of collaboration among informed and committed clinicians who understand patient population management. Like virtually all organization compensation formulas, the determination of relative contributions of the different providers in a given ACO, or care initiative within the ACO, will involve a certain amount of inherent subjectivity but will be guided by weighted criteria applied in good faith.
• Step 1: Break down each initiative into its value-adding elements and assign provider responsibility for each. The ACO will have a number of different care management initiatives. Some, like outpatient diabetes management, may be completely the responsibility of one provider specialty, (that is, primary care). Others may involve coordination across multiple settings for patients with multiple conditions involving multiple specialties. Each initiative was chosen for a reason – to drive value. In setting relative potential distribution percentages, envision the perfect implementation of each initiative. Next, look at what tasks or best practices are needed to drive success, and then who is assigned responsibility for each.
• Step 2: Assign relative percentages to each specialty relative to its potential to realize savings. For a pure primary care prevention initiative, they would get 100% in all categories. For multispecialty initiatives, the percentage is tied to the proportion of those savings predicted to flow from that provider class.
N.B.: Historically, cost centers are not necessarily the cost savers. A mature ACO will be able to allocate savings to each initiative and the relative savings distribution within each. But for a start-up ACO, because it is so apparently logical and fits the traditional fee-for-service mindset, it is tempting to look at claims differences in the various service categories, such as inpatient, outpatient, primary care, specialists, drugs, and ancillaries, and attribute savings to the provider historically billing for same (that is, hospitals get "credit" for reduced hospital costs). However, a successful wellness, prevention, or lifestyle counseling program in a medical home may be the reason those patients never go to the hospital. The radiologist embedded in the medical home diagnostic team may have helped make an informed image analysis confirming a negative result and avoided those admissions. But, do use those service categories to set cost targets.
• Step 3: Individual attribution. We now know every provider group’s potential savings, but how do we determine the actual distribution based on actual results? Select metrics that are accurately associated with the desired individual and collective conduct of that provider class. They should cover both quality and efficiency. In the value-based reimbursement world, even if the performance is superb, if it is not measured appropriately, it will not be rewarded.
Once the proper metrics are selected, each provider’s performance is measured.
Keep it simple and open
Pick a few of the very best quality and efficiency metrics and have them and the data collection process thoroughly vetted by the providers. Following the guiding principles, the distribution model will be a success if: (1) everyone understands that this is the best practical approach, (2) the process has been open, and (3) everyone is acting in good faith to have as fair a shared savings distribution process as the current sophistication level of the ACO’s infrastructure allows. It cannot be viewed as coming from a "black box." For a young ACO, it will be crude, at best, in the beginning.
Conclusion
Even at this dawning of the movement to value-based reimbursement in health care, a framework for a fair merit-based shared savings distribution is available to all ACOs. As ACOs gain actual performance data, their health information technology capabilities improve, and refined quality and efficiency metrics emerge, the process will evolve from an open and good-faith application of the guiding principles with limited tools, to more and more refined determinations of the sources of the ACO’s quality and savings results. The path will get easier over time, but the destination is always clear – distribution in proportion to contribution.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
Our nation is in the midst of an inexorable shift in health care delivery from "pay for volume" to "pay for value." It is well documented that our current largely fee-for-service system is unsustainable and a dramatic incentive shift must occur. Every provider needs to be committed to providing the highest quality at the lowest cost. This is the fundamental goal of the pay-for-value system.
If quality and patient satisfaction criteria are met and providers working together in an accountable care organization or similar entity create savings for a defined patient population, then the ACO usually gets a portion of the savings, commonly 50%. Unlike capitated arrangements, shared savings arrangements can avoid or limit downside financial risk and therefore can serve as stepping-stones toward fuller accountability and incentives. They are quite appropriate for start-up and smaller ACOs.
The ACO gets the savings, if there are any. But what the ACO does with them is crucial to the success and sustainability of the organization. "ACOs must offer a realistic and achievable opportunity for providers to share in the savings created from delivering higher-value care. The incentive system must reward providers for delivering efficient care as opposed to the current volume-driven system" (The ACO Toolkit; the Dartmouth Institute, p. 9, Jan. 2011).
If providers or hospital stakeholders feel that their efforts to drive value are not being fairly recognized, they will no longer participate meaningfully, the goals of value-based medicine will be thwarted, and savings will not occur in the long-run. Before signing a participation contract, physicians should scrutinize how each ACO plans to distribute the savings it receives.
The Centers for Medicare and Medicaid Services administers the Medicare Shared Savings Program (MSSP). The fact that CMS’s regulations concerning MSSP are not prescriptive about a given savings distribution formula gives ACOs flexibility in this area. But the regulations are specific about the ultimate purpose of distributions: "As part of its application, an ACO must describe the following: (1) how it plans to use shared savings payments, including the criteria it plans to employ for distributing shared savings among its ACO participants and ACO providers/suppliers, ... and (3) how the proposed plan will achieve the general aims of better care for individuals, better health for populations, and lower growth in expenditures" (42 CFR 425.204(d), 76 Fed. Reg. 6798 [Nov. 2, 2011]).
Fatal flaw?
Some ACOs, however, have lost sight of the fact that failure to have a fair shared savings distribution formula (linking relative distributions to relative contributions) will be fatal to its sustainability. Some view them as "profits" to go to the owners or shareholders. Some simply lock in a fixed allocation similar to fee-for-service payment ratios, without regard to who generated the savings. Some employers of physicians have contracted to compensate only on a work production basis with zero performance incentive payments at all. Other ACOs are putting off the issue because it is sensitive culturally. As health care moves more and more to value-based compensation, the distribution of savings must be viewed primarily as the providers’ professional remuneration and not corporate "profit." Payments for administrative services and debt service must, of course, come out of the savings distribution to "keep the pump primed," but they should be carefully managed. The bulk must be distributed in proportion to contribution toward quality and cost-effective care.
One physician stated, "No physician is going to join an ACO when someone else is telling them what they are worth unless they know that the savings distribution formula is impeccably fair." To those putting off design of a fair merit-based compensation system until there is more physician buy-in, we respectfully submit that you cannot get buy-in without one.
A need for honed metrics
Yes, this concept is pretty basic when you think about it. But though it may be easy to understand, it can be complex to implement, especially when multiple specialists and facilities are involved in an ACO’s care coordination. One not only needs to determine the relative potential and actual value contribution for each provider, but also the clinically valid metrics by which to measure them. Under fee for service, metrics for success were usually transactional and objective (in other words, volume of procedure times rate). An ACO’s success metrics may be neither. Success may come from things not happening (that is, fewer ED visits, avoidable admissions, and reduced readmissions). At the same time, the distribution model needs to be clear, practical, and capable of being understood by all.
But there can be a replicable framework for any ACO to use to create a fair and sustainable shared savings distribution model. There are necessary subjective judgments – at this time, many metrics are imprecise or nonexistent – and the sophistication of the distribution process must parallel the sophistication of the ACO’s infrastructure. But, if the right people are involved and apply the ACO’s guiding principles on savings allocation, participants will be appropriately incentivized. The precision of distribution application will grow over time. Don’t let the perfect be the enemy of the good.
The six guiding principles for shared savings distribution
Though application will vary widely because of differing circumstances and types of initiatives, chances for success will increase if every activity can be judged by whether it is consistent with a set of guiding principles viewed as fair by the ACO members. You may want to consider a savings distribution formula with the following principles:
• Eyes on the prize: Triple Aim. It offers incentives for the delivery of high-quality and cost-effective care to achieve the Triple Aim – better care for individuals, better health for populations, and lower per capita costs.
• Broad provider input. It is the result of input from a diverse spectrum of knowledgeable providers who understand what drives patient population value.
• Fairness. It is fair to all in that it links relative distribution to relative contribution to the organization’s total savings and quality performance, and adheres to measurable clinically valid metrics.
• Transparency. It is clear, transparent, practical to implement and replicable.
• Constant evolution. It adapts and improves as the capabilities and experience as the ACO grows.
• Maximized incentive to drive value by all participants. After prudently meeting overhead costs, it allows gradual transition as well as commercially reasonable return on capital investment or debt service. It makes the most of ongoing incentive programs for all to deliver value by distributing as much of the savings surplus as possible to those who generate them.
Weighting: How to assign relative percentage among providers
As mentioned, it is important that design of a fair distribution formula be the product of collaboration among informed and committed clinicians who understand patient population management. Like virtually all organization compensation formulas, the determination of relative contributions of the different providers in a given ACO, or care initiative within the ACO, will involve a certain amount of inherent subjectivity but will be guided by weighted criteria applied in good faith.
• Step 1: Break down each initiative into its value-adding elements and assign provider responsibility for each. The ACO will have a number of different care management initiatives. Some, like outpatient diabetes management, may be completely the responsibility of one provider specialty, (that is, primary care). Others may involve coordination across multiple settings for patients with multiple conditions involving multiple specialties. Each initiative was chosen for a reason – to drive value. In setting relative potential distribution percentages, envision the perfect implementation of each initiative. Next, look at what tasks or best practices are needed to drive success, and then who is assigned responsibility for each.
• Step 2: Assign relative percentages to each specialty relative to its potential to realize savings. For a pure primary care prevention initiative, they would get 100% in all categories. For multispecialty initiatives, the percentage is tied to the proportion of those savings predicted to flow from that provider class.
N.B.: Historically, cost centers are not necessarily the cost savers. A mature ACO will be able to allocate savings to each initiative and the relative savings distribution within each. But for a start-up ACO, because it is so apparently logical and fits the traditional fee-for-service mindset, it is tempting to look at claims differences in the various service categories, such as inpatient, outpatient, primary care, specialists, drugs, and ancillaries, and attribute savings to the provider historically billing for same (that is, hospitals get "credit" for reduced hospital costs). However, a successful wellness, prevention, or lifestyle counseling program in a medical home may be the reason those patients never go to the hospital. The radiologist embedded in the medical home diagnostic team may have helped make an informed image analysis confirming a negative result and avoided those admissions. But, do use those service categories to set cost targets.
• Step 3: Individual attribution. We now know every provider group’s potential savings, but how do we determine the actual distribution based on actual results? Select metrics that are accurately associated with the desired individual and collective conduct of that provider class. They should cover both quality and efficiency. In the value-based reimbursement world, even if the performance is superb, if it is not measured appropriately, it will not be rewarded.
Once the proper metrics are selected, each provider’s performance is measured.
Keep it simple and open
Pick a few of the very best quality and efficiency metrics and have them and the data collection process thoroughly vetted by the providers. Following the guiding principles, the distribution model will be a success if: (1) everyone understands that this is the best practical approach, (2) the process has been open, and (3) everyone is acting in good faith to have as fair a shared savings distribution process as the current sophistication level of the ACO’s infrastructure allows. It cannot be viewed as coming from a "black box." For a young ACO, it will be crude, at best, in the beginning.
Conclusion
Even at this dawning of the movement to value-based reimbursement in health care, a framework for a fair merit-based shared savings distribution is available to all ACOs. As ACOs gain actual performance data, their health information technology capabilities improve, and refined quality and efficiency metrics emerge, the process will evolve from an open and good-faith application of the guiding principles with limited tools, to more and more refined determinations of the sources of the ACO’s quality and savings results. The path will get easier over time, but the destination is always clear – distribution in proportion to contribution.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
CMS’ proposal to pay for care coordination: the ACO bridge?
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612).
Get ready now for 2014 Medicare ACO program
The Centers for Medicare and Medicaid Services has just announced key dates for the 2014 Medicare Shared Savings Program application cycle – and although the upcoming Jan. 1, 2014, start date for the MSSP seems far off, physicians should start organizing now.
Physician interest in participating is mounting, as physician-led accountable care organizations are emerging as leaders in improving quality while eradicating waste. In fact, there are now more physician-run ACOs than any other model (see chart below).
Physicians see opportunity
The MSSP has embraced the accountable care concept to improve the quality of care for Medicare fee-for-service beneficiaries. Eligible providers and suppliers may participate in the MSSP by creating or participating in an ACO. The MSSP rewards ACOs that lower their rate of growth in health care costs while meeting quality performance standards.
On Jan. 10, 2013, the Centers for Medicare and Medicaid Services (CMS) announced that 106 new organizations were selected to participate in the program. That’s in addition to the 87 ACOs approved in July 2012 and the 27 selected in April 2012 – bringing the total to 220 ACOs selected to participate in the MSSP. Early evidence indicates that these ACOs are decreasing costs while improving clinical outcomes.
For many of those ACOs, Medicare will be just the beginning. Private insurers such as Aetna, UnitedHealth Group, Humana, Cigna, and most Blue Cross plans are contracting with ACOs to care for more patients. Many state Medicaid programs have moved or are considering moving to accountable care.
These multiple streams of shared savings will be generated through the same ACO infrastructure needed for the MSSP, encouraging more physician-owned ACOs to form.
With the rise of ACOs, "providers are doing things in a positive way rather than a reactive way. We are seeing the beginnings of a tsunami," noted Dr. Michael Cryer, national medical director at employee benefits consultancy Aon Hewitt, in a New York Times article ("Small-picture approach flips medical economics," March 12, 2012).
According to a recent study by consulting firm Oliver Wyman entitled "The ACO Surprise," roughly 10% of the U.S. population, or from 25 million to 31 million patients, are being served by ACOs. "Successful ACOs won’t just siphon patients away from traditional providers. They will change the rules of the game," the report’s authors conclude.
Don’t miss these 2013 deadlines
CMS has just released its 2013 application cycle for 2014 (see table). The time to act is now. It will take time to understand ACOs and enlist a critical mass of informed and committed primary care providers. Though the notice of intent ("NOI") is not binding, failure to file in May is binding – you are barred from applying. Likewise, you must obtain your user ID by May 31.
The application is not hard, but it basically reflects your ACO game plan. You must be organized, have a focused care plan, and complete the application by the end of July – much earlier than last year’s deadline.
Bottom line: Do not let the start date lull you into procrastination.
Let’s have a closer look at some of the things that must be covered in the application. In addition to a culture of teamwork, patient engagement, and alignment of financial incentives, which are chief among the eight essential elements necessary for a successful ACO ("The essential elements of an ACO," Internal Medicine News, Oct. 1, 2012, p. 38), the MSSP application requires:
• Compliance with the required definitions of "ACO applicant" and "participant."
• A certification that the ACO, its ACO-provider participants, and its ACO providers/suppliers have agreed to become accountable for the quality, cost, and overall care of the Medicare fee-for-service beneficiaries assigned to the ACO.
• Establishment of a governing body.
• Implementation of a comprehensive compliance plan.
• Execution of an ACO Participation Agreement.
In addition, certain organizational milestones should be reached in advance of the application. In particular, planning for a successful ACO requires identification of a physician-champion, completion of a feasibility analysis, implementation of sufficient information technology, and internal reporting on quality and cost metrics. As in any entrepreneurial pursuit, timing is critical, and delay equates to lost potential.
Given that primary care providers are the only providers mandated for inclusion in the MSSP, it is apparent that CMS expects primary care to drive ACO value via prevention and wellness; chronic disease management; care transitions and navigation; reduced hospitalizations; and multispecialty care coordination of complex patients.
ACOs, in one form or another, are sure to be permanent fixtures in American health care, as the nation’s economy and its residents eagerly await the benefits stemming from primary care–driven innovation.
Opportunity knocks – get going!
For more information about the Medicare Shared Savings Program, click here.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, North Carolina. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612). Mr. McNeill is a practicing attorney pursuing his LLM at Duke University, currently focusing on accountable care.
Medicare Shared Savings Program deadlines
Key dates for Jan. 1, 2014, start:
| Notice of intent (NOI) accepted | May 1-31, 2013 |
| CMS user ID forms accepted | May 1-31, 2013 |
| Applications accepted | July 1-31, 2013 |
| Application approval or denial decision | Fall 2013 |
| Start date for MSSP ACO | Jan. 1, 2014 |
Source: Centers for Medicare and Medicaid Services
The Centers for Medicare and Medicaid Services has just announced key dates for the 2014 Medicare Shared Savings Program application cycle – and although the upcoming Jan. 1, 2014, start date for the MSSP seems far off, physicians should start organizing now.
Physician interest in participating is mounting, as physician-led accountable care organizations are emerging as leaders in improving quality while eradicating waste. In fact, there are now more physician-run ACOs than any other model (see chart below).
Physicians see opportunity
The MSSP has embraced the accountable care concept to improve the quality of care for Medicare fee-for-service beneficiaries. Eligible providers and suppliers may participate in the MSSP by creating or participating in an ACO. The MSSP rewards ACOs that lower their rate of growth in health care costs while meeting quality performance standards.
On Jan. 10, 2013, the Centers for Medicare and Medicaid Services (CMS) announced that 106 new organizations were selected to participate in the program. That’s in addition to the 87 ACOs approved in July 2012 and the 27 selected in April 2012 – bringing the total to 220 ACOs selected to participate in the MSSP. Early evidence indicates that these ACOs are decreasing costs while improving clinical outcomes.
For many of those ACOs, Medicare will be just the beginning. Private insurers such as Aetna, UnitedHealth Group, Humana, Cigna, and most Blue Cross plans are contracting with ACOs to care for more patients. Many state Medicaid programs have moved or are considering moving to accountable care.
These multiple streams of shared savings will be generated through the same ACO infrastructure needed for the MSSP, encouraging more physician-owned ACOs to form.
With the rise of ACOs, "providers are doing things in a positive way rather than a reactive way. We are seeing the beginnings of a tsunami," noted Dr. Michael Cryer, national medical director at employee benefits consultancy Aon Hewitt, in a New York Times article ("Small-picture approach flips medical economics," March 12, 2012).
According to a recent study by consulting firm Oliver Wyman entitled "The ACO Surprise," roughly 10% of the U.S. population, or from 25 million to 31 million patients, are being served by ACOs. "Successful ACOs won’t just siphon patients away from traditional providers. They will change the rules of the game," the report’s authors conclude.
Don’t miss these 2013 deadlines
CMS has just released its 2013 application cycle for 2014 (see table). The time to act is now. It will take time to understand ACOs and enlist a critical mass of informed and committed primary care providers. Though the notice of intent ("NOI") is not binding, failure to file in May is binding – you are barred from applying. Likewise, you must obtain your user ID by May 31.
The application is not hard, but it basically reflects your ACO game plan. You must be organized, have a focused care plan, and complete the application by the end of July – much earlier than last year’s deadline.
Bottom line: Do not let the start date lull you into procrastination.
Let’s have a closer look at some of the things that must be covered in the application. In addition to a culture of teamwork, patient engagement, and alignment of financial incentives, which are chief among the eight essential elements necessary for a successful ACO ("The essential elements of an ACO," Internal Medicine News, Oct. 1, 2012, p. 38), the MSSP application requires:
• Compliance with the required definitions of "ACO applicant" and "participant."
• A certification that the ACO, its ACO-provider participants, and its ACO providers/suppliers have agreed to become accountable for the quality, cost, and overall care of the Medicare fee-for-service beneficiaries assigned to the ACO.
• Establishment of a governing body.
• Implementation of a comprehensive compliance plan.
• Execution of an ACO Participation Agreement.
In addition, certain organizational milestones should be reached in advance of the application. In particular, planning for a successful ACO requires identification of a physician-champion, completion of a feasibility analysis, implementation of sufficient information technology, and internal reporting on quality and cost metrics. As in any entrepreneurial pursuit, timing is critical, and delay equates to lost potential.
Given that primary care providers are the only providers mandated for inclusion in the MSSP, it is apparent that CMS expects primary care to drive ACO value via prevention and wellness; chronic disease management; care transitions and navigation; reduced hospitalizations; and multispecialty care coordination of complex patients.
ACOs, in one form or another, are sure to be permanent fixtures in American health care, as the nation’s economy and its residents eagerly await the benefits stemming from primary care–driven innovation.
Opportunity knocks – get going!
For more information about the Medicare Shared Savings Program, click here.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, North Carolina. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612). Mr. McNeill is a practicing attorney pursuing his LLM at Duke University, currently focusing on accountable care.
Medicare Shared Savings Program deadlines
Key dates for Jan. 1, 2014, start:
| Notice of intent (NOI) accepted | May 1-31, 2013 |
| CMS user ID forms accepted | May 1-31, 2013 |
| Applications accepted | July 1-31, 2013 |
| Application approval or denial decision | Fall 2013 |
| Start date for MSSP ACO | Jan. 1, 2014 |
Source: Centers for Medicare and Medicaid Services
The Centers for Medicare and Medicaid Services has just announced key dates for the 2014 Medicare Shared Savings Program application cycle – and although the upcoming Jan. 1, 2014, start date for the MSSP seems far off, physicians should start organizing now.
Physician interest in participating is mounting, as physician-led accountable care organizations are emerging as leaders in improving quality while eradicating waste. In fact, there are now more physician-run ACOs than any other model (see chart below).
Physicians see opportunity
The MSSP has embraced the accountable care concept to improve the quality of care for Medicare fee-for-service beneficiaries. Eligible providers and suppliers may participate in the MSSP by creating or participating in an ACO. The MSSP rewards ACOs that lower their rate of growth in health care costs while meeting quality performance standards.
On Jan. 10, 2013, the Centers for Medicare and Medicaid Services (CMS) announced that 106 new organizations were selected to participate in the program. That’s in addition to the 87 ACOs approved in July 2012 and the 27 selected in April 2012 – bringing the total to 220 ACOs selected to participate in the MSSP. Early evidence indicates that these ACOs are decreasing costs while improving clinical outcomes.
For many of those ACOs, Medicare will be just the beginning. Private insurers such as Aetna, UnitedHealth Group, Humana, Cigna, and most Blue Cross plans are contracting with ACOs to care for more patients. Many state Medicaid programs have moved or are considering moving to accountable care.
These multiple streams of shared savings will be generated through the same ACO infrastructure needed for the MSSP, encouraging more physician-owned ACOs to form.
With the rise of ACOs, "providers are doing things in a positive way rather than a reactive way. We are seeing the beginnings of a tsunami," noted Dr. Michael Cryer, national medical director at employee benefits consultancy Aon Hewitt, in a New York Times article ("Small-picture approach flips medical economics," March 12, 2012).
According to a recent study by consulting firm Oliver Wyman entitled "The ACO Surprise," roughly 10% of the U.S. population, or from 25 million to 31 million patients, are being served by ACOs. "Successful ACOs won’t just siphon patients away from traditional providers. They will change the rules of the game," the report’s authors conclude.
Don’t miss these 2013 deadlines
CMS has just released its 2013 application cycle for 2014 (see table). The time to act is now. It will take time to understand ACOs and enlist a critical mass of informed and committed primary care providers. Though the notice of intent ("NOI") is not binding, failure to file in May is binding – you are barred from applying. Likewise, you must obtain your user ID by May 31.
The application is not hard, but it basically reflects your ACO game plan. You must be organized, have a focused care plan, and complete the application by the end of July – much earlier than last year’s deadline.
Bottom line: Do not let the start date lull you into procrastination.
Let’s have a closer look at some of the things that must be covered in the application. In addition to a culture of teamwork, patient engagement, and alignment of financial incentives, which are chief among the eight essential elements necessary for a successful ACO ("The essential elements of an ACO," Internal Medicine News, Oct. 1, 2012, p. 38), the MSSP application requires:
• Compliance with the required definitions of "ACO applicant" and "participant."
• A certification that the ACO, its ACO-provider participants, and its ACO providers/suppliers have agreed to become accountable for the quality, cost, and overall care of the Medicare fee-for-service beneficiaries assigned to the ACO.
• Establishment of a governing body.
• Implementation of a comprehensive compliance plan.
• Execution of an ACO Participation Agreement.
In addition, certain organizational milestones should be reached in advance of the application. In particular, planning for a successful ACO requires identification of a physician-champion, completion of a feasibility analysis, implementation of sufficient information technology, and internal reporting on quality and cost metrics. As in any entrepreneurial pursuit, timing is critical, and delay equates to lost potential.
Given that primary care providers are the only providers mandated for inclusion in the MSSP, it is apparent that CMS expects primary care to drive ACO value via prevention and wellness; chronic disease management; care transitions and navigation; reduced hospitalizations; and multispecialty care coordination of complex patients.
ACOs, in one form or another, are sure to be permanent fixtures in American health care, as the nation’s economy and its residents eagerly await the benefits stemming from primary care–driven innovation.
Opportunity knocks – get going!
For more information about the Medicare Shared Savings Program, click here.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, North Carolina. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author (bbobbitt@smithlaw.com or 919-821-6612). Mr. McNeill is a practicing attorney pursuing his LLM at Duke University, currently focusing on accountable care.
Medicare Shared Savings Program deadlines
Key dates for Jan. 1, 2014, start:
| Notice of intent (NOI) accepted | May 1-31, 2013 |
| CMS user ID forms accepted | May 1-31, 2013 |
| Applications accepted | July 1-31, 2013 |
| Application approval or denial decision | Fall 2013 |
| Start date for MSSP ACO | Jan. 1, 2014 |
Source: Centers for Medicare and Medicaid Services
ACO Insider: An Rx for rising health spending
With the looming federal "sequestration" threatening drastic spending cuts, our nation’s leaders are finally confronting the main drivers of our deficit dilemma: government "entitlement" programs such as Social Security, Medicare, and Medicaid.
Meanwhile, there is broad consensus that many of our runaway health care costs are avoidable. Our current fee-for-service health care payment system rewards higher-intensity care in greater volume, with no consequence for lack of coordination. It is a significant reason that our health care system is fragmented, inefficient, and too costly.
Federal government receipts total approximately 19% of our nation’s gross domestic product. Yet if our health care spending trends remain unchecked, by 2035 Medicare and Medicaid alone are predicted to consume 13% of GDP. By 2080, Medicare and Medicaid will consume all federal taxes, while total public and private health spending will claim almost 50% of GDP. We will have to borrow to pay for the rest of the federal government’s obligations: defense, education, transportation, etc.
As of 2012, our nation is already $16 trillion in the hole and counting. Sticking with the status quo would be a disastrous choice.
However, if medical providers work together and accept new payment incentives that reward value instead of volume, we can help fix America’s broken health care system.
That cannot be done remotely in Washington. It requires health care providers in each community cooperating to increase health care quality and cut cumulative costs.
Quality, savings, and patient satisfaction all must be achieved for providers to receive incentive payments under the new health care payment model, called "value-based reimbursement."
There is plenty of waste to be found and eliminated. Last summer, the Institute of Medicine concluded that America wastes about 30% of its health care spending – some $750 billion a year – on unneeded care, excessive paperwork, fraud, and other inefficiencies.
With basic health care becoming unaffordable for many ordinary working families and individuals, that amount of waste is unacceptable.
Although no one can hope to eradicate it overnight, it’s time somebody did something about it. America is asking physicians to step up and form teams, teams such as accountable care organizations.
By doing so, you can help ensure access, improve patient care, promote efficiency, stretch health care dollars, and make patients more of a partner in their treatment. ACOs typically receive 50% of the savings they create, which should be considered compensation to you for professional services.
As healers with a calling to serve, you have an opportunity to do your part to enhance patient care while helping to improve our nation’s fiscal health. Besides empowering, and paying, physicians to regain control of the physician/patient relationship, your patients, your profession, and your nation need you.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com, or at 919-821-6612.
With the looming federal "sequestration" threatening drastic spending cuts, our nation’s leaders are finally confronting the main drivers of our deficit dilemma: government "entitlement" programs such as Social Security, Medicare, and Medicaid.
Meanwhile, there is broad consensus that many of our runaway health care costs are avoidable. Our current fee-for-service health care payment system rewards higher-intensity care in greater volume, with no consequence for lack of coordination. It is a significant reason that our health care system is fragmented, inefficient, and too costly.
Federal government receipts total approximately 19% of our nation’s gross domestic product. Yet if our health care spending trends remain unchecked, by 2035 Medicare and Medicaid alone are predicted to consume 13% of GDP. By 2080, Medicare and Medicaid will consume all federal taxes, while total public and private health spending will claim almost 50% of GDP. We will have to borrow to pay for the rest of the federal government’s obligations: defense, education, transportation, etc.
As of 2012, our nation is already $16 trillion in the hole and counting. Sticking with the status quo would be a disastrous choice.
However, if medical providers work together and accept new payment incentives that reward value instead of volume, we can help fix America’s broken health care system.
That cannot be done remotely in Washington. It requires health care providers in each community cooperating to increase health care quality and cut cumulative costs.
Quality, savings, and patient satisfaction all must be achieved for providers to receive incentive payments under the new health care payment model, called "value-based reimbursement."
There is plenty of waste to be found and eliminated. Last summer, the Institute of Medicine concluded that America wastes about 30% of its health care spending – some $750 billion a year – on unneeded care, excessive paperwork, fraud, and other inefficiencies.
With basic health care becoming unaffordable for many ordinary working families and individuals, that amount of waste is unacceptable.
Although no one can hope to eradicate it overnight, it’s time somebody did something about it. America is asking physicians to step up and form teams, teams such as accountable care organizations.
By doing so, you can help ensure access, improve patient care, promote efficiency, stretch health care dollars, and make patients more of a partner in their treatment. ACOs typically receive 50% of the savings they create, which should be considered compensation to you for professional services.
As healers with a calling to serve, you have an opportunity to do your part to enhance patient care while helping to improve our nation’s fiscal health. Besides empowering, and paying, physicians to regain control of the physician/patient relationship, your patients, your profession, and your nation need you.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com, or at 919-821-6612.
With the looming federal "sequestration" threatening drastic spending cuts, our nation’s leaders are finally confronting the main drivers of our deficit dilemma: government "entitlement" programs such as Social Security, Medicare, and Medicaid.
Meanwhile, there is broad consensus that many of our runaway health care costs are avoidable. Our current fee-for-service health care payment system rewards higher-intensity care in greater volume, with no consequence for lack of coordination. It is a significant reason that our health care system is fragmented, inefficient, and too costly.
Federal government receipts total approximately 19% of our nation’s gross domestic product. Yet if our health care spending trends remain unchecked, by 2035 Medicare and Medicaid alone are predicted to consume 13% of GDP. By 2080, Medicare and Medicaid will consume all federal taxes, while total public and private health spending will claim almost 50% of GDP. We will have to borrow to pay for the rest of the federal government’s obligations: defense, education, transportation, etc.
As of 2012, our nation is already $16 trillion in the hole and counting. Sticking with the status quo would be a disastrous choice.
However, if medical providers work together and accept new payment incentives that reward value instead of volume, we can help fix America’s broken health care system.
That cannot be done remotely in Washington. It requires health care providers in each community cooperating to increase health care quality and cut cumulative costs.
Quality, savings, and patient satisfaction all must be achieved for providers to receive incentive payments under the new health care payment model, called "value-based reimbursement."
There is plenty of waste to be found and eliminated. Last summer, the Institute of Medicine concluded that America wastes about 30% of its health care spending – some $750 billion a year – on unneeded care, excessive paperwork, fraud, and other inefficiencies.
With basic health care becoming unaffordable for many ordinary working families and individuals, that amount of waste is unacceptable.
Although no one can hope to eradicate it overnight, it’s time somebody did something about it. America is asking physicians to step up and form teams, teams such as accountable care organizations.
By doing so, you can help ensure access, improve patient care, promote efficiency, stretch health care dollars, and make patients more of a partner in their treatment. ACOs typically receive 50% of the savings they create, which should be considered compensation to you for professional services.
As healers with a calling to serve, you have an opportunity to do your part to enhance patient care while helping to improve our nation’s fiscal health. Besides empowering, and paying, physicians to regain control of the physician/patient relationship, your patients, your profession, and your nation need you.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com, or at 919-821-6612.
Get the Government to Fund Your ACO Start-Up Costs
There seems to be a cruel irony at work: It is generally recognized that a primary care physician–based accountable care organization stands the greatest chance of successfully squeezing the waste out of our health care system – yet that same system has historically deprived primary care of the means to finance an ACO.
Worse, most of the payments that are necessary to fund and sustain ACOs are deferred for more than a year, because they come from savings created during the prior year. It is the proverbial "you can’t get there from here" problem.
How do we avoid this "Catch-22," in which the primary care–driven ACO model is best suited to meet the goals of ACOs but often is least able to afford the costs of creating ACOs?
The answer may be the federal government. There are several viable options available to have the government effectively fund 100% of your ACO start-up costs.
Consider the following:
• Meaningful use incentives. Why not have the government pay for your ACO technology platform? If you think ahead, the health information exchange you will want for your ACO will likely qualify you for stage 2 and stage 3 meaningful use incentives. You can earn up to $44,000 over 5 years from Medicare, or up to $63,750 over 6 years from Medicaid. Instead of data being a burden under fee for service, access to and exchange capability of data will be a huge asset.
You will need to make these investments anyway. If you have your ACO game plan in place, much of what you and your colleagues do to meet the meaningful use criteria can be used to fund your ACO.
• Advance payment model program. The Centers for Medicare and Medicaid Services apparently recognized the "you can’t get there from here" dilemma by creating the advance payment model program. Physician-run ACOs in rural areas have been singled out to receive enough up-front funding to completely pay for the development and implementation of the Medicare Shared Savings Program (MSSP) ACO until shared savings payments kick in.
In addition to the MSSP application, ACOs that wish to receive advance funding from the CMS Innovation Center must also complete the advance payment model application. The advance payment model is open to only two types of ACOs: ACOs that do not include any inpatient facilities and have less than $50 million in total annual revenue; and ACOs in which the only inpatient facilities are critical access hospitals and/or Medicare low-volume rural hospitals, and that have less than $80 million in total annual revenue. ACOs that are co-owned with a health plan will be ineligible, regardless of whether they also fall into one of the above categories.
The advance payment model application consists of two primary sections: the ACO’s financial characteristics; and the ACO’s investment plan.
With respect to the financial characteristics, the ACO will need to list the total annual revenue and total Medicaid revenue for each ACO participant during the preceding 3 years. The information submitted by the ACO will need to be based on either federal tax returns or audited financial statements.
The second key section of the advance payment model application is the ACO investment plan. The ACO must explain how it intends to use the advance payment funds awarded from CMS.
Specifically, the investment plan must include:
• A description of the types of staffing and infrastructure that the ACO will acquire and/or expand using the funding available through the advance payment model.
• The timing of such acquisitions or expansions, and the estimated unit costs.
• A description of how such investments build on staff and infrastructure the ACO already has or plans to acquire through its own upcoming investments.
• An explanation of how each investment will support the ACO in achieving the three-part aim of better health, better health care, and lower per capita costs for Medicare beneficiaries.
The advance payment model money may not be renewed once the initial $1 billion budgeted amount is exhausted. But if the results and return on investment are as powerful as predicted for the targeted ACOs, this could be viewed as a sound investment by CMS.
At current levels, an ACO will receive an up-front fixed amount of $250,000, a variable $36/member, and then $8/member per month. This will be repaid if there are ACO shared savings later on.
Beyond the dollars and cents impact, the APM program is vivid evidence for primary care physicians of just how promising CMS believes physician-directed ACOs are.
Primary care physicians are starting to understand the professional and financial rewards behind ACOs. They should not be dismayed by lack of funding. The payers know that funding these ACOs is a smart "investment" in reforming our inefficient and wasteful current system.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
There seems to be a cruel irony at work: It is generally recognized that a primary care physician–based accountable care organization stands the greatest chance of successfully squeezing the waste out of our health care system – yet that same system has historically deprived primary care of the means to finance an ACO.
Worse, most of the payments that are necessary to fund and sustain ACOs are deferred for more than a year, because they come from savings created during the prior year. It is the proverbial "you can’t get there from here" problem.
How do we avoid this "Catch-22," in which the primary care–driven ACO model is best suited to meet the goals of ACOs but often is least able to afford the costs of creating ACOs?
The answer may be the federal government. There are several viable options available to have the government effectively fund 100% of your ACO start-up costs.
Consider the following:
• Meaningful use incentives. Why not have the government pay for your ACO technology platform? If you think ahead, the health information exchange you will want for your ACO will likely qualify you for stage 2 and stage 3 meaningful use incentives. You can earn up to $44,000 over 5 years from Medicare, or up to $63,750 over 6 years from Medicaid. Instead of data being a burden under fee for service, access to and exchange capability of data will be a huge asset.
You will need to make these investments anyway. If you have your ACO game plan in place, much of what you and your colleagues do to meet the meaningful use criteria can be used to fund your ACO.
• Advance payment model program. The Centers for Medicare and Medicaid Services apparently recognized the "you can’t get there from here" dilemma by creating the advance payment model program. Physician-run ACOs in rural areas have been singled out to receive enough up-front funding to completely pay for the development and implementation of the Medicare Shared Savings Program (MSSP) ACO until shared savings payments kick in.
In addition to the MSSP application, ACOs that wish to receive advance funding from the CMS Innovation Center must also complete the advance payment model application. The advance payment model is open to only two types of ACOs: ACOs that do not include any inpatient facilities and have less than $50 million in total annual revenue; and ACOs in which the only inpatient facilities are critical access hospitals and/or Medicare low-volume rural hospitals, and that have less than $80 million in total annual revenue. ACOs that are co-owned with a health plan will be ineligible, regardless of whether they also fall into one of the above categories.
The advance payment model application consists of two primary sections: the ACO’s financial characteristics; and the ACO’s investment plan.
With respect to the financial characteristics, the ACO will need to list the total annual revenue and total Medicaid revenue for each ACO participant during the preceding 3 years. The information submitted by the ACO will need to be based on either federal tax returns or audited financial statements.
The second key section of the advance payment model application is the ACO investment plan. The ACO must explain how it intends to use the advance payment funds awarded from CMS.
Specifically, the investment plan must include:
• A description of the types of staffing and infrastructure that the ACO will acquire and/or expand using the funding available through the advance payment model.
• The timing of such acquisitions or expansions, and the estimated unit costs.
• A description of how such investments build on staff and infrastructure the ACO already has or plans to acquire through its own upcoming investments.
• An explanation of how each investment will support the ACO in achieving the three-part aim of better health, better health care, and lower per capita costs for Medicare beneficiaries.
The advance payment model money may not be renewed once the initial $1 billion budgeted amount is exhausted. But if the results and return on investment are as powerful as predicted for the targeted ACOs, this could be viewed as a sound investment by CMS.
At current levels, an ACO will receive an up-front fixed amount of $250,000, a variable $36/member, and then $8/member per month. This will be repaid if there are ACO shared savings later on.
Beyond the dollars and cents impact, the APM program is vivid evidence for primary care physicians of just how promising CMS believes physician-directed ACOs are.
Primary care physicians are starting to understand the professional and financial rewards behind ACOs. They should not be dismayed by lack of funding. The payers know that funding these ACOs is a smart "investment" in reforming our inefficient and wasteful current system.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
There seems to be a cruel irony at work: It is generally recognized that a primary care physician–based accountable care organization stands the greatest chance of successfully squeezing the waste out of our health care system – yet that same system has historically deprived primary care of the means to finance an ACO.
Worse, most of the payments that are necessary to fund and sustain ACOs are deferred for more than a year, because they come from savings created during the prior year. It is the proverbial "you can’t get there from here" problem.
How do we avoid this "Catch-22," in which the primary care–driven ACO model is best suited to meet the goals of ACOs but often is least able to afford the costs of creating ACOs?
The answer may be the federal government. There are several viable options available to have the government effectively fund 100% of your ACO start-up costs.
Consider the following:
• Meaningful use incentives. Why not have the government pay for your ACO technology platform? If you think ahead, the health information exchange you will want for your ACO will likely qualify you for stage 2 and stage 3 meaningful use incentives. You can earn up to $44,000 over 5 years from Medicare, or up to $63,750 over 6 years from Medicaid. Instead of data being a burden under fee for service, access to and exchange capability of data will be a huge asset.
You will need to make these investments anyway. If you have your ACO game plan in place, much of what you and your colleagues do to meet the meaningful use criteria can be used to fund your ACO.
• Advance payment model program. The Centers for Medicare and Medicaid Services apparently recognized the "you can’t get there from here" dilemma by creating the advance payment model program. Physician-run ACOs in rural areas have been singled out to receive enough up-front funding to completely pay for the development and implementation of the Medicare Shared Savings Program (MSSP) ACO until shared savings payments kick in.
In addition to the MSSP application, ACOs that wish to receive advance funding from the CMS Innovation Center must also complete the advance payment model application. The advance payment model is open to only two types of ACOs: ACOs that do not include any inpatient facilities and have less than $50 million in total annual revenue; and ACOs in which the only inpatient facilities are critical access hospitals and/or Medicare low-volume rural hospitals, and that have less than $80 million in total annual revenue. ACOs that are co-owned with a health plan will be ineligible, regardless of whether they also fall into one of the above categories.
The advance payment model application consists of two primary sections: the ACO’s financial characteristics; and the ACO’s investment plan.
With respect to the financial characteristics, the ACO will need to list the total annual revenue and total Medicaid revenue for each ACO participant during the preceding 3 years. The information submitted by the ACO will need to be based on either federal tax returns or audited financial statements.
The second key section of the advance payment model application is the ACO investment plan. The ACO must explain how it intends to use the advance payment funds awarded from CMS.
Specifically, the investment plan must include:
• A description of the types of staffing and infrastructure that the ACO will acquire and/or expand using the funding available through the advance payment model.
• The timing of such acquisitions or expansions, and the estimated unit costs.
• A description of how such investments build on staff and infrastructure the ACO already has or plans to acquire through its own upcoming investments.
• An explanation of how each investment will support the ACO in achieving the three-part aim of better health, better health care, and lower per capita costs for Medicare beneficiaries.
The advance payment model money may not be renewed once the initial $1 billion budgeted amount is exhausted. But if the results and return on investment are as powerful as predicted for the targeted ACOs, this could be viewed as a sound investment by CMS.
At current levels, an ACO will receive an up-front fixed amount of $250,000, a variable $36/member, and then $8/member per month. This will be repaid if there are ACO shared savings later on.
Beyond the dollars and cents impact, the APM program is vivid evidence for primary care physicians of just how promising CMS believes physician-directed ACOs are.
Primary care physicians are starting to understand the professional and financial rewards behind ACOs. They should not be dismayed by lack of funding. The payers know that funding these ACOs is a smart "investment" in reforming our inefficient and wasteful current system.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at bbobbitt@smithlaw.com or 919-821-6612.
From the Mailbag: Patient Engagement and ACOs
Many thanks for the thoughtful e-mails from many of you readers. Some express cautious hope, some skepticism, and all the curiosity and caring that reminds me of how fortunate I am to have been a physician advocate for my legal career.
Here is one reader’s concerns about patient engagement – or lack thereof – in accountable care organizations.
– Reader: "ACOs will never work because, once again, the patient has been left out of the equation."
We hear this quite often, and it is surely true in some cases – but not all. In fact, we are convinced that patient engagement is such an essential element necessary for every successful ACO, that an ACO should not be called an ACO without it.
Patient noncompliance is a problem, especially regarding chronic diseases and lifestyle management. It is difficult to accept a compensation model based on input on improved patient population health when that is dramatically affected by a variable outside of your control: patient adherence. But patient engagement is part of patient-centeredness, which is required by the Affordable Care Act for an ACO to qualify for CMS’ Shared Savings Program.
So, what can an ACO do to engage patients?
Consider the following approaches:
– The patient compact. Some ACOs, such as the Geisinger Clinic, engage the patient through a compact, or agreement. It may involve a written commitment by the patient to be responsible for his or her own wellness or chronic care management, coupled with rewards for so doing, education, tools, self-care modules, and shared decision-making empowerment. The providers will need to embrace the importance of patient involvement and hold up their end of the engagement bargain.
– Benefit differentials for lifestyle choices. The financial impact of many volitional patient lifestyle choices is actuarially measurable. A logical consequence of the patient choice could be a benefit or financial differential reflecting at least partially these avoidable health care costs.
– Stay in contact. A Kaiser Permanente study of more than 35,000 hypertensive and diabetic patients found that the blood pressure and cholesterol levels for those who engaged in secure messaging were better than for those who did not.
– More time with your patients. Develop personal relationships. One ACO saw its results jump when its primary care physicians started using Biosignia’s "Know Your Number," a computer-generated graphic depiction of a patient’s health risks based on lab results and the Framingham Study. It is used by the treating physician at the point of care.
– Patient remote access to test results. This can be achieved with tools such as a web portal with multiple functions.
– Care navigators. We predict that the demands for care navigators, or coordinators, will skyrocket as ACOs take hold. Their use will include home visits. This may be the best patient engagement method.
– Empathetic listening. In curriculum and residency programs of medical schools, the paternalistic model is yielding to empathetic listening and communication skills in physician training.
– Educational materials. This consists of patient-friendly educational material that explains the benefits of being linked to a medical home.
I agree so much with this reader’s assertion that an ACO without patient engagement will fail, that I consider it an essential, almost definitional, element of every successful ACO. It is crucial that we emphasize the role of the patient. It is truly the "other shoe" that must fall for the new outcomes-based health care to succeed.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact Mr. Bobbit at bbobbitt@smithlaw.com, or at 919-821-6612.
Many thanks for the thoughtful e-mails from many of you readers. Some express cautious hope, some skepticism, and all the curiosity and caring that reminds me of how fortunate I am to have been a physician advocate for my legal career.
Here is one reader’s concerns about patient engagement – or lack thereof – in accountable care organizations.
– Reader: "ACOs will never work because, once again, the patient has been left out of the equation."
We hear this quite often, and it is surely true in some cases – but not all. In fact, we are convinced that patient engagement is such an essential element necessary for every successful ACO, that an ACO should not be called an ACO without it.
Patient noncompliance is a problem, especially regarding chronic diseases and lifestyle management. It is difficult to accept a compensation model based on input on improved patient population health when that is dramatically affected by a variable outside of your control: patient adherence. But patient engagement is part of patient-centeredness, which is required by the Affordable Care Act for an ACO to qualify for CMS’ Shared Savings Program.
So, what can an ACO do to engage patients?
Consider the following approaches:
– The patient compact. Some ACOs, such as the Geisinger Clinic, engage the patient through a compact, or agreement. It may involve a written commitment by the patient to be responsible for his or her own wellness or chronic care management, coupled with rewards for so doing, education, tools, self-care modules, and shared decision-making empowerment. The providers will need to embrace the importance of patient involvement and hold up their end of the engagement bargain.
– Benefit differentials for lifestyle choices. The financial impact of many volitional patient lifestyle choices is actuarially measurable. A logical consequence of the patient choice could be a benefit or financial differential reflecting at least partially these avoidable health care costs.
– Stay in contact. A Kaiser Permanente study of more than 35,000 hypertensive and diabetic patients found that the blood pressure and cholesterol levels for those who engaged in secure messaging were better than for those who did not.
– More time with your patients. Develop personal relationships. One ACO saw its results jump when its primary care physicians started using Biosignia’s "Know Your Number," a computer-generated graphic depiction of a patient’s health risks based on lab results and the Framingham Study. It is used by the treating physician at the point of care.
– Patient remote access to test results. This can be achieved with tools such as a web portal with multiple functions.
– Care navigators. We predict that the demands for care navigators, or coordinators, will skyrocket as ACOs take hold. Their use will include home visits. This may be the best patient engagement method.
– Empathetic listening. In curriculum and residency programs of medical schools, the paternalistic model is yielding to empathetic listening and communication skills in physician training.
– Educational materials. This consists of patient-friendly educational material that explains the benefits of being linked to a medical home.
I agree so much with this reader’s assertion that an ACO without patient engagement will fail, that I consider it an essential, almost definitional, element of every successful ACO. It is crucial that we emphasize the role of the patient. It is truly the "other shoe" that must fall for the new outcomes-based health care to succeed.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact Mr. Bobbit at bbobbitt@smithlaw.com, or at 919-821-6612.
Many thanks for the thoughtful e-mails from many of you readers. Some express cautious hope, some skepticism, and all the curiosity and caring that reminds me of how fortunate I am to have been a physician advocate for my legal career.
Here is one reader’s concerns about patient engagement – or lack thereof – in accountable care organizations.
– Reader: "ACOs will never work because, once again, the patient has been left out of the equation."
We hear this quite often, and it is surely true in some cases – but not all. In fact, we are convinced that patient engagement is such an essential element necessary for every successful ACO, that an ACO should not be called an ACO without it.
Patient noncompliance is a problem, especially regarding chronic diseases and lifestyle management. It is difficult to accept a compensation model based on input on improved patient population health when that is dramatically affected by a variable outside of your control: patient adherence. But patient engagement is part of patient-centeredness, which is required by the Affordable Care Act for an ACO to qualify for CMS’ Shared Savings Program.
So, what can an ACO do to engage patients?
Consider the following approaches:
– The patient compact. Some ACOs, such as the Geisinger Clinic, engage the patient through a compact, or agreement. It may involve a written commitment by the patient to be responsible for his or her own wellness or chronic care management, coupled with rewards for so doing, education, tools, self-care modules, and shared decision-making empowerment. The providers will need to embrace the importance of patient involvement and hold up their end of the engagement bargain.
– Benefit differentials for lifestyle choices. The financial impact of many volitional patient lifestyle choices is actuarially measurable. A logical consequence of the patient choice could be a benefit or financial differential reflecting at least partially these avoidable health care costs.
– Stay in contact. A Kaiser Permanente study of more than 35,000 hypertensive and diabetic patients found that the blood pressure and cholesterol levels for those who engaged in secure messaging were better than for those who did not.
– More time with your patients. Develop personal relationships. One ACO saw its results jump when its primary care physicians started using Biosignia’s "Know Your Number," a computer-generated graphic depiction of a patient’s health risks based on lab results and the Framingham Study. It is used by the treating physician at the point of care.
– Patient remote access to test results. This can be achieved with tools such as a web portal with multiple functions.
– Care navigators. We predict that the demands for care navigators, or coordinators, will skyrocket as ACOs take hold. Their use will include home visits. This may be the best patient engagement method.
– Empathetic listening. In curriculum and residency programs of medical schools, the paternalistic model is yielding to empathetic listening and communication skills in physician training.
– Educational materials. This consists of patient-friendly educational material that explains the benefits of being linked to a medical home.
I agree so much with this reader’s assertion that an ACO without patient engagement will fail, that I consider it an essential, almost definitional, element of every successful ACO. It is crucial that we emphasize the role of the patient. It is truly the "other shoe" that must fall for the new outcomes-based health care to succeed.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact Mr. Bobbit at bbobbitt@smithlaw.com, or at 919-821-6612.