User login
Certain hairstyles can predispose patients to traction alopecia
ORLANDO – When it comes to preventing alopecia, it may be best to advise patients against certain trendy hairstyles that can cause early hair loss.
At the Orlando Dermatology Aesthetic and Clinical Conference, Dr. Wendy Roberts, a dermatologist practicing in Rancho Mirage, Calif., spoke about the risks of traction alopecia associated with some hairstyles and why it’s in patients’ best interest to avoid them if they don’t want to experience premature hair loss.
Dr. Roberts brings up the topic of hair loss with patients during the full-body exam. Full-body skin exams are “opportunities for us, as the skin and hair experts, to speak to our patients about hair loss, [but] it’s rarely asked about,” she said. “Typically, what I do is start my full-body skin exam from the head and I always ask the question right away ‘How’s your hair? Are you having any problems with your hair? How’s your scalp?’ And about 50% of the time, there’s a positive answer or an interest in learning more about it.”
To avoid traction alopecia, caused frequently by intense pulling or pressure on the hair follicles, patients should be advised against braiding their hair or, for male patients, styling their hair in a “man bun.” For braids, the tightness of the braid and pulling along the hairlines will cause intense pressure on follicles over time that can lead to hair loss. For the man bun, Dr. Roberts noted that dermatologists will likely see an uptick in male patients with traction alopecia as this hairstyle becomes more popular.
In the evaluation and treatment of traction alopecia – as with any form of alopecia – clinical presentation, ethnicity, and the age of the patient should be considered, Dr. Roberts said. Additionally, collection of evidence – hair pulls, biopsy, dermoscopy, and lab work should be obtained.
Labs will check for iron levels and anemia, thyroid disease, vitamin D deficiency, and perhaps signs of a connective tissue disorder, she noted. “It’s staggering the amount of African-American women who are deficient in vitamin D, [and] there is some soft evidence that perhaps vitamin D deficiency may be a culprit in some of the clinical signs of discoid lupus erythematosus, [so] check the vitamin D and zinc levels.”
After making a diagnosis, it is important to quickly begin rigorous treatment of the alopecia. Aggressive treatment is “the bottom line,” Dr. Roberts emphasized, “because people are losing their hair and when they come to you, they’ve really had enough.”
She did not report any relevant financial disclosures.
ORLANDO – When it comes to preventing alopecia, it may be best to advise patients against certain trendy hairstyles that can cause early hair loss.
At the Orlando Dermatology Aesthetic and Clinical Conference, Dr. Wendy Roberts, a dermatologist practicing in Rancho Mirage, Calif., spoke about the risks of traction alopecia associated with some hairstyles and why it’s in patients’ best interest to avoid them if they don’t want to experience premature hair loss.
Dr. Roberts brings up the topic of hair loss with patients during the full-body exam. Full-body skin exams are “opportunities for us, as the skin and hair experts, to speak to our patients about hair loss, [but] it’s rarely asked about,” she said. “Typically, what I do is start my full-body skin exam from the head and I always ask the question right away ‘How’s your hair? Are you having any problems with your hair? How’s your scalp?’ And about 50% of the time, there’s a positive answer or an interest in learning more about it.”
To avoid traction alopecia, caused frequently by intense pulling or pressure on the hair follicles, patients should be advised against braiding their hair or, for male patients, styling their hair in a “man bun.” For braids, the tightness of the braid and pulling along the hairlines will cause intense pressure on follicles over time that can lead to hair loss. For the man bun, Dr. Roberts noted that dermatologists will likely see an uptick in male patients with traction alopecia as this hairstyle becomes more popular.
In the evaluation and treatment of traction alopecia – as with any form of alopecia – clinical presentation, ethnicity, and the age of the patient should be considered, Dr. Roberts said. Additionally, collection of evidence – hair pulls, biopsy, dermoscopy, and lab work should be obtained.
Labs will check for iron levels and anemia, thyroid disease, vitamin D deficiency, and perhaps signs of a connective tissue disorder, she noted. “It’s staggering the amount of African-American women who are deficient in vitamin D, [and] there is some soft evidence that perhaps vitamin D deficiency may be a culprit in some of the clinical signs of discoid lupus erythematosus, [so] check the vitamin D and zinc levels.”
After making a diagnosis, it is important to quickly begin rigorous treatment of the alopecia. Aggressive treatment is “the bottom line,” Dr. Roberts emphasized, “because people are losing their hair and when they come to you, they’ve really had enough.”
She did not report any relevant financial disclosures.
ORLANDO – When it comes to preventing alopecia, it may be best to advise patients against certain trendy hairstyles that can cause early hair loss.
At the Orlando Dermatology Aesthetic and Clinical Conference, Dr. Wendy Roberts, a dermatologist practicing in Rancho Mirage, Calif., spoke about the risks of traction alopecia associated with some hairstyles and why it’s in patients’ best interest to avoid them if they don’t want to experience premature hair loss.
Dr. Roberts brings up the topic of hair loss with patients during the full-body exam. Full-body skin exams are “opportunities for us, as the skin and hair experts, to speak to our patients about hair loss, [but] it’s rarely asked about,” she said. “Typically, what I do is start my full-body skin exam from the head and I always ask the question right away ‘How’s your hair? Are you having any problems with your hair? How’s your scalp?’ And about 50% of the time, there’s a positive answer or an interest in learning more about it.”
To avoid traction alopecia, caused frequently by intense pulling or pressure on the hair follicles, patients should be advised against braiding their hair or, for male patients, styling their hair in a “man bun.” For braids, the tightness of the braid and pulling along the hairlines will cause intense pressure on follicles over time that can lead to hair loss. For the man bun, Dr. Roberts noted that dermatologists will likely see an uptick in male patients with traction alopecia as this hairstyle becomes more popular.
In the evaluation and treatment of traction alopecia – as with any form of alopecia – clinical presentation, ethnicity, and the age of the patient should be considered, Dr. Roberts said. Additionally, collection of evidence – hair pulls, biopsy, dermoscopy, and lab work should be obtained.
Labs will check for iron levels and anemia, thyroid disease, vitamin D deficiency, and perhaps signs of a connective tissue disorder, she noted. “It’s staggering the amount of African-American women who are deficient in vitamin D, [and] there is some soft evidence that perhaps vitamin D deficiency may be a culprit in some of the clinical signs of discoid lupus erythematosus, [so] check the vitamin D and zinc levels.”
After making a diagnosis, it is important to quickly begin rigorous treatment of the alopecia. Aggressive treatment is “the bottom line,” Dr. Roberts emphasized, “because people are losing their hair and when they come to you, they’ve really had enough.”
She did not report any relevant financial disclosures.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Aesthetics in men: what dermatologists need to know
ORLANDO – The increasing frequency with which men are seeking cosmetic procedures means that dermatologists need to have a firm grasp on the important, but often overlooked differences between treating their male and female patients.
“Cosmetic procedures performed on men have increased by 273% since 1997 [and] in the last year, about 10% of all cosmetic procedures were performed on men,” Dr. Whitney Bowe said at the Orlando Dermatology Aesthetic and Clinical Conference. “We want to make sure to keep in mind that the male anatomy is very different from the female anatomy, and so you want to make sure not to feminize the male face.”
In an interview at the meeting, Dr. Terrence Keaney of George Washington University, Washington, added that it’s important to take time with your male patients to really understand what they are looking for and how to deliver the most effective treatment in the most timely manner for them.
“Men are a harder nut to crack – they’re not really sure of what procedure they want because they just don’t know about them yet, so their initial concerns are less specific,” Dr. Keaney said. “You have to tease out what men are looking for [because] they’re less likely to be forthcoming about what’s bothering them.”
The two most commonly sought procedures by male patients are neuromodulators and dermal fillers, according to Dr. Bowe, a dermatologist at Mount Sinai Hospital, New York. When it comes to the former, it’s important to remember that men have flatter, more low-set brow lines that rest along the orbital rim. While women typically prefer to have a defined arch to their brow – “like what you’d see with Megan Fox or Kim Kardashian,” Dr. Bowe clarified – this can look highly feminine in male patients, and can lead to dissatisfaction with the overall treatment results.
Furthermore, in order to achieve clinically effective results, men tend to require double the amount of neuromodulator as women. It’s important for dermatologists – and, perhaps more importantly, their staff – to not only use the appropriate amount of neuromodulator, but also discuss what the true financial costs of such procedures will be with male patients ahead of time.
“You want to make sure that you’re dosing [men] appropriately, but it’s also important to consider that when you’re discussing budget,” Dr. Bowe said. “If your staff is used to quoting a certain budget range, for men, that range might actually be doubled as compared to women.”
Men typically seek dermal filler procedures to rejuvenate the area underneath the eyes. The tear trough is a particular area of concern because of its ability to make men look perpetually tired, due to loss of soft tissue in that area – “the greatest reduction in soft tissue as compared to anywhere else on their face,” Dr. Bowe pointed out.
Procedures for the jawline are also becoming increasingly routine among men and are sought after to provide more definition, while also allowing the skin to drape onto the neck. This helps reduce the appearance of girth and mitigate physically uncomfortable situations, such as wearing a button-down shirt that becomes very tight around the neck. For both this and rejuvenation of the tear trough, Dr. Bowe recommends hyaluronic acid fillers that have a high G prime, or poly-L-lactic acid (PLLA).
The other methods for dealing with submental fat in men are deoxycholic acid (Kybella), approved as a treatment for adults with moderate to severe submental fat in 2015; and cryolipolysis. With deoxycholic acid, Dr. Bowe explained, dermatologists can customize the approach because it is administered in a syringe, “something we’re very comfortable doing in our field.” However, the major drawbacks are that it’s difficult to address the lateral deposits of fat when getting close to the marginal mandibular nerve, along with significant swelling that occurs after that procedure for up to 2 weeks.
With cryolipolysis, new applicators on the market have proven effective for treating both submental fat and the lateral fat with minimal postprocedure downtime. However, applicators tend to be “one size fits all,” so if it doesn’t work for a patient, the procedure would have to be done with deoxycholic acid.
A consideration when treating male patients with fillers is that the cheek is more flat in men, who tend to have a flatter ogee curve, so an “upsweeping cheekbone [is] a feminizing look to a male patient” that dermatologists should be keen to avoid, Dr. Bowe said.
In addition, “men tend to have a higher degree of vasculature underneath the skin surface – in fact, Doppler studies show that they tend to have more vessels in their skin – and it’s most likely a result of the fact that they have increased numbers of coarse terminal hairs [which] need to sustain that growth,” cautioned Dr. Bowe. “But that also clinically translates into the fact that they’re much more prone to bruising, so that’s something you need to be very upfront with your male patients prior to engaging in any kind of injectables.”
While less common, noninvasive body contouring is something men often look for, too. Cryolipolysis can also be used for contouring, said Dr. Keaney, while Dr. Bowe advises keeping the golden ratio of shoulder-to-waist size in mind when consulting male patients about ways to improve their physique.
“There’s the ‘Adonis Ratio’ in which a man’s shoulder circumference is 1.68 times the size of his waist, and if you achieve that ratio it’s considered the ideal male physique,” Dr. Bowe explained. “By targeting the muffin top and the love handles [to] minimize the waist circumference, we can get patients closer to that ideal aesthetic.”
Dr. Keaney, who is also with the Washington Institute of Dermatologic Laser Surgery, added that in a not-yet-published study that he conducted, which surveyed 600 men about their most prominent aging concerns, hair loss was No. 1 “by far.” Dermatologists should know ahead of time that alopecia will be a frequent topic of discussion with men, far more so than with female patients, he pointed out.
Dr. Bowe disclosed consultancy relationships with Allergan and Galderma. Dr. Keaney disclosed relationships with Allergan, Restoration Robotics, and Skinceuticals.
ORLANDO – The increasing frequency with which men are seeking cosmetic procedures means that dermatologists need to have a firm grasp on the important, but often overlooked differences between treating their male and female patients.
“Cosmetic procedures performed on men have increased by 273% since 1997 [and] in the last year, about 10% of all cosmetic procedures were performed on men,” Dr. Whitney Bowe said at the Orlando Dermatology Aesthetic and Clinical Conference. “We want to make sure to keep in mind that the male anatomy is very different from the female anatomy, and so you want to make sure not to feminize the male face.”
In an interview at the meeting, Dr. Terrence Keaney of George Washington University, Washington, added that it’s important to take time with your male patients to really understand what they are looking for and how to deliver the most effective treatment in the most timely manner for them.
“Men are a harder nut to crack – they’re not really sure of what procedure they want because they just don’t know about them yet, so their initial concerns are less specific,” Dr. Keaney said. “You have to tease out what men are looking for [because] they’re less likely to be forthcoming about what’s bothering them.”
The two most commonly sought procedures by male patients are neuromodulators and dermal fillers, according to Dr. Bowe, a dermatologist at Mount Sinai Hospital, New York. When it comes to the former, it’s important to remember that men have flatter, more low-set brow lines that rest along the orbital rim. While women typically prefer to have a defined arch to their brow – “like what you’d see with Megan Fox or Kim Kardashian,” Dr. Bowe clarified – this can look highly feminine in male patients, and can lead to dissatisfaction with the overall treatment results.
Furthermore, in order to achieve clinically effective results, men tend to require double the amount of neuromodulator as women. It’s important for dermatologists – and, perhaps more importantly, their staff – to not only use the appropriate amount of neuromodulator, but also discuss what the true financial costs of such procedures will be with male patients ahead of time.
“You want to make sure that you’re dosing [men] appropriately, but it’s also important to consider that when you’re discussing budget,” Dr. Bowe said. “If your staff is used to quoting a certain budget range, for men, that range might actually be doubled as compared to women.”
Men typically seek dermal filler procedures to rejuvenate the area underneath the eyes. The tear trough is a particular area of concern because of its ability to make men look perpetually tired, due to loss of soft tissue in that area – “the greatest reduction in soft tissue as compared to anywhere else on their face,” Dr. Bowe pointed out.
Procedures for the jawline are also becoming increasingly routine among men and are sought after to provide more definition, while also allowing the skin to drape onto the neck. This helps reduce the appearance of girth and mitigate physically uncomfortable situations, such as wearing a button-down shirt that becomes very tight around the neck. For both this and rejuvenation of the tear trough, Dr. Bowe recommends hyaluronic acid fillers that have a high G prime, or poly-L-lactic acid (PLLA).
The other methods for dealing with submental fat in men are deoxycholic acid (Kybella), approved as a treatment for adults with moderate to severe submental fat in 2015; and cryolipolysis. With deoxycholic acid, Dr. Bowe explained, dermatologists can customize the approach because it is administered in a syringe, “something we’re very comfortable doing in our field.” However, the major drawbacks are that it’s difficult to address the lateral deposits of fat when getting close to the marginal mandibular nerve, along with significant swelling that occurs after that procedure for up to 2 weeks.
With cryolipolysis, new applicators on the market have proven effective for treating both submental fat and the lateral fat with minimal postprocedure downtime. However, applicators tend to be “one size fits all,” so if it doesn’t work for a patient, the procedure would have to be done with deoxycholic acid.
A consideration when treating male patients with fillers is that the cheek is more flat in men, who tend to have a flatter ogee curve, so an “upsweeping cheekbone [is] a feminizing look to a male patient” that dermatologists should be keen to avoid, Dr. Bowe said.
In addition, “men tend to have a higher degree of vasculature underneath the skin surface – in fact, Doppler studies show that they tend to have more vessels in their skin – and it’s most likely a result of the fact that they have increased numbers of coarse terminal hairs [which] need to sustain that growth,” cautioned Dr. Bowe. “But that also clinically translates into the fact that they’re much more prone to bruising, so that’s something you need to be very upfront with your male patients prior to engaging in any kind of injectables.”
While less common, noninvasive body contouring is something men often look for, too. Cryolipolysis can also be used for contouring, said Dr. Keaney, while Dr. Bowe advises keeping the golden ratio of shoulder-to-waist size in mind when consulting male patients about ways to improve their physique.
“There’s the ‘Adonis Ratio’ in which a man’s shoulder circumference is 1.68 times the size of his waist, and if you achieve that ratio it’s considered the ideal male physique,” Dr. Bowe explained. “By targeting the muffin top and the love handles [to] minimize the waist circumference, we can get patients closer to that ideal aesthetic.”
Dr. Keaney, who is also with the Washington Institute of Dermatologic Laser Surgery, added that in a not-yet-published study that he conducted, which surveyed 600 men about their most prominent aging concerns, hair loss was No. 1 “by far.” Dermatologists should know ahead of time that alopecia will be a frequent topic of discussion with men, far more so than with female patients, he pointed out.
Dr. Bowe disclosed consultancy relationships with Allergan and Galderma. Dr. Keaney disclosed relationships with Allergan, Restoration Robotics, and Skinceuticals.
ORLANDO – The increasing frequency with which men are seeking cosmetic procedures means that dermatologists need to have a firm grasp on the important, but often overlooked differences between treating their male and female patients.
“Cosmetic procedures performed on men have increased by 273% since 1997 [and] in the last year, about 10% of all cosmetic procedures were performed on men,” Dr. Whitney Bowe said at the Orlando Dermatology Aesthetic and Clinical Conference. “We want to make sure to keep in mind that the male anatomy is very different from the female anatomy, and so you want to make sure not to feminize the male face.”
In an interview at the meeting, Dr. Terrence Keaney of George Washington University, Washington, added that it’s important to take time with your male patients to really understand what they are looking for and how to deliver the most effective treatment in the most timely manner for them.
“Men are a harder nut to crack – they’re not really sure of what procedure they want because they just don’t know about them yet, so their initial concerns are less specific,” Dr. Keaney said. “You have to tease out what men are looking for [because] they’re less likely to be forthcoming about what’s bothering them.”
The two most commonly sought procedures by male patients are neuromodulators and dermal fillers, according to Dr. Bowe, a dermatologist at Mount Sinai Hospital, New York. When it comes to the former, it’s important to remember that men have flatter, more low-set brow lines that rest along the orbital rim. While women typically prefer to have a defined arch to their brow – “like what you’d see with Megan Fox or Kim Kardashian,” Dr. Bowe clarified – this can look highly feminine in male patients, and can lead to dissatisfaction with the overall treatment results.
Furthermore, in order to achieve clinically effective results, men tend to require double the amount of neuromodulator as women. It’s important for dermatologists – and, perhaps more importantly, their staff – to not only use the appropriate amount of neuromodulator, but also discuss what the true financial costs of such procedures will be with male patients ahead of time.
“You want to make sure that you’re dosing [men] appropriately, but it’s also important to consider that when you’re discussing budget,” Dr. Bowe said. “If your staff is used to quoting a certain budget range, for men, that range might actually be doubled as compared to women.”
Men typically seek dermal filler procedures to rejuvenate the area underneath the eyes. The tear trough is a particular area of concern because of its ability to make men look perpetually tired, due to loss of soft tissue in that area – “the greatest reduction in soft tissue as compared to anywhere else on their face,” Dr. Bowe pointed out.
Procedures for the jawline are also becoming increasingly routine among men and are sought after to provide more definition, while also allowing the skin to drape onto the neck. This helps reduce the appearance of girth and mitigate physically uncomfortable situations, such as wearing a button-down shirt that becomes very tight around the neck. For both this and rejuvenation of the tear trough, Dr. Bowe recommends hyaluronic acid fillers that have a high G prime, or poly-L-lactic acid (PLLA).
The other methods for dealing with submental fat in men are deoxycholic acid (Kybella), approved as a treatment for adults with moderate to severe submental fat in 2015; and cryolipolysis. With deoxycholic acid, Dr. Bowe explained, dermatologists can customize the approach because it is administered in a syringe, “something we’re very comfortable doing in our field.” However, the major drawbacks are that it’s difficult to address the lateral deposits of fat when getting close to the marginal mandibular nerve, along with significant swelling that occurs after that procedure for up to 2 weeks.
With cryolipolysis, new applicators on the market have proven effective for treating both submental fat and the lateral fat with minimal postprocedure downtime. However, applicators tend to be “one size fits all,” so if it doesn’t work for a patient, the procedure would have to be done with deoxycholic acid.
A consideration when treating male patients with fillers is that the cheek is more flat in men, who tend to have a flatter ogee curve, so an “upsweeping cheekbone [is] a feminizing look to a male patient” that dermatologists should be keen to avoid, Dr. Bowe said.
In addition, “men tend to have a higher degree of vasculature underneath the skin surface – in fact, Doppler studies show that they tend to have more vessels in their skin – and it’s most likely a result of the fact that they have increased numbers of coarse terminal hairs [which] need to sustain that growth,” cautioned Dr. Bowe. “But that also clinically translates into the fact that they’re much more prone to bruising, so that’s something you need to be very upfront with your male patients prior to engaging in any kind of injectables.”
While less common, noninvasive body contouring is something men often look for, too. Cryolipolysis can also be used for contouring, said Dr. Keaney, while Dr. Bowe advises keeping the golden ratio of shoulder-to-waist size in mind when consulting male patients about ways to improve their physique.
“There’s the ‘Adonis Ratio’ in which a man’s shoulder circumference is 1.68 times the size of his waist, and if you achieve that ratio it’s considered the ideal male physique,” Dr. Bowe explained. “By targeting the muffin top and the love handles [to] minimize the waist circumference, we can get patients closer to that ideal aesthetic.”
Dr. Keaney, who is also with the Washington Institute of Dermatologic Laser Surgery, added that in a not-yet-published study that he conducted, which surveyed 600 men about their most prominent aging concerns, hair loss was No. 1 “by far.” Dermatologists should know ahead of time that alopecia will be a frequent topic of discussion with men, far more so than with female patients, he pointed out.
Dr. Bowe disclosed consultancy relationships with Allergan and Galderma. Dr. Keaney disclosed relationships with Allergan, Restoration Robotics, and Skinceuticals.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Cosmeceuticals and rosacea: which ones are worth your time
ORLANDO – When treating rosacea, consider adding cosmeceuticals to more conventional prescriptions and over-the-counter treatments to improve the management of symptoms and patient satisfaction.
The recommendation comes from Dr. Julie Harper, a dermatologist at the University of Alabama-Birmingham, who spoke about the benefits of cosmeceuticals for rosacea at the Orlando Dermatology Aesthetic and Clinical Conference.
“I see about 40 people a day on my regular dermatology days [and] it’s easy to just write a prescription and hand it to that rosacea patient, but you do them a big disservice when you do that,” explained Dr. Harper. “We’ve got to talk about triggers, about skin care, about sun protection, [and] start that discussion from there.”
The most-important point for patients to understand is the main triggers of their rosacea, which can include ultraviolet light, spices, stress, exercise, heat, barrier disruption, and Demodex. Since sunlight is the No. 1 trigger for rosacea, treatment strategies often need to start there and revolve around how to avoid or manage the condition based on sun exposure.
As for cosmeceuticals, Dr. Harper focused on three types that have been shown to be effective against rosacea: niacinamide, licorice, and green tea.
The available data on niacinamide for rosacea are primarily from the 2006 Nicomide Improvement in Clinical Outcomes Study (NICOS), an open-label, multicenter, prospective cohort study that recruited people with acne vulgaris and acne rosacea from 100 centers and administered 750 mg of niacinamide with zinc and copper, while some got niacinamide plus oral antibiotics. The 49 people with rosacea who were enrolled received baseline assessments in the clinic, but 4-week and 8-week follow-ups were done via self-reported surveys (Cutis. 2006 Jan;77[1 Suppl]:17-28).
At 8 weeks, “75% of the rosacea group reported that appearance of their rosacea was moderately or much better [and] that there was also significant reduction in inflammatory lesions,” Dr. Harper said. “There was not a big difference in the group that had an oral antibiotic and niacinamide, versus niacinamide without the oral antibiotic,” although the design of the study leaves the findings somewhat questionable, she noted.
Topical niacinamide also has the potential to benefit certain rosacea patients, she said, referring to a 2005 study examining the effects of a niacinamide-containing moisturizer on the face and one forearm of 50 patients over 4 weeks. The primary outcome of the trial was barrier function, as measured by a dimethyl sulfoxide (DMSO) chemical probe (Cutis. 2005 Aug;76[2]:135-41).
While the results of this trial are “difficult” to interpret – due largely to the lack of any real measurement of facial improvement in barrier function and the confusion over whether any improvement on the forearm can be attributed to the niacinamide specifically or to the moisturizer itself – “long story short, niacinamide did seem to help the barrier function in this particular study,” Dr. Harper said. The takeaway, therefore, is that topical niacinamide treatments may offer some value to certain patients.
Moving on to licorice, Dr. Harper discussed an open label study recently published online in the Journal of the European Academy of Dermatology and Venereology, in which subjects were given a complete skin care system – which contained a cleanser, a day cream, a night cream, and a concealer product containing licochalcone A (licorice extract). They were evaluated over a period of 8 weeks for improvement in erythema, burning, stinging, tingling, and tightness, all of which were measured at baseline (J Eur Acad Dermatol Venereol. 2016 Feb;30 Suppl 1:21-7).
Results showed “improvement of statistical significance,” Dr. Harper said. “All groups had improvement over time, and did better at 8 weeks than at 4 weeks [although] the rosacea group did not reach statistical significance until week 8.”
Finally, with green tea, Dr. Harper pointed to a 2010 randomized double-blind split-face study of just four healthy individuals with erythema and telangiectasia of the face, treated for 6 weeks with a cream containing epigallocatechin-3-gallate (EGCG), the major catechin found in green tea, on one side of their face; a vehicle cream was applied to the other side and punch biopsies were performed to determine improvements (Int J Clin Exp Pathol. 2010;3[7]:705-9). EGCG cream was used because of its “antioxidant, immunomodulatory, photoprotective, antiangiogenic – that’s the standout here, that’s what we really need – and anti-inflammatory properties,” Dr. Harper said.
While biopsies did not reveal any changes to facial vasculature, there “was a significant reduction in hypoxia-inducible factor-1 and VEGF [vascular endothelial growth factor],” which are both markers of angiogenesis – indicating some degree of usefulness against rosacea, Dr. Harper said. However, a longer, more definitive study would be needed to substantiate these findings, she added.
Dr. Harper did not report any relevant financial disclosures.
ORLANDO – When treating rosacea, consider adding cosmeceuticals to more conventional prescriptions and over-the-counter treatments to improve the management of symptoms and patient satisfaction.
The recommendation comes from Dr. Julie Harper, a dermatologist at the University of Alabama-Birmingham, who spoke about the benefits of cosmeceuticals for rosacea at the Orlando Dermatology Aesthetic and Clinical Conference.
“I see about 40 people a day on my regular dermatology days [and] it’s easy to just write a prescription and hand it to that rosacea patient, but you do them a big disservice when you do that,” explained Dr. Harper. “We’ve got to talk about triggers, about skin care, about sun protection, [and] start that discussion from there.”
The most-important point for patients to understand is the main triggers of their rosacea, which can include ultraviolet light, spices, stress, exercise, heat, barrier disruption, and Demodex. Since sunlight is the No. 1 trigger for rosacea, treatment strategies often need to start there and revolve around how to avoid or manage the condition based on sun exposure.
As for cosmeceuticals, Dr. Harper focused on three types that have been shown to be effective against rosacea: niacinamide, licorice, and green tea.
The available data on niacinamide for rosacea are primarily from the 2006 Nicomide Improvement in Clinical Outcomes Study (NICOS), an open-label, multicenter, prospective cohort study that recruited people with acne vulgaris and acne rosacea from 100 centers and administered 750 mg of niacinamide with zinc and copper, while some got niacinamide plus oral antibiotics. The 49 people with rosacea who were enrolled received baseline assessments in the clinic, but 4-week and 8-week follow-ups were done via self-reported surveys (Cutis. 2006 Jan;77[1 Suppl]:17-28).
At 8 weeks, “75% of the rosacea group reported that appearance of their rosacea was moderately or much better [and] that there was also significant reduction in inflammatory lesions,” Dr. Harper said. “There was not a big difference in the group that had an oral antibiotic and niacinamide, versus niacinamide without the oral antibiotic,” although the design of the study leaves the findings somewhat questionable, she noted.
Topical niacinamide also has the potential to benefit certain rosacea patients, she said, referring to a 2005 study examining the effects of a niacinamide-containing moisturizer on the face and one forearm of 50 patients over 4 weeks. The primary outcome of the trial was barrier function, as measured by a dimethyl sulfoxide (DMSO) chemical probe (Cutis. 2005 Aug;76[2]:135-41).
While the results of this trial are “difficult” to interpret – due largely to the lack of any real measurement of facial improvement in barrier function and the confusion over whether any improvement on the forearm can be attributed to the niacinamide specifically or to the moisturizer itself – “long story short, niacinamide did seem to help the barrier function in this particular study,” Dr. Harper said. The takeaway, therefore, is that topical niacinamide treatments may offer some value to certain patients.
Moving on to licorice, Dr. Harper discussed an open label study recently published online in the Journal of the European Academy of Dermatology and Venereology, in which subjects were given a complete skin care system – which contained a cleanser, a day cream, a night cream, and a concealer product containing licochalcone A (licorice extract). They were evaluated over a period of 8 weeks for improvement in erythema, burning, stinging, tingling, and tightness, all of which were measured at baseline (J Eur Acad Dermatol Venereol. 2016 Feb;30 Suppl 1:21-7).
Results showed “improvement of statistical significance,” Dr. Harper said. “All groups had improvement over time, and did better at 8 weeks than at 4 weeks [although] the rosacea group did not reach statistical significance until week 8.”
Finally, with green tea, Dr. Harper pointed to a 2010 randomized double-blind split-face study of just four healthy individuals with erythema and telangiectasia of the face, treated for 6 weeks with a cream containing epigallocatechin-3-gallate (EGCG), the major catechin found in green tea, on one side of their face; a vehicle cream was applied to the other side and punch biopsies were performed to determine improvements (Int J Clin Exp Pathol. 2010;3[7]:705-9). EGCG cream was used because of its “antioxidant, immunomodulatory, photoprotective, antiangiogenic – that’s the standout here, that’s what we really need – and anti-inflammatory properties,” Dr. Harper said.
While biopsies did not reveal any changes to facial vasculature, there “was a significant reduction in hypoxia-inducible factor-1 and VEGF [vascular endothelial growth factor],” which are both markers of angiogenesis – indicating some degree of usefulness against rosacea, Dr. Harper said. However, a longer, more definitive study would be needed to substantiate these findings, she added.
Dr. Harper did not report any relevant financial disclosures.
ORLANDO – When treating rosacea, consider adding cosmeceuticals to more conventional prescriptions and over-the-counter treatments to improve the management of symptoms and patient satisfaction.
The recommendation comes from Dr. Julie Harper, a dermatologist at the University of Alabama-Birmingham, who spoke about the benefits of cosmeceuticals for rosacea at the Orlando Dermatology Aesthetic and Clinical Conference.
“I see about 40 people a day on my regular dermatology days [and] it’s easy to just write a prescription and hand it to that rosacea patient, but you do them a big disservice when you do that,” explained Dr. Harper. “We’ve got to talk about triggers, about skin care, about sun protection, [and] start that discussion from there.”
The most-important point for patients to understand is the main triggers of their rosacea, which can include ultraviolet light, spices, stress, exercise, heat, barrier disruption, and Demodex. Since sunlight is the No. 1 trigger for rosacea, treatment strategies often need to start there and revolve around how to avoid or manage the condition based on sun exposure.
As for cosmeceuticals, Dr. Harper focused on three types that have been shown to be effective against rosacea: niacinamide, licorice, and green tea.
The available data on niacinamide for rosacea are primarily from the 2006 Nicomide Improvement in Clinical Outcomes Study (NICOS), an open-label, multicenter, prospective cohort study that recruited people with acne vulgaris and acne rosacea from 100 centers and administered 750 mg of niacinamide with zinc and copper, while some got niacinamide plus oral antibiotics. The 49 people with rosacea who were enrolled received baseline assessments in the clinic, but 4-week and 8-week follow-ups were done via self-reported surveys (Cutis. 2006 Jan;77[1 Suppl]:17-28).
At 8 weeks, “75% of the rosacea group reported that appearance of their rosacea was moderately or much better [and] that there was also significant reduction in inflammatory lesions,” Dr. Harper said. “There was not a big difference in the group that had an oral antibiotic and niacinamide, versus niacinamide without the oral antibiotic,” although the design of the study leaves the findings somewhat questionable, she noted.
Topical niacinamide also has the potential to benefit certain rosacea patients, she said, referring to a 2005 study examining the effects of a niacinamide-containing moisturizer on the face and one forearm of 50 patients over 4 weeks. The primary outcome of the trial was barrier function, as measured by a dimethyl sulfoxide (DMSO) chemical probe (Cutis. 2005 Aug;76[2]:135-41).
While the results of this trial are “difficult” to interpret – due largely to the lack of any real measurement of facial improvement in barrier function and the confusion over whether any improvement on the forearm can be attributed to the niacinamide specifically or to the moisturizer itself – “long story short, niacinamide did seem to help the barrier function in this particular study,” Dr. Harper said. The takeaway, therefore, is that topical niacinamide treatments may offer some value to certain patients.
Moving on to licorice, Dr. Harper discussed an open label study recently published online in the Journal of the European Academy of Dermatology and Venereology, in which subjects were given a complete skin care system – which contained a cleanser, a day cream, a night cream, and a concealer product containing licochalcone A (licorice extract). They were evaluated over a period of 8 weeks for improvement in erythema, burning, stinging, tingling, and tightness, all of which were measured at baseline (J Eur Acad Dermatol Venereol. 2016 Feb;30 Suppl 1:21-7).
Results showed “improvement of statistical significance,” Dr. Harper said. “All groups had improvement over time, and did better at 8 weeks than at 4 weeks [although] the rosacea group did not reach statistical significance until week 8.”
Finally, with green tea, Dr. Harper pointed to a 2010 randomized double-blind split-face study of just four healthy individuals with erythema and telangiectasia of the face, treated for 6 weeks with a cream containing epigallocatechin-3-gallate (EGCG), the major catechin found in green tea, on one side of their face; a vehicle cream was applied to the other side and punch biopsies were performed to determine improvements (Int J Clin Exp Pathol. 2010;3[7]:705-9). EGCG cream was used because of its “antioxidant, immunomodulatory, photoprotective, antiangiogenic – that’s the standout here, that’s what we really need – and anti-inflammatory properties,” Dr. Harper said.
While biopsies did not reveal any changes to facial vasculature, there “was a significant reduction in hypoxia-inducible factor-1 and VEGF [vascular endothelial growth factor],” which are both markers of angiogenesis – indicating some degree of usefulness against rosacea, Dr. Harper said. However, a longer, more definitive study would be needed to substantiate these findings, she added.
Dr. Harper did not report any relevant financial disclosures.
AT THE ODAC CONFERENCE
Cosmeceuticals for managing acne: more useful than you might think
ORLANDO – The increasingly popular role of cosmeceuticals in treating acne has created some confusion among both dermatologists and their patients as to what’s really effective and worth recommending.
This was the focus of a presentation at the Orlando Dermatology Aesthetic and Clinical Conference by Dr. Hilary E. Baldwin, who reviewed the cosmeceuticals most likely to make a clinical impact on patients with acne.
While there are no definitive data that prove that cosmeceuticals are the most effective means of managing acne, “sometimes cosmeceuticals may actually be helpful as adjunctive therapy,” said Dr. Baldwin, vice chair of dermatology at the State University of New York at Brooklyn. “Compared to prescription medications, I think these are just a drop in the bucket, but they’re a drop in the right direction.”
The main benefit of using cosmeceuticals for acne is to improve the barrier function of the skin. With increasing evidence that acne either causes or is caused by barrier defects, cosmeceuticals can be used, at the very least, as “extraordinarily well-made moisturizers,” according to Dr. Baldwin. In addition, because moisturizers are anti-inflammatory, they can improve the tolerability of other topical treatments dermatologists recommend to their patients, both prescription and over-the-counter.
For reducing Propionibacterium acnes, consider tea tree oil and lily leaf oil, both of which have a small but promising amount of clinical data behind them. For tea tree oil, Dr. Baldwin referred to a randomized study of 124 patients, which compared 5% tea tree oil gel with 5% benzoyl peroxide for treatment of mild to moderate acne (Med J Aust. 1990 Oct 15;153[8]:455-8). The study found that although the onset of action was slower for tea tree oil, overall it had a significant effect in improving acne in the patients, by reducing the number of inflamed and non-inflamed lesions.
“Both of them worked, but benzoyl peroxide was statistically better,” Dr. Baldwin said. “There were fewer side effects in the tea tree oil group, with less people complaining about skin discomfort.”
There are less data regarding lily leaf extract, however, with only one study she said was worth mentioning: a 4-week trial comparing lily leaf extract and 5% benzoyl peroxide that was “so complicated, and had so many arms, that they ended up having only 4-5 patients in each arm, so I don’t think they can conclude anything,” she remarked.
For management of acne-related inflammation, there is good evidence to suggest botanicals are an effective treatment. A double-blind, randomized, 12-week study coauthored by Dr. Baldwin found that in a cohort of 80 patients, benzoyl peroxide and salicylic acid were more effective when combined with botanical extracts than when used on their own (Semin Cutan Med Surg. 2015 Sep;34[5S]:S82-S85).
Furthermore, explained Dr. Baldwin, “evidence suggests that patients were also using [the botanical extract treatment] more because there was a preference for that,” indicating the increasing desire for more natural, cosmeceutical approaches to treating skin ailments by the general public.
“[Cosmeceuticals] appeal to this increasingly mature and demanding acne patient population,” she said. “[Patients] have a preference for a natural approach to skin disease, they believe that strengthening the host is more important than killing a pathogen, they think [cosmeceuticals] have less of a potential for side effects, and it also gives [patients] a sense of control, which attenuates some of the psychological sequelae of acne.
Dr. Baldwin also recommended oatmeal-based cosmeceuticals for their potential benefit in barrier repair, licorice-based cosmeceuticals for their ability to reduce both postinflammatory hyperpigmentation and post inflammatory erythema, and niacinamide. Niacinamide has been shown to reduce postinflammatory hyperpigmentation when used with other treatment options.
Dr. Baldwin emphasized, however, that cosmeceuticals should always be considered as a supplement to other, ongoing treatments, not the main treatment for acne.
She did not report any relevant financial disclosures.
ORLANDO – The increasingly popular role of cosmeceuticals in treating acne has created some confusion among both dermatologists and their patients as to what’s really effective and worth recommending.
This was the focus of a presentation at the Orlando Dermatology Aesthetic and Clinical Conference by Dr. Hilary E. Baldwin, who reviewed the cosmeceuticals most likely to make a clinical impact on patients with acne.
While there are no definitive data that prove that cosmeceuticals are the most effective means of managing acne, “sometimes cosmeceuticals may actually be helpful as adjunctive therapy,” said Dr. Baldwin, vice chair of dermatology at the State University of New York at Brooklyn. “Compared to prescription medications, I think these are just a drop in the bucket, but they’re a drop in the right direction.”
The main benefit of using cosmeceuticals for acne is to improve the barrier function of the skin. With increasing evidence that acne either causes or is caused by barrier defects, cosmeceuticals can be used, at the very least, as “extraordinarily well-made moisturizers,” according to Dr. Baldwin. In addition, because moisturizers are anti-inflammatory, they can improve the tolerability of other topical treatments dermatologists recommend to their patients, both prescription and over-the-counter.
For reducing Propionibacterium acnes, consider tea tree oil and lily leaf oil, both of which have a small but promising amount of clinical data behind them. For tea tree oil, Dr. Baldwin referred to a randomized study of 124 patients, which compared 5% tea tree oil gel with 5% benzoyl peroxide for treatment of mild to moderate acne (Med J Aust. 1990 Oct 15;153[8]:455-8). The study found that although the onset of action was slower for tea tree oil, overall it had a significant effect in improving acne in the patients, by reducing the number of inflamed and non-inflamed lesions.
“Both of them worked, but benzoyl peroxide was statistically better,” Dr. Baldwin said. “There were fewer side effects in the tea tree oil group, with less people complaining about skin discomfort.”
There are less data regarding lily leaf extract, however, with only one study she said was worth mentioning: a 4-week trial comparing lily leaf extract and 5% benzoyl peroxide that was “so complicated, and had so many arms, that they ended up having only 4-5 patients in each arm, so I don’t think they can conclude anything,” she remarked.
For management of acne-related inflammation, there is good evidence to suggest botanicals are an effective treatment. A double-blind, randomized, 12-week study coauthored by Dr. Baldwin found that in a cohort of 80 patients, benzoyl peroxide and salicylic acid were more effective when combined with botanical extracts than when used on their own (Semin Cutan Med Surg. 2015 Sep;34[5S]:S82-S85).
Furthermore, explained Dr. Baldwin, “evidence suggests that patients were also using [the botanical extract treatment] more because there was a preference for that,” indicating the increasing desire for more natural, cosmeceutical approaches to treating skin ailments by the general public.
“[Cosmeceuticals] appeal to this increasingly mature and demanding acne patient population,” she said. “[Patients] have a preference for a natural approach to skin disease, they believe that strengthening the host is more important than killing a pathogen, they think [cosmeceuticals] have less of a potential for side effects, and it also gives [patients] a sense of control, which attenuates some of the psychological sequelae of acne.
Dr. Baldwin also recommended oatmeal-based cosmeceuticals for their potential benefit in barrier repair, licorice-based cosmeceuticals for their ability to reduce both postinflammatory hyperpigmentation and post inflammatory erythema, and niacinamide. Niacinamide has been shown to reduce postinflammatory hyperpigmentation when used with other treatment options.
Dr. Baldwin emphasized, however, that cosmeceuticals should always be considered as a supplement to other, ongoing treatments, not the main treatment for acne.
She did not report any relevant financial disclosures.
ORLANDO – The increasingly popular role of cosmeceuticals in treating acne has created some confusion among both dermatologists and their patients as to what’s really effective and worth recommending.
This was the focus of a presentation at the Orlando Dermatology Aesthetic and Clinical Conference by Dr. Hilary E. Baldwin, who reviewed the cosmeceuticals most likely to make a clinical impact on patients with acne.
While there are no definitive data that prove that cosmeceuticals are the most effective means of managing acne, “sometimes cosmeceuticals may actually be helpful as adjunctive therapy,” said Dr. Baldwin, vice chair of dermatology at the State University of New York at Brooklyn. “Compared to prescription medications, I think these are just a drop in the bucket, but they’re a drop in the right direction.”
The main benefit of using cosmeceuticals for acne is to improve the barrier function of the skin. With increasing evidence that acne either causes or is caused by barrier defects, cosmeceuticals can be used, at the very least, as “extraordinarily well-made moisturizers,” according to Dr. Baldwin. In addition, because moisturizers are anti-inflammatory, they can improve the tolerability of other topical treatments dermatologists recommend to their patients, both prescription and over-the-counter.
For reducing Propionibacterium acnes, consider tea tree oil and lily leaf oil, both of which have a small but promising amount of clinical data behind them. For tea tree oil, Dr. Baldwin referred to a randomized study of 124 patients, which compared 5% tea tree oil gel with 5% benzoyl peroxide for treatment of mild to moderate acne (Med J Aust. 1990 Oct 15;153[8]:455-8). The study found that although the onset of action was slower for tea tree oil, overall it had a significant effect in improving acne in the patients, by reducing the number of inflamed and non-inflamed lesions.
“Both of them worked, but benzoyl peroxide was statistically better,” Dr. Baldwin said. “There were fewer side effects in the tea tree oil group, with less people complaining about skin discomfort.”
There are less data regarding lily leaf extract, however, with only one study she said was worth mentioning: a 4-week trial comparing lily leaf extract and 5% benzoyl peroxide that was “so complicated, and had so many arms, that they ended up having only 4-5 patients in each arm, so I don’t think they can conclude anything,” she remarked.
For management of acne-related inflammation, there is good evidence to suggest botanicals are an effective treatment. A double-blind, randomized, 12-week study coauthored by Dr. Baldwin found that in a cohort of 80 patients, benzoyl peroxide and salicylic acid were more effective when combined with botanical extracts than when used on their own (Semin Cutan Med Surg. 2015 Sep;34[5S]:S82-S85).
Furthermore, explained Dr. Baldwin, “evidence suggests that patients were also using [the botanical extract treatment] more because there was a preference for that,” indicating the increasing desire for more natural, cosmeceutical approaches to treating skin ailments by the general public.
“[Cosmeceuticals] appeal to this increasingly mature and demanding acne patient population,” she said. “[Patients] have a preference for a natural approach to skin disease, they believe that strengthening the host is more important than killing a pathogen, they think [cosmeceuticals] have less of a potential for side effects, and it also gives [patients] a sense of control, which attenuates some of the psychological sequelae of acne.
Dr. Baldwin also recommended oatmeal-based cosmeceuticals for their potential benefit in barrier repair, licorice-based cosmeceuticals for their ability to reduce both postinflammatory hyperpigmentation and post inflammatory erythema, and niacinamide. Niacinamide has been shown to reduce postinflammatory hyperpigmentation when used with other treatment options.
Dr. Baldwin emphasized, however, that cosmeceuticals should always be considered as a supplement to other, ongoing treatments, not the main treatment for acne.
She did not report any relevant financial disclosures.
AT THE ODAC CONFERENCE
Adult immunization schedule undergoes minor changes for 2016
The federal Advisory Committee on Immunization Practices’ 2016 adult immunization schedule differs from the previous schedule in small but significant ways – chief among them that the nine-valent human papillomavirus vaccine (9vHPV) has been added.
“This vaccine can be used for routine vaccination against HPV as one of three HPV vaccines (bivalent HPV vaccine [2vHPV], quadrivalent HPV vaccine [4vHPV], and 9vHPV) recommended for females and one of two HPV vaccines (4vHPV and 9vHPV) recommended for males,” according to the new schedule, which is recommended and released by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (Ann Intern Med. 2016 Feb 2. doi: 10.7326/M15-3005).
Another noteworthy change is in the amount of time recommended between receiving the 13-valent pneumococcal conjugate vaccine (PCV13) and the subsequent 23-valent pneumococcal polysaccharide vaccine (PPSV23) in adults aged 65 years and older who are deemed “immunocompetent.” That interval has been increased to “at least 1 year”; previously, it was 6-12 months.
In addition, adults aged 19 years or older should receive the PPSV23 vaccine at least 8 weeks after PCV13 only if they have “anatomical or functional asplenia, cerebrospinal fluid leak, or cochlear implant,” or if they are deemed immunocompromised.
The schedule for meningococcal serogroup B (MenB) has also been changed slightly. It is now recommended for all individuals aged 10 years or older who are considered to be “at increased risk for [MenB],” which ACIP outlines as persons with “anatomical or functional asplenia or persistent complement component deficiencies, microbiologists who are routinely exposed to isolates of Neisseria meningitidis, and persons identified at increased risk because of a serogroup B meningococcal disease outbreak.”
The recommendations note that the MenB series of vaccines can be given to any adolescents and young adults between the ages of 16 and 23 years to provide protection against the disease on a short-term basis, with a recommended age range of 16-18 years as optimal for vaccination.
Other changes are more minor, consisting of alterations to the vaccine schedule’s figures and accompanying text.
The row pertaining to “Meningococcal” vaccinations has been changed to “Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4),” in order to clarify that “there are two types of serogroup A, C, W, and Y meningococcal vaccines available for adults.” Furthermore, MenB has been given its own row on the immunization schedule.
The text regarding hepatitis A has been amended from “2 doses” to “2 to 3 doses depending on vaccine” because of differences between the hepatitis A and B vaccine series. The other changes are to texts detailing alternate dosing schedules for common vaccines, such as “Measles, mumps, and rubella,” to show that those recommendations can be changed “depending on indication.”
The 2016 adult immunization schedule was reviewed and approved by the American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives.
The federal Advisory Committee on Immunization Practices’ 2016 adult immunization schedule differs from the previous schedule in small but significant ways – chief among them that the nine-valent human papillomavirus vaccine (9vHPV) has been added.
“This vaccine can be used for routine vaccination against HPV as one of three HPV vaccines (bivalent HPV vaccine [2vHPV], quadrivalent HPV vaccine [4vHPV], and 9vHPV) recommended for females and one of two HPV vaccines (4vHPV and 9vHPV) recommended for males,” according to the new schedule, which is recommended and released by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (Ann Intern Med. 2016 Feb 2. doi: 10.7326/M15-3005).
Another noteworthy change is in the amount of time recommended between receiving the 13-valent pneumococcal conjugate vaccine (PCV13) and the subsequent 23-valent pneumococcal polysaccharide vaccine (PPSV23) in adults aged 65 years and older who are deemed “immunocompetent.” That interval has been increased to “at least 1 year”; previously, it was 6-12 months.
In addition, adults aged 19 years or older should receive the PPSV23 vaccine at least 8 weeks after PCV13 only if they have “anatomical or functional asplenia, cerebrospinal fluid leak, or cochlear implant,” or if they are deemed immunocompromised.
The schedule for meningococcal serogroup B (MenB) has also been changed slightly. It is now recommended for all individuals aged 10 years or older who are considered to be “at increased risk for [MenB],” which ACIP outlines as persons with “anatomical or functional asplenia or persistent complement component deficiencies, microbiologists who are routinely exposed to isolates of Neisseria meningitidis, and persons identified at increased risk because of a serogroup B meningococcal disease outbreak.”
The recommendations note that the MenB series of vaccines can be given to any adolescents and young adults between the ages of 16 and 23 years to provide protection against the disease on a short-term basis, with a recommended age range of 16-18 years as optimal for vaccination.
Other changes are more minor, consisting of alterations to the vaccine schedule’s figures and accompanying text.
The row pertaining to “Meningococcal” vaccinations has been changed to “Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4),” in order to clarify that “there are two types of serogroup A, C, W, and Y meningococcal vaccines available for adults.” Furthermore, MenB has been given its own row on the immunization schedule.
The text regarding hepatitis A has been amended from “2 doses” to “2 to 3 doses depending on vaccine” because of differences between the hepatitis A and B vaccine series. The other changes are to texts detailing alternate dosing schedules for common vaccines, such as “Measles, mumps, and rubella,” to show that those recommendations can be changed “depending on indication.”
The 2016 adult immunization schedule was reviewed and approved by the American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives.
The federal Advisory Committee on Immunization Practices’ 2016 adult immunization schedule differs from the previous schedule in small but significant ways – chief among them that the nine-valent human papillomavirus vaccine (9vHPV) has been added.
“This vaccine can be used for routine vaccination against HPV as one of three HPV vaccines (bivalent HPV vaccine [2vHPV], quadrivalent HPV vaccine [4vHPV], and 9vHPV) recommended for females and one of two HPV vaccines (4vHPV and 9vHPV) recommended for males,” according to the new schedule, which is recommended and released by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (Ann Intern Med. 2016 Feb 2. doi: 10.7326/M15-3005).
Another noteworthy change is in the amount of time recommended between receiving the 13-valent pneumococcal conjugate vaccine (PCV13) and the subsequent 23-valent pneumococcal polysaccharide vaccine (PPSV23) in adults aged 65 years and older who are deemed “immunocompetent.” That interval has been increased to “at least 1 year”; previously, it was 6-12 months.
In addition, adults aged 19 years or older should receive the PPSV23 vaccine at least 8 weeks after PCV13 only if they have “anatomical or functional asplenia, cerebrospinal fluid leak, or cochlear implant,” or if they are deemed immunocompromised.
The schedule for meningococcal serogroup B (MenB) has also been changed slightly. It is now recommended for all individuals aged 10 years or older who are considered to be “at increased risk for [MenB],” which ACIP outlines as persons with “anatomical or functional asplenia or persistent complement component deficiencies, microbiologists who are routinely exposed to isolates of Neisseria meningitidis, and persons identified at increased risk because of a serogroup B meningococcal disease outbreak.”
The recommendations note that the MenB series of vaccines can be given to any adolescents and young adults between the ages of 16 and 23 years to provide protection against the disease on a short-term basis, with a recommended age range of 16-18 years as optimal for vaccination.
Other changes are more minor, consisting of alterations to the vaccine schedule’s figures and accompanying text.
The row pertaining to “Meningococcal” vaccinations has been changed to “Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4),” in order to clarify that “there are two types of serogroup A, C, W, and Y meningococcal vaccines available for adults.” Furthermore, MenB has been given its own row on the immunization schedule.
The text regarding hepatitis A has been amended from “2 doses” to “2 to 3 doses depending on vaccine” because of differences between the hepatitis A and B vaccine series. The other changes are to texts detailing alternate dosing schedules for common vaccines, such as “Measles, mumps, and rubella,” to show that those recommendations can be changed “depending on indication.”
The 2016 adult immunization schedule was reviewed and approved by the American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives.
FROM ANNALS OF INTERNAL MEDICINE
Zika virus: What clinicians must know
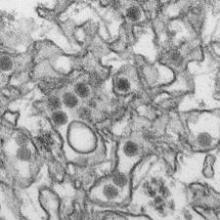
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
New Diagnostic, Treatment Methods for Fungal Infections
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ODAC 2016
VIDEO: New diagnostic, treatment methods for fungal infections
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – New diagnostic and treatment options are at the forefront of what’s new and exciting in the area of superficial cutaneous fungal infections, according to Dr. Adam Friedman.
“Although superficial cutaneous mycoses [are] extremely common, they can be quite a challenge for several reasons,” explained Dr. Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that “many of the common skin diseases are often confused for tineum, and vice versa.”
In this video interview, Dr. Friedman discusses what dermatologists should look for in terms of diagnosing and treating dermatophytes and onychomycosis, two of most common and increasingly treatable fungal infections patients are likely to present with.
Dr. Friedman did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ODAC 2016
VIDEO: Consider adding photodynamic therapy to your practice
ORLANDO – Dermatologists with the right patient population should consider incorporating photodynamic therapy (PDT) into their practices, as it is becoming an increasingly popular and effective.
Although most dermatologists know about PDT, “They’re not as comfortable setting up the office” and often don’t know the best ways to use PDT to achieve optimal treatment outcomes, explained Dr. Neal Bhatia, director of clinical dermatology at Therapeutics Clinical Research in San Diego, during his session at the Orlando Dermatology Aesthetic and Clinical annual meeting.
In this video interview, Dr. Bhatia, explains the benefits of PDT, what type of patient would be best suited for this treatment, and why it’s increasingly important for dermatologists to offer this treatment to their patients – even if they’ve never considered doing so before.
Dr. Bhatia is a clinical investigator and consultant with Dusa Pharmaceuticals and Biofrontera. He did not report any other relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Dermatologists with the right patient population should consider incorporating photodynamic therapy (PDT) into their practices, as it is becoming an increasingly popular and effective.
Although most dermatologists know about PDT, “They’re not as comfortable setting up the office” and often don’t know the best ways to use PDT to achieve optimal treatment outcomes, explained Dr. Neal Bhatia, director of clinical dermatology at Therapeutics Clinical Research in San Diego, during his session at the Orlando Dermatology Aesthetic and Clinical annual meeting.
In this video interview, Dr. Bhatia, explains the benefits of PDT, what type of patient would be best suited for this treatment, and why it’s increasingly important for dermatologists to offer this treatment to their patients – even if they’ve never considered doing so before.
Dr. Bhatia is a clinical investigator and consultant with Dusa Pharmaceuticals and Biofrontera. He did not report any other relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Dermatologists with the right patient population should consider incorporating photodynamic therapy (PDT) into their practices, as it is becoming an increasingly popular and effective.
Although most dermatologists know about PDT, “They’re not as comfortable setting up the office” and often don’t know the best ways to use PDT to achieve optimal treatment outcomes, explained Dr. Neal Bhatia, director of clinical dermatology at Therapeutics Clinical Research in San Diego, during his session at the Orlando Dermatology Aesthetic and Clinical annual meeting.
In this video interview, Dr. Bhatia, explains the benefits of PDT, what type of patient would be best suited for this treatment, and why it’s increasingly important for dermatologists to offer this treatment to their patients – even if they’ve never considered doing so before.
Dr. Bhatia is a clinical investigator and consultant with Dusa Pharmaceuticals and Biofrontera. He did not report any other relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM ODAC 2016
Treating Your Atopic Dermatitis Patients More Effectively
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ODAC 2016