User login
Here on Earth
We live inundated with promises that technology will solve our most challenging problems, yet we are regularly disappointed when it does not. New technological solutions seem to appear daily, and we feel like we are falling behind if we do not jump to join the people who are implementing, selling, or imposing new solutions. Often these solutions are offered before the problem is even fully understood, and no assessment has been made to determine if the solution actually helps to solve the challenge identified. With 80% of us now having transitioned to EHRs, we know full well their benefits as well as their pitfalls. While we have mostly accommodated to electronic documentation, we are now at the point where we are beginning to explore some of the most exciting potential benefits of our EHRs – population health, enhanced data on medication adherence, and improved patient communication. As we look at this next stage of growth, we are reminded of a lesson from an old joke:
A rabbi dies and goes to heaven. When he gets there he is given an old robe and a wooden walking stick and is told to get in line to the entrance to heaven. While the rabbi waits in the long line, a taxi driver walks up and is greeted by a group of angels blowing their horns announcing his arrival. One of the angels walks over to the driver and gives him a flowing white satin robe and a golden walking stick. Another angel then escorts him to the front of the line.
The angel turned toward him, smiled, and shook his head. “Yes, yes,” the angel replied, “We know all that. But, here in heaven we care about results, not intent. While you gave your sermons, people slept. When the cab driver drove, people prayed.”
As we look ahead to the next generation of electronic health records, there are going to be many creative ideas of how to use them to help patients improve their health and take care of their diseases. One of the more notable new technologies over the last 5 years is the development of wearable health devices. Innovations like the Apple Watch, Fitbit, and other wearables allow us to track our activity and diet, and encourage us to behave better. They do this by providing constant feedback on how we are doing, and they offer the ability to use social groups to encourage sustained behavioral change. Some devices tell us regularly how far we have walked while others let us know when we have been sitting too long. As we input information about diet, the devices and their associated apps give us feedback on how we are adhering to our dietary goals. Some even allow data to be funneled into the EHR so that physicians can review the behavioral changes and track patient progress. The challenge that arises is that the technology itself is so fascinating and so filled with promise that it is easy to forget what is most important: ensuring it works not just to keep us engaged and busy but also to help us accomplish the real goals we have defined for its use.
Wearable technology is now the most recent and dramatic example of how the excitement over technology may be outpacing its utility. Most of us have tried (or have patients, friends and family who have tried) wearable technology solutions to track and encourage behavioral change. A recent article published in JAMA looked at more than 400 individuals randomized to a standard behavioral weight-loss intervention vs. a technology-enhanced weight loss intervention using a wearable device over 24 months. It was fairly obvious that the group with the wearable device would do better, and have improved fitness and more weight loss. It was obvious … except that is not what happened. Both groups improved equally in fitness, and the standard intervention group lost significantly more weight over 24 months than did the wearable technology group.
There are many reasons that this might have happened. It may be that the idea of this quick feedback loop is in itself flawed, or it may be that the devices and/or the dietary input is simply imprecise, causing people to think that they are doing better than they really are (and then modifying their behavior in the wrong direction). Whatever the explanation, seeing those results, I think again of the moral handed down though generations by that old joke – that here on earth we need to care less about intent and more about results.
Reference
Jakicic JM, et al. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss The IDEA Randomized Clinical Trial. JAMA. 2016;316[11]:1161-71. doi: 10.1001/jama.2016.12858
Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
We live inundated with promises that technology will solve our most challenging problems, yet we are regularly disappointed when it does not. New technological solutions seem to appear daily, and we feel like we are falling behind if we do not jump to join the people who are implementing, selling, or imposing new solutions. Often these solutions are offered before the problem is even fully understood, and no assessment has been made to determine if the solution actually helps to solve the challenge identified. With 80% of us now having transitioned to EHRs, we know full well their benefits as well as their pitfalls. While we have mostly accommodated to electronic documentation, we are now at the point where we are beginning to explore some of the most exciting potential benefits of our EHRs – population health, enhanced data on medication adherence, and improved patient communication. As we look at this next stage of growth, we are reminded of a lesson from an old joke:
A rabbi dies and goes to heaven. When he gets there he is given an old robe and a wooden walking stick and is told to get in line to the entrance to heaven. While the rabbi waits in the long line, a taxi driver walks up and is greeted by a group of angels blowing their horns announcing his arrival. One of the angels walks over to the driver and gives him a flowing white satin robe and a golden walking stick. Another angel then escorts him to the front of the line.
The angel turned toward him, smiled, and shook his head. “Yes, yes,” the angel replied, “We know all that. But, here in heaven we care about results, not intent. While you gave your sermons, people slept. When the cab driver drove, people prayed.”
As we look ahead to the next generation of electronic health records, there are going to be many creative ideas of how to use them to help patients improve their health and take care of their diseases. One of the more notable new technologies over the last 5 years is the development of wearable health devices. Innovations like the Apple Watch, Fitbit, and other wearables allow us to track our activity and diet, and encourage us to behave better. They do this by providing constant feedback on how we are doing, and they offer the ability to use social groups to encourage sustained behavioral change. Some devices tell us regularly how far we have walked while others let us know when we have been sitting too long. As we input information about diet, the devices and their associated apps give us feedback on how we are adhering to our dietary goals. Some even allow data to be funneled into the EHR so that physicians can review the behavioral changes and track patient progress. The challenge that arises is that the technology itself is so fascinating and so filled with promise that it is easy to forget what is most important: ensuring it works not just to keep us engaged and busy but also to help us accomplish the real goals we have defined for its use.
Wearable technology is now the most recent and dramatic example of how the excitement over technology may be outpacing its utility. Most of us have tried (or have patients, friends and family who have tried) wearable technology solutions to track and encourage behavioral change. A recent article published in JAMA looked at more than 400 individuals randomized to a standard behavioral weight-loss intervention vs. a technology-enhanced weight loss intervention using a wearable device over 24 months. It was fairly obvious that the group with the wearable device would do better, and have improved fitness and more weight loss. It was obvious … except that is not what happened. Both groups improved equally in fitness, and the standard intervention group lost significantly more weight over 24 months than did the wearable technology group.
There are many reasons that this might have happened. It may be that the idea of this quick feedback loop is in itself flawed, or it may be that the devices and/or the dietary input is simply imprecise, causing people to think that they are doing better than they really are (and then modifying their behavior in the wrong direction). Whatever the explanation, seeing those results, I think again of the moral handed down though generations by that old joke – that here on earth we need to care less about intent and more about results.
Reference
Jakicic JM, et al. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss The IDEA Randomized Clinical Trial. JAMA. 2016;316[11]:1161-71. doi: 10.1001/jama.2016.12858
Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
We live inundated with promises that technology will solve our most challenging problems, yet we are regularly disappointed when it does not. New technological solutions seem to appear daily, and we feel like we are falling behind if we do not jump to join the people who are implementing, selling, or imposing new solutions. Often these solutions are offered before the problem is even fully understood, and no assessment has been made to determine if the solution actually helps to solve the challenge identified. With 80% of us now having transitioned to EHRs, we know full well their benefits as well as their pitfalls. While we have mostly accommodated to electronic documentation, we are now at the point where we are beginning to explore some of the most exciting potential benefits of our EHRs – population health, enhanced data on medication adherence, and improved patient communication. As we look at this next stage of growth, we are reminded of a lesson from an old joke:
A rabbi dies and goes to heaven. When he gets there he is given an old robe and a wooden walking stick and is told to get in line to the entrance to heaven. While the rabbi waits in the long line, a taxi driver walks up and is greeted by a group of angels blowing their horns announcing his arrival. One of the angels walks over to the driver and gives him a flowing white satin robe and a golden walking stick. Another angel then escorts him to the front of the line.
The angel turned toward him, smiled, and shook his head. “Yes, yes,” the angel replied, “We know all that. But, here in heaven we care about results, not intent. While you gave your sermons, people slept. When the cab driver drove, people prayed.”
As we look ahead to the next generation of electronic health records, there are going to be many creative ideas of how to use them to help patients improve their health and take care of their diseases. One of the more notable new technologies over the last 5 years is the development of wearable health devices. Innovations like the Apple Watch, Fitbit, and other wearables allow us to track our activity and diet, and encourage us to behave better. They do this by providing constant feedback on how we are doing, and they offer the ability to use social groups to encourage sustained behavioral change. Some devices tell us regularly how far we have walked while others let us know when we have been sitting too long. As we input information about diet, the devices and their associated apps give us feedback on how we are adhering to our dietary goals. Some even allow data to be funneled into the EHR so that physicians can review the behavioral changes and track patient progress. The challenge that arises is that the technology itself is so fascinating and so filled with promise that it is easy to forget what is most important: ensuring it works not just to keep us engaged and busy but also to help us accomplish the real goals we have defined for its use.
Wearable technology is now the most recent and dramatic example of how the excitement over technology may be outpacing its utility. Most of us have tried (or have patients, friends and family who have tried) wearable technology solutions to track and encourage behavioral change. A recent article published in JAMA looked at more than 400 individuals randomized to a standard behavioral weight-loss intervention vs. a technology-enhanced weight loss intervention using a wearable device over 24 months. It was fairly obvious that the group with the wearable device would do better, and have improved fitness and more weight loss. It was obvious … except that is not what happened. Both groups improved equally in fitness, and the standard intervention group lost significantly more weight over 24 months than did the wearable technology group.
There are many reasons that this might have happened. It may be that the idea of this quick feedback loop is in itself flawed, or it may be that the devices and/or the dietary input is simply imprecise, causing people to think that they are doing better than they really are (and then modifying their behavior in the wrong direction). Whatever the explanation, seeing those results, I think again of the moral handed down though generations by that old joke – that here on earth we need to care less about intent and more about results.
Reference
Jakicic JM, et al. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss The IDEA Randomized Clinical Trial. JAMA. 2016;316[11]:1161-71. doi: 10.1001/jama.2016.12858
Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
EHR Report: Take your medicine!
“Drugs don’t work in patients who don’t take them.”
–C. Everett Koop, M.D.
While it would be hard to imagine accountable care organizations being able to get the data they need to manage care without electronic health records, and EHRs are critical as payment has evolved to emphasize the outcomes of treatment, one area remains the holy grail of disease management: how to get patients to take the medications that are prescribed.
Poor adherence to medications is a critical issue in the management of chronic disease. The causes for suboptimal adherence are numerous, including the cost of medications, patient-physician communication, patient education, motivation, and simple forgetfulness.
Approximately 1.5 billion prescriptions, at a cost of more than $250 billion, are dispensed each year in the United States. A large body of evidence supports the use of these medications. For patients with diabetes, for instance, correct medication use can lower blood sugar, blood pressure, and cholesterol, and by so doing, decrease morbidity and mortality from both microvascular and macrovascular disease.
The act of taking medications is influenced by many factors, and all of these factors come together at a point in time when patients are not directly engaged with the health care system. It is at that moment that patients remember and decide whether to take their medications.
Numerous studies show that individuals often do not take their medicines as prescribed. Adherence rates for medications for chronic disease show that patients on average take only about 50% of prescribed doses. For patients with diabetes, the average adherence rate is about 70%, with rates ranging in different studies from 31% to 87%.
When patients do not take their medications correctly, there can be severe consequences. Poor medication adherence can lead to poorer clinical outcomes, including increased hospitalizations. One large dataset of more than 56,000 individuals with type 2 diabetes covered by employer-sponsored health insurance showed that increased adherence to medications significantly reduced hospitalizations and emergency department visits. When adherence rates increased, the hospitalization rate fell 23%, and the rate of emergency department visits decreased 46%, resulting in significant cost savings for the health system.1
In response to this issue, many strategies have emerged. We now regularly get correspondence from insurance companies alerting us to nonadherence of individual patients. This information tends to be of little benefit, because the information is received long after the decision to take or not take the medication is made. Our response in the office to our patients is generally to remind them to take their medications, which is not much different from the discussion we have with them without that information.
Recently, a new set of apps for smartphones and tablets has emerged to help patients organize their approach to taking medications. Examples of some of these apps include Care4Today, Dosecast, Medisafe, MedSimple, MyMedREc, MyMeds, and OnTimeRx. Most of these apps allow a patient to put in their medication schedule and are organized to provide reminders when it is time to take medications.
The problem with reminders, of course, is that they don’t always happen at a time when it is convenient for a person to take their medications. For example, if your app reminds you to take your medicines at 9 p.m. each night, and you are at the movies on a Saturday night, you may extinguish the reminder and not remember to take the medications when you get home.
Many of the apps also track adherence rates so that patients can see how well they are doing in taking their medications. The results are often startling to patients, and it is hoped that such information would encourage more effort in taking medications.
One problem with many of the apps currently available is that they essentially function as sophisticated alarm clocks. They do not get at some of the fundamental reasons that people do not take their medications, which would require more behavioral input.
In fact, a recent article in the American Journal of Preventive Medicine looked at 166 medication adherence apps and concluded that current apps contained little in the way of evidence-based behavioral change techniques that have been shown to help change behavior. In fact, only about one-third of apps contained any feedback on behavior at all.2
While adherence apps still have a way to go, they can be helpful, and many contain interesting, novel features. Some allow the patient to input the name of a medication by scanning the name from the medication’s pill bottle. Some have the ability not only to remind a patient to take a medication, but also to text that patient’s caregiver (or parent, in the case of a teenager) if the medication is not taken.
While not perfect, these adherence apps are worth learning more about. They may be helpful additions to our efforts to achieve the best outcomes for our patients by helping them to actually take the medications that we so carefully prescribe.
References
1. Encinosa, W.E.; Bernard, D.; Dor, A. Does prescription drug adherence reduce hospitalizations and costs? The case of diabetes. Advances in Health Economics and Health Services Research 22, pp. 151-73, 2010 (AHRQ Publication No. 11-R008).
2. Am J Prev Med. 2015 Nov 17. pii: S0749-3797(15)00637-6. doi: 10.1016/j.amepre.2015.09.034.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
“Drugs don’t work in patients who don’t take them.”
–C. Everett Koop, M.D.
While it would be hard to imagine accountable care organizations being able to get the data they need to manage care without electronic health records, and EHRs are critical as payment has evolved to emphasize the outcomes of treatment, one area remains the holy grail of disease management: how to get patients to take the medications that are prescribed.
Poor adherence to medications is a critical issue in the management of chronic disease. The causes for suboptimal adherence are numerous, including the cost of medications, patient-physician communication, patient education, motivation, and simple forgetfulness.
Approximately 1.5 billion prescriptions, at a cost of more than $250 billion, are dispensed each year in the United States. A large body of evidence supports the use of these medications. For patients with diabetes, for instance, correct medication use can lower blood sugar, blood pressure, and cholesterol, and by so doing, decrease morbidity and mortality from both microvascular and macrovascular disease.
The act of taking medications is influenced by many factors, and all of these factors come together at a point in time when patients are not directly engaged with the health care system. It is at that moment that patients remember and decide whether to take their medications.
Numerous studies show that individuals often do not take their medicines as prescribed. Adherence rates for medications for chronic disease show that patients on average take only about 50% of prescribed doses. For patients with diabetes, the average adherence rate is about 70%, with rates ranging in different studies from 31% to 87%.
When patients do not take their medications correctly, there can be severe consequences. Poor medication adherence can lead to poorer clinical outcomes, including increased hospitalizations. One large dataset of more than 56,000 individuals with type 2 diabetes covered by employer-sponsored health insurance showed that increased adherence to medications significantly reduced hospitalizations and emergency department visits. When adherence rates increased, the hospitalization rate fell 23%, and the rate of emergency department visits decreased 46%, resulting in significant cost savings for the health system.1
In response to this issue, many strategies have emerged. We now regularly get correspondence from insurance companies alerting us to nonadherence of individual patients. This information tends to be of little benefit, because the information is received long after the decision to take or not take the medication is made. Our response in the office to our patients is generally to remind them to take their medications, which is not much different from the discussion we have with them without that information.
Recently, a new set of apps for smartphones and tablets has emerged to help patients organize their approach to taking medications. Examples of some of these apps include Care4Today, Dosecast, Medisafe, MedSimple, MyMedREc, MyMeds, and OnTimeRx. Most of these apps allow a patient to put in their medication schedule and are organized to provide reminders when it is time to take medications.
The problem with reminders, of course, is that they don’t always happen at a time when it is convenient for a person to take their medications. For example, if your app reminds you to take your medicines at 9 p.m. each night, and you are at the movies on a Saturday night, you may extinguish the reminder and not remember to take the medications when you get home.
Many of the apps also track adherence rates so that patients can see how well they are doing in taking their medications. The results are often startling to patients, and it is hoped that such information would encourage more effort in taking medications.
One problem with many of the apps currently available is that they essentially function as sophisticated alarm clocks. They do not get at some of the fundamental reasons that people do not take their medications, which would require more behavioral input.
In fact, a recent article in the American Journal of Preventive Medicine looked at 166 medication adherence apps and concluded that current apps contained little in the way of evidence-based behavioral change techniques that have been shown to help change behavior. In fact, only about one-third of apps contained any feedback on behavior at all.2
While adherence apps still have a way to go, they can be helpful, and many contain interesting, novel features. Some allow the patient to input the name of a medication by scanning the name from the medication’s pill bottle. Some have the ability not only to remind a patient to take a medication, but also to text that patient’s caregiver (or parent, in the case of a teenager) if the medication is not taken.
While not perfect, these adherence apps are worth learning more about. They may be helpful additions to our efforts to achieve the best outcomes for our patients by helping them to actually take the medications that we so carefully prescribe.
References
1. Encinosa, W.E.; Bernard, D.; Dor, A. Does prescription drug adherence reduce hospitalizations and costs? The case of diabetes. Advances in Health Economics and Health Services Research 22, pp. 151-73, 2010 (AHRQ Publication No. 11-R008).
2. Am J Prev Med. 2015 Nov 17. pii: S0749-3797(15)00637-6. doi: 10.1016/j.amepre.2015.09.034.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
“Drugs don’t work in patients who don’t take them.”
–C. Everett Koop, M.D.
While it would be hard to imagine accountable care organizations being able to get the data they need to manage care without electronic health records, and EHRs are critical as payment has evolved to emphasize the outcomes of treatment, one area remains the holy grail of disease management: how to get patients to take the medications that are prescribed.
Poor adherence to medications is a critical issue in the management of chronic disease. The causes for suboptimal adherence are numerous, including the cost of medications, patient-physician communication, patient education, motivation, and simple forgetfulness.
Approximately 1.5 billion prescriptions, at a cost of more than $250 billion, are dispensed each year in the United States. A large body of evidence supports the use of these medications. For patients with diabetes, for instance, correct medication use can lower blood sugar, blood pressure, and cholesterol, and by so doing, decrease morbidity and mortality from both microvascular and macrovascular disease.
The act of taking medications is influenced by many factors, and all of these factors come together at a point in time when patients are not directly engaged with the health care system. It is at that moment that patients remember and decide whether to take their medications.
Numerous studies show that individuals often do not take their medicines as prescribed. Adherence rates for medications for chronic disease show that patients on average take only about 50% of prescribed doses. For patients with diabetes, the average adherence rate is about 70%, with rates ranging in different studies from 31% to 87%.
When patients do not take their medications correctly, there can be severe consequences. Poor medication adherence can lead to poorer clinical outcomes, including increased hospitalizations. One large dataset of more than 56,000 individuals with type 2 diabetes covered by employer-sponsored health insurance showed that increased adherence to medications significantly reduced hospitalizations and emergency department visits. When adherence rates increased, the hospitalization rate fell 23%, and the rate of emergency department visits decreased 46%, resulting in significant cost savings for the health system.1
In response to this issue, many strategies have emerged. We now regularly get correspondence from insurance companies alerting us to nonadherence of individual patients. This information tends to be of little benefit, because the information is received long after the decision to take or not take the medication is made. Our response in the office to our patients is generally to remind them to take their medications, which is not much different from the discussion we have with them without that information.
Recently, a new set of apps for smartphones and tablets has emerged to help patients organize their approach to taking medications. Examples of some of these apps include Care4Today, Dosecast, Medisafe, MedSimple, MyMedREc, MyMeds, and OnTimeRx. Most of these apps allow a patient to put in their medication schedule and are organized to provide reminders when it is time to take medications.
The problem with reminders, of course, is that they don’t always happen at a time when it is convenient for a person to take their medications. For example, if your app reminds you to take your medicines at 9 p.m. each night, and you are at the movies on a Saturday night, you may extinguish the reminder and not remember to take the medications when you get home.
Many of the apps also track adherence rates so that patients can see how well they are doing in taking their medications. The results are often startling to patients, and it is hoped that such information would encourage more effort in taking medications.
One problem with many of the apps currently available is that they essentially function as sophisticated alarm clocks. They do not get at some of the fundamental reasons that people do not take their medications, which would require more behavioral input.
In fact, a recent article in the American Journal of Preventive Medicine looked at 166 medication adherence apps and concluded that current apps contained little in the way of evidence-based behavioral change techniques that have been shown to help change behavior. In fact, only about one-third of apps contained any feedback on behavior at all.2
While adherence apps still have a way to go, they can be helpful, and many contain interesting, novel features. Some allow the patient to input the name of a medication by scanning the name from the medication’s pill bottle. Some have the ability not only to remind a patient to take a medication, but also to text that patient’s caregiver (or parent, in the case of a teenager) if the medication is not taken.
While not perfect, these adherence apps are worth learning more about. They may be helpful additions to our efforts to achieve the best outcomes for our patients by helping them to actually take the medications that we so carefully prescribe.
References
1. Encinosa, W.E.; Bernard, D.; Dor, A. Does prescription drug adherence reduce hospitalizations and costs? The case of diabetes. Advances in Health Economics and Health Services Research 22, pp. 151-73, 2010 (AHRQ Publication No. 11-R008).
2. Am J Prev Med. 2015 Nov 17. pii: S0749-3797(15)00637-6. doi: 10.1016/j.amepre.2015.09.034.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Baby, back back back it up
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
As many young physicians might recognize, the title of today’s column is from a song by Prince Royce featuring Jennifer Lopez and Pitbull. This article, though, is about what we believe is likely an urgent matter for many of our readers – the issue of appropriately backing up information that resides on their personal computers. We were prompted to write about this after a colleague came to one of us in a panic after losing all of the information on her meticulously performed, but poorly conceived backup. For years she has been developing and storing her lectures on a flash drive, and every month she has been backing up her flash drive to her personal computer. She even set a reminder in her calendar to make sure that she perform those backups each and every month. Unfortunately, she lost her flash drive, and even more unfortunately discovered that what she thought were copies of files on her computer were actually only shortcuts to the files on her now-missing flash drive. All her files were gone.
We are going to organize our discussion in three parts: First, we want to convince you of the importance of making backups, essentially informational life insurance. Unlike life insurance, however, you have a pretty good chance of using your backups at some point over the next 10 years. Second, we are going to discuss locally based backups, and then lastly, we’ll cover cloud-based backups. This may seem like an incredibly dull topic to some, but we anticipate receiving emails of thanks over many years for the knowledge and actions that come out of today’s column.
Hard drive failure rates, derived from data published by companies that professionally manage large numbers of hard drives, is about 3%-5% in the first year. This remains at about 3% per year for the next 2-3 years, and then can go up to 10% or more per year as hard drives continue to age. That means that over a 4-year period, 15%-20% of hard drives are likely to fail.1,2 This fact underscores the importance of backing up your data, because there is a good chance that over time, loss of data will happen to you.
One strategy is to back up to an external drive. The drive can be either a flash drive if you have less than 128 GB to store, or a traditional external hard drive – a very affordable option for memory up to 4 TB (4,000 GB). There are many excellent external hard drives and flash drives from which to choose, but you also need to have backup software that will take the information from your personal computer and place it in an organized manner on your external drive. Many drives now come bundled with backup software. An example of such a drive is the Western Digital My Passport Elite. If the hard drive you have does not already have backup software, there are lots of good choices out there. Backup software solutions include Time Machine (built into all Mac Computers), and many software choices for PCs.3
While the speed of backup and recovery is fast – often just a few hours – there are two main issues that make external drives suboptimal as your main backup strategy. The first is that most people simply don’t remember to plug their external drive into their computer regularly; months and sometimes years can go by without backing up your files. The second issue, which is usually not considered, is that the hard drive usually sits on your desk next to your computer. Therefore, if there is a fire, a flood, an electrical surge, or even a simple spill on your desk, you may lose both your main files and your backup in one fell swoop. For this reason, if you choose to use an external drive as your backup method, you should back up to two different external drives and keep one drive in your office and one at home.
The best method of backup, and the one we recommend to everyone, eliminates the major disadvantages of local backups. This method is cloud-based backup. For cloud-based backup, you purchase a subscription with an annual fee, then you download software from the backup vendor to your computer. It usually takes about 15 minutes to set up the software by selecting the file folders that you would like to back up, then the software does the rest. The first backup can take a long time, typically a few days, as the speed of the backup is limited by the speed of your Internet connection. After that first time, though, backups don’t take long because they back up only the files that have changed since the previous backup.
The main advantages to cloud-based solutions is that once it has been set up, the software ensures that incremental backups occur automatically every time your computer is connected to the Internet. In addition, since the cloud backups are off-site, you are protected from an adverse occurrence taking out your backup drive and your computer when they are sitting next to each other on your desk. In addition, most cloud backup services also allow you to access your file from any computer or smartphone for access where and when you need the files.
So, let us end where we began, with lyrics from the music video, with which we agree, “Word of advice: Want a happy life … Back it up one more time.”
References
1. http://www.extremetech.com/computing/170748-how-long-do-hard-drives-actually-live-for
2. http://www.pcworld.com/article/131168/article.html
3. The Best Backup Software at http://www.pcmag.com/article2/0,2817,2278661,00.asp
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Aunt Tillie and electronic health records
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Meaningful use – Stage 2 (Part 1 of 2)
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
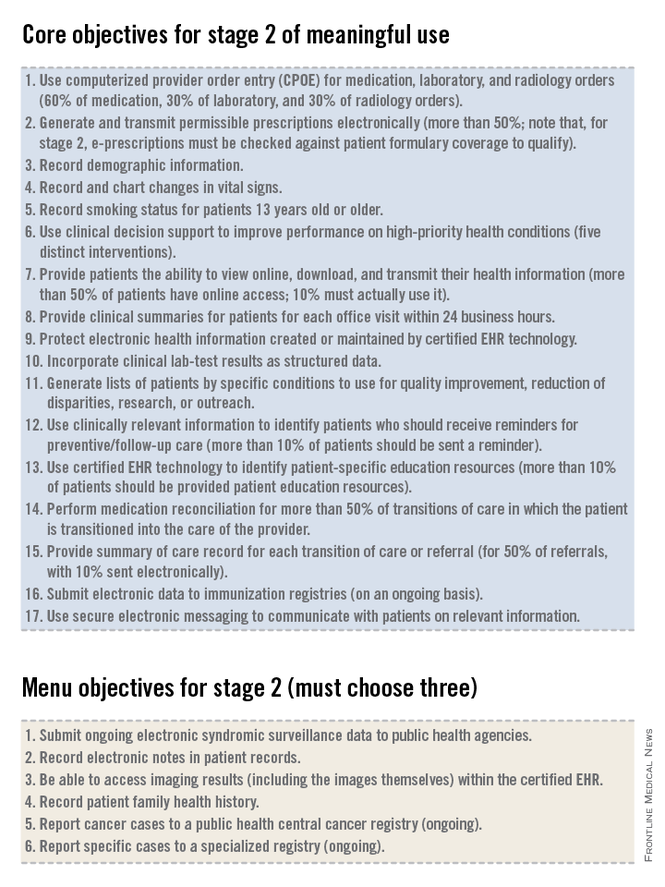
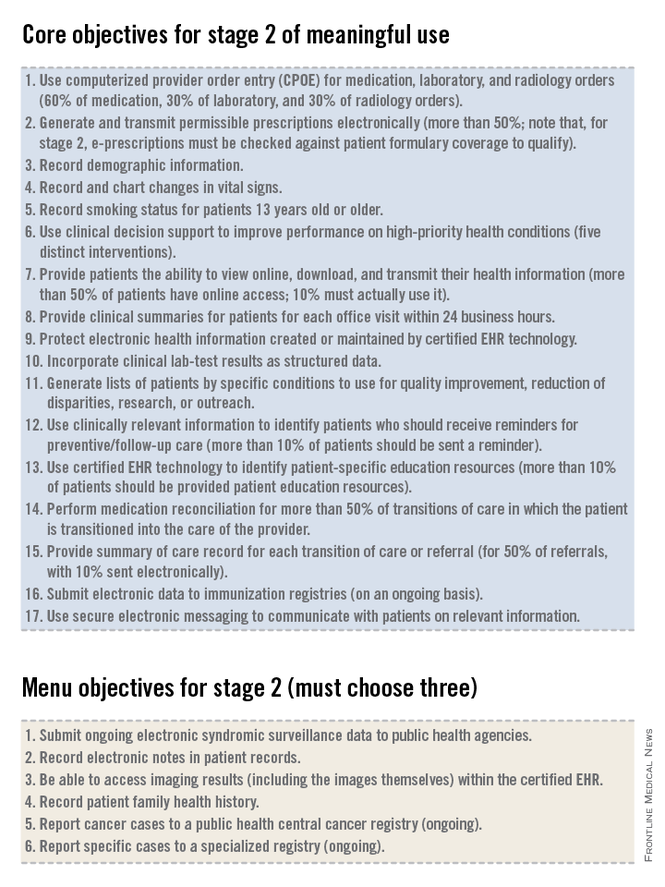
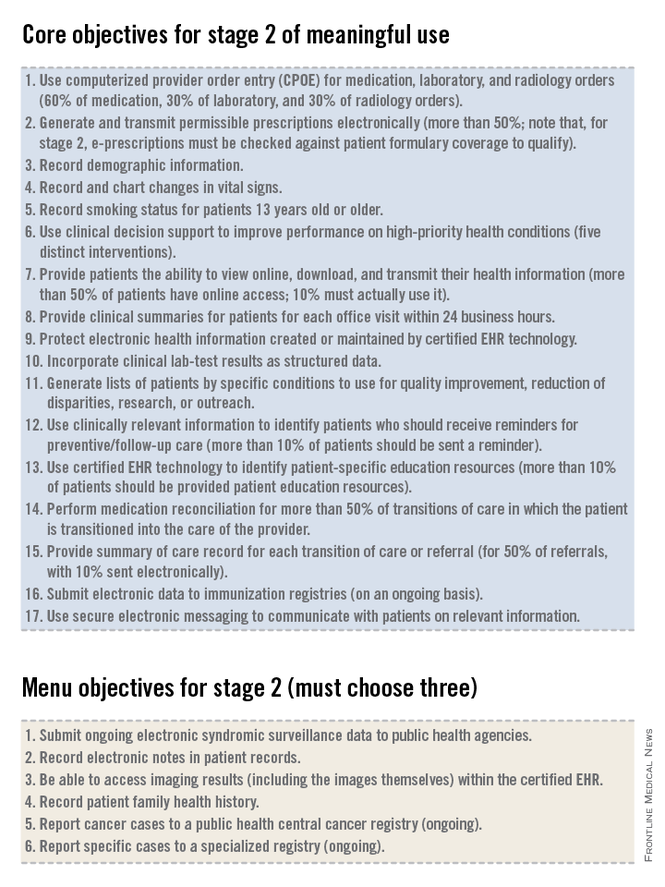
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Truly connected health care
For years, we have all been promised interconnected electronic patient records – the concept that information would follow patients and be available across all care settings. Unfortunately, this reality has yet to materialize.
Regional Health Information Organizations (RHIOs) exist all over (these are hospitals, physician practices, and health networks that exchange data on a local level), but they typically present a "brick wall" at their borders where the information sharing stops. Thankfully, that is poised to change, with a new push toward meaningful interconnectedness.
Finally, health information technology (HIT) thought leaders and electronic health records (EHR) vendors are homing in on standards that will allow physicians and other healthcare providers to exchange information seamlessly regardless of EHR system or geographical location. The goal, as usual, is to improve patient care and outcomes. In this column, we felt it would be useful to highlight some of the ideas driving this effort, as there is good reason to be optimistic about the possibility of true interoperability.
A view from the top
Recently, at the annual meeting of the Health Information Management Systems Society (HIMSS) in Orlando, Dr. Karen DeSalvo, national health IT coordinator, made a strong plea for interoperability by 2017. She said "We can do national health care exchange in 3 years. ... I want this as a doctor, I want this as patient, I want this as a daughter."
Dr. DeSalvo’s words resonate because this is a concept we all expected from the earliest days of electronic records. Unfortunately, barriers – both real and artificial – have stood in the way. First and foremost are patient privacy and information security. It is essential that patient data are protected and maintained as the data pass from one system to the next, but often, even the basic function of matching patients with the right records can be challenging. Many identifiers exist, including various medical record numbers and insurance codes. If a name is misspelled or middle initial omitted, this can also create significant chaos and allow sensitive data to file into the wrong place, creating HIPAA violations and distrust among patients.
In addition to concerns over data security, the lack of standard formatting for storing and sharing records has been a huge hurdle for EHR vendors. Not surprisingly, the simultaneous development of dozens of competing EHR products has created significant fragmentation throughout the market. Instead of starting from a common set of data elements, each EHR was essentially designed "in a vacuum," and only now are their creators attempting to find a way to get them to communicate. A number of cross-platform projects currently underway highlight this effort.
VHS or Betamax?
On Feb. 25, 2014, NextGen Healthcare and Cerner announced bilateral certification of their EHR products and affirmed their commitment to interoperability. According to the press release, they are committed to "creating proactive working relationships, expanding the boundaries of current interoperability ... and supporting the efforts of [their] clients to advance the health of their communities." These may not be novel goals, but at least both vendors have demonstrated their best attempt to achieve them. Also, both companies have a huge footprint in the market, so their collaboration is certain to raise the level of attention being paid to this topic. But this isn’t the only attempt at broad-based interoperability.
EClinicalWorks (eCW), another large player in the ambulatory EHR market, has developed a product know as P2P, or Provider to Provider. Originally conceived as a way to communicate between different users of the eCW platform, it has now been expanded to all providers, regardless of their EHR, as a secure communication tool. This new product is known as P2POpen and is free to any health care professional wishing to join "the network." According to their website, P2POpen now boasts close to 22,000 users and facilitates "improved quality, safety, and efficiency of care." Like the collaboration mentioned above, P2POpen has a shot at success, but both of these efforts may also portend more debate over standardization moving forward. Will the disparity in how each company addresses the issue of interoperability lead to further fragmentation? And how can we be sure that embracing one of these ideas won’t severely limit us in the future?
Setting the standard
The only way to answer these and other looming concerns over developing a consistent interoperability protocol is to start at the top and rapidly build consensus. In other words, Dr. DeSalvo’s words need to be quickly translated into action, as she and other thought leaders agree – not only on a standard – but also on a way to properly motivate EHR vendors to adopt that standard.
One possible opportunity to enforce this as Meaningful Use stage III. The requirements for stage III EHR certification, which have yet to be finalized, should include a necessity for every vendor to adopt a consistent format for information exchange and data transmission. Making this a certification requirement will ensure that all EHR products remain cooperative if they plan to stay competitive.
Another solution being considered involves the use of centralized "Health Information Exchanges," which could collect and warehouse data from multiple sources and then retransmit those data in a universally readable format. Either way, if a consensus can be reached and issues over privacy and security addressed, it will only spell a victory for physicians and patients and truly get us on the road to improved patient care and outcomes. We tend to agree with Dr. DeSalvo, and believe that victory is well within reach.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
For years, we have all been promised interconnected electronic patient records – the concept that information would follow patients and be available across all care settings. Unfortunately, this reality has yet to materialize.
Regional Health Information Organizations (RHIOs) exist all over (these are hospitals, physician practices, and health networks that exchange data on a local level), but they typically present a "brick wall" at their borders where the information sharing stops. Thankfully, that is poised to change, with a new push toward meaningful interconnectedness.
Finally, health information technology (HIT) thought leaders and electronic health records (EHR) vendors are homing in on standards that will allow physicians and other healthcare providers to exchange information seamlessly regardless of EHR system or geographical location. The goal, as usual, is to improve patient care and outcomes. In this column, we felt it would be useful to highlight some of the ideas driving this effort, as there is good reason to be optimistic about the possibility of true interoperability.
A view from the top
Recently, at the annual meeting of the Health Information Management Systems Society (HIMSS) in Orlando, Dr. Karen DeSalvo, national health IT coordinator, made a strong plea for interoperability by 2017. She said "We can do national health care exchange in 3 years. ... I want this as a doctor, I want this as patient, I want this as a daughter."
Dr. DeSalvo’s words resonate because this is a concept we all expected from the earliest days of electronic records. Unfortunately, barriers – both real and artificial – have stood in the way. First and foremost are patient privacy and information security. It is essential that patient data are protected and maintained as the data pass from one system to the next, but often, even the basic function of matching patients with the right records can be challenging. Many identifiers exist, including various medical record numbers and insurance codes. If a name is misspelled or middle initial omitted, this can also create significant chaos and allow sensitive data to file into the wrong place, creating HIPAA violations and distrust among patients.
In addition to concerns over data security, the lack of standard formatting for storing and sharing records has been a huge hurdle for EHR vendors. Not surprisingly, the simultaneous development of dozens of competing EHR products has created significant fragmentation throughout the market. Instead of starting from a common set of data elements, each EHR was essentially designed "in a vacuum," and only now are their creators attempting to find a way to get them to communicate. A number of cross-platform projects currently underway highlight this effort.
VHS or Betamax?
On Feb. 25, 2014, NextGen Healthcare and Cerner announced bilateral certification of their EHR products and affirmed their commitment to interoperability. According to the press release, they are committed to "creating proactive working relationships, expanding the boundaries of current interoperability ... and supporting the efforts of [their] clients to advance the health of their communities." These may not be novel goals, but at least both vendors have demonstrated their best attempt to achieve them. Also, both companies have a huge footprint in the market, so their collaboration is certain to raise the level of attention being paid to this topic. But this isn’t the only attempt at broad-based interoperability.
EClinicalWorks (eCW), another large player in the ambulatory EHR market, has developed a product know as P2P, or Provider to Provider. Originally conceived as a way to communicate between different users of the eCW platform, it has now been expanded to all providers, regardless of their EHR, as a secure communication tool. This new product is known as P2POpen and is free to any health care professional wishing to join "the network." According to their website, P2POpen now boasts close to 22,000 users and facilitates "improved quality, safety, and efficiency of care." Like the collaboration mentioned above, P2POpen has a shot at success, but both of these efforts may also portend more debate over standardization moving forward. Will the disparity in how each company addresses the issue of interoperability lead to further fragmentation? And how can we be sure that embracing one of these ideas won’t severely limit us in the future?
Setting the standard
The only way to answer these and other looming concerns over developing a consistent interoperability protocol is to start at the top and rapidly build consensus. In other words, Dr. DeSalvo’s words need to be quickly translated into action, as she and other thought leaders agree – not only on a standard – but also on a way to properly motivate EHR vendors to adopt that standard.
One possible opportunity to enforce this as Meaningful Use stage III. The requirements for stage III EHR certification, which have yet to be finalized, should include a necessity for every vendor to adopt a consistent format for information exchange and data transmission. Making this a certification requirement will ensure that all EHR products remain cooperative if they plan to stay competitive.
Another solution being considered involves the use of centralized "Health Information Exchanges," which could collect and warehouse data from multiple sources and then retransmit those data in a universally readable format. Either way, if a consensus can be reached and issues over privacy and security addressed, it will only spell a victory for physicians and patients and truly get us on the road to improved patient care and outcomes. We tend to agree with Dr. DeSalvo, and believe that victory is well within reach.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
For years, we have all been promised interconnected electronic patient records – the concept that information would follow patients and be available across all care settings. Unfortunately, this reality has yet to materialize.
Regional Health Information Organizations (RHIOs) exist all over (these are hospitals, physician practices, and health networks that exchange data on a local level), but they typically present a "brick wall" at their borders where the information sharing stops. Thankfully, that is poised to change, with a new push toward meaningful interconnectedness.
Finally, health information technology (HIT) thought leaders and electronic health records (EHR) vendors are homing in on standards that will allow physicians and other healthcare providers to exchange information seamlessly regardless of EHR system or geographical location. The goal, as usual, is to improve patient care and outcomes. In this column, we felt it would be useful to highlight some of the ideas driving this effort, as there is good reason to be optimistic about the possibility of true interoperability.
A view from the top
Recently, at the annual meeting of the Health Information Management Systems Society (HIMSS) in Orlando, Dr. Karen DeSalvo, national health IT coordinator, made a strong plea for interoperability by 2017. She said "We can do national health care exchange in 3 years. ... I want this as a doctor, I want this as patient, I want this as a daughter."
Dr. DeSalvo’s words resonate because this is a concept we all expected from the earliest days of electronic records. Unfortunately, barriers – both real and artificial – have stood in the way. First and foremost are patient privacy and information security. It is essential that patient data are protected and maintained as the data pass from one system to the next, but often, even the basic function of matching patients with the right records can be challenging. Many identifiers exist, including various medical record numbers and insurance codes. If a name is misspelled or middle initial omitted, this can also create significant chaos and allow sensitive data to file into the wrong place, creating HIPAA violations and distrust among patients.
In addition to concerns over data security, the lack of standard formatting for storing and sharing records has been a huge hurdle for EHR vendors. Not surprisingly, the simultaneous development of dozens of competing EHR products has created significant fragmentation throughout the market. Instead of starting from a common set of data elements, each EHR was essentially designed "in a vacuum," and only now are their creators attempting to find a way to get them to communicate. A number of cross-platform projects currently underway highlight this effort.
VHS or Betamax?
On Feb. 25, 2014, NextGen Healthcare and Cerner announced bilateral certification of their EHR products and affirmed their commitment to interoperability. According to the press release, they are committed to "creating proactive working relationships, expanding the boundaries of current interoperability ... and supporting the efforts of [their] clients to advance the health of their communities." These may not be novel goals, but at least both vendors have demonstrated their best attempt to achieve them. Also, both companies have a huge footprint in the market, so their collaboration is certain to raise the level of attention being paid to this topic. But this isn’t the only attempt at broad-based interoperability.
EClinicalWorks (eCW), another large player in the ambulatory EHR market, has developed a product know as P2P, or Provider to Provider. Originally conceived as a way to communicate between different users of the eCW platform, it has now been expanded to all providers, regardless of their EHR, as a secure communication tool. This new product is known as P2POpen and is free to any health care professional wishing to join "the network." According to their website, P2POpen now boasts close to 22,000 users and facilitates "improved quality, safety, and efficiency of care." Like the collaboration mentioned above, P2POpen has a shot at success, but both of these efforts may also portend more debate over standardization moving forward. Will the disparity in how each company addresses the issue of interoperability lead to further fragmentation? And how can we be sure that embracing one of these ideas won’t severely limit us in the future?
Setting the standard
The only way to answer these and other looming concerns over developing a consistent interoperability protocol is to start at the top and rapidly build consensus. In other words, Dr. DeSalvo’s words need to be quickly translated into action, as she and other thought leaders agree – not only on a standard – but also on a way to properly motivate EHR vendors to adopt that standard.
One possible opportunity to enforce this as Meaningful Use stage III. The requirements for stage III EHR certification, which have yet to be finalized, should include a necessity for every vendor to adopt a consistent format for information exchange and data transmission. Making this a certification requirement will ensure that all EHR products remain cooperative if they plan to stay competitive.
Another solution being considered involves the use of centralized "Health Information Exchanges," which could collect and warehouse data from multiple sources and then retransmit those data in a universally readable format. Either way, if a consensus can be reached and issues over privacy and security addressed, it will only spell a victory for physicians and patients and truly get us on the road to improved patient care and outcomes. We tend to agree with Dr. DeSalvo, and believe that victory is well within reach.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. An avid programmer, he has published software for handheld devices in partnership with national organizations, and he is always looking for new ways to bring evidence-based medicine to the point of care. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is also editor-in-chief of Redi-Reference Inc., a software company that creates mobile apps.
EHR Report: One step at a time
The response to our request for readers to comment on their experiences with electronic health records continues to astonish us, with the quantity, depth, and intensity of responses. The majority of e-mails discuss concerns about the way EHRs have affected both patient care and office workflow, and we have made an effort to make sure that these voices are heard.
This month, we thought that we would emphasize a response from Dr. Don Weinshenker, a general internist in Denver who has worked in the VA system since 1992 and who describes himself as a "champion" of the EHR for over a decade. What we like about Dr. Weinshenker’s comments is that while he acknowledges the challenges inherent in adopting electronic records, he also offers some solutions based on a decade of experience. Some of his suggestions remind us of columns we published about a year ago on Humanism and EHRs, two words seldom used together, but which present what we feel is an important concept – discerning how to use our new tools to carry out, not distract us from, our core goals of connecting with other human beings to help safely alleviate suffering and improve health using an empathic manner that communicates caring and understanding. Dr. Weinshenker shares his thoughts as follows:
I feel it is quite possible and relatively easy to integrate the computer into an exam room while maintaining the excellent clinician/patient experience for which we all strive.
The first thing I do when I walk into a room is greet the patient and look the patient in the eye. I don’t look at the computer at first. I then acknowledge the "elephant in the room." I usually say something to the effect of, "As you likely know, we do almost everything on the computer. I will be using the computer today during this visit." I have not had a single patient object.
Next I do bring the patient’s chart up on the computer, if I hadn’t already preloaded it, and open a progress note with my simple template. I then turn to the patient, away from the computer, and start to take a history. At an appropriate pause I say, "Let me get that into your chart." I do turn to the computer at that time and start to type. I repeat what the patient told me as I type. By doing this, patients know what I am typing as well as experiencing a version of "reflective listening" so that they know that I truly did hear them. Also, I always clarify as I type. "The left foot pain has been going on for 2 weeks, or was it 3 weeks?" I write my primary care note in real time while talking with the patient. The majority of the content of my notes is in natural language, as opposed to clicking on little phrases.
Then, I talk about what I am doing in terms of ordering on the computer. "I am going to go ahead and order that podiatry consult now. You said that you would prefer to be seen after the 15th, right? I’ll order that x-ray we talked about as well."
I am sitting at a desk with the patient next to me facing me. It only takes a small turn of my head to face the patient. It is common for me to turn the computer screen a little so it faces the patient. I involve the patients with the computer. Very frequently, they can actually see what I am typing into the computer. In addition, for many of the computerized clinical reminders that we use, I will have the patient read the questions off the screen, e.g., for depression screening, so that they can answer the questions directly.
It appears that some of your readers have misconceptions about the role of computers. At least one mentioned that the computers are essentially going to replace doctors. Ideally, the use of computers is synergistic. The whole is more than the sum of the parts. Using cars as an analogy, no one complains about having power steering or brakes in a car. They make the car easier to drive. It is more common to have a lane change warning if there is a car in the next lane. Some of the fanciest cars, such as the top-end Mercedes, monitor what is in front of the car and will automatically put on the brakes if a pedestrian is present. I can’t afford that car but would be grateful if I had it and it saved the life of a pedestrian who stepped in front of me.
This brings up the questions of alerts and alert fatigue. One wouldn’t want a beep and/or a warning light every time a car passes you in the next lane. Clearly, there has to be more work on alerts making them smarter and more configurable, as otherwise they just become noise. EHRs are far from perfect, but with good design and with thoughtful implementation, I am completely convinced that they are an aid rather than a hindrance.
We like Dr. Weinshenker’s thoughts – he has figured out and shared ways to incorporate and communicate his care for and attention to patients into his workflow with the EHR. We are still at the beginning of our transformation from paper to electronic records, and this change is not easy. It has been said, beginnings are always hard. It is through shared suggestions like those provided by Dr. Weinshenker that we will together develop a patient-oriented electronic approach. Keep those comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
The response to our request for readers to comment on their experiences with electronic health records continues to astonish us, with the quantity, depth, and intensity of responses. The majority of e-mails discuss concerns about the way EHRs have affected both patient care and office workflow, and we have made an effort to make sure that these voices are heard.
This month, we thought that we would emphasize a response from Dr. Don Weinshenker, a general internist in Denver who has worked in the VA system since 1992 and who describes himself as a "champion" of the EHR for over a decade. What we like about Dr. Weinshenker’s comments is that while he acknowledges the challenges inherent in adopting electronic records, he also offers some solutions based on a decade of experience. Some of his suggestions remind us of columns we published about a year ago on Humanism and EHRs, two words seldom used together, but which present what we feel is an important concept – discerning how to use our new tools to carry out, not distract us from, our core goals of connecting with other human beings to help safely alleviate suffering and improve health using an empathic manner that communicates caring and understanding. Dr. Weinshenker shares his thoughts as follows:
I feel it is quite possible and relatively easy to integrate the computer into an exam room while maintaining the excellent clinician/patient experience for which we all strive.
The first thing I do when I walk into a room is greet the patient and look the patient in the eye. I don’t look at the computer at first. I then acknowledge the "elephant in the room." I usually say something to the effect of, "As you likely know, we do almost everything on the computer. I will be using the computer today during this visit." I have not had a single patient object.
Next I do bring the patient’s chart up on the computer, if I hadn’t already preloaded it, and open a progress note with my simple template. I then turn to the patient, away from the computer, and start to take a history. At an appropriate pause I say, "Let me get that into your chart." I do turn to the computer at that time and start to type. I repeat what the patient told me as I type. By doing this, patients know what I am typing as well as experiencing a version of "reflective listening" so that they know that I truly did hear them. Also, I always clarify as I type. "The left foot pain has been going on for 2 weeks, or was it 3 weeks?" I write my primary care note in real time while talking with the patient. The majority of the content of my notes is in natural language, as opposed to clicking on little phrases.
Then, I talk about what I am doing in terms of ordering on the computer. "I am going to go ahead and order that podiatry consult now. You said that you would prefer to be seen after the 15th, right? I’ll order that x-ray we talked about as well."
I am sitting at a desk with the patient next to me facing me. It only takes a small turn of my head to face the patient. It is common for me to turn the computer screen a little so it faces the patient. I involve the patients with the computer. Very frequently, they can actually see what I am typing into the computer. In addition, for many of the computerized clinical reminders that we use, I will have the patient read the questions off the screen, e.g., for depression screening, so that they can answer the questions directly.
It appears that some of your readers have misconceptions about the role of computers. At least one mentioned that the computers are essentially going to replace doctors. Ideally, the use of computers is synergistic. The whole is more than the sum of the parts. Using cars as an analogy, no one complains about having power steering or brakes in a car. They make the car easier to drive. It is more common to have a lane change warning if there is a car in the next lane. Some of the fanciest cars, such as the top-end Mercedes, monitor what is in front of the car and will automatically put on the brakes if a pedestrian is present. I can’t afford that car but would be grateful if I had it and it saved the life of a pedestrian who stepped in front of me.
This brings up the questions of alerts and alert fatigue. One wouldn’t want a beep and/or a warning light every time a car passes you in the next lane. Clearly, there has to be more work on alerts making them smarter and more configurable, as otherwise they just become noise. EHRs are far from perfect, but with good design and with thoughtful implementation, I am completely convinced that they are an aid rather than a hindrance.
We like Dr. Weinshenker’s thoughts – he has figured out and shared ways to incorporate and communicate his care for and attention to patients into his workflow with the EHR. We are still at the beginning of our transformation from paper to electronic records, and this change is not easy. It has been said, beginnings are always hard. It is through shared suggestions like those provided by Dr. Weinshenker that we will together develop a patient-oriented electronic approach. Keep those comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
The response to our request for readers to comment on their experiences with electronic health records continues to astonish us, with the quantity, depth, and intensity of responses. The majority of e-mails discuss concerns about the way EHRs have affected both patient care and office workflow, and we have made an effort to make sure that these voices are heard.
This month, we thought that we would emphasize a response from Dr. Don Weinshenker, a general internist in Denver who has worked in the VA system since 1992 and who describes himself as a "champion" of the EHR for over a decade. What we like about Dr. Weinshenker’s comments is that while he acknowledges the challenges inherent in adopting electronic records, he also offers some solutions based on a decade of experience. Some of his suggestions remind us of columns we published about a year ago on Humanism and EHRs, two words seldom used together, but which present what we feel is an important concept – discerning how to use our new tools to carry out, not distract us from, our core goals of connecting with other human beings to help safely alleviate suffering and improve health using an empathic manner that communicates caring and understanding. Dr. Weinshenker shares his thoughts as follows:
I feel it is quite possible and relatively easy to integrate the computer into an exam room while maintaining the excellent clinician/patient experience for which we all strive.
The first thing I do when I walk into a room is greet the patient and look the patient in the eye. I don’t look at the computer at first. I then acknowledge the "elephant in the room." I usually say something to the effect of, "As you likely know, we do almost everything on the computer. I will be using the computer today during this visit." I have not had a single patient object.
Next I do bring the patient’s chart up on the computer, if I hadn’t already preloaded it, and open a progress note with my simple template. I then turn to the patient, away from the computer, and start to take a history. At an appropriate pause I say, "Let me get that into your chart." I do turn to the computer at that time and start to type. I repeat what the patient told me as I type. By doing this, patients know what I am typing as well as experiencing a version of "reflective listening" so that they know that I truly did hear them. Also, I always clarify as I type. "The left foot pain has been going on for 2 weeks, or was it 3 weeks?" I write my primary care note in real time while talking with the patient. The majority of the content of my notes is in natural language, as opposed to clicking on little phrases.
Then, I talk about what I am doing in terms of ordering on the computer. "I am going to go ahead and order that podiatry consult now. You said that you would prefer to be seen after the 15th, right? I’ll order that x-ray we talked about as well."
I am sitting at a desk with the patient next to me facing me. It only takes a small turn of my head to face the patient. It is common for me to turn the computer screen a little so it faces the patient. I involve the patients with the computer. Very frequently, they can actually see what I am typing into the computer. In addition, for many of the computerized clinical reminders that we use, I will have the patient read the questions off the screen, e.g., for depression screening, so that they can answer the questions directly.
It appears that some of your readers have misconceptions about the role of computers. At least one mentioned that the computers are essentially going to replace doctors. Ideally, the use of computers is synergistic. The whole is more than the sum of the parts. Using cars as an analogy, no one complains about having power steering or brakes in a car. They make the car easier to drive. It is more common to have a lane change warning if there is a car in the next lane. Some of the fanciest cars, such as the top-end Mercedes, monitor what is in front of the car and will automatically put on the brakes if a pedestrian is present. I can’t afford that car but would be grateful if I had it and it saved the life of a pedestrian who stepped in front of me.
This brings up the questions of alerts and alert fatigue. One wouldn’t want a beep and/or a warning light every time a car passes you in the next lane. Clearly, there has to be more work on alerts making them smarter and more configurable, as otherwise they just become noise. EHRs are far from perfect, but with good design and with thoughtful implementation, I am completely convinced that they are an aid rather than a hindrance.
We like Dr. Weinshenker’s thoughts – he has figured out and shared ways to incorporate and communicate his care for and attention to patients into his workflow with the EHR. We are still at the beginning of our transformation from paper to electronic records, and this change is not easy. It has been said, beginnings are always hard. It is through shared suggestions like those provided by Dr. Weinshenker that we will together develop a patient-oriented electronic approach. Keep those comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
Long days and distracted driving
The response to our request for readers to share their experiences with electronic health records continues to be intense, with comments that generally recognize the advantages of EHRs but emphasize the challenges they have presented for workflow and patient interactions. Some responses are downright negative, and reflect a level of frustration and disappointment in a system that they feel is no longer working for them or their patients.
Mark Goldberg is a family doctor in Alpharetta, Ga. He has practiced in a variety of settings over the last 29 years, and recently moved to urgent care from traditional primary care medicine in large part because of EHR implementation in his office practice.
His practice, part of a large health system, was located in a rural, underserved county. He had been a part of that practice for 16 years, and worked in an office with four other physicians. He describes their practice as serving the community in all capacities, including walk-in, same-day appointments. As he says it, "If our patients needed us, we saw them." Their average appointment load per doctor was about 25-30 patients per day. Their practice used paper charts, which where often dictated. Dr. Goldberg, on making the transition to an EHR:
At large cost, the owners of the clinic implemented an EHR, and initial users were dissatisfied with both the difficulty of using the system and the way it slowed workflow. Training was intensive. Nonetheless, dissatisfaction was high.
The handwriting was on the wall, and I left the practice coincident with the implementation of the EHR. Sadly, my fears were realized for my ex-partners and my patients. Productivity dropped dramatically, and stays low to this day. The practice no longer sees walk-ins. The physicians barely see 20-22 patients per day, down about 20% from the number of patients seen before the EHR. The physicians are often there 2-4 hours after the office closes to finish typing their notes, whereas we used to leave within a half-hour of closing. One physician told me that he would only allow his patients to tell him one complaint per visit, because he didn’t feel he had time to document more. He also felt his notes in the EHR were much less complete than his dictated notes in the paper chart. Physician quality of life and family time has been dramatically impacted. Patients are angry and frustrated. Two other physicians ultimately left our practice as well and have been very hard to replace.
In my opinion, implementing EHR destroyed a healthy and happy practice that served its patients well, and filled a huge need in an underserved county. Three out of five physicians left the practice, leaving primary care for good. I do not feel that this was due to "poor implementation," as everyone in the practice had extensive training prior to going live. I see it more as a failure of the EHR vender to understand the workflow needs of physicians in a busy office setting.
Dr. Goldberg voices a point of view that, unfortunately, we’ve heard before – that EHRs change the way a practice runs, decrease productivity, and distance physicians from patients. The experience in his practice serves as a warning to others to be careful both with their expectations for their EHR, the selection of which EHR to purchase, and how to implement its use in their office.
Dr. Mel Chandler, a 66-year-old family physician from Edmonds, Wash., shared insights informed by seeing many changes to the practice of medicine over his long career:
I have had many experiences over the years including an elderly practice partner in my first 3 years who managed to keep all of his records on 3-by-5 cards in his desk. In the left-hand top drawer were his patient notes on these cards and in the right-top drawer, his 3-by-5 cards with records of the loans he made to his patients, often at no interest. It worked well for him, but not so well for those of us needing information when on call. For our records, we dictated a SOAP [subjective, objective, assessment, and plan] note. This worked well enough for years.
I believe the EHR may help with record keeping in a very limited fashion. The programs I have seen are complex, use templates, and make it difficult to enter information. I have resisted the use of templates previously so that I could freely think rather than have my thinking directed by a prescribed format. Over the last decade, I have changed my practice to focus purely on those who have severe mental illness. It is important for me to maintain eye contact or at minimum watch my clients at all times while they are in my presence. In my state of residence it is illegal to text and drive an automobile. This is because of the disastrous effects of the distraction of typing. Is my interaction with my patients no less important to perform with full attention than driving? We meet with patients/clients to have a person-to-person interaction to problem solve, teach, and often console.
The major point of my note is that we must "protect" the patient/physician interaction. We must support the concept that the manner in which we take a history and perform an exam is important and cannot be "cut short" by electronic devices that require us to take our eyes from the road ahead.
We admire Dr. Chandler’s analogy relating the importance of full attention to patients to the driving experience and seeing what is on the road.
Keep those emails and comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
The response to our request for readers to share their experiences with electronic health records continues to be intense, with comments that generally recognize the advantages of EHRs but emphasize the challenges they have presented for workflow and patient interactions. Some responses are downright negative, and reflect a level of frustration and disappointment in a system that they feel is no longer working for them or their patients.
Mark Goldberg is a family doctor in Alpharetta, Ga. He has practiced in a variety of settings over the last 29 years, and recently moved to urgent care from traditional primary care medicine in large part because of EHR implementation in his office practice.
His practice, part of a large health system, was located in a rural, underserved county. He had been a part of that practice for 16 years, and worked in an office with four other physicians. He describes their practice as serving the community in all capacities, including walk-in, same-day appointments. As he says it, "If our patients needed us, we saw them." Their average appointment load per doctor was about 25-30 patients per day. Their practice used paper charts, which where often dictated. Dr. Goldberg, on making the transition to an EHR:
At large cost, the owners of the clinic implemented an EHR, and initial users were dissatisfied with both the difficulty of using the system and the way it slowed workflow. Training was intensive. Nonetheless, dissatisfaction was high.
The handwriting was on the wall, and I left the practice coincident with the implementation of the EHR. Sadly, my fears were realized for my ex-partners and my patients. Productivity dropped dramatically, and stays low to this day. The practice no longer sees walk-ins. The physicians barely see 20-22 patients per day, down about 20% from the number of patients seen before the EHR. The physicians are often there 2-4 hours after the office closes to finish typing their notes, whereas we used to leave within a half-hour of closing. One physician told me that he would only allow his patients to tell him one complaint per visit, because he didn’t feel he had time to document more. He also felt his notes in the EHR were much less complete than his dictated notes in the paper chart. Physician quality of life and family time has been dramatically impacted. Patients are angry and frustrated. Two other physicians ultimately left our practice as well and have been very hard to replace.
In my opinion, implementing EHR destroyed a healthy and happy practice that served its patients well, and filled a huge need in an underserved county. Three out of five physicians left the practice, leaving primary care for good. I do not feel that this was due to "poor implementation," as everyone in the practice had extensive training prior to going live. I see it more as a failure of the EHR vender to understand the workflow needs of physicians in a busy office setting.
Dr. Goldberg voices a point of view that, unfortunately, we’ve heard before – that EHRs change the way a practice runs, decrease productivity, and distance physicians from patients. The experience in his practice serves as a warning to others to be careful both with their expectations for their EHR, the selection of which EHR to purchase, and how to implement its use in their office.
Dr. Mel Chandler, a 66-year-old family physician from Edmonds, Wash., shared insights informed by seeing many changes to the practice of medicine over his long career:
I have had many experiences over the years including an elderly practice partner in my first 3 years who managed to keep all of his records on 3-by-5 cards in his desk. In the left-hand top drawer were his patient notes on these cards and in the right-top drawer, his 3-by-5 cards with records of the loans he made to his patients, often at no interest. It worked well for him, but not so well for those of us needing information when on call. For our records, we dictated a SOAP [subjective, objective, assessment, and plan] note. This worked well enough for years.
I believe the EHR may help with record keeping in a very limited fashion. The programs I have seen are complex, use templates, and make it difficult to enter information. I have resisted the use of templates previously so that I could freely think rather than have my thinking directed by a prescribed format. Over the last decade, I have changed my practice to focus purely on those who have severe mental illness. It is important for me to maintain eye contact or at minimum watch my clients at all times while they are in my presence. In my state of residence it is illegal to text and drive an automobile. This is because of the disastrous effects of the distraction of typing. Is my interaction with my patients no less important to perform with full attention than driving? We meet with patients/clients to have a person-to-person interaction to problem solve, teach, and often console.
The major point of my note is that we must "protect" the patient/physician interaction. We must support the concept that the manner in which we take a history and perform an exam is important and cannot be "cut short" by electronic devices that require us to take our eyes from the road ahead.
We admire Dr. Chandler’s analogy relating the importance of full attention to patients to the driving experience and seeing what is on the road.
Keep those emails and comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
The response to our request for readers to share their experiences with electronic health records continues to be intense, with comments that generally recognize the advantages of EHRs but emphasize the challenges they have presented for workflow and patient interactions. Some responses are downright negative, and reflect a level of frustration and disappointment in a system that they feel is no longer working for them or their patients.
Mark Goldberg is a family doctor in Alpharetta, Ga. He has practiced in a variety of settings over the last 29 years, and recently moved to urgent care from traditional primary care medicine in large part because of EHR implementation in his office practice.
His practice, part of a large health system, was located in a rural, underserved county. He had been a part of that practice for 16 years, and worked in an office with four other physicians. He describes their practice as serving the community in all capacities, including walk-in, same-day appointments. As he says it, "If our patients needed us, we saw them." Their average appointment load per doctor was about 25-30 patients per day. Their practice used paper charts, which where often dictated. Dr. Goldberg, on making the transition to an EHR:
At large cost, the owners of the clinic implemented an EHR, and initial users were dissatisfied with both the difficulty of using the system and the way it slowed workflow. Training was intensive. Nonetheless, dissatisfaction was high.
The handwriting was on the wall, and I left the practice coincident with the implementation of the EHR. Sadly, my fears were realized for my ex-partners and my patients. Productivity dropped dramatically, and stays low to this day. The practice no longer sees walk-ins. The physicians barely see 20-22 patients per day, down about 20% from the number of patients seen before the EHR. The physicians are often there 2-4 hours after the office closes to finish typing their notes, whereas we used to leave within a half-hour of closing. One physician told me that he would only allow his patients to tell him one complaint per visit, because he didn’t feel he had time to document more. He also felt his notes in the EHR were much less complete than his dictated notes in the paper chart. Physician quality of life and family time has been dramatically impacted. Patients are angry and frustrated. Two other physicians ultimately left our practice as well and have been very hard to replace.
In my opinion, implementing EHR destroyed a healthy and happy practice that served its patients well, and filled a huge need in an underserved county. Three out of five physicians left the practice, leaving primary care for good. I do not feel that this was due to "poor implementation," as everyone in the practice had extensive training prior to going live. I see it more as a failure of the EHR vender to understand the workflow needs of physicians in a busy office setting.
Dr. Goldberg voices a point of view that, unfortunately, we’ve heard before – that EHRs change the way a practice runs, decrease productivity, and distance physicians from patients. The experience in his practice serves as a warning to others to be careful both with their expectations for their EHR, the selection of which EHR to purchase, and how to implement its use in their office.
Dr. Mel Chandler, a 66-year-old family physician from Edmonds, Wash., shared insights informed by seeing many changes to the practice of medicine over his long career:
I have had many experiences over the years including an elderly practice partner in my first 3 years who managed to keep all of his records on 3-by-5 cards in his desk. In the left-hand top drawer were his patient notes on these cards and in the right-top drawer, his 3-by-5 cards with records of the loans he made to his patients, often at no interest. It worked well for him, but not so well for those of us needing information when on call. For our records, we dictated a SOAP [subjective, objective, assessment, and plan] note. This worked well enough for years.
I believe the EHR may help with record keeping in a very limited fashion. The programs I have seen are complex, use templates, and make it difficult to enter information. I have resisted the use of templates previously so that I could freely think rather than have my thinking directed by a prescribed format. Over the last decade, I have changed my practice to focus purely on those who have severe mental illness. It is important for me to maintain eye contact or at minimum watch my clients at all times while they are in my presence. In my state of residence it is illegal to text and drive an automobile. This is because of the disastrous effects of the distraction of typing. Is my interaction with my patients no less important to perform with full attention than driving? We meet with patients/clients to have a person-to-person interaction to problem solve, teach, and often console.
The major point of my note is that we must "protect" the patient/physician interaction. We must support the concept that the manner in which we take a history and perform an exam is important and cannot be "cut short" by electronic devices that require us to take our eyes from the road ahead.
We admire Dr. Chandler’s analogy relating the importance of full attention to patients to the driving experience and seeing what is on the road.
Keep those emails and comments coming.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
EHR Report: Reflections from our readers
In response to our request for comments, readers have graciously flooded our inbox with a variety of e-mails full of opinions on electronic health records.
This has been an overwhelmingly positive and educational experience. Through your comments, we have been reminded that health information technology is a field rife with debate. Here, unlike most other areas of medicine, it is still impossible to define a single best practice that can reliably be employed in every EHR implementation.
Although we are convinced that it is the timeliness of the subject matter that actually drives readership, we truly appreciate the personal words of affirmation we receive every month. And though we do try to respond to feedback individually whenever possible, we think it is important to again say thank you to everyone who has cared enough to read and respond. You help us to better navigate the murky waters of electronic health records and help make sure that our comments are grounded in the day-to-day experiences of a wide range of users.
Over thenext few columns (with the permission of the authors), we will be publishing many of the comments we have received. Not surprisingly, the majority of messages discuss negative experiences, with an occasional e-mail that speaks to the benefits of the EHR. The focus has really been on how the transition to electronic health records has changed the physician/patient experience and the efficiencies – or inefficiencies – introduced by the use of EHRs. Many respondents expressed appreciation for the opportunity to vent their frustrations, and this further underscores the need for better, more open discussion on the topic.
One letter that reflects a balanced sentiment, yet captures the overall flavor of the thoughts expressed by our fellow physicians, came from Dr. Marc D. Grobman, a solo family physician in Wilmington, Del. Dr. Grobman adopted Practice Fusion, a free ad-supported EHR that we mentioned in a previous column. He relates his experience before and after the EHR, and how it has affected his practice:
"So let’s start with my routine before EMR [electronic medical records]. I would arrive at the office at 8:30 a.m. after seeing my kids off at the school bus. I would greet my staff and start seeing patients at 9:00 a.m. During the day, messages would pile up in the little basket for me, and I would quickly jot answers to questions or requests and hand them back to my staff between patients. During lunch, I would quickly eat ... and then jump to the mail, sign everything then enter into a Word file for the patient (the poor-man’s EMR) and then bring it to the staff for filing. The filing would often take days to accomplish because, being solo, I have only two other staff members.
"Now my days at the office begin at 7:45 a.m. (after rising at 5:30 a.m. to shower, eat, and check the EMR for prescription renewals, use the Delaware Health Information Network [DHIN] to look for admissions to the local hospitals and download the lab results, H&Ps, consults, radiology reports, and so on) with a grab of incoming faxes off the fax machine. I then race to my desk and turn on the computer and scanner to scan everything. Then I race to upload the material before the patients start at 9:00 a.m. Between patients, or most often at lunch, I answer "Messages" on the EMR, write Rx’s and handle any other things that come up. During lunch I also take time to scan and upload as quickly as possible. Same routine after lunch. Before I go home @ 6 or 7 p.m., I make sure everything is scanned so I can upload after dinner at home. No filing any more for the staff, since I scan and upload everything."
On first glance, Dr. Grobman’s experience seems quite discouraging, as he has seemingly transitioned his job description from physician to staff. He even goes on to admit being "baffled" by trying to find any meaning in meaningful use. But his closing thoughts do not express regret. Instead, he shares this:
"I do like using the EMR. I like being green and not needing paper, files, folders, stickers. ... I do find it worthwhile to have [an electronic] copy of the paper forms I do fill out for prior authorizations or pre-exclusion questions or legal request-just in case, you know, someone on the other end loses it. Is the trade-off worth it? In the end I am just more than slightly positive about this whole process."
This letter does a wonderful job of articulating some of the advantages and irritations of a successful EHR implementation. Dr. Grobman also alludes to another interesting theme: frustration with the meaningful use incentive program. Again, he is not alone here. Some readers, like Dr. Michael Laidlaw of Rocklin, Calif., admit to rejecting the government incentive program altogether. Dr. Laidlaw writes:
"What made me abandon the incentive this year (I qualified for and was reimbursed for stage 1) is when I realized that I spent the first 2-5 minutes of each visit endlessly clicking a bunch of garbage to make all the green lights show up on the [meaningful use] meter. I said to myself: ‘I’m not wasting precious seconds of my life and my patients’ time to ensure some database gets filled with data. I didn’t go into medicine for this. It is not benefiting my patients or me. I hate it.’ I actually refused to take the $10K+ this year. I have even accepted that I would rather be penalized in the future. What is worth the most to me is AUTONOMY."
In reviewing all of the feedback we’ve received, this idea seems to come up again and again. Physicians are willing to accept the time-consuming idiosyncrasies of electronic health records but are offended by the idea of technologic or governmental intrusion into the physician-patient relationship. We will continue to explore this idea in the coming months as we share more reader comments and response to the column.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
In response to our request for comments, readers have graciously flooded our inbox with a variety of e-mails full of opinions on electronic health records.
This has been an overwhelmingly positive and educational experience. Through your comments, we have been reminded that health information technology is a field rife with debate. Here, unlike most other areas of medicine, it is still impossible to define a single best practice that can reliably be employed in every EHR implementation.
Although we are convinced that it is the timeliness of the subject matter that actually drives readership, we truly appreciate the personal words of affirmation we receive every month. And though we do try to respond to feedback individually whenever possible, we think it is important to again say thank you to everyone who has cared enough to read and respond. You help us to better navigate the murky waters of electronic health records and help make sure that our comments are grounded in the day-to-day experiences of a wide range of users.
Over thenext few columns (with the permission of the authors), we will be publishing many of the comments we have received. Not surprisingly, the majority of messages discuss negative experiences, with an occasional e-mail that speaks to the benefits of the EHR. The focus has really been on how the transition to electronic health records has changed the physician/patient experience and the efficiencies – or inefficiencies – introduced by the use of EHRs. Many respondents expressed appreciation for the opportunity to vent their frustrations, and this further underscores the need for better, more open discussion on the topic.
One letter that reflects a balanced sentiment, yet captures the overall flavor of the thoughts expressed by our fellow physicians, came from Dr. Marc D. Grobman, a solo family physician in Wilmington, Del. Dr. Grobman adopted Practice Fusion, a free ad-supported EHR that we mentioned in a previous column. He relates his experience before and after the EHR, and how it has affected his practice:
"So let’s start with my routine before EMR [electronic medical records]. I would arrive at the office at 8:30 a.m. after seeing my kids off at the school bus. I would greet my staff and start seeing patients at 9:00 a.m. During the day, messages would pile up in the little basket for me, and I would quickly jot answers to questions or requests and hand them back to my staff between patients. During lunch, I would quickly eat ... and then jump to the mail, sign everything then enter into a Word file for the patient (the poor-man’s EMR) and then bring it to the staff for filing. The filing would often take days to accomplish because, being solo, I have only two other staff members.
"Now my days at the office begin at 7:45 a.m. (after rising at 5:30 a.m. to shower, eat, and check the EMR for prescription renewals, use the Delaware Health Information Network [DHIN] to look for admissions to the local hospitals and download the lab results, H&Ps, consults, radiology reports, and so on) with a grab of incoming faxes off the fax machine. I then race to my desk and turn on the computer and scanner to scan everything. Then I race to upload the material before the patients start at 9:00 a.m. Between patients, or most often at lunch, I answer "Messages" on the EMR, write Rx’s and handle any other things that come up. During lunch I also take time to scan and upload as quickly as possible. Same routine after lunch. Before I go home @ 6 or 7 p.m., I make sure everything is scanned so I can upload after dinner at home. No filing any more for the staff, since I scan and upload everything."
On first glance, Dr. Grobman’s experience seems quite discouraging, as he has seemingly transitioned his job description from physician to staff. He even goes on to admit being "baffled" by trying to find any meaning in meaningful use. But his closing thoughts do not express regret. Instead, he shares this:
"I do like using the EMR. I like being green and not needing paper, files, folders, stickers. ... I do find it worthwhile to have [an electronic] copy of the paper forms I do fill out for prior authorizations or pre-exclusion questions or legal request-just in case, you know, someone on the other end loses it. Is the trade-off worth it? In the end I am just more than slightly positive about this whole process."
This letter does a wonderful job of articulating some of the advantages and irritations of a successful EHR implementation. Dr. Grobman also alludes to another interesting theme: frustration with the meaningful use incentive program. Again, he is not alone here. Some readers, like Dr. Michael Laidlaw of Rocklin, Calif., admit to rejecting the government incentive program altogether. Dr. Laidlaw writes:
"What made me abandon the incentive this year (I qualified for and was reimbursed for stage 1) is when I realized that I spent the first 2-5 minutes of each visit endlessly clicking a bunch of garbage to make all the green lights show up on the [meaningful use] meter. I said to myself: ‘I’m not wasting precious seconds of my life and my patients’ time to ensure some database gets filled with data. I didn’t go into medicine for this. It is not benefiting my patients or me. I hate it.’ I actually refused to take the $10K+ this year. I have even accepted that I would rather be penalized in the future. What is worth the most to me is AUTONOMY."
In reviewing all of the feedback we’ve received, this idea seems to come up again and again. Physicians are willing to accept the time-consuming idiosyncrasies of electronic health records but are offended by the idea of technologic or governmental intrusion into the physician-patient relationship. We will continue to explore this idea in the coming months as we share more reader comments and response to the column.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
In response to our request for comments, readers have graciously flooded our inbox with a variety of e-mails full of opinions on electronic health records.
This has been an overwhelmingly positive and educational experience. Through your comments, we have been reminded that health information technology is a field rife with debate. Here, unlike most other areas of medicine, it is still impossible to define a single best practice that can reliably be employed in every EHR implementation.
Although we are convinced that it is the timeliness of the subject matter that actually drives readership, we truly appreciate the personal words of affirmation we receive every month. And though we do try to respond to feedback individually whenever possible, we think it is important to again say thank you to everyone who has cared enough to read and respond. You help us to better navigate the murky waters of electronic health records and help make sure that our comments are grounded in the day-to-day experiences of a wide range of users.
Over thenext few columns (with the permission of the authors), we will be publishing many of the comments we have received. Not surprisingly, the majority of messages discuss negative experiences, with an occasional e-mail that speaks to the benefits of the EHR. The focus has really been on how the transition to electronic health records has changed the physician/patient experience and the efficiencies – or inefficiencies – introduced by the use of EHRs. Many respondents expressed appreciation for the opportunity to vent their frustrations, and this further underscores the need for better, more open discussion on the topic.
One letter that reflects a balanced sentiment, yet captures the overall flavor of the thoughts expressed by our fellow physicians, came from Dr. Marc D. Grobman, a solo family physician in Wilmington, Del. Dr. Grobman adopted Practice Fusion, a free ad-supported EHR that we mentioned in a previous column. He relates his experience before and after the EHR, and how it has affected his practice:
"So let’s start with my routine before EMR [electronic medical records]. I would arrive at the office at 8:30 a.m. after seeing my kids off at the school bus. I would greet my staff and start seeing patients at 9:00 a.m. During the day, messages would pile up in the little basket for me, and I would quickly jot answers to questions or requests and hand them back to my staff between patients. During lunch, I would quickly eat ... and then jump to the mail, sign everything then enter into a Word file for the patient (the poor-man’s EMR) and then bring it to the staff for filing. The filing would often take days to accomplish because, being solo, I have only two other staff members.
"Now my days at the office begin at 7:45 a.m. (after rising at 5:30 a.m. to shower, eat, and check the EMR for prescription renewals, use the Delaware Health Information Network [DHIN] to look for admissions to the local hospitals and download the lab results, H&Ps, consults, radiology reports, and so on) with a grab of incoming faxes off the fax machine. I then race to my desk and turn on the computer and scanner to scan everything. Then I race to upload the material before the patients start at 9:00 a.m. Between patients, or most often at lunch, I answer "Messages" on the EMR, write Rx’s and handle any other things that come up. During lunch I also take time to scan and upload as quickly as possible. Same routine after lunch. Before I go home @ 6 or 7 p.m., I make sure everything is scanned so I can upload after dinner at home. No filing any more for the staff, since I scan and upload everything."
On first glance, Dr. Grobman’s experience seems quite discouraging, as he has seemingly transitioned his job description from physician to staff. He even goes on to admit being "baffled" by trying to find any meaning in meaningful use. But his closing thoughts do not express regret. Instead, he shares this:
"I do like using the EMR. I like being green and not needing paper, files, folders, stickers. ... I do find it worthwhile to have [an electronic] copy of the paper forms I do fill out for prior authorizations or pre-exclusion questions or legal request-just in case, you know, someone on the other end loses it. Is the trade-off worth it? In the end I am just more than slightly positive about this whole process."
This letter does a wonderful job of articulating some of the advantages and irritations of a successful EHR implementation. Dr. Grobman also alludes to another interesting theme: frustration with the meaningful use incentive program. Again, he is not alone here. Some readers, like Dr. Michael Laidlaw of Rocklin, Calif., admit to rejecting the government incentive program altogether. Dr. Laidlaw writes:
"What made me abandon the incentive this year (I qualified for and was reimbursed for stage 1) is when I realized that I spent the first 2-5 minutes of each visit endlessly clicking a bunch of garbage to make all the green lights show up on the [meaningful use] meter. I said to myself: ‘I’m not wasting precious seconds of my life and my patients’ time to ensure some database gets filled with data. I didn’t go into medicine for this. It is not benefiting my patients or me. I hate it.’ I actually refused to take the $10K+ this year. I have even accepted that I would rather be penalized in the future. What is worth the most to me is AUTONOMY."
In reviewing all of the feedback we’ve received, this idea seems to come up again and again. Physicians are willing to accept the time-consuming idiosyncrasies of electronic health records but are offended by the idea of technologic or governmental intrusion into the physician-patient relationship. We will continue to explore this idea in the coming months as we share more reader comments and response to the column.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a company that creates mobile apps. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
How do you really feel about your EHR?
Every month we try to write about something that is both timely and relevant, but in general we choose topics that interest us. In response to our columns, we are typically greeted with e-mailed comments – both negative and positive – that highlight issues we haven’t covered or challenge the opinions we’ve expressed about health IT. We greatly enjoy the response from readers and welcome the criticism. In fact, we want to encourage it.
Over the next few columns, we hope to publish some of our readers’ comments and respond to them. If you have e-mailed us in the past, we may be contacting you to request your permission to publish your thoughts. If you have not yet sent us any correspondence, we would encourage you to do so over the next few weeks. Reach us at info@ehrpc.com and be sure to indicate whether or not you give permission to publish your words.
Historically, most of the correspondence we have received has been negative toward electronic health records. We anticipate this trend will continue as we move forward, and we are okay with that. There is no question that the national dialogue is presently quite critical of EHRs, frequently highlighting physician frustration with current electronic health record systems.
In fact, a recent survey conducted by the American College of Physicians and AmericanEHR Partners found that physician satisfaction with EHRs across multiple specialties dropped 12% from 2010 to 2012 (data presented at the 2013 Healthcare Information and Management Systems Society [HIMSS] annual meeting. Furthermore, 39% of respondents stated that they would not recommend their current EHR to a colleague. But what would cause such a negative downturn?
Ironically, many feel the reason for this, in large part, is the Meaningful Use program. The very same program designed to incentivize physicians to invest in technology has become the source of their growing dissatisfaction with it. Essentially, this government-sponsored program has forced the process of EHR adoption to move very quickly. Physicians who would have never before considered themselves "early adopters" have been encouraged to purchase an electronic record while the technology is still – in many ways – in its infancy. They have been motivated not only by the promise of financial gain, but also by the fear of looming penalties if they fail to comply.
This phenomenon is fairly novel and completely atypical of technology adoption. Traditionally, when any new innovation is brought to market, it is immediately embraced by a select few who always want to be on the bleeding edge (admittedly, the two of us are self-proclaimed geeks and often count ourselves among this group). Most people, however, have little interest and might not even take notice until that which once was innovative becomes "old hat."
The Facebook phenomenon is a prime example of this. The success of the social networking giant truly exploded once it moved from an online "college hangout" to a tool that "everyone and their grandmother" (literally) began relying on for essential communication. This was a completely organic process, not one artificially cultivated by government involvement. In other words, people began using Facebook not because they had to but because they wanted to. It simply provided a better way of communicating and managing information in the social domain.
Interestingly enough, EHRs promise to bring the same utility to the field of medicine. They are intended to enhance communication among physicians and streamline care by improving data management and clinical decision support. This is possible and even obtainable today in certain circumstances, but there is a great deal of inconsistency in quality among the various products available and the market has not had time to weed out those that are failing to deliver on their promises. In many ways, even we would agree that artificial influences have encouraged the market to move too fast, and we can sympathize with those who have found reason to question the value of many current EHR offerings.
Thankfully, there are many influential voices who have recently spoken out about the speed at which the world of health IT is moving. Most notably, Dr. James L. Madara, CEO and executive vice president of the American Medical Association, filed formal comments with the Centers for Medicare and Medicaid Services earlier this year encouraging them to "slow down" development of Meaningful Use stage 3. In the letter, Dr. Madara stated "It makes no sense to add stages and requirements to a program when even savvy EHR users and specialists are having difficulty meeting the Stage 1 measures."
It seems that the CMS agrees with this, as acting administrator Marilyn Tavenner announced in March that there will be a hiatus prior to further rulemaking to examine the program’s impact so far and solicit comments from clinicians.
With that in mind, here is your opportunity to bring your thoughts and criticisms to a public forum. As stated above, we look forward to receiving any perspective or status updates you might wish to offer and will review and publish these over the next few months. We hope that this will prove to be constructive, informative, and useful, and will reflect where our fellow clinicians stand on issues from meaningful (or unmeaningful) use to optimization strategies and techniques.
We are convinced that the true success of EHR adoption will take time and only come through the collective wisdom and feedback of clinicians, but we remain confident that eventually it will offer a path to improved patient care. Whether you agree or not, here’s your chance to let us know.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a software company that creates medical handheld references. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
Every month we try to write about something that is both timely and relevant, but in general we choose topics that interest us. In response to our columns, we are typically greeted with e-mailed comments – both negative and positive – that highlight issues we haven’t covered or challenge the opinions we’ve expressed about health IT. We greatly enjoy the response from readers and welcome the criticism. In fact, we want to encourage it.
Over the next few columns, we hope to publish some of our readers’ comments and respond to them. If you have e-mailed us in the past, we may be contacting you to request your permission to publish your thoughts. If you have not yet sent us any correspondence, we would encourage you to do so over the next few weeks. Reach us at info@ehrpc.com and be sure to indicate whether or not you give permission to publish your words.
Historically, most of the correspondence we have received has been negative toward electronic health records. We anticipate this trend will continue as we move forward, and we are okay with that. There is no question that the national dialogue is presently quite critical of EHRs, frequently highlighting physician frustration with current electronic health record systems.
In fact, a recent survey conducted by the American College of Physicians and AmericanEHR Partners found that physician satisfaction with EHRs across multiple specialties dropped 12% from 2010 to 2012 (data presented at the 2013 Healthcare Information and Management Systems Society [HIMSS] annual meeting. Furthermore, 39% of respondents stated that they would not recommend their current EHR to a colleague. But what would cause such a negative downturn?
Ironically, many feel the reason for this, in large part, is the Meaningful Use program. The very same program designed to incentivize physicians to invest in technology has become the source of their growing dissatisfaction with it. Essentially, this government-sponsored program has forced the process of EHR adoption to move very quickly. Physicians who would have never before considered themselves "early adopters" have been encouraged to purchase an electronic record while the technology is still – in many ways – in its infancy. They have been motivated not only by the promise of financial gain, but also by the fear of looming penalties if they fail to comply.
This phenomenon is fairly novel and completely atypical of technology adoption. Traditionally, when any new innovation is brought to market, it is immediately embraced by a select few who always want to be on the bleeding edge (admittedly, the two of us are self-proclaimed geeks and often count ourselves among this group). Most people, however, have little interest and might not even take notice until that which once was innovative becomes "old hat."
The Facebook phenomenon is a prime example of this. The success of the social networking giant truly exploded once it moved from an online "college hangout" to a tool that "everyone and their grandmother" (literally) began relying on for essential communication. This was a completely organic process, not one artificially cultivated by government involvement. In other words, people began using Facebook not because they had to but because they wanted to. It simply provided a better way of communicating and managing information in the social domain.
Interestingly enough, EHRs promise to bring the same utility to the field of medicine. They are intended to enhance communication among physicians and streamline care by improving data management and clinical decision support. This is possible and even obtainable today in certain circumstances, but there is a great deal of inconsistency in quality among the various products available and the market has not had time to weed out those that are failing to deliver on their promises. In many ways, even we would agree that artificial influences have encouraged the market to move too fast, and we can sympathize with those who have found reason to question the value of many current EHR offerings.
Thankfully, there are many influential voices who have recently spoken out about the speed at which the world of health IT is moving. Most notably, Dr. James L. Madara, CEO and executive vice president of the American Medical Association, filed formal comments with the Centers for Medicare and Medicaid Services earlier this year encouraging them to "slow down" development of Meaningful Use stage 3. In the letter, Dr. Madara stated "It makes no sense to add stages and requirements to a program when even savvy EHR users and specialists are having difficulty meeting the Stage 1 measures."
It seems that the CMS agrees with this, as acting administrator Marilyn Tavenner announced in March that there will be a hiatus prior to further rulemaking to examine the program’s impact so far and solicit comments from clinicians.
With that in mind, here is your opportunity to bring your thoughts and criticisms to a public forum. As stated above, we look forward to receiving any perspective or status updates you might wish to offer and will review and publish these over the next few months. We hope that this will prove to be constructive, informative, and useful, and will reflect where our fellow clinicians stand on issues from meaningful (or unmeaningful) use to optimization strategies and techniques.
We are convinced that the true success of EHR adoption will take time and only come through the collective wisdom and feedback of clinicians, but we remain confident that eventually it will offer a path to improved patient care. Whether you agree or not, here’s your chance to let us know.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a software company that creates medical handheld references. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.
Every month we try to write about something that is both timely and relevant, but in general we choose topics that interest us. In response to our columns, we are typically greeted with e-mailed comments – both negative and positive – that highlight issues we haven’t covered or challenge the opinions we’ve expressed about health IT. We greatly enjoy the response from readers and welcome the criticism. In fact, we want to encourage it.
Over the next few columns, we hope to publish some of our readers’ comments and respond to them. If you have e-mailed us in the past, we may be contacting you to request your permission to publish your thoughts. If you have not yet sent us any correspondence, we would encourage you to do so over the next few weeks. Reach us at info@ehrpc.com and be sure to indicate whether or not you give permission to publish your words.
Historically, most of the correspondence we have received has been negative toward electronic health records. We anticipate this trend will continue as we move forward, and we are okay with that. There is no question that the national dialogue is presently quite critical of EHRs, frequently highlighting physician frustration with current electronic health record systems.
In fact, a recent survey conducted by the American College of Physicians and AmericanEHR Partners found that physician satisfaction with EHRs across multiple specialties dropped 12% from 2010 to 2012 (data presented at the 2013 Healthcare Information and Management Systems Society [HIMSS] annual meeting. Furthermore, 39% of respondents stated that they would not recommend their current EHR to a colleague. But what would cause such a negative downturn?
Ironically, many feel the reason for this, in large part, is the Meaningful Use program. The very same program designed to incentivize physicians to invest in technology has become the source of their growing dissatisfaction with it. Essentially, this government-sponsored program has forced the process of EHR adoption to move very quickly. Physicians who would have never before considered themselves "early adopters" have been encouraged to purchase an electronic record while the technology is still – in many ways – in its infancy. They have been motivated not only by the promise of financial gain, but also by the fear of looming penalties if they fail to comply.
This phenomenon is fairly novel and completely atypical of technology adoption. Traditionally, when any new innovation is brought to market, it is immediately embraced by a select few who always want to be on the bleeding edge (admittedly, the two of us are self-proclaimed geeks and often count ourselves among this group). Most people, however, have little interest and might not even take notice until that which once was innovative becomes "old hat."
The Facebook phenomenon is a prime example of this. The success of the social networking giant truly exploded once it moved from an online "college hangout" to a tool that "everyone and their grandmother" (literally) began relying on for essential communication. This was a completely organic process, not one artificially cultivated by government involvement. In other words, people began using Facebook not because they had to but because they wanted to. It simply provided a better way of communicating and managing information in the social domain.
Interestingly enough, EHRs promise to bring the same utility to the field of medicine. They are intended to enhance communication among physicians and streamline care by improving data management and clinical decision support. This is possible and even obtainable today in certain circumstances, but there is a great deal of inconsistency in quality among the various products available and the market has not had time to weed out those that are failing to deliver on their promises. In many ways, even we would agree that artificial influences have encouraged the market to move too fast, and we can sympathize with those who have found reason to question the value of many current EHR offerings.
Thankfully, there are many influential voices who have recently spoken out about the speed at which the world of health IT is moving. Most notably, Dr. James L. Madara, CEO and executive vice president of the American Medical Association, filed formal comments with the Centers for Medicare and Medicaid Services earlier this year encouraging them to "slow down" development of Meaningful Use stage 3. In the letter, Dr. Madara stated "It makes no sense to add stages and requirements to a program when even savvy EHR users and specialists are having difficulty meeting the Stage 1 measures."
It seems that the CMS agrees with this, as acting administrator Marilyn Tavenner announced in March that there will be a hiatus prior to further rulemaking to examine the program’s impact so far and solicit comments from clinicians.
With that in mind, here is your opportunity to bring your thoughts and criticisms to a public forum. As stated above, we look forward to receiving any perspective or status updates you might wish to offer and will review and publish these over the next few months. We hope that this will prove to be constructive, informative, and useful, and will reflect where our fellow clinicians stand on issues from meaningful (or unmeaningful) use to optimization strategies and techniques.
We are convinced that the true success of EHR adoption will take time and only come through the collective wisdom and feedback of clinicians, but we remain confident that eventually it will offer a path to improved patient care. Whether you agree or not, here’s your chance to let us know.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference, a software company that creates medical handheld references. Dr. Notte practices family medicine and health care informatics at Abington Memorial. They are partners in EHR Practice Consultants. Contact them at info@ehrpc.com.















