User login
Advanced team-based care: How we made it work
Leaders in health care and practicing physicians recognize the need for changes in how health care is delivered.1-3 Despite this awareness, though, barriers to meaningful change persist and the current practice environment wherein physicians must routinely spend 2 hours on electronic health records (EHRs) and desk work for every hour of direct face time with patients4 is driving trainees away from ambulatory specialties and is contributing to physicians’ decisions to reduce their practices to part-time, retire early, or leave medicine altogether.5,6 Those who persevere in this environment with heavy administrative burdens run the increasing risk of burnout.7
Some physicians and practices are responding by taking creative measures to reform the way patient care is delivered. Bellin Health—a 160-provider, multispecialty health system in northeast Wisconsin where one of the authors (JJ) works—introduced an advanced team-based care (aTBC) model between November 2014 and November 2018, starting with our primary care providers. The development and introduction of this new model arose from an iterative, multidisciplinary process driven by the desire to transform the Triple Aim—enhancing patient experience, improving population health, and reducing costs—into a Quadruple Aim8 by additionally focusing on improving the work life of health care providers, which, in turn, will help achieve the first 3 goals. In introducing an aTBC model, Bellin Health focused on 3 elements: office visit redesign, in-basket management redesign, and the use of extended care team members and system and community resources to assist in the care of complex and high-risk patients.
Herein we describe the 3 components of our aTBC model,1,9 identify the barriers that existed in the minds of multiple stakeholders (from patients to clinicians and Bellin executives), and describe the strategies that enabled us to overcome these barriers.
The impetus behind our move to aTBC
Bellin Health considered a move to an aTBC model to be critical in light of factors in the health care environment, in general, and at Bellin, in particular. The factors included
- an industry-wide shift to value-based payments, which requires new models for long-term financial viability.
- recognition that physician and medical staff burnout leads to lower productivity and, in some cases, workforce losses.5,6 Replacing a physician in a practice can be difficult and expensive, with cost estimates of $500,000 to more than $1 million per physician.10,11
- a belief that aTBC could help the Bellin Health leadership team meet its organizational goals of improved patient satisfaction, achieve gains in quality measures, enhance engagement and loyalty among patients and employees, and lower recruitment costs.
A 3-part aTBC initiative
■ Part 1: Redesign the office visit
We redesigned staffing and workflow for office visits to maximize the core skills of physicians, which required distributing ancillary tasks among support staff. We up-trained certified medical assistants (CMAs) and licensed practical nurses (LPNs) to take on the new role of care team coordinator (CTC) and optimized the direct clinical support ratio for busier physicians. For physicians who were seeing 15 to 19 patients a day, a ratio of 3 CTCs to 2 physicians was implemented; for those seeing 20 or more patients a day, we used a support ratio of 2:1.
The role of CTC was designed so that he or she would accompany a patient throughout the entire appointment. Responsibilities were broken out as follows:
Pre-visit. Before the physician enters the room, the CTC would now perform expanded rooming functions including pending orders, refill management, care gap closure using standing orders, agenda setting, and preliminary documentation.12
Visit. The CTC would now hand off the patient to the physician and stay in the room to document details of the visit and record new orders for consults, x-ray films, referrals, or prescriptions.13 This intensive EHR support was established to ensure that the physician could focus directly on the patient without the distraction of the computer.
Continue to: Post-visit
Post-visit. After a physician leaves a room, the CTC was now charged with finishing the pending orders, setting up the patient’s next appointment and pre-visit labs, reviewing details of the after-visit summary, and doing any basic health coaching with the patient. During this time, the physician would use the co-location space to review and edit the documentation, cosign the orders and prescriptions submitted by the CTC, and close the chart before going into the next room with the second CTC. The need to revisit these details after clinic hours was eliminated.
Another change … The role of our phone triage registered nurses (RN) was expanded. Care team RNs began providing diabetes counseling, blood pressure checks, annual wellness visits (AWV), and follow-up through the Centers for Medicare and Medicaid Services (CMS)'s Chronic Care Management and Transitional Care Management programs.
■ Part 2: Redesign between-visit in-basket management
Responding to an increasing number of inbox messages had become overwhelming for our physicians. Bellin Health’s management was aware that strategic delegation of inbox messages could save an hour or more of a physician’s time each day.14 Bellin implemented a procedure whereby inbox test results would be handled by the same CTC who saw the patient, thereby extending continuity. If the results were normal, the CTC would contact the patient. If the results were abnormal, the physician and the CTC would discuss them and develop a plan. Co-location of the RN, the CTC, and the physician would leverage face-to-face communication and make in-basket management more efficient.
■ Part 3: Redesign population health management
We developed an Extended Care Team (ECT), including social workers, clinical pharmacists, RN care coordinators, and diabetes educators, to assist with the care of patients with high-risk disorders or otherwise complex issues. These team members would work closely with the CTC, care team RN, and physician to review patients, develop plans of care, optimize management, and improve outcomes. Patients would be identified as candidates for potential ECT involvement based on the physician’s judgment in consultation with an EHR-based risk score for hospitalization or emergency department visit.
As we developed new processes, such as screening for determinants of health, we engaged additional system and community resources to help meet the needs of our patients.
Continue to: A look at stakeholder concerns and overcoming the barriers
A look at stakeholder concerns and overcoming the barriers
Critical to our success was being attentive to the concerns of our stakeholders and addressing them. Along the way, we gained valuable implementation insights, which we share here along with some specifics about how, exactly, we did things at Bellin.
Patients
Some patients expressed hesitation at having a person other than their physician in the exam room. They worried that the intimacy and privacy with their physician would be lost. In light of this, we gave patients the option not to have the CTC remain in the room. However, patients quickly saw the value of this team-based care approach and seldom asked to be seen without the CTC.
Throughout the process, we surveyed patients for feedback on their experiences. Comments indicated that the presence of the CTC in our team-based model led to positive patient experiences:
My physician is fully attentive. Patients appreciated that physicians were not distracted by the computer in the exam room. “I feel like I’ve got my doctor back” has been a common refrain.
The office staff is more responsive. The CTC, having been present during the appointment, has a deeper understanding of the care plan and can respond to calls or emails between visits, thereby reducing the time patients must wait for answers. One patient commented that, “I love [the doctor’s] team; his nurses are willing to answer every question I have.”
Continue to: I increasingly feel that I'm understood
I increasingly feel that I’m understood. We have seen patients develop meaningful relationships with other team members, confiding in them in ways that they hadn’t always done with physicians and advanced practice clinicians (APCs). Team members, in turn, have added valuable insights that help optimize patients’ care. In particular, the care of patients with multiple needs has been enhanced with the addition of ECT members who work with the core team and use their expertise to optimize the care of these patients.
Certified medical assistants and licensed practical nurses
Bellin’s leadership knew that team documentation could cause stress for the CMA, who, acting as a CTC, wanted to avoid misrepresenting details of the clinical encounter.13 Adding to the stress were other duties that would need to be learned, including agenda setting, refill management, care gap closure, and health coaching. With thorough training and preparation, many—but not all—of our CMAs and LPNs were able to successfully make the transition and flourish.
Implementation strategies
Provide thorough training. Our training process started 8 weeks before it was time to “go live.” There were weekly hour-long training sessions in population health basics, team culture and change management, documentation basics, and new roles and responsibilities. In the final week, the entire aTBC team sat together for 3 days of EHR training. All new teams shadowed existing teams to get a clear picture of the new processes.
Create a community of support. As our CMAs adapted to their new CTC roles, it was critical that they had support from experienced CTCs. Encouragement and patience from physicians were—and are—essential for CTCs to develop confidence in their new roles.
Enable ongoing feedback. We introduced weekly team meetings to enhance team communication and dynamics. Forums for all roles are held periodically to facilitate discussion, share learning, and enable support between teams.
Continue to: Use EHR tools to facilitate this work
Use EHR tools to facilitate this work. Using standard templates and documentation tools helped CTCs develop the confidence needed to thrive in their new role. Knowing these tools were available helped CTCs become effective in helping the team manage the between-visit work.
Monitor workload. As we developed more workflows and processes, we took care to monitor the amount of additional work for those in this role. We offloaded work whenever possible. For example, coordinated refill management at time of service, coupled with a back-up centralized refill system, can significantly decrease the number of refill requests made to CTCs. We continue to adjust staffing, where appropriate, to provide adequate support for those in this valuable role.
Be prepared for turnover. As CTCs became empowered in their new roles, some decided to advance their training into other roles. We developed a plan for replacing and training new staff. Higher pay can also be used to help attract and retain these staff members. Bellin uses LPNs in this role to ensure adequate staffing. Other health systems have developed a tier system for CMAs to improve retention.
Registered nurses
Before our move to an aTBC model, our office RNs primarily managed phone triage. Now the nurses were enlisted to play a more active role in patient care and team leadership. Although it was a dramatic departure from prior responsibilities, the majority of Bellin’s RNs have found increased satisfaction in taking on direct patient care.
Implementation strategies
Define new roles and provide training. In addition to participating in acute patient visits, consider ways that care team RNs can expand responsibilities as they pertain to disease counseling, population health management, and team leadership.15 At Bellin, the expanded role of the RN is evident in diabetes education and Medicare AWVs. Specifically, RNs now provide diabetes education to appropriate patients following a warm handoff from the physician at the time of the visit. RNs now also complete Medicare AWVs, which frees up physicians for other tasks and helps ensure sustainability for the new RN roles. Rates of completed AWVs at Bellin are now more than 70%, compared with reported national rates of less than 30%.16
Continue to: Maximize co-location
Maximize co-location. It is helpful to have the team members whose work is closely related—such as the CTCs and the RN for the team—to be situated near each other, rather than down a hall or in separate offices. Since the RN is co-located with the core teams at Bellin, there is now greater opportunity for verbal interaction, rather than just electronic communications, for matters such as triage calls and results management. RNs also provide a valuable resource for CMAs and LPNs, as well as help oversee team management of the in-basket.
Evaluate sustainability. Additional roles for the RNs required additional RN staffing. We assessed the new workload duties and balanced that against potential revenue from RN visits. This analysis indicated that an optimal ratio was 1 RN to every 3000 patients. This would allow an adequate number of RNs to fulfill additional roles and was financially sustainable with the goal of 4 billable RN visits per day.
Physicians
Bellin’s leadership recognized that some physicians might perceive team-based care as eroding their primary responsibility for patients’ care. Physicians have historically been trained in a model based on the primacy of the individual physician and that can be a hurdle to embracing team culture as a new paradigm of care. Several strategies helped us and can help others, too.
Implementation strategies
Cultivate trust. Thorough training of CTCs and RNs is critical to helping physicians develop trust and reliance in the team. The physician retains final authority over the team for cosigning orders, editing and finalizing documentation, and overseeing results management. Physicians invested in training and educating their staff will reap the rewards of a highly functioning, more satisfied team.
Encourage leadership. This can be a cultural shift for physicians, yet it is critical that they take a leadership role in this transformation.17 Physicians and their team leaders attended training sessions in team culture and change management. Prior to the go-live date, team leaders also met with the physician individually to explore their concerns and discuss ways to effectively lead and support their teams.
Continue to: Urge acceptance of support
Urge acceptance of support. The complexity of patient care today makes it difficult for a physician to manage all of a patient’s needs single-handedly. Complexity arises from the variety of plan co-pays and deductibles, the number of patients with chronic diseases, and the increased emphasis on improving quality measures.18 Enhanced support during any office visit and the extra support of an ECT for complex patients improves the ability of the physician to more effectively meet the needs of the patient.
Emphasize the benefit of an empowered team. The demands of the EHR on physicians and the resultant frustrations are well chronicled.4,19-22 Strategically delegating much of this work to other team members allows the physician to focus on the patient and perform physician-level work. At Bellin, we observed that our most successful care teams were those in which the physician fully accepted team-based care principles and empowered the staff to work at the top of their skill set.
Advanced practice clinicians
APCs in our system had traditionally practiced in 1 of 3 ways: independently handling defined panels with physician supervision; handling overflow or acute visits; or working collaboratively with a supervising physician to share a larger “team panel.” The third approach has become our preferred model. aTBC provides opportunities for APCs to thrive and collaborate with the physician to provide excellent care for patients.
APCs underwent the same process changes as physicians, including appropriate CTC support. Implementation strategies for APCs were similar to those that were useful for physicians.
Risk management professionals
At Bellin, we found that risk-management professionals had concerns about the scope of practice assigned to various team members, particularly regarding documentation. CMS allows for elements of a patient visit to be documented by CMAs and other members of the care team in real time as authorized by the physician.23,24 CTCs at Bellin also have other clinical duties in patient and EHR management. aTBC practices generally prefer the term team documentation over scribing, since it more accurately reflects the scope of the CTC’s work.
Continue to: Implementation strategies
Implementation strategies
Clarify regulatory issues. Extensive use of standing orders and protocols allowed us to increase involvement of various team members. State laws vary in what functions CMAs and LPNs are allowed to perform, so it is important to check your state guidelines.25 There is a tendency for some risk managers to overinterpret regulations. Challenge them to provide exact documentation from regulatory agencies to support their decisions.
Give assurances of physician oversight and processes. The physician assumes responsibility for standing orders, protocols, and documentation. We made sure that we had clear and consistent processes in place and worked closely with our risk managers as we developed our model. aTBC provides checks and balances to ensure accurate records, since team members are able to contribute and check for accuracy. A recent study suggested that CMAs perform documentation that is of equal or higher quality than that performed by the physician.26
Financial leadership
Like any organization adopting aTBC, Bellin’s leadership was concerned about the expense of adopting this approach. However, the leadership also recognized that the transition to aTBC could increase revenue by more than the increased staffing costs. In addition, we expected that capacity, access, continuity, and financial margins would increase.2,3,27,28 We also anticipated a decrease in downstream services, such as unnecessary tests, emergency department visits, and hospitalizations—a benefit of accountable care payment models.
Our efforts have been successful from a financial point of view. We attribute the financial sustainability that we have experienced to 4 factors:
1. Increased productivity. We knew that the increased efficiency of team-based care enables physicians to see 1 to 2 more patients per half day, and sometimes more.3,28,29 An increase of at least 1 patient visit per half-day was expected of our physicians and APCs on aTBC. In addition, they were expected to support the care team RN in achieving at least 4 billable visits per day. Our current level of RN visits is at 3.5 per nurse per day. There is significant variability in the increase of patients seen by a physician per day, ranging from 1 to 4 additional patients. These increased visits have helped us achieve financial viability, even in a predominantly fee-for-service environment.
2. More thorough service. The ability to keep patients in primary care and to focus on the patient’s full range of needs has led to higher levels of service and, consequently, to appropriately higher levels of billing codes. For example, Bellin’s revenue from billing increased by $724 per patient, related (in part) to higher rates of immunizations, cancer screenings with mammography, and colonoscopies.
Continue to: 3. New billable services
3. New billable services. Billing for RN blood pressure checks, AWVs, and extended care team services have helped make aTBC at Bellin financially feasible. Revenue from RN visits, for example, was $630,000 in 2018.
4. Improved access for patients. Of the 130 primary care providers now on aTBC, 15 (11.5%) had closed their practices to new patients before aTBC. Now, all of their practices are open to new patients, which has improved access to care. In a 2018 patient access survey, 96.6% of patients obtained an appointment as soon as they thought it was needed, compared with 70.7% of patients before the transition to aTBC.
Greater opportunity for financial sustainability. The combination of improved quality measures and decreased cost of care in the Bellin aTBC bodes well for future success in a value-based world. We have realized a significant increase in value-based payments for improved quality, and in our Next Gen Accountable Care Organization (ACO) patients, we have seen a decrease of $29 in per-member-per-month costs, likely due to the use of nonphysicians in expanded roles. In addition, hospital admissions have decreased by 5% due to the ability of ambulatory teams to manage more complex patients in the office setting. This model has also allowed physicians and APCs to increase their panel size, another key value-based metric. From 2016 to 2018, panel size for primary care providers increased by an average of 8%.
Enhanced ability to retain and recruit. Several of Bellin’s primary care recruits indicated that they had interviewed only at practices incorporating team-based care. This trend may increase as residencies transition to team-based models of care.
So how did we do?
Metrics of Bellin’s aTBC success
By the end of 2018, all 130 primary care physicians and APCs at Bellin had made the transition to this model, representing family medicine, internal medicine, and pediatrics. We have now begun the transition of our non-primary care specialties to team-based care.
Continue to: In the aTBC model...
In the aTBC model, the percentage of patients receiving age-appropriate screening is higher than before in every domain we measure (FIGURE 1). There has also been improvement in major quality metrics (FIGURE 2).
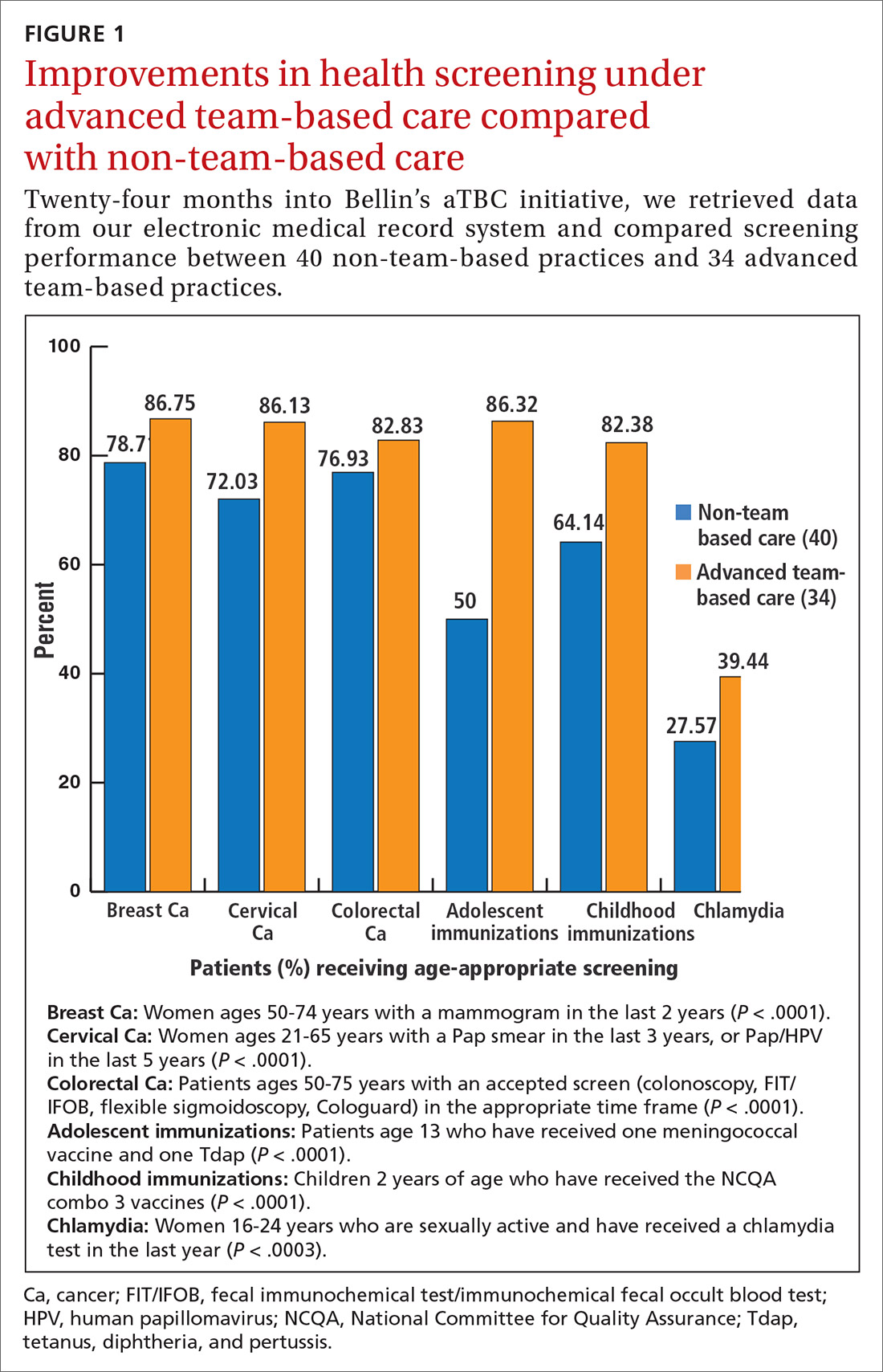
In a survey done in Spring 2018 by St. Norbert College Strategic Research Center, provider satisfaction increased, with 83% of physicians having made the transition to an aTBC practice moderately or very satisfied with their Bellin Health experience, compared with 70% in the traditional model. More recent 2019 survey data show a satisfaction rate of 90% for team-based care providers. Finally, in our aTBC model—in CMS’s Next-Gen ACO initiative—the cost per patient per month is significantly less than for those in a non-team-based care model ($796 vs $940).

CORRESPONDENCE
James Jerzak, MD, 1630 Commanche Ave, Green Bay, WI 54313; james.jerzak@bellin.org.
ACKNOWLEDGEMENTS
The authors would like to thank Lindsey E. Carlasare, MBA, from the American Medical Association, and Brad Wozney, MD, Kathy Kerscher, and Christopher Elfner from Bellin Health, for their contributions to the content and review of this manuscript.
1. Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
2. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
3. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
4. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
5. Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422-431.
6. Sinsky CA, Dyrbye LN, West CP, et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc. 2017;92:1625-1635.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
8. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
9. Sinsky CA, Sinsky TA, Althaus D, et al. Practice profile. ‘Core teams’: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Aff (Millwood). 2010;29:966-968.
10. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
11. Association for Advancing Physician and Provider Recruitment. Schutte L. What you don’t know can cost you: building a business case for recruitment and retention best practices. 2012. https://member.aappr.org/general/custom.asp?page=696. Accessed June 20, 2019.
12. American Medical Association. AMA STEPS Forward. Expanded rooming and discharge protocols. https://edhub.ama-assn.org/steps-forward/module/2702600. Accessed June 20, 2019.
13. American Medical Association. AMA STEPS Forward. Team documentation. https://edhub.ama-assn.org/steps-forward/module/2702598?resultClick=3&bypassSolrId=J_2702598. Accessed June 20, 2019.
14. American Medical Association. AMA STEPS Forward. EHR in-basket restructuring for improved efficiency. https://edhub.ama-assn.org/steps-forward/module/2702694?resultClick=3&bypassSolrId=J_2702694. Accessed June 20, 2019.
15. California Health Care Foundation. Bodenheimer T, Bauer L, Olayiwola JN. RN role reimagined: how empowering registered nurses can improve primary care. https://www.chcf.org/publication/rn-role-reimagined-how-empowering-registered-nurses-can-improve-primary-care/. Accessed June 20, 2019.
16. Chung S, Lesser LI, Lauderdale DS, et al. Medicare annual preventive care visits: use increased among fee-for-service patients, but many do not participate. Health Aff (Millwood). 2015;34:11-20.
17. American Medical Association. AMA Policy H-160.912. The structure and function of interprofessional health care teams. https://policysearch.ama-assn.org/policyfinder/detail/The%20Structure%20and%20Function%20of%20Interprofessional%20Health%20Care%20Teams?uri=%2FAMADoc%2FHOD.xml-0-727.xml. Accessed June 20, 2019.
18. Milani RV, Lavie CJ. Health care 2020: reengineering health care delivery to combat chronic disease. Am J Med. 2015;128:337-343.
19. Hill RG Jr, Sears LM, Melanson SW. 4000 clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med. 2013;31:1591-1594.
20. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21:e100-e106.
21. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
22. RAND Corporation. Friedberg MW, Chen PG, Ban Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. https://www.rand.org/pubs/research_reports/RR439.html. Accessed June 20, 2019.
23. Evaluation and Management (E/M) visit frequently asked questions (FAQs): physician fee schedule (PPS). https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/E-M-Visit-FAQs-PFS.pdf. Accessed August 27, 2019.
24. Centers for Medicare & Medicaid Services. Scribe services signature requirements. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2017-Transmittals-Items/R713PI.html. Accessed June 20, 2019.
25. American Association of Medical Assistants. State scope of practice laws. http://www.aama-ntl.org/employers/state-scope-of-practice-laws. Accessed June 20, 2019.
26. Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65:155-159.
27. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
28. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406.
29. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
Leaders in health care and practicing physicians recognize the need for changes in how health care is delivered.1-3 Despite this awareness, though, barriers to meaningful change persist and the current practice environment wherein physicians must routinely spend 2 hours on electronic health records (EHRs) and desk work for every hour of direct face time with patients4 is driving trainees away from ambulatory specialties and is contributing to physicians’ decisions to reduce their practices to part-time, retire early, or leave medicine altogether.5,6 Those who persevere in this environment with heavy administrative burdens run the increasing risk of burnout.7
Some physicians and practices are responding by taking creative measures to reform the way patient care is delivered. Bellin Health—a 160-provider, multispecialty health system in northeast Wisconsin where one of the authors (JJ) works—introduced an advanced team-based care (aTBC) model between November 2014 and November 2018, starting with our primary care providers. The development and introduction of this new model arose from an iterative, multidisciplinary process driven by the desire to transform the Triple Aim—enhancing patient experience, improving population health, and reducing costs—into a Quadruple Aim8 by additionally focusing on improving the work life of health care providers, which, in turn, will help achieve the first 3 goals. In introducing an aTBC model, Bellin Health focused on 3 elements: office visit redesign, in-basket management redesign, and the use of extended care team members and system and community resources to assist in the care of complex and high-risk patients.
Herein we describe the 3 components of our aTBC model,1,9 identify the barriers that existed in the minds of multiple stakeholders (from patients to clinicians and Bellin executives), and describe the strategies that enabled us to overcome these barriers.
The impetus behind our move to aTBC
Bellin Health considered a move to an aTBC model to be critical in light of factors in the health care environment, in general, and at Bellin, in particular. The factors included
- an industry-wide shift to value-based payments, which requires new models for long-term financial viability.
- recognition that physician and medical staff burnout leads to lower productivity and, in some cases, workforce losses.5,6 Replacing a physician in a practice can be difficult and expensive, with cost estimates of $500,000 to more than $1 million per physician.10,11
- a belief that aTBC could help the Bellin Health leadership team meet its organizational goals of improved patient satisfaction, achieve gains in quality measures, enhance engagement and loyalty among patients and employees, and lower recruitment costs.
A 3-part aTBC initiative
■ Part 1: Redesign the office visit
We redesigned staffing and workflow for office visits to maximize the core skills of physicians, which required distributing ancillary tasks among support staff. We up-trained certified medical assistants (CMAs) and licensed practical nurses (LPNs) to take on the new role of care team coordinator (CTC) and optimized the direct clinical support ratio for busier physicians. For physicians who were seeing 15 to 19 patients a day, a ratio of 3 CTCs to 2 physicians was implemented; for those seeing 20 or more patients a day, we used a support ratio of 2:1.
The role of CTC was designed so that he or she would accompany a patient throughout the entire appointment. Responsibilities were broken out as follows:
Pre-visit. Before the physician enters the room, the CTC would now perform expanded rooming functions including pending orders, refill management, care gap closure using standing orders, agenda setting, and preliminary documentation.12
Visit. The CTC would now hand off the patient to the physician and stay in the room to document details of the visit and record new orders for consults, x-ray films, referrals, or prescriptions.13 This intensive EHR support was established to ensure that the physician could focus directly on the patient without the distraction of the computer.
Continue to: Post-visit
Post-visit. After a physician leaves a room, the CTC was now charged with finishing the pending orders, setting up the patient’s next appointment and pre-visit labs, reviewing details of the after-visit summary, and doing any basic health coaching with the patient. During this time, the physician would use the co-location space to review and edit the documentation, cosign the orders and prescriptions submitted by the CTC, and close the chart before going into the next room with the second CTC. The need to revisit these details after clinic hours was eliminated.
Another change … The role of our phone triage registered nurses (RN) was expanded. Care team RNs began providing diabetes counseling, blood pressure checks, annual wellness visits (AWV), and follow-up through the Centers for Medicare and Medicaid Services (CMS)'s Chronic Care Management and Transitional Care Management programs.
■ Part 2: Redesign between-visit in-basket management
Responding to an increasing number of inbox messages had become overwhelming for our physicians. Bellin Health’s management was aware that strategic delegation of inbox messages could save an hour or more of a physician’s time each day.14 Bellin implemented a procedure whereby inbox test results would be handled by the same CTC who saw the patient, thereby extending continuity. If the results were normal, the CTC would contact the patient. If the results were abnormal, the physician and the CTC would discuss them and develop a plan. Co-location of the RN, the CTC, and the physician would leverage face-to-face communication and make in-basket management more efficient.
■ Part 3: Redesign population health management
We developed an Extended Care Team (ECT), including social workers, clinical pharmacists, RN care coordinators, and diabetes educators, to assist with the care of patients with high-risk disorders or otherwise complex issues. These team members would work closely with the CTC, care team RN, and physician to review patients, develop plans of care, optimize management, and improve outcomes. Patients would be identified as candidates for potential ECT involvement based on the physician’s judgment in consultation with an EHR-based risk score for hospitalization or emergency department visit.
As we developed new processes, such as screening for determinants of health, we engaged additional system and community resources to help meet the needs of our patients.
Continue to: A look at stakeholder concerns and overcoming the barriers
A look at stakeholder concerns and overcoming the barriers
Critical to our success was being attentive to the concerns of our stakeholders and addressing them. Along the way, we gained valuable implementation insights, which we share here along with some specifics about how, exactly, we did things at Bellin.
Patients
Some patients expressed hesitation at having a person other than their physician in the exam room. They worried that the intimacy and privacy with their physician would be lost. In light of this, we gave patients the option not to have the CTC remain in the room. However, patients quickly saw the value of this team-based care approach and seldom asked to be seen without the CTC.
Throughout the process, we surveyed patients for feedback on their experiences. Comments indicated that the presence of the CTC in our team-based model led to positive patient experiences:
My physician is fully attentive. Patients appreciated that physicians were not distracted by the computer in the exam room. “I feel like I’ve got my doctor back” has been a common refrain.
The office staff is more responsive. The CTC, having been present during the appointment, has a deeper understanding of the care plan and can respond to calls or emails between visits, thereby reducing the time patients must wait for answers. One patient commented that, “I love [the doctor’s] team; his nurses are willing to answer every question I have.”
Continue to: I increasingly feel that I'm understood
I increasingly feel that I’m understood. We have seen patients develop meaningful relationships with other team members, confiding in them in ways that they hadn’t always done with physicians and advanced practice clinicians (APCs). Team members, in turn, have added valuable insights that help optimize patients’ care. In particular, the care of patients with multiple needs has been enhanced with the addition of ECT members who work with the core team and use their expertise to optimize the care of these patients.
Certified medical assistants and licensed practical nurses
Bellin’s leadership knew that team documentation could cause stress for the CMA, who, acting as a CTC, wanted to avoid misrepresenting details of the clinical encounter.13 Adding to the stress were other duties that would need to be learned, including agenda setting, refill management, care gap closure, and health coaching. With thorough training and preparation, many—but not all—of our CMAs and LPNs were able to successfully make the transition and flourish.
Implementation strategies
Provide thorough training. Our training process started 8 weeks before it was time to “go live.” There were weekly hour-long training sessions in population health basics, team culture and change management, documentation basics, and new roles and responsibilities. In the final week, the entire aTBC team sat together for 3 days of EHR training. All new teams shadowed existing teams to get a clear picture of the new processes.
Create a community of support. As our CMAs adapted to their new CTC roles, it was critical that they had support from experienced CTCs. Encouragement and patience from physicians were—and are—essential for CTCs to develop confidence in their new roles.
Enable ongoing feedback. We introduced weekly team meetings to enhance team communication and dynamics. Forums for all roles are held periodically to facilitate discussion, share learning, and enable support between teams.
Continue to: Use EHR tools to facilitate this work
Use EHR tools to facilitate this work. Using standard templates and documentation tools helped CTCs develop the confidence needed to thrive in their new role. Knowing these tools were available helped CTCs become effective in helping the team manage the between-visit work.
Monitor workload. As we developed more workflows and processes, we took care to monitor the amount of additional work for those in this role. We offloaded work whenever possible. For example, coordinated refill management at time of service, coupled with a back-up centralized refill system, can significantly decrease the number of refill requests made to CTCs. We continue to adjust staffing, where appropriate, to provide adequate support for those in this valuable role.
Be prepared for turnover. As CTCs became empowered in their new roles, some decided to advance their training into other roles. We developed a plan for replacing and training new staff. Higher pay can also be used to help attract and retain these staff members. Bellin uses LPNs in this role to ensure adequate staffing. Other health systems have developed a tier system for CMAs to improve retention.
Registered nurses
Before our move to an aTBC model, our office RNs primarily managed phone triage. Now the nurses were enlisted to play a more active role in patient care and team leadership. Although it was a dramatic departure from prior responsibilities, the majority of Bellin’s RNs have found increased satisfaction in taking on direct patient care.
Implementation strategies
Define new roles and provide training. In addition to participating in acute patient visits, consider ways that care team RNs can expand responsibilities as they pertain to disease counseling, population health management, and team leadership.15 At Bellin, the expanded role of the RN is evident in diabetes education and Medicare AWVs. Specifically, RNs now provide diabetes education to appropriate patients following a warm handoff from the physician at the time of the visit. RNs now also complete Medicare AWVs, which frees up physicians for other tasks and helps ensure sustainability for the new RN roles. Rates of completed AWVs at Bellin are now more than 70%, compared with reported national rates of less than 30%.16
Continue to: Maximize co-location
Maximize co-location. It is helpful to have the team members whose work is closely related—such as the CTCs and the RN for the team—to be situated near each other, rather than down a hall or in separate offices. Since the RN is co-located with the core teams at Bellin, there is now greater opportunity for verbal interaction, rather than just electronic communications, for matters such as triage calls and results management. RNs also provide a valuable resource for CMAs and LPNs, as well as help oversee team management of the in-basket.
Evaluate sustainability. Additional roles for the RNs required additional RN staffing. We assessed the new workload duties and balanced that against potential revenue from RN visits. This analysis indicated that an optimal ratio was 1 RN to every 3000 patients. This would allow an adequate number of RNs to fulfill additional roles and was financially sustainable with the goal of 4 billable RN visits per day.
Physicians
Bellin’s leadership recognized that some physicians might perceive team-based care as eroding their primary responsibility for patients’ care. Physicians have historically been trained in a model based on the primacy of the individual physician and that can be a hurdle to embracing team culture as a new paradigm of care. Several strategies helped us and can help others, too.
Implementation strategies
Cultivate trust. Thorough training of CTCs and RNs is critical to helping physicians develop trust and reliance in the team. The physician retains final authority over the team for cosigning orders, editing and finalizing documentation, and overseeing results management. Physicians invested in training and educating their staff will reap the rewards of a highly functioning, more satisfied team.
Encourage leadership. This can be a cultural shift for physicians, yet it is critical that they take a leadership role in this transformation.17 Physicians and their team leaders attended training sessions in team culture and change management. Prior to the go-live date, team leaders also met with the physician individually to explore their concerns and discuss ways to effectively lead and support their teams.
Continue to: Urge acceptance of support
Urge acceptance of support. The complexity of patient care today makes it difficult for a physician to manage all of a patient’s needs single-handedly. Complexity arises from the variety of plan co-pays and deductibles, the number of patients with chronic diseases, and the increased emphasis on improving quality measures.18 Enhanced support during any office visit and the extra support of an ECT for complex patients improves the ability of the physician to more effectively meet the needs of the patient.
Emphasize the benefit of an empowered team. The demands of the EHR on physicians and the resultant frustrations are well chronicled.4,19-22 Strategically delegating much of this work to other team members allows the physician to focus on the patient and perform physician-level work. At Bellin, we observed that our most successful care teams were those in which the physician fully accepted team-based care principles and empowered the staff to work at the top of their skill set.
Advanced practice clinicians
APCs in our system had traditionally practiced in 1 of 3 ways: independently handling defined panels with physician supervision; handling overflow or acute visits; or working collaboratively with a supervising physician to share a larger “team panel.” The third approach has become our preferred model. aTBC provides opportunities for APCs to thrive and collaborate with the physician to provide excellent care for patients.
APCs underwent the same process changes as physicians, including appropriate CTC support. Implementation strategies for APCs were similar to those that were useful for physicians.
Risk management professionals
At Bellin, we found that risk-management professionals had concerns about the scope of practice assigned to various team members, particularly regarding documentation. CMS allows for elements of a patient visit to be documented by CMAs and other members of the care team in real time as authorized by the physician.23,24 CTCs at Bellin also have other clinical duties in patient and EHR management. aTBC practices generally prefer the term team documentation over scribing, since it more accurately reflects the scope of the CTC’s work.
Continue to: Implementation strategies
Implementation strategies
Clarify regulatory issues. Extensive use of standing orders and protocols allowed us to increase involvement of various team members. State laws vary in what functions CMAs and LPNs are allowed to perform, so it is important to check your state guidelines.25 There is a tendency for some risk managers to overinterpret regulations. Challenge them to provide exact documentation from regulatory agencies to support their decisions.
Give assurances of physician oversight and processes. The physician assumes responsibility for standing orders, protocols, and documentation. We made sure that we had clear and consistent processes in place and worked closely with our risk managers as we developed our model. aTBC provides checks and balances to ensure accurate records, since team members are able to contribute and check for accuracy. A recent study suggested that CMAs perform documentation that is of equal or higher quality than that performed by the physician.26
Financial leadership
Like any organization adopting aTBC, Bellin’s leadership was concerned about the expense of adopting this approach. However, the leadership also recognized that the transition to aTBC could increase revenue by more than the increased staffing costs. In addition, we expected that capacity, access, continuity, and financial margins would increase.2,3,27,28 We also anticipated a decrease in downstream services, such as unnecessary tests, emergency department visits, and hospitalizations—a benefit of accountable care payment models.
Our efforts have been successful from a financial point of view. We attribute the financial sustainability that we have experienced to 4 factors:
1. Increased productivity. We knew that the increased efficiency of team-based care enables physicians to see 1 to 2 more patients per half day, and sometimes more.3,28,29 An increase of at least 1 patient visit per half-day was expected of our physicians and APCs on aTBC. In addition, they were expected to support the care team RN in achieving at least 4 billable visits per day. Our current level of RN visits is at 3.5 per nurse per day. There is significant variability in the increase of patients seen by a physician per day, ranging from 1 to 4 additional patients. These increased visits have helped us achieve financial viability, even in a predominantly fee-for-service environment.
2. More thorough service. The ability to keep patients in primary care and to focus on the patient’s full range of needs has led to higher levels of service and, consequently, to appropriately higher levels of billing codes. For example, Bellin’s revenue from billing increased by $724 per patient, related (in part) to higher rates of immunizations, cancer screenings with mammography, and colonoscopies.
Continue to: 3. New billable services
3. New billable services. Billing for RN blood pressure checks, AWVs, and extended care team services have helped make aTBC at Bellin financially feasible. Revenue from RN visits, for example, was $630,000 in 2018.
4. Improved access for patients. Of the 130 primary care providers now on aTBC, 15 (11.5%) had closed their practices to new patients before aTBC. Now, all of their practices are open to new patients, which has improved access to care. In a 2018 patient access survey, 96.6% of patients obtained an appointment as soon as they thought it was needed, compared with 70.7% of patients before the transition to aTBC.
Greater opportunity for financial sustainability. The combination of improved quality measures and decreased cost of care in the Bellin aTBC bodes well for future success in a value-based world. We have realized a significant increase in value-based payments for improved quality, and in our Next Gen Accountable Care Organization (ACO) patients, we have seen a decrease of $29 in per-member-per-month costs, likely due to the use of nonphysicians in expanded roles. In addition, hospital admissions have decreased by 5% due to the ability of ambulatory teams to manage more complex patients in the office setting. This model has also allowed physicians and APCs to increase their panel size, another key value-based metric. From 2016 to 2018, panel size for primary care providers increased by an average of 8%.
Enhanced ability to retain and recruit. Several of Bellin’s primary care recruits indicated that they had interviewed only at practices incorporating team-based care. This trend may increase as residencies transition to team-based models of care.
So how did we do?
Metrics of Bellin’s aTBC success
By the end of 2018, all 130 primary care physicians and APCs at Bellin had made the transition to this model, representing family medicine, internal medicine, and pediatrics. We have now begun the transition of our non-primary care specialties to team-based care.
Continue to: In the aTBC model...
In the aTBC model, the percentage of patients receiving age-appropriate screening is higher than before in every domain we measure (FIGURE 1). There has also been improvement in major quality metrics (FIGURE 2).
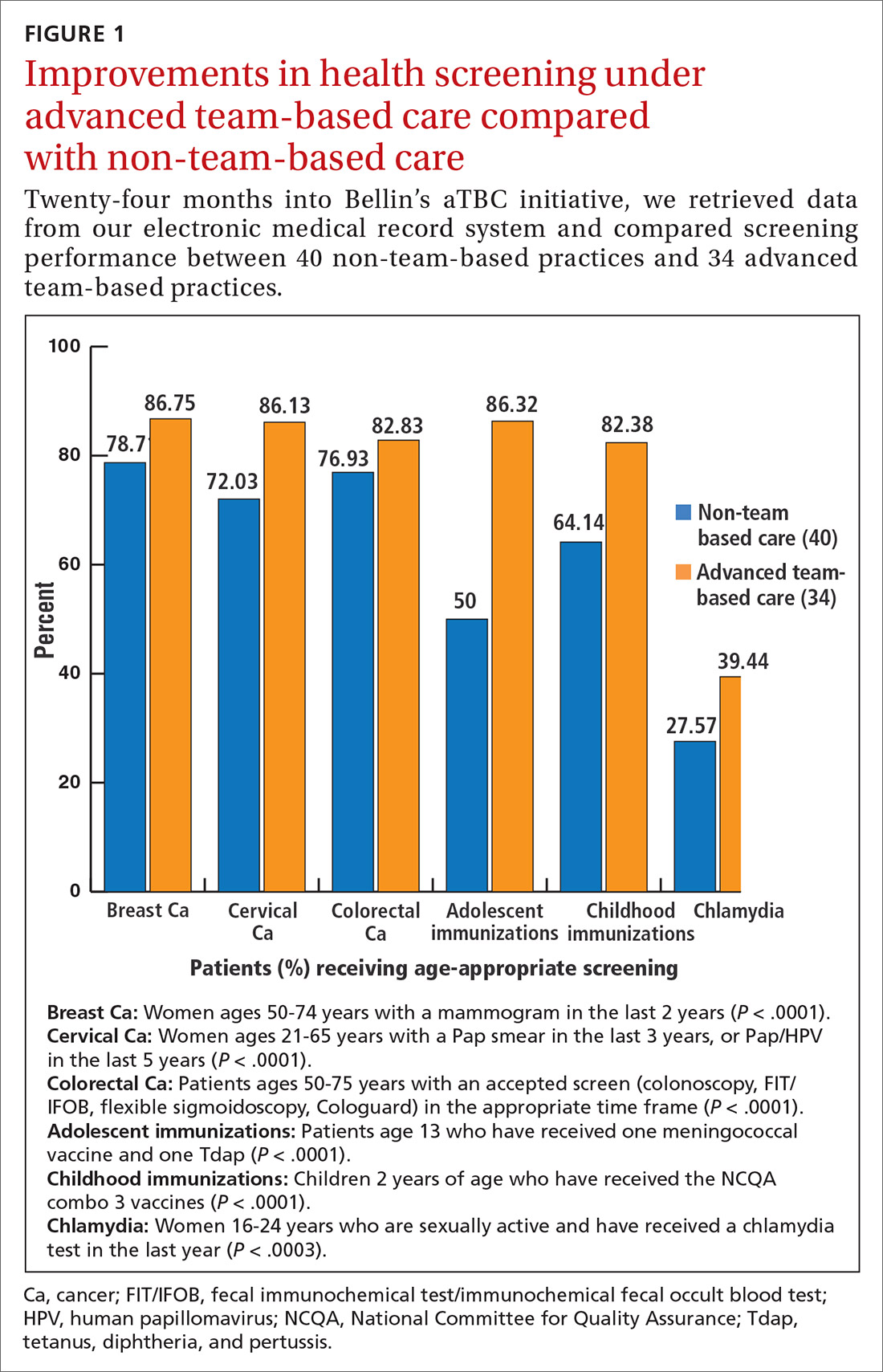
In a survey done in Spring 2018 by St. Norbert College Strategic Research Center, provider satisfaction increased, with 83% of physicians having made the transition to an aTBC practice moderately or very satisfied with their Bellin Health experience, compared with 70% in the traditional model. More recent 2019 survey data show a satisfaction rate of 90% for team-based care providers. Finally, in our aTBC model—in CMS’s Next-Gen ACO initiative—the cost per patient per month is significantly less than for those in a non-team-based care model ($796 vs $940).

CORRESPONDENCE
James Jerzak, MD, 1630 Commanche Ave, Green Bay, WI 54313; james.jerzak@bellin.org.
ACKNOWLEDGEMENTS
The authors would like to thank Lindsey E. Carlasare, MBA, from the American Medical Association, and Brad Wozney, MD, Kathy Kerscher, and Christopher Elfner from Bellin Health, for their contributions to the content and review of this manuscript.
Leaders in health care and practicing physicians recognize the need for changes in how health care is delivered.1-3 Despite this awareness, though, barriers to meaningful change persist and the current practice environment wherein physicians must routinely spend 2 hours on electronic health records (EHRs) and desk work for every hour of direct face time with patients4 is driving trainees away from ambulatory specialties and is contributing to physicians’ decisions to reduce their practices to part-time, retire early, or leave medicine altogether.5,6 Those who persevere in this environment with heavy administrative burdens run the increasing risk of burnout.7
Some physicians and practices are responding by taking creative measures to reform the way patient care is delivered. Bellin Health—a 160-provider, multispecialty health system in northeast Wisconsin where one of the authors (JJ) works—introduced an advanced team-based care (aTBC) model between November 2014 and November 2018, starting with our primary care providers. The development and introduction of this new model arose from an iterative, multidisciplinary process driven by the desire to transform the Triple Aim—enhancing patient experience, improving population health, and reducing costs—into a Quadruple Aim8 by additionally focusing on improving the work life of health care providers, which, in turn, will help achieve the first 3 goals. In introducing an aTBC model, Bellin Health focused on 3 elements: office visit redesign, in-basket management redesign, and the use of extended care team members and system and community resources to assist in the care of complex and high-risk patients.
Herein we describe the 3 components of our aTBC model,1,9 identify the barriers that existed in the minds of multiple stakeholders (from patients to clinicians and Bellin executives), and describe the strategies that enabled us to overcome these barriers.
The impetus behind our move to aTBC
Bellin Health considered a move to an aTBC model to be critical in light of factors in the health care environment, in general, and at Bellin, in particular. The factors included
- an industry-wide shift to value-based payments, which requires new models for long-term financial viability.
- recognition that physician and medical staff burnout leads to lower productivity and, in some cases, workforce losses.5,6 Replacing a physician in a practice can be difficult and expensive, with cost estimates of $500,000 to more than $1 million per physician.10,11
- a belief that aTBC could help the Bellin Health leadership team meet its organizational goals of improved patient satisfaction, achieve gains in quality measures, enhance engagement and loyalty among patients and employees, and lower recruitment costs.
A 3-part aTBC initiative
■ Part 1: Redesign the office visit
We redesigned staffing and workflow for office visits to maximize the core skills of physicians, which required distributing ancillary tasks among support staff. We up-trained certified medical assistants (CMAs) and licensed practical nurses (LPNs) to take on the new role of care team coordinator (CTC) and optimized the direct clinical support ratio for busier physicians. For physicians who were seeing 15 to 19 patients a day, a ratio of 3 CTCs to 2 physicians was implemented; for those seeing 20 or more patients a day, we used a support ratio of 2:1.
The role of CTC was designed so that he or she would accompany a patient throughout the entire appointment. Responsibilities were broken out as follows:
Pre-visit. Before the physician enters the room, the CTC would now perform expanded rooming functions including pending orders, refill management, care gap closure using standing orders, agenda setting, and preliminary documentation.12
Visit. The CTC would now hand off the patient to the physician and stay in the room to document details of the visit and record new orders for consults, x-ray films, referrals, or prescriptions.13 This intensive EHR support was established to ensure that the physician could focus directly on the patient without the distraction of the computer.
Continue to: Post-visit
Post-visit. After a physician leaves a room, the CTC was now charged with finishing the pending orders, setting up the patient’s next appointment and pre-visit labs, reviewing details of the after-visit summary, and doing any basic health coaching with the patient. During this time, the physician would use the co-location space to review and edit the documentation, cosign the orders and prescriptions submitted by the CTC, and close the chart before going into the next room with the second CTC. The need to revisit these details after clinic hours was eliminated.
Another change … The role of our phone triage registered nurses (RN) was expanded. Care team RNs began providing diabetes counseling, blood pressure checks, annual wellness visits (AWV), and follow-up through the Centers for Medicare and Medicaid Services (CMS)'s Chronic Care Management and Transitional Care Management programs.
■ Part 2: Redesign between-visit in-basket management
Responding to an increasing number of inbox messages had become overwhelming for our physicians. Bellin Health’s management was aware that strategic delegation of inbox messages could save an hour or more of a physician’s time each day.14 Bellin implemented a procedure whereby inbox test results would be handled by the same CTC who saw the patient, thereby extending continuity. If the results were normal, the CTC would contact the patient. If the results were abnormal, the physician and the CTC would discuss them and develop a plan. Co-location of the RN, the CTC, and the physician would leverage face-to-face communication and make in-basket management more efficient.
■ Part 3: Redesign population health management
We developed an Extended Care Team (ECT), including social workers, clinical pharmacists, RN care coordinators, and diabetes educators, to assist with the care of patients with high-risk disorders or otherwise complex issues. These team members would work closely with the CTC, care team RN, and physician to review patients, develop plans of care, optimize management, and improve outcomes. Patients would be identified as candidates for potential ECT involvement based on the physician’s judgment in consultation with an EHR-based risk score for hospitalization or emergency department visit.
As we developed new processes, such as screening for determinants of health, we engaged additional system and community resources to help meet the needs of our patients.
Continue to: A look at stakeholder concerns and overcoming the barriers
A look at stakeholder concerns and overcoming the barriers
Critical to our success was being attentive to the concerns of our stakeholders and addressing them. Along the way, we gained valuable implementation insights, which we share here along with some specifics about how, exactly, we did things at Bellin.
Patients
Some patients expressed hesitation at having a person other than their physician in the exam room. They worried that the intimacy and privacy with their physician would be lost. In light of this, we gave patients the option not to have the CTC remain in the room. However, patients quickly saw the value of this team-based care approach and seldom asked to be seen without the CTC.
Throughout the process, we surveyed patients for feedback on their experiences. Comments indicated that the presence of the CTC in our team-based model led to positive patient experiences:
My physician is fully attentive. Patients appreciated that physicians were not distracted by the computer in the exam room. “I feel like I’ve got my doctor back” has been a common refrain.
The office staff is more responsive. The CTC, having been present during the appointment, has a deeper understanding of the care plan and can respond to calls or emails between visits, thereby reducing the time patients must wait for answers. One patient commented that, “I love [the doctor’s] team; his nurses are willing to answer every question I have.”
Continue to: I increasingly feel that I'm understood
I increasingly feel that I’m understood. We have seen patients develop meaningful relationships with other team members, confiding in them in ways that they hadn’t always done with physicians and advanced practice clinicians (APCs). Team members, in turn, have added valuable insights that help optimize patients’ care. In particular, the care of patients with multiple needs has been enhanced with the addition of ECT members who work with the core team and use their expertise to optimize the care of these patients.
Certified medical assistants and licensed practical nurses
Bellin’s leadership knew that team documentation could cause stress for the CMA, who, acting as a CTC, wanted to avoid misrepresenting details of the clinical encounter.13 Adding to the stress were other duties that would need to be learned, including agenda setting, refill management, care gap closure, and health coaching. With thorough training and preparation, many—but not all—of our CMAs and LPNs were able to successfully make the transition and flourish.
Implementation strategies
Provide thorough training. Our training process started 8 weeks before it was time to “go live.” There were weekly hour-long training sessions in population health basics, team culture and change management, documentation basics, and new roles and responsibilities. In the final week, the entire aTBC team sat together for 3 days of EHR training. All new teams shadowed existing teams to get a clear picture of the new processes.
Create a community of support. As our CMAs adapted to their new CTC roles, it was critical that they had support from experienced CTCs. Encouragement and patience from physicians were—and are—essential for CTCs to develop confidence in their new roles.
Enable ongoing feedback. We introduced weekly team meetings to enhance team communication and dynamics. Forums for all roles are held periodically to facilitate discussion, share learning, and enable support between teams.
Continue to: Use EHR tools to facilitate this work
Use EHR tools to facilitate this work. Using standard templates and documentation tools helped CTCs develop the confidence needed to thrive in their new role. Knowing these tools were available helped CTCs become effective in helping the team manage the between-visit work.
Monitor workload. As we developed more workflows and processes, we took care to monitor the amount of additional work for those in this role. We offloaded work whenever possible. For example, coordinated refill management at time of service, coupled with a back-up centralized refill system, can significantly decrease the number of refill requests made to CTCs. We continue to adjust staffing, where appropriate, to provide adequate support for those in this valuable role.
Be prepared for turnover. As CTCs became empowered in their new roles, some decided to advance their training into other roles. We developed a plan for replacing and training new staff. Higher pay can also be used to help attract and retain these staff members. Bellin uses LPNs in this role to ensure adequate staffing. Other health systems have developed a tier system for CMAs to improve retention.
Registered nurses
Before our move to an aTBC model, our office RNs primarily managed phone triage. Now the nurses were enlisted to play a more active role in patient care and team leadership. Although it was a dramatic departure from prior responsibilities, the majority of Bellin’s RNs have found increased satisfaction in taking on direct patient care.
Implementation strategies
Define new roles and provide training. In addition to participating in acute patient visits, consider ways that care team RNs can expand responsibilities as they pertain to disease counseling, population health management, and team leadership.15 At Bellin, the expanded role of the RN is evident in diabetes education and Medicare AWVs. Specifically, RNs now provide diabetes education to appropriate patients following a warm handoff from the physician at the time of the visit. RNs now also complete Medicare AWVs, which frees up physicians for other tasks and helps ensure sustainability for the new RN roles. Rates of completed AWVs at Bellin are now more than 70%, compared with reported national rates of less than 30%.16
Continue to: Maximize co-location
Maximize co-location. It is helpful to have the team members whose work is closely related—such as the CTCs and the RN for the team—to be situated near each other, rather than down a hall or in separate offices. Since the RN is co-located with the core teams at Bellin, there is now greater opportunity for verbal interaction, rather than just electronic communications, for matters such as triage calls and results management. RNs also provide a valuable resource for CMAs and LPNs, as well as help oversee team management of the in-basket.
Evaluate sustainability. Additional roles for the RNs required additional RN staffing. We assessed the new workload duties and balanced that against potential revenue from RN visits. This analysis indicated that an optimal ratio was 1 RN to every 3000 patients. This would allow an adequate number of RNs to fulfill additional roles and was financially sustainable with the goal of 4 billable RN visits per day.
Physicians
Bellin’s leadership recognized that some physicians might perceive team-based care as eroding their primary responsibility for patients’ care. Physicians have historically been trained in a model based on the primacy of the individual physician and that can be a hurdle to embracing team culture as a new paradigm of care. Several strategies helped us and can help others, too.
Implementation strategies
Cultivate trust. Thorough training of CTCs and RNs is critical to helping physicians develop trust and reliance in the team. The physician retains final authority over the team for cosigning orders, editing and finalizing documentation, and overseeing results management. Physicians invested in training and educating their staff will reap the rewards of a highly functioning, more satisfied team.
Encourage leadership. This can be a cultural shift for physicians, yet it is critical that they take a leadership role in this transformation.17 Physicians and their team leaders attended training sessions in team culture and change management. Prior to the go-live date, team leaders also met with the physician individually to explore their concerns and discuss ways to effectively lead and support their teams.
Continue to: Urge acceptance of support
Urge acceptance of support. The complexity of patient care today makes it difficult for a physician to manage all of a patient’s needs single-handedly. Complexity arises from the variety of plan co-pays and deductibles, the number of patients with chronic diseases, and the increased emphasis on improving quality measures.18 Enhanced support during any office visit and the extra support of an ECT for complex patients improves the ability of the physician to more effectively meet the needs of the patient.
Emphasize the benefit of an empowered team. The demands of the EHR on physicians and the resultant frustrations are well chronicled.4,19-22 Strategically delegating much of this work to other team members allows the physician to focus on the patient and perform physician-level work. At Bellin, we observed that our most successful care teams were those in which the physician fully accepted team-based care principles and empowered the staff to work at the top of their skill set.
Advanced practice clinicians
APCs in our system had traditionally practiced in 1 of 3 ways: independently handling defined panels with physician supervision; handling overflow or acute visits; or working collaboratively with a supervising physician to share a larger “team panel.” The third approach has become our preferred model. aTBC provides opportunities for APCs to thrive and collaborate with the physician to provide excellent care for patients.
APCs underwent the same process changes as physicians, including appropriate CTC support. Implementation strategies for APCs were similar to those that were useful for physicians.
Risk management professionals
At Bellin, we found that risk-management professionals had concerns about the scope of practice assigned to various team members, particularly regarding documentation. CMS allows for elements of a patient visit to be documented by CMAs and other members of the care team in real time as authorized by the physician.23,24 CTCs at Bellin also have other clinical duties in patient and EHR management. aTBC practices generally prefer the term team documentation over scribing, since it more accurately reflects the scope of the CTC’s work.
Continue to: Implementation strategies
Implementation strategies
Clarify regulatory issues. Extensive use of standing orders and protocols allowed us to increase involvement of various team members. State laws vary in what functions CMAs and LPNs are allowed to perform, so it is important to check your state guidelines.25 There is a tendency for some risk managers to overinterpret regulations. Challenge them to provide exact documentation from regulatory agencies to support their decisions.
Give assurances of physician oversight and processes. The physician assumes responsibility for standing orders, protocols, and documentation. We made sure that we had clear and consistent processes in place and worked closely with our risk managers as we developed our model. aTBC provides checks and balances to ensure accurate records, since team members are able to contribute and check for accuracy. A recent study suggested that CMAs perform documentation that is of equal or higher quality than that performed by the physician.26
Financial leadership
Like any organization adopting aTBC, Bellin’s leadership was concerned about the expense of adopting this approach. However, the leadership also recognized that the transition to aTBC could increase revenue by more than the increased staffing costs. In addition, we expected that capacity, access, continuity, and financial margins would increase.2,3,27,28 We also anticipated a decrease in downstream services, such as unnecessary tests, emergency department visits, and hospitalizations—a benefit of accountable care payment models.
Our efforts have been successful from a financial point of view. We attribute the financial sustainability that we have experienced to 4 factors:
1. Increased productivity. We knew that the increased efficiency of team-based care enables physicians to see 1 to 2 more patients per half day, and sometimes more.3,28,29 An increase of at least 1 patient visit per half-day was expected of our physicians and APCs on aTBC. In addition, they were expected to support the care team RN in achieving at least 4 billable visits per day. Our current level of RN visits is at 3.5 per nurse per day. There is significant variability in the increase of patients seen by a physician per day, ranging from 1 to 4 additional patients. These increased visits have helped us achieve financial viability, even in a predominantly fee-for-service environment.
2. More thorough service. The ability to keep patients in primary care and to focus on the patient’s full range of needs has led to higher levels of service and, consequently, to appropriately higher levels of billing codes. For example, Bellin’s revenue from billing increased by $724 per patient, related (in part) to higher rates of immunizations, cancer screenings with mammography, and colonoscopies.
Continue to: 3. New billable services
3. New billable services. Billing for RN blood pressure checks, AWVs, and extended care team services have helped make aTBC at Bellin financially feasible. Revenue from RN visits, for example, was $630,000 in 2018.
4. Improved access for patients. Of the 130 primary care providers now on aTBC, 15 (11.5%) had closed their practices to new patients before aTBC. Now, all of their practices are open to new patients, which has improved access to care. In a 2018 patient access survey, 96.6% of patients obtained an appointment as soon as they thought it was needed, compared with 70.7% of patients before the transition to aTBC.
Greater opportunity for financial sustainability. The combination of improved quality measures and decreased cost of care in the Bellin aTBC bodes well for future success in a value-based world. We have realized a significant increase in value-based payments for improved quality, and in our Next Gen Accountable Care Organization (ACO) patients, we have seen a decrease of $29 in per-member-per-month costs, likely due to the use of nonphysicians in expanded roles. In addition, hospital admissions have decreased by 5% due to the ability of ambulatory teams to manage more complex patients in the office setting. This model has also allowed physicians and APCs to increase their panel size, another key value-based metric. From 2016 to 2018, panel size for primary care providers increased by an average of 8%.
Enhanced ability to retain and recruit. Several of Bellin’s primary care recruits indicated that they had interviewed only at practices incorporating team-based care. This trend may increase as residencies transition to team-based models of care.
So how did we do?
Metrics of Bellin’s aTBC success
By the end of 2018, all 130 primary care physicians and APCs at Bellin had made the transition to this model, representing family medicine, internal medicine, and pediatrics. We have now begun the transition of our non-primary care specialties to team-based care.
Continue to: In the aTBC model...
In the aTBC model, the percentage of patients receiving age-appropriate screening is higher than before in every domain we measure (FIGURE 1). There has also been improvement in major quality metrics (FIGURE 2).
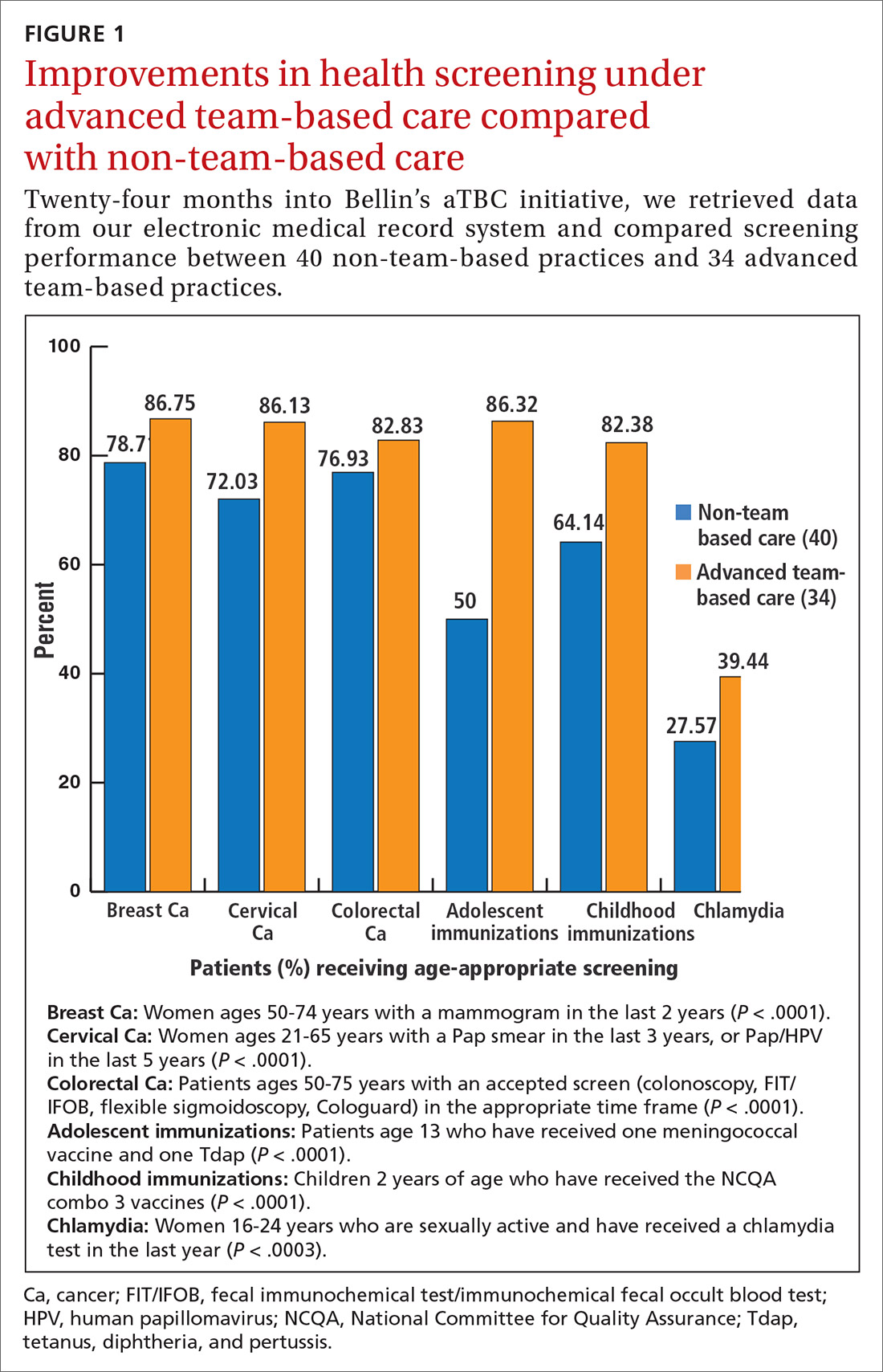
In a survey done in Spring 2018 by St. Norbert College Strategic Research Center, provider satisfaction increased, with 83% of physicians having made the transition to an aTBC practice moderately or very satisfied with their Bellin Health experience, compared with 70% in the traditional model. More recent 2019 survey data show a satisfaction rate of 90% for team-based care providers. Finally, in our aTBC model—in CMS’s Next-Gen ACO initiative—the cost per patient per month is significantly less than for those in a non-team-based care model ($796 vs $940).

CORRESPONDENCE
James Jerzak, MD, 1630 Commanche Ave, Green Bay, WI 54313; james.jerzak@bellin.org.
ACKNOWLEDGEMENTS
The authors would like to thank Lindsey E. Carlasare, MBA, from the American Medical Association, and Brad Wozney, MD, Kathy Kerscher, and Christopher Elfner from Bellin Health, for their contributions to the content and review of this manuscript.
1. Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
2. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
3. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
4. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
5. Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422-431.
6. Sinsky CA, Dyrbye LN, West CP, et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc. 2017;92:1625-1635.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
8. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
9. Sinsky CA, Sinsky TA, Althaus D, et al. Practice profile. ‘Core teams’: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Aff (Millwood). 2010;29:966-968.
10. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
11. Association for Advancing Physician and Provider Recruitment. Schutte L. What you don’t know can cost you: building a business case for recruitment and retention best practices. 2012. https://member.aappr.org/general/custom.asp?page=696. Accessed June 20, 2019.
12. American Medical Association. AMA STEPS Forward. Expanded rooming and discharge protocols. https://edhub.ama-assn.org/steps-forward/module/2702600. Accessed June 20, 2019.
13. American Medical Association. AMA STEPS Forward. Team documentation. https://edhub.ama-assn.org/steps-forward/module/2702598?resultClick=3&bypassSolrId=J_2702598. Accessed June 20, 2019.
14. American Medical Association. AMA STEPS Forward. EHR in-basket restructuring for improved efficiency. https://edhub.ama-assn.org/steps-forward/module/2702694?resultClick=3&bypassSolrId=J_2702694. Accessed June 20, 2019.
15. California Health Care Foundation. Bodenheimer T, Bauer L, Olayiwola JN. RN role reimagined: how empowering registered nurses can improve primary care. https://www.chcf.org/publication/rn-role-reimagined-how-empowering-registered-nurses-can-improve-primary-care/. Accessed June 20, 2019.
16. Chung S, Lesser LI, Lauderdale DS, et al. Medicare annual preventive care visits: use increased among fee-for-service patients, but many do not participate. Health Aff (Millwood). 2015;34:11-20.
17. American Medical Association. AMA Policy H-160.912. The structure and function of interprofessional health care teams. https://policysearch.ama-assn.org/policyfinder/detail/The%20Structure%20and%20Function%20of%20Interprofessional%20Health%20Care%20Teams?uri=%2FAMADoc%2FHOD.xml-0-727.xml. Accessed June 20, 2019.
18. Milani RV, Lavie CJ. Health care 2020: reengineering health care delivery to combat chronic disease. Am J Med. 2015;128:337-343.
19. Hill RG Jr, Sears LM, Melanson SW. 4000 clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med. 2013;31:1591-1594.
20. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21:e100-e106.
21. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
22. RAND Corporation. Friedberg MW, Chen PG, Ban Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. https://www.rand.org/pubs/research_reports/RR439.html. Accessed June 20, 2019.
23. Evaluation and Management (E/M) visit frequently asked questions (FAQs): physician fee schedule (PPS). https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/E-M-Visit-FAQs-PFS.pdf. Accessed August 27, 2019.
24. Centers for Medicare & Medicaid Services. Scribe services signature requirements. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2017-Transmittals-Items/R713PI.html. Accessed June 20, 2019.
25. American Association of Medical Assistants. State scope of practice laws. http://www.aama-ntl.org/employers/state-scope-of-practice-laws. Accessed June 20, 2019.
26. Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65:155-159.
27. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
28. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406.
29. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
1. Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
2. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
3. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
4. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
5. Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422-431.
6. Sinsky CA, Dyrbye LN, West CP, et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc. 2017;92:1625-1635.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613.
8. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
9. Sinsky CA, Sinsky TA, Althaus D, et al. Practice profile. ‘Core teams’: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Aff (Millwood). 2010;29:966-968.
10. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826-1832.
11. Association for Advancing Physician and Provider Recruitment. Schutte L. What you don’t know can cost you: building a business case for recruitment and retention best practices. 2012. https://member.aappr.org/general/custom.asp?page=696. Accessed June 20, 2019.
12. American Medical Association. AMA STEPS Forward. Expanded rooming and discharge protocols. https://edhub.ama-assn.org/steps-forward/module/2702600. Accessed June 20, 2019.
13. American Medical Association. AMA STEPS Forward. Team documentation. https://edhub.ama-assn.org/steps-forward/module/2702598?resultClick=3&bypassSolrId=J_2702598. Accessed June 20, 2019.
14. American Medical Association. AMA STEPS Forward. EHR in-basket restructuring for improved efficiency. https://edhub.ama-assn.org/steps-forward/module/2702694?resultClick=3&bypassSolrId=J_2702694. Accessed June 20, 2019.
15. California Health Care Foundation. Bodenheimer T, Bauer L, Olayiwola JN. RN role reimagined: how empowering registered nurses can improve primary care. https://www.chcf.org/publication/rn-role-reimagined-how-empowering-registered-nurses-can-improve-primary-care/. Accessed June 20, 2019.
16. Chung S, Lesser LI, Lauderdale DS, et al. Medicare annual preventive care visits: use increased among fee-for-service patients, but many do not participate. Health Aff (Millwood). 2015;34:11-20.
17. American Medical Association. AMA Policy H-160.912. The structure and function of interprofessional health care teams. https://policysearch.ama-assn.org/policyfinder/detail/The%20Structure%20and%20Function%20of%20Interprofessional%20Health%20Care%20Teams?uri=%2FAMADoc%2FHOD.xml-0-727.xml. Accessed June 20, 2019.
18. Milani RV, Lavie CJ. Health care 2020: reengineering health care delivery to combat chronic disease. Am J Med. 2015;128:337-343.
19. Hill RG Jr, Sears LM, Melanson SW. 4000 clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med. 2013;31:1591-1594.
20. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21:e100-e106.
21. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
22. RAND Corporation. Friedberg MW, Chen PG, Ban Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. https://www.rand.org/pubs/research_reports/RR439.html. Accessed June 20, 2019.
23. Evaluation and Management (E/M) visit frequently asked questions (FAQs): physician fee schedule (PPS). https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/E-M-Visit-FAQs-PFS.pdf. Accessed August 27, 2019.
24. Centers for Medicare & Medicaid Services. Scribe services signature requirements. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2017-Transmittals-Items/R713PI.html. Accessed June 20, 2019.
25. American Association of Medical Assistants. State scope of practice laws. http://www.aama-ntl.org/employers/state-scope-of-practice-laws. Accessed June 20, 2019.
26. Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract. 2016;65:155-159.
27. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med. 2010;17:490-494.
28. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res. 2013;5:399-406.
29. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
PRACTICE RECOMMENDATIONS
› Up-train staff to provide enhanced support for physicians during the office visit, such as handling most electronic health record work, including documentation. C
› Take a team approach to between-visit work, leveraging principles of team-based care (such as co-location) to optimize efficiency. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
TEAM approach reduced wait time, improved “face” time
ABSTRACT
Purpose In 2013-14, 2 clinics in the Watertown Regional Medical Center (WRMC; in southern Wisconsin) launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” as part of a quality improvement project to enhance the delivery experience for the patient, physician, and medical assistant (MA). New work flows, roles, and responsibilities were designed to reduce cycle time, increase patient time with physicians and staff, and reduce patient wait times.
Methods The new model increased the ratio of MAs to physicians from a baseline MA:MD ratio of 1:1 to 3:2, and trained MAs to assume expanded roles during exam-room entry and discharge, including assisting with documentation during the patient visit. A process engineer timed patient visits. The process engineer and a human resources associate conducted surveys to assess the level of satisfaction for patients, physicians, and MAs.
Results Cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased a mean of 2 minutes, from 24 to 26 minutes per patient; and waiting time decreased from 9 to 2 minutes per patient. Qualitative interviews with patients, physicians, and MAs identified a high level of satisfaction with the new model.
Conclusion The higher staffing ratios and expanded roles for MAs in the new model improved workflow, increased the face time between patients and their physician and MA, and decreased patient wait times. The TEAM model also appeared to improve patient, physician, and MA satisfaction. We faced many challenges while implementing the new model, which could be further evaluated during wide adoption.
In recent years, we observed that our physicians, nurses, and medical assistants (MAs) appeared to be spending more time on administrative and clerical tasks—including tasks in the exam room with the patient—and less time engaged in direct patient care.1,2 We recognized these factors contribute to burnout and threaten staff retention and anticipated that a new model would improve physician time spent in direct patient care, decrease the demands of administrative tasks, and increase patient, physician, and MA satisfaction.3-6 Burnout, known to affect more than half of US physicians, has a negative impact on quality of care and patient safety and satisfaction.7-11 Improving workflow has been shown to reduce burnout.12
Watertown Regional Medical Center (WRMC) is a small, financially stable integrated delivery system in rural southern Wisconsin, composed of a 90-bed hospital, 10 primary care clinics (7 owned and 3 affiliated), and 24 employed physicians in 9 specialties. Two clinics within WRMC launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” to improve the delivery experience for the entire team, defined as the patient, physician, and MA. New workflows, roles, and responsibilities were designed to reduce cycle time (the total amount of time patients spent in the clinic from check-in to check-out), increase the total time a patient spent with staff (physician and MA or in point-of-care testing and radiology), and reduce the total time a patient spent waiting.13
We describe here WRMC’s experience in developing and implementing workflow improvements as a means of reducing burnout and improving satisfaction.
Continue to: METHODS
METHODS
We selected 2 WRMC sites for TEAM re-engineering based on their experience with quality-improvement projects and perceived likelihood of success with a new transformation initiative. In early 2013, WRMC charged one physician (JM), 2 MAs, the clinic scheduler, and the clinic administrator with designing the details of the model including evaluation metrics. WRMC provided a .5 FTE process engineer (MS) to assist with the design and implementation of the model at no extra expense to the clinics. The model was implemented in late 2013 and into 2014 after regular TEAM planning meetings and observational visits to non-WRMC sites identified as examples of best practices in improving outpatient primary care patient satisfaction: Bellin Health (Green Bay, Wis); ThedaCare (Appleton, Wis); the University of Utah (Salt Lake City); and the University of Wisconsin Health Yahara Clinic (Madison, Wis).
TEAM model
The TEAM model—so named to create top-of-mind awareness of its benefits—increased the MA:MD ratio, maintained consistent team composition so that physician/MA teams learned to work together and become more efficient, and added new MA responsibilities. We trained MAs to assist with documentation in the exam room to ensure that physician time was spent in face-to-face direct patient care.14-20 In these ways, we sought not only to increase patient satisfaction but also to enhance our own “joy in practice,” defined primarily by a high level of work-life satisfaction, a low level of burnout, and a feeling that the medical practice is fulfilling.21
In our traditional model, an MA retrieved the patient from the waiting room, conducted initial assessment in the exam room, and then left the patient to wait for the physician to enter. Once the physician entered and conducted the exam, the patient would be left alone again to wait for the MA to return. In our revised model (TABLE 1), we assigned one MA to each patient from arrival to discharge. After greeting the patient in the waiting room, the MA conducted an initial patient interview in the exam room, then remained in the room with the physician to document the visit. After the physician exited the exam room, the MA completed follow-up orders and provided the patient with a visit summary.
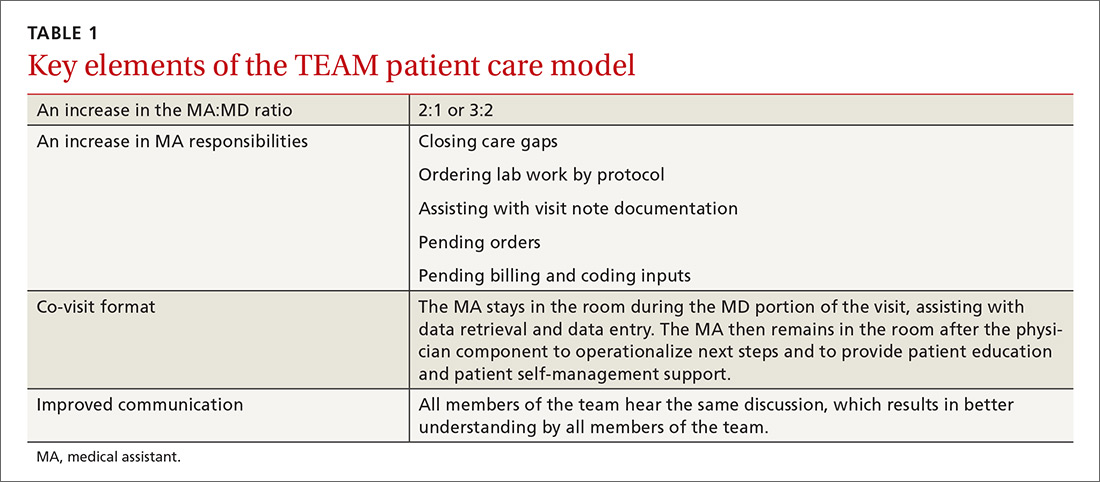
To facilitate consistency throughout the day, we designed a workflow similar to those created in lean models originally designed to increase efficiency in the manufacturing industry (TABLE 2). Visual and electronic cues triggered each step of the process and coordinated the movement of MAs and MDs. Cues included the conventional flag system outside each exam room, an electronic messaging system within the electronic health record (EHR) to indicate when a patient was ready to be seen, and a whiteboard in an area visible to all team members on which we wrote lab and radiology requests.
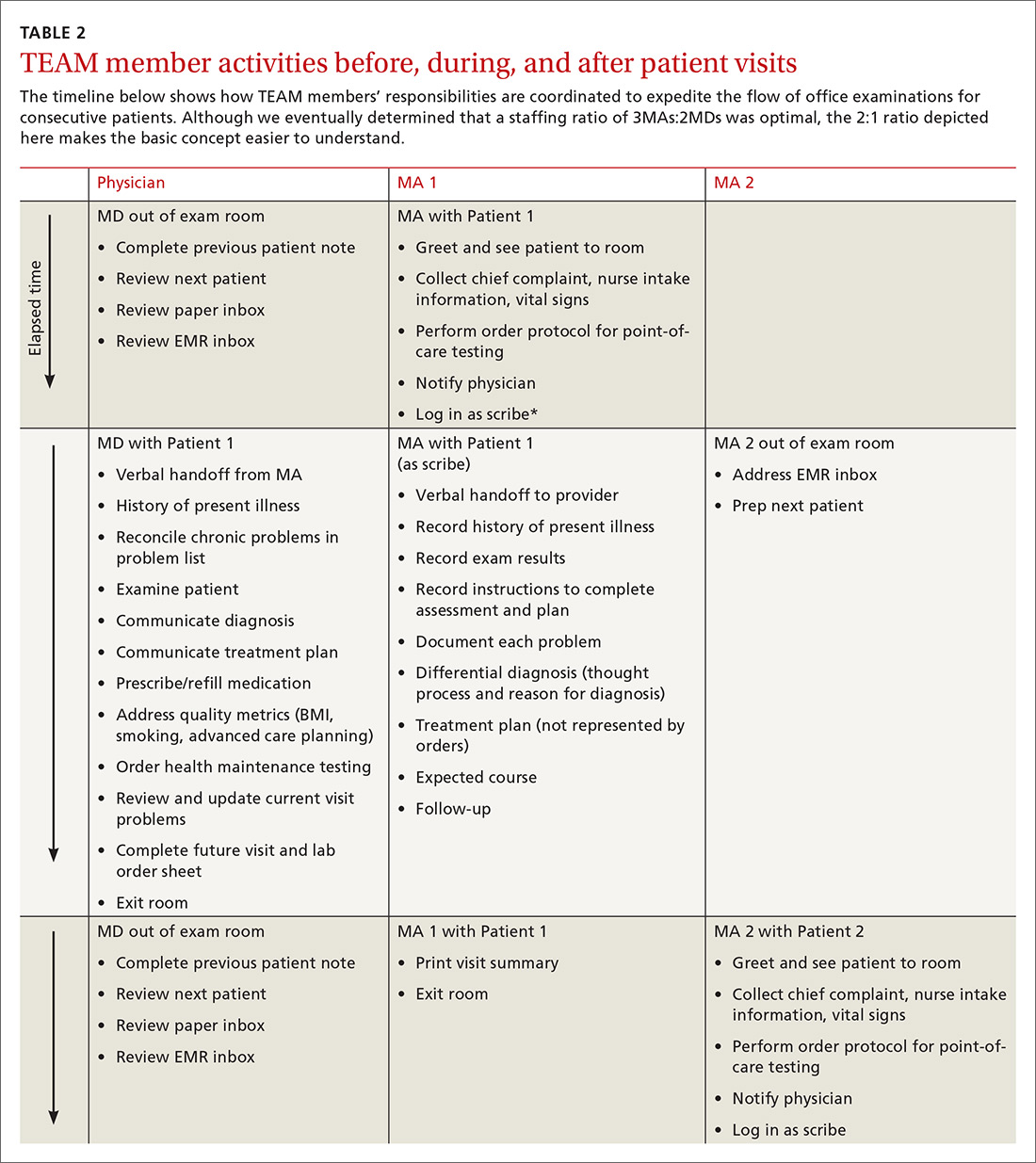
We experimented with the MA:MD ratio to identify the most effective and efficient team composition. On alternating weeks, we assigned one MA to one MD, 2 MAs to one MD, or 3 MAs to 2 MDs. Additionally, with the 2:1 MA:MD ratio, we varied the visit length in 2 tests; one spanning 30 minutes and the other 20 minutes. The MDs and MAs were seated at side-by-side workstations to make communication easier. We developed protocols and checklists that allowed MAs to enter health maintenance orders and conduct point-of-care testing before the physician entered the room. Such details included immunization management, strep screens, urine analyses, diabetic foot exams, extremity x-ray films, and mammogram and colonoscopy referrals.
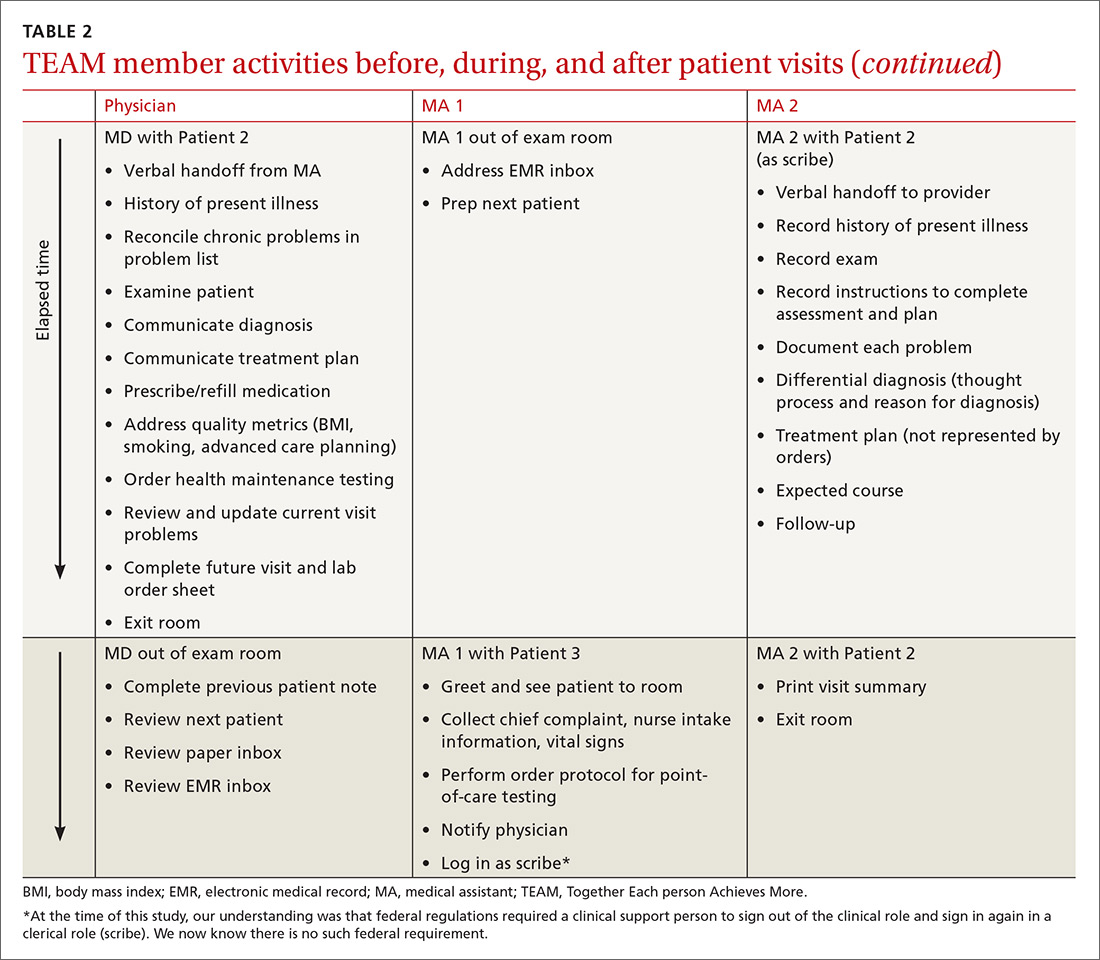
Continue to: To prepare MAs...
To prepare MAs, we obtained special permission for team documentation from our Chief Information Officer and developed associated policies and procedures. A physician assistant (PA) trained each MA, introducing the structure and content of subjective, objective, assessment, and plan (SOAP) notes. Training was continuous, as PAs provided feedback when MAs began team documentation. The MAs documented visits using templates, free form, and quick text. We measured visit cycle-time, face time with staff, and patient waiting times. A process engineer with a stopwatch observed and timed the flow (but did not enter the exam room). We also conducted patient interviews immediately post-visit and administered anonymous questionnaires to clinic staff at different phases of the model. Physicians and MAs met weekly to evaluate the design.
We used qualitative interviews of patients, physicians, and MAs to identify the level of satisfaction with the new model. During the first week of implementation, a nurse and our process engineer conducted brief in-person surveys with approximately 20 post-visit patients. Patients, chosen by convenience, were asked if the visit addressed their concerns, whether they left with a thorough understanding of next steps, and if their wait time was acceptable. Twice during the implementation phase, a human resources associate distributed 9-item anonymous questionnaires to staff members during scheduled department meetings.
RESULTS
Times per activity with different MA:MD ratios and visit lengths are shown in TABLE 3. After 6 months, cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased by a mean of 2 minutes, from 24 to 26 minutes per patient; and wait time decreased by a mean of 7 minutes, from 9 to 2 minutes per patient. We concluded the MA:MD ratio of 3:2 was most efficient because the 2:1 model left MAs with excess non-patient time.
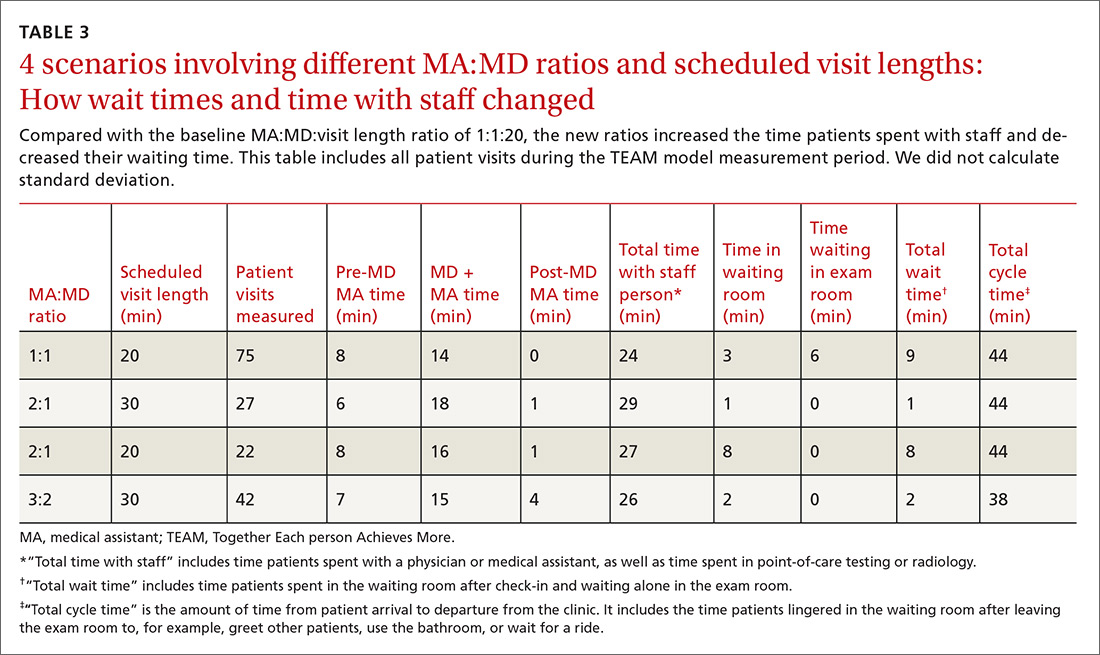
Our delivery model received consistently positive comments from patients. Many expressed gratitude for the extra set of ears and eyes guiding them through the process. One recalled the “old days” when a nurse joined the doctor in the exam room. Another appreciated that both the MA and physician could answer follow-up questions over the phone.
Employee satisfaction
Surveys to assess satisfaction were distributed to all employees whether they were involved in the new model or not. Sixteen employees responded to the pre-implementation questionnaire and 18 responded to the post-implementation one distributed 7 months later. The questionnaires showed an increase in employee satisfaction scores from 3.70 to 3.89 on a 5-point Likert scale, with 5 ranking highest. “I am learning from [Dr. Milford] and understanding things more fully,” wrote one respondent. Another said, “Dr. Milford and his clinical support staff are less stressed.” Individual observations such as, “I can leave sooner with less work left to do,” and “All documentation is done before [the] patient leaves,” reflect the reduction in time that patient records remained open or incomplete. Some physicians reported a reduction in at-home or after-hours work, from about 2 to 4 hours per day to approximately one hour per day.
Continue to: Additional outcomes
Additional outcomes
The TEAM model allowed us to more easily integrate new initiatives into our practice and meet quality metrics by placing needed components within our workflow and checklist. For example, achieving Stage II Meaningful Use measures required that we print and furnish patients with a visit summary and a reminder to access our portal; something we easily incorporated into the MAs’ expanded responsibilities. We also met specific predetermined quality metrics that were part of a payment-withhold program. During the study period, we achieved scores at the 90th percentile and earned back our total withhold.
Finally, more of our patients completed advanced care planning discussions than the other 7 sites in our Honoring Choices Wisconsin cohort. This was achieved not only by integrating the process into our checklist, but because the MAs observed the MD-led patient conversations which they then emulated, presenting the advanced care planning information to patients before or after MD time with the patient.
Errors and defects in care
With ongoing provider guidance and reinforcement, MAs became integral members of the primary care team. They were empowered through protocols to manage and order health maintenance testing and provide needed immunizations. They also began to identify potentially overlooked aspects of care. For example, MAs prompted physicians to retake vital signs, adjust medications, order labs, discuss previous lab results, and pursue specialty referrals or follow-up care.
Billing
Although we tracked billing, the TEAM model was not designed to influence revenue. We noted no significant change in level of evaluation and management billed regardless of staffing ratio. While our panel size increased as we implemented the new process, this change could have been due to normal variation. We do see opportunity to affect future billing by having coders train MAs, which could enhance documentation and increase revenue.
DISCUSSION
The TEAM Primary Care model reduced the time our patients sat unattended, increased our opportunities to meaningfully interact with them, and seemed to reduce our administrative load. By identifying and implementing ways to work as a more cohesive, interconnected unit, we began to address our work as a team rather than as individuals. After implementing the model, we noted several instances where the MAs caught potential errors in care, although we did not consistently track or measure changes in the rate of these occurrences.
Continue to: Achieving these results also came with...
Achieving these results also came with challenges. Investing in and maintaining a new model opened our eyes to unforeseen inconsistencies in our staff profile and to the cost and administrative support needed for implementation. Moreover, our entire team (patients, MAs, and physicians) had to undergo a major cultural shift to adopt a new model.
Personnel variation
We discovered that implementing and sustaining organization change is highly dependent on constancy in human resources. When one team member was on vacation, sick, or leaving the practice, the process tended to fall apart. Hiring replacements and training employees well enough to fill in at a moment’s notice proved difficult. Bringing new employees into this process was also labor intensive. Despite team members being very engaged in change, these staffing inconsistencies caused significant stress and necessitated pauses in the implementation of the new model (reflected in the timeline of our measures). Larger organizational buy-in and support would allow us to hire and train a larger pool of MAs in anticipation of these fluctuations.
Cost
Our small, rural family practice took advantage of WRMC’s Primary Care Transformation project and the half-time process engineer and additional MA they provided. We question whether this model could be implemented without such support. While a process engineer might not prove necessary, expertise in process improvement is vital to help design and measure workflow and to identify opportunities for improvement.
Cultural change
Adopting a new model required asking every member of the team (patient, MA, and physician) to accommodate change and tolerate disruption. We anticipated patients might resist having an additional person in the room. All patients were informed of our new model at the beginning of the visit and told they could opt out. While we did not document patient resistance, JM recalled only 2 patients who expressed a desire not to have the MA present because of personal and sensitive issues. It’s possible some patients did not feel comfortable opting out. But many patients expressed gratitude for having an extra set of ears and eyes to guide them through the visit.
It was more challenging to support MAs as they stepped out of their comfort zone to assist with documentation. It took time for MAs to grow accustomed to the protocols and checklists essential to our workflow. Without protocols, any point-of-care testing that could have been completed at the beginning of the appointment had to be done at the end. This disrupted our workflow and increased patient wait times.
Continue to: We correctly predicted MAs would have...
We correctly predicted MAs would have difficulty documenting the assessment, plan, and medical decision making. We discovered that MAs more easily categorized and articulated information when we reframed the assessment and plan in first-person and placed it under “Patient instructions.” For this to occur, physicians had to learn to accurately articulate their thought process and instructions to the patient.
When training was provided, as previously described, MAs grasped the subjective section quickly. Surprisingly, they had most difficulty understanding terminology within the objective section. In the future, we would avert this problem by working closely with the human resource department. We believe there should be a newly defined position and additional training for MAs in these roles, since duties such as patient-coaching and documentation assistance may warrant separate certification.
Limitations
Our findings should be interpreted in light of several limitations. Implementing the new model was carried out in a single organization. The patients who were selected and agreed to be interviewed may have differed from the patient population as a whole. We did not measure some important outcomes, such as cost effectiveness and patient morbidity. We did not analyze the data to determine whether the apparent improvements in wait time and cycle time were statistically significant. In addition, measurement of any adverse effects was beyond the scope of this study.
Looking forward
The traditional model of physicians working individually with minimal support staff is no longer viable. To echo our co-author (CAS)’s recent statements on physician dissatisfaction, “The days of hero medicine, with the doctor doing it all, belong in the past.”21 The new model appeared to alleviate some administrative burdens and increase physician time with patients. Pressures to achieve quality measures and growing administrative tasks have altered the role and responsibilities of each member of the team.
Any sustainable system must address the larger crisis of physician dissatisfaction.7,22 We cannot focus on a single perspective—patient, physician, or MA—at the expense of the system as a whole. If the health care system is to resolve the epidemic of burnout and physician dissatisfaction, new approaches to patient care must be imagined and realized. Although we faced many challenges in implementing and evaluating the TEAM model, attempts to overcome these challenges appear justified because of our overall favorable impression of it. Innovations like the TEAM Primary Care model may help us improve the well-being of not just our patients but also our health professionals and the health care industry as a whole.
CORRESPONDENCE
James Milford, MD, Three Oaks Health, S.C., 480 Village Walk Lane, Suite F, Johnson Creek, WI 53038; jam@threeoakshealthcare.com.
SUPPORT
Although the Watertown Regional Medical Center has provided general funding for its Primary Care Transformation project, no dollars were specifically earmarked for the TEAM Primary Care process. Support for editorial services in preparing this article was provided by Dr. James Milford.
PRIOR PRESENTATIONS
Co-author Michael R. Strasser, MPA, presented this project at the 2015 i-PrACTISE conference in Madison, Wis, April 12-14, 2015. http://www.fammed.wisc.edu/i-practise/. The proceedings were not published or recorded.
ACKNOWLEDGMENT
We thank Annalynn Skipper and Masarah Van Eyck for their valuable edits.
1. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
2. McDonald CJ, Callaghan FM, Weissman A, et al. Use of internist’s free time by ambulatory care electronic medical record systems. JAMA Intern Med. 2014;174:1860-1863.
3. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
4. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Available at: http://www.rand.org/pubs/research_reports/RR439.html#key-findings. Accessed October 25, 2016.
5. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc. 2014;21:e100-e106.
6. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. 2001.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proc. 2015;90:1600-1613.
8. DeMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychol. 1993;12:93-102.
9. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358-367.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122-128.
12. Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30:1105-1011.
13. Ferrer RL, Mody-Bailey P, Jaén CR, et al. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7:504-512.
14. Sinsky CA, Williard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
15. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
16. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
17. Yan C, Rose S, Rothberg MB, et al. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2016;31:990-995.
18. Misra-Hebert AD, Rabovsky A, Yan C, et al. A team-based model of primary care delivery and physician-patient interaction. Am J Med. 2015;128:1025-1028.
19. Anderson RJ. Optimizing the role of nursing staff to enhance physician productivity: one physician’s journey. Fam Pract Manag. 2013;20:18-22.
20. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008:15:35-40.
21. Sinsky CA. Dissatisfaction among Wisconsin physicians is part of a serious national trend. Wis Med J. 2015;114:132-133.
22. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
ABSTRACT
Purpose In 2013-14, 2 clinics in the Watertown Regional Medical Center (WRMC; in southern Wisconsin) launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” as part of a quality improvement project to enhance the delivery experience for the patient, physician, and medical assistant (MA). New work flows, roles, and responsibilities were designed to reduce cycle time, increase patient time with physicians and staff, and reduce patient wait times.
Methods The new model increased the ratio of MAs to physicians from a baseline MA:MD ratio of 1:1 to 3:2, and trained MAs to assume expanded roles during exam-room entry and discharge, including assisting with documentation during the patient visit. A process engineer timed patient visits. The process engineer and a human resources associate conducted surveys to assess the level of satisfaction for patients, physicians, and MAs.
Results Cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased a mean of 2 minutes, from 24 to 26 minutes per patient; and waiting time decreased from 9 to 2 minutes per patient. Qualitative interviews with patients, physicians, and MAs identified a high level of satisfaction with the new model.
Conclusion The higher staffing ratios and expanded roles for MAs in the new model improved workflow, increased the face time between patients and their physician and MA, and decreased patient wait times. The TEAM model also appeared to improve patient, physician, and MA satisfaction. We faced many challenges while implementing the new model, which could be further evaluated during wide adoption.
In recent years, we observed that our physicians, nurses, and medical assistants (MAs) appeared to be spending more time on administrative and clerical tasks—including tasks in the exam room with the patient—and less time engaged in direct patient care.1,2 We recognized these factors contribute to burnout and threaten staff retention and anticipated that a new model would improve physician time spent in direct patient care, decrease the demands of administrative tasks, and increase patient, physician, and MA satisfaction.3-6 Burnout, known to affect more than half of US physicians, has a negative impact on quality of care and patient safety and satisfaction.7-11 Improving workflow has been shown to reduce burnout.12
Watertown Regional Medical Center (WRMC) is a small, financially stable integrated delivery system in rural southern Wisconsin, composed of a 90-bed hospital, 10 primary care clinics (7 owned and 3 affiliated), and 24 employed physicians in 9 specialties. Two clinics within WRMC launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” to improve the delivery experience for the entire team, defined as the patient, physician, and MA. New workflows, roles, and responsibilities were designed to reduce cycle time (the total amount of time patients spent in the clinic from check-in to check-out), increase the total time a patient spent with staff (physician and MA or in point-of-care testing and radiology), and reduce the total time a patient spent waiting.13
We describe here WRMC’s experience in developing and implementing workflow improvements as a means of reducing burnout and improving satisfaction.
Continue to: METHODS
METHODS
We selected 2 WRMC sites for TEAM re-engineering based on their experience with quality-improvement projects and perceived likelihood of success with a new transformation initiative. In early 2013, WRMC charged one physician (JM), 2 MAs, the clinic scheduler, and the clinic administrator with designing the details of the model including evaluation metrics. WRMC provided a .5 FTE process engineer (MS) to assist with the design and implementation of the model at no extra expense to the clinics. The model was implemented in late 2013 and into 2014 after regular TEAM planning meetings and observational visits to non-WRMC sites identified as examples of best practices in improving outpatient primary care patient satisfaction: Bellin Health (Green Bay, Wis); ThedaCare (Appleton, Wis); the University of Utah (Salt Lake City); and the University of Wisconsin Health Yahara Clinic (Madison, Wis).
TEAM model
The TEAM model—so named to create top-of-mind awareness of its benefits—increased the MA:MD ratio, maintained consistent team composition so that physician/MA teams learned to work together and become more efficient, and added new MA responsibilities. We trained MAs to assist with documentation in the exam room to ensure that physician time was spent in face-to-face direct patient care.14-20 In these ways, we sought not only to increase patient satisfaction but also to enhance our own “joy in practice,” defined primarily by a high level of work-life satisfaction, a low level of burnout, and a feeling that the medical practice is fulfilling.21
In our traditional model, an MA retrieved the patient from the waiting room, conducted initial assessment in the exam room, and then left the patient to wait for the physician to enter. Once the physician entered and conducted the exam, the patient would be left alone again to wait for the MA to return. In our revised model (TABLE 1), we assigned one MA to each patient from arrival to discharge. After greeting the patient in the waiting room, the MA conducted an initial patient interview in the exam room, then remained in the room with the physician to document the visit. After the physician exited the exam room, the MA completed follow-up orders and provided the patient with a visit summary.
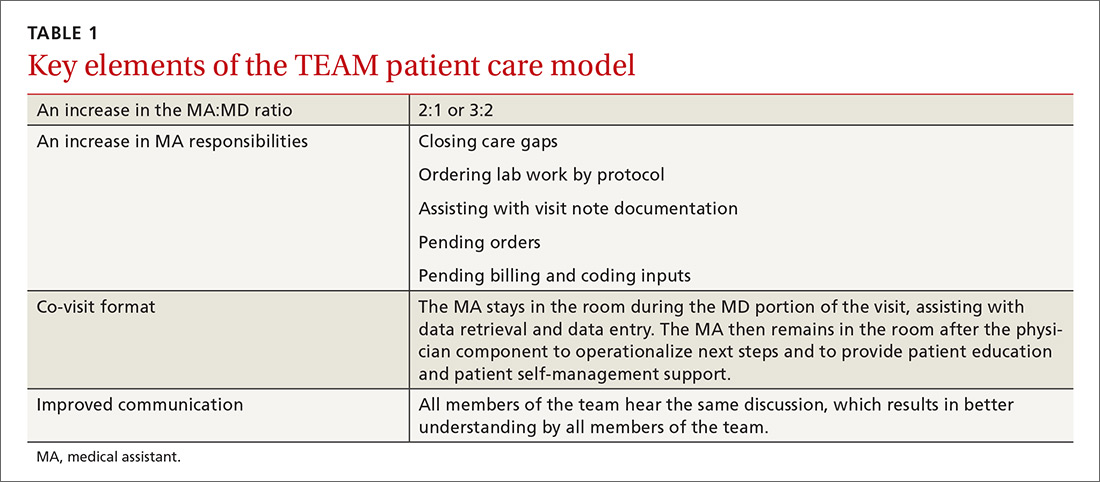
To facilitate consistency throughout the day, we designed a workflow similar to those created in lean models originally designed to increase efficiency in the manufacturing industry (TABLE 2). Visual and electronic cues triggered each step of the process and coordinated the movement of MAs and MDs. Cues included the conventional flag system outside each exam room, an electronic messaging system within the electronic health record (EHR) to indicate when a patient was ready to be seen, and a whiteboard in an area visible to all team members on which we wrote lab and radiology requests.
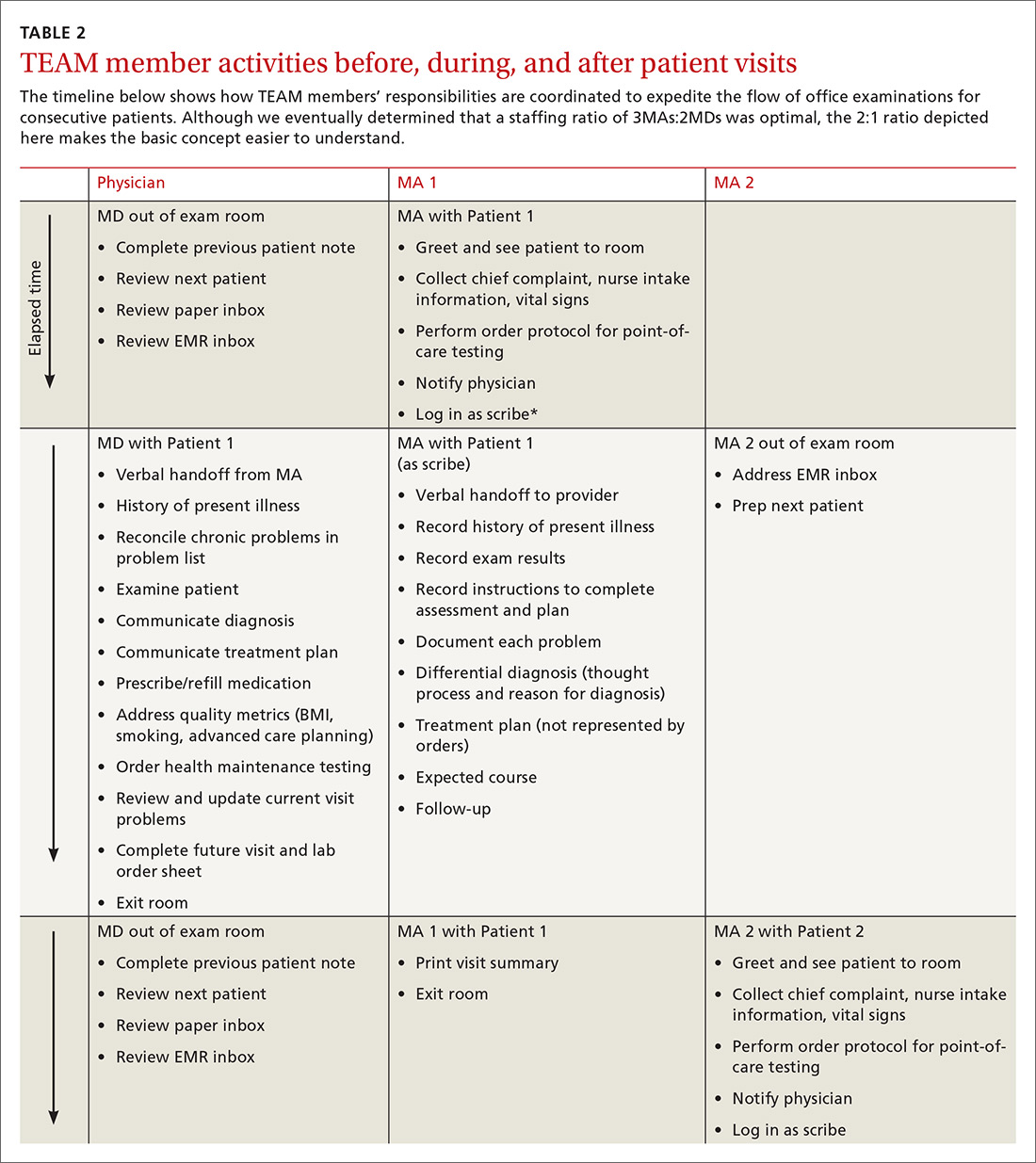
We experimented with the MA:MD ratio to identify the most effective and efficient team composition. On alternating weeks, we assigned one MA to one MD, 2 MAs to one MD, or 3 MAs to 2 MDs. Additionally, with the 2:1 MA:MD ratio, we varied the visit length in 2 tests; one spanning 30 minutes and the other 20 minutes. The MDs and MAs were seated at side-by-side workstations to make communication easier. We developed protocols and checklists that allowed MAs to enter health maintenance orders and conduct point-of-care testing before the physician entered the room. Such details included immunization management, strep screens, urine analyses, diabetic foot exams, extremity x-ray films, and mammogram and colonoscopy referrals.
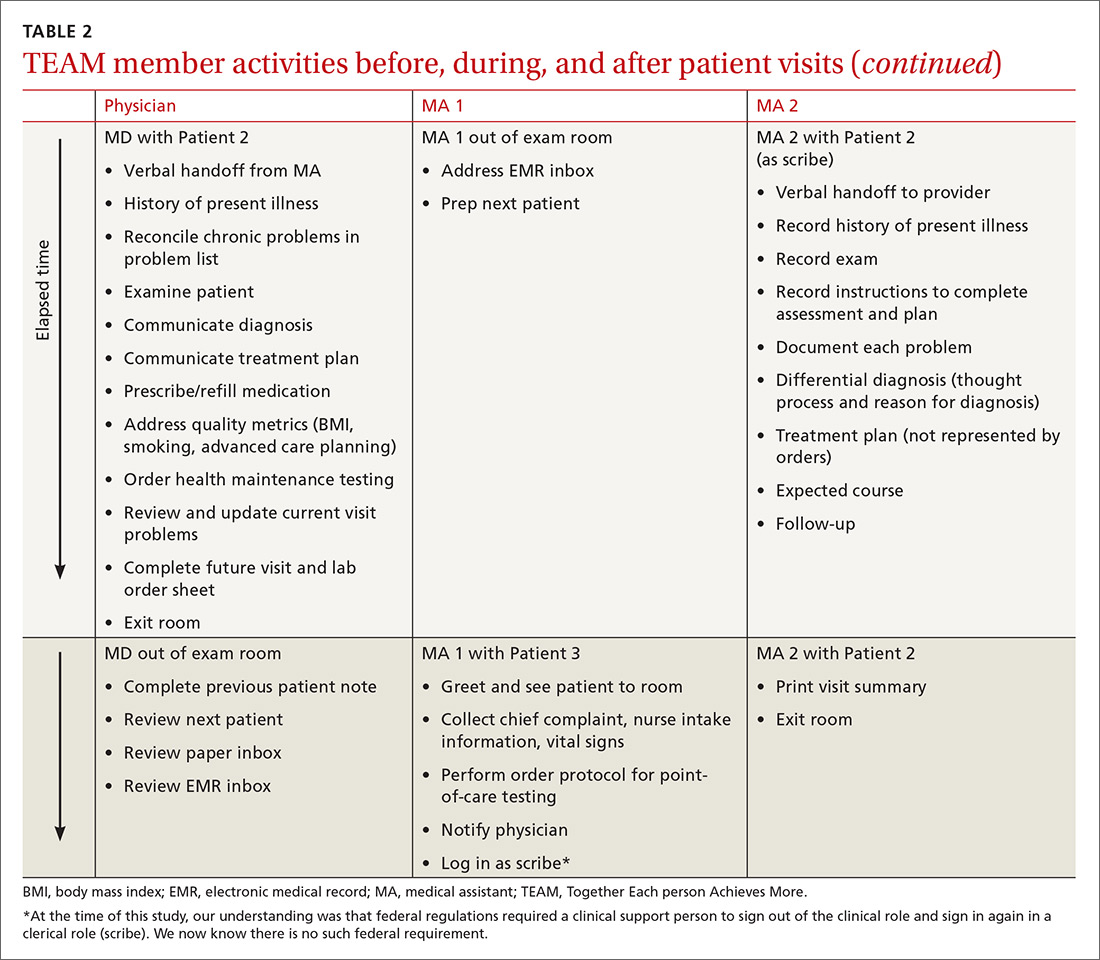
Continue to: To prepare MAs...
To prepare MAs, we obtained special permission for team documentation from our Chief Information Officer and developed associated policies and procedures. A physician assistant (PA) trained each MA, introducing the structure and content of subjective, objective, assessment, and plan (SOAP) notes. Training was continuous, as PAs provided feedback when MAs began team documentation. The MAs documented visits using templates, free form, and quick text. We measured visit cycle-time, face time with staff, and patient waiting times. A process engineer with a stopwatch observed and timed the flow (but did not enter the exam room). We also conducted patient interviews immediately post-visit and administered anonymous questionnaires to clinic staff at different phases of the model. Physicians and MAs met weekly to evaluate the design.
We used qualitative interviews of patients, physicians, and MAs to identify the level of satisfaction with the new model. During the first week of implementation, a nurse and our process engineer conducted brief in-person surveys with approximately 20 post-visit patients. Patients, chosen by convenience, were asked if the visit addressed their concerns, whether they left with a thorough understanding of next steps, and if their wait time was acceptable. Twice during the implementation phase, a human resources associate distributed 9-item anonymous questionnaires to staff members during scheduled department meetings.
RESULTS
Times per activity with different MA:MD ratios and visit lengths are shown in TABLE 3. After 6 months, cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased by a mean of 2 minutes, from 24 to 26 minutes per patient; and wait time decreased by a mean of 7 minutes, from 9 to 2 minutes per patient. We concluded the MA:MD ratio of 3:2 was most efficient because the 2:1 model left MAs with excess non-patient time.
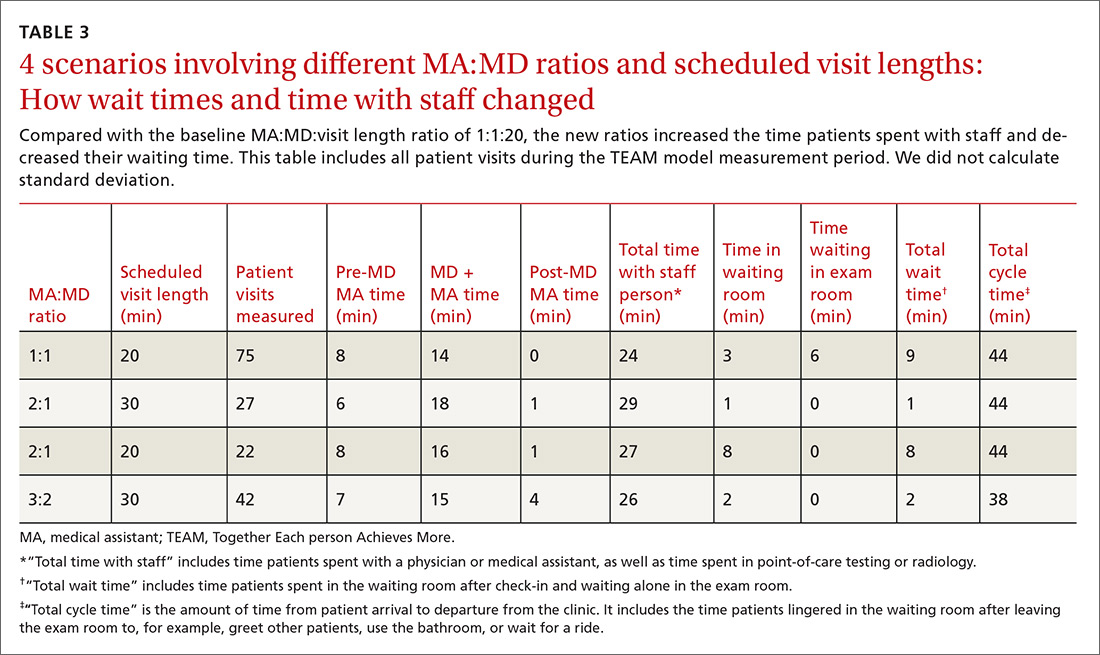
Our delivery model received consistently positive comments from patients. Many expressed gratitude for the extra set of ears and eyes guiding them through the process. One recalled the “old days” when a nurse joined the doctor in the exam room. Another appreciated that both the MA and physician could answer follow-up questions over the phone.
Employee satisfaction
Surveys to assess satisfaction were distributed to all employees whether they were involved in the new model or not. Sixteen employees responded to the pre-implementation questionnaire and 18 responded to the post-implementation one distributed 7 months later. The questionnaires showed an increase in employee satisfaction scores from 3.70 to 3.89 on a 5-point Likert scale, with 5 ranking highest. “I am learning from [Dr. Milford] and understanding things more fully,” wrote one respondent. Another said, “Dr. Milford and his clinical support staff are less stressed.” Individual observations such as, “I can leave sooner with less work left to do,” and “All documentation is done before [the] patient leaves,” reflect the reduction in time that patient records remained open or incomplete. Some physicians reported a reduction in at-home or after-hours work, from about 2 to 4 hours per day to approximately one hour per day.
Continue to: Additional outcomes
Additional outcomes
The TEAM model allowed us to more easily integrate new initiatives into our practice and meet quality metrics by placing needed components within our workflow and checklist. For example, achieving Stage II Meaningful Use measures required that we print and furnish patients with a visit summary and a reminder to access our portal; something we easily incorporated into the MAs’ expanded responsibilities. We also met specific predetermined quality metrics that were part of a payment-withhold program. During the study period, we achieved scores at the 90th percentile and earned back our total withhold.
Finally, more of our patients completed advanced care planning discussions than the other 7 sites in our Honoring Choices Wisconsin cohort. This was achieved not only by integrating the process into our checklist, but because the MAs observed the MD-led patient conversations which they then emulated, presenting the advanced care planning information to patients before or after MD time with the patient.
Errors and defects in care
With ongoing provider guidance and reinforcement, MAs became integral members of the primary care team. They were empowered through protocols to manage and order health maintenance testing and provide needed immunizations. They also began to identify potentially overlooked aspects of care. For example, MAs prompted physicians to retake vital signs, adjust medications, order labs, discuss previous lab results, and pursue specialty referrals or follow-up care.
Billing
Although we tracked billing, the TEAM model was not designed to influence revenue. We noted no significant change in level of evaluation and management billed regardless of staffing ratio. While our panel size increased as we implemented the new process, this change could have been due to normal variation. We do see opportunity to affect future billing by having coders train MAs, which could enhance documentation and increase revenue.
DISCUSSION
The TEAM Primary Care model reduced the time our patients sat unattended, increased our opportunities to meaningfully interact with them, and seemed to reduce our administrative load. By identifying and implementing ways to work as a more cohesive, interconnected unit, we began to address our work as a team rather than as individuals. After implementing the model, we noted several instances where the MAs caught potential errors in care, although we did not consistently track or measure changes in the rate of these occurrences.
Continue to: Achieving these results also came with...
Achieving these results also came with challenges. Investing in and maintaining a new model opened our eyes to unforeseen inconsistencies in our staff profile and to the cost and administrative support needed for implementation. Moreover, our entire team (patients, MAs, and physicians) had to undergo a major cultural shift to adopt a new model.
Personnel variation
We discovered that implementing and sustaining organization change is highly dependent on constancy in human resources. When one team member was on vacation, sick, or leaving the practice, the process tended to fall apart. Hiring replacements and training employees well enough to fill in at a moment’s notice proved difficult. Bringing new employees into this process was also labor intensive. Despite team members being very engaged in change, these staffing inconsistencies caused significant stress and necessitated pauses in the implementation of the new model (reflected in the timeline of our measures). Larger organizational buy-in and support would allow us to hire and train a larger pool of MAs in anticipation of these fluctuations.
Cost
Our small, rural family practice took advantage of WRMC’s Primary Care Transformation project and the half-time process engineer and additional MA they provided. We question whether this model could be implemented without such support. While a process engineer might not prove necessary, expertise in process improvement is vital to help design and measure workflow and to identify opportunities for improvement.
Cultural change
Adopting a new model required asking every member of the team (patient, MA, and physician) to accommodate change and tolerate disruption. We anticipated patients might resist having an additional person in the room. All patients were informed of our new model at the beginning of the visit and told they could opt out. While we did not document patient resistance, JM recalled only 2 patients who expressed a desire not to have the MA present because of personal and sensitive issues. It’s possible some patients did not feel comfortable opting out. But many patients expressed gratitude for having an extra set of ears and eyes to guide them through the visit.
It was more challenging to support MAs as they stepped out of their comfort zone to assist with documentation. It took time for MAs to grow accustomed to the protocols and checklists essential to our workflow. Without protocols, any point-of-care testing that could have been completed at the beginning of the appointment had to be done at the end. This disrupted our workflow and increased patient wait times.
Continue to: We correctly predicted MAs would have...
We correctly predicted MAs would have difficulty documenting the assessment, plan, and medical decision making. We discovered that MAs more easily categorized and articulated information when we reframed the assessment and plan in first-person and placed it under “Patient instructions.” For this to occur, physicians had to learn to accurately articulate their thought process and instructions to the patient.
When training was provided, as previously described, MAs grasped the subjective section quickly. Surprisingly, they had most difficulty understanding terminology within the objective section. In the future, we would avert this problem by working closely with the human resource department. We believe there should be a newly defined position and additional training for MAs in these roles, since duties such as patient-coaching and documentation assistance may warrant separate certification.
Limitations
Our findings should be interpreted in light of several limitations. Implementing the new model was carried out in a single organization. The patients who were selected and agreed to be interviewed may have differed from the patient population as a whole. We did not measure some important outcomes, such as cost effectiveness and patient morbidity. We did not analyze the data to determine whether the apparent improvements in wait time and cycle time were statistically significant. In addition, measurement of any adverse effects was beyond the scope of this study.
Looking forward
The traditional model of physicians working individually with minimal support staff is no longer viable. To echo our co-author (CAS)’s recent statements on physician dissatisfaction, “The days of hero medicine, with the doctor doing it all, belong in the past.”21 The new model appeared to alleviate some administrative burdens and increase physician time with patients. Pressures to achieve quality measures and growing administrative tasks have altered the role and responsibilities of each member of the team.
Any sustainable system must address the larger crisis of physician dissatisfaction.7,22 We cannot focus on a single perspective—patient, physician, or MA—at the expense of the system as a whole. If the health care system is to resolve the epidemic of burnout and physician dissatisfaction, new approaches to patient care must be imagined and realized. Although we faced many challenges in implementing and evaluating the TEAM model, attempts to overcome these challenges appear justified because of our overall favorable impression of it. Innovations like the TEAM Primary Care model may help us improve the well-being of not just our patients but also our health professionals and the health care industry as a whole.
CORRESPONDENCE
James Milford, MD, Three Oaks Health, S.C., 480 Village Walk Lane, Suite F, Johnson Creek, WI 53038; jam@threeoakshealthcare.com.
SUPPORT
Although the Watertown Regional Medical Center has provided general funding for its Primary Care Transformation project, no dollars were specifically earmarked for the TEAM Primary Care process. Support for editorial services in preparing this article was provided by Dr. James Milford.
PRIOR PRESENTATIONS
Co-author Michael R. Strasser, MPA, presented this project at the 2015 i-PrACTISE conference in Madison, Wis, April 12-14, 2015. http://www.fammed.wisc.edu/i-practise/. The proceedings were not published or recorded.
ACKNOWLEDGMENT
We thank Annalynn Skipper and Masarah Van Eyck for their valuable edits.
ABSTRACT
Purpose In 2013-14, 2 clinics in the Watertown Regional Medical Center (WRMC; in southern Wisconsin) launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” as part of a quality improvement project to enhance the delivery experience for the patient, physician, and medical assistant (MA). New work flows, roles, and responsibilities were designed to reduce cycle time, increase patient time with physicians and staff, and reduce patient wait times.
Methods The new model increased the ratio of MAs to physicians from a baseline MA:MD ratio of 1:1 to 3:2, and trained MAs to assume expanded roles during exam-room entry and discharge, including assisting with documentation during the patient visit. A process engineer timed patient visits. The process engineer and a human resources associate conducted surveys to assess the level of satisfaction for patients, physicians, and MAs.
Results Cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased a mean of 2 minutes, from 24 to 26 minutes per patient; and waiting time decreased from 9 to 2 minutes per patient. Qualitative interviews with patients, physicians, and MAs identified a high level of satisfaction with the new model.
Conclusion The higher staffing ratios and expanded roles for MAs in the new model improved workflow, increased the face time between patients and their physician and MA, and decreased patient wait times. The TEAM model also appeared to improve patient, physician, and MA satisfaction. We faced many challenges while implementing the new model, which could be further evaluated during wide adoption.
In recent years, we observed that our physicians, nurses, and medical assistants (MAs) appeared to be spending more time on administrative and clerical tasks—including tasks in the exam room with the patient—and less time engaged in direct patient care.1,2 We recognized these factors contribute to burnout and threaten staff retention and anticipated that a new model would improve physician time spent in direct patient care, decrease the demands of administrative tasks, and increase patient, physician, and MA satisfaction.3-6 Burnout, known to affect more than half of US physicians, has a negative impact on quality of care and patient safety and satisfaction.7-11 Improving workflow has been shown to reduce burnout.12
Watertown Regional Medical Center (WRMC) is a small, financially stable integrated delivery system in rural southern Wisconsin, composed of a 90-bed hospital, 10 primary care clinics (7 owned and 3 affiliated), and 24 employed physicians in 9 specialties. Two clinics within WRMC launched a new delivery model, “TEAM (Together Each person Achieves More) Primary Care,” to improve the delivery experience for the entire team, defined as the patient, physician, and MA. New workflows, roles, and responsibilities were designed to reduce cycle time (the total amount of time patients spent in the clinic from check-in to check-out), increase the total time a patient spent with staff (physician and MA or in point-of-care testing and radiology), and reduce the total time a patient spent waiting.13
We describe here WRMC’s experience in developing and implementing workflow improvements as a means of reducing burnout and improving satisfaction.
Continue to: METHODS
METHODS
We selected 2 WRMC sites for TEAM re-engineering based on their experience with quality-improvement projects and perceived likelihood of success with a new transformation initiative. In early 2013, WRMC charged one physician (JM), 2 MAs, the clinic scheduler, and the clinic administrator with designing the details of the model including evaluation metrics. WRMC provided a .5 FTE process engineer (MS) to assist with the design and implementation of the model at no extra expense to the clinics. The model was implemented in late 2013 and into 2014 after regular TEAM planning meetings and observational visits to non-WRMC sites identified as examples of best practices in improving outpatient primary care patient satisfaction: Bellin Health (Green Bay, Wis); ThedaCare (Appleton, Wis); the University of Utah (Salt Lake City); and the University of Wisconsin Health Yahara Clinic (Madison, Wis).
TEAM model
The TEAM model—so named to create top-of-mind awareness of its benefits—increased the MA:MD ratio, maintained consistent team composition so that physician/MA teams learned to work together and become more efficient, and added new MA responsibilities. We trained MAs to assist with documentation in the exam room to ensure that physician time was spent in face-to-face direct patient care.14-20 In these ways, we sought not only to increase patient satisfaction but also to enhance our own “joy in practice,” defined primarily by a high level of work-life satisfaction, a low level of burnout, and a feeling that the medical practice is fulfilling.21
In our traditional model, an MA retrieved the patient from the waiting room, conducted initial assessment in the exam room, and then left the patient to wait for the physician to enter. Once the physician entered and conducted the exam, the patient would be left alone again to wait for the MA to return. In our revised model (TABLE 1), we assigned one MA to each patient from arrival to discharge. After greeting the patient in the waiting room, the MA conducted an initial patient interview in the exam room, then remained in the room with the physician to document the visit. After the physician exited the exam room, the MA completed follow-up orders and provided the patient with a visit summary.
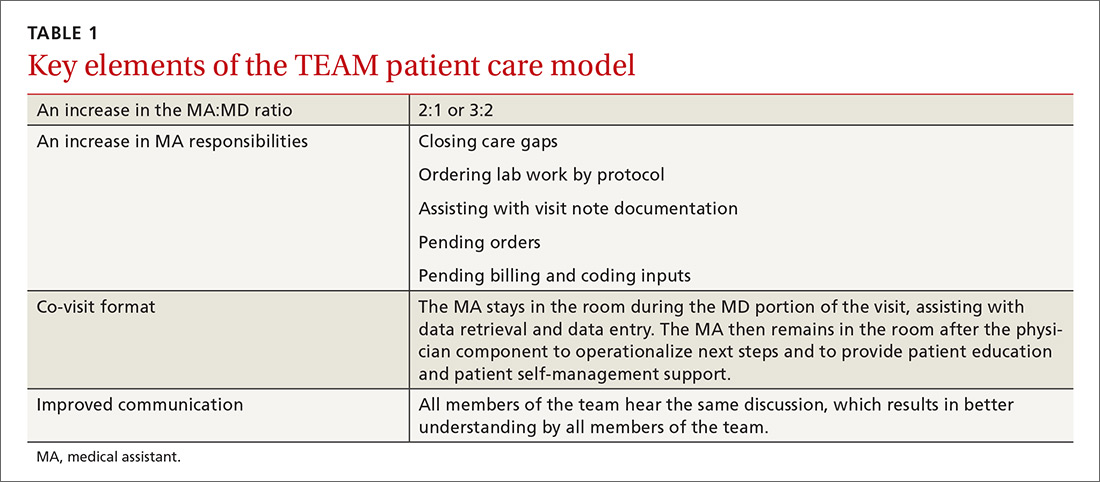
To facilitate consistency throughout the day, we designed a workflow similar to those created in lean models originally designed to increase efficiency in the manufacturing industry (TABLE 2). Visual and electronic cues triggered each step of the process and coordinated the movement of MAs and MDs. Cues included the conventional flag system outside each exam room, an electronic messaging system within the electronic health record (EHR) to indicate when a patient was ready to be seen, and a whiteboard in an area visible to all team members on which we wrote lab and radiology requests.
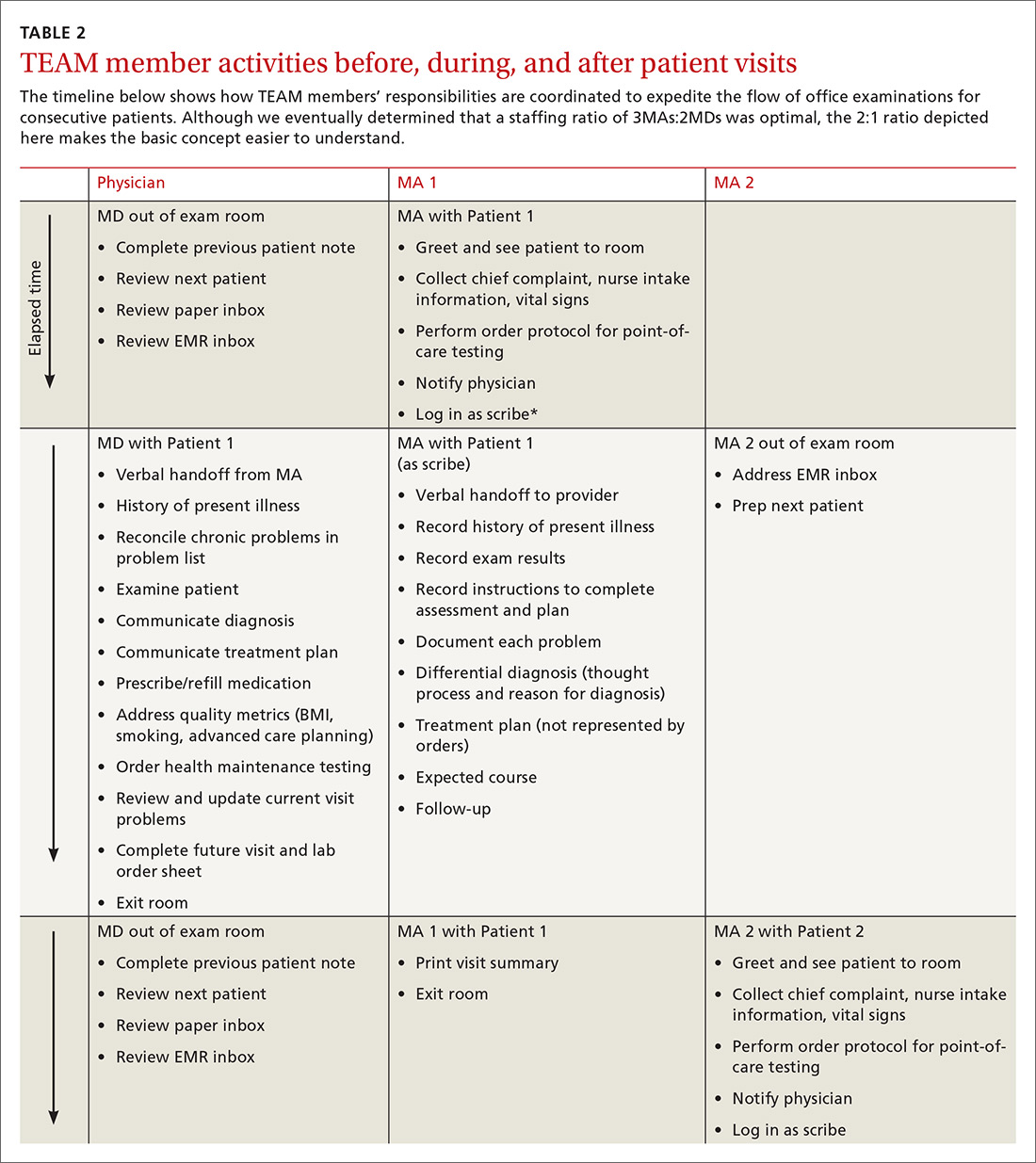
We experimented with the MA:MD ratio to identify the most effective and efficient team composition. On alternating weeks, we assigned one MA to one MD, 2 MAs to one MD, or 3 MAs to 2 MDs. Additionally, with the 2:1 MA:MD ratio, we varied the visit length in 2 tests; one spanning 30 minutes and the other 20 minutes. The MDs and MAs were seated at side-by-side workstations to make communication easier. We developed protocols and checklists that allowed MAs to enter health maintenance orders and conduct point-of-care testing before the physician entered the room. Such details included immunization management, strep screens, urine analyses, diabetic foot exams, extremity x-ray films, and mammogram and colonoscopy referrals.
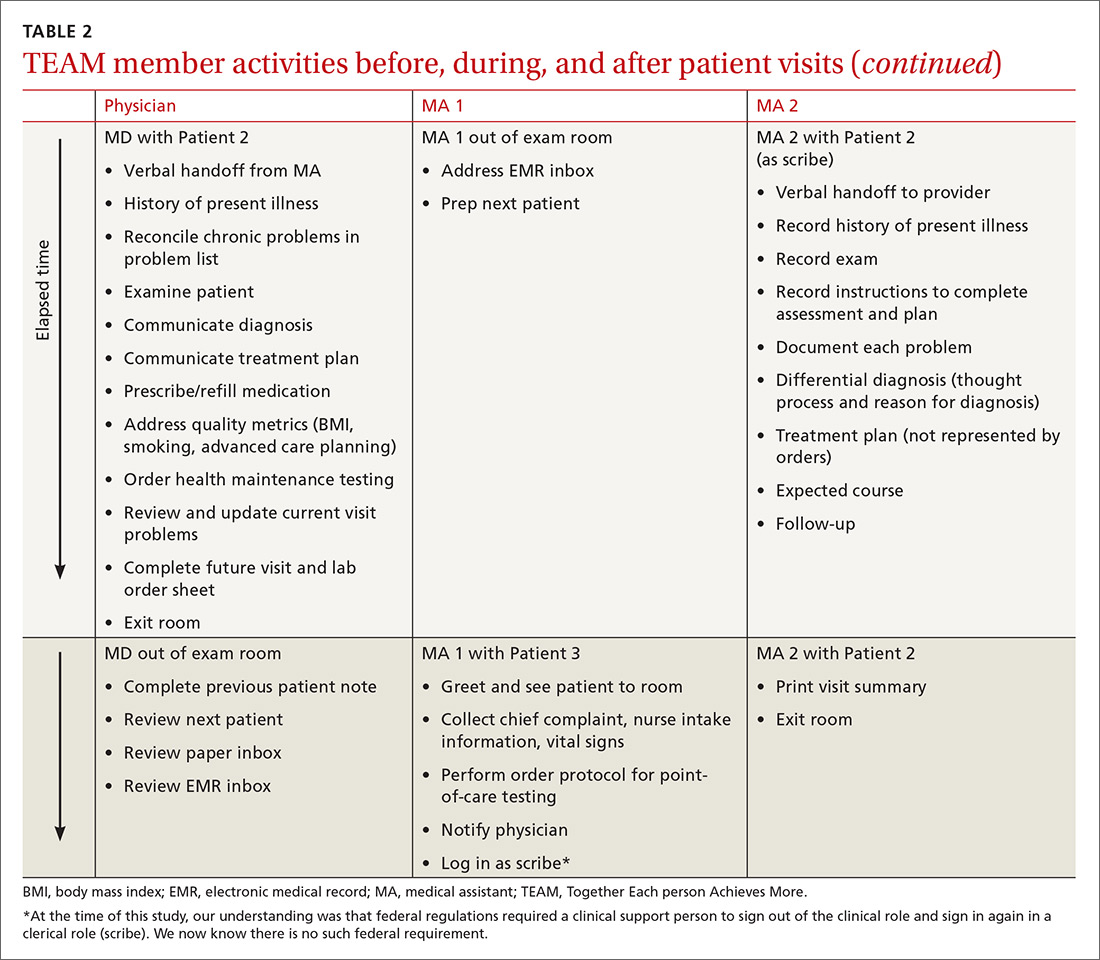
Continue to: To prepare MAs...
To prepare MAs, we obtained special permission for team documentation from our Chief Information Officer and developed associated policies and procedures. A physician assistant (PA) trained each MA, introducing the structure and content of subjective, objective, assessment, and plan (SOAP) notes. Training was continuous, as PAs provided feedback when MAs began team documentation. The MAs documented visits using templates, free form, and quick text. We measured visit cycle-time, face time with staff, and patient waiting times. A process engineer with a stopwatch observed and timed the flow (but did not enter the exam room). We also conducted patient interviews immediately post-visit and administered anonymous questionnaires to clinic staff at different phases of the model. Physicians and MAs met weekly to evaluate the design.
We used qualitative interviews of patients, physicians, and MAs to identify the level of satisfaction with the new model. During the first week of implementation, a nurse and our process engineer conducted brief in-person surveys with approximately 20 post-visit patients. Patients, chosen by convenience, were asked if the visit addressed their concerns, whether they left with a thorough understanding of next steps, and if their wait time was acceptable. Twice during the implementation phase, a human resources associate distributed 9-item anonymous questionnaires to staff members during scheduled department meetings.
RESULTS
Times per activity with different MA:MD ratios and visit lengths are shown in TABLE 3. After 6 months, cycle time decreased by a mean of 6 minutes, from 44 to 38 minutes per patient; time with staff increased by a mean of 2 minutes, from 24 to 26 minutes per patient; and wait time decreased by a mean of 7 minutes, from 9 to 2 minutes per patient. We concluded the MA:MD ratio of 3:2 was most efficient because the 2:1 model left MAs with excess non-patient time.
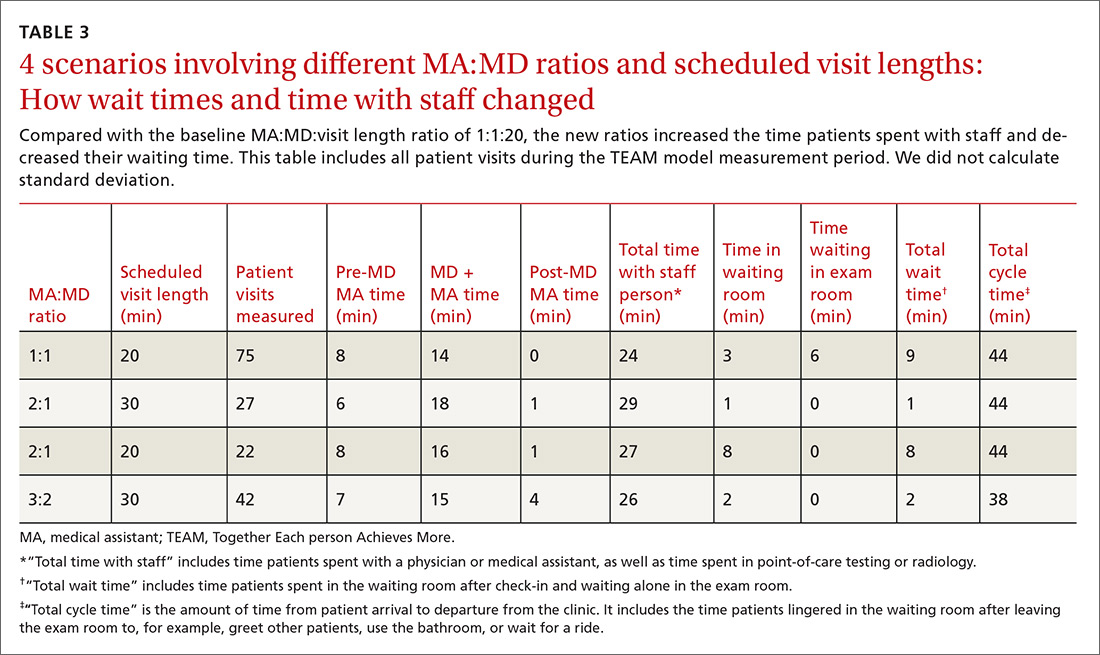
Our delivery model received consistently positive comments from patients. Many expressed gratitude for the extra set of ears and eyes guiding them through the process. One recalled the “old days” when a nurse joined the doctor in the exam room. Another appreciated that both the MA and physician could answer follow-up questions over the phone.
Employee satisfaction
Surveys to assess satisfaction were distributed to all employees whether they were involved in the new model or not. Sixteen employees responded to the pre-implementation questionnaire and 18 responded to the post-implementation one distributed 7 months later. The questionnaires showed an increase in employee satisfaction scores from 3.70 to 3.89 on a 5-point Likert scale, with 5 ranking highest. “I am learning from [Dr. Milford] and understanding things more fully,” wrote one respondent. Another said, “Dr. Milford and his clinical support staff are less stressed.” Individual observations such as, “I can leave sooner with less work left to do,” and “All documentation is done before [the] patient leaves,” reflect the reduction in time that patient records remained open or incomplete. Some physicians reported a reduction in at-home or after-hours work, from about 2 to 4 hours per day to approximately one hour per day.
Continue to: Additional outcomes
Additional outcomes
The TEAM model allowed us to more easily integrate new initiatives into our practice and meet quality metrics by placing needed components within our workflow and checklist. For example, achieving Stage II Meaningful Use measures required that we print and furnish patients with a visit summary and a reminder to access our portal; something we easily incorporated into the MAs’ expanded responsibilities. We also met specific predetermined quality metrics that were part of a payment-withhold program. During the study period, we achieved scores at the 90th percentile and earned back our total withhold.
Finally, more of our patients completed advanced care planning discussions than the other 7 sites in our Honoring Choices Wisconsin cohort. This was achieved not only by integrating the process into our checklist, but because the MAs observed the MD-led patient conversations which they then emulated, presenting the advanced care planning information to patients before or after MD time with the patient.
Errors and defects in care
With ongoing provider guidance and reinforcement, MAs became integral members of the primary care team. They were empowered through protocols to manage and order health maintenance testing and provide needed immunizations. They also began to identify potentially overlooked aspects of care. For example, MAs prompted physicians to retake vital signs, adjust medications, order labs, discuss previous lab results, and pursue specialty referrals or follow-up care.
Billing
Although we tracked billing, the TEAM model was not designed to influence revenue. We noted no significant change in level of evaluation and management billed regardless of staffing ratio. While our panel size increased as we implemented the new process, this change could have been due to normal variation. We do see opportunity to affect future billing by having coders train MAs, which could enhance documentation and increase revenue.
DISCUSSION
The TEAM Primary Care model reduced the time our patients sat unattended, increased our opportunities to meaningfully interact with them, and seemed to reduce our administrative load. By identifying and implementing ways to work as a more cohesive, interconnected unit, we began to address our work as a team rather than as individuals. After implementing the model, we noted several instances where the MAs caught potential errors in care, although we did not consistently track or measure changes in the rate of these occurrences.
Continue to: Achieving these results also came with...
Achieving these results also came with challenges. Investing in and maintaining a new model opened our eyes to unforeseen inconsistencies in our staff profile and to the cost and administrative support needed for implementation. Moreover, our entire team (patients, MAs, and physicians) had to undergo a major cultural shift to adopt a new model.
Personnel variation
We discovered that implementing and sustaining organization change is highly dependent on constancy in human resources. When one team member was on vacation, sick, or leaving the practice, the process tended to fall apart. Hiring replacements and training employees well enough to fill in at a moment’s notice proved difficult. Bringing new employees into this process was also labor intensive. Despite team members being very engaged in change, these staffing inconsistencies caused significant stress and necessitated pauses in the implementation of the new model (reflected in the timeline of our measures). Larger organizational buy-in and support would allow us to hire and train a larger pool of MAs in anticipation of these fluctuations.
Cost
Our small, rural family practice took advantage of WRMC’s Primary Care Transformation project and the half-time process engineer and additional MA they provided. We question whether this model could be implemented without such support. While a process engineer might not prove necessary, expertise in process improvement is vital to help design and measure workflow and to identify opportunities for improvement.
Cultural change
Adopting a new model required asking every member of the team (patient, MA, and physician) to accommodate change and tolerate disruption. We anticipated patients might resist having an additional person in the room. All patients were informed of our new model at the beginning of the visit and told they could opt out. While we did not document patient resistance, JM recalled only 2 patients who expressed a desire not to have the MA present because of personal and sensitive issues. It’s possible some patients did not feel comfortable opting out. But many patients expressed gratitude for having an extra set of ears and eyes to guide them through the visit.
It was more challenging to support MAs as they stepped out of their comfort zone to assist with documentation. It took time for MAs to grow accustomed to the protocols and checklists essential to our workflow. Without protocols, any point-of-care testing that could have been completed at the beginning of the appointment had to be done at the end. This disrupted our workflow and increased patient wait times.
Continue to: We correctly predicted MAs would have...
We correctly predicted MAs would have difficulty documenting the assessment, plan, and medical decision making. We discovered that MAs more easily categorized and articulated information when we reframed the assessment and plan in first-person and placed it under “Patient instructions.” For this to occur, physicians had to learn to accurately articulate their thought process and instructions to the patient.
When training was provided, as previously described, MAs grasped the subjective section quickly. Surprisingly, they had most difficulty understanding terminology within the objective section. In the future, we would avert this problem by working closely with the human resource department. We believe there should be a newly defined position and additional training for MAs in these roles, since duties such as patient-coaching and documentation assistance may warrant separate certification.
Limitations
Our findings should be interpreted in light of several limitations. Implementing the new model was carried out in a single organization. The patients who were selected and agreed to be interviewed may have differed from the patient population as a whole. We did not measure some important outcomes, such as cost effectiveness and patient morbidity. We did not analyze the data to determine whether the apparent improvements in wait time and cycle time were statistically significant. In addition, measurement of any adverse effects was beyond the scope of this study.
Looking forward
The traditional model of physicians working individually with minimal support staff is no longer viable. To echo our co-author (CAS)’s recent statements on physician dissatisfaction, “The days of hero medicine, with the doctor doing it all, belong in the past.”21 The new model appeared to alleviate some administrative burdens and increase physician time with patients. Pressures to achieve quality measures and growing administrative tasks have altered the role and responsibilities of each member of the team.
Any sustainable system must address the larger crisis of physician dissatisfaction.7,22 We cannot focus on a single perspective—patient, physician, or MA—at the expense of the system as a whole. If the health care system is to resolve the epidemic of burnout and physician dissatisfaction, new approaches to patient care must be imagined and realized. Although we faced many challenges in implementing and evaluating the TEAM model, attempts to overcome these challenges appear justified because of our overall favorable impression of it. Innovations like the TEAM Primary Care model may help us improve the well-being of not just our patients but also our health professionals and the health care industry as a whole.
CORRESPONDENCE
James Milford, MD, Three Oaks Health, S.C., 480 Village Walk Lane, Suite F, Johnson Creek, WI 53038; jam@threeoakshealthcare.com.
SUPPORT
Although the Watertown Regional Medical Center has provided general funding for its Primary Care Transformation project, no dollars were specifically earmarked for the TEAM Primary Care process. Support for editorial services in preparing this article was provided by Dr. James Milford.
PRIOR PRESENTATIONS
Co-author Michael R. Strasser, MPA, presented this project at the 2015 i-PrACTISE conference in Madison, Wis, April 12-14, 2015. http://www.fammed.wisc.edu/i-practise/. The proceedings were not published or recorded.
ACKNOWLEDGMENT
We thank Annalynn Skipper and Masarah Van Eyck for their valuable edits.
1. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
2. McDonald CJ, Callaghan FM, Weissman A, et al. Use of internist’s free time by ambulatory care electronic medical record systems. JAMA Intern Med. 2014;174:1860-1863.
3. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
4. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Available at: http://www.rand.org/pubs/research_reports/RR439.html#key-findings. Accessed October 25, 2016.
5. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc. 2014;21:e100-e106.
6. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. 2001.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proc. 2015;90:1600-1613.
8. DeMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychol. 1993;12:93-102.
9. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358-367.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122-128.
12. Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30:1105-1011.
13. Ferrer RL, Mody-Bailey P, Jaén CR, et al. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7:504-512.
14. Sinsky CA, Williard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
15. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
16. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
17. Yan C, Rose S, Rothberg MB, et al. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2016;31:990-995.
18. Misra-Hebert AD, Rabovsky A, Yan C, et al. A team-based model of primary care delivery and physician-patient interaction. Am J Med. 2015;128:1025-1028.
19. Anderson RJ. Optimizing the role of nursing staff to enhance physician productivity: one physician’s journey. Fam Pract Manag. 2013;20:18-22.
20. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008:15:35-40.
21. Sinsky CA. Dissatisfaction among Wisconsin physicians is part of a serious national trend. Wis Med J. 2015;114:132-133.
22. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
1. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-760.
2. McDonald CJ, Callaghan FM, Weissman A, et al. Use of internist’s free time by ambulatory care electronic medical record systems. JAMA Intern Med. 2014;174:1860-1863.
3. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-848.
4. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Available at: http://www.rand.org/pubs/research_reports/RR439.html#key-findings. Accessed October 25, 2016.
5. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc. 2014;21:e100-e106.
6. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. 2001.
7. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proc. 2015;90:1600-1613.
8. DeMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychol. 1993;12:93-102.
9. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358-367.
10. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995-1000.
11. Haas JS, Cook EF, Puopolo AL, et al. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122-128.
12. Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30:1105-1011.
13. Ferrer RL, Mody-Bailey P, Jaén CR, et al. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7:504-512.
14. Sinsky CA, Williard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11:272-278.
15. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med. 2014;174:1190-1193.
16. Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21:23-29.
17. Yan C, Rose S, Rothberg MB, et al. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med. 2016;31:990-995.
18. Misra-Hebert AD, Rabovsky A, Yan C, et al. A team-based model of primary care delivery and physician-patient interaction. Am J Med. 2015;128:1025-1028.
19. Anderson RJ. Optimizing the role of nursing staff to enhance physician productivity: one physician’s journey. Fam Pract Manag. 2013;20:18-22.
20. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008:15:35-40.
21. Sinsky CA. Dissatisfaction among Wisconsin physicians is part of a serious national trend. Wis Med J. 2015;114:132-133.
22. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576.
EMR notes should communicate and educate
To the Editor: Dr. Venkat1 was spot on when he identified the need for electronic medical records to communicate and educate, rather than document. Short and actionable notes are best. But with the focus on billing and compliance, annotated, informative assessments are actually discouraged. Our billing and coding department performs periodic chart audits and considers the note “out of compliance” if there is a difference between the list of free text assessments and the International Classification of Diseases, Ninth Revision (ICD-9) codes chosen. Therefore, many physicians just use the billing codes as their assessment and skip the free text assessment section of a SOAP (subjective-objective-assessment-plan) note, which means the notes convey even less of what the physician is thinking. A classic example is the note of a patient whom I knew had pernio, yet the assessment blandly reported “circulatory disorder.” The plan likewise is often reduced to the imported structured text of the tests and medications ordered rather than a rich discussion of the differential diagnosis and medical reasoning.
Imagine the notes we might write if their primary purpose was communication to ourselves and the others involved in our patients’ care. Imagine if the notes made us more knowledgeable about the uniqueness of this particular patient and also contributed to a continuous learning environment. More meaning, less filler. The notes would be shorter and sweeter, as Dr. Venkat suggested.
- Venkat KK. Short and sweet: writing better consult notes in the era of the electronic medical record. Cleve Clin J Med 2015; 82:13–17.
To the Editor: Dr. Venkat1 was spot on when he identified the need for electronic medical records to communicate and educate, rather than document. Short and actionable notes are best. But with the focus on billing and compliance, annotated, informative assessments are actually discouraged. Our billing and coding department performs periodic chart audits and considers the note “out of compliance” if there is a difference between the list of free text assessments and the International Classification of Diseases, Ninth Revision (ICD-9) codes chosen. Therefore, many physicians just use the billing codes as their assessment and skip the free text assessment section of a SOAP (subjective-objective-assessment-plan) note, which means the notes convey even less of what the physician is thinking. A classic example is the note of a patient whom I knew had pernio, yet the assessment blandly reported “circulatory disorder.” The plan likewise is often reduced to the imported structured text of the tests and medications ordered rather than a rich discussion of the differential diagnosis and medical reasoning.
Imagine the notes we might write if their primary purpose was communication to ourselves and the others involved in our patients’ care. Imagine if the notes made us more knowledgeable about the uniqueness of this particular patient and also contributed to a continuous learning environment. More meaning, less filler. The notes would be shorter and sweeter, as Dr. Venkat suggested.
To the Editor: Dr. Venkat1 was spot on when he identified the need for electronic medical records to communicate and educate, rather than document. Short and actionable notes are best. But with the focus on billing and compliance, annotated, informative assessments are actually discouraged. Our billing and coding department performs periodic chart audits and considers the note “out of compliance” if there is a difference between the list of free text assessments and the International Classification of Diseases, Ninth Revision (ICD-9) codes chosen. Therefore, many physicians just use the billing codes as their assessment and skip the free text assessment section of a SOAP (subjective-objective-assessment-plan) note, which means the notes convey even less of what the physician is thinking. A classic example is the note of a patient whom I knew had pernio, yet the assessment blandly reported “circulatory disorder.” The plan likewise is often reduced to the imported structured text of the tests and medications ordered rather than a rich discussion of the differential diagnosis and medical reasoning.
Imagine the notes we might write if their primary purpose was communication to ourselves and the others involved in our patients’ care. Imagine if the notes made us more knowledgeable about the uniqueness of this particular patient and also contributed to a continuous learning environment. More meaning, less filler. The notes would be shorter and sweeter, as Dr. Venkat suggested.
- Venkat KK. Short and sweet: writing better consult notes in the era of the electronic medical record. Cleve Clin J Med 2015; 82:13–17.
- Venkat KK. Short and sweet: writing better consult notes in the era of the electronic medical record. Cleve Clin J Med 2015; 82:13–17.

