User login
Judge dismisses doctors’ lawsuit against ABIM
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
A district court has dismissed a lawsuit levied by a group of physicians against the American Board of Internal Medicine (ABIM) over its maintenance of certification (MOC) program, calling the legal challenge “flawed.”
In a Sept. 26 decision, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim, the judge ruled.
“We disagree with plaintiffs and find that ABIM’s initial certification and MOC products are part of a single product and do not occupy distinct markets,” Judge Kelly wrote in his decision. “Not only are we unconvinced by plaintiffs’ arguments, we find that plaintiffs’ entire framing of the ABIM certification to be flawed. In essence, plaintiffs are arguing that, in order to purchase ABIM’s initial certification, internists are forced to purchase MOC products as well. However, this is not the case. ... Nowhere in the amended complaint do plaintiffs allege that they were forced to buy MOC products in order to purchase the initial certification.”
The judge dismissed the suit, but allowed the plaintiffs 14 days to submit an amended complaint reoutlining their claims of illegal monopolization and racketeering against the board. If the amended complaint passes legal muster, the judge could revive those claims.
ABIM President Richard J. Baron, MD, expressed satisfaction that the court granted the board’s motion to dismiss the case for failure to state a valid claim.
“ABIM is pleased that the United States District Court for the Eastern District of Pennsylvania dismissed in its entirety a lawsuit that alleged physicians were harmed by the requirements for maintaining ABIM board certification,” Dr. Baron said in a statement.
C. Philip Curley, a Chicago-based attorney for the physician plaintiffs, said the case is far from over.
“The four internists who brought the lawsuit were invited to file amended claims, which is certainly being considered,” Mr. Curley said in an interview. “If necessary, all available appeals will also be pursued to the fullest. No one was under the impression that the fight to bring MOC to an end would be quick or easy.”
The original lawsuit, filed Dec. 6, 2018, in a Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims.
The four plaintiff-physicians want the court to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing. A fourth lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology was filed in February.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America are funding the plaintiffs’ legal efforts through a fundraising campaign that has raised more than $300,000.
In an interview, Dr. Fisher called the legal fight against ABIM “a David versus Goliath effort” and said the battle will continue.
“The ABIM may have won this first round, but ... they have only dodged the antitrust tying claim and unjust enrichment claims,” Dr. Fisher said. “The monopoly claim and racketeering claims are still very much open. Plaintiffs have 14 days to amend their compliant.”
Legislators disagree on new drug-pricing proposal
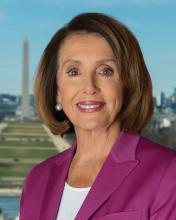
Legislators sparred about the best way to lower drug prices during a Sept. 25 hearing, bickering along partisan lines over new legislation by U.S. House Speaker Nancy Pelosi, (D-Calif.) that would require Medicare to negotiate drug prices with manufacturers.
The more than 4-hour hearing by the House Committee on Energy & Commerce Subcommittee on Health centered on HR 3, the “Lower Drug Costs Now Act of 2019,” introduced by Speaker Pelosi on Sept. 24, which would compel the Centers for Medicare & Medicaid Services to make deals with manufacturers on the maximum, reasonable price for the top 250 highest-cost drugs. If a drug maker refused to participate in the negotiation, the company would face a steep noncompliance fee, according to the bill, while manufacturers that overcharged Medicare or failed to offer the negotiated price would be subject to a civil penalty equal to 10 times the cost difference. The legislation includes a $2,000 out-of-pocket limit for Medicare patients.
If enacted, the legislation would transform the pricing landscape of medications and allow more families to access needed treatments, Speaker Pelosi said during the hearing.
“What it does, as you know; it ends the ban – imagine, there’s a ban on negotiating for lower drug prices,” she said. “So, it ends the ban for the [U.S. Department of Health and Human Services] Secretary now to have the opportunity to negotiate for lower prices. But, the even better news is that these drug prices will be lower not just for Medicare recipients, which was one of the original proposals, but for everyone. It will stop companies from ripping us off by charging five times, four times, three times what is charged in other countries.”
However, Republican legislators spent much of the hearing criticizing the bill, claiming the legislation was crafted behind closed doors by Democrats who made no efforts to gain Republican feedback.
“There is no debate that Republicans and Democrats want to work together to lower drug cost for consumers,” Ranking Member Greg Walden (R-Ore.) said during the hearing. “Madam chair, I have to strongly express my great frustration about the decision to sabotage both the tradition of this committee and the bipartisan work that you know was well underway to tackle high-cost drugs. ... We’ve worked in a bipartisan way up until now. I thought we were headed in a good faith down that same path until the speaker’s office dropped this partisan plan on our [progress]. This is partisan politics at its worst, and it’s an avoidable failure.”
Amid the partisan squabbling, legislators heard differing views from economists about the logistics of the legislation and whether the pricing negotiation model makes sense for the United States.
Gerard F. Anderson, PhD, a professor at Johns Hopkins University and director of the Johns Hopkins Center for Hospital Finance and Management in Baltimore told congressional leaders that negotiation between the government and drug makers is both possible and results in lower prices, even for drugs without therapeutic competition. He noted that the Medicaid program currently negotiates prices for supplemental rebates and that the Veterans Administration and the Department of Defense routinely negotiate discounts greater than the federal supply schedule. Dr. Anderson estimated that the Veterans Administration and the Department of Defense pay an average of 30%-40% less than Medicare prescription drug plans for the same medications.
“Allowing the federal government to negotiate prices for expensive drugs without competition in both the public and private sectors will be more effective in lowering drug prices for everyone,” Dr. Anderson said during testimony. “ Imposing financial penalties for drug companies will bring them to the table. International prices can be used to determine if the drug company is negotiating in good faith.”
But Benedic Ippolito, PhD, a research fellow for the American Enterprise Institute, Washington, raised concerns the legislation may cause reduced innovation. He said the United States accounts for about 60% of drug spending in the developed world, and that, because the market is so large, changes in spending will have first-order implications for the types of future drugs available, Dr. Ippolito said during testimony.
“Consider the incentives associated with the [bill’s] negotiation process,” he said. “Drugs that have no competitors would be subject to aggressive rate regulation by the [HHS] Secretary. The same is not true of drugs with at least one such competitor. It is entirely possible that being a second market entrant could prove substantially more profitable than bringing a novel therapeutic to market. Thus, the proposal could substantially depress incentives to pursue path-breaking drugs.”
Outside the hearing, Speaker Pelosi’s proposed bill is being praised by some physician groups, including the American College of Physicians. In a statement, ACP President Robert McLean, MD, said the college was pleased that the bill focuses on keeping drugs affordable for patients and includes provisions that would support research into new therapies and treatment options.
“ACP specifically supports the provisions that would allow Medicare to negotiate prices with manufacturers,” Dr. McLean said in the statement. “The College has longstanding policy supporting the ability of Medicare to leverage its purchasing power and directly negotiate with manufacturers for drug prices. Although ACP does not have policy on several of the specific provisions in the bill, we are supportive of its overall goals and direction, particularly the emphasis on negotiation and transparency in drug pricing.
Meanwhile, Senate Finance Chairman Charles E. Grassley, (R-Iowa) and Ranking Member Ron Wyden (D-Ore.) released the statutory text of their own drug-pricing legislation on Sept. 25, titled “the Prescription Drug Pricing Reduction Act of 2019 (S-2543).” The bill calls for a number of changes to the Medicare Part D program, such as reduced beneficiary cost sharing and linking drug price increases to the rate of inflation. The legislation would also make more information available regarding pharmacy benefit manager practices and change how Medicare calculates Part B prescription drug payment amounts to lower spending and out-of-pocket costs for patients.
“President Trump has called on Congress to work together on a bipartisan bill to lower prescription drug prices, [and] there’s only one bipartisan bill in Congress to lower prescription drug prices that’s passed the committee process,” Chairman Grassley said in a statement. “This is it. Making prescription drugs more affordable consistently ranks as a top issue for Americans from every corner of the country. I encourage my colleagues on both sides of the aisle to come to the table and work with us to get a bill passed and signed into law.”
Legislators sparred about the best way to lower drug prices during a Sept. 25 hearing, bickering along partisan lines over new legislation by U.S. House Speaker Nancy Pelosi, (D-Calif.) that would require Medicare to negotiate drug prices with manufacturers.
The more than 4-hour hearing by the House Committee on Energy & Commerce Subcommittee on Health centered on HR 3, the “Lower Drug Costs Now Act of 2019,” introduced by Speaker Pelosi on Sept. 24, which would compel the Centers for Medicare & Medicaid Services to make deals with manufacturers on the maximum, reasonable price for the top 250 highest-cost drugs. If a drug maker refused to participate in the negotiation, the company would face a steep noncompliance fee, according to the bill, while manufacturers that overcharged Medicare or failed to offer the negotiated price would be subject to a civil penalty equal to 10 times the cost difference. The legislation includes a $2,000 out-of-pocket limit for Medicare patients.
If enacted, the legislation would transform the pricing landscape of medications and allow more families to access needed treatments, Speaker Pelosi said during the hearing.
“What it does, as you know; it ends the ban – imagine, there’s a ban on negotiating for lower drug prices,” she said. “So, it ends the ban for the [U.S. Department of Health and Human Services] Secretary now to have the opportunity to negotiate for lower prices. But, the even better news is that these drug prices will be lower not just for Medicare recipients, which was one of the original proposals, but for everyone. It will stop companies from ripping us off by charging five times, four times, three times what is charged in other countries.”
However, Republican legislators spent much of the hearing criticizing the bill, claiming the legislation was crafted behind closed doors by Democrats who made no efforts to gain Republican feedback.
“There is no debate that Republicans and Democrats want to work together to lower drug cost for consumers,” Ranking Member Greg Walden (R-Ore.) said during the hearing. “Madam chair, I have to strongly express my great frustration about the decision to sabotage both the tradition of this committee and the bipartisan work that you know was well underway to tackle high-cost drugs. ... We’ve worked in a bipartisan way up until now. I thought we were headed in a good faith down that same path until the speaker’s office dropped this partisan plan on our [progress]. This is partisan politics at its worst, and it’s an avoidable failure.”
Amid the partisan squabbling, legislators heard differing views from economists about the logistics of the legislation and whether the pricing negotiation model makes sense for the United States.
Gerard F. Anderson, PhD, a professor at Johns Hopkins University and director of the Johns Hopkins Center for Hospital Finance and Management in Baltimore told congressional leaders that negotiation between the government and drug makers is both possible and results in lower prices, even for drugs without therapeutic competition. He noted that the Medicaid program currently negotiates prices for supplemental rebates and that the Veterans Administration and the Department of Defense routinely negotiate discounts greater than the federal supply schedule. Dr. Anderson estimated that the Veterans Administration and the Department of Defense pay an average of 30%-40% less than Medicare prescription drug plans for the same medications.
“Allowing the federal government to negotiate prices for expensive drugs without competition in both the public and private sectors will be more effective in lowering drug prices for everyone,” Dr. Anderson said during testimony. “ Imposing financial penalties for drug companies will bring them to the table. International prices can be used to determine if the drug company is negotiating in good faith.”
But Benedic Ippolito, PhD, a research fellow for the American Enterprise Institute, Washington, raised concerns the legislation may cause reduced innovation. He said the United States accounts for about 60% of drug spending in the developed world, and that, because the market is so large, changes in spending will have first-order implications for the types of future drugs available, Dr. Ippolito said during testimony.
“Consider the incentives associated with the [bill’s] negotiation process,” he said. “Drugs that have no competitors would be subject to aggressive rate regulation by the [HHS] Secretary. The same is not true of drugs with at least one such competitor. It is entirely possible that being a second market entrant could prove substantially more profitable than bringing a novel therapeutic to market. Thus, the proposal could substantially depress incentives to pursue path-breaking drugs.”
Outside the hearing, Speaker Pelosi’s proposed bill is being praised by some physician groups, including the American College of Physicians. In a statement, ACP President Robert McLean, MD, said the college was pleased that the bill focuses on keeping drugs affordable for patients and includes provisions that would support research into new therapies and treatment options.
“ACP specifically supports the provisions that would allow Medicare to negotiate prices with manufacturers,” Dr. McLean said in the statement. “The College has longstanding policy supporting the ability of Medicare to leverage its purchasing power and directly negotiate with manufacturers for drug prices. Although ACP does not have policy on several of the specific provisions in the bill, we are supportive of its overall goals and direction, particularly the emphasis on negotiation and transparency in drug pricing.
Meanwhile, Senate Finance Chairman Charles E. Grassley, (R-Iowa) and Ranking Member Ron Wyden (D-Ore.) released the statutory text of their own drug-pricing legislation on Sept. 25, titled “the Prescription Drug Pricing Reduction Act of 2019 (S-2543).” The bill calls for a number of changes to the Medicare Part D program, such as reduced beneficiary cost sharing and linking drug price increases to the rate of inflation. The legislation would also make more information available regarding pharmacy benefit manager practices and change how Medicare calculates Part B prescription drug payment amounts to lower spending and out-of-pocket costs for patients.
“President Trump has called on Congress to work together on a bipartisan bill to lower prescription drug prices, [and] there’s only one bipartisan bill in Congress to lower prescription drug prices that’s passed the committee process,” Chairman Grassley said in a statement. “This is it. Making prescription drugs more affordable consistently ranks as a top issue for Americans from every corner of the country. I encourage my colleagues on both sides of the aisle to come to the table and work with us to get a bill passed and signed into law.”
Legislators sparred about the best way to lower drug prices during a Sept. 25 hearing, bickering along partisan lines over new legislation by U.S. House Speaker Nancy Pelosi, (D-Calif.) that would require Medicare to negotiate drug prices with manufacturers.
The more than 4-hour hearing by the House Committee on Energy & Commerce Subcommittee on Health centered on HR 3, the “Lower Drug Costs Now Act of 2019,” introduced by Speaker Pelosi on Sept. 24, which would compel the Centers for Medicare & Medicaid Services to make deals with manufacturers on the maximum, reasonable price for the top 250 highest-cost drugs. If a drug maker refused to participate in the negotiation, the company would face a steep noncompliance fee, according to the bill, while manufacturers that overcharged Medicare or failed to offer the negotiated price would be subject to a civil penalty equal to 10 times the cost difference. The legislation includes a $2,000 out-of-pocket limit for Medicare patients.
If enacted, the legislation would transform the pricing landscape of medications and allow more families to access needed treatments, Speaker Pelosi said during the hearing.
“What it does, as you know; it ends the ban – imagine, there’s a ban on negotiating for lower drug prices,” she said. “So, it ends the ban for the [U.S. Department of Health and Human Services] Secretary now to have the opportunity to negotiate for lower prices. But, the even better news is that these drug prices will be lower not just for Medicare recipients, which was one of the original proposals, but for everyone. It will stop companies from ripping us off by charging five times, four times, three times what is charged in other countries.”
However, Republican legislators spent much of the hearing criticizing the bill, claiming the legislation was crafted behind closed doors by Democrats who made no efforts to gain Republican feedback.
“There is no debate that Republicans and Democrats want to work together to lower drug cost for consumers,” Ranking Member Greg Walden (R-Ore.) said during the hearing. “Madam chair, I have to strongly express my great frustration about the decision to sabotage both the tradition of this committee and the bipartisan work that you know was well underway to tackle high-cost drugs. ... We’ve worked in a bipartisan way up until now. I thought we were headed in a good faith down that same path until the speaker’s office dropped this partisan plan on our [progress]. This is partisan politics at its worst, and it’s an avoidable failure.”
Amid the partisan squabbling, legislators heard differing views from economists about the logistics of the legislation and whether the pricing negotiation model makes sense for the United States.
Gerard F. Anderson, PhD, a professor at Johns Hopkins University and director of the Johns Hopkins Center for Hospital Finance and Management in Baltimore told congressional leaders that negotiation between the government and drug makers is both possible and results in lower prices, even for drugs without therapeutic competition. He noted that the Medicaid program currently negotiates prices for supplemental rebates and that the Veterans Administration and the Department of Defense routinely negotiate discounts greater than the federal supply schedule. Dr. Anderson estimated that the Veterans Administration and the Department of Defense pay an average of 30%-40% less than Medicare prescription drug plans for the same medications.
“Allowing the federal government to negotiate prices for expensive drugs without competition in both the public and private sectors will be more effective in lowering drug prices for everyone,” Dr. Anderson said during testimony. “ Imposing financial penalties for drug companies will bring them to the table. International prices can be used to determine if the drug company is negotiating in good faith.”
But Benedic Ippolito, PhD, a research fellow for the American Enterprise Institute, Washington, raised concerns the legislation may cause reduced innovation. He said the United States accounts for about 60% of drug spending in the developed world, and that, because the market is so large, changes in spending will have first-order implications for the types of future drugs available, Dr. Ippolito said during testimony.
“Consider the incentives associated with the [bill’s] negotiation process,” he said. “Drugs that have no competitors would be subject to aggressive rate regulation by the [HHS] Secretary. The same is not true of drugs with at least one such competitor. It is entirely possible that being a second market entrant could prove substantially more profitable than bringing a novel therapeutic to market. Thus, the proposal could substantially depress incentives to pursue path-breaking drugs.”
Outside the hearing, Speaker Pelosi’s proposed bill is being praised by some physician groups, including the American College of Physicians. In a statement, ACP President Robert McLean, MD, said the college was pleased that the bill focuses on keeping drugs affordable for patients and includes provisions that would support research into new therapies and treatment options.
“ACP specifically supports the provisions that would allow Medicare to negotiate prices with manufacturers,” Dr. McLean said in the statement. “The College has longstanding policy supporting the ability of Medicare to leverage its purchasing power and directly negotiate with manufacturers for drug prices. Although ACP does not have policy on several of the specific provisions in the bill, we are supportive of its overall goals and direction, particularly the emphasis on negotiation and transparency in drug pricing.
Meanwhile, Senate Finance Chairman Charles E. Grassley, (R-Iowa) and Ranking Member Ron Wyden (D-Ore.) released the statutory text of their own drug-pricing legislation on Sept. 25, titled “the Prescription Drug Pricing Reduction Act of 2019 (S-2543).” The bill calls for a number of changes to the Medicare Part D program, such as reduced beneficiary cost sharing and linking drug price increases to the rate of inflation. The legislation would also make more information available regarding pharmacy benefit manager practices and change how Medicare calculates Part B prescription drug payment amounts to lower spending and out-of-pocket costs for patients.
“President Trump has called on Congress to work together on a bipartisan bill to lower prescription drug prices, [and] there’s only one bipartisan bill in Congress to lower prescription drug prices that’s passed the committee process,” Chairman Grassley said in a statement. “This is it. Making prescription drugs more affordable consistently ranks as a top issue for Americans from every corner of the country. I encourage my colleagues on both sides of the aisle to come to the table and work with us to get a bill passed and signed into law.”
Antisuicide program promotes resilience, peer support
As youth suicides continue to climb nationwide, a growing body of research shows that the deaths are happening at higher rates in rural communities.
In 2017, suicides reached their highest point since 2000, a trend driven by a sharp rise in male suicides and in youth aged 15-19 years, according to an analysis published recently in JAMA (2019 Jun 18. doi: 10.1001/jama.2019.5054). Among youth aged 15-19 years, the suicide rate was 12 per 100,000 in 2017 (18 per 100,000 in males and 5 per 100,000 in females), compared with 8 per 100,000 in 2000, the study found. Across all age groups, the highest suicide rates and greatest rate increases are in rural counties, according to data from the Centers for Disease Control and Prevention (CDC).
Now, a unique initiative in New Mexico is working to combat those alarming trends through an alliance of community leaders that strives to strengthen resilience and build peer support for at-risk youth.
The Alliance-Building for Suicide Prevention & Youth Resilience (ASPYR) program, created by the University of New Mexico (UNM), Albuquerque, focuses on training professionals and advocates within New Mexico communities in a strength-based, youth-directed, collaborative approach for the assessment and treatment of suicidality. A diversity of community members undergo the training, including health and behavioral health care providers, peer support and community support workers, youth and community advocates, educators, and first responders. The initiative also supports and facilitates the development of a communitywide crisis intervention plan that promotes youth safety and resilience.
“ASPYR is unique, in that we actively involve youth to guide our program, versus an adult-only led program,” says Laura Rombach, program manager for ASPYR and a senior program therapist in the department of psychiatry and behavioral sciences at UNM. “Youth offer feedback about our training and ideas about how to best prevent suicide in their schools and communities. New Mexico is underresourced, and individuals living in rural/frontier areas do not always have access to licensed behavioral health providers, so our training is developed for licensed providers as well as peers and paraprofessionals to increase the knowledge of care for individuals experiencing a suicidal crisis.”
Rural populations present challenges
The many rural pockets of New Mexico pose numerous obstacles for antisuicide advocates.
Of the 33 counties in New Mexico, six are identified by the Census Bureau as completely “rural,” and an additional six are defined as mostly rural, according to the University of New Mexico Bureau of Business & Economic Research. Even among counties considered “urban” however, a considerable amount of the population lives in rural areas, according to the bureau. San Juan County, for example, which is considered urban by the Census Bureau, had an estimated 34% of residents living in rural areas in 2010.
Poverty adds to the difficulty. In 2017, nearly one in five New Mexicans (20%) lived below the poverty line, and the state had the second-highest rate of children under 18 years living in poverty in the country, according to a report by the New Mexico Department of Workforce Solutions.
“New Mexico is an impoverished state with limited capacity, especially in regards to behavioral health services,” said Avi Kriechman, MD, principal investigator for ASPYR at UNM and a child, adolescent, and family psychiatrist at the university. “It is also challenging to create a truly statewide effort where there is limited public transportation, problematic Internet connection, and other barriers to involving those who live and work in rural and frontier New Mexico.”
Addressing suicide among the many native and Indigenous people in rural New Mexico presents another unique set of challenges, said Mary Roessel, MD, a Santa Fe, N.M.–based psychiatrist who specializes in cultural psychiatry. Native and Indigenous residents often have a general mistrust of outsiders and a stigma against mental illnesses, Dr. Roessel said in an interview.
“One of the problems is being able to identify when a person has attempted suicide in some of these small, private, Pueblo communities because they are very closed,” she said. “At times, we don’t get the information to go in and help them. They’re trying to address or deal with the problem themselves.”
To address the many barriers of rural New Mexico, ASPYR works hard to recognize, identify, and support preexisting community resources that are often neglected in needs assessment and stakeholder identification, Dr. Kriechman said. This can include food banks, church care committees, youth advocacy groups, local caregiving, and spiritual traditions, among others. Frequently, many community caregivers and agencies have not connected or communicated with one another and often are unaware of all they have to offer, he said.
“We try to build capacity through community trainings, which include a widely diverse group of providers, advocates, and supports,” he continued. “Our trainings involve highlighting and building upon local and cultural practices and traditions of healing, caregiving, and support. A significant part of our onsite training involves assembling a representative group of local providers in health care, behavioral health care, peer & community support and advocacy, education, first responders to community crises, and government and nonprofit agencies, then facilitating a community conversation between the panel and training attendees about how best to move forward in a synergistic and systemic manner to support youth safety and resilience.”
Peers support peers
While ASPYR encompasses elements of other suicide prevention models, two unique cornerstones of the program are its emphasis on resilience and promotion of peer support. The strength-based, youth-directed approach includes creating a youth-directed safety plan, enlisting peers as support and reducing access to lethal means.
Regarding the youth safety plan, Dr. Kriechman explained that, rather than being prescribed and instructed in expert-selected and expert-driven coping skills, youth are offered a menu of options that most speak to their strengths, values, experience, and preferences. Young people also select a peer who, if they wish, accompanies them to sessions, and supports and coaches them at home.
“Peers are often more influential than parents, siblings, family members, and adults regarding youth behavior,” Dr. Kriechman said. “Most often, it is a peer that a youth-at-risk turns to for support, counsel, role models, and understanding. Youth who wish to offer their peers support can quickly be trained to provide early identification of youth at risk, motivational support to seek help, and a ‘warm hand-off’ to community resources.”
In addition, a Youth Advisory Council established as part of the program draws from young people across New Mexico to participate in state and national conferences, and conduct outreach efforts to peers.
ASPYR Youth council member Serenity Gomez, a senior at the Public Academy for Performing Arts in Albuquerque, became interested in ASPYR after volunteering for the American Foundation for Suicide Prevention in 2016. As a youth council member, Ms. Gomez said she helps create projects to raise suicide awareness, whether through posters, stickers, social media, poetry, or songs.
“My experience as a youth council member has really opened my eyes and has made me more motivated to help others,” she said in an interview. “It has also showed me that talking about suicide doesn’t always have to be a slideshow of facts. You can reach people through music, poetry, storytelling, and so much more. Many people are afraid to talk about suicide because it’s such a scary idea, but if we all talk about it and bring more awareness, then we can find the support everyone needs. In ASPYR, specifically, I hope to reach youth and help all youth learn to support each other.”
Since ASPYR launched in 2017, the program has provided both onsite and online trainings to hundreds of New Mexicans, and has helped rural and frontier communities start working on collaborative approaches to promoting youth safety and resilience, Dr. Kriechman said. Following community consultations, numerous rural communities have since formed systems of care to identify, support, and treat youth at risk. In addition to the youth council, an Advisory Community Council has also been established that welcomes any New Mexico resident interested in working on the mission of preventing youth suicide.
For example, the program shifts from “no-suicide contracts” to safety planning, focusing on reasons for living rather than reasons for dying, and shifting from prescribing coping skills to strengthening preexisting coping skills in young people.
“An ultimate hope for ASPYR is emphasizing that recovery from any of life’s challenges is far more than symptom reduction or agency collaboration,” Dr. Kriechman said. “It is the understanding that a life of value and meaning, the instillation of hope and support for the unique strengths, competencies, skills, and understandings of each individual, is honored, respected, and supported.”
As youth suicides continue to climb nationwide, a growing body of research shows that the deaths are happening at higher rates in rural communities.
In 2017, suicides reached their highest point since 2000, a trend driven by a sharp rise in male suicides and in youth aged 15-19 years, according to an analysis published recently in JAMA (2019 Jun 18. doi: 10.1001/jama.2019.5054). Among youth aged 15-19 years, the suicide rate was 12 per 100,000 in 2017 (18 per 100,000 in males and 5 per 100,000 in females), compared with 8 per 100,000 in 2000, the study found. Across all age groups, the highest suicide rates and greatest rate increases are in rural counties, according to data from the Centers for Disease Control and Prevention (CDC).
Now, a unique initiative in New Mexico is working to combat those alarming trends through an alliance of community leaders that strives to strengthen resilience and build peer support for at-risk youth.
The Alliance-Building for Suicide Prevention & Youth Resilience (ASPYR) program, created by the University of New Mexico (UNM), Albuquerque, focuses on training professionals and advocates within New Mexico communities in a strength-based, youth-directed, collaborative approach for the assessment and treatment of suicidality. A diversity of community members undergo the training, including health and behavioral health care providers, peer support and community support workers, youth and community advocates, educators, and first responders. The initiative also supports and facilitates the development of a communitywide crisis intervention plan that promotes youth safety and resilience.
“ASPYR is unique, in that we actively involve youth to guide our program, versus an adult-only led program,” says Laura Rombach, program manager for ASPYR and a senior program therapist in the department of psychiatry and behavioral sciences at UNM. “Youth offer feedback about our training and ideas about how to best prevent suicide in their schools and communities. New Mexico is underresourced, and individuals living in rural/frontier areas do not always have access to licensed behavioral health providers, so our training is developed for licensed providers as well as peers and paraprofessionals to increase the knowledge of care for individuals experiencing a suicidal crisis.”
Rural populations present challenges
The many rural pockets of New Mexico pose numerous obstacles for antisuicide advocates.
Of the 33 counties in New Mexico, six are identified by the Census Bureau as completely “rural,” and an additional six are defined as mostly rural, according to the University of New Mexico Bureau of Business & Economic Research. Even among counties considered “urban” however, a considerable amount of the population lives in rural areas, according to the bureau. San Juan County, for example, which is considered urban by the Census Bureau, had an estimated 34% of residents living in rural areas in 2010.
Poverty adds to the difficulty. In 2017, nearly one in five New Mexicans (20%) lived below the poverty line, and the state had the second-highest rate of children under 18 years living in poverty in the country, according to a report by the New Mexico Department of Workforce Solutions.
“New Mexico is an impoverished state with limited capacity, especially in regards to behavioral health services,” said Avi Kriechman, MD, principal investigator for ASPYR at UNM and a child, adolescent, and family psychiatrist at the university. “It is also challenging to create a truly statewide effort where there is limited public transportation, problematic Internet connection, and other barriers to involving those who live and work in rural and frontier New Mexico.”
Addressing suicide among the many native and Indigenous people in rural New Mexico presents another unique set of challenges, said Mary Roessel, MD, a Santa Fe, N.M.–based psychiatrist who specializes in cultural psychiatry. Native and Indigenous residents often have a general mistrust of outsiders and a stigma against mental illnesses, Dr. Roessel said in an interview.
“One of the problems is being able to identify when a person has attempted suicide in some of these small, private, Pueblo communities because they are very closed,” she said. “At times, we don’t get the information to go in and help them. They’re trying to address or deal with the problem themselves.”
To address the many barriers of rural New Mexico, ASPYR works hard to recognize, identify, and support preexisting community resources that are often neglected in needs assessment and stakeholder identification, Dr. Kriechman said. This can include food banks, church care committees, youth advocacy groups, local caregiving, and spiritual traditions, among others. Frequently, many community caregivers and agencies have not connected or communicated with one another and often are unaware of all they have to offer, he said.
“We try to build capacity through community trainings, which include a widely diverse group of providers, advocates, and supports,” he continued. “Our trainings involve highlighting and building upon local and cultural practices and traditions of healing, caregiving, and support. A significant part of our onsite training involves assembling a representative group of local providers in health care, behavioral health care, peer & community support and advocacy, education, first responders to community crises, and government and nonprofit agencies, then facilitating a community conversation between the panel and training attendees about how best to move forward in a synergistic and systemic manner to support youth safety and resilience.”
Peers support peers
While ASPYR encompasses elements of other suicide prevention models, two unique cornerstones of the program are its emphasis on resilience and promotion of peer support. The strength-based, youth-directed approach includes creating a youth-directed safety plan, enlisting peers as support and reducing access to lethal means.
Regarding the youth safety plan, Dr. Kriechman explained that, rather than being prescribed and instructed in expert-selected and expert-driven coping skills, youth are offered a menu of options that most speak to their strengths, values, experience, and preferences. Young people also select a peer who, if they wish, accompanies them to sessions, and supports and coaches them at home.
“Peers are often more influential than parents, siblings, family members, and adults regarding youth behavior,” Dr. Kriechman said. “Most often, it is a peer that a youth-at-risk turns to for support, counsel, role models, and understanding. Youth who wish to offer their peers support can quickly be trained to provide early identification of youth at risk, motivational support to seek help, and a ‘warm hand-off’ to community resources.”
In addition, a Youth Advisory Council established as part of the program draws from young people across New Mexico to participate in state and national conferences, and conduct outreach efforts to peers.
ASPYR Youth council member Serenity Gomez, a senior at the Public Academy for Performing Arts in Albuquerque, became interested in ASPYR after volunteering for the American Foundation for Suicide Prevention in 2016. As a youth council member, Ms. Gomez said she helps create projects to raise suicide awareness, whether through posters, stickers, social media, poetry, or songs.
“My experience as a youth council member has really opened my eyes and has made me more motivated to help others,” she said in an interview. “It has also showed me that talking about suicide doesn’t always have to be a slideshow of facts. You can reach people through music, poetry, storytelling, and so much more. Many people are afraid to talk about suicide because it’s such a scary idea, but if we all talk about it and bring more awareness, then we can find the support everyone needs. In ASPYR, specifically, I hope to reach youth and help all youth learn to support each other.”
Since ASPYR launched in 2017, the program has provided both onsite and online trainings to hundreds of New Mexicans, and has helped rural and frontier communities start working on collaborative approaches to promoting youth safety and resilience, Dr. Kriechman said. Following community consultations, numerous rural communities have since formed systems of care to identify, support, and treat youth at risk. In addition to the youth council, an Advisory Community Council has also been established that welcomes any New Mexico resident interested in working on the mission of preventing youth suicide.
For example, the program shifts from “no-suicide contracts” to safety planning, focusing on reasons for living rather than reasons for dying, and shifting from prescribing coping skills to strengthening preexisting coping skills in young people.
“An ultimate hope for ASPYR is emphasizing that recovery from any of life’s challenges is far more than symptom reduction or agency collaboration,” Dr. Kriechman said. “It is the understanding that a life of value and meaning, the instillation of hope and support for the unique strengths, competencies, skills, and understandings of each individual, is honored, respected, and supported.”
As youth suicides continue to climb nationwide, a growing body of research shows that the deaths are happening at higher rates in rural communities.
In 2017, suicides reached their highest point since 2000, a trend driven by a sharp rise in male suicides and in youth aged 15-19 years, according to an analysis published recently in JAMA (2019 Jun 18. doi: 10.1001/jama.2019.5054). Among youth aged 15-19 years, the suicide rate was 12 per 100,000 in 2017 (18 per 100,000 in males and 5 per 100,000 in females), compared with 8 per 100,000 in 2000, the study found. Across all age groups, the highest suicide rates and greatest rate increases are in rural counties, according to data from the Centers for Disease Control and Prevention (CDC).
Now, a unique initiative in New Mexico is working to combat those alarming trends through an alliance of community leaders that strives to strengthen resilience and build peer support for at-risk youth.
The Alliance-Building for Suicide Prevention & Youth Resilience (ASPYR) program, created by the University of New Mexico (UNM), Albuquerque, focuses on training professionals and advocates within New Mexico communities in a strength-based, youth-directed, collaborative approach for the assessment and treatment of suicidality. A diversity of community members undergo the training, including health and behavioral health care providers, peer support and community support workers, youth and community advocates, educators, and first responders. The initiative also supports and facilitates the development of a communitywide crisis intervention plan that promotes youth safety and resilience.
“ASPYR is unique, in that we actively involve youth to guide our program, versus an adult-only led program,” says Laura Rombach, program manager for ASPYR and a senior program therapist in the department of psychiatry and behavioral sciences at UNM. “Youth offer feedback about our training and ideas about how to best prevent suicide in their schools and communities. New Mexico is underresourced, and individuals living in rural/frontier areas do not always have access to licensed behavioral health providers, so our training is developed for licensed providers as well as peers and paraprofessionals to increase the knowledge of care for individuals experiencing a suicidal crisis.”
Rural populations present challenges
The many rural pockets of New Mexico pose numerous obstacles for antisuicide advocates.
Of the 33 counties in New Mexico, six are identified by the Census Bureau as completely “rural,” and an additional six are defined as mostly rural, according to the University of New Mexico Bureau of Business & Economic Research. Even among counties considered “urban” however, a considerable amount of the population lives in rural areas, according to the bureau. San Juan County, for example, which is considered urban by the Census Bureau, had an estimated 34% of residents living in rural areas in 2010.
Poverty adds to the difficulty. In 2017, nearly one in five New Mexicans (20%) lived below the poverty line, and the state had the second-highest rate of children under 18 years living in poverty in the country, according to a report by the New Mexico Department of Workforce Solutions.
“New Mexico is an impoverished state with limited capacity, especially in regards to behavioral health services,” said Avi Kriechman, MD, principal investigator for ASPYR at UNM and a child, adolescent, and family psychiatrist at the university. “It is also challenging to create a truly statewide effort where there is limited public transportation, problematic Internet connection, and other barriers to involving those who live and work in rural and frontier New Mexico.”
Addressing suicide among the many native and Indigenous people in rural New Mexico presents another unique set of challenges, said Mary Roessel, MD, a Santa Fe, N.M.–based psychiatrist who specializes in cultural psychiatry. Native and Indigenous residents often have a general mistrust of outsiders and a stigma against mental illnesses, Dr. Roessel said in an interview.
“One of the problems is being able to identify when a person has attempted suicide in some of these small, private, Pueblo communities because they are very closed,” she said. “At times, we don’t get the information to go in and help them. They’re trying to address or deal with the problem themselves.”
To address the many barriers of rural New Mexico, ASPYR works hard to recognize, identify, and support preexisting community resources that are often neglected in needs assessment and stakeholder identification, Dr. Kriechman said. This can include food banks, church care committees, youth advocacy groups, local caregiving, and spiritual traditions, among others. Frequently, many community caregivers and agencies have not connected or communicated with one another and often are unaware of all they have to offer, he said.
“We try to build capacity through community trainings, which include a widely diverse group of providers, advocates, and supports,” he continued. “Our trainings involve highlighting and building upon local and cultural practices and traditions of healing, caregiving, and support. A significant part of our onsite training involves assembling a representative group of local providers in health care, behavioral health care, peer & community support and advocacy, education, first responders to community crises, and government and nonprofit agencies, then facilitating a community conversation between the panel and training attendees about how best to move forward in a synergistic and systemic manner to support youth safety and resilience.”
Peers support peers
While ASPYR encompasses elements of other suicide prevention models, two unique cornerstones of the program are its emphasis on resilience and promotion of peer support. The strength-based, youth-directed approach includes creating a youth-directed safety plan, enlisting peers as support and reducing access to lethal means.
Regarding the youth safety plan, Dr. Kriechman explained that, rather than being prescribed and instructed in expert-selected and expert-driven coping skills, youth are offered a menu of options that most speak to their strengths, values, experience, and preferences. Young people also select a peer who, if they wish, accompanies them to sessions, and supports and coaches them at home.
“Peers are often more influential than parents, siblings, family members, and adults regarding youth behavior,” Dr. Kriechman said. “Most often, it is a peer that a youth-at-risk turns to for support, counsel, role models, and understanding. Youth who wish to offer their peers support can quickly be trained to provide early identification of youth at risk, motivational support to seek help, and a ‘warm hand-off’ to community resources.”
In addition, a Youth Advisory Council established as part of the program draws from young people across New Mexico to participate in state and national conferences, and conduct outreach efforts to peers.
ASPYR Youth council member Serenity Gomez, a senior at the Public Academy for Performing Arts in Albuquerque, became interested in ASPYR after volunteering for the American Foundation for Suicide Prevention in 2016. As a youth council member, Ms. Gomez said she helps create projects to raise suicide awareness, whether through posters, stickers, social media, poetry, or songs.
“My experience as a youth council member has really opened my eyes and has made me more motivated to help others,” she said in an interview. “It has also showed me that talking about suicide doesn’t always have to be a slideshow of facts. You can reach people through music, poetry, storytelling, and so much more. Many people are afraid to talk about suicide because it’s such a scary idea, but if we all talk about it and bring more awareness, then we can find the support everyone needs. In ASPYR, specifically, I hope to reach youth and help all youth learn to support each other.”
Since ASPYR launched in 2017, the program has provided both onsite and online trainings to hundreds of New Mexicans, and has helped rural and frontier communities start working on collaborative approaches to promoting youth safety and resilience, Dr. Kriechman said. Following community consultations, numerous rural communities have since formed systems of care to identify, support, and treat youth at risk. In addition to the youth council, an Advisory Community Council has also been established that welcomes any New Mexico resident interested in working on the mission of preventing youth suicide.
For example, the program shifts from “no-suicide contracts” to safety planning, focusing on reasons for living rather than reasons for dying, and shifting from prescribing coping skills to strengthening preexisting coping skills in young people.
“An ultimate hope for ASPYR is emphasizing that recovery from any of life’s challenges is far more than symptom reduction or agency collaboration,” Dr. Kriechman said. “It is the understanding that a life of value and meaning, the instillation of hope and support for the unique strengths, competencies, skills, and understandings of each individual, is honored, respected, and supported.”
Most practices not screening for five social needs
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
FROM JAMA NETWORK OPEN
ABIM: Self-paced maintenance of certification pathway under development
Physician groups are praising a new option by the American Board of Internal Medicine (ABIM) that will offer doctors a self-paced pathway for maintenance of certification (MOC) in place of the traditional long-form assessment route.
The new longitudinal assessment option, announced in late August, would enable physicians to acquire and demonstrate ongoing knowledge through shorter evaluations of specific content. The option, currently under development, also would provide doctors with immediate feedback about their answers and share links to educational material to address knowledge gaps, according to an announcement. While details are still being fleshed out, a summary of the longitudinal assessment concept by the American Board of Medical Specialties explains that the approach draws on the principles of adult learning and modern technology “to promote learning, retention, and transfer of information.”
Developing a longitudinal assessment option is part of ABIM’s ongoing evolution, Marianne M. Green, MD, chair for ABIM’s board of directors and ABIM President Richard J. Baron, MD, wrote in a joint letter to internists posted on ABIM’s blog.
“We recognize that some physicians may prefer a more continuous process that easily integrates into their lives and allows them to engage seamlessly at their preferred pace, while being able to access the resources they use in practice,” the doctors wrote.
“Until recently, AGA [American Gastroenterological Association], along with AASLD [American Association for the Study of Liver Diseases], ACG [American College of Gastroenterology], and ASGE [American Society for Gastrointestinal Endoscopy], had been working on a new recertification pathway for GI. That effort has been temporarily suspended as ABIM pursues a pathway that will be available to all internal medicine specialties,” said Hashem El Serag, MD, MPH, AGAF, AGA president. “AGA appreciates that ABIM’s new longitudinal pathway appears to conform to the principles that the GI societies have espoused. We will monitor the development of the pathway as it moves toward implementation continuing to advocate for the needs of gastroenterologists.”
These GI societies are guided by these core principles in their campaign to reform MOC:
• MOC needs to be simpler, less intrusive, and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single-source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
Douglas DeLong, MD, chair of the American College of Physician’s (ACP) board of regents said the option is a positive, first step that will support lifelong learning. He noted the new option is in line with recommendations released in 2019 by the American Board of Medical Specialties’ Continuing Board Certification: Vision for the Future Commission, which included ACP concerns.
“It’s pretty clear that some of the principles of adult learning – frequent information with quick feedback, repetition of material, and identifying gaps in knowledge – is really how people most effectively learn,” Dr. DeLong said in an interview. “Just cramming for an examination every decade hasn’t ever really been shown to affect long-term retention of knowledge or even patient care outcomes.”
Alan Lichtin, MD, chair of the MOC working group for the American Society of Hematology (ASH), said the self-paced pathway is a much-needed option, particularly the immediate feedback on test questions.
“For years, ASH has been advocating that ABIM move from the traditional sit-down testing to an alternative form of ‘formative’ assessment that has been adapted by other specialty boards,” Dr. Lichtin said in an interview. Anesthesiology and pediatrics have novel testing methods that fit into physicians’ schedules without being so disruptive and anxiety provoking. There is instantaneous feedback about whether the answers are correct or not. It is not useful to study hard for a time-intensive, comprehensive test only to get a summary of what was missed a long time after the test. By that point, the exam material is no longer fresh in one’s mind and therefore the feedback is no longer useful.”
The new pathway is still under development, and ABIM has not said when the option might be launched. In the meantime, the current MOC program and its traditional exam will remain in effect. The ABIM is requesting feedback and comments from physicians about the option. Dr. Baron wrote that more information about the change will be forthcoming in the months ahead.
The ABIM announcement comes on the heels of several ongoing legal challenges levied at the board by a group of internists over its MOC process.
A lawsuit, filed Dec. 6, 2018, in Pennsylvania district court and later amended in 2019, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Sept. 26, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The judge ruled that the doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim.
Physicians in three other lawsuits are also suing medical boards over their respective MOC processes. In February 2019, a radiologist issued a legal challenge against the American Board of Radiology over its MOC regulations. Also in February, two emergency physicians and an anesthesiologist filed a lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology over MOC requirements. A month later, two psychiatrists issued a legal challenge against the American Board of Psychiatry and Neurology over its MOC process.
Attorneys for all three boards in the ABIM, American Board of Psychiatry and Neurology, and American Board of Radiology cases are seeking to dismiss the complaints. Judges have not yet ruled on the motions. In addition, a motion to consolidate all the cases was denied by the court.
A GoFundMe campaign launched by the Practicing Physicians of America to pay for plaintiffs’ costs associated with the class-action lawsuits has now garnered more than $300,000.
This story was updated on October 1, 2019.
Physician groups are praising a new option by the American Board of Internal Medicine (ABIM) that will offer doctors a self-paced pathway for maintenance of certification (MOC) in place of the traditional long-form assessment route.
The new longitudinal assessment option, announced in late August, would enable physicians to acquire and demonstrate ongoing knowledge through shorter evaluations of specific content. The option, currently under development, also would provide doctors with immediate feedback about their answers and share links to educational material to address knowledge gaps, according to an announcement. While details are still being fleshed out, a summary of the longitudinal assessment concept by the American Board of Medical Specialties explains that the approach draws on the principles of adult learning and modern technology “to promote learning, retention, and transfer of information.”
Developing a longitudinal assessment option is part of ABIM’s ongoing evolution, Marianne M. Green, MD, chair for ABIM’s board of directors and ABIM President Richard J. Baron, MD, wrote in a joint letter to internists posted on ABIM’s blog.
“We recognize that some physicians may prefer a more continuous process that easily integrates into their lives and allows them to engage seamlessly at their preferred pace, while being able to access the resources they use in practice,” the doctors wrote.
“Until recently, AGA [American Gastroenterological Association], along with AASLD [American Association for the Study of Liver Diseases], ACG [American College of Gastroenterology], and ASGE [American Society for Gastrointestinal Endoscopy], had been working on a new recertification pathway for GI. That effort has been temporarily suspended as ABIM pursues a pathway that will be available to all internal medicine specialties,” said Hashem El Serag, MD, MPH, AGAF, AGA president. “AGA appreciates that ABIM’s new longitudinal pathway appears to conform to the principles that the GI societies have espoused. We will monitor the development of the pathway as it moves toward implementation continuing to advocate for the needs of gastroenterologists.”
These GI societies are guided by these core principles in their campaign to reform MOC:
• MOC needs to be simpler, less intrusive, and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single-source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
Douglas DeLong, MD, chair of the American College of Physician’s (ACP) board of regents said the option is a positive, first step that will support lifelong learning. He noted the new option is in line with recommendations released in 2019 by the American Board of Medical Specialties’ Continuing Board Certification: Vision for the Future Commission, which included ACP concerns.
“It’s pretty clear that some of the principles of adult learning – frequent information with quick feedback, repetition of material, and identifying gaps in knowledge – is really how people most effectively learn,” Dr. DeLong said in an interview. “Just cramming for an examination every decade hasn’t ever really been shown to affect long-term retention of knowledge or even patient care outcomes.”
Alan Lichtin, MD, chair of the MOC working group for the American Society of Hematology (ASH), said the self-paced pathway is a much-needed option, particularly the immediate feedback on test questions.
“For years, ASH has been advocating that ABIM move from the traditional sit-down testing to an alternative form of ‘formative’ assessment that has been adapted by other specialty boards,” Dr. Lichtin said in an interview. Anesthesiology and pediatrics have novel testing methods that fit into physicians’ schedules without being so disruptive and anxiety provoking. There is instantaneous feedback about whether the answers are correct or not. It is not useful to study hard for a time-intensive, comprehensive test only to get a summary of what was missed a long time after the test. By that point, the exam material is no longer fresh in one’s mind and therefore the feedback is no longer useful.”
The new pathway is still under development, and ABIM has not said when the option might be launched. In the meantime, the current MOC program and its traditional exam will remain in effect. The ABIM is requesting feedback and comments from physicians about the option. Dr. Baron wrote that more information about the change will be forthcoming in the months ahead.
The ABIM announcement comes on the heels of several ongoing legal challenges levied at the board by a group of internists over its MOC process.
A lawsuit, filed Dec. 6, 2018, in Pennsylvania district court and later amended in 2019, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Sept. 26, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The judge ruled that the doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim.
Physicians in three other lawsuits are also suing medical boards over their respective MOC processes. In February 2019, a radiologist issued a legal challenge against the American Board of Radiology over its MOC regulations. Also in February, two emergency physicians and an anesthesiologist filed a lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology over MOC requirements. A month later, two psychiatrists issued a legal challenge against the American Board of Psychiatry and Neurology over its MOC process.
Attorneys for all three boards in the ABIM, American Board of Psychiatry and Neurology, and American Board of Radiology cases are seeking to dismiss the complaints. Judges have not yet ruled on the motions. In addition, a motion to consolidate all the cases was denied by the court.
A GoFundMe campaign launched by the Practicing Physicians of America to pay for plaintiffs’ costs associated with the class-action lawsuits has now garnered more than $300,000.
This story was updated on October 1, 2019.
Physician groups are praising a new option by the American Board of Internal Medicine (ABIM) that will offer doctors a self-paced pathway for maintenance of certification (MOC) in place of the traditional long-form assessment route.
The new longitudinal assessment option, announced in late August, would enable physicians to acquire and demonstrate ongoing knowledge through shorter evaluations of specific content. The option, currently under development, also would provide doctors with immediate feedback about their answers and share links to educational material to address knowledge gaps, according to an announcement. While details are still being fleshed out, a summary of the longitudinal assessment concept by the American Board of Medical Specialties explains that the approach draws on the principles of adult learning and modern technology “to promote learning, retention, and transfer of information.”
Developing a longitudinal assessment option is part of ABIM’s ongoing evolution, Marianne M. Green, MD, chair for ABIM’s board of directors and ABIM President Richard J. Baron, MD, wrote in a joint letter to internists posted on ABIM’s blog.
“We recognize that some physicians may prefer a more continuous process that easily integrates into their lives and allows them to engage seamlessly at their preferred pace, while being able to access the resources they use in practice,” the doctors wrote.
“Until recently, AGA [American Gastroenterological Association], along with AASLD [American Association for the Study of Liver Diseases], ACG [American College of Gastroenterology], and ASGE [American Society for Gastrointestinal Endoscopy], had been working on a new recertification pathway for GI. That effort has been temporarily suspended as ABIM pursues a pathway that will be available to all internal medicine specialties,” said Hashem El Serag, MD, MPH, AGAF, AGA president. “AGA appreciates that ABIM’s new longitudinal pathway appears to conform to the principles that the GI societies have espoused. We will monitor the development of the pathway as it moves toward implementation continuing to advocate for the needs of gastroenterologists.”
These GI societies are guided by these core principles in their campaign to reform MOC:
• MOC needs to be simpler, less intrusive, and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single-source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
Douglas DeLong, MD, chair of the American College of Physician’s (ACP) board of regents said the option is a positive, first step that will support lifelong learning. He noted the new option is in line with recommendations released in 2019 by the American Board of Medical Specialties’ Continuing Board Certification: Vision for the Future Commission, which included ACP concerns.
“It’s pretty clear that some of the principles of adult learning – frequent information with quick feedback, repetition of material, and identifying gaps in knowledge – is really how people most effectively learn,” Dr. DeLong said in an interview. “Just cramming for an examination every decade hasn’t ever really been shown to affect long-term retention of knowledge or even patient care outcomes.”
Alan Lichtin, MD, chair of the MOC working group for the American Society of Hematology (ASH), said the self-paced pathway is a much-needed option, particularly the immediate feedback on test questions.
“For years, ASH has been advocating that ABIM move from the traditional sit-down testing to an alternative form of ‘formative’ assessment that has been adapted by other specialty boards,” Dr. Lichtin said in an interview. Anesthesiology and pediatrics have novel testing methods that fit into physicians’ schedules without being so disruptive and anxiety provoking. There is instantaneous feedback about whether the answers are correct or not. It is not useful to study hard for a time-intensive, comprehensive test only to get a summary of what was missed a long time after the test. By that point, the exam material is no longer fresh in one’s mind and therefore the feedback is no longer useful.”
The new pathway is still under development, and ABIM has not said when the option might be launched. In the meantime, the current MOC program and its traditional exam will remain in effect. The ABIM is requesting feedback and comments from physicians about the option. Dr. Baron wrote that more information about the change will be forthcoming in the months ahead.
The ABIM announcement comes on the heels of several ongoing legal challenges levied at the board by a group of internists over its MOC process.
A lawsuit, filed Dec. 6, 2018, in Pennsylvania district court and later amended in 2019, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Sept. 26, U.S. District Court Judge for the Eastern District of Pennsylvania Robert F. Kelly Sr. said the plaintiffs failed to demonstrate sufficient evidence for their antitrust and unjust enrichment claims against ABIM. The judge ruled that the doctors also did not establish any showing of anticompetitive conduct by ABIM to support a monopolization claim.
Physicians in three other lawsuits are also suing medical boards over their respective MOC processes. In February 2019, a radiologist issued a legal challenge against the American Board of Radiology over its MOC regulations. Also in February, two emergency physicians and an anesthesiologist filed a lawsuit against the American Board of Medical Specialties, the American Board of Emergency Medicine, and the American Board of Anesthesiology over MOC requirements. A month later, two psychiatrists issued a legal challenge against the American Board of Psychiatry and Neurology over its MOC process.
Attorneys for all three boards in the ABIM, American Board of Psychiatry and Neurology, and American Board of Radiology cases are seeking to dismiss the complaints. Judges have not yet ruled on the motions. In addition, a motion to consolidate all the cases was denied by the court.
A GoFundMe campaign launched by the Practicing Physicians of America to pay for plaintiffs’ costs associated with the class-action lawsuits has now garnered more than $300,000.
This story was updated on October 1, 2019.
Trump administration finalizing ban on flavored e-cigarettes
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
Insurers to pay record number of rebates to patients
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
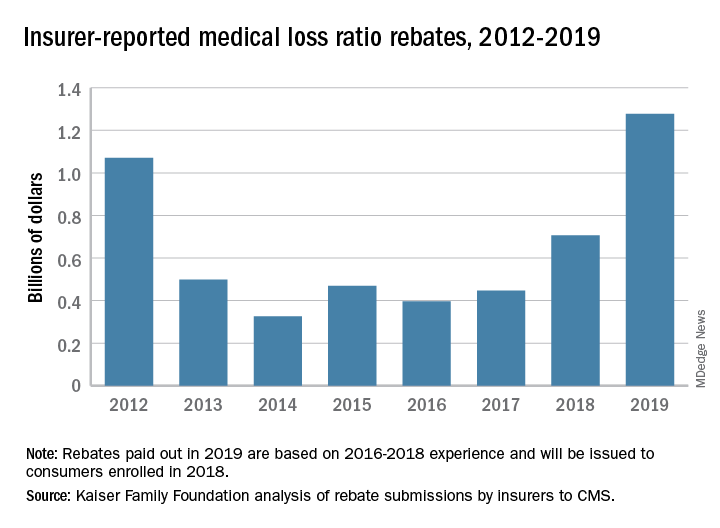
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
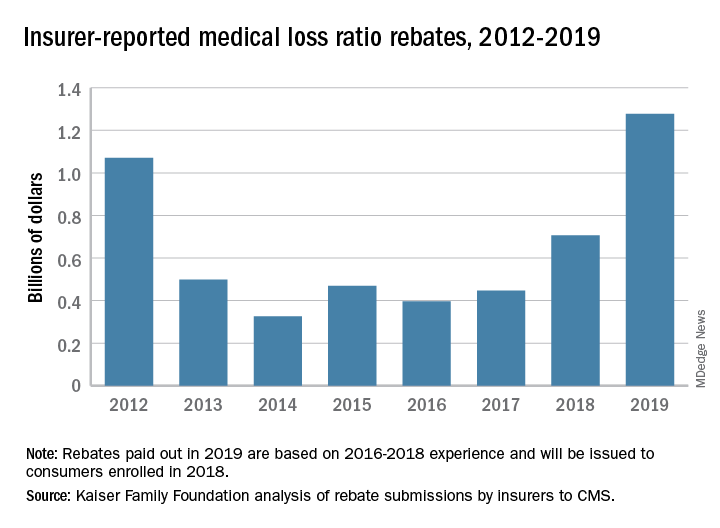
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
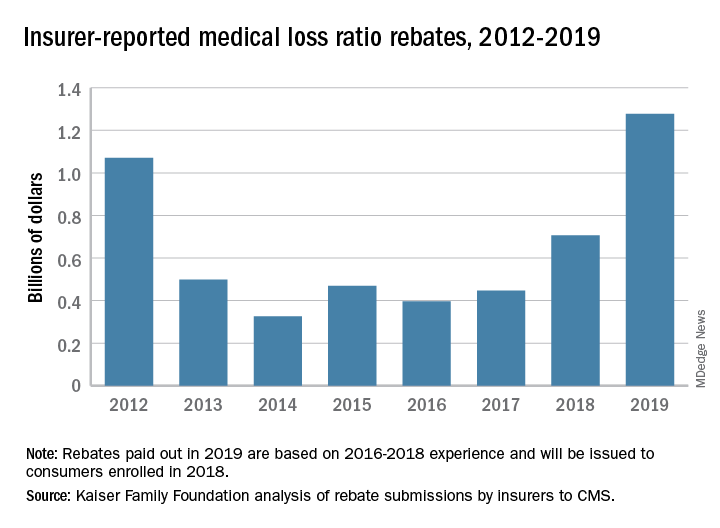
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Judge blocks North Dakota abortion law
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.
CVS-Aetna merger approval gets poor review from physicians
Physician groups are criticizing a judge’s decision to approve the merger of pharmacy chain CVS Health and health insurer Aetna, saying the deal will raise prices and lower quality.
Judge Richard J. Leon of the U.S. District Court for the District of Columbia allowed the merger to move forward on Sept. 4, ruling that the acquisition was legal under antitrust law. The merger was approved by the Department of Justice in October 2018 on the condition that Aetna sell its Medicare prescription drug plan (PDP) business to independently owned competitor, WellCare Health Plans. Judge Leon has been examining the government’s plan since late 2018.
In his decision, Judge Leon acknowledged that the merger will have widespread effects for millions of patients and noted the many industry stakeholders, consumer groups, and state regulatory bodies have raised concerns about the merger.
“Although [the opposition] raised substantial concerns that warranted serious consideration, CVS’s and the government’s witnesses, when combined with the existing record, persuasively support why the markets at issue are not only very competitive today, but are likely to remain so post merger,” Judge Leon wrote. “Consequently, the harms to the public interest the [opposition] raised were not sufficiently established to undermine the government’s conclusion to the contrary. As such, for all of the above reasons, I have concluded that the proposed settlement is well ‘within the reaches’ of the public interest and the government’s motion ... should therefore be granted.”
Patrice A. Harris, MD, president for the American Medical Association, said the judge’s decision fails patients and will likely raise prices, lower quality, reduce choice, and stifle innovation.
“The American people and our health system will not be served well by allowing a merger that combines health insurance giant Aetna Inc. with CVS Health Corporation,” Dr. Harris said in a statement. “For patients and employers struggling with recurrent increases to health insurance premiums, out-of-pocket costs, and prescription drug prices, it’s hard to find any upside to a merger that leaves them with fewer choices. Nothing in the deal guarantees reductions on insurance premiums or prescription drug costs. As for promised efficiency savings, that money will likely go straight to CVS’s bottom line.”
Angus Worthing, MD, government affairs committee chair for the American College of Rheumatology, said his group is concerned that the merger will hinder progress that has been made toward creating cost transparency and will make it easier for costs savings to remain secret.
“We hope that regulators will now actively watch the conduct of the merged company to ensure patients are protected,” Dr. Worthing said in a statement.
In a statement, CVS noted that CVS Health and Aetna have been one company since November 2018, stating that the court’s action “makes that 100 percent clear.”
“We remain focused on transforming the consumer health care experience in America,” they said.
CVS Health announced it would buy Aetna for $69 billion in 2017 and finalized the acquisition in 2018. CVS Health President and CEO Larry J. Merlo said the combined company would connect consumers with the powerful health resources of CVS Health in communities across the country and Aetna’s network of providers to help remove barriers to high quality care and build lasting relationships with patients.
Assistant Attorney General Makan Delrahim of the Justice Department’s antitrust division said the agency was pleased with the court’s decision to approve the government’s plan and finalize the merger.
“The divestiture of Aetna’s individual PDP business provides a comprehensive remedy to the harms the Justice Department identified,” Mr. Delrahim said in a statement. “The entry of the final judgment protects seniors and other vulnerable customers of individual PDPs from the anticompetitive effects that would have occurred if CVS and Aetna had merged their individual PDP businesses.”
Physician groups are criticizing a judge’s decision to approve the merger of pharmacy chain CVS Health and health insurer Aetna, saying the deal will raise prices and lower quality.
Judge Richard J. Leon of the U.S. District Court for the District of Columbia allowed the merger to move forward on Sept. 4, ruling that the acquisition was legal under antitrust law. The merger was approved by the Department of Justice in October 2018 on the condition that Aetna sell its Medicare prescription drug plan (PDP) business to independently owned competitor, WellCare Health Plans. Judge Leon has been examining the government’s plan since late 2018.
In his decision, Judge Leon acknowledged that the merger will have widespread effects for millions of patients and noted the many industry stakeholders, consumer groups, and state regulatory bodies have raised concerns about the merger.
“Although [the opposition] raised substantial concerns that warranted serious consideration, CVS’s and the government’s witnesses, when combined with the existing record, persuasively support why the markets at issue are not only very competitive today, but are likely to remain so post merger,” Judge Leon wrote. “Consequently, the harms to the public interest the [opposition] raised were not sufficiently established to undermine the government’s conclusion to the contrary. As such, for all of the above reasons, I have concluded that the proposed settlement is well ‘within the reaches’ of the public interest and the government’s motion ... should therefore be granted.”
Patrice A. Harris, MD, president for the American Medical Association, said the judge’s decision fails patients and will likely raise prices, lower quality, reduce choice, and stifle innovation.
“The American people and our health system will not be served well by allowing a merger that combines health insurance giant Aetna Inc. with CVS Health Corporation,” Dr. Harris said in a statement. “For patients and employers struggling with recurrent increases to health insurance premiums, out-of-pocket costs, and prescription drug prices, it’s hard to find any upside to a merger that leaves them with fewer choices. Nothing in the deal guarantees reductions on insurance premiums or prescription drug costs. As for promised efficiency savings, that money will likely go straight to CVS’s bottom line.”
Angus Worthing, MD, government affairs committee chair for the American College of Rheumatology, said his group is concerned that the merger will hinder progress that has been made toward creating cost transparency and will make it easier for costs savings to remain secret.
“We hope that regulators will now actively watch the conduct of the merged company to ensure patients are protected,” Dr. Worthing said in a statement.
In a statement, CVS noted that CVS Health and Aetna have been one company since November 2018, stating that the court’s action “makes that 100 percent clear.”
“We remain focused on transforming the consumer health care experience in America,” they said.
CVS Health announced it would buy Aetna for $69 billion in 2017 and finalized the acquisition in 2018. CVS Health President and CEO Larry J. Merlo said the combined company would connect consumers with the powerful health resources of CVS Health in communities across the country and Aetna’s network of providers to help remove barriers to high quality care and build lasting relationships with patients.
Assistant Attorney General Makan Delrahim of the Justice Department’s antitrust division said the agency was pleased with the court’s decision to approve the government’s plan and finalize the merger.
“The divestiture of Aetna’s individual PDP business provides a comprehensive remedy to the harms the Justice Department identified,” Mr. Delrahim said in a statement. “The entry of the final judgment protects seniors and other vulnerable customers of individual PDPs from the anticompetitive effects that would have occurred if CVS and Aetna had merged their individual PDP businesses.”
Physician groups are criticizing a judge’s decision to approve the merger of pharmacy chain CVS Health and health insurer Aetna, saying the deal will raise prices and lower quality.
Judge Richard J. Leon of the U.S. District Court for the District of Columbia allowed the merger to move forward on Sept. 4, ruling that the acquisition was legal under antitrust law. The merger was approved by the Department of Justice in October 2018 on the condition that Aetna sell its Medicare prescription drug plan (PDP) business to independently owned competitor, WellCare Health Plans. Judge Leon has been examining the government’s plan since late 2018.
In his decision, Judge Leon acknowledged that the merger will have widespread effects for millions of patients and noted the many industry stakeholders, consumer groups, and state regulatory bodies have raised concerns about the merger.
“Although [the opposition] raised substantial concerns that warranted serious consideration, CVS’s and the government’s witnesses, when combined with the existing record, persuasively support why the markets at issue are not only very competitive today, but are likely to remain so post merger,” Judge Leon wrote. “Consequently, the harms to the public interest the [opposition] raised were not sufficiently established to undermine the government’s conclusion to the contrary. As such, for all of the above reasons, I have concluded that the proposed settlement is well ‘within the reaches’ of the public interest and the government’s motion ... should therefore be granted.”
Patrice A. Harris, MD, president for the American Medical Association, said the judge’s decision fails patients and will likely raise prices, lower quality, reduce choice, and stifle innovation.
“The American people and our health system will not be served well by allowing a merger that combines health insurance giant Aetna Inc. with CVS Health Corporation,” Dr. Harris said in a statement. “For patients and employers struggling with recurrent increases to health insurance premiums, out-of-pocket costs, and prescription drug prices, it’s hard to find any upside to a merger that leaves them with fewer choices. Nothing in the deal guarantees reductions on insurance premiums or prescription drug costs. As for promised efficiency savings, that money will likely go straight to CVS’s bottom line.”
Angus Worthing, MD, government affairs committee chair for the American College of Rheumatology, said his group is concerned that the merger will hinder progress that has been made toward creating cost transparency and will make it easier for costs savings to remain secret.
“We hope that regulators will now actively watch the conduct of the merged company to ensure patients are protected,” Dr. Worthing said in a statement.
In a statement, CVS noted that CVS Health and Aetna have been one company since November 2018, stating that the court’s action “makes that 100 percent clear.”
“We remain focused on transforming the consumer health care experience in America,” they said.
CVS Health announced it would buy Aetna for $69 billion in 2017 and finalized the acquisition in 2018. CVS Health President and CEO Larry J. Merlo said the combined company would connect consumers with the powerful health resources of CVS Health in communities across the country and Aetna’s network of providers to help remove barriers to high quality care and build lasting relationships with patients.
Assistant Attorney General Makan Delrahim of the Justice Department’s antitrust division said the agency was pleased with the court’s decision to approve the government’s plan and finalize the merger.
“The divestiture of Aetna’s individual PDP business provides a comprehensive remedy to the harms the Justice Department identified,” Mr. Delrahim said in a statement. “The entry of the final judgment protects seniors and other vulnerable customers of individual PDPs from the anticompetitive effects that would have occurred if CVS and Aetna had merged their individual PDP businesses.”
New report cites mental health challenges faced by separated immigrant children
Care providers encountered significant challenges when addressing the mental health needs of unaccompanied immigrant children in federal custody, including overwhelming caseloads and the deteriorating mental health of some patients, according to a new report by the Office of Inspector General (OIG).
In the report, released Sept. 3, the OIG outlined findings from its analysis of 45 Office of Refugee Resettlement (ORR) facilities between August and September 2018. The U.S. Department of Health & Human Services ORR is the legal custodian of unaccompanied immigrant children in its care who have no parent or legal guardian available. This includes children who arrive in the United States unaccompanied and children who are separated from their parents or guardians by immigration authorities after arriving in the country.
For the analysis, OIG investigators collected data from interviews with mental health clinicians, medical coordinators, facility leadership, and ORR federal field specialists at the 45 selected facilities.
Investigators recorded numerous serious challenges experienced by providers when attempting to provide mental health care to the children. Namely, they cited overwhelming patient caseloads, and difficulty accessing external mental health clinicians and referring children to providers within ORR’s network, according to the OIG’s report.
Mental health clinicians reported that the high caseloads hurt their ability to build rapport with young patients – and allowed less time for counseling and less frequent sessions for children with greater needs. The heavy caseloads were generated by heightened immigration enforcement beginning in 2017, and the separation of many more families at the border and more children being placed in federal custody, according to the report.
In addition, providers reported challenges when addressing the mental health needs of children who had experienced significant trauma before coming into federal custody. This included trauma that occurred while the children lived in the countries of origin, trauma during their journey to the United States, and trauma upon their arrival in the United States.
Separation from parents and a chaotic reunification process added to the trauma that children had already experienced, providers reported, and put extreme pressure on facility staff. Separated children exhibited “more fear, feelings of abandonment, and posttraumatic stress than did children who were not separated,” according to the findings. Separated children also experienced elevated feelings of anxiety and loss as a consequence of unexpected separation from loved ones.
Also, facilities reported that longer lengths of stay resulted in deteriorating mental health for some children and increased demands on staff. Facilities reported that children who stayed in federal custody for longer periods experienced more stress, anxiety, and behavioral issues. According to the facilities, the longer stays resulted in higher levels of defiance, hopelessness, and frustration among children – in addition to more instances of self-harm and suicidal ideation.
It is not surprising that the OIG study reflects that mental health services at facilities for unaccompanied minors are understaffed, undertrained, and overwhelmed, said Craig L. Katz, MD, a clinical professor of psychiatry at Mount Sinai in New York.
“In some sense, this can probably be said for most of the U.S. and definitely the world when it comes to child mental health services,” Dr. Katz said in an interview. “But, what’s especially tough to stomach about this shortfall at these facilities is that they encompass an immensely high-risk population – an inevitably highly, if not multiply traumatized population of children who lack primary caregivers.”
Dr. Katz was coinvestigator of a recent study that assessed the mental health of children held at a U.S. immigration detention center through the Parent-Report Strengths and Difficulties Questionnaire. Among the 425 children evaluated, many demonstrated elevated scores for emotional problems, peer problems, and total difficulties, according to the June 2018 study, published in Social Science & Medicine (2019 Jun; 230:303-8). Younger children (aged 4-8 years) demonstrated more difficulties associated with conduct, hyperactivity, and total difficulties, compared with older children, the study found.
Children who had been forcibly separated from their mothers demonstrated significantly more emotional problems and total difficulties, compared with those who had never been separated. Of 150 children who completed the Posttraumatic Stress Disorder Reaction Index, 17% had a probable diagnosis of PTSD, results found.
Dr. Katz said the OIG reached the same basic conclusion as his quantitative study – that separated minors appear to have even greater mental health problems than do fellow unaccompanied minors.
“In our study, we found that children in family detention had greater mental health problems than [did] American community samples but that formerly separated children who had been reunited with their mothers had even more health problems than their fellow detainees,” Dr. Katz said. “Something about being separated per U.S. policy was especially pernicious, which we knew in our hearts; but now in this study and ours, we know empirically.”
As long as the United States continues to detain children, the psychological harm created by such detainments is likely to continue, said Kim A. Baranowski, PhD, a psychologist and lecturer at Columbia University in New York. At a minimum, unaccompanied minors should have access to highly trained licensed clinicians who can respond to their immediate mental health needs within the initial hours and days following their arrival in the United States, and such children should be released rapidly from government custody and reunited with their families, said Dr. Baranowski, a coauthor of the Social Science & Medicine study.
“We need to effectively support their integration into the community, and connect children and their families with linguistically, culturally, and developmentally appropriate trauma-informed pro bono treatment services that respond to their experiences” of premigration, migration, and postmigration stressors, “as well as potential exposure to trauma,” she said in an interview.
The OIG issued several recommendations for practical steps that ORR can take to assist facilities and better provide mental health care to immigrant children in federal custody. The agency advised that the ORR should provide facilities with evidence-based guidance on addressing trauma in short-term therapy and that the ORR also should develop strategies for overcoming challenges to hiring and retaining qualified mental health clinicians.
The Office of Inspector General also suggested that facilities consider maximum caseloads for individual clinicians. Finally, the OIG recommends that ORR address gaps in options for children who require more specialized treatment and that the office take reasonable steps to minimize the length of time that children remain in custody.
agallegos@mdedge.com
*This article was updated 9/5/2019.
Care providers encountered significant challenges when addressing the mental health needs of unaccompanied immigrant children in federal custody, including overwhelming caseloads and the deteriorating mental health of some patients, according to a new report by the Office of Inspector General (OIG).
In the report, released Sept. 3, the OIG outlined findings from its analysis of 45 Office of Refugee Resettlement (ORR) facilities between August and September 2018. The U.S. Department of Health & Human Services ORR is the legal custodian of unaccompanied immigrant children in its care who have no parent or legal guardian available. This includes children who arrive in the United States unaccompanied and children who are separated from their parents or guardians by immigration authorities after arriving in the country.
For the analysis, OIG investigators collected data from interviews with mental health clinicians, medical coordinators, facility leadership, and ORR federal field specialists at the 45 selected facilities.
Investigators recorded numerous serious challenges experienced by providers when attempting to provide mental health care to the children. Namely, they cited overwhelming patient caseloads, and difficulty accessing external mental health clinicians and referring children to providers within ORR’s network, according to the OIG’s report.
Mental health clinicians reported that the high caseloads hurt their ability to build rapport with young patients – and allowed less time for counseling and less frequent sessions for children with greater needs. The heavy caseloads were generated by heightened immigration enforcement beginning in 2017, and the separation of many more families at the border and more children being placed in federal custody, according to the report.
In addition, providers reported challenges when addressing the mental health needs of children who had experienced significant trauma before coming into federal custody. This included trauma that occurred while the children lived in the countries of origin, trauma during their journey to the United States, and trauma upon their arrival in the United States.
Separation from parents and a chaotic reunification process added to the trauma that children had already experienced, providers reported, and put extreme pressure on facility staff. Separated children exhibited “more fear, feelings of abandonment, and posttraumatic stress than did children who were not separated,” according to the findings. Separated children also experienced elevated feelings of anxiety and loss as a consequence of unexpected separation from loved ones.
Also, facilities reported that longer lengths of stay resulted in deteriorating mental health for some children and increased demands on staff. Facilities reported that children who stayed in federal custody for longer periods experienced more stress, anxiety, and behavioral issues. According to the facilities, the longer stays resulted in higher levels of defiance, hopelessness, and frustration among children – in addition to more instances of self-harm and suicidal ideation.
It is not surprising that the OIG study reflects that mental health services at facilities for unaccompanied minors are understaffed, undertrained, and overwhelmed, said Craig L. Katz, MD, a clinical professor of psychiatry at Mount Sinai in New York.
“In some sense, this can probably be said for most of the U.S. and definitely the world when it comes to child mental health services,” Dr. Katz said in an interview. “But, what’s especially tough to stomach about this shortfall at these facilities is that they encompass an immensely high-risk population – an inevitably highly, if not multiply traumatized population of children who lack primary caregivers.”
Dr. Katz was coinvestigator of a recent study that assessed the mental health of children held at a U.S. immigration detention center through the Parent-Report Strengths and Difficulties Questionnaire. Among the 425 children evaluated, many demonstrated elevated scores for emotional problems, peer problems, and total difficulties, according to the June 2018 study, published in Social Science & Medicine (2019 Jun; 230:303-8). Younger children (aged 4-8 years) demonstrated more difficulties associated with conduct, hyperactivity, and total difficulties, compared with older children, the study found.
Children who had been forcibly separated from their mothers demonstrated significantly more emotional problems and total difficulties, compared with those who had never been separated. Of 150 children who completed the Posttraumatic Stress Disorder Reaction Index, 17% had a probable diagnosis of PTSD, results found.
Dr. Katz said the OIG reached the same basic conclusion as his quantitative study – that separated minors appear to have even greater mental health problems than do fellow unaccompanied minors.
“In our study, we found that children in family detention had greater mental health problems than [did] American community samples but that formerly separated children who had been reunited with their mothers had even more health problems than their fellow detainees,” Dr. Katz said. “Something about being separated per U.S. policy was especially pernicious, which we knew in our hearts; but now in this study and ours, we know empirically.”
As long as the United States continues to detain children, the psychological harm created by such detainments is likely to continue, said Kim A. Baranowski, PhD, a psychologist and lecturer at Columbia University in New York. At a minimum, unaccompanied minors should have access to highly trained licensed clinicians who can respond to their immediate mental health needs within the initial hours and days following their arrival in the United States, and such children should be released rapidly from government custody and reunited with their families, said Dr. Baranowski, a coauthor of the Social Science & Medicine study.
“We need to effectively support their integration into the community, and connect children and their families with linguistically, culturally, and developmentally appropriate trauma-informed pro bono treatment services that respond to their experiences” of premigration, migration, and postmigration stressors, “as well as potential exposure to trauma,” she said in an interview.
The OIG issued several recommendations for practical steps that ORR can take to assist facilities and better provide mental health care to immigrant children in federal custody. The agency advised that the ORR should provide facilities with evidence-based guidance on addressing trauma in short-term therapy and that the ORR also should develop strategies for overcoming challenges to hiring and retaining qualified mental health clinicians.
The Office of Inspector General also suggested that facilities consider maximum caseloads for individual clinicians. Finally, the OIG recommends that ORR address gaps in options for children who require more specialized treatment and that the office take reasonable steps to minimize the length of time that children remain in custody.
agallegos@mdedge.com
*This article was updated 9/5/2019.
Care providers encountered significant challenges when addressing the mental health needs of unaccompanied immigrant children in federal custody, including overwhelming caseloads and the deteriorating mental health of some patients, according to a new report by the Office of Inspector General (OIG).
In the report, released Sept. 3, the OIG outlined findings from its analysis of 45 Office of Refugee Resettlement (ORR) facilities between August and September 2018. The U.S. Department of Health & Human Services ORR is the legal custodian of unaccompanied immigrant children in its care who have no parent or legal guardian available. This includes children who arrive in the United States unaccompanied and children who are separated from their parents or guardians by immigration authorities after arriving in the country.
For the analysis, OIG investigators collected data from interviews with mental health clinicians, medical coordinators, facility leadership, and ORR federal field specialists at the 45 selected facilities.
Investigators recorded numerous serious challenges experienced by providers when attempting to provide mental health care to the children. Namely, they cited overwhelming patient caseloads, and difficulty accessing external mental health clinicians and referring children to providers within ORR’s network, according to the OIG’s report.
Mental health clinicians reported that the high caseloads hurt their ability to build rapport with young patients – and allowed less time for counseling and less frequent sessions for children with greater needs. The heavy caseloads were generated by heightened immigration enforcement beginning in 2017, and the separation of many more families at the border and more children being placed in federal custody, according to the report.
In addition, providers reported challenges when addressing the mental health needs of children who had experienced significant trauma before coming into federal custody. This included trauma that occurred while the children lived in the countries of origin, trauma during their journey to the United States, and trauma upon their arrival in the United States.
Separation from parents and a chaotic reunification process added to the trauma that children had already experienced, providers reported, and put extreme pressure on facility staff. Separated children exhibited “more fear, feelings of abandonment, and posttraumatic stress than did children who were not separated,” according to the findings. Separated children also experienced elevated feelings of anxiety and loss as a consequence of unexpected separation from loved ones.
Also, facilities reported that longer lengths of stay resulted in deteriorating mental health for some children and increased demands on staff. Facilities reported that children who stayed in federal custody for longer periods experienced more stress, anxiety, and behavioral issues. According to the facilities, the longer stays resulted in higher levels of defiance, hopelessness, and frustration among children – in addition to more instances of self-harm and suicidal ideation.
It is not surprising that the OIG study reflects that mental health services at facilities for unaccompanied minors are understaffed, undertrained, and overwhelmed, said Craig L. Katz, MD, a clinical professor of psychiatry at Mount Sinai in New York.
“In some sense, this can probably be said for most of the U.S. and definitely the world when it comes to child mental health services,” Dr. Katz said in an interview. “But, what’s especially tough to stomach about this shortfall at these facilities is that they encompass an immensely high-risk population – an inevitably highly, if not multiply traumatized population of children who lack primary caregivers.”
Dr. Katz was coinvestigator of a recent study that assessed the mental health of children held at a U.S. immigration detention center through the Parent-Report Strengths and Difficulties Questionnaire. Among the 425 children evaluated, many demonstrated elevated scores for emotional problems, peer problems, and total difficulties, according to the June 2018 study, published in Social Science & Medicine (2019 Jun; 230:303-8). Younger children (aged 4-8 years) demonstrated more difficulties associated with conduct, hyperactivity, and total difficulties, compared with older children, the study found.
Children who had been forcibly separated from their mothers demonstrated significantly more emotional problems and total difficulties, compared with those who had never been separated. Of 150 children who completed the Posttraumatic Stress Disorder Reaction Index, 17% had a probable diagnosis of PTSD, results found.
Dr. Katz said the OIG reached the same basic conclusion as his quantitative study – that separated minors appear to have even greater mental health problems than do fellow unaccompanied minors.
“In our study, we found that children in family detention had greater mental health problems than [did] American community samples but that formerly separated children who had been reunited with their mothers had even more health problems than their fellow detainees,” Dr. Katz said. “Something about being separated per U.S. policy was especially pernicious, which we knew in our hearts; but now in this study and ours, we know empirically.”
As long as the United States continues to detain children, the psychological harm created by such detainments is likely to continue, said Kim A. Baranowski, PhD, a psychologist and lecturer at Columbia University in New York. At a minimum, unaccompanied minors should have access to highly trained licensed clinicians who can respond to their immediate mental health needs within the initial hours and days following their arrival in the United States, and such children should be released rapidly from government custody and reunited with their families, said Dr. Baranowski, a coauthor of the Social Science & Medicine study.
“We need to effectively support their integration into the community, and connect children and their families with linguistically, culturally, and developmentally appropriate trauma-informed pro bono treatment services that respond to their experiences” of premigration, migration, and postmigration stressors, “as well as potential exposure to trauma,” she said in an interview.
The OIG issued several recommendations for practical steps that ORR can take to assist facilities and better provide mental health care to immigrant children in federal custody. The agency advised that the ORR should provide facilities with evidence-based guidance on addressing trauma in short-term therapy and that the ORR also should develop strategies for overcoming challenges to hiring and retaining qualified mental health clinicians.
The Office of Inspector General also suggested that facilities consider maximum caseloads for individual clinicians. Finally, the OIG recommends that ORR address gaps in options for children who require more specialized treatment and that the office take reasonable steps to minimize the length of time that children remain in custody.
agallegos@mdedge.com
*This article was updated 9/5/2019.