User login
Commentary: Should AVFs be ligated after kidney transplant?
Hemodynamic complications of arteriovenous (AV) access are uncommon but can be potentially life threatening. Fistulas and grafts can cause a decrease in systemic vascular resistance and secondary increase in cardiac output in patients who may already have myocardial dysfunction secondary to their end-stage renal disease.1 This increased cardiac output is usually insignificant but in rare cases can result in clinically significant cardiac failure. Patients with high-output fistulas with volume flow greater than 2 L/min may be at increased risk of heart failure but volume flow less than 2 L/min does not preclude this complication.2
In patients with AV access–related heart failure, optimal medical management and reduction of fistula flow or ligation of the dialysis access should be considered. If continued hemodialysis is necessary, loss of a functioning dialysis access is problematic and difficult management decisions must be made. Following successful renal transplantation, ligation of vascular access in the presence of symptomatic heart failure may represent a straightforward decision. Nonetheless, there is no clear consensus of how to manage patent fistulas or grafts in patients following renal transplantation in the absence of significant cardiac symptoms with particular concern to the important issues of transplant survival and long-term cardiac prognosis. Yaffe and Greenstein3 recommend preservation of almost all fistulas after transplantation in the absence of significant complications such as venous hypertension, pseudoaneurysm, significant high-output cardiac failure or hand ischemia. They recommend taking into account the 10-year adjusted renal transplantation graft survival rates and the relative paucity of donors, recognizing the possibility that the patient may have to return to dialysis at some point in the future. They also reference the lack of information regarding the beneficial impact of fistula ligation on cardiac morphology and function as a rationale for access preservation.
A recent presentation at the American Heart Association Scientific Sessions by Michael B. Stokes, MD,4 from the department of cardiology at Royal Adelaide Hospital in Australia, suggests that cardiovascular disease is responsible for 40% of deaths among kidney transplant recipients and that left ventricular (LV) mass is strongly associated with cardiovascular mortality.
He states that, although there is no guideline consensus on the management of an AV fistula following successful renal transplantation, the fistula continues to contribute adversely to cardiac remodeling and function. The lack of previous randomized controlled trials in this area led Dr. Stokes and his colleagues to randomly assign 64 patients at least 1 year following successful kidney transplantation with stable renal function and a functioning AV fistula to either fistula ligation or no intervention. All patients underwent cardiac MRI at baseline and 6 months.
The primary endpoint of decrease in LV mass at 6 months was significant in the ligation group but not in the control group. The ligation group also had significant decrease in LV end diastolic volume, LV end systolic volume, and multiple other parameters. In addition, NT-proBNP levels and left atrial volume were significantly reduced in the ligation group when compared with the control group. Complications in the ligation group included six patients with thrombosis of their fistula vein and two infections, all of which resolved with outpatient anti-inflammatory or antimicrobial therapy.
Dr. Stokes believes that control patients in his study face “persisting and substantial deleterious cardiac remodeling” and that “further investigation would clarify the impact of AV fistula ligation on clinical outcomes following kidney transplantation.”
I believe this is important information and represents the first randomized controlled data regarding the long-term adverse cardiac effects of a patent fistula after renal transplantation. Unfortunately, information regarding baseline fistula volume flow is not provided in this abstract. As discussed earlier, patients with high-flow fistulas may be at increased risk of heart failure and hemodynamic data can be critical in establishing an algorithm for managing these challenging patients.
Ligation of a functioning and asymptomatic access in a patient with a successful renal transplant should be recommended only after informed discussion with the patient weighing the ongoing potential negative effects on cardiac function of continued access patency versus the potential need for future hemodialysis. Dr. Stokes presents interesting data that must be considered in this controversy. I believe that, in the absence of a universally applicable algorithm, the clinical decision to recommend AV fistula ligation after successful kidney transplantation should be individualized and based on ongoing assessment of cardiac and renal function and fistula complications and hemodynamics.
References
1. Eur Heart J 2017;38:1913-23.
2. Nephrol Dial Transplant 2008;23:282-7.
3. J Vasc Access 2012;13:405-8.
4. Stokes MB, et al. LBS.05 – Late Breaking Clinical Trial: Hot News in HF. Presented at American Heart Association Scientific Sessions. 2018 Nov 10-12. Chicago.
Larry A. Scher, MD, is a vascular surgeon at the Montefiore Greene Medical Arts Pavilion, New York, and an associate medical editor for Vascular Specialist.
Hemodynamic complications of arteriovenous (AV) access are uncommon but can be potentially life threatening. Fistulas and grafts can cause a decrease in systemic vascular resistance and secondary increase in cardiac output in patients who may already have myocardial dysfunction secondary to their end-stage renal disease.1 This increased cardiac output is usually insignificant but in rare cases can result in clinically significant cardiac failure. Patients with high-output fistulas with volume flow greater than 2 L/min may be at increased risk of heart failure but volume flow less than 2 L/min does not preclude this complication.2
In patients with AV access–related heart failure, optimal medical management and reduction of fistula flow or ligation of the dialysis access should be considered. If continued hemodialysis is necessary, loss of a functioning dialysis access is problematic and difficult management decisions must be made. Following successful renal transplantation, ligation of vascular access in the presence of symptomatic heart failure may represent a straightforward decision. Nonetheless, there is no clear consensus of how to manage patent fistulas or grafts in patients following renal transplantation in the absence of significant cardiac symptoms with particular concern to the important issues of transplant survival and long-term cardiac prognosis. Yaffe and Greenstein3 recommend preservation of almost all fistulas after transplantation in the absence of significant complications such as venous hypertension, pseudoaneurysm, significant high-output cardiac failure or hand ischemia. They recommend taking into account the 10-year adjusted renal transplantation graft survival rates and the relative paucity of donors, recognizing the possibility that the patient may have to return to dialysis at some point in the future. They also reference the lack of information regarding the beneficial impact of fistula ligation on cardiac morphology and function as a rationale for access preservation.
A recent presentation at the American Heart Association Scientific Sessions by Michael B. Stokes, MD,4 from the department of cardiology at Royal Adelaide Hospital in Australia, suggests that cardiovascular disease is responsible for 40% of deaths among kidney transplant recipients and that left ventricular (LV) mass is strongly associated with cardiovascular mortality.
He states that, although there is no guideline consensus on the management of an AV fistula following successful renal transplantation, the fistula continues to contribute adversely to cardiac remodeling and function. The lack of previous randomized controlled trials in this area led Dr. Stokes and his colleagues to randomly assign 64 patients at least 1 year following successful kidney transplantation with stable renal function and a functioning AV fistula to either fistula ligation or no intervention. All patients underwent cardiac MRI at baseline and 6 months.
The primary endpoint of decrease in LV mass at 6 months was significant in the ligation group but not in the control group. The ligation group also had significant decrease in LV end diastolic volume, LV end systolic volume, and multiple other parameters. In addition, NT-proBNP levels and left atrial volume were significantly reduced in the ligation group when compared with the control group. Complications in the ligation group included six patients with thrombosis of their fistula vein and two infections, all of which resolved with outpatient anti-inflammatory or antimicrobial therapy.
Dr. Stokes believes that control patients in his study face “persisting and substantial deleterious cardiac remodeling” and that “further investigation would clarify the impact of AV fistula ligation on clinical outcomes following kidney transplantation.”
I believe this is important information and represents the first randomized controlled data regarding the long-term adverse cardiac effects of a patent fistula after renal transplantation. Unfortunately, information regarding baseline fistula volume flow is not provided in this abstract. As discussed earlier, patients with high-flow fistulas may be at increased risk of heart failure and hemodynamic data can be critical in establishing an algorithm for managing these challenging patients.
Ligation of a functioning and asymptomatic access in a patient with a successful renal transplant should be recommended only after informed discussion with the patient weighing the ongoing potential negative effects on cardiac function of continued access patency versus the potential need for future hemodialysis. Dr. Stokes presents interesting data that must be considered in this controversy. I believe that, in the absence of a universally applicable algorithm, the clinical decision to recommend AV fistula ligation after successful kidney transplantation should be individualized and based on ongoing assessment of cardiac and renal function and fistula complications and hemodynamics.
References
1. Eur Heart J 2017;38:1913-23.
2. Nephrol Dial Transplant 2008;23:282-7.
3. J Vasc Access 2012;13:405-8.
4. Stokes MB, et al. LBS.05 – Late Breaking Clinical Trial: Hot News in HF. Presented at American Heart Association Scientific Sessions. 2018 Nov 10-12. Chicago.
Larry A. Scher, MD, is a vascular surgeon at the Montefiore Greene Medical Arts Pavilion, New York, and an associate medical editor for Vascular Specialist.
Hemodynamic complications of arteriovenous (AV) access are uncommon but can be potentially life threatening. Fistulas and grafts can cause a decrease in systemic vascular resistance and secondary increase in cardiac output in patients who may already have myocardial dysfunction secondary to their end-stage renal disease.1 This increased cardiac output is usually insignificant but in rare cases can result in clinically significant cardiac failure. Patients with high-output fistulas with volume flow greater than 2 L/min may be at increased risk of heart failure but volume flow less than 2 L/min does not preclude this complication.2
In patients with AV access–related heart failure, optimal medical management and reduction of fistula flow or ligation of the dialysis access should be considered. If continued hemodialysis is necessary, loss of a functioning dialysis access is problematic and difficult management decisions must be made. Following successful renal transplantation, ligation of vascular access in the presence of symptomatic heart failure may represent a straightforward decision. Nonetheless, there is no clear consensus of how to manage patent fistulas or grafts in patients following renal transplantation in the absence of significant cardiac symptoms with particular concern to the important issues of transplant survival and long-term cardiac prognosis. Yaffe and Greenstein3 recommend preservation of almost all fistulas after transplantation in the absence of significant complications such as venous hypertension, pseudoaneurysm, significant high-output cardiac failure or hand ischemia. They recommend taking into account the 10-year adjusted renal transplantation graft survival rates and the relative paucity of donors, recognizing the possibility that the patient may have to return to dialysis at some point in the future. They also reference the lack of information regarding the beneficial impact of fistula ligation on cardiac morphology and function as a rationale for access preservation.
A recent presentation at the American Heart Association Scientific Sessions by Michael B. Stokes, MD,4 from the department of cardiology at Royal Adelaide Hospital in Australia, suggests that cardiovascular disease is responsible for 40% of deaths among kidney transplant recipients and that left ventricular (LV) mass is strongly associated with cardiovascular mortality.
He states that, although there is no guideline consensus on the management of an AV fistula following successful renal transplantation, the fistula continues to contribute adversely to cardiac remodeling and function. The lack of previous randomized controlled trials in this area led Dr. Stokes and his colleagues to randomly assign 64 patients at least 1 year following successful kidney transplantation with stable renal function and a functioning AV fistula to either fistula ligation or no intervention. All patients underwent cardiac MRI at baseline and 6 months.
The primary endpoint of decrease in LV mass at 6 months was significant in the ligation group but not in the control group. The ligation group also had significant decrease in LV end diastolic volume, LV end systolic volume, and multiple other parameters. In addition, NT-proBNP levels and left atrial volume were significantly reduced in the ligation group when compared with the control group. Complications in the ligation group included six patients with thrombosis of their fistula vein and two infections, all of which resolved with outpatient anti-inflammatory or antimicrobial therapy.
Dr. Stokes believes that control patients in his study face “persisting and substantial deleterious cardiac remodeling” and that “further investigation would clarify the impact of AV fistula ligation on clinical outcomes following kidney transplantation.”
I believe this is important information and represents the first randomized controlled data regarding the long-term adverse cardiac effects of a patent fistula after renal transplantation. Unfortunately, information regarding baseline fistula volume flow is not provided in this abstract. As discussed earlier, patients with high-flow fistulas may be at increased risk of heart failure and hemodynamic data can be critical in establishing an algorithm for managing these challenging patients.
Ligation of a functioning and asymptomatic access in a patient with a successful renal transplant should be recommended only after informed discussion with the patient weighing the ongoing potential negative effects on cardiac function of continued access patency versus the potential need for future hemodialysis. Dr. Stokes presents interesting data that must be considered in this controversy. I believe that, in the absence of a universally applicable algorithm, the clinical decision to recommend AV fistula ligation after successful kidney transplantation should be individualized and based on ongoing assessment of cardiac and renal function and fistula complications and hemodynamics.
References
1. Eur Heart J 2017;38:1913-23.
2. Nephrol Dial Transplant 2008;23:282-7.
3. J Vasc Access 2012;13:405-8.
4. Stokes MB, et al. LBS.05 – Late Breaking Clinical Trial: Hot News in HF. Presented at American Heart Association Scientific Sessions. 2018 Nov 10-12. Chicago.
Larry A. Scher, MD, is a vascular surgeon at the Montefiore Greene Medical Arts Pavilion, New York, and an associate medical editor for Vascular Specialist.
Perceptions of liver transplantation for ALD are evolving
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
One of the most significant findings of the study by Brian P. Lee, MD, and his colleagues is the major shift in attitudes surrounding the eligibility criteria for patients with ALD to undergo liver transplantation.
More than 3 decades ago, a group of surgical experts gathered together to discuss evaluation criteria for candidacy of individuals to undergo liver transplantation. They recommended that patients with ALD be required to restrict alcohol consumption for 6 months prior to being listed eligible for surgery. The group presumed that a period of complete avoidance may induce some degree of disease remission, circumventing the need for transplant altogether.
However, these suggestions were given without the use of evidence, formed largely on the basis of opinion, and recent data dispute these recommendations. On the contrary, relapse rates for alcohol use disorder has been shown to be due to factors other than length of abstinence. While these findings have lessened bias surrounding ALD and liver transplantation, the assumption still remains prevalent in clinical practice today.
These results highlight the unanswered question of how to best approach treatment of individuals with ALD, and whether the recent rise of patients undergoing liver transplantation for ALD, without a continued duration of abstinence, should be a concern of clinicians.
Mack C. Mitchell, MD, is affiliated with the department of internal medicine at the University of Texas in Dallas. Dr. Mitchell reported having financial affiliations with the National Institute of Alcohol and Alcohol Abuse. These comments are adapted from his accompanying editorial (JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6532 ).
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
“The findings suggest that early liver transplant for alcoholic hepatitis may be leading to broader acceptance of ALD for liver transplant,” Brian P. Lee, MD, of the University of California, San Francisco, and his colleagues wrote in JAMA Internal Medicine.
The researchers conducted a prospective cohort study of 9,438 patients with ALD who received a liver transplant from 2002 to 2016. Data were obtained from the United Network for Organ Sharing national database.
Study participants were evaluated for patterns, both nationally and regionally, related to liver transplant for the treatment of ALD. In addition, Dr. Lee and his colleagues completed a sensitivity analysis, which evaluated specific clinical parameters, including patient and graft survival, hepatocellular carcinoma (HCC), and hepatitis C viral (HCV) infection.
“Because there is no national policy regarding early liver transplant, we hypothesized that changes may vary regionally as liver transplant programs shifted their attitudes toward increased acceptance of early liver transplant for alcoholic hepatitis and ALD,” the researchers wrote.
After analysis, the researchers found that liver transplantation for patients with ALD increased proportionally from 24.2% to 36.7% from 2002 to 2016, respectively. With HCV-infected recipients included, the proportion of liver transplants rose from 15.3% to 30.6% over the same period, representing a twofold increase of transplants received for this indication.
The degree of increase was reported to vary based on geographic region and was linked with differences in patient-specific factors.
“There may be regional disparities in access to liver transplant for ALD; whether this is related to different attitudes toward ALD and requirements for sobriety is unknown,” they added.
The researchers acknowledged that a key limitation of the study was the use of registry data. As a result, Dr. Lee and his colleagues reported that all conclusions are not causal, but rather only by association.
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interests.
SOURCE: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Liver transplantation for alcohol-associated liver disease (ALD) is occurring earlier and more frequently than before.
Major finding: The proportion of patients undergoing liver transplantation for ALD has nearly doubled from 2002 to 2016.
Study details: A prospective cohort study of 9,438 patients who underwent liver transplant for ALD in the United States from 2002 to 2016.
Disclosures: The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases UCSF Liver Center. The authors reported no conflicts of interest.
Source: Lee BP et al. JAMA Intern Med. 2019 Jan 22. doi: 10.1001/jamainternmed.2018.6536.
Renal transplant improves survival in lupus nephritis patients
, according to researchers who conducted a nationwide cohort study encompassing nearly all such patients treated in the United States over a 20-year period.
Transplant conferred a 70% reduction in overall death risk in these lupus nephritis end-stage renal disease (ESRD) patients, largely due to reduced deaths caused by infection and cardiovascular disease, according to the researchers, led by April Jorge, MD, and Zachary Wallace, MD, of Massachusetts General Hospital, Harvard Medical School, Boston.
Those findings suggest that patients with lupus nephritis ESRD should routinely be considered for renal transplant in a timely manner, the investigators wrote in Annals of Internal Medicine.
“Improved access to renal transplantation for this population may considerably improve outcomes,” they said.
The study was based on an analysis of 9,659 patients who had lupus nephritis ESRD between 1995 and 2014 and were waitlisted for renal transplant. The data came from the United States Renal Data System, which includes most ESRD patients treated in the country. Of those 9,659 patients, 5,738 (59%) underwent kidney transplant.
Mortality rates were 22.5 per 1,000 person-years for lupus nephritis ESRD patients who underwent transplant, and 56.3 per 1,000 person-years for those patients who did not receive transplant, the investigators found.
Renal transplant reduced risk of death by 70% in results of multivariate analysis (hazard ratio, 0.30; 95% CI, 0.27-0.33).
That lower risk of all-cause mortality was consistent across racial groups and for other characteristics, such as sex, age at ESRD onset, and Medicare enrollment status.
Risk of cardiovascular death was 74% lower with renal transplant (adjusted hazard ratio, 0.26; 95% CI, 0.23-0.30), and risk of death from infection was also markedly lower among those who underwent transplant (adjusted hazard ratio, 0.41; 95% CI, 0.32-0.52), investigators found in a cause-specific mortality analysis.
While transplant has been associated with improved survival in patients with ESRD from all causes, there are “unique concerns” regarding the potential for infections or other post-transplant complications from transplant in lupus nephritis patients with ESRD, Dr. Jorge and colleagues wrote.
“To that end, our study provides evidence for a substantial survival benefit of renal transplant among patients with lupus nephritis ESRD,” they noted.
Dr. Jorge reported grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases during the conduct of the study. One co-author provided additional disclosures related to Teva Pharmaceuticals and Gilead Sciences outside of the study conduct.
SOURCE: Jorge A, et al. Ann Intern Med 2019 Jan 21. doi: 10.7326/M18-1570.
This research by Jorge et al is “strong” and has two key implications for clinical practice, said authors of an accompanying editorial in the Annals of Internal Medicine.
The first is that transplantation should be incorporated into the treatment plan for lupus nephritis patients and is particularly important before kidney failure onset, according to Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD.
“This will allow patients, families, and clinicians to devote sufficient resources to completing the transplant evaluation and searching for living donors, the preferred donor source to maximize patient and allograft survival,” they wrote.
Secondly, the evidence to date suggests wider implementation of preemptive kidney transplants would be warranted in patients with lupus nephritis, they said.
Currently, only about 9% of lupus nephritis patients with kidney failure related to lupus nephritis undergo preemptive transplants, versus 17% of patients undergoing kidney transplants for other reasons, according to the authors.
Recent studies, however, suggest preemptive transplants and early kidney transplants in lupus nephritis are indeed linked to improved patient and allograft survival, just as in other conditions, they added.
Taken together, the findings of those studies and the current study by Dr. Jorge and colleagues underscore the pronounced survival advantage attributable to kidney transplant in patients with kidney failure due to lupus nephritis, they concluded.
“It is essential that transplant be considered as promptly as possible for patients with lupus nephritis and that barriers to early transplant be surmounted,” they wrote.
The editorial was authored by Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD, of Tufts Medical Center, Boston. Dr. Goyal and Dr. Levey reported no conflicts of interest. Dr. Weiner provided disclosures related to Keryx Biopharmaceuticals, Relypsa, Inc., Janssen Biopharmaceuticals, Akebia Therapeutics, and others.
This research by Jorge et al is “strong” and has two key implications for clinical practice, said authors of an accompanying editorial in the Annals of Internal Medicine.
The first is that transplantation should be incorporated into the treatment plan for lupus nephritis patients and is particularly important before kidney failure onset, according to Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD.
“This will allow patients, families, and clinicians to devote sufficient resources to completing the transplant evaluation and searching for living donors, the preferred donor source to maximize patient and allograft survival,” they wrote.
Secondly, the evidence to date suggests wider implementation of preemptive kidney transplants would be warranted in patients with lupus nephritis, they said.
Currently, only about 9% of lupus nephritis patients with kidney failure related to lupus nephritis undergo preemptive transplants, versus 17% of patients undergoing kidney transplants for other reasons, according to the authors.
Recent studies, however, suggest preemptive transplants and early kidney transplants in lupus nephritis are indeed linked to improved patient and allograft survival, just as in other conditions, they added.
Taken together, the findings of those studies and the current study by Dr. Jorge and colleagues underscore the pronounced survival advantage attributable to kidney transplant in patients with kidney failure due to lupus nephritis, they concluded.
“It is essential that transplant be considered as promptly as possible for patients with lupus nephritis and that barriers to early transplant be surmounted,” they wrote.
The editorial was authored by Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD, of Tufts Medical Center, Boston. Dr. Goyal and Dr. Levey reported no conflicts of interest. Dr. Weiner provided disclosures related to Keryx Biopharmaceuticals, Relypsa, Inc., Janssen Biopharmaceuticals, Akebia Therapeutics, and others.
This research by Jorge et al is “strong” and has two key implications for clinical practice, said authors of an accompanying editorial in the Annals of Internal Medicine.
The first is that transplantation should be incorporated into the treatment plan for lupus nephritis patients and is particularly important before kidney failure onset, according to Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD.
“This will allow patients, families, and clinicians to devote sufficient resources to completing the transplant evaluation and searching for living donors, the preferred donor source to maximize patient and allograft survival,” they wrote.
Secondly, the evidence to date suggests wider implementation of preemptive kidney transplants would be warranted in patients with lupus nephritis, they said.
Currently, only about 9% of lupus nephritis patients with kidney failure related to lupus nephritis undergo preemptive transplants, versus 17% of patients undergoing kidney transplants for other reasons, according to the authors.
Recent studies, however, suggest preemptive transplants and early kidney transplants in lupus nephritis are indeed linked to improved patient and allograft survival, just as in other conditions, they added.
Taken together, the findings of those studies and the current study by Dr. Jorge and colleagues underscore the pronounced survival advantage attributable to kidney transplant in patients with kidney failure due to lupus nephritis, they concluded.
“It is essential that transplant be considered as promptly as possible for patients with lupus nephritis and that barriers to early transplant be surmounted,” they wrote.
The editorial was authored by Nitender Goyal, MD, Daniel E. Weiner, MD, MS, and Andrew S. Levey, MD, of Tufts Medical Center, Boston. Dr. Goyal and Dr. Levey reported no conflicts of interest. Dr. Weiner provided disclosures related to Keryx Biopharmaceuticals, Relypsa, Inc., Janssen Biopharmaceuticals, Akebia Therapeutics, and others.
, according to researchers who conducted a nationwide cohort study encompassing nearly all such patients treated in the United States over a 20-year period.
Transplant conferred a 70% reduction in overall death risk in these lupus nephritis end-stage renal disease (ESRD) patients, largely due to reduced deaths caused by infection and cardiovascular disease, according to the researchers, led by April Jorge, MD, and Zachary Wallace, MD, of Massachusetts General Hospital, Harvard Medical School, Boston.
Those findings suggest that patients with lupus nephritis ESRD should routinely be considered for renal transplant in a timely manner, the investigators wrote in Annals of Internal Medicine.
“Improved access to renal transplantation for this population may considerably improve outcomes,” they said.
The study was based on an analysis of 9,659 patients who had lupus nephritis ESRD between 1995 and 2014 and were waitlisted for renal transplant. The data came from the United States Renal Data System, which includes most ESRD patients treated in the country. Of those 9,659 patients, 5,738 (59%) underwent kidney transplant.
Mortality rates were 22.5 per 1,000 person-years for lupus nephritis ESRD patients who underwent transplant, and 56.3 per 1,000 person-years for those patients who did not receive transplant, the investigators found.
Renal transplant reduced risk of death by 70% in results of multivariate analysis (hazard ratio, 0.30; 95% CI, 0.27-0.33).
That lower risk of all-cause mortality was consistent across racial groups and for other characteristics, such as sex, age at ESRD onset, and Medicare enrollment status.
Risk of cardiovascular death was 74% lower with renal transplant (adjusted hazard ratio, 0.26; 95% CI, 0.23-0.30), and risk of death from infection was also markedly lower among those who underwent transplant (adjusted hazard ratio, 0.41; 95% CI, 0.32-0.52), investigators found in a cause-specific mortality analysis.
While transplant has been associated with improved survival in patients with ESRD from all causes, there are “unique concerns” regarding the potential for infections or other post-transplant complications from transplant in lupus nephritis patients with ESRD, Dr. Jorge and colleagues wrote.
“To that end, our study provides evidence for a substantial survival benefit of renal transplant among patients with lupus nephritis ESRD,” they noted.
Dr. Jorge reported grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases during the conduct of the study. One co-author provided additional disclosures related to Teva Pharmaceuticals and Gilead Sciences outside of the study conduct.
SOURCE: Jorge A, et al. Ann Intern Med 2019 Jan 21. doi: 10.7326/M18-1570.
, according to researchers who conducted a nationwide cohort study encompassing nearly all such patients treated in the United States over a 20-year period.
Transplant conferred a 70% reduction in overall death risk in these lupus nephritis end-stage renal disease (ESRD) patients, largely due to reduced deaths caused by infection and cardiovascular disease, according to the researchers, led by April Jorge, MD, and Zachary Wallace, MD, of Massachusetts General Hospital, Harvard Medical School, Boston.
Those findings suggest that patients with lupus nephritis ESRD should routinely be considered for renal transplant in a timely manner, the investigators wrote in Annals of Internal Medicine.
“Improved access to renal transplantation for this population may considerably improve outcomes,” they said.
The study was based on an analysis of 9,659 patients who had lupus nephritis ESRD between 1995 and 2014 and were waitlisted for renal transplant. The data came from the United States Renal Data System, which includes most ESRD patients treated in the country. Of those 9,659 patients, 5,738 (59%) underwent kidney transplant.
Mortality rates were 22.5 per 1,000 person-years for lupus nephritis ESRD patients who underwent transplant, and 56.3 per 1,000 person-years for those patients who did not receive transplant, the investigators found.
Renal transplant reduced risk of death by 70% in results of multivariate analysis (hazard ratio, 0.30; 95% CI, 0.27-0.33).
That lower risk of all-cause mortality was consistent across racial groups and for other characteristics, such as sex, age at ESRD onset, and Medicare enrollment status.
Risk of cardiovascular death was 74% lower with renal transplant (adjusted hazard ratio, 0.26; 95% CI, 0.23-0.30), and risk of death from infection was also markedly lower among those who underwent transplant (adjusted hazard ratio, 0.41; 95% CI, 0.32-0.52), investigators found in a cause-specific mortality analysis.
While transplant has been associated with improved survival in patients with ESRD from all causes, there are “unique concerns” regarding the potential for infections or other post-transplant complications from transplant in lupus nephritis patients with ESRD, Dr. Jorge and colleagues wrote.
“To that end, our study provides evidence for a substantial survival benefit of renal transplant among patients with lupus nephritis ESRD,” they noted.
Dr. Jorge reported grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases during the conduct of the study. One co-author provided additional disclosures related to Teva Pharmaceuticals and Gilead Sciences outside of the study conduct.
SOURCE: Jorge A, et al. Ann Intern Med 2019 Jan 21. doi: 10.7326/M18-1570.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Renal transplant is associated with a substantial survival benefit in patients with end-stage renal disease (ESRD) due to lupus nephritis,
Major finding: Transplant conferred a 70% reduction in overall death risk in these lupus nephritis ESRD patients, largely due to reduced deaths caused by infection and cardiovascular disease,
Study details: Analysis of 9,659 patients with lupus nephritis ESRD in the United States Renal Data System.
Disclosures: Support for the study came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One co-author provided disclosures related to Teva Pharmaceuticals and Gilead Sciences.
Source: Jorge A, et al. Ann Intern Med. 2019 Jan 21. doi: 10.7326/M18-1570.
Normothermic machine perfusion found to salvage fatty livers for transplantation
SAN FRANCISCO – results from a small trial showed.
“This is important in the context of liver transplantation, because fatty livers do very badly when their time is blunted,” study coauthor Carlo Ceresa, MBChB, MRCS, said during a press briefing at the annual meeting of the American Association for the Study of Liver Diseases. “They’re susceptible to ischemia reperfusion injury, and as a result, a large number are discarded. In the U.S., it’s estimated that around 6,000 steatotic livers are discarded each year. In the U.K., the picture is very similar. Because up to 20% of patients die on the waiting list for liver transplant, we need to try to identify methods to use more marginal organs. Unfortunately, with the obesity epidemic and obesity being a risk factor for NAFLD [nonalcoholic fatty liver disease], we find more fatty livers in the donor pool, and we aren’t able to use them. Identifying methods to salvage these livers for transplantation [is] of great importance.”
NMP maintains the liver in a fully functioning state ex situ and provides oxygen and nutrition at 37° C, said Dr. Ceresa, who is a clinical research fellow with the Medical Research Council and a PhD candidate at the University of Oxford, England. In an effort to evaluate the impact of NMP and defatting adjuncts on human steatotic livers, he and his colleagues perfused 18 discarded human steatotic livers on a normothermic, blood-based circuit for 48 hours. Of these, six were perfused by normothermic machine perfusion alone (group 1), while six were perfused by NMP plus apheresis filtration, which removes lipoproteins (group 2). “The hypothesis here was that we could mechanically remove the fat that the liver releases,” he said. The remaining six livers were perfused with NMP, lipid apheresis filtration, and defatting agents including
The livers in group 1 “did pretty badly,” Dr. Ceresa said. “Their function wasn’t great and within 48 hours deteriorated, and there was a slight increase in liver fat. That’s probably attributable to de novo lipogenesis.” However, the livers in groups 2 and 3 demonstrated a significant reduction in circulating triglycerides and in perfusate total cholesterol by 48 hours, compared with those in group 1. The researchers also observed an increase in median fatty acid oxidation as measured by 3-hydroxybutyrate among the livers in group 3, compared with those in groups 1 and 2. In addition, the livers in group 3 were the only ones to show a mean reduction in tissue triglyceride level.
Dr. Ceresa described the findings as “exciting, because we have a captive organ we can manipulate, which could then result in a successful transplantation,” he said. “You also get to test drive and get an objective assessment of the organ’s function before you transplant it, so the result may be more predictable. It gives us a very useful model to study NAFLD.”
The next step, he said, is to plan a clinical trial to determine if clinical outcomes can be improved through these ex situ interventions on steatotic livers.
Dr. Ceresa reported having no financial disclosures.
Source: Hepatology 2018;68[S1], Abstract 3.
SAN FRANCISCO – results from a small trial showed.
“This is important in the context of liver transplantation, because fatty livers do very badly when their time is blunted,” study coauthor Carlo Ceresa, MBChB, MRCS, said during a press briefing at the annual meeting of the American Association for the Study of Liver Diseases. “They’re susceptible to ischemia reperfusion injury, and as a result, a large number are discarded. In the U.S., it’s estimated that around 6,000 steatotic livers are discarded each year. In the U.K., the picture is very similar. Because up to 20% of patients die on the waiting list for liver transplant, we need to try to identify methods to use more marginal organs. Unfortunately, with the obesity epidemic and obesity being a risk factor for NAFLD [nonalcoholic fatty liver disease], we find more fatty livers in the donor pool, and we aren’t able to use them. Identifying methods to salvage these livers for transplantation [is] of great importance.”
NMP maintains the liver in a fully functioning state ex situ and provides oxygen and nutrition at 37° C, said Dr. Ceresa, who is a clinical research fellow with the Medical Research Council and a PhD candidate at the University of Oxford, England. In an effort to evaluate the impact of NMP and defatting adjuncts on human steatotic livers, he and his colleagues perfused 18 discarded human steatotic livers on a normothermic, blood-based circuit for 48 hours. Of these, six were perfused by normothermic machine perfusion alone (group 1), while six were perfused by NMP plus apheresis filtration, which removes lipoproteins (group 2). “The hypothesis here was that we could mechanically remove the fat that the liver releases,” he said. The remaining six livers were perfused with NMP, lipid apheresis filtration, and defatting agents including
The livers in group 1 “did pretty badly,” Dr. Ceresa said. “Their function wasn’t great and within 48 hours deteriorated, and there was a slight increase in liver fat. That’s probably attributable to de novo lipogenesis.” However, the livers in groups 2 and 3 demonstrated a significant reduction in circulating triglycerides and in perfusate total cholesterol by 48 hours, compared with those in group 1. The researchers also observed an increase in median fatty acid oxidation as measured by 3-hydroxybutyrate among the livers in group 3, compared with those in groups 1 and 2. In addition, the livers in group 3 were the only ones to show a mean reduction in tissue triglyceride level.
Dr. Ceresa described the findings as “exciting, because we have a captive organ we can manipulate, which could then result in a successful transplantation,” he said. “You also get to test drive and get an objective assessment of the organ’s function before you transplant it, so the result may be more predictable. It gives us a very useful model to study NAFLD.”
The next step, he said, is to plan a clinical trial to determine if clinical outcomes can be improved through these ex situ interventions on steatotic livers.
Dr. Ceresa reported having no financial disclosures.
Source: Hepatology 2018;68[S1], Abstract 3.
SAN FRANCISCO – results from a small trial showed.
“This is important in the context of liver transplantation, because fatty livers do very badly when their time is blunted,” study coauthor Carlo Ceresa, MBChB, MRCS, said during a press briefing at the annual meeting of the American Association for the Study of Liver Diseases. “They’re susceptible to ischemia reperfusion injury, and as a result, a large number are discarded. In the U.S., it’s estimated that around 6,000 steatotic livers are discarded each year. In the U.K., the picture is very similar. Because up to 20% of patients die on the waiting list for liver transplant, we need to try to identify methods to use more marginal organs. Unfortunately, with the obesity epidemic and obesity being a risk factor for NAFLD [nonalcoholic fatty liver disease], we find more fatty livers in the donor pool, and we aren’t able to use them. Identifying methods to salvage these livers for transplantation [is] of great importance.”
NMP maintains the liver in a fully functioning state ex situ and provides oxygen and nutrition at 37° C, said Dr. Ceresa, who is a clinical research fellow with the Medical Research Council and a PhD candidate at the University of Oxford, England. In an effort to evaluate the impact of NMP and defatting adjuncts on human steatotic livers, he and his colleagues perfused 18 discarded human steatotic livers on a normothermic, blood-based circuit for 48 hours. Of these, six were perfused by normothermic machine perfusion alone (group 1), while six were perfused by NMP plus apheresis filtration, which removes lipoproteins (group 2). “The hypothesis here was that we could mechanically remove the fat that the liver releases,” he said. The remaining six livers were perfused with NMP, lipid apheresis filtration, and defatting agents including
The livers in group 1 “did pretty badly,” Dr. Ceresa said. “Their function wasn’t great and within 48 hours deteriorated, and there was a slight increase in liver fat. That’s probably attributable to de novo lipogenesis.” However, the livers in groups 2 and 3 demonstrated a significant reduction in circulating triglycerides and in perfusate total cholesterol by 48 hours, compared with those in group 1. The researchers also observed an increase in median fatty acid oxidation as measured by 3-hydroxybutyrate among the livers in group 3, compared with those in groups 1 and 2. In addition, the livers in group 3 were the only ones to show a mean reduction in tissue triglyceride level.
Dr. Ceresa described the findings as “exciting, because we have a captive organ we can manipulate, which could then result in a successful transplantation,” he said. “You also get to test drive and get an objective assessment of the organ’s function before you transplant it, so the result may be more predictable. It gives us a very useful model to study NAFLD.”
The next step, he said, is to plan a clinical trial to determine if clinical outcomes can be improved through these ex situ interventions on steatotic livers.
Dr. Ceresa reported having no financial disclosures.
Source: Hepatology 2018;68[S1], Abstract 3.
AT THE LIVER MEETING 2018
Key clinical point: The addition of apheresis filtration and defatting agents to normothermic machine perfusion led to significant improvements in liver function.
Major finding: Livers which received apheresis filtration and defatting agents fared better than those that did not.
Study details: An analysis of 18 discarded human steatotic livers that were perfused on a normothermic, blood-based circuit for 48 hours.
Disclosures: Dr. Ceresa reported having no financial disclosures.
Source: Hepatology 2018;68[S1], Abstract 3.
Despite interest, few liver transplant candidates discuss advance care planning with clinicians
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: There is a paucity of documentation of advance care planning or identification of a durable power of attorney in the medical record of liver transplant candidates.
Major finding: Only 9% of liver transplant candidates reported completing advanced care planning prior to their liver transplant evaluations and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record.
Study details: A retrospective review of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco.
Disclosures: One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]:Abstract 771.
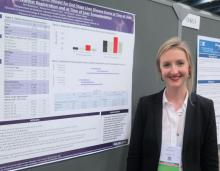
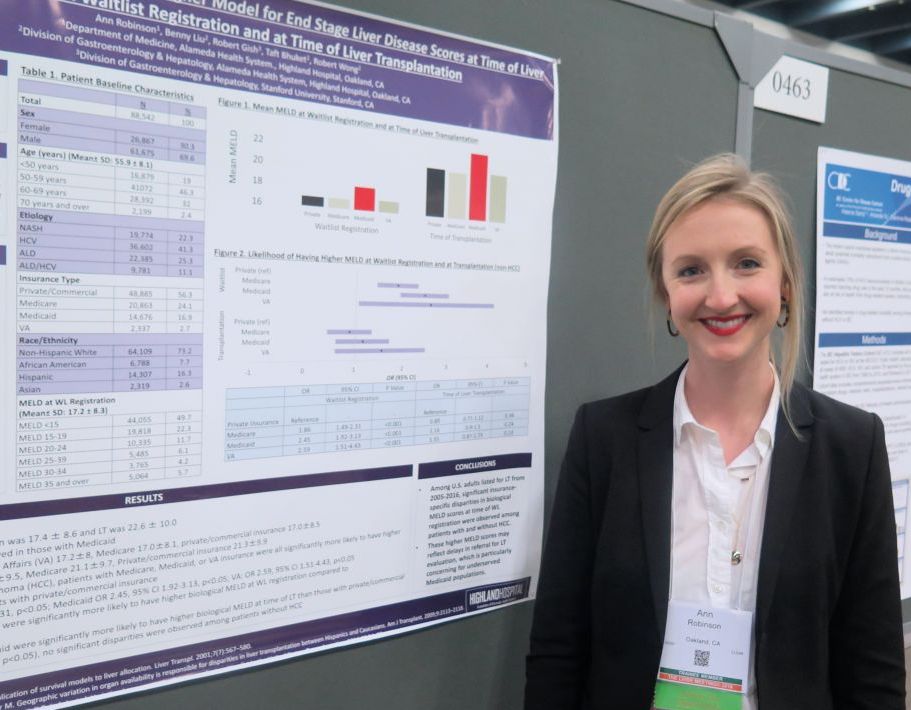
Medicaid patients have higher MELD scores at time of liver transplantation
SAN FRANCISCO – Despite implementation of the Model for End Stage Liver Disease score to prioritize liver transplantation, .
“It can be difficult for patients with Medicaid to access liver transplantation,” lead study author Ann Robinson, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “These patients may be living in underserved areas with limited resources.”
In an effort to evaluate insurance-specific disparities in severity of liver disease at the time of liver transplantation wait-list registration and at the time of liver transplantation, Dr. Robinson and her colleagues retrospectively evaluated the 2005-2016 United Network for Organ Sharing/Organ Procurement and Transplant Network liver transplant registry. They used multivariate linear regression models to make insurance-specific comparisons of MELD scores at wait-list registration and at liver transplantation, which included adjustments for age, sex, year, etiology of liver disease, body mass index, ascites, hepatocellular carcinoma (HCC), and hepatic encephalopathy.
Dr. Robinson, who is a third-year internal medicine resident at Highland Hospital, Oakland, Calif., reported findings from 88,542 liver transplantation wait-list registrants with a mean age of 56 years. Their overall mean MELD score was 17.4 at wait-list registration and 22.6 at time of liver transplantation. The greatest mean MELD score at the time of wait-list registration was observed in Medicaid patients (18.4, compared with 17.2 among Veterans Affairs patients, 17 among Medicare patients, and 17 among privately/commercially insured patients; P less than .01). Meanwhile, the greatest mean MELD score at the time of liver transplantation was observed in Medicaid patients (23.5, compared with 21.4 among VA patients, 21.3 among privately/commercially insured patients, and 21.1 among Medicare patients; P less than .01).
Multivariate regression analysis revealed that, among patients without hepatocellular carcinoma, those with coverage other than private or commercial insurance had significantly higher MELD scores at wait-list registration (P less than .01). Specifically, the odds ratio was highest for VA patients (odds ratio, 2.59), followed by those covered by Medicaid (OR, 2.45), and Medicare (OR, 1.86). Similar trends were observed in hepatocellular carcinoma patients, with the highest biological MELD score at wait-list seen in those covered by Medicaid.
On regression analysis, while Medicaid patients with hepatocellular carcinoma had significantly higher biological MELD scores at time of liver transplantation, compared with those with private/commercial insurance (Medicaid OR, 2.06; P less than .05), no differences were observed among patients without hepatocellular carcinoma.
Dr. Robinson reported having no financial disclosures.
Source: Hepatology 2018 Oct 1;68[S1], Abstract 464.
SAN FRANCISCO – Despite implementation of the Model for End Stage Liver Disease score to prioritize liver transplantation, .
“It can be difficult for patients with Medicaid to access liver transplantation,” lead study author Ann Robinson, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “These patients may be living in underserved areas with limited resources.”
In an effort to evaluate insurance-specific disparities in severity of liver disease at the time of liver transplantation wait-list registration and at the time of liver transplantation, Dr. Robinson and her colleagues retrospectively evaluated the 2005-2016 United Network for Organ Sharing/Organ Procurement and Transplant Network liver transplant registry. They used multivariate linear regression models to make insurance-specific comparisons of MELD scores at wait-list registration and at liver transplantation, which included adjustments for age, sex, year, etiology of liver disease, body mass index, ascites, hepatocellular carcinoma (HCC), and hepatic encephalopathy.
Dr. Robinson, who is a third-year internal medicine resident at Highland Hospital, Oakland, Calif., reported findings from 88,542 liver transplantation wait-list registrants with a mean age of 56 years. Their overall mean MELD score was 17.4 at wait-list registration and 22.6 at time of liver transplantation. The greatest mean MELD score at the time of wait-list registration was observed in Medicaid patients (18.4, compared with 17.2 among Veterans Affairs patients, 17 among Medicare patients, and 17 among privately/commercially insured patients; P less than .01). Meanwhile, the greatest mean MELD score at the time of liver transplantation was observed in Medicaid patients (23.5, compared with 21.4 among VA patients, 21.3 among privately/commercially insured patients, and 21.1 among Medicare patients; P less than .01).
Multivariate regression analysis revealed that, among patients without hepatocellular carcinoma, those with coverage other than private or commercial insurance had significantly higher MELD scores at wait-list registration (P less than .01). Specifically, the odds ratio was highest for VA patients (odds ratio, 2.59), followed by those covered by Medicaid (OR, 2.45), and Medicare (OR, 1.86). Similar trends were observed in hepatocellular carcinoma patients, with the highest biological MELD score at wait-list seen in those covered by Medicaid.
On regression analysis, while Medicaid patients with hepatocellular carcinoma had significantly higher biological MELD scores at time of liver transplantation, compared with those with private/commercial insurance (Medicaid OR, 2.06; P less than .05), no differences were observed among patients without hepatocellular carcinoma.
Dr. Robinson reported having no financial disclosures.
Source: Hepatology 2018 Oct 1;68[S1], Abstract 464.
SAN FRANCISCO – Despite implementation of the Model for End Stage Liver Disease score to prioritize liver transplantation, .
“It can be difficult for patients with Medicaid to access liver transplantation,” lead study author Ann Robinson, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “These patients may be living in underserved areas with limited resources.”
In an effort to evaluate insurance-specific disparities in severity of liver disease at the time of liver transplantation wait-list registration and at the time of liver transplantation, Dr. Robinson and her colleagues retrospectively evaluated the 2005-2016 United Network for Organ Sharing/Organ Procurement and Transplant Network liver transplant registry. They used multivariate linear regression models to make insurance-specific comparisons of MELD scores at wait-list registration and at liver transplantation, which included adjustments for age, sex, year, etiology of liver disease, body mass index, ascites, hepatocellular carcinoma (HCC), and hepatic encephalopathy.
Dr. Robinson, who is a third-year internal medicine resident at Highland Hospital, Oakland, Calif., reported findings from 88,542 liver transplantation wait-list registrants with a mean age of 56 years. Their overall mean MELD score was 17.4 at wait-list registration and 22.6 at time of liver transplantation. The greatest mean MELD score at the time of wait-list registration was observed in Medicaid patients (18.4, compared with 17.2 among Veterans Affairs patients, 17 among Medicare patients, and 17 among privately/commercially insured patients; P less than .01). Meanwhile, the greatest mean MELD score at the time of liver transplantation was observed in Medicaid patients (23.5, compared with 21.4 among VA patients, 21.3 among privately/commercially insured patients, and 21.1 among Medicare patients; P less than .01).
Multivariate regression analysis revealed that, among patients without hepatocellular carcinoma, those with coverage other than private or commercial insurance had significantly higher MELD scores at wait-list registration (P less than .01). Specifically, the odds ratio was highest for VA patients (odds ratio, 2.59), followed by those covered by Medicaid (OR, 2.45), and Medicare (OR, 1.86). Similar trends were observed in hepatocellular carcinoma patients, with the highest biological MELD score at wait-list seen in those covered by Medicaid.
On regression analysis, while Medicaid patients with hepatocellular carcinoma had significantly higher biological MELD scores at time of liver transplantation, compared with those with private/commercial insurance (Medicaid OR, 2.06; P less than .05), no differences were observed among patients without hepatocellular carcinoma.
Dr. Robinson reported having no financial disclosures.
Source: Hepatology 2018 Oct 1;68[S1], Abstract 464.
AT THE LIVER MEETING 2018
Key clinical point: Significant insurance-specific disparities in MELD scores at time of wait-list registration were observed among patients with and without hepatocellular carcinoma.
Major finding: Among patients without hepatocellular carcinoma, those with Medicaid coverage were 2.45 times more likely to have higher MELD scores at wait-list registration, compared with those covered by commercial or private insurance (P less than .01).
Study details: A retrospective analysis of 88,542 liver transplantation wait-list registrants.
Disclosures: Dr. Robinson reported having no disclosures.
Source: Hepatology 2018 Oct 1;68[S1], Abstract 464.
Hep C–infected livers are safe for transplant
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: Use of hepatitis C–positive livers can significantly increase the donor organ pool.
Major finding: Hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality.
Study details: Retrospective analysis of 16,858 liver transplants.
Disclosures: The study was funded internally. Dr. Paul has no financial disclosures.
Source: AASLD 2018, Abstract 0249.
High rates of prescription opioid, benzodiazepine use observed in chronic liver disease
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
dbrunk@mdedge.com
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
dbrunk@mdedge.com
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
dbrunk@mdedge.com
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: About one-fourth of patients with chronic hepatitis C use prescription opioids.
Major finding: In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with congestive heart failure, and 24% among those with chronic obstructive pulmonary disease.
Study details: An analysis of 210,191 patients who had chronic hepatitis C.
Disclosures: Dr. Konerman reported having no financial disclosures.
Black patients present as sicker, more likely to receive liver transplant
PHILADELPHIA – Black patients are more likely to be put on a transplant list because of acute liver failure, be listed as status 1, and receive a liver transplant, compared with white patients, according to a recent presentation at the annual meeting of the American College of Gastroenterology.
Lauren D. Nephew, MD, MSCE, of Indiana University in Indianapolis, and her colleagues performed a retrospective cohort study of black and white patients with a minimum age of 18 years in the United Network of Organ Sharing database who were wait-listed for a liver transplantation during 2002-2016. They examined patient clinical characteristics, acute liver failure (ALF) etiologies, wait-list status, and posttransplant survival outcomes through Kaplan Meier analysis.
“We really wanted to explore this topic in patients with acute liver failure, some of the sickest patients that we see,” Dr. Nephew said in her presentation. “We wanted to really determine whether or not there were differences in clinical characteristics and etiologies of acute liver failure in patients by race who are listed for liver transplantation.”
“Then, we wanted to compare wait-list outcomes,” she added, such as “differences by race in liver transplantation or wait-list removal because of death or becoming too sick for transplant.”
There were 11,289 patients in the white ALF group and 2,112 patients in the black ALF group; 2,876 (25.5%) of patients in the white ALF and 790 (37.4%) in the black ALF group were listed as status 1, which indicated an expected survival of 7 days or less. There were similar clinical characteristics for the white and black ALF status 1 patients regarding age (34.2 years vs. 36.3 years), Model for End-Stage Liver Disease (MELD) score (34 vs. 36; P less than .001), international normalized ratio (INR) test (mean 4.5 vs. mean 5.0; P = .001), creatinine levels (2.1 mg/dL vs. 1.9 mg/dL; P less than .001), and percentage of patients who were hepatic encephalopathy grade 3 or 4 (60.0% vs. 63.2%; P = .10). However, Dr. Nephew noted significantly higher bilirubin levels in the black ALF status 1 cohort (17.9 mg/dL), compared with the white ALF status 1 cohort (11.3 mg/dL; P less than .001).
The causes for ALF in each group included drug-induced liver failure (white status 1 cohort, 34.1%; black status 1 cohort, 20.6%), autoimmune hepatitis (2.7% vs. 9.4%), Wilson’s disease (0.58% vs. 0.13%), unknown etiology (34.5% vs. 42.5%), and other etiology (22.9% vs. 17%). For patients who underwent liver transplant and wait-list removal, there were no significant differences in wait-list removal “despite black patients being sicker at presentation,” Dr. Nephew said. Black patients were more likely to be listed to status 1 and transplanted at 62% (490 patients), compared with white patients at 53% (1,524 patients). There were 713 white patients (24.8%) removed from the transplant list, compared with 114 (13.8%) of black patients.
“If you are transplanted and you don’t die, then you are likely removed from the list for other reasons, and the most common reason is that you improved and became well, and so white patients were significantly more likely to be removed from the wait-list because of improvement, compared with black patients,” Dr. Nephew said.
In a competing risk analysis, the researchers found the hazard ratio for white patients who were status 1 and removed from the wait-list because of death or becoming too sick was 1.04 (95% confidence interval, 0.89-1.21) and those white patients who were listed as status 1 and then transplanted was 1.2 (95% CI, 1.08-1.30). In a multivariate analysis, the hazard ratio for white patients who were listed as status 1 and transplanted, which contained bilirubin at transplant, was 1.08 (95% CI, 0.98-1.19). Kaplan Meier 1-year survival post-transplant was 82.8% in white patients and 79.6% in black patients (P = .09).
“I think the question that we’ve been asking ourselves is, is this because black patients are presenting later with their acute liver disease and are sicker at presentation, or do they just have worse liver disease inherently on presentation that drove these findings?” Dr. Nephew said.
Dr. Nephew reports no relevant conflicts of interest.
SOURCE: Nephew L et al. ACG 2018, Presentation 59.
PHILADELPHIA – Black patients are more likely to be put on a transplant list because of acute liver failure, be listed as status 1, and receive a liver transplant, compared with white patients, according to a recent presentation at the annual meeting of the American College of Gastroenterology.
Lauren D. Nephew, MD, MSCE, of Indiana University in Indianapolis, and her colleagues performed a retrospective cohort study of black and white patients with a minimum age of 18 years in the United Network of Organ Sharing database who were wait-listed for a liver transplantation during 2002-2016. They examined patient clinical characteristics, acute liver failure (ALF) etiologies, wait-list status, and posttransplant survival outcomes through Kaplan Meier analysis.
“We really wanted to explore this topic in patients with acute liver failure, some of the sickest patients that we see,” Dr. Nephew said in her presentation. “We wanted to really determine whether or not there were differences in clinical characteristics and etiologies of acute liver failure in patients by race who are listed for liver transplantation.”
“Then, we wanted to compare wait-list outcomes,” she added, such as “differences by race in liver transplantation or wait-list removal because of death or becoming too sick for transplant.”
There were 11,289 patients in the white ALF group and 2,112 patients in the black ALF group; 2,876 (25.5%) of patients in the white ALF and 790 (37.4%) in the black ALF group were listed as status 1, which indicated an expected survival of 7 days or less. There were similar clinical characteristics for the white and black ALF status 1 patients regarding age (34.2 years vs. 36.3 years), Model for End-Stage Liver Disease (MELD) score (34 vs. 36; P less than .001), international normalized ratio (INR) test (mean 4.5 vs. mean 5.0; P = .001), creatinine levels (2.1 mg/dL vs. 1.9 mg/dL; P less than .001), and percentage of patients who were hepatic encephalopathy grade 3 or 4 (60.0% vs. 63.2%; P = .10). However, Dr. Nephew noted significantly higher bilirubin levels in the black ALF status 1 cohort (17.9 mg/dL), compared with the white ALF status 1 cohort (11.3 mg/dL; P less than .001).
The causes for ALF in each group included drug-induced liver failure (white status 1 cohort, 34.1%; black status 1 cohort, 20.6%), autoimmune hepatitis (2.7% vs. 9.4%), Wilson’s disease (0.58% vs. 0.13%), unknown etiology (34.5% vs. 42.5%), and other etiology (22.9% vs. 17%). For patients who underwent liver transplant and wait-list removal, there were no significant differences in wait-list removal “despite black patients being sicker at presentation,” Dr. Nephew said. Black patients were more likely to be listed to status 1 and transplanted at 62% (490 patients), compared with white patients at 53% (1,524 patients). There were 713 white patients (24.8%) removed from the transplant list, compared with 114 (13.8%) of black patients.
“If you are transplanted and you don’t die, then you are likely removed from the list for other reasons, and the most common reason is that you improved and became well, and so white patients were significantly more likely to be removed from the wait-list because of improvement, compared with black patients,” Dr. Nephew said.
In a competing risk analysis, the researchers found the hazard ratio for white patients who were status 1 and removed from the wait-list because of death or becoming too sick was 1.04 (95% confidence interval, 0.89-1.21) and those white patients who were listed as status 1 and then transplanted was 1.2 (95% CI, 1.08-1.30). In a multivariate analysis, the hazard ratio for white patients who were listed as status 1 and transplanted, which contained bilirubin at transplant, was 1.08 (95% CI, 0.98-1.19). Kaplan Meier 1-year survival post-transplant was 82.8% in white patients and 79.6% in black patients (P = .09).
“I think the question that we’ve been asking ourselves is, is this because black patients are presenting later with their acute liver disease and are sicker at presentation, or do they just have worse liver disease inherently on presentation that drove these findings?” Dr. Nephew said.
Dr. Nephew reports no relevant conflicts of interest.
SOURCE: Nephew L et al. ACG 2018, Presentation 59.
PHILADELPHIA – Black patients are more likely to be put on a transplant list because of acute liver failure, be listed as status 1, and receive a liver transplant, compared with white patients, according to a recent presentation at the annual meeting of the American College of Gastroenterology.
Lauren D. Nephew, MD, MSCE, of Indiana University in Indianapolis, and her colleagues performed a retrospective cohort study of black and white patients with a minimum age of 18 years in the United Network of Organ Sharing database who were wait-listed for a liver transplantation during 2002-2016. They examined patient clinical characteristics, acute liver failure (ALF) etiologies, wait-list status, and posttransplant survival outcomes through Kaplan Meier analysis.
“We really wanted to explore this topic in patients with acute liver failure, some of the sickest patients that we see,” Dr. Nephew said in her presentation. “We wanted to really determine whether or not there were differences in clinical characteristics and etiologies of acute liver failure in patients by race who are listed for liver transplantation.”
“Then, we wanted to compare wait-list outcomes,” she added, such as “differences by race in liver transplantation or wait-list removal because of death or becoming too sick for transplant.”
There were 11,289 patients in the white ALF group and 2,112 patients in the black ALF group; 2,876 (25.5%) of patients in the white ALF and 790 (37.4%) in the black ALF group were listed as status 1, which indicated an expected survival of 7 days or less. There were similar clinical characteristics for the white and black ALF status 1 patients regarding age (34.2 years vs. 36.3 years), Model for End-Stage Liver Disease (MELD) score (34 vs. 36; P less than .001), international normalized ratio (INR) test (mean 4.5 vs. mean 5.0; P = .001), creatinine levels (2.1 mg/dL vs. 1.9 mg/dL; P less than .001), and percentage of patients who were hepatic encephalopathy grade 3 or 4 (60.0% vs. 63.2%; P = .10). However, Dr. Nephew noted significantly higher bilirubin levels in the black ALF status 1 cohort (17.9 mg/dL), compared with the white ALF status 1 cohort (11.3 mg/dL; P less than .001).
The causes for ALF in each group included drug-induced liver failure (white status 1 cohort, 34.1%; black status 1 cohort, 20.6%), autoimmune hepatitis (2.7% vs. 9.4%), Wilson’s disease (0.58% vs. 0.13%), unknown etiology (34.5% vs. 42.5%), and other etiology (22.9% vs. 17%). For patients who underwent liver transplant and wait-list removal, there were no significant differences in wait-list removal “despite black patients being sicker at presentation,” Dr. Nephew said. Black patients were more likely to be listed to status 1 and transplanted at 62% (490 patients), compared with white patients at 53% (1,524 patients). There were 713 white patients (24.8%) removed from the transplant list, compared with 114 (13.8%) of black patients.
“If you are transplanted and you don’t die, then you are likely removed from the list for other reasons, and the most common reason is that you improved and became well, and so white patients were significantly more likely to be removed from the wait-list because of improvement, compared with black patients,” Dr. Nephew said.
In a competing risk analysis, the researchers found the hazard ratio for white patients who were status 1 and removed from the wait-list because of death or becoming too sick was 1.04 (95% confidence interval, 0.89-1.21) and those white patients who were listed as status 1 and then transplanted was 1.2 (95% CI, 1.08-1.30). In a multivariate analysis, the hazard ratio for white patients who were listed as status 1 and transplanted, which contained bilirubin at transplant, was 1.08 (95% CI, 0.98-1.19). Kaplan Meier 1-year survival post-transplant was 82.8% in white patients and 79.6% in black patients (P = .09).
“I think the question that we’ve been asking ourselves is, is this because black patients are presenting later with their acute liver disease and are sicker at presentation, or do they just have worse liver disease inherently on presentation that drove these findings?” Dr. Nephew said.
Dr. Nephew reports no relevant conflicts of interest.
SOURCE: Nephew L et al. ACG 2018, Presentation 59.
REPORTING FROM ACG 2018
Key clinical point: Black patients are sicker than white patients when they present with acute liver failure and are awaiting liver transplantation.
Major finding: Black patients with acute liver failure were more likely to be wait-listed, listed as status 1, and have higher Model for End-Stage Liver Disease (MELD) scores, creatinine levels, and INR tests, compared with white patients.
Study details: A retrospective cohort analysis of patients with acute liver failure awaiting a liver transplant in the United Network of Organ Sharing database.
Disclosures: Dr. Nephew reports no relevant conflicts of interest.
Source: Nephew L et al. ACG 2018, Presentation 59.
MELD sodium score tied to better transplant outcomes
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
FROM GASTROENTEROLOGY
Key clinical point: The implementation of the MELD sodium (MELD-Na) score for liver allocation was associated with significantly improved outcomes for wait-listed patients.
Major finding: During the MELD-Na era, mortality within 90 days on the liver wait list dropped significantly (HR, 0.74; P less than .001) while the probability of transplant rose significantly (HR, 1.2; P less than .001).
Study details: Comparison of 18,850 adult transplant candidates during the traditional MELD era versus 14,512 candidates during the MELD-Na era.
Disclosures: The investigators had no external funding sources or conflicts of interest.
Source: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.