User login
Nasal Cannula Dislodgement During Sleep in Veterans Receiving Long-term Oxygen Therapy for Hypoxemic Chronic Respiratory Failure
The prevalence of chronic obstructive pulmonary disease (COPD) among male US veterans is higher than in the general population.1 Veterans with COPD have higher rates of comorbidities and increased respiratory-related and all-cause health care use, including the use of long-term oxygen therapy (LTOT).2-5 It has been well established that LTOT reduces all-cause mortality in patients with COPD and
Delivery of domiciliary LTOT entails placing a nasal cannula into both nostrils and loosely securing it around both ears throughout the wake-sleep cycle. Several veterans with hypoxemic CRF due to COPD at the Jesse Brown Veterans Affairs Medical Center (JBVAMC) in Chicago, Illinois, who were receiving LTOT reported nasal cannula dislodgement (NCD) while they slept. However, the clinical significance and impact of these repeated episodes on respiratory-related health care utilization, such as frequent COPD exacerbations with hospitalization, were not recognized.
The purpose of this study was to determine whether veterans with hypoxemic CRF due to COPD and receiving 24-hour LTOT at JBVAMC were experiencing NCD during sleep and, if so, its impact on
METHODS
We reviewed electronic health records (EHRs) of veterans with hypoxemic CRF from COPD who received 24-hour LTOT administered through nasal cannula and were followed
Pertinent patient demographics, clinical and physiologic variables, and hospitalizations with length of JBVAMC stay for each physician-diagnosed COPD exacerbation in the preceding year from the date last seen in the clinic were abstracted from EHRs. Overall hospital cost, defined as a veteran overnight stay in either the medical intensive care unit (MICU) or a general acute medicine bed in a US Department of Veterans Affairs (VA) facility, was calculated for each hospitalization for physician-diagnosed COPD exacerbation using VA Managerial Cost Accounting System National Cost Extracts for inpatient encounters.15 We then contacted each veteran by telephone and asked whether they had experienced NCD and, if so, its weekly frequency ranging from once to nightly.
Data Analysis
Data were reported as mean (SD) where appropriate. The t test and Fisher exact test were used as indicated. P < .05 was considered statistically significant. The study protocol
RESULTS
During the study period,
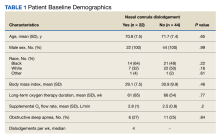
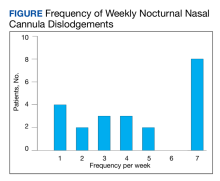
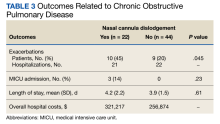
Of the 75 patients, 66 (88%) responded to the telephone survey and 22 patients (33%) reported weekly episodes of NCD while they slept (median, 4 dislodgments per week). (Table 1). Eight patients (36%) reported nightly NCDs (Figure). All 66 respondents were male and 14 of 22 in the NCD group as well as 21 of 44 in the no NCD group were Black veterans. The mean age was similar in both groups: 71 years in the NCD group and 72 years in the no NCD group. There were no statistically significant differences in demographics, including prevalence of obstructive sleep apnea (OSA), supplemental oxygen flow rate, and duration of LTOT, or in pulmonary function test results between patients who did and did not experience NCD while sleeping (Table 2).
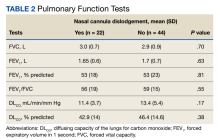
Ten of 22 patients (45%) with NCD and 9 of 44 patients (20%) without NCD were hospitalized at the JBVAMC for ≥ 1 COPD exacerbation in the preceding year that was diagnosed by a physician (P = .045). Three of 22 patients (14%) with NCD and no patients in the no NCD group were admitted to the MICU. No patients required intubation and mechanical ventilation during hospitalization, and no patients died. Overall hospital costs were 25% ($64,342) higher in NCD group compared with the no NCD group and were attributed to the MICU admissions in the NCD group (Table 3). Nine veterans did not respond to repeated telephone calls. One physician-diagnosed COPD exacerbation requiring hospitalization was documented in the nonresponder group; the patient was hospitalized for 2 days. One veteran died before being contacted.
DISCUSSION
There are 3 new findings in this study.
Nocturnal arterial oxygen desaturation in patients with COPD without evidence of OSA may contribute to the frequency of exacerbations.16 Although the mechanism(s) underlying this phenomenon is uncertain, we posit that prolonged nocturnal airway wall hypoxia could amplify underlying chronic inflammation through local generation of reactive oxygen species, thereby predisposing patients to exacerbations. Frequent COPD exacerbations promote disease progression and health status decline and are associated with increased mortality.11,13 Moreover, hospitalization of patients with COPD is the largest contributor to the annual direct cost of COPD per patient.10,12 The higher hospitalization rate observed in the NCD group in our study suggests that interruption of supplemental oxygen delivery while asleep may be a risk factor for COPD exacerbation. Alternatively, an independent factor or factors may have contributed to both NCD during sleep and COPD exacerbation in these patients or an impending exacerbation resulted in sleep disturbances that led to NCD. Additional research is warranted on veterans with hypoxemic CRF from COPD who are receiving LTOT and report frequent NCD during sleep that may support or refute these hypotheses.
To the best of our knowledge, NCD during sleep has not been previously reported in patients
Limitations
This was a small, single-site study, comprised entirely of male patients who are predominantly Black veterans. The telephone interviews with veterans self-reporting NCD during their sleep are prone to recall bias. In addition, the validity and reproducibility of NCD during sleep were not addressed in this study. Missing data from 9 nonresponders may have introduced a nonresponse bias in data analysis and interpretation. The overall hospital cost for a COPD exacerbation at JBVAMC was derived from VA data; US Centers for Medicare & Medicaid Services or commercial carrier data may be different.15,21 Lastly, access to LTOT for veterans with hypoxemic CRF from COPD is regulated and supervised at VA medical facilities.14 This process may be different for patients outside the VA. Taken together, it is difficult to generalize our initial observations to non-VA patients with hypoxemic CRF from COPD who are receiving LTOT. We suggest a large, prospective study of veterans be conducted to determine the prevalence of NCD during sleep and its relationship with COPD exacerbations in veterans receiving LTOT with hypoxemic CRF due to COPD.
CONCLUSIONS
Acknowledgments
We thank Yolanda Davis, RRT, and George Adam for their assistance with this project.
1. Boersma P, Cohen RA, Zelaya CE, Moy E. Multiple chronic conditions among veterans and nonveterans: United States, 2015-2018. Natl Health Stat Report. 2021;(153):1-13. doi:10.15620/cdc:101659
2. Sharafkhaneh A, Petersen NJ, Yu H-J, Dalal AA, Johnson ML, Hanania NA. Burden of COPD in a government health care system: a retrospective observational study using data from the US Veterans Affairs population. Int J Chron Obstruct Pulmon Dis. 2010;5:125-132. doi:10.2147/copd.s8047
3. LaBedz SL, Krishnan JA, Chung Y-C, et al. Chronic obstructive pulmonary disease outcomes at Veterans Affairs versus non-Veterans Affairs hospitals. Chronic Obstr Pulm Dis. 2021;8(3):306-313. doi:10.15326/jcopdf.2021.0201
4. Darnell K, Dwivedi AK, Weng Z, Panos RJ. Disproportionate utilization of healthcare resources among veterans with COPD: a retrospective analysis of factors associated with COPD healthcare cost. Cost Eff Resour Alloc. 2013;11:13. doi:10.1186/1478-7547-11-13
5. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US Veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
6. Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;2005(4):CD001744. doi:10.1002/14651858.CD001744.pub2
7. Lacasse Y, Tan AM, Maltais F, Krishnan JA. Home oxygen in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(10):1254-1264. doi:10.1164/rccm.201802-0382CI
8. Jacobs SS, Krishnan JA, Lederer DJ, et al. Home oxygen therapy for adults with chronic lung disease. An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(10):e121-e141. doi:10.1164/rccm.202009-3608ST
9. AARC. AARC clinical practice guideline. Oxygen therapy in the home or alternate site health care facility--2007 revision & update. Respir Care. 2007;52(8):1063-1068.
10. Foo J, Landis SH, Maskell J, et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi:10.1371/journal.pone.0152618
11. Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(4):464-471. doi:10.1164/rccm.201710-2029OC
12. Stanford RH, Engel-Nitz NM, Bancroft T, Essoi B. The identification and cost of acute chronic obstructive pulmonary disease exacerbations in a United States population healthcare claims database. COPD. 2020;17(5):499-508. doi:10.1080/15412555.2020.1817357
13. Hurst JR, Han MK, Singh B, et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir Res. 2022;23(1):213. doi:10.1186/s12931-022-02123-5
14. US Department of Veterans Affairs, Veterans Health Administration. Home oxygen program. VHA Directive 1173.13(1). Published August 5, 2020. Accessed February 28, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8947
15. Phibbs CS, Barnett PG, Fan A, Harden C, King SS, Scott JY. Research guide to decision support system national cost extracts. Health Economics Resource Center of Health Service R&D Services, US Department of Veterans Affairs. September 2010. Accessed February 14, 2024. https://www.herc.research.va.gov/files/book_621.pdf
16. Agusti A, Hedner J, Marin JM, Barbé F, Cazzola M, Rennard S. Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev. 2011;20(121):183-194. doi:10.1183/09059180.00004311
17. Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Respir Crit Care Med. 2006;174(4):373-378. doi:10.1164/rccm.200507-1161WS
18. Melani AS, Sestini P, Rottoli P. Home oxygen therapy: re-thinking the role of devices. Expert Rev Clin Pharmacol. 2018;11(3):279-289. doi:10.1080/17512433.2018.1421457
19. Sculley JA, Corbridge SJ, Prieto-Centurion V, et al. Home oxygen therapy for patients with COPD: time for a reboot. Respir Care. 2019;64(12):1574-1585. doi:10.4187/respcare.07135
20. Jacobs SS, Lindell KO, Collins EG, et al. Patient perceptions of the adequacy of supplemental oxygen therapy. Results of the American Thoracic Society Nursing Assembly Oxygen Working Group Survey. Ann Am Thorac Soc. 2018;15:24-32. doi:10.1513/AnnalsATS.201703-209OC
21. US Centers for Medicare & Medicaid Services. Home use of oxygen. Publication number 100-3. January 3, 2023. Accessed February 14, 2024. https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?NCDId=169
The prevalence of chronic obstructive pulmonary disease (COPD) among male US veterans is higher than in the general population.1 Veterans with COPD have higher rates of comorbidities and increased respiratory-related and all-cause health care use, including the use of long-term oxygen therapy (LTOT).2-5 It has been well established that LTOT reduces all-cause mortality in patients with COPD and
Delivery of domiciliary LTOT entails placing a nasal cannula into both nostrils and loosely securing it around both ears throughout the wake-sleep cycle. Several veterans with hypoxemic CRF due to COPD at the Jesse Brown Veterans Affairs Medical Center (JBVAMC) in Chicago, Illinois, who were receiving LTOT reported nasal cannula dislodgement (NCD) while they slept. However, the clinical significance and impact of these repeated episodes on respiratory-related health care utilization, such as frequent COPD exacerbations with hospitalization, were not recognized.
The purpose of this study was to determine whether veterans with hypoxemic CRF due to COPD and receiving 24-hour LTOT at JBVAMC were experiencing NCD during sleep and, if so, its impact on
METHODS
We reviewed electronic health records (EHRs) of veterans with hypoxemic CRF from COPD who received 24-hour LTOT administered through nasal cannula and were followed
Pertinent patient demographics, clinical and physiologic variables, and hospitalizations with length of JBVAMC stay for each physician-diagnosed COPD exacerbation in the preceding year from the date last seen in the clinic were abstracted from EHRs. Overall hospital cost, defined as a veteran overnight stay in either the medical intensive care unit (MICU) or a general acute medicine bed in a US Department of Veterans Affairs (VA) facility, was calculated for each hospitalization for physician-diagnosed COPD exacerbation using VA Managerial Cost Accounting System National Cost Extracts for inpatient encounters.15 We then contacted each veteran by telephone and asked whether they had experienced NCD and, if so, its weekly frequency ranging from once to nightly.
Data Analysis
Data were reported as mean (SD) where appropriate. The t test and Fisher exact test were used as indicated. P < .05 was considered statistically significant. The study protocol
RESULTS
During the study period,
Of the 75 patients, 66 (88%) responded to the telephone survey and 22 patients (33%) reported weekly episodes of NCD while they slept (median, 4 dislodgments per week). (Table 1). Eight patients (36%) reported nightly NCDs (Figure). All 66 respondents were male and 14 of 22 in the NCD group as well as 21 of 44 in the no NCD group were Black veterans. The mean age was similar in both groups: 71 years in the NCD group and 72 years in the no NCD group. There were no statistically significant differences in demographics, including prevalence of obstructive sleep apnea (OSA), supplemental oxygen flow rate, and duration of LTOT, or in pulmonary function test results between patients who did and did not experience NCD while sleeping (Table 2).
Ten of 22 patients (45%) with NCD and 9 of 44 patients (20%) without NCD were hospitalized at the JBVAMC for ≥ 1 COPD exacerbation in the preceding year that was diagnosed by a physician (P = .045). Three of 22 patients (14%) with NCD and no patients in the no NCD group were admitted to the MICU. No patients required intubation and mechanical ventilation during hospitalization, and no patients died. Overall hospital costs were 25% ($64,342) higher in NCD group compared with the no NCD group and were attributed to the MICU admissions in the NCD group (Table 3). Nine veterans did not respond to repeated telephone calls. One physician-diagnosed COPD exacerbation requiring hospitalization was documented in the nonresponder group; the patient was hospitalized for 2 days. One veteran died before being contacted.
DISCUSSION
There are 3 new findings in this study.
Nocturnal arterial oxygen desaturation in patients with COPD without evidence of OSA may contribute to the frequency of exacerbations.16 Although the mechanism(s) underlying this phenomenon is uncertain, we posit that prolonged nocturnal airway wall hypoxia could amplify underlying chronic inflammation through local generation of reactive oxygen species, thereby predisposing patients to exacerbations. Frequent COPD exacerbations promote disease progression and health status decline and are associated with increased mortality.11,13 Moreover, hospitalization of patients with COPD is the largest contributor to the annual direct cost of COPD per patient.10,12 The higher hospitalization rate observed in the NCD group in our study suggests that interruption of supplemental oxygen delivery while asleep may be a risk factor for COPD exacerbation. Alternatively, an independent factor or factors may have contributed to both NCD during sleep and COPD exacerbation in these patients or an impending exacerbation resulted in sleep disturbances that led to NCD. Additional research is warranted on veterans with hypoxemic CRF from COPD who are receiving LTOT and report frequent NCD during sleep that may support or refute these hypotheses.
To the best of our knowledge, NCD during sleep has not been previously reported in patients
Limitations
This was a small, single-site study, comprised entirely of male patients who are predominantly Black veterans. The telephone interviews with veterans self-reporting NCD during their sleep are prone to recall bias. In addition, the validity and reproducibility of NCD during sleep were not addressed in this study. Missing data from 9 nonresponders may have introduced a nonresponse bias in data analysis and interpretation. The overall hospital cost for a COPD exacerbation at JBVAMC was derived from VA data; US Centers for Medicare & Medicaid Services or commercial carrier data may be different.15,21 Lastly, access to LTOT for veterans with hypoxemic CRF from COPD is regulated and supervised at VA medical facilities.14 This process may be different for patients outside the VA. Taken together, it is difficult to generalize our initial observations to non-VA patients with hypoxemic CRF from COPD who are receiving LTOT. We suggest a large, prospective study of veterans be conducted to determine the prevalence of NCD during sleep and its relationship with COPD exacerbations in veterans receiving LTOT with hypoxemic CRF due to COPD.
CONCLUSIONS
Acknowledgments
We thank Yolanda Davis, RRT, and George Adam for their assistance with this project.
The prevalence of chronic obstructive pulmonary disease (COPD) among male US veterans is higher than in the general population.1 Veterans with COPD have higher rates of comorbidities and increased respiratory-related and all-cause health care use, including the use of long-term oxygen therapy (LTOT).2-5 It has been well established that LTOT reduces all-cause mortality in patients with COPD and
Delivery of domiciliary LTOT entails placing a nasal cannula into both nostrils and loosely securing it around both ears throughout the wake-sleep cycle. Several veterans with hypoxemic CRF due to COPD at the Jesse Brown Veterans Affairs Medical Center (JBVAMC) in Chicago, Illinois, who were receiving LTOT reported nasal cannula dislodgement (NCD) while they slept. However, the clinical significance and impact of these repeated episodes on respiratory-related health care utilization, such as frequent COPD exacerbations with hospitalization, were not recognized.
The purpose of this study was to determine whether veterans with hypoxemic CRF due to COPD and receiving 24-hour LTOT at JBVAMC were experiencing NCD during sleep and, if so, its impact on
METHODS
We reviewed electronic health records (EHRs) of veterans with hypoxemic CRF from COPD who received 24-hour LTOT administered through nasal cannula and were followed
Pertinent patient demographics, clinical and physiologic variables, and hospitalizations with length of JBVAMC stay for each physician-diagnosed COPD exacerbation in the preceding year from the date last seen in the clinic were abstracted from EHRs. Overall hospital cost, defined as a veteran overnight stay in either the medical intensive care unit (MICU) or a general acute medicine bed in a US Department of Veterans Affairs (VA) facility, was calculated for each hospitalization for physician-diagnosed COPD exacerbation using VA Managerial Cost Accounting System National Cost Extracts for inpatient encounters.15 We then contacted each veteran by telephone and asked whether they had experienced NCD and, if so, its weekly frequency ranging from once to nightly.
Data Analysis
Data were reported as mean (SD) where appropriate. The t test and Fisher exact test were used as indicated. P < .05 was considered statistically significant. The study protocol
RESULTS
During the study period,
Of the 75 patients, 66 (88%) responded to the telephone survey and 22 patients (33%) reported weekly episodes of NCD while they slept (median, 4 dislodgments per week). (Table 1). Eight patients (36%) reported nightly NCDs (Figure). All 66 respondents were male and 14 of 22 in the NCD group as well as 21 of 44 in the no NCD group were Black veterans. The mean age was similar in both groups: 71 years in the NCD group and 72 years in the no NCD group. There were no statistically significant differences in demographics, including prevalence of obstructive sleep apnea (OSA), supplemental oxygen flow rate, and duration of LTOT, or in pulmonary function test results between patients who did and did not experience NCD while sleeping (Table 2).
Ten of 22 patients (45%) with NCD and 9 of 44 patients (20%) without NCD were hospitalized at the JBVAMC for ≥ 1 COPD exacerbation in the preceding year that was diagnosed by a physician (P = .045). Three of 22 patients (14%) with NCD and no patients in the no NCD group were admitted to the MICU. No patients required intubation and mechanical ventilation during hospitalization, and no patients died. Overall hospital costs were 25% ($64,342) higher in NCD group compared with the no NCD group and were attributed to the MICU admissions in the NCD group (Table 3). Nine veterans did not respond to repeated telephone calls. One physician-diagnosed COPD exacerbation requiring hospitalization was documented in the nonresponder group; the patient was hospitalized for 2 days. One veteran died before being contacted.
DISCUSSION
There are 3 new findings in this study.
Nocturnal arterial oxygen desaturation in patients with COPD without evidence of OSA may contribute to the frequency of exacerbations.16 Although the mechanism(s) underlying this phenomenon is uncertain, we posit that prolonged nocturnal airway wall hypoxia could amplify underlying chronic inflammation through local generation of reactive oxygen species, thereby predisposing patients to exacerbations. Frequent COPD exacerbations promote disease progression and health status decline and are associated with increased mortality.11,13 Moreover, hospitalization of patients with COPD is the largest contributor to the annual direct cost of COPD per patient.10,12 The higher hospitalization rate observed in the NCD group in our study suggests that interruption of supplemental oxygen delivery while asleep may be a risk factor for COPD exacerbation. Alternatively, an independent factor or factors may have contributed to both NCD during sleep and COPD exacerbation in these patients or an impending exacerbation resulted in sleep disturbances that led to NCD. Additional research is warranted on veterans with hypoxemic CRF from COPD who are receiving LTOT and report frequent NCD during sleep that may support or refute these hypotheses.
To the best of our knowledge, NCD during sleep has not been previously reported in patients
Limitations
This was a small, single-site study, comprised entirely of male patients who are predominantly Black veterans. The telephone interviews with veterans self-reporting NCD during their sleep are prone to recall bias. In addition, the validity and reproducibility of NCD during sleep were not addressed in this study. Missing data from 9 nonresponders may have introduced a nonresponse bias in data analysis and interpretation. The overall hospital cost for a COPD exacerbation at JBVAMC was derived from VA data; US Centers for Medicare & Medicaid Services or commercial carrier data may be different.15,21 Lastly, access to LTOT for veterans with hypoxemic CRF from COPD is regulated and supervised at VA medical facilities.14 This process may be different for patients outside the VA. Taken together, it is difficult to generalize our initial observations to non-VA patients with hypoxemic CRF from COPD who are receiving LTOT. We suggest a large, prospective study of veterans be conducted to determine the prevalence of NCD during sleep and its relationship with COPD exacerbations in veterans receiving LTOT with hypoxemic CRF due to COPD.
CONCLUSIONS
Acknowledgments
We thank Yolanda Davis, RRT, and George Adam for their assistance with this project.
1. Boersma P, Cohen RA, Zelaya CE, Moy E. Multiple chronic conditions among veterans and nonveterans: United States, 2015-2018. Natl Health Stat Report. 2021;(153):1-13. doi:10.15620/cdc:101659
2. Sharafkhaneh A, Petersen NJ, Yu H-J, Dalal AA, Johnson ML, Hanania NA. Burden of COPD in a government health care system: a retrospective observational study using data from the US Veterans Affairs population. Int J Chron Obstruct Pulmon Dis. 2010;5:125-132. doi:10.2147/copd.s8047
3. LaBedz SL, Krishnan JA, Chung Y-C, et al. Chronic obstructive pulmonary disease outcomes at Veterans Affairs versus non-Veterans Affairs hospitals. Chronic Obstr Pulm Dis. 2021;8(3):306-313. doi:10.15326/jcopdf.2021.0201
4. Darnell K, Dwivedi AK, Weng Z, Panos RJ. Disproportionate utilization of healthcare resources among veterans with COPD: a retrospective analysis of factors associated with COPD healthcare cost. Cost Eff Resour Alloc. 2013;11:13. doi:10.1186/1478-7547-11-13
5. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US Veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
6. Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;2005(4):CD001744. doi:10.1002/14651858.CD001744.pub2
7. Lacasse Y, Tan AM, Maltais F, Krishnan JA. Home oxygen in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(10):1254-1264. doi:10.1164/rccm.201802-0382CI
8. Jacobs SS, Krishnan JA, Lederer DJ, et al. Home oxygen therapy for adults with chronic lung disease. An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(10):e121-e141. doi:10.1164/rccm.202009-3608ST
9. AARC. AARC clinical practice guideline. Oxygen therapy in the home or alternate site health care facility--2007 revision & update. Respir Care. 2007;52(8):1063-1068.
10. Foo J, Landis SH, Maskell J, et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi:10.1371/journal.pone.0152618
11. Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(4):464-471. doi:10.1164/rccm.201710-2029OC
12. Stanford RH, Engel-Nitz NM, Bancroft T, Essoi B. The identification and cost of acute chronic obstructive pulmonary disease exacerbations in a United States population healthcare claims database. COPD. 2020;17(5):499-508. doi:10.1080/15412555.2020.1817357
13. Hurst JR, Han MK, Singh B, et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir Res. 2022;23(1):213. doi:10.1186/s12931-022-02123-5
14. US Department of Veterans Affairs, Veterans Health Administration. Home oxygen program. VHA Directive 1173.13(1). Published August 5, 2020. Accessed February 28, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8947
15. Phibbs CS, Barnett PG, Fan A, Harden C, King SS, Scott JY. Research guide to decision support system national cost extracts. Health Economics Resource Center of Health Service R&D Services, US Department of Veterans Affairs. September 2010. Accessed February 14, 2024. https://www.herc.research.va.gov/files/book_621.pdf
16. Agusti A, Hedner J, Marin JM, Barbé F, Cazzola M, Rennard S. Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev. 2011;20(121):183-194. doi:10.1183/09059180.00004311
17. Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Respir Crit Care Med. 2006;174(4):373-378. doi:10.1164/rccm.200507-1161WS
18. Melani AS, Sestini P, Rottoli P. Home oxygen therapy: re-thinking the role of devices. Expert Rev Clin Pharmacol. 2018;11(3):279-289. doi:10.1080/17512433.2018.1421457
19. Sculley JA, Corbridge SJ, Prieto-Centurion V, et al. Home oxygen therapy for patients with COPD: time for a reboot. Respir Care. 2019;64(12):1574-1585. doi:10.4187/respcare.07135
20. Jacobs SS, Lindell KO, Collins EG, et al. Patient perceptions of the adequacy of supplemental oxygen therapy. Results of the American Thoracic Society Nursing Assembly Oxygen Working Group Survey. Ann Am Thorac Soc. 2018;15:24-32. doi:10.1513/AnnalsATS.201703-209OC
21. US Centers for Medicare & Medicaid Services. Home use of oxygen. Publication number 100-3. January 3, 2023. Accessed February 14, 2024. https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?NCDId=169
1. Boersma P, Cohen RA, Zelaya CE, Moy E. Multiple chronic conditions among veterans and nonveterans: United States, 2015-2018. Natl Health Stat Report. 2021;(153):1-13. doi:10.15620/cdc:101659
2. Sharafkhaneh A, Petersen NJ, Yu H-J, Dalal AA, Johnson ML, Hanania NA. Burden of COPD in a government health care system: a retrospective observational study using data from the US Veterans Affairs population. Int J Chron Obstruct Pulmon Dis. 2010;5:125-132. doi:10.2147/copd.s8047
3. LaBedz SL, Krishnan JA, Chung Y-C, et al. Chronic obstructive pulmonary disease outcomes at Veterans Affairs versus non-Veterans Affairs hospitals. Chronic Obstr Pulm Dis. 2021;8(3):306-313. doi:10.15326/jcopdf.2021.0201
4. Darnell K, Dwivedi AK, Weng Z, Panos RJ. Disproportionate utilization of healthcare resources among veterans with COPD: a retrospective analysis of factors associated with COPD healthcare cost. Cost Eff Resour Alloc. 2013;11:13. doi:10.1186/1478-7547-11-13
5. Bamonti PM, Robinson SA, Wan ES, Moy ML. Improving physiological, physical, and psychological health outcomes: a narrative review in US Veterans with COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1269-1283. doi:10.2147/COPD.S339323
6. Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;2005(4):CD001744. doi:10.1002/14651858.CD001744.pub2
7. Lacasse Y, Tan AM, Maltais F, Krishnan JA. Home oxygen in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(10):1254-1264. doi:10.1164/rccm.201802-0382CI
8. Jacobs SS, Krishnan JA, Lederer DJ, et al. Home oxygen therapy for adults with chronic lung disease. An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(10):e121-e141. doi:10.1164/rccm.202009-3608ST
9. AARC. AARC clinical practice guideline. Oxygen therapy in the home or alternate site health care facility--2007 revision & update. Respir Care. 2007;52(8):1063-1068.
10. Foo J, Landis SH, Maskell J, et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi:10.1371/journal.pone.0152618
11. Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(4):464-471. doi:10.1164/rccm.201710-2029OC
12. Stanford RH, Engel-Nitz NM, Bancroft T, Essoi B. The identification and cost of acute chronic obstructive pulmonary disease exacerbations in a United States population healthcare claims database. COPD. 2020;17(5):499-508. doi:10.1080/15412555.2020.1817357
13. Hurst JR, Han MK, Singh B, et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir Res. 2022;23(1):213. doi:10.1186/s12931-022-02123-5
14. US Department of Veterans Affairs, Veterans Health Administration. Home oxygen program. VHA Directive 1173.13(1). Published August 5, 2020. Accessed February 28, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8947
15. Phibbs CS, Barnett PG, Fan A, Harden C, King SS, Scott JY. Research guide to decision support system national cost extracts. Health Economics Resource Center of Health Service R&D Services, US Department of Veterans Affairs. September 2010. Accessed February 14, 2024. https://www.herc.research.va.gov/files/book_621.pdf
16. Agusti A, Hedner J, Marin JM, Barbé F, Cazzola M, Rennard S. Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev. 2011;20(121):183-194. doi:10.1183/09059180.00004311
17. Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Respir Crit Care Med. 2006;174(4):373-378. doi:10.1164/rccm.200507-1161WS
18. Melani AS, Sestini P, Rottoli P. Home oxygen therapy: re-thinking the role of devices. Expert Rev Clin Pharmacol. 2018;11(3):279-289. doi:10.1080/17512433.2018.1421457
19. Sculley JA, Corbridge SJ, Prieto-Centurion V, et al. Home oxygen therapy for patients with COPD: time for a reboot. Respir Care. 2019;64(12):1574-1585. doi:10.4187/respcare.07135
20. Jacobs SS, Lindell KO, Collins EG, et al. Patient perceptions of the adequacy of supplemental oxygen therapy. Results of the American Thoracic Society Nursing Assembly Oxygen Working Group Survey. Ann Am Thorac Soc. 2018;15:24-32. doi:10.1513/AnnalsATS.201703-209OC
21. US Centers for Medicare & Medicaid Services. Home use of oxygen. Publication number 100-3. January 3, 2023. Accessed February 14, 2024. https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?NCDId=169
Tuberculosis Prevention Brings Economic Gains, Says WHO
A new study conducted by the World Health Organization (WHO) suggests that in addition to providing significant improvements in public health, investment in the diagnosis and prevention of tuberculosis also generates economic benefits.
According to a survey conducted by governments and researchers from Brazil, Georgia, Kenya, and South Africa, even modest increases in funding for measures against tuberculosis can bring gains. Every $1 invested produces returns of as much as $39, it found.
The findings may remind governments and policymakers about the importance of investing in public health policies. According to the WHO, the study “provides strong economic arguments” about the true costs of tuberculosis and proves the benefits of increasing funding to accelerate the diagnosis and preventive treatment of the disease.
UN Targets Tuberculosis
In September 2023, during the last meeting of the United Nations General Assembly, following a widespread worsening of disease indicators because of the COVID-19 pandemic, world leaders signed a declaration committing to the expansion of efforts to combat tuberculosis during the next 5 years. The current WHO study was developed to provide a road map for the implementation of key measures against the disease.
The survey highlights two fundamental actions: The expansion of screening, especially in populations considered more vulnerable, and the provision of tuberculosis preventive treatment (TPT), which entails administering drugs to people who have been exposed to the disease but have not yet developed it.
“TPT is a proven and effective intervention to prevent the development of tuberculosis among exposed people, reducing the risk of developing the disease by about 60%-90% compared with individuals who did not receive it,” the document emphasized.
Investments Yield Returns
To achieve the necessary coverage levels, the study estimated that Brazil would need to increase annual per capita investment by $0.28 (about R$1.41) between 2024 and 2050. Brazilian society, in turn, would receive a return of $11 (R$55.27) for every dollar invested.
For South Africa, whose per capita investment increase is estimated at $1.10 per year, the return would be even more significant: $39 for every dollar allocated.
The WHO emphasized that funding for combating the disease is much lower than the value of the damage it causes to nations. “Tuberculosis has high costs for society. Only a small proportion of these costs go directly to the health system (ranging from 1.7% in South Africa to 7.8% in Kenya). Most are costs for patients and society.”
The study projected that between 2024 and 2050, the total cost of tuberculosis to Brazilian society would be $81.2 billion, with an average annual value of $3.01 billion. This figure represents, in 2024, 0.16% of the country’s gross domestic product.
Achieving screening and preventive treatment goals in Brazil would lead to a reduction of as much as 18% in the national incidence of the disease, as well as 1.9 million fewer deaths, between 2024 and 2050.
Although treatable and preventable, tuberculosis remains the leading cause of death from infectious agents worldwide. It is estimated that over 1.3 million people died from the disease in 2022.
The document provides the “health and economic justification for investing in evidence-based interventions recommended by WHO in tuberculosis screening and prevention,” according to WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
“Today we have the knowledge, tools, and political commitment that can end this age-old disease that continues to be one of the leading causes of death from infectious diseases worldwide,” he added.
Emerging Concerns
Although the WHO highlighted the global increase in access to tuberculosis diagnosis and treatment in 2022, which coincided with the recovery of healthcare systems in several countries after the beginning of the pandemic, it emphasized that the implementation of preventive treatment for exposed individuals and high-vulnerability populations remains slow.
Another concern is the increase in drug resistance. Multidrug-resistant tuberculosis is considered a public health crisis. It is estimated that about 410,000 people had multidrug-resistant tuberculosis or rifampicin-resistant tuberculosis in 2022, but only two of every five patients had access to treatment.This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com .
A new study conducted by the World Health Organization (WHO) suggests that in addition to providing significant improvements in public health, investment in the diagnosis and prevention of tuberculosis also generates economic benefits.
According to a survey conducted by governments and researchers from Brazil, Georgia, Kenya, and South Africa, even modest increases in funding for measures against tuberculosis can bring gains. Every $1 invested produces returns of as much as $39, it found.
The findings may remind governments and policymakers about the importance of investing in public health policies. According to the WHO, the study “provides strong economic arguments” about the true costs of tuberculosis and proves the benefits of increasing funding to accelerate the diagnosis and preventive treatment of the disease.
UN Targets Tuberculosis
In September 2023, during the last meeting of the United Nations General Assembly, following a widespread worsening of disease indicators because of the COVID-19 pandemic, world leaders signed a declaration committing to the expansion of efforts to combat tuberculosis during the next 5 years. The current WHO study was developed to provide a road map for the implementation of key measures against the disease.
The survey highlights two fundamental actions: The expansion of screening, especially in populations considered more vulnerable, and the provision of tuberculosis preventive treatment (TPT), which entails administering drugs to people who have been exposed to the disease but have not yet developed it.
“TPT is a proven and effective intervention to prevent the development of tuberculosis among exposed people, reducing the risk of developing the disease by about 60%-90% compared with individuals who did not receive it,” the document emphasized.
Investments Yield Returns
To achieve the necessary coverage levels, the study estimated that Brazil would need to increase annual per capita investment by $0.28 (about R$1.41) between 2024 and 2050. Brazilian society, in turn, would receive a return of $11 (R$55.27) for every dollar invested.
For South Africa, whose per capita investment increase is estimated at $1.10 per year, the return would be even more significant: $39 for every dollar allocated.
The WHO emphasized that funding for combating the disease is much lower than the value of the damage it causes to nations. “Tuberculosis has high costs for society. Only a small proportion of these costs go directly to the health system (ranging from 1.7% in South Africa to 7.8% in Kenya). Most are costs for patients and society.”
The study projected that between 2024 and 2050, the total cost of tuberculosis to Brazilian society would be $81.2 billion, with an average annual value of $3.01 billion. This figure represents, in 2024, 0.16% of the country’s gross domestic product.
Achieving screening and preventive treatment goals in Brazil would lead to a reduction of as much as 18% in the national incidence of the disease, as well as 1.9 million fewer deaths, between 2024 and 2050.
Although treatable and preventable, tuberculosis remains the leading cause of death from infectious agents worldwide. It is estimated that over 1.3 million people died from the disease in 2022.
The document provides the “health and economic justification for investing in evidence-based interventions recommended by WHO in tuberculosis screening and prevention,” according to WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
“Today we have the knowledge, tools, and political commitment that can end this age-old disease that continues to be one of the leading causes of death from infectious diseases worldwide,” he added.
Emerging Concerns
Although the WHO highlighted the global increase in access to tuberculosis diagnosis and treatment in 2022, which coincided with the recovery of healthcare systems in several countries after the beginning of the pandemic, it emphasized that the implementation of preventive treatment for exposed individuals and high-vulnerability populations remains slow.
Another concern is the increase in drug resistance. Multidrug-resistant tuberculosis is considered a public health crisis. It is estimated that about 410,000 people had multidrug-resistant tuberculosis or rifampicin-resistant tuberculosis in 2022, but only two of every five patients had access to treatment.This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com .
A new study conducted by the World Health Organization (WHO) suggests that in addition to providing significant improvements in public health, investment in the diagnosis and prevention of tuberculosis also generates economic benefits.
According to a survey conducted by governments and researchers from Brazil, Georgia, Kenya, and South Africa, even modest increases in funding for measures against tuberculosis can bring gains. Every $1 invested produces returns of as much as $39, it found.
The findings may remind governments and policymakers about the importance of investing in public health policies. According to the WHO, the study “provides strong economic arguments” about the true costs of tuberculosis and proves the benefits of increasing funding to accelerate the diagnosis and preventive treatment of the disease.
UN Targets Tuberculosis
In September 2023, during the last meeting of the United Nations General Assembly, following a widespread worsening of disease indicators because of the COVID-19 pandemic, world leaders signed a declaration committing to the expansion of efforts to combat tuberculosis during the next 5 years. The current WHO study was developed to provide a road map for the implementation of key measures against the disease.
The survey highlights two fundamental actions: The expansion of screening, especially in populations considered more vulnerable, and the provision of tuberculosis preventive treatment (TPT), which entails administering drugs to people who have been exposed to the disease but have not yet developed it.
“TPT is a proven and effective intervention to prevent the development of tuberculosis among exposed people, reducing the risk of developing the disease by about 60%-90% compared with individuals who did not receive it,” the document emphasized.
Investments Yield Returns
To achieve the necessary coverage levels, the study estimated that Brazil would need to increase annual per capita investment by $0.28 (about R$1.41) between 2024 and 2050. Brazilian society, in turn, would receive a return of $11 (R$55.27) for every dollar invested.
For South Africa, whose per capita investment increase is estimated at $1.10 per year, the return would be even more significant: $39 for every dollar allocated.
The WHO emphasized that funding for combating the disease is much lower than the value of the damage it causes to nations. “Tuberculosis has high costs for society. Only a small proportion of these costs go directly to the health system (ranging from 1.7% in South Africa to 7.8% in Kenya). Most are costs for patients and society.”
The study projected that between 2024 and 2050, the total cost of tuberculosis to Brazilian society would be $81.2 billion, with an average annual value of $3.01 billion. This figure represents, in 2024, 0.16% of the country’s gross domestic product.
Achieving screening and preventive treatment goals in Brazil would lead to a reduction of as much as 18% in the national incidence of the disease, as well as 1.9 million fewer deaths, between 2024 and 2050.
Although treatable and preventable, tuberculosis remains the leading cause of death from infectious agents worldwide. It is estimated that over 1.3 million people died from the disease in 2022.
The document provides the “health and economic justification for investing in evidence-based interventions recommended by WHO in tuberculosis screening and prevention,” according to WHO Director-General Tedros Adhanom Ghebreyesus, PhD.
“Today we have the knowledge, tools, and political commitment that can end this age-old disease that continues to be one of the leading causes of death from infectious diseases worldwide,” he added.
Emerging Concerns
Although the WHO highlighted the global increase in access to tuberculosis diagnosis and treatment in 2022, which coincided with the recovery of healthcare systems in several countries after the beginning of the pandemic, it emphasized that the implementation of preventive treatment for exposed individuals and high-vulnerability populations remains slow.
Another concern is the increase in drug resistance. Multidrug-resistant tuberculosis is considered a public health crisis. It is estimated that about 410,000 people had multidrug-resistant tuberculosis or rifampicin-resistant tuberculosis in 2022, but only two of every five patients had access to treatment.This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com .
Study Shows Nirmatrelvir–Ritonavir No More Effective Than Placebo for COVID-19 Symptom Relief
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Isoniazid Resistance Linked With Tuberculosis Deaths
In 2022, more than 78,000 new cases of tuberculosis (TB) were reported in Brazil, with an incidence of 36.3 cases per 100,000 inhabitants. According to researchers from the Regional Prospective Observational Research for Tuberculosis (RePORT)-Brazil consortium, the country could improve the control of this infection if all patients were subjected to a sensitivity test capable of early detection of resistance not only to rifampicin, but also to isoniazid, before starting treatment. A study by the consortium published this year in Open Forum Infectious Diseases found that monoresistance to isoniazid predicted unfavorable outcomes at the national level.
Isoniazid is part of the first-choice therapeutic regimen for patients with pulmonary TB. The regimen also includes rifampicin, pyrazinamide, and ethambutol. According to Bruno Andrade, MD, PhD, Afrânio Kritski, MD, PhD, and biotechnologist Mariana Araújo Pereira, PhD, researchers from RePORT International and RePORT-Brazil, this regimen is used during the intensive phase of treatment, which usually lasts for 2 months. It is followed by a maintenance phase of another 4 months, during which isoniazid and rifampicin continue to be administered. When monoresistance to isoniazid is detected, however, the recommendation is to use a regimen containing a quinolone instead of isoniazid.
Suboptimal Sensitivity Testing
Since 2015, Brazil’s Ministry of Health has recommended sensitivity testing for all suspected TB cases. In practice, however, this approach is not carried out in the ideal manner. The three researchers told the Medscape Portuguese edition that, according to data from the National Notifiable Diseases Information System (Sinan) of the Ministry of Health, culture testing is conducted in about 30% of cases. Sensitivity testing to identify resistance to first-line drugs (rifampicin, isoniazid, ethambutol, and pyrazinamide) and second-line drugs (quinolone and amikacin) is performed in only 12% of cases.
The initiative of the RePORT-Brazil group analyzed 21,197 TB cases registered in Sinan between June 2015 and June 2019 and identified a rate of monoresistance to isoniazid of 1.4%.
For the researchers, the problem of monoresistance to isoniazid in Brazil is still underestimated. This underestimation results from the infrequent performance of culture and sensitivity testing to detect resistance to first- and second-line drugs and because the XPERT MTB RIF test, which detects only rifampicin resistance, is still used.
Resistance and Worse Outcomes
The study also showed that the frequency of unfavorable outcomes in antituberculosis treatment (death or therapeutic failure) was significantly higher among patients with monoresistance to isoniazid (9.1% vs 3.05%).
The finding serves as a warning about the importance of increasing the administration of sensitivity tests to detect resistance to drugs used in tuberculosis treatment, including isoniazid.
Testing sensitivity to rifampicin and isoniazid before starting treatment could transform tuberculosis control in Brazil, allowing for more targeted and effective treatments from the outset, said the researchers. “This not only increases the chances of successful individual treatment but also helps prevent the transmission of resistant strains and develop a more accurate understanding of drug resistance trends,” they emphasized.
They pointed out, however, that implementing this testing in the Unified Health System depends on improvements in resource allocation, coordination between the national TB program and state and municipal programs, and improvements in infrastructure and the technical staff of the Central Public Health Laboratories.
“Although the initial cost is considerable, these investments can be offset by long-term savings resulting from the reduction in the use of more expensive and prolonged treatments for resistant tuberculosis,” said the researchers.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
In 2022, more than 78,000 new cases of tuberculosis (TB) were reported in Brazil, with an incidence of 36.3 cases per 100,000 inhabitants. According to researchers from the Regional Prospective Observational Research for Tuberculosis (RePORT)-Brazil consortium, the country could improve the control of this infection if all patients were subjected to a sensitivity test capable of early detection of resistance not only to rifampicin, but also to isoniazid, before starting treatment. A study by the consortium published this year in Open Forum Infectious Diseases found that monoresistance to isoniazid predicted unfavorable outcomes at the national level.
Isoniazid is part of the first-choice therapeutic regimen for patients with pulmonary TB. The regimen also includes rifampicin, pyrazinamide, and ethambutol. According to Bruno Andrade, MD, PhD, Afrânio Kritski, MD, PhD, and biotechnologist Mariana Araújo Pereira, PhD, researchers from RePORT International and RePORT-Brazil, this regimen is used during the intensive phase of treatment, which usually lasts for 2 months. It is followed by a maintenance phase of another 4 months, during which isoniazid and rifampicin continue to be administered. When monoresistance to isoniazid is detected, however, the recommendation is to use a regimen containing a quinolone instead of isoniazid.
Suboptimal Sensitivity Testing
Since 2015, Brazil’s Ministry of Health has recommended sensitivity testing for all suspected TB cases. In practice, however, this approach is not carried out in the ideal manner. The three researchers told the Medscape Portuguese edition that, according to data from the National Notifiable Diseases Information System (Sinan) of the Ministry of Health, culture testing is conducted in about 30% of cases. Sensitivity testing to identify resistance to first-line drugs (rifampicin, isoniazid, ethambutol, and pyrazinamide) and second-line drugs (quinolone and amikacin) is performed in only 12% of cases.
The initiative of the RePORT-Brazil group analyzed 21,197 TB cases registered in Sinan between June 2015 and June 2019 and identified a rate of monoresistance to isoniazid of 1.4%.
For the researchers, the problem of monoresistance to isoniazid in Brazil is still underestimated. This underestimation results from the infrequent performance of culture and sensitivity testing to detect resistance to first- and second-line drugs and because the XPERT MTB RIF test, which detects only rifampicin resistance, is still used.
Resistance and Worse Outcomes
The study also showed that the frequency of unfavorable outcomes in antituberculosis treatment (death or therapeutic failure) was significantly higher among patients with monoresistance to isoniazid (9.1% vs 3.05%).
The finding serves as a warning about the importance of increasing the administration of sensitivity tests to detect resistance to drugs used in tuberculosis treatment, including isoniazid.
Testing sensitivity to rifampicin and isoniazid before starting treatment could transform tuberculosis control in Brazil, allowing for more targeted and effective treatments from the outset, said the researchers. “This not only increases the chances of successful individual treatment but also helps prevent the transmission of resistant strains and develop a more accurate understanding of drug resistance trends,” they emphasized.
They pointed out, however, that implementing this testing in the Unified Health System depends on improvements in resource allocation, coordination between the national TB program and state and municipal programs, and improvements in infrastructure and the technical staff of the Central Public Health Laboratories.
“Although the initial cost is considerable, these investments can be offset by long-term savings resulting from the reduction in the use of more expensive and prolonged treatments for resistant tuberculosis,” said the researchers.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
In 2022, more than 78,000 new cases of tuberculosis (TB) were reported in Brazil, with an incidence of 36.3 cases per 100,000 inhabitants. According to researchers from the Regional Prospective Observational Research for Tuberculosis (RePORT)-Brazil consortium, the country could improve the control of this infection if all patients were subjected to a sensitivity test capable of early detection of resistance not only to rifampicin, but also to isoniazid, before starting treatment. A study by the consortium published this year in Open Forum Infectious Diseases found that monoresistance to isoniazid predicted unfavorable outcomes at the national level.
Isoniazid is part of the first-choice therapeutic regimen for patients with pulmonary TB. The regimen also includes rifampicin, pyrazinamide, and ethambutol. According to Bruno Andrade, MD, PhD, Afrânio Kritski, MD, PhD, and biotechnologist Mariana Araújo Pereira, PhD, researchers from RePORT International and RePORT-Brazil, this regimen is used during the intensive phase of treatment, which usually lasts for 2 months. It is followed by a maintenance phase of another 4 months, during which isoniazid and rifampicin continue to be administered. When monoresistance to isoniazid is detected, however, the recommendation is to use a regimen containing a quinolone instead of isoniazid.
Suboptimal Sensitivity Testing
Since 2015, Brazil’s Ministry of Health has recommended sensitivity testing for all suspected TB cases. In practice, however, this approach is not carried out in the ideal manner. The three researchers told the Medscape Portuguese edition that, according to data from the National Notifiable Diseases Information System (Sinan) of the Ministry of Health, culture testing is conducted in about 30% of cases. Sensitivity testing to identify resistance to first-line drugs (rifampicin, isoniazid, ethambutol, and pyrazinamide) and second-line drugs (quinolone and amikacin) is performed in only 12% of cases.
The initiative of the RePORT-Brazil group analyzed 21,197 TB cases registered in Sinan between June 2015 and June 2019 and identified a rate of monoresistance to isoniazid of 1.4%.
For the researchers, the problem of monoresistance to isoniazid in Brazil is still underestimated. This underestimation results from the infrequent performance of culture and sensitivity testing to detect resistance to first- and second-line drugs and because the XPERT MTB RIF test, which detects only rifampicin resistance, is still used.
Resistance and Worse Outcomes
The study also showed that the frequency of unfavorable outcomes in antituberculosis treatment (death or therapeutic failure) was significantly higher among patients with monoresistance to isoniazid (9.1% vs 3.05%).
The finding serves as a warning about the importance of increasing the administration of sensitivity tests to detect resistance to drugs used in tuberculosis treatment, including isoniazid.
Testing sensitivity to rifampicin and isoniazid before starting treatment could transform tuberculosis control in Brazil, allowing for more targeted and effective treatments from the outset, said the researchers. “This not only increases the chances of successful individual treatment but also helps prevent the transmission of resistant strains and develop a more accurate understanding of drug resistance trends,” they emphasized.
They pointed out, however, that implementing this testing in the Unified Health System depends on improvements in resource allocation, coordination between the national TB program and state and municipal programs, and improvements in infrastructure and the technical staff of the Central Public Health Laboratories.
“Although the initial cost is considerable, these investments can be offset by long-term savings resulting from the reduction in the use of more expensive and prolonged treatments for resistant tuberculosis,” said the researchers.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
The ED Sailed Smoothly in the Early COVID-19 Days
TOPLINE:
There were few cases of SARS-CoV-2 infections among emergency department (ED) healthcare personnel and no substantial changes in the delivery of emergency medical care during the initial phase of the COVID-19 pandemic.
METHODOLOGY:
- This multicenter prospective cohort study of US ED healthcare personnel called Project COVERED was conducted from May to December 2020 to evaluate the following outcomes:
- The possibility of infected ED personnel reporting to work
- The burden of COVID-19 symptoms on an ED personnel’s work status
- The association between SARS-CoV-2 infection levels and ED staffing
- Project COVERED enrolled 1673 ED healthcare personnel with 29,825 person weeks of observational data from 25 geographically diverse EDs.
- The presence of any SARS-CoV-2 infection was determined using reverse transcription polymerase chain reaction or IgG antibody testing at baseline, week 2, week 4, and every four subsequent weeks through week 20.
- Investigators also collected weekly data on ED staffing and the incidence of SARS-CoV-2 infections in healthcare facilities.
TAKEAWAY:
- Despite the absence of widespread natural immunity or COVID-19 vaccine availability during the time of this study, only 4.5% of ED healthcare personnel tested positive for SARS-CoV-2 infections, with more than half (57.3%) not experiencing any symptoms.
- Most personnel (83%) who experienced symptoms associated with COVID-19 reported working at least one shift in the ED and nearly all of them continued to work until they received laboratory confirmation of their infection.
- The working time lost as a result of COVID-19 and related concerns was minimal, as 89 healthcare personnel reported 90 person weeks of missed work (0.3% of all weeks).
- During this study, physician-staffing levels ranged from 98.7% to 102.0% of normal staffing, with similar values noted for nursing and nonclinical staffs. Reduced staffing was rare, even during COVID-19 surges.
IN PRACTICE:
“Our findings suggest that the cumulative interaction between infected healthcare personnel and others resulted in a negligible risk of transmission on the scale of public health emergencies,” the authors wrote.
SOURCE:
This study was led by Kurt D. Weber, MD, Department of Emergency Medicine, Orlando Health, Orlando, Florida, and published online in Annals of Emergency Medicine.
LIMITATIONS:
Data regarding the Delta variant surges that occurred toward the end of December and the ED status after the advent of the COVID-19 vaccine were not recorded. There may also have been a selection bias risk in this study because the volunteer participants may have exhibited behaviors like social distancing and use of protective equipment, which may have decreased their risk for infections.
DISCLOSURES:
This study was funded by a cooperative agreement from the Centers for Disease Control and Prevention and the Institute for Clinical and Translational Science at the University of Iowa through a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
There were few cases of SARS-CoV-2 infections among emergency department (ED) healthcare personnel and no substantial changes in the delivery of emergency medical care during the initial phase of the COVID-19 pandemic.
METHODOLOGY:
- This multicenter prospective cohort study of US ED healthcare personnel called Project COVERED was conducted from May to December 2020 to evaluate the following outcomes:
- The possibility of infected ED personnel reporting to work
- The burden of COVID-19 symptoms on an ED personnel’s work status
- The association between SARS-CoV-2 infection levels and ED staffing
- Project COVERED enrolled 1673 ED healthcare personnel with 29,825 person weeks of observational data from 25 geographically diverse EDs.
- The presence of any SARS-CoV-2 infection was determined using reverse transcription polymerase chain reaction or IgG antibody testing at baseline, week 2, week 4, and every four subsequent weeks through week 20.
- Investigators also collected weekly data on ED staffing and the incidence of SARS-CoV-2 infections in healthcare facilities.
TAKEAWAY:
- Despite the absence of widespread natural immunity or COVID-19 vaccine availability during the time of this study, only 4.5% of ED healthcare personnel tested positive for SARS-CoV-2 infections, with more than half (57.3%) not experiencing any symptoms.
- Most personnel (83%) who experienced symptoms associated with COVID-19 reported working at least one shift in the ED and nearly all of them continued to work until they received laboratory confirmation of their infection.
- The working time lost as a result of COVID-19 and related concerns was minimal, as 89 healthcare personnel reported 90 person weeks of missed work (0.3% of all weeks).
- During this study, physician-staffing levels ranged from 98.7% to 102.0% of normal staffing, with similar values noted for nursing and nonclinical staffs. Reduced staffing was rare, even during COVID-19 surges.
IN PRACTICE:
“Our findings suggest that the cumulative interaction between infected healthcare personnel and others resulted in a negligible risk of transmission on the scale of public health emergencies,” the authors wrote.
SOURCE:
This study was led by Kurt D. Weber, MD, Department of Emergency Medicine, Orlando Health, Orlando, Florida, and published online in Annals of Emergency Medicine.
LIMITATIONS:
Data regarding the Delta variant surges that occurred toward the end of December and the ED status after the advent of the COVID-19 vaccine were not recorded. There may also have been a selection bias risk in this study because the volunteer participants may have exhibited behaviors like social distancing and use of protective equipment, which may have decreased their risk for infections.
DISCLOSURES:
This study was funded by a cooperative agreement from the Centers for Disease Control and Prevention and the Institute for Clinical and Translational Science at the University of Iowa through a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
There were few cases of SARS-CoV-2 infections among emergency department (ED) healthcare personnel and no substantial changes in the delivery of emergency medical care during the initial phase of the COVID-19 pandemic.
METHODOLOGY:
- This multicenter prospective cohort study of US ED healthcare personnel called Project COVERED was conducted from May to December 2020 to evaluate the following outcomes:
- The possibility of infected ED personnel reporting to work
- The burden of COVID-19 symptoms on an ED personnel’s work status
- The association between SARS-CoV-2 infection levels and ED staffing
- Project COVERED enrolled 1673 ED healthcare personnel with 29,825 person weeks of observational data from 25 geographically diverse EDs.
- The presence of any SARS-CoV-2 infection was determined using reverse transcription polymerase chain reaction or IgG antibody testing at baseline, week 2, week 4, and every four subsequent weeks through week 20.
- Investigators also collected weekly data on ED staffing and the incidence of SARS-CoV-2 infections in healthcare facilities.
TAKEAWAY:
- Despite the absence of widespread natural immunity or COVID-19 vaccine availability during the time of this study, only 4.5% of ED healthcare personnel tested positive for SARS-CoV-2 infections, with more than half (57.3%) not experiencing any symptoms.
- Most personnel (83%) who experienced symptoms associated with COVID-19 reported working at least one shift in the ED and nearly all of them continued to work until they received laboratory confirmation of their infection.
- The working time lost as a result of COVID-19 and related concerns was minimal, as 89 healthcare personnel reported 90 person weeks of missed work (0.3% of all weeks).
- During this study, physician-staffing levels ranged from 98.7% to 102.0% of normal staffing, with similar values noted for nursing and nonclinical staffs. Reduced staffing was rare, even during COVID-19 surges.
IN PRACTICE:
“Our findings suggest that the cumulative interaction between infected healthcare personnel and others resulted in a negligible risk of transmission on the scale of public health emergencies,” the authors wrote.
SOURCE:
This study was led by Kurt D. Weber, MD, Department of Emergency Medicine, Orlando Health, Orlando, Florida, and published online in Annals of Emergency Medicine.
LIMITATIONS:
Data regarding the Delta variant surges that occurred toward the end of December and the ED status after the advent of the COVID-19 vaccine were not recorded. There may also have been a selection bias risk in this study because the volunteer participants may have exhibited behaviors like social distancing and use of protective equipment, which may have decreased their risk for infections.
DISCLOSURES:
This study was funded by a cooperative agreement from the Centers for Disease Control and Prevention and the Institute for Clinical and Translational Science at the University of Iowa through a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
EPR and CRP Predict Adverse Events in COPD Exacerbations
TOPLINE:
C-reactive protein (CRP) levels and eosinophil-to-platelet ratio (EPR) are significant independent predictors of adverse events in patients with chronic obstructive pulmonary disease (COPD) hospitalized with acute exacerbations.
METHODOLOGY:
- In a prospective, observational study at a single center, the researchers examined clinical and lab data including serum CRP levels, EPR, sarcopenia, lung function, nutrition, and frailty.
- The study population included 200 adults older than 40 years with COPD who were hospitalized for acute exacerbations; 50 experienced adverse events.
TAKEAWAY:
- Both elevated CRP and low EPR were significant predictors of adverse events in adjusted analysis in patients with COPD exacerbations (area under the curve, 0.71 and 0.76, respectively).
- In a multivariate analysis, EPR and CRP, as well as sarcopenia, were significantly associated with adverse events (adjusted odds ratios, 2.33, 2.09, and 1.97, respectively).
- COPD symptom scores, frailty, and malnutrition showed predictive value in bivariate but not multivariate analysis.
IN PRACTICE:
“Screening for these biomarkers [EPR and CRP] on admission could help identify high-risk patients who need more aggressive monitoring and treatment,” the researchers wrote in their discussion.
SOURCE:
The lead author on the study was Rohankumar Gandhi, MD, of Guru Gobind Singh Government Hospital, Jamnagar, India. The study was published online in Cureus.
LIMITATIONS:
The use of data from a single center, lack of information on nutritional interventions and counseling, and lack of data on outpatient outcomes limited the study findings.
DISCLOSURES:
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
C-reactive protein (CRP) levels and eosinophil-to-platelet ratio (EPR) are significant independent predictors of adverse events in patients with chronic obstructive pulmonary disease (COPD) hospitalized with acute exacerbations.
METHODOLOGY:
- In a prospective, observational study at a single center, the researchers examined clinical and lab data including serum CRP levels, EPR, sarcopenia, lung function, nutrition, and frailty.
- The study population included 200 adults older than 40 years with COPD who were hospitalized for acute exacerbations; 50 experienced adverse events.
TAKEAWAY:
- Both elevated CRP and low EPR were significant predictors of adverse events in adjusted analysis in patients with COPD exacerbations (area under the curve, 0.71 and 0.76, respectively).
- In a multivariate analysis, EPR and CRP, as well as sarcopenia, were significantly associated with adverse events (adjusted odds ratios, 2.33, 2.09, and 1.97, respectively).
- COPD symptom scores, frailty, and malnutrition showed predictive value in bivariate but not multivariate analysis.
IN PRACTICE:
“Screening for these biomarkers [EPR and CRP] on admission could help identify high-risk patients who need more aggressive monitoring and treatment,” the researchers wrote in their discussion.
SOURCE:
The lead author on the study was Rohankumar Gandhi, MD, of Guru Gobind Singh Government Hospital, Jamnagar, India. The study was published online in Cureus.
LIMITATIONS:
The use of data from a single center, lack of information on nutritional interventions and counseling, and lack of data on outpatient outcomes limited the study findings.
DISCLOSURES:
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
C-reactive protein (CRP) levels and eosinophil-to-platelet ratio (EPR) are significant independent predictors of adverse events in patients with chronic obstructive pulmonary disease (COPD) hospitalized with acute exacerbations.
METHODOLOGY:
- In a prospective, observational study at a single center, the researchers examined clinical and lab data including serum CRP levels, EPR, sarcopenia, lung function, nutrition, and frailty.
- The study population included 200 adults older than 40 years with COPD who were hospitalized for acute exacerbations; 50 experienced adverse events.
TAKEAWAY:
- Both elevated CRP and low EPR were significant predictors of adverse events in adjusted analysis in patients with COPD exacerbations (area under the curve, 0.71 and 0.76, respectively).
- In a multivariate analysis, EPR and CRP, as well as sarcopenia, were significantly associated with adverse events (adjusted odds ratios, 2.33, 2.09, and 1.97, respectively).
- COPD symptom scores, frailty, and malnutrition showed predictive value in bivariate but not multivariate analysis.
IN PRACTICE:
“Screening for these biomarkers [EPR and CRP] on admission could help identify high-risk patients who need more aggressive monitoring and treatment,” the researchers wrote in their discussion.
SOURCE:
The lead author on the study was Rohankumar Gandhi, MD, of Guru Gobind Singh Government Hospital, Jamnagar, India. The study was published online in Cureus.
LIMITATIONS:
The use of data from a single center, lack of information on nutritional interventions and counseling, and lack of data on outpatient outcomes limited the study findings.
DISCLOSURES:
The study received no outside funding. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Managing severe asthma exacerbations in the ED: We need answers beyond albuterol
Evidence-based medicine (EBM) stems from making the best patient-centered decision from the highest-quality data available that comports with our understanding of pathophysiology. In some situations, clinicians are forced to draw conclusions from data that are imperfect and apply it to patients who are complex and dynamic.
The Centers for Disease Control and Prevention (CDC) estimates that about 7.7% of the United States population has asthma. There were about 1 million ED visits in 2020, with asthma listed as the primary diagnosis, and only 94,000 required hospitalization.1 There are many tools we employ that have greatly decreased inpatient admissions for asthma. The uptake of inhaled corticosteroids (ICS) has significantly reduced asthma-related morbidity and mortality and reduced exacerbations that require admission to a hospital. This treatment strategy is supported by the Global Initiative for Asthma (GINA) and National Asthma Education and Prevention Program (NAEPP) guidelines.2,3 While we should celebrate the impact that EBM and ICS have had on asthma outcomes, we continue to struggle to control severe asthma.
Bronchodilator therapy in the hospital is ubiquitous. House staff and hospitalists click the bronchodilator order set early and often. However, the optimal frequency, dose, and duration of inhaled bronchodilator therapy for acute asthma exacerbation are unknown. Do frequency, dose, and duration change with exacerbation severity? Nothing gets ED, inpatient, or ICU physicians more jittery than the phrase “exacerbation of asthma on BiPap” or “intubated for asthma.” With its enormous clinical impact and notoriously difficult hospital and ICU course, the lack of evidence we have for managing these patients outside of the initial 24- to 48-hour visit is concerning. Neither NAEPP nor GINA provide management recommendations for the patient with severe asthma exacerbation that necessitates admission.
Albuterol is a commonly used medication for asthma and chronic obstructive airway disease. It is rapid acting and effective—few medications give patients (or clinicians) such instant satisfaction. As an internal medicine resident and pulmonary fellow, I ordered it countless times without ever looking at the dose. Sometimes, patients would come up from the emergency department after receiving a “continuous dose.” I would often wonder exactly what that meant. After some investigation, I found that in my hospital at the time, one dose of albuterol was 2.5 mg in 2 mL, and a continuous nebulization was four doses for a total of 10 mg.
Shrestha et al. found that high-dose albuterol (7.5 mg) administered continuously was superior to 2.5 mg albuterol delivered three times over 1.5 hours. There were demonstrable improvements in FEV1 and no ICU admissions.4 This study is one of many that compared intermittent to continuous and high-dose vs low-dose albuterol in the emergency department. Most are small and occur over the first 24 hours of presentation to the hospital. They often use short-term changes in spirometry as their primary outcome measure. Being a pulmonary and critical care doctor, I see patients who require advanced rescue maneuvers such as noninvasive positive pressure ventilation (NIPPV) or other pharmacologic adjuncts, for which the current evidence is limited.
Because studies of inhaled bronchodilators in acute asthma exacerbation use spirometry as their primary outcome, those with more severe disease and higher acuity are excluded. Patients on NIPPV can’t perform spirometry. There is essentially no literature to guide treatment for a patient with asthma in the adult ICU. In pediatric intensive care units, there are some data to support either continuous or intermittent inhaled bronchodilator that extends beyond the initial ED visit up to about 60 hours.5 Much of the pediatric data revolve about the amount of albuterol given, which can be as high as 75 mg/hr though is typically closer to 10-20 mg/hr.6 This rate is continued until respiratory improvement occurs.
With poor evidence to guide us and no specific direction from major guidelines, how should providers manage severe asthma exacerbation? The amount of drug deposited in the lung varies by the device used to deliver it. For nebulization, only about 10% of the nebulized amount reaches the lungs for effect; this is a smaller amount compared with all other devices one could use, such as MDI or DPI.7 Once a patient with asthma reaches the emergency department, that person is usually placed on some form of nebulizer treatment. But based on local hospital protocols, the amount and duration can vary widely. Sometimes, in patients with severe exacerbation, there is trepidation to continuing albuterol therapy due to ongoing tachycardia. This seems reasonable given increased albuterol administration could beget an ongoing cycle of dyspnea and anxiety. It could also lead to choosing therapies that are less evidence based.
In closing, this seemingly mundane topic takes on new meaning when a patient is in severe exacerbation. Fortunately, providers are not often faced with the decision to wade into the evidence-free territory of severe asthma exacerbation that is unresponsive to first-line treatments. This narrative should serve as a general alert that this pathophysiologic state is understudied. When encountered, thoughtful consideration of pathology, physiology, and pharmacology is required to reverse it.
References
1. Centers for Disease Control and Prevention. (2023, May 10). Most recent national asthma data. Centers for Disease Control and Prevention. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Global Initiative for Asthma - GINA. (2023, August 15). 2023 GINA Main Report - Global Initiative for Asthma - GINA. https://ginasthma.org/2023-gina-main-report/
3. Kiley J, Mensah GA, Boyce CA, et al (A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group). 2020 Focused updates to the: Asthma Management Guidelines. US Department of Health and Human Services, NIH, NHLBI 2020.
4. Shrestha M, Bidadi K, Gourlay S, Hayes J. Continuous vs intermittent albuterol, at high and low doses, in the treatment of severe acute asthma in adults. Chest. 1996 Jul;110(1):42-7. doi: 10.1378/chest.110.1.42. PMID: 8681661.
5. Kulalert P, Phinyo P, Patumanond J, Smathakanee C, Chuenjit W, Nanthapisal S. Continuous versus intermittent short-acting β2-agonists nebulization as first-line therapy in hospitalized children with severe asthma exacerbation: a propensity score matching analysis. Asthma Res Pract. 2020 Jul 2;6:6. doi: 10.1186/s40733-020-00059-5. PMID: 32632352; PMCID: PMC7329360.
6. Phumeetham S, Bahk TJ, Abd-Allah S, Mathur M. Effect of high-dose continuous albuterol nebulization on clinical variables in children with status asthmaticus. Pediatr Crit Care Med. 2015 Feb;16(2):e41-6. doi: 10.1097/PCC.0000000000000314. PMID: 25560428.
7. Gardenhire DS, Burnett D, Strickland S, Myers, TR. A guide to aerosol delivery devices for respiratory therapists. American Association for Respiratory Care, Dallas, Texas 2017.
Evidence-based medicine (EBM) stems from making the best patient-centered decision from the highest-quality data available that comports with our understanding of pathophysiology. In some situations, clinicians are forced to draw conclusions from data that are imperfect and apply it to patients who are complex and dynamic.
The Centers for Disease Control and Prevention (CDC) estimates that about 7.7% of the United States population has asthma. There were about 1 million ED visits in 2020, with asthma listed as the primary diagnosis, and only 94,000 required hospitalization.1 There are many tools we employ that have greatly decreased inpatient admissions for asthma. The uptake of inhaled corticosteroids (ICS) has significantly reduced asthma-related morbidity and mortality and reduced exacerbations that require admission to a hospital. This treatment strategy is supported by the Global Initiative for Asthma (GINA) and National Asthma Education and Prevention Program (NAEPP) guidelines.2,3 While we should celebrate the impact that EBM and ICS have had on asthma outcomes, we continue to struggle to control severe asthma.
Bronchodilator therapy in the hospital is ubiquitous. House staff and hospitalists click the bronchodilator order set early and often. However, the optimal frequency, dose, and duration of inhaled bronchodilator therapy for acute asthma exacerbation are unknown. Do frequency, dose, and duration change with exacerbation severity? Nothing gets ED, inpatient, or ICU physicians more jittery than the phrase “exacerbation of asthma on BiPap” or “intubated for asthma.” With its enormous clinical impact and notoriously difficult hospital and ICU course, the lack of evidence we have for managing these patients outside of the initial 24- to 48-hour visit is concerning. Neither NAEPP nor GINA provide management recommendations for the patient with severe asthma exacerbation that necessitates admission.
Albuterol is a commonly used medication for asthma and chronic obstructive airway disease. It is rapid acting and effective—few medications give patients (or clinicians) such instant satisfaction. As an internal medicine resident and pulmonary fellow, I ordered it countless times without ever looking at the dose. Sometimes, patients would come up from the emergency department after receiving a “continuous dose.” I would often wonder exactly what that meant. After some investigation, I found that in my hospital at the time, one dose of albuterol was 2.5 mg in 2 mL, and a continuous nebulization was four doses for a total of 10 mg.
Shrestha et al. found that high-dose albuterol (7.5 mg) administered continuously was superior to 2.5 mg albuterol delivered three times over 1.5 hours. There were demonstrable improvements in FEV1 and no ICU admissions.4 This study is one of many that compared intermittent to continuous and high-dose vs low-dose albuterol in the emergency department. Most are small and occur over the first 24 hours of presentation to the hospital. They often use short-term changes in spirometry as their primary outcome measure. Being a pulmonary and critical care doctor, I see patients who require advanced rescue maneuvers such as noninvasive positive pressure ventilation (NIPPV) or other pharmacologic adjuncts, for which the current evidence is limited.
Because studies of inhaled bronchodilators in acute asthma exacerbation use spirometry as their primary outcome, those with more severe disease and higher acuity are excluded. Patients on NIPPV can’t perform spirometry. There is essentially no literature to guide treatment for a patient with asthma in the adult ICU. In pediatric intensive care units, there are some data to support either continuous or intermittent inhaled bronchodilator that extends beyond the initial ED visit up to about 60 hours.5 Much of the pediatric data revolve about the amount of albuterol given, which can be as high as 75 mg/hr though is typically closer to 10-20 mg/hr.6 This rate is continued until respiratory improvement occurs.
With poor evidence to guide us and no specific direction from major guidelines, how should providers manage severe asthma exacerbation? The amount of drug deposited in the lung varies by the device used to deliver it. For nebulization, only about 10% of the nebulized amount reaches the lungs for effect; this is a smaller amount compared with all other devices one could use, such as MDI or DPI.7 Once a patient with asthma reaches the emergency department, that person is usually placed on some form of nebulizer treatment. But based on local hospital protocols, the amount and duration can vary widely. Sometimes, in patients with severe exacerbation, there is trepidation to continuing albuterol therapy due to ongoing tachycardia. This seems reasonable given increased albuterol administration could beget an ongoing cycle of dyspnea and anxiety. It could also lead to choosing therapies that are less evidence based.
In closing, this seemingly mundane topic takes on new meaning when a patient is in severe exacerbation. Fortunately, providers are not often faced with the decision to wade into the evidence-free territory of severe asthma exacerbation that is unresponsive to first-line treatments. This narrative should serve as a general alert that this pathophysiologic state is understudied. When encountered, thoughtful consideration of pathology, physiology, and pharmacology is required to reverse it.
References
1. Centers for Disease Control and Prevention. (2023, May 10). Most recent national asthma data. Centers for Disease Control and Prevention. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Global Initiative for Asthma - GINA. (2023, August 15). 2023 GINA Main Report - Global Initiative for Asthma - GINA. https://ginasthma.org/2023-gina-main-report/
3. Kiley J, Mensah GA, Boyce CA, et al (A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group). 2020 Focused updates to the: Asthma Management Guidelines. US Department of Health and Human Services, NIH, NHLBI 2020.
4. Shrestha M, Bidadi K, Gourlay S, Hayes J. Continuous vs intermittent albuterol, at high and low doses, in the treatment of severe acute asthma in adults. Chest. 1996 Jul;110(1):42-7. doi: 10.1378/chest.110.1.42. PMID: 8681661.
5. Kulalert P, Phinyo P, Patumanond J, Smathakanee C, Chuenjit W, Nanthapisal S. Continuous versus intermittent short-acting β2-agonists nebulization as first-line therapy in hospitalized children with severe asthma exacerbation: a propensity score matching analysis. Asthma Res Pract. 2020 Jul 2;6:6. doi: 10.1186/s40733-020-00059-5. PMID: 32632352; PMCID: PMC7329360.
6. Phumeetham S, Bahk TJ, Abd-Allah S, Mathur M. Effect of high-dose continuous albuterol nebulization on clinical variables in children with status asthmaticus. Pediatr Crit Care Med. 2015 Feb;16(2):e41-6. doi: 10.1097/PCC.0000000000000314. PMID: 25560428.
7. Gardenhire DS, Burnett D, Strickland S, Myers, TR. A guide to aerosol delivery devices for respiratory therapists. American Association for Respiratory Care, Dallas, Texas 2017.
Evidence-based medicine (EBM) stems from making the best patient-centered decision from the highest-quality data available that comports with our understanding of pathophysiology. In some situations, clinicians are forced to draw conclusions from data that are imperfect and apply it to patients who are complex and dynamic.
The Centers for Disease Control and Prevention (CDC) estimates that about 7.7% of the United States population has asthma. There were about 1 million ED visits in 2020, with asthma listed as the primary diagnosis, and only 94,000 required hospitalization.1 There are many tools we employ that have greatly decreased inpatient admissions for asthma. The uptake of inhaled corticosteroids (ICS) has significantly reduced asthma-related morbidity and mortality and reduced exacerbations that require admission to a hospital. This treatment strategy is supported by the Global Initiative for Asthma (GINA) and National Asthma Education and Prevention Program (NAEPP) guidelines.2,3 While we should celebrate the impact that EBM and ICS have had on asthma outcomes, we continue to struggle to control severe asthma.
Bronchodilator therapy in the hospital is ubiquitous. House staff and hospitalists click the bronchodilator order set early and often. However, the optimal frequency, dose, and duration of inhaled bronchodilator therapy for acute asthma exacerbation are unknown. Do frequency, dose, and duration change with exacerbation severity? Nothing gets ED, inpatient, or ICU physicians more jittery than the phrase “exacerbation of asthma on BiPap” or “intubated for asthma.” With its enormous clinical impact and notoriously difficult hospital and ICU course, the lack of evidence we have for managing these patients outside of the initial 24- to 48-hour visit is concerning. Neither NAEPP nor GINA provide management recommendations for the patient with severe asthma exacerbation that necessitates admission.
Albuterol is a commonly used medication for asthma and chronic obstructive airway disease. It is rapid acting and effective—few medications give patients (or clinicians) such instant satisfaction. As an internal medicine resident and pulmonary fellow, I ordered it countless times without ever looking at the dose. Sometimes, patients would come up from the emergency department after receiving a “continuous dose.” I would often wonder exactly what that meant. After some investigation, I found that in my hospital at the time, one dose of albuterol was 2.5 mg in 2 mL, and a continuous nebulization was four doses for a total of 10 mg.
Shrestha et al. found that high-dose albuterol (7.5 mg) administered continuously was superior to 2.5 mg albuterol delivered three times over 1.5 hours. There were demonstrable improvements in FEV1 and no ICU admissions.4 This study is one of many that compared intermittent to continuous and high-dose vs low-dose albuterol in the emergency department. Most are small and occur over the first 24 hours of presentation to the hospital. They often use short-term changes in spirometry as their primary outcome measure. Being a pulmonary and critical care doctor, I see patients who require advanced rescue maneuvers such as noninvasive positive pressure ventilation (NIPPV) or other pharmacologic adjuncts, for which the current evidence is limited.
Because studies of inhaled bronchodilators in acute asthma exacerbation use spirometry as their primary outcome, those with more severe disease and higher acuity are excluded. Patients on NIPPV can’t perform spirometry. There is essentially no literature to guide treatment for a patient with asthma in the adult ICU. In pediatric intensive care units, there are some data to support either continuous or intermittent inhaled bronchodilator that extends beyond the initial ED visit up to about 60 hours.5 Much of the pediatric data revolve about the amount of albuterol given, which can be as high as 75 mg/hr though is typically closer to 10-20 mg/hr.6 This rate is continued until respiratory improvement occurs.
With poor evidence to guide us and no specific direction from major guidelines, how should providers manage severe asthma exacerbation? The amount of drug deposited in the lung varies by the device used to deliver it. For nebulization, only about 10% of the nebulized amount reaches the lungs for effect; this is a smaller amount compared with all other devices one could use, such as MDI or DPI.7 Once a patient with asthma reaches the emergency department, that person is usually placed on some form of nebulizer treatment. But based on local hospital protocols, the amount and duration can vary widely. Sometimes, in patients with severe exacerbation, there is trepidation to continuing albuterol therapy due to ongoing tachycardia. This seems reasonable given increased albuterol administration could beget an ongoing cycle of dyspnea and anxiety. It could also lead to choosing therapies that are less evidence based.
In closing, this seemingly mundane topic takes on new meaning when a patient is in severe exacerbation. Fortunately, providers are not often faced with the decision to wade into the evidence-free territory of severe asthma exacerbation that is unresponsive to first-line treatments. This narrative should serve as a general alert that this pathophysiologic state is understudied. When encountered, thoughtful consideration of pathology, physiology, and pharmacology is required to reverse it.
References
1. Centers for Disease Control and Prevention. (2023, May 10). Most recent national asthma data. Centers for Disease Control and Prevention. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
2. Global Initiative for Asthma - GINA. (2023, August 15). 2023 GINA Main Report - Global Initiative for Asthma - GINA. https://ginasthma.org/2023-gina-main-report/
3. Kiley J, Mensah GA, Boyce CA, et al (A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group). 2020 Focused updates to the: Asthma Management Guidelines. US Department of Health and Human Services, NIH, NHLBI 2020.
4. Shrestha M, Bidadi K, Gourlay S, Hayes J. Continuous vs intermittent albuterol, at high and low doses, in the treatment of severe acute asthma in adults. Chest. 1996 Jul;110(1):42-7. doi: 10.1378/chest.110.1.42. PMID: 8681661.
5. Kulalert P, Phinyo P, Patumanond J, Smathakanee C, Chuenjit W, Nanthapisal S. Continuous versus intermittent short-acting β2-agonists nebulization as first-line therapy in hospitalized children with severe asthma exacerbation: a propensity score matching analysis. Asthma Res Pract. 2020 Jul 2;6:6. doi: 10.1186/s40733-020-00059-5. PMID: 32632352; PMCID: PMC7329360.
6. Phumeetham S, Bahk TJ, Abd-Allah S, Mathur M. Effect of high-dose continuous albuterol nebulization on clinical variables in children with status asthmaticus. Pediatr Crit Care Med. 2015 Feb;16(2):e41-6. doi: 10.1097/PCC.0000000000000314. PMID: 25560428.
7. Gardenhire DS, Burnett D, Strickland S, Myers, TR. A guide to aerosol delivery devices for respiratory therapists. American Association for Respiratory Care, Dallas, Texas 2017.
The Nose Knows
A few weeks ago I stumbled upon a two-sentence blurb in a pediatric newsletter summarizing the results of a study comparing the chemical profile of infant body odor with that of postpubertal adolescents. The investigators found that, not surprisingly, the smell of the chemical constituents wafting from babies was more appealing than that emanating from sweaty teenagers. I quickly moved on to the next blurb hoping to find something I hadn’t already experienced or figured out on my own.
But, as I navigated through the rest of my day filled with pickleball, bicycling, and the smell of home-cooked food, something about that study of body odor nagged at me. Who had funded that voyage into the obvious? Were my tax dollars involved? Had I been duped by some alleged nonprofit that had promised my donation would save lives or at least ameliorate suffering? Finally, as the sun dipped below the horizon, my curiosity got the best of me and I searched out the original study. Within minutes I fell down a rabbit hole into the cavernous world of odor science.
Having had zero experience in this niche field, I was amazed at the lengths to which these German odor investigators had gone to analyze the chemicals on and around their subjects. Just trying to ensure that materials and microclimates in the experimental environment were scent-free was a heroic effort. There was “Mono-trap sampling of volatiles, followed by thermodesorption-comprehensive gas chromatography, and time of flight-mass spectrometry analysis.” There were graphs and charts galore. This is serious science, folks. However, they still use the abbreviation “BO” freely, just as I learned to do in junior high. And, in some situations, the investigators relied on the observation of a panel of trained human sniffers to assess the detection threshold and the degree of pleasantness.
Ultimately, the authors’ conclusion was “sexual maturation coincides with changes in body odor chemical composition. Whether those changes explain differences in parental olfactory perception needs to be determined in future studies.” Again, no surprises here.
Exhausted by my venture into the realm of odor science, I finally found the answer to my burning question. The study was supported by the German Research Foundation and the European Union. Phew! Not on my nickel.
Lest you think that I believe any investigation into the potential role of smell in our health and well-being is pure bunk, let me make it clear that I think the role of odor detection is one of the least well-studied and potentially most valuable areas of medical research. Having had one family tell me that their black lab had twice successfully “diagnosed” their pre-verbal child’s ear infection (which I confirmed with an otoscope and the tympanic membrane was intact) I have been keenly interested in the role of animal-assisted diagnosis.
If you also have wondered whether you could write off your pedigreed Portuguese Water Dog as an office expense, I would direct you to an article titled “Canine olfactory detection and its relevance to medical detection.” The authors note that there is some evidence of dogs successfully alerting physicians to Parkinson’s disease, some cancers, malaria, and COVID-19, among others. However, they caution that the reliability is, in most cases, not of a quality that would be helpful on a larger scale.
I can understand the reasons for their caution. However, from my own personal experience, I am completely confident that I can diagnose strep throat by smell, sometimes simply on opening the examination room door. My false-positive rate over 40 years of practice is zero. Of course I still test and, not surprisingly, my false-negative rate is nothing to brag about. However, if a dog can produce even close to my zero false negative with a given disease, that information is valuable and suggests that we should be pointing the odor investigators and their tool box of skills in that direction. I’m pretty sure we don’t need them to dig much deeper into why babies smell better than teenagers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
A few weeks ago I stumbled upon a two-sentence blurb in a pediatric newsletter summarizing the results of a study comparing the chemical profile of infant body odor with that of postpubertal adolescents. The investigators found that, not surprisingly, the smell of the chemical constituents wafting from babies was more appealing than that emanating from sweaty teenagers. I quickly moved on to the next blurb hoping to find something I hadn’t already experienced or figured out on my own.
But, as I navigated through the rest of my day filled with pickleball, bicycling, and the smell of home-cooked food, something about that study of body odor nagged at me. Who had funded that voyage into the obvious? Were my tax dollars involved? Had I been duped by some alleged nonprofit that had promised my donation would save lives or at least ameliorate suffering? Finally, as the sun dipped below the horizon, my curiosity got the best of me and I searched out the original study. Within minutes I fell down a rabbit hole into the cavernous world of odor science.
Having had zero experience in this niche field, I was amazed at the lengths to which these German odor investigators had gone to analyze the chemicals on and around their subjects. Just trying to ensure that materials and microclimates in the experimental environment were scent-free was a heroic effort. There was “Mono-trap sampling of volatiles, followed by thermodesorption-comprehensive gas chromatography, and time of flight-mass spectrometry analysis.” There were graphs and charts galore. This is serious science, folks. However, they still use the abbreviation “BO” freely, just as I learned to do in junior high. And, in some situations, the investigators relied on the observation of a panel of trained human sniffers to assess the detection threshold and the degree of pleasantness.
Ultimately, the authors’ conclusion was “sexual maturation coincides with changes in body odor chemical composition. Whether those changes explain differences in parental olfactory perception needs to be determined in future studies.” Again, no surprises here.
Exhausted by my venture into the realm of odor science, I finally found the answer to my burning question. The study was supported by the German Research Foundation and the European Union. Phew! Not on my nickel.
Lest you think that I believe any investigation into the potential role of smell in our health and well-being is pure bunk, let me make it clear that I think the role of odor detection is one of the least well-studied and potentially most valuable areas of medical research. Having had one family tell me that their black lab had twice successfully “diagnosed” their pre-verbal child’s ear infection (which I confirmed with an otoscope and the tympanic membrane was intact) I have been keenly interested in the role of animal-assisted diagnosis.
If you also have wondered whether you could write off your pedigreed Portuguese Water Dog as an office expense, I would direct you to an article titled “Canine olfactory detection and its relevance to medical detection.” The authors note that there is some evidence of dogs successfully alerting physicians to Parkinson’s disease, some cancers, malaria, and COVID-19, among others. However, they caution that the reliability is, in most cases, not of a quality that would be helpful on a larger scale.
I can understand the reasons for their caution. However, from my own personal experience, I am completely confident that I can diagnose strep throat by smell, sometimes simply on opening the examination room door. My false-positive rate over 40 years of practice is zero. Of course I still test and, not surprisingly, my false-negative rate is nothing to brag about. However, if a dog can produce even close to my zero false negative with a given disease, that information is valuable and suggests that we should be pointing the odor investigators and their tool box of skills in that direction. I’m pretty sure we don’t need them to dig much deeper into why babies smell better than teenagers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
A few weeks ago I stumbled upon a two-sentence blurb in a pediatric newsletter summarizing the results of a study comparing the chemical profile of infant body odor with that of postpubertal adolescents. The investigators found that, not surprisingly, the smell of the chemical constituents wafting from babies was more appealing than that emanating from sweaty teenagers. I quickly moved on to the next blurb hoping to find something I hadn’t already experienced or figured out on my own.
But, as I navigated through the rest of my day filled with pickleball, bicycling, and the smell of home-cooked food, something about that study of body odor nagged at me. Who had funded that voyage into the obvious? Were my tax dollars involved? Had I been duped by some alleged nonprofit that had promised my donation would save lives or at least ameliorate suffering? Finally, as the sun dipped below the horizon, my curiosity got the best of me and I searched out the original study. Within minutes I fell down a rabbit hole into the cavernous world of odor science.
Having had zero experience in this niche field, I was amazed at the lengths to which these German odor investigators had gone to analyze the chemicals on and around their subjects. Just trying to ensure that materials and microclimates in the experimental environment were scent-free was a heroic effort. There was “Mono-trap sampling of volatiles, followed by thermodesorption-comprehensive gas chromatography, and time of flight-mass spectrometry analysis.” There were graphs and charts galore. This is serious science, folks. However, they still use the abbreviation “BO” freely, just as I learned to do in junior high. And, in some situations, the investigators relied on the observation of a panel of trained human sniffers to assess the detection threshold and the degree of pleasantness.
Ultimately, the authors’ conclusion was “sexual maturation coincides with changes in body odor chemical composition. Whether those changes explain differences in parental olfactory perception needs to be determined in future studies.” Again, no surprises here.
Exhausted by my venture into the realm of odor science, I finally found the answer to my burning question. The study was supported by the German Research Foundation and the European Union. Phew! Not on my nickel.
Lest you think that I believe any investigation into the potential role of smell in our health and well-being is pure bunk, let me make it clear that I think the role of odor detection is one of the least well-studied and potentially most valuable areas of medical research. Having had one family tell me that their black lab had twice successfully “diagnosed” their pre-verbal child’s ear infection (which I confirmed with an otoscope and the tympanic membrane was intact) I have been keenly interested in the role of animal-assisted diagnosis.
If you also have wondered whether you could write off your pedigreed Portuguese Water Dog as an office expense, I would direct you to an article titled “Canine olfactory detection and its relevance to medical detection.” The authors note that there is some evidence of dogs successfully alerting physicians to Parkinson’s disease, some cancers, malaria, and COVID-19, among others. However, they caution that the reliability is, in most cases, not of a quality that would be helpful on a larger scale.
I can understand the reasons for their caution. However, from my own personal experience, I am completely confident that I can diagnose strep throat by smell, sometimes simply on opening the examination room door. My false-positive rate over 40 years of practice is zero. Of course I still test and, not surprisingly, my false-negative rate is nothing to brag about. However, if a dog can produce even close to my zero false negative with a given disease, that information is valuable and suggests that we should be pointing the odor investigators and their tool box of skills in that direction. I’m pretty sure we don’t need them to dig much deeper into why babies smell better than teenagers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
No Increased Stroke Risk After COVID-19 Bivalent Vaccine
TOPLINE:
, a new study of Medicare beneficiaries showed.
METHODOLOGY:
- The analysis included 5.4 million people age ≥ 65 years who received either the Pfizer-BioNTech COVID-19 bivalent vaccine or the Moderna bivalent vaccine, or the Pfizer vaccine and a high-dose or adjuvanted concomitant influenza vaccine (ie, administered on the same day).
- A total of 11,001 of the cohort experienced a stroke in the first 90 days after vaccination.
- The main outcome was stroke risk (nonhemorrhagic stroke, transient ischemic attack [TIA], or hemorrhagic stroke) during the 1- to 21-day or 22- to 42-day window after vaccination vs the 43- to 90-day control window.
- The mean age of participants was 74 years, and 56% were female.
TAKEAWAY:
- There was no statistically significant association with either brand of the COVID-19 bivalent vaccine or any of the stroke outcomes during the 1- to 21-day or 22- to 42-day risk window compared with the 43- to 90-day control window (incidence rate ratio [IRR] range, 0.72-1.12).
- Vaccination with COVID-19 bivalent vaccine plus a high-dose or adjuvanted influenza vaccine (n = 4596) was associated with a significantly greater risk for nonhemorrhagic stroke 22-42 days after vaccination with Pfizer-BioNTech (IRR, 1.20; risk difference/100,000 doses, 3.13) and an increase in TIA risk 1-21 days after vaccination with Moderna (IRR, 1.35; risk difference/100,000 doses, 3.33).
- There was a significant association between vaccination with a high-dose or adjuvanted influenza vaccine (n = 21,345) and nonhemorrhagic stroke 22-42 days after vaccination (IRR, 1.09; risk difference/100,000 doses, 1.65).
IN PRACTICE:
“The clinical significance of the risk of stroke after vaccination must be carefully considered together with the significant benefits of receiving an influenza vaccination,” the authors wrote. “Because the framework of the current self-controlled case series study does not compare the populations who were vaccinated vs those who were unvaccinated, it does not account for the reduced rate of severe influenza after vaccination. More studies are needed to better understand the association between high-dose or adjuvanted influenza vaccination and stroke.”
SOURCE:
Yun Lu, PhD, of the Center for Biologics Evaluation and Research, US Food and Drug Administration, Silver Spring, Maryland, was the lead and corresponding author of the study. It was published online on March 19 in JAMA.
LIMITATIONS:
Some stroke cases may have been missed or misclassified. The study included only vaccinated individuals — a population considered to have health-seeking behaviors — which may limit the generalizability of the findings. The study was conducted using COVID-19 bivalent vaccines, which are no longer available.
DISCLOSURES:
This work was funded by the US Food and Drug Administration through an interagency agreement with the Centers for Medicare & Medicaid Services. Dr. Lu reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new study of Medicare beneficiaries showed.
METHODOLOGY:
- The analysis included 5.4 million people age ≥ 65 years who received either the Pfizer-BioNTech COVID-19 bivalent vaccine or the Moderna bivalent vaccine, or the Pfizer vaccine and a high-dose or adjuvanted concomitant influenza vaccine (ie, administered on the same day).
- A total of 11,001 of the cohort experienced a stroke in the first 90 days after vaccination.
- The main outcome was stroke risk (nonhemorrhagic stroke, transient ischemic attack [TIA], or hemorrhagic stroke) during the 1- to 21-day or 22- to 42-day window after vaccination vs the 43- to 90-day control window.
- The mean age of participants was 74 years, and 56% were female.
TAKEAWAY:
- There was no statistically significant association with either brand of the COVID-19 bivalent vaccine or any of the stroke outcomes during the 1- to 21-day or 22- to 42-day risk window compared with the 43- to 90-day control window (incidence rate ratio [IRR] range, 0.72-1.12).
- Vaccination with COVID-19 bivalent vaccine plus a high-dose or adjuvanted influenza vaccine (n = 4596) was associated with a significantly greater risk for nonhemorrhagic stroke 22-42 days after vaccination with Pfizer-BioNTech (IRR, 1.20; risk difference/100,000 doses, 3.13) and an increase in TIA risk 1-21 days after vaccination with Moderna (IRR, 1.35; risk difference/100,000 doses, 3.33).
- There was a significant association between vaccination with a high-dose or adjuvanted influenza vaccine (n = 21,345) and nonhemorrhagic stroke 22-42 days after vaccination (IRR, 1.09; risk difference/100,000 doses, 1.65).
IN PRACTICE:
“The clinical significance of the risk of stroke after vaccination must be carefully considered together with the significant benefits of receiving an influenza vaccination,” the authors wrote. “Because the framework of the current self-controlled case series study does not compare the populations who were vaccinated vs those who were unvaccinated, it does not account for the reduced rate of severe influenza after vaccination. More studies are needed to better understand the association between high-dose or adjuvanted influenza vaccination and stroke.”
SOURCE:
Yun Lu, PhD, of the Center for Biologics Evaluation and Research, US Food and Drug Administration, Silver Spring, Maryland, was the lead and corresponding author of the study. It was published online on March 19 in JAMA.
LIMITATIONS:
Some stroke cases may have been missed or misclassified. The study included only vaccinated individuals — a population considered to have health-seeking behaviors — which may limit the generalizability of the findings. The study was conducted using COVID-19 bivalent vaccines, which are no longer available.
DISCLOSURES:
This work was funded by the US Food and Drug Administration through an interagency agreement with the Centers for Medicare & Medicaid Services. Dr. Lu reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new study of Medicare beneficiaries showed.
METHODOLOGY:
- The analysis included 5.4 million people age ≥ 65 years who received either the Pfizer-BioNTech COVID-19 bivalent vaccine or the Moderna bivalent vaccine, or the Pfizer vaccine and a high-dose or adjuvanted concomitant influenza vaccine (ie, administered on the same day).
- A total of 11,001 of the cohort experienced a stroke in the first 90 days after vaccination.
- The main outcome was stroke risk (nonhemorrhagic stroke, transient ischemic attack [TIA], or hemorrhagic stroke) during the 1- to 21-day or 22- to 42-day window after vaccination vs the 43- to 90-day control window.
- The mean age of participants was 74 years, and 56% were female.
TAKEAWAY:
- There was no statistically significant association with either brand of the COVID-19 bivalent vaccine or any of the stroke outcomes during the 1- to 21-day or 22- to 42-day risk window compared with the 43- to 90-day control window (incidence rate ratio [IRR] range, 0.72-1.12).
- Vaccination with COVID-19 bivalent vaccine plus a high-dose or adjuvanted influenza vaccine (n = 4596) was associated with a significantly greater risk for nonhemorrhagic stroke 22-42 days after vaccination with Pfizer-BioNTech (IRR, 1.20; risk difference/100,000 doses, 3.13) and an increase in TIA risk 1-21 days after vaccination with Moderna (IRR, 1.35; risk difference/100,000 doses, 3.33).
- There was a significant association between vaccination with a high-dose or adjuvanted influenza vaccine (n = 21,345) and nonhemorrhagic stroke 22-42 days after vaccination (IRR, 1.09; risk difference/100,000 doses, 1.65).
IN PRACTICE:
“The clinical significance of the risk of stroke after vaccination must be carefully considered together with the significant benefits of receiving an influenza vaccination,” the authors wrote. “Because the framework of the current self-controlled case series study does not compare the populations who were vaccinated vs those who were unvaccinated, it does not account for the reduced rate of severe influenza after vaccination. More studies are needed to better understand the association between high-dose or adjuvanted influenza vaccination and stroke.”
SOURCE:
Yun Lu, PhD, of the Center for Biologics Evaluation and Research, US Food and Drug Administration, Silver Spring, Maryland, was the lead and corresponding author of the study. It was published online on March 19 in JAMA.
LIMITATIONS:
Some stroke cases may have been missed or misclassified. The study included only vaccinated individuals — a population considered to have health-seeking behaviors — which may limit the generalizability of the findings. The study was conducted using COVID-19 bivalent vaccines, which are no longer available.
DISCLOSURES:
This work was funded by the US Food and Drug Administration through an interagency agreement with the Centers for Medicare & Medicaid Services. Dr. Lu reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
Tarlatamab Shows Promise in Tackling Previously Treated SCLC
The investigational bispecific T-cell engager tarlatamab achieved durable responses and clinically meaningful survival outcomes in patients with small-cell lung cancer (SCLC), particularly at lower doses, according to a follow-up analysis of the phase 1 DeLLphi-300 trial.
Most patients with central nervous system tumors also sustained tumor shrinkage long after receiving radiotherapy, providing “encouraging evidence” of the new agent’s intracranial activity, said study presenter Horst-Dieter Hummel, MD, Comprehensive Cancer Center Mainfranken, Würzburg, Germany.
The research was presented at the European Lung Cancer Congress 2024 on March 22.
Data from the phase 1 and phase 2 DeLLphi trials, published last year, showed the compound achieved “encouraging clinical activity” in pretreated patients, said Dr. Hummel.
The initial phase 1 DeLLphi study found that after a median follow-up of 8.7 months, the immunotherapy led to a disease control rate of 51.4%, a median progression-free survival of 3.7 months, and median overall survival of 13.2 months.
At the meeting, Dr. Hummel reported longer-term outcomes from the phase 1 study over a median of 12.1 months as well as intracranial activity in patients who received clinically relevant doses of tarlatamab, defined as ≥ 10 mg.
The 152 patients included in the analysis had a median of two prior lines of therapy; 76.3% had undergone radiotherapy, and 63.2% had received immunotherapy. Liver metastases were present in 42.1% of patients, and 25.0% had brain metastases.
Doses varied among participants, with 76 patients (50.0%) receiving 100 mg, 32 (21.0%) receiving 100 mg via extended intravenous infusion, 17 (11.2%) receiving 10 mg, and 8 (5.3%) receiving 30 mg.
The overall objective response rate was 25.0%, with a median duration of response of 11.2 months. Among patients given the 10-mg dose, the objective response rate was higher, at 35.3%, as was the median duration of response, at 14.9 months.
Tarlatamab was associated with a median overall survival of 17.5 months, with 57.9% of patients alive at 12 months. Patients receiving the 10 mg dose had a better median overall survival of 20.3 months.
Of the 16 patients with analyzable central nervous system tumors, 62.5% experienced tumor shrinkage by ≥ 30% and 87.5% experienced intracranial disease control, which lasted for a median of 7.4 months.
In this follow-up study, tarlatamab demonstrated “clinically meaningful survival outcomes in patients with previously treated SCLC, particularly with the 10 mg dose,” Dr. Hummel concluded in his presentation.
No new safety signals emerged, though almost all patients did experience tarlatamab-related adverse events (94.8% for doses > 10 mg and 100% of patients with 10 mg doses). Overall, 66.4% of the total cohort experienced cytokine release syndrome of any grade, and 11.8% developed immune effector cell-associated neurotoxicity syndrome.
Discontinuation due to treatment-related adverse events occurred in 9 patients overall, and adverse events that led to dose interruption or reduction occurred in 32 patients overall.
“After many efforts at DLL3 targeting, we finally have an agent that shows activity and efficacy, and with convincing data,” said Jessica Menis, MD, a medical oncologist at the oncology department of the University Hospital of Verona, Italy, who was not involved in the study. The intracranial activity of tarlatamab “needs to be further evaluated in untreated patients,” Dr. Menis noted, because the study included only patients with stable, treated brain metastases.
And given the high rates of adverse events, Dr. Menis cautioned that adverse event management “will be a challenge.”
On X (Twitter), Tom Newsom-Davis, MBBS, PhD, a consultant in medical oncology at Chelsea and Westminster Hospital, London, said that tarlatamab is “not a straightforward drug to use,” highlighting the occurrence of cytokine release syndrome.
“But in this significantly pretreated population and in this hard-to-treat tumor type,” the rate and duration of responses seen with the extended follow-up are ‘impressive’,” he added.
DeLLphi-300, 301, and 304 were funded by Amgen Inc. Dr. Hummel declared relationships with several companies, including Amgen, Bristol Myers Squibb, AstraZeneca, Celgene, Merck, Novartis, Daiichi Sankyo, and Roche. Dr. Menis declared relationships with AstraZeneca, BMS, MSD, Roche, and Novartis.
A version of this article appeared on Medscape.com.
The investigational bispecific T-cell engager tarlatamab achieved durable responses and clinically meaningful survival outcomes in patients with small-cell lung cancer (SCLC), particularly at lower doses, according to a follow-up analysis of the phase 1 DeLLphi-300 trial.
Most patients with central nervous system tumors also sustained tumor shrinkage long after receiving radiotherapy, providing “encouraging evidence” of the new agent’s intracranial activity, said study presenter Horst-Dieter Hummel, MD, Comprehensive Cancer Center Mainfranken, Würzburg, Germany.
The research was presented at the European Lung Cancer Congress 2024 on March 22.
Data from the phase 1 and phase 2 DeLLphi trials, published last year, showed the compound achieved “encouraging clinical activity” in pretreated patients, said Dr. Hummel.
The initial phase 1 DeLLphi study found that after a median follow-up of 8.7 months, the immunotherapy led to a disease control rate of 51.4%, a median progression-free survival of 3.7 months, and median overall survival of 13.2 months.
At the meeting, Dr. Hummel reported longer-term outcomes from the phase 1 study over a median of 12.1 months as well as intracranial activity in patients who received clinically relevant doses of tarlatamab, defined as ≥ 10 mg.
The 152 patients included in the analysis had a median of two prior lines of therapy; 76.3% had undergone radiotherapy, and 63.2% had received immunotherapy. Liver metastases were present in 42.1% of patients, and 25.0% had brain metastases.
Doses varied among participants, with 76 patients (50.0%) receiving 100 mg, 32 (21.0%) receiving 100 mg via extended intravenous infusion, 17 (11.2%) receiving 10 mg, and 8 (5.3%) receiving 30 mg.
The overall objective response rate was 25.0%, with a median duration of response of 11.2 months. Among patients given the 10-mg dose, the objective response rate was higher, at 35.3%, as was the median duration of response, at 14.9 months.
Tarlatamab was associated with a median overall survival of 17.5 months, with 57.9% of patients alive at 12 months. Patients receiving the 10 mg dose had a better median overall survival of 20.3 months.
Of the 16 patients with analyzable central nervous system tumors, 62.5% experienced tumor shrinkage by ≥ 30% and 87.5% experienced intracranial disease control, which lasted for a median of 7.4 months.
In this follow-up study, tarlatamab demonstrated “clinically meaningful survival outcomes in patients with previously treated SCLC, particularly with the 10 mg dose,” Dr. Hummel concluded in his presentation.
No new safety signals emerged, though almost all patients did experience tarlatamab-related adverse events (94.8% for doses > 10 mg and 100% of patients with 10 mg doses). Overall, 66.4% of the total cohort experienced cytokine release syndrome of any grade, and 11.8% developed immune effector cell-associated neurotoxicity syndrome.
Discontinuation due to treatment-related adverse events occurred in 9 patients overall, and adverse events that led to dose interruption or reduction occurred in 32 patients overall.
“After many efforts at DLL3 targeting, we finally have an agent that shows activity and efficacy, and with convincing data,” said Jessica Menis, MD, a medical oncologist at the oncology department of the University Hospital of Verona, Italy, who was not involved in the study. The intracranial activity of tarlatamab “needs to be further evaluated in untreated patients,” Dr. Menis noted, because the study included only patients with stable, treated brain metastases.
And given the high rates of adverse events, Dr. Menis cautioned that adverse event management “will be a challenge.”
On X (Twitter), Tom Newsom-Davis, MBBS, PhD, a consultant in medical oncology at Chelsea and Westminster Hospital, London, said that tarlatamab is “not a straightforward drug to use,” highlighting the occurrence of cytokine release syndrome.
“But in this significantly pretreated population and in this hard-to-treat tumor type,” the rate and duration of responses seen with the extended follow-up are ‘impressive’,” he added.
DeLLphi-300, 301, and 304 were funded by Amgen Inc. Dr. Hummel declared relationships with several companies, including Amgen, Bristol Myers Squibb, AstraZeneca, Celgene, Merck, Novartis, Daiichi Sankyo, and Roche. Dr. Menis declared relationships with AstraZeneca, BMS, MSD, Roche, and Novartis.
A version of this article appeared on Medscape.com.
The investigational bispecific T-cell engager tarlatamab achieved durable responses and clinically meaningful survival outcomes in patients with small-cell lung cancer (SCLC), particularly at lower doses, according to a follow-up analysis of the phase 1 DeLLphi-300 trial.
Most patients with central nervous system tumors also sustained tumor shrinkage long after receiving radiotherapy, providing “encouraging evidence” of the new agent’s intracranial activity, said study presenter Horst-Dieter Hummel, MD, Comprehensive Cancer Center Mainfranken, Würzburg, Germany.
The research was presented at the European Lung Cancer Congress 2024 on March 22.
Data from the phase 1 and phase 2 DeLLphi trials, published last year, showed the compound achieved “encouraging clinical activity” in pretreated patients, said Dr. Hummel.
The initial phase 1 DeLLphi study found that after a median follow-up of 8.7 months, the immunotherapy led to a disease control rate of 51.4%, a median progression-free survival of 3.7 months, and median overall survival of 13.2 months.
At the meeting, Dr. Hummel reported longer-term outcomes from the phase 1 study over a median of 12.1 months as well as intracranial activity in patients who received clinically relevant doses of tarlatamab, defined as ≥ 10 mg.
The 152 patients included in the analysis had a median of two prior lines of therapy; 76.3% had undergone radiotherapy, and 63.2% had received immunotherapy. Liver metastases were present in 42.1% of patients, and 25.0% had brain metastases.
Doses varied among participants, with 76 patients (50.0%) receiving 100 mg, 32 (21.0%) receiving 100 mg via extended intravenous infusion, 17 (11.2%) receiving 10 mg, and 8 (5.3%) receiving 30 mg.
The overall objective response rate was 25.0%, with a median duration of response of 11.2 months. Among patients given the 10-mg dose, the objective response rate was higher, at 35.3%, as was the median duration of response, at 14.9 months.
Tarlatamab was associated with a median overall survival of 17.5 months, with 57.9% of patients alive at 12 months. Patients receiving the 10 mg dose had a better median overall survival of 20.3 months.
Of the 16 patients with analyzable central nervous system tumors, 62.5% experienced tumor shrinkage by ≥ 30% and 87.5% experienced intracranial disease control, which lasted for a median of 7.4 months.
In this follow-up study, tarlatamab demonstrated “clinically meaningful survival outcomes in patients with previously treated SCLC, particularly with the 10 mg dose,” Dr. Hummel concluded in his presentation.
No new safety signals emerged, though almost all patients did experience tarlatamab-related adverse events (94.8% for doses > 10 mg and 100% of patients with 10 mg doses). Overall, 66.4% of the total cohort experienced cytokine release syndrome of any grade, and 11.8% developed immune effector cell-associated neurotoxicity syndrome.
Discontinuation due to treatment-related adverse events occurred in 9 patients overall, and adverse events that led to dose interruption or reduction occurred in 32 patients overall.
“After many efforts at DLL3 targeting, we finally have an agent that shows activity and efficacy, and with convincing data,” said Jessica Menis, MD, a medical oncologist at the oncology department of the University Hospital of Verona, Italy, who was not involved in the study. The intracranial activity of tarlatamab “needs to be further evaluated in untreated patients,” Dr. Menis noted, because the study included only patients with stable, treated brain metastases.
And given the high rates of adverse events, Dr. Menis cautioned that adverse event management “will be a challenge.”
On X (Twitter), Tom Newsom-Davis, MBBS, PhD, a consultant in medical oncology at Chelsea and Westminster Hospital, London, said that tarlatamab is “not a straightforward drug to use,” highlighting the occurrence of cytokine release syndrome.
“But in this significantly pretreated population and in this hard-to-treat tumor type,” the rate and duration of responses seen with the extended follow-up are ‘impressive’,” he added.
DeLLphi-300, 301, and 304 were funded by Amgen Inc. Dr. Hummel declared relationships with several companies, including Amgen, Bristol Myers Squibb, AstraZeneca, Celgene, Merck, Novartis, Daiichi Sankyo, and Roche. Dr. Menis declared relationships with AstraZeneca, BMS, MSD, Roche, and Novartis.
A version of this article appeared on Medscape.com.
FROM ELCC 2024