User login
Higher rates of PTSD, BPD in transgender vs. cisgender psych patients
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
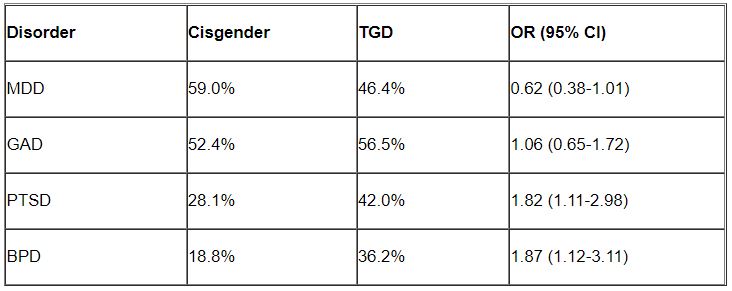
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF CLINICAL PSYCHIATRY
Borderline personality disorder raises relapse risk for MDD patients after ECT
ECT has demonstrated effectiveness for treatment of unipolar and bipolar major depression, but relapses within 6 months are frequent, and potential factors affecting relapse have not been well studied, wrote Matthieu Hein, MD, PhD, of Erasme Hospital, Université Libre de Bruxelles, and colleagues.
Borderline personality disorder (BPD) is a common comorbidity among individuals with major depressive disorder, and previous research suggests a possible negative effect of BPD on ECT response in MDD patients, they wrote.
In a study published in Psychiatry Research, the researchers recruited 68 females and 41 males aged 18 years and older with diagnosed MDD who had partial or complete response to ECT after receiving treatment at a single center. Approximately two-thirds of the patients were aged 50 years and older, and 22 met criteria for BPD. The ECT consisted of three sessions per week; the total number of sessions ranged from 6 to 18.
The primary outcome was relapse at 6 months after ECT treatment. Relapse was defined as a score of 16 or higher on the Hamilton Depression Rating Scale in combination with a mean absolute increase of at least 10 points from the psychiatric interview at the end of the ECT.
Relapse rates at 6 months were 37.6% for the study population overall, but significantly higher for those with BPD, compared with those without BPD (72.7% vs. 28.7%; P < .001).
In a multivariate analysis, adjusting for age, gender, and mood stabilizer use after ECT, relapse was approximately four times more likely among individuals with BPD, compared with those without (hazard ratio, 4.14). No significant association appeared between increased relapse and other comorbid personality disorders, anxiety disorders, alcohol or substance use disorders, or hospitalization during the ECT treatment period.
Potential reasons for the increased relapse risk among individuals with MDD and BPD include the younger age of the individuals with BPD, which has been shown to increase MDD relapse risk; the direct negative impact of BPD on mental functioning; and the documented tendency to poor treatment adherence, the researchers wrote in their discussion.
“Given these different elements, it seems important to screen more systematically for BPD in major depressed individuals treated with ECT in order to allow the implementation of more effective prevention strategies for relapse within 6 months in this particular subpopulation,” they emphasized.
“The demonstration of this higher risk of relapse within 6 months associated with BPD in major depressed individuals treated with ECT could open new therapeutic perspectives to allow better maintenance of euthymia in this particular subpopulation,” they added.
The study findings were limited by several factors including the retrospective design and the focus on only BPD, which may not generalize to other personality disorders, the researchers noted.
However, the results support data from previous studies and highlight the need for more systematic BPD screening in MDD patients to prevent relapse after ECT, they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
ECT has demonstrated effectiveness for treatment of unipolar and bipolar major depression, but relapses within 6 months are frequent, and potential factors affecting relapse have not been well studied, wrote Matthieu Hein, MD, PhD, of Erasme Hospital, Université Libre de Bruxelles, and colleagues.
Borderline personality disorder (BPD) is a common comorbidity among individuals with major depressive disorder, and previous research suggests a possible negative effect of BPD on ECT response in MDD patients, they wrote.
In a study published in Psychiatry Research, the researchers recruited 68 females and 41 males aged 18 years and older with diagnosed MDD who had partial or complete response to ECT after receiving treatment at a single center. Approximately two-thirds of the patients were aged 50 years and older, and 22 met criteria for BPD. The ECT consisted of three sessions per week; the total number of sessions ranged from 6 to 18.
The primary outcome was relapse at 6 months after ECT treatment. Relapse was defined as a score of 16 or higher on the Hamilton Depression Rating Scale in combination with a mean absolute increase of at least 10 points from the psychiatric interview at the end of the ECT.
Relapse rates at 6 months were 37.6% for the study population overall, but significantly higher for those with BPD, compared with those without BPD (72.7% vs. 28.7%; P < .001).
In a multivariate analysis, adjusting for age, gender, and mood stabilizer use after ECT, relapse was approximately four times more likely among individuals with BPD, compared with those without (hazard ratio, 4.14). No significant association appeared between increased relapse and other comorbid personality disorders, anxiety disorders, alcohol or substance use disorders, or hospitalization during the ECT treatment period.
Potential reasons for the increased relapse risk among individuals with MDD and BPD include the younger age of the individuals with BPD, which has been shown to increase MDD relapse risk; the direct negative impact of BPD on mental functioning; and the documented tendency to poor treatment adherence, the researchers wrote in their discussion.
“Given these different elements, it seems important to screen more systematically for BPD in major depressed individuals treated with ECT in order to allow the implementation of more effective prevention strategies for relapse within 6 months in this particular subpopulation,” they emphasized.
“The demonstration of this higher risk of relapse within 6 months associated with BPD in major depressed individuals treated with ECT could open new therapeutic perspectives to allow better maintenance of euthymia in this particular subpopulation,” they added.
The study findings were limited by several factors including the retrospective design and the focus on only BPD, which may not generalize to other personality disorders, the researchers noted.
However, the results support data from previous studies and highlight the need for more systematic BPD screening in MDD patients to prevent relapse after ECT, they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
ECT has demonstrated effectiveness for treatment of unipolar and bipolar major depression, but relapses within 6 months are frequent, and potential factors affecting relapse have not been well studied, wrote Matthieu Hein, MD, PhD, of Erasme Hospital, Université Libre de Bruxelles, and colleagues.
Borderline personality disorder (BPD) is a common comorbidity among individuals with major depressive disorder, and previous research suggests a possible negative effect of BPD on ECT response in MDD patients, they wrote.
In a study published in Psychiatry Research, the researchers recruited 68 females and 41 males aged 18 years and older with diagnosed MDD who had partial or complete response to ECT after receiving treatment at a single center. Approximately two-thirds of the patients were aged 50 years and older, and 22 met criteria for BPD. The ECT consisted of three sessions per week; the total number of sessions ranged from 6 to 18.
The primary outcome was relapse at 6 months after ECT treatment. Relapse was defined as a score of 16 or higher on the Hamilton Depression Rating Scale in combination with a mean absolute increase of at least 10 points from the psychiatric interview at the end of the ECT.
Relapse rates at 6 months were 37.6% for the study population overall, but significantly higher for those with BPD, compared with those without BPD (72.7% vs. 28.7%; P < .001).
In a multivariate analysis, adjusting for age, gender, and mood stabilizer use after ECT, relapse was approximately four times more likely among individuals with BPD, compared with those without (hazard ratio, 4.14). No significant association appeared between increased relapse and other comorbid personality disorders, anxiety disorders, alcohol or substance use disorders, or hospitalization during the ECT treatment period.
Potential reasons for the increased relapse risk among individuals with MDD and BPD include the younger age of the individuals with BPD, which has been shown to increase MDD relapse risk; the direct negative impact of BPD on mental functioning; and the documented tendency to poor treatment adherence, the researchers wrote in their discussion.
“Given these different elements, it seems important to screen more systematically for BPD in major depressed individuals treated with ECT in order to allow the implementation of more effective prevention strategies for relapse within 6 months in this particular subpopulation,” they emphasized.
“The demonstration of this higher risk of relapse within 6 months associated with BPD in major depressed individuals treated with ECT could open new therapeutic perspectives to allow better maintenance of euthymia in this particular subpopulation,” they added.
The study findings were limited by several factors including the retrospective design and the focus on only BPD, which may not generalize to other personality disorders, the researchers noted.
However, the results support data from previous studies and highlight the need for more systematic BPD screening in MDD patients to prevent relapse after ECT, they said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRY RESEARCH
From neuroplasticity to psychoplasticity: Psilocybin may reverse personality disorders and political fanaticism
One of psychiatry’s long-standing dogmas is that personality disorders are enduring, unchangeable, and not amenable to treatment with potent psychotropics or intensive psychotherapy. I propose that this dogma may soon be shattered.
Several other dogmas in psychiatry have been demolished over the past several decades:
- that “insanity” is completely irreversible and requires lifetime institutionalization. The serendipitous discovery of chlorpromazine1 annihilated this centuries-old dogma
- that chronic, severe, refractory depression (with ongoing suicidal urges) that fails to improve with pharmacotherapy or electroconvulsive therapy (ECT) is hopeless and untreatable, until ketamine not only pulverized this dogma, but did it with lightning speed, dazzling us all2
- that dissociative agents such as ketamine are dangerous and condemnable drugs of abuse, until the therapeutic effect of ketamine slayed that dragon3
- that ECT “fries” the brain (as malevolently propagated by antipsychiatry cults), which was completely disproven by neuroimaging studies that show the hippocampus (which shrinks during depression) actually grows by >10% after a few ECT sessions4
- that psychotherapy is not a “real” treatment because talking cannot reverse a psychiatric brain disorder, until studies showed significant neuroplasticity with psychotherapy and decrease in inflammatory biomarkers with cognitive-behavioral therapy (CBT)5
- that persons with refractory hallucinations and delusions are doomed to a life of disability, until clozapine torpedoed that pessimistic dogma6
- that hallucinogens/psychedelics are dangerous and should be banned, until a jarring paradigm shift occurred with the discovery of psilocybin’s transformative effects, and the remarkable therapeutic effects of its mystical trips.7
Psilocybin’s therapeutic effects
Psilocybin has already proved to have a strong and lasting effect on depression and promises to have therapeutic benefits for patients with substance use disorders, posttraumatic stress disorder (PTSD), and anxiety.8 In addition, when the multiple psychological and neurobiological effects of psilocybin (and of other psychedelics) are examined, I see a very promising path to amelioration of severe personality disorders such as psychopathy, antisocial behavior, and narcissism. The mechanism(s) of action of psilocybin on the human brain are drastically different from any man-made psychotropic agent. As a psychiatric neuroscientist, I envision the neurologic impact of psilocybin to be conducive to a complete transformation of a patient’s view of themself, other people, and the meaning of life. It is reminiscent of religious conversion.
The psychological effects of psilocybin in humans have been described as follows:
- emotional breakthrough9
- increased psychological flexibility,10,11 a very cortical effect
- mystical experience,12 which results in sudden and significant changes in behavior and perception and includes the following dimensions: sacredness, noetic quality, deeply felt positive mood, ineffability, paradoxicality, and transcendence of time and space13
- oceanic boundlessness, feeling “one with the universe”14
- universal interconnectedness, insightfulness, blissful state, spiritual experience14
- ego dissolution,15 with loss of one’s personal identity
- increased neuroplasticity16
- changes in cognition and increase in insight.17
The neurobiological effects of psilocybin are mediated by serotonin 5HT2A agonism and include the following18:
- reduction in the activity of the medial prefrontal cortex, which regulates memory, attention, inhibitory control, and habit
- a decrease in the connectivity between the medial prefrontal cortex and the posterior cingulate cortex, which regulates memory and emotions
- reducing the default mode network, which is active during rest, stimulating internal thoughts and reminiscing about previous feelings and events, sometimes including ruminations. Psilocybin reverses those processes to thinking about others, not just the self, and becoming more open-minded about the world and other people. This can be therapeutic for depression, which is often associated with negative ruminations but also with entrenched habits (addictive behaviors), anxiety, PTSD, and obsessive-compulsive disorders
- increased global functional connectivity among various brain networks, leading to stronger functional integration of behavior
- collapse of major cortical oscillatory rhythms such as alpha and others that perpetuate “prior” beliefs
- extensive neuroplasticity and recalibration of thought processes and decomposition of pathological beliefs, referred to as REBUS (relaxed beliefs under psychedelics).
The bottom line is psilocybin and other psychedelics can dramatically alter, reshape, and relax rigid beliefs and personality traits by decreasing “neuroticism” and increasing “extraversion,” insightfulness, openness, and possibly conscientiousness.19 Although no studies of psychedelics in psychopathic, antisocial, or narcissistic personality disorders have been conducted, it is very reasonable to speculate that psilocybin may reverse traits of these disorders such as callousness, lack of empathy, and pathological self-centeredness.
Going further, a preliminary report suggests psilocybin can modify political views by decreasing authoritarianism and increasing libertarianism.20,21 In the current political zeitgeist, could psychedelics such as psilocybin reduce or even eliminate political extremism and visceral hatred on all sides? It would be remarkable research to carry out to heal a politically divided populace.The dogma of untreatable personality disorders or hopelessly entrenched political extremism is on the chopping block, and psychedelics offer hope to splinter those beliefs by concurrently remodeling brain tissue (neuroplasticity) and rectifying the mindset (psychoplasticity).
1. Delay J, Deniker P. Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry. J Clin Exp Psychopathol. 1955;16(2):104-112.
2. Walsh Z, Mollaahmetoglu OM, Rootman, J, et al. Ketamine for the treatment of mental health and substance use disorders: comprehensive systematic review. BJPsych Open. 2021;8(1):e19. doi:10.1192/bjo.2021.1061
3. Lener MS, Kadriu B, Zarate CA Jr. Ketamine and beyond: investigations into the potential of glutamatergic agents to treat depression. Drugs. 2017;77(4):381-401.
4. Ayers B, Leaver A, Woods RP, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry. 2016;79(4):282-292.
5. Cao B, Li R, Ding L, Xu J, et al. Does cognitive behaviour therapy affect peripheral inflammation of depression? A protocol for the systematic review and meta-analysis. BMJ Open. 2021;11(12):e048162. doi:10.1136/bmjopen-2020-048162
6. Wagner E, Siafis S, Fernando P, et al. Efficacy and safety of clozapine in psychotic disorders—a systematic quantitative meta-review. Transl Psychiatry. 2021;11(1):487.
7. Daws RE, Timmermann C, Giribaldi B, et al. Increased global integration in the brain after psilocybin therapy for depression. Nat Med. 2022;28(4):844-851.
8. Pearson C, Siegel J, Gold JA. Psilocybin-assisted psychotherapy for depression: emerging research on a psychedelic compound with a rich history. J Neurol Sci. 2022;434:120096. doi:10.1016/j.jns.2021.120096
9. Roseman L, Haijen E, Idialu-Ikato K, et al. Emotional breakthrough and psychedelics: validation of the Emotional Breakthrough Inventory. J Psychopharmacol. 2019;33(9):1076-1087.
10. Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J Contextual Behav Sci. 2020;15:39-45.
11. Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1-25.
12. Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165-1180.
13. Stace WT. Mysticism and Philosophy. Macmillan Pub Ltd; 1960:37.
14. Barrett FS, Griffiths RR. Classic hallucinogens and mystical experiences: phenomenology and neural correlates. Curr Top Behav Neurosci. 2018;36:393-430.
15. Nour MM, Evans L, Nutt D, et al. Ego-dissolution and psychedelics: validation of the Ego-Dissolution Inventory (EDI). Front Hum Neurosci. 2016;10:269. doi:10.3389/fnhum.2016.00269
16. Olson DE. The subjective effects of psychedelics may not be necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. 2020;4(2):563-567.
17. Carhart-Harris RL, Bolstridge M, Day CMJ, et al. Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology (Berl). 2018;235(2):399-408.
18. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
19. Erritzoe D, Roseman L, Nour MM, et al. Effects of psilocybin therapy on personality structure. Acta Psychiatr Scand. 2018;138(5):368-378.
20. Lyons T, Carhart-Harris RL. Increased nature relatedness and decreased authoritarian political views after psilocybin for treatment-resistant depression. J Psychopharmacol. 2018;32(7):811-819.
21. Nour MM, Evans L, Carhart-Harris RL. Psychedelics, personality and political perspectives. J Psychoactive Drugs. 2017;49(3):182-191.
One of psychiatry’s long-standing dogmas is that personality disorders are enduring, unchangeable, and not amenable to treatment with potent psychotropics or intensive psychotherapy. I propose that this dogma may soon be shattered.
Several other dogmas in psychiatry have been demolished over the past several decades:
- that “insanity” is completely irreversible and requires lifetime institutionalization. The serendipitous discovery of chlorpromazine1 annihilated this centuries-old dogma
- that chronic, severe, refractory depression (with ongoing suicidal urges) that fails to improve with pharmacotherapy or electroconvulsive therapy (ECT) is hopeless and untreatable, until ketamine not only pulverized this dogma, but did it with lightning speed, dazzling us all2
- that dissociative agents such as ketamine are dangerous and condemnable drugs of abuse, until the therapeutic effect of ketamine slayed that dragon3
- that ECT “fries” the brain (as malevolently propagated by antipsychiatry cults), which was completely disproven by neuroimaging studies that show the hippocampus (which shrinks during depression) actually grows by >10% after a few ECT sessions4
- that psychotherapy is not a “real” treatment because talking cannot reverse a psychiatric brain disorder, until studies showed significant neuroplasticity with psychotherapy and decrease in inflammatory biomarkers with cognitive-behavioral therapy (CBT)5
- that persons with refractory hallucinations and delusions are doomed to a life of disability, until clozapine torpedoed that pessimistic dogma6
- that hallucinogens/psychedelics are dangerous and should be banned, until a jarring paradigm shift occurred with the discovery of psilocybin’s transformative effects, and the remarkable therapeutic effects of its mystical trips.7
Psilocybin’s therapeutic effects
Psilocybin has already proved to have a strong and lasting effect on depression and promises to have therapeutic benefits for patients with substance use disorders, posttraumatic stress disorder (PTSD), and anxiety.8 In addition, when the multiple psychological and neurobiological effects of psilocybin (and of other psychedelics) are examined, I see a very promising path to amelioration of severe personality disorders such as psychopathy, antisocial behavior, and narcissism. The mechanism(s) of action of psilocybin on the human brain are drastically different from any man-made psychotropic agent. As a psychiatric neuroscientist, I envision the neurologic impact of psilocybin to be conducive to a complete transformation of a patient’s view of themself, other people, and the meaning of life. It is reminiscent of religious conversion.
The psychological effects of psilocybin in humans have been described as follows:
- emotional breakthrough9
- increased psychological flexibility,10,11 a very cortical effect
- mystical experience,12 which results in sudden and significant changes in behavior and perception and includes the following dimensions: sacredness, noetic quality, deeply felt positive mood, ineffability, paradoxicality, and transcendence of time and space13
- oceanic boundlessness, feeling “one with the universe”14
- universal interconnectedness, insightfulness, blissful state, spiritual experience14
- ego dissolution,15 with loss of one’s personal identity
- increased neuroplasticity16
- changes in cognition and increase in insight.17
The neurobiological effects of psilocybin are mediated by serotonin 5HT2A agonism and include the following18:
- reduction in the activity of the medial prefrontal cortex, which regulates memory, attention, inhibitory control, and habit
- a decrease in the connectivity between the medial prefrontal cortex and the posterior cingulate cortex, which regulates memory and emotions
- reducing the default mode network, which is active during rest, stimulating internal thoughts and reminiscing about previous feelings and events, sometimes including ruminations. Psilocybin reverses those processes to thinking about others, not just the self, and becoming more open-minded about the world and other people. This can be therapeutic for depression, which is often associated with negative ruminations but also with entrenched habits (addictive behaviors), anxiety, PTSD, and obsessive-compulsive disorders
- increased global functional connectivity among various brain networks, leading to stronger functional integration of behavior
- collapse of major cortical oscillatory rhythms such as alpha and others that perpetuate “prior” beliefs
- extensive neuroplasticity and recalibration of thought processes and decomposition of pathological beliefs, referred to as REBUS (relaxed beliefs under psychedelics).
The bottom line is psilocybin and other psychedelics can dramatically alter, reshape, and relax rigid beliefs and personality traits by decreasing “neuroticism” and increasing “extraversion,” insightfulness, openness, and possibly conscientiousness.19 Although no studies of psychedelics in psychopathic, antisocial, or narcissistic personality disorders have been conducted, it is very reasonable to speculate that psilocybin may reverse traits of these disorders such as callousness, lack of empathy, and pathological self-centeredness.
Going further, a preliminary report suggests psilocybin can modify political views by decreasing authoritarianism and increasing libertarianism.20,21 In the current political zeitgeist, could psychedelics such as psilocybin reduce or even eliminate political extremism and visceral hatred on all sides? It would be remarkable research to carry out to heal a politically divided populace.The dogma of untreatable personality disorders or hopelessly entrenched political extremism is on the chopping block, and psychedelics offer hope to splinter those beliefs by concurrently remodeling brain tissue (neuroplasticity) and rectifying the mindset (psychoplasticity).
One of psychiatry’s long-standing dogmas is that personality disorders are enduring, unchangeable, and not amenable to treatment with potent psychotropics or intensive psychotherapy. I propose that this dogma may soon be shattered.
Several other dogmas in psychiatry have been demolished over the past several decades:
- that “insanity” is completely irreversible and requires lifetime institutionalization. The serendipitous discovery of chlorpromazine1 annihilated this centuries-old dogma
- that chronic, severe, refractory depression (with ongoing suicidal urges) that fails to improve with pharmacotherapy or electroconvulsive therapy (ECT) is hopeless and untreatable, until ketamine not only pulverized this dogma, but did it with lightning speed, dazzling us all2
- that dissociative agents such as ketamine are dangerous and condemnable drugs of abuse, until the therapeutic effect of ketamine slayed that dragon3
- that ECT “fries” the brain (as malevolently propagated by antipsychiatry cults), which was completely disproven by neuroimaging studies that show the hippocampus (which shrinks during depression) actually grows by >10% after a few ECT sessions4
- that psychotherapy is not a “real” treatment because talking cannot reverse a psychiatric brain disorder, until studies showed significant neuroplasticity with psychotherapy and decrease in inflammatory biomarkers with cognitive-behavioral therapy (CBT)5
- that persons with refractory hallucinations and delusions are doomed to a life of disability, until clozapine torpedoed that pessimistic dogma6
- that hallucinogens/psychedelics are dangerous and should be banned, until a jarring paradigm shift occurred with the discovery of psilocybin’s transformative effects, and the remarkable therapeutic effects of its mystical trips.7
Psilocybin’s therapeutic effects
Psilocybin has already proved to have a strong and lasting effect on depression and promises to have therapeutic benefits for patients with substance use disorders, posttraumatic stress disorder (PTSD), and anxiety.8 In addition, when the multiple psychological and neurobiological effects of psilocybin (and of other psychedelics) are examined, I see a very promising path to amelioration of severe personality disorders such as psychopathy, antisocial behavior, and narcissism. The mechanism(s) of action of psilocybin on the human brain are drastically different from any man-made psychotropic agent. As a psychiatric neuroscientist, I envision the neurologic impact of psilocybin to be conducive to a complete transformation of a patient’s view of themself, other people, and the meaning of life. It is reminiscent of religious conversion.
The psychological effects of psilocybin in humans have been described as follows:
- emotional breakthrough9
- increased psychological flexibility,10,11 a very cortical effect
- mystical experience,12 which results in sudden and significant changes in behavior and perception and includes the following dimensions: sacredness, noetic quality, deeply felt positive mood, ineffability, paradoxicality, and transcendence of time and space13
- oceanic boundlessness, feeling “one with the universe”14
- universal interconnectedness, insightfulness, blissful state, spiritual experience14
- ego dissolution,15 with loss of one’s personal identity
- increased neuroplasticity16
- changes in cognition and increase in insight.17
The neurobiological effects of psilocybin are mediated by serotonin 5HT2A agonism and include the following18:
- reduction in the activity of the medial prefrontal cortex, which regulates memory, attention, inhibitory control, and habit
- a decrease in the connectivity between the medial prefrontal cortex and the posterior cingulate cortex, which regulates memory and emotions
- reducing the default mode network, which is active during rest, stimulating internal thoughts and reminiscing about previous feelings and events, sometimes including ruminations. Psilocybin reverses those processes to thinking about others, not just the self, and becoming more open-minded about the world and other people. This can be therapeutic for depression, which is often associated with negative ruminations but also with entrenched habits (addictive behaviors), anxiety, PTSD, and obsessive-compulsive disorders
- increased global functional connectivity among various brain networks, leading to stronger functional integration of behavior
- collapse of major cortical oscillatory rhythms such as alpha and others that perpetuate “prior” beliefs
- extensive neuroplasticity and recalibration of thought processes and decomposition of pathological beliefs, referred to as REBUS (relaxed beliefs under psychedelics).
The bottom line is psilocybin and other psychedelics can dramatically alter, reshape, and relax rigid beliefs and personality traits by decreasing “neuroticism” and increasing “extraversion,” insightfulness, openness, and possibly conscientiousness.19 Although no studies of psychedelics in psychopathic, antisocial, or narcissistic personality disorders have been conducted, it is very reasonable to speculate that psilocybin may reverse traits of these disorders such as callousness, lack of empathy, and pathological self-centeredness.
Going further, a preliminary report suggests psilocybin can modify political views by decreasing authoritarianism and increasing libertarianism.20,21 In the current political zeitgeist, could psychedelics such as psilocybin reduce or even eliminate political extremism and visceral hatred on all sides? It would be remarkable research to carry out to heal a politically divided populace.The dogma of untreatable personality disorders or hopelessly entrenched political extremism is on the chopping block, and psychedelics offer hope to splinter those beliefs by concurrently remodeling brain tissue (neuroplasticity) and rectifying the mindset (psychoplasticity).
1. Delay J, Deniker P. Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry. J Clin Exp Psychopathol. 1955;16(2):104-112.
2. Walsh Z, Mollaahmetoglu OM, Rootman, J, et al. Ketamine for the treatment of mental health and substance use disorders: comprehensive systematic review. BJPsych Open. 2021;8(1):e19. doi:10.1192/bjo.2021.1061
3. Lener MS, Kadriu B, Zarate CA Jr. Ketamine and beyond: investigations into the potential of glutamatergic agents to treat depression. Drugs. 2017;77(4):381-401.
4. Ayers B, Leaver A, Woods RP, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry. 2016;79(4):282-292.
5. Cao B, Li R, Ding L, Xu J, et al. Does cognitive behaviour therapy affect peripheral inflammation of depression? A protocol for the systematic review and meta-analysis. BMJ Open. 2021;11(12):e048162. doi:10.1136/bmjopen-2020-048162
6. Wagner E, Siafis S, Fernando P, et al. Efficacy and safety of clozapine in psychotic disorders—a systematic quantitative meta-review. Transl Psychiatry. 2021;11(1):487.
7. Daws RE, Timmermann C, Giribaldi B, et al. Increased global integration in the brain after psilocybin therapy for depression. Nat Med. 2022;28(4):844-851.
8. Pearson C, Siegel J, Gold JA. Psilocybin-assisted psychotherapy for depression: emerging research on a psychedelic compound with a rich history. J Neurol Sci. 2022;434:120096. doi:10.1016/j.jns.2021.120096
9. Roseman L, Haijen E, Idialu-Ikato K, et al. Emotional breakthrough and psychedelics: validation of the Emotional Breakthrough Inventory. J Psychopharmacol. 2019;33(9):1076-1087.
10. Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J Contextual Behav Sci. 2020;15:39-45.
11. Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1-25.
12. Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165-1180.
13. Stace WT. Mysticism and Philosophy. Macmillan Pub Ltd; 1960:37.
14. Barrett FS, Griffiths RR. Classic hallucinogens and mystical experiences: phenomenology and neural correlates. Curr Top Behav Neurosci. 2018;36:393-430.
15. Nour MM, Evans L, Nutt D, et al. Ego-dissolution and psychedelics: validation of the Ego-Dissolution Inventory (EDI). Front Hum Neurosci. 2016;10:269. doi:10.3389/fnhum.2016.00269
16. Olson DE. The subjective effects of psychedelics may not be necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. 2020;4(2):563-567.
17. Carhart-Harris RL, Bolstridge M, Day CMJ, et al. Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology (Berl). 2018;235(2):399-408.
18. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
19. Erritzoe D, Roseman L, Nour MM, et al. Effects of psilocybin therapy on personality structure. Acta Psychiatr Scand. 2018;138(5):368-378.
20. Lyons T, Carhart-Harris RL. Increased nature relatedness and decreased authoritarian political views after psilocybin for treatment-resistant depression. J Psychopharmacol. 2018;32(7):811-819.
21. Nour MM, Evans L, Carhart-Harris RL. Psychedelics, personality and political perspectives. J Psychoactive Drugs. 2017;49(3):182-191.
1. Delay J, Deniker P. Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry. J Clin Exp Psychopathol. 1955;16(2):104-112.
2. Walsh Z, Mollaahmetoglu OM, Rootman, J, et al. Ketamine for the treatment of mental health and substance use disorders: comprehensive systematic review. BJPsych Open. 2021;8(1):e19. doi:10.1192/bjo.2021.1061
3. Lener MS, Kadriu B, Zarate CA Jr. Ketamine and beyond: investigations into the potential of glutamatergic agents to treat depression. Drugs. 2017;77(4):381-401.
4. Ayers B, Leaver A, Woods RP, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry. 2016;79(4):282-292.
5. Cao B, Li R, Ding L, Xu J, et al. Does cognitive behaviour therapy affect peripheral inflammation of depression? A protocol for the systematic review and meta-analysis. BMJ Open. 2021;11(12):e048162. doi:10.1136/bmjopen-2020-048162
6. Wagner E, Siafis S, Fernando P, et al. Efficacy and safety of clozapine in psychotic disorders—a systematic quantitative meta-review. Transl Psychiatry. 2021;11(1):487.
7. Daws RE, Timmermann C, Giribaldi B, et al. Increased global integration in the brain after psilocybin therapy for depression. Nat Med. 2022;28(4):844-851.
8. Pearson C, Siegel J, Gold JA. Psilocybin-assisted psychotherapy for depression: emerging research on a psychedelic compound with a rich history. J Neurol Sci. 2022;434:120096. doi:10.1016/j.jns.2021.120096
9. Roseman L, Haijen E, Idialu-Ikato K, et al. Emotional breakthrough and psychedelics: validation of the Emotional Breakthrough Inventory. J Psychopharmacol. 2019;33(9):1076-1087.
10. Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J Contextual Behav Sci. 2020;15:39-45.
11. Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1-25.
12. Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165-1180.
13. Stace WT. Mysticism and Philosophy. Macmillan Pub Ltd; 1960:37.
14. Barrett FS, Griffiths RR. Classic hallucinogens and mystical experiences: phenomenology and neural correlates. Curr Top Behav Neurosci. 2018;36:393-430.
15. Nour MM, Evans L, Nutt D, et al. Ego-dissolution and psychedelics: validation of the Ego-Dissolution Inventory (EDI). Front Hum Neurosci. 2016;10:269. doi:10.3389/fnhum.2016.00269
16. Olson DE. The subjective effects of psychedelics may not be necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. 2020;4(2):563-567.
17. Carhart-Harris RL, Bolstridge M, Day CMJ, et al. Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology (Berl). 2018;235(2):399-408.
18. Carhart-Harris RL. How do psychedelics work? Curr Opin Psychiatry. 2019;32(1):16-21.
19. Erritzoe D, Roseman L, Nour MM, et al. Effects of psilocybin therapy on personality structure. Acta Psychiatr Scand. 2018;138(5):368-378.
20. Lyons T, Carhart-Harris RL. Increased nature relatedness and decreased authoritarian political views after psilocybin for treatment-resistant depression. J Psychopharmacol. 2018;32(7):811-819.
21. Nour MM, Evans L, Carhart-Harris RL. Psychedelics, personality and political perspectives. J Psychoactive Drugs. 2017;49(3):182-191.
Brief Psychiatric Rating Scale succeeds as transdiagnostic measure
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
“Current DSM and ICD diagnoses do not depict psychopathology accurately, therefore their validity in research and utility in clinical practice is questioned,” wrote Andreas B. Hofmann, PhD, of the University of Zürich and colleagues.
The BPRS was developed to assess changes in psychopathology across a range of severe psychiatric disorders, but its potential to assess symptoms in nonpsychotic disorders has not been explored, the researchers said.
In a study published in Psychiatry Research, the investigators analyzed data from 600 adult psychiatric inpatients divided equally into six diagnostic categories: alcohol use disorder, major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and personality disorders. The mean age of the patients was 41.5 years and 45.5% were women. The demographic characteristics were similar across most groups, although patients with a personality disorder were significantly more likely than other patients to be younger and female.
Patients were assessed using the BPRS based on their main diagnosis. The mini-ICF-APP, another validated measure for assessing psychiatric disorders, served as a comparator, and both were compared to the Clinical Global Impression Scale (CGI).
Overall, the BPRS and mini-ICF-APP showed moderate correlation and good agreement, the researchers said. The Pearson correlation coefficient for the BPRS and mini-ICF-APP scales was 0.53 and the concordance correlation coefficient was 0.52. The mean sum scores for the BPRS, the mini-ICF-APP, and the CGI were 45.4 (standard deviation, 14.4), 19.93 (SD, 8.21), and 5.55 (SD, 0.84), respectively, which indicated “markedly ill” to “severely ill” patients, the researchers said.
The researchers were able to detect three clusters of symptoms corresponding to externalizing, internalizing, and thought disturbance domains using the BPRS, and four clusters using the mini-ICF-APP.
The symptoms using BPRS and the functionality domains using the mini-ICF-APP “showed a close interplay,” the researchers noted.
“The symptoms and functional domains we found to be central within the network structure are among the first targets of any psychiatric or psychotherapeutic intervention, namely the building of a common language and understanding as well as the establishment of confidence in relationships and a trustworthy therapeutic alliance,” they wrote in their discussion.
The study findings were limited by several factors including the collection of data from routine practice rather than clinical trials, the focus on only the main diagnosis without comorbidities, and the inclusion only of patients requiring hospitalization, the researchers noted.
However, the results were strengthened by the large sample size, and demonstrate the validity of the BPRS as a measurement tool across a range of psychiatric diagnoses, they said.
“Since the BPRS is a widely known and readily available psychometric scale, our results support its use as a transdiagnostic measurement instrument of psychopathology,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRY RESEARCH
New panic disorder model flags risk for recurrence, persistence
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.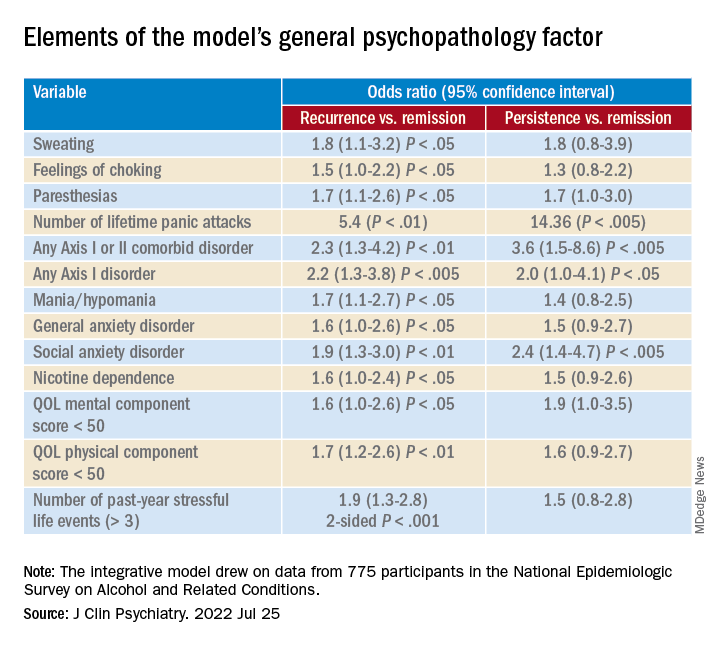
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.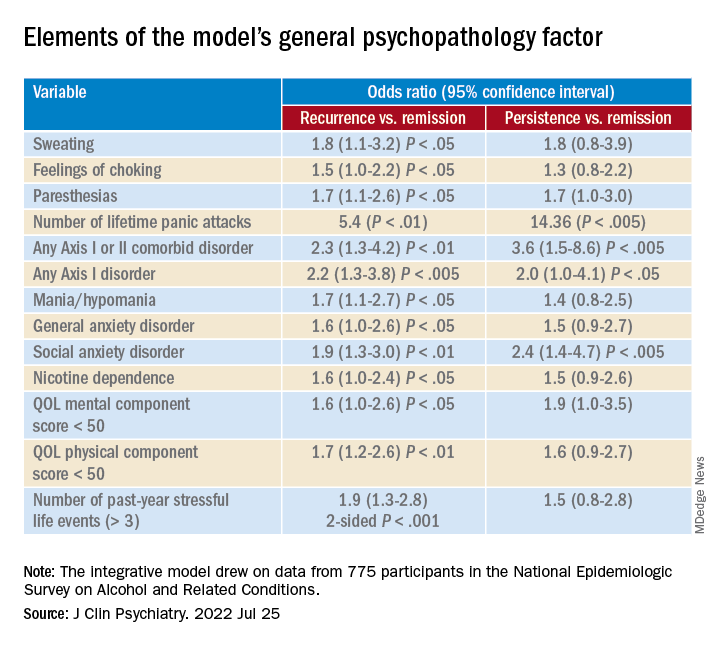
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.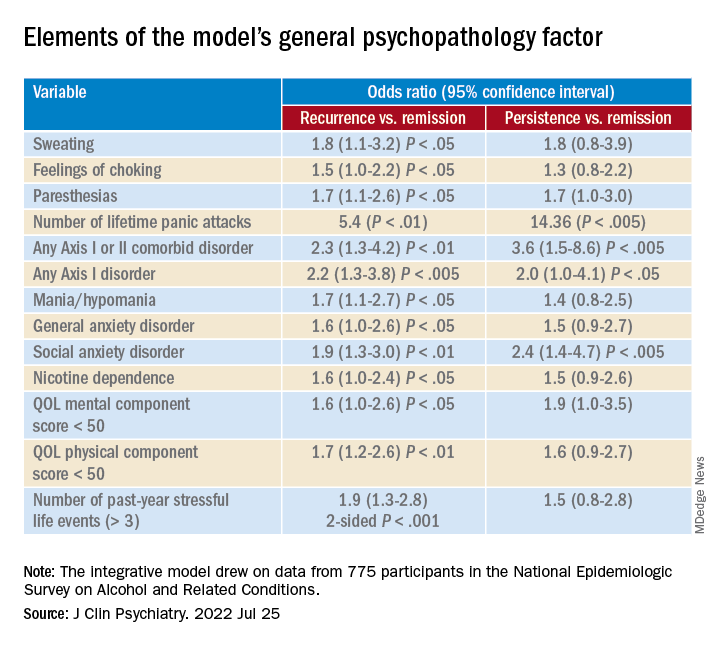
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Diagnostic criterion may hide borderline personality disorder
Investigators compared characteristics of almost 400 psychiatric outpatients diagnosed with BPD. About half of the participants met the suicidality/self-injury diagnostic criterion for the disorder, while the other half did not.
Results showed no differences between the two groups in degree of impairment in occupational or social functioning, comorbid psychiatric disorders, history of childhood trauma, or severity of depression, anxiety, or anger.
“Just because a person doesn’t engage in self-harm or suicidal behavior doesn’t mean that the person is free of borderline personality disorder,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Clinicians need to screen for borderline personality disorder in patients with other suggestive symptoms, even if those patients don’t self-harm, just as they would for similar patients who do self-harm,” said Dr. Zimmerman, who is also the director of the Outpatient Division at the Partial Hospital Program, Rhode Island Hospital.
The findings were published online in Psychological Medicine.
A ‘polythetic diagnosis’
Dr. Zimmerman noted the impetus for conducting the study originated with a patient he saw who had all of the features of BPD except for self-harm and suicidality. However, because she didn’t have those two features, she was told by her therapist she could not have BPD.
“This sparked the idea that perhaps there are other individuals whose BPD may not be recognized because they don’t engage in self-harm or suicidal behavior,” Dr. Zimmerman said.
“Most individuals with BPD don’t present for treatment saying, ‘I’m here because I don’t have a sense of myself’ or ‘I feel empty inside’ – but they do say, ‘I’m here because I’m cutting myself’ or ‘I’m suicidal,’ ” he added.
The investigators wondered if there were other “hidden” cases of BPD that were being missed by therapists.
They had previously analyzed each diagnostic criterion for BPD to ascertain its sensitivity. “We had been interested in wanting to see whether there was a criterion so frequent in BPD that every patient with BPD has it,” Dr. Zimmerman said.
BPD is a “polythetic diagnosis,” he added. It is “based on a list of features, with a certain minimum number of those features necessary to make the diagnosis rather than one specific criterion.”
His group’s previous research showed affective instability criterion to be present in more than 90% of individuals with BPD. “It had a very high negative predictive value, meaning that if you didn’t have affective instability, you didn’t have the disorder,” he said.
“Given the clinical and public health significance of suicidal and self-harm behavior in patients with BPD, an important question is whether the absence of this criterion, which might attenuate the likelihood of recognizing and diagnosing the disorder, identifies a subgroup of patients with BPD who are ‘less borderline’ than patients with BPD who do not manifest this criterion,” the investigators write.
The researchers wanted to see if a similar finding applied to self-injury and suicidal behavior and turned to the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project to compare the demographic and clinical characteristics of patients with BPD who do and do not engage in repeated suicidal and self-harm behavior.
MIDAS project
The study population was derived from 3,800 psychiatric outpatients who had been evaluated in the MIDAS project with semi-structured diagnostic interviews.
Of these, 390 patients were diagnosed with BPD. Since the suicidality/self-harm item was not rated in one patient, the analyzed sample consisted of 389 individuals with BPD (28.3% male; mean age, 32.6 years; 86.3% White). A little more than half the participants (54%) met the BPD suicidality/ self-harm criterion.
Only one-fifth (20.5%) of patients with BPD presented with a chief complaint that was related to a feature of BPD and had received BPD as their principal diagnosis.
Patients who met the suicidality/self-injury criterion were almost twice as likely to be diagnosed with BPD as the principal diagnosis, compared with those who did not have that criterion (24.8% vs. 14.5%, respectively; P < .01).
On the other hand, there was no difference in the mean number of BPD criteria that were met, other than suicidality/self-harm, between those who did and did not present with suicidality/self-harm (5.5 ± 1.2 vs. 5.7 ± 0.8, t = 1.44). The investigators note that this finding was “not significant.”
There also was no difference between patients who did and did not meet the criterion in number of psychiatric diagnoses at time of evaluation (3.4 ± 1.9 vs. 3.5 ± 1.8, t = 0.56).
Hidden BPD
Similarly, there was no difference in any specific Axis I or personality disorder – except for generalized anxiety disorder (GAD) and histrionic personality disorder. Both were more frequent in the patients who did not meet the suicidality/self-injury criterion. However, after controlling for age, the group difference in GAD was no longer deemed significant (F = 3.45, P = .064).
By contrast, histrionic personality disorder remained significant with age as the covariate (F = 6.03, P = .015).
“The patients who met the suicidality/self-injury criterion were significantly more likely to have been hospitalized and reported more suicidal ideation at the time of the evaluation,” the researchers write. Both variables remained significant even after including age as a covariate.
There were no between-group differences on severity of depression, anxiety, or anger at initial evaluation nor were there differences in social functioning, adolescent social functioning, likelihood of persistent unemployment or receiving disability payments, childhood trauma, or neglect.
“I suspect that there are a number of individuals whose BPD is not recognized because they don’t have the more overt feature of self-injury or suicidal behavior,” said Dr. Zimmerman, noting that these patients might be considered as having “hidden” BPD.
“Repeated self-injurious and suicidal behavior is not synonymous with BPD, and clinicians should be aware that the absence of these behaviors does not rule out a diagnosis of BPD,” he added.
Stigmatizing diagnosis?
Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and senior fellow, Personality Disorders Institute, Weill Cornell Medical College, New York, said the study “will be particularly useful in the education of clinicians about the characteristics of individuals with BPD.”
Dr. Carsky, who is also an adjunct assistant professor in the NYU Postdoctoral Program in Psychoanalysis and Psychotherapy, was not involved with the study. She noted that other factors “can contribute to misdiagnosis of the borderline patients who do not have suicidality/self-harm.”
Clinicians and patients “may see BPD as a stigmatizing diagnosis so that clinicians become reluctant to make, share, and explain this personality disorder diagnosis,” she said.
Dr. Carsky suggested that increasing use of the Alternate Model for Personality Disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), which first rates the severity level of personality by assessing identity and relationship problems and then notes traits of specific personality disorders, “will help clinicians who dread telling patients they are ‘borderline.’ ”
No source of study funding has been reported. The investigators and Dr. Carsky reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared characteristics of almost 400 psychiatric outpatients diagnosed with BPD. About half of the participants met the suicidality/self-injury diagnostic criterion for the disorder, while the other half did not.
Results showed no differences between the two groups in degree of impairment in occupational or social functioning, comorbid psychiatric disorders, history of childhood trauma, or severity of depression, anxiety, or anger.
“Just because a person doesn’t engage in self-harm or suicidal behavior doesn’t mean that the person is free of borderline personality disorder,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Clinicians need to screen for borderline personality disorder in patients with other suggestive symptoms, even if those patients don’t self-harm, just as they would for similar patients who do self-harm,” said Dr. Zimmerman, who is also the director of the Outpatient Division at the Partial Hospital Program, Rhode Island Hospital.
The findings were published online in Psychological Medicine.
A ‘polythetic diagnosis’
Dr. Zimmerman noted the impetus for conducting the study originated with a patient he saw who had all of the features of BPD except for self-harm and suicidality. However, because she didn’t have those two features, she was told by her therapist she could not have BPD.
“This sparked the idea that perhaps there are other individuals whose BPD may not be recognized because they don’t engage in self-harm or suicidal behavior,” Dr. Zimmerman said.
“Most individuals with BPD don’t present for treatment saying, ‘I’m here because I don’t have a sense of myself’ or ‘I feel empty inside’ – but they do say, ‘I’m here because I’m cutting myself’ or ‘I’m suicidal,’ ” he added.
The investigators wondered if there were other “hidden” cases of BPD that were being missed by therapists.
They had previously analyzed each diagnostic criterion for BPD to ascertain its sensitivity. “We had been interested in wanting to see whether there was a criterion so frequent in BPD that every patient with BPD has it,” Dr. Zimmerman said.
BPD is a “polythetic diagnosis,” he added. It is “based on a list of features, with a certain minimum number of those features necessary to make the diagnosis rather than one specific criterion.”
His group’s previous research showed affective instability criterion to be present in more than 90% of individuals with BPD. “It had a very high negative predictive value, meaning that if you didn’t have affective instability, you didn’t have the disorder,” he said.
“Given the clinical and public health significance of suicidal and self-harm behavior in patients with BPD, an important question is whether the absence of this criterion, which might attenuate the likelihood of recognizing and diagnosing the disorder, identifies a subgroup of patients with BPD who are ‘less borderline’ than patients with BPD who do not manifest this criterion,” the investigators write.
The researchers wanted to see if a similar finding applied to self-injury and suicidal behavior and turned to the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project to compare the demographic and clinical characteristics of patients with BPD who do and do not engage in repeated suicidal and self-harm behavior.
MIDAS project
The study population was derived from 3,800 psychiatric outpatients who had been evaluated in the MIDAS project with semi-structured diagnostic interviews.
Of these, 390 patients were diagnosed with BPD. Since the suicidality/self-harm item was not rated in one patient, the analyzed sample consisted of 389 individuals with BPD (28.3% male; mean age, 32.6 years; 86.3% White). A little more than half the participants (54%) met the BPD suicidality/ self-harm criterion.
Only one-fifth (20.5%) of patients with BPD presented with a chief complaint that was related to a feature of BPD and had received BPD as their principal diagnosis.
Patients who met the suicidality/self-injury criterion were almost twice as likely to be diagnosed with BPD as the principal diagnosis, compared with those who did not have that criterion (24.8% vs. 14.5%, respectively; P < .01).
On the other hand, there was no difference in the mean number of BPD criteria that were met, other than suicidality/self-harm, between those who did and did not present with suicidality/self-harm (5.5 ± 1.2 vs. 5.7 ± 0.8, t = 1.44). The investigators note that this finding was “not significant.”
There also was no difference between patients who did and did not meet the criterion in number of psychiatric diagnoses at time of evaluation (3.4 ± 1.9 vs. 3.5 ± 1.8, t = 0.56).
Hidden BPD
Similarly, there was no difference in any specific Axis I or personality disorder – except for generalized anxiety disorder (GAD) and histrionic personality disorder. Both were more frequent in the patients who did not meet the suicidality/self-injury criterion. However, after controlling for age, the group difference in GAD was no longer deemed significant (F = 3.45, P = .064).
By contrast, histrionic personality disorder remained significant with age as the covariate (F = 6.03, P = .015).
“The patients who met the suicidality/self-injury criterion were significantly more likely to have been hospitalized and reported more suicidal ideation at the time of the evaluation,” the researchers write. Both variables remained significant even after including age as a covariate.
There were no between-group differences on severity of depression, anxiety, or anger at initial evaluation nor were there differences in social functioning, adolescent social functioning, likelihood of persistent unemployment or receiving disability payments, childhood trauma, or neglect.
“I suspect that there are a number of individuals whose BPD is not recognized because they don’t have the more overt feature of self-injury or suicidal behavior,” said Dr. Zimmerman, noting that these patients might be considered as having “hidden” BPD.
“Repeated self-injurious and suicidal behavior is not synonymous with BPD, and clinicians should be aware that the absence of these behaviors does not rule out a diagnosis of BPD,” he added.
Stigmatizing diagnosis?
Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and senior fellow, Personality Disorders Institute, Weill Cornell Medical College, New York, said the study “will be particularly useful in the education of clinicians about the characteristics of individuals with BPD.”
Dr. Carsky, who is also an adjunct assistant professor in the NYU Postdoctoral Program in Psychoanalysis and Psychotherapy, was not involved with the study. She noted that other factors “can contribute to misdiagnosis of the borderline patients who do not have suicidality/self-harm.”
Clinicians and patients “may see BPD as a stigmatizing diagnosis so that clinicians become reluctant to make, share, and explain this personality disorder diagnosis,” she said.
Dr. Carsky suggested that increasing use of the Alternate Model for Personality Disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), which first rates the severity level of personality by assessing identity and relationship problems and then notes traits of specific personality disorders, “will help clinicians who dread telling patients they are ‘borderline.’ ”
No source of study funding has been reported. The investigators and Dr. Carsky reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared characteristics of almost 400 psychiatric outpatients diagnosed with BPD. About half of the participants met the suicidality/self-injury diagnostic criterion for the disorder, while the other half did not.
Results showed no differences between the two groups in degree of impairment in occupational or social functioning, comorbid psychiatric disorders, history of childhood trauma, or severity of depression, anxiety, or anger.
“Just because a person doesn’t engage in self-harm or suicidal behavior doesn’t mean that the person is free of borderline personality disorder,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Clinicians need to screen for borderline personality disorder in patients with other suggestive symptoms, even if those patients don’t self-harm, just as they would for similar patients who do self-harm,” said Dr. Zimmerman, who is also the director of the Outpatient Division at the Partial Hospital Program, Rhode Island Hospital.
The findings were published online in Psychological Medicine.
A ‘polythetic diagnosis’
Dr. Zimmerman noted the impetus for conducting the study originated with a patient he saw who had all of the features of BPD except for self-harm and suicidality. However, because she didn’t have those two features, she was told by her therapist she could not have BPD.
“This sparked the idea that perhaps there are other individuals whose BPD may not be recognized because they don’t engage in self-harm or suicidal behavior,” Dr. Zimmerman said.
“Most individuals with BPD don’t present for treatment saying, ‘I’m here because I don’t have a sense of myself’ or ‘I feel empty inside’ – but they do say, ‘I’m here because I’m cutting myself’ or ‘I’m suicidal,’ ” he added.
The investigators wondered if there were other “hidden” cases of BPD that were being missed by therapists.
They had previously analyzed each diagnostic criterion for BPD to ascertain its sensitivity. “We had been interested in wanting to see whether there was a criterion so frequent in BPD that every patient with BPD has it,” Dr. Zimmerman said.
BPD is a “polythetic diagnosis,” he added. It is “based on a list of features, with a certain minimum number of those features necessary to make the diagnosis rather than one specific criterion.”
His group’s previous research showed affective instability criterion to be present in more than 90% of individuals with BPD. “It had a very high negative predictive value, meaning that if you didn’t have affective instability, you didn’t have the disorder,” he said.
“Given the clinical and public health significance of suicidal and self-harm behavior in patients with BPD, an important question is whether the absence of this criterion, which might attenuate the likelihood of recognizing and diagnosing the disorder, identifies a subgroup of patients with BPD who are ‘less borderline’ than patients with BPD who do not manifest this criterion,” the investigators write.
The researchers wanted to see if a similar finding applied to self-injury and suicidal behavior and turned to the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project to compare the demographic and clinical characteristics of patients with BPD who do and do not engage in repeated suicidal and self-harm behavior.
MIDAS project
The study population was derived from 3,800 psychiatric outpatients who had been evaluated in the MIDAS project with semi-structured diagnostic interviews.
Of these, 390 patients were diagnosed with BPD. Since the suicidality/self-harm item was not rated in one patient, the analyzed sample consisted of 389 individuals with BPD (28.3% male; mean age, 32.6 years; 86.3% White). A little more than half the participants (54%) met the BPD suicidality/ self-harm criterion.
Only one-fifth (20.5%) of patients with BPD presented with a chief complaint that was related to a feature of BPD and had received BPD as their principal diagnosis.
Patients who met the suicidality/self-injury criterion were almost twice as likely to be diagnosed with BPD as the principal diagnosis, compared with those who did not have that criterion (24.8% vs. 14.5%, respectively; P < .01).
On the other hand, there was no difference in the mean number of BPD criteria that were met, other than suicidality/self-harm, between those who did and did not present with suicidality/self-harm (5.5 ± 1.2 vs. 5.7 ± 0.8, t = 1.44). The investigators note that this finding was “not significant.”
There also was no difference between patients who did and did not meet the criterion in number of psychiatric diagnoses at time of evaluation (3.4 ± 1.9 vs. 3.5 ± 1.8, t = 0.56).
Hidden BPD
Similarly, there was no difference in any specific Axis I or personality disorder – except for generalized anxiety disorder (GAD) and histrionic personality disorder. Both were more frequent in the patients who did not meet the suicidality/self-injury criterion. However, after controlling for age, the group difference in GAD was no longer deemed significant (F = 3.45, P = .064).
By contrast, histrionic personality disorder remained significant with age as the covariate (F = 6.03, P = .015).
“The patients who met the suicidality/self-injury criterion were significantly more likely to have been hospitalized and reported more suicidal ideation at the time of the evaluation,” the researchers write. Both variables remained significant even after including age as a covariate.
There were no between-group differences on severity of depression, anxiety, or anger at initial evaluation nor were there differences in social functioning, adolescent social functioning, likelihood of persistent unemployment or receiving disability payments, childhood trauma, or neglect.
“I suspect that there are a number of individuals whose BPD is not recognized because they don’t have the more overt feature of self-injury or suicidal behavior,” said Dr. Zimmerman, noting that these patients might be considered as having “hidden” BPD.
“Repeated self-injurious and suicidal behavior is not synonymous with BPD, and clinicians should be aware that the absence of these behaviors does not rule out a diagnosis of BPD,” he added.
Stigmatizing diagnosis?
Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and senior fellow, Personality Disorders Institute, Weill Cornell Medical College, New York, said the study “will be particularly useful in the education of clinicians about the characteristics of individuals with BPD.”
Dr. Carsky, who is also an adjunct assistant professor in the NYU Postdoctoral Program in Psychoanalysis and Psychotherapy, was not involved with the study. She noted that other factors “can contribute to misdiagnosis of the borderline patients who do not have suicidality/self-harm.”
Clinicians and patients “may see BPD as a stigmatizing diagnosis so that clinicians become reluctant to make, share, and explain this personality disorder diagnosis,” she said.
Dr. Carsky suggested that increasing use of the Alternate Model for Personality Disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), which first rates the severity level of personality by assessing identity and relationship problems and then notes traits of specific personality disorders, “will help clinicians who dread telling patients they are ‘borderline.’ ”
No source of study funding has been reported. The investigators and Dr. Carsky reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mixed results for intensive home care for psychiatric crises
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intensive home treatment may offer an alternative to inpatient care for patients in acute psychiatric crisis – but the intervention is no outright substitute, new research suggests.
However, there was no difference between treatment groups in improvement in quality of life or patient satisfaction; and a reduction in symptom severity noted after 6 weeks of home treatment faded within 6 months.
“We found no differences in admission rates either, which suggests that intensive home treatment is not a substitute for inpatient care but a different treatment opportunity for psychiatric patients in crisis,” Jurgen Cornelis, MD, Arkin Institute for Mental Health, Amsterdam, and colleagues write.
The findings were published online in The Lancet Psychiatry.
Increasingly popular
“Intensive home treatment is increasingly popular as an alternative to hospitalization. It was developed to prevent or reduce levels of inpatient care and facilitate the transition between inpatient care and low-intensity outpatient care,” the investigators write.
However, there have previously been only two randomized controlled trials published that assessed this type of care, resulting in “somewhat conflicting findings,” they add.
For the current study, participants presented to psychiatric emergency wards at two medical centers in the Netherlands. They were included only if they were able to offer informed consent within 14 days.
The intensive home treatment group (n = 183) worked with a multidisciplinary team that designed a care plan tailored to their specific crisis. Treatment components included pharmacotherapy, up to three home visits each day, psychoeducation, brief supportive and cognitive behavioral therapy, social care, and support and empowerment of the patient’s informal care system.
The usual care group (n = 63) commonly received a combination of highly intensive inpatient treatment in the first phase and outpatient treatment up to two times a week in the second phase. Treatment included similar components as those in intensive home treatment.
The most common primary clinical diagnosis in both groups was mood disorder, followed by psychotic disorders, personality disorders, or anxiety disorders.
The home treatment group had a significantly higher total mean item score on the Brief Psychiatric Rating Scale (BPRS) at baseline (2.23 vs. 2.04, P = .04).
Mixed results
Results at 6 weeks showed the number of hospital days was 25.3% lower in the home treatment group, compared with those who received usual care.
That trend continued at 1 year, with the intensive home treatment group recording 36.6% fewer hospital days than the usual care group (mean, 42.5 days vs. 67 days, respectively; P = .03).
However, the number of patients who were admitted in the first 6 weeks and at 1 year stayed the same, as did the mean number of admissions per patient over 12 months.
The home treatment group reported significantly fewer symptoms on the BPRS depression and anxiety scale at 6 weeks, compared with the usual treatment group (P = .025), but that difference was not maintained after 6 months.
The number of adverse events, including suicide attempts, was similar between the groups. Three patients in the home treatment group and two in the usual care group died by suicide.
“Future research should focus on which components of intensive home treatment or hospitalization can be used when, for whom, and meet which goals, so that both hospital care and intensive home treatment can be used proportionally and efficiently for patients in psychiatric crisis,” the investigators write.
Not generalizable?
In an accompanying editorial, Claire Henderson, PhD, Institute of Psychiatry, Psychology, and Neuroscience at King’s College London, noted that generalizing the study’s results to other countries could be problematic, especially to regions such as North America, which have shorter lengths of stay for psychiatric hospitalization.
“Future trials looking at intensive home treatment would be most informative if done in countries with relatively short lengths of stay, and without separate crisis services for people receiving assertive community treatment,” Dr. Henderson writes.
The study was funded by De Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes-en Zenuwzieken. The investigators and Dr. Henderson have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY
Understanding the neuroscience of narcissism
Editor’s Note: The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
The cognitive features and phenotypic diversity of narcissism subtypes are partially unknown.
This study integrates both grandiose and vulnerable narcissism into a common framework with cognitive components connected to these traits.
Study design
This study enrolled 478 participants (397 female and 4 did not reveal their gender).
The average age of participants was 35 years (standard deviation, 14.97), with a range of 18-76 years.
A 25-item version of the Narcissistic Personality Inventory (NPI), a 40-item self-report measure of narcissism traits, was used to assess the level of authority, grandiose exhibitionism, and entitlement/exploitativeness characteristics of study participants.
The Maladaptive Covert Narcissism Scale, an expanded version of the 23-item self-report Hypersensitive Narcissism Scale, was used to assess the level of hypersensitivity, vulnerability, and entitlement of study participants.
The Rosenberg Self-Esteem Scale, a 10-item self-report scale, was used to assess the level of self-esteem of study participants.
The Young Schema Questionnaire is a 244-item measure of 19 different maladaptive schemas and was used to observe Emotional Deprivation, Vulnerability to Harm and Illness, and Entitlement schemas of study participants.
The Empathizing Quotient is a self-report measure and was used to assess the emotional intelligence of study participants.
Key results
Moderate correlation between grandiose and vulnerable narcissism and the Entitlement schema was observed.
A moderate/strong connection was observed between vulnerable narcissism and the Vulnerability to Harm and Illness schema and a moderate connection with the Emotional Deprivation schema.
No significant correlation was observed between grandiose narcissism and the Emotional Deprivation schema.
A moderate, negative correlation between vulnerable narcissism and emotional skills was observed.
A positive, weak connection between grandiose narcissism and self-esteem; and a negative, moderate connection between vulnerable narcissism and self-esteem were observed.
Gender and age were associated with empathic skills, and age was weakly/moderately connected with self-esteem and vulnerable narcissism.
Limitations
This was a cross-sectional analysis investigating a temporally specific state of personality and cognitive functioning.
The gender ratio was shifted toward women in this study.
Conclusions drawn from connections between observed components are interchangeable and cause/effect connections cannot be discerned.
Disclosures
The study was supported by the National Research, Development, and Innovation Office (Grant No. NRDI–138040) and by the Human Resource Development Operational Program – Comprehensive developments at the University of Pécs for the implementation of intelligent specialization (EFOP-3.6.1-16-2016-00004). First author Dorian Vida’s work was supported by the Collegium Talentum Programme of Hungary. None of the authors disclosed any competing interests.
This is a summary of a preprint research study, “In the mind of Narcissus: the mediating role of emotional regulation in the emergence of distorted cognitions,” written by Dorian Vida from the University of Pécs, Hungary and colleagues on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.
A version of this article first appeared on Medscape.com
Editor’s Note: The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
The cognitive features and phenotypic diversity of narcissism subtypes are partially unknown.
This study integrates both grandiose and vulnerable narcissism into a common framework with cognitive components connected to these traits.
Study design
This study enrolled 478 participants (397 female and 4 did not reveal their gender).
The average age of participants was 35 years (standard deviation, 14.97), with a range of 18-76 years.
A 25-item version of the Narcissistic Personality Inventory (NPI), a 40-item self-report measure of narcissism traits, was used to assess the level of authority, grandiose exhibitionism, and entitlement/exploitativeness characteristics of study participants.
The Maladaptive Covert Narcissism Scale, an expanded version of the 23-item self-report Hypersensitive Narcissism Scale, was used to assess the level of hypersensitivity, vulnerability, and entitlement of study participants.
The Rosenberg Self-Esteem Scale, a 10-item self-report scale, was used to assess the level of self-esteem of study participants.
The Young Schema Questionnaire is a 244-item measure of 19 different maladaptive schemas and was used to observe Emotional Deprivation, Vulnerability to Harm and Illness, and Entitlement schemas of study participants.
The Empathizing Quotient is a self-report measure and was used to assess the emotional intelligence of study participants.
Key results
Moderate correlation between grandiose and vulnerable narcissism and the Entitlement schema was observed.
A moderate/strong connection was observed between vulnerable narcissism and the Vulnerability to Harm and Illness schema and a moderate connection with the Emotional Deprivation schema.
No significant correlation was observed between grandiose narcissism and the Emotional Deprivation schema.
A moderate, negative correlation between vulnerable narcissism and emotional skills was observed.
A positive, weak connection between grandiose narcissism and self-esteem; and a negative, moderate connection between vulnerable narcissism and self-esteem were observed.
Gender and age were associated with empathic skills, and age was weakly/moderately connected with self-esteem and vulnerable narcissism.
Limitations
This was a cross-sectional analysis investigating a temporally specific state of personality and cognitive functioning.
The gender ratio was shifted toward women in this study.
Conclusions drawn from connections between observed components are interchangeable and cause/effect connections cannot be discerned.
Disclosures
The study was supported by the National Research, Development, and Innovation Office (Grant No. NRDI–138040) and by the Human Resource Development Operational Program – Comprehensive developments at the University of Pécs for the implementation of intelligent specialization (EFOP-3.6.1-16-2016-00004). First author Dorian Vida’s work was supported by the Collegium Talentum Programme of Hungary. None of the authors disclosed any competing interests.
This is a summary of a preprint research study, “In the mind of Narcissus: the mediating role of emotional regulation in the emergence of distorted cognitions,” written by Dorian Vida from the University of Pécs, Hungary and colleagues on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.
A version of this article first appeared on Medscape.com
Editor’s Note: The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer reviewed.
Key takeaway
Why this matters
The cognitive features and phenotypic diversity of narcissism subtypes are partially unknown.
This study integrates both grandiose and vulnerable narcissism into a common framework with cognitive components connected to these traits.
Study design
This study enrolled 478 participants (397 female and 4 did not reveal their gender).
The average age of participants was 35 years (standard deviation, 14.97), with a range of 18-76 years.
A 25-item version of the Narcissistic Personality Inventory (NPI), a 40-item self-report measure of narcissism traits, was used to assess the level of authority, grandiose exhibitionism, and entitlement/exploitativeness characteristics of study participants.
The Maladaptive Covert Narcissism Scale, an expanded version of the 23-item self-report Hypersensitive Narcissism Scale, was used to assess the level of hypersensitivity, vulnerability, and entitlement of study participants.
The Rosenberg Self-Esteem Scale, a 10-item self-report scale, was used to assess the level of self-esteem of study participants.
The Young Schema Questionnaire is a 244-item measure of 19 different maladaptive schemas and was used to observe Emotional Deprivation, Vulnerability to Harm and Illness, and Entitlement schemas of study participants.
The Empathizing Quotient is a self-report measure and was used to assess the emotional intelligence of study participants.
Key results
Moderate correlation between grandiose and vulnerable narcissism and the Entitlement schema was observed.
A moderate/strong connection was observed between vulnerable narcissism and the Vulnerability to Harm and Illness schema and a moderate connection with the Emotional Deprivation schema.
No significant correlation was observed between grandiose narcissism and the Emotional Deprivation schema.
A moderate, negative correlation between vulnerable narcissism and emotional skills was observed.
A positive, weak connection between grandiose narcissism and self-esteem; and a negative, moderate connection between vulnerable narcissism and self-esteem were observed.
Gender and age were associated with empathic skills, and age was weakly/moderately connected with self-esteem and vulnerable narcissism.
Limitations
This was a cross-sectional analysis investigating a temporally specific state of personality and cognitive functioning.
The gender ratio was shifted toward women in this study.
Conclusions drawn from connections between observed components are interchangeable and cause/effect connections cannot be discerned.
Disclosures
The study was supported by the National Research, Development, and Innovation Office (Grant No. NRDI–138040) and by the Human Resource Development Operational Program – Comprehensive developments at the University of Pécs for the implementation of intelligent specialization (EFOP-3.6.1-16-2016-00004). First author Dorian Vida’s work was supported by the Collegium Talentum Programme of Hungary. None of the authors disclosed any competing interests.
This is a summary of a preprint research study, “In the mind of Narcissus: the mediating role of emotional regulation in the emergence of distorted cognitions,” written by Dorian Vida from the University of Pécs, Hungary and colleagues on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.
A version of this article first appeared on Medscape.com
When suffering defies diagnosis
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A prescription for de-diagnosing
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.