User login
Regular skin exams reduced advanced KCs in posttransplant patients
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
REPORTING FROM IID 2018
Key clinical point: Transplant patients need help to ensure they get annual dermatology checkups.
Major finding: Just 2.1% of the patients in the review had annual exams, and less than half saw a dermatologist even once during an average of 5-years follow-up.
Study details: A review of 10,198 solid organ transplant cases.
Disclosures: There was no industry funding, and the lead investigator had no disclosures.
Source: Chan A et al. IID 2018, Abstract 522
Keratinocyte carcinoma added no VTE risk in cohort study
Keratinocyte carcinoma patients were not at increased risk of venous thromboembolism (VTE) compared with controls in a recent population-based study of more than 700,000 insurance claims, according to investigators.
That finding suggests that clinicians should more carefully consider use of prophylactic anticoagulation in patients with squamous or basal cell carcinoma, said Shannon F. Rudy, MD, of Stanford (Calif.) University, and her coinvestigators. The report was published in JAMA Facial Plastic Surgery.
“While chemoprophylaxis is important when treating patients with an increased risk of VTE, it is equally important that such agents are not administered inappropriately because they can lead to perioperative complications,” wrote Dr. Rudy and her coauthors.
In current practice, patients with keratinocyte carcinomas (i.e., squamous cell carcinoma or basal cell carcinoma) are routinely classified at higher risk of thromboembolic events because of their diagnosis. That subsequently impacts treatment decisions regarding perioperative anticoagulation, the investigators noted.
Their population-based, retrospective analysis was based on insurance claims made between Jan. 1, 2007, and Dec. 31, 2014. The investigators identified three cohorts: 417,839 keratinocyte carcinoma patients, 314,736 controls at average risk of VTE, and 7,671 individuals considered to be at high risk of VTE because of a prior diagnosis of acute myeloid leukemia or pancreatic cancer.
In the keratinocyte carcinoma cohort, investigators found VTE risk was lower compared with the high-risk cohort in univariable analysis, multivariable analysis, and after matching patient characteristics and risk factors (odds ratio, 0.52; 95% confidence interval, 0.35-0.78; P = .001).
Compared with the control cohort, the keratinocyte carcinoma cohort had a higher risk of VTE in univariable analysis; however, the risk was lower in multivariable analysis, and not statistically different when patient characteristics and risk factors were matched (OR, 0.95; 95% CI, 0.89-1.01; P = .08).
“These results argue for careful consideration of risk assessment models, such as the Caprini score, when a surgical procedure is planned for a patient with keratinocyte carcinoma and no other risk factors for VTE in order to limit unnecessary exposure to the potential risk of VTE chemoprophylaxis,” Dr. Rudy and her coauthors wrote.
The Caprini score is a commonly used, validated, VTE risk stratification model that assigns points to specific risk factors, producing a score that can be used to decide on prophylaxis regimens, they noted.
A present or previous cancer diagnosis is worth 2 points in the Caprini system, which would put a patient at the upper end of the “low risk” category, while one additional risk factor such as planned minor surgery would indicate moderate risk.
“Recently, Caprini has begun to exclude basal cell carcinoma from this calculation, but no reference to evidence is given,” the researchers wrote.
Dr. Rudy and her coauthors had no conflicts of interest to disclose.
SOURCE: Rudy SF et al. JAMA Facial Plast Surg. 2018 May 24. doi: 10.1001/jamafacial.2018.0331.
Keratinocyte carcinoma patients were not at increased risk of venous thromboembolism (VTE) compared with controls in a recent population-based study of more than 700,000 insurance claims, according to investigators.
That finding suggests that clinicians should more carefully consider use of prophylactic anticoagulation in patients with squamous or basal cell carcinoma, said Shannon F. Rudy, MD, of Stanford (Calif.) University, and her coinvestigators. The report was published in JAMA Facial Plastic Surgery.
“While chemoprophylaxis is important when treating patients with an increased risk of VTE, it is equally important that such agents are not administered inappropriately because they can lead to perioperative complications,” wrote Dr. Rudy and her coauthors.
In current practice, patients with keratinocyte carcinomas (i.e., squamous cell carcinoma or basal cell carcinoma) are routinely classified at higher risk of thromboembolic events because of their diagnosis. That subsequently impacts treatment decisions regarding perioperative anticoagulation, the investigators noted.
Their population-based, retrospective analysis was based on insurance claims made between Jan. 1, 2007, and Dec. 31, 2014. The investigators identified three cohorts: 417,839 keratinocyte carcinoma patients, 314,736 controls at average risk of VTE, and 7,671 individuals considered to be at high risk of VTE because of a prior diagnosis of acute myeloid leukemia or pancreatic cancer.
In the keratinocyte carcinoma cohort, investigators found VTE risk was lower compared with the high-risk cohort in univariable analysis, multivariable analysis, and after matching patient characteristics and risk factors (odds ratio, 0.52; 95% confidence interval, 0.35-0.78; P = .001).
Compared with the control cohort, the keratinocyte carcinoma cohort had a higher risk of VTE in univariable analysis; however, the risk was lower in multivariable analysis, and not statistically different when patient characteristics and risk factors were matched (OR, 0.95; 95% CI, 0.89-1.01; P = .08).
“These results argue for careful consideration of risk assessment models, such as the Caprini score, when a surgical procedure is planned for a patient with keratinocyte carcinoma and no other risk factors for VTE in order to limit unnecessary exposure to the potential risk of VTE chemoprophylaxis,” Dr. Rudy and her coauthors wrote.
The Caprini score is a commonly used, validated, VTE risk stratification model that assigns points to specific risk factors, producing a score that can be used to decide on prophylaxis regimens, they noted.
A present or previous cancer diagnosis is worth 2 points in the Caprini system, which would put a patient at the upper end of the “low risk” category, while one additional risk factor such as planned minor surgery would indicate moderate risk.
“Recently, Caprini has begun to exclude basal cell carcinoma from this calculation, but no reference to evidence is given,” the researchers wrote.
Dr. Rudy and her coauthors had no conflicts of interest to disclose.
SOURCE: Rudy SF et al. JAMA Facial Plast Surg. 2018 May 24. doi: 10.1001/jamafacial.2018.0331.
Keratinocyte carcinoma patients were not at increased risk of venous thromboembolism (VTE) compared with controls in a recent population-based study of more than 700,000 insurance claims, according to investigators.
That finding suggests that clinicians should more carefully consider use of prophylactic anticoagulation in patients with squamous or basal cell carcinoma, said Shannon F. Rudy, MD, of Stanford (Calif.) University, and her coinvestigators. The report was published in JAMA Facial Plastic Surgery.
“While chemoprophylaxis is important when treating patients with an increased risk of VTE, it is equally important that such agents are not administered inappropriately because they can lead to perioperative complications,” wrote Dr. Rudy and her coauthors.
In current practice, patients with keratinocyte carcinomas (i.e., squamous cell carcinoma or basal cell carcinoma) are routinely classified at higher risk of thromboembolic events because of their diagnosis. That subsequently impacts treatment decisions regarding perioperative anticoagulation, the investigators noted.
Their population-based, retrospective analysis was based on insurance claims made between Jan. 1, 2007, and Dec. 31, 2014. The investigators identified three cohorts: 417,839 keratinocyte carcinoma patients, 314,736 controls at average risk of VTE, and 7,671 individuals considered to be at high risk of VTE because of a prior diagnosis of acute myeloid leukemia or pancreatic cancer.
In the keratinocyte carcinoma cohort, investigators found VTE risk was lower compared with the high-risk cohort in univariable analysis, multivariable analysis, and after matching patient characteristics and risk factors (odds ratio, 0.52; 95% confidence interval, 0.35-0.78; P = .001).
Compared with the control cohort, the keratinocyte carcinoma cohort had a higher risk of VTE in univariable analysis; however, the risk was lower in multivariable analysis, and not statistically different when patient characteristics and risk factors were matched (OR, 0.95; 95% CI, 0.89-1.01; P = .08).
“These results argue for careful consideration of risk assessment models, such as the Caprini score, when a surgical procedure is planned for a patient with keratinocyte carcinoma and no other risk factors for VTE in order to limit unnecessary exposure to the potential risk of VTE chemoprophylaxis,” Dr. Rudy and her coauthors wrote.
The Caprini score is a commonly used, validated, VTE risk stratification model that assigns points to specific risk factors, producing a score that can be used to decide on prophylaxis regimens, they noted.
A present or previous cancer diagnosis is worth 2 points in the Caprini system, which would put a patient at the upper end of the “low risk” category, while one additional risk factor such as planned minor surgery would indicate moderate risk.
“Recently, Caprini has begun to exclude basal cell carcinoma from this calculation, but no reference to evidence is given,” the researchers wrote.
Dr. Rudy and her coauthors had no conflicts of interest to disclose.
SOURCE: Rudy SF et al. JAMA Facial Plast Surg. 2018 May 24. doi: 10.1001/jamafacial.2018.0331.
FROM JAMA FACIAL PLASTIC SURGERY
Key clinical point: Keratinocyte patients had no increased risk of venous thromboembolism (VTE) versus controls, suggesting the need to carefully consider whether prophylactic anticoagulation is needed at the time of surgery in these patients.
Major finding: Risk of VTE in the keratinocyte carcinoma cohort was not different compared with controls after adjustment for patient characteristics and risk factors (OR, 0.95; 95% CI, 0.89-1.01; P = .08).
Study details: A population-based retrospective analysis of insurance claims made between Jan. 1, 2007, and Dec. 31, 2014, including 417,839 keratinocyte carcinoma patients, 314,736 controls, and a high-risk cohort of 7,671 individuals.
Disclosures: The authors declared no conflicts of interest.
Source: Rudy SF et al. JAMA Facial Plast Surg. 2018 May 24. doi: 10.1001/jamafacial.2018.0331.
Spotlight on nonmelanoma skin cancer’s true burden
CHICAGO – The true extent of the burden imposed by nonmelanoma skin cancer remains widely underappreciated by health policy makers, the public, employers, and nondermatologist physicians, Marta J. Van Beek, MD, asserted at the annual meeting of the American College of Mohs Surgery.
It’s very much in the interest of Mohs surgeons, as the experts in cutaneous malignancies, to get the accurate message out, she added.
Abundant evidence indicates there is an ongoing epidemic of nonmelanoma skin cancer (NMSC) in the United States – and it is associated with a surprising amount of morbidity and mortality, the dermatologic surgeon observed.
For example, while the American Academy of Dermatology’s 93-page Burden of Skin Disease report identified melanoma as the No. 1 cause of mortality because of skin disease – no surprise there – what may come as news to many is that NMSC was No. 2, accounting for 4,376 deaths in 2013, or 19% of the total. That’s more deaths than occurred because of wounds and burns.
And while the number of cases of NMSC is going up year after year as the population ages, it’s also the case that patients with complex NMSC are developing it at a younger and younger age. As documented in the AAD’s DataDerm registry encompassing more than 6 million patients seen by dermatologists during 2015-2017, well over 20,000 patients who underwent Mohs micrographic surgery for NMSC were aged 45-55 years, and another 60,000 were aged 55-65 years. That being said, Mohs surgery was used to treat 477,365 NMSCs in 318,933 patients included in DataDerm during 2015-2017, and in that population, basal cell carcinomas outnumbered squamous cell carcinomas 2:1.
An interesting aspect of the burden imparted by NMSC is that patients with NMSC have a higher risk of other types of cancer, and when they develop those other primary cancers they tend to do more poorly than cancer patients without a history of NMSC, Dr. Van Beek continued.
She cited a comprehensive study by investigators at the Medical University of South Carolina, Charleston, who concluded that the odds of developing a noncutaneous second primary malignancy were 27% greater in individuals with a history of NMSC than in those without such a history. The increased risk was statistically significant for 26 types of noncutaneous cancer, consistent in both men and women, and the younger a patient’s age at onset of NMSC, the stronger the association with noncutaneous cancers (Adv Cancer Res. 2016;130:257-91).
In a separate systematic review by some of the same investigators, patients with a history of squamous cell carcinoma were at a 30% increased risk of all-cause mortality and 117% greater cancer-specific mortality than those without a history of the disease. The associations were less potent for basal cell carcinoma (Arch Dermatol Res. 2017 May;309[4]:243-51).
“You are more likely to die of your nonskin cancer if you’ve ever had a skin cancer, regardless of what that other cancer is. This may mean that once you have a skin cancer, maybe that proves you have poor protoplasm that makes you more prone to other cancers, but even if that’s the case I think it demonstrates that nonmelanoma skin cancer has a substantial contribution to morbidity and mortality outside of what we normally think about,” Dr. Van Beek said.
Another underappreciated aspect of the burden of NMSC is what economists call lost opportunity cost. This isn’t the direct medical cost, but work time missed because of disease. In 2013, according to the AAD Burden of Skin Disease report, melanoma was responsible for $88 million worth of lost productivity, while for NMSC, the figure was $376 million.
“When you’re talking about the burden of disease, it’s important to actually talk to employers about how important it is to pay for the treatment of skin cancer because that keeps people at work and productive,” the dermatologist said.
Investigators for the World Health Organization’s Global Burden of Disease project estimate that the total years lost to disability for patients with NMSC are comparable with the figures for patients with thyroid, esophageal, or ovarian cancer, Dr. Van Beek noted.
Payers and health policy makers are unnerved by the growing utilization of Mohs surgery, she warned.
“This is really important: If you want to substantiate our utilization, you have to make policy makers understand that we are doing this because more people have skin cancer,” she emphasized.
Dr. Van Beek reported no financial conflicts regarding her presentation.
CHICAGO – The true extent of the burden imposed by nonmelanoma skin cancer remains widely underappreciated by health policy makers, the public, employers, and nondermatologist physicians, Marta J. Van Beek, MD, asserted at the annual meeting of the American College of Mohs Surgery.
It’s very much in the interest of Mohs surgeons, as the experts in cutaneous malignancies, to get the accurate message out, she added.
Abundant evidence indicates there is an ongoing epidemic of nonmelanoma skin cancer (NMSC) in the United States – and it is associated with a surprising amount of morbidity and mortality, the dermatologic surgeon observed.
For example, while the American Academy of Dermatology’s 93-page Burden of Skin Disease report identified melanoma as the No. 1 cause of mortality because of skin disease – no surprise there – what may come as news to many is that NMSC was No. 2, accounting for 4,376 deaths in 2013, or 19% of the total. That’s more deaths than occurred because of wounds and burns.
And while the number of cases of NMSC is going up year after year as the population ages, it’s also the case that patients with complex NMSC are developing it at a younger and younger age. As documented in the AAD’s DataDerm registry encompassing more than 6 million patients seen by dermatologists during 2015-2017, well over 20,000 patients who underwent Mohs micrographic surgery for NMSC were aged 45-55 years, and another 60,000 were aged 55-65 years. That being said, Mohs surgery was used to treat 477,365 NMSCs in 318,933 patients included in DataDerm during 2015-2017, and in that population, basal cell carcinomas outnumbered squamous cell carcinomas 2:1.
An interesting aspect of the burden imparted by NMSC is that patients with NMSC have a higher risk of other types of cancer, and when they develop those other primary cancers they tend to do more poorly than cancer patients without a history of NMSC, Dr. Van Beek continued.
She cited a comprehensive study by investigators at the Medical University of South Carolina, Charleston, who concluded that the odds of developing a noncutaneous second primary malignancy were 27% greater in individuals with a history of NMSC than in those without such a history. The increased risk was statistically significant for 26 types of noncutaneous cancer, consistent in both men and women, and the younger a patient’s age at onset of NMSC, the stronger the association with noncutaneous cancers (Adv Cancer Res. 2016;130:257-91).
In a separate systematic review by some of the same investigators, patients with a history of squamous cell carcinoma were at a 30% increased risk of all-cause mortality and 117% greater cancer-specific mortality than those without a history of the disease. The associations were less potent for basal cell carcinoma (Arch Dermatol Res. 2017 May;309[4]:243-51).
“You are more likely to die of your nonskin cancer if you’ve ever had a skin cancer, regardless of what that other cancer is. This may mean that once you have a skin cancer, maybe that proves you have poor protoplasm that makes you more prone to other cancers, but even if that’s the case I think it demonstrates that nonmelanoma skin cancer has a substantial contribution to morbidity and mortality outside of what we normally think about,” Dr. Van Beek said.
Another underappreciated aspect of the burden of NMSC is what economists call lost opportunity cost. This isn’t the direct medical cost, but work time missed because of disease. In 2013, according to the AAD Burden of Skin Disease report, melanoma was responsible for $88 million worth of lost productivity, while for NMSC, the figure was $376 million.
“When you’re talking about the burden of disease, it’s important to actually talk to employers about how important it is to pay for the treatment of skin cancer because that keeps people at work and productive,” the dermatologist said.
Investigators for the World Health Organization’s Global Burden of Disease project estimate that the total years lost to disability for patients with NMSC are comparable with the figures for patients with thyroid, esophageal, or ovarian cancer, Dr. Van Beek noted.
Payers and health policy makers are unnerved by the growing utilization of Mohs surgery, she warned.
“This is really important: If you want to substantiate our utilization, you have to make policy makers understand that we are doing this because more people have skin cancer,” she emphasized.
Dr. Van Beek reported no financial conflicts regarding her presentation.
CHICAGO – The true extent of the burden imposed by nonmelanoma skin cancer remains widely underappreciated by health policy makers, the public, employers, and nondermatologist physicians, Marta J. Van Beek, MD, asserted at the annual meeting of the American College of Mohs Surgery.
It’s very much in the interest of Mohs surgeons, as the experts in cutaneous malignancies, to get the accurate message out, she added.
Abundant evidence indicates there is an ongoing epidemic of nonmelanoma skin cancer (NMSC) in the United States – and it is associated with a surprising amount of morbidity and mortality, the dermatologic surgeon observed.
For example, while the American Academy of Dermatology’s 93-page Burden of Skin Disease report identified melanoma as the No. 1 cause of mortality because of skin disease – no surprise there – what may come as news to many is that NMSC was No. 2, accounting for 4,376 deaths in 2013, or 19% of the total. That’s more deaths than occurred because of wounds and burns.
And while the number of cases of NMSC is going up year after year as the population ages, it’s also the case that patients with complex NMSC are developing it at a younger and younger age. As documented in the AAD’s DataDerm registry encompassing more than 6 million patients seen by dermatologists during 2015-2017, well over 20,000 patients who underwent Mohs micrographic surgery for NMSC were aged 45-55 years, and another 60,000 were aged 55-65 years. That being said, Mohs surgery was used to treat 477,365 NMSCs in 318,933 patients included in DataDerm during 2015-2017, and in that population, basal cell carcinomas outnumbered squamous cell carcinomas 2:1.
An interesting aspect of the burden imparted by NMSC is that patients with NMSC have a higher risk of other types of cancer, and when they develop those other primary cancers they tend to do more poorly than cancer patients without a history of NMSC, Dr. Van Beek continued.
She cited a comprehensive study by investigators at the Medical University of South Carolina, Charleston, who concluded that the odds of developing a noncutaneous second primary malignancy were 27% greater in individuals with a history of NMSC than in those without such a history. The increased risk was statistically significant for 26 types of noncutaneous cancer, consistent in both men and women, and the younger a patient’s age at onset of NMSC, the stronger the association with noncutaneous cancers (Adv Cancer Res. 2016;130:257-91).
In a separate systematic review by some of the same investigators, patients with a history of squamous cell carcinoma were at a 30% increased risk of all-cause mortality and 117% greater cancer-specific mortality than those without a history of the disease. The associations were less potent for basal cell carcinoma (Arch Dermatol Res. 2017 May;309[4]:243-51).
“You are more likely to die of your nonskin cancer if you’ve ever had a skin cancer, regardless of what that other cancer is. This may mean that once you have a skin cancer, maybe that proves you have poor protoplasm that makes you more prone to other cancers, but even if that’s the case I think it demonstrates that nonmelanoma skin cancer has a substantial contribution to morbidity and mortality outside of what we normally think about,” Dr. Van Beek said.
Another underappreciated aspect of the burden of NMSC is what economists call lost opportunity cost. This isn’t the direct medical cost, but work time missed because of disease. In 2013, according to the AAD Burden of Skin Disease report, melanoma was responsible for $88 million worth of lost productivity, while for NMSC, the figure was $376 million.
“When you’re talking about the burden of disease, it’s important to actually talk to employers about how important it is to pay for the treatment of skin cancer because that keeps people at work and productive,” the dermatologist said.
Investigators for the World Health Organization’s Global Burden of Disease project estimate that the total years lost to disability for patients with NMSC are comparable with the figures for patients with thyroid, esophageal, or ovarian cancer, Dr. Van Beek noted.
Payers and health policy makers are unnerved by the growing utilization of Mohs surgery, she warned.
“This is really important: If you want to substantiate our utilization, you have to make policy makers understand that we are doing this because more people have skin cancer,” she emphasized.
Dr. Van Beek reported no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM THE ACMS ANNUAL MEETING
Cemiplimab impresses in advanced CSCC
CHICAGO – The investigational programmed cell death protein 1 checkpoint inhibitor cemiplimab proved highly effective for the treatment of locally advanced or metastatic cutaneous squamous cell carcinoma in a phase 1 clinical trial, Michael R. Migden, MD, reported at the annual meeting of the American College of Mohs Surgery.
And this was no ordinary phase 1 study, he noted. Because there is no Food and Drug Administration–approved treatment for advanced cutaneous squamous cell carcinoma (CSCC), cemiplimab has been granted both Breakthrough Drug and Orphan Drug status by the FDA and the European Medicines Agency.
Given the likelihood that cemiplimab will receive expeditious regulatory approval to address this major unmet need, he offered his colleagues practical tips on its use, including information about the drug’s chief side effects as well as a heads-up regarding the importance of early recognition of the pseudoprogression phenomenon that can occur with the drug.
He predicted this fully human monoclonal antibody directed at programmed cell death protein 1 (PD-1) is going to be an important drug for Mohs surgeons.
“Immunotherapy is becoming increasingly relevant to micrographic surgery and dermatologic oncology practice and fellowship training. Care for larger, advanced CSCC falls within our scope of practice and we should play an essential role, inclusive of multidisciplinary care, in the management and follow-up of these patients,” asserted Dr. Migden, a dermatologic surgeon at the University of Texas MD Anderson Cancer Center, Houston.
The open-label, phase 1 study included seven patients with distant metastatic CSCC and nine with locally and/or regionally advanced disease. They were treated with 3 mg/kg IV cemiplimab every 2 weeks for 48 weeks, with Response Evaluation Criteria In Solid Tumors 1.1 criteria used for assessment of response status every 8 weeks. More than 80% of the tumors were located in the head and neck. The great majority of study participants had previously been treated with radiation therapy and systemic agents, to little effect.
The complete response rate at 48 weeks was 12.5%, with tumor clearance occurring as quickly as 14 weeks. Another 25% of patients had a partial response, for an overall response rate of 37.5%. But that’s not the full success story, as another 31% of patients had stable disease. Thus, 11 of 16 patients, or 69%, experienced disease control.
“A disease-control rate of nearly 70% is really important because these are patients with life-threatening tumors. To be able to hold them steady is a big deal,” Dr. Migden observed.
One-quarter of study participants experienced progressive disease. The remainder weren’t evaluated for various reasons.
The dermatologist pointed out that locally advanced disease was particularly responsive to cemiplimab, with four of nine affected patients experiencing complete or partial response, for an overall response rate of 44%. This is consistent with the preliminary results of the pivotal phase 2 study, in which the overall response rate in the 78 participants with unresectable, locally advanced CSCC was 46%.
The phase 2 trial also includes another 59 patients with metastatic CSCC on 3 mg/kg IV cemiplimab every 14 days, as well as 56 patients with metastatic disease assigned to flat-dose 350-mg IV cemiplimab every 21 days.
Treatment side effects
In the phase 1 study, immunotherapy with cemiplimab was far better tolerated than in traditional cancer chemotherapy. There were two grade 3 cases of elevated liver enzymes and one of arthralgia, but no significant fatigue or nausea and no hypothyroidism. However, judging from the cumulative experience accrued with the five PD-1 checkpoint inhibitors already approved for treatment of other cancers, one must be prepared to encounter hypothyroidism and other endocrinopathies, pneumonitis, hepatitis, and rashes.
“The clinician must have a very high index of suspicion for these immune-related adverse events and a low threshold to consult with colleagues in other specialties – pulmonary, endocrine, and medical oncology – for evaluation and management of these possible side effects. I tell all the patients who are on cemiplimab, ‘Any new anything – a slight cough, mild diarrhea – you’re coming in and you’re getting checked,’ ” according to Dr. Migden.
That being said, the majority of immune-related adverse events because of PD-1 inhibitors are mild to moderate. Of the few that reach grade 3 or above, most can be successfully managed by pausing or discontinuing anti–PD-1 therapy coupled with prompt initiation of immunosuppressive therapy, typically with high-dose steroids, he added.
Look sharp for pseudoprogression
Pseudoprogression is a phenomenon whereby immunotherapy results in inflammatory changes bringing about a temporary increase in tumor size that precedes tumor shrinkage. It’s uncommon, occurring in 3 of 16 patients in the phase 1 study. The mechanism probably involves tumor infiltration by massive numbers of activated T cells. And there is evidence from other PD-1 inhibitor studies in advanced cancers that pseudoprogression may actually be a marker for increased likelihood of survival beyond 1 year.
“Pseudoprogression is important to recognize because the patients you treat with cemiplimab can get worse before they get better,” the dermatologist explained. “So you don’t want to prematurely discontinue treatment because you’re misclassifying it as tumor progression.”
The rationale for anti-PD-1 therapy in CSCC
Tumors that express PD-1 bind to PD–ligand 1 on T cells, switching off T-cell mediated tumor destruction and thereby allowing the malignancy to thrive.
“Simplified, the strategy here is to interfere with the interaction at the T-cell off switch, either with an antibody to PD–ligand 1, such as atezolizumab [Tecentriq], or an antibody to the PD-1 receptor, where cemiplimab works. By turning off the off switch, we get a T cell fully on and attacking the tumor cell,” Dr. Migden said.
“The more the tumor mutation burden, the better immunotherapy works – and CSCC has the highest tumor mutation burden of any tumor type in the Cancer Genome Atlas, several times higher than melanoma. Interestingly, basal cell carcinoma has an even higher tumor mutation burden than CSCC, but it’s not part of the atlas,” he continued.
Although the proportion of CSCCs that are locally advanced hasn’t been well established, it’s clear that CSCC is the deadliest nonmelanoma skin cancer, accounting for 3,900-8,800 deaths annually in the United States.
The cemiplimab phase 1 and 2 clinical trials for CSCC were jointly sponsored by Regeneron and Sanofi. The monoclonal antibody is also being developed for treatment of myeloma and lung cancer. Dr. Migden reported receiving honoraria from Regeneron and Sanofi, as well as from Genentech, Lilly, Novartis, and Sun Pharmaceuticals.
CHICAGO – The investigational programmed cell death protein 1 checkpoint inhibitor cemiplimab proved highly effective for the treatment of locally advanced or metastatic cutaneous squamous cell carcinoma in a phase 1 clinical trial, Michael R. Migden, MD, reported at the annual meeting of the American College of Mohs Surgery.
And this was no ordinary phase 1 study, he noted. Because there is no Food and Drug Administration–approved treatment for advanced cutaneous squamous cell carcinoma (CSCC), cemiplimab has been granted both Breakthrough Drug and Orphan Drug status by the FDA and the European Medicines Agency.
Given the likelihood that cemiplimab will receive expeditious regulatory approval to address this major unmet need, he offered his colleagues practical tips on its use, including information about the drug’s chief side effects as well as a heads-up regarding the importance of early recognition of the pseudoprogression phenomenon that can occur with the drug.
He predicted this fully human monoclonal antibody directed at programmed cell death protein 1 (PD-1) is going to be an important drug for Mohs surgeons.
“Immunotherapy is becoming increasingly relevant to micrographic surgery and dermatologic oncology practice and fellowship training. Care for larger, advanced CSCC falls within our scope of practice and we should play an essential role, inclusive of multidisciplinary care, in the management and follow-up of these patients,” asserted Dr. Migden, a dermatologic surgeon at the University of Texas MD Anderson Cancer Center, Houston.
The open-label, phase 1 study included seven patients with distant metastatic CSCC and nine with locally and/or regionally advanced disease. They were treated with 3 mg/kg IV cemiplimab every 2 weeks for 48 weeks, with Response Evaluation Criteria In Solid Tumors 1.1 criteria used for assessment of response status every 8 weeks. More than 80% of the tumors were located in the head and neck. The great majority of study participants had previously been treated with radiation therapy and systemic agents, to little effect.
The complete response rate at 48 weeks was 12.5%, with tumor clearance occurring as quickly as 14 weeks. Another 25% of patients had a partial response, for an overall response rate of 37.5%. But that’s not the full success story, as another 31% of patients had stable disease. Thus, 11 of 16 patients, or 69%, experienced disease control.
“A disease-control rate of nearly 70% is really important because these are patients with life-threatening tumors. To be able to hold them steady is a big deal,” Dr. Migden observed.
One-quarter of study participants experienced progressive disease. The remainder weren’t evaluated for various reasons.
The dermatologist pointed out that locally advanced disease was particularly responsive to cemiplimab, with four of nine affected patients experiencing complete or partial response, for an overall response rate of 44%. This is consistent with the preliminary results of the pivotal phase 2 study, in which the overall response rate in the 78 participants with unresectable, locally advanced CSCC was 46%.
The phase 2 trial also includes another 59 patients with metastatic CSCC on 3 mg/kg IV cemiplimab every 14 days, as well as 56 patients with metastatic disease assigned to flat-dose 350-mg IV cemiplimab every 21 days.
Treatment side effects
In the phase 1 study, immunotherapy with cemiplimab was far better tolerated than in traditional cancer chemotherapy. There were two grade 3 cases of elevated liver enzymes and one of arthralgia, but no significant fatigue or nausea and no hypothyroidism. However, judging from the cumulative experience accrued with the five PD-1 checkpoint inhibitors already approved for treatment of other cancers, one must be prepared to encounter hypothyroidism and other endocrinopathies, pneumonitis, hepatitis, and rashes.
“The clinician must have a very high index of suspicion for these immune-related adverse events and a low threshold to consult with colleagues in other specialties – pulmonary, endocrine, and medical oncology – for evaluation and management of these possible side effects. I tell all the patients who are on cemiplimab, ‘Any new anything – a slight cough, mild diarrhea – you’re coming in and you’re getting checked,’ ” according to Dr. Migden.
That being said, the majority of immune-related adverse events because of PD-1 inhibitors are mild to moderate. Of the few that reach grade 3 or above, most can be successfully managed by pausing or discontinuing anti–PD-1 therapy coupled with prompt initiation of immunosuppressive therapy, typically with high-dose steroids, he added.
Look sharp for pseudoprogression
Pseudoprogression is a phenomenon whereby immunotherapy results in inflammatory changes bringing about a temporary increase in tumor size that precedes tumor shrinkage. It’s uncommon, occurring in 3 of 16 patients in the phase 1 study. The mechanism probably involves tumor infiltration by massive numbers of activated T cells. And there is evidence from other PD-1 inhibitor studies in advanced cancers that pseudoprogression may actually be a marker for increased likelihood of survival beyond 1 year.
“Pseudoprogression is important to recognize because the patients you treat with cemiplimab can get worse before they get better,” the dermatologist explained. “So you don’t want to prematurely discontinue treatment because you’re misclassifying it as tumor progression.”
The rationale for anti-PD-1 therapy in CSCC
Tumors that express PD-1 bind to PD–ligand 1 on T cells, switching off T-cell mediated tumor destruction and thereby allowing the malignancy to thrive.
“Simplified, the strategy here is to interfere with the interaction at the T-cell off switch, either with an antibody to PD–ligand 1, such as atezolizumab [Tecentriq], or an antibody to the PD-1 receptor, where cemiplimab works. By turning off the off switch, we get a T cell fully on and attacking the tumor cell,” Dr. Migden said.
“The more the tumor mutation burden, the better immunotherapy works – and CSCC has the highest tumor mutation burden of any tumor type in the Cancer Genome Atlas, several times higher than melanoma. Interestingly, basal cell carcinoma has an even higher tumor mutation burden than CSCC, but it’s not part of the atlas,” he continued.
Although the proportion of CSCCs that are locally advanced hasn’t been well established, it’s clear that CSCC is the deadliest nonmelanoma skin cancer, accounting for 3,900-8,800 deaths annually in the United States.
The cemiplimab phase 1 and 2 clinical trials for CSCC were jointly sponsored by Regeneron and Sanofi. The monoclonal antibody is also being developed for treatment of myeloma and lung cancer. Dr. Migden reported receiving honoraria from Regeneron and Sanofi, as well as from Genentech, Lilly, Novartis, and Sun Pharmaceuticals.
CHICAGO – The investigational programmed cell death protein 1 checkpoint inhibitor cemiplimab proved highly effective for the treatment of locally advanced or metastatic cutaneous squamous cell carcinoma in a phase 1 clinical trial, Michael R. Migden, MD, reported at the annual meeting of the American College of Mohs Surgery.
And this was no ordinary phase 1 study, he noted. Because there is no Food and Drug Administration–approved treatment for advanced cutaneous squamous cell carcinoma (CSCC), cemiplimab has been granted both Breakthrough Drug and Orphan Drug status by the FDA and the European Medicines Agency.
Given the likelihood that cemiplimab will receive expeditious regulatory approval to address this major unmet need, he offered his colleagues practical tips on its use, including information about the drug’s chief side effects as well as a heads-up regarding the importance of early recognition of the pseudoprogression phenomenon that can occur with the drug.
He predicted this fully human monoclonal antibody directed at programmed cell death protein 1 (PD-1) is going to be an important drug for Mohs surgeons.
“Immunotherapy is becoming increasingly relevant to micrographic surgery and dermatologic oncology practice and fellowship training. Care for larger, advanced CSCC falls within our scope of practice and we should play an essential role, inclusive of multidisciplinary care, in the management and follow-up of these patients,” asserted Dr. Migden, a dermatologic surgeon at the University of Texas MD Anderson Cancer Center, Houston.
The open-label, phase 1 study included seven patients with distant metastatic CSCC and nine with locally and/or regionally advanced disease. They were treated with 3 mg/kg IV cemiplimab every 2 weeks for 48 weeks, with Response Evaluation Criteria In Solid Tumors 1.1 criteria used for assessment of response status every 8 weeks. More than 80% of the tumors were located in the head and neck. The great majority of study participants had previously been treated with radiation therapy and systemic agents, to little effect.
The complete response rate at 48 weeks was 12.5%, with tumor clearance occurring as quickly as 14 weeks. Another 25% of patients had a partial response, for an overall response rate of 37.5%. But that’s not the full success story, as another 31% of patients had stable disease. Thus, 11 of 16 patients, or 69%, experienced disease control.
“A disease-control rate of nearly 70% is really important because these are patients with life-threatening tumors. To be able to hold them steady is a big deal,” Dr. Migden observed.
One-quarter of study participants experienced progressive disease. The remainder weren’t evaluated for various reasons.
The dermatologist pointed out that locally advanced disease was particularly responsive to cemiplimab, with four of nine affected patients experiencing complete or partial response, for an overall response rate of 44%. This is consistent with the preliminary results of the pivotal phase 2 study, in which the overall response rate in the 78 participants with unresectable, locally advanced CSCC was 46%.
The phase 2 trial also includes another 59 patients with metastatic CSCC on 3 mg/kg IV cemiplimab every 14 days, as well as 56 patients with metastatic disease assigned to flat-dose 350-mg IV cemiplimab every 21 days.
Treatment side effects
In the phase 1 study, immunotherapy with cemiplimab was far better tolerated than in traditional cancer chemotherapy. There were two grade 3 cases of elevated liver enzymes and one of arthralgia, but no significant fatigue or nausea and no hypothyroidism. However, judging from the cumulative experience accrued with the five PD-1 checkpoint inhibitors already approved for treatment of other cancers, one must be prepared to encounter hypothyroidism and other endocrinopathies, pneumonitis, hepatitis, and rashes.
“The clinician must have a very high index of suspicion for these immune-related adverse events and a low threshold to consult with colleagues in other specialties – pulmonary, endocrine, and medical oncology – for evaluation and management of these possible side effects. I tell all the patients who are on cemiplimab, ‘Any new anything – a slight cough, mild diarrhea – you’re coming in and you’re getting checked,’ ” according to Dr. Migden.
That being said, the majority of immune-related adverse events because of PD-1 inhibitors are mild to moderate. Of the few that reach grade 3 or above, most can be successfully managed by pausing or discontinuing anti–PD-1 therapy coupled with prompt initiation of immunosuppressive therapy, typically with high-dose steroids, he added.
Look sharp for pseudoprogression
Pseudoprogression is a phenomenon whereby immunotherapy results in inflammatory changes bringing about a temporary increase in tumor size that precedes tumor shrinkage. It’s uncommon, occurring in 3 of 16 patients in the phase 1 study. The mechanism probably involves tumor infiltration by massive numbers of activated T cells. And there is evidence from other PD-1 inhibitor studies in advanced cancers that pseudoprogression may actually be a marker for increased likelihood of survival beyond 1 year.
“Pseudoprogression is important to recognize because the patients you treat with cemiplimab can get worse before they get better,” the dermatologist explained. “So you don’t want to prematurely discontinue treatment because you’re misclassifying it as tumor progression.”
The rationale for anti-PD-1 therapy in CSCC
Tumors that express PD-1 bind to PD–ligand 1 on T cells, switching off T-cell mediated tumor destruction and thereby allowing the malignancy to thrive.
“Simplified, the strategy here is to interfere with the interaction at the T-cell off switch, either with an antibody to PD–ligand 1, such as atezolizumab [Tecentriq], or an antibody to the PD-1 receptor, where cemiplimab works. By turning off the off switch, we get a T cell fully on and attacking the tumor cell,” Dr. Migden said.
“The more the tumor mutation burden, the better immunotherapy works – and CSCC has the highest tumor mutation burden of any tumor type in the Cancer Genome Atlas, several times higher than melanoma. Interestingly, basal cell carcinoma has an even higher tumor mutation burden than CSCC, but it’s not part of the atlas,” he continued.
Although the proportion of CSCCs that are locally advanced hasn’t been well established, it’s clear that CSCC is the deadliest nonmelanoma skin cancer, accounting for 3,900-8,800 deaths annually in the United States.
The cemiplimab phase 1 and 2 clinical trials for CSCC were jointly sponsored by Regeneron and Sanofi. The monoclonal antibody is also being developed for treatment of myeloma and lung cancer. Dr. Migden reported receiving honoraria from Regeneron and Sanofi, as well as from Genentech, Lilly, Novartis, and Sun Pharmaceuticals.
REPORTING FROM THE ACMS ANNUAL MEETING
Key clinical point:
Major finding: Disease control was achieved in 11 of 16 patients (69%).
Study details: The open-label, phase 1 study included seven patients with distant metastatic cutaneous squamous cell carcinoma and nine with locally and/or regionally advanced disease.
Disclosures: The cemiplimab phase 1 and 2 clinical trials for CSCC were jointly sponsored by Regeneron and Sanofi. Dr. Migden reported receiving honoraria from Regeneron and Sanofi as well as from Genentech, Lilly, Novartis, and Sun Pharmaceuticals.
Patidegib, the first topical hedgehog inhibitor, scores in Gorlin syndrome
CHICAGO – in a phase 2 study, and did so without causing the problematic adverse events that prompt many Gorlin patients to discontinue systemic hedgehog inhibitor drugs, Ervin Epstein Jr., MD, said at the annual meeting of the American College of Mohs Surgery.
He characterized patidegib, a small-molecule cyclopamine derivative, as “a Goldilocks drug, a topical hedgehog inhibitor with percutaneous absorption that’s just right: sufficient to have anti-hedgehog and anti–basal cell carcinoma efficacy, but not enough to cause systemic exposure or systemic adverse events.”
A complete response – tumor clinical disappearance – occurred in 25% of the BCCs in the two active treatment arms. In contrast, none of the BCCs in the control group cleared. Patients on patidegib developed one or more new surgically eligible BCCs after study week 2 at a rate of 0.4 tumors per patient, markedly less than the rate of 1.4 tumors per patient in controls.
“We think that prevention is really the place to go with this drug,” said Dr. Epstein, cofounder and chief medical officer at PellePharm, the company based in Menlo Park, Calif., that is developing patidegib.
Indeed, he envisions patidegib gel as lifetime therapy for Gorlin patients.
Tumor shrinkage was significantly greater with 2% patidegib than with the 4% concentration. But so was treatment adherence: Patients in the 2% patidegib arm missed on average just 2 days of therapy over the course of 6 months, while those in the 4% arm missed 50 days. Dr. Epstein attributed this discrepancy to a freak of randomization that can occur in such a small study: 5 of 6 patients in the 2% patidegib group were women, while most in the 4% arm were men. And the men were far less adherent to treatment, possibly because men are less accustomed to applying a product on their face daily, he noted.
In any case, it’s the 2% gel formulation that is moving on to a phase 3, double-blind, randomized trial. The 150-patient U.S. and European study, scheduled to start this summer, will have as its primary endpoint the rate of new BCCs over the course of 1 year. The Food and Drug Administration has granted topical patidegib Breakthrough Drug and Orphan Drug status.
Dr. Epstein said that, in the phase 2 study, BCC shrinkage occurred only in patients whose hedgehog pathway activity decreased after 6 weeks of topical therapy as evidenced by a reduction in the GLI1 mRNA biomarker. Of note, circulating blood levels of patidegib in study participants were more than 500-fold lower than when the drug is given orally. And of greatest importance, rates of the hallmark side effects of oral hedgehog inhibitor therapy that cause so many patients to discontinue therapy – muscle cramps, taste loss, and hair loss – were no different in patients on patidegib gel than in those on placebo.
“In the randomized trial of vismodegib [Erivedge], half of patients stopped taking it within 1 year despite good results. And indeed, when they stopped taking the drug, the basal cell carcinomas returned,” the dermatologist noted.
Dr. Epstein is an employee of PellePharm, which is developing patidegib. Dermatologists with patients with Gorlin syndrome who are interested in participating in the phase 3 trial can contact him at eepstein@pellepharm.com.
CHICAGO – in a phase 2 study, and did so without causing the problematic adverse events that prompt many Gorlin patients to discontinue systemic hedgehog inhibitor drugs, Ervin Epstein Jr., MD, said at the annual meeting of the American College of Mohs Surgery.
He characterized patidegib, a small-molecule cyclopamine derivative, as “a Goldilocks drug, a topical hedgehog inhibitor with percutaneous absorption that’s just right: sufficient to have anti-hedgehog and anti–basal cell carcinoma efficacy, but not enough to cause systemic exposure or systemic adverse events.”
A complete response – tumor clinical disappearance – occurred in 25% of the BCCs in the two active treatment arms. In contrast, none of the BCCs in the control group cleared. Patients on patidegib developed one or more new surgically eligible BCCs after study week 2 at a rate of 0.4 tumors per patient, markedly less than the rate of 1.4 tumors per patient in controls.
“We think that prevention is really the place to go with this drug,” said Dr. Epstein, cofounder and chief medical officer at PellePharm, the company based in Menlo Park, Calif., that is developing patidegib.
Indeed, he envisions patidegib gel as lifetime therapy for Gorlin patients.
Tumor shrinkage was significantly greater with 2% patidegib than with the 4% concentration. But so was treatment adherence: Patients in the 2% patidegib arm missed on average just 2 days of therapy over the course of 6 months, while those in the 4% arm missed 50 days. Dr. Epstein attributed this discrepancy to a freak of randomization that can occur in such a small study: 5 of 6 patients in the 2% patidegib group were women, while most in the 4% arm were men. And the men were far less adherent to treatment, possibly because men are less accustomed to applying a product on their face daily, he noted.
In any case, it’s the 2% gel formulation that is moving on to a phase 3, double-blind, randomized trial. The 150-patient U.S. and European study, scheduled to start this summer, will have as its primary endpoint the rate of new BCCs over the course of 1 year. The Food and Drug Administration has granted topical patidegib Breakthrough Drug and Orphan Drug status.
Dr. Epstein said that, in the phase 2 study, BCC shrinkage occurred only in patients whose hedgehog pathway activity decreased after 6 weeks of topical therapy as evidenced by a reduction in the GLI1 mRNA biomarker. Of note, circulating blood levels of patidegib in study participants were more than 500-fold lower than when the drug is given orally. And of greatest importance, rates of the hallmark side effects of oral hedgehog inhibitor therapy that cause so many patients to discontinue therapy – muscle cramps, taste loss, and hair loss – were no different in patients on patidegib gel than in those on placebo.
“In the randomized trial of vismodegib [Erivedge], half of patients stopped taking it within 1 year despite good results. And indeed, when they stopped taking the drug, the basal cell carcinomas returned,” the dermatologist noted.
Dr. Epstein is an employee of PellePharm, which is developing patidegib. Dermatologists with patients with Gorlin syndrome who are interested in participating in the phase 3 trial can contact him at eepstein@pellepharm.com.
CHICAGO – in a phase 2 study, and did so without causing the problematic adverse events that prompt many Gorlin patients to discontinue systemic hedgehog inhibitor drugs, Ervin Epstein Jr., MD, said at the annual meeting of the American College of Mohs Surgery.
He characterized patidegib, a small-molecule cyclopamine derivative, as “a Goldilocks drug, a topical hedgehog inhibitor with percutaneous absorption that’s just right: sufficient to have anti-hedgehog and anti–basal cell carcinoma efficacy, but not enough to cause systemic exposure or systemic adverse events.”
A complete response – tumor clinical disappearance – occurred in 25% of the BCCs in the two active treatment arms. In contrast, none of the BCCs in the control group cleared. Patients on patidegib developed one or more new surgically eligible BCCs after study week 2 at a rate of 0.4 tumors per patient, markedly less than the rate of 1.4 tumors per patient in controls.
“We think that prevention is really the place to go with this drug,” said Dr. Epstein, cofounder and chief medical officer at PellePharm, the company based in Menlo Park, Calif., that is developing patidegib.
Indeed, he envisions patidegib gel as lifetime therapy for Gorlin patients.
Tumor shrinkage was significantly greater with 2% patidegib than with the 4% concentration. But so was treatment adherence: Patients in the 2% patidegib arm missed on average just 2 days of therapy over the course of 6 months, while those in the 4% arm missed 50 days. Dr. Epstein attributed this discrepancy to a freak of randomization that can occur in such a small study: 5 of 6 patients in the 2% patidegib group were women, while most in the 4% arm were men. And the men were far less adherent to treatment, possibly because men are less accustomed to applying a product on their face daily, he noted.
In any case, it’s the 2% gel formulation that is moving on to a phase 3, double-blind, randomized trial. The 150-patient U.S. and European study, scheduled to start this summer, will have as its primary endpoint the rate of new BCCs over the course of 1 year. The Food and Drug Administration has granted topical patidegib Breakthrough Drug and Orphan Drug status.
Dr. Epstein said that, in the phase 2 study, BCC shrinkage occurred only in patients whose hedgehog pathway activity decreased after 6 weeks of topical therapy as evidenced by a reduction in the GLI1 mRNA biomarker. Of note, circulating blood levels of patidegib in study participants were more than 500-fold lower than when the drug is given orally. And of greatest importance, rates of the hallmark side effects of oral hedgehog inhibitor therapy that cause so many patients to discontinue therapy – muscle cramps, taste loss, and hair loss – were no different in patients on patidegib gel than in those on placebo.
“In the randomized trial of vismodegib [Erivedge], half of patients stopped taking it within 1 year despite good results. And indeed, when they stopped taking the drug, the basal cell carcinomas returned,” the dermatologist noted.
Dr. Epstein is an employee of PellePharm, which is developing patidegib. Dermatologists with patients with Gorlin syndrome who are interested in participating in the phase 3 trial can contact him at eepstein@pellepharm.com.
REPORTING FROM THE ACMS ANNUAL MEETING
Mask provides effective, cheap protection from hazardous electrocautery plumes
CHICAGO – Routine use of an N95 mask during electrocautery is an effective and inexpensive way for dermatologic surgeons to protect themselves from toxic, airborne particulate matter in the smoke generated during the procedure, Emily de Golian, MD, said at the annual meeting of the American College of Mohs Surgery.
“Our data suggest clear as well as superiority to the laser masks that are used in hair removal procedures and ablative procedures in cosmetic clinics,” commented Dr. de Golian, a Mohs micrographic surgery fellow at the University of California, San Diego.
This matter of self-protection from the effects of electrocautery smoke plumes deserves greater attention from the dermatologic community, according to Dr. de Golian. There is solid evidence that these plumes contain high concentrations of known carcinogens, including benzene, acetonitrile, and butadiene – indeed, concentrations far in excess of what’s found in second-hand cigarette smoke. Moreover, many of these airborne carcinogens and other toxins have been linked to leukemia, neurologic disorders, lung cancer, thrombotic disorders, lung disease, and infectious disease transmission, albeit not convincingly so to date in dermatologic surgeons. But why wait for definitive evidence to accrue?
“In light of these hazards – and according to governmental guidelines – dermatologic surgeons would be wise to adopt protective measures during surgical procedures,” Dr. de Golian said.
But they haven’t. She cited a national survey conducted several years ago by a colleague in which 79% of the 316 responding dermatologic surgeons indicated they use no smoke management whatsoever, neither masks nor a local exhaust evacuation system. Only 10% employed smoke management 25%-50% of the time during electrocautery, and a scant 11% of dermatologic surgeons did so at least 75% of the time (Dermatol Surg. 2014 Dec;40[12]:1373-7).
Given the far more substantial expense of installing an office smoke evacuation system, mask filtration becomes an attractive alternative. But the relative efficacy of the various types of masks in blocking fine and ultrafine particulate matter contained in electrocautery plumes hadn’t previously been systematically studied. This created the impetus for Dr. de Golian’s study.
The N95 masks were the clear winner, particularly when it came to filtering the ultrafine particles, which are of greatest concern because they remain suspended in air longer and penetrate deeper into the respiratory tract than larger particles. The N95 masks proved superior to procedural masks, which in turn were significantly more effective than the laser masks. The differences between mask performance for larger particle filtration were smaller, although the N95 remained number one. She noted that the study results probably underestimate the true filtration efficacy of N95 masks, since they form a tighter seal with the face in clinical practice than with the other two mask types.
Mask self-protection “is easily applicable in your own practice, and it meets NIOSH-recommended [National Institute for Occupational Safety and Health] standards for safety in the workplace,” the dermatologist noted.
In the next phase of her research, she plans to evaluate the optimal technology and techniques of smoke evacuation in the surgical suite. That’s an attractive method because it protects everyone in the room, not just the surgeon. And while the practitioner survey indicates this technology isn’t widely used by dermatologic surgeons on a routine basis at present, that could change, particularly in the current era in which patient-reported outcomes and satisfaction surveys have taken on added weight.
“Patients prefer not smelling their own tissue burning,” Dr. de Golian said.
She reported no financial conflicts regarding her study, which was conducted free of commercial support.
CHICAGO – Routine use of an N95 mask during electrocautery is an effective and inexpensive way for dermatologic surgeons to protect themselves from toxic, airborne particulate matter in the smoke generated during the procedure, Emily de Golian, MD, said at the annual meeting of the American College of Mohs Surgery.
“Our data suggest clear as well as superiority to the laser masks that are used in hair removal procedures and ablative procedures in cosmetic clinics,” commented Dr. de Golian, a Mohs micrographic surgery fellow at the University of California, San Diego.
This matter of self-protection from the effects of electrocautery smoke plumes deserves greater attention from the dermatologic community, according to Dr. de Golian. There is solid evidence that these plumes contain high concentrations of known carcinogens, including benzene, acetonitrile, and butadiene – indeed, concentrations far in excess of what’s found in second-hand cigarette smoke. Moreover, many of these airborne carcinogens and other toxins have been linked to leukemia, neurologic disorders, lung cancer, thrombotic disorders, lung disease, and infectious disease transmission, albeit not convincingly so to date in dermatologic surgeons. But why wait for definitive evidence to accrue?
“In light of these hazards – and according to governmental guidelines – dermatologic surgeons would be wise to adopt protective measures during surgical procedures,” Dr. de Golian said.
But they haven’t. She cited a national survey conducted several years ago by a colleague in which 79% of the 316 responding dermatologic surgeons indicated they use no smoke management whatsoever, neither masks nor a local exhaust evacuation system. Only 10% employed smoke management 25%-50% of the time during electrocautery, and a scant 11% of dermatologic surgeons did so at least 75% of the time (Dermatol Surg. 2014 Dec;40[12]:1373-7).
Given the far more substantial expense of installing an office smoke evacuation system, mask filtration becomes an attractive alternative. But the relative efficacy of the various types of masks in blocking fine and ultrafine particulate matter contained in electrocautery plumes hadn’t previously been systematically studied. This created the impetus for Dr. de Golian’s study.
The N95 masks were the clear winner, particularly when it came to filtering the ultrafine particles, which are of greatest concern because they remain suspended in air longer and penetrate deeper into the respiratory tract than larger particles. The N95 masks proved superior to procedural masks, which in turn were significantly more effective than the laser masks. The differences between mask performance for larger particle filtration were smaller, although the N95 remained number one. She noted that the study results probably underestimate the true filtration efficacy of N95 masks, since they form a tighter seal with the face in clinical practice than with the other two mask types.
Mask self-protection “is easily applicable in your own practice, and it meets NIOSH-recommended [National Institute for Occupational Safety and Health] standards for safety in the workplace,” the dermatologist noted.
In the next phase of her research, she plans to evaluate the optimal technology and techniques of smoke evacuation in the surgical suite. That’s an attractive method because it protects everyone in the room, not just the surgeon. And while the practitioner survey indicates this technology isn’t widely used by dermatologic surgeons on a routine basis at present, that could change, particularly in the current era in which patient-reported outcomes and satisfaction surveys have taken on added weight.
“Patients prefer not smelling their own tissue burning,” Dr. de Golian said.
She reported no financial conflicts regarding her study, which was conducted free of commercial support.
CHICAGO – Routine use of an N95 mask during electrocautery is an effective and inexpensive way for dermatologic surgeons to protect themselves from toxic, airborne particulate matter in the smoke generated during the procedure, Emily de Golian, MD, said at the annual meeting of the American College of Mohs Surgery.
“Our data suggest clear as well as superiority to the laser masks that are used in hair removal procedures and ablative procedures in cosmetic clinics,” commented Dr. de Golian, a Mohs micrographic surgery fellow at the University of California, San Diego.
This matter of self-protection from the effects of electrocautery smoke plumes deserves greater attention from the dermatologic community, according to Dr. de Golian. There is solid evidence that these plumes contain high concentrations of known carcinogens, including benzene, acetonitrile, and butadiene – indeed, concentrations far in excess of what’s found in second-hand cigarette smoke. Moreover, many of these airborne carcinogens and other toxins have been linked to leukemia, neurologic disorders, lung cancer, thrombotic disorders, lung disease, and infectious disease transmission, albeit not convincingly so to date in dermatologic surgeons. But why wait for definitive evidence to accrue?
“In light of these hazards – and according to governmental guidelines – dermatologic surgeons would be wise to adopt protective measures during surgical procedures,” Dr. de Golian said.
But they haven’t. She cited a national survey conducted several years ago by a colleague in which 79% of the 316 responding dermatologic surgeons indicated they use no smoke management whatsoever, neither masks nor a local exhaust evacuation system. Only 10% employed smoke management 25%-50% of the time during electrocautery, and a scant 11% of dermatologic surgeons did so at least 75% of the time (Dermatol Surg. 2014 Dec;40[12]:1373-7).
Given the far more substantial expense of installing an office smoke evacuation system, mask filtration becomes an attractive alternative. But the relative efficacy of the various types of masks in blocking fine and ultrafine particulate matter contained in electrocautery plumes hadn’t previously been systematically studied. This created the impetus for Dr. de Golian’s study.
The N95 masks were the clear winner, particularly when it came to filtering the ultrafine particles, which are of greatest concern because they remain suspended in air longer and penetrate deeper into the respiratory tract than larger particles. The N95 masks proved superior to procedural masks, which in turn were significantly more effective than the laser masks. The differences between mask performance for larger particle filtration were smaller, although the N95 remained number one. She noted that the study results probably underestimate the true filtration efficacy of N95 masks, since they form a tighter seal with the face in clinical practice than with the other two mask types.
Mask self-protection “is easily applicable in your own practice, and it meets NIOSH-recommended [National Institute for Occupational Safety and Health] standards for safety in the workplace,” the dermatologist noted.
In the next phase of her research, she plans to evaluate the optimal technology and techniques of smoke evacuation in the surgical suite. That’s an attractive method because it protects everyone in the room, not just the surgeon. And while the practitioner survey indicates this technology isn’t widely used by dermatologic surgeons on a routine basis at present, that could change, particularly in the current era in which patient-reported outcomes and satisfaction surveys have taken on added weight.
“Patients prefer not smelling their own tissue burning,” Dr. de Golian said.
She reported no financial conflicts regarding her study, which was conducted free of commercial support.
REPORTING FROM THE ACMS ANNUAL MEETING
Key clinical point: Electrocautery smoke is bad news, and wearing an N95 mask affords protection.
Major finding: The N95 mask was significantly more effective than basic procedural or laser masks at filtering particulate matter less than 1 mcm in size contained in electrocautery smoke.
Study details: This study utilized highly sensitive airborne particle counting devices to assess the relative protective filtration afforded by three types of masks.
Disclosures: The presenter reported no financial conflicts regarding this study, which was conducted free of commercial support.
Metastatic Meningioma of the Scalp
Meningiomas generally present as slow-growing, expanding intracranial lesions and are the most common benign intracranial tumor in adults.1 Rarely, meningioma exhibits malignant potential and presents as an extracranial soft-tissue mass through extension or as a primary extracranial cutaneous neoplasm. The differential diagnosis of scalp neoplasms must be broadened to include uncommon tumors such as meningioma. We present a rare case of a 68-year-old woman with scalp metastasis of meningioma 11 years after initial resection of the primary tumor.
Case Report
A 68-year-old woman presented for evaluation of an asymptomatic nodule on the left parietal scalp of 2 years’ duration. She denied any headaches, difficulty with balance, vision changes, or changes in mentation. Her medical history was remarkable for a benign meningioma removed from the right parietal scalp 11 years prior without radiation therapy, as well as type 2 diabetes mellitus and arthritis. The patient’s son died from a brain tumor, but the exact tumor type and age at the time of death were unknown. Her current medications included metformin, insulin glargine, aspirin, and a daily multivitamin. She denied any allergies or history of smoking.
Physical examination of the scalp revealed 4 fixed, nontender, flesh-colored nodules: 2 on the left parietal scalp measuring 3.0 cm and 0.8 cm, respectively (Figure 1A); a 0.4-cm nodule on the right posterior occipital scalp; and a 1.6-cm sausage-shaped nodule on the right temple (Figure 1B). No positive lymph nodes were appreciated, and no additional lesions were noted. No additional atypical lesions were noted on full cutaneous examination.
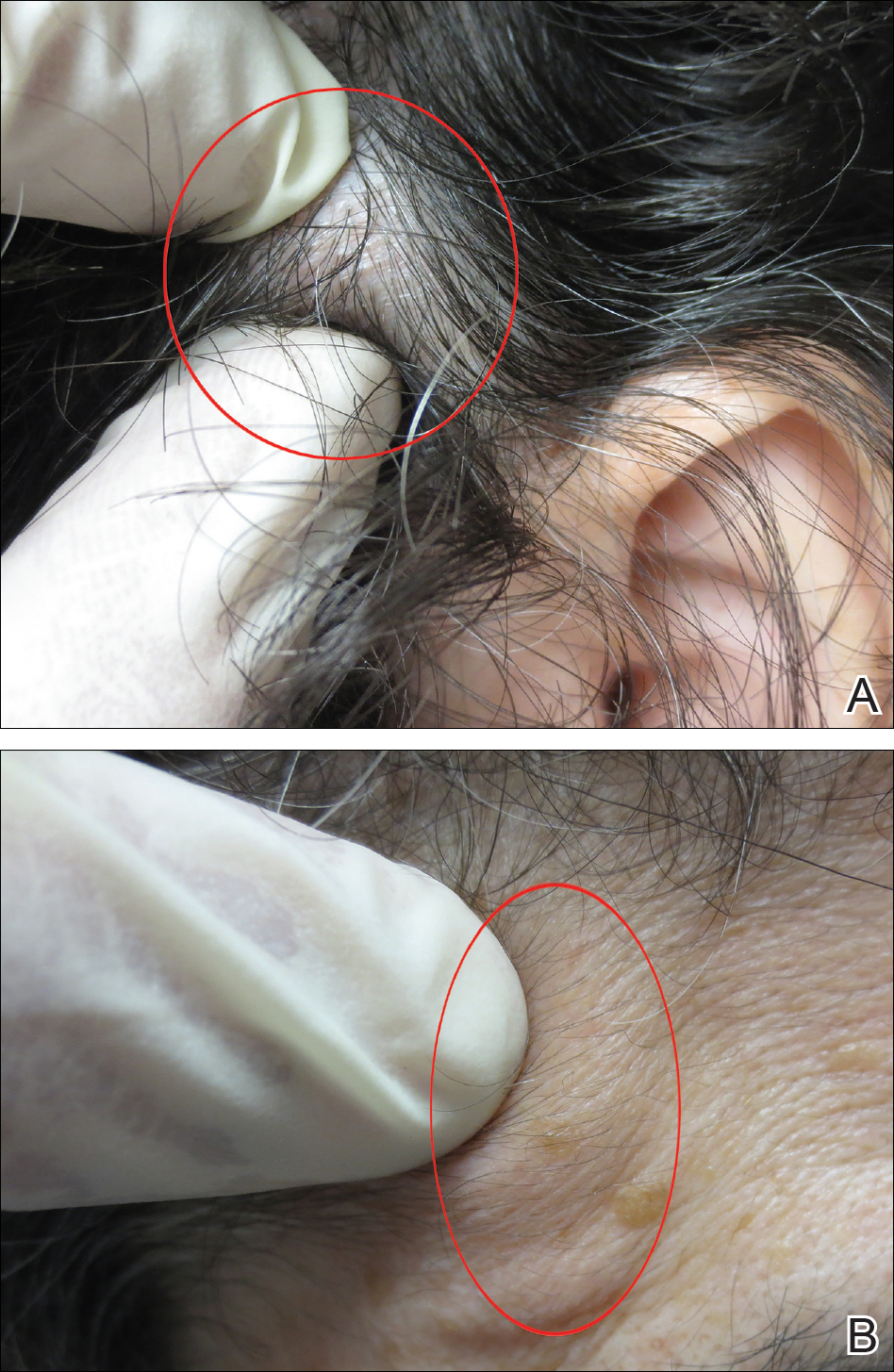
A diagnostic 6-mm punch biopsy of the largest nodule was performed. Intraoperatively, there was no apparent cyst wall, but coiled, loose, stringlike, pink-yellow tissue was removed from the base of the wound before closing with sutures.
The primary histologic finding was cells within fibrous tissue containing delicate round-oval nuclei, inconspicuous nucleoli, and lightly eosinophilic cytoplasm with an indistinct border (Figure 2). Immunohistochemical studies for S100 protein were focal and limited to the cytoplasm of a subset of neoplastic cells (Figure 3). Tumor cells stained positive for epithelial membrane antigen (EMA) and were focally positive for progesterone receptor (Figure 4). Tumor cells were negative for CD31 and CD34. Based on the clinical and histologic findings, a diagnosis of metastatic meningioma of the scalp was made.
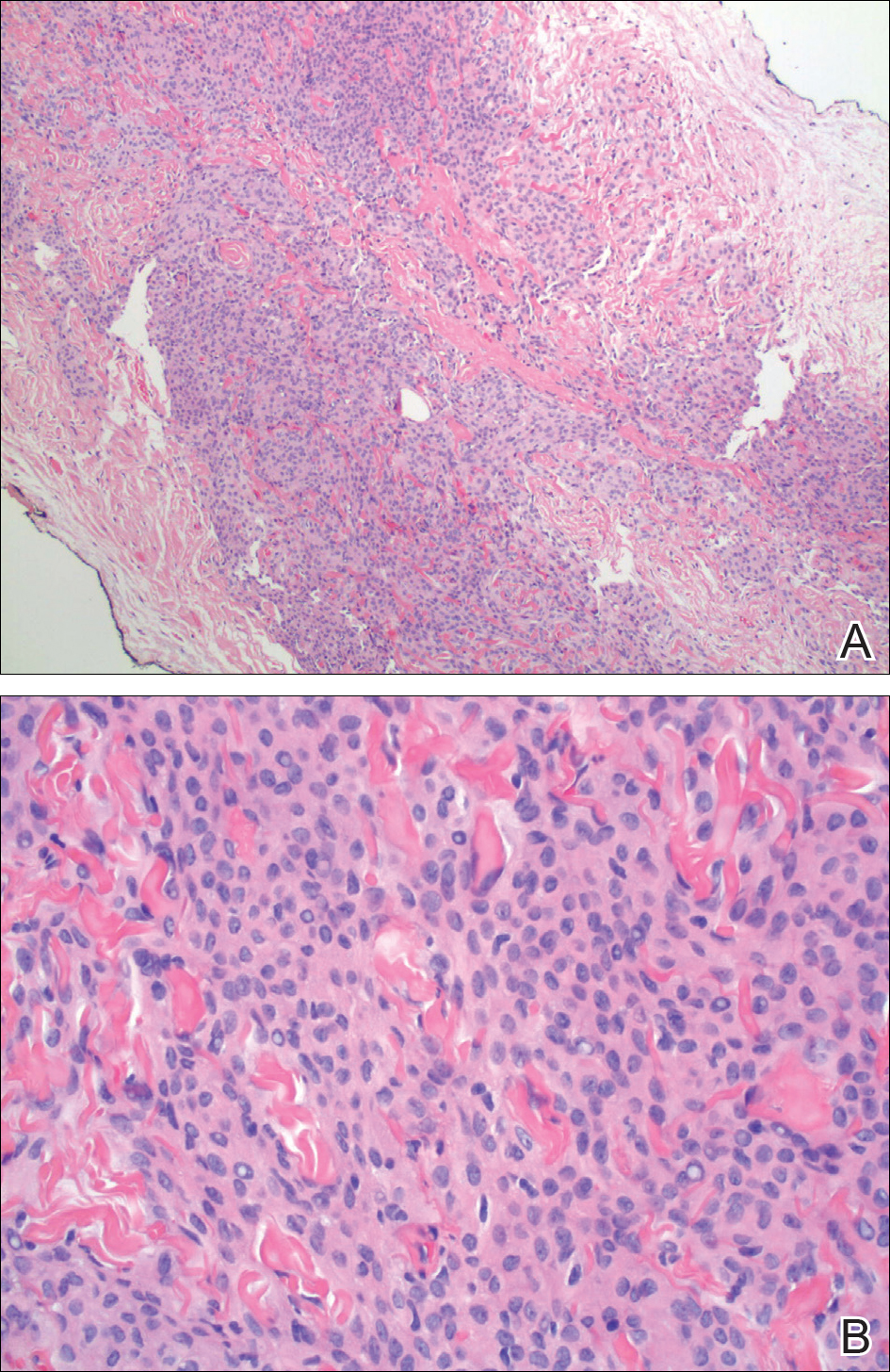
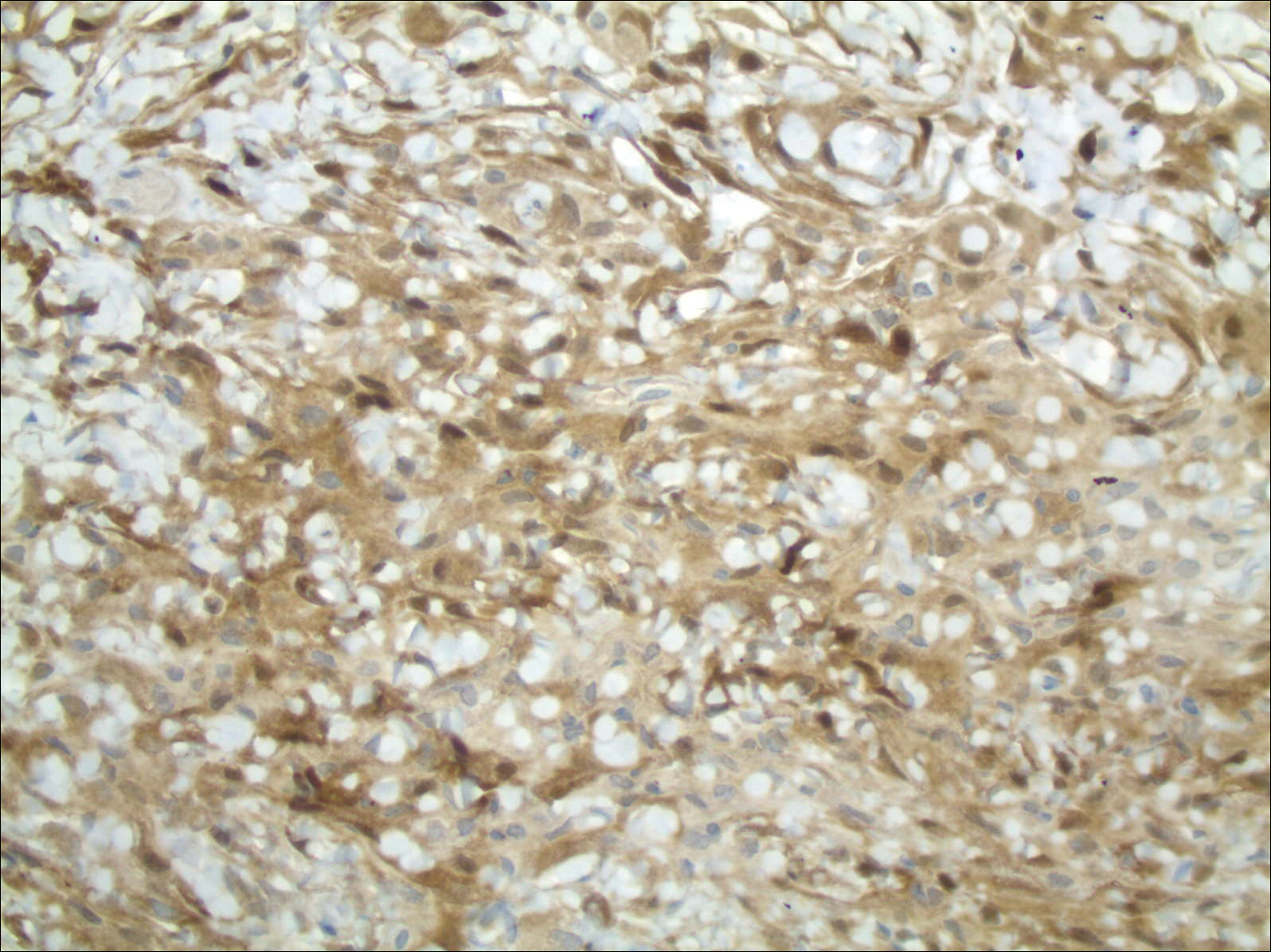
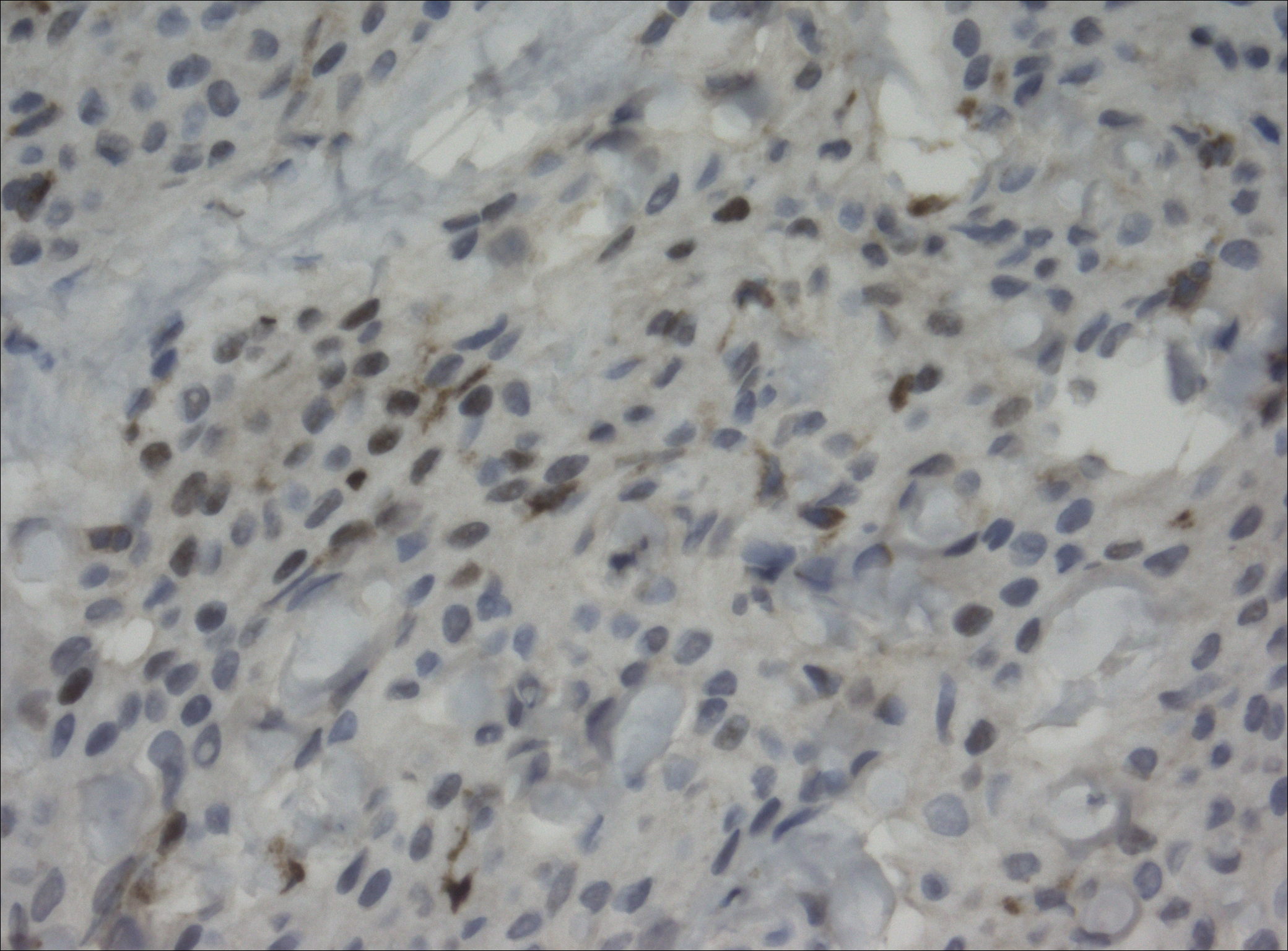
Magnetic resonance imaging and positron emission tomography of the head, neck, and chest demonstrated 3 residual subcutaneous nodules on the scalp and an indeterminate subcentimeter nodule in the right lung. The 0.4-cm nodule on the right posterior occipital scalp was removed without complication, and no radiation therapy was administered. The rest of the lesions were monitored. She remained under the close observation of a neurosurgeon and underwent repeat imaging of the scalp nodules and lungs, initially at 3 months and then routinely at the patient’s comfort. The patient currently denies any neurologic symptoms.
Comment
Meningiomas are derived from meningothelial cells found in the leptomeninges and in the choroid plexus of the ventricles of the brain.2 They are common intracranial neoplasms that generally are associated with a benign course and present during the fourth to sixth decades of life. Meningiomas constitute 13% to 30% of intracranial neoplasms and usually are female predominant (3:1).3,4 Rarely, malignant transformation can lead to local and distant metastasis to the lungs,5,6 liver,7 and skeletal system.8 In cases of metastatic spread, there is an increased incidence in males versus females.9-11
Risk Factors
Although many meningiomas are sporadic, numerous risk factors have been associated with the disease development. One study showed a link between exposure to ionizing radiation and subsequent development of meningioma.12 Another study found a population link between a higher incidence of meningioma and nuclear exposure in Hiroshima, Japan, after the atomic bomb blast in 1980.13 There is an increased incidence of meningioma in patients exposed to radiography from frequent dental imaging, particularly when older machines with higher levels of radiation exposure are used.14Another study demonstrated a correlation between meningioma and hormonal factors (eg, estrogen for hormone therapy) and exacerbation of symptoms during pregnancy.15 There also is an increased incidence of meningioma in breast cancer patients.4 Genetic alterations also have been implicated in the development of meningioma. It was found that 50% of patients with a mutation in the neurofibromatosis 2 gene (which codes for the merlin protein) had associated meningiomas.16,17 Scalp nodules in patients with neurofibromatosis type 2 increases suspicion of a scalp meningioma and necessitates biopsy.
Clinical Presentation
Cutaneous meningiomas typically present as firm, subcutaneous nodules. Scalp nodules ranging from alopecia18,19 to hypertrichosis20 have been reported. These neoplasms can be painless or painful, depending on mass effect and location.
Classification
The primary clinical classification system of metastatic meningioma was first described in 1974.21 Type 1 meningioma refers to congenital lesions that tend to cluster closer to the midline. Type 2 refers to ectopic soft-tissue lesions that extend to the skin from likely remnants of arachnoid cells. These lesions are more likely to be found around the eyes, ears, nose, and mouth. Type 3 meningiomas extend from intracranial tumors that secondarily involve the skin through proliferation through bone or anatomic defects. Type 3 is the result of direct extension and the location of the cutaneous presentation depends on the location of the intracranial lesion.4,22,23
Pathology
Meningiomas exhibit a range of morphologic appearances on histopathology. In almost all meningiomas, tumor cells are concentrically wrapped in tight whorls with round-oval nuclei and delicate chromatin, central clearing, and pale pseudonuclear inclusions. Lamellate calcifications known as psammoma bodies are a common finding. Immunohistochemical studies show that most meningiomas are positive for EMA, vimentin, and progesterone receptor. S100 protein expression, if present, usually is focal.
Differential Diagnosis
Asymptomatic nodules on the scalp may present a diagnostic challenge to physicians. Most common scalp lesions tend to be cystic or lipomatous. In children, a broad differential diagnosis should be considered, including dermoid and epidermoid tumors, dermal sinus tumors, hemangiomas, metastasis of another tumor, aplasia cutis congenita, pilomatricoma, and lipoma. In adults, the differential should focus on epidermoid cysts, lipomas, metastasis of other tumors, osteomas, arteriovenous fistulae, and heterotopic brain tissue. Often, microscopic examination is necessary, along with additional immunohistochemical staining (eg, EMA, vimentin).
Treatment
Treatment options for meningioma include observation, surgical resection, radiotherapy, and systemic therapy, as well as a combination of these modalities. The choice of therapy depends on such variables as patient age; performance status; comorbidities; presence or absence of symptoms (including focal neurologic deficits); and tumor location, size, and grade. It is important to note that there is limited knowledge looking at the results of various treatment modalities, and no consensus approach has been established.
Conclusion
Our patient’s medical history was remarkable for an intracranial meningioma 11 years prior to the current presentation, and she was found to have biopsy-proven metastatic meningioma without recurrence of the initial tumor. Patients presenting with a scalp nodule warrant a thorough medical history and consideration beyond common cysts and lipomas.
- Mackay B, Bruner JM, Luna MA. Malignant meningioma of the scalp. Ultrastruc Pathol. 1994;18:235-240.
- Whittle IR, Smith C, Navoo P, et al. Meningiomas. Lancet. 2004;363:1535-1543.
- Bauman G, Fisher B, Schild S, et al. Meningioma, ependymoma, and other adult brain tumors. In: Gunderson LL, Tepper JE, eds. Clinical Radiation Oncology. Philadelphia, PA: Elsevier Churchill Livingstone; 2007:539-566.
- Claus EB, Bondy ML, Schildkraut JM, et al. Epidemiology of intracranial meningioma. Neurosurgery. 2005;57:1088-1095.
- Tworek JA, Mikhail AA, Blaivas M. Meningioma: local recurrence and pulmonary metastasis diagnosed by fine needle aspiration. Acta Cytol. 1997;41:946-947.
- Shin MS, Holman WL, Herrera GA, et al. Extensive pulmonary metastasis of an intracranial meningioma with repeated recurrence: radiographic and pathologic features. South Med J. 1996;89:313-318.
- Ferguson JM, Flinn J. Intracranial meningioma with hepatic metastases and hypoglycaemia treated by selective hepatic arterial chemo-embolization. Australas Radiol.1995;39:97-99.
- Palmer JD, Cook PL, Ellison DW. Extracranial osseous metastases from intracranial meningioma. Br J Neurosurg. 1994;8:215-218.
- Glasauer FE, Yuan RH. Intracranial tumours with extracranial metastases. case report and review of the literature. J Neurosurg. 1963;20:474-493.
- Shuangshoti S, Hongsaprabhas C, Netsky MG. Metastasizing meningioma. Cancer. 1970;26:832-841.
- Ohta M, Iwaki T, Kitamoto T, et al. MIB-1 staining index and scoring of histological features in meningioma. Cancer. 1994;74:3176-3189.
- Wrensch M, Minn Y, Chew T, et al. Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro Oncol. 2002;4:278-299.
- Shintani T, Hayakawa N, Hoshi M, et al. High incidence of meningioma among Hiroshima atomic bomb survivors. J Rad Res. 1999;40:49-57.
- Claus EB, Calvocoressi L, Bondy ML, et al. Dental x-rays and risk of meningioma. Cancer. 2012;118:4530-4537.
- Blitshteyn S, Crook JE, Jaeckle KA. Is there an association between meningioma and hormone replacement therapy? J Clin Oncol. 2008;26:279-282.
- Fontaine B, Rouleau GA, Seizinger BR, et al. Molecular genetics of neurofibromatosis 2 and related tumors (acoustic neuromas and meningioma). Ann N Y Acad Sci. 1991;615:338-343.
- Rabin BM, Meyer JR, Berlin JW, et al. Radiation-induced changes of the central nervous system and head and neck. Radiographics. 1996;16:1055-1072.
- Tanaka S, Okazaki M, Egusa G, et al. A case of pheochromocytoma associated with meningioma. J Intern Med. 1991;229:371-373.
- Zeikus P, Robinson-Bostom L, Stopa E. Primary cutaneous meningioma in association with a sinus pericranii. J Am Acad Dermatol. 2006;54(2 suppl):S49-S50.
- Junaid TA, Nkposong EO, Kolawole TM. Cutaneous meningiomas and an ovarian fibroma in a three-year-old girl. J Pathol. 1972;108:165-167.
- Lopez DA, Silvers DN, Helwig EB. Cutaneous meningioma—a clinicopathologic study. Cancer. 1974;34:728-744.
- Shuangshoti S, Boonjunwetwat D, Kaoroptham S. Association of primary intraspinal meningiomas and subcutaneous meningioma of the cervical region: case report and review of literature. Surg Neurol. 1992;38:129-134.
- Miedema JR, Zedek D. Cutaneous meningioma. Arch Pathol. 2012;136:208-211.
Meningiomas generally present as slow-growing, expanding intracranial lesions and are the most common benign intracranial tumor in adults.1 Rarely, meningioma exhibits malignant potential and presents as an extracranial soft-tissue mass through extension or as a primary extracranial cutaneous neoplasm. The differential diagnosis of scalp neoplasms must be broadened to include uncommon tumors such as meningioma. We present a rare case of a 68-year-old woman with scalp metastasis of meningioma 11 years after initial resection of the primary tumor.
Case Report
A 68-year-old woman presented for evaluation of an asymptomatic nodule on the left parietal scalp of 2 years’ duration. She denied any headaches, difficulty with balance, vision changes, or changes in mentation. Her medical history was remarkable for a benign meningioma removed from the right parietal scalp 11 years prior without radiation therapy, as well as type 2 diabetes mellitus and arthritis. The patient’s son died from a brain tumor, but the exact tumor type and age at the time of death were unknown. Her current medications included metformin, insulin glargine, aspirin, and a daily multivitamin. She denied any allergies or history of smoking.
Physical examination of the scalp revealed 4 fixed, nontender, flesh-colored nodules: 2 on the left parietal scalp measuring 3.0 cm and 0.8 cm, respectively (Figure 1A); a 0.4-cm nodule on the right posterior occipital scalp; and a 1.6-cm sausage-shaped nodule on the right temple (Figure 1B). No positive lymph nodes were appreciated, and no additional lesions were noted. No additional atypical lesions were noted on full cutaneous examination.
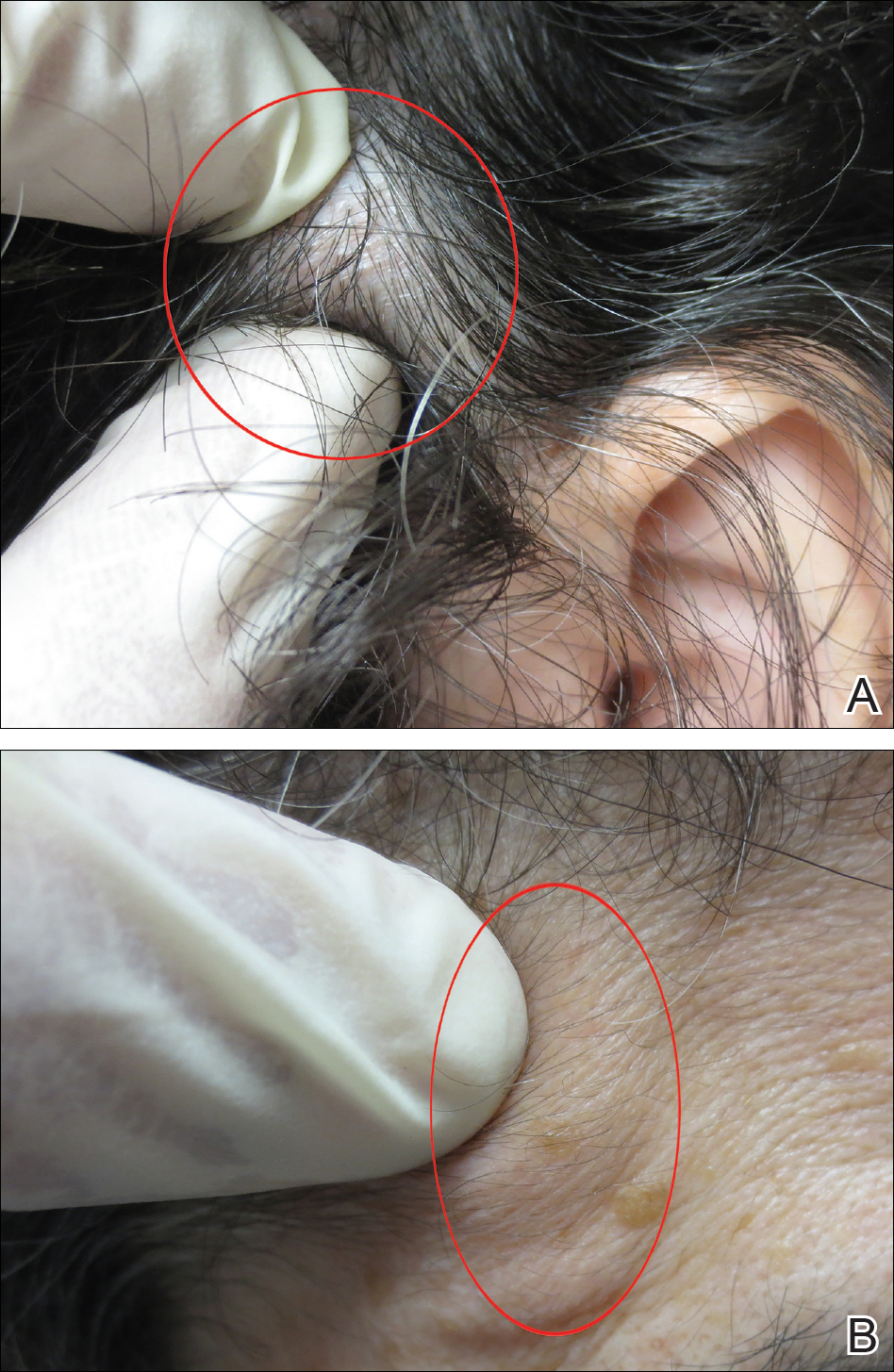
A diagnostic 6-mm punch biopsy of the largest nodule was performed. Intraoperatively, there was no apparent cyst wall, but coiled, loose, stringlike, pink-yellow tissue was removed from the base of the wound before closing with sutures.
The primary histologic finding was cells within fibrous tissue containing delicate round-oval nuclei, inconspicuous nucleoli, and lightly eosinophilic cytoplasm with an indistinct border (Figure 2). Immunohistochemical studies for S100 protein were focal and limited to the cytoplasm of a subset of neoplastic cells (Figure 3). Tumor cells stained positive for epithelial membrane antigen (EMA) and were focally positive for progesterone receptor (Figure 4). Tumor cells were negative for CD31 and CD34. Based on the clinical and histologic findings, a diagnosis of metastatic meningioma of the scalp was made.
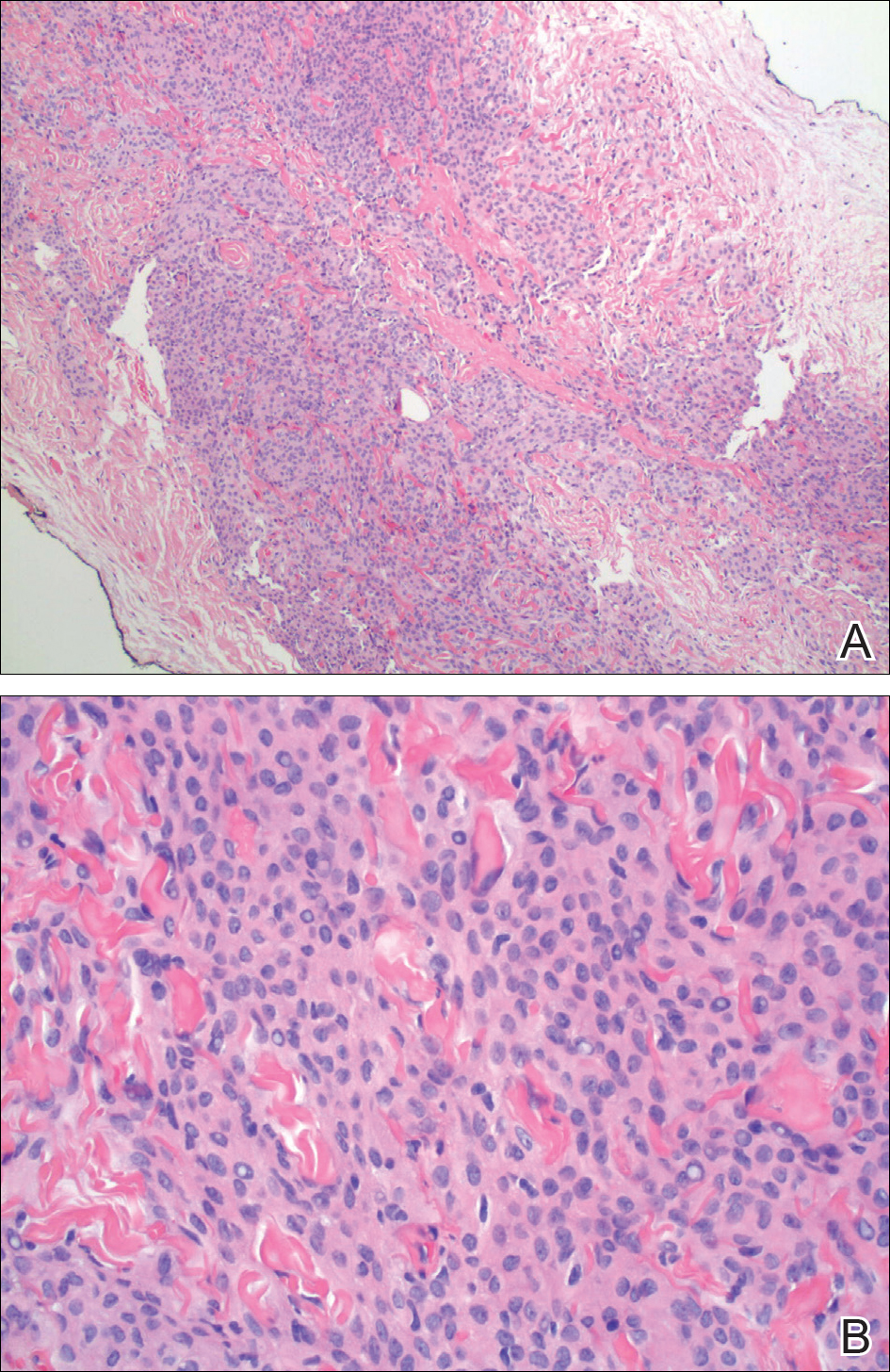
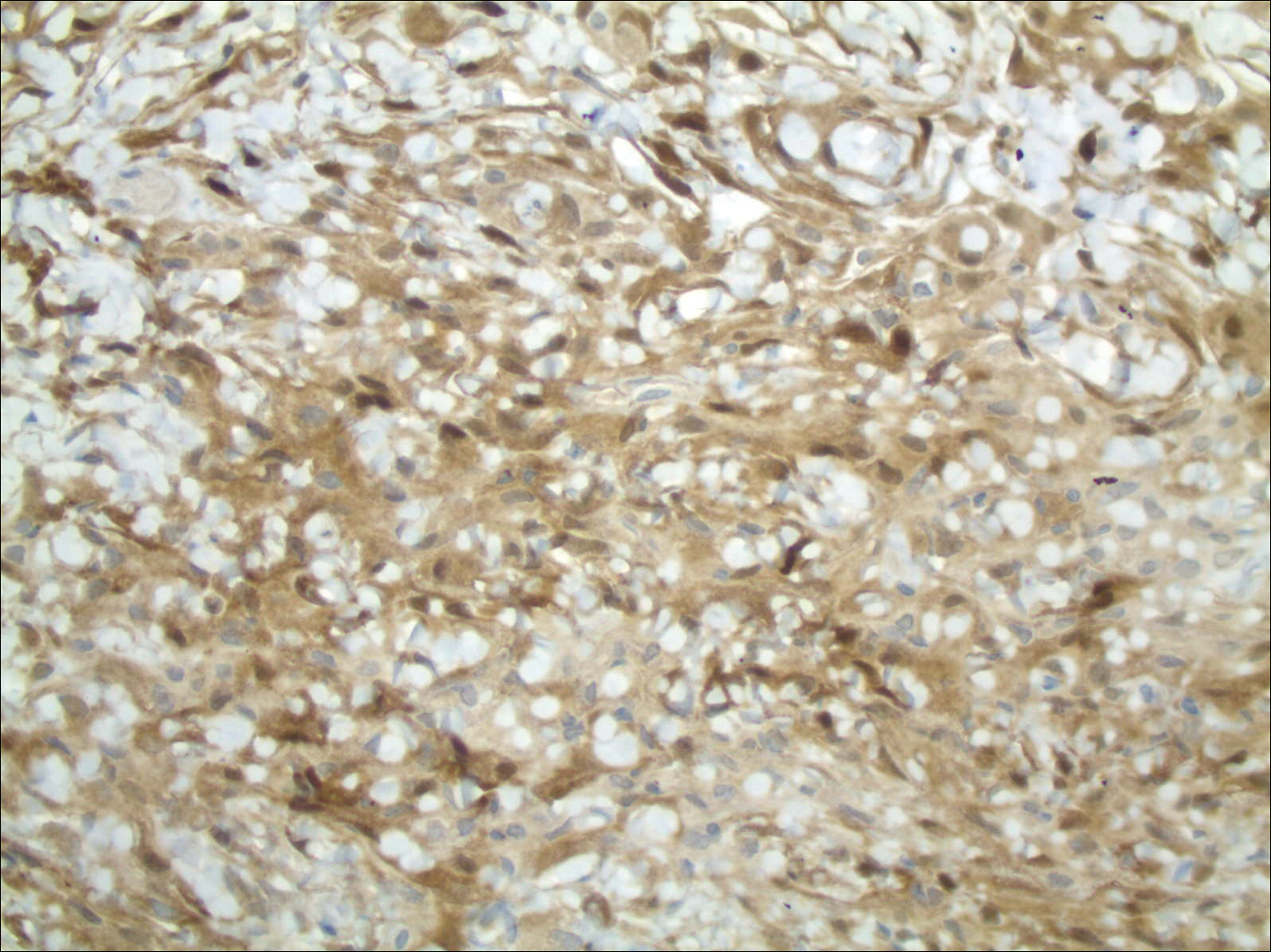
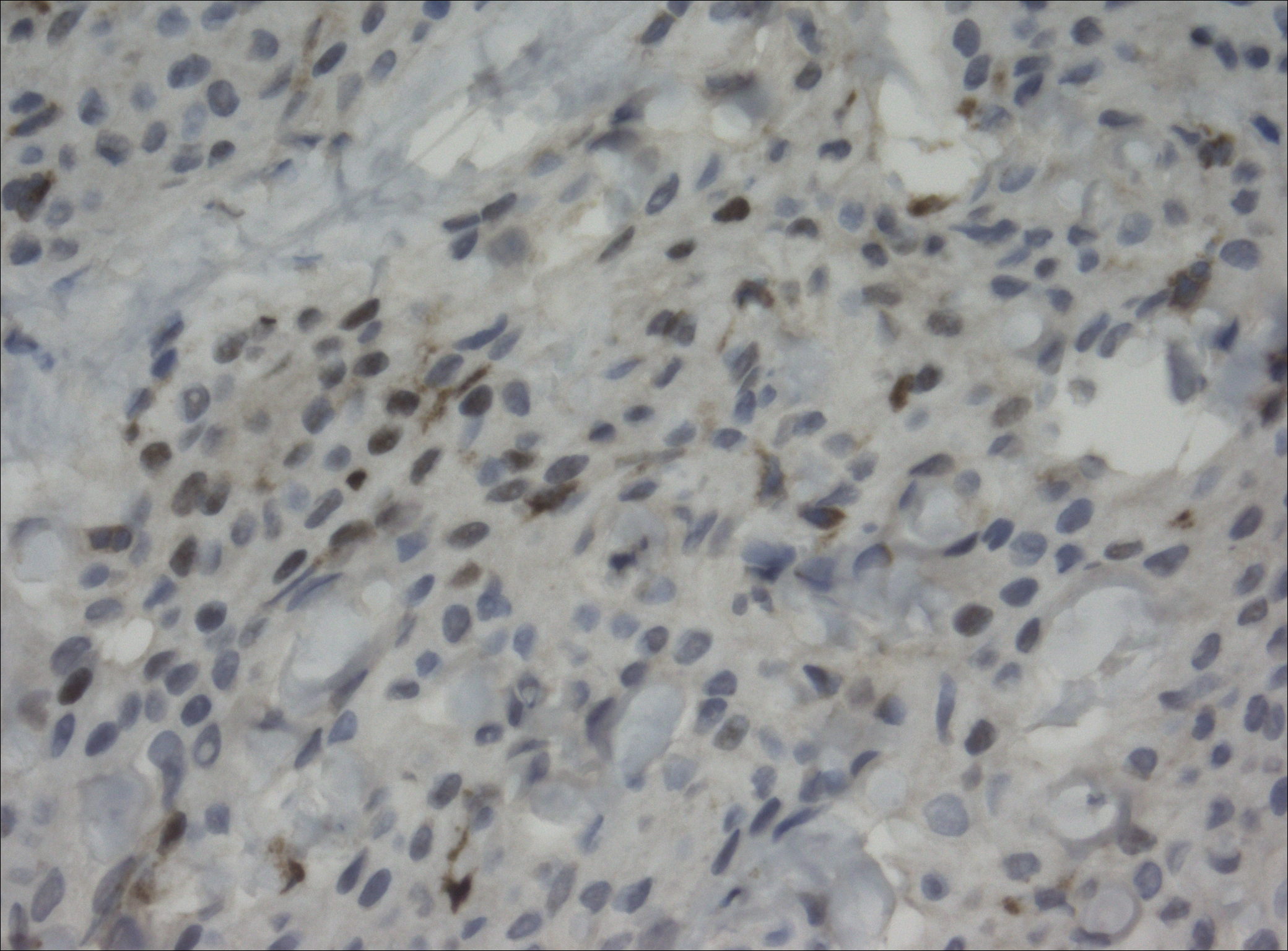
Magnetic resonance imaging and positron emission tomography of the head, neck, and chest demonstrated 3 residual subcutaneous nodules on the scalp and an indeterminate subcentimeter nodule in the right lung. The 0.4-cm nodule on the right posterior occipital scalp was removed without complication, and no radiation therapy was administered. The rest of the lesions were monitored. She remained under the close observation of a neurosurgeon and underwent repeat imaging of the scalp nodules and lungs, initially at 3 months and then routinely at the patient’s comfort. The patient currently denies any neurologic symptoms.
Comment
Meningiomas are derived from meningothelial cells found in the leptomeninges and in the choroid plexus of the ventricles of the brain.2 They are common intracranial neoplasms that generally are associated with a benign course and present during the fourth to sixth decades of life. Meningiomas constitute 13% to 30% of intracranial neoplasms and usually are female predominant (3:1).3,4 Rarely, malignant transformation can lead to local and distant metastasis to the lungs,5,6 liver,7 and skeletal system.8 In cases of metastatic spread, there is an increased incidence in males versus females.9-11
Risk Factors
Although many meningiomas are sporadic, numerous risk factors have been associated with the disease development. One study showed a link between exposure to ionizing radiation and subsequent development of meningioma.12 Another study found a population link between a higher incidence of meningioma and nuclear exposure in Hiroshima, Japan, after the atomic bomb blast in 1980.13 There is an increased incidence of meningioma in patients exposed to radiography from frequent dental imaging, particularly when older machines with higher levels of radiation exposure are used.14Another study demonstrated a correlation between meningioma and hormonal factors (eg, estrogen for hormone therapy) and exacerbation of symptoms during pregnancy.15 There also is an increased incidence of meningioma in breast cancer patients.4 Genetic alterations also have been implicated in the development of meningioma. It was found that 50% of patients with a mutation in the neurofibromatosis 2 gene (which codes for the merlin protein) had associated meningiomas.16,17 Scalp nodules in patients with neurofibromatosis type 2 increases suspicion of a scalp meningioma and necessitates biopsy.
Clinical Presentation
Cutaneous meningiomas typically present as firm, subcutaneous nodules. Scalp nodules ranging from alopecia18,19 to hypertrichosis20 have been reported. These neoplasms can be painless or painful, depending on mass effect and location.
Classification
The primary clinical classification system of metastatic meningioma was first described in 1974.21 Type 1 meningioma refers to congenital lesions that tend to cluster closer to the midline. Type 2 refers to ectopic soft-tissue lesions that extend to the skin from likely remnants of arachnoid cells. These lesions are more likely to be found around the eyes, ears, nose, and mouth. Type 3 meningiomas extend from intracranial tumors that secondarily involve the skin through proliferation through bone or anatomic defects. Type 3 is the result of direct extension and the location of the cutaneous presentation depends on the location of the intracranial lesion.4,22,23
Pathology
Meningiomas exhibit a range of morphologic appearances on histopathology. In almost all meningiomas, tumor cells are concentrically wrapped in tight whorls with round-oval nuclei and delicate chromatin, central clearing, and pale pseudonuclear inclusions. Lamellate calcifications known as psammoma bodies are a common finding. Immunohistochemical studies show that most meningiomas are positive for EMA, vimentin, and progesterone receptor. S100 protein expression, if present, usually is focal.
Differential Diagnosis
Asymptomatic nodules on the scalp may present a diagnostic challenge to physicians. Most common scalp lesions tend to be cystic or lipomatous. In children, a broad differential diagnosis should be considered, including dermoid and epidermoid tumors, dermal sinus tumors, hemangiomas, metastasis of another tumor, aplasia cutis congenita, pilomatricoma, and lipoma. In adults, the differential should focus on epidermoid cysts, lipomas, metastasis of other tumors, osteomas, arteriovenous fistulae, and heterotopic brain tissue. Often, microscopic examination is necessary, along with additional immunohistochemical staining (eg, EMA, vimentin).
Treatment
Treatment options for meningioma include observation, surgical resection, radiotherapy, and systemic therapy, as well as a combination of these modalities. The choice of therapy depends on such variables as patient age; performance status; comorbidities; presence or absence of symptoms (including focal neurologic deficits); and tumor location, size, and grade. It is important to note that there is limited knowledge looking at the results of various treatment modalities, and no consensus approach has been established.
Conclusion
Our patient’s medical history was remarkable for an intracranial meningioma 11 years prior to the current presentation, and she was found to have biopsy-proven metastatic meningioma without recurrence of the initial tumor. Patients presenting with a scalp nodule warrant a thorough medical history and consideration beyond common cysts and lipomas.
Meningiomas generally present as slow-growing, expanding intracranial lesions and are the most common benign intracranial tumor in adults.1 Rarely, meningioma exhibits malignant potential and presents as an extracranial soft-tissue mass through extension or as a primary extracranial cutaneous neoplasm. The differential diagnosis of scalp neoplasms must be broadened to include uncommon tumors such as meningioma. We present a rare case of a 68-year-old woman with scalp metastasis of meningioma 11 years after initial resection of the primary tumor.
Case Report
A 68-year-old woman presented for evaluation of an asymptomatic nodule on the left parietal scalp of 2 years’ duration. She denied any headaches, difficulty with balance, vision changes, or changes in mentation. Her medical history was remarkable for a benign meningioma removed from the right parietal scalp 11 years prior without radiation therapy, as well as type 2 diabetes mellitus and arthritis. The patient’s son died from a brain tumor, but the exact tumor type and age at the time of death were unknown. Her current medications included metformin, insulin glargine, aspirin, and a daily multivitamin. She denied any allergies or history of smoking.
Physical examination of the scalp revealed 4 fixed, nontender, flesh-colored nodules: 2 on the left parietal scalp measuring 3.0 cm and 0.8 cm, respectively (Figure 1A); a 0.4-cm nodule on the right posterior occipital scalp; and a 1.6-cm sausage-shaped nodule on the right temple (Figure 1B). No positive lymph nodes were appreciated, and no additional lesions were noted. No additional atypical lesions were noted on full cutaneous examination.
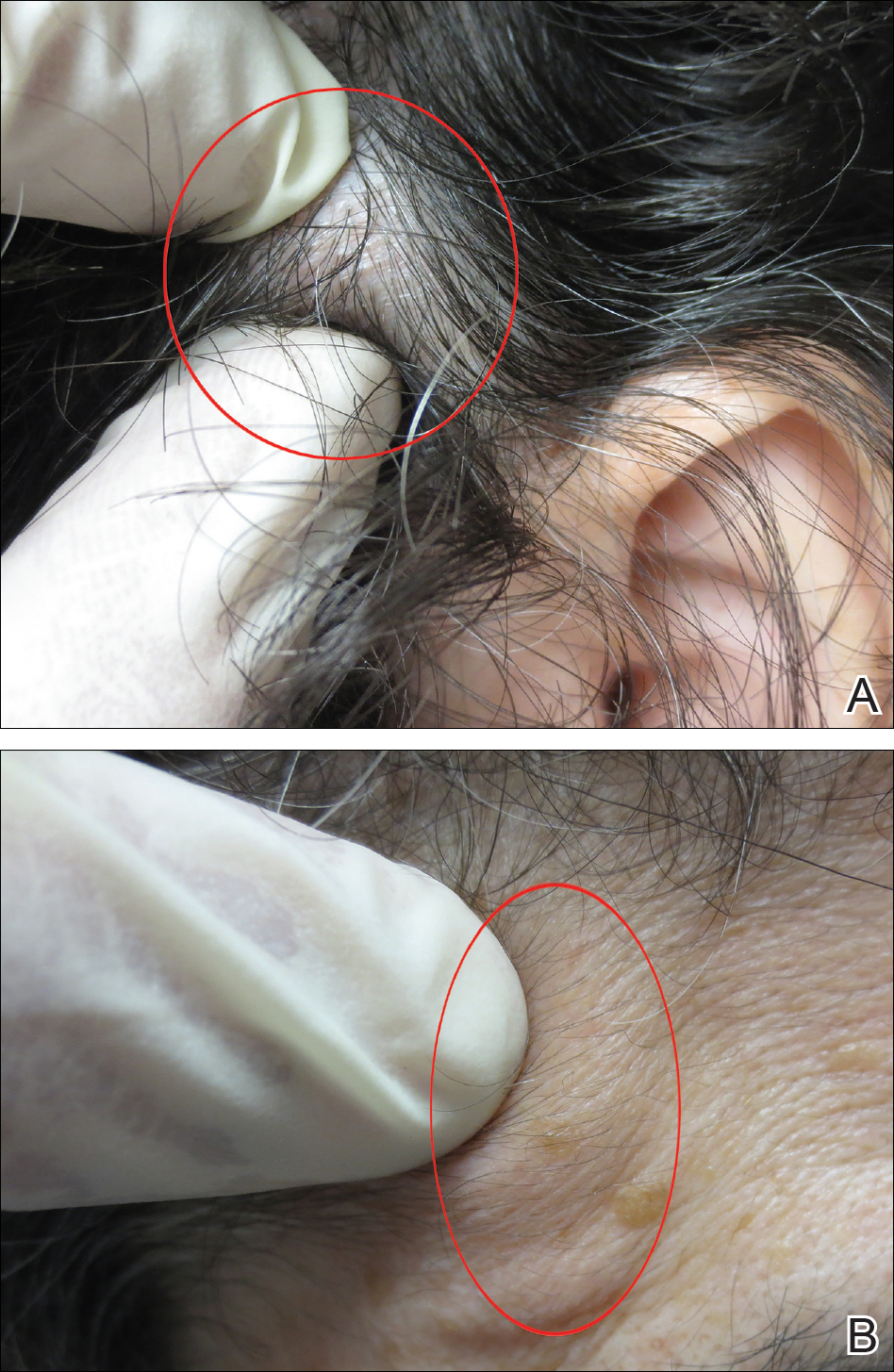
A diagnostic 6-mm punch biopsy of the largest nodule was performed. Intraoperatively, there was no apparent cyst wall, but coiled, loose, stringlike, pink-yellow tissue was removed from the base of the wound before closing with sutures.
The primary histologic finding was cells within fibrous tissue containing delicate round-oval nuclei, inconspicuous nucleoli, and lightly eosinophilic cytoplasm with an indistinct border (Figure 2). Immunohistochemical studies for S100 protein were focal and limited to the cytoplasm of a subset of neoplastic cells (Figure 3). Tumor cells stained positive for epithelial membrane antigen (EMA) and were focally positive for progesterone receptor (Figure 4). Tumor cells were negative for CD31 and CD34. Based on the clinical and histologic findings, a diagnosis of metastatic meningioma of the scalp was made.
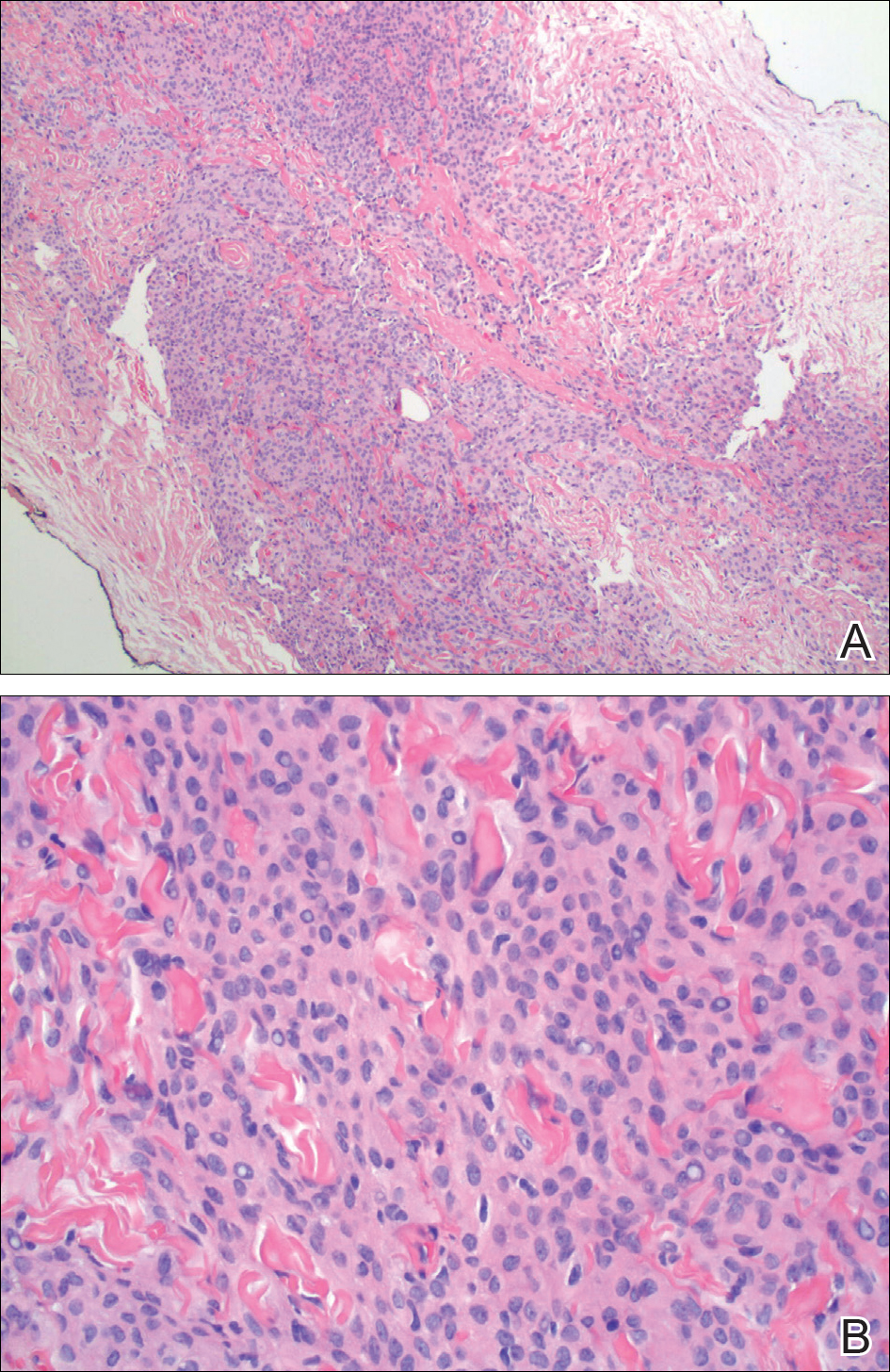
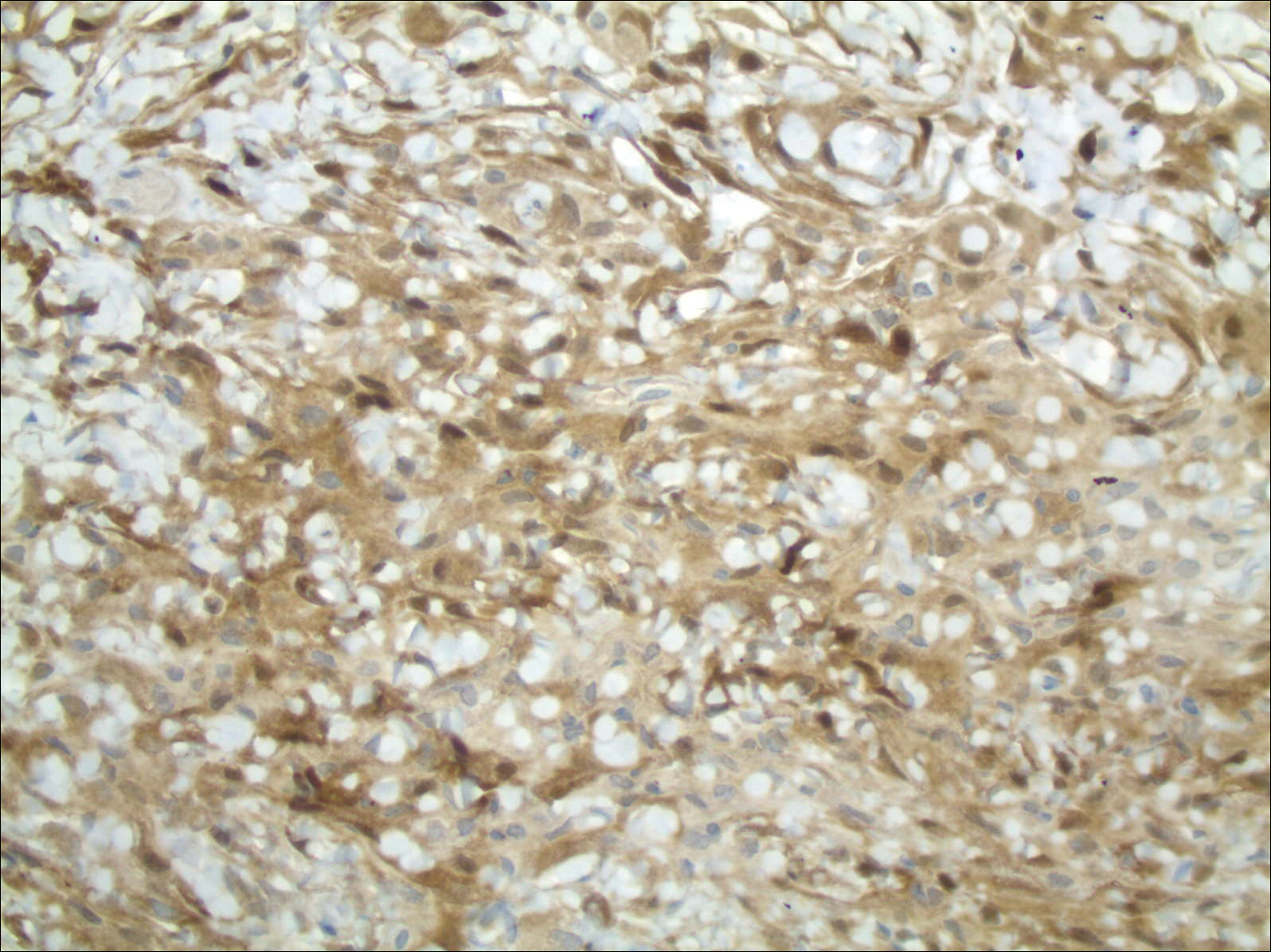
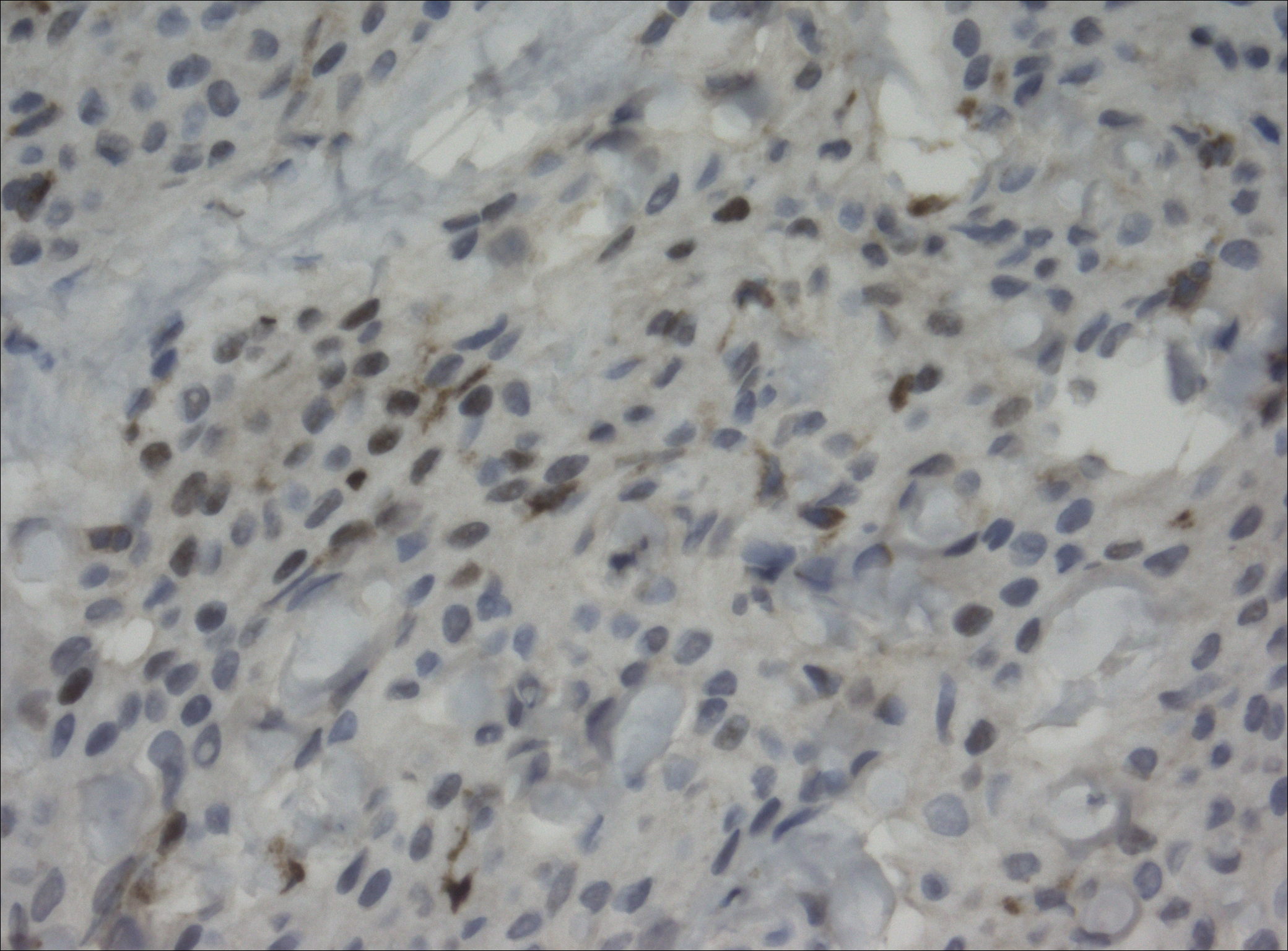
Magnetic resonance imaging and positron emission tomography of the head, neck, and chest demonstrated 3 residual subcutaneous nodules on the scalp and an indeterminate subcentimeter nodule in the right lung. The 0.4-cm nodule on the right posterior occipital scalp was removed without complication, and no radiation therapy was administered. The rest of the lesions were monitored. She remained under the close observation of a neurosurgeon and underwent repeat imaging of the scalp nodules and lungs, initially at 3 months and then routinely at the patient’s comfort. The patient currently denies any neurologic symptoms.
Comment
Meningiomas are derived from meningothelial cells found in the leptomeninges and in the choroid plexus of the ventricles of the brain.2 They are common intracranial neoplasms that generally are associated with a benign course and present during the fourth to sixth decades of life. Meningiomas constitute 13% to 30% of intracranial neoplasms and usually are female predominant (3:1).3,4 Rarely, malignant transformation can lead to local and distant metastasis to the lungs,5,6 liver,7 and skeletal system.8 In cases of metastatic spread, there is an increased incidence in males versus females.9-11
Risk Factors
Although many meningiomas are sporadic, numerous risk factors have been associated with the disease development. One study showed a link between exposure to ionizing radiation and subsequent development of meningioma.12 Another study found a population link between a higher incidence of meningioma and nuclear exposure in Hiroshima, Japan, after the atomic bomb blast in 1980.13 There is an increased incidence of meningioma in patients exposed to radiography from frequent dental imaging, particularly when older machines with higher levels of radiation exposure are used.14Another study demonstrated a correlation between meningioma and hormonal factors (eg, estrogen for hormone therapy) and exacerbation of symptoms during pregnancy.15 There also is an increased incidence of meningioma in breast cancer patients.4 Genetic alterations also have been implicated in the development of meningioma. It was found that 50% of patients with a mutation in the neurofibromatosis 2 gene (which codes for the merlin protein) had associated meningiomas.16,17 Scalp nodules in patients with neurofibromatosis type 2 increases suspicion of a scalp meningioma and necessitates biopsy.
Clinical Presentation
Cutaneous meningiomas typically present as firm, subcutaneous nodules. Scalp nodules ranging from alopecia18,19 to hypertrichosis20 have been reported. These neoplasms can be painless or painful, depending on mass effect and location.
Classification
The primary clinical classification system of metastatic meningioma was first described in 1974.21 Type 1 meningioma refers to congenital lesions that tend to cluster closer to the midline. Type 2 refers to ectopic soft-tissue lesions that extend to the skin from likely remnants of arachnoid cells. These lesions are more likely to be found around the eyes, ears, nose, and mouth. Type 3 meningiomas extend from intracranial tumors that secondarily involve the skin through proliferation through bone or anatomic defects. Type 3 is the result of direct extension and the location of the cutaneous presentation depends on the location of the intracranial lesion.4,22,23
Pathology
Meningiomas exhibit a range of morphologic appearances on histopathology. In almost all meningiomas, tumor cells are concentrically wrapped in tight whorls with round-oval nuclei and delicate chromatin, central clearing, and pale pseudonuclear inclusions. Lamellate calcifications known as psammoma bodies are a common finding. Immunohistochemical studies show that most meningiomas are positive for EMA, vimentin, and progesterone receptor. S100 protein expression, if present, usually is focal.
Differential Diagnosis
Asymptomatic nodules on the scalp may present a diagnostic challenge to physicians. Most common scalp lesions tend to be cystic or lipomatous. In children, a broad differential diagnosis should be considered, including dermoid and epidermoid tumors, dermal sinus tumors, hemangiomas, metastasis of another tumor, aplasia cutis congenita, pilomatricoma, and lipoma. In adults, the differential should focus on epidermoid cysts, lipomas, metastasis of other tumors, osteomas, arteriovenous fistulae, and heterotopic brain tissue. Often, microscopic examination is necessary, along with additional immunohistochemical staining (eg, EMA, vimentin).
Treatment
Treatment options for meningioma include observation, surgical resection, radiotherapy, and systemic therapy, as well as a combination of these modalities. The choice of therapy depends on such variables as patient age; performance status; comorbidities; presence or absence of symptoms (including focal neurologic deficits); and tumor location, size, and grade. It is important to note that there is limited knowledge looking at the results of various treatment modalities, and no consensus approach has been established.
Conclusion
Our patient’s medical history was remarkable for an intracranial meningioma 11 years prior to the current presentation, and she was found to have biopsy-proven metastatic meningioma without recurrence of the initial tumor. Patients presenting with a scalp nodule warrant a thorough medical history and consideration beyond common cysts and lipomas.
- Mackay B, Bruner JM, Luna MA. Malignant meningioma of the scalp. Ultrastruc Pathol. 1994;18:235-240.
- Whittle IR, Smith C, Navoo P, et al. Meningiomas. Lancet. 2004;363:1535-1543.
- Bauman G, Fisher B, Schild S, et al. Meningioma, ependymoma, and other adult brain tumors. In: Gunderson LL, Tepper JE, eds. Clinical Radiation Oncology. Philadelphia, PA: Elsevier Churchill Livingstone; 2007:539-566.
- Claus EB, Bondy ML, Schildkraut JM, et al. Epidemiology of intracranial meningioma. Neurosurgery. 2005;57:1088-1095.
- Tworek JA, Mikhail AA, Blaivas M. Meningioma: local recurrence and pulmonary metastasis diagnosed by fine needle aspiration. Acta Cytol. 1997;41:946-947.
- Shin MS, Holman WL, Herrera GA, et al. Extensive pulmonary metastasis of an intracranial meningioma with repeated recurrence: radiographic and pathologic features. South Med J. 1996;89:313-318.
- Ferguson JM, Flinn J. Intracranial meningioma with hepatic metastases and hypoglycaemia treated by selective hepatic arterial chemo-embolization. Australas Radiol.1995;39:97-99.
- Palmer JD, Cook PL, Ellison DW. Extracranial osseous metastases from intracranial meningioma. Br J Neurosurg. 1994;8:215-218.
- Glasauer FE, Yuan RH. Intracranial tumours with extracranial metastases. case report and review of the literature. J Neurosurg. 1963;20:474-493.
- Shuangshoti S, Hongsaprabhas C, Netsky MG. Metastasizing meningioma. Cancer. 1970;26:832-841.
- Ohta M, Iwaki T, Kitamoto T, et al. MIB-1 staining index and scoring of histological features in meningioma. Cancer. 1994;74:3176-3189.
- Wrensch M, Minn Y, Chew T, et al. Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro Oncol. 2002;4:278-299.
- Shintani T, Hayakawa N, Hoshi M, et al. High incidence of meningioma among Hiroshima atomic bomb survivors. J Rad Res. 1999;40:49-57.
- Claus EB, Calvocoressi L, Bondy ML, et al. Dental x-rays and risk of meningioma. Cancer. 2012;118:4530-4537.
- Blitshteyn S, Crook JE, Jaeckle KA. Is there an association between meningioma and hormone replacement therapy? J Clin Oncol. 2008;26:279-282.
- Fontaine B, Rouleau GA, Seizinger BR, et al. Molecular genetics of neurofibromatosis 2 and related tumors (acoustic neuromas and meningioma). Ann N Y Acad Sci. 1991;615:338-343.
- Rabin BM, Meyer JR, Berlin JW, et al. Radiation-induced changes of the central nervous system and head and neck. Radiographics. 1996;16:1055-1072.
- Tanaka S, Okazaki M, Egusa G, et al. A case of pheochromocytoma associated with meningioma. J Intern Med. 1991;229:371-373.
- Zeikus P, Robinson-Bostom L, Stopa E. Primary cutaneous meningioma in association with a sinus pericranii. J Am Acad Dermatol. 2006;54(2 suppl):S49-S50.
- Junaid TA, Nkposong EO, Kolawole TM. Cutaneous meningiomas and an ovarian fibroma in a three-year-old girl. J Pathol. 1972;108:165-167.
- Lopez DA, Silvers DN, Helwig EB. Cutaneous meningioma—a clinicopathologic study. Cancer. 1974;34:728-744.
- Shuangshoti S, Boonjunwetwat D, Kaoroptham S. Association of primary intraspinal meningiomas and subcutaneous meningioma of the cervical region: case report and review of literature. Surg Neurol. 1992;38:129-134.
- Miedema JR, Zedek D. Cutaneous meningioma. Arch Pathol. 2012;136:208-211.
- Mackay B, Bruner JM, Luna MA. Malignant meningioma of the scalp. Ultrastruc Pathol. 1994;18:235-240.
- Whittle IR, Smith C, Navoo P, et al. Meningiomas. Lancet. 2004;363:1535-1543.
- Bauman G, Fisher B, Schild S, et al. Meningioma, ependymoma, and other adult brain tumors. In: Gunderson LL, Tepper JE, eds. Clinical Radiation Oncology. Philadelphia, PA: Elsevier Churchill Livingstone; 2007:539-566.
- Claus EB, Bondy ML, Schildkraut JM, et al. Epidemiology of intracranial meningioma. Neurosurgery. 2005;57:1088-1095.
- Tworek JA, Mikhail AA, Blaivas M. Meningioma: local recurrence and pulmonary metastasis diagnosed by fine needle aspiration. Acta Cytol. 1997;41:946-947.
- Shin MS, Holman WL, Herrera GA, et al. Extensive pulmonary metastasis of an intracranial meningioma with repeated recurrence: radiographic and pathologic features. South Med J. 1996;89:313-318.
- Ferguson JM, Flinn J. Intracranial meningioma with hepatic metastases and hypoglycaemia treated by selective hepatic arterial chemo-embolization. Australas Radiol.1995;39:97-99.
- Palmer JD, Cook PL, Ellison DW. Extracranial osseous metastases from intracranial meningioma. Br J Neurosurg. 1994;8:215-218.
- Glasauer FE, Yuan RH. Intracranial tumours with extracranial metastases. case report and review of the literature. J Neurosurg. 1963;20:474-493.
- Shuangshoti S, Hongsaprabhas C, Netsky MG. Metastasizing meningioma. Cancer. 1970;26:832-841.
- Ohta M, Iwaki T, Kitamoto T, et al. MIB-1 staining index and scoring of histological features in meningioma. Cancer. 1994;74:3176-3189.
- Wrensch M, Minn Y, Chew T, et al. Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro Oncol. 2002;4:278-299.
- Shintani T, Hayakawa N, Hoshi M, et al. High incidence of meningioma among Hiroshima atomic bomb survivors. J Rad Res. 1999;40:49-57.
- Claus EB, Calvocoressi L, Bondy ML, et al. Dental x-rays and risk of meningioma. Cancer. 2012;118:4530-4537.
- Blitshteyn S, Crook JE, Jaeckle KA. Is there an association between meningioma and hormone replacement therapy? J Clin Oncol. 2008;26:279-282.
- Fontaine B, Rouleau GA, Seizinger BR, et al. Molecular genetics of neurofibromatosis 2 and related tumors (acoustic neuromas and meningioma). Ann N Y Acad Sci. 1991;615:338-343.
- Rabin BM, Meyer JR, Berlin JW, et al. Radiation-induced changes of the central nervous system and head and neck. Radiographics. 1996;16:1055-1072.
- Tanaka S, Okazaki M, Egusa G, et al. A case of pheochromocytoma associated with meningioma. J Intern Med. 1991;229:371-373.
- Zeikus P, Robinson-Bostom L, Stopa E. Primary cutaneous meningioma in association with a sinus pericranii. J Am Acad Dermatol. 2006;54(2 suppl):S49-S50.
- Junaid TA, Nkposong EO, Kolawole TM. Cutaneous meningiomas and an ovarian fibroma in a three-year-old girl. J Pathol. 1972;108:165-167.
- Lopez DA, Silvers DN, Helwig EB. Cutaneous meningioma—a clinicopathologic study. Cancer. 1974;34:728-744.
- Shuangshoti S, Boonjunwetwat D, Kaoroptham S. Association of primary intraspinal meningiomas and subcutaneous meningioma of the cervical region: case report and review of literature. Surg Neurol. 1992;38:129-134.
- Miedema JR, Zedek D. Cutaneous meningioma. Arch Pathol. 2012;136:208-211.
Squamoid Eccrine Ductal Carcinoma
Eccrine carcinomas are uncommon cutaneous neoplasms demonstrating nonuniform histologic features, behavior, and nomenclature. Given the rarity of these tumors, no known criteria by which to diagnose the tumor or guidelines for treatment have been proposed. We report a rare case of an immunocompromised patient with a primary squamoid eccrine ductal carcinoma (SEDC) who was subsequently treated with radical resection and axillary dissection. It was later determined that the patient had distant metastasis of SEDC. A review of the literature on the diagnosis, treatment, and surveillance of SEDC also is provided.
Case Report
A 77-year-old man whose medical history was remarkable for chronic lymphocytic leukemia (CLL) and numerous previous basal cell carcinomas and squamous cell carcinomas (SCCs) presented with a 5-cm, stellate, sclerotic plaque on the left chest of approximately 2 years’ duration (Figure 1) and a 3-mm pink papule on the right nasal sidewall of 2 months’ duration. Initial histology of both lesions revealed carcinoma with squamous and ductal differentiation extending from the undersurface of the epidermis, favoring a diagnosis of SEDC (Figure 2). At the time of initial presentation, the patient also had a 6-mm pink papule on the right chest of several months duration that was consistent with a well-differentiated sebaceous carcinoma on histology.

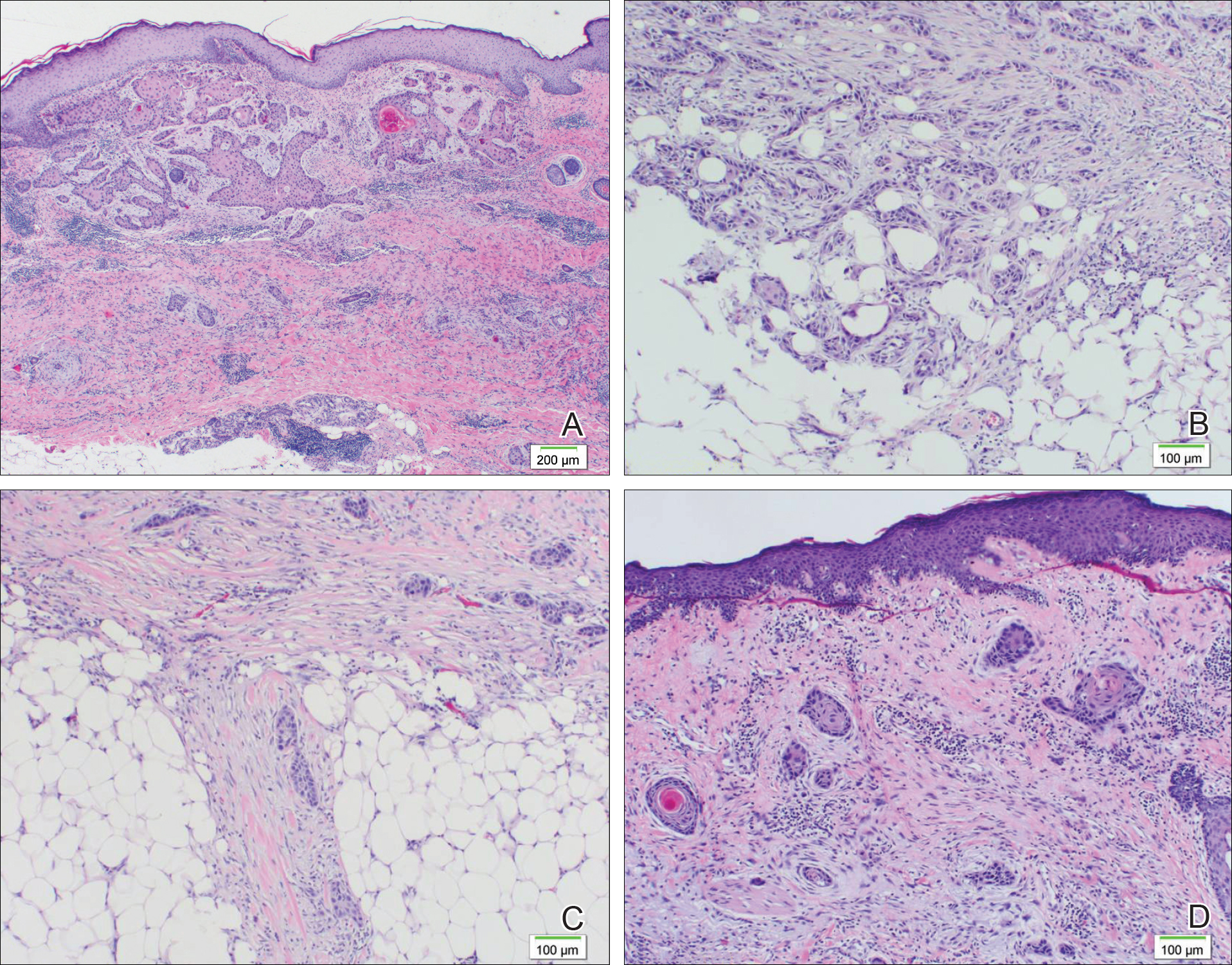
Further analysis of the lesion on the left chest revealed positive staining for cytokeratin (CK) 5/14 and p63, suggestive of a cutaneous malignancy. Staining for S100 protein highlighted rare cells in the basal layer of tumor aggregates. The immunohistochemical profile showed negative staining for CK7, CK5D3, epithelial membrane antigen (EMA), estrogen receptor, progesterone receptor, and human epidermal growth factor 2.
Diagnosis of SEDC of the chest and nasal lesions was based on the morphologic architecture, which included ductal formation noted within the tumor. The chest lesion also had prominent squamoid differentiation. Another histologic feature consistent with SEDC was poorly demarcated, infiltrative neoplastic cells extending into the dermis and subcutis. Although there was some positive focal staining for carcinoembryonic antigen (CEA), variegation within the tumor and the prominent squamoid component might have contributed to this unexpected staining pattern.
The patient was admitted to the hospital for excision of the lesion on the chest wall. Initial workup revealed macrocytic anemia, which required transfusion, and an incidental finding of non–small-cell lung cancer. The chest lesion was unrelated to the non–small-cell lung cancer based on the staining profile. Material from the lung stained positive for thyroid transcription factor 1 (TTF-1) and exhibited rare staining for p63; however, the chest lesion did not stain positive for TTF-1 and had strong staining affinity for p63, indicative of a cutaneous malignancy.
The lesion on the chest wall was definitively excised. Pathologic analysis revealed a dermal-based infiltrative tumor of irregular nests and cords of squamoid cells with focal ductal formation in a fibromyxoid background stroma, suggestive of an adnexal carcinoma with a considerable degree of squamous differentiation and favoring a diagnosis of SEDC. Focal perineural invasion was noted, but no lymphovascular spread was identified; however, metastasis was identified in 1 of 26 axillary lymph nodes. The patient underwent 9 sessions of radiation therapy for the lung cancer and also was given cetuximab.
Three months later, the nasal tumor was subsequently excised in an outpatient procedure, and the final biopsy report indicated a diagnosis of basal cell carcinoma. One-and-a-half years later, in follow-up with surgery after removal of the chest lesion, a 2×3-cm mass was excised from the left neck that demonstrated lymph nodes consistent with metastatic SEDC. Careful evaluation of this patient, including family history and genetic screening, was considered. Our patient continues to follow-up with the dermatology department every 3 months. He has been doing well and has had multiple additional primary SCCs in the subsequent 5 years of follow-up.
Comment
Eccrine carcinoma is the most common subtype of adnexal carcinoma, representing 0.01% of all cutaneous tumors.1 S
Eccrine carcinoma is observed clinically as a slow-growing, nodular plaque on the scalp, arms, legs, or trunk in middle-aged and elderly individuals.1 Squamoid eccrine ductal carcinoma also has been reported in a young woman.5 Another immunocompromised patient was identified in the literature with a great toe lesion that showed follicular differentiation along with the usual SEDC features of squamoid and ductal differentiation.6 The etiology of SEDC is controversial but is thought to be an SCC arising from eccrine glands, a subtype of eccrine carcinoma with extensive squamoid differentiation, or a biphenotypic carcinoma.1,7
Histologically, SEDC is poorly circumscribed with an infiltrative growth pattern and deep extension into the dermis and subcutaneous tissue. The lesion is characterized by prominent squamous epithelial proliferation superficially with cellular atypia, keratinous cyst formation, squamous eddies, and eccrine ductal differentiation.1
The differential diagnosis of SEDC includes SCC; metastatic carcinoma with squamoid features; and eccrine tumors, including eccrine poroma, microcystic adnexal carcinoma, and porocarcinoma with squamous differentiation.1
Immunohistochemistry has a role in the diagnosis of SEDC. Findings include positive staining for S100 protein, EMA, CKs, and CEA. Glandular tissue stains positive for EMA and CEA, supporting an adnexal origin.1 Positivity for p63 and CK5/6 supports the conclusion that this is a primary cutaneous malignancy, not a metastatic disease.1
Squamoid eccrine ductal carcinoma has an indeterminate malignant potential. There is a disparity of clinical behavior between SCC and eccrine cancers; however, because squamous differentiation sometimes dominates the histological picture, eccrine carcinomas can be misdiagnosed as SCC.1,8 Eccrine adnexal tumors are characterized by multiple local recurrences (70%–80% of cases); perineural invasion; and metastasis (50% of cases) to regional lymph nodes and viscera, including the lungs, liver, bones, and brain.1 Squamous cell carcinoma, however, has a markedly lower recurrence rate (3.1%–18.7% of cases) and rate of metastasis (5.2%–37.8%).1
Squamoid eccrine ductal carcinoma is classified as one of the less aggressive eccrine tumors, although the low number of cases makes it a controversial conclusion.1 To our knowledge, no cases of SEDC metastasis have been reported with SEDC. Recurrence of SEDC has been reported locally, and perineural or perivascular invasion (or both) has been demonstrated in 3 cases.1
Since SEDC has invasive and metastatic potential, as demonstrated in our case, along with elevated local recurrence rates, physicians must be able to properly diagnose this rare entity and recommend an appropriate surgical modality. Due to the low incidence of SEDC, there are no known randomized studies comparing treatment modalities.1 O
Surgical extirpation with complete margin examination is recommended, as SEDC tends to be underestimated in size, is aggressive in its infiltration, and is predisposed to perineural and perivascular invasion. T
Along with the rarity of SEDC in our patient, the simultaneous occurrence of 3 primary malignancies also is unusual. Patients with CLL have progressive defects of cell- and humoral-mediated immunity, causing immunosuppression. In a retrospective study, Tsimberidou et al9 reviewed the records of 2028 untreated CLL patients and determined that 27% had another primary malignancy, including skin (30%) and lung cancers (6%), which were two of the malignancies seen in our patient. The investigators concluded that patients with CLL have more than twice the risk of developing a second primary malignancy and an increased frequency of certain cancer types.9 Furthermore, treatment regimens for CLL have been considered to increase cell- and humoral-mediated immune defects at specific cancer sites,10 although the exact mechanism of this action is unknown. Development of a second primary malignancy (or even a third) in patients with SEDC is increasingly being reported in CLL patients.9,10
A high index of suspicion with SEDC in the differential diagnosis should be maintained in elderly men with slow-growing, solitary, nodular lesions of the scalp, nose, arms, legs, or trunk.
- Clark S, Young A, Piatigorsky E, et al. Mohs micrographic surgery in the setting of squamoid eccrine ductal carcinoma: addressing a diagnostic and therapeutic challenge. Clin Aesthet Dermatol. 2013;6:33-36.
- Saraiva MI, Vieira MA, Portocarrero LK, et al. Squamoid eccrine ductal carcinoma. An Bras Dermatol. 2016;916:799-802.
- van der Horst MP, Garcia-Herrera A, Markiewicz D, et al. Squamoid eccrine ductal carcinoma: a clinicopathologic study of 30 cases. Am J Surg Pathol. 2016;40:755-760.
- Frouin E, Vignon-Pennamen MD, Balme B, et al. Anatomoclinical study of 30 cases of sclerosing sweat duct carcinomas (microcystic adnexal carcinoma, syringomatous carcinoma and squamoid eccrine ductal carcinoma)[published online April 15, 2015]. J Eur Acad Dermatol Venereol. 2015;29:1978-1994.
- Kim YJ, Kim AR, Yu DS. Mohs micrographic surgery for squamoid eccrine ductal carcinoma. Dermatol Surg. 2005;31:1462-1464.
- Kavand S, Cassarino DS. Squamoid eccrine ductal carcinoma: an unusual low-grade case with follicular differentiation. are these tumors squamoid variants of microcystic adnexal carcinoma? Am J Dermatopathol. 2009;31:849-852.
- Terushkin E, Leffell DJ, Futoryan T, et al. Squamoid eccrine ductal carcinoma: a case report and review of the literature. Am J Dermatopathol. 2010;32:287-292.
- Chhibber V, Lyle S, Mahalingam M. Ductal eccrine carcinoma with squamous differentiation: apropos a case. J Cutan Pathol. 2007;34:503-507.
- Tsimberidou AM, Wen S, McLaughlin P, et al. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol. 2009;27:904-910.
- Dasanu CA, Alexandrescu DT. Risk for second nonlymphoid neoplasms in chronic lymphocytic leukemia. Med Gen Med. 2007;9:35.
Eccrine carcinomas are uncommon cutaneous neoplasms demonstrating nonuniform histologic features, behavior, and nomenclature. Given the rarity of these tumors, no known criteria by which to diagnose the tumor or guidelines for treatment have been proposed. We report a rare case of an immunocompromised patient with a primary squamoid eccrine ductal carcinoma (SEDC) who was subsequently treated with radical resection and axillary dissection. It was later determined that the patient had distant metastasis of SEDC. A review of the literature on the diagnosis, treatment, and surveillance of SEDC also is provided.
Case Report
A 77-year-old man whose medical history was remarkable for chronic lymphocytic leukemia (CLL) and numerous previous basal cell carcinomas and squamous cell carcinomas (SCCs) presented with a 5-cm, stellate, sclerotic plaque on the left chest of approximately 2 years’ duration (Figure 1) and a 3-mm pink papule on the right nasal sidewall of 2 months’ duration. Initial histology of both lesions revealed carcinoma with squamous and ductal differentiation extending from the undersurface of the epidermis, favoring a diagnosis of SEDC (Figure 2). At the time of initial presentation, the patient also had a 6-mm pink papule on the right chest of several months duration that was consistent with a well-differentiated sebaceous carcinoma on histology.

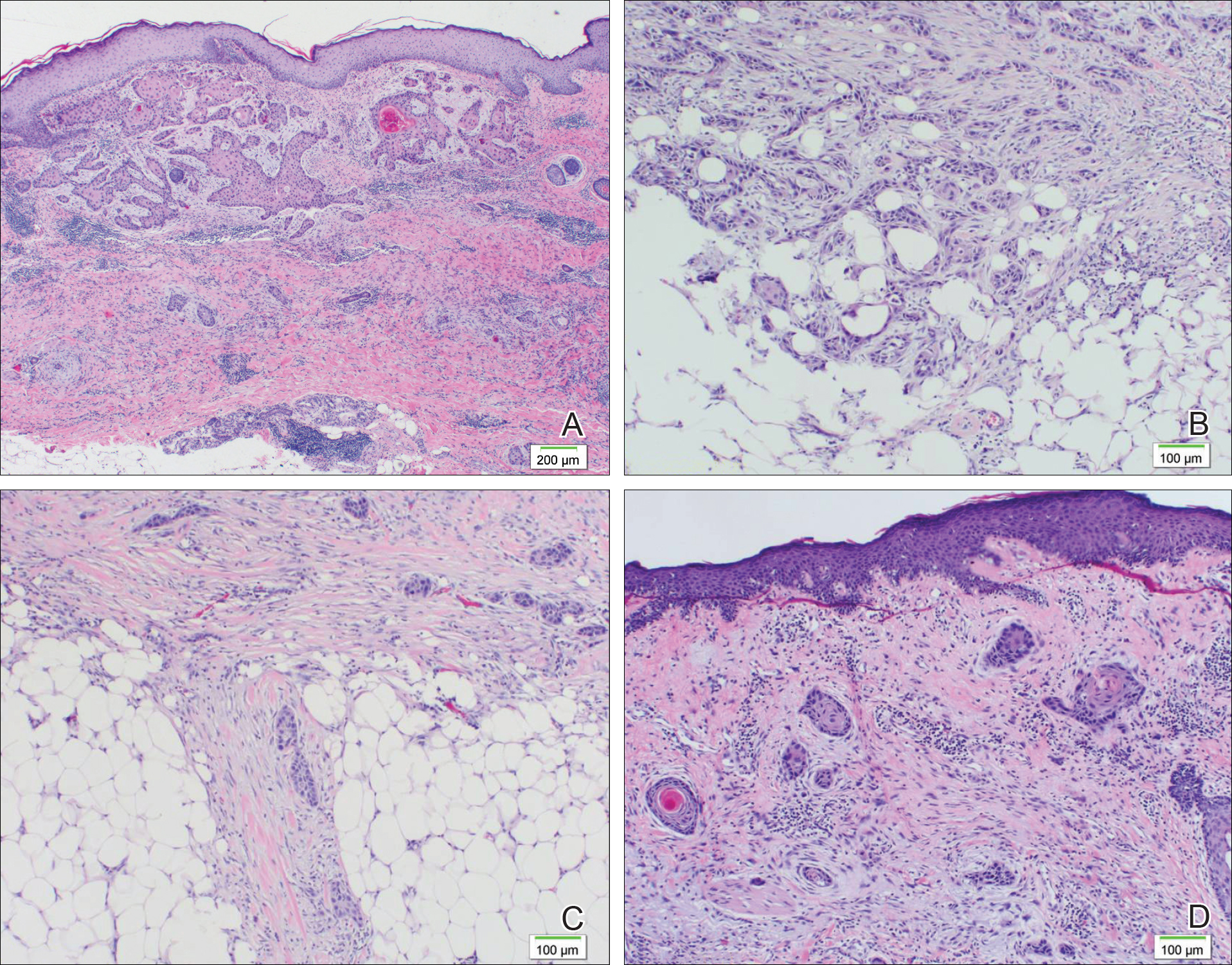
Further analysis of the lesion on the left chest revealed positive staining for cytokeratin (CK) 5/14 and p63, suggestive of a cutaneous malignancy. Staining for S100 protein highlighted rare cells in the basal layer of tumor aggregates. The immunohistochemical profile showed negative staining for CK7, CK5D3, epithelial membrane antigen (EMA), estrogen receptor, progesterone receptor, and human epidermal growth factor 2.
Diagnosis of SEDC of the chest and nasal lesions was based on the morphologic architecture, which included ductal formation noted within the tumor. The chest lesion also had prominent squamoid differentiation. Another histologic feature consistent with SEDC was poorly demarcated, infiltrative neoplastic cells extending into the dermis and subcutis. Although there was some positive focal staining for carcinoembryonic antigen (CEA), variegation within the tumor and the prominent squamoid component might have contributed to this unexpected staining pattern.
The patient was admitted to the hospital for excision of the lesion on the chest wall. Initial workup revealed macrocytic anemia, which required transfusion, and an incidental finding of non–small-cell lung cancer. The chest lesion was unrelated to the non–small-cell lung cancer based on the staining profile. Material from the lung stained positive for thyroid transcription factor 1 (TTF-1) and exhibited rare staining for p63; however, the chest lesion did not stain positive for TTF-1 and had strong staining affinity for p63, indicative of a cutaneous malignancy.
The lesion on the chest wall was definitively excised. Pathologic analysis revealed a dermal-based infiltrative tumor of irregular nests and cords of squamoid cells with focal ductal formation in a fibromyxoid background stroma, suggestive of an adnexal carcinoma with a considerable degree of squamous differentiation and favoring a diagnosis of SEDC. Focal perineural invasion was noted, but no lymphovascular spread was identified; however, metastasis was identified in 1 of 26 axillary lymph nodes. The patient underwent 9 sessions of radiation therapy for the lung cancer and also was given cetuximab.
Three months later, the nasal tumor was subsequently excised in an outpatient procedure, and the final biopsy report indicated a diagnosis of basal cell carcinoma. One-and-a-half years later, in follow-up with surgery after removal of the chest lesion, a 2×3-cm mass was excised from the left neck that demonstrated lymph nodes consistent with metastatic SEDC. Careful evaluation of this patient, including family history and genetic screening, was considered. Our patient continues to follow-up with the dermatology department every 3 months. He has been doing well and has had multiple additional primary SCCs in the subsequent 5 years of follow-up.
Comment
Eccrine carcinoma is the most common subtype of adnexal carcinoma, representing 0.01% of all cutaneous tumors.1 S
Eccrine carcinoma is observed clinically as a slow-growing, nodular plaque on the scalp, arms, legs, or trunk in middle-aged and elderly individuals.1 Squamoid eccrine ductal carcinoma also has been reported in a young woman.5 Another immunocompromised patient was identified in the literature with a great toe lesion that showed follicular differentiation along with the usual SEDC features of squamoid and ductal differentiation.6 The etiology of SEDC is controversial but is thought to be an SCC arising from eccrine glands, a subtype of eccrine carcinoma with extensive squamoid differentiation, or a biphenotypic carcinoma.1,7
Histologically, SEDC is poorly circumscribed with an infiltrative growth pattern and deep extension into the dermis and subcutaneous tissue. The lesion is characterized by prominent squamous epithelial proliferation superficially with cellular atypia, keratinous cyst formation, squamous eddies, and eccrine ductal differentiation.1
The differential diagnosis of SEDC includes SCC; metastatic carcinoma with squamoid features; and eccrine tumors, including eccrine poroma, microcystic adnexal carcinoma, and porocarcinoma with squamous differentiation.1
Immunohistochemistry has a role in the diagnosis of SEDC. Findings include positive staining for S100 protein, EMA, CKs, and CEA. Glandular tissue stains positive for EMA and CEA, supporting an adnexal origin.1 Positivity for p63 and CK5/6 supports the conclusion that this is a primary cutaneous malignancy, not a metastatic disease.1
Squamoid eccrine ductal carcinoma has an indeterminate malignant potential. There is a disparity of clinical behavior between SCC and eccrine cancers; however, because squamous differentiation sometimes dominates the histological picture, eccrine carcinomas can be misdiagnosed as SCC.1,8 Eccrine adnexal tumors are characterized by multiple local recurrences (70%–80% of cases); perineural invasion; and metastasis (50% of cases) to regional lymph nodes and viscera, including the lungs, liver, bones, and brain.1 Squamous cell carcinoma, however, has a markedly lower recurrence rate (3.1%–18.7% of cases) and rate of metastasis (5.2%–37.8%).1
Squamoid eccrine ductal carcinoma is classified as one of the less aggressive eccrine tumors, although the low number of cases makes it a controversial conclusion.1 To our knowledge, no cases of SEDC metastasis have been reported with SEDC. Recurrence of SEDC has been reported locally, and perineural or perivascular invasion (or both) has been demonstrated in 3 cases.1
Since SEDC has invasive and metastatic potential, as demonstrated in our case, along with elevated local recurrence rates, physicians must be able to properly diagnose this rare entity and recommend an appropriate surgical modality. Due to the low incidence of SEDC, there are no known randomized studies comparing treatment modalities.1 O
Surgical extirpation with complete margin examination is recommended, as SEDC tends to be underestimated in size, is aggressive in its infiltration, and is predisposed to perineural and perivascular invasion. T
Along with the rarity of SEDC in our patient, the simultaneous occurrence of 3 primary malignancies also is unusual. Patients with CLL have progressive defects of cell- and humoral-mediated immunity, causing immunosuppression. In a retrospective study, Tsimberidou et al9 reviewed the records of 2028 untreated CLL patients and determined that 27% had another primary malignancy, including skin (30%) and lung cancers (6%), which were two of the malignancies seen in our patient. The investigators concluded that patients with CLL have more than twice the risk of developing a second primary malignancy and an increased frequency of certain cancer types.9 Furthermore, treatment regimens for CLL have been considered to increase cell- and humoral-mediated immune defects at specific cancer sites,10 although the exact mechanism of this action is unknown. Development of a second primary malignancy (or even a third) in patients with SEDC is increasingly being reported in CLL patients.9,10
A high index of suspicion with SEDC in the differential diagnosis should be maintained in elderly men with slow-growing, solitary, nodular lesions of the scalp, nose, arms, legs, or trunk.
Eccrine carcinomas are uncommon cutaneous neoplasms demonstrating nonuniform histologic features, behavior, and nomenclature. Given the rarity of these tumors, no known criteria by which to diagnose the tumor or guidelines for treatment have been proposed. We report a rare case of an immunocompromised patient with a primary squamoid eccrine ductal carcinoma (SEDC) who was subsequently treated with radical resection and axillary dissection. It was later determined that the patient had distant metastasis of SEDC. A review of the literature on the diagnosis, treatment, and surveillance of SEDC also is provided.
Case Report
A 77-year-old man whose medical history was remarkable for chronic lymphocytic leukemia (CLL) and numerous previous basal cell carcinomas and squamous cell carcinomas (SCCs) presented with a 5-cm, stellate, sclerotic plaque on the left chest of approximately 2 years’ duration (Figure 1) and a 3-mm pink papule on the right nasal sidewall of 2 months’ duration. Initial histology of both lesions revealed carcinoma with squamous and ductal differentiation extending from the undersurface of the epidermis, favoring a diagnosis of SEDC (Figure 2). At the time of initial presentation, the patient also had a 6-mm pink papule on the right chest of several months duration that was consistent with a well-differentiated sebaceous carcinoma on histology.

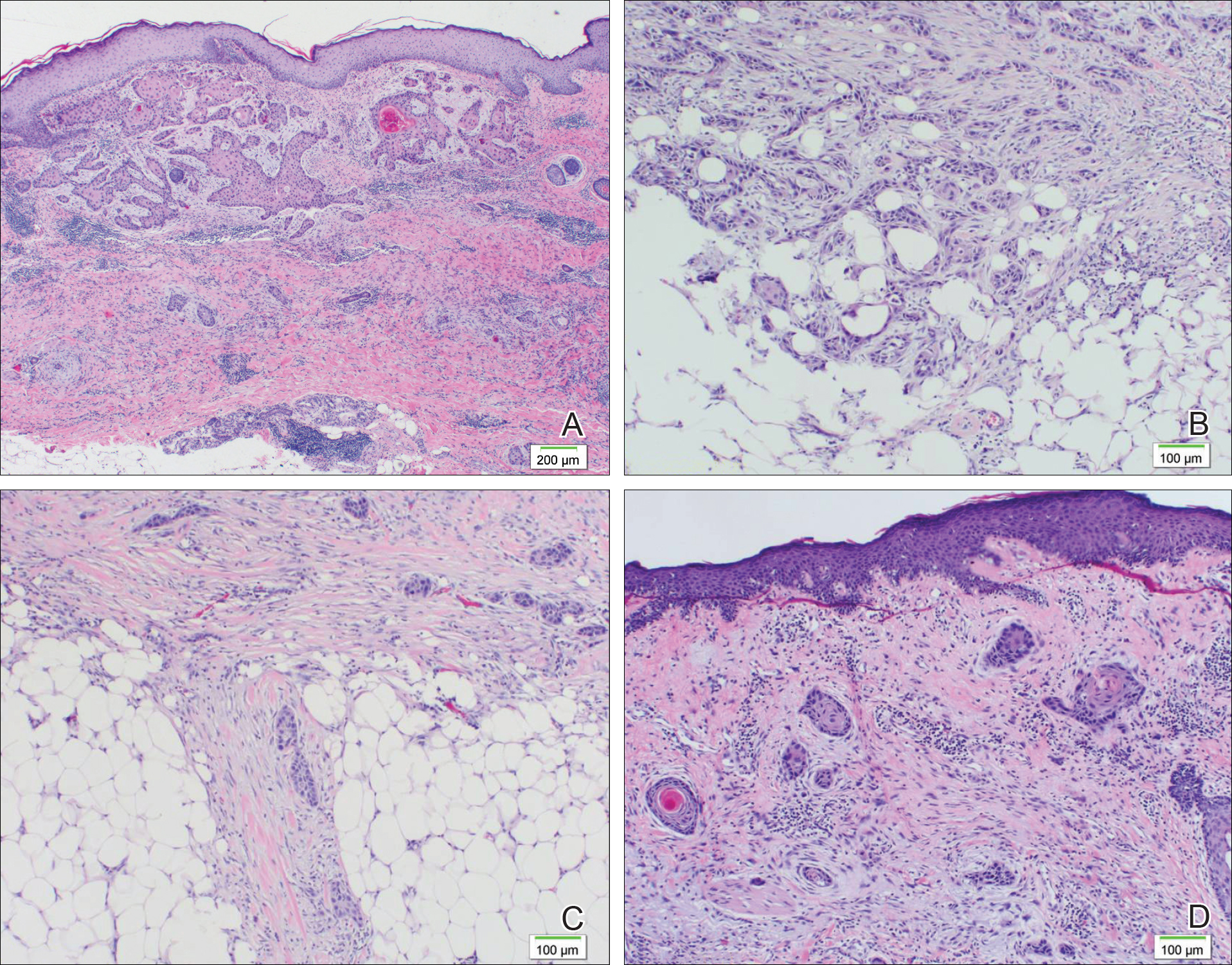
Further analysis of the lesion on the left chest revealed positive staining for cytokeratin (CK) 5/14 and p63, suggestive of a cutaneous malignancy. Staining for S100 protein highlighted rare cells in the basal layer of tumor aggregates. The immunohistochemical profile showed negative staining for CK7, CK5D3, epithelial membrane antigen (EMA), estrogen receptor, progesterone receptor, and human epidermal growth factor 2.
Diagnosis of SEDC of the chest and nasal lesions was based on the morphologic architecture, which included ductal formation noted within the tumor. The chest lesion also had prominent squamoid differentiation. Another histologic feature consistent with SEDC was poorly demarcated, infiltrative neoplastic cells extending into the dermis and subcutis. Although there was some positive focal staining for carcinoembryonic antigen (CEA), variegation within the tumor and the prominent squamoid component might have contributed to this unexpected staining pattern.
The patient was admitted to the hospital for excision of the lesion on the chest wall. Initial workup revealed macrocytic anemia, which required transfusion, and an incidental finding of non–small-cell lung cancer. The chest lesion was unrelated to the non–small-cell lung cancer based on the staining profile. Material from the lung stained positive for thyroid transcription factor 1 (TTF-1) and exhibited rare staining for p63; however, the chest lesion did not stain positive for TTF-1 and had strong staining affinity for p63, indicative of a cutaneous malignancy.
The lesion on the chest wall was definitively excised. Pathologic analysis revealed a dermal-based infiltrative tumor of irregular nests and cords of squamoid cells with focal ductal formation in a fibromyxoid background stroma, suggestive of an adnexal carcinoma with a considerable degree of squamous differentiation and favoring a diagnosis of SEDC. Focal perineural invasion was noted, but no lymphovascular spread was identified; however, metastasis was identified in 1 of 26 axillary lymph nodes. The patient underwent 9 sessions of radiation therapy for the lung cancer and also was given cetuximab.
Three months later, the nasal tumor was subsequently excised in an outpatient procedure, and the final biopsy report indicated a diagnosis of basal cell carcinoma. One-and-a-half years later, in follow-up with surgery after removal of the chest lesion, a 2×3-cm mass was excised from the left neck that demonstrated lymph nodes consistent with metastatic SEDC. Careful evaluation of this patient, including family history and genetic screening, was considered. Our patient continues to follow-up with the dermatology department every 3 months. He has been doing well and has had multiple additional primary SCCs in the subsequent 5 years of follow-up.
Comment
Eccrine carcinoma is the most common subtype of adnexal carcinoma, representing 0.01% of all cutaneous tumors.1 S
Eccrine carcinoma is observed clinically as a slow-growing, nodular plaque on the scalp, arms, legs, or trunk in middle-aged and elderly individuals.1 Squamoid eccrine ductal carcinoma also has been reported in a young woman.5 Another immunocompromised patient was identified in the literature with a great toe lesion that showed follicular differentiation along with the usual SEDC features of squamoid and ductal differentiation.6 The etiology of SEDC is controversial but is thought to be an SCC arising from eccrine glands, a subtype of eccrine carcinoma with extensive squamoid differentiation, or a biphenotypic carcinoma.1,7
Histologically, SEDC is poorly circumscribed with an infiltrative growth pattern and deep extension into the dermis and subcutaneous tissue. The lesion is characterized by prominent squamous epithelial proliferation superficially with cellular atypia, keratinous cyst formation, squamous eddies, and eccrine ductal differentiation.1
The differential diagnosis of SEDC includes SCC; metastatic carcinoma with squamoid features; and eccrine tumors, including eccrine poroma, microcystic adnexal carcinoma, and porocarcinoma with squamous differentiation.1
Immunohistochemistry has a role in the diagnosis of SEDC. Findings include positive staining for S100 protein, EMA, CKs, and CEA. Glandular tissue stains positive for EMA and CEA, supporting an adnexal origin.1 Positivity for p63 and CK5/6 supports the conclusion that this is a primary cutaneous malignancy, not a metastatic disease.1
Squamoid eccrine ductal carcinoma has an indeterminate malignant potential. There is a disparity of clinical behavior between SCC and eccrine cancers; however, because squamous differentiation sometimes dominates the histological picture, eccrine carcinomas can be misdiagnosed as SCC.1,8 Eccrine adnexal tumors are characterized by multiple local recurrences (70%–80% of cases); perineural invasion; and metastasis (50% of cases) to regional lymph nodes and viscera, including the lungs, liver, bones, and brain.1 Squamous cell carcinoma, however, has a markedly lower recurrence rate (3.1%–18.7% of cases) and rate of metastasis (5.2%–37.8%).1
Squamoid eccrine ductal carcinoma is classified as one of the less aggressive eccrine tumors, although the low number of cases makes it a controversial conclusion.1 To our knowledge, no cases of SEDC metastasis have been reported with SEDC. Recurrence of SEDC has been reported locally, and perineural or perivascular invasion (or both) has been demonstrated in 3 cases.1
Since SEDC has invasive and metastatic potential, as demonstrated in our case, along with elevated local recurrence rates, physicians must be able to properly diagnose this rare entity and recommend an appropriate surgical modality. Due to the low incidence of SEDC, there are no known randomized studies comparing treatment modalities.1 O
Surgical extirpation with complete margin examination is recommended, as SEDC tends to be underestimated in size, is aggressive in its infiltration, and is predisposed to perineural and perivascular invasion. T
Along with the rarity of SEDC in our patient, the simultaneous occurrence of 3 primary malignancies also is unusual. Patients with CLL have progressive defects of cell- and humoral-mediated immunity, causing immunosuppression. In a retrospective study, Tsimberidou et al9 reviewed the records of 2028 untreated CLL patients and determined that 27% had another primary malignancy, including skin (30%) and lung cancers (6%), which were two of the malignancies seen in our patient. The investigators concluded that patients with CLL have more than twice the risk of developing a second primary malignancy and an increased frequency of certain cancer types.9 Furthermore, treatment regimens for CLL have been considered to increase cell- and humoral-mediated immune defects at specific cancer sites,10 although the exact mechanism of this action is unknown. Development of a second primary malignancy (or even a third) in patients with SEDC is increasingly being reported in CLL patients.9,10
A high index of suspicion with SEDC in the differential diagnosis should be maintained in elderly men with slow-growing, solitary, nodular lesions of the scalp, nose, arms, legs, or trunk.
- Clark S, Young A, Piatigorsky E, et al. Mohs micrographic surgery in the setting of squamoid eccrine ductal carcinoma: addressing a diagnostic and therapeutic challenge. Clin Aesthet Dermatol. 2013;6:33-36.
- Saraiva MI, Vieira MA, Portocarrero LK, et al. Squamoid eccrine ductal carcinoma. An Bras Dermatol. 2016;916:799-802.
- van der Horst MP, Garcia-Herrera A, Markiewicz D, et al. Squamoid eccrine ductal carcinoma: a clinicopathologic study of 30 cases. Am J Surg Pathol. 2016;40:755-760.
- Frouin E, Vignon-Pennamen MD, Balme B, et al. Anatomoclinical study of 30 cases of sclerosing sweat duct carcinomas (microcystic adnexal carcinoma, syringomatous carcinoma and squamoid eccrine ductal carcinoma)[published online April 15, 2015]. J Eur Acad Dermatol Venereol. 2015;29:1978-1994.
- Kim YJ, Kim AR, Yu DS. Mohs micrographic surgery for squamoid eccrine ductal carcinoma. Dermatol Surg. 2005;31:1462-1464.
- Kavand S, Cassarino DS. Squamoid eccrine ductal carcinoma: an unusual low-grade case with follicular differentiation. are these tumors squamoid variants of microcystic adnexal carcinoma? Am J Dermatopathol. 2009;31:849-852.
- Terushkin E, Leffell DJ, Futoryan T, et al. Squamoid eccrine ductal carcinoma: a case report and review of the literature. Am J Dermatopathol. 2010;32:287-292.
- Chhibber V, Lyle S, Mahalingam M. Ductal eccrine carcinoma with squamous differentiation: apropos a case. J Cutan Pathol. 2007;34:503-507.
- Tsimberidou AM, Wen S, McLaughlin P, et al. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol. 2009;27:904-910.
- Dasanu CA, Alexandrescu DT. Risk for second nonlymphoid neoplasms in chronic lymphocytic leukemia. Med Gen Med. 2007;9:35.
- Clark S, Young A, Piatigorsky E, et al. Mohs micrographic surgery in the setting of squamoid eccrine ductal carcinoma: addressing a diagnostic and therapeutic challenge. Clin Aesthet Dermatol. 2013;6:33-36.
- Saraiva MI, Vieira MA, Portocarrero LK, et al. Squamoid eccrine ductal carcinoma. An Bras Dermatol. 2016;916:799-802.
- van der Horst MP, Garcia-Herrera A, Markiewicz D, et al. Squamoid eccrine ductal carcinoma: a clinicopathologic study of 30 cases. Am J Surg Pathol. 2016;40:755-760.
- Frouin E, Vignon-Pennamen MD, Balme B, et al. Anatomoclinical study of 30 cases of sclerosing sweat duct carcinomas (microcystic adnexal carcinoma, syringomatous carcinoma and squamoid eccrine ductal carcinoma)[published online April 15, 2015]. J Eur Acad Dermatol Venereol. 2015;29:1978-1994.
- Kim YJ, Kim AR, Yu DS. Mohs micrographic surgery for squamoid eccrine ductal carcinoma. Dermatol Surg. 2005;31:1462-1464.
- Kavand S, Cassarino DS. Squamoid eccrine ductal carcinoma: an unusual low-grade case with follicular differentiation. are these tumors squamoid variants of microcystic adnexal carcinoma? Am J Dermatopathol. 2009;31:849-852.
- Terushkin E, Leffell DJ, Futoryan T, et al. Squamoid eccrine ductal carcinoma: a case report and review of the literature. Am J Dermatopathol. 2010;32:287-292.
- Chhibber V, Lyle S, Mahalingam M. Ductal eccrine carcinoma with squamous differentiation: apropos a case. J Cutan Pathol. 2007;34:503-507.
- Tsimberidou AM, Wen S, McLaughlin P, et al. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol. 2009;27:904-910.
- Dasanu CA, Alexandrescu DT. Risk for second nonlymphoid neoplasms in chronic lymphocytic leukemia. Med Gen Med. 2007;9:35.
Practice Points
- Squamoid eccrine ductal carcinoma (SEDC) is an extremely rare cutaneous tumor of unknown etiology.
- A high index of suspicion with SEDC in the differential diagnosis should be maintained in elderly men with slow-growing, solitary, nodular lesions of the scalp, nose, arms, legs, or trunk.
- Development of a second or even a third primary malignancy in patients with SEDC is increasingly being reported in CLL patients.
Pigmented Squamous Cell Carcinoma Presenting as Longitudinal Melanonychia in a Transplant Recipient
Case Report
A 62-year-old black man presented for examination of a dark longitudinal streak located adjacent to the lateral nail fold on the third finger of the left hand. The lesion had been present for several months, during which time it had slowly expanded in size. The fingertip had recently become tender, which interfered with the patient’s ability to work. His past medical history was remarkable for end-stage renal disease secondary to glomerulonephritis with nephrotic syndrome of unclear etiology. He initially was treated by an outside physician using peritoneal dialysis for 3 years until he underwent renal transplantation in 2004 with a cadaveric organ. Other remarkable medical conditions included posttransplantation diabetes, hyperlipidemia, and gout. His multidrug regimen included 2 immunosuppressive medications: oral cyclosporine 125 mg twice daily and oral mycophenolate mofetil 250 mg twice daily.
A broad, irregular, black, pigmented, subungual band was noted on the left third finger. The lesion appeared to emanate from below the nail cuticle and traveled along the nail longitudinally toward the distal tip. The band appeared darker at the edge adjacent to the lateral nail fold and grew lighter near the middle of the nail where its free edge was noted to be irregular. A slightly thickened lateral nail fold with an irregular, small, sawtoothlike hyperkeratosis and hyperpigmentation also was noted (Figure 1).

Subungual melanoma, onychomycosis, squamous cell carcinoma (SCC), and a verruca copresenting with onychomycosis were considered in the differential diagnosis. The patient underwent nail avulsion and biopsy of the nail bed as well as the nail matrix. Histopathology was notable for malignant dyskeratosis with a lack of nuclear maturation, occasional mitoses, multinucleation, and individual cell keratinization (Figure 2). Immunostaining for S100 was negative, while staining for cytokeratins AE1/AE3 was positive. Deposition of melanin pigment in the malignant dyskeratotic cells was noted. Periodic acid–Schiff staining identified pseudohyphae without invasion of the nail plate. A diagnosis of pigmented SCC (pSCC) was made. The patient’s nail also was sent for fungal cultures that later grew Candida glabrata and Candida parapsilosis.
The patient underwent Mohs micrographic surgery for removal of the pSCC, which was found to be more extensive than originally suspected and required en bloc excision of the nail repaired with a full-thickness skin graft from the left forearm. The area healed well with some hyperpigmentation (Figure 3).
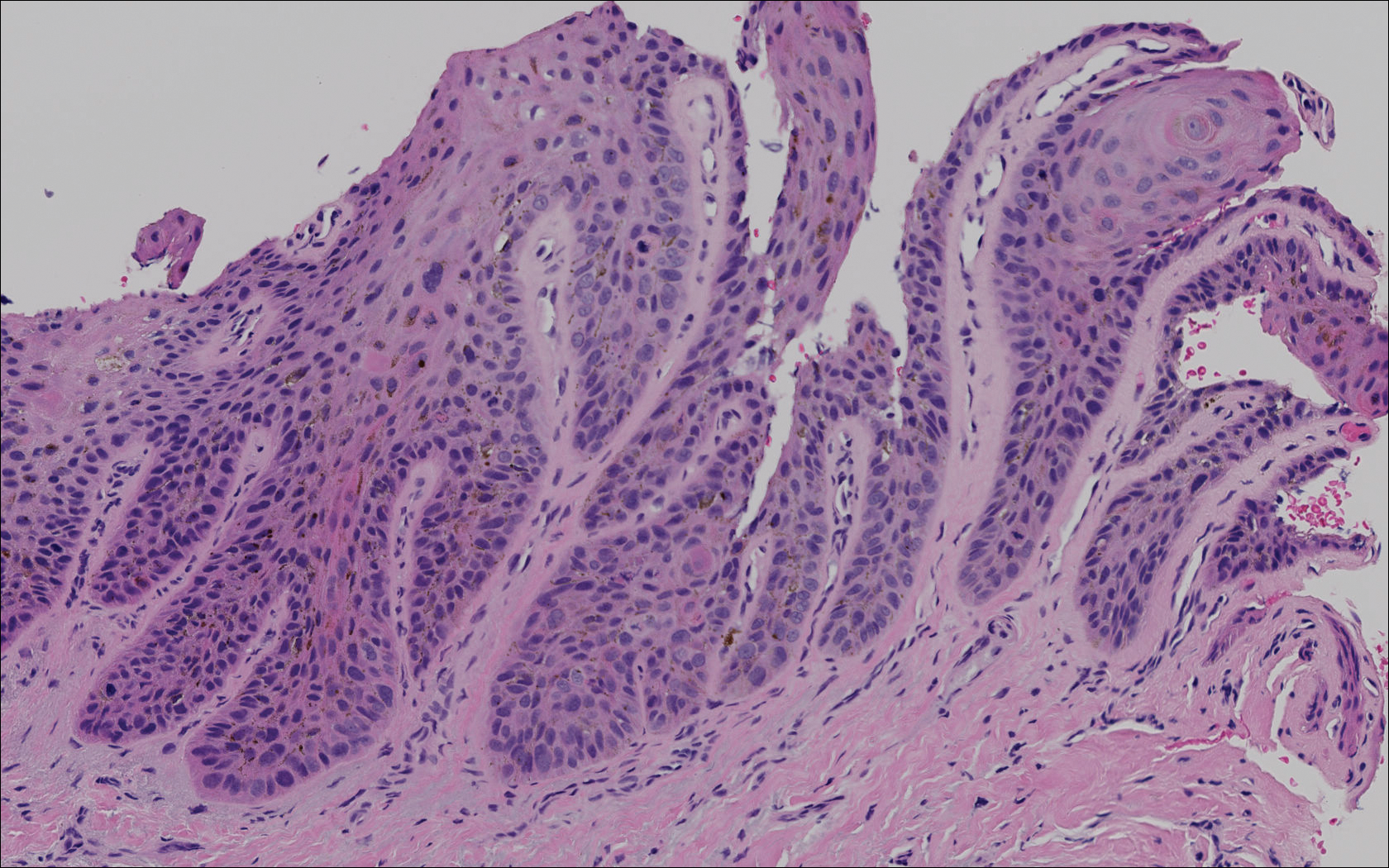

Comment
Among the various types of skin cancer, an estimated 700,000 patients are diagnosed with SCC annually, making it the second most common form of skin cancer in the United States.1 Basal cell carcinoma (BCC) is the most common skin cancer among whites in the United States, while in contrast SCC is the most common skin cancer in patients with skin of color.2 Only an estimated 2% to 5% of all SCCs are pigmented, and this variant is more commonly seen in patients with skin of color.3-5 One analysis of 52 cases of pSCC showed that common features included a flat or slightly raised appearance and hyperpigmentation with varying levels of scaling.6 Studies have shown an altered presentation of pSCC in black skin with increased melanin production and thickness of the stratum corneum in contrast with cases seen in white patients.7 Other potential features include scaling, erosive changes, and sharply demarcated borders. Squamous cell carcinoma typically occurs in sun-exposed areas, reflecting its association with UV light damage; however, SCC in skin of color patients has been noted to occur in sun-protected areas and in areas of chronic scarring.8 Pigmented SCC also appears to follow this distribution, as affected areas are not necessarily in direct exposure to the sun. Pigmented SCCs have been associated with pruritus and/or burning pain, which also was seen in our case when our patient complained of tenderness at the site.
We describe the case of a subungual pSCC clinically presenting as longitudinal melanonychia. Pigmented SCC presenting as longitudinal melanonychia was first described by Baran and Simon in 1988.9 Since that time, it has been reported that approximately 10% of subungual pSCCs clinically present as longitudinal melanonychia.10,11 A retrospective study reviewing 35 cases of SCC of the nail apparatus found that 5 (14.3%) cases presented as longitudinal melanonychia.10 Another retrospective study found that 6 of 51 (11.8%) cases of SCCs affecting the nail unit presented as the warty type of SCC in association with longitudinal melanonychia.12 Cases of pSCC in situ appearing as longitudinal melanonychia also have been reported.13,14
Risk factors for the development of pSCC include advanced age, male sex, presence of human papilloma virus, and use of immunosuppressants.15 Male predominance and advanced age at the time of diagnosis (mean age, 67 years) have been observed in pSCC cases.16 It is now well established that renal transplant recipients have an increased risk of SCC, with a reported incidence rate of 5% to 6%.16 When these patients develop an SCC, they typically follow a more aggressive course. Renal transplantation has a higher ratio than cardiac transplantation for SCC development (2.37:1), whereas cardiac transplantation is associated with a higher risk of BCC development.17 A study of 384 transplant recipients found that 96 (25.0%) had a postsurgical nonmelanoma skin cancer (NMSC), with a ratio of SCC to BCC of 1.2:1.16 The calculated incidence of NMSC at 10 and 20 years posttransplantation was 24.2% and 54.4%, respectively. Another study also determined that SCC rates (50.0%) in postrenal transplant recipients were approximately twice that of BCC (27.0%).18
A daily regimen of immunosuppressive medications such as cyclosporine and mycophenolate mofetil showed an increased risk for development of NMSC.15 Immunosuppressive medications play an important role in the pathogenesis of SCC due to a direct oncogenic effect as well as impairment of the immune system’s ability to fight precancerous developments.15 A 4-year study of 100 renal transplant recipients using mycophenolate mofetil as part of an immunosuppressive regimen reported 22% NMSC findings among 9 patients.19 On average, patients developed an NMSC approximately 61 months posttransplantation, with a wide range from 2 to 120 months.
Advanced age was another important risk factor, with each decade of life producing a 60% increase in instantaneous risk of SCC development for transplant recipients.15 A steady increase in risk was related to the length of time adhering to an immunosuppressive regimen, especially from 2 to 6 years, and then remaining constant in subsequent years. For older patients on immunosuppressant regimens for more than 8 years, the calculated relative risk was noted to be over 200 times greater than the normal population’s development of skin cancers.18
Conclusion
Although cases of pSCC presenting as longitudinal melanonychia have previously been reported,9-14,20 our case is unique in that it describes pSCC in a renal transplant recipient. Our patient had many of the known risk factors for the development of pSCC including male sex, advanced age, skin of color, history of renal transplantation, and immunosuppressive therapy. Although regular full-body skin examinations are an accepted part of renal transplantation follow-up due to SCC risk, our case emphasizes the need to remain vigilant due to possible atypical presentations among the immunosuppressed. The nail unit should not be overlooked during the clinical examination of renal transplant recipients as demonstrated by our patient’s rare presentation of pSCC in the nail.
- Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012 [published online February 1, 2013]. J Am Acad Dermatol. 2013;68:957-966.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- McCall CO, Chen SC. Squamous cell carcinoma of the legs in African Americans. J Am Acad Dermatol. 2002;47:524-529.
- Krishna R, Lewis A, Orengo IF, et al. Pigmented Bowen’s disease (squamous cell carcinoma in situ): a mimic of malignant melanoma. Dermatol Surg. 2001;27:673-674.
- Brinca A, Teixeira V, Goncalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-818.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease. J Am Acad Dermatol. 2010;62:597-604.
- Singh B, Bhaya M, Shaha A, et al. Presentation, course, and outcome of head and neck cancers in African Americans: a case-control study. Laryngoscope. 1998;108(8 pt 1):1159-1163.
- Cancer Facts and Figures 2006. Atlanta, GA: American Cancer Society; 2006.
- Baran R, Simon C. Longitudinal melanonychia: a symptom of Bowen’s disease. J Am Acad Dermatol. 1988;18:1359-1360.
- Dalle S, Depape L, Phan A, et al. Squamous cell carcinoma of the nail apparatus: clinicopathological study of 35 cases. Br J Dermatol. 2007;156:871-874.
- Ishida M, Iwai M, Yoshida K, et al. Subungual pigmented squamous cell carcinoma presenting as longitudinal melanonychia: a case report with review of the literature. Int J Clin Exp Pathol. 2014;7:844-847.
- Lecerf P, Richert B, Theunis A, et al. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol. 2013;69:253-261.
- Saito T, Uchi H, Moroi Y, et al. Subungual Bowen disease revealed by longitudinal melanonychia. J Am Acad Dermatol. 2012;67:E240-E241.
- Saxena A, Kasper DA, Campanelli CD, et al. Pigmented Bowen’s disease clinically mimicking melanoma on the nail. Dermatol Surg. 2006;32:1522-1525.
- Mackenzie KA, Wells JE, Lynn KL, et al. First and subsequent nonmelanoma skin cancers: incidence and predictors in a population of New Zealand renal transplant recipients. Nephrol Dial Transplant. 2010;25:300-306.
- Gutiérrez-Mendoza D, Narro-Llorente R, Karam-Orantes M, et al. Dermoscopy clues in pigmented Bowen’s disease [published online ahead of print September 16, 2010]. Dermatol Res Pract. 2010;2010.
- Euvards S, Kanitakis J, Pouteil-Noble C, et al. Comparative epidemiologic study of premalignant and malignant epithelial cutaneous lesions developing after kidney and heart transplantation. J Am Acad Dermatol. 1995;33(2 pt 1):222-229.
- Moloney FJ, Comber H, O’Lorcain P, et al. A population-based study of skin cancer incidence and prevalence in renal transplant patients. Br J Dermatol. 2006;154:498-504.
- Formicone F, Fargnoli MC, Pisani F, et al. Cutaneous manifestations in Italian kidney transplant recipients. Transplant Proc. 2005;37:2527-2528.
- Fernandes Massa A, Debarbieux S, Depaepe L, et al. Pigmented squamous cell carcinoma of the nail bed presenting as a melanonychia striata: diagnosis by perioperative reflectance confocal microscopy. Br J Dermatol. 2013;169:198-199.
Case Report
A 62-year-old black man presented for examination of a dark longitudinal streak located adjacent to the lateral nail fold on the third finger of the left hand. The lesion had been present for several months, during which time it had slowly expanded in size. The fingertip had recently become tender, which interfered with the patient’s ability to work. His past medical history was remarkable for end-stage renal disease secondary to glomerulonephritis with nephrotic syndrome of unclear etiology. He initially was treated by an outside physician using peritoneal dialysis for 3 years until he underwent renal transplantation in 2004 with a cadaveric organ. Other remarkable medical conditions included posttransplantation diabetes, hyperlipidemia, and gout. His multidrug regimen included 2 immunosuppressive medications: oral cyclosporine 125 mg twice daily and oral mycophenolate mofetil 250 mg twice daily.
A broad, irregular, black, pigmented, subungual band was noted on the left third finger. The lesion appeared to emanate from below the nail cuticle and traveled along the nail longitudinally toward the distal tip. The band appeared darker at the edge adjacent to the lateral nail fold and grew lighter near the middle of the nail where its free edge was noted to be irregular. A slightly thickened lateral nail fold with an irregular, small, sawtoothlike hyperkeratosis and hyperpigmentation also was noted (Figure 1).

Subungual melanoma, onychomycosis, squamous cell carcinoma (SCC), and a verruca copresenting with onychomycosis were considered in the differential diagnosis. The patient underwent nail avulsion and biopsy of the nail bed as well as the nail matrix. Histopathology was notable for malignant dyskeratosis with a lack of nuclear maturation, occasional mitoses, multinucleation, and individual cell keratinization (Figure 2). Immunostaining for S100 was negative, while staining for cytokeratins AE1/AE3 was positive. Deposition of melanin pigment in the malignant dyskeratotic cells was noted. Periodic acid–Schiff staining identified pseudohyphae without invasion of the nail plate. A diagnosis of pigmented SCC (pSCC) was made. The patient’s nail also was sent for fungal cultures that later grew Candida glabrata and Candida parapsilosis.
The patient underwent Mohs micrographic surgery for removal of the pSCC, which was found to be more extensive than originally suspected and required en bloc excision of the nail repaired with a full-thickness skin graft from the left forearm. The area healed well with some hyperpigmentation (Figure 3).
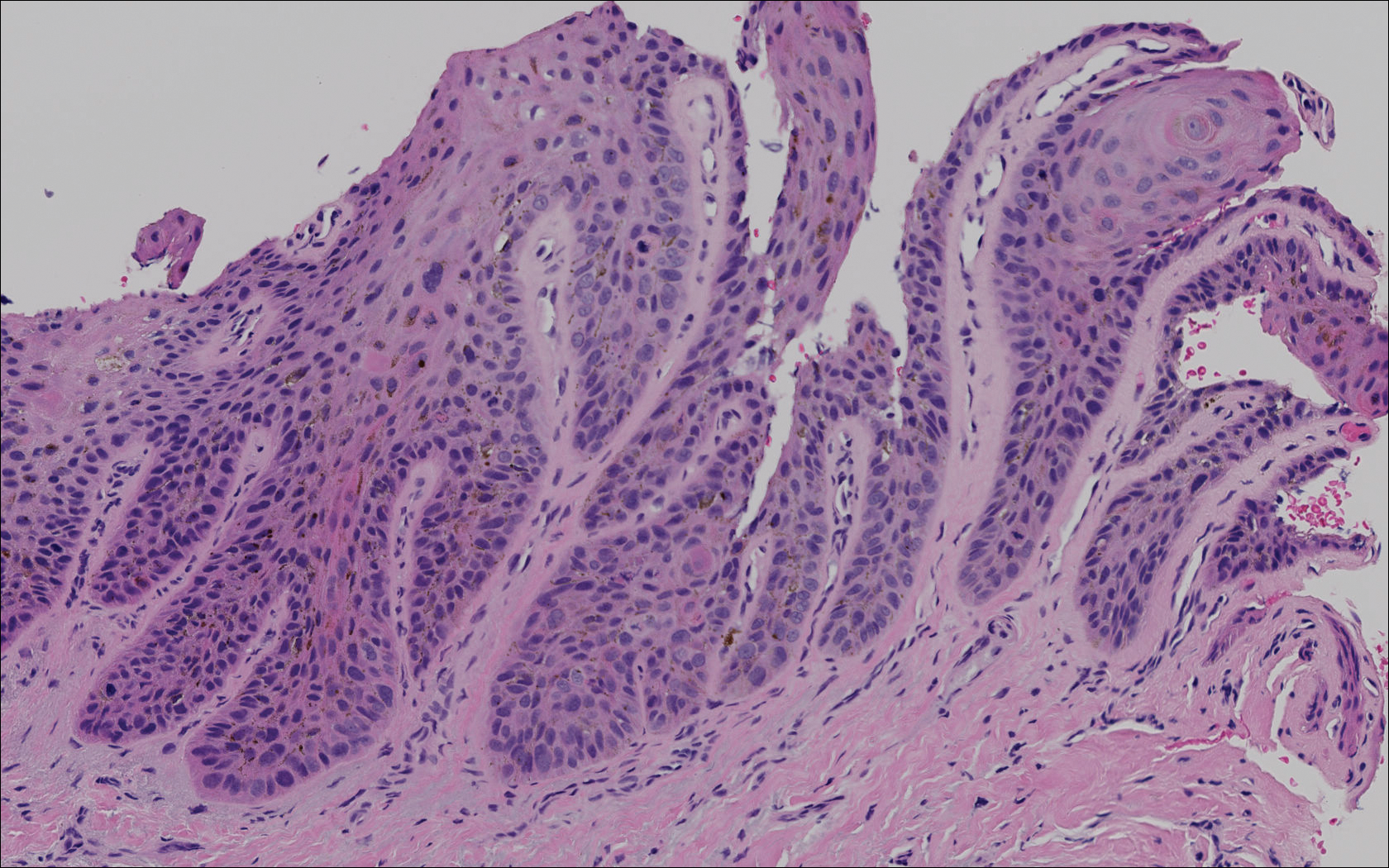

Comment
Among the various types of skin cancer, an estimated 700,000 patients are diagnosed with SCC annually, making it the second most common form of skin cancer in the United States.1 Basal cell carcinoma (BCC) is the most common skin cancer among whites in the United States, while in contrast SCC is the most common skin cancer in patients with skin of color.2 Only an estimated 2% to 5% of all SCCs are pigmented, and this variant is more commonly seen in patients with skin of color.3-5 One analysis of 52 cases of pSCC showed that common features included a flat or slightly raised appearance and hyperpigmentation with varying levels of scaling.6 Studies have shown an altered presentation of pSCC in black skin with increased melanin production and thickness of the stratum corneum in contrast with cases seen in white patients.7 Other potential features include scaling, erosive changes, and sharply demarcated borders. Squamous cell carcinoma typically occurs in sun-exposed areas, reflecting its association with UV light damage; however, SCC in skin of color patients has been noted to occur in sun-protected areas and in areas of chronic scarring.8 Pigmented SCC also appears to follow this distribution, as affected areas are not necessarily in direct exposure to the sun. Pigmented SCCs have been associated with pruritus and/or burning pain, which also was seen in our case when our patient complained of tenderness at the site.
We describe the case of a subungual pSCC clinically presenting as longitudinal melanonychia. Pigmented SCC presenting as longitudinal melanonychia was first described by Baran and Simon in 1988.9 Since that time, it has been reported that approximately 10% of subungual pSCCs clinically present as longitudinal melanonychia.10,11 A retrospective study reviewing 35 cases of SCC of the nail apparatus found that 5 (14.3%) cases presented as longitudinal melanonychia.10 Another retrospective study found that 6 of 51 (11.8%) cases of SCCs affecting the nail unit presented as the warty type of SCC in association with longitudinal melanonychia.12 Cases of pSCC in situ appearing as longitudinal melanonychia also have been reported.13,14
Risk factors for the development of pSCC include advanced age, male sex, presence of human papilloma virus, and use of immunosuppressants.15 Male predominance and advanced age at the time of diagnosis (mean age, 67 years) have been observed in pSCC cases.16 It is now well established that renal transplant recipients have an increased risk of SCC, with a reported incidence rate of 5% to 6%.16 When these patients develop an SCC, they typically follow a more aggressive course. Renal transplantation has a higher ratio than cardiac transplantation for SCC development (2.37:1), whereas cardiac transplantation is associated with a higher risk of BCC development.17 A study of 384 transplant recipients found that 96 (25.0%) had a postsurgical nonmelanoma skin cancer (NMSC), with a ratio of SCC to BCC of 1.2:1.16 The calculated incidence of NMSC at 10 and 20 years posttransplantation was 24.2% and 54.4%, respectively. Another study also determined that SCC rates (50.0%) in postrenal transplant recipients were approximately twice that of BCC (27.0%).18
A daily regimen of immunosuppressive medications such as cyclosporine and mycophenolate mofetil showed an increased risk for development of NMSC.15 Immunosuppressive medications play an important role in the pathogenesis of SCC due to a direct oncogenic effect as well as impairment of the immune system’s ability to fight precancerous developments.15 A 4-year study of 100 renal transplant recipients using mycophenolate mofetil as part of an immunosuppressive regimen reported 22% NMSC findings among 9 patients.19 On average, patients developed an NMSC approximately 61 months posttransplantation, with a wide range from 2 to 120 months.
Advanced age was another important risk factor, with each decade of life producing a 60% increase in instantaneous risk of SCC development for transplant recipients.15 A steady increase in risk was related to the length of time adhering to an immunosuppressive regimen, especially from 2 to 6 years, and then remaining constant in subsequent years. For older patients on immunosuppressant regimens for more than 8 years, the calculated relative risk was noted to be over 200 times greater than the normal population’s development of skin cancers.18
Conclusion
Although cases of pSCC presenting as longitudinal melanonychia have previously been reported,9-14,20 our case is unique in that it describes pSCC in a renal transplant recipient. Our patient had many of the known risk factors for the development of pSCC including male sex, advanced age, skin of color, history of renal transplantation, and immunosuppressive therapy. Although regular full-body skin examinations are an accepted part of renal transplantation follow-up due to SCC risk, our case emphasizes the need to remain vigilant due to possible atypical presentations among the immunosuppressed. The nail unit should not be overlooked during the clinical examination of renal transplant recipients as demonstrated by our patient’s rare presentation of pSCC in the nail.
Case Report
A 62-year-old black man presented for examination of a dark longitudinal streak located adjacent to the lateral nail fold on the third finger of the left hand. The lesion had been present for several months, during which time it had slowly expanded in size. The fingertip had recently become tender, which interfered with the patient’s ability to work. His past medical history was remarkable for end-stage renal disease secondary to glomerulonephritis with nephrotic syndrome of unclear etiology. He initially was treated by an outside physician using peritoneal dialysis for 3 years until he underwent renal transplantation in 2004 with a cadaveric organ. Other remarkable medical conditions included posttransplantation diabetes, hyperlipidemia, and gout. His multidrug regimen included 2 immunosuppressive medications: oral cyclosporine 125 mg twice daily and oral mycophenolate mofetil 250 mg twice daily.
A broad, irregular, black, pigmented, subungual band was noted on the left third finger. The lesion appeared to emanate from below the nail cuticle and traveled along the nail longitudinally toward the distal tip. The band appeared darker at the edge adjacent to the lateral nail fold and grew lighter near the middle of the nail where its free edge was noted to be irregular. A slightly thickened lateral nail fold with an irregular, small, sawtoothlike hyperkeratosis and hyperpigmentation also was noted (Figure 1).

Subungual melanoma, onychomycosis, squamous cell carcinoma (SCC), and a verruca copresenting with onychomycosis were considered in the differential diagnosis. The patient underwent nail avulsion and biopsy of the nail bed as well as the nail matrix. Histopathology was notable for malignant dyskeratosis with a lack of nuclear maturation, occasional mitoses, multinucleation, and individual cell keratinization (Figure 2). Immunostaining for S100 was negative, while staining for cytokeratins AE1/AE3 was positive. Deposition of melanin pigment in the malignant dyskeratotic cells was noted. Periodic acid–Schiff staining identified pseudohyphae without invasion of the nail plate. A diagnosis of pigmented SCC (pSCC) was made. The patient’s nail also was sent for fungal cultures that later grew Candida glabrata and Candida parapsilosis.
The patient underwent Mohs micrographic surgery for removal of the pSCC, which was found to be more extensive than originally suspected and required en bloc excision of the nail repaired with a full-thickness skin graft from the left forearm. The area healed well with some hyperpigmentation (Figure 3).
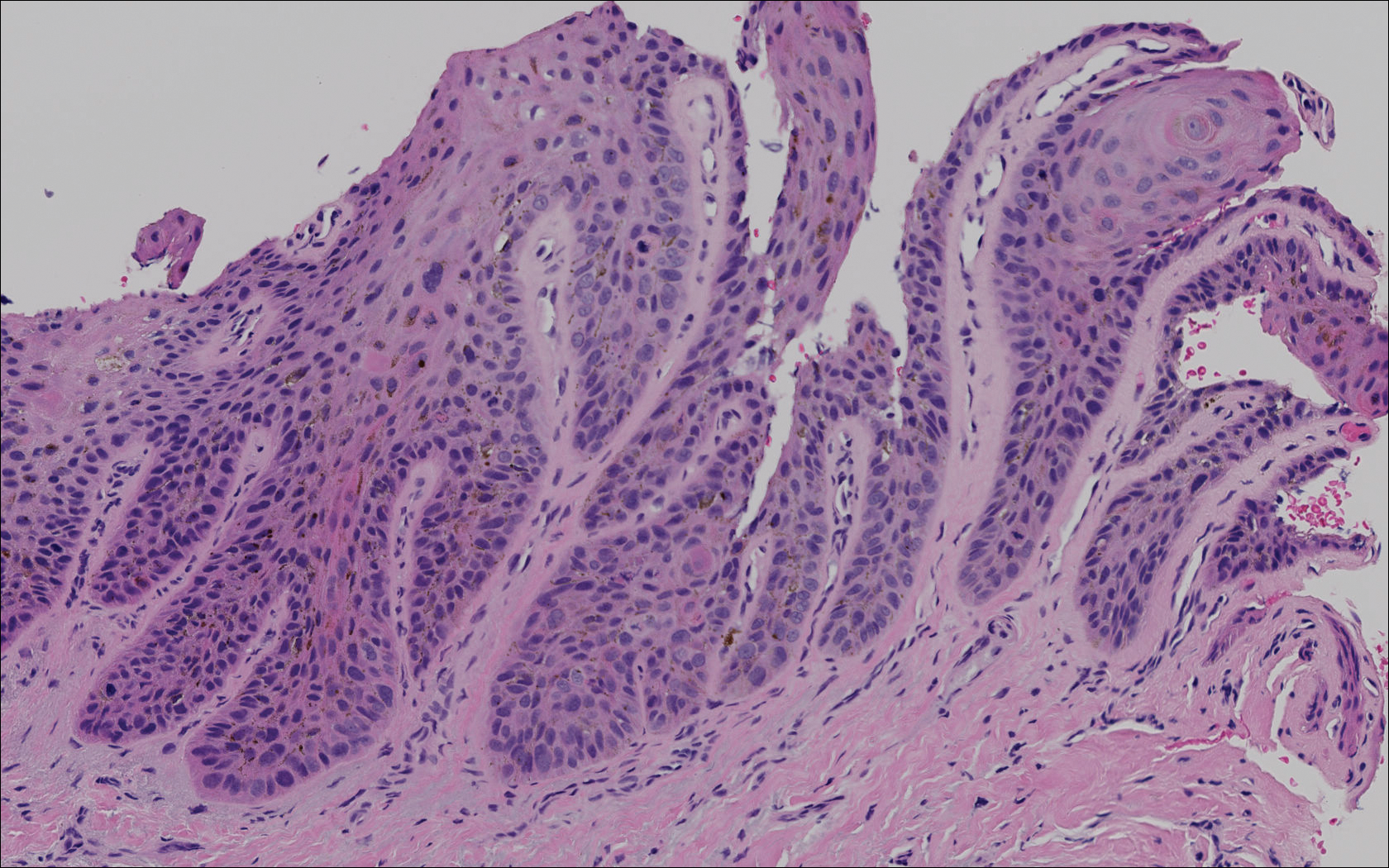

Comment
Among the various types of skin cancer, an estimated 700,000 patients are diagnosed with SCC annually, making it the second most common form of skin cancer in the United States.1 Basal cell carcinoma (BCC) is the most common skin cancer among whites in the United States, while in contrast SCC is the most common skin cancer in patients with skin of color.2 Only an estimated 2% to 5% of all SCCs are pigmented, and this variant is more commonly seen in patients with skin of color.3-5 One analysis of 52 cases of pSCC showed that common features included a flat or slightly raised appearance and hyperpigmentation with varying levels of scaling.6 Studies have shown an altered presentation of pSCC in black skin with increased melanin production and thickness of the stratum corneum in contrast with cases seen in white patients.7 Other potential features include scaling, erosive changes, and sharply demarcated borders. Squamous cell carcinoma typically occurs in sun-exposed areas, reflecting its association with UV light damage; however, SCC in skin of color patients has been noted to occur in sun-protected areas and in areas of chronic scarring.8 Pigmented SCC also appears to follow this distribution, as affected areas are not necessarily in direct exposure to the sun. Pigmented SCCs have been associated with pruritus and/or burning pain, which also was seen in our case when our patient complained of tenderness at the site.
We describe the case of a subungual pSCC clinically presenting as longitudinal melanonychia. Pigmented SCC presenting as longitudinal melanonychia was first described by Baran and Simon in 1988.9 Since that time, it has been reported that approximately 10% of subungual pSCCs clinically present as longitudinal melanonychia.10,11 A retrospective study reviewing 35 cases of SCC of the nail apparatus found that 5 (14.3%) cases presented as longitudinal melanonychia.10 Another retrospective study found that 6 of 51 (11.8%) cases of SCCs affecting the nail unit presented as the warty type of SCC in association with longitudinal melanonychia.12 Cases of pSCC in situ appearing as longitudinal melanonychia also have been reported.13,14
Risk factors for the development of pSCC include advanced age, male sex, presence of human papilloma virus, and use of immunosuppressants.15 Male predominance and advanced age at the time of diagnosis (mean age, 67 years) have been observed in pSCC cases.16 It is now well established that renal transplant recipients have an increased risk of SCC, with a reported incidence rate of 5% to 6%.16 When these patients develop an SCC, they typically follow a more aggressive course. Renal transplantation has a higher ratio than cardiac transplantation for SCC development (2.37:1), whereas cardiac transplantation is associated with a higher risk of BCC development.17 A study of 384 transplant recipients found that 96 (25.0%) had a postsurgical nonmelanoma skin cancer (NMSC), with a ratio of SCC to BCC of 1.2:1.16 The calculated incidence of NMSC at 10 and 20 years posttransplantation was 24.2% and 54.4%, respectively. Another study also determined that SCC rates (50.0%) in postrenal transplant recipients were approximately twice that of BCC (27.0%).18
A daily regimen of immunosuppressive medications such as cyclosporine and mycophenolate mofetil showed an increased risk for development of NMSC.15 Immunosuppressive medications play an important role in the pathogenesis of SCC due to a direct oncogenic effect as well as impairment of the immune system’s ability to fight precancerous developments.15 A 4-year study of 100 renal transplant recipients using mycophenolate mofetil as part of an immunosuppressive regimen reported 22% NMSC findings among 9 patients.19 On average, patients developed an NMSC approximately 61 months posttransplantation, with a wide range from 2 to 120 months.
Advanced age was another important risk factor, with each decade of life producing a 60% increase in instantaneous risk of SCC development for transplant recipients.15 A steady increase in risk was related to the length of time adhering to an immunosuppressive regimen, especially from 2 to 6 years, and then remaining constant in subsequent years. For older patients on immunosuppressant regimens for more than 8 years, the calculated relative risk was noted to be over 200 times greater than the normal population’s development of skin cancers.18
Conclusion
Although cases of pSCC presenting as longitudinal melanonychia have previously been reported,9-14,20 our case is unique in that it describes pSCC in a renal transplant recipient. Our patient had many of the known risk factors for the development of pSCC including male sex, advanced age, skin of color, history of renal transplantation, and immunosuppressive therapy. Although regular full-body skin examinations are an accepted part of renal transplantation follow-up due to SCC risk, our case emphasizes the need to remain vigilant due to possible atypical presentations among the immunosuppressed. The nail unit should not be overlooked during the clinical examination of renal transplant recipients as demonstrated by our patient’s rare presentation of pSCC in the nail.
- Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012 [published online February 1, 2013]. J Am Acad Dermatol. 2013;68:957-966.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- McCall CO, Chen SC. Squamous cell carcinoma of the legs in African Americans. J Am Acad Dermatol. 2002;47:524-529.
- Krishna R, Lewis A, Orengo IF, et al. Pigmented Bowen’s disease (squamous cell carcinoma in situ): a mimic of malignant melanoma. Dermatol Surg. 2001;27:673-674.
- Brinca A, Teixeira V, Goncalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-818.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease. J Am Acad Dermatol. 2010;62:597-604.
- Singh B, Bhaya M, Shaha A, et al. Presentation, course, and outcome of head and neck cancers in African Americans: a case-control study. Laryngoscope. 1998;108(8 pt 1):1159-1163.
- Cancer Facts and Figures 2006. Atlanta, GA: American Cancer Society; 2006.
- Baran R, Simon C. Longitudinal melanonychia: a symptom of Bowen’s disease. J Am Acad Dermatol. 1988;18:1359-1360.
- Dalle S, Depape L, Phan A, et al. Squamous cell carcinoma of the nail apparatus: clinicopathological study of 35 cases. Br J Dermatol. 2007;156:871-874.
- Ishida M, Iwai M, Yoshida K, et al. Subungual pigmented squamous cell carcinoma presenting as longitudinal melanonychia: a case report with review of the literature. Int J Clin Exp Pathol. 2014;7:844-847.
- Lecerf P, Richert B, Theunis A, et al. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol. 2013;69:253-261.
- Saito T, Uchi H, Moroi Y, et al. Subungual Bowen disease revealed by longitudinal melanonychia. J Am Acad Dermatol. 2012;67:E240-E241.
- Saxena A, Kasper DA, Campanelli CD, et al. Pigmented Bowen’s disease clinically mimicking melanoma on the nail. Dermatol Surg. 2006;32:1522-1525.
- Mackenzie KA, Wells JE, Lynn KL, et al. First and subsequent nonmelanoma skin cancers: incidence and predictors in a population of New Zealand renal transplant recipients. Nephrol Dial Transplant. 2010;25:300-306.
- Gutiérrez-Mendoza D, Narro-Llorente R, Karam-Orantes M, et al. Dermoscopy clues in pigmented Bowen’s disease [published online ahead of print September 16, 2010]. Dermatol Res Pract. 2010;2010.
- Euvards S, Kanitakis J, Pouteil-Noble C, et al. Comparative epidemiologic study of premalignant and malignant epithelial cutaneous lesions developing after kidney and heart transplantation. J Am Acad Dermatol. 1995;33(2 pt 1):222-229.
- Moloney FJ, Comber H, O’Lorcain P, et al. A population-based study of skin cancer incidence and prevalence in renal transplant patients. Br J Dermatol. 2006;154:498-504.
- Formicone F, Fargnoli MC, Pisani F, et al. Cutaneous manifestations in Italian kidney transplant recipients. Transplant Proc. 2005;37:2527-2528.
- Fernandes Massa A, Debarbieux S, Depaepe L, et al. Pigmented squamous cell carcinoma of the nail bed presenting as a melanonychia striata: diagnosis by perioperative reflectance confocal microscopy. Br J Dermatol. 2013;169:198-199.
- Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012 [published online February 1, 2013]. J Am Acad Dermatol. 2013;68:957-966.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- McCall CO, Chen SC. Squamous cell carcinoma of the legs in African Americans. J Am Acad Dermatol. 2002;47:524-529.
- Krishna R, Lewis A, Orengo IF, et al. Pigmented Bowen’s disease (squamous cell carcinoma in situ): a mimic of malignant melanoma. Dermatol Surg. 2001;27:673-674.
- Brinca A, Teixeira V, Goncalo M, et al. A large pigmented lesion mimicking malignant melanoma. Clin Exp Dermatol. 2012;37:817-818.
- Cameron A, Rosendahl C, Tschandl P, et al. Dermatoscopy of pigmented Bowen’s disease. J Am Acad Dermatol. 2010;62:597-604.
- Singh B, Bhaya M, Shaha A, et al. Presentation, course, and outcome of head and neck cancers in African Americans: a case-control study. Laryngoscope. 1998;108(8 pt 1):1159-1163.
- Cancer Facts and Figures 2006. Atlanta, GA: American Cancer Society; 2006.
- Baran R, Simon C. Longitudinal melanonychia: a symptom of Bowen’s disease. J Am Acad Dermatol. 1988;18:1359-1360.
- Dalle S, Depape L, Phan A, et al. Squamous cell carcinoma of the nail apparatus: clinicopathological study of 35 cases. Br J Dermatol. 2007;156:871-874.
- Ishida M, Iwai M, Yoshida K, et al. Subungual pigmented squamous cell carcinoma presenting as longitudinal melanonychia: a case report with review of the literature. Int J Clin Exp Pathol. 2014;7:844-847.
- Lecerf P, Richert B, Theunis A, et al. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol. 2013;69:253-261.
- Saito T, Uchi H, Moroi Y, et al. Subungual Bowen disease revealed by longitudinal melanonychia. J Am Acad Dermatol. 2012;67:E240-E241.
- Saxena A, Kasper DA, Campanelli CD, et al. Pigmented Bowen’s disease clinically mimicking melanoma on the nail. Dermatol Surg. 2006;32:1522-1525.
- Mackenzie KA, Wells JE, Lynn KL, et al. First and subsequent nonmelanoma skin cancers: incidence and predictors in a population of New Zealand renal transplant recipients. Nephrol Dial Transplant. 2010;25:300-306.
- Gutiérrez-Mendoza D, Narro-Llorente R, Karam-Orantes M, et al. Dermoscopy clues in pigmented Bowen’s disease [published online ahead of print September 16, 2010]. Dermatol Res Pract. 2010;2010.
- Euvards S, Kanitakis J, Pouteil-Noble C, et al. Comparative epidemiologic study of premalignant and malignant epithelial cutaneous lesions developing after kidney and heart transplantation. J Am Acad Dermatol. 1995;33(2 pt 1):222-229.
- Moloney FJ, Comber H, O’Lorcain P, et al. A population-based study of skin cancer incidence and prevalence in renal transplant patients. Br J Dermatol. 2006;154:498-504.
- Formicone F, Fargnoli MC, Pisani F, et al. Cutaneous manifestations in Italian kidney transplant recipients. Transplant Proc. 2005;37:2527-2528.
- Fernandes Massa A, Debarbieux S, Depaepe L, et al. Pigmented squamous cell carcinoma of the nail bed presenting as a melanonychia striata: diagnosis by perioperative reflectance confocal microscopy. Br J Dermatol. 2013;169:198-199.
Practice Points
- Risk factors for the development of pigmented squamous cell carcinoma (pSCC) include older age, male sex, and use of immunosuppressant medications.
- Subungual pSCC can present as longitudinal melanonychia and should be considered in the differential diagnosis for melanonychia in patients with skin of color or those who are immunosuppressed.
Discoid Lupus Erythematosus Following Herpes Zoster
Cutaneous manifestations of systemic lupus erythematosus (SLE) can be classified as lupus-specific or lupus-nonspecific skin lesions. Lupus-specific lesions commonly are photodistributed, with involvement of the malar region, arms, and trunk. The development of discoid lupus erythematosus (DLE) in areas of trauma, including sun-exposed skin, is not uncommon and may be associated with an isomorphic response. We present a rare case of an isomorphic response following herpes zoster (HZ) in a young woman undergoing treatment with immunosuppressive agents for SLE and DLE. Potential prophylactic therapy also is discussed.
Case Report
A 19-year-old woman initially presented to an outside dermatologist for evaluation of new-onset scarring alopecia, crusted erythematous plaques on the face and arms, and arthralgia. A punch biopsy of a lesion on the left arm demonstrated a lichenoid and perivascular lymphocytic infiltrate with scattered necrotic keratinocytes, perifollicular inflammation, and focally thickened basement membrane at the dermoepidermal junction consistent with discoid lupus erythematosus (DLE). A laboratory workup for SLE revealed 1:1280 antinuclear antibodies (reference range, negative <1:80) with elevated titers of double-stranded DNA, Smith, ribonucleoprotein, Sjögren syndrome A, and Sjögren syndrome B autoantibodies with low complement levels. Based on these findings, a diagnosis of SLE and DLE was made.
At that time, the patient was started on hydroxychloroquine 200 mg twice daily for SLE. Four days later she developed swelling in both hands and feet, and hydroxychloroquine was stopped due to a presumed adverse reaction; however, her symptoms subsequently were determined to be polyarthritis secondary to a lupus flare. Prednisone 10 mg once daily was then initiated. The patient was encouraged to restart hydroxychloroquine, but she declined.
Over the next 13 months, the patient developed severe photosensitivity, oral ulcers, Raynaud phenomenon, anemia, and nephrotic-range proteinuria. She ultimately was diagnosed by the nephrology department at our institution with mixed diffuse proliferative and membranous glomerulonephritis. Induction therapy with oral mycophenolate mofetil 1000 mg twice daily and prednisone 60 mg once daily was started, followed by the addition of tacrolimus 1 mg twice daily. Despite immunosuppressive therapy, she continued to develop new discoid lesions on the face, chest, and arms. Th
After 4 weeks of treatment with mycophenolate mofetil, prednisone, and tacrolimus, the patient developed a painful vesicular rash on the left breast with extension over the left axilla and scapula in a T3 to T4 dermatomal distribution. A clinical diagnosis of HZ was made, and she was started on intravenous acyclovir 10 mg/kg in dextrose 5% every 8 hours for 4 days followed by oral valacyclovir 1000 mg every 8 hours for 14 days, which led to resolution of the eruption.
Over the next 4 months, the patient continued to experience pain confined to the same dermatomal area as the HZ, which was consistent with postherpetic neuralgia. Mycophenolate mofetil was discontinued after she developed acute liver toxicity attributed to the drug. Upon discontinuation, the patient developed a new pruritic rash on both arms and the back. Physical examination by the dermatology department at our institution revealed diffuse, scaly, hyperpigmented papules and annular plaques with central pink hypopigmentation on the face, ears, anterior chest, arms, hands, and back. On the left anterior chest and back, the distribution was strikingly unilateral and multidermatomal (Figure 1). Upon further questioning, the patient confirmed that the areas of the new rash coincided with areas previously affected by HZ. Histologic examination of a representative lesion from the left lateral breast revealed hyperkeratosis, follicular plugging, a patchy lichenoid and perivascular mononuclear cell infiltrate, and pigment incontinence (Figure 2A). These histologic features were subtle and were not diagnostic for lupus; however, direct immunofluorescence demonstrated a continuous granular band of IgG and C3 along the dermoepidermal junction, confirming the diagnosis of DLE (Figure 2B). The histologic findings and clinical presentation were consistent with the development of DLE in areas of previous trauma from HZ. The patient continues to follow-up with the rheumatology and nephrology departments but was lost to dermatology follow-up.

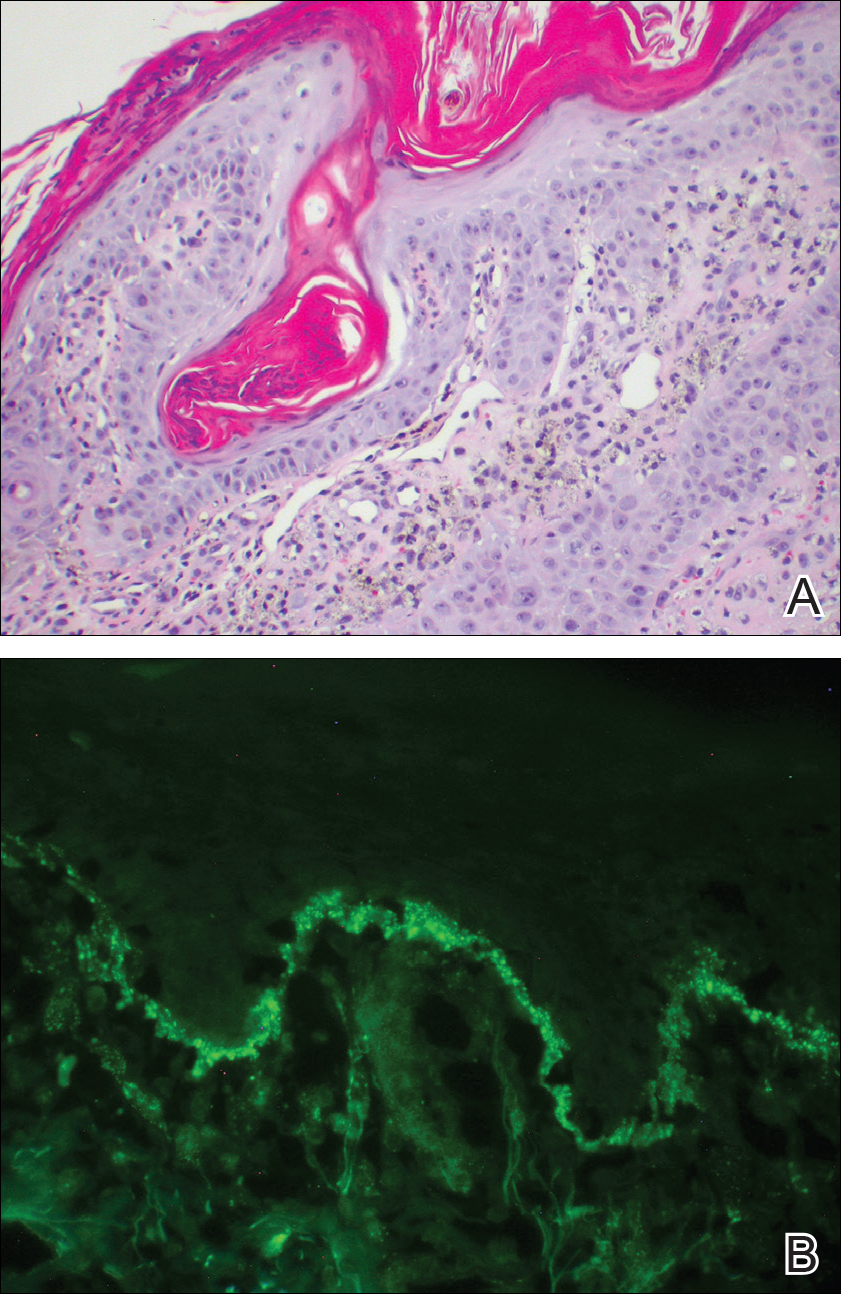
Comment
The pathogenesis of DLE is poorly understood but is thought to be multifactorial, involving genetics, sun exposure, and immune dysregulation.1 Development of DLE lesions in skin traumatized by tattoos, scratches, scars, and prolonged heat exposure has been reported.2 Clarification of the mechanism(s) underlying these traumatized areas may provide insight into the pathophysiology of DLE.
The isomorphic response, also known as the Köbner phenomenon, is the development of a preexisting skin condition at a site of trauma. This phenomenon has been observed in several dermatologic conditions including psoriasis, lichen planus, systemic sclerosis, dermatomyositis, sarcoidosis, vitiligo, and DLE.3 Koebnerization may result from trauma to the skin caused by scratches, sun exposure, radiography, prolonged heat and cold exposure, pressure, tattoos, scars, and inflammatory dermatoses.2,4 Ueki4 suggested that localized trauma to the skin stimulates an immune response that makes the traumatized site a target for a preexisting skin condition. Inflammatory mediators such as IL-1, tumor necrosis factor α, IL-6, and interferon γ have been implicated in the pathophysiology of the isomorphic response.4
Wolf isotopic response is a similar entity that refers to the development of a novel skin condition at the site of a distinct, previously resolved skin disorder. This phenomenon was described by Wolf et al5 in 1995, and since then over 170 cases have been reported.5-7 In most cases the initial skin condition is HZ, although herpes simplex virus has also been implicated. The common resulting skin conditions include granulomatous reactions, malignant tumors, lichen planus, morphea, and infections. The notion that the antecedent skin disease alters the affected site and causes it to be more susceptible to autoimmunity has been proposed as a mechanism for the isotopic response.7,8 While one might consider our presentation of DLE following HZ to be an isotopic response, we believe this case is best classified as an isomorphic response, as the patient already had an established diagnosis of DLE.
The development of DLE at the site of a previous HZ eruption has been described in 2 other cases of young women with SLE.9,10 Unique to our case is the development of a multidermatomal eruption, which may be an indication of her degree of immunosuppression, as immunosuppressed patients are more likely to present with multidermatomal reactivation of varicella zoster virus and postherpetic neuralgia.11 The similarities between our case and the 2 prior reports—including the patients’ age, sex, history of SLE, and degree of immunosuppression—are noteworthy in that they may represent a subset of SLE patients who are predisposed to developing koebnerization following HZ. Physicians should be aware of this phenomenon and consider being proactive in preventing long-term damage.
When feasible, physicians should consider administering the HZ vaccine to reduce the course and severity of HZ before prescribing immunosuppressive agents. When HZ presents in young, immunosuppressed women with a history of SLE, we suggest monitoring the affected sites closely for any evidence of DLE. Topical corticosteroids should be applied to involved areas of the face or body at the earliest appearance of such lesions, which may prevent the isomorphic response and its potentially scarring DLE lesions. This will be our therapeutic approach if we encounter a similar clinical situation in the future. Fur
Acknowledgment
We thank Carolyn E. Grotkowski, MD, from the Department of Pathology, Cooper Medical School of Rowan University, Camden, New Jersey, for her assistance in photographing the pathology slides.
- Lin JH, Dutz JP, Sontheimer RD, et al. Pathophysiology of cutaneous lupus erythematosus. Clinic Rev Allerg Immunol. 2007;33:85-106.
- Ueki H. Köbner phenomenon in lupus erythematosus [in German]. Hautarzt. 1994;45:154-160.
- Boyd AS, Neldner KH. The isomorphic response of Koebner. Int J Dermatol. 1990;29:401-410.
- Ueki H. Koebner phenomenon in lupus erythematosus with special consideration of clinical findings. Autoimmun Rev. 2005;4:219-223.
- Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Wolf R, Wolf D, Ruocco E, et al. Wolf’s isotopic response. Clin Dermatol. 2011;29:237-240.
- Ruocco V, Brunetti G, Puca RV, et al. The immunocompromised district: a unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-1373.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-vs-host disease to sites of skin injury. Arch Dermatol. 2011;147:1081-1086.
- Lee NY, Daniel AS, Dasher DA, et al. Cutaneous lupus after herpes zoster: isomorphic, isotopic, or both [published online May 29, 2012]? Pediatr Dermatol. 2013;30:e110-e113.
- Longhi BS, Centeville M, Marini R, et al. Koebner’s phenomenon in systemic lupus erythematosus. Rheumatol Int. 2012;32:1403-1405.
- Failla V, Jacques J, Castronovo C, et al. Herpes zoster in patients treated with biologicals. Dermatology. 2012;224:251-256.
Cutaneous manifestations of systemic lupus erythematosus (SLE) can be classified as lupus-specific or lupus-nonspecific skin lesions. Lupus-specific lesions commonly are photodistributed, with involvement of the malar region, arms, and trunk. The development of discoid lupus erythematosus (DLE) in areas of trauma, including sun-exposed skin, is not uncommon and may be associated with an isomorphic response. We present a rare case of an isomorphic response following herpes zoster (HZ) in a young woman undergoing treatment with immunosuppressive agents for SLE and DLE. Potential prophylactic therapy also is discussed.
Case Report
A 19-year-old woman initially presented to an outside dermatologist for evaluation of new-onset scarring alopecia, crusted erythematous plaques on the face and arms, and arthralgia. A punch biopsy of a lesion on the left arm demonstrated a lichenoid and perivascular lymphocytic infiltrate with scattered necrotic keratinocytes, perifollicular inflammation, and focally thickened basement membrane at the dermoepidermal junction consistent with discoid lupus erythematosus (DLE). A laboratory workup for SLE revealed 1:1280 antinuclear antibodies (reference range, negative <1:80) with elevated titers of double-stranded DNA, Smith, ribonucleoprotein, Sjögren syndrome A, and Sjögren syndrome B autoantibodies with low complement levels. Based on these findings, a diagnosis of SLE and DLE was made.
At that time, the patient was started on hydroxychloroquine 200 mg twice daily for SLE. Four days later she developed swelling in both hands and feet, and hydroxychloroquine was stopped due to a presumed adverse reaction; however, her symptoms subsequently were determined to be polyarthritis secondary to a lupus flare. Prednisone 10 mg once daily was then initiated. The patient was encouraged to restart hydroxychloroquine, but she declined.
Over the next 13 months, the patient developed severe photosensitivity, oral ulcers, Raynaud phenomenon, anemia, and nephrotic-range proteinuria. She ultimately was diagnosed by the nephrology department at our institution with mixed diffuse proliferative and membranous glomerulonephritis. Induction therapy with oral mycophenolate mofetil 1000 mg twice daily and prednisone 60 mg once daily was started, followed by the addition of tacrolimus 1 mg twice daily. Despite immunosuppressive therapy, she continued to develop new discoid lesions on the face, chest, and arms. Th
After 4 weeks of treatment with mycophenolate mofetil, prednisone, and tacrolimus, the patient developed a painful vesicular rash on the left breast with extension over the left axilla and scapula in a T3 to T4 dermatomal distribution. A clinical diagnosis of HZ was made, and she was started on intravenous acyclovir 10 mg/kg in dextrose 5% every 8 hours for 4 days followed by oral valacyclovir 1000 mg every 8 hours for 14 days, which led to resolution of the eruption.
Over the next 4 months, the patient continued to experience pain confined to the same dermatomal area as the HZ, which was consistent with postherpetic neuralgia. Mycophenolate mofetil was discontinued after she developed acute liver toxicity attributed to the drug. Upon discontinuation, the patient developed a new pruritic rash on both arms and the back. Physical examination by the dermatology department at our institution revealed diffuse, scaly, hyperpigmented papules and annular plaques with central pink hypopigmentation on the face, ears, anterior chest, arms, hands, and back. On the left anterior chest and back, the distribution was strikingly unilateral and multidermatomal (Figure 1). Upon further questioning, the patient confirmed that the areas of the new rash coincided with areas previously affected by HZ. Histologic examination of a representative lesion from the left lateral breast revealed hyperkeratosis, follicular plugging, a patchy lichenoid and perivascular mononuclear cell infiltrate, and pigment incontinence (Figure 2A). These histologic features were subtle and were not diagnostic for lupus; however, direct immunofluorescence demonstrated a continuous granular band of IgG and C3 along the dermoepidermal junction, confirming the diagnosis of DLE (Figure 2B). The histologic findings and clinical presentation were consistent with the development of DLE in areas of previous trauma from HZ. The patient continues to follow-up with the rheumatology and nephrology departments but was lost to dermatology follow-up.

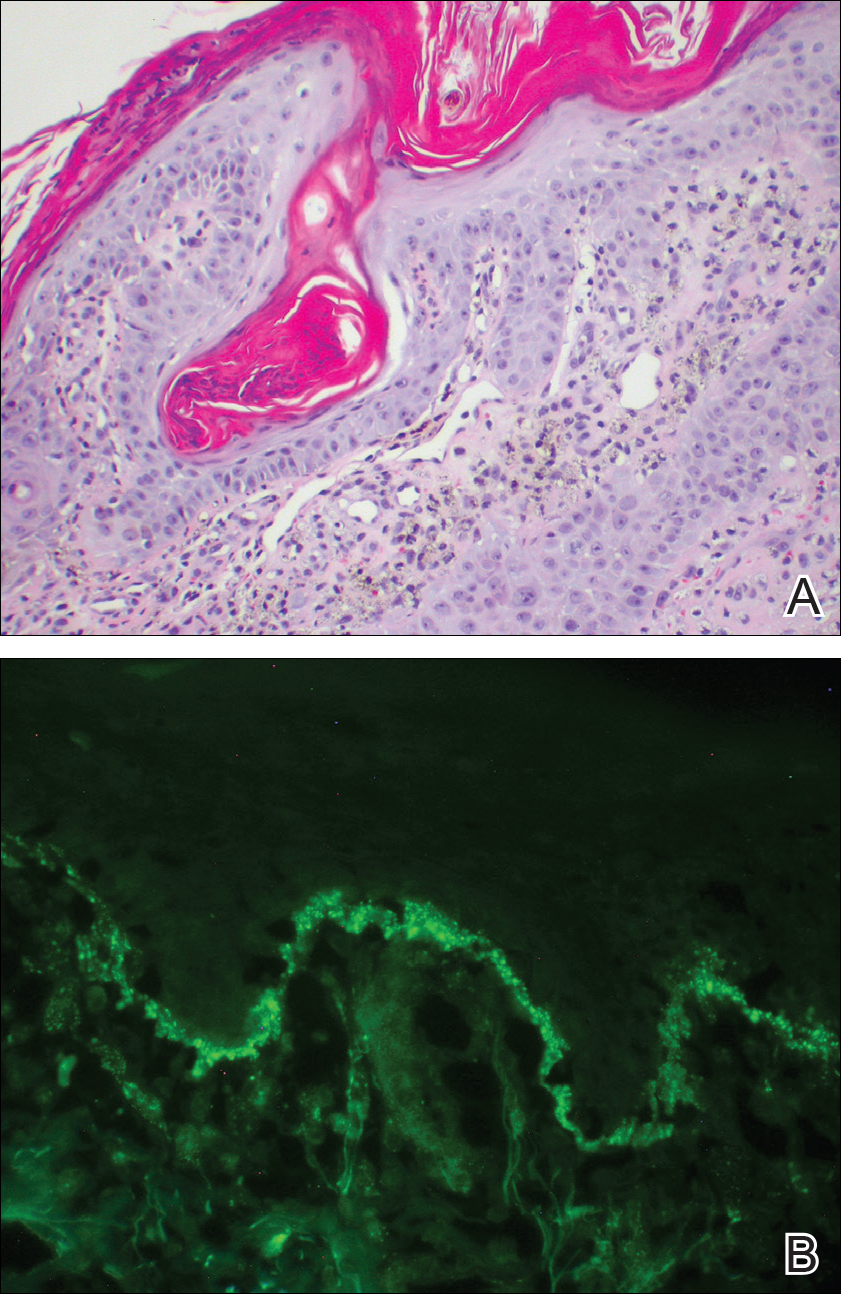
Comment
The pathogenesis of DLE is poorly understood but is thought to be multifactorial, involving genetics, sun exposure, and immune dysregulation.1 Development of DLE lesions in skin traumatized by tattoos, scratches, scars, and prolonged heat exposure has been reported.2 Clarification of the mechanism(s) underlying these traumatized areas may provide insight into the pathophysiology of DLE.
The isomorphic response, also known as the Köbner phenomenon, is the development of a preexisting skin condition at a site of trauma. This phenomenon has been observed in several dermatologic conditions including psoriasis, lichen planus, systemic sclerosis, dermatomyositis, sarcoidosis, vitiligo, and DLE.3 Koebnerization may result from trauma to the skin caused by scratches, sun exposure, radiography, prolonged heat and cold exposure, pressure, tattoos, scars, and inflammatory dermatoses.2,4 Ueki4 suggested that localized trauma to the skin stimulates an immune response that makes the traumatized site a target for a preexisting skin condition. Inflammatory mediators such as IL-1, tumor necrosis factor α, IL-6, and interferon γ have been implicated in the pathophysiology of the isomorphic response.4
Wolf isotopic response is a similar entity that refers to the development of a novel skin condition at the site of a distinct, previously resolved skin disorder. This phenomenon was described by Wolf et al5 in 1995, and since then over 170 cases have been reported.5-7 In most cases the initial skin condition is HZ, although herpes simplex virus has also been implicated. The common resulting skin conditions include granulomatous reactions, malignant tumors, lichen planus, morphea, and infections. The notion that the antecedent skin disease alters the affected site and causes it to be more susceptible to autoimmunity has been proposed as a mechanism for the isotopic response.7,8 While one might consider our presentation of DLE following HZ to be an isotopic response, we believe this case is best classified as an isomorphic response, as the patient already had an established diagnosis of DLE.
The development of DLE at the site of a previous HZ eruption has been described in 2 other cases of young women with SLE.9,10 Unique to our case is the development of a multidermatomal eruption, which may be an indication of her degree of immunosuppression, as immunosuppressed patients are more likely to present with multidermatomal reactivation of varicella zoster virus and postherpetic neuralgia.11 The similarities between our case and the 2 prior reports—including the patients’ age, sex, history of SLE, and degree of immunosuppression—are noteworthy in that they may represent a subset of SLE patients who are predisposed to developing koebnerization following HZ. Physicians should be aware of this phenomenon and consider being proactive in preventing long-term damage.
When feasible, physicians should consider administering the HZ vaccine to reduce the course and severity of HZ before prescribing immunosuppressive agents. When HZ presents in young, immunosuppressed women with a history of SLE, we suggest monitoring the affected sites closely for any evidence of DLE. Topical corticosteroids should be applied to involved areas of the face or body at the earliest appearance of such lesions, which may prevent the isomorphic response and its potentially scarring DLE lesions. This will be our therapeutic approach if we encounter a similar clinical situation in the future. Fur
Acknowledgment
We thank Carolyn E. Grotkowski, MD, from the Department of Pathology, Cooper Medical School of Rowan University, Camden, New Jersey, for her assistance in photographing the pathology slides.
Cutaneous manifestations of systemic lupus erythematosus (SLE) can be classified as lupus-specific or lupus-nonspecific skin lesions. Lupus-specific lesions commonly are photodistributed, with involvement of the malar region, arms, and trunk. The development of discoid lupus erythematosus (DLE) in areas of trauma, including sun-exposed skin, is not uncommon and may be associated with an isomorphic response. We present a rare case of an isomorphic response following herpes zoster (HZ) in a young woman undergoing treatment with immunosuppressive agents for SLE and DLE. Potential prophylactic therapy also is discussed.
Case Report
A 19-year-old woman initially presented to an outside dermatologist for evaluation of new-onset scarring alopecia, crusted erythematous plaques on the face and arms, and arthralgia. A punch biopsy of a lesion on the left arm demonstrated a lichenoid and perivascular lymphocytic infiltrate with scattered necrotic keratinocytes, perifollicular inflammation, and focally thickened basement membrane at the dermoepidermal junction consistent with discoid lupus erythematosus (DLE). A laboratory workup for SLE revealed 1:1280 antinuclear antibodies (reference range, negative <1:80) with elevated titers of double-stranded DNA, Smith, ribonucleoprotein, Sjögren syndrome A, and Sjögren syndrome B autoantibodies with low complement levels. Based on these findings, a diagnosis of SLE and DLE was made.
At that time, the patient was started on hydroxychloroquine 200 mg twice daily for SLE. Four days later she developed swelling in both hands and feet, and hydroxychloroquine was stopped due to a presumed adverse reaction; however, her symptoms subsequently were determined to be polyarthritis secondary to a lupus flare. Prednisone 10 mg once daily was then initiated. The patient was encouraged to restart hydroxychloroquine, but she declined.
Over the next 13 months, the patient developed severe photosensitivity, oral ulcers, Raynaud phenomenon, anemia, and nephrotic-range proteinuria. She ultimately was diagnosed by the nephrology department at our institution with mixed diffuse proliferative and membranous glomerulonephritis. Induction therapy with oral mycophenolate mofetil 1000 mg twice daily and prednisone 60 mg once daily was started, followed by the addition of tacrolimus 1 mg twice daily. Despite immunosuppressive therapy, she continued to develop new discoid lesions on the face, chest, and arms. Th
After 4 weeks of treatment with mycophenolate mofetil, prednisone, and tacrolimus, the patient developed a painful vesicular rash on the left breast with extension over the left axilla and scapula in a T3 to T4 dermatomal distribution. A clinical diagnosis of HZ was made, and she was started on intravenous acyclovir 10 mg/kg in dextrose 5% every 8 hours for 4 days followed by oral valacyclovir 1000 mg every 8 hours for 14 days, which led to resolution of the eruption.
Over the next 4 months, the patient continued to experience pain confined to the same dermatomal area as the HZ, which was consistent with postherpetic neuralgia. Mycophenolate mofetil was discontinued after she developed acute liver toxicity attributed to the drug. Upon discontinuation, the patient developed a new pruritic rash on both arms and the back. Physical examination by the dermatology department at our institution revealed diffuse, scaly, hyperpigmented papules and annular plaques with central pink hypopigmentation on the face, ears, anterior chest, arms, hands, and back. On the left anterior chest and back, the distribution was strikingly unilateral and multidermatomal (Figure 1). Upon further questioning, the patient confirmed that the areas of the new rash coincided with areas previously affected by HZ. Histologic examination of a representative lesion from the left lateral breast revealed hyperkeratosis, follicular plugging, a patchy lichenoid and perivascular mononuclear cell infiltrate, and pigment incontinence (Figure 2A). These histologic features were subtle and were not diagnostic for lupus; however, direct immunofluorescence demonstrated a continuous granular band of IgG and C3 along the dermoepidermal junction, confirming the diagnosis of DLE (Figure 2B). The histologic findings and clinical presentation were consistent with the development of DLE in areas of previous trauma from HZ. The patient continues to follow-up with the rheumatology and nephrology departments but was lost to dermatology follow-up.

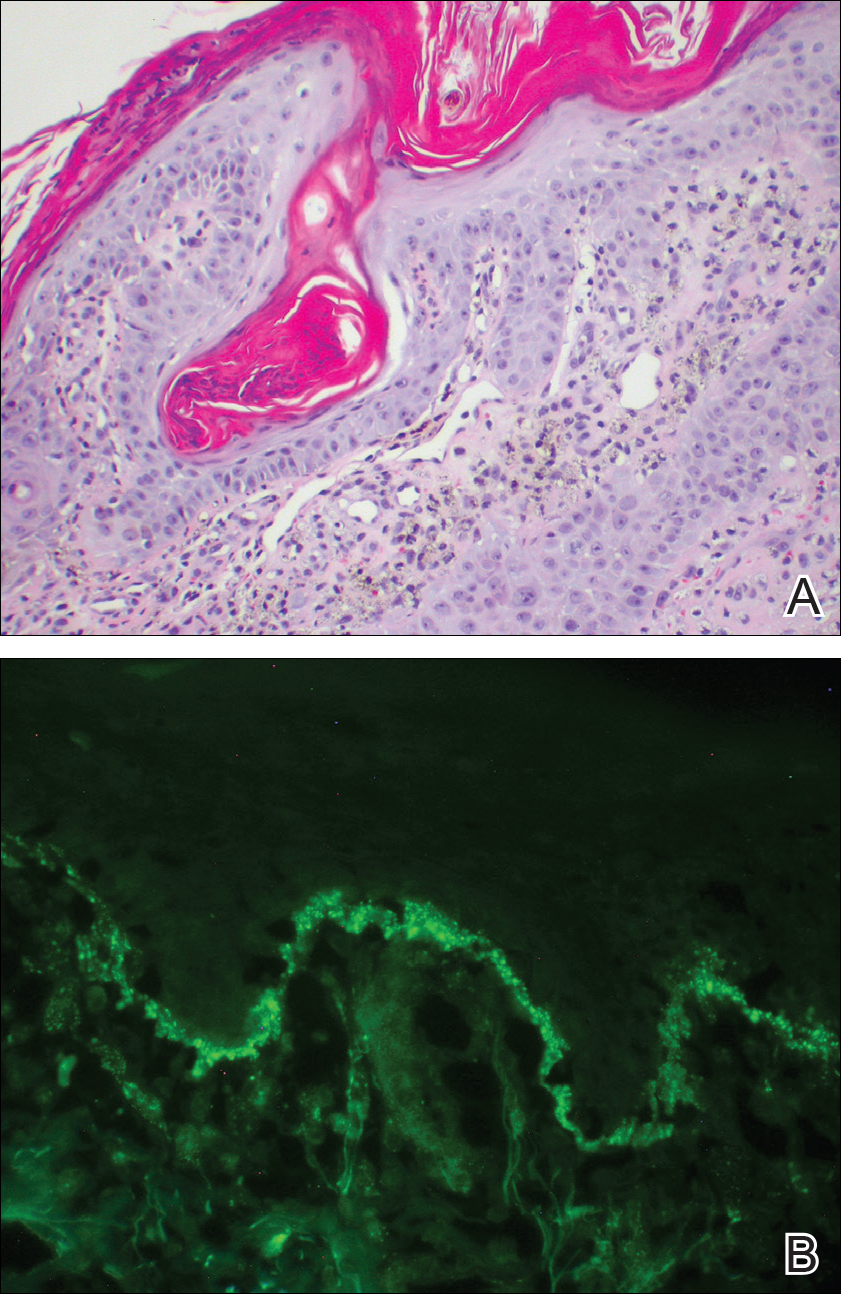
Comment
The pathogenesis of DLE is poorly understood but is thought to be multifactorial, involving genetics, sun exposure, and immune dysregulation.1 Development of DLE lesions in skin traumatized by tattoos, scratches, scars, and prolonged heat exposure has been reported.2 Clarification of the mechanism(s) underlying these traumatized areas may provide insight into the pathophysiology of DLE.
The isomorphic response, also known as the Köbner phenomenon, is the development of a preexisting skin condition at a site of trauma. This phenomenon has been observed in several dermatologic conditions including psoriasis, lichen planus, systemic sclerosis, dermatomyositis, sarcoidosis, vitiligo, and DLE.3 Koebnerization may result from trauma to the skin caused by scratches, sun exposure, radiography, prolonged heat and cold exposure, pressure, tattoos, scars, and inflammatory dermatoses.2,4 Ueki4 suggested that localized trauma to the skin stimulates an immune response that makes the traumatized site a target for a preexisting skin condition. Inflammatory mediators such as IL-1, tumor necrosis factor α, IL-6, and interferon γ have been implicated in the pathophysiology of the isomorphic response.4
Wolf isotopic response is a similar entity that refers to the development of a novel skin condition at the site of a distinct, previously resolved skin disorder. This phenomenon was described by Wolf et al5 in 1995, and since then over 170 cases have been reported.5-7 In most cases the initial skin condition is HZ, although herpes simplex virus has also been implicated. The common resulting skin conditions include granulomatous reactions, malignant tumors, lichen planus, morphea, and infections. The notion that the antecedent skin disease alters the affected site and causes it to be more susceptible to autoimmunity has been proposed as a mechanism for the isotopic response.7,8 While one might consider our presentation of DLE following HZ to be an isotopic response, we believe this case is best classified as an isomorphic response, as the patient already had an established diagnosis of DLE.
The development of DLE at the site of a previous HZ eruption has been described in 2 other cases of young women with SLE.9,10 Unique to our case is the development of a multidermatomal eruption, which may be an indication of her degree of immunosuppression, as immunosuppressed patients are more likely to present with multidermatomal reactivation of varicella zoster virus and postherpetic neuralgia.11 The similarities between our case and the 2 prior reports—including the patients’ age, sex, history of SLE, and degree of immunosuppression—are noteworthy in that they may represent a subset of SLE patients who are predisposed to developing koebnerization following HZ. Physicians should be aware of this phenomenon and consider being proactive in preventing long-term damage.
When feasible, physicians should consider administering the HZ vaccine to reduce the course and severity of HZ before prescribing immunosuppressive agents. When HZ presents in young, immunosuppressed women with a history of SLE, we suggest monitoring the affected sites closely for any evidence of DLE. Topical corticosteroids should be applied to involved areas of the face or body at the earliest appearance of such lesions, which may prevent the isomorphic response and its potentially scarring DLE lesions. This will be our therapeutic approach if we encounter a similar clinical situation in the future. Fur
Acknowledgment
We thank Carolyn E. Grotkowski, MD, from the Department of Pathology, Cooper Medical School of Rowan University, Camden, New Jersey, for her assistance in photographing the pathology slides.
- Lin JH, Dutz JP, Sontheimer RD, et al. Pathophysiology of cutaneous lupus erythematosus. Clinic Rev Allerg Immunol. 2007;33:85-106.
- Ueki H. Köbner phenomenon in lupus erythematosus [in German]. Hautarzt. 1994;45:154-160.
- Boyd AS, Neldner KH. The isomorphic response of Koebner. Int J Dermatol. 1990;29:401-410.
- Ueki H. Koebner phenomenon in lupus erythematosus with special consideration of clinical findings. Autoimmun Rev. 2005;4:219-223.
- Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Wolf R, Wolf D, Ruocco E, et al. Wolf’s isotopic response. Clin Dermatol. 2011;29:237-240.
- Ruocco V, Brunetti G, Puca RV, et al. The immunocompromised district: a unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-1373.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-vs-host disease to sites of skin injury. Arch Dermatol. 2011;147:1081-1086.
- Lee NY, Daniel AS, Dasher DA, et al. Cutaneous lupus after herpes zoster: isomorphic, isotopic, or both [published online May 29, 2012]? Pediatr Dermatol. 2013;30:e110-e113.
- Longhi BS, Centeville M, Marini R, et al. Koebner’s phenomenon in systemic lupus erythematosus. Rheumatol Int. 2012;32:1403-1405.
- Failla V, Jacques J, Castronovo C, et al. Herpes zoster in patients treated with biologicals. Dermatology. 2012;224:251-256.
- Lin JH, Dutz JP, Sontheimer RD, et al. Pathophysiology of cutaneous lupus erythematosus. Clinic Rev Allerg Immunol. 2007;33:85-106.
- Ueki H. Köbner phenomenon in lupus erythematosus [in German]. Hautarzt. 1994;45:154-160.
- Boyd AS, Neldner KH. The isomorphic response of Koebner. Int J Dermatol. 1990;29:401-410.
- Ueki H. Koebner phenomenon in lupus erythematosus with special consideration of clinical findings. Autoimmun Rev. 2005;4:219-223.
- Wolf R, Brenner S, Ruocco V, et al. Isotopic response. Int J Dermatol. 1995;34:341-348.
- Wolf R, Wolf D, Ruocco E, et al. Wolf’s isotopic response. Clin Dermatol. 2011;29:237-240.
- Ruocco V, Brunetti G, Puca RV, et al. The immunocompromised district: a unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-1373.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-vs-host disease to sites of skin injury. Arch Dermatol. 2011;147:1081-1086.
- Lee NY, Daniel AS, Dasher DA, et al. Cutaneous lupus after herpes zoster: isomorphic, isotopic, or both [published online May 29, 2012]? Pediatr Dermatol. 2013;30:e110-e113.
- Longhi BS, Centeville M, Marini R, et al. Koebner’s phenomenon in systemic lupus erythematosus. Rheumatol Int. 2012;32:1403-1405.
- Failla V, Jacques J, Castronovo C, et al. Herpes zoster in patients treated with biologicals. Dermatology. 2012;224:251-256.
Practice Points
- Discoid lupus erythematosus (DLE) most commonly presents as scaling and crusted plaques in sun-exposed areas of the face and arms. It also may present in skin traumatized by tattoos, scratches, scars, prolonged heat exposure, andherpes zoster (HZ).
- Patients with a history of DLE who subsequently develop HZ should be followed closely for the development of DLE in HZ-affected dermatomes.
- Following resolution of HZ, topical corticosteroids may have a role in prevention of DLE in HZ-affected dermatomes.














