User login
Celebrating 50 years of Dermatology News
The first issue of Skin & Allergy News, now Dermatology News, was published in January 1970. One front-page story highlighted the "continued improvement and more widespread use of steroids" as the most important development of the 1960s in dermatology. Another covered the launch of a national program for dermatology "to design a pattern for its future instead of simply drifting and letting its fate be determined by others."
Throughout 2020, look for articles and features marking the publication's golden anniversary. And read the first ever issue in the PDF above.
The first issue of Skin & Allergy News, now Dermatology News, was published in January 1970. One front-page story highlighted the "continued improvement and more widespread use of steroids" as the most important development of the 1960s in dermatology. Another covered the launch of a national program for dermatology "to design a pattern for its future instead of simply drifting and letting its fate be determined by others."
Throughout 2020, look for articles and features marking the publication's golden anniversary. And read the first ever issue in the PDF above.
The first issue of Skin & Allergy News, now Dermatology News, was published in January 1970. One front-page story highlighted the "continued improvement and more widespread use of steroids" as the most important development of the 1960s in dermatology. Another covered the launch of a national program for dermatology "to design a pattern for its future instead of simply drifting and letting its fate be determined by others."
Throughout 2020, look for articles and features marking the publication's golden anniversary. And read the first ever issue in the PDF above.
Spring
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
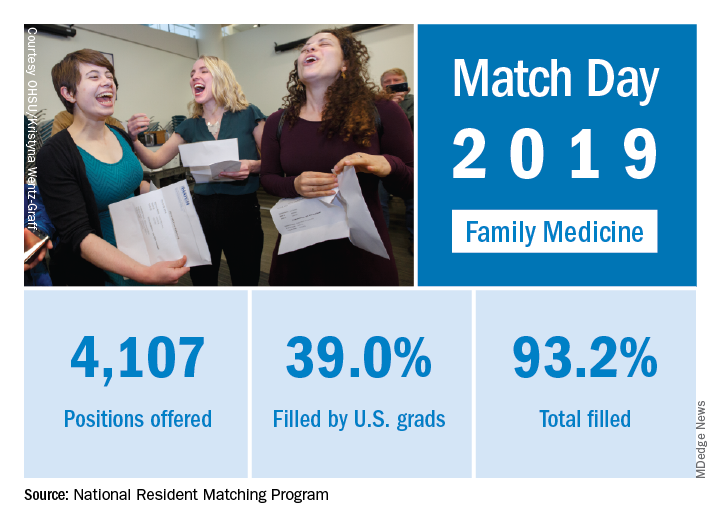
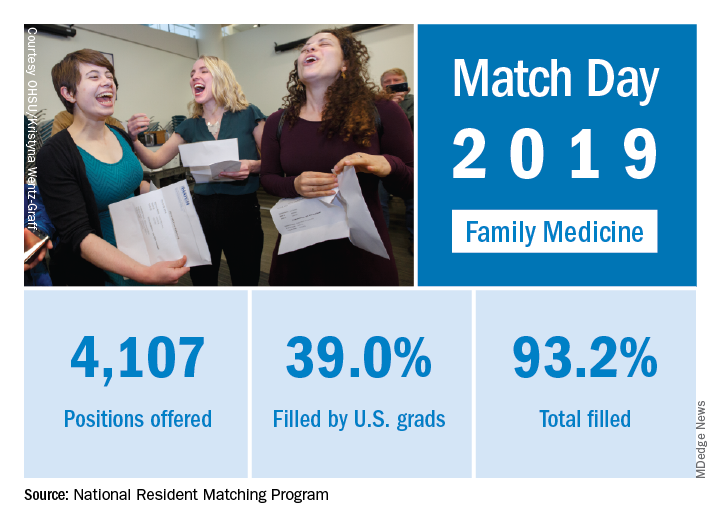
Match Day 2019: Residency spots increase, but improvements needed
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
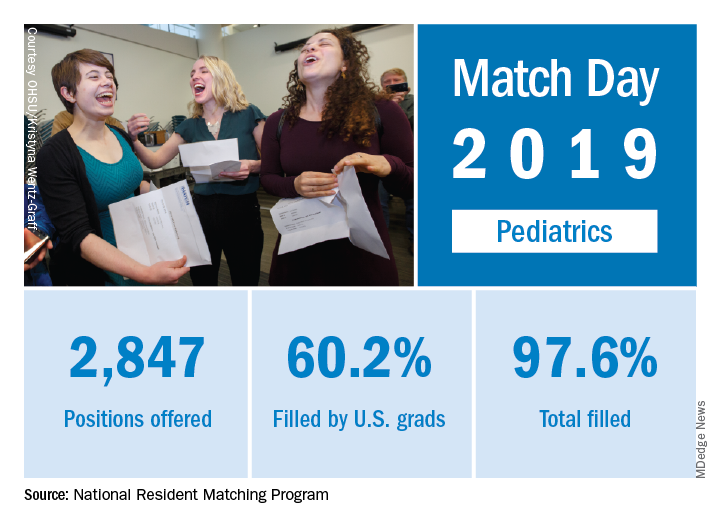
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
Match Day 2019: Pediatrics up from last year
The pediatrics specialty filled 97.6% of its offered positions, according to the National Resident Matching Program (NRMP). Of these, 60.2% were filled by U.S. seniors, which was down from last year’s 63.1%.
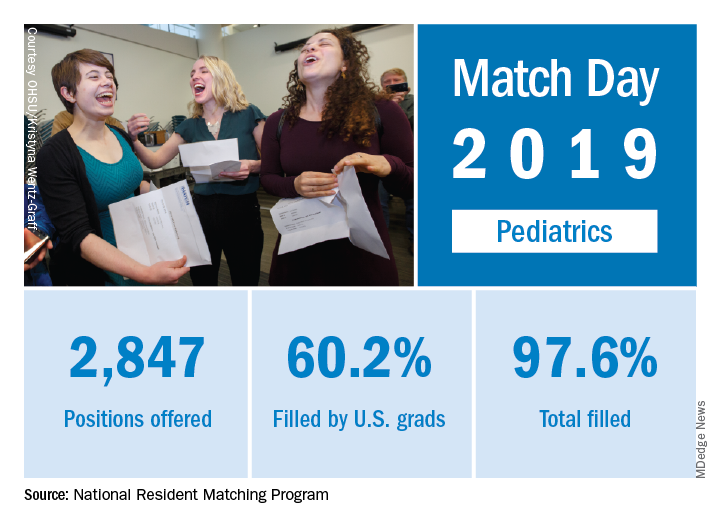
Pediatrics brought 2,847 first-year positions to the 2019 Main Resident Match day, up from 2,768 in 2018. However, a slightly higher proportion (97.9%) of Match Day offerings were filled in 2018 than in 2019. Internal medicine/pediatrics offered 390 positions, more than 2018’s 382 positions. Although a slightly smaller proportion were filled in 2019 (98.2% vs. 98.7% ), a slightly larger proportion of positions in 2019 were filled by U.S. graduates (80.8% in 2019 vs. 80.1% in 2018). For all specialties, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP in its 2019 Main Resident Match report.
Overall, the 2019 Match set a new high for total positions offered at 35,135, for which there were a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
The pediatrics specialty filled 97.6% of its offered positions, according to the National Resident Matching Program (NRMP). Of these, 60.2% were filled by U.S. seniors, which was down from last year’s 63.1%.
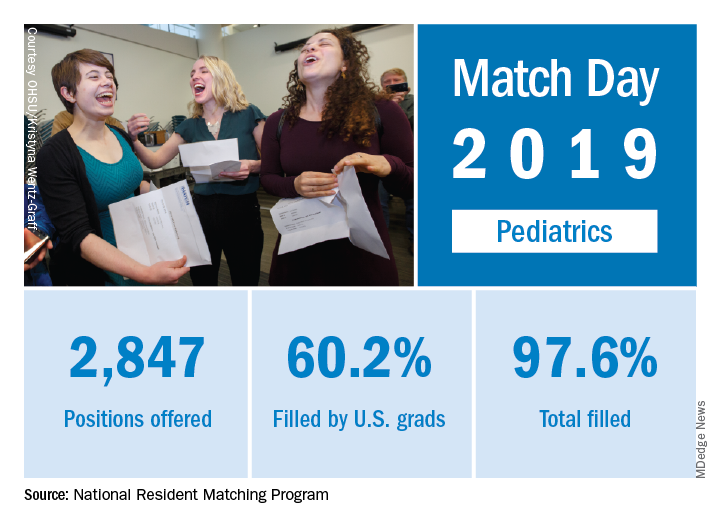
Pediatrics brought 2,847 first-year positions to the 2019 Main Resident Match day, up from 2,768 in 2018. However, a slightly higher proportion (97.9%) of Match Day offerings were filled in 2018 than in 2019. Internal medicine/pediatrics offered 390 positions, more than 2018’s 382 positions. Although a slightly smaller proportion were filled in 2019 (98.2% vs. 98.7% ), a slightly larger proportion of positions in 2019 were filled by U.S. graduates (80.8% in 2019 vs. 80.1% in 2018). For all specialties, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP in its 2019 Main Resident Match report.
Overall, the 2019 Match set a new high for total positions offered at 35,135, for which there were a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
The pediatrics specialty filled 97.6% of its offered positions, according to the National Resident Matching Program (NRMP). Of these, 60.2% were filled by U.S. seniors, which was down from last year’s 63.1%.
Pediatrics brought 2,847 first-year positions to the 2019 Main Resident Match day, up from 2,768 in 2018. However, a slightly higher proportion (97.9%) of Match Day offerings were filled in 2018 than in 2019. Internal medicine/pediatrics offered 390 positions, more than 2018’s 382 positions. Although a slightly smaller proportion were filled in 2019 (98.2% vs. 98.7% ), a slightly larger proportion of positions in 2019 were filled by U.S. graduates (80.8% in 2019 vs. 80.1% in 2018). For all specialties, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP in its 2019 Main Resident Match report.
Overall, the 2019 Match set a new high for total positions offered at 35,135, for which there were a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Match Day 2019: Family medicine slots up by 13%
for the first time since 2009, according to the National Resident Matching Program (NRMP).
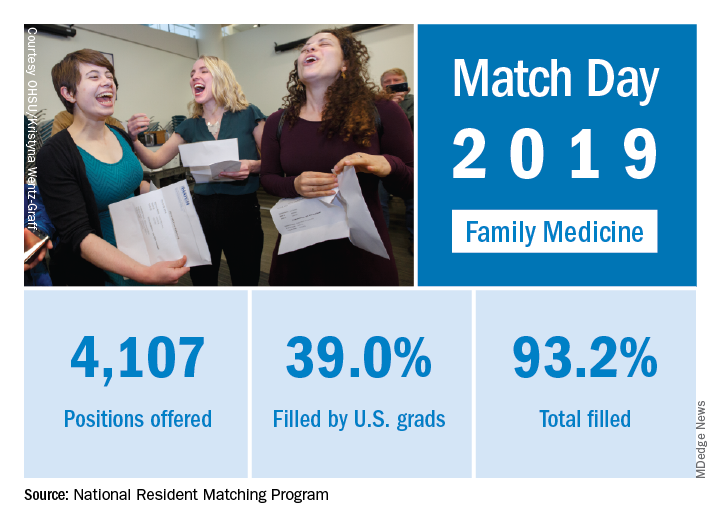
First-year FP slots rose from 3,629 to 4,107 as family medicine doubled the 6.5% increase in all first-year positions over 2018. The numbers of applicants (38,376) and total positions offered (35,185) were both record highs for the Match,although they were affected, in part, by “increased numbers of osteopathic programs that joined the Main Residency Match as a result of the ongoing transition to a single accreditation system for graduate medical education programs,” the NRMP noted.
Family medicine programs filled 39.0% of first-year positions with U.S. allopathic seniors, which was down from 44.9% in 2018 and 45.1% in 2017. In terms of the numbers of U.S. seniors involved, the drop was fairly small: from 1,628 in 2018 to 1,601 in 2019; however, the 986 osteopathic students and graduates who matched set a new record and accounted for almost 26% of all successful FP applicants, the NRMP reported.“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said in a written statement.
for the first time since 2009, according to the National Resident Matching Program (NRMP).
First-year FP slots rose from 3,629 to 4,107 as family medicine doubled the 6.5% increase in all first-year positions over 2018. The numbers of applicants (38,376) and total positions offered (35,185) were both record highs for the Match,although they were affected, in part, by “increased numbers of osteopathic programs that joined the Main Residency Match as a result of the ongoing transition to a single accreditation system for graduate medical education programs,” the NRMP noted.
Family medicine programs filled 39.0% of first-year positions with U.S. allopathic seniors, which was down from 44.9% in 2018 and 45.1% in 2017. In terms of the numbers of U.S. seniors involved, the drop was fairly small: from 1,628 in 2018 to 1,601 in 2019; however, the 986 osteopathic students and graduates who matched set a new record and accounted for almost 26% of all successful FP applicants, the NRMP reported.“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said in a written statement.
for the first time since 2009, according to the National Resident Matching Program (NRMP).
First-year FP slots rose from 3,629 to 4,107 as family medicine doubled the 6.5% increase in all first-year positions over 2018. The numbers of applicants (38,376) and total positions offered (35,185) were both record highs for the Match,although they were affected, in part, by “increased numbers of osteopathic programs that joined the Main Residency Match as a result of the ongoing transition to a single accreditation system for graduate medical education programs,” the NRMP noted.
Family medicine programs filled 39.0% of first-year positions with U.S. allopathic seniors, which was down from 44.9% in 2018 and 45.1% in 2017. In terms of the numbers of U.S. seniors involved, the drop was fairly small: from 1,628 in 2018 to 1,601 in 2019; however, the 986 osteopathic students and graduates who matched set a new record and accounted for almost 26% of all successful FP applicants, the NRMP reported.“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said in a written statement.
Match Day 2019: Dermatology steps up growth after slow 2018
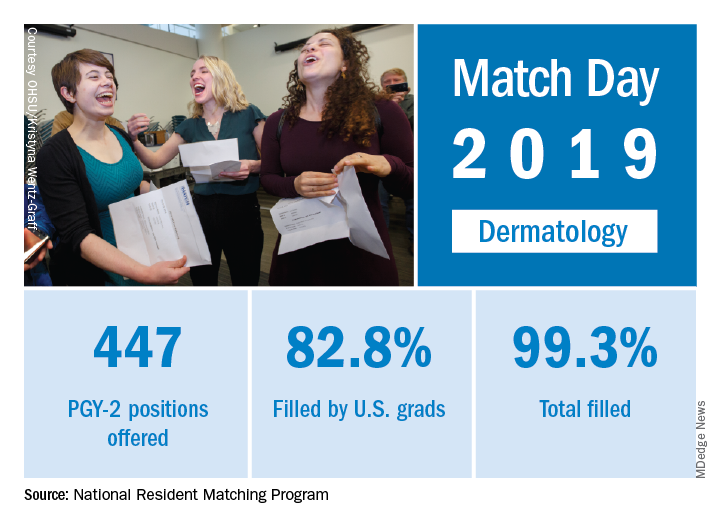
Available dermatology PGY-2 slots rose by 4.9% from 426 in 2018 to 447 in 2019, while slots filled grew by 5.5% from 420 to 443, for an overall fill rate of 99.3%. In addition, the fill rate for U.S. graduates grew for the first time since 2015, rising from 81.7% to 82.8%.
An overall total of 2,756 PGY-2 slots were offered, 97.2% of which were filled; 67.5% were filled by U.S. graduates, the NRMP said in its 2019 Main Residency Match report.
The 2019 Match set a record for most positions offered (35,185; up 6.1%), most positions filled (up 4.8%), most PGY-1 positions offered (32,194; up 6.5%), and total applicants (38,376; up 3.4%).
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” NRMP officials said in a statement.
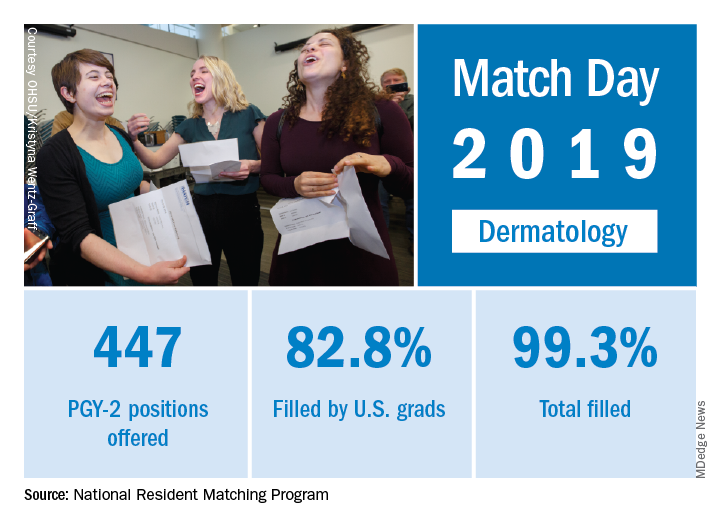
Available dermatology PGY-2 slots rose by 4.9% from 426 in 2018 to 447 in 2019, while slots filled grew by 5.5% from 420 to 443, for an overall fill rate of 99.3%. In addition, the fill rate for U.S. graduates grew for the first time since 2015, rising from 81.7% to 82.8%.
An overall total of 2,756 PGY-2 slots were offered, 97.2% of which were filled; 67.5% were filled by U.S. graduates, the NRMP said in its 2019 Main Residency Match report.
The 2019 Match set a record for most positions offered (35,185; up 6.1%), most positions filled (up 4.8%), most PGY-1 positions offered (32,194; up 6.5%), and total applicants (38,376; up 3.4%).
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” NRMP officials said in a statement.
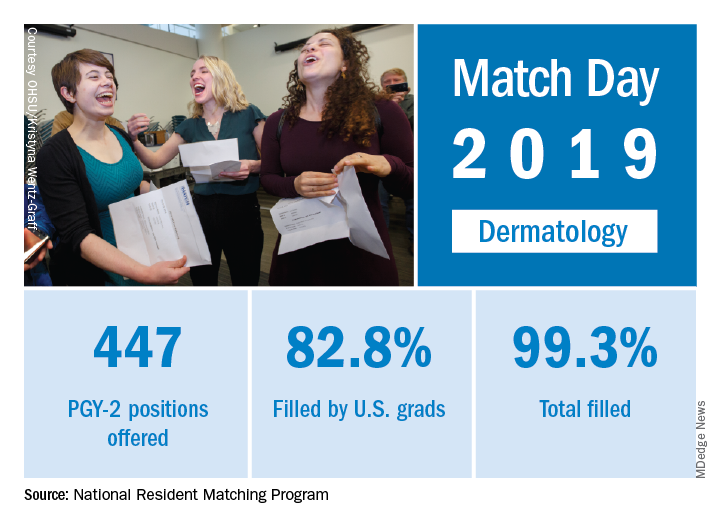
Available dermatology PGY-2 slots rose by 4.9% from 426 in 2018 to 447 in 2019, while slots filled grew by 5.5% from 420 to 443, for an overall fill rate of 99.3%. In addition, the fill rate for U.S. graduates grew for the first time since 2015, rising from 81.7% to 82.8%.
An overall total of 2,756 PGY-2 slots were offered, 97.2% of which were filled; 67.5% were filled by U.S. graduates, the NRMP said in its 2019 Main Residency Match report.
The 2019 Match set a record for most positions offered (35,185; up 6.1%), most positions filled (up 4.8%), most PGY-1 positions offered (32,194; up 6.5%), and total applicants (38,376; up 3.4%).
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” NRMP officials said in a statement.
Match Day 2019: Ob.gyn. up from last year
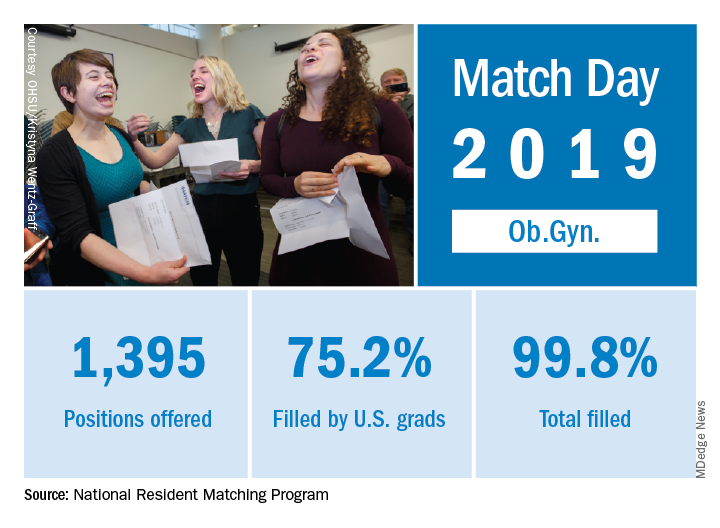
Ob.gyn. brought 1,395 first-year positions to the 2019 Main Resident Match, up from 1,336 in 2018. Also up from last year is the fill rate, with 2018’s Match Day filling 99.6% of available positions.
For all specialties in the main Match, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP report.
The 2019 Match also set a new high for total positions offered at 35,135, for which there was a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
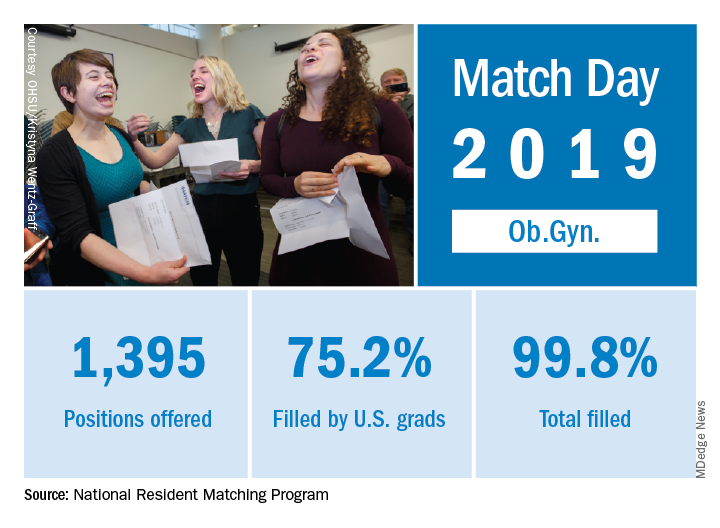
Ob.gyn. brought 1,395 first-year positions to the 2019 Main Resident Match, up from 1,336 in 2018. Also up from last year is the fill rate, with 2018’s Match Day filling 99.6% of available positions.
For all specialties in the main Match, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP report.
The 2019 Match also set a new high for total positions offered at 35,135, for which there was a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
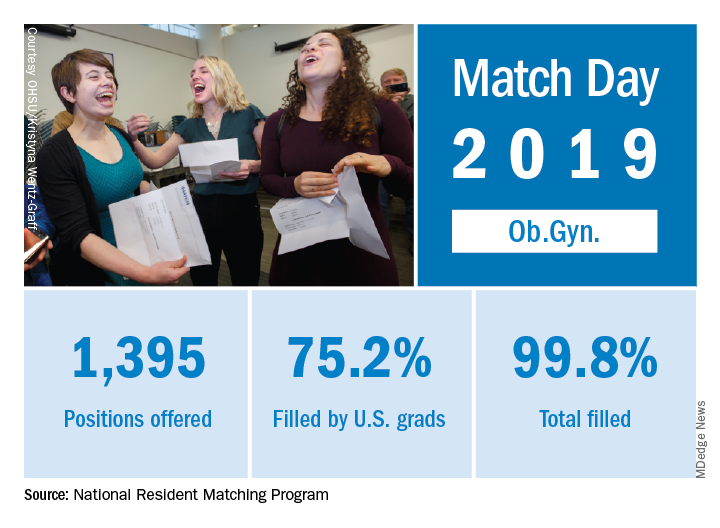
Ob.gyn. brought 1,395 first-year positions to the 2019 Main Resident Match, up from 1,336 in 2018. Also up from last year is the fill rate, with 2018’s Match Day filling 99.6% of available positions.
For all specialties in the main Match, U.S. first-year applicants filled 55.2%, and the overall fill rate was 94.9% of the 32,194 available positions, an increase of 6.5% over the number of positions available in 2018, according to the NRMP report.
The 2019 Match also set a new high for total positions offered at 35,135, for which there was a record-high 38,376 applicants. The increases are likely related, in part, to the greater number of osteopathic programs joining the Match Day offerings because of an ongoing move toward a single accreditation system.
“The results of the Match are closely watched because they can be predictors of future physician workforce supply. There also is significant interest in the competitiveness of specialties, as measured by the percentage of positions filled overall and the percentage filled by senior students in U.S. allopathic medical schools,” the NRMP said.
Cancer-battling breath, Zombie Bambi, and hops as health food
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
Online vitriol’s expansion into doctor discussion sites
The web is full of doctor discussion sites. Sermo, Doximity, and many others. Each is slightly different, but the idea is similar. Give docs a place to joke, discuss cases, etc. A virtual doctors’ lounge.
Roughly 10 years ago I was active on Sermo. It was fun to check in a few days a week after work, ask questions about my own cases, and see if anyone had ideas on them, make a few suggestions on others, occasionally gripe about administrative issues at my hospital and commiserate about such online.
I don’t do that anymore.
This morning I logged in to see if anyone had previously encountered an unusual case, but was quickly pushed off by venom.
Yes, they do have a political discussion board, but staying away from politics is easier said than done online. Like mud, it tends to ooze into places it doesn’t belong. Even a routine post asking about new treatments for multiple sclerosis quickly degenerates. In a demonstration of Godwin’s Law, any comment about the pros and cons of a new agent devolves into a fight over government vs. private insurance, the United States’ vs. other countries’ health systems, and, inevitably, Trump, Obama, and name calling.
Makes it hard to actually kick around thoughts on Ocrevus (or whatever).
Generally, this won’t happen in a real doctors’ lounge because you know each other. Even if you’re not friends, people generally (not always) tend to be civil in person. Even differences are usually handled with a polite agreement to disagree.
I suspect the majority of people on Sermo and similar sites are reasonable and joined the sites for the same reasons I did. Unfortunately, we’ve been drowned out by a handful of angry voices who hijack these sites by posting intentionally inflammatory statements just to pick a fight or derail a thoughtful discussion on epilepsy management with nasty jabs relating medical issues directly to politics.
So my time using these sites has dropped. Occasionally, if I was bored, I’d log in to see if there were any interesting cases in my field, but even those often get dragged down by the angry as you try to contribute thoughts and answer questions in the comments.
Sadly, this has became the norm rather then the exception. For me, at least, it’s easier to just walk away entirely.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The web is full of doctor discussion sites. Sermo, Doximity, and many others. Each is slightly different, but the idea is similar. Give docs a place to joke, discuss cases, etc. A virtual doctors’ lounge.
Roughly 10 years ago I was active on Sermo. It was fun to check in a few days a week after work, ask questions about my own cases, and see if anyone had ideas on them, make a few suggestions on others, occasionally gripe about administrative issues at my hospital and commiserate about such online.
I don’t do that anymore.
This morning I logged in to see if anyone had previously encountered an unusual case, but was quickly pushed off by venom.
Yes, they do have a political discussion board, but staying away from politics is easier said than done online. Like mud, it tends to ooze into places it doesn’t belong. Even a routine post asking about new treatments for multiple sclerosis quickly degenerates. In a demonstration of Godwin’s Law, any comment about the pros and cons of a new agent devolves into a fight over government vs. private insurance, the United States’ vs. other countries’ health systems, and, inevitably, Trump, Obama, and name calling.
Makes it hard to actually kick around thoughts on Ocrevus (or whatever).
Generally, this won’t happen in a real doctors’ lounge because you know each other. Even if you’re not friends, people generally (not always) tend to be civil in person. Even differences are usually handled with a polite agreement to disagree.
I suspect the majority of people on Sermo and similar sites are reasonable and joined the sites for the same reasons I did. Unfortunately, we’ve been drowned out by a handful of angry voices who hijack these sites by posting intentionally inflammatory statements just to pick a fight or derail a thoughtful discussion on epilepsy management with nasty jabs relating medical issues directly to politics.
So my time using these sites has dropped. Occasionally, if I was bored, I’d log in to see if there were any interesting cases in my field, but even those often get dragged down by the angry as you try to contribute thoughts and answer questions in the comments.
Sadly, this has became the norm rather then the exception. For me, at least, it’s easier to just walk away entirely.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The web is full of doctor discussion sites. Sermo, Doximity, and many others. Each is slightly different, but the idea is similar. Give docs a place to joke, discuss cases, etc. A virtual doctors’ lounge.
Roughly 10 years ago I was active on Sermo. It was fun to check in a few days a week after work, ask questions about my own cases, and see if anyone had ideas on them, make a few suggestions on others, occasionally gripe about administrative issues at my hospital and commiserate about such online.
I don’t do that anymore.
This morning I logged in to see if anyone had previously encountered an unusual case, but was quickly pushed off by venom.
Yes, they do have a political discussion board, but staying away from politics is easier said than done online. Like mud, it tends to ooze into places it doesn’t belong. Even a routine post asking about new treatments for multiple sclerosis quickly degenerates. In a demonstration of Godwin’s Law, any comment about the pros and cons of a new agent devolves into a fight over government vs. private insurance, the United States’ vs. other countries’ health systems, and, inevitably, Trump, Obama, and name calling.
Makes it hard to actually kick around thoughts on Ocrevus (or whatever).
Generally, this won’t happen in a real doctors’ lounge because you know each other. Even if you’re not friends, people generally (not always) tend to be civil in person. Even differences are usually handled with a polite agreement to disagree.
I suspect the majority of people on Sermo and similar sites are reasonable and joined the sites for the same reasons I did. Unfortunately, we’ve been drowned out by a handful of angry voices who hijack these sites by posting intentionally inflammatory statements just to pick a fight or derail a thoughtful discussion on epilepsy management with nasty jabs relating medical issues directly to politics.
So my time using these sites has dropped. Occasionally, if I was bored, I’d log in to see if there were any interesting cases in my field, but even those often get dragged down by the angry as you try to contribute thoughts and answer questions in the comments.
Sadly, this has became the norm rather then the exception. For me, at least, it’s easier to just walk away entirely.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Prevent burnout by tapping into passions
To fight burnout, Griffin Myers, MD, wants more out of the physicians who work at Chicago-based Oak Street Health.
Not more time, or more patients, or more codes billed – but more passion and a more meaningful professional experience, said Dr. Myers, cofounder and chief medical officer of the 42-practice group that cares for Medicare patients.
Oak Street seems to be on to something. According to the health care consultancy The Advisory Board, there are three key ways to avoid physician burnout: involve physicians in strategic decision making, recognize physicians’ contributions, and create time-limited leadership opportunities for physicians.
“What do you want to be when you grow up?”
That’s the question Dr. Myers asks physicians during job interviews. He wants to discover their personal and professional passions.
Health care leaders can’t expect physicians to prevent burnout on their own, insists Dr. Myers. “You have to change the way your organization supports clinicians.”
At Oak Street, that includes supporting physicians with medical scribes and ensuring that they aren’t bogged down with paperwork or “fighting with the fax machines,” said Dr. Myers.
Once a physician is hired at Oak Street, they’re partnered with a medical director who uses the practice’s resources to support the physician’s clinical and professional passions. Specifically, that means providing physicians with administrative time (nonpatient time) and support – both organizationally and financially – for professional development. Medical directors meet with physicians quarterly to check in and assess performance.
Take, for example, Tina Valdez, DO, an internist at Oak Street’s Englewood, Ill., location, who previously practiced at Advocate Lutheran General Hospital in Park Ridge, Ill. During the job interview process, Dr. Myers discovered that Dr. Valdez wanted to keep teaching and mentoring residents as they transitioned to attending physicians.
Dr. Myers was on board, so Dr. Valdez uses her administrative time to meet with early-career physicians on a quarterly basis.
Resident physicians are used to having a more senior physician monitor their work, Dr. Valdez noted. Without that oversight, many first-year physicians can get anxious. To support them, she leads small group discussions on topics including patient cases and ways to better work with other members of the care team, such as relying on a medical assistant to capture vital signs and conduct a thorough medication reconciliation.
In the program’s first year, 10 new physicians split into two groups for 2-hour sessions at an off-site meeting location once a quarter.
As much as early-career physicians need support, so, too, do future leaders.
When Andrea Khosropour, MD, first joined Oak Street in 2012, her mentor invested a lot of time in coaching her to become a better leader. For example, her mentor taught her the right way to have difficult conversations.
Dr. Khosropour, now a senior medical director who practices at the group’s Edgewater, Ill., location, said she finds balance at work because Oak Street gives her administrative time to attend to her management responsibilities. She also values the assistance of the medical scribes who document every patient encounter in the EHR. “That’s rare for primary care,” says Dr. Khosropour.
What qualities does Oak Street look for in its physician leaders? Dr. Myers said it starts with a physician who shares the group’s values, demonstrates clinical excellence and “scrappiness,” and has good intentions. He pointed out that Dr. Khosropour, who now oversees four practices, came to Oak Street with no experience running multiple practices.
Dr. Myers said Oak Street can grow its physicians internally as long as they share the group’s cultural values. “You can’t wait for people who already have those skills.”
Oak Street doesn’t rely on a fee-for-service model, in which physicians are paid by the volume of patients they treat. Specifically, that means 80% of its patients are in value-based contracts with private payers and the remaining patients are covered in the Medicare Shared Savings Program. About half of patients are dually eligible for Medicare and Medicaid, Dr. Myers said.
Because the group receives a set amount to manage the care of each of its attributed patients, Oak Street has the flexibility to invest in professional development, scribes, and other programs to support physicians, Dr. Myers said. That’s provided the group can successfully manage the care of their patients and keep them out of the hospital.
He advises practices that are more dependent on fee-for-service contracts to prioritize the following initiatives to prevent burnout: investing in professional development, reducing physicians’ administrative burdens, and celebrating physicians’ victories.
“Our goal is to provide the highest-quality health care employee experience possible. People will stay as long as you set that as a clear goal,” Dr. Myers said.
To fight burnout, Griffin Myers, MD, wants more out of the physicians who work at Chicago-based Oak Street Health.
Not more time, or more patients, or more codes billed – but more passion and a more meaningful professional experience, said Dr. Myers, cofounder and chief medical officer of the 42-practice group that cares for Medicare patients.
Oak Street seems to be on to something. According to the health care consultancy The Advisory Board, there are three key ways to avoid physician burnout: involve physicians in strategic decision making, recognize physicians’ contributions, and create time-limited leadership opportunities for physicians.
“What do you want to be when you grow up?”
That’s the question Dr. Myers asks physicians during job interviews. He wants to discover their personal and professional passions.
Health care leaders can’t expect physicians to prevent burnout on their own, insists Dr. Myers. “You have to change the way your organization supports clinicians.”
At Oak Street, that includes supporting physicians with medical scribes and ensuring that they aren’t bogged down with paperwork or “fighting with the fax machines,” said Dr. Myers.
Once a physician is hired at Oak Street, they’re partnered with a medical director who uses the practice’s resources to support the physician’s clinical and professional passions. Specifically, that means providing physicians with administrative time (nonpatient time) and support – both organizationally and financially – for professional development. Medical directors meet with physicians quarterly to check in and assess performance.
Take, for example, Tina Valdez, DO, an internist at Oak Street’s Englewood, Ill., location, who previously practiced at Advocate Lutheran General Hospital in Park Ridge, Ill. During the job interview process, Dr. Myers discovered that Dr. Valdez wanted to keep teaching and mentoring residents as they transitioned to attending physicians.
Dr. Myers was on board, so Dr. Valdez uses her administrative time to meet with early-career physicians on a quarterly basis.
Resident physicians are used to having a more senior physician monitor their work, Dr. Valdez noted. Without that oversight, many first-year physicians can get anxious. To support them, she leads small group discussions on topics including patient cases and ways to better work with other members of the care team, such as relying on a medical assistant to capture vital signs and conduct a thorough medication reconciliation.
In the program’s first year, 10 new physicians split into two groups for 2-hour sessions at an off-site meeting location once a quarter.
As much as early-career physicians need support, so, too, do future leaders.
When Andrea Khosropour, MD, first joined Oak Street in 2012, her mentor invested a lot of time in coaching her to become a better leader. For example, her mentor taught her the right way to have difficult conversations.
Dr. Khosropour, now a senior medical director who practices at the group’s Edgewater, Ill., location, said she finds balance at work because Oak Street gives her administrative time to attend to her management responsibilities. She also values the assistance of the medical scribes who document every patient encounter in the EHR. “That’s rare for primary care,” says Dr. Khosropour.
What qualities does Oak Street look for in its physician leaders? Dr. Myers said it starts with a physician who shares the group’s values, demonstrates clinical excellence and “scrappiness,” and has good intentions. He pointed out that Dr. Khosropour, who now oversees four practices, came to Oak Street with no experience running multiple practices.
Dr. Myers said Oak Street can grow its physicians internally as long as they share the group’s cultural values. “You can’t wait for people who already have those skills.”
Oak Street doesn’t rely on a fee-for-service model, in which physicians are paid by the volume of patients they treat. Specifically, that means 80% of its patients are in value-based contracts with private payers and the remaining patients are covered in the Medicare Shared Savings Program. About half of patients are dually eligible for Medicare and Medicaid, Dr. Myers said.
Because the group receives a set amount to manage the care of each of its attributed patients, Oak Street has the flexibility to invest in professional development, scribes, and other programs to support physicians, Dr. Myers said. That’s provided the group can successfully manage the care of their patients and keep them out of the hospital.
He advises practices that are more dependent on fee-for-service contracts to prioritize the following initiatives to prevent burnout: investing in professional development, reducing physicians’ administrative burdens, and celebrating physicians’ victories.
“Our goal is to provide the highest-quality health care employee experience possible. People will stay as long as you set that as a clear goal,” Dr. Myers said.
To fight burnout, Griffin Myers, MD, wants more out of the physicians who work at Chicago-based Oak Street Health.
Not more time, or more patients, or more codes billed – but more passion and a more meaningful professional experience, said Dr. Myers, cofounder and chief medical officer of the 42-practice group that cares for Medicare patients.
Oak Street seems to be on to something. According to the health care consultancy The Advisory Board, there are three key ways to avoid physician burnout: involve physicians in strategic decision making, recognize physicians’ contributions, and create time-limited leadership opportunities for physicians.
“What do you want to be when you grow up?”
That’s the question Dr. Myers asks physicians during job interviews. He wants to discover their personal and professional passions.
Health care leaders can’t expect physicians to prevent burnout on their own, insists Dr. Myers. “You have to change the way your organization supports clinicians.”
At Oak Street, that includes supporting physicians with medical scribes and ensuring that they aren’t bogged down with paperwork or “fighting with the fax machines,” said Dr. Myers.
Once a physician is hired at Oak Street, they’re partnered with a medical director who uses the practice’s resources to support the physician’s clinical and professional passions. Specifically, that means providing physicians with administrative time (nonpatient time) and support – both organizationally and financially – for professional development. Medical directors meet with physicians quarterly to check in and assess performance.
Take, for example, Tina Valdez, DO, an internist at Oak Street’s Englewood, Ill., location, who previously practiced at Advocate Lutheran General Hospital in Park Ridge, Ill. During the job interview process, Dr. Myers discovered that Dr. Valdez wanted to keep teaching and mentoring residents as they transitioned to attending physicians.
Dr. Myers was on board, so Dr. Valdez uses her administrative time to meet with early-career physicians on a quarterly basis.
Resident physicians are used to having a more senior physician monitor their work, Dr. Valdez noted. Without that oversight, many first-year physicians can get anxious. To support them, she leads small group discussions on topics including patient cases and ways to better work with other members of the care team, such as relying on a medical assistant to capture vital signs and conduct a thorough medication reconciliation.
In the program’s first year, 10 new physicians split into two groups for 2-hour sessions at an off-site meeting location once a quarter.
As much as early-career physicians need support, so, too, do future leaders.
When Andrea Khosropour, MD, first joined Oak Street in 2012, her mentor invested a lot of time in coaching her to become a better leader. For example, her mentor taught her the right way to have difficult conversations.
Dr. Khosropour, now a senior medical director who practices at the group’s Edgewater, Ill., location, said she finds balance at work because Oak Street gives her administrative time to attend to her management responsibilities. She also values the assistance of the medical scribes who document every patient encounter in the EHR. “That’s rare for primary care,” says Dr. Khosropour.
What qualities does Oak Street look for in its physician leaders? Dr. Myers said it starts with a physician who shares the group’s values, demonstrates clinical excellence and “scrappiness,” and has good intentions. He pointed out that Dr. Khosropour, who now oversees four practices, came to Oak Street with no experience running multiple practices.
Dr. Myers said Oak Street can grow its physicians internally as long as they share the group’s cultural values. “You can’t wait for people who already have those skills.”
Oak Street doesn’t rely on a fee-for-service model, in which physicians are paid by the volume of patients they treat. Specifically, that means 80% of its patients are in value-based contracts with private payers and the remaining patients are covered in the Medicare Shared Savings Program. About half of patients are dually eligible for Medicare and Medicaid, Dr. Myers said.
Because the group receives a set amount to manage the care of each of its attributed patients, Oak Street has the flexibility to invest in professional development, scribes, and other programs to support physicians, Dr. Myers said. That’s provided the group can successfully manage the care of their patients and keep them out of the hospital.
He advises practices that are more dependent on fee-for-service contracts to prioritize the following initiatives to prevent burnout: investing in professional development, reducing physicians’ administrative burdens, and celebrating physicians’ victories.
“Our goal is to provide the highest-quality health care employee experience possible. People will stay as long as you set that as a clear goal,” Dr. Myers said.