User login
Associations Between Colorectal Cancer Progression and Dietary Patterns of US Veterans in CSP #380
PURPOSE
To analyze associations between colorectal cancer progression and diet scores calculated using published scoring approaches for three dietary patterns: Healthy Eating Index (HEI), Mediterranean Diet (Mediterranean), and Dietary Approaches to Stop Hypertension Diet (DASH).
BACKGROUND
Little is known about whether longterm risk for progression to colorectal cancer is associated with recommended healthy dietary patterns among US veterans. Previous studies of veterans have shown higher intake of fiber and vitamin D reduced risk, and red meat increased risk for finding colorectal cancer precursors during colonoscopy. However, studying dietary patterns in aggregate may be more clinically relevant for longitudinal studies of colorectal cancer prevention.
METHODS
3,121 asymptomatic US veterans aged 50-75 received colonoscopy between 1994-97 and were followed through 2009. Most significant colonoscopy findings (MSCF) across the study period were: (i) no neoplasia (NN), (ii) non-advanced adenomas (NAAs) or (iii) advanced neoplasia (AN). Baseline dietary questionnaire data were used to calculate three dietary pattern (HEI, Mediterranean, and DASH) scores.
DATA ANALYSIS
Multinomial logistic regression models were used in a cross-sectional analysis to test for associations represented by adjusted odds ratios (aOR) between MSCF and dietary pattern scores, controlling for demographics and clinical risk factors.
RESULTS
Among 3,023 participants with complete data, 97% were male, and 83.8% were White. Increasing scores, representing healthier diets, for each dietary pattern had similar or lower odds for NAAs and AN, respectively, versus NN. They were HEI: aOR: 1.00, 95% CI: 0.99-1.01 and aOR 0.97, 95% CI: 0.99-1.01; Mediterranean: aOR: 0.98, 95% CI: 0.95-1.02 and aOR 0.95, 95% CI: 0.90-0.999; DASH: aOR: 0.99, 95% CI: 0.99- 1.00 and aOR 0.99, 95% CI: 0.98-0.999. Across each dietary pattern, higher whole grain and fiber category scores generally had lower odds for NAAs and AN.
CONCLUSIONS
Study results revealed that overall higher dietary quality and specific dietary components of whole grain or fiber intake, based on three different dietary patterns suggest lower odds for CRC precursors. Findings indicate potential differences in dietary intake patterns and more research is needed to determine the benefit of developing tailored CRC screening and surveillance clinical guidelines.
PURPOSE
To analyze associations between colorectal cancer progression and diet scores calculated using published scoring approaches for three dietary patterns: Healthy Eating Index (HEI), Mediterranean Diet (Mediterranean), and Dietary Approaches to Stop Hypertension Diet (DASH).
BACKGROUND
Little is known about whether longterm risk for progression to colorectal cancer is associated with recommended healthy dietary patterns among US veterans. Previous studies of veterans have shown higher intake of fiber and vitamin D reduced risk, and red meat increased risk for finding colorectal cancer precursors during colonoscopy. However, studying dietary patterns in aggregate may be more clinically relevant for longitudinal studies of colorectal cancer prevention.
METHODS
3,121 asymptomatic US veterans aged 50-75 received colonoscopy between 1994-97 and were followed through 2009. Most significant colonoscopy findings (MSCF) across the study period were: (i) no neoplasia (NN), (ii) non-advanced adenomas (NAAs) or (iii) advanced neoplasia (AN). Baseline dietary questionnaire data were used to calculate three dietary pattern (HEI, Mediterranean, and DASH) scores.
DATA ANALYSIS
Multinomial logistic regression models were used in a cross-sectional analysis to test for associations represented by adjusted odds ratios (aOR) between MSCF and dietary pattern scores, controlling for demographics and clinical risk factors.
RESULTS
Among 3,023 participants with complete data, 97% were male, and 83.8% were White. Increasing scores, representing healthier diets, for each dietary pattern had similar or lower odds for NAAs and AN, respectively, versus NN. They were HEI: aOR: 1.00, 95% CI: 0.99-1.01 and aOR 0.97, 95% CI: 0.99-1.01; Mediterranean: aOR: 0.98, 95% CI: 0.95-1.02 and aOR 0.95, 95% CI: 0.90-0.999; DASH: aOR: 0.99, 95% CI: 0.99- 1.00 and aOR 0.99, 95% CI: 0.98-0.999. Across each dietary pattern, higher whole grain and fiber category scores generally had lower odds for NAAs and AN.
CONCLUSIONS
Study results revealed that overall higher dietary quality and specific dietary components of whole grain or fiber intake, based on three different dietary patterns suggest lower odds for CRC precursors. Findings indicate potential differences in dietary intake patterns and more research is needed to determine the benefit of developing tailored CRC screening and surveillance clinical guidelines.
PURPOSE
To analyze associations between colorectal cancer progression and diet scores calculated using published scoring approaches for three dietary patterns: Healthy Eating Index (HEI), Mediterranean Diet (Mediterranean), and Dietary Approaches to Stop Hypertension Diet (DASH).
BACKGROUND
Little is known about whether longterm risk for progression to colorectal cancer is associated with recommended healthy dietary patterns among US veterans. Previous studies of veterans have shown higher intake of fiber and vitamin D reduced risk, and red meat increased risk for finding colorectal cancer precursors during colonoscopy. However, studying dietary patterns in aggregate may be more clinically relevant for longitudinal studies of colorectal cancer prevention.
METHODS
3,121 asymptomatic US veterans aged 50-75 received colonoscopy between 1994-97 and were followed through 2009. Most significant colonoscopy findings (MSCF) across the study period were: (i) no neoplasia (NN), (ii) non-advanced adenomas (NAAs) or (iii) advanced neoplasia (AN). Baseline dietary questionnaire data were used to calculate three dietary pattern (HEI, Mediterranean, and DASH) scores.
DATA ANALYSIS
Multinomial logistic regression models were used in a cross-sectional analysis to test for associations represented by adjusted odds ratios (aOR) between MSCF and dietary pattern scores, controlling for demographics and clinical risk factors.
RESULTS
Among 3,023 participants with complete data, 97% were male, and 83.8% were White. Increasing scores, representing healthier diets, for each dietary pattern had similar or lower odds for NAAs and AN, respectively, versus NN. They were HEI: aOR: 1.00, 95% CI: 0.99-1.01 and aOR 0.97, 95% CI: 0.99-1.01; Mediterranean: aOR: 0.98, 95% CI: 0.95-1.02 and aOR 0.95, 95% CI: 0.90-0.999; DASH: aOR: 0.99, 95% CI: 0.99- 1.00 and aOR 0.99, 95% CI: 0.98-0.999. Across each dietary pattern, higher whole grain and fiber category scores generally had lower odds for NAAs and AN.
CONCLUSIONS
Study results revealed that overall higher dietary quality and specific dietary components of whole grain or fiber intake, based on three different dietary patterns suggest lower odds for CRC precursors. Findings indicate potential differences in dietary intake patterns and more research is needed to determine the benefit of developing tailored CRC screening and surveillance clinical guidelines.
Mucinous Adenocarcinoma of the Rectum: Clinical Outcomes and Characteristics of 14,044 Patients From the National Cancer Database
PURPOSE
Study clinical characteristics of Rectal Mucinous Adenocarcinoma (RMA).
BACKGROUND
RMA is a rare histological subtype with an impaired response to chemoradiotherapy and an overall poor prognosis. High-grade tumors are associated with older age. Previous studies have shown conflicting results on prognosis.
METHODS
Retrospective analysis of National Cancer Database was conducted from 2004-2020 for subjects with histology code 8480 in primary sites C19 and C20 (rectosigmoid-junction and rectum, n = 14,044), using multivariate analysis with Cox regression.
RESULTS
Median age of diagnosis was 65 years with 69.5% were in the 45-75 years age range. 59.2% were male while 40.8% were female. 84.7% were White, 9.7% were Black, 0.4% were American Indian and 3.4% were Asian. 6.9% were Hispanic. 33.9% were in the upper-income quartile. 40.6% were seen at community cancer programs while 33% went to academic programs. 36.5% had stage III RMA. Out of the 14,044 patients with RMA, 10,546 received surgery, 5,179 received chemotherapy, 233 received immunotherapy and 55 received hormone therapy. Patients >75 years had significantly lower overall survival (OS) compared to those <45 years (HR 0.67). Female patients had significantly higher OS than male (HR - 0.07). Black patients had significantly lower OS than White (HR 0.08). Hispanic patients had significantly higher OS than non- Hispanic (HR - 0.14). Patients with private and government insurance had significantly higher OS than noninsured patients (HR - 0.35 and - 0.26 respectively). Patients with median higher-income quartiles had significantly higher OS than lower quartiles (HR - 0.13). Academic facilities had significantly higher OS than community programs (HR - 0.13). Patients who received surgery had significantly higher OS than those that did not (HR - 0.67); median survival for patients who received surgery was 71 months vs 28 months for non-surgical candidates.
CONCLUSIONS
Surgery is the most important treatment modality in RMA. Uninsured, older Black male patients from lower-income quartiles had significantly lower OS. Access to academic centers also contributed to differences in OS outcomes which throws light on healthcare disparities.
IMPLICATIONS
Additional studies need to be conducted for viable solutions to assist with social determinants of healthcare in RMA.
PURPOSE
Study clinical characteristics of Rectal Mucinous Adenocarcinoma (RMA).
BACKGROUND
RMA is a rare histological subtype with an impaired response to chemoradiotherapy and an overall poor prognosis. High-grade tumors are associated with older age. Previous studies have shown conflicting results on prognosis.
METHODS
Retrospective analysis of National Cancer Database was conducted from 2004-2020 for subjects with histology code 8480 in primary sites C19 and C20 (rectosigmoid-junction and rectum, n = 14,044), using multivariate analysis with Cox regression.
RESULTS
Median age of diagnosis was 65 years with 69.5% were in the 45-75 years age range. 59.2% were male while 40.8% were female. 84.7% were White, 9.7% were Black, 0.4% were American Indian and 3.4% were Asian. 6.9% were Hispanic. 33.9% were in the upper-income quartile. 40.6% were seen at community cancer programs while 33% went to academic programs. 36.5% had stage III RMA. Out of the 14,044 patients with RMA, 10,546 received surgery, 5,179 received chemotherapy, 233 received immunotherapy and 55 received hormone therapy. Patients >75 years had significantly lower overall survival (OS) compared to those <45 years (HR 0.67). Female patients had significantly higher OS than male (HR - 0.07). Black patients had significantly lower OS than White (HR 0.08). Hispanic patients had significantly higher OS than non- Hispanic (HR - 0.14). Patients with private and government insurance had significantly higher OS than noninsured patients (HR - 0.35 and - 0.26 respectively). Patients with median higher-income quartiles had significantly higher OS than lower quartiles (HR - 0.13). Academic facilities had significantly higher OS than community programs (HR - 0.13). Patients who received surgery had significantly higher OS than those that did not (HR - 0.67); median survival for patients who received surgery was 71 months vs 28 months for non-surgical candidates.
CONCLUSIONS
Surgery is the most important treatment modality in RMA. Uninsured, older Black male patients from lower-income quartiles had significantly lower OS. Access to academic centers also contributed to differences in OS outcomes which throws light on healthcare disparities.
IMPLICATIONS
Additional studies need to be conducted for viable solutions to assist with social determinants of healthcare in RMA.
PURPOSE
Study clinical characteristics of Rectal Mucinous Adenocarcinoma (RMA).
BACKGROUND
RMA is a rare histological subtype with an impaired response to chemoradiotherapy and an overall poor prognosis. High-grade tumors are associated with older age. Previous studies have shown conflicting results on prognosis.
METHODS
Retrospective analysis of National Cancer Database was conducted from 2004-2020 for subjects with histology code 8480 in primary sites C19 and C20 (rectosigmoid-junction and rectum, n = 14,044), using multivariate analysis with Cox regression.
RESULTS
Median age of diagnosis was 65 years with 69.5% were in the 45-75 years age range. 59.2% were male while 40.8% were female. 84.7% were White, 9.7% were Black, 0.4% were American Indian and 3.4% were Asian. 6.9% were Hispanic. 33.9% were in the upper-income quartile. 40.6% were seen at community cancer programs while 33% went to academic programs. 36.5% had stage III RMA. Out of the 14,044 patients with RMA, 10,546 received surgery, 5,179 received chemotherapy, 233 received immunotherapy and 55 received hormone therapy. Patients >75 years had significantly lower overall survival (OS) compared to those <45 years (HR 0.67). Female patients had significantly higher OS than male (HR - 0.07). Black patients had significantly lower OS than White (HR 0.08). Hispanic patients had significantly higher OS than non- Hispanic (HR - 0.14). Patients with private and government insurance had significantly higher OS than noninsured patients (HR - 0.35 and - 0.26 respectively). Patients with median higher-income quartiles had significantly higher OS than lower quartiles (HR - 0.13). Academic facilities had significantly higher OS than community programs (HR - 0.13). Patients who received surgery had significantly higher OS than those that did not (HR - 0.67); median survival for patients who received surgery was 71 months vs 28 months for non-surgical candidates.
CONCLUSIONS
Surgery is the most important treatment modality in RMA. Uninsured, older Black male patients from lower-income quartiles had significantly lower OS. Access to academic centers also contributed to differences in OS outcomes which throws light on healthcare disparities.
IMPLICATIONS
Additional studies need to be conducted for viable solutions to assist with social determinants of healthcare in RMA.
High-intensity interval training before major surgery may boost postoperative outcomes
TOPLINE:
It cuts the risk of postoperative complications and may shorten hospital length of stay and improve postoperative quality of life.
METHODOLOGY:
Evidence suggests CRF – which improves physical and cognitive function and is associated with a reduction in cardiovascular risk – can be enhanced before major surgeries, but reported postoperative outcomes in previous reviews have been inconsistent.
In the study, HIIT involved repeated aerobic high-intensity exercise intervals at about 80% of maximum heart rate, followed by active recovery.
The meta-analysis included 12 studies with 832 patients (mean age, 67) that compared preoperative HIIT – supervised at hospitals, gyms, or community or physical therapy centers, or unsupervised at home – with standard care for patients slated for major surgery, including liver, lung, colorectal, urologic, and mixed major abdominal operations.
The primary outcome was change in CRF by peak VO2 or 6-minute walk test; other endpoints included change in endurance time and postoperative outcomes.
TAKEAWAY:
Preoperative HIIT (median total, 160 minutes; range, 80-240 minutes; intense exercise during 6-40 sessions) was associated with an increase in peak oxygen consumption (VO2 peak) by 2.59 mL/kg/min (95% confidence interval, 1.52-3.65 mL/kg/min; P < .001), compared with standard care, which represents about a 10% increase in CRF.
In eight studies that involved 770 patients, there was moderate evidence that preoperative HIIT cut the odds ratio for postoperative complications by more than half (OR, 0.44; 95% CI, 0.32-0.60; P < .001); there was a similar apparent benefit in an analysis that was limited to patients who were slated for abdominal surgery (OR, 0.45; 95% CI, 0.29-0.68; P < .001).
An analysis that was limited to studies that reported hospital length of stay showed a clinically relevant but nonsignificant 3-day reduction among patients in the HIIT groups.
Most quality of life assessments did not show post-HIIT improvements; some showed a significant benefit 6 weeks after surgery.
IN PRACTICE:
The results suggest preoperative HIIT may improve postoperative outcomes. By extension, it could be cost-effective and “should be included in prehabilitation programs,” the report states.
SOURCE:
The study was carried out by Kari Clifford, PhD, Otago Medical School, University of Otago, Dunedin, New Zealand, and colleagues. It was published online June 30, 2023, in JAMA Network Open.
LIMITATIONS:
Included studies were heterogeneous in methodology; for example, HIIT definitions and protocols varied across almost every study. Data reporting was incomplete, the samples sizes in the studies were limited, and patients could not be blinded to their intervention. The patients could not be stratified on the basis of frailty. There were limited HIIT data from patients who underwent orthopedic surgeries.
DISCLOSURES:
The study received funding from the University of Otago. The authors reported no conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
It cuts the risk of postoperative complications and may shorten hospital length of stay and improve postoperative quality of life.
METHODOLOGY:
Evidence suggests CRF – which improves physical and cognitive function and is associated with a reduction in cardiovascular risk – can be enhanced before major surgeries, but reported postoperative outcomes in previous reviews have been inconsistent.
In the study, HIIT involved repeated aerobic high-intensity exercise intervals at about 80% of maximum heart rate, followed by active recovery.
The meta-analysis included 12 studies with 832 patients (mean age, 67) that compared preoperative HIIT – supervised at hospitals, gyms, or community or physical therapy centers, or unsupervised at home – with standard care for patients slated for major surgery, including liver, lung, colorectal, urologic, and mixed major abdominal operations.
The primary outcome was change in CRF by peak VO2 or 6-minute walk test; other endpoints included change in endurance time and postoperative outcomes.
TAKEAWAY:
Preoperative HIIT (median total, 160 minutes; range, 80-240 minutes; intense exercise during 6-40 sessions) was associated with an increase in peak oxygen consumption (VO2 peak) by 2.59 mL/kg/min (95% confidence interval, 1.52-3.65 mL/kg/min; P < .001), compared with standard care, which represents about a 10% increase in CRF.
In eight studies that involved 770 patients, there was moderate evidence that preoperative HIIT cut the odds ratio for postoperative complications by more than half (OR, 0.44; 95% CI, 0.32-0.60; P < .001); there was a similar apparent benefit in an analysis that was limited to patients who were slated for abdominal surgery (OR, 0.45; 95% CI, 0.29-0.68; P < .001).
An analysis that was limited to studies that reported hospital length of stay showed a clinically relevant but nonsignificant 3-day reduction among patients in the HIIT groups.
Most quality of life assessments did not show post-HIIT improvements; some showed a significant benefit 6 weeks after surgery.
IN PRACTICE:
The results suggest preoperative HIIT may improve postoperative outcomes. By extension, it could be cost-effective and “should be included in prehabilitation programs,” the report states.
SOURCE:
The study was carried out by Kari Clifford, PhD, Otago Medical School, University of Otago, Dunedin, New Zealand, and colleagues. It was published online June 30, 2023, in JAMA Network Open.
LIMITATIONS:
Included studies were heterogeneous in methodology; for example, HIIT definitions and protocols varied across almost every study. Data reporting was incomplete, the samples sizes in the studies were limited, and patients could not be blinded to their intervention. The patients could not be stratified on the basis of frailty. There were limited HIIT data from patients who underwent orthopedic surgeries.
DISCLOSURES:
The study received funding from the University of Otago. The authors reported no conflicts.
A version of this article first appeared on Medscape.com.
TOPLINE:
It cuts the risk of postoperative complications and may shorten hospital length of stay and improve postoperative quality of life.
METHODOLOGY:
Evidence suggests CRF – which improves physical and cognitive function and is associated with a reduction in cardiovascular risk – can be enhanced before major surgeries, but reported postoperative outcomes in previous reviews have been inconsistent.
In the study, HIIT involved repeated aerobic high-intensity exercise intervals at about 80% of maximum heart rate, followed by active recovery.
The meta-analysis included 12 studies with 832 patients (mean age, 67) that compared preoperative HIIT – supervised at hospitals, gyms, or community or physical therapy centers, or unsupervised at home – with standard care for patients slated for major surgery, including liver, lung, colorectal, urologic, and mixed major abdominal operations.
The primary outcome was change in CRF by peak VO2 or 6-minute walk test; other endpoints included change in endurance time and postoperative outcomes.
TAKEAWAY:
Preoperative HIIT (median total, 160 minutes; range, 80-240 minutes; intense exercise during 6-40 sessions) was associated with an increase in peak oxygen consumption (VO2 peak) by 2.59 mL/kg/min (95% confidence interval, 1.52-3.65 mL/kg/min; P < .001), compared with standard care, which represents about a 10% increase in CRF.
In eight studies that involved 770 patients, there was moderate evidence that preoperative HIIT cut the odds ratio for postoperative complications by more than half (OR, 0.44; 95% CI, 0.32-0.60; P < .001); there was a similar apparent benefit in an analysis that was limited to patients who were slated for abdominal surgery (OR, 0.45; 95% CI, 0.29-0.68; P < .001).
An analysis that was limited to studies that reported hospital length of stay showed a clinically relevant but nonsignificant 3-day reduction among patients in the HIIT groups.
Most quality of life assessments did not show post-HIIT improvements; some showed a significant benefit 6 weeks after surgery.
IN PRACTICE:
The results suggest preoperative HIIT may improve postoperative outcomes. By extension, it could be cost-effective and “should be included in prehabilitation programs,” the report states.
SOURCE:
The study was carried out by Kari Clifford, PhD, Otago Medical School, University of Otago, Dunedin, New Zealand, and colleagues. It was published online June 30, 2023, in JAMA Network Open.
LIMITATIONS:
Included studies were heterogeneous in methodology; for example, HIIT definitions and protocols varied across almost every study. Data reporting was incomplete, the samples sizes in the studies were limited, and patients could not be blinded to their intervention. The patients could not be stratified on the basis of frailty. There were limited HIIT data from patients who underwent orthopedic surgeries.
DISCLOSURES:
The study received funding from the University of Otago. The authors reported no conflicts.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Does timing of surgery affect rectal cancer outcomes?
TOPLINE:
METHODOLOGY:
- A total of 1,506 patients with locally advanced rectal cancer who underwent neoadjuvant therapy followed by total mesorectal excision were divided into three groups based on the time interval between therapy and surgery: short (8 weeks), intermediate (> 8 to 12 weeks), and long (> 12 weeks).
- The primary outcome was pathologic complete response, and secondary outcomes included other histopathologic results, perioperative events, and survival outcomes.
- Median follow-up was 33 months.
TAKEAWAY:
- Overall, a pathologic complete response was observed in 255 patients (17.2%).
- Compared with the intermediate interval (reference) group, investigators found no association between time interval and pathologic complete response in the short-interval (odds ratio, 0.74; 95% CI, 0.55-1.01) or long-interval groups (OR, 1.07; P = .70).
- A long interval was significantly associated with a lower risk of a bad response as measured by tumor regression grade 2-3, compared with the reference category (OR, 0.47), but a higher risk of minor postoperative complications (OR, 1.43), conversion to open surgery (OR, 3.14), and longer operative time.
- The long-interval group was associated with a significantly reduced risk of systemic recurrence, compared with the reference group (hazard ratio, 0.59; P = .04), but not improved overall survival (HR, 1.38; P = .11) or locoregional recurrence (HR, 0.53; P = .18); no significant findings occurred for the short versus intermediate group.
IN PRACTICE:
“Findings suggest that delaying surgery may improve tumor regression and decrease risk of distant metastasis but increase surgical complexity,” the authors conclude. “Nonetheless, the reported improvements in tumor regression and systemic recurrence in the long-interval group were unexpectedly not followed by improved [overall survival].”
SOURCE:
F. Borja de Lacy, MD, PhD, Hospital Clinic of Barcelona, University of Barcelona, led the study, published online in JAMA Surgery, with an accompanying editorial.
LIMITATIONS:
- The study’s main limitation was its retrospective design, which could have resulted in missing or inconsistent data, as well as the short follow-up time.
- Decisions about time interval were based more on professional preference rather than specific tumor characteristics.
DISCLOSURES:
Dr. de Lacy has reported no relevant financial relationships. No outside funding source was disclosed.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A total of 1,506 patients with locally advanced rectal cancer who underwent neoadjuvant therapy followed by total mesorectal excision were divided into three groups based on the time interval between therapy and surgery: short (8 weeks), intermediate (> 8 to 12 weeks), and long (> 12 weeks).
- The primary outcome was pathologic complete response, and secondary outcomes included other histopathologic results, perioperative events, and survival outcomes.
- Median follow-up was 33 months.
TAKEAWAY:
- Overall, a pathologic complete response was observed in 255 patients (17.2%).
- Compared with the intermediate interval (reference) group, investigators found no association between time interval and pathologic complete response in the short-interval (odds ratio, 0.74; 95% CI, 0.55-1.01) or long-interval groups (OR, 1.07; P = .70).
- A long interval was significantly associated with a lower risk of a bad response as measured by tumor regression grade 2-3, compared with the reference category (OR, 0.47), but a higher risk of minor postoperative complications (OR, 1.43), conversion to open surgery (OR, 3.14), and longer operative time.
- The long-interval group was associated with a significantly reduced risk of systemic recurrence, compared with the reference group (hazard ratio, 0.59; P = .04), but not improved overall survival (HR, 1.38; P = .11) or locoregional recurrence (HR, 0.53; P = .18); no significant findings occurred for the short versus intermediate group.
IN PRACTICE:
“Findings suggest that delaying surgery may improve tumor regression and decrease risk of distant metastasis but increase surgical complexity,” the authors conclude. “Nonetheless, the reported improvements in tumor regression and systemic recurrence in the long-interval group were unexpectedly not followed by improved [overall survival].”
SOURCE:
F. Borja de Lacy, MD, PhD, Hospital Clinic of Barcelona, University of Barcelona, led the study, published online in JAMA Surgery, with an accompanying editorial.
LIMITATIONS:
- The study’s main limitation was its retrospective design, which could have resulted in missing or inconsistent data, as well as the short follow-up time.
- Decisions about time interval were based more on professional preference rather than specific tumor characteristics.
DISCLOSURES:
Dr. de Lacy has reported no relevant financial relationships. No outside funding source was disclosed.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A total of 1,506 patients with locally advanced rectal cancer who underwent neoadjuvant therapy followed by total mesorectal excision were divided into three groups based on the time interval between therapy and surgery: short (8 weeks), intermediate (> 8 to 12 weeks), and long (> 12 weeks).
- The primary outcome was pathologic complete response, and secondary outcomes included other histopathologic results, perioperative events, and survival outcomes.
- Median follow-up was 33 months.
TAKEAWAY:
- Overall, a pathologic complete response was observed in 255 patients (17.2%).
- Compared with the intermediate interval (reference) group, investigators found no association between time interval and pathologic complete response in the short-interval (odds ratio, 0.74; 95% CI, 0.55-1.01) or long-interval groups (OR, 1.07; P = .70).
- A long interval was significantly associated with a lower risk of a bad response as measured by tumor regression grade 2-3, compared with the reference category (OR, 0.47), but a higher risk of minor postoperative complications (OR, 1.43), conversion to open surgery (OR, 3.14), and longer operative time.
- The long-interval group was associated with a significantly reduced risk of systemic recurrence, compared with the reference group (hazard ratio, 0.59; P = .04), but not improved overall survival (HR, 1.38; P = .11) or locoregional recurrence (HR, 0.53; P = .18); no significant findings occurred for the short versus intermediate group.
IN PRACTICE:
“Findings suggest that delaying surgery may improve tumor regression and decrease risk of distant metastasis but increase surgical complexity,” the authors conclude. “Nonetheless, the reported improvements in tumor regression and systemic recurrence in the long-interval group were unexpectedly not followed by improved [overall survival].”
SOURCE:
F. Borja de Lacy, MD, PhD, Hospital Clinic of Barcelona, University of Barcelona, led the study, published online in JAMA Surgery, with an accompanying editorial.
LIMITATIONS:
- The study’s main limitation was its retrospective design, which could have resulted in missing or inconsistent data, as well as the short follow-up time.
- Decisions about time interval were based more on professional preference rather than specific tumor characteristics.
DISCLOSURES:
Dr. de Lacy has reported no relevant financial relationships. No outside funding source was disclosed.
A version of this article first appeared on Medscape.com.
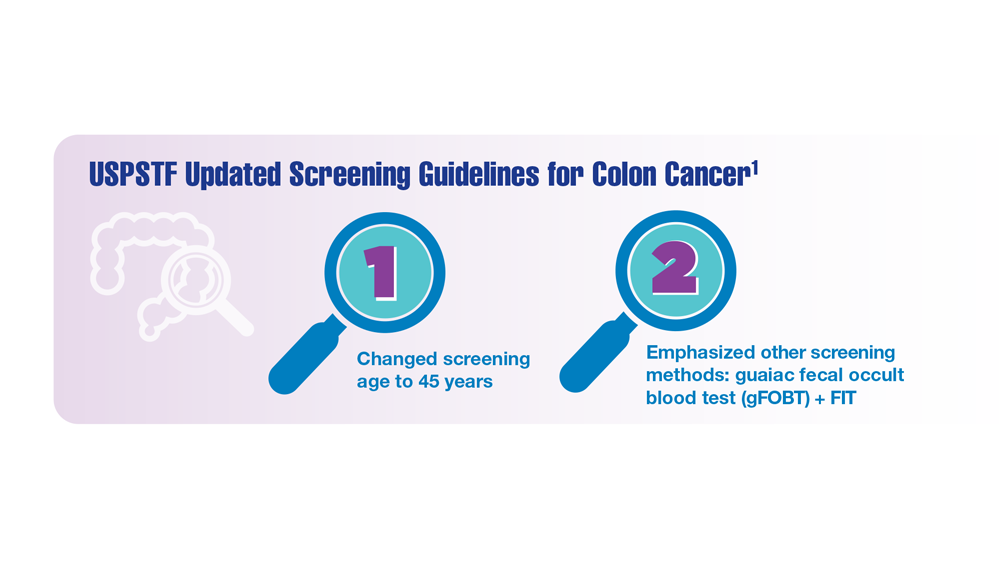
Screening Guideline Updates and New Treatments in Colon Cancer
- Ng K et al. JAMA. 2021;325(19):1943-1945. doi:10.1001/jama.2021.4133
- Xie YH et al. Signal Transduct Target Ther. 2020;5(1):22. doi:10.1038/s41392-020-0116-z
- Muller C et al. Cells. 2021;10(5):1018. doi:10.3390/cells10051018
- Clebak KT et al. Am Fam Physician. 2022;105(2):198-200.
- May FP et al. Dig Dis Sci. 2017;62(8):1923-1932. doi:10.1007/s10620-017-4607-x
- May FP et al. Med Care. 2019;57(10):773-780. doi:10.1097/MLR.0000000000001186
- US Department of Veterans Affairs, National Oncology Program Office. National Precision Oncology Program (NPOP). Updated June 24, 2022. Accessed December 14, 2022. http://www.cancer.va.gov/CANCER/NPOP.asp
- André T et al; KEYNOTE-177 Investigators. N Engl J Med. 2020;383(23):2207-2218. doi:10.1056/NEJMoa2017699
- Naidoo M et al. Cancers (Basel). 2021;13(2):346. doi:10.3390/cancers13020346
- Kasi PM et al. BMJ Open. 2021;11(9):e047831. doi:10.1136/bmjopen-2020-047831
- Jin S et al. Proc Natl Acad Sci U S A. 2021;118(5):e2017421118. doi:10.1073/pnas.2017421118
- Ng K et al. JAMA. 2021;325(19):1943-1945. doi:10.1001/jama.2021.4133
- Xie YH et al. Signal Transduct Target Ther. 2020;5(1):22. doi:10.1038/s41392-020-0116-z
- Muller C et al. Cells. 2021;10(5):1018. doi:10.3390/cells10051018
- Clebak KT et al. Am Fam Physician. 2022;105(2):198-200.
- May FP et al. Dig Dis Sci. 2017;62(8):1923-1932. doi:10.1007/s10620-017-4607-x
- May FP et al. Med Care. 2019;57(10):773-780. doi:10.1097/MLR.0000000000001186
- US Department of Veterans Affairs, National Oncology Program Office. National Precision Oncology Program (NPOP). Updated June 24, 2022. Accessed December 14, 2022. http://www.cancer.va.gov/CANCER/NPOP.asp
- André T et al; KEYNOTE-177 Investigators. N Engl J Med. 2020;383(23):2207-2218. doi:10.1056/NEJMoa2017699
- Naidoo M et al. Cancers (Basel). 2021;13(2):346. doi:10.3390/cancers13020346
- Kasi PM et al. BMJ Open. 2021;11(9):e047831. doi:10.1136/bmjopen-2020-047831
- Jin S et al. Proc Natl Acad Sci U S A. 2021;118(5):e2017421118. doi:10.1073/pnas.2017421118
- Ng K et al. JAMA. 2021;325(19):1943-1945. doi:10.1001/jama.2021.4133
- Xie YH et al. Signal Transduct Target Ther. 2020;5(1):22. doi:10.1038/s41392-020-0116-z
- Muller C et al. Cells. 2021;10(5):1018. doi:10.3390/cells10051018
- Clebak KT et al. Am Fam Physician. 2022;105(2):198-200.
- May FP et al. Dig Dis Sci. 2017;62(8):1923-1932. doi:10.1007/s10620-017-4607-x
- May FP et al. Med Care. 2019;57(10):773-780. doi:10.1097/MLR.0000000000001186
- US Department of Veterans Affairs, National Oncology Program Office. National Precision Oncology Program (NPOP). Updated June 24, 2022. Accessed December 14, 2022. http://www.cancer.va.gov/CANCER/NPOP.asp
- André T et al; KEYNOTE-177 Investigators. N Engl J Med. 2020;383(23):2207-2218. doi:10.1056/NEJMoa2017699
- Naidoo M et al. Cancers (Basel). 2021;13(2):346. doi:10.3390/cancers13020346
- Kasi PM et al. BMJ Open. 2021;11(9):e047831. doi:10.1136/bmjopen-2020-047831
- Jin S et al. Proc Natl Acad Sci U S A. 2021;118(5):e2017421118. doi:10.1073/pnas.2017421118
Cancer Data Trends 2023
Federal Practitioner and the Association of VA Hematology/Oncology (AVAHO) present the 2023 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- COVID-19 Outcomes in Veterans With Hematologic Cancers
- Promising New Approaches for Testicular and Prostate Cancer
- Screening Guideline Updates and New Treatments in Colon Cancer
- Exposure-Related Cancers: A Look at the PACT Act
- New Classifications and Emerging Treatments in Brain Cancer
- Gender Disparity in Breast Cancer Among US Veterans
- Lung Cancer Screening in Veterans
- Necessary Updates to Skin Cancer Risk Stratification
- Innovation in Cancer Treatment
Federal Practitioner and the Association of VA Hematology/Oncology (AVAHO) present the 2023 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- COVID-19 Outcomes in Veterans With Hematologic Cancers
- Promising New Approaches for Testicular and Prostate Cancer
- Screening Guideline Updates and New Treatments in Colon Cancer
- Exposure-Related Cancers: A Look at the PACT Act
- New Classifications and Emerging Treatments in Brain Cancer
- Gender Disparity in Breast Cancer Among US Veterans
- Lung Cancer Screening in Veterans
- Necessary Updates to Skin Cancer Risk Stratification
- Innovation in Cancer Treatment
Federal Practitioner and the Association of VA Hematology/Oncology (AVAHO) present the 2023 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- COVID-19 Outcomes in Veterans With Hematologic Cancers
- Promising New Approaches for Testicular and Prostate Cancer
- Screening Guideline Updates and New Treatments in Colon Cancer
- Exposure-Related Cancers: A Look at the PACT Act
- New Classifications and Emerging Treatments in Brain Cancer
- Gender Disparity in Breast Cancer Among US Veterans
- Lung Cancer Screening in Veterans
- Necessary Updates to Skin Cancer Risk Stratification
- Innovation in Cancer Treatment
Key red flags for early-onset colorectal cancer
As the number of cases of early-onset colorectal cancer (CRC) diagnosed before age 50 continues to rise, early detection has become increasingly important.
The signs and symptoms are abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia.
Two symptoms in particular – rectal bleeding and iron-deficiency anemia – point to the need for timely endoscopy and follow-up, the researchers say.
“Colorectal cancer is not simply a disease affecting older people; we want younger adults to be aware of and act on these potentially very telling signs and symptoms – particularly because people under 50 are considered to be at low risk, and they don’t receive routine colorectal cancer screening,” senior investigator Yin Cao, ScD, with Washington University School of Medicine, St. Louis, said in a news release.
“It’s also crucial to spread awareness among primary care doctors, gastroenterologists, and emergency medicine doctors,” Dr. Cao added. “To date, many early-onset colorectal cancers are detected in emergency rooms, and there often are significant diagnostic delays with this cancer.”
The study was published online in the Journal of the National Cancer Institute.
Although previous research has identified rectal bleeding, iron-deficiency anemia, and rectal/abdominal pain as symptoms of early-onset CRC, most studies “have aggregated symptoms till the time of diagnosis,” which limits their use for early detection, the authors explain.
In the current study, the researchers analyzed data from more than 5,000 cases of early-onset CRC and from more than 22,000 control patients using the IBM MarketScan commercial database.
Dr. Cao and colleagues found that between 3 months and 2 years before diagnosis, abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia each indicated an increased risk for early-onset CRC.
Among patients with early-onset CRC, 19.3% presented with one or more of the four red flags between 3 months and 2 years prior to the index date; 15.6% had one symptom, and 3.7% had two or more.
After multivariable adjustment, having one symptom almost doubled the risk for early-onset CRC (odds ratio, 1.94); having two symptoms increased risk by more than threefold (OR, 3.59); and having three or more boosted the risk by more than 6.5-fold (OR, 6.52).
Abdominal pain was associated with a 34% higher risk of early-onset CRC (11.6% among case patients vs. 7.7% among controls; OR, 1.34).
Although not as common, rectal bleeding was associated with the highest odds for early-onset CRC (7.2% case patients vs. 1.3% controls; OR, 5.13).
The other predictive signs and symptoms included diarrhea (2.8% case patients vs. 1.4% controls; OR, 1.43) and iron-deficiency anemia (2.3% case patients vs. 0.9% controls; OR, 2.07).
No differences were observed by gender for each sign or symptom.
Among patients with a red-flag symptom who presented between 3 months and 2 years before diagnosis, for those with early-onset CRC, the median diagnostic interval was 8.7 months.
The researchers suggest that clinicians prioritize prompt diagnostic workups for patients younger than 50 who present with rectal bleeding and/or iron-deficiency anemia and that they also keep abdominal pain and diarrhea in mind as early symptoms.
Dr. Cao noted that since most early-onset CRC cases “have been and will continue to be diagnosed after symptom presentation, it is crucial to recognize these red-flag signs and symptoms promptly and conduct a diagnostic workup as soon as possible.
“By doing so, we can diagnose the disease earlier, which in turn can reduce the need for more aggressive treatment and improve patients’ quality of life and survival rates,” said Dr. Cao.
The study was supported by grants from the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article originally appeared on Medscape.com.
As the number of cases of early-onset colorectal cancer (CRC) diagnosed before age 50 continues to rise, early detection has become increasingly important.
The signs and symptoms are abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia.
Two symptoms in particular – rectal bleeding and iron-deficiency anemia – point to the need for timely endoscopy and follow-up, the researchers say.
“Colorectal cancer is not simply a disease affecting older people; we want younger adults to be aware of and act on these potentially very telling signs and symptoms – particularly because people under 50 are considered to be at low risk, and they don’t receive routine colorectal cancer screening,” senior investigator Yin Cao, ScD, with Washington University School of Medicine, St. Louis, said in a news release.
“It’s also crucial to spread awareness among primary care doctors, gastroenterologists, and emergency medicine doctors,” Dr. Cao added. “To date, many early-onset colorectal cancers are detected in emergency rooms, and there often are significant diagnostic delays with this cancer.”
The study was published online in the Journal of the National Cancer Institute.
Although previous research has identified rectal bleeding, iron-deficiency anemia, and rectal/abdominal pain as symptoms of early-onset CRC, most studies “have aggregated symptoms till the time of diagnosis,” which limits their use for early detection, the authors explain.
In the current study, the researchers analyzed data from more than 5,000 cases of early-onset CRC and from more than 22,000 control patients using the IBM MarketScan commercial database.
Dr. Cao and colleagues found that between 3 months and 2 years before diagnosis, abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia each indicated an increased risk for early-onset CRC.
Among patients with early-onset CRC, 19.3% presented with one or more of the four red flags between 3 months and 2 years prior to the index date; 15.6% had one symptom, and 3.7% had two or more.
After multivariable adjustment, having one symptom almost doubled the risk for early-onset CRC (odds ratio, 1.94); having two symptoms increased risk by more than threefold (OR, 3.59); and having three or more boosted the risk by more than 6.5-fold (OR, 6.52).
Abdominal pain was associated with a 34% higher risk of early-onset CRC (11.6% among case patients vs. 7.7% among controls; OR, 1.34).
Although not as common, rectal bleeding was associated with the highest odds for early-onset CRC (7.2% case patients vs. 1.3% controls; OR, 5.13).
The other predictive signs and symptoms included diarrhea (2.8% case patients vs. 1.4% controls; OR, 1.43) and iron-deficiency anemia (2.3% case patients vs. 0.9% controls; OR, 2.07).
No differences were observed by gender for each sign or symptom.
Among patients with a red-flag symptom who presented between 3 months and 2 years before diagnosis, for those with early-onset CRC, the median diagnostic interval was 8.7 months.
The researchers suggest that clinicians prioritize prompt diagnostic workups for patients younger than 50 who present with rectal bleeding and/or iron-deficiency anemia and that they also keep abdominal pain and diarrhea in mind as early symptoms.
Dr. Cao noted that since most early-onset CRC cases “have been and will continue to be diagnosed after symptom presentation, it is crucial to recognize these red-flag signs and symptoms promptly and conduct a diagnostic workup as soon as possible.
“By doing so, we can diagnose the disease earlier, which in turn can reduce the need for more aggressive treatment and improve patients’ quality of life and survival rates,” said Dr. Cao.
The study was supported by grants from the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article originally appeared on Medscape.com.
As the number of cases of early-onset colorectal cancer (CRC) diagnosed before age 50 continues to rise, early detection has become increasingly important.
The signs and symptoms are abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia.
Two symptoms in particular – rectal bleeding and iron-deficiency anemia – point to the need for timely endoscopy and follow-up, the researchers say.
“Colorectal cancer is not simply a disease affecting older people; we want younger adults to be aware of and act on these potentially very telling signs and symptoms – particularly because people under 50 are considered to be at low risk, and they don’t receive routine colorectal cancer screening,” senior investigator Yin Cao, ScD, with Washington University School of Medicine, St. Louis, said in a news release.
“It’s also crucial to spread awareness among primary care doctors, gastroenterologists, and emergency medicine doctors,” Dr. Cao added. “To date, many early-onset colorectal cancers are detected in emergency rooms, and there often are significant diagnostic delays with this cancer.”
The study was published online in the Journal of the National Cancer Institute.
Although previous research has identified rectal bleeding, iron-deficiency anemia, and rectal/abdominal pain as symptoms of early-onset CRC, most studies “have aggregated symptoms till the time of diagnosis,” which limits their use for early detection, the authors explain.
In the current study, the researchers analyzed data from more than 5,000 cases of early-onset CRC and from more than 22,000 control patients using the IBM MarketScan commercial database.
Dr. Cao and colleagues found that between 3 months and 2 years before diagnosis, abdominal pain, rectal bleeding, diarrhea, and iron-deficiency anemia each indicated an increased risk for early-onset CRC.
Among patients with early-onset CRC, 19.3% presented with one or more of the four red flags between 3 months and 2 years prior to the index date; 15.6% had one symptom, and 3.7% had two or more.
After multivariable adjustment, having one symptom almost doubled the risk for early-onset CRC (odds ratio, 1.94); having two symptoms increased risk by more than threefold (OR, 3.59); and having three or more boosted the risk by more than 6.5-fold (OR, 6.52).
Abdominal pain was associated with a 34% higher risk of early-onset CRC (11.6% among case patients vs. 7.7% among controls; OR, 1.34).
Although not as common, rectal bleeding was associated with the highest odds for early-onset CRC (7.2% case patients vs. 1.3% controls; OR, 5.13).
The other predictive signs and symptoms included diarrhea (2.8% case patients vs. 1.4% controls; OR, 1.43) and iron-deficiency anemia (2.3% case patients vs. 0.9% controls; OR, 2.07).
No differences were observed by gender for each sign or symptom.
Among patients with a red-flag symptom who presented between 3 months and 2 years before diagnosis, for those with early-onset CRC, the median diagnostic interval was 8.7 months.
The researchers suggest that clinicians prioritize prompt diagnostic workups for patients younger than 50 who present with rectal bleeding and/or iron-deficiency anemia and that they also keep abdominal pain and diarrhea in mind as early symptoms.
Dr. Cao noted that since most early-onset CRC cases “have been and will continue to be diagnosed after symptom presentation, it is crucial to recognize these red-flag signs and symptoms promptly and conduct a diagnostic workup as soon as possible.
“By doing so, we can diagnose the disease earlier, which in turn can reduce the need for more aggressive treatment and improve patients’ quality of life and survival rates,” said Dr. Cao.
The study was supported by grants from the National Institutes of Health. The authors declared no conflicts of interest.
A version of this article originally appeared on Medscape.com.
FROM JOURNAL OF THE NATIONAL CANCER INSTITUTE
Longitudinal Dynamic in Weight Loss Impacts Clinical Outcomes for Veterans Undergoing Curative Surgery for Colorectal Cancer
In patients with gastrointestinal (GI) malignancies, malnutrition is common. In addition, it has various negative implications, including high risk for surgical complications, prolonged hospitalization, decreased quality of life (QOL), increased mortality, and poor tolerance for treatments such as chemotherapy and radiotherapy.1
A 2014 French study of 1903 patients hospitalized for cancer reported a 39% overall prevalence of malnutrition; 39% in patients with cancers of the colon/rectum, 60% for pancreatic cancer, and 67% for cancers of the esophagus/stomach.2 Malnutrition was defined as body mass index (BMI) < 18.5 for individuals aged < 75 years or BMI < 21 for individuals aged ≥ 75 years, and/or weight loss > 10% since disease onset. Malnutrition also was strongly associated with worsened performance status.
The etiology of malnutrition in GI cancers is often multifactorial. It includes systemic tumor effects, such as inflammatory mediators contributing to hypermetabolism and cachexia, local tumor-associated mechanical obstruction, GI toxicities caused by antineoplastic therapy or other medications, and psychological factors that contribute to anorexia.3 Patient-related risk factors such as older age, other chronic diseases, and history of other GI surgeries also play a role.1
Other studies have demonstrated that malnutrition in patients with GI malignancies undergoing surgical resection is associated with high rates of severe postoperative complications, increased length of stay (LOS) and time on a ventilator for patients treated in the intensive care unit, and poor QOL in the postoperative survival period.4-6 Several randomized controlled trials conducted in patients with GI cancers have shown that enteral and parenteral nutrition supplementations in the perioperative period improve various outcomes, such as reduction of postoperative complication rates, fewer readmissions, improved chemotherapy tolerance, and improved QOL.7-10 Thus, in the management of patients with GI malignancies, it is highly important to implement early nutritional screening and establish a diagnosis of malnutrition to intervene and reduce postoperative morbidity and mortality.1
However, tools and predictors of malnutrition are often imperfect. The Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (AND/ASPEN) weight-based criteria define malnutrition and nutritionally-at-risk as BMI < 18.5, involuntary loss of at least 10% of body weight within 6 months or 5% within 1 month, or loss of 10 lb within 6 months.11 While the ASPEN criteria are often used to define malnourishment, they may not fully capture the population at risk, and there does not exist a gold-standard tool for nutritional screening. A 2002 study that performed a critical appraisal of 44 nutritional screening tools found that no single tool was fully sufficient for application, development, evaluation, and consistent screening.12 As such, consistently screening for malnutrition to target interventions in the perioperative period for GI surgical oncology has been challenging.13 More recent tools such as the perioperative nutrition screen (PONS) have been validated as rapid, effective screening tools to predict postoperative outcomes.14 Additionally, implementation of perioperative nutritional protocols, such as enhanced recovery after surgery (ERAS) in colon cancer (CC) surgery, also has shown improved perioperative care and outcomes.15
Preoperative nutritional interventions have been implemented in practice and have focused mostly on the immediate perioperative period. This has been shown to improve surgical outcomes. The Veterans Health Administration (VHA) provides comprehensive care to patients in a single-payer system, allowing for capture of perioperative data and the opportunity for focused preoperative interventions to improve outcomes.
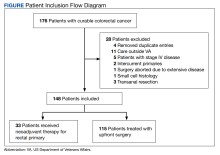
Methods
This was a retrospective record review of colorectal malignancies treated with curative intent at the Veterans Affairs Ann Arbor Healthcare System (VAAAHS) in Michigan between January 1, 2015, and December 31, 2019. We examined nutritional status, degree of longitudinal weight loss, and subsequent clinical outcomes, including delayed postoperative recovery and delays in chemotherapy in 115 patients with CC and 33 patients with rectal cancer (RC) undergoing curative surgical resection at VAAAHS. To avoid additional confounding effects of advanced cancer, only early-stage, curable disease was included. This study was approved by the VAAAHS Institutional Review Board.
Patients with postoperative follow-up outside of VAAAHS were excluded. Patients were excluded if their surgery had noncurative intent or if they had distant metastatic disease. Data on patient weights, laboratory results, nutrition consultations, postoperative complications, delayed recovery, readmissions, and chemotherapy tolerance were abstracted by patient chart review in the VHA Computerized Patient Record System and Joint Legacy Viewer by 2 researchers.
Delayed recovery was defined as any abnormal clinical development described in inpatient progress notes, outpatient follow-up notes within 60 days, or in hospital discharge summaries. Excluded were psychiatric events without additional medical complications, postoperative bleeding not requiring an invasive intervention, urinary retention, postoperative glycemic control difficulties, cardiac events that happened before postoperative hospital discharge and not requiring readmission, and postoperative alcohol withdrawal. Complications were defined similarly to delayed recovery but excluded isolated prolonged postoperative ileus. LOS was defined in days as time from admission to discharge.
Adjuvant management course was derived from reviewing documentation from medical oncology consultations and progress notes. In patients for whom adjuvant chemotherapy was indicated and prescribed, chemotherapy was considered complete if chemotherapy was started and completed as indicated. Adjuvant chemotherapy was considered incomplete if the patient declined chemotherapy, if chemotherapy was not started when indicated, or if chemotherapy was not completed as indicated. Neoadjuvant therapy data were abstracted from medical and radiation oncology notes.
Recorded data were collected on both weight and BMI. Weights were extracted as follows: Weight 1 year before time of diagnosis, ± 4 months; weight 6 months before diagnosis ± 3 months; weight at time of diagnosis ± 2 weeks; weight at time of surgery ± 2 weeks; weight 30 days postsurgery ± 2 weeks; weight 60 days postsurgery ± 2 weeks; weight 1 year postsurgery ± 4 months. Mean percent change in weight was calculated from recorded weights between each allocated time point. A weight loss of ≥ 3% was found to be clinically relevant and was chosen as the minimal cutoff value when analyzing outcomes associated with weight trends.
Nutrition consultations were abstracted as follows: Preoperative nutrition consultations were defined as occurring between time of cancer diagnosis and surgery in either the inpatient or outpatient setting; inpatient postoperative nutrition consultations occurred during admission for surgery; readmission nutrition consultations occurred on readmission in inpatient setting, if applicable; outpatient postoperative nutrition consultations were defined as occurring up to 2 months postdischarge in the outpatient setting.
Albumin values were extracted as follows: Preoperative albumin levels were defined as up to 4 months prior to diagnosis, and postoperative albumin levels were defined as 2 to 6 months after surgery.
Analysis
The data were described using mean (SD) for continuous variables and number and percentages for categorical variables. Where appropriate, Fisher exact test, Pearson χ2 test, Spearman ρ, and Mann-Whitney U test were used for tests of significance. SAS (SAS Institute) was utilized for multivariable analysis. The significance level was P = .05 for all tests.
Results
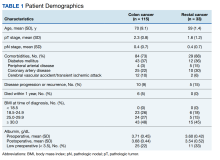
There were 115 patients in the CC cohort and 33 in the RC cohort. The mean (SD) age at diagnosis was 70 (9.1) for CC group and 59 (1.4) for RC group (Table 1).
Weight Trends
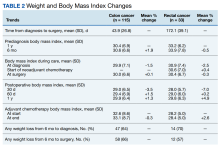
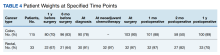
From 1 year to 6 months before diagnosis, 40 of 80 patients lost weight in the CC cohort (mean change, +1.9%) and 6 of 22 patients lost weight in the RC cohort (mean change, + 0.5%). From 6 months before diagnosis to time of diagnosis, 47 of 74 patients lost weight in the CC cohort (mean change, -1.5%) and 14 of 21 patients lost weight in the RC cohort (mean change, -2.5%). From time of diagnosis to time of surgery, 36 of 104 patients with CC and 14 of 32 patients with RC lost weight with a mean weight change of and +0.1% and -0.3%, respectively. In the 6 months before surgery, any amount of weight loss was observed in 58 patients (66%) in the CC group and in 12 patients (57%) in the RC group. In this time frame, in the CC cohort, 32 patients (36%) were observed to have at least 3% weight loss, and 23 (26%) were observed to have at least 5% weight loss (Table 3).
In patients who completed adjuvant chemotherapy in the CC group, mean (SD) BMI at the beginning and end of chemotherapy was 32.6 (8.6) and 33.1 (8.7), respectively, and a -0.3% mean change in weight was observed. In the RC group, mean (SD) BMI was 28.2 (5.0) at the initiation of adjuvant chemotherapy and 28.4 (5.0) at its completion, with a +2.6% mean change in weight.
In the immediate postoperative period, most patients were losing weight in both the CC and RC groups (mean, -3.5% and -7.0% at 1 month postoperative, respectively). At 1-year after surgery, patients had modest mean increases in weight: +1.3% for patients with CC and +4.9% for patients with RC.
A relatively large proportion of patients had missing data on weights at various data points (Table 4).
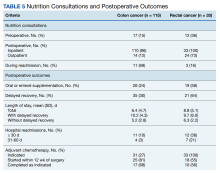
Nutrition Consultations
In the CC group, preoperative nutrition consultations (either inpatient or outpatient) occurred in 17 patients (15%). Inpatient postoperative nutrition evaluations occurred in 110 patients (96%) (Table 5).
In the RC group, preoperative inpatient or outpatient nutrition consultations occurred in 12 patients (36%). Eight of those occurred before initiation of neoadjuvant chemoradiotherapy. All 33 patients received an inpatient postoperative nutrition evaluation during admission. Oral or enteral nutrition supplements were prescribed 19 times (58%). Postoperative outpatient nutrition consultations occurred for 24 patients (73%). Of the 19 patients who were readmitted to the hospital, 3 (16%) had a nutrition reconsultation on readmission.
Outcomes
The primary outcomes observed were delayed recovery, hospital readmission and LOS, and completion of adjuvant chemotherapy as indicated. Delayed recovery was observed in 35 patients with CC (40%) and 21 patients with RC (64%). Multivariable analysis in the CC cohort demonstrated that weight change was significantly associated with delayed recovery. Among those with ≥ 3% weight loss in the 6-month preoperative period (the weight measurement 6 months prior to diagnosis to date of surgery), 20 patients (63%) had delayed recovery compared with 15 patients (27%) without ≥ 3% weight loss who experienced delayed recovery (χ2 = 10.84; P < .001).
Weight loss of ≥ 3% in the 6-month preoperative period also was significantly associated with complications. Of patients with at least 3% preoperative weight loss, 16 (50%) experienced complications, while 8 (14%) with < 3% preoperative weight loss experienced complications (χ2 = 11.20; P < .001). Notably, ≥ 3% weight loss in the 1-year preoperative period before surgery was not significantly associated with delayed recovery. Any degree of 30-day postoperative weight loss was not correlated with delayed recovery. Finally, low preoperative albumin also was not correlated with delayed recovery (Fisher exact; P = .13). Table 3 displays differences based on presence of delayed recovery in the 88 patients with CC 6 months before surgery. Of note, ≥ 10-lb weight loss in the 6 months preceding surgery also correlated with delayed recovery (P = .01).In our cohort, 3% weight loss over 6 months had a sensitivity of 57%, specificity of 77%, positive predictive value 63%, and negative predictive value 73% for delayed recovery. By comparison, a 10-lb weight loss in 6 months per ASPEN criteria had a sensitivity of 40%, specificity of 85%, positive predictive value 64%, and negative predictive value 68% for delayed recovery.
Hospital Readmissions and LOS
Hospital readmissions occurred within the first 30 days in 11 patients (10%) in the CC cohort and 12 patients (36%) in the RC cohort. Readmissions occurred between 31 and 60 days in 4 (3%) and 7 (21%) of CC and RC cohorts, respectively. The presence of ≥ 3% weight loss in the 6-month
Mean (SD) LOS was 6.4 (4.7) days (range, 1-28) for patients with CC and 8.8 (5.1) days (range, 3-23) for patients with RC. Mean (SD) LOS increased to 10.2 (4.3) days and 9.7 (6.0) days in patients with delayed recovery in the CC and RC cohorts, respectively. The mean (SD) LOS was 5.2 (2.8) days and 6.3 (2.2) days in patients without delayed recovery in the CC and RC cohorts, respectively. There was no significant difference when examining association between percent weight change and LOS for either initial admission (rs= -0.1409; 2-tailed P = .19) or for initial and readmission combined (rs = -0.13532; 2-tailed P = .21) within the CC cohort.
Chemotherapy
Within the CC cohort, 31 patients (27%) had an indication for adjuvant chemotherapy. Of these, 25 of 31 (81%) started chemotherapy within 12 weeks of surgical resection, and of these, 17 of 25 patients (68%) completed chemotherapy as indicated. Within the RC cohort all 33 patients had an indication for adjuvant chemotherapy, of these 18 of 33 patients (55%) began within 12 weeks of surgical resection, and 10 of 18 (56%) completed chemotherapy as indicated.
Among the CC cohort who began but did not complete adjuvant chemotherapy, there was no significant association between completion of chemotherapy and
Discussion
This study highlights several important findings. There were no patients in our cohort that met ASPEN malnourishment criteria with a BMI < 18.5. Twenty percent of patients lost at least 10 lb in 6 months before the operation. Notably, patients had significant associations with adverse outcomes with less pronounced weight loss than previously noted. As has been established previously, malnourishment can be difficult to screen for, and BMI also is often an imprecise tool.12 In the CC cohort, weight loss
Our findings imply that the effects of even mild malnutrition are even more profound than previously thought. Significantly, this applies to overweight and obese patients as well, as these constituted a significant fraction of our cohort. A finding of ≥ 3% weight loss at the time of CC diagnosis may provide an opportunity for a focused nutrition intervention up to the time of surgery. Second, although nutrition consultation was frequent in the inpatient setting during the hospital admission (96%-100%), rates of nutrition evaluation were as low as 15% before surgery and 12% after surgery, representing a key area for improvement and focused intervention. An optimal time for intervention and nutrition prehabilitation would be at time of diagnosis before surgery with plans for continued aggressive monitoring and subsequent follow-up. Our finding seems to provide a more sensitive tool to identify patients at risk for delayed recovery compared with the ASPEN-driven assessment. Given the simplicity and the clinical significance, our test consisting of 3% weight loss over 6 months, with its sensitivity of 57%, may be superior to the ASPEN 10-lb weight loss, with its sensitivity of 40% in our cohort.
Previous Studies
Our findings are consistent with previous studies that have demonstrated that perioperative weight loss and malnutrition are correlated with delayed recovery and complications, such as wound healing, in patients with GI cancer.2,4,5,8 In a retrospective study of more than 7000 patients with CC, those who were overweight or obese were found to have an improved overall survival compared with other BMI categories, and those who were underweight had an increased 30-day mortality and postoperative complications.16
In another retrospective study of 3799 patients with CC, those who were overweight and obese had an improved 5-year survival rate compared with patients whose weight was normal or underweight. Outcomes were found to be stage dependent.17 In this study cohort, all patients were either overweight or obese and remained in that category even with weight loss. This may have contributed to overall improved outcomes.
Implications and Next Steps
Our study has several implications. One is that BMI criteria < 18.5 may not be a good measure for malnutrition given that about 75% of the patients in our cohort were overweight or obese and none were underweight. We also show a concrete, easily identifiable finding of percent weight change that could be addressed as an automated electronic notification and potentially identify a patient at risk and serve as a trigger for both timely and early nutrition intervention. It seems to be more sensitive than the ASPEN criterion of 10-lb weight loss in 6 months before surgery. Sensitivity is especially appealing given the ease and potential of embedding this tool in an electronic health record and the clinical importance of the consequent intervention. Preoperative as opposed to perioperative nutrition optimization at time of CC diagnosis is essential, as it may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Finally, although our study found that rates of inpatient postoperative nutrition consultation were high, rates of outpatient nutrition consultation in the preoperative period were low. This represents a missed opportunity for intervention before surgery. Similarly, rates of postoperative nutrition follow-up period were low, which points to an area for improvement in longitudinal and holistic care.
We suggest modifications to nutrition intervention protocols, such as ERAS, which should start at the time of GI malignancy diagnosis.18 Other suggestions include standard involvement of nutritionists in inpatient and outpatient settings with longitudinal follow-up in the preoperative and postoperative periods and patient enrollment in a nutrition program with monitoring at time of diagnosis at the VHA. Our findings as well as previous literature suggest that the preoperative period is the most important time to intervene with regard to nutrition optimization and represents an opportunity for intensive prehabilitation. Future areas of research include incorporating other important measures of malnourishment independent of BMI into future study designs, such as sarcopenia and adipose tissue density, to better assess body composition and predict prognostic risk in CC.18,19
Strengths and Limitations
This study is limited by its single-center, retrospective design and small sample sizes, and we acknowledge the limitations of our data set. However, the strength of this VHA-based study is that the single-payer system allows for complete capture of perioperative data as well as the opportunity for focused preoperative interventions to improve outcomes. To our knowledge, there is no currently existing literature on improving nutrition protocols at the VHA for patients with a GI malignancy. These retrospective data will help inform current gaps in quality improvement and supportive oncology as it relates to optimizing malnourishment in veterans undergoing surgical resection for their cancer.
Conclusions
In the CC cohort, weight loss of ≥ 3% from 6 months prior to time of surgery was significantly associated with delayed recovery, complications, and hospital readmissions. Our findings suggest that patients with CC undergoing surgery may benefit from an intensive, early nutrition prehabilitation. Preoperative nutrition optimization may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Further research would be able to clarify these hypotheses.
1. Benoist S, Brouquet A. Nutritional assessment and screening for malnutrition. J Visc Surg. 2015;152:S3-S7. doi:10.1016/S1878-7886(15)30003-5
2. Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. J Parenter Enter Nutr. 2014;38(2):196-204. doi:10.1177/0148607113502674
3. Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9:S51-S63. doi:10.1016/j.ejon.2005.09.007
4. Nishiyama VKG, Albertini SM, de Moraes CMZG, et al. Malnutrition and clinical outcomes in surgical patients with colorectal disease. Arq Gastroenterol. 2018;55(4):397-402. doi:10.1590/s0004-2803.201800000-85
5. Shpata V, Prendushi X, Kreka M, Kola I, Kurti F, Ohri I. Malnutrition at the time of surgery affects negatively the clinical outcome of critically ill patients with gastrointestinal cancer. Med Arch Sarajevo Bosnia Herzeg. 2014;68(4):263-267. doi:10.5455/medarh.2014.68.263-267
6. Lim HS, Cho GS, Park YH, Kim SK. Comparison of quality of life and nutritional status in gastric cancer patients undergoing gastrectomies. Clin Nutr Res. 2015;4(3):153-159. doi:10.7762/cnr.2015.4.3.153
7. Bozzetti F, Gavazzi C, Miceli R, et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. J Parenter Enter Nutr. 2000;24(1):7-14. doi:10.1177/014860710002400107
8. Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr. 2007;26(6):698-709. doi:10.1016/j.clnu.2007.06.009
9. Bozzetti F, Braga M, Gianotti L, Gavazzi C, Mariani L. Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet. 2001; 358(9292):1487-1492. doi:10.1016/S0140-6736(01)06578-3
10. Meng Q, Tan S, Jiang Y, et al. Post-discharge oral nutritional supplements with dietary advice in patients at nutritional risk after surgery for gastric cancer: a randomized clinical trial. Clin Nutr Edinb Scotl. 2021;40(1):40-46. doi:10.1016/j.clnu.2020.04.043 start
11. White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738. doi:10.1016/j.jand.2012.03.012
12. Jones JM. The methodology of nutritional screening and assessment tools. J Hum Nutr Diet. 2002;15(1):59-71. doi:10.1046/j.1365-277X.2002.00327.x
13. Williams J, Wischmeyer P. Assessment of perioperative nutrition practices and attitudes—a national survey of colorectal and GI surgical oncology programs. Am J Surg. 2017;213(6):1010-1018. doi:10.1016/j.amjsurg.2016.10.008
14. Williams DG, Aronson S, Murray S, et al. Validation of the perioperative nutrition screen for prediction of postoperative outcomes. JPEN J Parenter Enteral Nutr. 2022;46(6):1307-1315. doi:10.1002/jpen.2310
15. Besson AJ, Kei C, Djordjevic A, Carter V, Deftereos I, Yeung J. Does implementation of and adherence to enhanced recovery after surgery improve perioperative nutritional management in colorectal cancer surgery? ANZ J Surg. 2022;92(6):1382-1387. doi:10.1111/ans.17599
16. Arkenbosch JHC, van Erning FN, Rutten HJ, Zimmerman D, de Wilt JHW, Beijer S. The association between body mass index and postoperative complications, 30-day mortality and long-term survival in Dutch patients with colorectal cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2019;45(2):160-166. doi:10.1016/j.ejso.2018.09.012
17. Shahjehan F, Merchea A, Cochuyt JJ, Li Z, Colibaseanu DT, Kasi PM. Body mass index and long-term outcomes in patients with colorectal cancer. Front Oncol. 2018;8:620. doi:10.3389/fonc.2018.00620
18. Nishigori T, Obama K, Sakai Y. Assessment of body composition and impact of sarcopenia and sarcopenic obesity in patients with gastric cancer. Transl Gastroenterol Hepatol. 2020;5:22. doi:10.21037/tgh.2019.10.13
19. Feliciano EMC, Winkels RM, Meyerhardt JA, Prado CM, Afman LA, Caan BJ. Abdominal adipose tissue radiodensity is associated with survival after colorectal cancer. Am J Clin Nutr. 2021;114(6):1917-1924. doi:10.1093/ajcn/nqab285
In patients with gastrointestinal (GI) malignancies, malnutrition is common. In addition, it has various negative implications, including high risk for surgical complications, prolonged hospitalization, decreased quality of life (QOL), increased mortality, and poor tolerance for treatments such as chemotherapy and radiotherapy.1
A 2014 French study of 1903 patients hospitalized for cancer reported a 39% overall prevalence of malnutrition; 39% in patients with cancers of the colon/rectum, 60% for pancreatic cancer, and 67% for cancers of the esophagus/stomach.2 Malnutrition was defined as body mass index (BMI) < 18.5 for individuals aged < 75 years or BMI < 21 for individuals aged ≥ 75 years, and/or weight loss > 10% since disease onset. Malnutrition also was strongly associated with worsened performance status.
The etiology of malnutrition in GI cancers is often multifactorial. It includes systemic tumor effects, such as inflammatory mediators contributing to hypermetabolism and cachexia, local tumor-associated mechanical obstruction, GI toxicities caused by antineoplastic therapy or other medications, and psychological factors that contribute to anorexia.3 Patient-related risk factors such as older age, other chronic diseases, and history of other GI surgeries also play a role.1
Other studies have demonstrated that malnutrition in patients with GI malignancies undergoing surgical resection is associated with high rates of severe postoperative complications, increased length of stay (LOS) and time on a ventilator for patients treated in the intensive care unit, and poor QOL in the postoperative survival period.4-6 Several randomized controlled trials conducted in patients with GI cancers have shown that enteral and parenteral nutrition supplementations in the perioperative period improve various outcomes, such as reduction of postoperative complication rates, fewer readmissions, improved chemotherapy tolerance, and improved QOL.7-10 Thus, in the management of patients with GI malignancies, it is highly important to implement early nutritional screening and establish a diagnosis of malnutrition to intervene and reduce postoperative morbidity and mortality.1
However, tools and predictors of malnutrition are often imperfect. The Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (AND/ASPEN) weight-based criteria define malnutrition and nutritionally-at-risk as BMI < 18.5, involuntary loss of at least 10% of body weight within 6 months or 5% within 1 month, or loss of 10 lb within 6 months.11 While the ASPEN criteria are often used to define malnourishment, they may not fully capture the population at risk, and there does not exist a gold-standard tool for nutritional screening. A 2002 study that performed a critical appraisal of 44 nutritional screening tools found that no single tool was fully sufficient for application, development, evaluation, and consistent screening.12 As such, consistently screening for malnutrition to target interventions in the perioperative period for GI surgical oncology has been challenging.13 More recent tools such as the perioperative nutrition screen (PONS) have been validated as rapid, effective screening tools to predict postoperative outcomes.14 Additionally, implementation of perioperative nutritional protocols, such as enhanced recovery after surgery (ERAS) in colon cancer (CC) surgery, also has shown improved perioperative care and outcomes.15
Preoperative nutritional interventions have been implemented in practice and have focused mostly on the immediate perioperative period. This has been shown to improve surgical outcomes. The Veterans Health Administration (VHA) provides comprehensive care to patients in a single-payer system, allowing for capture of perioperative data and the opportunity for focused preoperative interventions to improve outcomes.
Methods
This was a retrospective record review of colorectal malignancies treated with curative intent at the Veterans Affairs Ann Arbor Healthcare System (VAAAHS) in Michigan between January 1, 2015, and December 31, 2019. We examined nutritional status, degree of longitudinal weight loss, and subsequent clinical outcomes, including delayed postoperative recovery and delays in chemotherapy in 115 patients with CC and 33 patients with rectal cancer (RC) undergoing curative surgical resection at VAAAHS. To avoid additional confounding effects of advanced cancer, only early-stage, curable disease was included. This study was approved by the VAAAHS Institutional Review Board.
Patients with postoperative follow-up outside of VAAAHS were excluded. Patients were excluded if their surgery had noncurative intent or if they had distant metastatic disease. Data on patient weights, laboratory results, nutrition consultations, postoperative complications, delayed recovery, readmissions, and chemotherapy tolerance were abstracted by patient chart review in the VHA Computerized Patient Record System and Joint Legacy Viewer by 2 researchers.
Delayed recovery was defined as any abnormal clinical development described in inpatient progress notes, outpatient follow-up notes within 60 days, or in hospital discharge summaries. Excluded were psychiatric events without additional medical complications, postoperative bleeding not requiring an invasive intervention, urinary retention, postoperative glycemic control difficulties, cardiac events that happened before postoperative hospital discharge and not requiring readmission, and postoperative alcohol withdrawal. Complications were defined similarly to delayed recovery but excluded isolated prolonged postoperative ileus. LOS was defined in days as time from admission to discharge.
Adjuvant management course was derived from reviewing documentation from medical oncology consultations and progress notes. In patients for whom adjuvant chemotherapy was indicated and prescribed, chemotherapy was considered complete if chemotherapy was started and completed as indicated. Adjuvant chemotherapy was considered incomplete if the patient declined chemotherapy, if chemotherapy was not started when indicated, or if chemotherapy was not completed as indicated. Neoadjuvant therapy data were abstracted from medical and radiation oncology notes.
Recorded data were collected on both weight and BMI. Weights were extracted as follows: Weight 1 year before time of diagnosis, ± 4 months; weight 6 months before diagnosis ± 3 months; weight at time of diagnosis ± 2 weeks; weight at time of surgery ± 2 weeks; weight 30 days postsurgery ± 2 weeks; weight 60 days postsurgery ± 2 weeks; weight 1 year postsurgery ± 4 months. Mean percent change in weight was calculated from recorded weights between each allocated time point. A weight loss of ≥ 3% was found to be clinically relevant and was chosen as the minimal cutoff value when analyzing outcomes associated with weight trends.
Nutrition consultations were abstracted as follows: Preoperative nutrition consultations were defined as occurring between time of cancer diagnosis and surgery in either the inpatient or outpatient setting; inpatient postoperative nutrition consultations occurred during admission for surgery; readmission nutrition consultations occurred on readmission in inpatient setting, if applicable; outpatient postoperative nutrition consultations were defined as occurring up to 2 months postdischarge in the outpatient setting.
Albumin values were extracted as follows: Preoperative albumin levels were defined as up to 4 months prior to diagnosis, and postoperative albumin levels were defined as 2 to 6 months after surgery.
Analysis
The data were described using mean (SD) for continuous variables and number and percentages for categorical variables. Where appropriate, Fisher exact test, Pearson χ2 test, Spearman ρ, and Mann-Whitney U test were used for tests of significance. SAS (SAS Institute) was utilized for multivariable analysis. The significance level was P = .05 for all tests.
Results
There were 115 patients in the CC cohort and 33 in the RC cohort. The mean (SD) age at diagnosis was 70 (9.1) for CC group and 59 (1.4) for RC group (Table 1).
Weight Trends
From 1 year to 6 months before diagnosis, 40 of 80 patients lost weight in the CC cohort (mean change, +1.9%) and 6 of 22 patients lost weight in the RC cohort (mean change, + 0.5%). From 6 months before diagnosis to time of diagnosis, 47 of 74 patients lost weight in the CC cohort (mean change, -1.5%) and 14 of 21 patients lost weight in the RC cohort (mean change, -2.5%). From time of diagnosis to time of surgery, 36 of 104 patients with CC and 14 of 32 patients with RC lost weight with a mean weight change of and +0.1% and -0.3%, respectively. In the 6 months before surgery, any amount of weight loss was observed in 58 patients (66%) in the CC group and in 12 patients (57%) in the RC group. In this time frame, in the CC cohort, 32 patients (36%) were observed to have at least 3% weight loss, and 23 (26%) were observed to have at least 5% weight loss (Table 3).
In patients who completed adjuvant chemotherapy in the CC group, mean (SD) BMI at the beginning and end of chemotherapy was 32.6 (8.6) and 33.1 (8.7), respectively, and a -0.3% mean change in weight was observed. In the RC group, mean (SD) BMI was 28.2 (5.0) at the initiation of adjuvant chemotherapy and 28.4 (5.0) at its completion, with a +2.6% mean change in weight.
In the immediate postoperative period, most patients were losing weight in both the CC and RC groups (mean, -3.5% and -7.0% at 1 month postoperative, respectively). At 1-year after surgery, patients had modest mean increases in weight: +1.3% for patients with CC and +4.9% for patients with RC.
A relatively large proportion of patients had missing data on weights at various data points (Table 4).
Nutrition Consultations
In the CC group, preoperative nutrition consultations (either inpatient or outpatient) occurred in 17 patients (15%). Inpatient postoperative nutrition evaluations occurred in 110 patients (96%) (Table 5).
In the RC group, preoperative inpatient or outpatient nutrition consultations occurred in 12 patients (36%). Eight of those occurred before initiation of neoadjuvant chemoradiotherapy. All 33 patients received an inpatient postoperative nutrition evaluation during admission. Oral or enteral nutrition supplements were prescribed 19 times (58%). Postoperative outpatient nutrition consultations occurred for 24 patients (73%). Of the 19 patients who were readmitted to the hospital, 3 (16%) had a nutrition reconsultation on readmission.
Outcomes
The primary outcomes observed were delayed recovery, hospital readmission and LOS, and completion of adjuvant chemotherapy as indicated. Delayed recovery was observed in 35 patients with CC (40%) and 21 patients with RC (64%). Multivariable analysis in the CC cohort demonstrated that weight change was significantly associated with delayed recovery. Among those with ≥ 3% weight loss in the 6-month preoperative period (the weight measurement 6 months prior to diagnosis to date of surgery), 20 patients (63%) had delayed recovery compared with 15 patients (27%) without ≥ 3% weight loss who experienced delayed recovery (χ2 = 10.84; P < .001).
Weight loss of ≥ 3% in the 6-month preoperative period also was significantly associated with complications. Of patients with at least 3% preoperative weight loss, 16 (50%) experienced complications, while 8 (14%) with < 3% preoperative weight loss experienced complications (χ2 = 11.20; P < .001). Notably, ≥ 3% weight loss in the 1-year preoperative period before surgery was not significantly associated with delayed recovery. Any degree of 30-day postoperative weight loss was not correlated with delayed recovery. Finally, low preoperative albumin also was not correlated with delayed recovery (Fisher exact; P = .13). Table 3 displays differences based on presence of delayed recovery in the 88 patients with CC 6 months before surgery. Of note, ≥ 10-lb weight loss in the 6 months preceding surgery also correlated with delayed recovery (P = .01).In our cohort, 3% weight loss over 6 months had a sensitivity of 57%, specificity of 77%, positive predictive value 63%, and negative predictive value 73% for delayed recovery. By comparison, a 10-lb weight loss in 6 months per ASPEN criteria had a sensitivity of 40%, specificity of 85%, positive predictive value 64%, and negative predictive value 68% for delayed recovery.
Hospital Readmissions and LOS
Hospital readmissions occurred within the first 30 days in 11 patients (10%) in the CC cohort and 12 patients (36%) in the RC cohort. Readmissions occurred between 31 and 60 days in 4 (3%) and 7 (21%) of CC and RC cohorts, respectively. The presence of ≥ 3% weight loss in the 6-month
Mean (SD) LOS was 6.4 (4.7) days (range, 1-28) for patients with CC and 8.8 (5.1) days (range, 3-23) for patients with RC. Mean (SD) LOS increased to 10.2 (4.3) days and 9.7 (6.0) days in patients with delayed recovery in the CC and RC cohorts, respectively. The mean (SD) LOS was 5.2 (2.8) days and 6.3 (2.2) days in patients without delayed recovery in the CC and RC cohorts, respectively. There was no significant difference when examining association between percent weight change and LOS for either initial admission (rs= -0.1409; 2-tailed P = .19) or for initial and readmission combined (rs = -0.13532; 2-tailed P = .21) within the CC cohort.
Chemotherapy
Within the CC cohort, 31 patients (27%) had an indication for adjuvant chemotherapy. Of these, 25 of 31 (81%) started chemotherapy within 12 weeks of surgical resection, and of these, 17 of 25 patients (68%) completed chemotherapy as indicated. Within the RC cohort all 33 patients had an indication for adjuvant chemotherapy, of these 18 of 33 patients (55%) began within 12 weeks of surgical resection, and 10 of 18 (56%) completed chemotherapy as indicated.
Among the CC cohort who began but did not complete adjuvant chemotherapy, there was no significant association between completion of chemotherapy and
Discussion
This study highlights several important findings. There were no patients in our cohort that met ASPEN malnourishment criteria with a BMI < 18.5. Twenty percent of patients lost at least 10 lb in 6 months before the operation. Notably, patients had significant associations with adverse outcomes with less pronounced weight loss than previously noted. As has been established previously, malnourishment can be difficult to screen for, and BMI also is often an imprecise tool.12 In the CC cohort, weight loss
Our findings imply that the effects of even mild malnutrition are even more profound than previously thought. Significantly, this applies to overweight and obese patients as well, as these constituted a significant fraction of our cohort. A finding of ≥ 3% weight loss at the time of CC diagnosis may provide an opportunity for a focused nutrition intervention up to the time of surgery. Second, although nutrition consultation was frequent in the inpatient setting during the hospital admission (96%-100%), rates of nutrition evaluation were as low as 15% before surgery and 12% after surgery, representing a key area for improvement and focused intervention. An optimal time for intervention and nutrition prehabilitation would be at time of diagnosis before surgery with plans for continued aggressive monitoring and subsequent follow-up. Our finding seems to provide a more sensitive tool to identify patients at risk for delayed recovery compared with the ASPEN-driven assessment. Given the simplicity and the clinical significance, our test consisting of 3% weight loss over 6 months, with its sensitivity of 57%, may be superior to the ASPEN 10-lb weight loss, with its sensitivity of 40% in our cohort.
Previous Studies
Our findings are consistent with previous studies that have demonstrated that perioperative weight loss and malnutrition are correlated with delayed recovery and complications, such as wound healing, in patients with GI cancer.2,4,5,8 In a retrospective study of more than 7000 patients with CC, those who were overweight or obese were found to have an improved overall survival compared with other BMI categories, and those who were underweight had an increased 30-day mortality and postoperative complications.16
In another retrospective study of 3799 patients with CC, those who were overweight and obese had an improved 5-year survival rate compared with patients whose weight was normal or underweight. Outcomes were found to be stage dependent.17 In this study cohort, all patients were either overweight or obese and remained in that category even with weight loss. This may have contributed to overall improved outcomes.
Implications and Next Steps
Our study has several implications. One is that BMI criteria < 18.5 may not be a good measure for malnutrition given that about 75% of the patients in our cohort were overweight or obese and none were underweight. We also show a concrete, easily identifiable finding of percent weight change that could be addressed as an automated electronic notification and potentially identify a patient at risk and serve as a trigger for both timely and early nutrition intervention. It seems to be more sensitive than the ASPEN criterion of 10-lb weight loss in 6 months before surgery. Sensitivity is especially appealing given the ease and potential of embedding this tool in an electronic health record and the clinical importance of the consequent intervention. Preoperative as opposed to perioperative nutrition optimization at time of CC diagnosis is essential, as it may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Finally, although our study found that rates of inpatient postoperative nutrition consultation were high, rates of outpatient nutrition consultation in the preoperative period were low. This represents a missed opportunity for intervention before surgery. Similarly, rates of postoperative nutrition follow-up period were low, which points to an area for improvement in longitudinal and holistic care.
We suggest modifications to nutrition intervention protocols, such as ERAS, which should start at the time of GI malignancy diagnosis.18 Other suggestions include standard involvement of nutritionists in inpatient and outpatient settings with longitudinal follow-up in the preoperative and postoperative periods and patient enrollment in a nutrition program with monitoring at time of diagnosis at the VHA. Our findings as well as previous literature suggest that the preoperative period is the most important time to intervene with regard to nutrition optimization and represents an opportunity for intensive prehabilitation. Future areas of research include incorporating other important measures of malnourishment independent of BMI into future study designs, such as sarcopenia and adipose tissue density, to better assess body composition and predict prognostic risk in CC.18,19
Strengths and Limitations
This study is limited by its single-center, retrospective design and small sample sizes, and we acknowledge the limitations of our data set. However, the strength of this VHA-based study is that the single-payer system allows for complete capture of perioperative data as well as the opportunity for focused preoperative interventions to improve outcomes. To our knowledge, there is no currently existing literature on improving nutrition protocols at the VHA for patients with a GI malignancy. These retrospective data will help inform current gaps in quality improvement and supportive oncology as it relates to optimizing malnourishment in veterans undergoing surgical resection for their cancer.
Conclusions
In the CC cohort, weight loss of ≥ 3% from 6 months prior to time of surgery was significantly associated with delayed recovery, complications, and hospital readmissions. Our findings suggest that patients with CC undergoing surgery may benefit from an intensive, early nutrition prehabilitation. Preoperative nutrition optimization may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Further research would be able to clarify these hypotheses.
In patients with gastrointestinal (GI) malignancies, malnutrition is common. In addition, it has various negative implications, including high risk for surgical complications, prolonged hospitalization, decreased quality of life (QOL), increased mortality, and poor tolerance for treatments such as chemotherapy and radiotherapy.1
A 2014 French study of 1903 patients hospitalized for cancer reported a 39% overall prevalence of malnutrition; 39% in patients with cancers of the colon/rectum, 60% for pancreatic cancer, and 67% for cancers of the esophagus/stomach.2 Malnutrition was defined as body mass index (BMI) < 18.5 for individuals aged < 75 years or BMI < 21 for individuals aged ≥ 75 years, and/or weight loss > 10% since disease onset. Malnutrition also was strongly associated with worsened performance status.
The etiology of malnutrition in GI cancers is often multifactorial. It includes systemic tumor effects, such as inflammatory mediators contributing to hypermetabolism and cachexia, local tumor-associated mechanical obstruction, GI toxicities caused by antineoplastic therapy or other medications, and psychological factors that contribute to anorexia.3 Patient-related risk factors such as older age, other chronic diseases, and history of other GI surgeries also play a role.1
Other studies have demonstrated that malnutrition in patients with GI malignancies undergoing surgical resection is associated with high rates of severe postoperative complications, increased length of stay (LOS) and time on a ventilator for patients treated in the intensive care unit, and poor QOL in the postoperative survival period.4-6 Several randomized controlled trials conducted in patients with GI cancers have shown that enteral and parenteral nutrition supplementations in the perioperative period improve various outcomes, such as reduction of postoperative complication rates, fewer readmissions, improved chemotherapy tolerance, and improved QOL.7-10 Thus, in the management of patients with GI malignancies, it is highly important to implement early nutritional screening and establish a diagnosis of malnutrition to intervene and reduce postoperative morbidity and mortality.1
However, tools and predictors of malnutrition are often imperfect. The Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (AND/ASPEN) weight-based criteria define malnutrition and nutritionally-at-risk as BMI < 18.5, involuntary loss of at least 10% of body weight within 6 months or 5% within 1 month, or loss of 10 lb within 6 months.11 While the ASPEN criteria are often used to define malnourishment, they may not fully capture the population at risk, and there does not exist a gold-standard tool for nutritional screening. A 2002 study that performed a critical appraisal of 44 nutritional screening tools found that no single tool was fully sufficient for application, development, evaluation, and consistent screening.12 As such, consistently screening for malnutrition to target interventions in the perioperative period for GI surgical oncology has been challenging.13 More recent tools such as the perioperative nutrition screen (PONS) have been validated as rapid, effective screening tools to predict postoperative outcomes.14 Additionally, implementation of perioperative nutritional protocols, such as enhanced recovery after surgery (ERAS) in colon cancer (CC) surgery, also has shown improved perioperative care and outcomes.15
Preoperative nutritional interventions have been implemented in practice and have focused mostly on the immediate perioperative period. This has been shown to improve surgical outcomes. The Veterans Health Administration (VHA) provides comprehensive care to patients in a single-payer system, allowing for capture of perioperative data and the opportunity for focused preoperative interventions to improve outcomes.
Methods
This was a retrospective record review of colorectal malignancies treated with curative intent at the Veterans Affairs Ann Arbor Healthcare System (VAAAHS) in Michigan between January 1, 2015, and December 31, 2019. We examined nutritional status, degree of longitudinal weight loss, and subsequent clinical outcomes, including delayed postoperative recovery and delays in chemotherapy in 115 patients with CC and 33 patients with rectal cancer (RC) undergoing curative surgical resection at VAAAHS. To avoid additional confounding effects of advanced cancer, only early-stage, curable disease was included. This study was approved by the VAAAHS Institutional Review Board.
Patients with postoperative follow-up outside of VAAAHS were excluded. Patients were excluded if their surgery had noncurative intent or if they had distant metastatic disease. Data on patient weights, laboratory results, nutrition consultations, postoperative complications, delayed recovery, readmissions, and chemotherapy tolerance were abstracted by patient chart review in the VHA Computerized Patient Record System and Joint Legacy Viewer by 2 researchers.
Delayed recovery was defined as any abnormal clinical development described in inpatient progress notes, outpatient follow-up notes within 60 days, or in hospital discharge summaries. Excluded were psychiatric events without additional medical complications, postoperative bleeding not requiring an invasive intervention, urinary retention, postoperative glycemic control difficulties, cardiac events that happened before postoperative hospital discharge and not requiring readmission, and postoperative alcohol withdrawal. Complications were defined similarly to delayed recovery but excluded isolated prolonged postoperative ileus. LOS was defined in days as time from admission to discharge.
Adjuvant management course was derived from reviewing documentation from medical oncology consultations and progress notes. In patients for whom adjuvant chemotherapy was indicated and prescribed, chemotherapy was considered complete if chemotherapy was started and completed as indicated. Adjuvant chemotherapy was considered incomplete if the patient declined chemotherapy, if chemotherapy was not started when indicated, or if chemotherapy was not completed as indicated. Neoadjuvant therapy data were abstracted from medical and radiation oncology notes.
Recorded data were collected on both weight and BMI. Weights were extracted as follows: Weight 1 year before time of diagnosis, ± 4 months; weight 6 months before diagnosis ± 3 months; weight at time of diagnosis ± 2 weeks; weight at time of surgery ± 2 weeks; weight 30 days postsurgery ± 2 weeks; weight 60 days postsurgery ± 2 weeks; weight 1 year postsurgery ± 4 months. Mean percent change in weight was calculated from recorded weights between each allocated time point. A weight loss of ≥ 3% was found to be clinically relevant and was chosen as the minimal cutoff value when analyzing outcomes associated with weight trends.
Nutrition consultations were abstracted as follows: Preoperative nutrition consultations were defined as occurring between time of cancer diagnosis and surgery in either the inpatient or outpatient setting; inpatient postoperative nutrition consultations occurred during admission for surgery; readmission nutrition consultations occurred on readmission in inpatient setting, if applicable; outpatient postoperative nutrition consultations were defined as occurring up to 2 months postdischarge in the outpatient setting.
Albumin values were extracted as follows: Preoperative albumin levels were defined as up to 4 months prior to diagnosis, and postoperative albumin levels were defined as 2 to 6 months after surgery.
Analysis
The data were described using mean (SD) for continuous variables and number and percentages for categorical variables. Where appropriate, Fisher exact test, Pearson χ2 test, Spearman ρ, and Mann-Whitney U test were used for tests of significance. SAS (SAS Institute) was utilized for multivariable analysis. The significance level was P = .05 for all tests.
Results
There were 115 patients in the CC cohort and 33 in the RC cohort. The mean (SD) age at diagnosis was 70 (9.1) for CC group and 59 (1.4) for RC group (Table 1).
Weight Trends
From 1 year to 6 months before diagnosis, 40 of 80 patients lost weight in the CC cohort (mean change, +1.9%) and 6 of 22 patients lost weight in the RC cohort (mean change, + 0.5%). From 6 months before diagnosis to time of diagnosis, 47 of 74 patients lost weight in the CC cohort (mean change, -1.5%) and 14 of 21 patients lost weight in the RC cohort (mean change, -2.5%). From time of diagnosis to time of surgery, 36 of 104 patients with CC and 14 of 32 patients with RC lost weight with a mean weight change of and +0.1% and -0.3%, respectively. In the 6 months before surgery, any amount of weight loss was observed in 58 patients (66%) in the CC group and in 12 patients (57%) in the RC group. In this time frame, in the CC cohort, 32 patients (36%) were observed to have at least 3% weight loss, and 23 (26%) were observed to have at least 5% weight loss (Table 3).
In patients who completed adjuvant chemotherapy in the CC group, mean (SD) BMI at the beginning and end of chemotherapy was 32.6 (8.6) and 33.1 (8.7), respectively, and a -0.3% mean change in weight was observed. In the RC group, mean (SD) BMI was 28.2 (5.0) at the initiation of adjuvant chemotherapy and 28.4 (5.0) at its completion, with a +2.6% mean change in weight.
In the immediate postoperative period, most patients were losing weight in both the CC and RC groups (mean, -3.5% and -7.0% at 1 month postoperative, respectively). At 1-year after surgery, patients had modest mean increases in weight: +1.3% for patients with CC and +4.9% for patients with RC.
A relatively large proportion of patients had missing data on weights at various data points (Table 4).
Nutrition Consultations
In the CC group, preoperative nutrition consultations (either inpatient or outpatient) occurred in 17 patients (15%). Inpatient postoperative nutrition evaluations occurred in 110 patients (96%) (Table 5).
In the RC group, preoperative inpatient or outpatient nutrition consultations occurred in 12 patients (36%). Eight of those occurred before initiation of neoadjuvant chemoradiotherapy. All 33 patients received an inpatient postoperative nutrition evaluation during admission. Oral or enteral nutrition supplements were prescribed 19 times (58%). Postoperative outpatient nutrition consultations occurred for 24 patients (73%). Of the 19 patients who were readmitted to the hospital, 3 (16%) had a nutrition reconsultation on readmission.
Outcomes
The primary outcomes observed were delayed recovery, hospital readmission and LOS, and completion of adjuvant chemotherapy as indicated. Delayed recovery was observed in 35 patients with CC (40%) and 21 patients with RC (64%). Multivariable analysis in the CC cohort demonstrated that weight change was significantly associated with delayed recovery. Among those with ≥ 3% weight loss in the 6-month preoperative period (the weight measurement 6 months prior to diagnosis to date of surgery), 20 patients (63%) had delayed recovery compared with 15 patients (27%) without ≥ 3% weight loss who experienced delayed recovery (χ2 = 10.84; P < .001).
Weight loss of ≥ 3% in the 6-month preoperative period also was significantly associated with complications. Of patients with at least 3% preoperative weight loss, 16 (50%) experienced complications, while 8 (14%) with < 3% preoperative weight loss experienced complications (χ2 = 11.20; P < .001). Notably, ≥ 3% weight loss in the 1-year preoperative period before surgery was not significantly associated with delayed recovery. Any degree of 30-day postoperative weight loss was not correlated with delayed recovery. Finally, low preoperative albumin also was not correlated with delayed recovery (Fisher exact; P = .13). Table 3 displays differences based on presence of delayed recovery in the 88 patients with CC 6 months before surgery. Of note, ≥ 10-lb weight loss in the 6 months preceding surgery also correlated with delayed recovery (P = .01).In our cohort, 3% weight loss over 6 months had a sensitivity of 57%, specificity of 77%, positive predictive value 63%, and negative predictive value 73% for delayed recovery. By comparison, a 10-lb weight loss in 6 months per ASPEN criteria had a sensitivity of 40%, specificity of 85%, positive predictive value 64%, and negative predictive value 68% for delayed recovery.
Hospital Readmissions and LOS
Hospital readmissions occurred within the first 30 days in 11 patients (10%) in the CC cohort and 12 patients (36%) in the RC cohort. Readmissions occurred between 31 and 60 days in 4 (3%) and 7 (21%) of CC and RC cohorts, respectively. The presence of ≥ 3% weight loss in the 6-month
Mean (SD) LOS was 6.4 (4.7) days (range, 1-28) for patients with CC and 8.8 (5.1) days (range, 3-23) for patients with RC. Mean (SD) LOS increased to 10.2 (4.3) days and 9.7 (6.0) days in patients with delayed recovery in the CC and RC cohorts, respectively. The mean (SD) LOS was 5.2 (2.8) days and 6.3 (2.2) days in patients without delayed recovery in the CC and RC cohorts, respectively. There was no significant difference when examining association between percent weight change and LOS for either initial admission (rs= -0.1409; 2-tailed P = .19) or for initial and readmission combined (rs = -0.13532; 2-tailed P = .21) within the CC cohort.
Chemotherapy
Within the CC cohort, 31 patients (27%) had an indication for adjuvant chemotherapy. Of these, 25 of 31 (81%) started chemotherapy within 12 weeks of surgical resection, and of these, 17 of 25 patients (68%) completed chemotherapy as indicated. Within the RC cohort all 33 patients had an indication for adjuvant chemotherapy, of these 18 of 33 patients (55%) began within 12 weeks of surgical resection, and 10 of 18 (56%) completed chemotherapy as indicated.
Among the CC cohort who began but did not complete adjuvant chemotherapy, there was no significant association between completion of chemotherapy and
Discussion
This study highlights several important findings. There were no patients in our cohort that met ASPEN malnourishment criteria with a BMI < 18.5. Twenty percent of patients lost at least 10 lb in 6 months before the operation. Notably, patients had significant associations with adverse outcomes with less pronounced weight loss than previously noted. As has been established previously, malnourishment can be difficult to screen for, and BMI also is often an imprecise tool.12 In the CC cohort, weight loss
Our findings imply that the effects of even mild malnutrition are even more profound than previously thought. Significantly, this applies to overweight and obese patients as well, as these constituted a significant fraction of our cohort. A finding of ≥ 3% weight loss at the time of CC diagnosis may provide an opportunity for a focused nutrition intervention up to the time of surgery. Second, although nutrition consultation was frequent in the inpatient setting during the hospital admission (96%-100%), rates of nutrition evaluation were as low as 15% before surgery and 12% after surgery, representing a key area for improvement and focused intervention. An optimal time for intervention and nutrition prehabilitation would be at time of diagnosis before surgery with plans for continued aggressive monitoring and subsequent follow-up. Our finding seems to provide a more sensitive tool to identify patients at risk for delayed recovery compared with the ASPEN-driven assessment. Given the simplicity and the clinical significance, our test consisting of 3% weight loss over 6 months, with its sensitivity of 57%, may be superior to the ASPEN 10-lb weight loss, with its sensitivity of 40% in our cohort.
Previous Studies
Our findings are consistent with previous studies that have demonstrated that perioperative weight loss and malnutrition are correlated with delayed recovery and complications, such as wound healing, in patients with GI cancer.2,4,5,8 In a retrospective study of more than 7000 patients with CC, those who were overweight or obese were found to have an improved overall survival compared with other BMI categories, and those who were underweight had an increased 30-day mortality and postoperative complications.16
In another retrospective study of 3799 patients with CC, those who were overweight and obese had an improved 5-year survival rate compared with patients whose weight was normal or underweight. Outcomes were found to be stage dependent.17 In this study cohort, all patients were either overweight or obese and remained in that category even with weight loss. This may have contributed to overall improved outcomes.
Implications and Next Steps
Our study has several implications. One is that BMI criteria < 18.5 may not be a good measure for malnutrition given that about 75% of the patients in our cohort were overweight or obese and none were underweight. We also show a concrete, easily identifiable finding of percent weight change that could be addressed as an automated electronic notification and potentially identify a patient at risk and serve as a trigger for both timely and early nutrition intervention. It seems to be more sensitive than the ASPEN criterion of 10-lb weight loss in 6 months before surgery. Sensitivity is especially appealing given the ease and potential of embedding this tool in an electronic health record and the clinical importance of the consequent intervention. Preoperative as opposed to perioperative nutrition optimization at time of CC diagnosis is essential, as it may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Finally, although our study found that rates of inpatient postoperative nutrition consultation were high, rates of outpatient nutrition consultation in the preoperative period were low. This represents a missed opportunity for intervention before surgery. Similarly, rates of postoperative nutrition follow-up period were low, which points to an area for improvement in longitudinal and holistic care.
We suggest modifications to nutrition intervention protocols, such as ERAS, which should start at the time of GI malignancy diagnosis.18 Other suggestions include standard involvement of nutritionists in inpatient and outpatient settings with longitudinal follow-up in the preoperative and postoperative periods and patient enrollment in a nutrition program with monitoring at time of diagnosis at the VHA. Our findings as well as previous literature suggest that the preoperative period is the most important time to intervene with regard to nutrition optimization and represents an opportunity for intensive prehabilitation. Future areas of research include incorporating other important measures of malnourishment independent of BMI into future study designs, such as sarcopenia and adipose tissue density, to better assess body composition and predict prognostic risk in CC.18,19
Strengths and Limitations
This study is limited by its single-center, retrospective design and small sample sizes, and we acknowledge the limitations of our data set. However, the strength of this VHA-based study is that the single-payer system allows for complete capture of perioperative data as well as the opportunity for focused preoperative interventions to improve outcomes. To our knowledge, there is no currently existing literature on improving nutrition protocols at the VHA for patients with a GI malignancy. These retrospective data will help inform current gaps in quality improvement and supportive oncology as it relates to optimizing malnourishment in veterans undergoing surgical resection for their cancer.
Conclusions
In the CC cohort, weight loss of ≥ 3% from 6 months prior to time of surgery was significantly associated with delayed recovery, complications, and hospital readmissions. Our findings suggest that patients with CC undergoing surgery may benefit from an intensive, early nutrition prehabilitation. Preoperative nutrition optimization may help improve postsurgical outcomes as well as oncologic outcomes, including completion of adjuvant chemotherapy. Further research would be able to clarify these hypotheses.
1. Benoist S, Brouquet A. Nutritional assessment and screening for malnutrition. J Visc Surg. 2015;152:S3-S7. doi:10.1016/S1878-7886(15)30003-5
2. Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. J Parenter Enter Nutr. 2014;38(2):196-204. doi:10.1177/0148607113502674
3. Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9:S51-S63. doi:10.1016/j.ejon.2005.09.007
4. Nishiyama VKG, Albertini SM, de Moraes CMZG, et al. Malnutrition and clinical outcomes in surgical patients with colorectal disease. Arq Gastroenterol. 2018;55(4):397-402. doi:10.1590/s0004-2803.201800000-85
5. Shpata V, Prendushi X, Kreka M, Kola I, Kurti F, Ohri I. Malnutrition at the time of surgery affects negatively the clinical outcome of critically ill patients with gastrointestinal cancer. Med Arch Sarajevo Bosnia Herzeg. 2014;68(4):263-267. doi:10.5455/medarh.2014.68.263-267
6. Lim HS, Cho GS, Park YH, Kim SK. Comparison of quality of life and nutritional status in gastric cancer patients undergoing gastrectomies. Clin Nutr Res. 2015;4(3):153-159. doi:10.7762/cnr.2015.4.3.153
7. Bozzetti F, Gavazzi C, Miceli R, et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. J Parenter Enter Nutr. 2000;24(1):7-14. doi:10.1177/014860710002400107
8. Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr. 2007;26(6):698-709. doi:10.1016/j.clnu.2007.06.009
9. Bozzetti F, Braga M, Gianotti L, Gavazzi C, Mariani L. Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet. 2001; 358(9292):1487-1492. doi:10.1016/S0140-6736(01)06578-3
10. Meng Q, Tan S, Jiang Y, et al. Post-discharge oral nutritional supplements with dietary advice in patients at nutritional risk after surgery for gastric cancer: a randomized clinical trial. Clin Nutr Edinb Scotl. 2021;40(1):40-46. doi:10.1016/j.clnu.2020.04.043 start
11. White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738. doi:10.1016/j.jand.2012.03.012
12. Jones JM. The methodology of nutritional screening and assessment tools. J Hum Nutr Diet. 2002;15(1):59-71. doi:10.1046/j.1365-277X.2002.00327.x
13. Williams J, Wischmeyer P. Assessment of perioperative nutrition practices and attitudes—a national survey of colorectal and GI surgical oncology programs. Am J Surg. 2017;213(6):1010-1018. doi:10.1016/j.amjsurg.2016.10.008
14. Williams DG, Aronson S, Murray S, et al. Validation of the perioperative nutrition screen for prediction of postoperative outcomes. JPEN J Parenter Enteral Nutr. 2022;46(6):1307-1315. doi:10.1002/jpen.2310
15. Besson AJ, Kei C, Djordjevic A, Carter V, Deftereos I, Yeung J. Does implementation of and adherence to enhanced recovery after surgery improve perioperative nutritional management in colorectal cancer surgery? ANZ J Surg. 2022;92(6):1382-1387. doi:10.1111/ans.17599
16. Arkenbosch JHC, van Erning FN, Rutten HJ, Zimmerman D, de Wilt JHW, Beijer S. The association between body mass index and postoperative complications, 30-day mortality and long-term survival in Dutch patients with colorectal cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2019;45(2):160-166. doi:10.1016/j.ejso.2018.09.012
17. Shahjehan F, Merchea A, Cochuyt JJ, Li Z, Colibaseanu DT, Kasi PM. Body mass index and long-term outcomes in patients with colorectal cancer. Front Oncol. 2018;8:620. doi:10.3389/fonc.2018.00620
18. Nishigori T, Obama K, Sakai Y. Assessment of body composition and impact of sarcopenia and sarcopenic obesity in patients with gastric cancer. Transl Gastroenterol Hepatol. 2020;5:22. doi:10.21037/tgh.2019.10.13
19. Feliciano EMC, Winkels RM, Meyerhardt JA, Prado CM, Afman LA, Caan BJ. Abdominal adipose tissue radiodensity is associated with survival after colorectal cancer. Am J Clin Nutr. 2021;114(6):1917-1924. doi:10.1093/ajcn/nqab285
1. Benoist S, Brouquet A. Nutritional assessment and screening for malnutrition. J Visc Surg. 2015;152:S3-S7. doi:10.1016/S1878-7886(15)30003-5
2. Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. J Parenter Enter Nutr. 2014;38(2):196-204. doi:10.1177/0148607113502674
3. Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9:S51-S63. doi:10.1016/j.ejon.2005.09.007
4. Nishiyama VKG, Albertini SM, de Moraes CMZG, et al. Malnutrition and clinical outcomes in surgical patients with colorectal disease. Arq Gastroenterol. 2018;55(4):397-402. doi:10.1590/s0004-2803.201800000-85
5. Shpata V, Prendushi X, Kreka M, Kola I, Kurti F, Ohri I. Malnutrition at the time of surgery affects negatively the clinical outcome of critically ill patients with gastrointestinal cancer. Med Arch Sarajevo Bosnia Herzeg. 2014;68(4):263-267. doi:10.5455/medarh.2014.68.263-267
6. Lim HS, Cho GS, Park YH, Kim SK. Comparison of quality of life and nutritional status in gastric cancer patients undergoing gastrectomies. Clin Nutr Res. 2015;4(3):153-159. doi:10.7762/cnr.2015.4.3.153
7. Bozzetti F, Gavazzi C, Miceli R, et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. J Parenter Enter Nutr. 2000;24(1):7-14. doi:10.1177/014860710002400107
8. Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr. 2007;26(6):698-709. doi:10.1016/j.clnu.2007.06.009
9. Bozzetti F, Braga M, Gianotti L, Gavazzi C, Mariani L. Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet. 2001; 358(9292):1487-1492. doi:10.1016/S0140-6736(01)06578-3
10. Meng Q, Tan S, Jiang Y, et al. Post-discharge oral nutritional supplements with dietary advice in patients at nutritional risk after surgery for gastric cancer: a randomized clinical trial. Clin Nutr Edinb Scotl. 2021;40(1):40-46. doi:10.1016/j.clnu.2020.04.043 start
11. White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738. doi:10.1016/j.jand.2012.03.012
12. Jones JM. The methodology of nutritional screening and assessment tools. J Hum Nutr Diet. 2002;15(1):59-71. doi:10.1046/j.1365-277X.2002.00327.x
13. Williams J, Wischmeyer P. Assessment of perioperative nutrition practices and attitudes—a national survey of colorectal and GI surgical oncology programs. Am J Surg. 2017;213(6):1010-1018. doi:10.1016/j.amjsurg.2016.10.008
14. Williams DG, Aronson S, Murray S, et al. Validation of the perioperative nutrition screen for prediction of postoperative outcomes. JPEN J Parenter Enteral Nutr. 2022;46(6):1307-1315. doi:10.1002/jpen.2310
15. Besson AJ, Kei C, Djordjevic A, Carter V, Deftereos I, Yeung J. Does implementation of and adherence to enhanced recovery after surgery improve perioperative nutritional management in colorectal cancer surgery? ANZ J Surg. 2022;92(6):1382-1387. doi:10.1111/ans.17599
16. Arkenbosch JHC, van Erning FN, Rutten HJ, Zimmerman D, de Wilt JHW, Beijer S. The association between body mass index and postoperative complications, 30-day mortality and long-term survival in Dutch patients with colorectal cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2019;45(2):160-166. doi:10.1016/j.ejso.2018.09.012
17. Shahjehan F, Merchea A, Cochuyt JJ, Li Z, Colibaseanu DT, Kasi PM. Body mass index and long-term outcomes in patients with colorectal cancer. Front Oncol. 2018;8:620. doi:10.3389/fonc.2018.00620
18. Nishigori T, Obama K, Sakai Y. Assessment of body composition and impact of sarcopenia and sarcopenic obesity in patients with gastric cancer. Transl Gastroenterol Hepatol. 2020;5:22. doi:10.21037/tgh.2019.10.13
19. Feliciano EMC, Winkels RM, Meyerhardt JA, Prado CM, Afman LA, Caan BJ. Abdominal adipose tissue radiodensity is associated with survival after colorectal cancer. Am J Clin Nutr. 2021;114(6):1917-1924. doi:10.1093/ajcn/nqab285
Adult stem cells can heal intractable perianal Crohn’s fistulae
AURORA, COLO. – Perianal Crohn’s disease with fistula is notoriously difficult to treat and can make patients’ lives miserable, but a new, minimally invasive approach involving local injection of mesenchymal stem cells is both safe and, in a significant proportion of patients, highly effective, according to a colorectal surgeon.
“It’s a really debilitating phenotype, a spectrum of phenotypes,” Amy Lightner, MD, of the Cleveland Clinic said at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Although some patients have minimal symptoms, others may require multiple setons to aid in drainage and healing, while others may require fistulotomy, endorectal advancement flap, intersphincteric fistula tract (LIFT) procedure, diversion, or proctectomy.
“Why is it so difficult to treat? Well, part of it is that this is an anatomic defect, and this is why 90% of patients will come to the operating room and will see their surgeons on a frequent basis. The other part of that is that we have medical therapies to treat these fistulas but they’re really largely ineffective, because there is that anatomical defect, the hole there that needs to be closed,” Dr. Lightner said.
Up to 20% of patients may require a permanent stoma, and an additional 20% may require temporary fecal diversion.
Mesenchymal stem cells (MSC) are derived from bone marrow, fat stores, or umbilical cord tissues. Unlike embryonic stem cells, which have the ability to metamorphose into a multitude of other cell types, mesenchymal stem cells are differentiated “adult” cells.
They work by secreting anti-inflammatory cytokines and recruiting immune cells to stimulate tissue repair and healing. The cells are delivered in a minimally invasive outpatient setting, and there is no risk of incontinence compared with more invasive procedures such as fistulotomy or advancement flaps.
Effective and safe
MSCs were first used in Spain in 2003 to successfully treat a young women with a complex fistula with five perianal tracts converging into a rectovaginal fistula. The investigators injected a single dose of 9 x 106 MSCs into the site, and the fistula healed within 3 months.
Since then in multiple clinical trials involving more than 400 patients, injection of MSCs has resulted in fistula closure and complete healing by 8-12 weeks in 50%-85% of patients, Dr. Lightner said.
The treatment effect is also durable, she said, pointing to data from the ADMIRE-CD study, in which 51.5% of Crohn’s disease patients with treatment-refractory complex perianal fistula were healed at 24 weeks following injection of adipose-derived stem cells, compared with 35.6% of controls. At 1 year of follow-up, respective rates of healing were 56.3% vs. 38.6%.
Dr. Lightner also cited a case report of a patient whose fistula remained healed 4 years after receiving MSCs for refractory perianal Crohn’s fistulas.
Although MSCs are derived from healthy donors, they do not bear cellular surface antigens that would instigate a destructive host immune response, and to date, there have been no reports from clinical trials of systemic infections or complications. The most frequently reported adverse events have been injection-site pain in about 12%-15% of patients, and perianal abscess in 5%-13%, with similar frequencies in treatment and control groups.
Dr. Lightner and colleagues are currently exploring additional indications for stem cell therapy with MSCs, including other complex fistula phenotypes, intestinal Crohn’s disease, and ulcerative colitis.
Other approaches
In a separate presentation, James D. Lewis, MD, MSCE, of the University of Pennsylvania in Philadelphia talked about what would be needed to achieve a “medical moonshot” with the goal of curing inflammatory bowel disease (IBD), and touched on hematopoietic stem cell transplants as a potential option for patients with chronic, severe, and intractable disease.
One of his patients was a woman in her 60s who was diagnosed with stricturing and penetrating Crohn’s disease in her 30s, with the disease involving the ileum and entire colon. She had previously undergone three small bowel resections and a partial colon resection, and had never experienced remission despite taking steroids, azathioprine, methotrexate, four anti-TNF drugs, ustekinumab (Stelara), and vedolizumab (Entyvio).
Following an autologous hematopoietic stem cell transplant, she had a Simple Endoscopic Score for Crohn’s Disease (SES-CD) of 0. Her course was complicated by demand ischemia and acute kidney injury.
An IBD specialist who was not involved in either study commented in an interview that both MSCs and stem cell transplants show promise for treatment-refractory IBD,
“Both approaches are very promising, but stem cell transplants for IBD haven’t been formally studied yet so the data aren’t as strong, but there is promise for the future,” said Berkeley N. Limketkai, MD, PhD, from the University of California, Los Angeles.
“The challenges, however, are also the morbidity associated with actually undergoing such procedures,” he continued. Short- and long-term morbidities associated with hematopoietic stem cell transplants may include mucositis; hemorrhagic cystitis; prolonged, severe pancytopenia; infection; graft-versus-host disease; graft failure; pulmonary complications, veno-occlusive disease of the liver; and thrombotic microangiopathy.
Dr. Limketkai said that over time as the protocols for stem cell transplants in IBD improve, the benefits for select patients may more clearly outweigh the risks.
Dr. Lightner’s work is supported by the Leona M. and Harry B. Helmsley Charitable Trust and the American Society of Colon and Rectal Surgery. She disclosed consulting fees from Boomerang Medical, Mesoblast Limited, Ossium Health, and Takeda Pharmaceuticals USA. Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has also served as a consultant to and data safety monitoring board member for several entities. Dr. Limketkai disclosed consulting for Azora Therapeutics.
AURORA, COLO. – Perianal Crohn’s disease with fistula is notoriously difficult to treat and can make patients’ lives miserable, but a new, minimally invasive approach involving local injection of mesenchymal stem cells is both safe and, in a significant proportion of patients, highly effective, according to a colorectal surgeon.
“It’s a really debilitating phenotype, a spectrum of phenotypes,” Amy Lightner, MD, of the Cleveland Clinic said at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Although some patients have minimal symptoms, others may require multiple setons to aid in drainage and healing, while others may require fistulotomy, endorectal advancement flap, intersphincteric fistula tract (LIFT) procedure, diversion, or proctectomy.
“Why is it so difficult to treat? Well, part of it is that this is an anatomic defect, and this is why 90% of patients will come to the operating room and will see their surgeons on a frequent basis. The other part of that is that we have medical therapies to treat these fistulas but they’re really largely ineffective, because there is that anatomical defect, the hole there that needs to be closed,” Dr. Lightner said.
Up to 20% of patients may require a permanent stoma, and an additional 20% may require temporary fecal diversion.
Mesenchymal stem cells (MSC) are derived from bone marrow, fat stores, or umbilical cord tissues. Unlike embryonic stem cells, which have the ability to metamorphose into a multitude of other cell types, mesenchymal stem cells are differentiated “adult” cells.
They work by secreting anti-inflammatory cytokines and recruiting immune cells to stimulate tissue repair and healing. The cells are delivered in a minimally invasive outpatient setting, and there is no risk of incontinence compared with more invasive procedures such as fistulotomy or advancement flaps.
Effective and safe
MSCs were first used in Spain in 2003 to successfully treat a young women with a complex fistula with five perianal tracts converging into a rectovaginal fistula. The investigators injected a single dose of 9 x 106 MSCs into the site, and the fistula healed within 3 months.
Since then in multiple clinical trials involving more than 400 patients, injection of MSCs has resulted in fistula closure and complete healing by 8-12 weeks in 50%-85% of patients, Dr. Lightner said.
The treatment effect is also durable, she said, pointing to data from the ADMIRE-CD study, in which 51.5% of Crohn’s disease patients with treatment-refractory complex perianal fistula were healed at 24 weeks following injection of adipose-derived stem cells, compared with 35.6% of controls. At 1 year of follow-up, respective rates of healing were 56.3% vs. 38.6%.
Dr. Lightner also cited a case report of a patient whose fistula remained healed 4 years after receiving MSCs for refractory perianal Crohn’s fistulas.
Although MSCs are derived from healthy donors, they do not bear cellular surface antigens that would instigate a destructive host immune response, and to date, there have been no reports from clinical trials of systemic infections or complications. The most frequently reported adverse events have been injection-site pain in about 12%-15% of patients, and perianal abscess in 5%-13%, with similar frequencies in treatment and control groups.
Dr. Lightner and colleagues are currently exploring additional indications for stem cell therapy with MSCs, including other complex fistula phenotypes, intestinal Crohn’s disease, and ulcerative colitis.
Other approaches
In a separate presentation, James D. Lewis, MD, MSCE, of the University of Pennsylvania in Philadelphia talked about what would be needed to achieve a “medical moonshot” with the goal of curing inflammatory bowel disease (IBD), and touched on hematopoietic stem cell transplants as a potential option for patients with chronic, severe, and intractable disease.
One of his patients was a woman in her 60s who was diagnosed with stricturing and penetrating Crohn’s disease in her 30s, with the disease involving the ileum and entire colon. She had previously undergone three small bowel resections and a partial colon resection, and had never experienced remission despite taking steroids, azathioprine, methotrexate, four anti-TNF drugs, ustekinumab (Stelara), and vedolizumab (Entyvio).
Following an autologous hematopoietic stem cell transplant, she had a Simple Endoscopic Score for Crohn’s Disease (SES-CD) of 0. Her course was complicated by demand ischemia and acute kidney injury.
An IBD specialist who was not involved in either study commented in an interview that both MSCs and stem cell transplants show promise for treatment-refractory IBD,
“Both approaches are very promising, but stem cell transplants for IBD haven’t been formally studied yet so the data aren’t as strong, but there is promise for the future,” said Berkeley N. Limketkai, MD, PhD, from the University of California, Los Angeles.
“The challenges, however, are also the morbidity associated with actually undergoing such procedures,” he continued. Short- and long-term morbidities associated with hematopoietic stem cell transplants may include mucositis; hemorrhagic cystitis; prolonged, severe pancytopenia; infection; graft-versus-host disease; graft failure; pulmonary complications, veno-occlusive disease of the liver; and thrombotic microangiopathy.
Dr. Limketkai said that over time as the protocols for stem cell transplants in IBD improve, the benefits for select patients may more clearly outweigh the risks.
Dr. Lightner’s work is supported by the Leona M. and Harry B. Helmsley Charitable Trust and the American Society of Colon and Rectal Surgery. She disclosed consulting fees from Boomerang Medical, Mesoblast Limited, Ossium Health, and Takeda Pharmaceuticals USA. Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has also served as a consultant to and data safety monitoring board member for several entities. Dr. Limketkai disclosed consulting for Azora Therapeutics.
AURORA, COLO. – Perianal Crohn’s disease with fistula is notoriously difficult to treat and can make patients’ lives miserable, but a new, minimally invasive approach involving local injection of mesenchymal stem cells is both safe and, in a significant proportion of patients, highly effective, according to a colorectal surgeon.
“It’s a really debilitating phenotype, a spectrum of phenotypes,” Amy Lightner, MD, of the Cleveland Clinic said at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Although some patients have minimal symptoms, others may require multiple setons to aid in drainage and healing, while others may require fistulotomy, endorectal advancement flap, intersphincteric fistula tract (LIFT) procedure, diversion, or proctectomy.
“Why is it so difficult to treat? Well, part of it is that this is an anatomic defect, and this is why 90% of patients will come to the operating room and will see their surgeons on a frequent basis. The other part of that is that we have medical therapies to treat these fistulas but they’re really largely ineffective, because there is that anatomical defect, the hole there that needs to be closed,” Dr. Lightner said.
Up to 20% of patients may require a permanent stoma, and an additional 20% may require temporary fecal diversion.
Mesenchymal stem cells (MSC) are derived from bone marrow, fat stores, or umbilical cord tissues. Unlike embryonic stem cells, which have the ability to metamorphose into a multitude of other cell types, mesenchymal stem cells are differentiated “adult” cells.
They work by secreting anti-inflammatory cytokines and recruiting immune cells to stimulate tissue repair and healing. The cells are delivered in a minimally invasive outpatient setting, and there is no risk of incontinence compared with more invasive procedures such as fistulotomy or advancement flaps.
Effective and safe
MSCs were first used in Spain in 2003 to successfully treat a young women with a complex fistula with five perianal tracts converging into a rectovaginal fistula. The investigators injected a single dose of 9 x 106 MSCs into the site, and the fistula healed within 3 months.
Since then in multiple clinical trials involving more than 400 patients, injection of MSCs has resulted in fistula closure and complete healing by 8-12 weeks in 50%-85% of patients, Dr. Lightner said.
The treatment effect is also durable, she said, pointing to data from the ADMIRE-CD study, in which 51.5% of Crohn’s disease patients with treatment-refractory complex perianal fistula were healed at 24 weeks following injection of adipose-derived stem cells, compared with 35.6% of controls. At 1 year of follow-up, respective rates of healing were 56.3% vs. 38.6%.
Dr. Lightner also cited a case report of a patient whose fistula remained healed 4 years after receiving MSCs for refractory perianal Crohn’s fistulas.
Although MSCs are derived from healthy donors, they do not bear cellular surface antigens that would instigate a destructive host immune response, and to date, there have been no reports from clinical trials of systemic infections or complications. The most frequently reported adverse events have been injection-site pain in about 12%-15% of patients, and perianal abscess in 5%-13%, with similar frequencies in treatment and control groups.
Dr. Lightner and colleagues are currently exploring additional indications for stem cell therapy with MSCs, including other complex fistula phenotypes, intestinal Crohn’s disease, and ulcerative colitis.
Other approaches
In a separate presentation, James D. Lewis, MD, MSCE, of the University of Pennsylvania in Philadelphia talked about what would be needed to achieve a “medical moonshot” with the goal of curing inflammatory bowel disease (IBD), and touched on hematopoietic stem cell transplants as a potential option for patients with chronic, severe, and intractable disease.
One of his patients was a woman in her 60s who was diagnosed with stricturing and penetrating Crohn’s disease in her 30s, with the disease involving the ileum and entire colon. She had previously undergone three small bowel resections and a partial colon resection, and had never experienced remission despite taking steroids, azathioprine, methotrexate, four anti-TNF drugs, ustekinumab (Stelara), and vedolizumab (Entyvio).
Following an autologous hematopoietic stem cell transplant, she had a Simple Endoscopic Score for Crohn’s Disease (SES-CD) of 0. Her course was complicated by demand ischemia and acute kidney injury.
An IBD specialist who was not involved in either study commented in an interview that both MSCs and stem cell transplants show promise for treatment-refractory IBD,
“Both approaches are very promising, but stem cell transplants for IBD haven’t been formally studied yet so the data aren’t as strong, but there is promise for the future,” said Berkeley N. Limketkai, MD, PhD, from the University of California, Los Angeles.
“The challenges, however, are also the morbidity associated with actually undergoing such procedures,” he continued. Short- and long-term morbidities associated with hematopoietic stem cell transplants may include mucositis; hemorrhagic cystitis; prolonged, severe pancytopenia; infection; graft-versus-host disease; graft failure; pulmonary complications, veno-occlusive disease of the liver; and thrombotic microangiopathy.
Dr. Limketkai said that over time as the protocols for stem cell transplants in IBD improve, the benefits for select patients may more clearly outweigh the risks.
Dr. Lightner’s work is supported by the Leona M. and Harry B. Helmsley Charitable Trust and the American Society of Colon and Rectal Surgery. She disclosed consulting fees from Boomerang Medical, Mesoblast Limited, Ossium Health, and Takeda Pharmaceuticals USA. Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has also served as a consultant to and data safety monitoring board member for several entities. Dr. Limketkai disclosed consulting for Azora Therapeutics.
AT CROHN’S & COLITIS CONGRESS
Does appendectomy raise the risk for colorectal cancer?
In one part of a three-part analysis, researchers observed a 73% increase in CRC risk among appendectomy cases compared, with controls over a 20-year follow-up.
The study, published in Oncogene, suggests that appendectomy may promote colorectal tumorigenesis by influencing the gut microbiome and that surgeons should “more cautiously consider the necessity of appendectomy,” the authors concluded.
Charles Dinerstein, MD, who was not involved in the research, said that the findings are “intriguing,” but it’s “too soon to tell” what the potential clinical implications may be. For now, “I would not think those patients having undergone an appendectomy should have more intense screening,” said Dr. Dinerstein, medical director of the American Council on Science and Health.
A growing body of evidence suggests that microbes in the gut may play a role in CRC risk, and other research indicates that the appendix might play a role in maintaining the diversity of the gut microbiome. However, whether removing the appendix influences a person’s risk for CRC remains controversial.
In the current study, Feiyu Shi, MD, of The First Affiliated Hospital of Xi’an Jiaotong University, and colleagues sought to better understand a possible association between appendectomy and CRC risk.
The team performed a three-part study: (1) analyzed a population of 129,155 adults who had an appendectomy and those who did not to assess a possible clinical connection between appendectomy and CRC risk; (2) performed fecal metagenomics sequencing to evaluate characteristics of the gut microbiome in appendectomy cases versus matched normal controls without appendectomy; and (3) investigated a CRC mouse model with appendectomy to uncover a mechanism of appendectomy-induced colorectal tumorigenesis.
In the large epidemiological study, Dr. Shi and colleagues compared CRC risk in almost 44,000 appendectomy cases versus more than 85,000 age- and gender-matched nonappendectomy controls. The researchers found that, over the 20-year follow-up, the risk for CRC increased by 73% in appendectomy cases (adjusted hazard ratio, 1.73; P < .001). CRC risk and gut dysbiosis were more pronounced in adults older than 50 years with a history of appendectomy.
In the gut microbiome analysis, Dr. Shi’s team performed metagenomic sequencing on fecal samples from 314 participants – 157 appendectomy cases and 157 controls – and found significant alterations in the gut microbiome in appendectomy cases. The changes were characterized by enrichment of seven CRC-promoting bacteria, including Bacteroides vulgatus and Bacteroides fragilis, and depletion of five beneficial bacteria, including Collinsella aerofaciens and Enterococcus hirae.
Finally, to examine the influence of appendectomy on microbial dysbiosis and CRC tumorigenesis, Dr. Shi’s team performed an appendectomy or a sham procedure in a carcinogen-induced CRC mouse model and found that appendectomy appeared to promote CRC tumorigenesis by prompting gut dysbiosis.
Aasma Shaukat, MD, MPH, a gastroenterologist at NYU Langone Health, who was not involved in the research, urged caution in interpreting the findings, which “need confirmation in larger diverse cohorts.”
First, Dr. Shaukat explained, “the two groups are not comparable, even though [they were] matched for age and gender, and many known and unknown factors can explain the results.” For instance, information on which subjects underwent colon cancer screening is not known, which may explain differences.
Dr. Shaukat also cautioned that the researchers only profiled the microbiome in “a small group of individuals and a cross-sectional analysis is not sufficient to explain causation.”
The study had no commercial funding. Dr. Shi, Dr. Dinerstein, and Dr. Shaukat have no relevant conflicts of interest to report.
A version of this article first appeared on Medscape.com.
In one part of a three-part analysis, researchers observed a 73% increase in CRC risk among appendectomy cases compared, with controls over a 20-year follow-up.
The study, published in Oncogene, suggests that appendectomy may promote colorectal tumorigenesis by influencing the gut microbiome and that surgeons should “more cautiously consider the necessity of appendectomy,” the authors concluded.
Charles Dinerstein, MD, who was not involved in the research, said that the findings are “intriguing,” but it’s “too soon to tell” what the potential clinical implications may be. For now, “I would not think those patients having undergone an appendectomy should have more intense screening,” said Dr. Dinerstein, medical director of the American Council on Science and Health.
A growing body of evidence suggests that microbes in the gut may play a role in CRC risk, and other research indicates that the appendix might play a role in maintaining the diversity of the gut microbiome. However, whether removing the appendix influences a person’s risk for CRC remains controversial.
In the current study, Feiyu Shi, MD, of The First Affiliated Hospital of Xi’an Jiaotong University, and colleagues sought to better understand a possible association between appendectomy and CRC risk.
The team performed a three-part study: (1) analyzed a population of 129,155 adults who had an appendectomy and those who did not to assess a possible clinical connection between appendectomy and CRC risk; (2) performed fecal metagenomics sequencing to evaluate characteristics of the gut microbiome in appendectomy cases versus matched normal controls without appendectomy; and (3) investigated a CRC mouse model with appendectomy to uncover a mechanism of appendectomy-induced colorectal tumorigenesis.
In the large epidemiological study, Dr. Shi and colleagues compared CRC risk in almost 44,000 appendectomy cases versus more than 85,000 age- and gender-matched nonappendectomy controls. The researchers found that, over the 20-year follow-up, the risk for CRC increased by 73% in appendectomy cases (adjusted hazard ratio, 1.73; P < .001). CRC risk and gut dysbiosis were more pronounced in adults older than 50 years with a history of appendectomy.
In the gut microbiome analysis, Dr. Shi’s team performed metagenomic sequencing on fecal samples from 314 participants – 157 appendectomy cases and 157 controls – and found significant alterations in the gut microbiome in appendectomy cases. The changes were characterized by enrichment of seven CRC-promoting bacteria, including Bacteroides vulgatus and Bacteroides fragilis, and depletion of five beneficial bacteria, including Collinsella aerofaciens and Enterococcus hirae.
Finally, to examine the influence of appendectomy on microbial dysbiosis and CRC tumorigenesis, Dr. Shi’s team performed an appendectomy or a sham procedure in a carcinogen-induced CRC mouse model and found that appendectomy appeared to promote CRC tumorigenesis by prompting gut dysbiosis.
Aasma Shaukat, MD, MPH, a gastroenterologist at NYU Langone Health, who was not involved in the research, urged caution in interpreting the findings, which “need confirmation in larger diverse cohorts.”
First, Dr. Shaukat explained, “the two groups are not comparable, even though [they were] matched for age and gender, and many known and unknown factors can explain the results.” For instance, information on which subjects underwent colon cancer screening is not known, which may explain differences.
Dr. Shaukat also cautioned that the researchers only profiled the microbiome in “a small group of individuals and a cross-sectional analysis is not sufficient to explain causation.”
The study had no commercial funding. Dr. Shi, Dr. Dinerstein, and Dr. Shaukat have no relevant conflicts of interest to report.
A version of this article first appeared on Medscape.com.
In one part of a three-part analysis, researchers observed a 73% increase in CRC risk among appendectomy cases compared, with controls over a 20-year follow-up.
The study, published in Oncogene, suggests that appendectomy may promote colorectal tumorigenesis by influencing the gut microbiome and that surgeons should “more cautiously consider the necessity of appendectomy,” the authors concluded.
Charles Dinerstein, MD, who was not involved in the research, said that the findings are “intriguing,” but it’s “too soon to tell” what the potential clinical implications may be. For now, “I would not think those patients having undergone an appendectomy should have more intense screening,” said Dr. Dinerstein, medical director of the American Council on Science and Health.
A growing body of evidence suggests that microbes in the gut may play a role in CRC risk, and other research indicates that the appendix might play a role in maintaining the diversity of the gut microbiome. However, whether removing the appendix influences a person’s risk for CRC remains controversial.
In the current study, Feiyu Shi, MD, of The First Affiliated Hospital of Xi’an Jiaotong University, and colleagues sought to better understand a possible association between appendectomy and CRC risk.
The team performed a three-part study: (1) analyzed a population of 129,155 adults who had an appendectomy and those who did not to assess a possible clinical connection between appendectomy and CRC risk; (2) performed fecal metagenomics sequencing to evaluate characteristics of the gut microbiome in appendectomy cases versus matched normal controls without appendectomy; and (3) investigated a CRC mouse model with appendectomy to uncover a mechanism of appendectomy-induced colorectal tumorigenesis.
In the large epidemiological study, Dr. Shi and colleagues compared CRC risk in almost 44,000 appendectomy cases versus more than 85,000 age- and gender-matched nonappendectomy controls. The researchers found that, over the 20-year follow-up, the risk for CRC increased by 73% in appendectomy cases (adjusted hazard ratio, 1.73; P < .001). CRC risk and gut dysbiosis were more pronounced in adults older than 50 years with a history of appendectomy.
In the gut microbiome analysis, Dr. Shi’s team performed metagenomic sequencing on fecal samples from 314 participants – 157 appendectomy cases and 157 controls – and found significant alterations in the gut microbiome in appendectomy cases. The changes were characterized by enrichment of seven CRC-promoting bacteria, including Bacteroides vulgatus and Bacteroides fragilis, and depletion of five beneficial bacteria, including Collinsella aerofaciens and Enterococcus hirae.
Finally, to examine the influence of appendectomy on microbial dysbiosis and CRC tumorigenesis, Dr. Shi’s team performed an appendectomy or a sham procedure in a carcinogen-induced CRC mouse model and found that appendectomy appeared to promote CRC tumorigenesis by prompting gut dysbiosis.
Aasma Shaukat, MD, MPH, a gastroenterologist at NYU Langone Health, who was not involved in the research, urged caution in interpreting the findings, which “need confirmation in larger diverse cohorts.”
First, Dr. Shaukat explained, “the two groups are not comparable, even though [they were] matched for age and gender, and many known and unknown factors can explain the results.” For instance, information on which subjects underwent colon cancer screening is not known, which may explain differences.
Dr. Shaukat also cautioned that the researchers only profiled the microbiome in “a small group of individuals and a cross-sectional analysis is not sufficient to explain causation.”
The study had no commercial funding. Dr. Shi, Dr. Dinerstein, and Dr. Shaukat have no relevant conflicts of interest to report.
A version of this article first appeared on Medscape.com.
FROM ONCOGENE