User login
Contralateral Constrictor Dose Predicts Swallowing Function After Radiation for Head and Neck Cancer
Radiation therapy can cause long-term dysphagia that seriously affects quality of life for survivors of head and neck (H&N) cancer.1-3 Numerous studies have linked pharyngeal constrictor dose to long-term dysphagia, but conclusions about the dose distribution that can be safely tolerated have been inconsistent. For example, a group from the Netherlands found that the mean dose to the superior pharyngeal constrictor muscle and the supraglottic larynx were each predictive of dysphagia.4 A subsequent Vanderbilt study refuted these findings, reporting that these structures were not predictive but that dose to the inferior pharyngeal constrictor muscle was.5 Other studies have connected late dysphagia with dose to the middle pharyngeal constrictor muscle, total larynx, oral cavity, contralateral submandibular gland, contralateral parotid gland, or a combination of these structures.6-14 NRG Oncology trials commonly evaluate dose to the “uninvolved pharynx,” which is the total pharyngeal constrictor muscle volume minus the planning target volume for the lowest dose target volume. NRG H&N trials 3, 4, 5, 6, 8, and 9 all use uninvolved pharynx mean dose ≤ 45 Gy as a constraint to judge radiation plan quality.
Differences in methodology or patient population may explain the inconsistency of prior studies on dosimetric predictors of dysphagia, but it is possible that these studies did not evaluate the optimal metric for dysphagia. This study evaluates a novel organ at risk, the contralateral pharyngeal constrictor muscle, to determine whether dose to this structure is predictive of late swallowing function. The study also compares a constraint based on this structure to the NRG uninvolved pharynx constraint mentioned earlier.
Methods
This study is a retrospective review of patients treated at the Richard L. Roudebush Veterans Affairs (VA) Medical Center in Indianapolis, Indiana. Patients were identified by searching the VA Cancer Registry for patients treated for H&N squamous cell carcinoma between September 1, 2016, and August 30, 2019. Eligible sites included cancers of the nasopharynx, oropharynx, hypopharynx, larynx and oral cavity, as well as H&N cancer of an unknown primary site. Only patients treated with primary radiation with concurrent systemic therapy were included. Patients were excluded if they had prior surgery or radiation to the H&N.
The pharyngeal constrictor muscles were contoured per the techniques described by Bhide and colleagues.11 The contralateral constrictor was defined as the half of the constrictor volume contralateral to the primary site. For midline tumors, the side of the neck with a lower volume of lymph node metastases was judged to be the contralateral side.
One-year dysphagia was defined as having a gastronomy tube (G-tube) in place or an abnormal modified barium swallow (MBS) ≥ 12 months after the completion of radiation. At the study institution, MBS is not routinely done after therapy but is ordered if a patient or clinician has concerns about swallowing function. MBS was considered abnormal if there was laryngeal penetration that reached the level of the glottis or was not ejected from the larynx.
Results
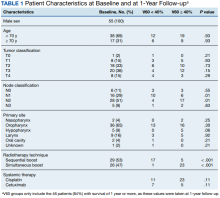
The VA Cancer Registry identified 113 patients treated for H&N cancer during the study period. Of these, 55 patients met the inclusion criteria. No patients were lost to follow-up. The median follow-up was 29 months. The median age was 67 years (range, 41-83) (Table 1).
All patients were treated with intensity-modulated radiotherapy (IMRT). Patients treated with a sequential boost had an initial dose of 54 Gy and/or 50 Gy, followed by a boost to a total of 70 Gy at 2 Gy per fraction. Patients treated with a simultaneous integrated boost (SIB) technique received 69.96 Gy in 33 fractions, with elective volumes treated to 54.45 Gy in 33 fractions. Both patients with nasopharyngeal cancer were treated with SIB plans and had an intermediate dose volume of 59.4 Gy.
Systemic therapy was weekly cisplatin in 41 patients (75%) and cetuximab in 14 (25%). Twenty percent of patients receiving cisplatin switched to an alternative agent during treatment, most commonly carboplatin.
Forty-nine patients (89%) had a G-tube placed before starting radiation. G-tubes were in place for an interval of 0 to 47 months (mean, 8.6); 12 (22%) had a G-tube > 12 months. After completion of radiation, 18 patients (33%) had an abnormal MBS. These were done 1 to 50 months (mean, 14.8) after completion of radiation. Abnormal MBS occurred ≥ 12 months after radiation in 9 patients, 5 of whom had their G-tube in place for less than a year.
Forty-six patients (84%) survived more than 1 year and could be evaluated for late swallowing function. One-year dysphagia was seen in 17 (37%) of these patients. Recurrence was seen in 20 patients (36%), with locoregional recurrence in 12 (60%) of these cases. Recurrence occurred at a range of 0 to 15 months (mean, 5.6). Neither recurrence (P = .69) nor locoregional recurrence (P = .11) was associated with increased 1-year dysphagia.
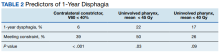
In patients who could be evaluated for long-term swallowing function, contralateral constrictor V60 ranged from 0% to 100% (median, 51%). V60 was < 40% in 18 patients (39%). With V60 < 40%, there was a 6% rate of 1-year dysphagia compared with 57% for V60 ≥ 40% (P < .001).
Patients with contralateral constrictor V60 < 40 and V60 ≥ 40 both had a mean age of 65 years. χ2 analysis did not show a difference in T stage or systemic treatment but did show that patients with V60 < 40% were more likely to have N1 disease (P = .01), and less likely to have N2 disease (P = .01) compared with patients with V60 ≥ 40%. The difference in 1-year dysphagia between N0 to N1 patients (27%) and N2 to N3 patients (46%) was not statistically significant (P = .19).
In patients who could be evaluated for long-term swallowing function, the uninvolved pharynx volume median of the total constrictor volume was 32% (range, < 1%-62%). The uninvolved pharynx mean dose ranged from 28 to 68 Gy (median, 45). When the uninvolved pharynx mean dose was < 45 Gy, 1-year dysphagia was 22% compared with 52% with a dose ≥ 45 Gy (P = .03).
Air cavity editing was performed in 27 patients (49%). One-year survival was 93% with air cavity editing, and 75% without, which was not statistically significant. Locoregional recurrence occurred in 3 patients (11%) with air cavity editing, and 9 (32%) without, which was not statistically significant. In patients surviving at least 1 year, contralateral constrictor V60 averaged 33% with editing and 62% without editing (P < .001). One-year dysphagia was 12% with air cavity editing and 67% without editing (P < .001).
An SIB technique was done in 26 patients (47%). One-year survival was 85% (n = 22) with SIB and 83% (n = 24) with sequential boost, which was not statistically significant. Locoregional recurrence occurred in 19% with SIB, and 32% with sequential boost, which was not statistically significant. For SIB patients alive at 1 year, the median contralateral V60 was 28%, compared with 66% for patients treated with sequential technique. Seventeen patients (77%) with SIB had V60 < 40%. Nineteen (86%) of SIB plans also had air cavity editing. One patient (5%) with SIB had dysphagia at 1 year, compared with 16 (67%) sequential patients (P < .001).
Discussion
This is the first study to link contralateral constrictor dose to long-term dysphagia in patients treated with radiation for H&N cancer. Editing the boost volume off air cavities was associated with lower contralateral constrictor V60 and with less long-term dysphagia. This may indicate that optimizing plans to meet a contralateral constrictor constraint can reduce rates of long-term dysphagia.
The most useful clinical predictors are those that identify a patient at low risk for toxicity. These constraints are useful because they reassure physicians that treatments will have a favorable risk/benefit ratio while identifying plans that may need modification before starting treatment.
The contralateral constrictor outperformed the uninvolved pharynx in identifying patients at low risk for long-term dysphagia. This difference could not be overcome by decreasing the threshold of the pharynx constraint, as 17% of patients with dysphagia had a mean dose of < 40 Gy to the uninvolved pharynx, which was not statistically significant.
An advantage of contralateral constrictor is that it is independent of planning target volume (PTV) size. The uninvolved pharynx structure depends on the PTV contour, so it may obscure a connection between PTV size and dysphagia.
In the context of a clinical trial, only measuring dose to the uninvolved pharynx may allow more plans to meet constraints, but even in NRG trials, physicians have some control over target volumes. For example, NRG HN009, a national trial for patients with H&N cancer, recommends editing the CTV_7000 (clinical target volume treated to 70 Gy) off air cavities but does not define how much the volume should be cropped or specify protocol violations if the volume is not cropped.15 Furthermore, constraints used in clinical trials are often adopted for use outside the trial, where physicians have extensive control over target volumes.
The broad range of uninvolved pharynx volume relative to total constrictor volume confounds predictions using this variable. For example, according to the NRG constraint, a patient with an uninvolved pharynx mean dose of 44 Gy will have a low risk of dysphagia even if this structure is only 1% of the total constrictor. The contralateral constrictor is always about 50% of the total constrictor volume, which means that predictions using this structure will not be confounded by the same variation in volume size.
Figure 2 shows a representative patient who met the NRG uninvolved pharynx constraint but developed long-term dysphagia.
Pharyngoesophageal stricture is a common cause of dysphagia after IMRT for H&N cancer.16 Radiation has been shown to decrease pharyngeal function in patients with H&N cancer.17 Sparing one side of the pharynx may allow for better pharyngeal compliance throughout the length of the pharynx, possibly decreasing the rate of pharyngoesophageal stricture. Additionally, constraining the contralateral constrictor may preserve strength on this side, allowing it to compensate for weakness on the side of the primary cancer. An exercise sometimes used for dysphagia involves head rotation toward the affected side during swallowing. This technique has been shown to cause food to move to the unaffected side.18 Sparing the contralateral constrictor may help such techniques work better in patients with H&N cancer.
Few studies have commented specifically on dose to swallowing structures contralateral to the primary tumor. Two studies have proposed contralateral submandibular gland constraints for dysphagia (not xerostomia), but neither measured the dose to the contralateral constrictor muscle.9,10 Although the contralateral submandibular dose may correlate with dose to the constrictor on that side, the submandibular gland may have a less direct impact on swallowing than the constrictor muscle, and its limited dimensions may make constraints based on the gland less robust for cancers outside the oropharynx.
Another study reported improved quality of life in patients who were not treated with elective contralateral retropharyngeal radiation.19 Although it is likely that doses to the contralateral constrictor were lower in patients who did not receive elective radiation to this area, this study did not measure or constrain doses to the contralateral constrictors.
Limitations
This study is limited by its single institution, retrospective design, small sample size, and by all patients being male. The high correlation between air cavity editing and the use of SIB makes it impossible to assess the impact of each technique individually. Patients with contralateral constrictor V60 < 40% were less likely to have N2 disease, but N2 to N3 disease did not predict higher 1-year dysphagia, so the difference in N-category cannot fully explain the difference in 1-year dysphagia. It is possible that unreported factors, such as CTV, may contribute significantly to swallowing function. Nevertheless, within the study population, contralateral constrictor dose was able to identify a group with a low rate of long-term dysphagia.
Conclusions
Contralateral constrictor dose is a promising predictor of late dysphagia for patients with H&N cancer treated with radiation with concurrent systemic therapy. Contralateral constrictor V60 < 40% was able to identify a group of patients with a low rate of 1-year dysphagia in this single-center retrospective study. The correlation between air cavity editing and contralateral constrictor V60 suggests that contralateral constrictor dose may depend partly on technique. Further studies are needed to see if the contralateral constrictor dose can be used to predict long-term dysphagia prospectively and in other patient populations.
1. Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, et al. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 2008;26(22):3770-3776. doi:10.1200/JCO.2007.14.6647
2. Nguyen NP, Frank C, Moltz CC, et al. Impact of dysphagia on quality of life after treatment of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2005;61(3):772-778. doi:10.1016/j.ijrobp.2004.06.017
3. Ramaekers BLT, Joore MA, Grutters JPC, et al. The impact of late treatment-toxicity on generic health-related quality of life in head and neck cancer patients after radiotherapy. Oral Oncol. 2011;47(8):768-774. doi:10.1016/j.oraloncology.2011.05.012
4. Christianen MEMC, Schilstra C, Beetz I, et al. Predictive modelling for swallowing dysfunction after primary (chemo)radiation: results of a prospective observational study. Radiother Oncol. 2012;105(1):107-114. doi:10.1016/j.radonc.2011.08.009
5. Vlachich G, Spratt DE, Diaz R, et al. Dose to inferior pharyngeal conctrictor predicts prolonged gastrostomy tube dependence with concurrent intensity-modulated radiation therapy and chemotherapy for locally-advanced head and neck cancer. Radiother Oncol. 2014;110(3):435-440. doi:10.1016/j.radonc.2013.12.007
6. Mogadas S, Busch CJ, Pflug Cet al. Influence of radiation dose to pharyngeal constrictor muscles on late dysphagia and quality of life in patients with locally advanced oropharyngeal carcinoma. Strahlenther Onkol. 2020;196(6):522-529. doi:10.1007/s00066-019-01572-0
7. Caglar HB, Tishler RB, Othus M, et al. Dose to larynx predicts of swallowing complications after intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72(4):1110-1118. doi:10.1016/j.ijrobp.2008.02.048
8. Schwartz DL, Hutcheson K, Barringer D, et al. Candidate dosimetric predictors of long-term swallowing dysfunction after oropharyngeal intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78(5):1356-1365. doi:10.1016/j.ijrobp.2009.10.002
9. Gensheimer MF, Nyflot M, Laramore GE, Laio JL, Parvathaneni U. Contribution of submandibular gland and swallowing structure sparing to post-radiation therapy peg dependence in oropharynx cancer patients treated with split-neck IMRT technique. Radiat Oncol. 2015;11(1):1-7. doi:10.1186/s13014-016-0726-3
10. Hedström J, Tuomi L, Finizia C, Olsson C. Identifying organs at risk for radiation-induced late dysphagia in head and neck cancer patients. Clin Transl Radiat Oncol. 2019;19:87-95. doi:10.1016/j.ctro.2019.08.005
11. Bhide SA, Gulliford S, Kazi R, et al. Correlation between dose to the pharyngeal constrictors and patient quality of life and late dysphagia following chemo-IMRT for head and neck cancer. Radiother Oncol. 2009;93(3):539-544. doi:10.1016/j.radonc.2009.09.017
12. Caudell JJ, Schaner PE, Desmond RA, Meredith RF, Spencer SA, Bonner JA. Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2010;76(2):403-409. doi:10.1016/j.ijrobp.2009.02.017
13. Levendag PC, Teguh DN, Voet P, et al. Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiother Oncol. 2007;85(1):64-73. doi:10.1016/j.radonc.2007.07.009
14. Eisbruch A, Schwartz M, Rasch C, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004;60(5):1425-1439. doi:10.1016/j.ijrobp.2004.05.050
15. Harari PM; NRG Oncology. Comparing high-dose cisplatin every three weeks to low-dose cisplatin weekly when combined with radiation for patients with advanced head and neck cancer. ClinicalTrials.gov identifier: NCT05050162. Updated November 25, 2022. Accessed December 7, 2022. https://clinicaltrials.gov/ct2/show/NCT05050162
16. Wang JJ, Goldsmith TA, Holman AS, Cianchetti M, Chan AW. Pharyngoesophageal stricture after treatment for head and neck cancer. Head Neck. 2011;34(7):967-973. doi:10.1002/hed.21842
17. Kendall KA, McKenzie SW, Leonard RJ, Jones CU. Timing of swallowing events after single-modality treatment of head and neck carcinoma with radiotherapy. Ann Otol Rhinol Laryngol. 2000;109(8, pt 1):767-775. doi:10.1177/000348940010900812
18. Ohmae Y, Ogura M, Kitahara S. Effects of head rotation on pharyngeal function during normal swallow. Ann Otol Rhinol Laryngol. 1998;107(4):344-348. doi:10.1177/000348949810700414
19. Spencer CR, Gay HA, Haughey BH, et al. Eliminating radiotherapy to the contralateral retropharyngeal and high level II lymph nodes in head and neck squamous cell carcinoma is safe and improves quality of life. Cancer. 2014;120(24):3994-4002. doi:10.1002/cncr.28938
Radiation therapy can cause long-term dysphagia that seriously affects quality of life for survivors of head and neck (H&N) cancer.1-3 Numerous studies have linked pharyngeal constrictor dose to long-term dysphagia, but conclusions about the dose distribution that can be safely tolerated have been inconsistent. For example, a group from the Netherlands found that the mean dose to the superior pharyngeal constrictor muscle and the supraglottic larynx were each predictive of dysphagia.4 A subsequent Vanderbilt study refuted these findings, reporting that these structures were not predictive but that dose to the inferior pharyngeal constrictor muscle was.5 Other studies have connected late dysphagia with dose to the middle pharyngeal constrictor muscle, total larynx, oral cavity, contralateral submandibular gland, contralateral parotid gland, or a combination of these structures.6-14 NRG Oncology trials commonly evaluate dose to the “uninvolved pharynx,” which is the total pharyngeal constrictor muscle volume minus the planning target volume for the lowest dose target volume. NRG H&N trials 3, 4, 5, 6, 8, and 9 all use uninvolved pharynx mean dose ≤ 45 Gy as a constraint to judge radiation plan quality.
Differences in methodology or patient population may explain the inconsistency of prior studies on dosimetric predictors of dysphagia, but it is possible that these studies did not evaluate the optimal metric for dysphagia. This study evaluates a novel organ at risk, the contralateral pharyngeal constrictor muscle, to determine whether dose to this structure is predictive of late swallowing function. The study also compares a constraint based on this structure to the NRG uninvolved pharynx constraint mentioned earlier.
Methods
This study is a retrospective review of patients treated at the Richard L. Roudebush Veterans Affairs (VA) Medical Center in Indianapolis, Indiana. Patients were identified by searching the VA Cancer Registry for patients treated for H&N squamous cell carcinoma between September 1, 2016, and August 30, 2019. Eligible sites included cancers of the nasopharynx, oropharynx, hypopharynx, larynx and oral cavity, as well as H&N cancer of an unknown primary site. Only patients treated with primary radiation with concurrent systemic therapy were included. Patients were excluded if they had prior surgery or radiation to the H&N.
The pharyngeal constrictor muscles were contoured per the techniques described by Bhide and colleagues.11 The contralateral constrictor was defined as the half of the constrictor volume contralateral to the primary site. For midline tumors, the side of the neck with a lower volume of lymph node metastases was judged to be the contralateral side.
One-year dysphagia was defined as having a gastronomy tube (G-tube) in place or an abnormal modified barium swallow (MBS) ≥ 12 months after the completion of radiation. At the study institution, MBS is not routinely done after therapy but is ordered if a patient or clinician has concerns about swallowing function. MBS was considered abnormal if there was laryngeal penetration that reached the level of the glottis or was not ejected from the larynx.
Results
The VA Cancer Registry identified 113 patients treated for H&N cancer during the study period. Of these, 55 patients met the inclusion criteria. No patients were lost to follow-up. The median follow-up was 29 months. The median age was 67 years (range, 41-83) (Table 1).
All patients were treated with intensity-modulated radiotherapy (IMRT). Patients treated with a sequential boost had an initial dose of 54 Gy and/or 50 Gy, followed by a boost to a total of 70 Gy at 2 Gy per fraction. Patients treated with a simultaneous integrated boost (SIB) technique received 69.96 Gy in 33 fractions, with elective volumes treated to 54.45 Gy in 33 fractions. Both patients with nasopharyngeal cancer were treated with SIB plans and had an intermediate dose volume of 59.4 Gy.
Systemic therapy was weekly cisplatin in 41 patients (75%) and cetuximab in 14 (25%). Twenty percent of patients receiving cisplatin switched to an alternative agent during treatment, most commonly carboplatin.
Forty-nine patients (89%) had a G-tube placed before starting radiation. G-tubes were in place for an interval of 0 to 47 months (mean, 8.6); 12 (22%) had a G-tube > 12 months. After completion of radiation, 18 patients (33%) had an abnormal MBS. These were done 1 to 50 months (mean, 14.8) after completion of radiation. Abnormal MBS occurred ≥ 12 months after radiation in 9 patients, 5 of whom had their G-tube in place for less than a year.
Forty-six patients (84%) survived more than 1 year and could be evaluated for late swallowing function. One-year dysphagia was seen in 17 (37%) of these patients. Recurrence was seen in 20 patients (36%), with locoregional recurrence in 12 (60%) of these cases. Recurrence occurred at a range of 0 to 15 months (mean, 5.6). Neither recurrence (P = .69) nor locoregional recurrence (P = .11) was associated with increased 1-year dysphagia.
In patients who could be evaluated for long-term swallowing function, contralateral constrictor V60 ranged from 0% to 100% (median, 51%). V60 was < 40% in 18 patients (39%). With V60 < 40%, there was a 6% rate of 1-year dysphagia compared with 57% for V60 ≥ 40% (P < .001).
Patients with contralateral constrictor V60 < 40 and V60 ≥ 40 both had a mean age of 65 years. χ2 analysis did not show a difference in T stage or systemic treatment but did show that patients with V60 < 40% were more likely to have N1 disease (P = .01), and less likely to have N2 disease (P = .01) compared with patients with V60 ≥ 40%. The difference in 1-year dysphagia between N0 to N1 patients (27%) and N2 to N3 patients (46%) was not statistically significant (P = .19).
In patients who could be evaluated for long-term swallowing function, the uninvolved pharynx volume median of the total constrictor volume was 32% (range, < 1%-62%). The uninvolved pharynx mean dose ranged from 28 to 68 Gy (median, 45). When the uninvolved pharynx mean dose was < 45 Gy, 1-year dysphagia was 22% compared with 52% with a dose ≥ 45 Gy (P = .03).
Air cavity editing was performed in 27 patients (49%). One-year survival was 93% with air cavity editing, and 75% without, which was not statistically significant. Locoregional recurrence occurred in 3 patients (11%) with air cavity editing, and 9 (32%) without, which was not statistically significant. In patients surviving at least 1 year, contralateral constrictor V60 averaged 33% with editing and 62% without editing (P < .001). One-year dysphagia was 12% with air cavity editing and 67% without editing (P < .001).
An SIB technique was done in 26 patients (47%). One-year survival was 85% (n = 22) with SIB and 83% (n = 24) with sequential boost, which was not statistically significant. Locoregional recurrence occurred in 19% with SIB, and 32% with sequential boost, which was not statistically significant. For SIB patients alive at 1 year, the median contralateral V60 was 28%, compared with 66% for patients treated with sequential technique. Seventeen patients (77%) with SIB had V60 < 40%. Nineteen (86%) of SIB plans also had air cavity editing. One patient (5%) with SIB had dysphagia at 1 year, compared with 16 (67%) sequential patients (P < .001).
Discussion
This is the first study to link contralateral constrictor dose to long-term dysphagia in patients treated with radiation for H&N cancer. Editing the boost volume off air cavities was associated with lower contralateral constrictor V60 and with less long-term dysphagia. This may indicate that optimizing plans to meet a contralateral constrictor constraint can reduce rates of long-term dysphagia.
The most useful clinical predictors are those that identify a patient at low risk for toxicity. These constraints are useful because they reassure physicians that treatments will have a favorable risk/benefit ratio while identifying plans that may need modification before starting treatment.
The contralateral constrictor outperformed the uninvolved pharynx in identifying patients at low risk for long-term dysphagia. This difference could not be overcome by decreasing the threshold of the pharynx constraint, as 17% of patients with dysphagia had a mean dose of < 40 Gy to the uninvolved pharynx, which was not statistically significant.
An advantage of contralateral constrictor is that it is independent of planning target volume (PTV) size. The uninvolved pharynx structure depends on the PTV contour, so it may obscure a connection between PTV size and dysphagia.
In the context of a clinical trial, only measuring dose to the uninvolved pharynx may allow more plans to meet constraints, but even in NRG trials, physicians have some control over target volumes. For example, NRG HN009, a national trial for patients with H&N cancer, recommends editing the CTV_7000 (clinical target volume treated to 70 Gy) off air cavities but does not define how much the volume should be cropped or specify protocol violations if the volume is not cropped.15 Furthermore, constraints used in clinical trials are often adopted for use outside the trial, where physicians have extensive control over target volumes.
The broad range of uninvolved pharynx volume relative to total constrictor volume confounds predictions using this variable. For example, according to the NRG constraint, a patient with an uninvolved pharynx mean dose of 44 Gy will have a low risk of dysphagia even if this structure is only 1% of the total constrictor. The contralateral constrictor is always about 50% of the total constrictor volume, which means that predictions using this structure will not be confounded by the same variation in volume size.
Figure 2 shows a representative patient who met the NRG uninvolved pharynx constraint but developed long-term dysphagia.
Pharyngoesophageal stricture is a common cause of dysphagia after IMRT for H&N cancer.16 Radiation has been shown to decrease pharyngeal function in patients with H&N cancer.17 Sparing one side of the pharynx may allow for better pharyngeal compliance throughout the length of the pharynx, possibly decreasing the rate of pharyngoesophageal stricture. Additionally, constraining the contralateral constrictor may preserve strength on this side, allowing it to compensate for weakness on the side of the primary cancer. An exercise sometimes used for dysphagia involves head rotation toward the affected side during swallowing. This technique has been shown to cause food to move to the unaffected side.18 Sparing the contralateral constrictor may help such techniques work better in patients with H&N cancer.
Few studies have commented specifically on dose to swallowing structures contralateral to the primary tumor. Two studies have proposed contralateral submandibular gland constraints for dysphagia (not xerostomia), but neither measured the dose to the contralateral constrictor muscle.9,10 Although the contralateral submandibular dose may correlate with dose to the constrictor on that side, the submandibular gland may have a less direct impact on swallowing than the constrictor muscle, and its limited dimensions may make constraints based on the gland less robust for cancers outside the oropharynx.
Another study reported improved quality of life in patients who were not treated with elective contralateral retropharyngeal radiation.19 Although it is likely that doses to the contralateral constrictor were lower in patients who did not receive elective radiation to this area, this study did not measure or constrain doses to the contralateral constrictors.
Limitations
This study is limited by its single institution, retrospective design, small sample size, and by all patients being male. The high correlation between air cavity editing and the use of SIB makes it impossible to assess the impact of each technique individually. Patients with contralateral constrictor V60 < 40% were less likely to have N2 disease, but N2 to N3 disease did not predict higher 1-year dysphagia, so the difference in N-category cannot fully explain the difference in 1-year dysphagia. It is possible that unreported factors, such as CTV, may contribute significantly to swallowing function. Nevertheless, within the study population, contralateral constrictor dose was able to identify a group with a low rate of long-term dysphagia.
Conclusions
Contralateral constrictor dose is a promising predictor of late dysphagia for patients with H&N cancer treated with radiation with concurrent systemic therapy. Contralateral constrictor V60 < 40% was able to identify a group of patients with a low rate of 1-year dysphagia in this single-center retrospective study. The correlation between air cavity editing and contralateral constrictor V60 suggests that contralateral constrictor dose may depend partly on technique. Further studies are needed to see if the contralateral constrictor dose can be used to predict long-term dysphagia prospectively and in other patient populations.
Radiation therapy can cause long-term dysphagia that seriously affects quality of life for survivors of head and neck (H&N) cancer.1-3 Numerous studies have linked pharyngeal constrictor dose to long-term dysphagia, but conclusions about the dose distribution that can be safely tolerated have been inconsistent. For example, a group from the Netherlands found that the mean dose to the superior pharyngeal constrictor muscle and the supraglottic larynx were each predictive of dysphagia.4 A subsequent Vanderbilt study refuted these findings, reporting that these structures were not predictive but that dose to the inferior pharyngeal constrictor muscle was.5 Other studies have connected late dysphagia with dose to the middle pharyngeal constrictor muscle, total larynx, oral cavity, contralateral submandibular gland, contralateral parotid gland, or a combination of these structures.6-14 NRG Oncology trials commonly evaluate dose to the “uninvolved pharynx,” which is the total pharyngeal constrictor muscle volume minus the planning target volume for the lowest dose target volume. NRG H&N trials 3, 4, 5, 6, 8, and 9 all use uninvolved pharynx mean dose ≤ 45 Gy as a constraint to judge radiation plan quality.
Differences in methodology or patient population may explain the inconsistency of prior studies on dosimetric predictors of dysphagia, but it is possible that these studies did not evaluate the optimal metric for dysphagia. This study evaluates a novel organ at risk, the contralateral pharyngeal constrictor muscle, to determine whether dose to this structure is predictive of late swallowing function. The study also compares a constraint based on this structure to the NRG uninvolved pharynx constraint mentioned earlier.
Methods
This study is a retrospective review of patients treated at the Richard L. Roudebush Veterans Affairs (VA) Medical Center in Indianapolis, Indiana. Patients were identified by searching the VA Cancer Registry for patients treated for H&N squamous cell carcinoma between September 1, 2016, and August 30, 2019. Eligible sites included cancers of the nasopharynx, oropharynx, hypopharynx, larynx and oral cavity, as well as H&N cancer of an unknown primary site. Only patients treated with primary radiation with concurrent systemic therapy were included. Patients were excluded if they had prior surgery or radiation to the H&N.
The pharyngeal constrictor muscles were contoured per the techniques described by Bhide and colleagues.11 The contralateral constrictor was defined as the half of the constrictor volume contralateral to the primary site. For midline tumors, the side of the neck with a lower volume of lymph node metastases was judged to be the contralateral side.
One-year dysphagia was defined as having a gastronomy tube (G-tube) in place or an abnormal modified barium swallow (MBS) ≥ 12 months after the completion of radiation. At the study institution, MBS is not routinely done after therapy but is ordered if a patient or clinician has concerns about swallowing function. MBS was considered abnormal if there was laryngeal penetration that reached the level of the glottis or was not ejected from the larynx.
Results
The VA Cancer Registry identified 113 patients treated for H&N cancer during the study period. Of these, 55 patients met the inclusion criteria. No patients were lost to follow-up. The median follow-up was 29 months. The median age was 67 years (range, 41-83) (Table 1).
All patients were treated with intensity-modulated radiotherapy (IMRT). Patients treated with a sequential boost had an initial dose of 54 Gy and/or 50 Gy, followed by a boost to a total of 70 Gy at 2 Gy per fraction. Patients treated with a simultaneous integrated boost (SIB) technique received 69.96 Gy in 33 fractions, with elective volumes treated to 54.45 Gy in 33 fractions. Both patients with nasopharyngeal cancer were treated with SIB plans and had an intermediate dose volume of 59.4 Gy.
Systemic therapy was weekly cisplatin in 41 patients (75%) and cetuximab in 14 (25%). Twenty percent of patients receiving cisplatin switched to an alternative agent during treatment, most commonly carboplatin.
Forty-nine patients (89%) had a G-tube placed before starting radiation. G-tubes were in place for an interval of 0 to 47 months (mean, 8.6); 12 (22%) had a G-tube > 12 months. After completion of radiation, 18 patients (33%) had an abnormal MBS. These were done 1 to 50 months (mean, 14.8) after completion of radiation. Abnormal MBS occurred ≥ 12 months after radiation in 9 patients, 5 of whom had their G-tube in place for less than a year.
Forty-six patients (84%) survived more than 1 year and could be evaluated for late swallowing function. One-year dysphagia was seen in 17 (37%) of these patients. Recurrence was seen in 20 patients (36%), with locoregional recurrence in 12 (60%) of these cases. Recurrence occurred at a range of 0 to 15 months (mean, 5.6). Neither recurrence (P = .69) nor locoregional recurrence (P = .11) was associated with increased 1-year dysphagia.
In patients who could be evaluated for long-term swallowing function, contralateral constrictor V60 ranged from 0% to 100% (median, 51%). V60 was < 40% in 18 patients (39%). With V60 < 40%, there was a 6% rate of 1-year dysphagia compared with 57% for V60 ≥ 40% (P < .001).
Patients with contralateral constrictor V60 < 40 and V60 ≥ 40 both had a mean age of 65 years. χ2 analysis did not show a difference in T stage or systemic treatment but did show that patients with V60 < 40% were more likely to have N1 disease (P = .01), and less likely to have N2 disease (P = .01) compared with patients with V60 ≥ 40%. The difference in 1-year dysphagia between N0 to N1 patients (27%) and N2 to N3 patients (46%) was not statistically significant (P = .19).
In patients who could be evaluated for long-term swallowing function, the uninvolved pharynx volume median of the total constrictor volume was 32% (range, < 1%-62%). The uninvolved pharynx mean dose ranged from 28 to 68 Gy (median, 45). When the uninvolved pharynx mean dose was < 45 Gy, 1-year dysphagia was 22% compared with 52% with a dose ≥ 45 Gy (P = .03).
Air cavity editing was performed in 27 patients (49%). One-year survival was 93% with air cavity editing, and 75% without, which was not statistically significant. Locoregional recurrence occurred in 3 patients (11%) with air cavity editing, and 9 (32%) without, which was not statistically significant. In patients surviving at least 1 year, contralateral constrictor V60 averaged 33% with editing and 62% without editing (P < .001). One-year dysphagia was 12% with air cavity editing and 67% without editing (P < .001).
An SIB technique was done in 26 patients (47%). One-year survival was 85% (n = 22) with SIB and 83% (n = 24) with sequential boost, which was not statistically significant. Locoregional recurrence occurred in 19% with SIB, and 32% with sequential boost, which was not statistically significant. For SIB patients alive at 1 year, the median contralateral V60 was 28%, compared with 66% for patients treated with sequential technique. Seventeen patients (77%) with SIB had V60 < 40%. Nineteen (86%) of SIB plans also had air cavity editing. One patient (5%) with SIB had dysphagia at 1 year, compared with 16 (67%) sequential patients (P < .001).
Discussion
This is the first study to link contralateral constrictor dose to long-term dysphagia in patients treated with radiation for H&N cancer. Editing the boost volume off air cavities was associated with lower contralateral constrictor V60 and with less long-term dysphagia. This may indicate that optimizing plans to meet a contralateral constrictor constraint can reduce rates of long-term dysphagia.
The most useful clinical predictors are those that identify a patient at low risk for toxicity. These constraints are useful because they reassure physicians that treatments will have a favorable risk/benefit ratio while identifying plans that may need modification before starting treatment.
The contralateral constrictor outperformed the uninvolved pharynx in identifying patients at low risk for long-term dysphagia. This difference could not be overcome by decreasing the threshold of the pharynx constraint, as 17% of patients with dysphagia had a mean dose of < 40 Gy to the uninvolved pharynx, which was not statistically significant.
An advantage of contralateral constrictor is that it is independent of planning target volume (PTV) size. The uninvolved pharynx structure depends on the PTV contour, so it may obscure a connection between PTV size and dysphagia.
In the context of a clinical trial, only measuring dose to the uninvolved pharynx may allow more plans to meet constraints, but even in NRG trials, physicians have some control over target volumes. For example, NRG HN009, a national trial for patients with H&N cancer, recommends editing the CTV_7000 (clinical target volume treated to 70 Gy) off air cavities but does not define how much the volume should be cropped or specify protocol violations if the volume is not cropped.15 Furthermore, constraints used in clinical trials are often adopted for use outside the trial, where physicians have extensive control over target volumes.
The broad range of uninvolved pharynx volume relative to total constrictor volume confounds predictions using this variable. For example, according to the NRG constraint, a patient with an uninvolved pharynx mean dose of 44 Gy will have a low risk of dysphagia even if this structure is only 1% of the total constrictor. The contralateral constrictor is always about 50% of the total constrictor volume, which means that predictions using this structure will not be confounded by the same variation in volume size.
Figure 2 shows a representative patient who met the NRG uninvolved pharynx constraint but developed long-term dysphagia.
Pharyngoesophageal stricture is a common cause of dysphagia after IMRT for H&N cancer.16 Radiation has been shown to decrease pharyngeal function in patients with H&N cancer.17 Sparing one side of the pharynx may allow for better pharyngeal compliance throughout the length of the pharynx, possibly decreasing the rate of pharyngoesophageal stricture. Additionally, constraining the contralateral constrictor may preserve strength on this side, allowing it to compensate for weakness on the side of the primary cancer. An exercise sometimes used for dysphagia involves head rotation toward the affected side during swallowing. This technique has been shown to cause food to move to the unaffected side.18 Sparing the contralateral constrictor may help such techniques work better in patients with H&N cancer.
Few studies have commented specifically on dose to swallowing structures contralateral to the primary tumor. Two studies have proposed contralateral submandibular gland constraints for dysphagia (not xerostomia), but neither measured the dose to the contralateral constrictor muscle.9,10 Although the contralateral submandibular dose may correlate with dose to the constrictor on that side, the submandibular gland may have a less direct impact on swallowing than the constrictor muscle, and its limited dimensions may make constraints based on the gland less robust for cancers outside the oropharynx.
Another study reported improved quality of life in patients who were not treated with elective contralateral retropharyngeal radiation.19 Although it is likely that doses to the contralateral constrictor were lower in patients who did not receive elective radiation to this area, this study did not measure or constrain doses to the contralateral constrictors.
Limitations
This study is limited by its single institution, retrospective design, small sample size, and by all patients being male. The high correlation between air cavity editing and the use of SIB makes it impossible to assess the impact of each technique individually. Patients with contralateral constrictor V60 < 40% were less likely to have N2 disease, but N2 to N3 disease did not predict higher 1-year dysphagia, so the difference in N-category cannot fully explain the difference in 1-year dysphagia. It is possible that unreported factors, such as CTV, may contribute significantly to swallowing function. Nevertheless, within the study population, contralateral constrictor dose was able to identify a group with a low rate of long-term dysphagia.
Conclusions
Contralateral constrictor dose is a promising predictor of late dysphagia for patients with H&N cancer treated with radiation with concurrent systemic therapy. Contralateral constrictor V60 < 40% was able to identify a group of patients with a low rate of 1-year dysphagia in this single-center retrospective study. The correlation between air cavity editing and contralateral constrictor V60 suggests that contralateral constrictor dose may depend partly on technique. Further studies are needed to see if the contralateral constrictor dose can be used to predict long-term dysphagia prospectively and in other patient populations.
1. Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, et al. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 2008;26(22):3770-3776. doi:10.1200/JCO.2007.14.6647
2. Nguyen NP, Frank C, Moltz CC, et al. Impact of dysphagia on quality of life after treatment of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2005;61(3):772-778. doi:10.1016/j.ijrobp.2004.06.017
3. Ramaekers BLT, Joore MA, Grutters JPC, et al. The impact of late treatment-toxicity on generic health-related quality of life in head and neck cancer patients after radiotherapy. Oral Oncol. 2011;47(8):768-774. doi:10.1016/j.oraloncology.2011.05.012
4. Christianen MEMC, Schilstra C, Beetz I, et al. Predictive modelling for swallowing dysfunction after primary (chemo)radiation: results of a prospective observational study. Radiother Oncol. 2012;105(1):107-114. doi:10.1016/j.radonc.2011.08.009
5. Vlachich G, Spratt DE, Diaz R, et al. Dose to inferior pharyngeal conctrictor predicts prolonged gastrostomy tube dependence with concurrent intensity-modulated radiation therapy and chemotherapy for locally-advanced head and neck cancer. Radiother Oncol. 2014;110(3):435-440. doi:10.1016/j.radonc.2013.12.007
6. Mogadas S, Busch CJ, Pflug Cet al. Influence of radiation dose to pharyngeal constrictor muscles on late dysphagia and quality of life in patients with locally advanced oropharyngeal carcinoma. Strahlenther Onkol. 2020;196(6):522-529. doi:10.1007/s00066-019-01572-0
7. Caglar HB, Tishler RB, Othus M, et al. Dose to larynx predicts of swallowing complications after intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72(4):1110-1118. doi:10.1016/j.ijrobp.2008.02.048
8. Schwartz DL, Hutcheson K, Barringer D, et al. Candidate dosimetric predictors of long-term swallowing dysfunction after oropharyngeal intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78(5):1356-1365. doi:10.1016/j.ijrobp.2009.10.002
9. Gensheimer MF, Nyflot M, Laramore GE, Laio JL, Parvathaneni U. Contribution of submandibular gland and swallowing structure sparing to post-radiation therapy peg dependence in oropharynx cancer patients treated with split-neck IMRT technique. Radiat Oncol. 2015;11(1):1-7. doi:10.1186/s13014-016-0726-3
10. Hedström J, Tuomi L, Finizia C, Olsson C. Identifying organs at risk for radiation-induced late dysphagia in head and neck cancer patients. Clin Transl Radiat Oncol. 2019;19:87-95. doi:10.1016/j.ctro.2019.08.005
11. Bhide SA, Gulliford S, Kazi R, et al. Correlation between dose to the pharyngeal constrictors and patient quality of life and late dysphagia following chemo-IMRT for head and neck cancer. Radiother Oncol. 2009;93(3):539-544. doi:10.1016/j.radonc.2009.09.017
12. Caudell JJ, Schaner PE, Desmond RA, Meredith RF, Spencer SA, Bonner JA. Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2010;76(2):403-409. doi:10.1016/j.ijrobp.2009.02.017
13. Levendag PC, Teguh DN, Voet P, et al. Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiother Oncol. 2007;85(1):64-73. doi:10.1016/j.radonc.2007.07.009
14. Eisbruch A, Schwartz M, Rasch C, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004;60(5):1425-1439. doi:10.1016/j.ijrobp.2004.05.050
15. Harari PM; NRG Oncology. Comparing high-dose cisplatin every three weeks to low-dose cisplatin weekly when combined with radiation for patients with advanced head and neck cancer. ClinicalTrials.gov identifier: NCT05050162. Updated November 25, 2022. Accessed December 7, 2022. https://clinicaltrials.gov/ct2/show/NCT05050162
16. Wang JJ, Goldsmith TA, Holman AS, Cianchetti M, Chan AW. Pharyngoesophageal stricture after treatment for head and neck cancer. Head Neck. 2011;34(7):967-973. doi:10.1002/hed.21842
17. Kendall KA, McKenzie SW, Leonard RJ, Jones CU. Timing of swallowing events after single-modality treatment of head and neck carcinoma with radiotherapy. Ann Otol Rhinol Laryngol. 2000;109(8, pt 1):767-775. doi:10.1177/000348940010900812
18. Ohmae Y, Ogura M, Kitahara S. Effects of head rotation on pharyngeal function during normal swallow. Ann Otol Rhinol Laryngol. 1998;107(4):344-348. doi:10.1177/000348949810700414
19. Spencer CR, Gay HA, Haughey BH, et al. Eliminating radiotherapy to the contralateral retropharyngeal and high level II lymph nodes in head and neck squamous cell carcinoma is safe and improves quality of life. Cancer. 2014;120(24):3994-4002. doi:10.1002/cncr.28938
1. Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, et al. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 2008;26(22):3770-3776. doi:10.1200/JCO.2007.14.6647
2. Nguyen NP, Frank C, Moltz CC, et al. Impact of dysphagia on quality of life after treatment of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2005;61(3):772-778. doi:10.1016/j.ijrobp.2004.06.017
3. Ramaekers BLT, Joore MA, Grutters JPC, et al. The impact of late treatment-toxicity on generic health-related quality of life in head and neck cancer patients after radiotherapy. Oral Oncol. 2011;47(8):768-774. doi:10.1016/j.oraloncology.2011.05.012
4. Christianen MEMC, Schilstra C, Beetz I, et al. Predictive modelling for swallowing dysfunction after primary (chemo)radiation: results of a prospective observational study. Radiother Oncol. 2012;105(1):107-114. doi:10.1016/j.radonc.2011.08.009
5. Vlachich G, Spratt DE, Diaz R, et al. Dose to inferior pharyngeal conctrictor predicts prolonged gastrostomy tube dependence with concurrent intensity-modulated radiation therapy and chemotherapy for locally-advanced head and neck cancer. Radiother Oncol. 2014;110(3):435-440. doi:10.1016/j.radonc.2013.12.007
6. Mogadas S, Busch CJ, Pflug Cet al. Influence of radiation dose to pharyngeal constrictor muscles on late dysphagia and quality of life in patients with locally advanced oropharyngeal carcinoma. Strahlenther Onkol. 2020;196(6):522-529. doi:10.1007/s00066-019-01572-0
7. Caglar HB, Tishler RB, Othus M, et al. Dose to larynx predicts of swallowing complications after intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72(4):1110-1118. doi:10.1016/j.ijrobp.2008.02.048
8. Schwartz DL, Hutcheson K, Barringer D, et al. Candidate dosimetric predictors of long-term swallowing dysfunction after oropharyngeal intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78(5):1356-1365. doi:10.1016/j.ijrobp.2009.10.002
9. Gensheimer MF, Nyflot M, Laramore GE, Laio JL, Parvathaneni U. Contribution of submandibular gland and swallowing structure sparing to post-radiation therapy peg dependence in oropharynx cancer patients treated with split-neck IMRT technique. Radiat Oncol. 2015;11(1):1-7. doi:10.1186/s13014-016-0726-3
10. Hedström J, Tuomi L, Finizia C, Olsson C. Identifying organs at risk for radiation-induced late dysphagia in head and neck cancer patients. Clin Transl Radiat Oncol. 2019;19:87-95. doi:10.1016/j.ctro.2019.08.005
11. Bhide SA, Gulliford S, Kazi R, et al. Correlation between dose to the pharyngeal constrictors and patient quality of life and late dysphagia following chemo-IMRT for head and neck cancer. Radiother Oncol. 2009;93(3):539-544. doi:10.1016/j.radonc.2009.09.017
12. Caudell JJ, Schaner PE, Desmond RA, Meredith RF, Spencer SA, Bonner JA. Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2010;76(2):403-409. doi:10.1016/j.ijrobp.2009.02.017
13. Levendag PC, Teguh DN, Voet P, et al. Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiother Oncol. 2007;85(1):64-73. doi:10.1016/j.radonc.2007.07.009
14. Eisbruch A, Schwartz M, Rasch C, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004;60(5):1425-1439. doi:10.1016/j.ijrobp.2004.05.050
15. Harari PM; NRG Oncology. Comparing high-dose cisplatin every three weeks to low-dose cisplatin weekly when combined with radiation for patients with advanced head and neck cancer. ClinicalTrials.gov identifier: NCT05050162. Updated November 25, 2022. Accessed December 7, 2022. https://clinicaltrials.gov/ct2/show/NCT05050162
16. Wang JJ, Goldsmith TA, Holman AS, Cianchetti M, Chan AW. Pharyngoesophageal stricture after treatment for head and neck cancer. Head Neck. 2011;34(7):967-973. doi:10.1002/hed.21842
17. Kendall KA, McKenzie SW, Leonard RJ, Jones CU. Timing of swallowing events after single-modality treatment of head and neck carcinoma with radiotherapy. Ann Otol Rhinol Laryngol. 2000;109(8, pt 1):767-775. doi:10.1177/000348940010900812
18. Ohmae Y, Ogura M, Kitahara S. Effects of head rotation on pharyngeal function during normal swallow. Ann Otol Rhinol Laryngol. 1998;107(4):344-348. doi:10.1177/000348949810700414
19. Spencer CR, Gay HA, Haughey BH, et al. Eliminating radiotherapy to the contralateral retropharyngeal and high level II lymph nodes in head and neck squamous cell carcinoma is safe and improves quality of life. Cancer. 2014;120(24):3994-4002. doi:10.1002/cncr.28938
Consider radiologic imaging for high-risk cutaneous SCC, expert advises
DENVER –
In a study published in 2020, Emily Ruiz, MD, MPH, and colleagues identified 87 CSCC tumors in 83 patients who underwent baseline or surveillance imaging primary at the Brigham and Women’s Hospital Mohs Surgery Clinic and the Dana-Farber Cancer Institute High-Risk Skin Cancer Clinic, both in Boston, from Jan. 1, 2017, to June 1, 2019. Of the 87 primary CSCCs, 48 (58%) underwent surveillance imaging. The researchers found that imaging detected additional disease in 26 patients, or 30% of cases, “whether that be nodal metastasis, local invasion beyond what was clinically accepted, or in-transit disease,” Dr. Ruiz, academic director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s, said during the annual meeting of the American Society for Dermatologic Surgery. “But if you look at the 16 nodal metastases in this cohort, all were picked up on imaging and not on clinical exam.”
Since publication of these results, Dr. Ruiz routinely considers baseline radiologic imaging in T2b and T3 tumors; borderline T2a tumors (which she said they are now calling “T2a high,” for those who have one risk factor plus another intermediate risk factor),” and T2a tumors in patients who are profoundly immunosuppressed.
“My preference is to always do [the imaging] before treatment unless I’m up-staging them during surgery,” said Dr. Ruiz, who also directs the High-Risk Skin Cancer Clinic at Dana Farber. “We have picked up nodal metastases before surgery, which enables us to create a good therapeutic plan for our patients before we start operating. Then we image them every 6 months or so for about 2 years. Sometimes we will extend that out to 3 years.”
Some clinicians use sentinel lymph node biopsy (SLNB) as a diagnostic test, but there are mixed results about its prognostic significance. A retrospective observational study of 720 patients with CSCC found that SLNB provided no benefit regarding further metastasis or tumor-specific survival, compared with those who received routine observation and follow-up, “but head and neck surgeons in the U.S. are putting together some prospective data from multiple centers,” Dr. Ruiz said. “I think in the coming years, you will have more multicenter data to inform us as to whether to do SLNB or not.”
Surgery may be the mainstay of treatment for resectable SCC, but the emerging role of neoadjuvant therapeutics is changing the way oncologists treat these tumors. For example, in a phase 2 trial recently published in the New England Journal of Medicine, 79 patients with stage II-IV CSCC received up to four doses of immunotherapy with the programmed death receptor–1 (PD-1) blocker cemiplimab administered every 3 weeks. The primary endpoint was a pathologic complete response, defined as the absence of viable tumor cells in the surgical specimen at a central laboratory. The researchers observed that 68% of patients had an objective response.
“These were patients with localized tumors that were either very aggressive or had nodal metastases,” said Dr, Ruiz, who was the site primary investigator at Dana Farber and a coauthor of the NEJM study. “This has altered the way we approach treating our larger tumors that could be resectable but have a lot of disease either locally or in the nodal basin. We think that we can shrink down the tumor and make it easier to resect, but also there is the possibility or improving outcomes.”
At Brigham and Women’s and the Dana Farber, she and her colleagues consider immunotherapy for multiple recurrent tumors that have been previously irradiated; cases of large tumor burden locally or in the nodal basin; tumors that have a complex surgical plan; cases where there is a low likelihood of achieving clear surgical margins; and cases of in-transit disease.
“We use two to four doses of immunotherapy prior to surgery and assess the tumor response after two doses both clinically and radiologically,” she said. “If the tumor continues to grow, we would do surgery sooner.”
The side-effect profile of immunotherapy is another consideration. “Some patients are not appropriate for a neoadjuvant immunotherapy approach, such as transplant patients,” she said.
According to the latest National Comprehensive Cancer Network guidelines, surgery with or without adjuvant radiation is the current standard of care for treating CSCC. These guidelines were developed without much data to support the use of radiation, but a 20-year retrospective cohort study at Brigham and Women’s Hospital and the Cleveland Clinic Foundation found that adjuvant radiation following margin resection in high T-stage CSCC cut the risk of local and locoregional recurrence in half.
“This is something that radiation oncologists have told us for years, but there was no data to support it, so it was nice to see that borne out in clinical data,” said Dr. Ruiz, the study’s lead author. The 10% risk of local recurrence observed in the study “may not be high enough for some of our older patients, so we wanted to see if we could identify a group of high tumors that had higher risk of local recurrence,” she said. They found that patients who had a greater than 20% risk of poor outcome were those with recurrent tumors, those with tumors 6 cm or greater in size, and those with all four BWH risk factors (tumor diameter ≥ 2 cm, poorly differentiated histology, perineural invasion ≥ 0.1 mm, or tumor invasion beyond fat excluding bone invasion).
“Those risks were also cut in half if you added radiation,” she said. “So, the way I now approach counseling patients is, I try to estimate their baseline risk as best I can based on the tumor itself. I tell them that if they want to do adjuvant radiation it would cut the risk in half. Some patients are too frail and want to pass on it, while others are very interested.”
Of patients who did not receive radiation but had a disease recurrence, just under half of tumors were salvageable, about 25% died of their disease, and 23% had persistent disease. “I think this does support using radiation earlier on for the appropriate patient,” Dr. Ruiz said. “I consider the baseline risks [and] balance that with the patient’s comorbidities.”
Limited data exists on adjuvant immunotherapy for CSCC, but two ongoing randomized prospective clinical trials underway are studying the PD-1 inhibitors cemiplimab and pembrolizumab versus placebo. “We don’t have data yet, but prior to randomization, patients undergo surgery with macroscopic gross resection of all disease,” Dr. Ruiz said. “All tumors receive ART [adjuvant radiation therapy] prior to randomization”
Dr. Ruiz disclosed that she is a consultant for Sanofi, Regeneron, Genentech, and Jaunce Therapeutics. She is also a member of the advisory board for Checkpoint Therapeutics and is an investigator for Merck, Sanofi, and Regeneron.
DENVER –
In a study published in 2020, Emily Ruiz, MD, MPH, and colleagues identified 87 CSCC tumors in 83 patients who underwent baseline or surveillance imaging primary at the Brigham and Women’s Hospital Mohs Surgery Clinic and the Dana-Farber Cancer Institute High-Risk Skin Cancer Clinic, both in Boston, from Jan. 1, 2017, to June 1, 2019. Of the 87 primary CSCCs, 48 (58%) underwent surveillance imaging. The researchers found that imaging detected additional disease in 26 patients, or 30% of cases, “whether that be nodal metastasis, local invasion beyond what was clinically accepted, or in-transit disease,” Dr. Ruiz, academic director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s, said during the annual meeting of the American Society for Dermatologic Surgery. “But if you look at the 16 nodal metastases in this cohort, all were picked up on imaging and not on clinical exam.”
Since publication of these results, Dr. Ruiz routinely considers baseline radiologic imaging in T2b and T3 tumors; borderline T2a tumors (which she said they are now calling “T2a high,” for those who have one risk factor plus another intermediate risk factor),” and T2a tumors in patients who are profoundly immunosuppressed.
“My preference is to always do [the imaging] before treatment unless I’m up-staging them during surgery,” said Dr. Ruiz, who also directs the High-Risk Skin Cancer Clinic at Dana Farber. “We have picked up nodal metastases before surgery, which enables us to create a good therapeutic plan for our patients before we start operating. Then we image them every 6 months or so for about 2 years. Sometimes we will extend that out to 3 years.”
Some clinicians use sentinel lymph node biopsy (SLNB) as a diagnostic test, but there are mixed results about its prognostic significance. A retrospective observational study of 720 patients with CSCC found that SLNB provided no benefit regarding further metastasis or tumor-specific survival, compared with those who received routine observation and follow-up, “but head and neck surgeons in the U.S. are putting together some prospective data from multiple centers,” Dr. Ruiz said. “I think in the coming years, you will have more multicenter data to inform us as to whether to do SLNB or not.”
Surgery may be the mainstay of treatment for resectable SCC, but the emerging role of neoadjuvant therapeutics is changing the way oncologists treat these tumors. For example, in a phase 2 trial recently published in the New England Journal of Medicine, 79 patients with stage II-IV CSCC received up to four doses of immunotherapy with the programmed death receptor–1 (PD-1) blocker cemiplimab administered every 3 weeks. The primary endpoint was a pathologic complete response, defined as the absence of viable tumor cells in the surgical specimen at a central laboratory. The researchers observed that 68% of patients had an objective response.
“These were patients with localized tumors that were either very aggressive or had nodal metastases,” said Dr, Ruiz, who was the site primary investigator at Dana Farber and a coauthor of the NEJM study. “This has altered the way we approach treating our larger tumors that could be resectable but have a lot of disease either locally or in the nodal basin. We think that we can shrink down the tumor and make it easier to resect, but also there is the possibility or improving outcomes.”
At Brigham and Women’s and the Dana Farber, she and her colleagues consider immunotherapy for multiple recurrent tumors that have been previously irradiated; cases of large tumor burden locally or in the nodal basin; tumors that have a complex surgical plan; cases where there is a low likelihood of achieving clear surgical margins; and cases of in-transit disease.
“We use two to four doses of immunotherapy prior to surgery and assess the tumor response after two doses both clinically and radiologically,” she said. “If the tumor continues to grow, we would do surgery sooner.”
The side-effect profile of immunotherapy is another consideration. “Some patients are not appropriate for a neoadjuvant immunotherapy approach, such as transplant patients,” she said.
According to the latest National Comprehensive Cancer Network guidelines, surgery with or without adjuvant radiation is the current standard of care for treating CSCC. These guidelines were developed without much data to support the use of radiation, but a 20-year retrospective cohort study at Brigham and Women’s Hospital and the Cleveland Clinic Foundation found that adjuvant radiation following margin resection in high T-stage CSCC cut the risk of local and locoregional recurrence in half.
“This is something that radiation oncologists have told us for years, but there was no data to support it, so it was nice to see that borne out in clinical data,” said Dr. Ruiz, the study’s lead author. The 10% risk of local recurrence observed in the study “may not be high enough for some of our older patients, so we wanted to see if we could identify a group of high tumors that had higher risk of local recurrence,” she said. They found that patients who had a greater than 20% risk of poor outcome were those with recurrent tumors, those with tumors 6 cm or greater in size, and those with all four BWH risk factors (tumor diameter ≥ 2 cm, poorly differentiated histology, perineural invasion ≥ 0.1 mm, or tumor invasion beyond fat excluding bone invasion).
“Those risks were also cut in half if you added radiation,” she said. “So, the way I now approach counseling patients is, I try to estimate their baseline risk as best I can based on the tumor itself. I tell them that if they want to do adjuvant radiation it would cut the risk in half. Some patients are too frail and want to pass on it, while others are very interested.”
Of patients who did not receive radiation but had a disease recurrence, just under half of tumors were salvageable, about 25% died of their disease, and 23% had persistent disease. “I think this does support using radiation earlier on for the appropriate patient,” Dr. Ruiz said. “I consider the baseline risks [and] balance that with the patient’s comorbidities.”
Limited data exists on adjuvant immunotherapy for CSCC, but two ongoing randomized prospective clinical trials underway are studying the PD-1 inhibitors cemiplimab and pembrolizumab versus placebo. “We don’t have data yet, but prior to randomization, patients undergo surgery with macroscopic gross resection of all disease,” Dr. Ruiz said. “All tumors receive ART [adjuvant radiation therapy] prior to randomization”
Dr. Ruiz disclosed that she is a consultant for Sanofi, Regeneron, Genentech, and Jaunce Therapeutics. She is also a member of the advisory board for Checkpoint Therapeutics and is an investigator for Merck, Sanofi, and Regeneron.
DENVER –
In a study published in 2020, Emily Ruiz, MD, MPH, and colleagues identified 87 CSCC tumors in 83 patients who underwent baseline or surveillance imaging primary at the Brigham and Women’s Hospital Mohs Surgery Clinic and the Dana-Farber Cancer Institute High-Risk Skin Cancer Clinic, both in Boston, from Jan. 1, 2017, to June 1, 2019. Of the 87 primary CSCCs, 48 (58%) underwent surveillance imaging. The researchers found that imaging detected additional disease in 26 patients, or 30% of cases, “whether that be nodal metastasis, local invasion beyond what was clinically accepted, or in-transit disease,” Dr. Ruiz, academic director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s, said during the annual meeting of the American Society for Dermatologic Surgery. “But if you look at the 16 nodal metastases in this cohort, all were picked up on imaging and not on clinical exam.”
Since publication of these results, Dr. Ruiz routinely considers baseline radiologic imaging in T2b and T3 tumors; borderline T2a tumors (which she said they are now calling “T2a high,” for those who have one risk factor plus another intermediate risk factor),” and T2a tumors in patients who are profoundly immunosuppressed.
“My preference is to always do [the imaging] before treatment unless I’m up-staging them during surgery,” said Dr. Ruiz, who also directs the High-Risk Skin Cancer Clinic at Dana Farber. “We have picked up nodal metastases before surgery, which enables us to create a good therapeutic plan for our patients before we start operating. Then we image them every 6 months or so for about 2 years. Sometimes we will extend that out to 3 years.”
Some clinicians use sentinel lymph node biopsy (SLNB) as a diagnostic test, but there are mixed results about its prognostic significance. A retrospective observational study of 720 patients with CSCC found that SLNB provided no benefit regarding further metastasis or tumor-specific survival, compared with those who received routine observation and follow-up, “but head and neck surgeons in the U.S. are putting together some prospective data from multiple centers,” Dr. Ruiz said. “I think in the coming years, you will have more multicenter data to inform us as to whether to do SLNB or not.”
Surgery may be the mainstay of treatment for resectable SCC, but the emerging role of neoadjuvant therapeutics is changing the way oncologists treat these tumors. For example, in a phase 2 trial recently published in the New England Journal of Medicine, 79 patients with stage II-IV CSCC received up to four doses of immunotherapy with the programmed death receptor–1 (PD-1) blocker cemiplimab administered every 3 weeks. The primary endpoint was a pathologic complete response, defined as the absence of viable tumor cells in the surgical specimen at a central laboratory. The researchers observed that 68% of patients had an objective response.
“These were patients with localized tumors that were either very aggressive or had nodal metastases,” said Dr, Ruiz, who was the site primary investigator at Dana Farber and a coauthor of the NEJM study. “This has altered the way we approach treating our larger tumors that could be resectable but have a lot of disease either locally or in the nodal basin. We think that we can shrink down the tumor and make it easier to resect, but also there is the possibility or improving outcomes.”
At Brigham and Women’s and the Dana Farber, she and her colleagues consider immunotherapy for multiple recurrent tumors that have been previously irradiated; cases of large tumor burden locally or in the nodal basin; tumors that have a complex surgical plan; cases where there is a low likelihood of achieving clear surgical margins; and cases of in-transit disease.
“We use two to four doses of immunotherapy prior to surgery and assess the tumor response after two doses both clinically and radiologically,” she said. “If the tumor continues to grow, we would do surgery sooner.”
The side-effect profile of immunotherapy is another consideration. “Some patients are not appropriate for a neoadjuvant immunotherapy approach, such as transplant patients,” she said.
According to the latest National Comprehensive Cancer Network guidelines, surgery with or without adjuvant radiation is the current standard of care for treating CSCC. These guidelines were developed without much data to support the use of radiation, but a 20-year retrospective cohort study at Brigham and Women’s Hospital and the Cleveland Clinic Foundation found that adjuvant radiation following margin resection in high T-stage CSCC cut the risk of local and locoregional recurrence in half.
“This is something that radiation oncologists have told us for years, but there was no data to support it, so it was nice to see that borne out in clinical data,” said Dr. Ruiz, the study’s lead author. The 10% risk of local recurrence observed in the study “may not be high enough for some of our older patients, so we wanted to see if we could identify a group of high tumors that had higher risk of local recurrence,” she said. They found that patients who had a greater than 20% risk of poor outcome were those with recurrent tumors, those with tumors 6 cm or greater in size, and those with all four BWH risk factors (tumor diameter ≥ 2 cm, poorly differentiated histology, perineural invasion ≥ 0.1 mm, or tumor invasion beyond fat excluding bone invasion).
“Those risks were also cut in half if you added radiation,” she said. “So, the way I now approach counseling patients is, I try to estimate their baseline risk as best I can based on the tumor itself. I tell them that if they want to do adjuvant radiation it would cut the risk in half. Some patients are too frail and want to pass on it, while others are very interested.”
Of patients who did not receive radiation but had a disease recurrence, just under half of tumors were salvageable, about 25% died of their disease, and 23% had persistent disease. “I think this does support using radiation earlier on for the appropriate patient,” Dr. Ruiz said. “I consider the baseline risks [and] balance that with the patient’s comorbidities.”
Limited data exists on adjuvant immunotherapy for CSCC, but two ongoing randomized prospective clinical trials underway are studying the PD-1 inhibitors cemiplimab and pembrolizumab versus placebo. “We don’t have data yet, but prior to randomization, patients undergo surgery with macroscopic gross resection of all disease,” Dr. Ruiz said. “All tumors receive ART [adjuvant radiation therapy] prior to randomization”
Dr. Ruiz disclosed that she is a consultant for Sanofi, Regeneron, Genentech, and Jaunce Therapeutics. She is also a member of the advisory board for Checkpoint Therapeutics and is an investigator for Merck, Sanofi, and Regeneron.
AT ASDS 2022
Pain in Cancer Survivors: Assess, Monitor, and Ask for Help
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
VA Center Dramatically Shrinks Wait Times for Bone Marrow Biopsies
SAN DIEGO–The Louis Stokes Cleveland VA Medical Center in Ohio dramatically reduced wait times for bone marrow biopsies and treatment by ditching the radiology department and opening a weekly clinic devoted to the procedures, a cancer care team reported at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) September 16 to 18, 2022.
The average time from biopsy order to procedure fell by more than two-thirds from 23.1 days to 7.0 days, and the time from order to diagnosis dipped from 27.8 days to 11.6 days. The time from treatment fell from 54.8 days to 20.2 days.
The new strategy aims to avoid sending patients to the radiology department and treat them in a clinic within the cancer center instead. “It’s great to be able to keep as many hematology/oncology–related things such as infusion, scheduling, and procedures within our department. It provides continuity for the veteran, and it’s helpful for them from that aspect,” said nurse practitioner Kyle Stimpert, MSN, RN, ACNP, of VA Northeast Ohio Healthcare System.
As the cancer team reported in an abstract presented at the AVAHO meeting, “bone marrow biopsies often need to be performed expeditiously to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization, there are fewer hematology/oncology providers available to perform this procedure.”
The Cleveland VA tried to address this problem by sending patients to interventional radiology, but it still took weeks for bone marrow biopsies to be performed: From August 4, 2020, to August 12, 2021, when 140 biopsies were performed, the average time from order to procedure was 23.1 days. The time from order to diagnosis was 27.8 days, and from order to treatment was 54.8 days.
The bone marrow biopsies provide insight into diseases such as hematologic malignancies and myelodysplastic syndromes, Stimpert said. The procedures may lead to diagnoses or reveal how treatment is progressing.
In 2021, new leadership sought to shrink the wait times. “We put together a small team and started brainstorming,” said oncology clinical nurse specialist Alecia Smalheer, MSN, APRN, OCN, in an interview. With the help of staff who’d come from other facilities, she said, “we were able to see what was being done in surrounding community hospitals and come up with a model and a checklist.”
The team modified a space to create a new weekly, half-day bone marrow biopsy clinic. They also worked on procedures, documentation, education of patients, and training of staff, Smalheer said.
After implementation in the summer of 2021, the biopsy clinic performed 89 procedures through August 31, 2022. The average time from order to procedure was 7.0 days. The time to diagnosis was 11.6 days, and the time to treatment was 20.2 days. The differences between the pre-implementation and postimplementation periods were statistically significant. (P < .001 for each).
The biopsy clinic now sees about 3 to 4 patients a week. “Just yesterday, I had a vet whose cancer was going down. I was able to just do this bone marrow right there, and it was amazing. He didn’t have to go home [and come back],” Stimpert said. “A lot of patients travel a far distance or on oxygen, or it’s hard for them to get around. Coming to the facility for repeat appointments can just take a lot out of them. So it’s really nice to be able to get it all done in one visit.”
There are multiple benefits to shortening wait times, Smalheer said. “They can start treatment much sooner… but it also alleviates some of the emotional distress of waiting. They still have some waiting to do, but it’s definitely not as long.”
And, Stimpert added, patients are familiar with the infusion center and will see faces they know.
As for cost, the biopsy clinic may save money due to several factors related to how and where the biopsy procedures are performed, Stimpert said.
No disclosures are reported.
SAN DIEGO–The Louis Stokes Cleveland VA Medical Center in Ohio dramatically reduced wait times for bone marrow biopsies and treatment by ditching the radiology department and opening a weekly clinic devoted to the procedures, a cancer care team reported at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) September 16 to 18, 2022.
The average time from biopsy order to procedure fell by more than two-thirds from 23.1 days to 7.0 days, and the time from order to diagnosis dipped from 27.8 days to 11.6 days. The time from treatment fell from 54.8 days to 20.2 days.
The new strategy aims to avoid sending patients to the radiology department and treat them in a clinic within the cancer center instead. “It’s great to be able to keep as many hematology/oncology–related things such as infusion, scheduling, and procedures within our department. It provides continuity for the veteran, and it’s helpful for them from that aspect,” said nurse practitioner Kyle Stimpert, MSN, RN, ACNP, of VA Northeast Ohio Healthcare System.
As the cancer team reported in an abstract presented at the AVAHO meeting, “bone marrow biopsies often need to be performed expeditiously to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization, there are fewer hematology/oncology providers available to perform this procedure.”
The Cleveland VA tried to address this problem by sending patients to interventional radiology, but it still took weeks for bone marrow biopsies to be performed: From August 4, 2020, to August 12, 2021, when 140 biopsies were performed, the average time from order to procedure was 23.1 days. The time from order to diagnosis was 27.8 days, and from order to treatment was 54.8 days.
The bone marrow biopsies provide insight into diseases such as hematologic malignancies and myelodysplastic syndromes, Stimpert said. The procedures may lead to diagnoses or reveal how treatment is progressing.
In 2021, new leadership sought to shrink the wait times. “We put together a small team and started brainstorming,” said oncology clinical nurse specialist Alecia Smalheer, MSN, APRN, OCN, in an interview. With the help of staff who’d come from other facilities, she said, “we were able to see what was being done in surrounding community hospitals and come up with a model and a checklist.”
The team modified a space to create a new weekly, half-day bone marrow biopsy clinic. They also worked on procedures, documentation, education of patients, and training of staff, Smalheer said.
After implementation in the summer of 2021, the biopsy clinic performed 89 procedures through August 31, 2022. The average time from order to procedure was 7.0 days. The time to diagnosis was 11.6 days, and the time to treatment was 20.2 days. The differences between the pre-implementation and postimplementation periods were statistically significant. (P < .001 for each).
The biopsy clinic now sees about 3 to 4 patients a week. “Just yesterday, I had a vet whose cancer was going down. I was able to just do this bone marrow right there, and it was amazing. He didn’t have to go home [and come back],” Stimpert said. “A lot of patients travel a far distance or on oxygen, or it’s hard for them to get around. Coming to the facility for repeat appointments can just take a lot out of them. So it’s really nice to be able to get it all done in one visit.”
There are multiple benefits to shortening wait times, Smalheer said. “They can start treatment much sooner… but it also alleviates some of the emotional distress of waiting. They still have some waiting to do, but it’s definitely not as long.”
And, Stimpert added, patients are familiar with the infusion center and will see faces they know.
As for cost, the biopsy clinic may save money due to several factors related to how and where the biopsy procedures are performed, Stimpert said.
No disclosures are reported.
SAN DIEGO–The Louis Stokes Cleveland VA Medical Center in Ohio dramatically reduced wait times for bone marrow biopsies and treatment by ditching the radiology department and opening a weekly clinic devoted to the procedures, a cancer care team reported at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) September 16 to 18, 2022.
The average time from biopsy order to procedure fell by more than two-thirds from 23.1 days to 7.0 days, and the time from order to diagnosis dipped from 27.8 days to 11.6 days. The time from treatment fell from 54.8 days to 20.2 days.
The new strategy aims to avoid sending patients to the radiology department and treat them in a clinic within the cancer center instead. “It’s great to be able to keep as many hematology/oncology–related things such as infusion, scheduling, and procedures within our department. It provides continuity for the veteran, and it’s helpful for them from that aspect,” said nurse practitioner Kyle Stimpert, MSN, RN, ACNP, of VA Northeast Ohio Healthcare System.
As the cancer team reported in an abstract presented at the AVAHO meeting, “bone marrow biopsies often need to be performed expeditiously to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization, there are fewer hematology/oncology providers available to perform this procedure.”
The Cleveland VA tried to address this problem by sending patients to interventional radiology, but it still took weeks for bone marrow biopsies to be performed: From August 4, 2020, to August 12, 2021, when 140 biopsies were performed, the average time from order to procedure was 23.1 days. The time from order to diagnosis was 27.8 days, and from order to treatment was 54.8 days.
The bone marrow biopsies provide insight into diseases such as hematologic malignancies and myelodysplastic syndromes, Stimpert said. The procedures may lead to diagnoses or reveal how treatment is progressing.
In 2021, new leadership sought to shrink the wait times. “We put together a small team and started brainstorming,” said oncology clinical nurse specialist Alecia Smalheer, MSN, APRN, OCN, in an interview. With the help of staff who’d come from other facilities, she said, “we were able to see what was being done in surrounding community hospitals and come up with a model and a checklist.”
The team modified a space to create a new weekly, half-day bone marrow biopsy clinic. They also worked on procedures, documentation, education of patients, and training of staff, Smalheer said.
After implementation in the summer of 2021, the biopsy clinic performed 89 procedures through August 31, 2022. The average time from order to procedure was 7.0 days. The time to diagnosis was 11.6 days, and the time to treatment was 20.2 days. The differences between the pre-implementation and postimplementation periods were statistically significant. (P < .001 for each).
The biopsy clinic now sees about 3 to 4 patients a week. “Just yesterday, I had a vet whose cancer was going down. I was able to just do this bone marrow right there, and it was amazing. He didn’t have to go home [and come back],” Stimpert said. “A lot of patients travel a far distance or on oxygen, or it’s hard for them to get around. Coming to the facility for repeat appointments can just take a lot out of them. So it’s really nice to be able to get it all done in one visit.”
There are multiple benefits to shortening wait times, Smalheer said. “They can start treatment much sooner… but it also alleviates some of the emotional distress of waiting. They still have some waiting to do, but it’s definitely not as long.”
And, Stimpert added, patients are familiar with the infusion center and will see faces they know.
As for cost, the biopsy clinic may save money due to several factors related to how and where the biopsy procedures are performed, Stimpert said.
No disclosures are reported.
In VA Oncology, Discussion Groups Are Transforming the Workplace
SAN DIEGO—From coast to coast, 10 US Department of Veterans Affairs (VA) medical centers are holding meetings designed to help clinicians and colleagues talk openly about touchy workplace topics, such as compassion, burnout, and medical errors. New data suggests that “Schwartz Rounds” have tremendous power to change how medical professionals cope, communicate, and commiserate.
At the VA Connecticut Healthcare System (VACHS), nearly all (98%) respondents who took part in Schwartz Round sessions rated them as either good or excellent, 89% reported feeling less isolated in their work with patients, 98% had new insights into the perspectives and experiences of colleagues, and 93% felt more open to communicating with colleagues, reported oncologist Edward Perry, MD, of VA Connecticut and Yale University School of Medicine, in a presentation here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) held September 16 to 18, 2022.
Schwartz Rounds have been around for 25 years and are named after the late Ken Schwartz, a 40-year-old Boston health care attorney who wrote movingly in 1995 about the “exquisite compassion” he experienced while being treated for advanced lung cancer—and the risk that the rapidly evolving health care system would lose its sense of empathy.
The Boston-based nonprofit Schwartz Center for Compassionate Healthcare facilitates Schwartz Rounds, which are now held at about 600 health care organizations around the world. That number includes the 10 VA medical centers, mostly in the Northeast (Massachusetts, New York, Connecticut, and New Hampshire) but also in California, Illinois, and Minnesota.
Site teams work with the Schwartz Center to plan the rounds and gather data about their effectiveness. “Unlike traditional clinical or ethics rounds, this is not a didactic or problem-solving session. The focus is not on what happened, but how those who were involved felt. In other words, the human dimension of medicine,” Dr. Perry said. “There are no right or wrong answers. Everything that is said during short rounds is confidential. We do encourage people to continue discussion of the general themes afterward but not to share any specifics of what was discussed.”
At VACHS, Schwartz rounds began shortly before the COVID-19 pandemic, Perry said, and they’ve been held virtually since the first meeting. “Schwartz Rounds are open to all employees, trainees, and students at the institution. Anyone with a VA badge is welcome to attend,” he said. “We're averaging about 150 attendees per session.”
Speakers have addressed social/emotional topics, including delivering bad news to patients, maintaining compassion during adversity, and providing compassionate care to patients with substance use disorders.
The VACHS survey of Schwartz Rounds participants had a 50% response rate, with about 400 people responding to each question. Nearly all (98%) said they planned to attend the rounds again, and 55% agreed that a specific discussion “suggests that changes may be needed in departmental or institutional policies or practices.”
The administration has agreed to continue the Schwartz Rounds in light of the positive results, Perry said. As he noted, the Schwartz Center charges dues and initiation fees. The Marjorie Stanzler Financial Aid Fund underwrites the initiation fees for qualifying organizations, including VA facilities.
As for lessons, he said the topics of Schwartz Rounds “should be emotionally resonant. They should involve multiple disciplines and perspectives. They should illuminate an issue or experience that is not often discussed. And should inspire participants to share their own experiences and highlight instances of compassionate care—or barriers to providing compassionate care.”
Dr. Perry has no disclosures.
SAN DIEGO—From coast to coast, 10 US Department of Veterans Affairs (VA) medical centers are holding meetings designed to help clinicians and colleagues talk openly about touchy workplace topics, such as compassion, burnout, and medical errors. New data suggests that “Schwartz Rounds” have tremendous power to change how medical professionals cope, communicate, and commiserate.
At the VA Connecticut Healthcare System (VACHS), nearly all (98%) respondents who took part in Schwartz Round sessions rated them as either good or excellent, 89% reported feeling less isolated in their work with patients, 98% had new insights into the perspectives and experiences of colleagues, and 93% felt more open to communicating with colleagues, reported oncologist Edward Perry, MD, of VA Connecticut and Yale University School of Medicine, in a presentation here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) held September 16 to 18, 2022.
Schwartz Rounds have been around for 25 years and are named after the late Ken Schwartz, a 40-year-old Boston health care attorney who wrote movingly in 1995 about the “exquisite compassion” he experienced while being treated for advanced lung cancer—and the risk that the rapidly evolving health care system would lose its sense of empathy.
The Boston-based nonprofit Schwartz Center for Compassionate Healthcare facilitates Schwartz Rounds, which are now held at about 600 health care organizations around the world. That number includes the 10 VA medical centers, mostly in the Northeast (Massachusetts, New York, Connecticut, and New Hampshire) but also in California, Illinois, and Minnesota.
Site teams work with the Schwartz Center to plan the rounds and gather data about their effectiveness. “Unlike traditional clinical or ethics rounds, this is not a didactic or problem-solving session. The focus is not on what happened, but how those who were involved felt. In other words, the human dimension of medicine,” Dr. Perry said. “There are no right or wrong answers. Everything that is said during short rounds is confidential. We do encourage people to continue discussion of the general themes afterward but not to share any specifics of what was discussed.”
At VACHS, Schwartz rounds began shortly before the COVID-19 pandemic, Perry said, and they’ve been held virtually since the first meeting. “Schwartz Rounds are open to all employees, trainees, and students at the institution. Anyone with a VA badge is welcome to attend,” he said. “We're averaging about 150 attendees per session.”
Speakers have addressed social/emotional topics, including delivering bad news to patients, maintaining compassion during adversity, and providing compassionate care to patients with substance use disorders.
The VACHS survey of Schwartz Rounds participants had a 50% response rate, with about 400 people responding to each question. Nearly all (98%) said they planned to attend the rounds again, and 55% agreed that a specific discussion “suggests that changes may be needed in departmental or institutional policies or practices.”
The administration has agreed to continue the Schwartz Rounds in light of the positive results, Perry said. As he noted, the Schwartz Center charges dues and initiation fees. The Marjorie Stanzler Financial Aid Fund underwrites the initiation fees for qualifying organizations, including VA facilities.
As for lessons, he said the topics of Schwartz Rounds “should be emotionally resonant. They should involve multiple disciplines and perspectives. They should illuminate an issue or experience that is not often discussed. And should inspire participants to share their own experiences and highlight instances of compassionate care—or barriers to providing compassionate care.”
Dr. Perry has no disclosures.
SAN DIEGO—From coast to coast, 10 US Department of Veterans Affairs (VA) medical centers are holding meetings designed to help clinicians and colleagues talk openly about touchy workplace topics, such as compassion, burnout, and medical errors. New data suggests that “Schwartz Rounds” have tremendous power to change how medical professionals cope, communicate, and commiserate.
At the VA Connecticut Healthcare System (VACHS), nearly all (98%) respondents who took part in Schwartz Round sessions rated them as either good or excellent, 89% reported feeling less isolated in their work with patients, 98% had new insights into the perspectives and experiences of colleagues, and 93% felt more open to communicating with colleagues, reported oncologist Edward Perry, MD, of VA Connecticut and Yale University School of Medicine, in a presentation here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) held September 16 to 18, 2022.
Schwartz Rounds have been around for 25 years and are named after the late Ken Schwartz, a 40-year-old Boston health care attorney who wrote movingly in 1995 about the “exquisite compassion” he experienced while being treated for advanced lung cancer—and the risk that the rapidly evolving health care system would lose its sense of empathy.
The Boston-based nonprofit Schwartz Center for Compassionate Healthcare facilitates Schwartz Rounds, which are now held at about 600 health care organizations around the world. That number includes the 10 VA medical centers, mostly in the Northeast (Massachusetts, New York, Connecticut, and New Hampshire) but also in California, Illinois, and Minnesota.
Site teams work with the Schwartz Center to plan the rounds and gather data about their effectiveness. “Unlike traditional clinical or ethics rounds, this is not a didactic or problem-solving session. The focus is not on what happened, but how those who were involved felt. In other words, the human dimension of medicine,” Dr. Perry said. “There are no right or wrong answers. Everything that is said during short rounds is confidential. We do encourage people to continue discussion of the general themes afterward but not to share any specifics of what was discussed.”
At VACHS, Schwartz rounds began shortly before the COVID-19 pandemic, Perry said, and they’ve been held virtually since the first meeting. “Schwartz Rounds are open to all employees, trainees, and students at the institution. Anyone with a VA badge is welcome to attend,” he said. “We're averaging about 150 attendees per session.”
Speakers have addressed social/emotional topics, including delivering bad news to patients, maintaining compassion during adversity, and providing compassionate care to patients with substance use disorders.
The VACHS survey of Schwartz Rounds participants had a 50% response rate, with about 400 people responding to each question. Nearly all (98%) said they planned to attend the rounds again, and 55% agreed that a specific discussion “suggests that changes may be needed in departmental or institutional policies or practices.”
The administration has agreed to continue the Schwartz Rounds in light of the positive results, Perry said. As he noted, the Schwartz Center charges dues and initiation fees. The Marjorie Stanzler Financial Aid Fund underwrites the initiation fees for qualifying organizations, including VA facilities.
As for lessons, he said the topics of Schwartz Rounds “should be emotionally resonant. They should involve multiple disciplines and perspectives. They should illuminate an issue or experience that is not often discussed. And should inspire participants to share their own experiences and highlight instances of compassionate care—or barriers to providing compassionate care.”
Dr. Perry has no disclosures.
AI tool may improve prediction of colorectal cancer recurrence
Using artificial intelligence, researchers have developed an algorithm that can help improve the prediction of colorectal cancer (CRC) recurrence.
The QuantCRC algorithm can identify patients with CRC who might be able to skip chemotherapy, given a low probability of recurrence, and identify those patients at high risk for recurrence who may benefit from more intensive treatment or follow-up, the researchers say.
“For patients with colon cancer, the algorithm gives oncologists another tool to help guide therapy and follow-up,” Rish Pai, MD, PhD, a pathologist at Mayo Clinic, Phoenix, who developed the tool, said in a news release.
The study was published online in the journal Gastroenterology.
The tool is a deep-learning segmentation algorithm developed using 6,468 digitized CRC images. It quantifies 15 features from a CRC image and uses them to improve prediction of recurrence.
“QuantCRC can identify different regions within the tumor and extract quantitative data from these regions,” Dr. Pai explained.
“The algorithm converts an image into a set of numbers that is unique to that tumor. The large number of tumors that we analyzed allowed us to learn which features were most predictive of tumor behavior. We can now apply what we have learned to new colon cancers to predict how the tumor will behave,” Dr. Pai said.
The researchers developed a prognostic model incorporating stage, mismatch repair, and QuantCRC that resulted in a concordance (c)-index of 0.714 in the internal test and 0.744 in the external cohort. Removing QuantCRC from the model reduced the c-index to 0.679 in the external cohort.
Using QuantCRC, they identified prognostic risk groups for recurrence, which provided a hazard ratio of 2.24 for low- versus high-risk stage III CRC and 2.36 for low- versus high-risk stage II CRC, in the external cohort after adjusting for established risk factors.
The predicted median 36-month recurrence rate for high-risk stage III CRC was 32.7% versus 13.4% for low-risk stage III CRC and 15.8% for high-risk stage II CRC versus 5.4% for low-risk stage II CRC, the researchers report.
QuantCRC provides a “powerful adjunct” to routine pathologic reporting of CRC, and a prognostic model using QuantCRC can improve prediction of recurrence-free survival, they write.
Looking ahead, Dr. Pai plans to use QuantCRC to better understand mechanisms of tumor recurrence and see if it can predict the response to certain treatments, like immunotherapy, he said.
Funding for this study was provided in part by the Colon Cancer Family Registry, which is supported in part by funding from the National Cancer Institute and National Institutes of Health. Dr. Pai reports consulting income from Alimentiv, Eli Lilly, AbbVie, Allergan, Genentech, and PathAI outside of the submitted work.
A version of this article first appeared on Medscape.com.
Using artificial intelligence, researchers have developed an algorithm that can help improve the prediction of colorectal cancer (CRC) recurrence.
The QuantCRC algorithm can identify patients with CRC who might be able to skip chemotherapy, given a low probability of recurrence, and identify those patients at high risk for recurrence who may benefit from more intensive treatment or follow-up, the researchers say.
“For patients with colon cancer, the algorithm gives oncologists another tool to help guide therapy and follow-up,” Rish Pai, MD, PhD, a pathologist at Mayo Clinic, Phoenix, who developed the tool, said in a news release.
The study was published online in the journal Gastroenterology.
The tool is a deep-learning segmentation algorithm developed using 6,468 digitized CRC images. It quantifies 15 features from a CRC image and uses them to improve prediction of recurrence.
“QuantCRC can identify different regions within the tumor and extract quantitative data from these regions,” Dr. Pai explained.
“The algorithm converts an image into a set of numbers that is unique to that tumor. The large number of tumors that we analyzed allowed us to learn which features were most predictive of tumor behavior. We can now apply what we have learned to new colon cancers to predict how the tumor will behave,” Dr. Pai said.
The researchers developed a prognostic model incorporating stage, mismatch repair, and QuantCRC that resulted in a concordance (c)-index of 0.714 in the internal test and 0.744 in the external cohort. Removing QuantCRC from the model reduced the c-index to 0.679 in the external cohort.
Using QuantCRC, they identified prognostic risk groups for recurrence, which provided a hazard ratio of 2.24 for low- versus high-risk stage III CRC and 2.36 for low- versus high-risk stage II CRC, in the external cohort after adjusting for established risk factors.
The predicted median 36-month recurrence rate for high-risk stage III CRC was 32.7% versus 13.4% for low-risk stage III CRC and 15.8% for high-risk stage II CRC versus 5.4% for low-risk stage II CRC, the researchers report.
QuantCRC provides a “powerful adjunct” to routine pathologic reporting of CRC, and a prognostic model using QuantCRC can improve prediction of recurrence-free survival, they write.
Looking ahead, Dr. Pai plans to use QuantCRC to better understand mechanisms of tumor recurrence and see if it can predict the response to certain treatments, like immunotherapy, he said.
Funding for this study was provided in part by the Colon Cancer Family Registry, which is supported in part by funding from the National Cancer Institute and National Institutes of Health. Dr. Pai reports consulting income from Alimentiv, Eli Lilly, AbbVie, Allergan, Genentech, and PathAI outside of the submitted work.
A version of this article first appeared on Medscape.com.
Using artificial intelligence, researchers have developed an algorithm that can help improve the prediction of colorectal cancer (CRC) recurrence.
The QuantCRC algorithm can identify patients with CRC who might be able to skip chemotherapy, given a low probability of recurrence, and identify those patients at high risk for recurrence who may benefit from more intensive treatment or follow-up, the researchers say.
“For patients with colon cancer, the algorithm gives oncologists another tool to help guide therapy and follow-up,” Rish Pai, MD, PhD, a pathologist at Mayo Clinic, Phoenix, who developed the tool, said in a news release.
The study was published online in the journal Gastroenterology.
The tool is a deep-learning segmentation algorithm developed using 6,468 digitized CRC images. It quantifies 15 features from a CRC image and uses them to improve prediction of recurrence.
“QuantCRC can identify different regions within the tumor and extract quantitative data from these regions,” Dr. Pai explained.
“The algorithm converts an image into a set of numbers that is unique to that tumor. The large number of tumors that we analyzed allowed us to learn which features were most predictive of tumor behavior. We can now apply what we have learned to new colon cancers to predict how the tumor will behave,” Dr. Pai said.
The researchers developed a prognostic model incorporating stage, mismatch repair, and QuantCRC that resulted in a concordance (c)-index of 0.714 in the internal test and 0.744 in the external cohort. Removing QuantCRC from the model reduced the c-index to 0.679 in the external cohort.
Using QuantCRC, they identified prognostic risk groups for recurrence, which provided a hazard ratio of 2.24 for low- versus high-risk stage III CRC and 2.36 for low- versus high-risk stage II CRC, in the external cohort after adjusting for established risk factors.
The predicted median 36-month recurrence rate for high-risk stage III CRC was 32.7% versus 13.4% for low-risk stage III CRC and 15.8% for high-risk stage II CRC versus 5.4% for low-risk stage II CRC, the researchers report.
QuantCRC provides a “powerful adjunct” to routine pathologic reporting of CRC, and a prognostic model using QuantCRC can improve prediction of recurrence-free survival, they write.
Looking ahead, Dr. Pai plans to use QuantCRC to better understand mechanisms of tumor recurrence and see if it can predict the response to certain treatments, like immunotherapy, he said.
Funding for this study was provided in part by the Colon Cancer Family Registry, which is supported in part by funding from the National Cancer Institute and National Institutes of Health. Dr. Pai reports consulting income from Alimentiv, Eli Lilly, AbbVie, Allergan, Genentech, and PathAI outside of the submitted work.
A version of this article first appeared on Medscape.com.
FROM GASTROENTEROLOGY
Novel blood test for early-stage liver cancer shows promise
, increasing the likelihood of potentially curative therapy and improved patient prognosis.
HCC accounts for the majority of primary liver cancers and mainly occurs in patients with cirrhosis or chronic hepatitis B virus infection. The prognosis of HCC is poor, largely owing to advanced disease stage at diagnosis.
The current guidelines recommend surveillance with twice-yearly liver ultrasound, with or without serum alpha-fetoprotein, for patients at risk for HCC, although the diagnostic performance is suboptimal.
The new “liquid biopsy” uses HCC-associated extracellular vesicles (EVs) to establish an HCC EV ECG score for distinguishing patients with early-stage HCC from at-risk controls with cirrhosis from a 400-mcL plasma sample.
“We’re the first team looking at extracellular vesicles as a detection biomarker for early-stage liver cancer, and our study showed it had outstanding performance,” study investigator Ju Dong Yang, MD, with Cedars-Sinai Medical Center, Los Angeles, said in a news release.
The study was published online in Hepatology.
In a phase 2 biomarker (case-control) study, the investigators tested their blood test in a training cohort of 106 individuals (45 patients with treatment-naive early-stage HCC and 61 with cirrhosis) and an independent validation cohort with 72 participants (35 patients with treatment-naive early-stage HCC and 37 with cirrhosis).
The HCC EV ECG score had “excellent accuracy” for discriminating between HCC and cirrhosis, with an area under the receiver operating characteristic curve (AUROC) of 0.95 and 0.93 in the training and validation cohorts, respectively, they report.
The diagnostic performance “remained excellent” among the subpopulations of HCC etiology and those with tumors within the Milan criteria.
Adding the serum alpha-fetoprotein level to the HCC EV ECG score did not improve its performance.
The researchers say that further validation of the blood test in a larger phase 2 study and a subsequent phase 3 study are needed to confirm its utility in clinical settings.
“We are planning on doing larger-scale studies to further validate this test and bring it into routine clinical practice here – and globally,” Dr. Yang said.
“In addition to its excellent performance, this marker has the advantages of being user friendly, cost efficient, and having a fast turnaround time – within 6 hours from sample collection to result,” Dan Theodorescu, MD, PhD, director of Cedars-Sinai Cancer, who is not an author on the study, said in the news release.
“Once this marker has been validated in subsequent studies, it can be easily adopted by existing PCR [polymerase chain reaction] facilities,” Dr. Theodorescu added.
The study was supported by an American College of Gastroenterology Junior Faculty Development Award, a Department of Defense Peer Reviewed Cancer Research Program Career Development Award, and the National Institutes of Health. Dr. Yang provides a consulting service for Exact Sciences, Gilead Sciences, and Eisai. Dr. Theodorescu reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, increasing the likelihood of potentially curative therapy and improved patient prognosis.
HCC accounts for the majority of primary liver cancers and mainly occurs in patients with cirrhosis or chronic hepatitis B virus infection. The prognosis of HCC is poor, largely owing to advanced disease stage at diagnosis.
The current guidelines recommend surveillance with twice-yearly liver ultrasound, with or without serum alpha-fetoprotein, for patients at risk for HCC, although the diagnostic performance is suboptimal.
The new “liquid biopsy” uses HCC-associated extracellular vesicles (EVs) to establish an HCC EV ECG score for distinguishing patients with early-stage HCC from at-risk controls with cirrhosis from a 400-mcL plasma sample.
“We’re the first team looking at extracellular vesicles as a detection biomarker for early-stage liver cancer, and our study showed it had outstanding performance,” study investigator Ju Dong Yang, MD, with Cedars-Sinai Medical Center, Los Angeles, said in a news release.
The study was published online in Hepatology.
In a phase 2 biomarker (case-control) study, the investigators tested their blood test in a training cohort of 106 individuals (45 patients with treatment-naive early-stage HCC and 61 with cirrhosis) and an independent validation cohort with 72 participants (35 patients with treatment-naive early-stage HCC and 37 with cirrhosis).
The HCC EV ECG score had “excellent accuracy” for discriminating between HCC and cirrhosis, with an area under the receiver operating characteristic curve (AUROC) of 0.95 and 0.93 in the training and validation cohorts, respectively, they report.
The diagnostic performance “remained excellent” among the subpopulations of HCC etiology and those with tumors within the Milan criteria.
Adding the serum alpha-fetoprotein level to the HCC EV ECG score did not improve its performance.
The researchers say that further validation of the blood test in a larger phase 2 study and a subsequent phase 3 study are needed to confirm its utility in clinical settings.
“We are planning on doing larger-scale studies to further validate this test and bring it into routine clinical practice here – and globally,” Dr. Yang said.
“In addition to its excellent performance, this marker has the advantages of being user friendly, cost efficient, and having a fast turnaround time – within 6 hours from sample collection to result,” Dan Theodorescu, MD, PhD, director of Cedars-Sinai Cancer, who is not an author on the study, said in the news release.
“Once this marker has been validated in subsequent studies, it can be easily adopted by existing PCR [polymerase chain reaction] facilities,” Dr. Theodorescu added.
The study was supported by an American College of Gastroenterology Junior Faculty Development Award, a Department of Defense Peer Reviewed Cancer Research Program Career Development Award, and the National Institutes of Health. Dr. Yang provides a consulting service for Exact Sciences, Gilead Sciences, and Eisai. Dr. Theodorescu reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, increasing the likelihood of potentially curative therapy and improved patient prognosis.
HCC accounts for the majority of primary liver cancers and mainly occurs in patients with cirrhosis or chronic hepatitis B virus infection. The prognosis of HCC is poor, largely owing to advanced disease stage at diagnosis.
The current guidelines recommend surveillance with twice-yearly liver ultrasound, with or without serum alpha-fetoprotein, for patients at risk for HCC, although the diagnostic performance is suboptimal.
The new “liquid biopsy” uses HCC-associated extracellular vesicles (EVs) to establish an HCC EV ECG score for distinguishing patients with early-stage HCC from at-risk controls with cirrhosis from a 400-mcL plasma sample.
“We’re the first team looking at extracellular vesicles as a detection biomarker for early-stage liver cancer, and our study showed it had outstanding performance,” study investigator Ju Dong Yang, MD, with Cedars-Sinai Medical Center, Los Angeles, said in a news release.
The study was published online in Hepatology.
In a phase 2 biomarker (case-control) study, the investigators tested their blood test in a training cohort of 106 individuals (45 patients with treatment-naive early-stage HCC and 61 with cirrhosis) and an independent validation cohort with 72 participants (35 patients with treatment-naive early-stage HCC and 37 with cirrhosis).
The HCC EV ECG score had “excellent accuracy” for discriminating between HCC and cirrhosis, with an area under the receiver operating characteristic curve (AUROC) of 0.95 and 0.93 in the training and validation cohorts, respectively, they report.
The diagnostic performance “remained excellent” among the subpopulations of HCC etiology and those with tumors within the Milan criteria.
Adding the serum alpha-fetoprotein level to the HCC EV ECG score did not improve its performance.
The researchers say that further validation of the blood test in a larger phase 2 study and a subsequent phase 3 study are needed to confirm its utility in clinical settings.
“We are planning on doing larger-scale studies to further validate this test and bring it into routine clinical practice here – and globally,” Dr. Yang said.
“In addition to its excellent performance, this marker has the advantages of being user friendly, cost efficient, and having a fast turnaround time – within 6 hours from sample collection to result,” Dan Theodorescu, MD, PhD, director of Cedars-Sinai Cancer, who is not an author on the study, said in the news release.
“Once this marker has been validated in subsequent studies, it can be easily adopted by existing PCR [polymerase chain reaction] facilities,” Dr. Theodorescu added.
The study was supported by an American College of Gastroenterology Junior Faculty Development Award, a Department of Defense Peer Reviewed Cancer Research Program Career Development Award, and the National Institutes of Health. Dr. Yang provides a consulting service for Exact Sciences, Gilead Sciences, and Eisai. Dr. Theodorescu reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HEPATOLOGY
VA Launches Virtual Tumor Board
SAN DIEGO – The US Department of Veterans Affairs (VA) TeleOncology program has rolled out a virtual tumor board that brings medical professionals together to offer insight and guidance about challenging hematology cases. Over the past 6 months the board has held 10 sessions and reviewed about 20 cases. A small survey found that participants think the meetings are beneficial.
“Virtual tumor boards help to connect experts across the country to leverage the expertise within the VA,” he-matologist/oncologist Thomas Rodgers, MD, of the Duke Cancer Institute and Durham Veterans Affairs Medical Center, told Federal Practitioner in an interview. He is the lead author of a poster about the program that was pre-sented here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO).
As Dr. Rodgers noted, tumor boards are already in place at some VA centers. However, “they are not available at every VA and often are not set up to cover every cancer type.”
The VA National TeleOncology program created the virtual tumor board program as part of its mission to ex-tend hematology/oncology services across the system. “Cancer care has become increasingly complex. Beyond ad-vancing therapeutics, patient care often involves multiple specialties and medical disciplines,” Dr. Rodgers said. “A tumor board offers a forum for these specialists to communicate with each other in real time, not only to help estab-lish the correct diagnosis and stage of cancer but also to form a consensus on the most fitting treatment option. Think of it as getting all of the people involved in a person’s care in the same room.”
Currently, he said, the virtual tumor boards cover patients with malignant hematology diagnoses such as leuke-mia, multiple myeloma, and lymphomas. “We welcome submissions. If a provider is interested in submitting a case, they can email us and will be provided with a short intake form. Once submitted, we will collect necessary imaging and pathology for review. The provider will then present the patient case on the day of the tumor board.”
Typically, more than 30 medical professionals participate in the virtual tumor boards, Dr. Rodgers said, repre-senting medical oncology/hematology, pathology, radiology, palliative care, pharmacy, social work, and die-tary/nutrition.
According to the poster presented at AVAHO, 9 participants responded to a survey after 4 tumor board sessions. All found the boards to be beneficial or somewhat beneficial, and 55% reported that they were “highly applicable” to their practice.
Pathologist Claudio A. Mosse, MD, PhD, of Vanderbilt University Medical Center and VA Tennessee Valley Healthcare System, praised the virtual tumor board program. “It’s been incredibly useful from my end as a pathologist as it shows me which diagnoses are most challenging for my colleagues,” Dr. Mosse said in an inter-view. “Reviewing and then presenting these challenging cases forces me to go into the published literature to come to a unitary diagnosis based on the patient history, radiology, various laboratory tests, and the biopsy I was asked to review.”
He added that “as a pathologist, I learn so much from the hematologists as they discuss the possible therapeutic options, and that strengthens my ability as a pathologist because I have to understand how one diagnosis versus an-other affects their therapeutic decision tree.”
What’s next for the virtual tumor board program? The next step is to expand to solid tumors, said VA Pittsburgh Healthcare System hematologist/oncologist Vida Almario Passero, MD, MBA, chief medical officer of National TeleOncology, in an interview.
No disclosures were reported.
SAN DIEGO – The US Department of Veterans Affairs (VA) TeleOncology program has rolled out a virtual tumor board that brings medical professionals together to offer insight and guidance about challenging hematology cases. Over the past 6 months the board has held 10 sessions and reviewed about 20 cases. A small survey found that participants think the meetings are beneficial.
“Virtual tumor boards help to connect experts across the country to leverage the expertise within the VA,” he-matologist/oncologist Thomas Rodgers, MD, of the Duke Cancer Institute and Durham Veterans Affairs Medical Center, told Federal Practitioner in an interview. He is the lead author of a poster about the program that was pre-sented here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO).
As Dr. Rodgers noted, tumor boards are already in place at some VA centers. However, “they are not available at every VA and often are not set up to cover every cancer type.”
The VA National TeleOncology program created the virtual tumor board program as part of its mission to ex-tend hematology/oncology services across the system. “Cancer care has become increasingly complex. Beyond ad-vancing therapeutics, patient care often involves multiple specialties and medical disciplines,” Dr. Rodgers said. “A tumor board offers a forum for these specialists to communicate with each other in real time, not only to help estab-lish the correct diagnosis and stage of cancer but also to form a consensus on the most fitting treatment option. Think of it as getting all of the people involved in a person’s care in the same room.”
Currently, he said, the virtual tumor boards cover patients with malignant hematology diagnoses such as leuke-mia, multiple myeloma, and lymphomas. “We welcome submissions. If a provider is interested in submitting a case, they can email us and will be provided with a short intake form. Once submitted, we will collect necessary imaging and pathology for review. The provider will then present the patient case on the day of the tumor board.”
Typically, more than 30 medical professionals participate in the virtual tumor boards, Dr. Rodgers said, repre-senting medical oncology/hematology, pathology, radiology, palliative care, pharmacy, social work, and die-tary/nutrition.
According to the poster presented at AVAHO, 9 participants responded to a survey after 4 tumor board sessions. All found the boards to be beneficial or somewhat beneficial, and 55% reported that they were “highly applicable” to their practice.
Pathologist Claudio A. Mosse, MD, PhD, of Vanderbilt University Medical Center and VA Tennessee Valley Healthcare System, praised the virtual tumor board program. “It’s been incredibly useful from my end as a pathologist as it shows me which diagnoses are most challenging for my colleagues,” Dr. Mosse said in an inter-view. “Reviewing and then presenting these challenging cases forces me to go into the published literature to come to a unitary diagnosis based on the patient history, radiology, various laboratory tests, and the biopsy I was asked to review.”
He added that “as a pathologist, I learn so much from the hematologists as they discuss the possible therapeutic options, and that strengthens my ability as a pathologist because I have to understand how one diagnosis versus an-other affects their therapeutic decision tree.”
What’s next for the virtual tumor board program? The next step is to expand to solid tumors, said VA Pittsburgh Healthcare System hematologist/oncologist Vida Almario Passero, MD, MBA, chief medical officer of National TeleOncology, in an interview.
No disclosures were reported.
SAN DIEGO – The US Department of Veterans Affairs (VA) TeleOncology program has rolled out a virtual tumor board that brings medical professionals together to offer insight and guidance about challenging hematology cases. Over the past 6 months the board has held 10 sessions and reviewed about 20 cases. A small survey found that participants think the meetings are beneficial.
“Virtual tumor boards help to connect experts across the country to leverage the expertise within the VA,” he-matologist/oncologist Thomas Rodgers, MD, of the Duke Cancer Institute and Durham Veterans Affairs Medical Center, told Federal Practitioner in an interview. He is the lead author of a poster about the program that was pre-sented here at the annual meeting of the Association of VA Hematology/Oncology (AVAHO).
As Dr. Rodgers noted, tumor boards are already in place at some VA centers. However, “they are not available at every VA and often are not set up to cover every cancer type.”
The VA National TeleOncology program created the virtual tumor board program as part of its mission to ex-tend hematology/oncology services across the system. “Cancer care has become increasingly complex. Beyond ad-vancing therapeutics, patient care often involves multiple specialties and medical disciplines,” Dr. Rodgers said. “A tumor board offers a forum for these specialists to communicate with each other in real time, not only to help estab-lish the correct diagnosis and stage of cancer but also to form a consensus on the most fitting treatment option. Think of it as getting all of the people involved in a person’s care in the same room.”
Currently, he said, the virtual tumor boards cover patients with malignant hematology diagnoses such as leuke-mia, multiple myeloma, and lymphomas. “We welcome submissions. If a provider is interested in submitting a case, they can email us and will be provided with a short intake form. Once submitted, we will collect necessary imaging and pathology for review. The provider will then present the patient case on the day of the tumor board.”
Typically, more than 30 medical professionals participate in the virtual tumor boards, Dr. Rodgers said, repre-senting medical oncology/hematology, pathology, radiology, palliative care, pharmacy, social work, and die-tary/nutrition.
According to the poster presented at AVAHO, 9 participants responded to a survey after 4 tumor board sessions. All found the boards to be beneficial or somewhat beneficial, and 55% reported that they were “highly applicable” to their practice.
Pathologist Claudio A. Mosse, MD, PhD, of Vanderbilt University Medical Center and VA Tennessee Valley Healthcare System, praised the virtual tumor board program. “It’s been incredibly useful from my end as a pathologist as it shows me which diagnoses are most challenging for my colleagues,” Dr. Mosse said in an inter-view. “Reviewing and then presenting these challenging cases forces me to go into the published literature to come to a unitary diagnosis based on the patient history, radiology, various laboratory tests, and the biopsy I was asked to review.”
He added that “as a pathologist, I learn so much from the hematologists as they discuss the possible therapeutic options, and that strengthens my ability as a pathologist because I have to understand how one diagnosis versus an-other affects their therapeutic decision tree.”
What’s next for the virtual tumor board program? The next step is to expand to solid tumors, said VA Pittsburgh Healthcare System hematologist/oncologist Vida Almario Passero, MD, MBA, chief medical officer of National TeleOncology, in an interview.
No disclosures were reported.
Implementation of a Bone Marrow Biopsy Clinic: Effect on Wait Times for the Procedure, Diagnosis and Treatment Initiation
Clinical Situation
Bone marrow biopsies often need to be performed expeditiously in order to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization there are fewer hematology/oncology providers available to perform this procedure.
Literature
Our VA previously addressed this issue by having all bone marrow biopsies performed through Interventional Radiology (IR). The average time from order to procedure, though, was 18.6 days (Arfons LM, AVAHO 2016).
Intervention
A weekly bone marrow biopsy clinic was formed, utilizing a small group (heme/onc physician, nurse practitioner and key nursing staff). In collaboration with pathology, interior design, pharmacy, facilities and environmental services, a standard operating procedure was developed, which included a staffing model, procedural checklist, documentation template, scheduling and ordering system.
Outcomes/Implications
Bone marrow biopsies performed before and after initiation of the bone marrow biopsy clinic were tracked for time from order placement to: procedure being done; diagnosis rendered; and for those whose biopsy result needed therapy, initiation of treatment. From 8/4/2020 to 8/12/2021 there were 140 bone marrow biopsies performed, all through IR. The average time from order to the procedure was 23.1 days; from order to diagnosis was 27.8 days and from order to treatment was 54.8 days. After implementation of the bone marrow biopsy clinic, from 9/8/2021 to 5/25/2022 there have been 61 bone marrow biopsies performed (those ordered through IR were excluded). The average time from order to the procedure was 6.8 days; from order to diagnosis was 11.4 days and from order to treatment was 27.3 days. The differences in the average wait times for all 3 measures (time to procedure, diagnosis and treatment) were highly statistically significant (P < .001 for each), in favor of shorter wait times for those performed in the bone marrow clinic as compared to those done through IR. Implementation of a dedicated weekly bone marrow biopsy clinic significantly reduced wait times for the procedure, diagnosis and treatment initiation. This should be considered at other VA centers to improve the care of our veterans.
Clinical Situation
Bone marrow biopsies often need to be performed expeditiously in order to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization there are fewer hematology/oncology providers available to perform this procedure.
Literature
Our VA previously addressed this issue by having all bone marrow biopsies performed through Interventional Radiology (IR). The average time from order to procedure, though, was 18.6 days (Arfons LM, AVAHO 2016).
Intervention
A weekly bone marrow biopsy clinic was formed, utilizing a small group (heme/onc physician, nurse practitioner and key nursing staff). In collaboration with pathology, interior design, pharmacy, facilities and environmental services, a standard operating procedure was developed, which included a staffing model, procedural checklist, documentation template, scheduling and ordering system.
Outcomes/Implications
Bone marrow biopsies performed before and after initiation of the bone marrow biopsy clinic were tracked for time from order placement to: procedure being done; diagnosis rendered; and for those whose biopsy result needed therapy, initiation of treatment. From 8/4/2020 to 8/12/2021 there were 140 bone marrow biopsies performed, all through IR. The average time from order to the procedure was 23.1 days; from order to diagnosis was 27.8 days and from order to treatment was 54.8 days. After implementation of the bone marrow biopsy clinic, from 9/8/2021 to 5/25/2022 there have been 61 bone marrow biopsies performed (those ordered through IR were excluded). The average time from order to the procedure was 6.8 days; from order to diagnosis was 11.4 days and from order to treatment was 27.3 days. The differences in the average wait times for all 3 measures (time to procedure, diagnosis and treatment) were highly statistically significant (P < .001 for each), in favor of shorter wait times for those performed in the bone marrow clinic as compared to those done through IR. Implementation of a dedicated weekly bone marrow biopsy clinic significantly reduced wait times for the procedure, diagnosis and treatment initiation. This should be considered at other VA centers to improve the care of our veterans.
Clinical Situation
Bone marrow biopsies often need to be performed expeditiously in order to alleviate patient concerns and quickly determine a diagnosis and treatment plan. However, with increasing subspecialization there are fewer hematology/oncology providers available to perform this procedure.
Literature
Our VA previously addressed this issue by having all bone marrow biopsies performed through Interventional Radiology (IR). The average time from order to procedure, though, was 18.6 days (Arfons LM, AVAHO 2016).
Intervention
A weekly bone marrow biopsy clinic was formed, utilizing a small group (heme/onc physician, nurse practitioner and key nursing staff). In collaboration with pathology, interior design, pharmacy, facilities and environmental services, a standard operating procedure was developed, which included a staffing model, procedural checklist, documentation template, scheduling and ordering system.
Outcomes/Implications
Bone marrow biopsies performed before and after initiation of the bone marrow biopsy clinic were tracked for time from order placement to: procedure being done; diagnosis rendered; and for those whose biopsy result needed therapy, initiation of treatment. From 8/4/2020 to 8/12/2021 there were 140 bone marrow biopsies performed, all through IR. The average time from order to the procedure was 23.1 days; from order to diagnosis was 27.8 days and from order to treatment was 54.8 days. After implementation of the bone marrow biopsy clinic, from 9/8/2021 to 5/25/2022 there have been 61 bone marrow biopsies performed (those ordered through IR were excluded). The average time from order to the procedure was 6.8 days; from order to diagnosis was 11.4 days and from order to treatment was 27.3 days. The differences in the average wait times for all 3 measures (time to procedure, diagnosis and treatment) were highly statistically significant (P < .001 for each), in favor of shorter wait times for those performed in the bone marrow clinic as compared to those done through IR. Implementation of a dedicated weekly bone marrow biopsy clinic significantly reduced wait times for the procedure, diagnosis and treatment initiation. This should be considered at other VA centers to improve the care of our veterans.
NP-Led Suspicion of Cancer Clinic Improves Timeliness of Care for Veterans
Clinical Situation
Delays in diagnosis affect outcomes in veterans with cancer. Veterans sent into the community for suspected cancer frequently experience delays in diagnosis and treatment. This is further complicated by inappropriate workup, resulting in additional delays. Retaining veterans within the VA system for care and providing guidance to primary care providers (PCPs) to assist with expedited workup was an identified need. The Suspicion of Cancer Clinic (SOCC) was developed to address barriers to timely cancer diagnosis and care.
Literature
Researched private sector models of rapid cancer diagnostic and suspicion clinics. Literature analyzed showed improved outcomes through reduction of diagnostic delay. Nurse practitioner (NP)-led clinics were determined to be effective in expediting diagnosis and reducing cancer care delays.
Intervention
The Suspicion of Cancer Clinic is a tele-clinic, staffed with a NP. Diagnostic consult for the NP to assume the workup upon discovery of high suspicion of cancer, or via non-visit consult (NVC) to provide diagnostic guidance are available to PCPs. Outreach and education were performed prior initial clinic launch and post-launch, when need for further clarification of role and scope of the clinic was identified, based on consult trends.
Outcomes/Implications
The SOCC received 133 consults between 9/1/2021 and 6/6/2022 for veterans ranging age 29-94 years. Of these consults, 25 were expedited, diagnostic workups, 47 were NVCs, eliminating unnecessary or incomplete workups, yielding 23 veterans diagnosed with one of 8 types cancer. An additional 34 consults were forwarded to other appropriate service, and 27 were not appropriate for clinic and cancelled. Further outreach and education resulted in a 55% decrease in inappropriate consults. The NP retained 10 veterans (50%) within the VA for diagnostics, who had planned to receive community workup, which is an average four-week delay to schedule in the community. The SOCC was developed utilizing existing staff. The tele-clinic relieves workspace burden. Veterans received timely and appropriate cancer workups, reducing diagnostic delays. PCPs received additional support and guidance. Veterans retained within the VA system is more cost-effective and avoids community care delays. NP-led suspicion/rapid diagnostic clinic effectively reduced care delays by immediate initiation of further diagnostics and appropriate utilization of resources.
References
Campbell C, Nowell A, Karagheusian K, Giroux J, Kiteley C, Martelli L, McQuestion M, Quinn M, Rowe Samadhin YP, Touw M, Moody L. Practical innovation: Advanced practice nurses in cancer care. Can Oncol Nurs J. 2020 Jan 1;30(1):9-15. doi:10.5737/23688076301915. PMID: 33119001; PMCID: PMC7585714.
Drudge-Coates L, Khati V, Ballesteros R, Martyn-Hemphill C, Brown C, Green J, Challacombe B, Muir G. A nurse practitioner model for the assessment of suspected prostate cancer referrals is safe, cost and time efficient. Ecancermedicalscience. 2019 Dec 18;13:994. doi:10.3332/ecancer.2019.994. PMID: 32010218; PMCID: PMC6974368.
Nixon S, Bezverbnaya K, Maganti M, Gullane P, Reedijk M, Kuruvilla J, Prica A, Kridel R, Kukreti V, Bennett S, Rogalla P, Delabie J, Pintilie M, Crump M. Evaluation of Lymphadenopathy and Suspected Lymphoma in a Lymphoma Rapid Diagnosis Clinic. JCO Oncol Pract. 2020 Jan;16(1):e29-e36. doi:10.1200/JOP.19.00202. Epub 2019 Oct 1. PMID: 31573831.
Vasilakis C, Forte P. Setting up a rapid diagnostic clinic for patients with vague symptoms of cancer: a mixed method process evaluation study. BMC Health Serv Res. 2021 Apr 17;21(1):357. doi: 10.1186/s12913-021-06360-0. PMID: 33865373; PMCID: PMC8052708.
Clinical Situation
Delays in diagnosis affect outcomes in veterans with cancer. Veterans sent into the community for suspected cancer frequently experience delays in diagnosis and treatment. This is further complicated by inappropriate workup, resulting in additional delays. Retaining veterans within the VA system for care and providing guidance to primary care providers (PCPs) to assist with expedited workup was an identified need. The Suspicion of Cancer Clinic (SOCC) was developed to address barriers to timely cancer diagnosis and care.
Literature
Researched private sector models of rapid cancer diagnostic and suspicion clinics. Literature analyzed showed improved outcomes through reduction of diagnostic delay. Nurse practitioner (NP)-led clinics were determined to be effective in expediting diagnosis and reducing cancer care delays.
Intervention
The Suspicion of Cancer Clinic is a tele-clinic, staffed with a NP. Diagnostic consult for the NP to assume the workup upon discovery of high suspicion of cancer, or via non-visit consult (NVC) to provide diagnostic guidance are available to PCPs. Outreach and education were performed prior initial clinic launch and post-launch, when need for further clarification of role and scope of the clinic was identified, based on consult trends.
Outcomes/Implications
The SOCC received 133 consults between 9/1/2021 and 6/6/2022 for veterans ranging age 29-94 years. Of these consults, 25 were expedited, diagnostic workups, 47 were NVCs, eliminating unnecessary or incomplete workups, yielding 23 veterans diagnosed with one of 8 types cancer. An additional 34 consults were forwarded to other appropriate service, and 27 were not appropriate for clinic and cancelled. Further outreach and education resulted in a 55% decrease in inappropriate consults. The NP retained 10 veterans (50%) within the VA for diagnostics, who had planned to receive community workup, which is an average four-week delay to schedule in the community. The SOCC was developed utilizing existing staff. The tele-clinic relieves workspace burden. Veterans received timely and appropriate cancer workups, reducing diagnostic delays. PCPs received additional support and guidance. Veterans retained within the VA system is more cost-effective and avoids community care delays. NP-led suspicion/rapid diagnostic clinic effectively reduced care delays by immediate initiation of further diagnostics and appropriate utilization of resources.
References
Campbell C, Nowell A, Karagheusian K, Giroux J, Kiteley C, Martelli L, McQuestion M, Quinn M, Rowe Samadhin YP, Touw M, Moody L. Practical innovation: Advanced practice nurses in cancer care. Can Oncol Nurs J. 2020 Jan 1;30(1):9-15. doi:10.5737/23688076301915. PMID: 33119001; PMCID: PMC7585714.
Drudge-Coates L, Khati V, Ballesteros R, Martyn-Hemphill C, Brown C, Green J, Challacombe B, Muir G. A nurse practitioner model for the assessment of suspected prostate cancer referrals is safe, cost and time efficient. Ecancermedicalscience. 2019 Dec 18;13:994. doi:10.3332/ecancer.2019.994. PMID: 32010218; PMCID: PMC6974368.
Nixon S, Bezverbnaya K, Maganti M, Gullane P, Reedijk M, Kuruvilla J, Prica A, Kridel R, Kukreti V, Bennett S, Rogalla P, Delabie J, Pintilie M, Crump M. Evaluation of Lymphadenopathy and Suspected Lymphoma in a Lymphoma Rapid Diagnosis Clinic. JCO Oncol Pract. 2020 Jan;16(1):e29-e36. doi:10.1200/JOP.19.00202. Epub 2019 Oct 1. PMID: 31573831.
Vasilakis C, Forte P. Setting up a rapid diagnostic clinic for patients with vague symptoms of cancer: a mixed method process evaluation study. BMC Health Serv Res. 2021 Apr 17;21(1):357. doi: 10.1186/s12913-021-06360-0. PMID: 33865373; PMCID: PMC8052708.
Clinical Situation
Delays in diagnosis affect outcomes in veterans with cancer. Veterans sent into the community for suspected cancer frequently experience delays in diagnosis and treatment. This is further complicated by inappropriate workup, resulting in additional delays. Retaining veterans within the VA system for care and providing guidance to primary care providers (PCPs) to assist with expedited workup was an identified need. The Suspicion of Cancer Clinic (SOCC) was developed to address barriers to timely cancer diagnosis and care.
Literature
Researched private sector models of rapid cancer diagnostic and suspicion clinics. Literature analyzed showed improved outcomes through reduction of diagnostic delay. Nurse practitioner (NP)-led clinics were determined to be effective in expediting diagnosis and reducing cancer care delays.
Intervention
The Suspicion of Cancer Clinic is a tele-clinic, staffed with a NP. Diagnostic consult for the NP to assume the workup upon discovery of high suspicion of cancer, or via non-visit consult (NVC) to provide diagnostic guidance are available to PCPs. Outreach and education were performed prior initial clinic launch and post-launch, when need for further clarification of role and scope of the clinic was identified, based on consult trends.
Outcomes/Implications
The SOCC received 133 consults between 9/1/2021 and 6/6/2022 for veterans ranging age 29-94 years. Of these consults, 25 were expedited, diagnostic workups, 47 were NVCs, eliminating unnecessary or incomplete workups, yielding 23 veterans diagnosed with one of 8 types cancer. An additional 34 consults were forwarded to other appropriate service, and 27 were not appropriate for clinic and cancelled. Further outreach and education resulted in a 55% decrease in inappropriate consults. The NP retained 10 veterans (50%) within the VA for diagnostics, who had planned to receive community workup, which is an average four-week delay to schedule in the community. The SOCC was developed utilizing existing staff. The tele-clinic relieves workspace burden. Veterans received timely and appropriate cancer workups, reducing diagnostic delays. PCPs received additional support and guidance. Veterans retained within the VA system is more cost-effective and avoids community care delays. NP-led suspicion/rapid diagnostic clinic effectively reduced care delays by immediate initiation of further diagnostics and appropriate utilization of resources.