User login
New antibiotics targeting MDR pathogens are expensive, but not impressive
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
The U.S. Food and Drug Administration has approved a number of new antibiotics targeting multidrug-resistant bacteria in the past 5 years, but the new drugs have not led to a substantial improvement in patient outcomes when compared with existing antibiotics, according to a recent analysis in the Annals of Internal Medicine.
The eight new antibiotics approved by the FDA between January 2010 and December 2015 were ceftaroline, fidaxomicin, bedaquiline, dalbavancin, tedizolid, oritavancin, ceftolozane/tazobactam, and ceftazidime/avibactam. Of those eight drugs, only three showed in vitro activity against the so-called ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumonia, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species). Only one drug, fidaxomicin, demonstrated in vitro activity against an urgent-threat pathogen from the Centers for Disease Control and Prevention, Clostridium difficile. Bedaquiline was the only new antibiotic specifically indicated for a disease from a multidrug-resistant pathogen, although the investigators said most of the drugs demonstrated in vitro activity against gram-positive drug-resistant pathogens.
Importantly, the authors noted that in vitro activity does not necessarily reflect benefits on actual patient clinical outcomes, as exemplified by such drugs as tigecycline and doripenem.
The researchers found what they called “important deficiencies in the clinical trials leading to approval of these new antibiotic products.” Most pivotal trial designs were primarily noninferiority trials, and the antibiotics were not studied to evaluate whether they have substantial benefits in efficacy over what is currently available, they noted. Additionally, none of the trials evaluated direct patient outcomes as primary end points, and some drugs did not have confirmatory evidence from a second independent trial or did not have any confirmatory trials.
Researchers also examined the prices of a single dose of the new antibiotics. The prices ranged from $1,195 to $4,183 (4-14 days of ceftolozane/tazobactam for acute pyelonephritis and intra-abdominal infections) to $69,702 (24 weeks of bedaquiline) – quite a premium for antibiotics showing unclear evidence of additional benefit.
“As antibiotic innovation continues to move forward, greater attention needs to be paid to incentives for developing high-quality new products with demonstrated superiority to existing products on outcomes in patients with multidrug-resistant disease, replacing the current focus on quantity and presumed future benefits,” researchers concluded.
Read the full study in the Annals of Internal Medicine (doi: 10.7326/M16-0291).
FROM ANNALS OF INTERNAL MEDICINE
Recurrent C. diff infection much more costly to treat
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
FROM THE JOURNAL OF HOSPITAL INFECTION
Key clinical point: The economic cost burden increased significantly for patients with recurrent C. difficile infections, compared with patients with primary CDI.
Major finding: Median hospital length of stay and costs attributable to C. difficile infections increased from 7 days and $13,168 for patients with primary CDI only, vs. 15 days and $28,218 for patients with recurrent CDI.
Data source: A prospective, observational cohort study of 540 hospitalized adult patients with primary CDI followed for 3 months to assess for recurrent CDI episodes.
Disclosures: The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
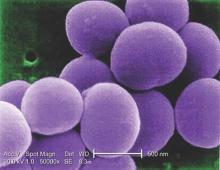
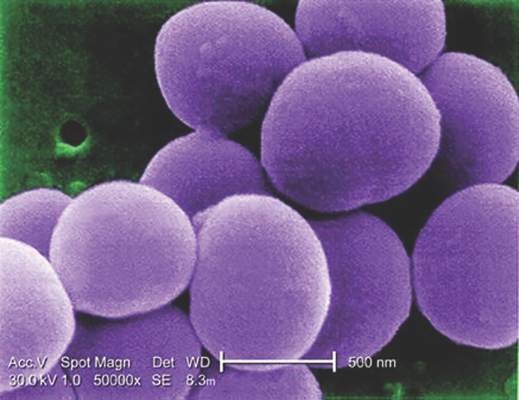
Glucocorticoids increase risk of S. aureus bacteremia
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
FROM MAYO CLINIC PROCEEDINGS
Key clinical point: Taking glucocorticoids can significantly increase the risk of contracting community-acquired Staphylococcus aureus bacteremia (CA-SAB).
Major finding: New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Data source: Retrospective, case-control study of all adults with first-time CA-SAB in Northern Denmark medical registries between 2000 and 2011.
Disclosures: Study supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Bezlotoxumab beats placebo at preventing recurrent C. difficile infections in high-risk patients
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
SAN DIEGO – Bezlotoxumab prevented recurrent Clostridium difficile infections (CDIs) among high-risk patients even more effectively than in the overall populations of the placebo-controlled MODIFY I and MODIFY II trials, according to a report at the annual Digestive Disease Week.
“In those key subpopulations at high risk for recurrence [of C. difficile infection], bezlotoxumab both reduced recurrence and increased rates of global cure,” said Dr. Ciaran P. Kelly of Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. The biologic was especially effective among older adults and patients with at least one recent episode of CDI, Dr. Kelly and his associates found.
Bezlotoxumab is a monoclonal antibody targeting Clostridium difficile toxin B. The international, randomized, double-blind, 12-week MODIFY I and II trials included 2,656 patients with laboratory-confirmed CDI who were randomly assigned to receive either a single intravenous dose of the biologic (10 mg per kg) or placebo in addition to standard care antibiotics – that is, oral metronidazole and vancomycin; intravenous metronidazole with oral vancomycin; oral fidaxomicin; or oral fidaxomicin with intravenous metronidazole.
In both trials, bezlotoxumab was associated with a 10% decrease in rates of recurrent CDI, compared with placebo (P = .0003). Bezlotoxumab also achieved a 9.7% increase in rates of global cure, defined as clinical cure of the initial episode with no recurrence, Dr. Kelly said.
For the current analysis, he and his associates examined the efficacy of bezlotoxumab among patients at increased risk for recurrent CDI. These patients were older than 65 years, were immunocompromised, had a history of recurrent CDI, had been diagnosed with CDI within 6 months, and/or had severe CDI or were infected with hypervirulent, binary toxin positive strain. Most patients in the trials fell into at least one of these categories, Dr. Kelly said.
For each subgroup, bezlotoxumab was associated with lower rates of CDI recurrence and higher rates of global cure than in the overall study population, he emphasized. Compared with placebo, the most dramatic improvements in recurrence and global cure rates were among older patients (a 16% decrease and a 16% increase, respectively), patients with recent CDI (a 16% increase and a 12% decrease), patients with a history of recurrent CDI (a 13% decrease and a 12% increase) and immunocompromised patients (a 13% decrease and a 15% increase).
Neither trial generated a concerning safety signal, according to Dr. Kelly. There were “slight increases” in infusion reactions in the bezlotoxumab arms, but these were mostly minor and short lived, he added. “Serious adverse events were, in fact, slightly more common in the placebo group, mainly because of adverse events related to recurrence.”
The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
AT DDW® 2016
Key clinical point: The monoclonal antibody bezlotoxumab prevented recurrent CDIs among patients at high risk for this outcome.
Major finding: Compared with placebo, bezlotoxumab achieved the most dramatic differences in rates of CDI recurrence and global cure for older patients (a 16% decrease and a 16% increase, respectively).
Data source: An analysis of the international, randomized, double-blind, 12-week MODIFY I and II trials, which included 2,656 patients with laboratory-confirmed CDI.
Disclosures: The MODIFY trials were funded by Merck. Dr. Kelly reported consulting and advisory relationships with Merck, Sanofi Pasteur, Seres Therapeutics, Summit, and Alba.
QUIZ: What Is Next Step for Diagnosing Cavitary Lesion with No Improvement after Serial Chest X-Rays, Antibiotics?
[WpProQuiz 9]
[WpProQuiz_toplist 9]
[WpProQuiz 9]
[WpProQuiz_toplist 9]
[WpProQuiz 9]
[WpProQuiz_toplist 9]
Case of colistin-resistant E. coli identified in the United States
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
In what is believed to be the first case of its kind in the United States, researchers identified a female patient with colistin-resistant Escherichia coli. The patient harbored mcr-1, a gene resistant to colistin, an antibiotic used as a last resort for infections that are resistant to carbapenems.
The finding comes at a time when a search for colistin-resistant bacteria by officials from the U.S. Department of Agriculture and the U.S. Department of Health and Human Services revealed colistin-resistant E. coli in a single sample from a pig intestine. Combined, “these discoveries are of concern because colistin is used as a last-resort drug to treat patients with multidrug resistant infections,” according to a communication from the HHS dated May 26. “Finding colistin-resistant bacteria in the United States is important, as it was only last November that scientists in China first reported that the mcr-1 gene in bacteria confers colistin resistance.”
Researchers led by Patrick McGann, Ph.D., who reported the human case in an article published online May 26 in Antimicrobial Agents and Chemotherapy, wrote that the recent discovery of a plasmid-borne colistin resistance gene, mcr-1, “heralds the emergence of truly pan-drug resistant bacteria. The gene has been found primarily in Escherichia coli, but has also been identified in other members of the Enterobacteriaceae from human, animal, food and environmental samples on every continent” (Antimicrob Agents Chemother. 2016 May 26. doi: 10.1128/AAC.01103-16).
As a result of this threat, in May, Dr. McGann, of the Department of Defense’s Multidrug-resistant Organism Repository and Surveillance Network at Walter Reed Army Institute of Research, Silver Spring, Md., and his associates began analyzing all extended-spectrum beta-lactamase (ESBL)–producing E. coli clinical isolates submitted to Walter Reed National Military Medical Center for analysis for resistance to colistin by E-test.
The case of interest was the presence of mcr-1 in an E. coli isolate cultured from a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection, and who reported no travel history within the prior 5 months. Susceptibility testing at Walter Reed indicated an ESBL phenotype.
“The isolate was included in the first 6 ESBL-producing E. coli selected for colistin susceptibility testing, and it was the only isolate to have a MIC of colistin of 4 mcg/mL [all others had MICs of 0.25 mcg/mL or less]. Colistin MIC was confirmed by microbroth dilution and mcr-1 detected by real-time PCR.”
Since mcr-1 testing at Walter Reed has been underway for a short time, “it remains unclear what the true prevalence of mcr-1 is in the population,” the researchers noted. “The association between mcr-1 and IncF plasmids is concerning as these plasmids are vehicles for the dissemination of antibiotic resistance and virulence genes against Enterobacteriaceae. Continued surveillance to determine the true frequency for this gene in the USA is critical.”
The researchers reported having no financial disclosures.
FROM ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Key clinical point: Researchers have identified the first case of colistin-resistant E. coli in the United States.
Major finding: Mcr-1 was present in an E. coli sampled from a patient with a urinary tract infection in the United States.
Data source: A case report of a 49-year-old woman who presented to a military clinic in Pennsylvania with symptoms suggestive of a urinary tract infection.
Disclosures: The researchers reported having no financial disclosures.
Risk Factors for Pseudomonas, MRSA in Healthcare-Associated Pneumonia
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Clinical question: What risk factors could predict the likelihood of Pseudomonas and methicillin-resistant Staphylococcus aureus (MRSA) in patients hospitalized with healthcare-associated pneumonia (HCAP)?
Background: Patients identified with HCAP have an increased risk for multi-drug-resistant pathogens, such as gram-negative (GNR) organisms and MRSA. Meeting criteria for HCAP does not discriminate between the different infections, which require different antibiotic classes for treatment. Risk factors need to be identified to determine the most likely infectious organism to help guide initial empiric antibiotic therapy.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: Of 61,651 veterans with HCAP diagnosis, 1,156 (1.9%) had a discharge diagnosis of Pseudomonas pneumonia and were found to be younger and more likely to be immunocompromised; have hemiplegia; have a history of chronic obstructive pulmonary disease; have had corticosteroid exposure; and have been exposed to a fluoroquinolone, β-lactam, cephalosporin, or carbapenem antiobiotic within 90 days prior to admission. Pseudomonas pneumonia was negatively associated with age >84, drug abuse, diabetes, and higher socioeconomic status. A discharge diagnosis of MRSA pneumonia was found in 641 patients (1.0%), who also were positively associated with the male gender, age >74, recent nursing home stay, and recent exposure to fluoroquinolone antibiotics within 90 days prior to admission.
MRSA pneumonia was negatively associated with complicated diabetes. Neither diagnosis was present in 59,854 patients (97.1%).
This study was limited due to its predominantly male veteran population, low incidence of Pseudomonas and MRSA pneumonia being identified, and Pseudomonas as the only GNR organism analyzed.
Bottom line: Risk factors identified for Pseudomonas and MRSA pneumonia can help guide targeted antibiotics for HCAP patients.
Citation: Metersky ML, Frei CR, Mortenson EM. Predictors of Pseudomonas and methicillin-resistant Staphylococcus aureus in hospitalized patients with healthcare-associated pneumonia. Respirology. 2016;21(1):157-163.
Short Take
Hematuria as Marker of Urologic Cancer
Narrative literature review did not demonstrate beneficial role of screening urinalysis for cancer detection in asymptomatic patients, but it did suggest including gross hematuria as part of routine review of systems.
Citation: Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a marker of occult urinary tract cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2016;164(7):488-497. doi:10.7326/M15-1496.
Bile salts may be biomarker for recurrent C. difficile infection
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
SAN DIEGO – Bile acid salts in the stool may be a potential biomarker for recurrent episodes of Clostridium difficile infection, a preliminary study suggests.
Although the finding needs to be validated in a prospective study, it could have therapeutic implications, the study investigators said.
“If our results are validated, we could take bile salt profiles of patients who come in with their first episode of C. difficile infection and, using this biomarker, adjust therapy accordingly,” said study lead author Dr. Jessica Allegretti, who presented the findings at the annual Digestive Disease Week. “A patient at high risk of recurrence could get fecal transplant earlier. Right now, fecal transplant is used for recurrent infection.”
C. difficile represents a major public health threat, and recurrent disease complicates 20%-30% of cases.
The disease is communicated by spores that are resistant to heat and antibiotics, and they germinate in the gastrointestinal tract. Bile acids are part of that process. Bile acids assist in the digestion of fat, and a small proportion pass into the colon where primary bile acids undergo transformation into secondary bile acids such as deoxycholate and lithocholate.
In vitro, primary acids can stimulate C. difficile, explained Dr. Allegretti of Brigham and Women’s Hospital, Cambridge, Mass. “Antibiotic therapy may ablate critical members of the microbiota. We aimed to assess bile acid profiles in patients with C. difficile infection, compared with controls, to understand their role in pathogenesis and hopefully identify a biomarker for recurrence.”
The cross-sectional study collected serum and a single stool sample from three groups of 60 patients: patients with a first episode of C. difficile (fCDI) prior to antibiotics (20 patients), patients with a recurrent episode (rCDI) on treatment with chronic vancomycin at the time of sampling (19), and healthy controls who were fecal transplant donors (21).
The researchers sequenced stool microbial components and conducted bile salt metabolomic profiling. Significant differences were revealed in microbial analysis of the stool samples: Primary bile salts (which induce germination) were significantly elevated in rCDI, compared with fCDI and controls – while secondary bile salts in the stool (which are protective) such as deoxycholate and lithocholate were significantly elevated in controls, compared with fCDI and rCDI (P = .0002 and P = .0007, respectively).
“The same trends were seen in the plasma samples, but were less dramatic than in the stool,” Dr. Allegretti noted.
The median predicted bile salt hydrolase (BSH) gene abundance in rCDI was 20% of the median value in controls (P = .001), and it also was significantly lower than fCDI (P = .001). No significant difference was seen between predicted BSH gene abundance between controls and the fCDI groups.
“An association with reduced predicted bacterial bile salt hydrolase gene abundance may be associated with a diminished capacity to metabolize bile acids,” she said.
The difference in BSH gene abundance between controls and rCDI was largely due to changes in the abundance of 10 bacterial taxa, Dr. Allegretti said.
“This study reinforces the importance of bile salts in CDI and demonstrates for the first time in humans that this shift can be appreciated as early as the first episode of CDI in patients who are antibiotic naive,” Dr Allegretti said.
She noted that rCDI samples were collected in patients on chronic antibiotic therapy, and that may explain some of the decrease in biological microdiversity seen in the study.
In search of a biomarker, “secondary bile acids clearly seem to be the winner, and for now, stool seems to make more sense than blood for samples,” she stated.
Dr. Allegretti and her colleagues are conducting a prospective validation study.
The American College of Gastroenterology funded the study.
AT DDW® 2016
Key clinical point: Bile salt acids may identify patients at risk of recurrent Clostridium difficile infection who require more aggressive first-line therapy.
Major finding: Secondary bile acids in stool can distinguish between first-episode patients, recurrent-episode patients, and healthy controls.
Data source: A prospective cross-sectional study of 60 participants.
Disclosures: The American College of Gastroenterology funded the study.
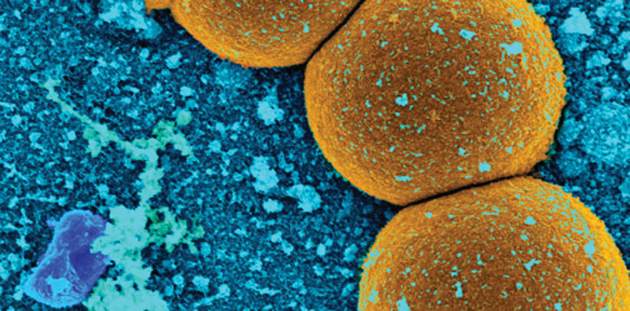
Study: Number of MRSA cases in Japan may be underestimated
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
In Japan, sentinel disease surveillance systems may underestimate the actual number of patients with methicillin-resistant Staphylococcus aureus (MRSA) infection because they do not include information about patients who visit nonsentinel medical facilities, according to a study published in Epidemiology and Infection.
Dr. Shinichi Tanihara of the department of public health and preventive medicine in the School of Medicine at Fukuoka University and Dr. Satowa Suzuki of the department of bacteriology II at the National Institute of Infectious Diseases in Tokyo assessed and compared the incidences of MRSA patients based on health insurance claims data and data reported to the Japan Nosocomial Infections Surveillance system (Epidemiol Infect. 2016 April 8. doi: 10.1017/S0950268816000674).
The study results suggested that health insurance claims data for MRSA cases were more useful for determining the incidence of MRSA cases in Japan from 2011 to 2012. For example, of the 2,052 eligible hospitals with 200 or more beds in 2011, roughly one-quarter (495, 23.8%) participated in the Japan Nosocomial Infections Surveillance system. Data from this relatively low percentage of eligible facilities most likely underestimated the true number of MRSA patients in Japan, the authors said.
Based on their findings, the investigators noted three major advantages of using health insurance claims data for infection surveillance. Firstly, information from health insurance claims data is not affected by health care providers’ notifications to surveillance systems. Secondly, data on patients with MRSA can be collected at low cost because of Japan’s uniform and computerized health insurance system, and the data are easy to access. Lastly, health insurance claims data prevent the duplication of patient information, as insurers can determine if a patient was treated at multiple medical facilities for the same disease.
The only noted drawback involving the use of health insurance claims data for infection surveillance pertained to its timeliness, the researchers wrote. This issue arises because these data are submitted monthly rather than immediately, which may limit their use in surveillance systems.
According to Dr. Tanihara and Dr. Suzuki, strengths of the study include its evaluation of sentinel surveillance quality through the use of data that were not based on physician reports, as well as the calculation of MRSA incidence by use of a standardized definition in a specific population. Reported limitations included the assessment of anti-MRSA medicine use and patients’ age only, and the lack of information on the degree of drug resistance from health insurance claims data.
Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
Key clinical point: Sentinel surveillance systems may substantially underestimate the number of methicillin-resistant Staphylococcus aureus cases in Japan.
Major finding: Direct notification to the Japan Nosocomial Infections Surveillance system regarding methicillin-resistant Staphylococcus aureus patients was not affected by patients’ age, and information from health insurance claims was useful for evaluation of the sentinel infection surveillance system.
Data sources: The Japan Nosocomial Infections Surveillance system and the National Health Insurance Organization.
Disclosures: Funding was provided by the Ministry of Health, Labour, and Welfare of Japan, and by the Research Programme on Emerging and Re-emerging Infectious Diseases from the Japan Agency for Medical Research and Development. Neither author reported any conflicts of interest.
FDA warns against routine fluoroquinolone use
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi