User login
VIDEO: Rifamycin matches ciprofloxacin’s efficacy in travelers’ diarrhea with less antibiotic resistance
CHICAGO – An investigational antibiotic was just as effective as ciprofloxacin at curing travelers’ diarrhea but was associated with a significantly lower rate of colonization with extended spectrum beta-lactam–resistant Escherichia coli, a phase III trial has determined.
“Rifamycin was noninferior to ciprofloxacin on every endpoint in this trial,” Robert Steffen, MD, said at the annual Digestive Disease Week. “However, there was no increase in extended spectrum beta-lactamase–producing Enterobacteriaceae (ESBL-E) associated with rifamycin, and significantly less new acquisition of these pathogens than in the ciprofloxacin group.”
Rifamycin is a poorly absorbed, broad-spectrum antibiotic in the same chemical family as rifaximin. It’s designed, both molecularly and in packaging, to become active only in the lower ileum and colon with limited systemic absorption. The drug is approved in Europe for infectious colitis, Clostridium difficile, diverticulitis, and also as supportive treatment of inflammatory bowel diseases and hepatic encephalopathy.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Subjects were randomized to 3 days of rifamycin 800 mg, or ciprofloxacin 1,000 mg. Follow-up visits occurred on days 2, 5, and 6, with a final follow-up by mail 4 weeks later. The primary endpoint was time to last unformed stool from the first dose of study medication. Secondary endpoints were clinical cure (24 hours with no clinical symptoms, fever, or watery stools, or 48 hours with no fever; and either no stools or only formed stools), need for rescue therapy, treatment failure, pathogen eradication in posttreatment stool, and the rate of ESBL-E colonization.
The time to last unformed stool was 43 hours in the rifamycin group and 37 hours in the ciprofloxacin group, which were not significantly different. The results were similar when broken down by infective organism, by gender, and by study location.
Rifamycin was also noninferior to ciprofloxacin in several secondary endpoints, including clinical cure (85% each), treatment failure (15% each), and need for rescue therapy (1% vs. 2.6%). The drugs were also virtually identical in the number of unformed stools per 24-hour interval, which fell precipitously from 5.5 on day 1, to 1 by day 5, and in complete resolution of gastrointestinal symptoms, which were about 75% resolved in each group by day 5.
Rifamycin was equally effective in eradicating all of the pathogens identified in the cohort. This included all pathogens in the E. coli group, all in the potentially invasive group (Shigella, Campylobacter, Salmonella, and Aeromonas), norovirus, giardia, and Cryptosporidium.
Treatment-emergent adverse events occurred in 12% of each group; none were serious. About 8% of each group experienced an adverse drug reaction.
Where the drugs did differ, and sharply so, was in antibiotic resistance, said Dr. Steffen, of the University of Zürich and the University of Texas School of Public Health, Houston. At baseline, about 16% of the group was infected with ESBL–E coli. At last follow-up, those species were present in 16% of the rifamycin group, but in 21% of the ciprofloxacin group. Similarly, there was less new ESBL–E. coli colonization in patients who had been negative at baseline (10% vs. 17%).
The findings are particularly important in light of the increasing worldwide emergence of antibiotic-resistant bacteria, Dr. Steffen said. In fact, new guidelines released April 29 by the International Society of Travel Medicine recommend that antibiotics be reserved for moderate to severe cases of traveler’s diarrhea and not be used at all in milder cases (J Travel Med. 2017 Apr 29;24[suppl. 1]:S57-S74).
“The widespread use of ciprofloxacin and other antibiotics for travelers’ diarrhea has contributed to the rise of these resistant bacteria,” Dr. Steffen said in an interview. “We need to rethink the way we use these drugs and to focus instead on drugs that are not systemically absorbed. If rifamycin is eventually approved for this indication, it would be a good alternative to systemic antibiotics, curing the acute illness, and not contributing as much to the emergence of these worrisome pathogens.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
In a video interview at the meeting, Dr. Steffen spoke about the trial and concerns about antibiotic resistance that are addressed in the new guidelines and by this new study.
Dr. Falk Pharma GmbH of Freiburg, Germany, is developing rifamycin and conducted the study. Dr. Steffen has received consulting and travel fees from the company.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
CHICAGO – An investigational antibiotic was just as effective as ciprofloxacin at curing travelers’ diarrhea but was associated with a significantly lower rate of colonization with extended spectrum beta-lactam–resistant Escherichia coli, a phase III trial has determined.
“Rifamycin was noninferior to ciprofloxacin on every endpoint in this trial,” Robert Steffen, MD, said at the annual Digestive Disease Week. “However, there was no increase in extended spectrum beta-lactamase–producing Enterobacteriaceae (ESBL-E) associated with rifamycin, and significantly less new acquisition of these pathogens than in the ciprofloxacin group.”
Rifamycin is a poorly absorbed, broad-spectrum antibiotic in the same chemical family as rifaximin. It’s designed, both molecularly and in packaging, to become active only in the lower ileum and colon with limited systemic absorption. The drug is approved in Europe for infectious colitis, Clostridium difficile, diverticulitis, and also as supportive treatment of inflammatory bowel diseases and hepatic encephalopathy.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Subjects were randomized to 3 days of rifamycin 800 mg, or ciprofloxacin 1,000 mg. Follow-up visits occurred on days 2, 5, and 6, with a final follow-up by mail 4 weeks later. The primary endpoint was time to last unformed stool from the first dose of study medication. Secondary endpoints were clinical cure (24 hours with no clinical symptoms, fever, or watery stools, or 48 hours with no fever; and either no stools or only formed stools), need for rescue therapy, treatment failure, pathogen eradication in posttreatment stool, and the rate of ESBL-E colonization.
The time to last unformed stool was 43 hours in the rifamycin group and 37 hours in the ciprofloxacin group, which were not significantly different. The results were similar when broken down by infective organism, by gender, and by study location.
Rifamycin was also noninferior to ciprofloxacin in several secondary endpoints, including clinical cure (85% each), treatment failure (15% each), and need for rescue therapy (1% vs. 2.6%). The drugs were also virtually identical in the number of unformed stools per 24-hour interval, which fell precipitously from 5.5 on day 1, to 1 by day 5, and in complete resolution of gastrointestinal symptoms, which were about 75% resolved in each group by day 5.
Rifamycin was equally effective in eradicating all of the pathogens identified in the cohort. This included all pathogens in the E. coli group, all in the potentially invasive group (Shigella, Campylobacter, Salmonella, and Aeromonas), norovirus, giardia, and Cryptosporidium.
Treatment-emergent adverse events occurred in 12% of each group; none were serious. About 8% of each group experienced an adverse drug reaction.
Where the drugs did differ, and sharply so, was in antibiotic resistance, said Dr. Steffen, of the University of Zürich and the University of Texas School of Public Health, Houston. At baseline, about 16% of the group was infected with ESBL–E coli. At last follow-up, those species were present in 16% of the rifamycin group, but in 21% of the ciprofloxacin group. Similarly, there was less new ESBL–E. coli colonization in patients who had been negative at baseline (10% vs. 17%).
The findings are particularly important in light of the increasing worldwide emergence of antibiotic-resistant bacteria, Dr. Steffen said. In fact, new guidelines released April 29 by the International Society of Travel Medicine recommend that antibiotics be reserved for moderate to severe cases of traveler’s diarrhea and not be used at all in milder cases (J Travel Med. 2017 Apr 29;24[suppl. 1]:S57-S74).
“The widespread use of ciprofloxacin and other antibiotics for travelers’ diarrhea has contributed to the rise of these resistant bacteria,” Dr. Steffen said in an interview. “We need to rethink the way we use these drugs and to focus instead on drugs that are not systemically absorbed. If rifamycin is eventually approved for this indication, it would be a good alternative to systemic antibiotics, curing the acute illness, and not contributing as much to the emergence of these worrisome pathogens.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
In a video interview at the meeting, Dr. Steffen spoke about the trial and concerns about antibiotic resistance that are addressed in the new guidelines and by this new study.
Dr. Falk Pharma GmbH of Freiburg, Germany, is developing rifamycin and conducted the study. Dr. Steffen has received consulting and travel fees from the company.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
CHICAGO – An investigational antibiotic was just as effective as ciprofloxacin at curing travelers’ diarrhea but was associated with a significantly lower rate of colonization with extended spectrum beta-lactam–resistant Escherichia coli, a phase III trial has determined.
“Rifamycin was noninferior to ciprofloxacin on every endpoint in this trial,” Robert Steffen, MD, said at the annual Digestive Disease Week. “However, there was no increase in extended spectrum beta-lactamase–producing Enterobacteriaceae (ESBL-E) associated with rifamycin, and significantly less new acquisition of these pathogens than in the ciprofloxacin group.”
Rifamycin is a poorly absorbed, broad-spectrum antibiotic in the same chemical family as rifaximin. It’s designed, both molecularly and in packaging, to become active only in the lower ileum and colon with limited systemic absorption. The drug is approved in Europe for infectious colitis, Clostridium difficile, diverticulitis, and also as supportive treatment of inflammatory bowel diseases and hepatic encephalopathy.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Subjects were randomized to 3 days of rifamycin 800 mg, or ciprofloxacin 1,000 mg. Follow-up visits occurred on days 2, 5, and 6, with a final follow-up by mail 4 weeks later. The primary endpoint was time to last unformed stool from the first dose of study medication. Secondary endpoints were clinical cure (24 hours with no clinical symptoms, fever, or watery stools, or 48 hours with no fever; and either no stools or only formed stools), need for rescue therapy, treatment failure, pathogen eradication in posttreatment stool, and the rate of ESBL-E colonization.
The time to last unformed stool was 43 hours in the rifamycin group and 37 hours in the ciprofloxacin group, which were not significantly different. The results were similar when broken down by infective organism, by gender, and by study location.
Rifamycin was also noninferior to ciprofloxacin in several secondary endpoints, including clinical cure (85% each), treatment failure (15% each), and need for rescue therapy (1% vs. 2.6%). The drugs were also virtually identical in the number of unformed stools per 24-hour interval, which fell precipitously from 5.5 on day 1, to 1 by day 5, and in complete resolution of gastrointestinal symptoms, which were about 75% resolved in each group by day 5.
Rifamycin was equally effective in eradicating all of the pathogens identified in the cohort. This included all pathogens in the E. coli group, all in the potentially invasive group (Shigella, Campylobacter, Salmonella, and Aeromonas), norovirus, giardia, and Cryptosporidium.
Treatment-emergent adverse events occurred in 12% of each group; none were serious. About 8% of each group experienced an adverse drug reaction.
Where the drugs did differ, and sharply so, was in antibiotic resistance, said Dr. Steffen, of the University of Zürich and the University of Texas School of Public Health, Houston. At baseline, about 16% of the group was infected with ESBL–E coli. At last follow-up, those species were present in 16% of the rifamycin group, but in 21% of the ciprofloxacin group. Similarly, there was less new ESBL–E. coli colonization in patients who had been negative at baseline (10% vs. 17%).
The findings are particularly important in light of the increasing worldwide emergence of antibiotic-resistant bacteria, Dr. Steffen said. In fact, new guidelines released April 29 by the International Society of Travel Medicine recommend that antibiotics be reserved for moderate to severe cases of traveler’s diarrhea and not be used at all in milder cases (J Travel Med. 2017 Apr 29;24[suppl. 1]:S57-S74).
“The widespread use of ciprofloxacin and other antibiotics for travelers’ diarrhea has contributed to the rise of these resistant bacteria,” Dr. Steffen said in an interview. “We need to rethink the way we use these drugs and to focus instead on drugs that are not systemically absorbed. If rifamycin is eventually approved for this indication, it would be a good alternative to systemic antibiotics, curing the acute illness, and not contributing as much to the emergence of these worrisome pathogens.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
In a video interview at the meeting, Dr. Steffen spoke about the trial and concerns about antibiotic resistance that are addressed in the new guidelines and by this new study.
Dr. Falk Pharma GmbH of Freiburg, Germany, is developing rifamycin and conducted the study. Dr. Steffen has received consulting and travel fees from the company.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
AT DDW
Key clinical point:
Major finding: Clinical cure occurred in 85% of each group, but new beta-lactam–resistant E. coli colonization occurred in 16% of the rifamycin group and 21% of the ciprofloxacin group.
Data source: The randomized study comprised 835 subjects.
Disclosures: Dr. Falk Pharma GmbH of Freiburg, Germany, is developing the drug and sponsored the study. Dr. Steffen has received consulting and travel fees from the company.
Each added day of pediatric MRSA bacteremia upped complication risk 50%
Every additional day of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia in hospitalized children was associated with a 50% increased risk of developing a complication, reported Rana F. Hamdy, MD, of Children’s National Health System, Washington, and her associates.
That was one of the findings of a study performed to determine the epidemiology, clinical outcomes, and risk factors for treatment failure in pediatric MRSA bacteremia. It took place in three hospitals, one each in Philadelphia, Baltimore, and Salt Lake City.
“This finding is in contrast to the epidemiology of MRSA bacteremia in adults, in whom bacteremia is more frequently attributed to catheter-related infections (31%-36%), endovascular infections (13%-15%), or an unknown source (15%-20%), and the durations of MRSA bacteremia are typically more prolonged (median duration of bacteremia is 8-9 days),” Dr. Hamdy and her associates wrote.
“Differences in the epidemiology of MRSA bacteremia between children and adults emphasize the need for dedicated pediatric studies to better understand the clinical characteristics and outcomes specific to children,” the researchers noted.
Musculoskeletal infections and endovascular infections were linked with treatment failure, possibly reflecting “the relatively higher burden of bacteria and/or decreased drug penetration into bone and endovascular infection sites,” the investigators said. Catheter-related infections were tied to reduced odds of treatment failure, “these episodes being localized to the catheter and therefore potentially less-invasive S. aureus infections.”
Mortality among these children with MRSA bacteremia was low, at 2%, but “nearly one-quarter of all patients experienced complications,” the study authors said (Pediatrics. 2017 May 5. doi: 10.1542/peds.2017-0183).
There was progression of infection in 7% of cases, and hematogenous complications or sequelae occurred in 23%. Twenty percent of children developed septic emboli or another metastatic focus of infection.
“This association between the duration of bacteremia and the development of complications has been previously reported among adults with S. aureus bacteremia,” Dr. Hamdy noted, “and provides important epidemiologic data that could inform decisions relating to the timing of additional imaging, such as echocardiograms, to identify metastatic foci.”
The children were treated with vancomycin, and some received additional anti-MRSA antibiotics. “Vancomycin trough concentrations or [minimum inhibitory concentrations] were not associated with treatment failure,” the investigators said. “Future studies to determine the appropriate vancomycin dose, duration, and approach to therapeutic drug monitoring are warranted to optimize patient outcomes.”
The National Institutes of Health funded the study. Dr. Hamdy and her associates disclosed they have no relevant financial relationships.
Every additional day of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia in hospitalized children was associated with a 50% increased risk of developing a complication, reported Rana F. Hamdy, MD, of Children’s National Health System, Washington, and her associates.
That was one of the findings of a study performed to determine the epidemiology, clinical outcomes, and risk factors for treatment failure in pediatric MRSA bacteremia. It took place in three hospitals, one each in Philadelphia, Baltimore, and Salt Lake City.
“This finding is in contrast to the epidemiology of MRSA bacteremia in adults, in whom bacteremia is more frequently attributed to catheter-related infections (31%-36%), endovascular infections (13%-15%), or an unknown source (15%-20%), and the durations of MRSA bacteremia are typically more prolonged (median duration of bacteremia is 8-9 days),” Dr. Hamdy and her associates wrote.
“Differences in the epidemiology of MRSA bacteremia between children and adults emphasize the need for dedicated pediatric studies to better understand the clinical characteristics and outcomes specific to children,” the researchers noted.
Musculoskeletal infections and endovascular infections were linked with treatment failure, possibly reflecting “the relatively higher burden of bacteria and/or decreased drug penetration into bone and endovascular infection sites,” the investigators said. Catheter-related infections were tied to reduced odds of treatment failure, “these episodes being localized to the catheter and therefore potentially less-invasive S. aureus infections.”
Mortality among these children with MRSA bacteremia was low, at 2%, but “nearly one-quarter of all patients experienced complications,” the study authors said (Pediatrics. 2017 May 5. doi: 10.1542/peds.2017-0183).
There was progression of infection in 7% of cases, and hematogenous complications or sequelae occurred in 23%. Twenty percent of children developed septic emboli or another metastatic focus of infection.
“This association between the duration of bacteremia and the development of complications has been previously reported among adults with S. aureus bacteremia,” Dr. Hamdy noted, “and provides important epidemiologic data that could inform decisions relating to the timing of additional imaging, such as echocardiograms, to identify metastatic foci.”
The children were treated with vancomycin, and some received additional anti-MRSA antibiotics. “Vancomycin trough concentrations or [minimum inhibitory concentrations] were not associated with treatment failure,” the investigators said. “Future studies to determine the appropriate vancomycin dose, duration, and approach to therapeutic drug monitoring are warranted to optimize patient outcomes.”
The National Institutes of Health funded the study. Dr. Hamdy and her associates disclosed they have no relevant financial relationships.
Every additional day of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia in hospitalized children was associated with a 50% increased risk of developing a complication, reported Rana F. Hamdy, MD, of Children’s National Health System, Washington, and her associates.
That was one of the findings of a study performed to determine the epidemiology, clinical outcomes, and risk factors for treatment failure in pediatric MRSA bacteremia. It took place in three hospitals, one each in Philadelphia, Baltimore, and Salt Lake City.
“This finding is in contrast to the epidemiology of MRSA bacteremia in adults, in whom bacteremia is more frequently attributed to catheter-related infections (31%-36%), endovascular infections (13%-15%), or an unknown source (15%-20%), and the durations of MRSA bacteremia are typically more prolonged (median duration of bacteremia is 8-9 days),” Dr. Hamdy and her associates wrote.
“Differences in the epidemiology of MRSA bacteremia between children and adults emphasize the need for dedicated pediatric studies to better understand the clinical characteristics and outcomes specific to children,” the researchers noted.
Musculoskeletal infections and endovascular infections were linked with treatment failure, possibly reflecting “the relatively higher burden of bacteria and/or decreased drug penetration into bone and endovascular infection sites,” the investigators said. Catheter-related infections were tied to reduced odds of treatment failure, “these episodes being localized to the catheter and therefore potentially less-invasive S. aureus infections.”
Mortality among these children with MRSA bacteremia was low, at 2%, but “nearly one-quarter of all patients experienced complications,” the study authors said (Pediatrics. 2017 May 5. doi: 10.1542/peds.2017-0183).
There was progression of infection in 7% of cases, and hematogenous complications or sequelae occurred in 23%. Twenty percent of children developed septic emboli or another metastatic focus of infection.
“This association between the duration of bacteremia and the development of complications has been previously reported among adults with S. aureus bacteremia,” Dr. Hamdy noted, “and provides important epidemiologic data that could inform decisions relating to the timing of additional imaging, such as echocardiograms, to identify metastatic foci.”
The children were treated with vancomycin, and some received additional anti-MRSA antibiotics. “Vancomycin trough concentrations or [minimum inhibitory concentrations] were not associated with treatment failure,” the investigators said. “Future studies to determine the appropriate vancomycin dose, duration, and approach to therapeutic drug monitoring are warranted to optimize patient outcomes.”
The National Institutes of Health funded the study. Dr. Hamdy and her associates disclosed they have no relevant financial relationships.
FROM PEDIATRICS
Key clinical point:
Major finding: The primary sources of infection were osteomyelitis (31%), catheter-related bloodstream infections (22%), and skin and soft tissue infections (16%); endocarditis occurred in only 2% – a different epidemiology than in adults.
Data source: A study of 174 hospitalized children (younger than 19 years) with MRSA bacteremia at three hospitals in different states.
Disclosures: The National Institutes of Health funded the study. Dr. Hamdy and her associates disclosed they have no relevant financial relationships.
Adjunctive rifampicin doesn’t improve any outcome in S. aureus bacteremia
VIENNA – When given in conjunction with an antibiotic, rifampicin didn’t improve treatment response or mortality in patients with Staphylococcus aureus bacteremia, either in an overall analysis or in any of 18 subgroups.
The only hints of benefit associated with the drug were decreases in treatment failure and recurrence, but the numbers needed to treat were excessive (29 and 26, respectively). They didn’t translate into any long-term survival benefit and couldn’t balance out other findings that rifampicin increased drug interactions and complicated treatment, Guy Thwaites, MD, said at the European Conference on Clinical Microbiology and Infectious Diseases.
He presented the results of the randomized, placebo-controlled ARREST (Adjunctive Rifampicin to Reduce Early Mortality From Staphylococcus aureus bacteremia) study. ARREST was conducted at 29 sites in the United Kingdom. It enrolled 758 adults with proven S. aureus bacteremia who were already on standard antibiotic therapy and switched them to either adjunctive rifampicin or placebo for 2 weeks. Clinicians could choose rifampicin in either 600 mg or 900 mg, oral or IV formulations, once or twice daily doses.
Patients were followed with clinical assessments and blood cultures for 12 weeks and for overall mortality for 102 weeks. The primary endpoint was bacteriologically confirmed treatment failure or recurrence by week 12.
Patients were a mean of 65 years old. Most infections (64%) were community acquired, with the remainder associated with a stay in a health care facility, and 6% were methicillin resistant. Serious comorbidities were common, including cancer (17%), chronic lung disease (12%), kidney disease (18%), and diabetes (30%).
The largest portion of infections (40%) had a deep focus, including native cardiac valve or joint, prosthetic cardiac valve or implant, and deep tissue infections. Other sites of infection were indwelling lines, skin/soft tissue, surgical sites, pneumonia, and urinary tract. For 18%, no specific focus was ever established.
Rifampicin was initiated a mean of 68 hours after main antibiotic therapy. Most patients (86%) received it orally, in the 900-mg dose (78%). The mean rifampicin treatment duration was 13 days.
Treatment failure rates through week 12 were practically identical for rifampicin and placebo (17.5% vs. 18.9%) in the overall analysis. Clinical failure or recurrence through week 12 was also similar for rifampicin and placebo (21.4% vs. 22.9%). Dr. Thwaites didn’t present all 18 subgroup analyses but said the results were similar no matter how patients were divided.
There was no significant difference in 12-week mortality for rifampicin vs. placebo (15.7% vs. 14.8%). There were 112 deaths, 56 in each group. Of these, 28 were directly related to the S. aureus infection. There was no difference in long-term survival measured at 102 weeks.
When an independent endpoint review committee examined some of the composite endpoints separately, it determined that rifampicin did confer a significant advantage in both bacterial and clinical recurrence. However, 29 patients needed to be treated to avoid a bacteriologic recurrence and 26 to avoid a clinical recurrence. Two cases of rifampicin resistance developed.
One-quarter of the group experienced serious adverse events. Dr. Thwaites didn’t review these but said they were evenly distributed between the groups. He also said that rifampicin was associated with an increase in drug-drug interactions, some of which required changing the backbone antibiotic.
There was a small, but nonsignificant, increase in acute kidney injury in the rifampicin group.
The study was funded by the National Institute of Health Research in the United Kingdom. Dr. Thwaites had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
VIENNA – When given in conjunction with an antibiotic, rifampicin didn’t improve treatment response or mortality in patients with Staphylococcus aureus bacteremia, either in an overall analysis or in any of 18 subgroups.
The only hints of benefit associated with the drug were decreases in treatment failure and recurrence, but the numbers needed to treat were excessive (29 and 26, respectively). They didn’t translate into any long-term survival benefit and couldn’t balance out other findings that rifampicin increased drug interactions and complicated treatment, Guy Thwaites, MD, said at the European Conference on Clinical Microbiology and Infectious Diseases.
He presented the results of the randomized, placebo-controlled ARREST (Adjunctive Rifampicin to Reduce Early Mortality From Staphylococcus aureus bacteremia) study. ARREST was conducted at 29 sites in the United Kingdom. It enrolled 758 adults with proven S. aureus bacteremia who were already on standard antibiotic therapy and switched them to either adjunctive rifampicin or placebo for 2 weeks. Clinicians could choose rifampicin in either 600 mg or 900 mg, oral or IV formulations, once or twice daily doses.
Patients were followed with clinical assessments and blood cultures for 12 weeks and for overall mortality for 102 weeks. The primary endpoint was bacteriologically confirmed treatment failure or recurrence by week 12.
Patients were a mean of 65 years old. Most infections (64%) were community acquired, with the remainder associated with a stay in a health care facility, and 6% were methicillin resistant. Serious comorbidities were common, including cancer (17%), chronic lung disease (12%), kidney disease (18%), and diabetes (30%).
The largest portion of infections (40%) had a deep focus, including native cardiac valve or joint, prosthetic cardiac valve or implant, and deep tissue infections. Other sites of infection were indwelling lines, skin/soft tissue, surgical sites, pneumonia, and urinary tract. For 18%, no specific focus was ever established.
Rifampicin was initiated a mean of 68 hours after main antibiotic therapy. Most patients (86%) received it orally, in the 900-mg dose (78%). The mean rifampicin treatment duration was 13 days.
Treatment failure rates through week 12 were practically identical for rifampicin and placebo (17.5% vs. 18.9%) in the overall analysis. Clinical failure or recurrence through week 12 was also similar for rifampicin and placebo (21.4% vs. 22.9%). Dr. Thwaites didn’t present all 18 subgroup analyses but said the results were similar no matter how patients were divided.
There was no significant difference in 12-week mortality for rifampicin vs. placebo (15.7% vs. 14.8%). There were 112 deaths, 56 in each group. Of these, 28 were directly related to the S. aureus infection. There was no difference in long-term survival measured at 102 weeks.
When an independent endpoint review committee examined some of the composite endpoints separately, it determined that rifampicin did confer a significant advantage in both bacterial and clinical recurrence. However, 29 patients needed to be treated to avoid a bacteriologic recurrence and 26 to avoid a clinical recurrence. Two cases of rifampicin resistance developed.
One-quarter of the group experienced serious adverse events. Dr. Thwaites didn’t review these but said they were evenly distributed between the groups. He also said that rifampicin was associated with an increase in drug-drug interactions, some of which required changing the backbone antibiotic.
There was a small, but nonsignificant, increase in acute kidney injury in the rifampicin group.
The study was funded by the National Institute of Health Research in the United Kingdom. Dr. Thwaites had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
VIENNA – When given in conjunction with an antibiotic, rifampicin didn’t improve treatment response or mortality in patients with Staphylococcus aureus bacteremia, either in an overall analysis or in any of 18 subgroups.
The only hints of benefit associated with the drug were decreases in treatment failure and recurrence, but the numbers needed to treat were excessive (29 and 26, respectively). They didn’t translate into any long-term survival benefit and couldn’t balance out other findings that rifampicin increased drug interactions and complicated treatment, Guy Thwaites, MD, said at the European Conference on Clinical Microbiology and Infectious Diseases.
He presented the results of the randomized, placebo-controlled ARREST (Adjunctive Rifampicin to Reduce Early Mortality From Staphylococcus aureus bacteremia) study. ARREST was conducted at 29 sites in the United Kingdom. It enrolled 758 adults with proven S. aureus bacteremia who were already on standard antibiotic therapy and switched them to either adjunctive rifampicin or placebo for 2 weeks. Clinicians could choose rifampicin in either 600 mg or 900 mg, oral or IV formulations, once or twice daily doses.
Patients were followed with clinical assessments and blood cultures for 12 weeks and for overall mortality for 102 weeks. The primary endpoint was bacteriologically confirmed treatment failure or recurrence by week 12.
Patients were a mean of 65 years old. Most infections (64%) were community acquired, with the remainder associated with a stay in a health care facility, and 6% were methicillin resistant. Serious comorbidities were common, including cancer (17%), chronic lung disease (12%), kidney disease (18%), and diabetes (30%).
The largest portion of infections (40%) had a deep focus, including native cardiac valve or joint, prosthetic cardiac valve or implant, and deep tissue infections. Other sites of infection were indwelling lines, skin/soft tissue, surgical sites, pneumonia, and urinary tract. For 18%, no specific focus was ever established.
Rifampicin was initiated a mean of 68 hours after main antibiotic therapy. Most patients (86%) received it orally, in the 900-mg dose (78%). The mean rifampicin treatment duration was 13 days.
Treatment failure rates through week 12 were practically identical for rifampicin and placebo (17.5% vs. 18.9%) in the overall analysis. Clinical failure or recurrence through week 12 was also similar for rifampicin and placebo (21.4% vs. 22.9%). Dr. Thwaites didn’t present all 18 subgroup analyses but said the results were similar no matter how patients were divided.
There was no significant difference in 12-week mortality for rifampicin vs. placebo (15.7% vs. 14.8%). There were 112 deaths, 56 in each group. Of these, 28 were directly related to the S. aureus infection. There was no difference in long-term survival measured at 102 weeks.
When an independent endpoint review committee examined some of the composite endpoints separately, it determined that rifampicin did confer a significant advantage in both bacterial and clinical recurrence. However, 29 patients needed to be treated to avoid a bacteriologic recurrence and 26 to avoid a clinical recurrence. Two cases of rifampicin resistance developed.
One-quarter of the group experienced serious adverse events. Dr. Thwaites didn’t review these but said they were evenly distributed between the groups. He also said that rifampicin was associated with an increase in drug-drug interactions, some of which required changing the backbone antibiotic.
There was a small, but nonsignificant, increase in acute kidney injury in the rifampicin group.
The study was funded by the National Institute of Health Research in the United Kingdom. Dr. Thwaites had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
Key clinical point:
Major finding: Treatment failure was nearly identical with rifampicin and placebo (17.5% vs. 18.9%).
Data source: A placebo-controlled trial enrolling 758 adults.
Disclosures: The study was funded by the National Institute of Health Research in the United Kingdom. Dr. Thwaites had no financial disclosures.
VIDEO: Hospitalists can help improve antibiotic stewardship
Hospitalists can – and should – help curb unnecessary antibiotic use, according to an expert who spoke at HM17.
Nearly three-quarters of patients who have been diagnosed with community acquired pneumonia are receiving antibiotics for longer periods than necessary, either because the severity of their illness doesn’t warrant them or because they do not have pneumonia, according to Valerie M. Vaughn, MD, a research scientist in the division of hospital medicine and the Patient Safety Enhancement Program at Michigan Medicine, Ann Arbor.
“As hospitalists, we have a role to play in antibiotic stewardship,” Dr. Vaughn said in this interview recorded at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Hospitalists can – and should – help curb unnecessary antibiotic use, according to an expert who spoke at HM17.
Nearly three-quarters of patients who have been diagnosed with community acquired pneumonia are receiving antibiotics for longer periods than necessary, either because the severity of their illness doesn’t warrant them or because they do not have pneumonia, according to Valerie M. Vaughn, MD, a research scientist in the division of hospital medicine and the Patient Safety Enhancement Program at Michigan Medicine, Ann Arbor.
“As hospitalists, we have a role to play in antibiotic stewardship,” Dr. Vaughn said in this interview recorded at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Hospitalists can – and should – help curb unnecessary antibiotic use, according to an expert who spoke at HM17.
Nearly three-quarters of patients who have been diagnosed with community acquired pneumonia are receiving antibiotics for longer periods than necessary, either because the severity of their illness doesn’t warrant them or because they do not have pneumonia, according to Valerie M. Vaughn, MD, a research scientist in the division of hospital medicine and the Patient Safety Enhancement Program at Michigan Medicine, Ann Arbor.
“As hospitalists, we have a role to play in antibiotic stewardship,” Dr. Vaughn said in this interview recorded at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Enjoy Las Vegas and HM17
Welcome to HM17 and Las Vegas! We invite you to network and get to know more than 4,000 of your closest colleagues over the next 3 days. Please have fun taking advantage of the many unique learning opportunities we have developed for this year’s meeting. We hope you will be pleased with the offerings that our Annual Meeting Committee has produced on your behalf. You will see committee members wearing buttons that identify them as members of the Annual Meeting Committee. Please take the time to give them your feedback about the meeting and, if you feel so inclined, thank them for the time and energy they committed to create this year’s meeting.
We think you will find this meeting and the precourses have something (many things!) for everyone. Whether you are a community or an academic hospitalist, a newly minted hospitalist or a seasoned veteran, a clinician who takes care of the young or the old (and everyone in between), an advanced practice clinician or hospital medicine administrator, a researcher or educator or clinician (or any combination of the three), we had you in mind as we developed the content for HM17.
We have added medical education and health policy tracks and are bringing back favorites like the young-hospitalist, academic, pediatric, practice management, and quality tracks. Don’t forget to attend our interactive workshops. More than 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Finally, your HM17 experience will not be complete until you attend the much-anticipated Updates in Hospital Medicine talks and plenary sessions; network with your colleagues at the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition; roam the Exhibit Hall; and join in a Special Interest Forum.
This meeting would not be possible without the tireless effort of the SHM staff and leadership, conference faculty, and committee members. Most importantly, we sincerely thank all of you for attending HM17. We have created this meeting for you, and we hope it is your most valuable educational and networking opportunity of 2017.
Enjoy Las Vegas and HM17, and we will see you in 2018 in Orlando!
Dr. Feldman is a hospitalist at Johns Hopkins in Baltimore and course director for HM17.
Welcome to HM17 and Las Vegas! We invite you to network and get to know more than 4,000 of your closest colleagues over the next 3 days. Please have fun taking advantage of the many unique learning opportunities we have developed for this year’s meeting. We hope you will be pleased with the offerings that our Annual Meeting Committee has produced on your behalf. You will see committee members wearing buttons that identify them as members of the Annual Meeting Committee. Please take the time to give them your feedback about the meeting and, if you feel so inclined, thank them for the time and energy they committed to create this year’s meeting.
We think you will find this meeting and the precourses have something (many things!) for everyone. Whether you are a community or an academic hospitalist, a newly minted hospitalist or a seasoned veteran, a clinician who takes care of the young or the old (and everyone in between), an advanced practice clinician or hospital medicine administrator, a researcher or educator or clinician (or any combination of the three), we had you in mind as we developed the content for HM17.
We have added medical education and health policy tracks and are bringing back favorites like the young-hospitalist, academic, pediatric, practice management, and quality tracks. Don’t forget to attend our interactive workshops. More than 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Finally, your HM17 experience will not be complete until you attend the much-anticipated Updates in Hospital Medicine talks and plenary sessions; network with your colleagues at the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition; roam the Exhibit Hall; and join in a Special Interest Forum.
This meeting would not be possible without the tireless effort of the SHM staff and leadership, conference faculty, and committee members. Most importantly, we sincerely thank all of you for attending HM17. We have created this meeting for you, and we hope it is your most valuable educational and networking opportunity of 2017.
Enjoy Las Vegas and HM17, and we will see you in 2018 in Orlando!
Dr. Feldman is a hospitalist at Johns Hopkins in Baltimore and course director for HM17.
Welcome to HM17 and Las Vegas! We invite you to network and get to know more than 4,000 of your closest colleagues over the next 3 days. Please have fun taking advantage of the many unique learning opportunities we have developed for this year’s meeting. We hope you will be pleased with the offerings that our Annual Meeting Committee has produced on your behalf. You will see committee members wearing buttons that identify them as members of the Annual Meeting Committee. Please take the time to give them your feedback about the meeting and, if you feel so inclined, thank them for the time and energy they committed to create this year’s meeting.
We think you will find this meeting and the precourses have something (many things!) for everyone. Whether you are a community or an academic hospitalist, a newly minted hospitalist or a seasoned veteran, a clinician who takes care of the young or the old (and everyone in between), an advanced practice clinician or hospital medicine administrator, a researcher or educator or clinician (or any combination of the three), we had you in mind as we developed the content for HM17.
We have added medical education and health policy tracks and are bringing back favorites like the young-hospitalist, academic, pediatric, practice management, and quality tracks. Don’t forget to attend our interactive workshops. More than 150 workshop ideas were submitted, and we are proud to feature 18 of the best.
Finally, your HM17 experience will not be complete until you attend the much-anticipated Updates in Hospital Medicine talks and plenary sessions; network with your colleagues at the Research, Innovations, and Clinical Vignettes (RIV) Poster Competition; roam the Exhibit Hall; and join in a Special Interest Forum.
This meeting would not be possible without the tireless effort of the SHM staff and leadership, conference faculty, and committee members. Most importantly, we sincerely thank all of you for attending HM17. We have created this meeting for you, and we hope it is your most valuable educational and networking opportunity of 2017.
Enjoy Las Vegas and HM17, and we will see you in 2018 in Orlando!
Dr. Feldman is a hospitalist at Johns Hopkins in Baltimore and course director for HM17.
Hospital infections top WHO’s list of priority pathogens
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
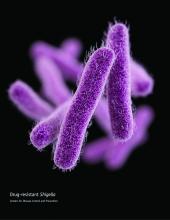
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
VHA warns of a ‘second epidemic’ of carbapenem-resistant E. cloacae complex
Veterans Health Administration monitoring of carbapenem-resistant Enterobacteriaceae (CRE) trends from 2006 to 2015 shows a rise in resistance rates of E. cloacae complex nationwide.
The first major CRE outbreak, Klebsiella pneumoniae, occurred in the eastern United States in the early 2000s and has since spread across the country. K. pneumoniae has recently shown a decrease in resistance rates in the region including New York, both in the current VHA-based study and in a 2016 study of three New York City hospitals.
“CRE trends during 2006-2015 in the VHA recapitulate the epidemic of carbapenem-resistant K. pneumoniae in the United States and indicate that a ‘second epidemic’ of carbapenem-resistant E. cloacae complex appears to be unfolding,” wrote Brigid M. Wilson, PhD, of Louis Stokes Cleveland Department of Veterans Affairs Medical Center, and her coauthors.
The researchers used VHA network data to identify 128,431 K. pneumoniae and 38,219 E. cloacae complex (which refers to the species E. cloacae, E. asburiae, E. kobei, E. hormaechei, and E. xiafangensis) isolates from patients hospitalized in 140 facilities in 40 states, the District of Columbia, and Puerto Rico from 2006 to 2015. These isolates, paired with their carbapenem susceptibility test results, show the rise and geographic concentration of the CRE cases over the decade.
The increased E. cloacae complex resistance in 2014-2015 was centered around the Pacific Coast and Southwest regions. The researchers noted that E. cloacae complex has a less well defined genetic makeup, compared with K. pneumoniae.
“We hypothesize that E. cloacae complex contains genotypes with epidemic potential associated with increasing rates of carbapenem resistance observed in the VHA,” they wrote, concluding that “the VHA may serve as a vantage point for detecting nationwide trends in antimicrobial drug resistance” (Emerg Infect Dis. 2017 Mar. doi: 10.3201/eid2305.162034).
Veterans Health Administration monitoring of carbapenem-resistant Enterobacteriaceae (CRE) trends from 2006 to 2015 shows a rise in resistance rates of E. cloacae complex nationwide.
The first major CRE outbreak, Klebsiella pneumoniae, occurred in the eastern United States in the early 2000s and has since spread across the country. K. pneumoniae has recently shown a decrease in resistance rates in the region including New York, both in the current VHA-based study and in a 2016 study of three New York City hospitals.
“CRE trends during 2006-2015 in the VHA recapitulate the epidemic of carbapenem-resistant K. pneumoniae in the United States and indicate that a ‘second epidemic’ of carbapenem-resistant E. cloacae complex appears to be unfolding,” wrote Brigid M. Wilson, PhD, of Louis Stokes Cleveland Department of Veterans Affairs Medical Center, and her coauthors.
The researchers used VHA network data to identify 128,431 K. pneumoniae and 38,219 E. cloacae complex (which refers to the species E. cloacae, E. asburiae, E. kobei, E. hormaechei, and E. xiafangensis) isolates from patients hospitalized in 140 facilities in 40 states, the District of Columbia, and Puerto Rico from 2006 to 2015. These isolates, paired with their carbapenem susceptibility test results, show the rise and geographic concentration of the CRE cases over the decade.
The increased E. cloacae complex resistance in 2014-2015 was centered around the Pacific Coast and Southwest regions. The researchers noted that E. cloacae complex has a less well defined genetic makeup, compared with K. pneumoniae.
“We hypothesize that E. cloacae complex contains genotypes with epidemic potential associated with increasing rates of carbapenem resistance observed in the VHA,” they wrote, concluding that “the VHA may serve as a vantage point for detecting nationwide trends in antimicrobial drug resistance” (Emerg Infect Dis. 2017 Mar. doi: 10.3201/eid2305.162034).
Veterans Health Administration monitoring of carbapenem-resistant Enterobacteriaceae (CRE) trends from 2006 to 2015 shows a rise in resistance rates of E. cloacae complex nationwide.
The first major CRE outbreak, Klebsiella pneumoniae, occurred in the eastern United States in the early 2000s and has since spread across the country. K. pneumoniae has recently shown a decrease in resistance rates in the region including New York, both in the current VHA-based study and in a 2016 study of three New York City hospitals.
“CRE trends during 2006-2015 in the VHA recapitulate the epidemic of carbapenem-resistant K. pneumoniae in the United States and indicate that a ‘second epidemic’ of carbapenem-resistant E. cloacae complex appears to be unfolding,” wrote Brigid M. Wilson, PhD, of Louis Stokes Cleveland Department of Veterans Affairs Medical Center, and her coauthors.
The researchers used VHA network data to identify 128,431 K. pneumoniae and 38,219 E. cloacae complex (which refers to the species E. cloacae, E. asburiae, E. kobei, E. hormaechei, and E. xiafangensis) isolates from patients hospitalized in 140 facilities in 40 states, the District of Columbia, and Puerto Rico from 2006 to 2015. These isolates, paired with their carbapenem susceptibility test results, show the rise and geographic concentration of the CRE cases over the decade.
The increased E. cloacae complex resistance in 2014-2015 was centered around the Pacific Coast and Southwest regions. The researchers noted that E. cloacae complex has a less well defined genetic makeup, compared with K. pneumoniae.
“We hypothesize that E. cloacae complex contains genotypes with epidemic potential associated with increasing rates of carbapenem resistance observed in the VHA,” they wrote, concluding that “the VHA may serve as a vantage point for detecting nationwide trends in antimicrobial drug resistance” (Emerg Infect Dis. 2017 Mar. doi: 10.3201/eid2305.162034).
Monotherapy as good as combo for antibiotic-resistant infections in low-risk patients
VIENNA – A single, well-targeted antibiotic may be enough to effectively combat serous bloodstream infections in patients who have a low baseline mortality risk.
Among these patients, overall mortality was similar among those receiving a single antibiotic and those getting multiple antibiotics (35% vs. 41%). Patients with a high baseline mortality risk, however, did experience a significant 44% survival benefit when treated with a combination regimen, Jesus Rodríguez-Baño, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
The finding is important when considering the ever-increasing imperative of antibiotic stewardship, Dr. Rodríguez-Baño said in an interview.
“In areas where these pathogens are common, particularly in intensive care units, where they can become epidemic and infect many patients, the overuse of combination therapy will be fueling the problem,” said Dr. Rodríguez-Baño, head of infectious diseases and clinical microbiology at the University Hospital Virgin Macarena, Seville, Spain. “This is a way to avoid the overuse of some broad-spectrum antibiotics. Selecting the patients who should not receive combination therapy may significantly reduce the total consumption” on a unit.
The retrospective study, dubbed INCREMENT, was conducted at 37 hospitals in 10 countries. It enrolled patients with bloodstream infections caused by extended-spectrum beta-lactamase- or carbapenemase-producing Enterobacteriaceae. Dr. Rodríguez-Baño reported results for 437 patients whose infections were caused by the carbapenemase-producing strain.
It was simultaneously published in Lancet Infectious Diseases (Lancet Inf Dis 2017; DOI: http://dx.doi.org/10.1016/S1473-3099(17)30228-1).
These patients were a mean of 66 years old; most (60%) were male. The primary infective agent was Klebsiella pneumonia (86%); most infections were nosocomial. The origin of infections varied, but most (80%) arose from places other than the urinary or biliary tract. Sources were vascular catheters, pneumonia, intraabdominal, and skin and soft tissue. About half of the patients were in severe sepsis or septic shock when treated.
The group was first divided into those who received appropriate or inappropriate therapy (78% vs. 22%). Appropriate therapy was considered to be the early administration of a drug that could effectively target the infective organism. Next, those who got appropriate therapy were parsed by whether they received mono- or combination therapy (61%, 39%). Finally, these patients were stratified by a specially designed mortality risk score, the INCREMENT Carbapenemase-Producing Enterobacteriaceae (CPE) Mortality Score (Mayo Clinic Proceedings. doi.org/10.1016/j.mayocp.2016.06.024).
- Severe sepsis or shock at presentation (5 points)
- Pitt score of 6 or more (4 points)
- Charlson comorbidity index of 2 or more (3 points)
- Source of bloodstream infection other than urinary or biliary tract (3 points)
- Inappropriate empirical therapy and inappropriate early targeted therapy (2 points)
Patients were considered low risk if they had a score of 0-7, and high of they had a score of 8 or more.
The risk assessment took is quick, easy to figure, and extremely important, Dr. Rodríguez-Baño noted. “This is a very easy-to-use tool that can help us make many patient management decisions. All of the information is already available in the patient’s chart, so it doesn’t require any additional assessments. It’s a very good way to individualize treatment.”
In the initial analysis, all-cause mortality at 30 days was 22% lower among patients who received appropriate early therapy than those who did not (38.5% vs. 60.6%). This translated to a 55% decrease in the risk of death (HR 0.45 in the fully adjusted model).
The investigators next turned their attention toward the group that received appropriate therapy. All-cause 30-day mortality was 41% in those who got monotherapy and 34.8% among those who got combination therapy..
Finally, this group was stratified according to the INCREMENT-CPE mortality risk score.
In the low-risk category, combination therapy did not confer a survival advantage over monotherapy. Death occurred in 20% of those getting monotherapy and 24% receiving combination treatment – not a significant difference (HR 1.21).
Combination therapy did, however, confer a significant survival benefit in the high-risk group. Death occurred in 62% of those receiving monotherapy and 48% of those receiving combination therapy – a 44% risk reduction (HR 0.56).
As long as they were appropriately targeted against the infective organism, all drugs used in the high-mortality risk group were similarly effective at reducing the risk of death. Compared to colistin monotherapy, a combination that included tigecycline reduced the risk of death by 55% (HR 0.45); combination with aminoglycosides by 58% (HR 0.42); and combination with carbapenems by 44% (HR 0.56).
A secondary analysis of this group determined that time was a critical factor in survival. Each day delay after day 2 significantly increased the risk of death, Dr. Rodríguez-Baño said. This 48-hour period gives clinicians a chance to wait for the culture and antibiogram to return, and then choose and initiate the best treatment. Before the results come back, empiric antibiotic therapy is appropriate, but changes should be made immediately after the results come back.
“We tend to think we must give the very best antibiotic at the very first moment that we see a patient with a serious infection,” he said. “But what we found is that it’s not critical to give the perfect antibiotic on the first day. It is critical, however, to give the correct one once you know which bacteria is causing the infection. Since it takes 48 hours for those results to come back, this is perfect timing.”
INCREMENT was funded in large part by the Spanish Network for Research in Infectious Diseases. Dr. Rodríguez-Baño has been a scientific advisor for Merck, AstraZeneca, and InfectoPharm.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
VIENNA – A single, well-targeted antibiotic may be enough to effectively combat serous bloodstream infections in patients who have a low baseline mortality risk.
Among these patients, overall mortality was similar among those receiving a single antibiotic and those getting multiple antibiotics (35% vs. 41%). Patients with a high baseline mortality risk, however, did experience a significant 44% survival benefit when treated with a combination regimen, Jesus Rodríguez-Baño, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
The finding is important when considering the ever-increasing imperative of antibiotic stewardship, Dr. Rodríguez-Baño said in an interview.
“In areas where these pathogens are common, particularly in intensive care units, where they can become epidemic and infect many patients, the overuse of combination therapy will be fueling the problem,” said Dr. Rodríguez-Baño, head of infectious diseases and clinical microbiology at the University Hospital Virgin Macarena, Seville, Spain. “This is a way to avoid the overuse of some broad-spectrum antibiotics. Selecting the patients who should not receive combination therapy may significantly reduce the total consumption” on a unit.
The retrospective study, dubbed INCREMENT, was conducted at 37 hospitals in 10 countries. It enrolled patients with bloodstream infections caused by extended-spectrum beta-lactamase- or carbapenemase-producing Enterobacteriaceae. Dr. Rodríguez-Baño reported results for 437 patients whose infections were caused by the carbapenemase-producing strain.
It was simultaneously published in Lancet Infectious Diseases (Lancet Inf Dis 2017; DOI: http://dx.doi.org/10.1016/S1473-3099(17)30228-1).
These patients were a mean of 66 years old; most (60%) were male. The primary infective agent was Klebsiella pneumonia (86%); most infections were nosocomial. The origin of infections varied, but most (80%) arose from places other than the urinary or biliary tract. Sources were vascular catheters, pneumonia, intraabdominal, and skin and soft tissue. About half of the patients were in severe sepsis or septic shock when treated.
The group was first divided into those who received appropriate or inappropriate therapy (78% vs. 22%). Appropriate therapy was considered to be the early administration of a drug that could effectively target the infective organism. Next, those who got appropriate therapy were parsed by whether they received mono- or combination therapy (61%, 39%). Finally, these patients were stratified by a specially designed mortality risk score, the INCREMENT Carbapenemase-Producing Enterobacteriaceae (CPE) Mortality Score (Mayo Clinic Proceedings. doi.org/10.1016/j.mayocp.2016.06.024).
- Severe sepsis or shock at presentation (5 points)
- Pitt score of 6 or more (4 points)
- Charlson comorbidity index of 2 or more (3 points)
- Source of bloodstream infection other than urinary or biliary tract (3 points)
- Inappropriate empirical therapy and inappropriate early targeted therapy (2 points)
Patients were considered low risk if they had a score of 0-7, and high of they had a score of 8 or more.
The risk assessment took is quick, easy to figure, and extremely important, Dr. Rodríguez-Baño noted. “This is a very easy-to-use tool that can help us make many patient management decisions. All of the information is already available in the patient’s chart, so it doesn’t require any additional assessments. It’s a very good way to individualize treatment.”
In the initial analysis, all-cause mortality at 30 days was 22% lower among patients who received appropriate early therapy than those who did not (38.5% vs. 60.6%). This translated to a 55% decrease in the risk of death (HR 0.45 in the fully adjusted model).
The investigators next turned their attention toward the group that received appropriate therapy. All-cause 30-day mortality was 41% in those who got monotherapy and 34.8% among those who got combination therapy..
Finally, this group was stratified according to the INCREMENT-CPE mortality risk score.
In the low-risk category, combination therapy did not confer a survival advantage over monotherapy. Death occurred in 20% of those getting monotherapy and 24% receiving combination treatment – not a significant difference (HR 1.21).
Combination therapy did, however, confer a significant survival benefit in the high-risk group. Death occurred in 62% of those receiving monotherapy and 48% of those receiving combination therapy – a 44% risk reduction (HR 0.56).
As long as they were appropriately targeted against the infective organism, all drugs used in the high-mortality risk group were similarly effective at reducing the risk of death. Compared to colistin monotherapy, a combination that included tigecycline reduced the risk of death by 55% (HR 0.45); combination with aminoglycosides by 58% (HR 0.42); and combination with carbapenems by 44% (HR 0.56).
A secondary analysis of this group determined that time was a critical factor in survival. Each day delay after day 2 significantly increased the risk of death, Dr. Rodríguez-Baño said. This 48-hour period gives clinicians a chance to wait for the culture and antibiogram to return, and then choose and initiate the best treatment. Before the results come back, empiric antibiotic therapy is appropriate, but changes should be made immediately after the results come back.
“We tend to think we must give the very best antibiotic at the very first moment that we see a patient with a serious infection,” he said. “But what we found is that it’s not critical to give the perfect antibiotic on the first day. It is critical, however, to give the correct one once you know which bacteria is causing the infection. Since it takes 48 hours for those results to come back, this is perfect timing.”
INCREMENT was funded in large part by the Spanish Network for Research in Infectious Diseases. Dr. Rodríguez-Baño has been a scientific advisor for Merck, AstraZeneca, and InfectoPharm.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
VIENNA – A single, well-targeted antibiotic may be enough to effectively combat serous bloodstream infections in patients who have a low baseline mortality risk.
Among these patients, overall mortality was similar among those receiving a single antibiotic and those getting multiple antibiotics (35% vs. 41%). Patients with a high baseline mortality risk, however, did experience a significant 44% survival benefit when treated with a combination regimen, Jesus Rodríguez-Baño, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
The finding is important when considering the ever-increasing imperative of antibiotic stewardship, Dr. Rodríguez-Baño said in an interview.
“In areas where these pathogens are common, particularly in intensive care units, where they can become epidemic and infect many patients, the overuse of combination therapy will be fueling the problem,” said Dr. Rodríguez-Baño, head of infectious diseases and clinical microbiology at the University Hospital Virgin Macarena, Seville, Spain. “This is a way to avoid the overuse of some broad-spectrum antibiotics. Selecting the patients who should not receive combination therapy may significantly reduce the total consumption” on a unit.
The retrospective study, dubbed INCREMENT, was conducted at 37 hospitals in 10 countries. It enrolled patients with bloodstream infections caused by extended-spectrum beta-lactamase- or carbapenemase-producing Enterobacteriaceae. Dr. Rodríguez-Baño reported results for 437 patients whose infections were caused by the carbapenemase-producing strain.
It was simultaneously published in Lancet Infectious Diseases (Lancet Inf Dis 2017; DOI: http://dx.doi.org/10.1016/S1473-3099(17)30228-1).
These patients were a mean of 66 years old; most (60%) were male. The primary infective agent was Klebsiella pneumonia (86%); most infections were nosocomial. The origin of infections varied, but most (80%) arose from places other than the urinary or biliary tract. Sources were vascular catheters, pneumonia, intraabdominal, and skin and soft tissue. About half of the patients were in severe sepsis or septic shock when treated.
The group was first divided into those who received appropriate or inappropriate therapy (78% vs. 22%). Appropriate therapy was considered to be the early administration of a drug that could effectively target the infective organism. Next, those who got appropriate therapy were parsed by whether they received mono- or combination therapy (61%, 39%). Finally, these patients were stratified by a specially designed mortality risk score, the INCREMENT Carbapenemase-Producing Enterobacteriaceae (CPE) Mortality Score (Mayo Clinic Proceedings. doi.org/10.1016/j.mayocp.2016.06.024).
- Severe sepsis or shock at presentation (5 points)
- Pitt score of 6 or more (4 points)
- Charlson comorbidity index of 2 or more (3 points)
- Source of bloodstream infection other than urinary or biliary tract (3 points)
- Inappropriate empirical therapy and inappropriate early targeted therapy (2 points)
Patients were considered low risk if they had a score of 0-7, and high of they had a score of 8 or more.
The risk assessment took is quick, easy to figure, and extremely important, Dr. Rodríguez-Baño noted. “This is a very easy-to-use tool that can help us make many patient management decisions. All of the information is already available in the patient’s chart, so it doesn’t require any additional assessments. It’s a very good way to individualize treatment.”
In the initial analysis, all-cause mortality at 30 days was 22% lower among patients who received appropriate early therapy than those who did not (38.5% vs. 60.6%). This translated to a 55% decrease in the risk of death (HR 0.45 in the fully adjusted model).
The investigators next turned their attention toward the group that received appropriate therapy. All-cause 30-day mortality was 41% in those who got monotherapy and 34.8% among those who got combination therapy..
Finally, this group was stratified according to the INCREMENT-CPE mortality risk score.
In the low-risk category, combination therapy did not confer a survival advantage over monotherapy. Death occurred in 20% of those getting monotherapy and 24% receiving combination treatment – not a significant difference (HR 1.21).
Combination therapy did, however, confer a significant survival benefit in the high-risk group. Death occurred in 62% of those receiving monotherapy and 48% of those receiving combination therapy – a 44% risk reduction (HR 0.56).
As long as they were appropriately targeted against the infective organism, all drugs used in the high-mortality risk group were similarly effective at reducing the risk of death. Compared to colistin monotherapy, a combination that included tigecycline reduced the risk of death by 55% (HR 0.45); combination with aminoglycosides by 58% (HR 0.42); and combination with carbapenems by 44% (HR 0.56).
A secondary analysis of this group determined that time was a critical factor in survival. Each day delay after day 2 significantly increased the risk of death, Dr. Rodríguez-Baño said. This 48-hour period gives clinicians a chance to wait for the culture and antibiogram to return, and then choose and initiate the best treatment. Before the results come back, empiric antibiotic therapy is appropriate, but changes should be made immediately after the results come back.
“We tend to think we must give the very best antibiotic at the very first moment that we see a patient with a serious infection,” he said. “But what we found is that it’s not critical to give the perfect antibiotic on the first day. It is critical, however, to give the correct one once you know which bacteria is causing the infection. Since it takes 48 hours for those results to come back, this is perfect timing.”
INCREMENT was funded in large part by the Spanish Network for Research in Infectious Diseases. Dr. Rodríguez-Baño has been a scientific advisor for Merck, AstraZeneca, and InfectoPharm.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
Key clinical point:
Major finding: Among these patients, correctly targeted monotherapy decreased the risk of death by 44% – just about the same risk reduction as conferred by combination therapy.
Data source: The INCREMENT retrospective study comprised 437 patients.
Disclosures: INCREMENT was funded in large part by the Spanish Network for Research in Infectious Diseases. Dr. Rodríguez-Baño has been a scientific advisor for Merck, AstraZeneca, and InfectoPharm.
Plazomicin beats gold standard antibiotics in complex, gram-negative bacterial infections
VIENNA – An investigational antibiotic effective against several types of gram-negative antibiotic-resistant bacteria has proved its mettle against serious infections of the urinary tract, respiratory tract, and bloodstream.
Plazomicin (Achaogen, San Francisco) posted good results in two phase III studies, handily besting comparator drugs considered gold standard for treating complicated urinary tract infections and pyelonephritis, as well as bloodstream infections and hospital- and ventilator-associated bacterial pneumonia.
Both the EPIC (Evaluating Plazomicin In cUTI) and CARE (Combating Antibiotic Resistant Enterobacteriaceae) trials have provided enough positive data for the company to move forward with a new drug application later this year. The company also plans to seek European Medicines Agency approval in 2018.
Plazomicin is an aminoglycoside that has been modified with several side chains that block aminoglycoside-modifying enzymes, Daniel Cloutier, PhD, principal clinical scientist of Achaogen said at the European Society of Clinical Microbiology and Infectious Disease annual congress.
“Aminoglycoside enzymes tend to travel along with beta-lactamases and carbapenemases as well, so this drug retains potent bactericidal activity against extended spectrum beta-lactamase producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and aminoglycoside-resistant Enterobacteriaceae,” said Dr. Cloutier, who presented the results of the EPIC trial. The drug is given once-daily as a 30-minute intravenous infusion.
EPIC enrolled 609 adult patients with complicated urinary tract infections or acute pyelonephritis; Dr. Cloutier presented a modified intent-to-treat analysis comprising 388 of these. They were randomized to plazomicin 15 mg/kg every 25 hours or to IV meropenem 1 gram every 24 hours. Treatment proceeded for 4-7 days, after which patients could step down to oral therapy (levofloxacin 500 m/day), for a total of 7-10 days of treatment. About 80% of patients had both IV and oral therapy. At 15-19 days from the first dose, patients had a test of cure; at 24-32 days from first dose, they returned for a safety follow-up.
Patients were a mean of 60 years old. About 60% had a complicated UTI; the rest had acute pyelonephritis. About 35% had a mean creatinine clearance of more than 30-60 mL/min; the rest had a mean clearance of more than 60-90 mL/min.
The primary efficacy endpoint was microbial eradication. Plazomicin performed significantly better than meropenem in this measure (87% vs.72%), a mean difference of about 15%. Patients with pyelonephritis responded marginally better than those with complicated UTI, both groups favoring plazomicin (mean treatment differences of 17.5% and 13.7%, respectively).
The results were similar when the investigators examined groups by whether they needed oral step-down treatment. In the IV-only groups, plazomicin bested meropenem in microbiological eradication by almost 19% (84% vs. 65%). In the IV plus oral therapy group, the mean difference was 14%, also in favor of plazomicin (88% vs. 74%).
Plazomicin was significantly more effective then meropenem in all of the resistant Enterobacteriaceae groups (ESBL-positive, and levofloxacin- and aminoglycoside-resistant). It was also significantly more effective against E. coli (17% treatment difference), Klebsiella pneumonia (9%), and Proteus mirabilis (25%). However, it was 20% less effective than meropenem against E. cloacae.
At late follow-up, 2% of the plazomicin group and 8% of the meropenem group had relapsed – a significant difference.
Plazomicin and meropenem had similar safety profiles. Diarrhea and hypertension were the most common adverse events (about 2% in each group). Headache occurred in 3% of the meropenem patients and 1% of the plazomicin patients. Nausea, vomiting, and anemia occurred in about 1% of each group.
More patients taking plazomicin experienced a serum creatinine clearance increase of at least 0.5 mg/dL during treatment (7% vs. 4%). All but two patients taking plazomicin experienced a full recovery by the last follow-up visit.
The CARE trial was much smaller, comprised of 39 patients who had either bloodstream infections, or hospital-acquired or ventilator-associated bacterial pneumonia caused by carbapenem-resistant Enterobacteriaceae. Lynn Connolly, MD, senior medical director and head of late development at Achaogen, presented the data. Recruitment for such a narrow diagnosis was difficult, and hampered patient accrual, she noted.
CARE’s primary endpoints were a combination of all-cause mortality and significant disease-related complications, and all-cause mortality only, both at 28 days.
Patients were randomized 1:1 to either plazomicin 15 mg/kg every 24 hours, or colistin in a 300-mg loading dose, followed by daily infusions of 5 mg/kg. Everyone, regardless of treatment group, could also receive meropenem or tigecycline if deemed necessary. Treatment lasted 7-14 days. There was a test of cure at 7 days from the last IV dose, a safety assessment at 28 days, and a long-term follow-up at 60 days.
The patients’ mean age was about 65 years. Most (about 80%) had a bloodstream infection; bacterial pneumonias were present in the remainder. Most infections (85%) were monomicrobial, with polymicrobial infections making up the balance. Tigecycline was the favored adjunctive therapy (60%), followed by meropenem.
At day 28, plazomicin was associated with significantly better overall outcomes than colistin. It reduced the combination mortality/significant disease complications endpoint by 26% (23% vs. 50% meropenem). This translated to a 53% relative reduction in the risk of death.
Plazomicin also reduced all-cause mortality only by 28% (12% vs. 40% meropenem). This translated to a relative risk reduction of 70.5%.
The study drug performed well in the subgroup of patients with bloodstream infections, reducing the occurrence of the composite endpoint by 39% (14% vs. 53%), and of the mortality-only endpoint by 33% (7% vs. 40%). This translated to a 63% increased chance of 60-day survival in the plazomicin group.
Almost all patients in each group experienced at least one adverse event; 28% were deemed related to plazomicin and 43% to colistin. Many of these events were related to renal function (33% plazomicin, 52% colistin). Serum creatinine increases of at least 0.5 mg/dL during IV treatment occurred in fewer taking plazomicin (1 vs. 6 taking colistin). Full renal recovery occurred in the patient taking plazomicin, but only in three taking colistin.
“These data suggest that plazomicin could offer an important new treatment option for patients with serious infections due to carbapenem-resistant Enterobacteriaceae,” Dr. Connolly said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
VIENNA – An investigational antibiotic effective against several types of gram-negative antibiotic-resistant bacteria has proved its mettle against serious infections of the urinary tract, respiratory tract, and bloodstream.
Plazomicin (Achaogen, San Francisco) posted good results in two phase III studies, handily besting comparator drugs considered gold standard for treating complicated urinary tract infections and pyelonephritis, as well as bloodstream infections and hospital- and ventilator-associated bacterial pneumonia.
Both the EPIC (Evaluating Plazomicin In cUTI) and CARE (Combating Antibiotic Resistant Enterobacteriaceae) trials have provided enough positive data for the company to move forward with a new drug application later this year. The company also plans to seek European Medicines Agency approval in 2018.
Plazomicin is an aminoglycoside that has been modified with several side chains that block aminoglycoside-modifying enzymes, Daniel Cloutier, PhD, principal clinical scientist of Achaogen said at the European Society of Clinical Microbiology and Infectious Disease annual congress.
“Aminoglycoside enzymes tend to travel along with beta-lactamases and carbapenemases as well, so this drug retains potent bactericidal activity against extended spectrum beta-lactamase producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and aminoglycoside-resistant Enterobacteriaceae,” said Dr. Cloutier, who presented the results of the EPIC trial. The drug is given once-daily as a 30-minute intravenous infusion.
EPIC enrolled 609 adult patients with complicated urinary tract infections or acute pyelonephritis; Dr. Cloutier presented a modified intent-to-treat analysis comprising 388 of these. They were randomized to plazomicin 15 mg/kg every 25 hours or to IV meropenem 1 gram every 24 hours. Treatment proceeded for 4-7 days, after which patients could step down to oral therapy (levofloxacin 500 m/day), for a total of 7-10 days of treatment. About 80% of patients had both IV and oral therapy. At 15-19 days from the first dose, patients had a test of cure; at 24-32 days from first dose, they returned for a safety follow-up.
Patients were a mean of 60 years old. About 60% had a complicated UTI; the rest had acute pyelonephritis. About 35% had a mean creatinine clearance of more than 30-60 mL/min; the rest had a mean clearance of more than 60-90 mL/min.
The primary efficacy endpoint was microbial eradication. Plazomicin performed significantly better than meropenem in this measure (87% vs.72%), a mean difference of about 15%. Patients with pyelonephritis responded marginally better than those with complicated UTI, both groups favoring plazomicin (mean treatment differences of 17.5% and 13.7%, respectively).
The results were similar when the investigators examined groups by whether they needed oral step-down treatment. In the IV-only groups, plazomicin bested meropenem in microbiological eradication by almost 19% (84% vs. 65%). In the IV plus oral therapy group, the mean difference was 14%, also in favor of plazomicin (88% vs. 74%).
Plazomicin was significantly more effective then meropenem in all of the resistant Enterobacteriaceae groups (ESBL-positive, and levofloxacin- and aminoglycoside-resistant). It was also significantly more effective against E. coli (17% treatment difference), Klebsiella pneumonia (9%), and Proteus mirabilis (25%). However, it was 20% less effective than meropenem against E. cloacae.
At late follow-up, 2% of the plazomicin group and 8% of the meropenem group had relapsed – a significant difference.
Plazomicin and meropenem had similar safety profiles. Diarrhea and hypertension were the most common adverse events (about 2% in each group). Headache occurred in 3% of the meropenem patients and 1% of the plazomicin patients. Nausea, vomiting, and anemia occurred in about 1% of each group.
More patients taking plazomicin experienced a serum creatinine clearance increase of at least 0.5 mg/dL during treatment (7% vs. 4%). All but two patients taking plazomicin experienced a full recovery by the last follow-up visit.
The CARE trial was much smaller, comprised of 39 patients who had either bloodstream infections, or hospital-acquired or ventilator-associated bacterial pneumonia caused by carbapenem-resistant Enterobacteriaceae. Lynn Connolly, MD, senior medical director and head of late development at Achaogen, presented the data. Recruitment for such a narrow diagnosis was difficult, and hampered patient accrual, she noted.
CARE’s primary endpoints were a combination of all-cause mortality and significant disease-related complications, and all-cause mortality only, both at 28 days.
Patients were randomized 1:1 to either plazomicin 15 mg/kg every 24 hours, or colistin in a 300-mg loading dose, followed by daily infusions of 5 mg/kg. Everyone, regardless of treatment group, could also receive meropenem or tigecycline if deemed necessary. Treatment lasted 7-14 days. There was a test of cure at 7 days from the last IV dose, a safety assessment at 28 days, and a long-term follow-up at 60 days.
The patients’ mean age was about 65 years. Most (about 80%) had a bloodstream infection; bacterial pneumonias were present in the remainder. Most infections (85%) were monomicrobial, with polymicrobial infections making up the balance. Tigecycline was the favored adjunctive therapy (60%), followed by meropenem.
At day 28, plazomicin was associated with significantly better overall outcomes than colistin. It reduced the combination mortality/significant disease complications endpoint by 26% (23% vs. 50% meropenem). This translated to a 53% relative reduction in the risk of death.
Plazomicin also reduced all-cause mortality only by 28% (12% vs. 40% meropenem). This translated to a relative risk reduction of 70.5%.
The study drug performed well in the subgroup of patients with bloodstream infections, reducing the occurrence of the composite endpoint by 39% (14% vs. 53%), and of the mortality-only endpoint by 33% (7% vs. 40%). This translated to a 63% increased chance of 60-day survival in the plazomicin group.
Almost all patients in each group experienced at least one adverse event; 28% were deemed related to plazomicin and 43% to colistin. Many of these events were related to renal function (33% plazomicin, 52% colistin). Serum creatinine increases of at least 0.5 mg/dL during IV treatment occurred in fewer taking plazomicin (1 vs. 6 taking colistin). Full renal recovery occurred in the patient taking plazomicin, but only in three taking colistin.
“These data suggest that plazomicin could offer an important new treatment option for patients with serious infections due to carbapenem-resistant Enterobacteriaceae,” Dr. Connolly said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
VIENNA – An investigational antibiotic effective against several types of gram-negative antibiotic-resistant bacteria has proved its mettle against serious infections of the urinary tract, respiratory tract, and bloodstream.
Plazomicin (Achaogen, San Francisco) posted good results in two phase III studies, handily besting comparator drugs considered gold standard for treating complicated urinary tract infections and pyelonephritis, as well as bloodstream infections and hospital- and ventilator-associated bacterial pneumonia.
Both the EPIC (Evaluating Plazomicin In cUTI) and CARE (Combating Antibiotic Resistant Enterobacteriaceae) trials have provided enough positive data for the company to move forward with a new drug application later this year. The company also plans to seek European Medicines Agency approval in 2018.
Plazomicin is an aminoglycoside that has been modified with several side chains that block aminoglycoside-modifying enzymes, Daniel Cloutier, PhD, principal clinical scientist of Achaogen said at the European Society of Clinical Microbiology and Infectious Disease annual congress.
“Aminoglycoside enzymes tend to travel along with beta-lactamases and carbapenemases as well, so this drug retains potent bactericidal activity against extended spectrum beta-lactamase producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and aminoglycoside-resistant Enterobacteriaceae,” said Dr. Cloutier, who presented the results of the EPIC trial. The drug is given once-daily as a 30-minute intravenous infusion.
EPIC enrolled 609 adult patients with complicated urinary tract infections or acute pyelonephritis; Dr. Cloutier presented a modified intent-to-treat analysis comprising 388 of these. They were randomized to plazomicin 15 mg/kg every 25 hours or to IV meropenem 1 gram every 24 hours. Treatment proceeded for 4-7 days, after which patients could step down to oral therapy (levofloxacin 500 m/day), for a total of 7-10 days of treatment. About 80% of patients had both IV and oral therapy. At 15-19 days from the first dose, patients had a test of cure; at 24-32 days from first dose, they returned for a safety follow-up.
Patients were a mean of 60 years old. About 60% had a complicated UTI; the rest had acute pyelonephritis. About 35% had a mean creatinine clearance of more than 30-60 mL/min; the rest had a mean clearance of more than 60-90 mL/min.
The primary efficacy endpoint was microbial eradication. Plazomicin performed significantly better than meropenem in this measure (87% vs.72%), a mean difference of about 15%. Patients with pyelonephritis responded marginally better than those with complicated UTI, both groups favoring plazomicin (mean treatment differences of 17.5% and 13.7%, respectively).
The results were similar when the investigators examined groups by whether they needed oral step-down treatment. In the IV-only groups, plazomicin bested meropenem in microbiological eradication by almost 19% (84% vs. 65%). In the IV plus oral therapy group, the mean difference was 14%, also in favor of plazomicin (88% vs. 74%).
Plazomicin was significantly more effective then meropenem in all of the resistant Enterobacteriaceae groups (ESBL-positive, and levofloxacin- and aminoglycoside-resistant). It was also significantly more effective against E. coli (17% treatment difference), Klebsiella pneumonia (9%), and Proteus mirabilis (25%). However, it was 20% less effective than meropenem against E. cloacae.
At late follow-up, 2% of the plazomicin group and 8% of the meropenem group had relapsed – a significant difference.
Plazomicin and meropenem had similar safety profiles. Diarrhea and hypertension were the most common adverse events (about 2% in each group). Headache occurred in 3% of the meropenem patients and 1% of the plazomicin patients. Nausea, vomiting, and anemia occurred in about 1% of each group.
More patients taking plazomicin experienced a serum creatinine clearance increase of at least 0.5 mg/dL during treatment (7% vs. 4%). All but two patients taking plazomicin experienced a full recovery by the last follow-up visit.
The CARE trial was much smaller, comprised of 39 patients who had either bloodstream infections, or hospital-acquired or ventilator-associated bacterial pneumonia caused by carbapenem-resistant Enterobacteriaceae. Lynn Connolly, MD, senior medical director and head of late development at Achaogen, presented the data. Recruitment for such a narrow diagnosis was difficult, and hampered patient accrual, she noted.
CARE’s primary endpoints were a combination of all-cause mortality and significant disease-related complications, and all-cause mortality only, both at 28 days.
Patients were randomized 1:1 to either plazomicin 15 mg/kg every 24 hours, or colistin in a 300-mg loading dose, followed by daily infusions of 5 mg/kg. Everyone, regardless of treatment group, could also receive meropenem or tigecycline if deemed necessary. Treatment lasted 7-14 days. There was a test of cure at 7 days from the last IV dose, a safety assessment at 28 days, and a long-term follow-up at 60 days.
The patients’ mean age was about 65 years. Most (about 80%) had a bloodstream infection; bacterial pneumonias were present in the remainder. Most infections (85%) were monomicrobial, with polymicrobial infections making up the balance. Tigecycline was the favored adjunctive therapy (60%), followed by meropenem.
At day 28, plazomicin was associated with significantly better overall outcomes than colistin. It reduced the combination mortality/significant disease complications endpoint by 26% (23% vs. 50% meropenem). This translated to a 53% relative reduction in the risk of death.
Plazomicin also reduced all-cause mortality only by 28% (12% vs. 40% meropenem). This translated to a relative risk reduction of 70.5%.
The study drug performed well in the subgroup of patients with bloodstream infections, reducing the occurrence of the composite endpoint by 39% (14% vs. 53%), and of the mortality-only endpoint by 33% (7% vs. 40%). This translated to a 63% increased chance of 60-day survival in the plazomicin group.
Almost all patients in each group experienced at least one adverse event; 28% were deemed related to plazomicin and 43% to colistin. Many of these events were related to renal function (33% plazomicin, 52% colistin). Serum creatinine increases of at least 0.5 mg/dL during IV treatment occurred in fewer taking plazomicin (1 vs. 6 taking colistin). Full renal recovery occurred in the patient taking plazomicin, but only in three taking colistin.
“These data suggest that plazomicin could offer an important new treatment option for patients with serious infections due to carbapenem-resistant Enterobacteriaceae,” Dr. Connolly said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
CDC: Some Shigella strains show reduced ciprofloxacin susceptibility
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.