User login
Researchers honored by ACS, IASLC
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
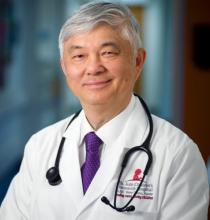
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
Phase 2 data: Inotuzumab, approved in adults with B-ALL, shows promise in kids, too
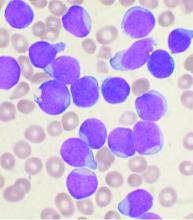
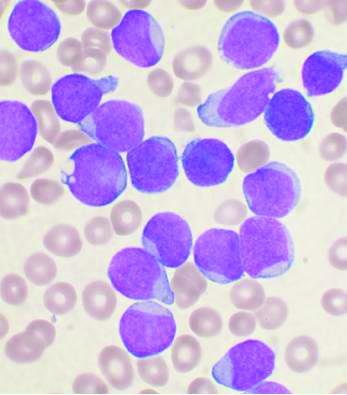
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
REPORTING FROM ASH 2019
Phase 2 study shows regimen benefit with dasatinib in Ph+ALL therapy
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
REPORTING FROM ASH 2019
UKALL14: Rituximab improves EFS in B-ALL, but four doses not enough
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
REPORTING FROM ASH 2019
Promising early efficacy of venetoclax/navitoclax in r/r acute lymphoblastic leukemia
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
REPORTING FROM ASH 2019
Chemo-free induction-consolidation protocol for Ph+ ALL improved survival
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
REPORTING FROM ASH 2019
High response, survival rates with ponatinib/hCVAD in Ph-positive ALL
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
ORLANDO – For adults with newly diagnosed acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL), the combination of hyper-CVAD chemotherapy and ponatinib is associated with high complete molecular response and 5-year overall survival rates, investigators reported.
Long-term follow-up of 86 adults with Ph+ALL treated in the front line with chemotherapy plus ponatinib (Iclusig), a third-generation tyrosine kinase inhibitor (TKI), showed a complete remission (CR) rate of 100%, complete molecular remission (CMR) rate of 86%, and a 5-year overall survival (OS) rate of 74%, reported Nicholas J. Short, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Although we observed two treatment-related cardiovascular deaths with the original trial design, with almost 50 patients treated since instituting a risk-adapted dosing schedule with lower doses of ponatinib, no additional ponatinib-related deaths have been observed,” he said at the annual meeting of the American Society of Hematology.
The standard of care for adults with Ph+ALL is chemotherapy plus a TKI. With a first- or second-generation TKI plus chemotherapy, reported 5-year OS rates range from 35% to 50%.
“However, relapses are still common, and these are usually driven by the development of new resistance mutations in the ABL gene, particularly the T315I gatekeeper mutation which has been reported in up to 75% of patients at the time of relapse,” he said.
Ponatinib is a pan-BCR-ABL TKI with activity against ALL with T315I mutations, and the combination of this agent with hyper-CVAD chemotherapy (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) has been associated with higher response rates than those seen with earlier-generation TKIs, as well as higher levels of minimal residual disease (MRD) negativity, he noted.
Dr. Short and colleagues hypothesized that, compared with the standard of care, hyper-CVAD plus ponatinib would be associated with higher MRD levels, low relapse rates by suppression of T315I subclones, decreased reliance on stem cell transplantation in first remission, and improved long-term survival.
To test this, they treated 86 adults with newly diagnosed Ph+ALL, including those who had undergone one or two previous courses of chemotherapy with a TKI other than ponatinib. The patients had Eastern Cooperative Oncology Group performance status 0-2, adequate organ function, and no clinically significant cardiovascular disease.
The patients underwent eight cycles of hyper-CVAD alternating with high-dose methotrexate/cytarabine approximately every 21 days. The first 37 patients were treated with, ponatinib 45 mg daily for the first 14 days of cycle 1, then continuously for subsequent cycles. Patients with CD20 expression of 20% or greater also received rituximab during the first four cycles. CNS prophylaxis was also administered with 12 doses of intrathecal chemotherapy with alternating methotrexate and cytarabine.
Patients who had a CR received maintenance with ponatinib and vincristine/prednisone monthly for 2 years, followed by ponatinib indefinitely.
Out of concern for vascular toxicity with long-term use of high-dose ponatinib, including the two deaths mentioned before, the protocol was amended after the first 37 patients were treated. The amended protocol reduced ponatinib to 30 mg starting at cycle 2, with further reduction to 15 mg once a CMR (absence of BCR-ABL on polymerase chain reaction) was achieved.
At a median follow-up of 44 months, the event-free survival rates – the primary endpoint – were 71% at 3 years and 68% at 5 years. The 3-year OS rate was 78%, and the 5-year OS rate was 74%.
All patients had complete remission and complete cytogenetic remission as assessed by conventional karyotyping. Additionally, 73 of 85 evaluable patients (86%) achieved a CMR at some point during therapy.
“We had previously reported that achievement of a complete molecular response by 3 months is associated with superior outcomes. Approximately three quarters of patients achieved this milestone,” Dr. Short said.
Grade 3 or greater adverse events of particular concern included transaminase elevations in 29% of patients, elevated bilirubin and pancreatitis in 15% each, and hypertension in 14%.
Four patients had grade 3 or greater venous thromboembolic or arterial events, including the two previously noted deaths from myocardial infarction, both of which occurred prior to the protocol amendment.
At the most recent follow-up, 11 patients had experienced relapse (no CNS-only relapses), and of this group, 5 died and 6 were still alive. Nineteen patients underwent hematopoietic stem cell transplant, and of this group, 13 were still alive and 6 died.
Causes of death in the nine patients who died while in CR included the two myocardial infarction deaths on study, three deaths from sepsis during consolidation, one from lung cancer, one from a head injury after a fall, one from myocardial infarction in a 79-year-old patient 4 years after stopping ponatinib (off study), and one from preexisting congestive heart failure in a 74-year-old patient.
In all, 47 patients were either in ongoing therapy or observation at last follow-up, including three patients who were transitioned to MRD-directed therapy including blinatumomab (Blincyto).
“As a next step, we are now evaluating lower-intensity regimens with ponatinib and blinatumomab in both the frontline and relapsed/refractory settings, with the goals of decreased chemotherapy-related toxicity, increased MRD-negativity rates, further decreased reliance on transplant, and improved long-term outcomes,” Dr. Short said.
The study was sponsored by MD Anderson with support from the National Cancer Institute. Dr. Short reported consulting for AstraZenca, honoraria from Amgen, and consulting and receiving research funding from Takeda Oncology.
SOURCE: Short NJ et al. ASH 2019, Abstract 283.
REPORTING FROM ASH 2019
CAR T cells produce complete responses in T-cell malignancies
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
ORLANDO – Anti-CD5 chimeric antigen receptor (CAR) T cells can produce complete responses (CRs) in patients with relapsed or refractory T-cell malignancies, according to findings from a phase 1 trial.
Three of 11 patients achieved a CR after CAR T-cell therapy, and one patient achieved a mixed response that deepened to a CR after transplant. Three responders, all of whom had T-cell lymphoma, were still alive and in CR at last follow-up.
There were no cases of severe cytokine release syndrome (CRS) or severe neurotoxicity, no serious infectious complications, and no nonhematologic grade 4 adverse events in this trial.
LaQuisa C. Hill, MD, of Baylor College of Medicine, Houston, presented these results at the annual meeting of the American Society of Hematology.
“While CD19 CAR T cells have revolutionized the treatment of relapsed/refractory B-cell malignancies, development of CAR T-cell platforms targeting T-cell-driven malignancies have been hindered by three main factors: CAR T-cell fratricide due to shared expression of target antigens leading to impaired expansion, ablation of normal T cells continuing to cause profound immunodeficiency, and the potential of transduced tumor cells providing a means of tumor escape,” Dr. Hill said.
Researchers have theorized that anti-CD5 CAR T cells can overcome these obstacles. In preclinical studies, anti-CD5 CAR T cells eliminated malignant blasts in vitro and in vivo and resulted in “limited and transient” fratricide (Blood. 2015 Aug 20;126[8]:983-92).
With this in mind, Dr. Hill and her colleagues tested CD5.28z CAR T cells in a phase 1 trial (NCT03081910). Eleven patients have been treated thus far – five with T-cell acute lymphoblastic leukemia (T-ALL), three with peripheral T-cell lymphoma (PTCL), two with angioimmunoblastic T-cell lymphoma (AITL), and one with Sézary syndrome.
The patients’ median age at baseline was 62 years (range, 21-71 years), and 63% were men. They had received a median of 5 prior therapies (range, 3-18). Two patients had relapsed after allogeneic hematopoietic stem cell transplant (HSCT), three had relapsed after autologous HSCT, and five were primary refractory.
Patients underwent lymphodepletion with fludarabine and cyclophosphamide, then received CAR T cells at doses of 1 x 107 or 5 x 107.
Response
Three lymphoma patients – two with AITL and one with PTCL – were still alive and in CR at last follow-up. The PTCL patient achieved a CR after CAR T-cell therapy and declined a subsequent HSCT. The patient has not received additional therapy and has retained the CR for 7 months.
One AITL patient achieved a CR and declined transplant as well. He relapsed after 7 months but received subsequent therapy and achieved another CR. The other AITL patient had a mixed response to CAR T-cell therapy but proceeded to allogeneic HSCT and achieved a CR that has lasted 9 months.
The remaining three lymphoma patients – two with PTCL and one with Sézary syndrome – progressed and died.
One T-ALL patient achieved a CR lasting 6 weeks, but the patient died while undergoing transplant workup. Two T-ALL patients did not respond to treatment and died. The remaining two patients progressed, and one of them died. The other patient who progressed is still alive and in CR after receiving subsequent therapy.
Factors associated with response
Dr. Hill said a shortened manufacturing process may be associated with enhanced response, as all responders received CAR T cells produced via a shorter manufacturing process. The shortened process involves freezing cells on day 4-5 post transduction, as opposed to day 7.
“While the numbers are too small to make any definitive conclusions, this seems to correlate with less terminal differentiation, which might improve potency,” Dr. Hill said. “However, additional analyses are ongoing.”
Dr. Hill also pointed out that CAR T-cell expansion was observed in all patients, with higher peak levels observed at the higher dose. In addition, CAR T-cell persistence was durable at both dose levels.
“We have been able to detect the CAR transgene at all follow-up time points, out to 9 months for some patients,” Dr. Hill said. “While limited persistence may play a role in nonresponders, it does not appear to be the only factor.”
Safety
“Surprisingly, no selective ablation of normal T cells has been observed,” Dr. Hill said. “As CAR T cells dwindled [after infusion], we were able to see recovery of normal T cells, all of which expressed normal levels of CD5. This was observed in all patients on study, except for one patient who had prolonged pancytopenia.”
Cytopenias were the most common grade 3/4 adverse events, including neutropenia (n = 8), anemia (n = 7), and thrombocytopenia (n = 5). Other grade 3/4 events included elevated aspartate aminotransferase (n = 2), hypoalbuminemia (n = 1), hyponatremia (n = 1), hypophosphatemia (n = 1), and elevated alanine aminotransferase (n = 1). There were no grade 5 adverse events.
Two patients developed grade 1 CRS, and two had grade 2 CRS. Both patients with grade 2 CRS were treated with tocilizumab, and their symptoms resolved.
One patient developed grade 2 immune effector cell-associated neurotoxicity syndrome, but this resolved with supportive care.
One patient had a central line–associated bloodstream infection (coagulase-negative staphylococci), and one had cytomegalovirus and BK virus reactivation. There were no fungal infections.
“We have demonstrated that CD5 CAR T cells can be manufactured from heavily pretreated patients with T-cell malignancies, and therapy is well tolerated,” Dr. Hill said. “We have seen strong and promising activity in T-cell lymphoma, which we hope to be able to translate to T-ALL as well.”
Dr. Hill said she and her colleagues hope to improve upon these results with a higher dose level of CD5 CAR T cells (1 x 108), which the team plans to start testing soon. The researchers may also investigate other target antigens, such as CD7, as well as the use of donor-derived CAR T cells for patients who have relapsed after allogeneic HSCT.
Dr. Hill said she has no relevant disclosures. Baylor College of Medicine is sponsoring this trial.
SOURCE: Hill L et al. ASH 2019. Abstract 199.
REPORTING FROM ASH 2019
Blinatumomab instead of chemo in young patients with relapsed ALL
ORLANDO – In young patients who experience relapse after chemotherapy for B-cell acute lymphoblastic leukemia (B-ALL), the novel agent blinatumomab (Blincyto, Amgen) can be used instead of intensive chemotherapy to try to achieve a second remission, experts say.
In fact, blinatumomab should be the new standard of care in these patients because it yielded better overall survival, was less toxic, and allowed more patients to proceed to transplant, said Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
Dr. Brodsky was commenting on new data presented in a late-breaking abstract (LBA1) at the annual meeting of the American Society of Hematology, for which he holds the role of secretary.
These results are “truly practice changing,” he told journalists at a press briefing.
Cure rates for B-ALL in children and adolescents and young adults (AYAs) are high, but for the small group of patients who experience relapse (about 15%), the prognosis is poor.
When relapse occurs in these patients, “it’s a real problem,” Dr. Brodsky explained. “At that point, the major emphasis is trying to get them back into full remission and get them to a transplant,” he continued, “but it’s very hard to get these patients back into remission.”
The standard treatment approach for these patients includes intensive chemotherapy. In the new study, this was compared to monotherapy with blinatumomab, which is described as a bispecific T-cell engager antibody.
The results were presented by Patrick A. Brown, MD, from the division of pediatric oncology at the Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University.
The Children’s Oncology Group Study AALL1331 trial was conducted in 208 children and AYA patients with B-ALL after a first relapse. Median follow-up was 1.4 years.
Blinatumomab was superior in achieving both disease-free survival (59.3 plus or minus 5.4% at 2 years vs. 41% plus or minus 6.2% at 2 years with chemo; P = .05) and overall survival (79.4 plus or minus 4.5% at 2 years vs. 59.2 plus or minus 6% at 2 years with chemo; P = .05).
In addition, more patients who received blinatumomab subsequently underwent transplant (79% vs. 45% with chemo; P less than .0001).
The drug was also better tolerated than chemotherapy, causing fewer and less severe toxicities, including fewer cases of grade 3+ infection, sepsis, and mucositis.
Dr. Brown concluded that, for children and AYA patients with high- or intermediate-risk first relapse of B-ALL, blinatumomab is superior to standard chemotherapy as postreinduction consolidation prior to transplant, resulting in fewer and less severe toxicities, higher rates of minimum residual disease response, greater likelihood of proceeding to hematopoietic stem cell transplant, and improved disease-free and overall survival.
Dr. Brown noted that blinatumomab already has conditional approval from the Food and Drug Administration for use in relapsed ALL in both adults and children, but that approval was based on clinical trial data in adults. This is now the definitive trial in children and AYAs, and it should support full approval for this indication, he said.
Dr. Brown has relationships with Novartis, Servier, and Jazz. Many coauthors also have relationships with pharmaceutical companies. Dr. Brodsky has relationships with Achillion, Alexion, and UpToDate.
A version of this story originally appeared on Medscape.com.
ORLANDO – In young patients who experience relapse after chemotherapy for B-cell acute lymphoblastic leukemia (B-ALL), the novel agent blinatumomab (Blincyto, Amgen) can be used instead of intensive chemotherapy to try to achieve a second remission, experts say.
In fact, blinatumomab should be the new standard of care in these patients because it yielded better overall survival, was less toxic, and allowed more patients to proceed to transplant, said Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
Dr. Brodsky was commenting on new data presented in a late-breaking abstract (LBA1) at the annual meeting of the American Society of Hematology, for which he holds the role of secretary.
These results are “truly practice changing,” he told journalists at a press briefing.
Cure rates for B-ALL in children and adolescents and young adults (AYAs) are high, but for the small group of patients who experience relapse (about 15%), the prognosis is poor.
When relapse occurs in these patients, “it’s a real problem,” Dr. Brodsky explained. “At that point, the major emphasis is trying to get them back into full remission and get them to a transplant,” he continued, “but it’s very hard to get these patients back into remission.”
The standard treatment approach for these patients includes intensive chemotherapy. In the new study, this was compared to monotherapy with blinatumomab, which is described as a bispecific T-cell engager antibody.
The results were presented by Patrick A. Brown, MD, from the division of pediatric oncology at the Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University.
The Children’s Oncology Group Study AALL1331 trial was conducted in 208 children and AYA patients with B-ALL after a first relapse. Median follow-up was 1.4 years.
Blinatumomab was superior in achieving both disease-free survival (59.3 plus or minus 5.4% at 2 years vs. 41% plus or minus 6.2% at 2 years with chemo; P = .05) and overall survival (79.4 plus or minus 4.5% at 2 years vs. 59.2 plus or minus 6% at 2 years with chemo; P = .05).
In addition, more patients who received blinatumomab subsequently underwent transplant (79% vs. 45% with chemo; P less than .0001).
The drug was also better tolerated than chemotherapy, causing fewer and less severe toxicities, including fewer cases of grade 3+ infection, sepsis, and mucositis.
Dr. Brown concluded that, for children and AYA patients with high- or intermediate-risk first relapse of B-ALL, blinatumomab is superior to standard chemotherapy as postreinduction consolidation prior to transplant, resulting in fewer and less severe toxicities, higher rates of minimum residual disease response, greater likelihood of proceeding to hematopoietic stem cell transplant, and improved disease-free and overall survival.
Dr. Brown noted that blinatumomab already has conditional approval from the Food and Drug Administration for use in relapsed ALL in both adults and children, but that approval was based on clinical trial data in adults. This is now the definitive trial in children and AYAs, and it should support full approval for this indication, he said.
Dr. Brown has relationships with Novartis, Servier, and Jazz. Many coauthors also have relationships with pharmaceutical companies. Dr. Brodsky has relationships with Achillion, Alexion, and UpToDate.
A version of this story originally appeared on Medscape.com.
ORLANDO – In young patients who experience relapse after chemotherapy for B-cell acute lymphoblastic leukemia (B-ALL), the novel agent blinatumomab (Blincyto, Amgen) can be used instead of intensive chemotherapy to try to achieve a second remission, experts say.
In fact, blinatumomab should be the new standard of care in these patients because it yielded better overall survival, was less toxic, and allowed more patients to proceed to transplant, said Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
Dr. Brodsky was commenting on new data presented in a late-breaking abstract (LBA1) at the annual meeting of the American Society of Hematology, for which he holds the role of secretary.
These results are “truly practice changing,” he told journalists at a press briefing.
Cure rates for B-ALL in children and adolescents and young adults (AYAs) are high, but for the small group of patients who experience relapse (about 15%), the prognosis is poor.
When relapse occurs in these patients, “it’s a real problem,” Dr. Brodsky explained. “At that point, the major emphasis is trying to get them back into full remission and get them to a transplant,” he continued, “but it’s very hard to get these patients back into remission.”
The standard treatment approach for these patients includes intensive chemotherapy. In the new study, this was compared to monotherapy with blinatumomab, which is described as a bispecific T-cell engager antibody.
The results were presented by Patrick A. Brown, MD, from the division of pediatric oncology at the Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University.
The Children’s Oncology Group Study AALL1331 trial was conducted in 208 children and AYA patients with B-ALL after a first relapse. Median follow-up was 1.4 years.
Blinatumomab was superior in achieving both disease-free survival (59.3 plus or minus 5.4% at 2 years vs. 41% plus or minus 6.2% at 2 years with chemo; P = .05) and overall survival (79.4 plus or minus 4.5% at 2 years vs. 59.2 plus or minus 6% at 2 years with chemo; P = .05).
In addition, more patients who received blinatumomab subsequently underwent transplant (79% vs. 45% with chemo; P less than .0001).
The drug was also better tolerated than chemotherapy, causing fewer and less severe toxicities, including fewer cases of grade 3+ infection, sepsis, and mucositis.
Dr. Brown concluded that, for children and AYA patients with high- or intermediate-risk first relapse of B-ALL, blinatumomab is superior to standard chemotherapy as postreinduction consolidation prior to transplant, resulting in fewer and less severe toxicities, higher rates of minimum residual disease response, greater likelihood of proceeding to hematopoietic stem cell transplant, and improved disease-free and overall survival.
Dr. Brown noted that blinatumomab already has conditional approval from the Food and Drug Administration for use in relapsed ALL in both adults and children, but that approval was based on clinical trial data in adults. This is now the definitive trial in children and AYAs, and it should support full approval for this indication, he said.
Dr. Brown has relationships with Novartis, Servier, and Jazz. Many coauthors also have relationships with pharmaceutical companies. Dr. Brodsky has relationships with Achillion, Alexion, and UpToDate.
A version of this story originally appeared on Medscape.com.
ASH preview: Key themes include tackling CAR T obstacles, sickle cell advances, VTE
Chimeric antigen receptor (CAR) T-cell therapies have garnered a great deal of attention given their “incredible efficacy” in treating B-cell malignancies, and new findings are taking aim at the drawbacks of therapy, such as the time, expense, and toxicity involved, according to Robert A. Brodsky, MD.
One example, from a study slated for presentation during a plenary session at the upcoming annual meeting of the American Society of Hematology involves the investigational T-cell bispecific antibody mosunetuzumab, which targets both CD20 on the surface of malignant B cells, and CD3 on cytotoxic T cells, engaging the T cells and directing their cytotoxicity against B cells.
In a study (Abstract 6) of 218 non-Hodgkin lymphoma patients, including 23 who had already received CAR T-cell therapy and had relapsed or were refractory to the treatment, 64% responded, 42% had a complete response, and the median duration of response is now out to 9 months, Dr. Brodsky, ASH secretary and director of the division of hematology at Johns Hopkins University, Baltimore, said during a premeeting press conference.
“It’s basically an antibody using the patient’s own T cell to do what a CAR-T cell would do – [a] very exciting study and large study,” he said. “It is an off-the-shelf product, it completely gets around the problem of the time to generate the CAR T-cell product, and because it’s going to be much simpler and faster to produce, it’s likely going to be much cheaper than CAR T cells.”
The preliminary results also suggest it is less toxic than CAR T-cell therapy, he added.
Two other CAR T-cell therapy–related studies highlighted during the press conference address its use for multiple myeloma. One, the phase 1b/2 CARTITUDE study (Abstract 577) uses CAR T cells against the B-cell maturation antigen (BCMA) in the relapsed/refractory setting.
Of 25 patients treated with chemotherapy followed by CAR T-cell infusion and followed for a median of 3 months, 91% responded, two achieved a complete remission, and “many other responses were very deep responses,” Dr. Brodsky said, noting that the second featured multiple myeloma trial (Abstract 930) looked at bispecific CAR T-cell therapy targeting BCMA and CD38 in an effort to reduce resistance to the therapy.
“Again, very interesting preliminary results,” he said, noting that of 16 patients followed for a median of 36 weeks, 87.5% responded, the treatment was well tolerated, and progression-free survival at 9 months was 75%.
In addition to the “key theme” of overcoming CAR T-cell therapy obstacles, three other themes have emerged from among the thousands of abstracts submitted for presentation at ASH. These, as presented during the press conference, include new venous thromboembolism (VTE) therapies and approaches to research; inclusive medicine, with abstracts focused on age- and race-related issues in clinical trials; and new advances in the treatment of sickle cell disease. All of these have potentially practice-changing implications, as do the six late-breaking abstracts selected from 93 abstracts submitted for consideration for oral presentation at ASH, Dr. Brodsky said.
One of the “truly practice-changing” late-breakers is a randomized phase 3 trial (Abstract LBA-1) comparing the bispecific antibody blinatumomab to chemotherapy for post-re-induction therapy in high- and intermediate-risk acute lymphoblastic leukemia (ALL) at first relapse in children, adolescents and young adults.
The study demonstrated the superiority of blinatumomab for efficacy and tolerability, which is particularly encouraging given the challenges in getting relapsed ALL patients back into remission so they can undergo bone marrow transplant, Dr. Brodsky said.
Of 208 patients randomized, 73% vs. 45% in the blinatumomab vs. chemotherapy arms were able to get to transplant – and therefore to potential cure, he said.
“Of note, the blinatumomab arm was less toxic and there was marked improvement in disease-free and overall survival, so this is clearly going to become a new standard of care for relapsed and refractory ALL,” he added.
Chimeric antigen receptor (CAR) T-cell therapies have garnered a great deal of attention given their “incredible efficacy” in treating B-cell malignancies, and new findings are taking aim at the drawbacks of therapy, such as the time, expense, and toxicity involved, according to Robert A. Brodsky, MD.
One example, from a study slated for presentation during a plenary session at the upcoming annual meeting of the American Society of Hematology involves the investigational T-cell bispecific antibody mosunetuzumab, which targets both CD20 on the surface of malignant B cells, and CD3 on cytotoxic T cells, engaging the T cells and directing their cytotoxicity against B cells.
In a study (Abstract 6) of 218 non-Hodgkin lymphoma patients, including 23 who had already received CAR T-cell therapy and had relapsed or were refractory to the treatment, 64% responded, 42% had a complete response, and the median duration of response is now out to 9 months, Dr. Brodsky, ASH secretary and director of the division of hematology at Johns Hopkins University, Baltimore, said during a premeeting press conference.
“It’s basically an antibody using the patient’s own T cell to do what a CAR-T cell would do – [a] very exciting study and large study,” he said. “It is an off-the-shelf product, it completely gets around the problem of the time to generate the CAR T-cell product, and because it’s going to be much simpler and faster to produce, it’s likely going to be much cheaper than CAR T cells.”
The preliminary results also suggest it is less toxic than CAR T-cell therapy, he added.
Two other CAR T-cell therapy–related studies highlighted during the press conference address its use for multiple myeloma. One, the phase 1b/2 CARTITUDE study (Abstract 577) uses CAR T cells against the B-cell maturation antigen (BCMA) in the relapsed/refractory setting.
Of 25 patients treated with chemotherapy followed by CAR T-cell infusion and followed for a median of 3 months, 91% responded, two achieved a complete remission, and “many other responses were very deep responses,” Dr. Brodsky said, noting that the second featured multiple myeloma trial (Abstract 930) looked at bispecific CAR T-cell therapy targeting BCMA and CD38 in an effort to reduce resistance to the therapy.
“Again, very interesting preliminary results,” he said, noting that of 16 patients followed for a median of 36 weeks, 87.5% responded, the treatment was well tolerated, and progression-free survival at 9 months was 75%.
In addition to the “key theme” of overcoming CAR T-cell therapy obstacles, three other themes have emerged from among the thousands of abstracts submitted for presentation at ASH. These, as presented during the press conference, include new venous thromboembolism (VTE) therapies and approaches to research; inclusive medicine, with abstracts focused on age- and race-related issues in clinical trials; and new advances in the treatment of sickle cell disease. All of these have potentially practice-changing implications, as do the six late-breaking abstracts selected from 93 abstracts submitted for consideration for oral presentation at ASH, Dr. Brodsky said.
One of the “truly practice-changing” late-breakers is a randomized phase 3 trial (Abstract LBA-1) comparing the bispecific antibody blinatumomab to chemotherapy for post-re-induction therapy in high- and intermediate-risk acute lymphoblastic leukemia (ALL) at first relapse in children, adolescents and young adults.
The study demonstrated the superiority of blinatumomab for efficacy and tolerability, which is particularly encouraging given the challenges in getting relapsed ALL patients back into remission so they can undergo bone marrow transplant, Dr. Brodsky said.
Of 208 patients randomized, 73% vs. 45% in the blinatumomab vs. chemotherapy arms were able to get to transplant – and therefore to potential cure, he said.
“Of note, the blinatumomab arm was less toxic and there was marked improvement in disease-free and overall survival, so this is clearly going to become a new standard of care for relapsed and refractory ALL,” he added.
Chimeric antigen receptor (CAR) T-cell therapies have garnered a great deal of attention given their “incredible efficacy” in treating B-cell malignancies, and new findings are taking aim at the drawbacks of therapy, such as the time, expense, and toxicity involved, according to Robert A. Brodsky, MD.
One example, from a study slated for presentation during a plenary session at the upcoming annual meeting of the American Society of Hematology involves the investigational T-cell bispecific antibody mosunetuzumab, which targets both CD20 on the surface of malignant B cells, and CD3 on cytotoxic T cells, engaging the T cells and directing their cytotoxicity against B cells.
In a study (Abstract 6) of 218 non-Hodgkin lymphoma patients, including 23 who had already received CAR T-cell therapy and had relapsed or were refractory to the treatment, 64% responded, 42% had a complete response, and the median duration of response is now out to 9 months, Dr. Brodsky, ASH secretary and director of the division of hematology at Johns Hopkins University, Baltimore, said during a premeeting press conference.
“It’s basically an antibody using the patient’s own T cell to do what a CAR-T cell would do – [a] very exciting study and large study,” he said. “It is an off-the-shelf product, it completely gets around the problem of the time to generate the CAR T-cell product, and because it’s going to be much simpler and faster to produce, it’s likely going to be much cheaper than CAR T cells.”
The preliminary results also suggest it is less toxic than CAR T-cell therapy, he added.
Two other CAR T-cell therapy–related studies highlighted during the press conference address its use for multiple myeloma. One, the phase 1b/2 CARTITUDE study (Abstract 577) uses CAR T cells against the B-cell maturation antigen (BCMA) in the relapsed/refractory setting.
Of 25 patients treated with chemotherapy followed by CAR T-cell infusion and followed for a median of 3 months, 91% responded, two achieved a complete remission, and “many other responses were very deep responses,” Dr. Brodsky said, noting that the second featured multiple myeloma trial (Abstract 930) looked at bispecific CAR T-cell therapy targeting BCMA and CD38 in an effort to reduce resistance to the therapy.
“Again, very interesting preliminary results,” he said, noting that of 16 patients followed for a median of 36 weeks, 87.5% responded, the treatment was well tolerated, and progression-free survival at 9 months was 75%.
In addition to the “key theme” of overcoming CAR T-cell therapy obstacles, three other themes have emerged from among the thousands of abstracts submitted for presentation at ASH. These, as presented during the press conference, include new venous thromboembolism (VTE) therapies and approaches to research; inclusive medicine, with abstracts focused on age- and race-related issues in clinical trials; and new advances in the treatment of sickle cell disease. All of these have potentially practice-changing implications, as do the six late-breaking abstracts selected from 93 abstracts submitted for consideration for oral presentation at ASH, Dr. Brodsky said.
One of the “truly practice-changing” late-breakers is a randomized phase 3 trial (Abstract LBA-1) comparing the bispecific antibody blinatumomab to chemotherapy for post-re-induction therapy in high- and intermediate-risk acute lymphoblastic leukemia (ALL) at first relapse in children, adolescents and young adults.
The study demonstrated the superiority of blinatumomab for efficacy and tolerability, which is particularly encouraging given the challenges in getting relapsed ALL patients back into remission so they can undergo bone marrow transplant, Dr. Brodsky said.
Of 208 patients randomized, 73% vs. 45% in the blinatumomab vs. chemotherapy arms were able to get to transplant – and therefore to potential cure, he said.
“Of note, the blinatumomab arm was less toxic and there was marked improvement in disease-free and overall survival, so this is clearly going to become a new standard of care for relapsed and refractory ALL,” he added.