User login
‘Screen-time transferential interference’ in encounters with patients
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.
Trading in work-life balance for a well-balanced life
My residency supervisor candidly asked me today – Isn’t stressing out about writing an article on work-life balance kind of missing the point? Well, yeah, that’s why she’s my supervisor. This brings me to one of the lesser advertised tips to avoiding burnout, which is: Get yourself a great mensch. But I’m getting ahead of myself here. The plan was to have 10 perfectly delineated rules, because if it worked for Letterman and Moses, it should work for residency. More to come on that.
Another part of the plan was to have this article finished by last weekend, but long call was Saturday. This was followed by long call recovery consisting of sleeping in so late my dad texted and left a voicemail asking, what happened? I haven’t heard from you all weekend. Then there was the obligatory run on the treadmill so the gooey cinnamon rolls the nurses baked and generously invited me to on Thursday would not stick around long enough for my husband to wonder if this was the beginning of me letting myself go. Isn’t that a lovely phrase?
Monday was Monday. How does anyone get anything done on Mondays? I had a new team, two new patients to learn and discharge. Plus, it was the first day that cracked 50 degrees in 5 months. I had to meet up with a friend, grab some coffee, and gossip walk around the lake. This was before we found out another friend was being slammed with consults in the emergency room. So there I was right back at the hospital Monday night with a cream cheese cherry pastry to cheer up my compatriot in the struggle.
This brings me to Tuesday. I had planned to be at the editing stage of this article on Tuesday. But didactics ran long due to everyone being so engaged in our formulations lecture, I didn’t have a shot at looking at this thing until lunchtime. Lunchtime came, and as I opened Microsoft Word among my dollar turkey sandwich and mini Purell bottles stationed around me like glorious little sergeants, I heard the gingerly utterings of a medical student: Um, if you have a moment, could you tell me the difference between the side-effect profile of first-generation and second-generation antipsychotics?
An hour later, I was informed that an admit was on the way and was traveling from out of state, set to arrive a half-hour before shift’s end. Did I mention he arrived with two family members in tow who wanted to talk about how things went wrong starting 20 years ago? Then there was the patient to see who I knew would pout if I didn’t spend at least a half-hour checking in. You know, the one the nurses always try to save me from even though I secretly never wanted to be saved.
I finally drove home 2 hours later than anticipated with a smile on my face. I should repeat that, WITH A SMILE ON MY FACE. I felt good because I’d done good. After all, there’s even a little sunlight left. When I walk in the front door, I kiss my husband and then immediately delve into a new story from the day. We laugh. We warm up leftovers, sit on the couch with our bare feet on the table, and catch an hour of American Idol (talent never gets old). Then it’s time to meet this maker.
The strange thing is, the person who began this column with all of her well-intentioned plans feels very different from the person who has made it to the deadline. There is a whole life lived in between. All of the readings I had done, notations I had made, seem kind of beside the point. I could pepper you with statistics and evidence-based outcomes warning of divorce, substance abuse, physician suicide, patient errors, and the like, which are all very real outcomes of poorly balanced lives. But I think we know all of that. It’s the in between space, the living part where so many of us lose our way. So instead of referenced journals, I offer you my journey. Because I can truly say that for the last 3 months of the most difficult year of residency, I have been happy. May this piece be also with you.
Dr. Schmidt, a second-year psychiatry resident at the Mayo Clinic in Rochester, Minn., is interested in psychodynamic therapy and in pursuing a fellowship in addictions. After obtaining a bachelor of arts at the University of California, Berkeley, she earned a master of arts degree in philosophy and humanities at the University of Chicago. She attended medical school at the University of Illinois College of Medicine at Peoria.
My residency supervisor candidly asked me today – Isn’t stressing out about writing an article on work-life balance kind of missing the point? Well, yeah, that’s why she’s my supervisor. This brings me to one of the lesser advertised tips to avoiding burnout, which is: Get yourself a great mensch. But I’m getting ahead of myself here. The plan was to have 10 perfectly delineated rules, because if it worked for Letterman and Moses, it should work for residency. More to come on that.
Another part of the plan was to have this article finished by last weekend, but long call was Saturday. This was followed by long call recovery consisting of sleeping in so late my dad texted and left a voicemail asking, what happened? I haven’t heard from you all weekend. Then there was the obligatory run on the treadmill so the gooey cinnamon rolls the nurses baked and generously invited me to on Thursday would not stick around long enough for my husband to wonder if this was the beginning of me letting myself go. Isn’t that a lovely phrase?
Monday was Monday. How does anyone get anything done on Mondays? I had a new team, two new patients to learn and discharge. Plus, it was the first day that cracked 50 degrees in 5 months. I had to meet up with a friend, grab some coffee, and gossip walk around the lake. This was before we found out another friend was being slammed with consults in the emergency room. So there I was right back at the hospital Monday night with a cream cheese cherry pastry to cheer up my compatriot in the struggle.
This brings me to Tuesday. I had planned to be at the editing stage of this article on Tuesday. But didactics ran long due to everyone being so engaged in our formulations lecture, I didn’t have a shot at looking at this thing until lunchtime. Lunchtime came, and as I opened Microsoft Word among my dollar turkey sandwich and mini Purell bottles stationed around me like glorious little sergeants, I heard the gingerly utterings of a medical student: Um, if you have a moment, could you tell me the difference between the side-effect profile of first-generation and second-generation antipsychotics?
An hour later, I was informed that an admit was on the way and was traveling from out of state, set to arrive a half-hour before shift’s end. Did I mention he arrived with two family members in tow who wanted to talk about how things went wrong starting 20 years ago? Then there was the patient to see who I knew would pout if I didn’t spend at least a half-hour checking in. You know, the one the nurses always try to save me from even though I secretly never wanted to be saved.
I finally drove home 2 hours later than anticipated with a smile on my face. I should repeat that, WITH A SMILE ON MY FACE. I felt good because I’d done good. After all, there’s even a little sunlight left. When I walk in the front door, I kiss my husband and then immediately delve into a new story from the day. We laugh. We warm up leftovers, sit on the couch with our bare feet on the table, and catch an hour of American Idol (talent never gets old). Then it’s time to meet this maker.
The strange thing is, the person who began this column with all of her well-intentioned plans feels very different from the person who has made it to the deadline. There is a whole life lived in between. All of the readings I had done, notations I had made, seem kind of beside the point. I could pepper you with statistics and evidence-based outcomes warning of divorce, substance abuse, physician suicide, patient errors, and the like, which are all very real outcomes of poorly balanced lives. But I think we know all of that. It’s the in between space, the living part where so many of us lose our way. So instead of referenced journals, I offer you my journey. Because I can truly say that for the last 3 months of the most difficult year of residency, I have been happy. May this piece be also with you.
Dr. Schmidt, a second-year psychiatry resident at the Mayo Clinic in Rochester, Minn., is interested in psychodynamic therapy and in pursuing a fellowship in addictions. After obtaining a bachelor of arts at the University of California, Berkeley, she earned a master of arts degree in philosophy and humanities at the University of Chicago. She attended medical school at the University of Illinois College of Medicine at Peoria.
My residency supervisor candidly asked me today – Isn’t stressing out about writing an article on work-life balance kind of missing the point? Well, yeah, that’s why she’s my supervisor. This brings me to one of the lesser advertised tips to avoiding burnout, which is: Get yourself a great mensch. But I’m getting ahead of myself here. The plan was to have 10 perfectly delineated rules, because if it worked for Letterman and Moses, it should work for residency. More to come on that.
Another part of the plan was to have this article finished by last weekend, but long call was Saturday. This was followed by long call recovery consisting of sleeping in so late my dad texted and left a voicemail asking, what happened? I haven’t heard from you all weekend. Then there was the obligatory run on the treadmill so the gooey cinnamon rolls the nurses baked and generously invited me to on Thursday would not stick around long enough for my husband to wonder if this was the beginning of me letting myself go. Isn’t that a lovely phrase?
Monday was Monday. How does anyone get anything done on Mondays? I had a new team, two new patients to learn and discharge. Plus, it was the first day that cracked 50 degrees in 5 months. I had to meet up with a friend, grab some coffee, and gossip walk around the lake. This was before we found out another friend was being slammed with consults in the emergency room. So there I was right back at the hospital Monday night with a cream cheese cherry pastry to cheer up my compatriot in the struggle.
This brings me to Tuesday. I had planned to be at the editing stage of this article on Tuesday. But didactics ran long due to everyone being so engaged in our formulations lecture, I didn’t have a shot at looking at this thing until lunchtime. Lunchtime came, and as I opened Microsoft Word among my dollar turkey sandwich and mini Purell bottles stationed around me like glorious little sergeants, I heard the gingerly utterings of a medical student: Um, if you have a moment, could you tell me the difference between the side-effect profile of first-generation and second-generation antipsychotics?
An hour later, I was informed that an admit was on the way and was traveling from out of state, set to arrive a half-hour before shift’s end. Did I mention he arrived with two family members in tow who wanted to talk about how things went wrong starting 20 years ago? Then there was the patient to see who I knew would pout if I didn’t spend at least a half-hour checking in. You know, the one the nurses always try to save me from even though I secretly never wanted to be saved.
I finally drove home 2 hours later than anticipated with a smile on my face. I should repeat that, WITH A SMILE ON MY FACE. I felt good because I’d done good. After all, there’s even a little sunlight left. When I walk in the front door, I kiss my husband and then immediately delve into a new story from the day. We laugh. We warm up leftovers, sit on the couch with our bare feet on the table, and catch an hour of American Idol (talent never gets old). Then it’s time to meet this maker.
The strange thing is, the person who began this column with all of her well-intentioned plans feels very different from the person who has made it to the deadline. There is a whole life lived in between. All of the readings I had done, notations I had made, seem kind of beside the point. I could pepper you with statistics and evidence-based outcomes warning of divorce, substance abuse, physician suicide, patient errors, and the like, which are all very real outcomes of poorly balanced lives. But I think we know all of that. It’s the in between space, the living part where so many of us lose our way. So instead of referenced journals, I offer you my journey. Because I can truly say that for the last 3 months of the most difficult year of residency, I have been happy. May this piece be also with you.
Dr. Schmidt, a second-year psychiatry resident at the Mayo Clinic in Rochester, Minn., is interested in psychodynamic therapy and in pursuing a fellowship in addictions. After obtaining a bachelor of arts at the University of California, Berkeley, she earned a master of arts degree in philosophy and humanities at the University of Chicago. She attended medical school at the University of Illinois College of Medicine at Peoria.
The patient refuses to cooperate. What can you do? What should you do?
The real estate business embraces the concept of ownership using the term “bundle of rights.” Real estate agents view full, unaffected ownership of a real property as complete (ie, undivided) and, when ownership is shared, talk about percentages of that bundle.
The same principle can be applied to guardianship. Because we are our own guardians, we own a full, undivided bundle of rights, including all our constitutional rights and the right to make decisions— even bad ones. Of course, an undivided bundle also means that we are fully responsible for the decisions we make.
When a patient requires representation
There may be a situation when we would give someone else the authority to represent us for a specific reason. In this case we would authorize this person to act on our behalf as we would do ourselves—yet we still retain 100% ownership of the “bundle,” and therefore can revoke this authorization at any time. The person we hire (appoint) to represent us will become our power of attorney (POA), and because we appoint this person for a specific situation (handle certain medical affairs, manage some financial affairs, sign real estate documents, etc.), this kind or POA is called “specific” or “special.” When we give someone the right to represent us in any or all of our affairs, this POA is called “general” or “durable.”
It is important to mention that as long as we continue to have psychological capacity and are willing to continue to be our own guardians (own 100% of the bundle of rights), we can terminate any POA we have appointed previously or designate another person to represent us as a “special” or “general” POA. Because of this, if an older patient—who is legally competent but physically unable to live on his (her) own— refuses to enter a long-term care facility, he (she) cannot be sent there against his will, even if the POA insists on it. Because of this, if the patient’s primary team strongly disagrees with this patient’s decision, his (her) “decision-making capacity” should be assessed and, if necessary, a competency hearing will need to be conducted. The court will then decide if this person is able (or unable) to handle his own affairs, and if the court decides that the person cannot be responsible to provide himself with food, health care, housing, and other necessities, the guardian (relative, friend, public administrator, etc.) will be appointed to do so.
Evaluating decision-making capacity
Determining “decision-making capacity” should not be confused with the legal concept of “competence.” We, physicians, often are called to evaluate a patient and give our opinion of the current level of this patient’s functioning (including his [her] decision-making capacity), and we—ourselves and a requesting team—need to be clear that it is merely our opinion and should be used as such. We need to remember that even if a patient is judged to be legally incompetent to handle financial affairs, he (she) might retain sufficient ability to make decisions about treatments.
We also need to remember that decision-making capacity can change, depending on medical conditions (severe anxiety, delirium), successful treatments, substance intoxication, etc. Because of this, we need to communicate to the requesting team that “decision-making ability” is situation-specific and time-specific, and that failure to make a decision on one issue should not be generalized to other aspects of the patient’s life.
Any physician can evaluate patient’s decision-making ability, but traditionally the psychiatry team is called to do so. It usually happens because the primary medical team needs us to provide “a third-party validation,” or because of the common misperception that only the psychiatric team can initiate a civil involuntary detention when necessary.
In any case, regardless of who evaluates the patient, specific points need to be addressed and the following questions need to be answered:
• Does the patient understand the nature of his (her) condition?
• Does the patient understand what treatment we are proposing or what he should do?
• Does the patient understand the consequences (good or bad) if he rejects our proposed action or treatment?
When information (discharge plan, treatment plan, etc.) is presented to patients, we should ask them to repeat it in their own words. We should not expect them to understand all of the technical aspects. We should consider patients’ intelligence level and their ability to communicate; if they can clearly verbalize their understanding of information and be consistent in their wish to continue with their decision, we have to declare that they have decision-making capability and able to proceed with their chosen treatment.
More matters that need to be mentioned
Restrictions on the patient. We need to remember that, even if a patient is thought to be able to make his own decisions, there may be some situations when he can be held in the hospital against his will. These usually are the cases when the patient is psychiatrically or medically unstable (unable to care of himself), but also if the patient is at risk of harming himself or others, subject of elder abuse, or suspected of being an abuser.
Restrictions on the practitioner. Even if the patient is determined to be lacking decision-making capacity, we, physicians, cannot perform tests, procedures, or do the placements without the patient’s agreement.
Informed consent doctrine is applicable in this case, and if performing a test or procedure is necessary (except life- or limb-saving emergencies, when doctrine of physician prerogative applies), or if there a disagreement in post-discharge placement, the emergency guardianship may need to be pursued.
Disclosure
Dr. Graypel reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
The real estate business embraces the concept of ownership using the term “bundle of rights.” Real estate agents view full, unaffected ownership of a real property as complete (ie, undivided) and, when ownership is shared, talk about percentages of that bundle.
The same principle can be applied to guardianship. Because we are our own guardians, we own a full, undivided bundle of rights, including all our constitutional rights and the right to make decisions— even bad ones. Of course, an undivided bundle also means that we are fully responsible for the decisions we make.
When a patient requires representation
There may be a situation when we would give someone else the authority to represent us for a specific reason. In this case we would authorize this person to act on our behalf as we would do ourselves—yet we still retain 100% ownership of the “bundle,” and therefore can revoke this authorization at any time. The person we hire (appoint) to represent us will become our power of attorney (POA), and because we appoint this person for a specific situation (handle certain medical affairs, manage some financial affairs, sign real estate documents, etc.), this kind or POA is called “specific” or “special.” When we give someone the right to represent us in any or all of our affairs, this POA is called “general” or “durable.”
It is important to mention that as long as we continue to have psychological capacity and are willing to continue to be our own guardians (own 100% of the bundle of rights), we can terminate any POA we have appointed previously or designate another person to represent us as a “special” or “general” POA. Because of this, if an older patient—who is legally competent but physically unable to live on his (her) own— refuses to enter a long-term care facility, he (she) cannot be sent there against his will, even if the POA insists on it. Because of this, if the patient’s primary team strongly disagrees with this patient’s decision, his (her) “decision-making capacity” should be assessed and, if necessary, a competency hearing will need to be conducted. The court will then decide if this person is able (or unable) to handle his own affairs, and if the court decides that the person cannot be responsible to provide himself with food, health care, housing, and other necessities, the guardian (relative, friend, public administrator, etc.) will be appointed to do so.
Evaluating decision-making capacity
Determining “decision-making capacity” should not be confused with the legal concept of “competence.” We, physicians, often are called to evaluate a patient and give our opinion of the current level of this patient’s functioning (including his [her] decision-making capacity), and we—ourselves and a requesting team—need to be clear that it is merely our opinion and should be used as such. We need to remember that even if a patient is judged to be legally incompetent to handle financial affairs, he (she) might retain sufficient ability to make decisions about treatments.
We also need to remember that decision-making capacity can change, depending on medical conditions (severe anxiety, delirium), successful treatments, substance intoxication, etc. Because of this, we need to communicate to the requesting team that “decision-making ability” is situation-specific and time-specific, and that failure to make a decision on one issue should not be generalized to other aspects of the patient’s life.
Any physician can evaluate patient’s decision-making ability, but traditionally the psychiatry team is called to do so. It usually happens because the primary medical team needs us to provide “a third-party validation,” or because of the common misperception that only the psychiatric team can initiate a civil involuntary detention when necessary.
In any case, regardless of who evaluates the patient, specific points need to be addressed and the following questions need to be answered:
• Does the patient understand the nature of his (her) condition?
• Does the patient understand what treatment we are proposing or what he should do?
• Does the patient understand the consequences (good or bad) if he rejects our proposed action or treatment?
When information (discharge plan, treatment plan, etc.) is presented to patients, we should ask them to repeat it in their own words. We should not expect them to understand all of the technical aspects. We should consider patients’ intelligence level and their ability to communicate; if they can clearly verbalize their understanding of information and be consistent in their wish to continue with their decision, we have to declare that they have decision-making capability and able to proceed with their chosen treatment.
More matters that need to be mentioned
Restrictions on the patient. We need to remember that, even if a patient is thought to be able to make his own decisions, there may be some situations when he can be held in the hospital against his will. These usually are the cases when the patient is psychiatrically or medically unstable (unable to care of himself), but also if the patient is at risk of harming himself or others, subject of elder abuse, or suspected of being an abuser.
Restrictions on the practitioner. Even if the patient is determined to be lacking decision-making capacity, we, physicians, cannot perform tests, procedures, or do the placements without the patient’s agreement.
Informed consent doctrine is applicable in this case, and if performing a test or procedure is necessary (except life- or limb-saving emergencies, when doctrine of physician prerogative applies), or if there a disagreement in post-discharge placement, the emergency guardianship may need to be pursued.
Disclosure
Dr. Graypel reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
The real estate business embraces the concept of ownership using the term “bundle of rights.” Real estate agents view full, unaffected ownership of a real property as complete (ie, undivided) and, when ownership is shared, talk about percentages of that bundle.
The same principle can be applied to guardianship. Because we are our own guardians, we own a full, undivided bundle of rights, including all our constitutional rights and the right to make decisions— even bad ones. Of course, an undivided bundle also means that we are fully responsible for the decisions we make.
When a patient requires representation
There may be a situation when we would give someone else the authority to represent us for a specific reason. In this case we would authorize this person to act on our behalf as we would do ourselves—yet we still retain 100% ownership of the “bundle,” and therefore can revoke this authorization at any time. The person we hire (appoint) to represent us will become our power of attorney (POA), and because we appoint this person for a specific situation (handle certain medical affairs, manage some financial affairs, sign real estate documents, etc.), this kind or POA is called “specific” or “special.” When we give someone the right to represent us in any or all of our affairs, this POA is called “general” or “durable.”
It is important to mention that as long as we continue to have psychological capacity and are willing to continue to be our own guardians (own 100% of the bundle of rights), we can terminate any POA we have appointed previously or designate another person to represent us as a “special” or “general” POA. Because of this, if an older patient—who is legally competent but physically unable to live on his (her) own— refuses to enter a long-term care facility, he (she) cannot be sent there against his will, even if the POA insists on it. Because of this, if the patient’s primary team strongly disagrees with this patient’s decision, his (her) “decision-making capacity” should be assessed and, if necessary, a competency hearing will need to be conducted. The court will then decide if this person is able (or unable) to handle his own affairs, and if the court decides that the person cannot be responsible to provide himself with food, health care, housing, and other necessities, the guardian (relative, friend, public administrator, etc.) will be appointed to do so.
Evaluating decision-making capacity
Determining “decision-making capacity” should not be confused with the legal concept of “competence.” We, physicians, often are called to evaluate a patient and give our opinion of the current level of this patient’s functioning (including his [her] decision-making capacity), and we—ourselves and a requesting team—need to be clear that it is merely our opinion and should be used as such. We need to remember that even if a patient is judged to be legally incompetent to handle financial affairs, he (she) might retain sufficient ability to make decisions about treatments.
We also need to remember that decision-making capacity can change, depending on medical conditions (severe anxiety, delirium), successful treatments, substance intoxication, etc. Because of this, we need to communicate to the requesting team that “decision-making ability” is situation-specific and time-specific, and that failure to make a decision on one issue should not be generalized to other aspects of the patient’s life.
Any physician can evaluate patient’s decision-making ability, but traditionally the psychiatry team is called to do so. It usually happens because the primary medical team needs us to provide “a third-party validation,” or because of the common misperception that only the psychiatric team can initiate a civil involuntary detention when necessary.
In any case, regardless of who evaluates the patient, specific points need to be addressed and the following questions need to be answered:
• Does the patient understand the nature of his (her) condition?
• Does the patient understand what treatment we are proposing or what he should do?
• Does the patient understand the consequences (good or bad) if he rejects our proposed action or treatment?
When information (discharge plan, treatment plan, etc.) is presented to patients, we should ask them to repeat it in their own words. We should not expect them to understand all of the technical aspects. We should consider patients’ intelligence level and their ability to communicate; if they can clearly verbalize their understanding of information and be consistent in their wish to continue with their decision, we have to declare that they have decision-making capability and able to proceed with their chosen treatment.
More matters that need to be mentioned
Restrictions on the patient. We need to remember that, even if a patient is thought to be able to make his own decisions, there may be some situations when he can be held in the hospital against his will. These usually are the cases when the patient is psychiatrically or medically unstable (unable to care of himself), but also if the patient is at risk of harming himself or others, subject of elder abuse, or suspected of being an abuser.
Restrictions on the practitioner. Even if the patient is determined to be lacking decision-making capacity, we, physicians, cannot perform tests, procedures, or do the placements without the patient’s agreement.
Informed consent doctrine is applicable in this case, and if performing a test or procedure is necessary (except life- or limb-saving emergencies, when doctrine of physician prerogative applies), or if there a disagreement in post-discharge placement, the emergency guardianship may need to be pursued.
Disclosure
Dr. Graypel reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Should the use of ‘endorse’ be endorsed in writing in psychiatry?
The word “endorse” often appears in the medical literature and is heard in oral presentations; psychiatrists use the term to mean that a person is reporting psychiatric symptoms or problems. However, such usage may be a stylistic catachresis—one that has the potential for misinterpretation or misunderstanding.
Finding ‘endorse’ in the psychiatric literature
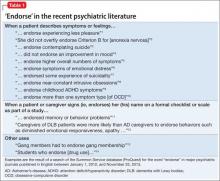
We conducted a literature search to identify instances of “endorse” in scholarly articles published in psychiatric journals between January 1, 2012, and November 25, 2013. Table 11-14 shows examples of typical uses of “endorse” in recent publications.
Even when “endorse” is used as a synonym for “report” or “describe,” use of the word in that context can seem out of place. We could not find any rationale in the medical literature for using “endorse” as a synonym for “report” or “describe.”
The definition of “endorse” in Merriam-Webster15 and Oxford Dictionaries16 includes:
• inscribing or signing a legal document, check, or bill
• approving or recommending an idea, product, or candidate.
We believe that using “endorse” in a psychiatric context could create confusion among medical trainees and professionals who are familiar with the correct meanings of the word.
Survey: Some residents use ‘endorse’ in oral presentations
We asked residents in the Department of Psychiatry at Drexel University College of Medicine to respond to a questionnaire regarding their understanding of the use of “endorse.” Their responses are summarized in Table 2.
What is wrong with using ‘endorse’? Except when “endorse” describes a patient formally affixing her (his) signature to a document for the purpose of (1) certification or (2) giving or showing one’s support for a cause, we think that use of the word in psychiatry is not in keeping with its formal, accepted definition. Furthermore, residents’ responses to our survey suggest that there is the danger of causing confusion in using the word“endorse” when “report” or “describe” is meant.
For example, if a patient “endorses” antisocial behavior, is she stating that she feels justified in exhibiting such behavior? Do students who “endorse” drug use approve of drug use? Another example: Youth who “endorse” gang membership have merely confirmed that they belonged to a gang at some time.
The intended meaning of “endorse” in these examples is probably closer to “admit” or “acknowledge.” The patient replies “yes” when the physician asks if she uses drugs or has had behavior problems; she is not necessarily recommending or approving these behaviors.
Usage is shifting. In the past, “complain” was common medical parlance for a patient’s report of symptoms or other health-related problems. In fact, medical, surgical, and psychiatric evaluations still begin with a “chief complaint” section. It’s possible that, because “complaint” might suggest that the patient is whining, the word fell out of favor in the medical lexicon and was replaced in the scholarly literature by the construction “the patient reports….”
Avoid jargon. Employ accurate terminology
We propose that “endorse,” like “complain,” is a cant of psychiatrists. We recommend that, when describing a patient’s statement or report of symptoms or experiences, practitioners should avoid “endorse” and write or say “report,” “express,” “exhibit,” or similar words. Using accurate terminology and avoiding imprecise or misleading jargon is not only linguistically appropriate but also can help avoid misunderstanding and improve patient care.
Acknowledgment
Diana Winters, Academic Publishing Services, Drexel University College of Medicine, provided editorial assistance in preparing the manuscript of this article and offered comment on the use of medical jargon.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strauss GP, Gold JM. A new perspective on anhedonia in schizophrenia. Am J Psychiatry. 2012;169(4):364-373.
2. Thomas JJ, Weigel TJ, Lawton RK, et al. Cognitive-behavioral treatment of body image disturbance in a congenitally blind patient with anorexia nervosa. Am J Psychiatry. 2012;169(1):16-20.
3. Purcell B, Heisel MJ, Speice J, et al. Family connectedness moderates the association between living alone and suicide ideation in a clinical sample of adults 50 years and older. Am J Geriatr Psychiatry. 2012;20(8):717-723.
4. Dakin EK, Areán P. Patient perspectives on the benefits of psychotherapy for late-life depression. Am J Geriatr Psychiatry. 2013;21(2):155-163.
5. Mezuk B, Lohman M, Dumenci, L, et al. Are depression and frailty overlapping syndromes in mid- and late-life? A latent variable analysis. Am J Geriatr Psychiatry. 2013;21(6):560-569.
6. Boindala NS, Tucker P, Trautman RP. “Culture and psychiatry”: a course for second-year psychiatry residents. Acad Psychiatry. 2013;37(1):46-50.
7. Henry A, Kisicki MD, Varley C. Efficacy and safety of antidepressant drug treatment in children and adolescents. Mol Psychiatry. 2012;17(12):1186-1193.
8. Rodriguez CI, Kegeles LS, Levinson A, et al. A randomized controlled crossover trial of ketamine in obsessive-compulsive disorder (abstract W7). Neuropsychopharmacology. 2012;38:S317.
9. Whelan R, Garavan H. Fractionating the impulsivity construct in adolescence. Neuropsychopharmacology. 2013;38(1):250-251.
10. Rück C, Larsson KJ, Mataix-Cols D. Predictors of medium and long-term outcome following capsulotomy for obsessive-compulsive disorder: one site may not fit all. Eur Neuropsychopharmacol. 2012;22(6):406-414.
11. Mausbach BT, Chattillion EA, Roepke SK, et al. A comparison of psychosocial outcomes in elderly Alzheimer caregivers and noncaregivers. Am J Geriatr Psychiatry. 2013;21(1):5-13.
12. Peavy GM, Salmon DP, Edland SD, et al. Neuropsychiatric features of frontal lobe dysfunction in autopsy-confirmed patients with lewy bodies and “pure” Alzheimer disease. Am J Geriatr Psychiatry. 2013;21(6):509-519.
13. Coid JW, Ullrich S, Keers R, et al. Gang membership, violence, and psychiatric morbidity. Am J Psychiatry. 2013;170(9):985-993.
14. Choi D, Tolova V, Socha E, et al. Substance use and attitudes on professional conduct among medical students: a single-institution study. Acad Psychiatry. 2013;37(3):191-195.
15. Endorse. Merriam-Webster. http://www.merriam-webster. com/dictionary/endorse. Accessed January 14, 2014.
16. Endorse. Oxford Dictionaries. http://www.oxforddictionaries. com/definition/english/endorse. Accessed January 14, 2014.
The word “endorse” often appears in the medical literature and is heard in oral presentations; psychiatrists use the term to mean that a person is reporting psychiatric symptoms or problems. However, such usage may be a stylistic catachresis—one that has the potential for misinterpretation or misunderstanding.
Finding ‘endorse’ in the psychiatric literature
We conducted a literature search to identify instances of “endorse” in scholarly articles published in psychiatric journals between January 1, 2012, and November 25, 2013. Table 11-14 shows examples of typical uses of “endorse” in recent publications.
Even when “endorse” is used as a synonym for “report” or “describe,” use of the word in that context can seem out of place. We could not find any rationale in the medical literature for using “endorse” as a synonym for “report” or “describe.”
The definition of “endorse” in Merriam-Webster15 and Oxford Dictionaries16 includes:
• inscribing or signing a legal document, check, or bill
• approving or recommending an idea, product, or candidate.
We believe that using “endorse” in a psychiatric context could create confusion among medical trainees and professionals who are familiar with the correct meanings of the word.
Survey: Some residents use ‘endorse’ in oral presentations
We asked residents in the Department of Psychiatry at Drexel University College of Medicine to respond to a questionnaire regarding their understanding of the use of “endorse.” Their responses are summarized in Table 2.
What is wrong with using ‘endorse’? Except when “endorse” describes a patient formally affixing her (his) signature to a document for the purpose of (1) certification or (2) giving or showing one’s support for a cause, we think that use of the word in psychiatry is not in keeping with its formal, accepted definition. Furthermore, residents’ responses to our survey suggest that there is the danger of causing confusion in using the word“endorse” when “report” or “describe” is meant.
For example, if a patient “endorses” antisocial behavior, is she stating that she feels justified in exhibiting such behavior? Do students who “endorse” drug use approve of drug use? Another example: Youth who “endorse” gang membership have merely confirmed that they belonged to a gang at some time.
The intended meaning of “endorse” in these examples is probably closer to “admit” or “acknowledge.” The patient replies “yes” when the physician asks if she uses drugs or has had behavior problems; she is not necessarily recommending or approving these behaviors.
Usage is shifting. In the past, “complain” was common medical parlance for a patient’s report of symptoms or other health-related problems. In fact, medical, surgical, and psychiatric evaluations still begin with a “chief complaint” section. It’s possible that, because “complaint” might suggest that the patient is whining, the word fell out of favor in the medical lexicon and was replaced in the scholarly literature by the construction “the patient reports….”
Avoid jargon. Employ accurate terminology
We propose that “endorse,” like “complain,” is a cant of psychiatrists. We recommend that, when describing a patient’s statement or report of symptoms or experiences, practitioners should avoid “endorse” and write or say “report,” “express,” “exhibit,” or similar words. Using accurate terminology and avoiding imprecise or misleading jargon is not only linguistically appropriate but also can help avoid misunderstanding and improve patient care.
Acknowledgment
Diana Winters, Academic Publishing Services, Drexel University College of Medicine, provided editorial assistance in preparing the manuscript of this article and offered comment on the use of medical jargon.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
The word “endorse” often appears in the medical literature and is heard in oral presentations; psychiatrists use the term to mean that a person is reporting psychiatric symptoms or problems. However, such usage may be a stylistic catachresis—one that has the potential for misinterpretation or misunderstanding.
Finding ‘endorse’ in the psychiatric literature
We conducted a literature search to identify instances of “endorse” in scholarly articles published in psychiatric journals between January 1, 2012, and November 25, 2013. Table 11-14 shows examples of typical uses of “endorse” in recent publications.
Even when “endorse” is used as a synonym for “report” or “describe,” use of the word in that context can seem out of place. We could not find any rationale in the medical literature for using “endorse” as a synonym for “report” or “describe.”
The definition of “endorse” in Merriam-Webster15 and Oxford Dictionaries16 includes:
• inscribing or signing a legal document, check, or bill
• approving or recommending an idea, product, or candidate.
We believe that using “endorse” in a psychiatric context could create confusion among medical trainees and professionals who are familiar with the correct meanings of the word.
Survey: Some residents use ‘endorse’ in oral presentations
We asked residents in the Department of Psychiatry at Drexel University College of Medicine to respond to a questionnaire regarding their understanding of the use of “endorse.” Their responses are summarized in Table 2.
What is wrong with using ‘endorse’? Except when “endorse” describes a patient formally affixing her (his) signature to a document for the purpose of (1) certification or (2) giving or showing one’s support for a cause, we think that use of the word in psychiatry is not in keeping with its formal, accepted definition. Furthermore, residents’ responses to our survey suggest that there is the danger of causing confusion in using the word“endorse” when “report” or “describe” is meant.
For example, if a patient “endorses” antisocial behavior, is she stating that she feels justified in exhibiting such behavior? Do students who “endorse” drug use approve of drug use? Another example: Youth who “endorse” gang membership have merely confirmed that they belonged to a gang at some time.
The intended meaning of “endorse” in these examples is probably closer to “admit” or “acknowledge.” The patient replies “yes” when the physician asks if she uses drugs or has had behavior problems; she is not necessarily recommending or approving these behaviors.
Usage is shifting. In the past, “complain” was common medical parlance for a patient’s report of symptoms or other health-related problems. In fact, medical, surgical, and psychiatric evaluations still begin with a “chief complaint” section. It’s possible that, because “complaint” might suggest that the patient is whining, the word fell out of favor in the medical lexicon and was replaced in the scholarly literature by the construction “the patient reports….”
Avoid jargon. Employ accurate terminology
We propose that “endorse,” like “complain,” is a cant of psychiatrists. We recommend that, when describing a patient’s statement or report of symptoms or experiences, practitioners should avoid “endorse” and write or say “report,” “express,” “exhibit,” or similar words. Using accurate terminology and avoiding imprecise or misleading jargon is not only linguistically appropriate but also can help avoid misunderstanding and improve patient care.
Acknowledgment
Diana Winters, Academic Publishing Services, Drexel University College of Medicine, provided editorial assistance in preparing the manuscript of this article and offered comment on the use of medical jargon.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strauss GP, Gold JM. A new perspective on anhedonia in schizophrenia. Am J Psychiatry. 2012;169(4):364-373.
2. Thomas JJ, Weigel TJ, Lawton RK, et al. Cognitive-behavioral treatment of body image disturbance in a congenitally blind patient with anorexia nervosa. Am J Psychiatry. 2012;169(1):16-20.
3. Purcell B, Heisel MJ, Speice J, et al. Family connectedness moderates the association between living alone and suicide ideation in a clinical sample of adults 50 years and older. Am J Geriatr Psychiatry. 2012;20(8):717-723.
4. Dakin EK, Areán P. Patient perspectives on the benefits of psychotherapy for late-life depression. Am J Geriatr Psychiatry. 2013;21(2):155-163.
5. Mezuk B, Lohman M, Dumenci, L, et al. Are depression and frailty overlapping syndromes in mid- and late-life? A latent variable analysis. Am J Geriatr Psychiatry. 2013;21(6):560-569.
6. Boindala NS, Tucker P, Trautman RP. “Culture and psychiatry”: a course for second-year psychiatry residents. Acad Psychiatry. 2013;37(1):46-50.
7. Henry A, Kisicki MD, Varley C. Efficacy and safety of antidepressant drug treatment in children and adolescents. Mol Psychiatry. 2012;17(12):1186-1193.
8. Rodriguez CI, Kegeles LS, Levinson A, et al. A randomized controlled crossover trial of ketamine in obsessive-compulsive disorder (abstract W7). Neuropsychopharmacology. 2012;38:S317.
9. Whelan R, Garavan H. Fractionating the impulsivity construct in adolescence. Neuropsychopharmacology. 2013;38(1):250-251.
10. Rück C, Larsson KJ, Mataix-Cols D. Predictors of medium and long-term outcome following capsulotomy for obsessive-compulsive disorder: one site may not fit all. Eur Neuropsychopharmacol. 2012;22(6):406-414.
11. Mausbach BT, Chattillion EA, Roepke SK, et al. A comparison of psychosocial outcomes in elderly Alzheimer caregivers and noncaregivers. Am J Geriatr Psychiatry. 2013;21(1):5-13.
12. Peavy GM, Salmon DP, Edland SD, et al. Neuropsychiatric features of frontal lobe dysfunction in autopsy-confirmed patients with lewy bodies and “pure” Alzheimer disease. Am J Geriatr Psychiatry. 2013;21(6):509-519.
13. Coid JW, Ullrich S, Keers R, et al. Gang membership, violence, and psychiatric morbidity. Am J Psychiatry. 2013;170(9):985-993.
14. Choi D, Tolova V, Socha E, et al. Substance use and attitudes on professional conduct among medical students: a single-institution study. Acad Psychiatry. 2013;37(3):191-195.
15. Endorse. Merriam-Webster. http://www.merriam-webster. com/dictionary/endorse. Accessed January 14, 2014.
16. Endorse. Oxford Dictionaries. http://www.oxforddictionaries. com/definition/english/endorse. Accessed January 14, 2014.
1. Strauss GP, Gold JM. A new perspective on anhedonia in schizophrenia. Am J Psychiatry. 2012;169(4):364-373.
2. Thomas JJ, Weigel TJ, Lawton RK, et al. Cognitive-behavioral treatment of body image disturbance in a congenitally blind patient with anorexia nervosa. Am J Psychiatry. 2012;169(1):16-20.
3. Purcell B, Heisel MJ, Speice J, et al. Family connectedness moderates the association between living alone and suicide ideation in a clinical sample of adults 50 years and older. Am J Geriatr Psychiatry. 2012;20(8):717-723.
4. Dakin EK, Areán P. Patient perspectives on the benefits of psychotherapy for late-life depression. Am J Geriatr Psychiatry. 2013;21(2):155-163.
5. Mezuk B, Lohman M, Dumenci, L, et al. Are depression and frailty overlapping syndromes in mid- and late-life? A latent variable analysis. Am J Geriatr Psychiatry. 2013;21(6):560-569.
6. Boindala NS, Tucker P, Trautman RP. “Culture and psychiatry”: a course for second-year psychiatry residents. Acad Psychiatry. 2013;37(1):46-50.
7. Henry A, Kisicki MD, Varley C. Efficacy and safety of antidepressant drug treatment in children and adolescents. Mol Psychiatry. 2012;17(12):1186-1193.
8. Rodriguez CI, Kegeles LS, Levinson A, et al. A randomized controlled crossover trial of ketamine in obsessive-compulsive disorder (abstract W7). Neuropsychopharmacology. 2012;38:S317.
9. Whelan R, Garavan H. Fractionating the impulsivity construct in adolescence. Neuropsychopharmacology. 2013;38(1):250-251.
10. Rück C, Larsson KJ, Mataix-Cols D. Predictors of medium and long-term outcome following capsulotomy for obsessive-compulsive disorder: one site may not fit all. Eur Neuropsychopharmacol. 2012;22(6):406-414.
11. Mausbach BT, Chattillion EA, Roepke SK, et al. A comparison of psychosocial outcomes in elderly Alzheimer caregivers and noncaregivers. Am J Geriatr Psychiatry. 2013;21(1):5-13.
12. Peavy GM, Salmon DP, Edland SD, et al. Neuropsychiatric features of frontal lobe dysfunction in autopsy-confirmed patients with lewy bodies and “pure” Alzheimer disease. Am J Geriatr Psychiatry. 2013;21(6):509-519.
13. Coid JW, Ullrich S, Keers R, et al. Gang membership, violence, and psychiatric morbidity. Am J Psychiatry. 2013;170(9):985-993.
14. Choi D, Tolova V, Socha E, et al. Substance use and attitudes on professional conduct among medical students: a single-institution study. Acad Psychiatry. 2013;37(3):191-195.
15. Endorse. Merriam-Webster. http://www.merriam-webster. com/dictionary/endorse. Accessed January 14, 2014.
16. Endorse. Oxford Dictionaries. http://www.oxforddictionaries. com/definition/english/endorse. Accessed January 14, 2014.
Discharging your patient: A complex process
Let me begin with a story.
A few years ago, when I was hoping to get into a psychiatry residency program, I did a month-long rotation in the intensive care unit (ICU) of a local hospital. One of our patients was a long-term resident of a nearby assisted living facility, who was treated for exacerbation of a chronic medical illness. Eventually this patient was stabilized to the point at which he could be discharged.
When the ICU physician decided to discharge this patient, he told the team that the man would need to be “sent back to a nursing home.” The social worker, assuming that the physician wanted to place the patient in a skilled nursing facility, spent several hours trying to place the man in one of the local facilities. When the patient’s daughter arrived to visit her father and began asking questions about why he was being placed in a nursing home, staff immediately realized that the physician had simply meant for him to go back “home”—that is, to the facility from which he had come and where he had been living for several years.
Being the only person in the ICU who was a licensed nursing home administrator, with more than 10 years experience in a long-term care, I should have pointed out this miscommunication or, at least, should have raised the question to clarify the physician’s intent. At the time, however, I wasn’t comfortable expressing my concern because I was “just an FMG observer” trying to stay on the attending’s good side.
I made a commitment to myself, however, to always talk about patients’ long-term care options and discharge planning algorithm with medical students, fellow residents, and other medical professionals I meet in my work. The following is an expression of that commitment.
Why focus on discharge when care is still underway?
Discharge planning usually begins on the first day of hospitalization. Before we are ready to discharge any patient, we, the physicians, usually have had many conversations with members of the multidisciplinary team and, always, with the patient and his (her) guardian(s). Why do we do all of this? The answer is simple: Physicians make the ultimate decision about what kind of environment (clinical, social, etc.) the patient is safe to be discharged to; after that decision is made, everything else is the patient’s choice. Our decision should be based on, first, global assessment of functioning—the ability to perform activities of daily living (ADL) and instrumental (non-essential) ADL—and, second, essential input from members of multidisciplinary team.
Here is an example to illustrate this point: If we (the multidisciplinary team) believe that a patient who has lived alone and, up to this point, was able to handle his own affairs, will not be safe if he is discharged to his home (based on observation of his overall daily functioning) but he refuses to be institutionalized, we can evaluate his competency and initiate a motion to obtain a temporary guardianship.
If, on the other hand, we think that a patient needs to be placed in a skilled nursing facility and he, being fully aware of his condition, agrees with the decision of the multidisciplinary team, we cannot place him in a facility of our choosing (if it is against his will). Rather, we must give him options of facilities with similar services that meet his needs and let him or his guardian select the facility in which he’s to be placed.
How do we decide on the best course?
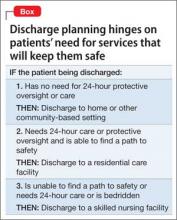
To choose what kind of environment a patient needs to be placed in after discharge, we can apply a simple algorithm (Box):
The patient does not need 24-hour protective oversight or needs some, but not 24-hour, care. Discharge him to a home-and community-based care setting—with arrangements for home health agency services or a home-modification program. The patient would either live independently or in a group home setting, depending on how much assistance he requires.
The patient does need 24-hour protective oversight and more than minimal assistance with ADL but doesn’t need 24-hour care, IV medication, etc.). In this case, the patient can be discharged to an assisted living or residential care facility, assuming that he is able to 1) find a so-called path to safety in an emergency (this why facilities are required to perform 1 fire drill per shift per month) and 2) afford rent, because Medicaid, Medicare, and many private insurance policies do not cover housing expenses (see “Keep financing in mind,” in the next section).
The patient is bed-bound or needs 24-hour treatment (eg, receives IV medication or needs total nursing care) or is not bed-bound but is unable to find a path to safety (eg, a person with dementia). This kind of patient must be placed in a skilled nursing facility
Keep financing in mind
The patient’s ability to pay, as well as having access to insurance or a financial assistance program, is a major contributing factor in discharge planning. All financial options need to be considered by the physicians leading the discharge planning team.
Neither Medicaid nor Medicare benefits are available to pay rent; these insurance programs pay for medical services only. Medicaid does provide some money for assistance with ADL in home- and community-based settings (such assistance is arranged through, and provided by, home health care agencies) and to Medicaid-eligible residents of an assisted living facility.
Medicaid covers 100% of a nursing home stay for an eligible resident. Medicare might cover the cost of skilled-nursing facility care if the placement falls under the criterion of an “episode of care.”
It is worth mentioning that some Veterans’ Administration money might be available to a veteran or his (her) surviving spouse for assistance with ADL in home- and community-based settings or if he (she) is institutionalized. Other local programs might provide eligible recipients with long-term care services; discharge social workers, as members of the multidisciplinary team, usually are resourceful at identifying such programs.
All in all, a complex project
Discharge planning is almost as important as the treatment given to the patient. It can be difficult to put all the pieces of the discharge plan together; sometimes, unclear disposition is the only reason a patient is kept in the hospital after being stabilized.
Above all, our ability to work with the multidisciplinary team and our knowledge of these simple steps will help us navigate our patients’ care plan successfully.
Disclosure
Dr. Graypel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Let me begin with a story.
A few years ago, when I was hoping to get into a psychiatry residency program, I did a month-long rotation in the intensive care unit (ICU) of a local hospital. One of our patients was a long-term resident of a nearby assisted living facility, who was treated for exacerbation of a chronic medical illness. Eventually this patient was stabilized to the point at which he could be discharged.
When the ICU physician decided to discharge this patient, he told the team that the man would need to be “sent back to a nursing home.” The social worker, assuming that the physician wanted to place the patient in a skilled nursing facility, spent several hours trying to place the man in one of the local facilities. When the patient’s daughter arrived to visit her father and began asking questions about why he was being placed in a nursing home, staff immediately realized that the physician had simply meant for him to go back “home”—that is, to the facility from which he had come and where he had been living for several years.
Being the only person in the ICU who was a licensed nursing home administrator, with more than 10 years experience in a long-term care, I should have pointed out this miscommunication or, at least, should have raised the question to clarify the physician’s intent. At the time, however, I wasn’t comfortable expressing my concern because I was “just an FMG observer” trying to stay on the attending’s good side.
I made a commitment to myself, however, to always talk about patients’ long-term care options and discharge planning algorithm with medical students, fellow residents, and other medical professionals I meet in my work. The following is an expression of that commitment.
Why focus on discharge when care is still underway?
Discharge planning usually begins on the first day of hospitalization. Before we are ready to discharge any patient, we, the physicians, usually have had many conversations with members of the multidisciplinary team and, always, with the patient and his (her) guardian(s). Why do we do all of this? The answer is simple: Physicians make the ultimate decision about what kind of environment (clinical, social, etc.) the patient is safe to be discharged to; after that decision is made, everything else is the patient’s choice. Our decision should be based on, first, global assessment of functioning—the ability to perform activities of daily living (ADL) and instrumental (non-essential) ADL—and, second, essential input from members of multidisciplinary team.
Here is an example to illustrate this point: If we (the multidisciplinary team) believe that a patient who has lived alone and, up to this point, was able to handle his own affairs, will not be safe if he is discharged to his home (based on observation of his overall daily functioning) but he refuses to be institutionalized, we can evaluate his competency and initiate a motion to obtain a temporary guardianship.
If, on the other hand, we think that a patient needs to be placed in a skilled nursing facility and he, being fully aware of his condition, agrees with the decision of the multidisciplinary team, we cannot place him in a facility of our choosing (if it is against his will). Rather, we must give him options of facilities with similar services that meet his needs and let him or his guardian select the facility in which he’s to be placed.
How do we decide on the best course?
To choose what kind of environment a patient needs to be placed in after discharge, we can apply a simple algorithm (Box):
The patient does not need 24-hour protective oversight or needs some, but not 24-hour, care. Discharge him to a home-and community-based care setting—with arrangements for home health agency services or a home-modification program. The patient would either live independently or in a group home setting, depending on how much assistance he requires.
The patient does need 24-hour protective oversight and more than minimal assistance with ADL but doesn’t need 24-hour care, IV medication, etc.). In this case, the patient can be discharged to an assisted living or residential care facility, assuming that he is able to 1) find a so-called path to safety in an emergency (this why facilities are required to perform 1 fire drill per shift per month) and 2) afford rent, because Medicaid, Medicare, and many private insurance policies do not cover housing expenses (see “Keep financing in mind,” in the next section).
The patient is bed-bound or needs 24-hour treatment (eg, receives IV medication or needs total nursing care) or is not bed-bound but is unable to find a path to safety (eg, a person with dementia). This kind of patient must be placed in a skilled nursing facility
Keep financing in mind
The patient’s ability to pay, as well as having access to insurance or a financial assistance program, is a major contributing factor in discharge planning. All financial options need to be considered by the physicians leading the discharge planning team.
Neither Medicaid nor Medicare benefits are available to pay rent; these insurance programs pay for medical services only. Medicaid does provide some money for assistance with ADL in home- and community-based settings (such assistance is arranged through, and provided by, home health care agencies) and to Medicaid-eligible residents of an assisted living facility.
Medicaid covers 100% of a nursing home stay for an eligible resident. Medicare might cover the cost of skilled-nursing facility care if the placement falls under the criterion of an “episode of care.”
It is worth mentioning that some Veterans’ Administration money might be available to a veteran or his (her) surviving spouse for assistance with ADL in home- and community-based settings or if he (she) is institutionalized. Other local programs might provide eligible recipients with long-term care services; discharge social workers, as members of the multidisciplinary team, usually are resourceful at identifying such programs.
All in all, a complex project
Discharge planning is almost as important as the treatment given to the patient. It can be difficult to put all the pieces of the discharge plan together; sometimes, unclear disposition is the only reason a patient is kept in the hospital after being stabilized.
Above all, our ability to work with the multidisciplinary team and our knowledge of these simple steps will help us navigate our patients’ care plan successfully.
Disclosure
Dr. Graypel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Let me begin with a story.
A few years ago, when I was hoping to get into a psychiatry residency program, I did a month-long rotation in the intensive care unit (ICU) of a local hospital. One of our patients was a long-term resident of a nearby assisted living facility, who was treated for exacerbation of a chronic medical illness. Eventually this patient was stabilized to the point at which he could be discharged.
When the ICU physician decided to discharge this patient, he told the team that the man would need to be “sent back to a nursing home.” The social worker, assuming that the physician wanted to place the patient in a skilled nursing facility, spent several hours trying to place the man in one of the local facilities. When the patient’s daughter arrived to visit her father and began asking questions about why he was being placed in a nursing home, staff immediately realized that the physician had simply meant for him to go back “home”—that is, to the facility from which he had come and where he had been living for several years.
Being the only person in the ICU who was a licensed nursing home administrator, with more than 10 years experience in a long-term care, I should have pointed out this miscommunication or, at least, should have raised the question to clarify the physician’s intent. At the time, however, I wasn’t comfortable expressing my concern because I was “just an FMG observer” trying to stay on the attending’s good side.
I made a commitment to myself, however, to always talk about patients’ long-term care options and discharge planning algorithm with medical students, fellow residents, and other medical professionals I meet in my work. The following is an expression of that commitment.
Why focus on discharge when care is still underway?
Discharge planning usually begins on the first day of hospitalization. Before we are ready to discharge any patient, we, the physicians, usually have had many conversations with members of the multidisciplinary team and, always, with the patient and his (her) guardian(s). Why do we do all of this? The answer is simple: Physicians make the ultimate decision about what kind of environment (clinical, social, etc.) the patient is safe to be discharged to; after that decision is made, everything else is the patient’s choice. Our decision should be based on, first, global assessment of functioning—the ability to perform activities of daily living (ADL) and instrumental (non-essential) ADL—and, second, essential input from members of multidisciplinary team.
Here is an example to illustrate this point: If we (the multidisciplinary team) believe that a patient who has lived alone and, up to this point, was able to handle his own affairs, will not be safe if he is discharged to his home (based on observation of his overall daily functioning) but he refuses to be institutionalized, we can evaluate his competency and initiate a motion to obtain a temporary guardianship.
If, on the other hand, we think that a patient needs to be placed in a skilled nursing facility and he, being fully aware of his condition, agrees with the decision of the multidisciplinary team, we cannot place him in a facility of our choosing (if it is against his will). Rather, we must give him options of facilities with similar services that meet his needs and let him or his guardian select the facility in which he’s to be placed.
How do we decide on the best course?
To choose what kind of environment a patient needs to be placed in after discharge, we can apply a simple algorithm (Box):
The patient does not need 24-hour protective oversight or needs some, but not 24-hour, care. Discharge him to a home-and community-based care setting—with arrangements for home health agency services or a home-modification program. The patient would either live independently or in a group home setting, depending on how much assistance he requires.
The patient does need 24-hour protective oversight and more than minimal assistance with ADL but doesn’t need 24-hour care, IV medication, etc.). In this case, the patient can be discharged to an assisted living or residential care facility, assuming that he is able to 1) find a so-called path to safety in an emergency (this why facilities are required to perform 1 fire drill per shift per month) and 2) afford rent, because Medicaid, Medicare, and many private insurance policies do not cover housing expenses (see “Keep financing in mind,” in the next section).
The patient is bed-bound or needs 24-hour treatment (eg, receives IV medication or needs total nursing care) or is not bed-bound but is unable to find a path to safety (eg, a person with dementia). This kind of patient must be placed in a skilled nursing facility
Keep financing in mind
The patient’s ability to pay, as well as having access to insurance or a financial assistance program, is a major contributing factor in discharge planning. All financial options need to be considered by the physicians leading the discharge planning team.
Neither Medicaid nor Medicare benefits are available to pay rent; these insurance programs pay for medical services only. Medicaid does provide some money for assistance with ADL in home- and community-based settings (such assistance is arranged through, and provided by, home health care agencies) and to Medicaid-eligible residents of an assisted living facility.
Medicaid covers 100% of a nursing home stay for an eligible resident. Medicare might cover the cost of skilled-nursing facility care if the placement falls under the criterion of an “episode of care.”
It is worth mentioning that some Veterans’ Administration money might be available to a veteran or his (her) surviving spouse for assistance with ADL in home- and community-based settings or if he (she) is institutionalized. Other local programs might provide eligible recipients with long-term care services; discharge social workers, as members of the multidisciplinary team, usually are resourceful at identifying such programs.
All in all, a complex project
Discharge planning is almost as important as the treatment given to the patient. It can be difficult to put all the pieces of the discharge plan together; sometimes, unclear disposition is the only reason a patient is kept in the hospital after being stabilized.
Above all, our ability to work with the multidisciplinary team and our knowledge of these simple steps will help us navigate our patients’ care plan successfully.
Disclosure
Dr. Graypel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
In the drafty call room, a miracle unfolds
I’ve found that, as a resident in psychiatry, it’s rare to experience a moment of truly unbridled achievement while on call. Manning the revolving door of acute psychiatric admissions can be frustrating, not to mention unfulfilling. Maybe that’s why accomplishing a small miracle, you might say, while on call recently felt so satisfying.
Broken window = workplace woes
When working a 12-hour shift, especially overnight, it’s important to have an environment that is conducive to work. As fatigue and stress build, physical comfort means a lot.
Our problem finding physical comfort in the psychiatry resident call room at Saint Louis University was that a fixture on one of the windows had been broken for several years. You could push the window open, but you could not close it. If you called the janitor, he would come and close the window, but there was no guarantee when he’d show up. You might end up typing your notes all evening in the path of a chilly stream of air.
The residents had made a formal request to have the window repaired in a more permanent manner, but this resulted in it being bolted shut. That was a solution, but an imperfect one: Now we had no way to cool the call room in the winter, and it was beginning to smell of body odor.
The psychiatry resident call room is one of the nicer ones I’ve seen, but the building it occupies is a few decades old, and no replacement parts were available for the fixtures. We were stuck with a closed window—so I thought.
That miraculous morning
I was supervising an intern one Saturday, and she had not been paged yet to see patients. The call room was a mess; I telephoned housekeeping to have the beds changed, and maintenance to unclog the sink. When the maintenance man (I’ll call him “Tom”) arrived and fixed the sink, I praised him and asked him to take a look at the window.
“It’s my dream,” I said to no one in particular, “to have a window we can open and shut.”
I didn’t get angry or exert pressure. Tom explained to me that there were no replacement parts.
“Hmm… I see…,” I said.
To my delight, Tom seemed excited to be given a problem to solve. He left to pilfer parts from other windows on the floor.
No luck. The parts were all gone. Tom apologized and suggested we purchase a suction cup, with a cord attached, to pull the window closed.
“Good idea!” I said, thanking him as he went on his way.
But 2 hours later, our maintenance hero, Tom reappeared in the doorway.
“I’ve been thinking about your window all morning,” he announced.
Tom approached the window, unbolted it, and screwed one end of a chain into the frame, creating a makeshift handle. He demonstrated how to pull the window shut.
Voilà! A window we could open and close. The intern’s jaw dropped in amazement. I turned to dance a little jig.
Satisfaction
It’s important to be able to control the temperature in the call room; even more important to have a comfortable, healthy work environment. But knowing I can influence my surroundings to get what I need at work? That’s more important than anything else at all.
Disclosure
Dr. Jennings reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
I’ve found that, as a resident in psychiatry, it’s rare to experience a moment of truly unbridled achievement while on call. Manning the revolving door of acute psychiatric admissions can be frustrating, not to mention unfulfilling. Maybe that’s why accomplishing a small miracle, you might say, while on call recently felt so satisfying.
Broken window = workplace woes
When working a 12-hour shift, especially overnight, it’s important to have an environment that is conducive to work. As fatigue and stress build, physical comfort means a lot.
Our problem finding physical comfort in the psychiatry resident call room at Saint Louis University was that a fixture on one of the windows had been broken for several years. You could push the window open, but you could not close it. If you called the janitor, he would come and close the window, but there was no guarantee when he’d show up. You might end up typing your notes all evening in the path of a chilly stream of air.
The residents had made a formal request to have the window repaired in a more permanent manner, but this resulted in it being bolted shut. That was a solution, but an imperfect one: Now we had no way to cool the call room in the winter, and it was beginning to smell of body odor.
The psychiatry resident call room is one of the nicer ones I’ve seen, but the building it occupies is a few decades old, and no replacement parts were available for the fixtures. We were stuck with a closed window—so I thought.
That miraculous morning
I was supervising an intern one Saturday, and she had not been paged yet to see patients. The call room was a mess; I telephoned housekeeping to have the beds changed, and maintenance to unclog the sink. When the maintenance man (I’ll call him “Tom”) arrived and fixed the sink, I praised him and asked him to take a look at the window.
“It’s my dream,” I said to no one in particular, “to have a window we can open and shut.”
I didn’t get angry or exert pressure. Tom explained to me that there were no replacement parts.
“Hmm… I see…,” I said.
To my delight, Tom seemed excited to be given a problem to solve. He left to pilfer parts from other windows on the floor.
No luck. The parts were all gone. Tom apologized and suggested we purchase a suction cup, with a cord attached, to pull the window closed.
“Good idea!” I said, thanking him as he went on his way.
But 2 hours later, our maintenance hero, Tom reappeared in the doorway.
“I’ve been thinking about your window all morning,” he announced.
Tom approached the window, unbolted it, and screwed one end of a chain into the frame, creating a makeshift handle. He demonstrated how to pull the window shut.
Voilà! A window we could open and close. The intern’s jaw dropped in amazement. I turned to dance a little jig.
Satisfaction
It’s important to be able to control the temperature in the call room; even more important to have a comfortable, healthy work environment. But knowing I can influence my surroundings to get what I need at work? That’s more important than anything else at all.
Disclosure
Dr. Jennings reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
I’ve found that, as a resident in psychiatry, it’s rare to experience a moment of truly unbridled achievement while on call. Manning the revolving door of acute psychiatric admissions can be frustrating, not to mention unfulfilling. Maybe that’s why accomplishing a small miracle, you might say, while on call recently felt so satisfying.
Broken window = workplace woes
When working a 12-hour shift, especially overnight, it’s important to have an environment that is conducive to work. As fatigue and stress build, physical comfort means a lot.
Our problem finding physical comfort in the psychiatry resident call room at Saint Louis University was that a fixture on one of the windows had been broken for several years. You could push the window open, but you could not close it. If you called the janitor, he would come and close the window, but there was no guarantee when he’d show up. You might end up typing your notes all evening in the path of a chilly stream of air.
The residents had made a formal request to have the window repaired in a more permanent manner, but this resulted in it being bolted shut. That was a solution, but an imperfect one: Now we had no way to cool the call room in the winter, and it was beginning to smell of body odor.
The psychiatry resident call room is one of the nicer ones I’ve seen, but the building it occupies is a few decades old, and no replacement parts were available for the fixtures. We were stuck with a closed window—so I thought.
That miraculous morning
I was supervising an intern one Saturday, and she had not been paged yet to see patients. The call room was a mess; I telephoned housekeeping to have the beds changed, and maintenance to unclog the sink. When the maintenance man (I’ll call him “Tom”) arrived and fixed the sink, I praised him and asked him to take a look at the window.
“It’s my dream,” I said to no one in particular, “to have a window we can open and shut.”
I didn’t get angry or exert pressure. Tom explained to me that there were no replacement parts.
“Hmm… I see…,” I said.
To my delight, Tom seemed excited to be given a problem to solve. He left to pilfer parts from other windows on the floor.
No luck. The parts were all gone. Tom apologized and suggested we purchase a suction cup, with a cord attached, to pull the window closed.
“Good idea!” I said, thanking him as he went on his way.
But 2 hours later, our maintenance hero, Tom reappeared in the doorway.
“I’ve been thinking about your window all morning,” he announced.
Tom approached the window, unbolted it, and screwed one end of a chain into the frame, creating a makeshift handle. He demonstrated how to pull the window shut.
Voilà! A window we could open and close. The intern’s jaw dropped in amazement. I turned to dance a little jig.
Satisfaction
It’s important to be able to control the temperature in the call room; even more important to have a comfortable, healthy work environment. But knowing I can influence my surroundings to get what I need at work? That’s more important than anything else at all.
Disclosure
Dr. Jennings reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Blueprint for building a psychiatrist: How residency has prepared us
Becoming a psychiatrist entails a shift in how we see ourselves and those around us. We learn—sometimes the hard way—about cultural self-assessment and the relative nature of our perspective on social, cultural, and clinical matters. What do I mean?
As psychiatrists in the making, we are unaware that we’ve been given this persona-suit, so to speak, with its social expectations and misperceptions. We start noticing how telling people what we do shapes our interactions at cocktail parties, informal gatherings, and in day-to-day life. A new acquaintance might disclose more about herself than she otherwise would or, on the contrary, might become reserved, even guarded. Awkward jokes sometimes are thrown into the mix to lighten the mood. All this is part of the package we’ve been handed, because we chose to specialize in the diagnosis and treatment of mental illness and brain disorders.
So, as I enter my final year of training, I find myself reflecting on just how intense a journey residency has been.
We were physicians first…
We’re psychiatrists now, but first we learned the germ theory of disease, the pathophysiology of every well-known illness, and the scientific basis of the practice of medicine. Many of us weren’t fully aware of the challenges that come with psychiatric training when we signed up. But we powered through— trading set measures and laboratory values for subjective experiences and nonverbal cues. Along the way, we realized that we had to master not only an array of neuropsychiatric facts but other implicit skills: “active listening,” the capacity to make on-the-go complex ethical decisions, and the difficult task of being empathetically detached.
It might be only in retrospect that we can appreciate how residency has shaped us in a personal way—almost as much as it has professionally.
We think of physicians broadly as healers who save lives. Psychiatrists are no different; preventing the most hopeless from dying is something that we do the same way a cardiologist prevents a patient from dying of a massive heart attack. Winning the battle over mortality, by whatever imprecise measures of risk we use, ranks at the top of our therapeutic priorities. We find ourselves scrambling so that catastrophe never happens on our watch. Sometimes, we don’t stop to realize how much of a lifesaver we are— especially because, as junior residents, we’re too pressed for time to reflect and are focused on mastering clinical skills.
New tool to measure success in residency
The Accreditation Council for Graduate Medical Education (ACGME) recently released the “Milestones Project,”1 a thorough evaluation system for residency programs to apply to their trainees. This is a great effort to push for more field-specific evaluation measures among the specialties.
In psychiatry, subjects now considered when evaluating a resident’s progress and preparedness for promotion include competence in applied neuroscience; the practitioner’s emotional response to patients’ problems; and regulatory compliance. Ways doctors learn are changing: Emphasis is now on problem-based learning.2 Patient safety is a priority; to respect that, we are betting strongly on the physician’s aptitude to provide good care by decreasing burnout.3 I am pleased to learn that there are ongoing efforts to improve the way we prepare psychiatrists.
In line with ACGME practices, residency programs also need to continue revisiting their didactic curricula to include innovative, emerging topics. Social media, the antipsychiatry movement, Internet forums, opinionated bloggers, and public figures gone viral—these are some current issues that shouldn’t be ignored during training just because they aren’t discussed in texts or academic journals. Programs that teach and stimulate the inclusion of social sciences and critical thinking should yield better, more holistic psychiatrists.4
For me, these avenues of study have made a huge difference. I feel incredibly grateful for the opportunities that my residency program has provided to me as a psychiatrist-in-training, including a year-long course that touches on novel topics, a weekly process group for all residents, and a broad support network to depend on when personal matters arise.
Mentoring: Invaluable part of the process
As part of the journey through residency, we have the opportunity to work alongside renowned academic psychiatrists, most of who also happen to be amazing people. Mentoring has incredible value at this stage of professional development; don’t shy from taking advantage of that opportunity!
Mentors help us make more informed decisions about our career path. I love hearing the personal stories that my attending physicians tell. On hectic days, when we are beleaguered by managed care and electronic health records, those stories touch us in ways that abstract learning cannot. Internalizing our role models is a conscious and an unconscious element of the process of becoming a psychiatrist.
About that process: It’s far from perfect, always changing, and only the start of our mastery over the tough but rewarding daily tasks of listening… reflecting… prescribing, and, well, saving lives.
Disclosure
Dr. Jovel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Accreditation Council for Graduate Medical Education and American Board of Psychiatry and Neurology. The Psychiatry Milestone Project. http://acgme.org/acgmeweb/ Portals/0/PDFs/Milestones/PsychiatryMilestones.pdf. Published November 2013. Accessed June 23, 2014.
2. Koh GC, Khoo HE, Wong ML, et al. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178(1):34-41.
3. Block L, Wu AW, Feldman L, et al. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J. 2013;89(1055):495-500.
4. Bromley E, Braslow J. Teaching critical thinking in psychiatric training: a role for the social sciences. Am J Psychiatry. 2008; 165(11):1396-1401.
Becoming a psychiatrist entails a shift in how we see ourselves and those around us. We learn—sometimes the hard way—about cultural self-assessment and the relative nature of our perspective on social, cultural, and clinical matters. What do I mean?
As psychiatrists in the making, we are unaware that we’ve been given this persona-suit, so to speak, with its social expectations and misperceptions. We start noticing how telling people what we do shapes our interactions at cocktail parties, informal gatherings, and in day-to-day life. A new acquaintance might disclose more about herself than she otherwise would or, on the contrary, might become reserved, even guarded. Awkward jokes sometimes are thrown into the mix to lighten the mood. All this is part of the package we’ve been handed, because we chose to specialize in the diagnosis and treatment of mental illness and brain disorders.
So, as I enter my final year of training, I find myself reflecting on just how intense a journey residency has been.
We were physicians first…
We’re psychiatrists now, but first we learned the germ theory of disease, the pathophysiology of every well-known illness, and the scientific basis of the practice of medicine. Many of us weren’t fully aware of the challenges that come with psychiatric training when we signed up. But we powered through— trading set measures and laboratory values for subjective experiences and nonverbal cues. Along the way, we realized that we had to master not only an array of neuropsychiatric facts but other implicit skills: “active listening,” the capacity to make on-the-go complex ethical decisions, and the difficult task of being empathetically detached.
It might be only in retrospect that we can appreciate how residency has shaped us in a personal way—almost as much as it has professionally.
We think of physicians broadly as healers who save lives. Psychiatrists are no different; preventing the most hopeless from dying is something that we do the same way a cardiologist prevents a patient from dying of a massive heart attack. Winning the battle over mortality, by whatever imprecise measures of risk we use, ranks at the top of our therapeutic priorities. We find ourselves scrambling so that catastrophe never happens on our watch. Sometimes, we don’t stop to realize how much of a lifesaver we are— especially because, as junior residents, we’re too pressed for time to reflect and are focused on mastering clinical skills.
New tool to measure success in residency
The Accreditation Council for Graduate Medical Education (ACGME) recently released the “Milestones Project,”1 a thorough evaluation system for residency programs to apply to their trainees. This is a great effort to push for more field-specific evaluation measures among the specialties.
In psychiatry, subjects now considered when evaluating a resident’s progress and preparedness for promotion include competence in applied neuroscience; the practitioner’s emotional response to patients’ problems; and regulatory compliance. Ways doctors learn are changing: Emphasis is now on problem-based learning.2 Patient safety is a priority; to respect that, we are betting strongly on the physician’s aptitude to provide good care by decreasing burnout.3 I am pleased to learn that there are ongoing efforts to improve the way we prepare psychiatrists.
In line with ACGME practices, residency programs also need to continue revisiting their didactic curricula to include innovative, emerging topics. Social media, the antipsychiatry movement, Internet forums, opinionated bloggers, and public figures gone viral—these are some current issues that shouldn’t be ignored during training just because they aren’t discussed in texts or academic journals. Programs that teach and stimulate the inclusion of social sciences and critical thinking should yield better, more holistic psychiatrists.4
For me, these avenues of study have made a huge difference. I feel incredibly grateful for the opportunities that my residency program has provided to me as a psychiatrist-in-training, including a year-long course that touches on novel topics, a weekly process group for all residents, and a broad support network to depend on when personal matters arise.
Mentoring: Invaluable part of the process
As part of the journey through residency, we have the opportunity to work alongside renowned academic psychiatrists, most of who also happen to be amazing people. Mentoring has incredible value at this stage of professional development; don’t shy from taking advantage of that opportunity!
Mentors help us make more informed decisions about our career path. I love hearing the personal stories that my attending physicians tell. On hectic days, when we are beleaguered by managed care and electronic health records, those stories touch us in ways that abstract learning cannot. Internalizing our role models is a conscious and an unconscious element of the process of becoming a psychiatrist.
About that process: It’s far from perfect, always changing, and only the start of our mastery over the tough but rewarding daily tasks of listening… reflecting… prescribing, and, well, saving lives.
Disclosure
Dr. Jovel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Becoming a psychiatrist entails a shift in how we see ourselves and those around us. We learn—sometimes the hard way—about cultural self-assessment and the relative nature of our perspective on social, cultural, and clinical matters. What do I mean?
As psychiatrists in the making, we are unaware that we’ve been given this persona-suit, so to speak, with its social expectations and misperceptions. We start noticing how telling people what we do shapes our interactions at cocktail parties, informal gatherings, and in day-to-day life. A new acquaintance might disclose more about herself than she otherwise would or, on the contrary, might become reserved, even guarded. Awkward jokes sometimes are thrown into the mix to lighten the mood. All this is part of the package we’ve been handed, because we chose to specialize in the diagnosis and treatment of mental illness and brain disorders.
So, as I enter my final year of training, I find myself reflecting on just how intense a journey residency has been.
We were physicians first…
We’re psychiatrists now, but first we learned the germ theory of disease, the pathophysiology of every well-known illness, and the scientific basis of the practice of medicine. Many of us weren’t fully aware of the challenges that come with psychiatric training when we signed up. But we powered through— trading set measures and laboratory values for subjective experiences and nonverbal cues. Along the way, we realized that we had to master not only an array of neuropsychiatric facts but other implicit skills: “active listening,” the capacity to make on-the-go complex ethical decisions, and the difficult task of being empathetically detached.
It might be only in retrospect that we can appreciate how residency has shaped us in a personal way—almost as much as it has professionally.
We think of physicians broadly as healers who save lives. Psychiatrists are no different; preventing the most hopeless from dying is something that we do the same way a cardiologist prevents a patient from dying of a massive heart attack. Winning the battle over mortality, by whatever imprecise measures of risk we use, ranks at the top of our therapeutic priorities. We find ourselves scrambling so that catastrophe never happens on our watch. Sometimes, we don’t stop to realize how much of a lifesaver we are— especially because, as junior residents, we’re too pressed for time to reflect and are focused on mastering clinical skills.
New tool to measure success in residency
The Accreditation Council for Graduate Medical Education (ACGME) recently released the “Milestones Project,”1 a thorough evaluation system for residency programs to apply to their trainees. This is a great effort to push for more field-specific evaluation measures among the specialties.
In psychiatry, subjects now considered when evaluating a resident’s progress and preparedness for promotion include competence in applied neuroscience; the practitioner’s emotional response to patients’ problems; and regulatory compliance. Ways doctors learn are changing: Emphasis is now on problem-based learning.2 Patient safety is a priority; to respect that, we are betting strongly on the physician’s aptitude to provide good care by decreasing burnout.3 I am pleased to learn that there are ongoing efforts to improve the way we prepare psychiatrists.
In line with ACGME practices, residency programs also need to continue revisiting their didactic curricula to include innovative, emerging topics. Social media, the antipsychiatry movement, Internet forums, opinionated bloggers, and public figures gone viral—these are some current issues that shouldn’t be ignored during training just because they aren’t discussed in texts or academic journals. Programs that teach and stimulate the inclusion of social sciences and critical thinking should yield better, more holistic psychiatrists.4
For me, these avenues of study have made a huge difference. I feel incredibly grateful for the opportunities that my residency program has provided to me as a psychiatrist-in-training, including a year-long course that touches on novel topics, a weekly process group for all residents, and a broad support network to depend on when personal matters arise.
Mentoring: Invaluable part of the process
As part of the journey through residency, we have the opportunity to work alongside renowned academic psychiatrists, most of who also happen to be amazing people. Mentoring has incredible value at this stage of professional development; don’t shy from taking advantage of that opportunity!
Mentors help us make more informed decisions about our career path. I love hearing the personal stories that my attending physicians tell. On hectic days, when we are beleaguered by managed care and electronic health records, those stories touch us in ways that abstract learning cannot. Internalizing our role models is a conscious and an unconscious element of the process of becoming a psychiatrist.
About that process: It’s far from perfect, always changing, and only the start of our mastery over the tough but rewarding daily tasks of listening… reflecting… prescribing, and, well, saving lives.
Disclosure
Dr. Jovel reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Accreditation Council for Graduate Medical Education and American Board of Psychiatry and Neurology. The Psychiatry Milestone Project. http://acgme.org/acgmeweb/ Portals/0/PDFs/Milestones/PsychiatryMilestones.pdf. Published November 2013. Accessed June 23, 2014.
2. Koh GC, Khoo HE, Wong ML, et al. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178(1):34-41.
3. Block L, Wu AW, Feldman L, et al. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J. 2013;89(1055):495-500.
4. Bromley E, Braslow J. Teaching critical thinking in psychiatric training: a role for the social sciences. Am J Psychiatry. 2008; 165(11):1396-1401.
1. Accreditation Council for Graduate Medical Education and American Board of Psychiatry and Neurology. The Psychiatry Milestone Project. http://acgme.org/acgmeweb/ Portals/0/PDFs/Milestones/PsychiatryMilestones.pdf. Published November 2013. Accessed June 23, 2014.
2. Koh GC, Khoo HE, Wong ML, et al. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178(1):34-41.
3. Block L, Wu AW, Feldman L, et al. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J. 2013;89(1055):495-500.
4. Bromley E, Braslow J. Teaching critical thinking in psychiatric training: a role for the social sciences. Am J Psychiatry. 2008; 165(11):1396-1401.
What we ought to talk about when we’re talking about decriminalizing Cannabis
A green revolution is sweeping through the social and political landscape of the United States—a shifting tide in the way American law and society conceptualize Cannabis as a recreational and a medical substance. In light of the unprecedented legalization of Cannabis in several states, and decriminalization campaigns in other jurisdictions—such as the nation’s capital, where we work—the topic of marijuana has grabbed the nation’s attention and reinvigorated debate about its use.
No dearth of opinion on marijuana use
Legal and economic positions seem to be the pivot points of argument on recreational use of Cannabis—but not, surprisingly, health considerations. Even to the Cannabis non-user, the pending changes in state laws are relevant; after all, every illicit substance can lead to a pathological process and thus a public economic burden.
Articulations of marijuana’s “safety” are nothing new: Consider President Barack Obama’s recent comment that pot is no more dangerous than alcohol (the danger of alcohol is a different argument altogether). There is another layer of Cannabis use—the drug’s psychiatric effects—that is seldom visible to the public eye but quite palpable in the field of mental health—a troubling disconnect because those psychiatric effects have been softened to inconsequence, or are not spoken of at all.
When Cannabis is juxtaposed with other illicit substances, it seems almost innocuous; dependence and withdrawal have not been detailed empirically and are continuously debated. True, consumption of marijuana is not immediately life-threatening, compared with the risk of stroke and myocardial infarction with cocaine use or respiratory depression with narcotic agents. Despite this facade, however, the psychiatric morbidities of marijuana are real and incapacitating, ranging from extreme anxiety and dysregulated mood to chronic psychotic debilitation.
Even after only a few years in psychiatric residency, it has become a common experience for us to observe acute and chronic psychosis in patients after they have used Cannabis. Many require hospitalization or a leave of absence from academics or employment; one of our patients re-matriculated to college after 7 years of intensive care.
Every mental health professional can tell similar tales.
Beyond anecdote
Numerous publications have shown that Cannabis expedites onset of psychotic and prodromal symptoms of schizophrenia. The age range of onset of psychotic symptoms—typically, late adolescence into early 20s—is critical, prognostically.1,2 This epidemiological fact is dangerously in tandem with Cannabis use patterns in America and its college culture. It is known that modifiable risk factors are decisive in the development of psychopathology. Additionally, environmental exposures in the developing brain elicit a more ominous concern because the brain does not complete neural development until early or mid-20s.3
Another concern is the effect of Cannabis on cognition, during periods of acute intoxication and after chronic use. Research on this topic is limited, but evidence suggests that heavy Cannabis use at an early age affects cognition, as measured by a diminished IQ.4 Regrettably, unknowns in this area of study are far more abundant than what we know. This gray area might serve to placate legislators and frequent users and cool discussion.
Rx Cannabis?
Another aspect of the controversy concerns medicinal use of marijuana. Perhaps legalization of medical marijuana has served simply as an antecedent to recreational legalization, as was the case for Colorado and Washington. But under the heading of “medical marijuana” lies a poorly defined, amorphous designation—one that borders on arbitrariness regarding standards of use.
Cancer treatment, pain, glaucoma, HIV, multiple sclerosis are examples of conditions in the bucket list for discretionary use of Cannabis, yet none has a formal FDA indication.5 This absence of approval underscores the lack of empirical validation, quality control, and standardization that are required of every other sanctioned pharmaceutical agent.
Lack of validation also might explain why the collective opinion of major medical associations, including the American Medical Association and the National Council on Alcoholism and Drug Dependence, are opposed to wide availability of smoked marijuana. The American Society of Addiction Medicine, an interdisciplinary organization of physicians, has posted a policy statement affirming that medical marijuana should 1) be held to FDA standards and 2) not be kept under the jurisdiction of state law and regulation.6
Why are psychiatric morbidities of marijuana reported so timidly?
Perhaps the rarity and randomness of long-term illness associated with Cannabis use pacifies individual concerns. Psychiatry understands this reality: All people respond to stresses differently and have specific, individual vulnerabilities. The diathesis-stress model plainly explains this hypothesis— and, sometimes, Cannabis is that stressor. Perhaps a more academic hypothesis is the concept of “ecophenotypes,” which posits that our heritability is not fixed but is in constant calibration with our environment and our adaptability to it. Environment often is a choice that people make.
The fact remains: This drug is risky
Cannabis can precipitate mood and anxiety disorders, alter development of the brain, and serve as a trigger for schizophrenia. The scary truth is that medical science cannot yet tell us who is predisposed to these ill effects and to what degree. In the meantime, society is missing the voice of psychiatry on individual and public health risks that might be the consequences of sweeping legal changes.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Compton MT, Kelley ME, Ramsay CE, et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. Am J Psychiatry. 2009;166(11):1251-1257.
2. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
3. Saez TM, Aronne MP, Caltana L, et al. Prenatal exposure to the CB1 and CB2 cannabinoid receptor agonist WIN 55,212-2 alters migration of early-born glutamatergic neurons and GABAergic interneurons in the rat cerebral cortex. J Neurochem. 2014; 129(4):637-648.
4. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657-E2664.
5. Medical marijuana program physician frequently asked questions. Government of the District of Columbia Department of Health. http://doh.dc.gov/sites/default/files/dc/sites/ doh/publication/attachments/120430FAQPhysicians%20 Final.pdf. Published April 2012. Accessed March 20, 2014.
6. The role of the physician in “medical” marijuana. American Society of Addiction Medicine. http://www.asam.org/ advocacy/find-a-policy-statement/view-policy-statement/ public-policy-statements/2011/11/28/the-role-of-the-physician-in-medical-marijuana. Published April 12, 2010. Accessed March 20, 2014.
A green revolution is sweeping through the social and political landscape of the United States—a shifting tide in the way American law and society conceptualize Cannabis as a recreational and a medical substance. In light of the unprecedented legalization of Cannabis in several states, and decriminalization campaigns in other jurisdictions—such as the nation’s capital, where we work—the topic of marijuana has grabbed the nation’s attention and reinvigorated debate about its use.
No dearth of opinion on marijuana use
Legal and economic positions seem to be the pivot points of argument on recreational use of Cannabis—but not, surprisingly, health considerations. Even to the Cannabis non-user, the pending changes in state laws are relevant; after all, every illicit substance can lead to a pathological process and thus a public economic burden.
Articulations of marijuana’s “safety” are nothing new: Consider President Barack Obama’s recent comment that pot is no more dangerous than alcohol (the danger of alcohol is a different argument altogether). There is another layer of Cannabis use—the drug’s psychiatric effects—that is seldom visible to the public eye but quite palpable in the field of mental health—a troubling disconnect because those psychiatric effects have been softened to inconsequence, or are not spoken of at all.
When Cannabis is juxtaposed with other illicit substances, it seems almost innocuous; dependence and withdrawal have not been detailed empirically and are continuously debated. True, consumption of marijuana is not immediately life-threatening, compared with the risk of stroke and myocardial infarction with cocaine use or respiratory depression with narcotic agents. Despite this facade, however, the psychiatric morbidities of marijuana are real and incapacitating, ranging from extreme anxiety and dysregulated mood to chronic psychotic debilitation.
Even after only a few years in psychiatric residency, it has become a common experience for us to observe acute and chronic psychosis in patients after they have used Cannabis. Many require hospitalization or a leave of absence from academics or employment; one of our patients re-matriculated to college after 7 years of intensive care.
Every mental health professional can tell similar tales.
Beyond anecdote
Numerous publications have shown that Cannabis expedites onset of psychotic and prodromal symptoms of schizophrenia. The age range of onset of psychotic symptoms—typically, late adolescence into early 20s—is critical, prognostically.1,2 This epidemiological fact is dangerously in tandem with Cannabis use patterns in America and its college culture. It is known that modifiable risk factors are decisive in the development of psychopathology. Additionally, environmental exposures in the developing brain elicit a more ominous concern because the brain does not complete neural development until early or mid-20s.3
Another concern is the effect of Cannabis on cognition, during periods of acute intoxication and after chronic use. Research on this topic is limited, but evidence suggests that heavy Cannabis use at an early age affects cognition, as measured by a diminished IQ.4 Regrettably, unknowns in this area of study are far more abundant than what we know. This gray area might serve to placate legislators and frequent users and cool discussion.
Rx Cannabis?
Another aspect of the controversy concerns medicinal use of marijuana. Perhaps legalization of medical marijuana has served simply as an antecedent to recreational legalization, as was the case for Colorado and Washington. But under the heading of “medical marijuana” lies a poorly defined, amorphous designation—one that borders on arbitrariness regarding standards of use.
Cancer treatment, pain, glaucoma, HIV, multiple sclerosis are examples of conditions in the bucket list for discretionary use of Cannabis, yet none has a formal FDA indication.5 This absence of approval underscores the lack of empirical validation, quality control, and standardization that are required of every other sanctioned pharmaceutical agent.
Lack of validation also might explain why the collective opinion of major medical associations, including the American Medical Association and the National Council on Alcoholism and Drug Dependence, are opposed to wide availability of smoked marijuana. The American Society of Addiction Medicine, an interdisciplinary organization of physicians, has posted a policy statement affirming that medical marijuana should 1) be held to FDA standards and 2) not be kept under the jurisdiction of state law and regulation.6
Why are psychiatric morbidities of marijuana reported so timidly?
Perhaps the rarity and randomness of long-term illness associated with Cannabis use pacifies individual concerns. Psychiatry understands this reality: All people respond to stresses differently and have specific, individual vulnerabilities. The diathesis-stress model plainly explains this hypothesis— and, sometimes, Cannabis is that stressor. Perhaps a more academic hypothesis is the concept of “ecophenotypes,” which posits that our heritability is not fixed but is in constant calibration with our environment and our adaptability to it. Environment often is a choice that people make.
The fact remains: This drug is risky
Cannabis can precipitate mood and anxiety disorders, alter development of the brain, and serve as a trigger for schizophrenia. The scary truth is that medical science cannot yet tell us who is predisposed to these ill effects and to what degree. In the meantime, society is missing the voice of psychiatry on individual and public health risks that might be the consequences of sweeping legal changes.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
A green revolution is sweeping through the social and political landscape of the United States—a shifting tide in the way American law and society conceptualize Cannabis as a recreational and a medical substance. In light of the unprecedented legalization of Cannabis in several states, and decriminalization campaigns in other jurisdictions—such as the nation’s capital, where we work—the topic of marijuana has grabbed the nation’s attention and reinvigorated debate about its use.
No dearth of opinion on marijuana use
Legal and economic positions seem to be the pivot points of argument on recreational use of Cannabis—but not, surprisingly, health considerations. Even to the Cannabis non-user, the pending changes in state laws are relevant; after all, every illicit substance can lead to a pathological process and thus a public economic burden.
Articulations of marijuana’s “safety” are nothing new: Consider President Barack Obama’s recent comment that pot is no more dangerous than alcohol (the danger of alcohol is a different argument altogether). There is another layer of Cannabis use—the drug’s psychiatric effects—that is seldom visible to the public eye but quite palpable in the field of mental health—a troubling disconnect because those psychiatric effects have been softened to inconsequence, or are not spoken of at all.
When Cannabis is juxtaposed with other illicit substances, it seems almost innocuous; dependence and withdrawal have not been detailed empirically and are continuously debated. True, consumption of marijuana is not immediately life-threatening, compared with the risk of stroke and myocardial infarction with cocaine use or respiratory depression with narcotic agents. Despite this facade, however, the psychiatric morbidities of marijuana are real and incapacitating, ranging from extreme anxiety and dysregulated mood to chronic psychotic debilitation.
Even after only a few years in psychiatric residency, it has become a common experience for us to observe acute and chronic psychosis in patients after they have used Cannabis. Many require hospitalization or a leave of absence from academics or employment; one of our patients re-matriculated to college after 7 years of intensive care.
Every mental health professional can tell similar tales.
Beyond anecdote
Numerous publications have shown that Cannabis expedites onset of psychotic and prodromal symptoms of schizophrenia. The age range of onset of psychotic symptoms—typically, late adolescence into early 20s—is critical, prognostically.1,2 This epidemiological fact is dangerously in tandem with Cannabis use patterns in America and its college culture. It is known that modifiable risk factors are decisive in the development of psychopathology. Additionally, environmental exposures in the developing brain elicit a more ominous concern because the brain does not complete neural development until early or mid-20s.3
Another concern is the effect of Cannabis on cognition, during periods of acute intoxication and after chronic use. Research on this topic is limited, but evidence suggests that heavy Cannabis use at an early age affects cognition, as measured by a diminished IQ.4 Regrettably, unknowns in this area of study are far more abundant than what we know. This gray area might serve to placate legislators and frequent users and cool discussion.
Rx Cannabis?
Another aspect of the controversy concerns medicinal use of marijuana. Perhaps legalization of medical marijuana has served simply as an antecedent to recreational legalization, as was the case for Colorado and Washington. But under the heading of “medical marijuana” lies a poorly defined, amorphous designation—one that borders on arbitrariness regarding standards of use.
Cancer treatment, pain, glaucoma, HIV, multiple sclerosis are examples of conditions in the bucket list for discretionary use of Cannabis, yet none has a formal FDA indication.5 This absence of approval underscores the lack of empirical validation, quality control, and standardization that are required of every other sanctioned pharmaceutical agent.
Lack of validation also might explain why the collective opinion of major medical associations, including the American Medical Association and the National Council on Alcoholism and Drug Dependence, are opposed to wide availability of smoked marijuana. The American Society of Addiction Medicine, an interdisciplinary organization of physicians, has posted a policy statement affirming that medical marijuana should 1) be held to FDA standards and 2) not be kept under the jurisdiction of state law and regulation.6
Why are psychiatric morbidities of marijuana reported so timidly?
Perhaps the rarity and randomness of long-term illness associated with Cannabis use pacifies individual concerns. Psychiatry understands this reality: All people respond to stresses differently and have specific, individual vulnerabilities. The diathesis-stress model plainly explains this hypothesis— and, sometimes, Cannabis is that stressor. Perhaps a more academic hypothesis is the concept of “ecophenotypes,” which posits that our heritability is not fixed but is in constant calibration with our environment and our adaptability to it. Environment often is a choice that people make.
The fact remains: This drug is risky
Cannabis can precipitate mood and anxiety disorders, alter development of the brain, and serve as a trigger for schizophrenia. The scary truth is that medical science cannot yet tell us who is predisposed to these ill effects and to what degree. In the meantime, society is missing the voice of psychiatry on individual and public health risks that might be the consequences of sweeping legal changes.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Compton MT, Kelley ME, Ramsay CE, et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. Am J Psychiatry. 2009;166(11):1251-1257.
2. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
3. Saez TM, Aronne MP, Caltana L, et al. Prenatal exposure to the CB1 and CB2 cannabinoid receptor agonist WIN 55,212-2 alters migration of early-born glutamatergic neurons and GABAergic interneurons in the rat cerebral cortex. J Neurochem. 2014; 129(4):637-648.
4. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657-E2664.
5. Medical marijuana program physician frequently asked questions. Government of the District of Columbia Department of Health. http://doh.dc.gov/sites/default/files/dc/sites/ doh/publication/attachments/120430FAQPhysicians%20 Final.pdf. Published April 2012. Accessed March 20, 2014.
6. The role of the physician in “medical” marijuana. American Society of Addiction Medicine. http://www.asam.org/ advocacy/find-a-policy-statement/view-policy-statement/ public-policy-statements/2011/11/28/the-role-of-the-physician-in-medical-marijuana. Published April 12, 2010. Accessed March 20, 2014.
1. Compton MT, Kelley ME, Ramsay CE, et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. Am J Psychiatry. 2009;166(11):1251-1257.
2. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
3. Saez TM, Aronne MP, Caltana L, et al. Prenatal exposure to the CB1 and CB2 cannabinoid receptor agonist WIN 55,212-2 alters migration of early-born glutamatergic neurons and GABAergic interneurons in the rat cerebral cortex. J Neurochem. 2014; 129(4):637-648.
4. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657-E2664.
5. Medical marijuana program physician frequently asked questions. Government of the District of Columbia Department of Health. http://doh.dc.gov/sites/default/files/dc/sites/ doh/publication/attachments/120430FAQPhysicians%20 Final.pdf. Published April 2012. Accessed March 20, 2014.
6. The role of the physician in “medical” marijuana. American Society of Addiction Medicine. http://www.asam.org/ advocacy/find-a-policy-statement/view-policy-statement/ public-policy-statements/2011/11/28/the-role-of-the-physician-in-medical-marijuana. Published April 12, 2010. Accessed March 20, 2014.
Making a practical case for marrying psychiatry and neurology
Historically and recently, leaders within psychiatry have expressed disdain over the public’s misunderstanding of the specialty.1 There are many factors—cultural and sociopolitical influences, for example—that contribute to a generalized suspicion of the intent and the abilities of psychiatry. Few observers, however, have focused on how a lack of cohesion within the discipline might be an important, underappreciated influence in the misconceptions and mistrust.
One way to view the recent publication of the DSM-5 is as further positive application of evidence-based medicine and an indicator of the flexible, progressive adaptability of psychiatry. Indeed, Gawande has demonstrated the benefit of implementing a high degree of standardization in terms of maximizing economic efficiency and minimizing medical error.2
Yet critics of psychiatry use the DSM-5 to substantiate their claim that the field is still murky and unsure of itself. Major changes in classification and diagnostic criteria might support a Szaszian fallacy that we somehow create mental illness and simply fit individuals into the framework at our whim. In the midst of what is, at best, lateral movement in psychiatry, the extremism of critics of the specialty, such as Peter Breggin, might gain undeserved credence. Furthermore, the merits of these critics’ arguments remain largely unchallenged in the public arena.
It is worth noting 2 additional factors within psychiatry that contribute to its stagnation:
- Knowledge and practice are grossly misaligned. What practitioners know and what they do are quite different, and the best way to treat mental illness often takes a back seat to tradition or convenience. Consider neuroimaging, which has illustrated structural and functional changes in the brain that have contributed to the phenomenology of schizophrenia. Schizophrenia is considered a clinical diagnosis, but the value of imaging in predicting prognosis, progression, response to treatment, etc. is well known. Yet neuroimaging is underutilized and the cost-benefit analysis of this modality remains unexplored. Likewise, cognitive testing, an important tool in the diagnosis and prognosis of schizophrenia, is not standard practice. These are good reasons why psychiatry shouldn’t shy from the push toward medicalization: Incorporating imaging and genetic analysis into practice will go a long way toward building legitimacy.
- Mental illness is stigmatized within. The stigma of mental illness that psychiatry must overcome is rooted in ignorance and misunderstanding. However, psychiatry itself has done little to eliminate the stigma of mental illness among its practitioners. This is apparent in the punitive, non-progressive nature of most state programs for impaired physicians.3 This type of “individual discrimination” described by Carl Hart4 undoubtedly permeates the residency match and ranking process, even in psychiatry. How can any headway be made in curbing societal intolerance of, say, addiction when it thrives in the academic environment?
A marriage that will dispel ignorance
In light of the continued undervaluation and ignorance of psychiatry, we can start by heeding the Buddhist teaching that change must come from within. To undertake change means to consolidate information and begin to change the inner workings, practices, and structure of the field itself. It means taking seriously the Research Domain Criteria outlined by Thomas Insel, MD, Director of the National Institute of Mental Health.5
It is increasingly apparent that psychiatry and neurology are inseparable.6 Why is there still reluctance to collaborate between the specialties? Why are these 2 fields’ research efforts still relatively distinct from one another, and not being built upon what is already known?
Based on current knowledge, sophisticated proponents of neuropsychiatry aren’t being unreasonable in their desire to push for an elevated status. If the field is to move in the most constructive direction, we should encourage a marriage—a fusion—of psychiatry and neurology. We shouldn’t be satisfied with connecting the specialties in theory and discussion; we should seek a structural unison of departments, journals, teaching, texts, research efforts, and fellowship options and accreditations.
Disclosure
Dr. Siragusa reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Nawkova L, Nawka A, Adamkova T, et al. The picture of mental health/illness in the printed media in three Central European countries. J Health Commun. 2012;17(1):22-40.
2. Gawande A. The checklist manifesto: how to get things right. New York, NY: Henry Holt and Company; 2009.
3. Chander K. Licensing boards and the stigma of mental illness. JAMA. 1999;281(7):606-607.
4. Hart C. High price: a neuroscientist’s journey of self-discovery that challenges everything you know about drugs and society. New York, NY: Harper Collins; 2013.
5. National Institute of Mental Health. Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml. Accessed December 18, 2013.
6. Nasrallah HA. Let’s tear down the silos and reunify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
Historically and recently, leaders within psychiatry have expressed disdain over the public’s misunderstanding of the specialty.1 There are many factors—cultural and sociopolitical influences, for example—that contribute to a generalized suspicion of the intent and the abilities of psychiatry. Few observers, however, have focused on how a lack of cohesion within the discipline might be an important, underappreciated influence in the misconceptions and mistrust.
One way to view the recent publication of the DSM-5 is as further positive application of evidence-based medicine and an indicator of the flexible, progressive adaptability of psychiatry. Indeed, Gawande has demonstrated the benefit of implementing a high degree of standardization in terms of maximizing economic efficiency and minimizing medical error.2
Yet critics of psychiatry use the DSM-5 to substantiate their claim that the field is still murky and unsure of itself. Major changes in classification and diagnostic criteria might support a Szaszian fallacy that we somehow create mental illness and simply fit individuals into the framework at our whim. In the midst of what is, at best, lateral movement in psychiatry, the extremism of critics of the specialty, such as Peter Breggin, might gain undeserved credence. Furthermore, the merits of these critics’ arguments remain largely unchallenged in the public arena.
It is worth noting 2 additional factors within psychiatry that contribute to its stagnation:
- Knowledge and practice are grossly misaligned. What practitioners know and what they do are quite different, and the best way to treat mental illness often takes a back seat to tradition or convenience. Consider neuroimaging, which has illustrated structural and functional changes in the brain that have contributed to the phenomenology of schizophrenia. Schizophrenia is considered a clinical diagnosis, but the value of imaging in predicting prognosis, progression, response to treatment, etc. is well known. Yet neuroimaging is underutilized and the cost-benefit analysis of this modality remains unexplored. Likewise, cognitive testing, an important tool in the diagnosis and prognosis of schizophrenia, is not standard practice. These are good reasons why psychiatry shouldn’t shy from the push toward medicalization: Incorporating imaging and genetic analysis into practice will go a long way toward building legitimacy.
- Mental illness is stigmatized within. The stigma of mental illness that psychiatry must overcome is rooted in ignorance and misunderstanding. However, psychiatry itself has done little to eliminate the stigma of mental illness among its practitioners. This is apparent in the punitive, non-progressive nature of most state programs for impaired physicians.3 This type of “individual discrimination” described by Carl Hart4 undoubtedly permeates the residency match and ranking process, even in psychiatry. How can any headway be made in curbing societal intolerance of, say, addiction when it thrives in the academic environment?
A marriage that will dispel ignorance
In light of the continued undervaluation and ignorance of psychiatry, we can start by heeding the Buddhist teaching that change must come from within. To undertake change means to consolidate information and begin to change the inner workings, practices, and structure of the field itself. It means taking seriously the Research Domain Criteria outlined by Thomas Insel, MD, Director of the National Institute of Mental Health.5
It is increasingly apparent that psychiatry and neurology are inseparable.6 Why is there still reluctance to collaborate between the specialties? Why are these 2 fields’ research efforts still relatively distinct from one another, and not being built upon what is already known?
Based on current knowledge, sophisticated proponents of neuropsychiatry aren’t being unreasonable in their desire to push for an elevated status. If the field is to move in the most constructive direction, we should encourage a marriage—a fusion—of psychiatry and neurology. We shouldn’t be satisfied with connecting the specialties in theory and discussion; we should seek a structural unison of departments, journals, teaching, texts, research efforts, and fellowship options and accreditations.
Disclosure
Dr. Siragusa reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Historically and recently, leaders within psychiatry have expressed disdain over the public’s misunderstanding of the specialty.1 There are many factors—cultural and sociopolitical influences, for example—that contribute to a generalized suspicion of the intent and the abilities of psychiatry. Few observers, however, have focused on how a lack of cohesion within the discipline might be an important, underappreciated influence in the misconceptions and mistrust.
One way to view the recent publication of the DSM-5 is as further positive application of evidence-based medicine and an indicator of the flexible, progressive adaptability of psychiatry. Indeed, Gawande has demonstrated the benefit of implementing a high degree of standardization in terms of maximizing economic efficiency and minimizing medical error.2
Yet critics of psychiatry use the DSM-5 to substantiate their claim that the field is still murky and unsure of itself. Major changes in classification and diagnostic criteria might support a Szaszian fallacy that we somehow create mental illness and simply fit individuals into the framework at our whim. In the midst of what is, at best, lateral movement in psychiatry, the extremism of critics of the specialty, such as Peter Breggin, might gain undeserved credence. Furthermore, the merits of these critics’ arguments remain largely unchallenged in the public arena.
It is worth noting 2 additional factors within psychiatry that contribute to its stagnation:
- Knowledge and practice are grossly misaligned. What practitioners know and what they do are quite different, and the best way to treat mental illness often takes a back seat to tradition or convenience. Consider neuroimaging, which has illustrated structural and functional changes in the brain that have contributed to the phenomenology of schizophrenia. Schizophrenia is considered a clinical diagnosis, but the value of imaging in predicting prognosis, progression, response to treatment, etc. is well known. Yet neuroimaging is underutilized and the cost-benefit analysis of this modality remains unexplored. Likewise, cognitive testing, an important tool in the diagnosis and prognosis of schizophrenia, is not standard practice. These are good reasons why psychiatry shouldn’t shy from the push toward medicalization: Incorporating imaging and genetic analysis into practice will go a long way toward building legitimacy.
- Mental illness is stigmatized within. The stigma of mental illness that psychiatry must overcome is rooted in ignorance and misunderstanding. However, psychiatry itself has done little to eliminate the stigma of mental illness among its practitioners. This is apparent in the punitive, non-progressive nature of most state programs for impaired physicians.3 This type of “individual discrimination” described by Carl Hart4 undoubtedly permeates the residency match and ranking process, even in psychiatry. How can any headway be made in curbing societal intolerance of, say, addiction when it thrives in the academic environment?
A marriage that will dispel ignorance
In light of the continued undervaluation and ignorance of psychiatry, we can start by heeding the Buddhist teaching that change must come from within. To undertake change means to consolidate information and begin to change the inner workings, practices, and structure of the field itself. It means taking seriously the Research Domain Criteria outlined by Thomas Insel, MD, Director of the National Institute of Mental Health.5
It is increasingly apparent that psychiatry and neurology are inseparable.6 Why is there still reluctance to collaborate between the specialties? Why are these 2 fields’ research efforts still relatively distinct from one another, and not being built upon what is already known?
Based on current knowledge, sophisticated proponents of neuropsychiatry aren’t being unreasonable in their desire to push for an elevated status. If the field is to move in the most constructive direction, we should encourage a marriage—a fusion—of psychiatry and neurology. We shouldn’t be satisfied with connecting the specialties in theory and discussion; we should seek a structural unison of departments, journals, teaching, texts, research efforts, and fellowship options and accreditations.
Disclosure
Dr. Siragusa reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Nawkova L, Nawka A, Adamkova T, et al. The picture of mental health/illness in the printed media in three Central European countries. J Health Commun. 2012;17(1):22-40.
2. Gawande A. The checklist manifesto: how to get things right. New York, NY: Henry Holt and Company; 2009.
3. Chander K. Licensing boards and the stigma of mental illness. JAMA. 1999;281(7):606-607.
4. Hart C. High price: a neuroscientist’s journey of self-discovery that challenges everything you know about drugs and society. New York, NY: Harper Collins; 2013.
5. National Institute of Mental Health. Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml. Accessed December 18, 2013.
6. Nasrallah HA. Let’s tear down the silos and reunify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
1. Nawkova L, Nawka A, Adamkova T, et al. The picture of mental health/illness in the printed media in three Central European countries. J Health Commun. 2012;17(1):22-40.
2. Gawande A. The checklist manifesto: how to get things right. New York, NY: Henry Holt and Company; 2009.
3. Chander K. Licensing boards and the stigma of mental illness. JAMA. 1999;281(7):606-607.
4. Hart C. High price: a neuroscientist’s journey of self-discovery that challenges everything you know about drugs and society. New York, NY: Harper Collins; 2013.
5. National Institute of Mental Health. Research Domain Criteria (RDoC). http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml. Accessed December 18, 2013.
6. Nasrallah HA. Let’s tear down the silos and reunify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
Lessons on the path from clinician to forensic expert
As physicians, we strive to heal suffering; as psychiatry trainees, we are taught to relieve that suffering through careful assessment, development of rapport, and empathic care. What then of the forensic expert, whose role is to provide the courts with objective assessment of the “defendant,” free of a therapeutic alliance1,2? Learning to navigate between these different roles is a necessary part of forensic training.2
In my journey to become a forensic psychiatrist equipped to treat adults and youth, I’ve had the good fortune to learn from those who appear to have mastered this balancing act. In this article, I present some of those lessons, with the hope that they will resonate with others—both those who are forensically inclined and those who wish to ease the jolt of being subpoenaed to appear before the court.
A day spent in the system
One of my earliest forensic experiences occurred during my training at Johns Hopkins, when I worked in the municipal court. I learned several lessons when I was assigned to pre-screen a defendant for competency to stand trial3 and criminal responsibility,4 both determined by the court but often informed by forensic evaluation.
Lesson #1: Answer only the question that you have been asked. En route to call for the defendant, I scanned my “how-to” guides and was relieved to learn that I was not to serve as decision-maker or treating clinician.5 I realized that I was not being asked to determine guilt or even give treatment recommendations; having a circumscribed task made that first evaluation less overwhelming. Learning to answer only the question you are being asked is a valuable lesson—one that ought to be remembered by those preparing for forensic evaluations and court testimony.
Lesson #2: There is a place for role induction. Entering a nearly empty office at municipal court, I sat behind a large metal desk and waited for the defendant. When he arrived, dressed in orange and escorted by the armed court officer, I rose to my feet awkwardly. I thought that I should shake hands with him, but stopped my hand in mid-air when I saw his handcuffed wrists.
As the guard knelt to chain the defendant’s ankle shackle to the floor, I waited patiently. Once the guard was outside, I introduced myself and read from my script. I explained the purpose of the evaluation and informed him that, unlike a
physician-patient relationship, this evaluation would not be confidential and would be shared with the court in a written report. Although the content of this introductory segment was in stark contrast to my usual patient encounters, this role induction6 was not. The purpose of role induction in a forensic setting is not to affect prognosis, yet such explanation is necessary to maintain ethical boundaries.1
Lesson #3: Know your phenomenology. Proceeding with the evaluation, I inquired about aspects of the defendant’s life. I attempted to assess his knowledge of the charges against him and how the court works,3 and obtained his account of the reported criminal events.4 Having an interest in psychotic illness and an appreciation for Jaspers’ descriptions of psychiatric phenomenology,7 I confidently delved into questions about the source, number, quality, and content of the voices he reported hearing.
Although not fail-proof, knowledge of phenomenology is necessary to discern whether reported symptoms should be trusted.8,9 In his writings10 and during my brief mentorship by him, Phillip Resnick, MD, stressed the importance of being able to detect malingering through knowledge of classic phenomenology and by maintaining a healthy level of suspicion.
Lesson #4: Impartiality is difficult but necessary. I concluded the interview, thanked the defendant, and asked if he had any questions. He declined. I motioned for the court officer to enter the room, unshackle the defendant from the floor, and escort him out. Exiting the room, I turned off the lights and shut the heavy door. The coldness of the physical environment seemed a metaphor for how I felt during the evaluation: In seeking the “truth,”11 had I lost a vital humanistic element?
Performing that early assessment, I felt as if such work challenged the reason I had decided to enter the medical profession. I struggled to see how such objective work contributed to relieving human suffering.
Now, only slightly more seasoned in this trade, I have a better appreciation for this necessarily impartial work. Although the role of the treating provider and the role of the forensic evaluator are distinct,12 both can be rewarding and both provide a valuable service.
Service in the name of Justice
I believe that, by presenting assessments free of bias, one can further the goal of justice: Forensic psychiatry provides the courts with the means to better understand and gain access to the mental health system. The task seemed daunting at first; now, I welcome opportunities to make such contributions to the fair and just treatment of all people.
Disclosure
Dr. Graham reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Academy of Psychiatry and the Law. AAPL ethical guidelines for the practice of forensic psychiatry (adopted 2005). http://www.aapl.org/ethics.htm. Accessed August 21, 2013.
2. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154(4):448-456.
3. Mossman D, Noffsinger SG, Ash P, et al. AAPL Practice Guideline for the forensic psychiatric evaluation of competence to stand trial. J Am Acad Psychiatry Law. 2007;35(4 suppl): S3-S72.
4. Giorgi-Guarnieri D, Janofsky J, Keram E, et al. AAPL Practice Guideline for forensic psychiatric evaluation of defendants raising the insanity defense. J Am Acad Psychiatry Law. 2002; 30(2 suppl):S3-S40.
5. Rappeport JR. Differences between forensic and general psychiatry. Am J Psychiatry. 1982;139(3):331-334.
6. Chisolm MS, Lyketsos CG. Systematic psychiatric evaluation: a step-by-step guide to applying The Perspectives of Psychiatry. Baltimore, MD: The Johns Hopkins University Press; 2002.
7. Jaspers K. Allgemeine psychopathologie. Berlin, Germany: J Springer; 1913.
8. Soliman S, Resnick PJ. Feigning in adjudicative competence valuations. Behav Sci Law. 2010;28:614-629.
9. Taylor FK. The role of phenomenology in psychiatry. Br J Psychiatry. 1967;113:765-770.
10. Resnick PJ. My favorite tips for detecting malingering and violence risk. Psychiatr Clin North Am. 2007;30(2):227-232
11. Palermo GB. Forensic mental health experts in the court—an ethical dilemma. Int J Offender Ther Comp Criminol. 2003;47(2):122-125.
12. Appelbaum PS. A theory of ethics for forensic psychiatry. J Am Acad Psychiatry Law. 1997;25(3):233-247.
As physicians, we strive to heal suffering; as psychiatry trainees, we are taught to relieve that suffering through careful assessment, development of rapport, and empathic care. What then of the forensic expert, whose role is to provide the courts with objective assessment of the “defendant,” free of a therapeutic alliance1,2? Learning to navigate between these different roles is a necessary part of forensic training.2
In my journey to become a forensic psychiatrist equipped to treat adults and youth, I’ve had the good fortune to learn from those who appear to have mastered this balancing act. In this article, I present some of those lessons, with the hope that they will resonate with others—both those who are forensically inclined and those who wish to ease the jolt of being subpoenaed to appear before the court.
A day spent in the system
One of my earliest forensic experiences occurred during my training at Johns Hopkins, when I worked in the municipal court. I learned several lessons when I was assigned to pre-screen a defendant for competency to stand trial3 and criminal responsibility,4 both determined by the court but often informed by forensic evaluation.
Lesson #1: Answer only the question that you have been asked. En route to call for the defendant, I scanned my “how-to” guides and was relieved to learn that I was not to serve as decision-maker or treating clinician.5 I realized that I was not being asked to determine guilt or even give treatment recommendations; having a circumscribed task made that first evaluation less overwhelming. Learning to answer only the question you are being asked is a valuable lesson—one that ought to be remembered by those preparing for forensic evaluations and court testimony.
Lesson #2: There is a place for role induction. Entering a nearly empty office at municipal court, I sat behind a large metal desk and waited for the defendant. When he arrived, dressed in orange and escorted by the armed court officer, I rose to my feet awkwardly. I thought that I should shake hands with him, but stopped my hand in mid-air when I saw his handcuffed wrists.
As the guard knelt to chain the defendant’s ankle shackle to the floor, I waited patiently. Once the guard was outside, I introduced myself and read from my script. I explained the purpose of the evaluation and informed him that, unlike a
physician-patient relationship, this evaluation would not be confidential and would be shared with the court in a written report. Although the content of this introductory segment was in stark contrast to my usual patient encounters, this role induction6 was not. The purpose of role induction in a forensic setting is not to affect prognosis, yet such explanation is necessary to maintain ethical boundaries.1
Lesson #3: Know your phenomenology. Proceeding with the evaluation, I inquired about aspects of the defendant’s life. I attempted to assess his knowledge of the charges against him and how the court works,3 and obtained his account of the reported criminal events.4 Having an interest in psychotic illness and an appreciation for Jaspers’ descriptions of psychiatric phenomenology,7 I confidently delved into questions about the source, number, quality, and content of the voices he reported hearing.
Although not fail-proof, knowledge of phenomenology is necessary to discern whether reported symptoms should be trusted.8,9 In his writings10 and during my brief mentorship by him, Phillip Resnick, MD, stressed the importance of being able to detect malingering through knowledge of classic phenomenology and by maintaining a healthy level of suspicion.
Lesson #4: Impartiality is difficult but necessary. I concluded the interview, thanked the defendant, and asked if he had any questions. He declined. I motioned for the court officer to enter the room, unshackle the defendant from the floor, and escort him out. Exiting the room, I turned off the lights and shut the heavy door. The coldness of the physical environment seemed a metaphor for how I felt during the evaluation: In seeking the “truth,”11 had I lost a vital humanistic element?
Performing that early assessment, I felt as if such work challenged the reason I had decided to enter the medical profession. I struggled to see how such objective work contributed to relieving human suffering.
Now, only slightly more seasoned in this trade, I have a better appreciation for this necessarily impartial work. Although the role of the treating provider and the role of the forensic evaluator are distinct,12 both can be rewarding and both provide a valuable service.
Service in the name of Justice
I believe that, by presenting assessments free of bias, one can further the goal of justice: Forensic psychiatry provides the courts with the means to better understand and gain access to the mental health system. The task seemed daunting at first; now, I welcome opportunities to make such contributions to the fair and just treatment of all people.
Disclosure
Dr. Graham reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
As physicians, we strive to heal suffering; as psychiatry trainees, we are taught to relieve that suffering through careful assessment, development of rapport, and empathic care. What then of the forensic expert, whose role is to provide the courts with objective assessment of the “defendant,” free of a therapeutic alliance1,2? Learning to navigate between these different roles is a necessary part of forensic training.2
In my journey to become a forensic psychiatrist equipped to treat adults and youth, I’ve had the good fortune to learn from those who appear to have mastered this balancing act. In this article, I present some of those lessons, with the hope that they will resonate with others—both those who are forensically inclined and those who wish to ease the jolt of being subpoenaed to appear before the court.
A day spent in the system
One of my earliest forensic experiences occurred during my training at Johns Hopkins, when I worked in the municipal court. I learned several lessons when I was assigned to pre-screen a defendant for competency to stand trial3 and criminal responsibility,4 both determined by the court but often informed by forensic evaluation.
Lesson #1: Answer only the question that you have been asked. En route to call for the defendant, I scanned my “how-to” guides and was relieved to learn that I was not to serve as decision-maker or treating clinician.5 I realized that I was not being asked to determine guilt or even give treatment recommendations; having a circumscribed task made that first evaluation less overwhelming. Learning to answer only the question you are being asked is a valuable lesson—one that ought to be remembered by those preparing for forensic evaluations and court testimony.
Lesson #2: There is a place for role induction. Entering a nearly empty office at municipal court, I sat behind a large metal desk and waited for the defendant. When he arrived, dressed in orange and escorted by the armed court officer, I rose to my feet awkwardly. I thought that I should shake hands with him, but stopped my hand in mid-air when I saw his handcuffed wrists.
As the guard knelt to chain the defendant’s ankle shackle to the floor, I waited patiently. Once the guard was outside, I introduced myself and read from my script. I explained the purpose of the evaluation and informed him that, unlike a
physician-patient relationship, this evaluation would not be confidential and would be shared with the court in a written report. Although the content of this introductory segment was in stark contrast to my usual patient encounters, this role induction6 was not. The purpose of role induction in a forensic setting is not to affect prognosis, yet such explanation is necessary to maintain ethical boundaries.1
Lesson #3: Know your phenomenology. Proceeding with the evaluation, I inquired about aspects of the defendant’s life. I attempted to assess his knowledge of the charges against him and how the court works,3 and obtained his account of the reported criminal events.4 Having an interest in psychotic illness and an appreciation for Jaspers’ descriptions of psychiatric phenomenology,7 I confidently delved into questions about the source, number, quality, and content of the voices he reported hearing.
Although not fail-proof, knowledge of phenomenology is necessary to discern whether reported symptoms should be trusted.8,9 In his writings10 and during my brief mentorship by him, Phillip Resnick, MD, stressed the importance of being able to detect malingering through knowledge of classic phenomenology and by maintaining a healthy level of suspicion.
Lesson #4: Impartiality is difficult but necessary. I concluded the interview, thanked the defendant, and asked if he had any questions. He declined. I motioned for the court officer to enter the room, unshackle the defendant from the floor, and escort him out. Exiting the room, I turned off the lights and shut the heavy door. The coldness of the physical environment seemed a metaphor for how I felt during the evaluation: In seeking the “truth,”11 had I lost a vital humanistic element?
Performing that early assessment, I felt as if such work challenged the reason I had decided to enter the medical profession. I struggled to see how such objective work contributed to relieving human suffering.
Now, only slightly more seasoned in this trade, I have a better appreciation for this necessarily impartial work. Although the role of the treating provider and the role of the forensic evaluator are distinct,12 both can be rewarding and both provide a valuable service.
Service in the name of Justice
I believe that, by presenting assessments free of bias, one can further the goal of justice: Forensic psychiatry provides the courts with the means to better understand and gain access to the mental health system. The task seemed daunting at first; now, I welcome opportunities to make such contributions to the fair and just treatment of all people.
Disclosure
Dr. Graham reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Academy of Psychiatry and the Law. AAPL ethical guidelines for the practice of forensic psychiatry (adopted 2005). http://www.aapl.org/ethics.htm. Accessed August 21, 2013.
2. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154(4):448-456.
3. Mossman D, Noffsinger SG, Ash P, et al. AAPL Practice Guideline for the forensic psychiatric evaluation of competence to stand trial. J Am Acad Psychiatry Law. 2007;35(4 suppl): S3-S72.
4. Giorgi-Guarnieri D, Janofsky J, Keram E, et al. AAPL Practice Guideline for forensic psychiatric evaluation of defendants raising the insanity defense. J Am Acad Psychiatry Law. 2002; 30(2 suppl):S3-S40.
5. Rappeport JR. Differences between forensic and general psychiatry. Am J Psychiatry. 1982;139(3):331-334.
6. Chisolm MS, Lyketsos CG. Systematic psychiatric evaluation: a step-by-step guide to applying The Perspectives of Psychiatry. Baltimore, MD: The Johns Hopkins University Press; 2002.
7. Jaspers K. Allgemeine psychopathologie. Berlin, Germany: J Springer; 1913.
8. Soliman S, Resnick PJ. Feigning in adjudicative competence valuations. Behav Sci Law. 2010;28:614-629.
9. Taylor FK. The role of phenomenology in psychiatry. Br J Psychiatry. 1967;113:765-770.
10. Resnick PJ. My favorite tips for detecting malingering and violence risk. Psychiatr Clin North Am. 2007;30(2):227-232
11. Palermo GB. Forensic mental health experts in the court—an ethical dilemma. Int J Offender Ther Comp Criminol. 2003;47(2):122-125.
12. Appelbaum PS. A theory of ethics for forensic psychiatry. J Am Acad Psychiatry Law. 1997;25(3):233-247.
1. American Academy of Psychiatry and the Law. AAPL ethical guidelines for the practice of forensic psychiatry (adopted 2005). http://www.aapl.org/ethics.htm. Accessed August 21, 2013.
2. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154(4):448-456.
3. Mossman D, Noffsinger SG, Ash P, et al. AAPL Practice Guideline for the forensic psychiatric evaluation of competence to stand trial. J Am Acad Psychiatry Law. 2007;35(4 suppl): S3-S72.
4. Giorgi-Guarnieri D, Janofsky J, Keram E, et al. AAPL Practice Guideline for forensic psychiatric evaluation of defendants raising the insanity defense. J Am Acad Psychiatry Law. 2002; 30(2 suppl):S3-S40.
5. Rappeport JR. Differences between forensic and general psychiatry. Am J Psychiatry. 1982;139(3):331-334.
6. Chisolm MS, Lyketsos CG. Systematic psychiatric evaluation: a step-by-step guide to applying The Perspectives of Psychiatry. Baltimore, MD: The Johns Hopkins University Press; 2002.
7. Jaspers K. Allgemeine psychopathologie. Berlin, Germany: J Springer; 1913.
8. Soliman S, Resnick PJ. Feigning in adjudicative competence valuations. Behav Sci Law. 2010;28:614-629.
9. Taylor FK. The role of phenomenology in psychiatry. Br J Psychiatry. 1967;113:765-770.
10. Resnick PJ. My favorite tips for detecting malingering and violence risk. Psychiatr Clin North Am. 2007;30(2):227-232
11. Palermo GB. Forensic mental health experts in the court—an ethical dilemma. Int J Offender Ther Comp Criminol. 2003;47(2):122-125.
12. Appelbaum PS. A theory of ethics for forensic psychiatry. J Am Acad Psychiatry Law. 1997;25(3):233-247.