User login
The Hospitalist only
Open ICUs giveth and taketh away
Background: Some academic medical centers and many community centers use “open” ICU models in which primary services longitudinally follow patients into the ICU with intensivist comanagement.
Design: Semistructured interviews with 12 hospitalists and 8 intensivists.
Setting: Open 16-bed ICUs at the University of California, San Francisco. Teams round separately at the bedside and are informally encouraged to check in daily.
Synopsis: The authors iteratively developed the interview questions. Participants were selected using purposive sampling. The main themes were communication, education, and structure. Communication was challenging among teams as well as with patients and families. The open ICU was felt to affect handoffs and care continuity positively. Hospitalists focused more on longitudinal relationships, smoother transitions, and opportunities to observe disease evolution. Intensivists focused more on fragmentation during the ICU stay and noted cognitive disengagement among some team members with certain aspects of patient care. Intensivists did not identify any educational or structural benefits of the open ICU model.
This is the first qualitative study of hospitalist and intensivist perceptions of the open ICU model. The most significant limitation is the risk of bias from the single-center design and purposive sampling. These findings have implications for other models of medical comanagement.
Bottom line: Open ICU models offer a mix of communication, educational, and structural barriers as well as opportunities. Role clarity may help optimize the open ICU model.
Citation: Santhosh L and Sewell J. Hospital and intensivist experiences of the “open” intensive care unit environment: A qualitative exploration. J Gen Intern Med. 2020;35(8):2338-46.
Dr. Sweigart is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: Some academic medical centers and many community centers use “open” ICU models in which primary services longitudinally follow patients into the ICU with intensivist comanagement.
Design: Semistructured interviews with 12 hospitalists and 8 intensivists.
Setting: Open 16-bed ICUs at the University of California, San Francisco. Teams round separately at the bedside and are informally encouraged to check in daily.
Synopsis: The authors iteratively developed the interview questions. Participants were selected using purposive sampling. The main themes were communication, education, and structure. Communication was challenging among teams as well as with patients and families. The open ICU was felt to affect handoffs and care continuity positively. Hospitalists focused more on longitudinal relationships, smoother transitions, and opportunities to observe disease evolution. Intensivists focused more on fragmentation during the ICU stay and noted cognitive disengagement among some team members with certain aspects of patient care. Intensivists did not identify any educational or structural benefits of the open ICU model.
This is the first qualitative study of hospitalist and intensivist perceptions of the open ICU model. The most significant limitation is the risk of bias from the single-center design and purposive sampling. These findings have implications for other models of medical comanagement.
Bottom line: Open ICU models offer a mix of communication, educational, and structural barriers as well as opportunities. Role clarity may help optimize the open ICU model.
Citation: Santhosh L and Sewell J. Hospital and intensivist experiences of the “open” intensive care unit environment: A qualitative exploration. J Gen Intern Med. 2020;35(8):2338-46.
Dr. Sweigart is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: Some academic medical centers and many community centers use “open” ICU models in which primary services longitudinally follow patients into the ICU with intensivist comanagement.
Design: Semistructured interviews with 12 hospitalists and 8 intensivists.
Setting: Open 16-bed ICUs at the University of California, San Francisco. Teams round separately at the bedside and are informally encouraged to check in daily.
Synopsis: The authors iteratively developed the interview questions. Participants were selected using purposive sampling. The main themes were communication, education, and structure. Communication was challenging among teams as well as with patients and families. The open ICU was felt to affect handoffs and care continuity positively. Hospitalists focused more on longitudinal relationships, smoother transitions, and opportunities to observe disease evolution. Intensivists focused more on fragmentation during the ICU stay and noted cognitive disengagement among some team members with certain aspects of patient care. Intensivists did not identify any educational or structural benefits of the open ICU model.
This is the first qualitative study of hospitalist and intensivist perceptions of the open ICU model. The most significant limitation is the risk of bias from the single-center design and purposive sampling. These findings have implications for other models of medical comanagement.
Bottom line: Open ICU models offer a mix of communication, educational, and structural barriers as well as opportunities. Role clarity may help optimize the open ICU model.
Citation: Santhosh L and Sewell J. Hospital and intensivist experiences of the “open” intensive care unit environment: A qualitative exploration. J Gen Intern Med. 2020;35(8):2338-46.
Dr. Sweigart is a hospitalist at the Lexington (Ky.) VA Health Care System.
Resident physician work-hour regulations associated with improved physician safety and health
Background: In 2011, the Accreditation Council for Graduate Medical Education (ACGME) enacted a consecutive work-hour restriction of 16 hours for first-year residents. Reports of these changes have focused on patient safety, resident education, and resident well-being. The impact on resident safety had not been addressed.
Study design: Prospective cohort study.
Setting: U.S. Academic institutions training resident physicians.
Synopsis: This study compared first-year resident physicians from 2002 to 2007 (pre-implementation) and 2014 to 2017 (post-implementation). In all, 5,680 pre-implementation residents and 9,596 post-implementation residents consented to the study. With the 2011 ACGME restriction, the risk of motor vehicle crash decreased 24% (relative risk [RR] .76; .67-.85), and percutaneous injury risk decreased more than 40% (RR .54; .48-.61). Although weekly work hours were significantly higher pre-implementation, self-reported hours involved in patient care were similar for both groups.
While this large, well-powered study suggests extended work-hour restrictions for resident physicians improve their safety, the study is limited by self-reporting of resident physicians. As the ACGME has re-introduced extended duration shifts for first-year resident physicians, hospitalists should advocate for objective physician safety studies in relation to extended-hour shifts.
Bottom line: The 2011 ACGME work-hour reform for first-year physicians improved their safety and health.
Citation: Weaver MD et al. The association between resident physician work-hour regulations and physician safety and health. Am J Med. 2020 July;133(7):e343-54.
Dr. Fletcher is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: In 2011, the Accreditation Council for Graduate Medical Education (ACGME) enacted a consecutive work-hour restriction of 16 hours for first-year residents. Reports of these changes have focused on patient safety, resident education, and resident well-being. The impact on resident safety had not been addressed.
Study design: Prospective cohort study.
Setting: U.S. Academic institutions training resident physicians.
Synopsis: This study compared first-year resident physicians from 2002 to 2007 (pre-implementation) and 2014 to 2017 (post-implementation). In all, 5,680 pre-implementation residents and 9,596 post-implementation residents consented to the study. With the 2011 ACGME restriction, the risk of motor vehicle crash decreased 24% (relative risk [RR] .76; .67-.85), and percutaneous injury risk decreased more than 40% (RR .54; .48-.61). Although weekly work hours were significantly higher pre-implementation, self-reported hours involved in patient care were similar for both groups.
While this large, well-powered study suggests extended work-hour restrictions for resident physicians improve their safety, the study is limited by self-reporting of resident physicians. As the ACGME has re-introduced extended duration shifts for first-year resident physicians, hospitalists should advocate for objective physician safety studies in relation to extended-hour shifts.
Bottom line: The 2011 ACGME work-hour reform for first-year physicians improved their safety and health.
Citation: Weaver MD et al. The association between resident physician work-hour regulations and physician safety and health. Am J Med. 2020 July;133(7):e343-54.
Dr. Fletcher is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: In 2011, the Accreditation Council for Graduate Medical Education (ACGME) enacted a consecutive work-hour restriction of 16 hours for first-year residents. Reports of these changes have focused on patient safety, resident education, and resident well-being. The impact on resident safety had not been addressed.
Study design: Prospective cohort study.
Setting: U.S. Academic institutions training resident physicians.
Synopsis: This study compared first-year resident physicians from 2002 to 2007 (pre-implementation) and 2014 to 2017 (post-implementation). In all, 5,680 pre-implementation residents and 9,596 post-implementation residents consented to the study. With the 2011 ACGME restriction, the risk of motor vehicle crash decreased 24% (relative risk [RR] .76; .67-.85), and percutaneous injury risk decreased more than 40% (RR .54; .48-.61). Although weekly work hours were significantly higher pre-implementation, self-reported hours involved in patient care were similar for both groups.
While this large, well-powered study suggests extended work-hour restrictions for resident physicians improve their safety, the study is limited by self-reporting of resident physicians. As the ACGME has re-introduced extended duration shifts for first-year resident physicians, hospitalists should advocate for objective physician safety studies in relation to extended-hour shifts.
Bottom line: The 2011 ACGME work-hour reform for first-year physicians improved their safety and health.
Citation: Weaver MD et al. The association between resident physician work-hour regulations and physician safety and health. Am J Med. 2020 July;133(7):e343-54.
Dr. Fletcher is a hospitalist at the Lexington (Ky.) VA Health Care System.
Major insurers running billions of dollars behind on payments to hospitals and doctors
Anthem Blue Cross, the country’s second-biggest health insurance company, is behind on billions of dollars in payments owed to hospitals and doctors because of onerous new reimbursement rules, computer problems and mishandled claims, say hospital officials in multiple states.
Anthem, like other big insurers, is using the COVID-19 crisis as cover to institute “egregious” policies that harm patients and pinch hospital finances, said Molly Smith, group vice president at the American Hospital Association. “There’s this sense of ‘Everyone’s distracted. We can get this through.’ ”
Hospitals are also dealing with a spike in retroactive claims denials by UnitedHealthcare, the biggest health insurer, for ED care, the AHA said.
Hospitals say it is hurting their finances as many cope with COVID surges – even after the industry has received tens of billions of dollars in emergency assistance from the federal government.
“We recognize there have been some challenges” to prompt payments caused by claims-processing changes and “a new set of dynamics” amid the pandemic, Anthem spokesperson Colin Manning said in an email. “We apologize for any delays or inconvenience this may have caused.”
Virginia law requires insurers to pay claims within 40 days. In a Sept. 24 letter to state insurance regulators, VCU Health, a system that operates a large teaching hospital in Richmond associated with Virginia Commonwealth University, said Anthem owes it $385 million. More than 40% of the claims are more than 90 days old, VCU said.
For all Virginia hospitals, Anthem’s late, unpaid claims amount to “hundreds of millions of dollars,” the Virginia Hospital and Healthcare Association said in a June 23 letter to state regulators.
Nationwide, the payment delays “are creating an untenable situation,” the American Hospital Association said in a Sept. 9 letter to Anthem CEO Gail Boudreaux. “Patients are facing greater hurdles to accessing care; clinicians are burning out on unnecessary administrative tasks; and the system is straining to finance the personnel and supplies” needed to fight Covid.
Complaints about Anthem extend “from sea to shining sea, from New Hampshire to California,” AHA CEO Rick Pollack told KHN.
Substantial payment delays can be seen on Anthem’s books. On June 30, 2019, before the pandemic, 43% of the insurer’s medical bills for that quarter were unpaid, according to regulatory filings. Two years later that figure had risen to 53% – a difference of $2.5 billion.
Anthem profits were $4.6 billion in 2020 and $3.5 billion in the first half of 2021.
Alexis Thurber, who lives near Seattle, was insured by Anthem when she got an $18,192 hospital bill in May for radiation therapy that doctors said was essential to treat her breast cancer.
The treatments were “experimental” and “not medically necessary,” Anthem said, according to Ms. Thurber. She spent much of the summer trying to get the insurer to pay up – placing two dozen phone calls, spending hours on hold, sending multiple emails and enduring unmeasurable stress and worry. It finally covered the claim months later.
“It’s so egregious. It’s a game they’re playing,” said Ms. Thurber, 51, whose cancer was diagnosed in November. “Trying to get true help was impossible.”
Privacy rules prevent Anthem from commenting on Ms. Thurber’s case, said Anthem spokesperson Colin Manning.
When insurers fail to promptly pay medical bills, patients are left in the lurch. They might first get a notice saying payment is pending or denied. A hospital might bill them for treatment they thought would be covered. Hospitals and doctors often sue patients whose insurance didn’t pay up.
Hospitals point to a variety of Anthem practices contributing to payment delays or denials, including new layers of document requirements, prior-authorization hurdles for routine procedures and requirements that doctors themselves – not support staffers – speak to insurance gatekeepers. “This requires providers to literally leave the patient[’s] bedside to get on the phone with Anthem,” AHA said in its letter.
Anthem often hinders coverage for outpatient surgery, specialty pharmacy and other services in health systems listed as in network, amounting to a “bait and switch” on Anthem members, AHA officials said.
“Demanding that patients be treated outside of the hospital setting, against the advice of the patient’s in-network treating physician, appears to be motivated by a desire to drive up Empire’s profits,” the Greater New York Hospital Association wrote in an April letter to Empire Blue Cross, which is owned by Anthem.
Anthem officials pushed back in a recent letter to the AHA, saying the insurer’s changing rules are intended partly to control excessive prices charged by hospitals for specialty drugs and nonemergency surgery, screening and diagnostic procedures.
Severe problems with Anthem’s new claims management system surfaced months ago and “persist without meaningful improvement,” AHA said in its letter.
Claims have gotten lost in Anthem’s computers, and in some cases VCU Health has had to print medical records and mail them to get paid, VCU said in its letter. The cash slowdown imposes “an unmanageable disruption that threatens to undermine our financial footing,” VCU said.
United denied $31,557 in claims for Emily Long’s care after she was struck in June by a motorcycle in New York City. She needed surgery to repair a fractured cheekbone. United said there was a lack of documentation for “medical necessity” – an “incredibly aggravating” response on top of the distress of the accident, Ms. Long said.
The Brooklyn hospital that treated Ms. Long was “paid appropriately under her plan and within the required time frame,” said United spokesperson Maria Gordon Shydlo. “The facility has the right to appeal the decision.”
United’s unpaid claims came to 54% as of June 30, about the same level as 2 years previously.
When Erin Conlisk initially had trouble gaining approval for a piece of medical equipment for her elderly father this summer, United employees told her the insurer’s entire prior-authorization database had gone down for weeks, said Ms. Conlisk, who lives in California.
“There was a brief issue with our prior-authorization process in mid-July, which was resolved quickly,” Gordon Shydlo said.
When asked by Wall Street analysts about the payment backups, Anthem executives said it partly reflects their decision to increase financial reserves amid the health crisis.
“Really a ton of uncertainty associated with this environment,” John Gallina, the company’s chief financial officer, said on a conference call in July. “We’ve tried to be extremely prudent and conservative in our approach.”
During the pandemic, hospitals have benefited from two extraordinary cash infusions. They and other medical providers have received more than $100 billion through the CARES Act of 2020 and the American Rescue Plan of 2021. Last year United, Anthem and other insurers accelerated billions in hospital reimbursements.
The federal payments enriched many of the biggest, wealthiest systems while poorer hospitals serving low-income patients and rural areas struggled.
Those are the systems most hurt now by insurer payment delays, hospital officials said. Federal relief funds “have been a lifeline, but they don’t make people whole in terms of the losses from increased expenses and lost revenue as a result of the COVID experience,” Mr. Pollack said.
Several health systems declined to comment about claims payment delays or didn’t respond to a reporter’s queries. Among individual hospitals “there is a deep fear of talking on the record about your largest business partner,” AHA’s Ms. Smith said.
Alexis Thurber worried she might have to pay her $18,192 radiation bill herself, and she’s not confident her Anthem policy will do a better job next time of covering the cost of her care.
“It makes me not want to go to the doctor anymore,” she said. “I’m scared to get another mammogram because you can’t rely on it.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Anthem Blue Cross, the country’s second-biggest health insurance company, is behind on billions of dollars in payments owed to hospitals and doctors because of onerous new reimbursement rules, computer problems and mishandled claims, say hospital officials in multiple states.
Anthem, like other big insurers, is using the COVID-19 crisis as cover to institute “egregious” policies that harm patients and pinch hospital finances, said Molly Smith, group vice president at the American Hospital Association. “There’s this sense of ‘Everyone’s distracted. We can get this through.’ ”
Hospitals are also dealing with a spike in retroactive claims denials by UnitedHealthcare, the biggest health insurer, for ED care, the AHA said.
Hospitals say it is hurting their finances as many cope with COVID surges – even after the industry has received tens of billions of dollars in emergency assistance from the federal government.
“We recognize there have been some challenges” to prompt payments caused by claims-processing changes and “a new set of dynamics” amid the pandemic, Anthem spokesperson Colin Manning said in an email. “We apologize for any delays or inconvenience this may have caused.”
Virginia law requires insurers to pay claims within 40 days. In a Sept. 24 letter to state insurance regulators, VCU Health, a system that operates a large teaching hospital in Richmond associated with Virginia Commonwealth University, said Anthem owes it $385 million. More than 40% of the claims are more than 90 days old, VCU said.
For all Virginia hospitals, Anthem’s late, unpaid claims amount to “hundreds of millions of dollars,” the Virginia Hospital and Healthcare Association said in a June 23 letter to state regulators.
Nationwide, the payment delays “are creating an untenable situation,” the American Hospital Association said in a Sept. 9 letter to Anthem CEO Gail Boudreaux. “Patients are facing greater hurdles to accessing care; clinicians are burning out on unnecessary administrative tasks; and the system is straining to finance the personnel and supplies” needed to fight Covid.
Complaints about Anthem extend “from sea to shining sea, from New Hampshire to California,” AHA CEO Rick Pollack told KHN.
Substantial payment delays can be seen on Anthem’s books. On June 30, 2019, before the pandemic, 43% of the insurer’s medical bills for that quarter were unpaid, according to regulatory filings. Two years later that figure had risen to 53% – a difference of $2.5 billion.
Anthem profits were $4.6 billion in 2020 and $3.5 billion in the first half of 2021.
Alexis Thurber, who lives near Seattle, was insured by Anthem when she got an $18,192 hospital bill in May for radiation therapy that doctors said was essential to treat her breast cancer.
The treatments were “experimental” and “not medically necessary,” Anthem said, according to Ms. Thurber. She spent much of the summer trying to get the insurer to pay up – placing two dozen phone calls, spending hours on hold, sending multiple emails and enduring unmeasurable stress and worry. It finally covered the claim months later.
“It’s so egregious. It’s a game they’re playing,” said Ms. Thurber, 51, whose cancer was diagnosed in November. “Trying to get true help was impossible.”
Privacy rules prevent Anthem from commenting on Ms. Thurber’s case, said Anthem spokesperson Colin Manning.
When insurers fail to promptly pay medical bills, patients are left in the lurch. They might first get a notice saying payment is pending or denied. A hospital might bill them for treatment they thought would be covered. Hospitals and doctors often sue patients whose insurance didn’t pay up.
Hospitals point to a variety of Anthem practices contributing to payment delays or denials, including new layers of document requirements, prior-authorization hurdles for routine procedures and requirements that doctors themselves – not support staffers – speak to insurance gatekeepers. “This requires providers to literally leave the patient[’s] bedside to get on the phone with Anthem,” AHA said in its letter.
Anthem often hinders coverage for outpatient surgery, specialty pharmacy and other services in health systems listed as in network, amounting to a “bait and switch” on Anthem members, AHA officials said.
“Demanding that patients be treated outside of the hospital setting, against the advice of the patient’s in-network treating physician, appears to be motivated by a desire to drive up Empire’s profits,” the Greater New York Hospital Association wrote in an April letter to Empire Blue Cross, which is owned by Anthem.
Anthem officials pushed back in a recent letter to the AHA, saying the insurer’s changing rules are intended partly to control excessive prices charged by hospitals for specialty drugs and nonemergency surgery, screening and diagnostic procedures.
Severe problems with Anthem’s new claims management system surfaced months ago and “persist without meaningful improvement,” AHA said in its letter.
Claims have gotten lost in Anthem’s computers, and in some cases VCU Health has had to print medical records and mail them to get paid, VCU said in its letter. The cash slowdown imposes “an unmanageable disruption that threatens to undermine our financial footing,” VCU said.
United denied $31,557 in claims for Emily Long’s care after she was struck in June by a motorcycle in New York City. She needed surgery to repair a fractured cheekbone. United said there was a lack of documentation for “medical necessity” – an “incredibly aggravating” response on top of the distress of the accident, Ms. Long said.
The Brooklyn hospital that treated Ms. Long was “paid appropriately under her plan and within the required time frame,” said United spokesperson Maria Gordon Shydlo. “The facility has the right to appeal the decision.”
United’s unpaid claims came to 54% as of June 30, about the same level as 2 years previously.
When Erin Conlisk initially had trouble gaining approval for a piece of medical equipment for her elderly father this summer, United employees told her the insurer’s entire prior-authorization database had gone down for weeks, said Ms. Conlisk, who lives in California.
“There was a brief issue with our prior-authorization process in mid-July, which was resolved quickly,” Gordon Shydlo said.
When asked by Wall Street analysts about the payment backups, Anthem executives said it partly reflects their decision to increase financial reserves amid the health crisis.
“Really a ton of uncertainty associated with this environment,” John Gallina, the company’s chief financial officer, said on a conference call in July. “We’ve tried to be extremely prudent and conservative in our approach.”
During the pandemic, hospitals have benefited from two extraordinary cash infusions. They and other medical providers have received more than $100 billion through the CARES Act of 2020 and the American Rescue Plan of 2021. Last year United, Anthem and other insurers accelerated billions in hospital reimbursements.
The federal payments enriched many of the biggest, wealthiest systems while poorer hospitals serving low-income patients and rural areas struggled.
Those are the systems most hurt now by insurer payment delays, hospital officials said. Federal relief funds “have been a lifeline, but they don’t make people whole in terms of the losses from increased expenses and lost revenue as a result of the COVID experience,” Mr. Pollack said.
Several health systems declined to comment about claims payment delays or didn’t respond to a reporter’s queries. Among individual hospitals “there is a deep fear of talking on the record about your largest business partner,” AHA’s Ms. Smith said.
Alexis Thurber worried she might have to pay her $18,192 radiation bill herself, and she’s not confident her Anthem policy will do a better job next time of covering the cost of her care.
“It makes me not want to go to the doctor anymore,” she said. “I’m scared to get another mammogram because you can’t rely on it.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Anthem Blue Cross, the country’s second-biggest health insurance company, is behind on billions of dollars in payments owed to hospitals and doctors because of onerous new reimbursement rules, computer problems and mishandled claims, say hospital officials in multiple states.
Anthem, like other big insurers, is using the COVID-19 crisis as cover to institute “egregious” policies that harm patients and pinch hospital finances, said Molly Smith, group vice president at the American Hospital Association. “There’s this sense of ‘Everyone’s distracted. We can get this through.’ ”
Hospitals are also dealing with a spike in retroactive claims denials by UnitedHealthcare, the biggest health insurer, for ED care, the AHA said.
Hospitals say it is hurting their finances as many cope with COVID surges – even after the industry has received tens of billions of dollars in emergency assistance from the federal government.
“We recognize there have been some challenges” to prompt payments caused by claims-processing changes and “a new set of dynamics” amid the pandemic, Anthem spokesperson Colin Manning said in an email. “We apologize for any delays or inconvenience this may have caused.”
Virginia law requires insurers to pay claims within 40 days. In a Sept. 24 letter to state insurance regulators, VCU Health, a system that operates a large teaching hospital in Richmond associated with Virginia Commonwealth University, said Anthem owes it $385 million. More than 40% of the claims are more than 90 days old, VCU said.
For all Virginia hospitals, Anthem’s late, unpaid claims amount to “hundreds of millions of dollars,” the Virginia Hospital and Healthcare Association said in a June 23 letter to state regulators.
Nationwide, the payment delays “are creating an untenable situation,” the American Hospital Association said in a Sept. 9 letter to Anthem CEO Gail Boudreaux. “Patients are facing greater hurdles to accessing care; clinicians are burning out on unnecessary administrative tasks; and the system is straining to finance the personnel and supplies” needed to fight Covid.
Complaints about Anthem extend “from sea to shining sea, from New Hampshire to California,” AHA CEO Rick Pollack told KHN.
Substantial payment delays can be seen on Anthem’s books. On June 30, 2019, before the pandemic, 43% of the insurer’s medical bills for that quarter were unpaid, according to regulatory filings. Two years later that figure had risen to 53% – a difference of $2.5 billion.
Anthem profits were $4.6 billion in 2020 and $3.5 billion in the first half of 2021.
Alexis Thurber, who lives near Seattle, was insured by Anthem when she got an $18,192 hospital bill in May for radiation therapy that doctors said was essential to treat her breast cancer.
The treatments were “experimental” and “not medically necessary,” Anthem said, according to Ms. Thurber. She spent much of the summer trying to get the insurer to pay up – placing two dozen phone calls, spending hours on hold, sending multiple emails and enduring unmeasurable stress and worry. It finally covered the claim months later.
“It’s so egregious. It’s a game they’re playing,” said Ms. Thurber, 51, whose cancer was diagnosed in November. “Trying to get true help was impossible.”
Privacy rules prevent Anthem from commenting on Ms. Thurber’s case, said Anthem spokesperson Colin Manning.
When insurers fail to promptly pay medical bills, patients are left in the lurch. They might first get a notice saying payment is pending or denied. A hospital might bill them for treatment they thought would be covered. Hospitals and doctors often sue patients whose insurance didn’t pay up.
Hospitals point to a variety of Anthem practices contributing to payment delays or denials, including new layers of document requirements, prior-authorization hurdles for routine procedures and requirements that doctors themselves – not support staffers – speak to insurance gatekeepers. “This requires providers to literally leave the patient[’s] bedside to get on the phone with Anthem,” AHA said in its letter.
Anthem often hinders coverage for outpatient surgery, specialty pharmacy and other services in health systems listed as in network, amounting to a “bait and switch” on Anthem members, AHA officials said.
“Demanding that patients be treated outside of the hospital setting, against the advice of the patient’s in-network treating physician, appears to be motivated by a desire to drive up Empire’s profits,” the Greater New York Hospital Association wrote in an April letter to Empire Blue Cross, which is owned by Anthem.
Anthem officials pushed back in a recent letter to the AHA, saying the insurer’s changing rules are intended partly to control excessive prices charged by hospitals for specialty drugs and nonemergency surgery, screening and diagnostic procedures.
Severe problems with Anthem’s new claims management system surfaced months ago and “persist without meaningful improvement,” AHA said in its letter.
Claims have gotten lost in Anthem’s computers, and in some cases VCU Health has had to print medical records and mail them to get paid, VCU said in its letter. The cash slowdown imposes “an unmanageable disruption that threatens to undermine our financial footing,” VCU said.
United denied $31,557 in claims for Emily Long’s care after she was struck in June by a motorcycle in New York City. She needed surgery to repair a fractured cheekbone. United said there was a lack of documentation for “medical necessity” – an “incredibly aggravating” response on top of the distress of the accident, Ms. Long said.
The Brooklyn hospital that treated Ms. Long was “paid appropriately under her plan and within the required time frame,” said United spokesperson Maria Gordon Shydlo. “The facility has the right to appeal the decision.”
United’s unpaid claims came to 54% as of June 30, about the same level as 2 years previously.
When Erin Conlisk initially had trouble gaining approval for a piece of medical equipment for her elderly father this summer, United employees told her the insurer’s entire prior-authorization database had gone down for weeks, said Ms. Conlisk, who lives in California.
“There was a brief issue with our prior-authorization process in mid-July, which was resolved quickly,” Gordon Shydlo said.
When asked by Wall Street analysts about the payment backups, Anthem executives said it partly reflects their decision to increase financial reserves amid the health crisis.
“Really a ton of uncertainty associated with this environment,” John Gallina, the company’s chief financial officer, said on a conference call in July. “We’ve tried to be extremely prudent and conservative in our approach.”
During the pandemic, hospitals have benefited from two extraordinary cash infusions. They and other medical providers have received more than $100 billion through the CARES Act of 2020 and the American Rescue Plan of 2021. Last year United, Anthem and other insurers accelerated billions in hospital reimbursements.
The federal payments enriched many of the biggest, wealthiest systems while poorer hospitals serving low-income patients and rural areas struggled.
Those are the systems most hurt now by insurer payment delays, hospital officials said. Federal relief funds “have been a lifeline, but they don’t make people whole in terms of the losses from increased expenses and lost revenue as a result of the COVID experience,” Mr. Pollack said.
Several health systems declined to comment about claims payment delays or didn’t respond to a reporter’s queries. Among individual hospitals “there is a deep fear of talking on the record about your largest business partner,” AHA’s Ms. Smith said.
Alexis Thurber worried she might have to pay her $18,192 radiation bill herself, and she’s not confident her Anthem policy will do a better job next time of covering the cost of her care.
“It makes me not want to go to the doctor anymore,” she said. “I’m scared to get another mammogram because you can’t rely on it.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Two Colorado nurses admit to stealing drugs from hospital patients
, according to the US Attorney’s Office in Denver.
Alicia Nickel-Tangeman, 44, formerly of Woodland Park, Colo., pled guilty to four counts of obtaining controlled substances using fraud and deception. She gained access to rooms of patients who weren’t assigned to her and diverted drugs from their pain-on-demand devices, according to federal officials.
The defendant told patients she was conducting a study on the pumps that deliver drugs to relieve pain when the patient pushes a button, the officials stated. She would open the machine and would remove a portion of the drug with a syringe. She obtained drugs in this way from three patients on four occasions, a press release stated.
When questioned by law enforcement, Ms. Nickel-Tangeman continued to lie about her conduct and produced a false email address to substantiate her claims, the Department of Justice reported. She is scheduled to be sentenced November 30.
Ms. Nickel-Tangeman’s LinkedIn profile shows that she was a nurse with UCHealth in Colorado for 17 years, ending in May 2019.
Katie Muhs, 34, of Littleton, Colo., was convicted of a felony for using fraud and deception to divert fentanyl for her personal use while serving as an intensive care nurse.
The defendant admitted that between June and September 2019 she stole fentanyl by removing it from the IV bags of patients using a syringe. She also admitted to stealing fentanyl that remained in vials after fentanyl had been administered to patients. She would replace the stolen drug with saline and would “then have a fellow nurse witness her ‘waste,’ or dispose of the saline.”
U.S. District Judge Raymond Moore sentenced Ms. Muhs to 3 months of probation as a result of “the defendant’s confession and her cooperation in disclosing full information on her diversion, which is a matter potentially affecting the public health and the integrity of the health care system. The felony offense is punishable by up to four years of imprisonment and a fine of $250,000, per count.”
In pleading guilty to the single count in the case, Ms. Muhs admitted that on September 8, 2019, “she removed a bag of fentanyl from the automated medication control machine at the hospital under a different nurse’s login credentials. She then removed fentanyl from the IV bag for personal use.”
In April, the Colorado Court of Appeals denied her request for unemployment benefits. Court documents reveal that Ms. Muhs lost her job at St. Anthony Hospital after it was discovered that she stole and self-injected fentanyl while working as a registered nurse there.
The investigations in these cases were conducted by the U.S. Food and Drug Administration, the Office of Criminal Investigations, and the Drug Enforcement Administration (DEA).
“We want it to be known that healthcare professionals who take advantage of patients in need by stealing their medications will be held accountable to the law,” said Deanne Reuter, DEA Denver Field Division special agent in charge.
A version of this article first appeared on Medscape.com.
, according to the US Attorney’s Office in Denver.
Alicia Nickel-Tangeman, 44, formerly of Woodland Park, Colo., pled guilty to four counts of obtaining controlled substances using fraud and deception. She gained access to rooms of patients who weren’t assigned to her and diverted drugs from their pain-on-demand devices, according to federal officials.
The defendant told patients she was conducting a study on the pumps that deliver drugs to relieve pain when the patient pushes a button, the officials stated. She would open the machine and would remove a portion of the drug with a syringe. She obtained drugs in this way from three patients on four occasions, a press release stated.
When questioned by law enforcement, Ms. Nickel-Tangeman continued to lie about her conduct and produced a false email address to substantiate her claims, the Department of Justice reported. She is scheduled to be sentenced November 30.
Ms. Nickel-Tangeman’s LinkedIn profile shows that she was a nurse with UCHealth in Colorado for 17 years, ending in May 2019.
Katie Muhs, 34, of Littleton, Colo., was convicted of a felony for using fraud and deception to divert fentanyl for her personal use while serving as an intensive care nurse.
The defendant admitted that between June and September 2019 she stole fentanyl by removing it from the IV bags of patients using a syringe. She also admitted to stealing fentanyl that remained in vials after fentanyl had been administered to patients. She would replace the stolen drug with saline and would “then have a fellow nurse witness her ‘waste,’ or dispose of the saline.”
U.S. District Judge Raymond Moore sentenced Ms. Muhs to 3 months of probation as a result of “the defendant’s confession and her cooperation in disclosing full information on her diversion, which is a matter potentially affecting the public health and the integrity of the health care system. The felony offense is punishable by up to four years of imprisonment and a fine of $250,000, per count.”
In pleading guilty to the single count in the case, Ms. Muhs admitted that on September 8, 2019, “she removed a bag of fentanyl from the automated medication control machine at the hospital under a different nurse’s login credentials. She then removed fentanyl from the IV bag for personal use.”
In April, the Colorado Court of Appeals denied her request for unemployment benefits. Court documents reveal that Ms. Muhs lost her job at St. Anthony Hospital after it was discovered that she stole and self-injected fentanyl while working as a registered nurse there.
The investigations in these cases were conducted by the U.S. Food and Drug Administration, the Office of Criminal Investigations, and the Drug Enforcement Administration (DEA).
“We want it to be known that healthcare professionals who take advantage of patients in need by stealing their medications will be held accountable to the law,” said Deanne Reuter, DEA Denver Field Division special agent in charge.
A version of this article first appeared on Medscape.com.
, according to the US Attorney’s Office in Denver.
Alicia Nickel-Tangeman, 44, formerly of Woodland Park, Colo., pled guilty to four counts of obtaining controlled substances using fraud and deception. She gained access to rooms of patients who weren’t assigned to her and diverted drugs from their pain-on-demand devices, according to federal officials.
The defendant told patients she was conducting a study on the pumps that deliver drugs to relieve pain when the patient pushes a button, the officials stated. She would open the machine and would remove a portion of the drug with a syringe. She obtained drugs in this way from three patients on four occasions, a press release stated.
When questioned by law enforcement, Ms. Nickel-Tangeman continued to lie about her conduct and produced a false email address to substantiate her claims, the Department of Justice reported. She is scheduled to be sentenced November 30.
Ms. Nickel-Tangeman’s LinkedIn profile shows that she was a nurse with UCHealth in Colorado for 17 years, ending in May 2019.
Katie Muhs, 34, of Littleton, Colo., was convicted of a felony for using fraud and deception to divert fentanyl for her personal use while serving as an intensive care nurse.
The defendant admitted that between June and September 2019 she stole fentanyl by removing it from the IV bags of patients using a syringe. She also admitted to stealing fentanyl that remained in vials after fentanyl had been administered to patients. She would replace the stolen drug with saline and would “then have a fellow nurse witness her ‘waste,’ or dispose of the saline.”
U.S. District Judge Raymond Moore sentenced Ms. Muhs to 3 months of probation as a result of “the defendant’s confession and her cooperation in disclosing full information on her diversion, which is a matter potentially affecting the public health and the integrity of the health care system. The felony offense is punishable by up to four years of imprisonment and a fine of $250,000, per count.”
In pleading guilty to the single count in the case, Ms. Muhs admitted that on September 8, 2019, “she removed a bag of fentanyl from the automated medication control machine at the hospital under a different nurse’s login credentials. She then removed fentanyl from the IV bag for personal use.”
In April, the Colorado Court of Appeals denied her request for unemployment benefits. Court documents reveal that Ms. Muhs lost her job at St. Anthony Hospital after it was discovered that she stole and self-injected fentanyl while working as a registered nurse there.
The investigations in these cases were conducted by the U.S. Food and Drug Administration, the Office of Criminal Investigations, and the Drug Enforcement Administration (DEA).
“We want it to be known that healthcare professionals who take advantage of patients in need by stealing their medications will be held accountable to the law,” said Deanne Reuter, DEA Denver Field Division special agent in charge.
A version of this article first appeared on Medscape.com.
Telehealth models of care for pediatric hospital medicine
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
Mean leadership
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
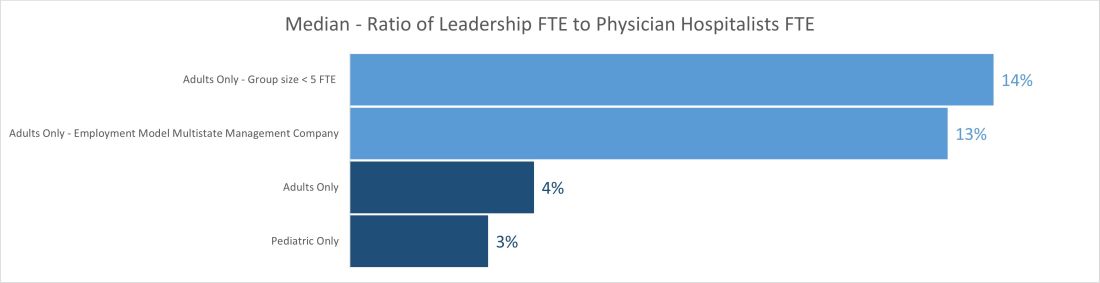
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
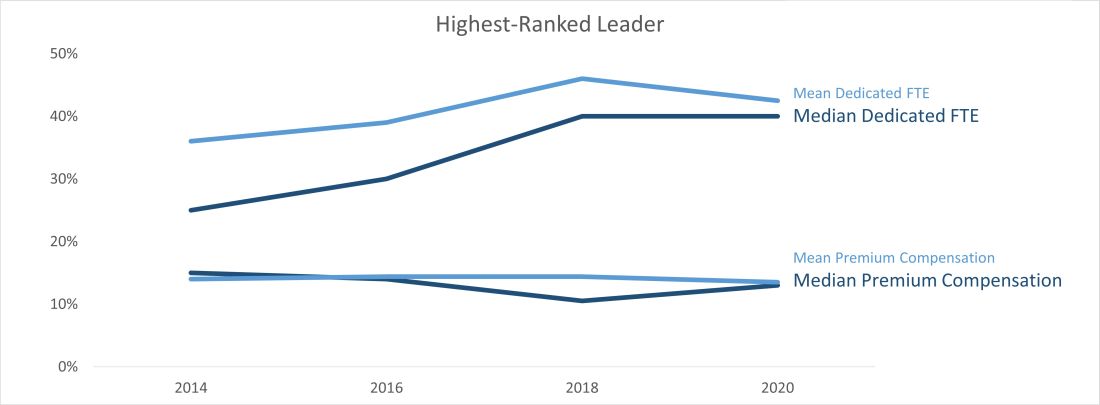
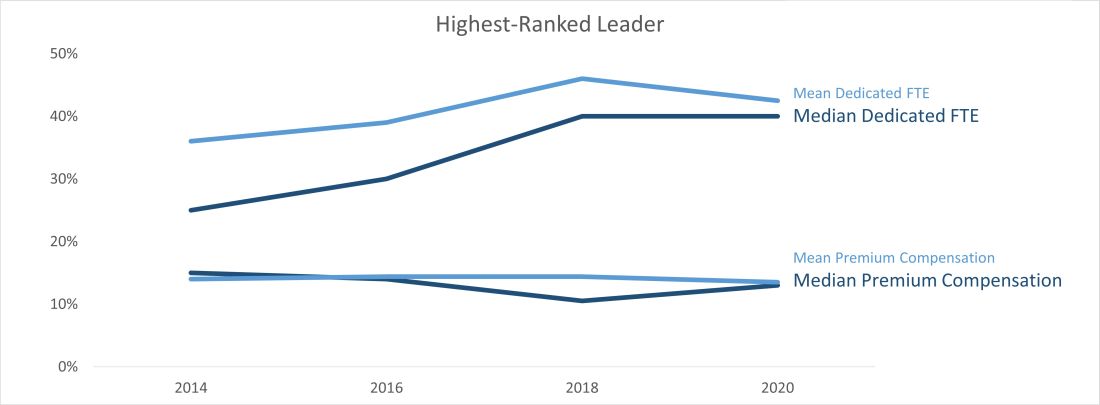
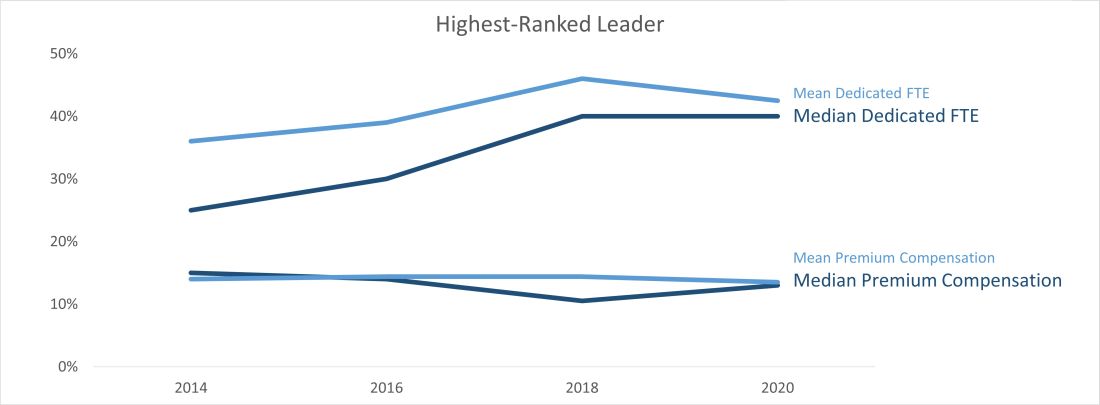
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
The differences between the mean and median of leadership data
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
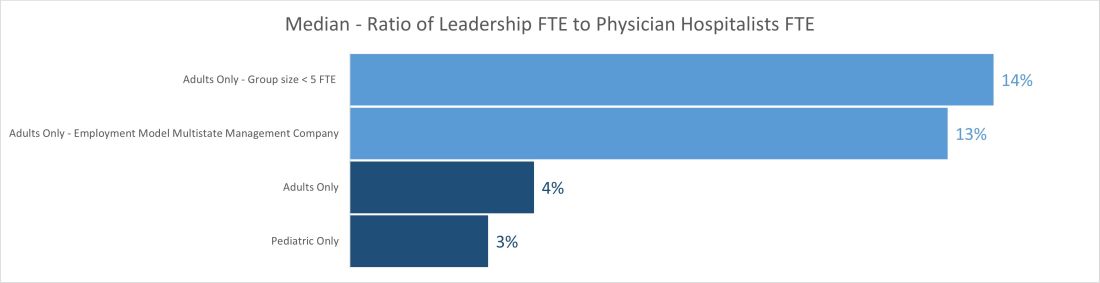
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
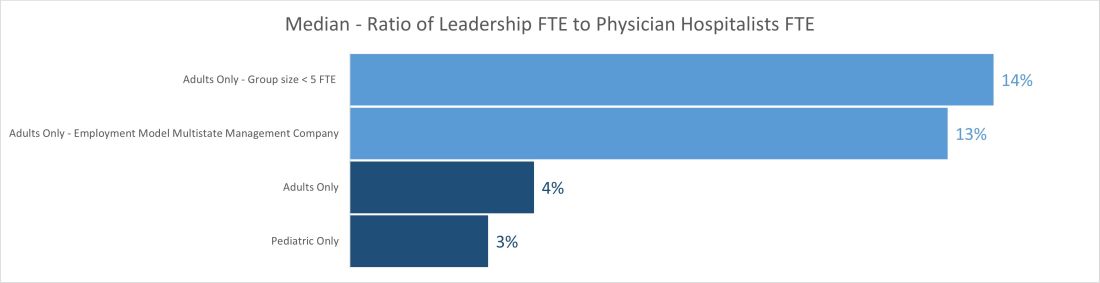
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Nurses ‘at the breaking point,’ consider quitting due to COVID issues: Survey
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 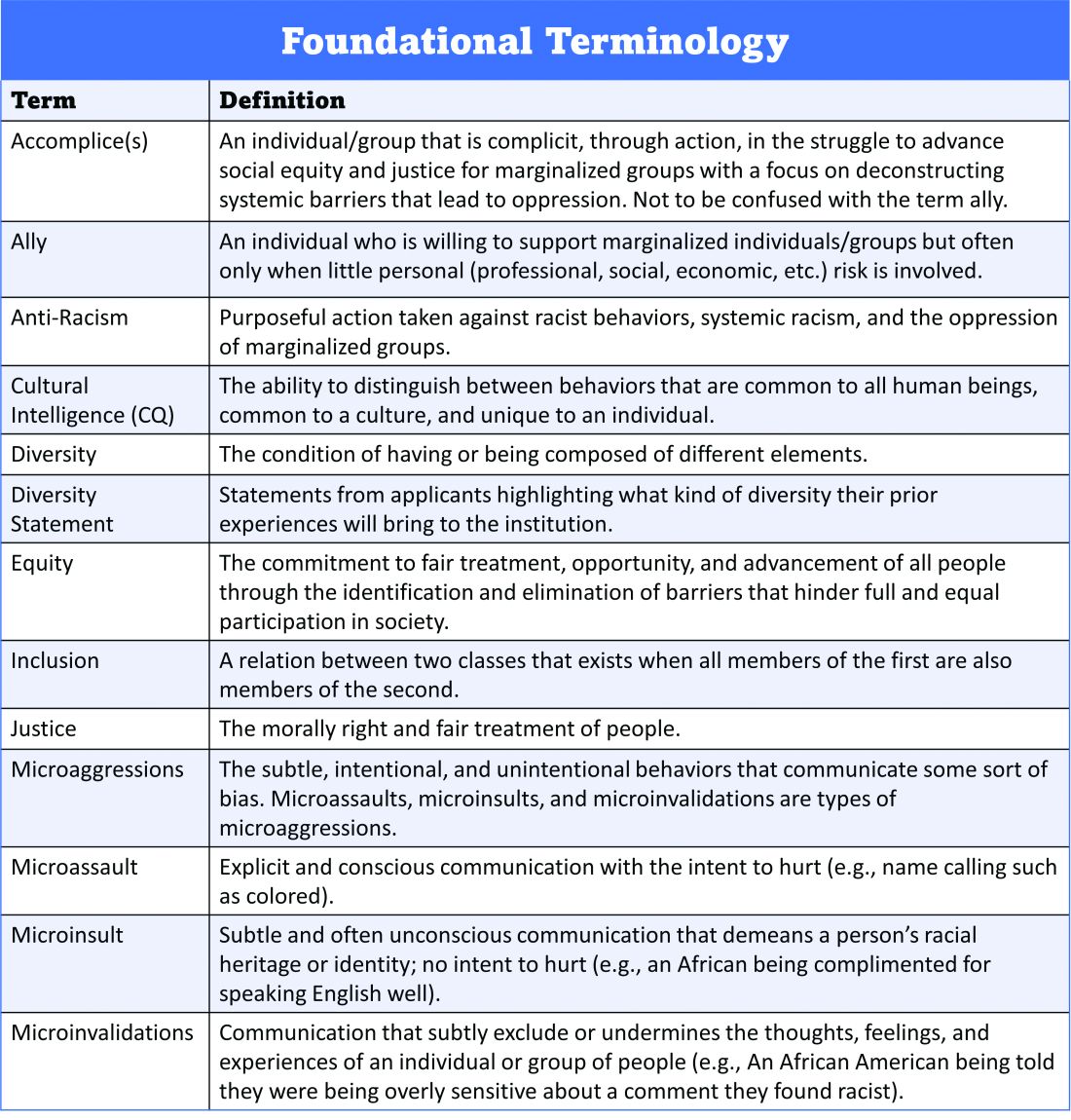
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 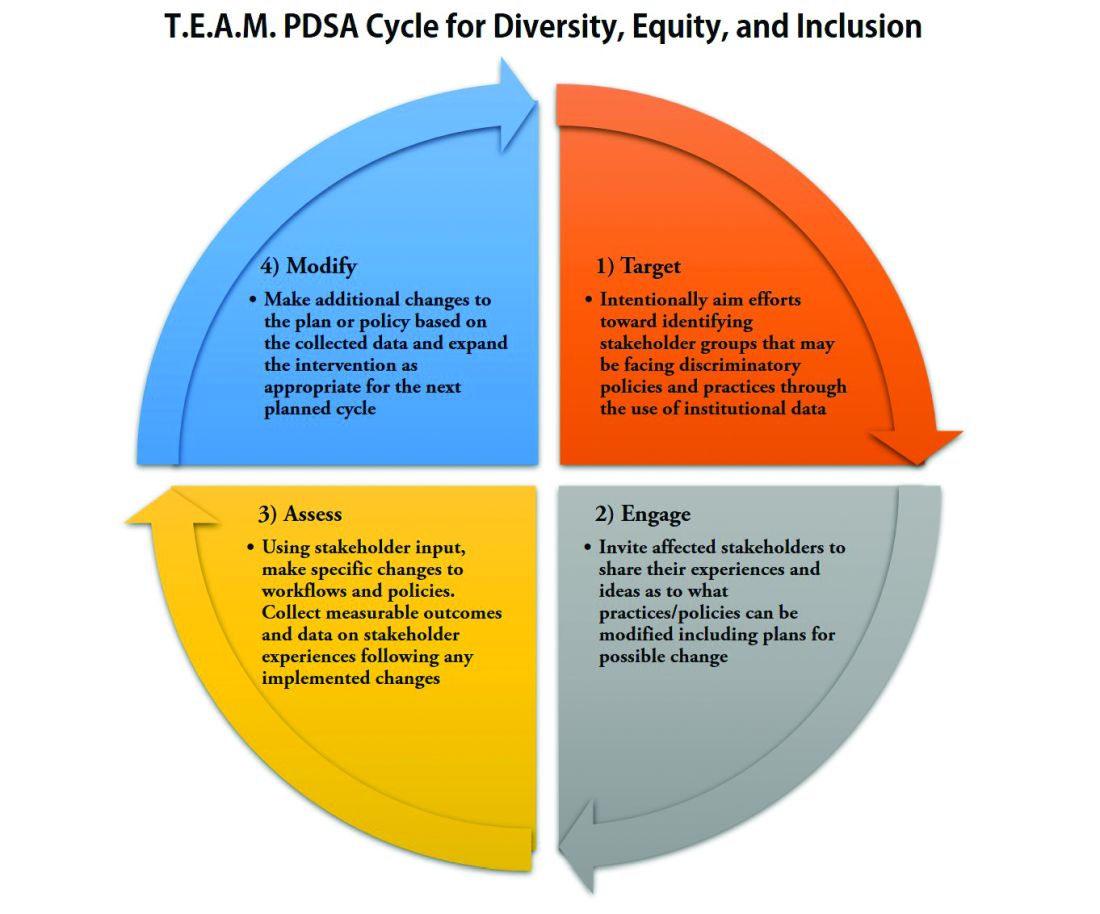
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 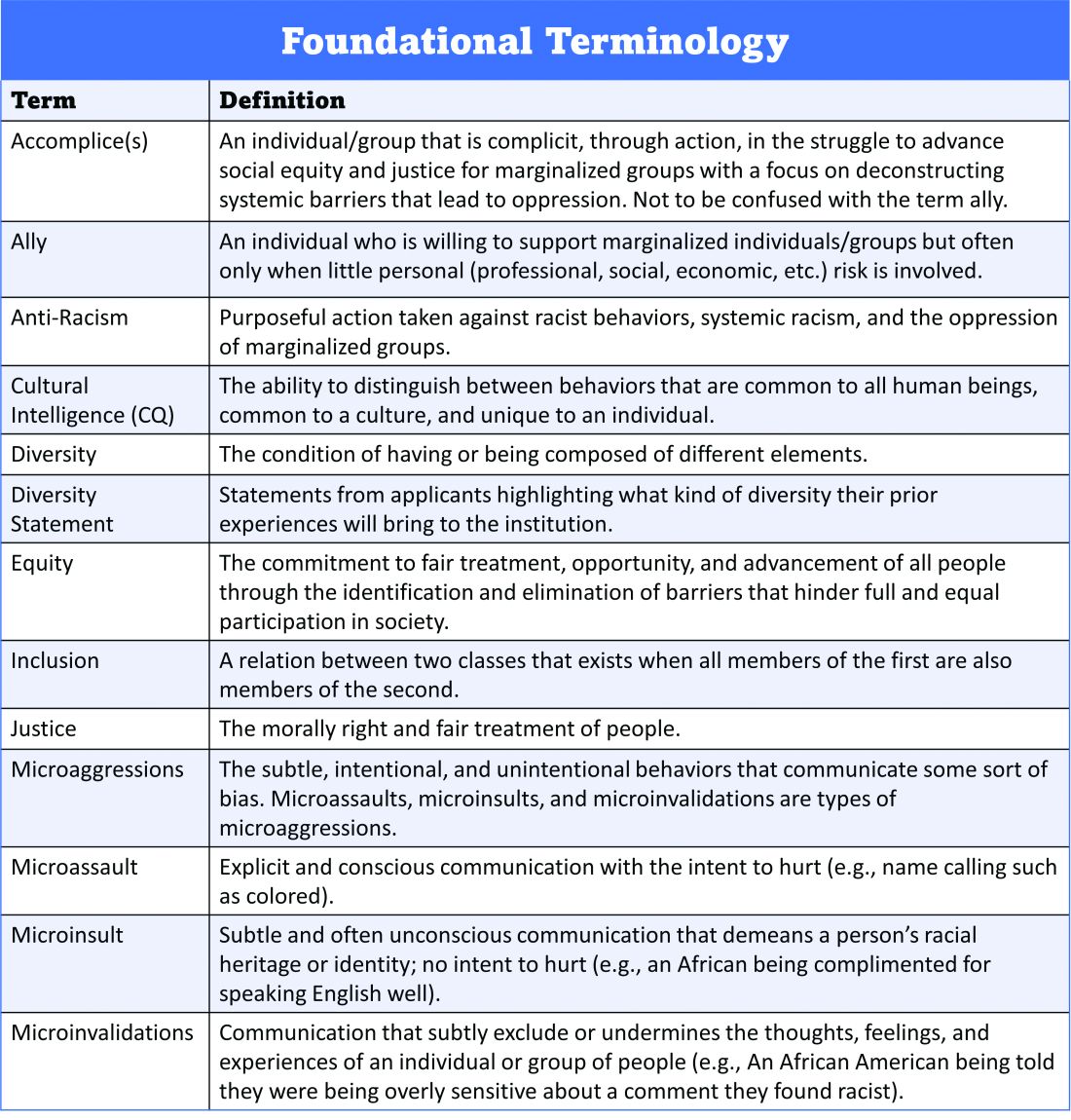
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 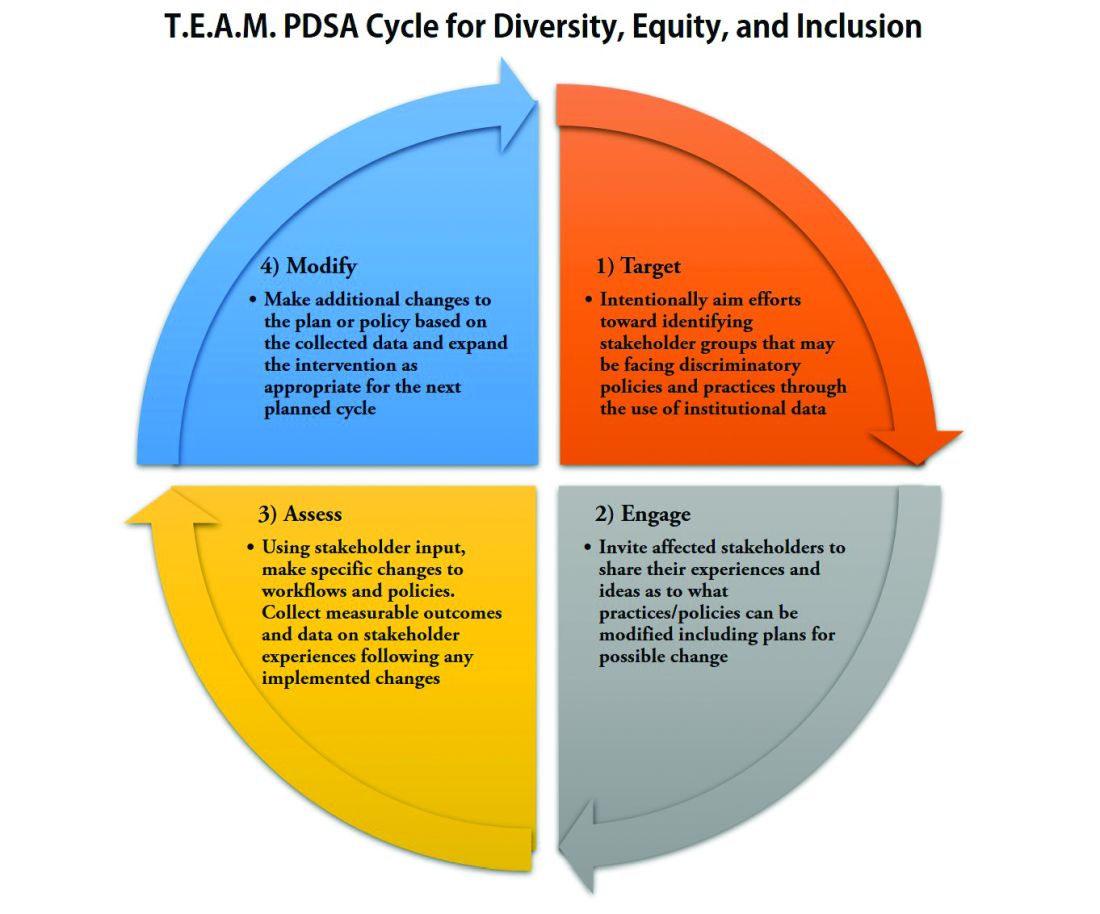
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 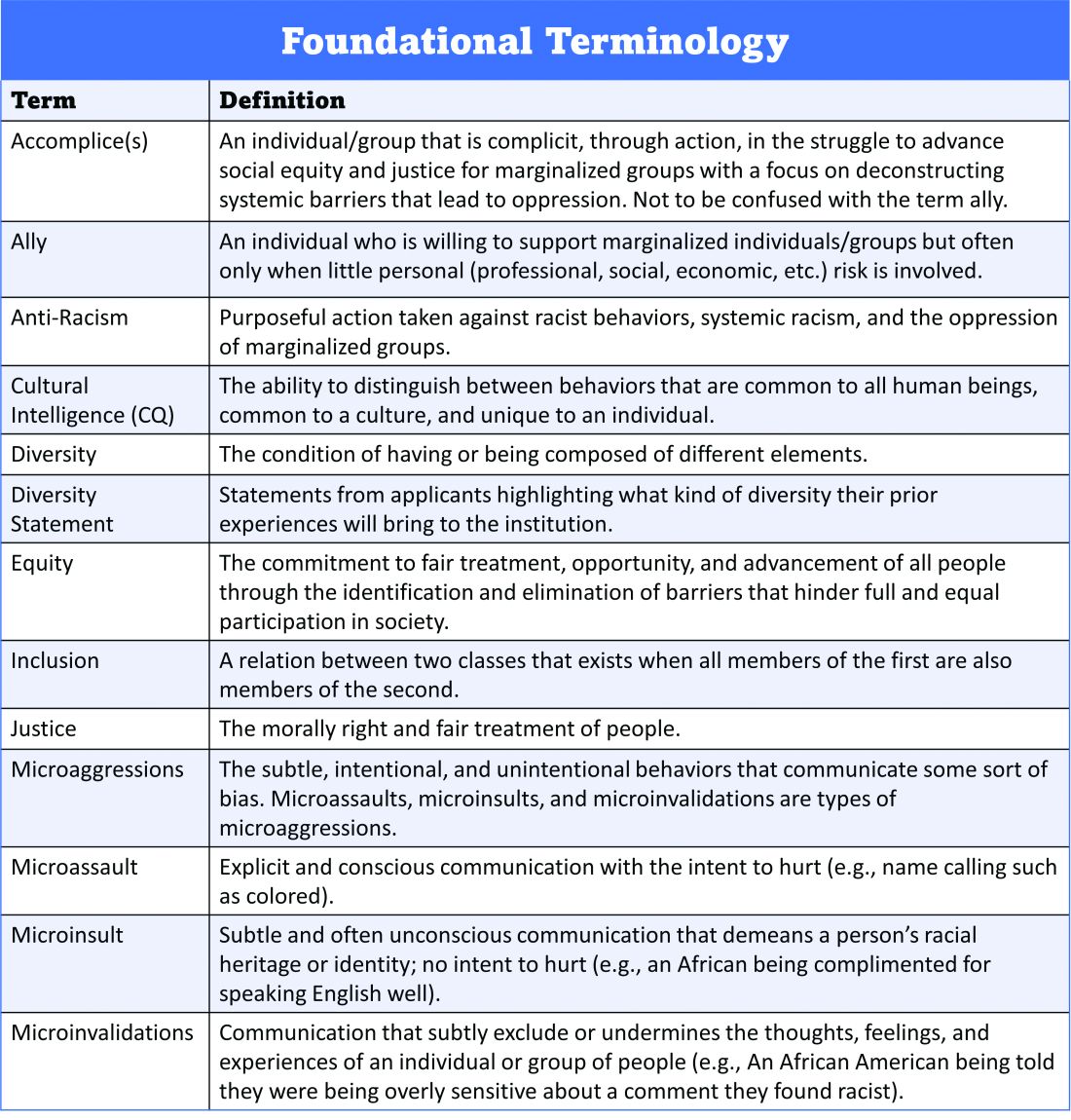
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 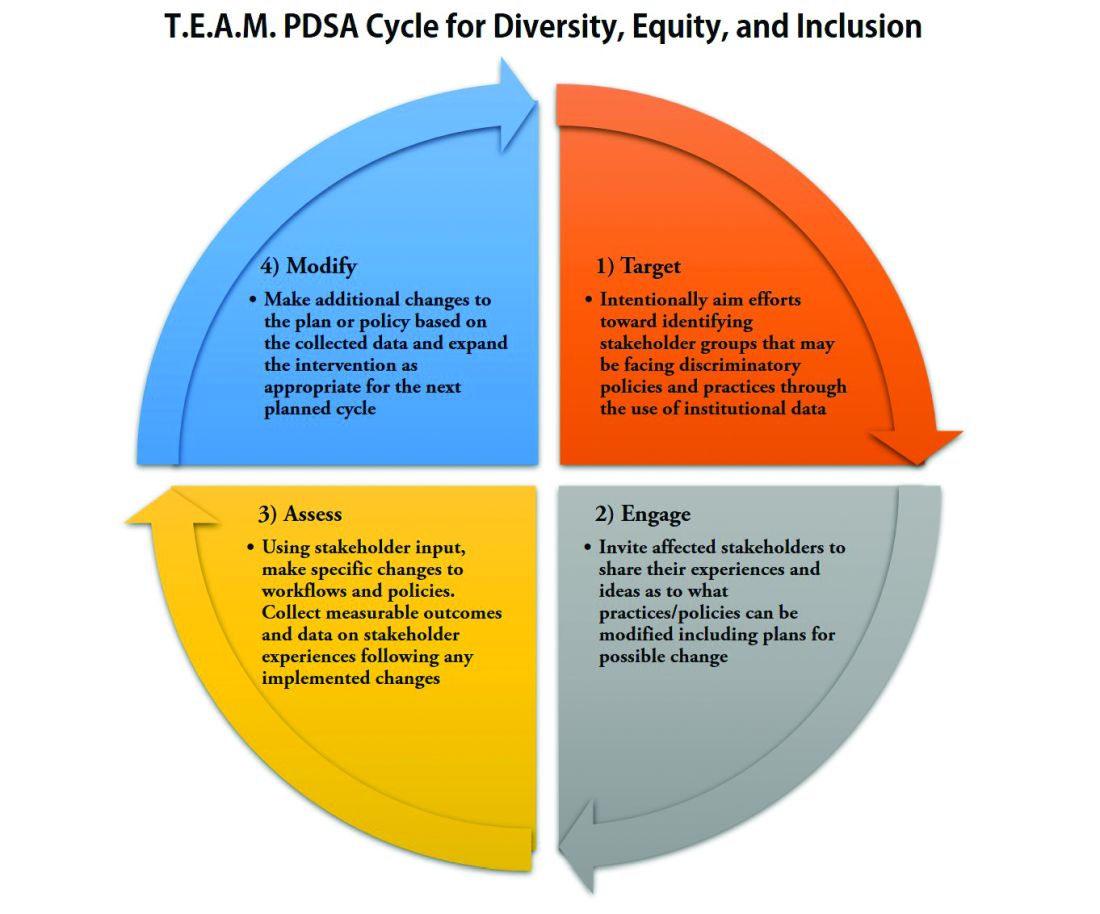
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Baylor gets restraining order against COVID-19 vaccine–skeptic doc
in which he agreed to stop mentioning his prior leadership and academic appointments.
Baylor was the first institution to cut ties with Dr. McCullough, who has promoted the use of therapies seen as unproven for the treatment of COVID-19 and has questioned the effectiveness of COVID-19 vaccines. Since the Baylor suit, the Texas A&M College of Medicine, and the Texas Christian University (TCU) and University of North Texas Health Science Center (UNTHSC) School of Medicine have both removed Dr. McCullough from their faculties.
Granted by the 191st District Court in Dallas County, Tex., the Baylor restraining order – which is in effect at least until a hearing on the case on September 30 – was sought as part of Baylor Scott & White’s breach of contract suit against McCullough, who had previously been known as a well-respected expert in cardiorenal issues. The suit is seeking $1 million in damages, as well as attorneys’ fees.
The suit seeks to “enforce the terms” of the confidential employment separation agreement signed by Dr. McCullough in February and prevent Dr. McCullough from continuing “improper use of titles and claimed affiliations that have already confused the media, the medical community and the public,” it reads.
“This ongoing confusion regarding [Dr.] McCullough’s affiliations, and whether Plaintiffs support his opinions, is exactly what Plaintiffs bargained to avoid in the Separation Agreement,” and is likely to cause “irreparable reputational and business harm that is incapable of remedy by money damages alone,” the suit states.
One of Dr. McCullough’s attorneys, Clinton Mikel, maintains that all the times the physician was identified in the “thousands of hours of media interviews and countless publications since his departure from Baylor” were “said/printed by a third party with no encouragement from Dr. McCullough,” and that the doctor “does not and cannot control third parties.”
Mr. Mikel said in a statement emailed to this news organization by Dr. McCullough that the suit is “a politically motivated attempt to silence Dr. McCullough,” because it was filed on the same day the organization mandated COVID-19 vaccination for employees.
Dr. McCullough “intends to vigorously defend against Baylor’s unfounded lawsuit,” will seek to dissolve the restraining order, and recover “all payments due him from Baylor under the terms of the settlement agreement,” wrote Mr. Mikel.
The cardiologist’s legal team filed a motion to dismiss the suit on Aug. 9, essentially arguing that Baylor Scott & White’s action restricted Dr. McCullough’s right to free speech under the Texas Citizen’s Participation Act.
COVID-19 vaccines = bioterrorism?
Dr. McCullough accumulated a following in 2020 by promoting early at-home multidrug treatment of COVID-19 in interviews with conservative websites and at a U.S. Senate hearing in November.
Although Dr. McCullough does not appear to have any personal social media accounts, his broadcast and podcast interviews are tweeted by thousands daily around the world and featured on Facebook pages like “Pandemic Debate.”
Some Facebook posts with Dr. McCullough’s pronouncements have been labeled as misinformation or removed. Some of his videos remain on YouTube, where they are posted by the Association of American Physicians and Surgeons, a group that believes Dr. McCullough is “under fierce attack for speaking out about COVID-19 early treatment and vaccine safety.”
Dr. McCullough’s March 2021 testimony to the Texas Senate’s Health and Human Services Committee – in which he claimed that COVID-19 patients are being denied what he called proven treatments like hydroxychloroquine – has been viewed more than 3.7 million times on YouTube. The appearance has also been tweeted repeatedly.
Most of Dr. McCullough’s interviews and presentations are aggregated on Rumble, an alternative to YouTube.
In interviews, Dr. McCullough promotes the use of zinc, hydroxychloroquine, azithromycin, doxycycline, favipiravir, prednisone, and ivermectin as COVID-19 treatments – based on an outpatient treatment algorithm published in August 2020 in the American Journal of Medicine. The cardiologist was the lead author of that paper, which proposed treating people with COVID-like symptoms whether or not they had confirmed infection.
Dr. McCullough and colleagues published a follow-up paper that added colchicine to the mix in Reviews in Cardiovascular Medicine. Dr. McCullough is editor-in-chief of the journal, but this was not noted in the disclosures.
Similarly, Dr. McCullough has not disclosed in his COVID-19 publications or any interviews that he has received consulting fees from a host of pharmaceutical manufacturers that produce COVID-19 drugs and vaccines, including AstraZeneca, Eli Lilly, and Regeneron Pharmaceuticals. According to the Centers for Medicare & Medicaid Services’ Open Payments database, Dr. McCullough was paid about $300,000 annually by drug companies from 2014 to 2019, mostly for consulting on cardiovascular and diabetes medications. His payments dropped to $169,406.06 in 2020.
Dr. McCullough appeared on “The Ingraham Angle” on Fox News in December 2020, claiming that sequential, early treatment with “anti-infectives, corticosteroids, and then antithrombotics” could “reduce [COVID-19] hospitalizations by 85% and cut mortality in half.”
He repeated the claim on the Ingraham show in July and agreed with host Laura Ingraham that the vast majority of healthy people would do fine if they got COVID. He also made the claim that 84% of the COVID-19 cases in Israel were in people who had been vaccinated. “So it’s clear, we can’t vaccinate our way out of this,” he said. An Associated Press “fact check” report has pushed back on similar assertions about vaccine data from Israel.
In a separate interview posted in June, Dr. McCullough called the pandemic the first phase of a bioterrorism event, which was “all about keeping the population in fear and in isolation and preparing them to accept the vaccine, which appears to be phase two of a bioterrorism operation.”
In addition, he said, “good doctors are doing unthinkable things like injecting biologically active messenger RNA that produces this pathogenic spike protein into pregnant women.”
According to the Centers for Disease Control and Prevention, the vaccines teach the body to produce the spike protein, which then triggers an immune response that creates antibodies that will attack the virus.
A PolitiFact review debunks the notion that the mRNA vaccines are toxic, cytotoxic, or introduce live, active virus proteins into the body.
FactCheck.org also disputed Dr. McCullough’s claim in a July 13 Ingraham Angle appearance that the mRNA vaccines are ineffective against the Delta variant.
In the FactCheck article, Frederic Bushman, codirector of the University of Pennsylvania’s Center for Research on Coronaviruses and Other Emerging Pathogens, said that people were much better off being vaccinated than not,” adding, “the Delta variant may reduce the effectiveness [of the vaccines] a little, but still, they’re so effective that you get a lot of benefit.”
“The vaccines are failing,” Dr. McCullough asserted in an Aug. 3 video interview posted on Odysee. “As we sit here today, we have 11,000 Americans that the CDC has certified have died after the vaccine,” he said, citing two analyses – one by Jessica Rose, PhD, and another by British researchers.
Similar figures reportedly based on cases reported to the Food and Drug Administration’s Vaccine Adverse Events Reporting System (VAERS) were forwarded to this news organization by Dr. McCullough.
The CDC website notes that the agency has received reports of 7,653 deaths in people who received a vaccine as of Sept. 13 (0.0020% of vaccine doses given since Dec. 14, 2020), but it cautions that those deaths do not mean the vaccine was the cause.
Dr. McCullough repeatedly claimed in the Aug. 3 interview that the government has not been transparent on vaccine safety. Since June 2020, the CDC’s Advisory Committee on Immunization Practices has held 16 public meetings on the COVID-19 vaccines.
To date, the agency has advised clinicians to monitor for rare side effects including Guillain-Barré syndrome and thrombosis with thrombocytopenia syndrome after the Johnson & Johnson vaccine and myocarditis after mRNA (Pfizer-BioNTech and Moderna) vaccines.
Med schools distance themselves
According to the Baylor Scott & White suit, Dr. McCullough agreed on Feb. 24 in a confidential separation agreement that he would no longer use his academic or leadership titles nor hold himself out to be affiliated with Baylor University Medical Center, Baylor Heart and Vascular Institute, the Baylor Research Institute, or any other related institutions.
However, as of August, according to a Baylor spokesperson, McCullough continued to have privileges at Baylor University Medical Center and Baylor Scott & White Heart and Vascular Hospital, Dallas.
The lawsuit points to three interviews posted in June and July where Dr. McCullough is identified as a “vice chief of medicine” or a “vice chief of internal medicine,” both at Baylor University. It also cites a profile at the Cardiometabolic Health Congress website – which this news organization had also viewed – that was still active in late July with a similar title. The profile was later scrubbed from the site.
Social media posts and other media continue to refer to Dr. McCullough’s Baylor credentials. An episode of the Faith and Freedom podcast posted on Aug. 2 identified McCullough as a “professor of medicine at Baylor University Medical Center.”
As of Sept. 16, Dr. McCullough’s bio page at his current practice, Heart Place, lists him as a professor of medicine at Texas A&M College of Medicine. A spokesperson for Texas A&M told this news organization that McCullough is no longer affiliated with the school.
Dr. McCullough acknowledged in the Aug. 3 interview that his Texas A&M title had been “stripped away” at “around the same time this lawsuit was filed.”
He was still a professor of medicine at the TCU and UNTHSC School of Medicine in Fort Worth, but a school spokesperson notified this news organization on Aug. 19 that Dr. McCullough was no longer with the school.
Dr. McCullough has portrayed himself as both a victim and a truth-teller, a “concerned physician” warning the world about the dangers of COVID-19 vaccines. The Baylor Scott & White lawsuit “is really a strong-armed tactic,” he said in the Aug. 3 interview. “I’m just a little guy, so I have to hire my legal teams, and in a sense be drained dry on legal fees,” he said.
But Dr. McCullough apparently has a plan for helping to defray his legal costs. In the Aug. 3 interview, he said a foundation he helped start, Truth for Health, has a “donation side to it,” adding “some of that may be used for legal expense.”
Cheryl Jones, an attorney with PK Law in Towson, Md., said that might draw interest from the Internal Revenue Service. “I would expect IRS scrutiny if contributions to the Medical Censorship Defense Fund are used to defend Dr McCullough in his personal breach of contract lawsuit,” she told this news organization.
The IRS generally recognizes defending “human and civil rights secured by law” as a legitimate charitable purpose for a legal defense fund, she said, adding that such a fund “must serve only public, rather than private, interests.”
Misinformation from a physician more damaging?
Some in the medical field have refuted Dr. McCullough’s pronouncements on how to treat COVID-19, including two infectious disease specialists with Monash University, Melbourne, who responded to the cardiologist’s original paper in the American Journal of Medicine.
Tony Korman, MBBS, a professor at the Centre for Inflammatory Diseases at Monash, told this news organization, “we had concerns that reputable medical journals would accept and publish papers proposing treatment of COVID-19 which was not supported by evidence.”
The website Healthfeedback.org has also challenged McCullough’s and his supporters’ claims, including that the American Journal of Medicine endorsed the use of hydroxychloroquine and that the COVID-19 vaccines have caused thousands of deaths.
David Broniatowski, PhD, associate director for the Institute for Data, Democracy and Politics at George Washington University, Washington, said in an interview that Dr. McCullough’s casting himself as a “rebel doctor” is a well-known trope in the vaccine misinformation universe.
Although he was not familiar with Dr. McCullough, Dr. Broniatowski said the cardiologist’s claims are not unique – they’ve been circulating among antivaccine and conspiracy-oriented groups for months.
For instance, Dr. McCullough has claimed in interviews that a whistleblower within the CDC knows of 50,000 vaccine-related deaths. Using data from the supposed whistleblower, the group America’s Frontline Doctors sued the federal government in July to stop the administration of COVID-19 vaccines to those under 18, people who have already had COVID, and individuals who the group said have not been adequately informed about the risks.
The idea of a whistleblower inside the CDC is recycled from antivaccine claims from decades ago, Dr. Broniatowski said.
But, he added, “somebody who speaks with the credibility of a major institution will be more likely to be listened to by some people.” That vulnerable group is “being taken advantage of by a relatively small number of disinformation purveyors, who, in some cases, profit from that disinformation,” said Dr. Broniatowski.
“We rely on our doctors because we trust them,” he said. “And we trust them because we believe that as physicians, their value system places the patient’s best interests first. That’s why it’s so much of a disappointment when you have a physician that appears to be exercising this sort of bad judgment.”
Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, also said that he was not familiar with Dr. McCullough. But apprised of his claims, Dr. Offit told this news organization, “Peter McCullough is a friend of the virus.”
“The kind of information he promotes allows the virus to continue to spread, continue to do an enormous amount of harm, and continue to mutate and create variants that have become more contagious and more resistant to vaccine-induced immunity,” said Dr. Offit, the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia.
Dr. Offit added that the war should be against SARS-CoV-2, but “because this virus has so many supporters, the war in essence becomes a war against ourselves, which is much harder.”
Dr. McCullough maintains he is doing a service to his patients. “I’m just giving and trying to help America understand the pandemic,” he told Ms. Ingraham on Fox News on July 29.
But he acknowledged concern about the Federation of State Medical Board’s announcement that physicians who spread COVID-19 vaccine misinformation risk suspension or revocation of their license.
“I have to tell you I’m worried – that no matter what I do and how careful I am to cite the scientific studies, I’m still gonna be hunted down for quote, misinformation,” he said in the Aug. 3 interview.
A version of this article first appeared on Medscape.com.
in which he agreed to stop mentioning his prior leadership and academic appointments.
Baylor was the first institution to cut ties with Dr. McCullough, who has promoted the use of therapies seen as unproven for the treatment of COVID-19 and has questioned the effectiveness of COVID-19 vaccines. Since the Baylor suit, the Texas A&M College of Medicine, and the Texas Christian University (TCU) and University of North Texas Health Science Center (UNTHSC) School of Medicine have both removed Dr. McCullough from their faculties.
Granted by the 191st District Court in Dallas County, Tex., the Baylor restraining order – which is in effect at least until a hearing on the case on September 30 – was sought as part of Baylor Scott & White’s breach of contract suit against McCullough, who had previously been known as a well-respected expert in cardiorenal issues. The suit is seeking $1 million in damages, as well as attorneys’ fees.
The suit seeks to “enforce the terms” of the confidential employment separation agreement signed by Dr. McCullough in February and prevent Dr. McCullough from continuing “improper use of titles and claimed affiliations that have already confused the media, the medical community and the public,” it reads.
“This ongoing confusion regarding [Dr.] McCullough’s affiliations, and whether Plaintiffs support his opinions, is exactly what Plaintiffs bargained to avoid in the Separation Agreement,” and is likely to cause “irreparable reputational and business harm that is incapable of remedy by money damages alone,” the suit states.
One of Dr. McCullough’s attorneys, Clinton Mikel, maintains that all the times the physician was identified in the “thousands of hours of media interviews and countless publications since his departure from Baylor” were “said/printed by a third party with no encouragement from Dr. McCullough,” and that the doctor “does not and cannot control third parties.”
Mr. Mikel said in a statement emailed to this news organization by Dr. McCullough that the suit is “a politically motivated attempt to silence Dr. McCullough,” because it was filed on the same day the organization mandated COVID-19 vaccination for employees.
Dr. McCullough “intends to vigorously defend against Baylor’s unfounded lawsuit,” will seek to dissolve the restraining order, and recover “all payments due him from Baylor under the terms of the settlement agreement,” wrote Mr. Mikel.
The cardiologist’s legal team filed a motion to dismiss the suit on Aug. 9, essentially arguing that Baylor Scott & White’s action restricted Dr. McCullough’s right to free speech under the Texas Citizen’s Participation Act.
COVID-19 vaccines = bioterrorism?
Dr. McCullough accumulated a following in 2020 by promoting early at-home multidrug treatment of COVID-19 in interviews with conservative websites and at a U.S. Senate hearing in November.
Although Dr. McCullough does not appear to have any personal social media accounts, his broadcast and podcast interviews are tweeted by thousands daily around the world and featured on Facebook pages like “Pandemic Debate.”
Some Facebook posts with Dr. McCullough’s pronouncements have been labeled as misinformation or removed. Some of his videos remain on YouTube, where they are posted by the Association of American Physicians and Surgeons, a group that believes Dr. McCullough is “under fierce attack for speaking out about COVID-19 early treatment and vaccine safety.”
Dr. McCullough’s March 2021 testimony to the Texas Senate’s Health and Human Services Committee – in which he claimed that COVID-19 patients are being denied what he called proven treatments like hydroxychloroquine – has been viewed more than 3.7 million times on YouTube. The appearance has also been tweeted repeatedly.
Most of Dr. McCullough’s interviews and presentations are aggregated on Rumble, an alternative to YouTube.
In interviews, Dr. McCullough promotes the use of zinc, hydroxychloroquine, azithromycin, doxycycline, favipiravir, prednisone, and ivermectin as COVID-19 treatments – based on an outpatient treatment algorithm published in August 2020 in the American Journal of Medicine. The cardiologist was the lead author of that paper, which proposed treating people with COVID-like symptoms whether or not they had confirmed infection.
Dr. McCullough and colleagues published a follow-up paper that added colchicine to the mix in Reviews in Cardiovascular Medicine. Dr. McCullough is editor-in-chief of the journal, but this was not noted in the disclosures.
Similarly, Dr. McCullough has not disclosed in his COVID-19 publications or any interviews that he has received consulting fees from a host of pharmaceutical manufacturers that produce COVID-19 drugs and vaccines, including AstraZeneca, Eli Lilly, and Regeneron Pharmaceuticals. According to the Centers for Medicare & Medicaid Services’ Open Payments database, Dr. McCullough was paid about $300,000 annually by drug companies from 2014 to 2019, mostly for consulting on cardiovascular and diabetes medications. His payments dropped to $169,406.06 in 2020.
Dr. McCullough appeared on “The Ingraham Angle” on Fox News in December 2020, claiming that sequential, early treatment with “anti-infectives, corticosteroids, and then antithrombotics” could “reduce [COVID-19] hospitalizations by 85% and cut mortality in half.”
He repeated the claim on the Ingraham show in July and agreed with host Laura Ingraham that the vast majority of healthy people would do fine if they got COVID. He also made the claim that 84% of the COVID-19 cases in Israel were in people who had been vaccinated. “So it’s clear, we can’t vaccinate our way out of this,” he said. An Associated Press “fact check” report has pushed back on similar assertions about vaccine data from Israel.
In a separate interview posted in June, Dr. McCullough called the pandemic the first phase of a bioterrorism event, which was “all about keeping the population in fear and in isolation and preparing them to accept the vaccine, which appears to be phase two of a bioterrorism operation.”
In addition, he said, “good doctors are doing unthinkable things like injecting biologically active messenger RNA that produces this pathogenic spike protein into pregnant women.”
According to the Centers for Disease Control and Prevention, the vaccines teach the body to produce the spike protein, which then triggers an immune response that creates antibodies that will attack the virus.
A PolitiFact review debunks the notion that the mRNA vaccines are toxic, cytotoxic, or introduce live, active virus proteins into the body.
FactCheck.org also disputed Dr. McCullough’s claim in a July 13 Ingraham Angle appearance that the mRNA vaccines are ineffective against the Delta variant.
In the FactCheck article, Frederic Bushman, codirector of the University of Pennsylvania’s Center for Research on Coronaviruses and Other Emerging Pathogens, said that people were much better off being vaccinated than not,” adding, “the Delta variant may reduce the effectiveness [of the vaccines] a little, but still, they’re so effective that you get a lot of benefit.”
“The vaccines are failing,” Dr. McCullough asserted in an Aug. 3 video interview posted on Odysee. “As we sit here today, we have 11,000 Americans that the CDC has certified have died after the vaccine,” he said, citing two analyses – one by Jessica Rose, PhD, and another by British researchers.
Similar figures reportedly based on cases reported to the Food and Drug Administration’s Vaccine Adverse Events Reporting System (VAERS) were forwarded to this news organization by Dr. McCullough.
The CDC website notes that the agency has received reports of 7,653 deaths in people who received a vaccine as of Sept. 13 (0.0020% of vaccine doses given since Dec. 14, 2020), but it cautions that those deaths do not mean the vaccine was the cause.
Dr. McCullough repeatedly claimed in the Aug. 3 interview that the government has not been transparent on vaccine safety. Since June 2020, the CDC’s Advisory Committee on Immunization Practices has held 16 public meetings on the COVID-19 vaccines.
To date, the agency has advised clinicians to monitor for rare side effects including Guillain-Barré syndrome and thrombosis with thrombocytopenia syndrome after the Johnson & Johnson vaccine and myocarditis after mRNA (Pfizer-BioNTech and Moderna) vaccines.
Med schools distance themselves
According to the Baylor Scott & White suit, Dr. McCullough agreed on Feb. 24 in a confidential separation agreement that he would no longer use his academic or leadership titles nor hold himself out to be affiliated with Baylor University Medical Center, Baylor Heart and Vascular Institute, the Baylor Research Institute, or any other related institutions.
However, as of August, according to a Baylor spokesperson, McCullough continued to have privileges at Baylor University Medical Center and Baylor Scott & White Heart and Vascular Hospital, Dallas.
The lawsuit points to three interviews posted in June and July where Dr. McCullough is identified as a “vice chief of medicine” or a “vice chief of internal medicine,” both at Baylor University. It also cites a profile at the Cardiometabolic Health Congress website – which this news organization had also viewed – that was still active in late July with a similar title. The profile was later scrubbed from the site.
Social media posts and other media continue to refer to Dr. McCullough’s Baylor credentials. An episode of the Faith and Freedom podcast posted on Aug. 2 identified McCullough as a “professor of medicine at Baylor University Medical Center.”
As of Sept. 16, Dr. McCullough’s bio page at his current practice, Heart Place, lists him as a professor of medicine at Texas A&M College of Medicine. A spokesperson for Texas A&M told this news organization that McCullough is no longer affiliated with the school.
Dr. McCullough acknowledged in the Aug. 3 interview that his Texas A&M title had been “stripped away” at “around the same time this lawsuit was filed.”
He was still a professor of medicine at the TCU and UNTHSC School of Medicine in Fort Worth, but a school spokesperson notified this news organization on Aug. 19 that Dr. McCullough was no longer with the school.
Dr. McCullough has portrayed himself as both a victim and a truth-teller, a “concerned physician” warning the world about the dangers of COVID-19 vaccines. The Baylor Scott & White lawsuit “is really a strong-armed tactic,” he said in the Aug. 3 interview. “I’m just a little guy, so I have to hire my legal teams, and in a sense be drained dry on legal fees,” he said.
But Dr. McCullough apparently has a plan for helping to defray his legal costs. In the Aug. 3 interview, he said a foundation he helped start, Truth for Health, has a “donation side to it,” adding “some of that may be used for legal expense.”
Cheryl Jones, an attorney with PK Law in Towson, Md., said that might draw interest from the Internal Revenue Service. “I would expect IRS scrutiny if contributions to the Medical Censorship Defense Fund are used to defend Dr McCullough in his personal breach of contract lawsuit,” she told this news organization.
The IRS generally recognizes defending “human and civil rights secured by law” as a legitimate charitable purpose for a legal defense fund, she said, adding that such a fund “must serve only public, rather than private, interests.”
Misinformation from a physician more damaging?
Some in the medical field have refuted Dr. McCullough’s pronouncements on how to treat COVID-19, including two infectious disease specialists with Monash University, Melbourne, who responded to the cardiologist’s original paper in the American Journal of Medicine.
Tony Korman, MBBS, a professor at the Centre for Inflammatory Diseases at Monash, told this news organization, “we had concerns that reputable medical journals would accept and publish papers proposing treatment of COVID-19 which was not supported by evidence.”
The website Healthfeedback.org has also challenged McCullough’s and his supporters’ claims, including that the American Journal of Medicine endorsed the use of hydroxychloroquine and that the COVID-19 vaccines have caused thousands of deaths.
David Broniatowski, PhD, associate director for the Institute for Data, Democracy and Politics at George Washington University, Washington, said in an interview that Dr. McCullough’s casting himself as a “rebel doctor” is a well-known trope in the vaccine misinformation universe.
Although he was not familiar with Dr. McCullough, Dr. Broniatowski said the cardiologist’s claims are not unique – they’ve been circulating among antivaccine and conspiracy-oriented groups for months.
For instance, Dr. McCullough has claimed in interviews that a whistleblower within the CDC knows of 50,000 vaccine-related deaths. Using data from the supposed whistleblower, the group America’s Frontline Doctors sued the federal government in July to stop the administration of COVID-19 vaccines to those under 18, people who have already had COVID, and individuals who the group said have not been adequately informed about the risks.
The idea of a whistleblower inside the CDC is recycled from antivaccine claims from decades ago, Dr. Broniatowski said.
But, he added, “somebody who speaks with the credibility of a major institution will be more likely to be listened to by some people.” That vulnerable group is “being taken advantage of by a relatively small number of disinformation purveyors, who, in some cases, profit from that disinformation,” said Dr. Broniatowski.
“We rely on our doctors because we trust them,” he said. “And we trust them because we believe that as physicians, their value system places the patient’s best interests first. That’s why it’s so much of a disappointment when you have a physician that appears to be exercising this sort of bad judgment.”
Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, also said that he was not familiar with Dr. McCullough. But apprised of his claims, Dr. Offit told this news organization, “Peter McCullough is a friend of the virus.”
“The kind of information he promotes allows the virus to continue to spread, continue to do an enormous amount of harm, and continue to mutate and create variants that have become more contagious and more resistant to vaccine-induced immunity,” said Dr. Offit, the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia.
Dr. Offit added that the war should be against SARS-CoV-2, but “because this virus has so many supporters, the war in essence becomes a war against ourselves, which is much harder.”
Dr. McCullough maintains he is doing a service to his patients. “I’m just giving and trying to help America understand the pandemic,” he told Ms. Ingraham on Fox News on July 29.
But he acknowledged concern about the Federation of State Medical Board’s announcement that physicians who spread COVID-19 vaccine misinformation risk suspension or revocation of their license.
“I have to tell you I’m worried – that no matter what I do and how careful I am to cite the scientific studies, I’m still gonna be hunted down for quote, misinformation,” he said in the Aug. 3 interview.
A version of this article first appeared on Medscape.com.
in which he agreed to stop mentioning his prior leadership and academic appointments.
Baylor was the first institution to cut ties with Dr. McCullough, who has promoted the use of therapies seen as unproven for the treatment of COVID-19 and has questioned the effectiveness of COVID-19 vaccines. Since the Baylor suit, the Texas A&M College of Medicine, and the Texas Christian University (TCU) and University of North Texas Health Science Center (UNTHSC) School of Medicine have both removed Dr. McCullough from their faculties.
Granted by the 191st District Court in Dallas County, Tex., the Baylor restraining order – which is in effect at least until a hearing on the case on September 30 – was sought as part of Baylor Scott & White’s breach of contract suit against McCullough, who had previously been known as a well-respected expert in cardiorenal issues. The suit is seeking $1 million in damages, as well as attorneys’ fees.
The suit seeks to “enforce the terms” of the confidential employment separation agreement signed by Dr. McCullough in February and prevent Dr. McCullough from continuing “improper use of titles and claimed affiliations that have already confused the media, the medical community and the public,” it reads.
“This ongoing confusion regarding [Dr.] McCullough’s affiliations, and whether Plaintiffs support his opinions, is exactly what Plaintiffs bargained to avoid in the Separation Agreement,” and is likely to cause “irreparable reputational and business harm that is incapable of remedy by money damages alone,” the suit states.
One of Dr. McCullough’s attorneys, Clinton Mikel, maintains that all the times the physician was identified in the “thousands of hours of media interviews and countless publications since his departure from Baylor” were “said/printed by a third party with no encouragement from Dr. McCullough,” and that the doctor “does not and cannot control third parties.”
Mr. Mikel said in a statement emailed to this news organization by Dr. McCullough that the suit is “a politically motivated attempt to silence Dr. McCullough,” because it was filed on the same day the organization mandated COVID-19 vaccination for employees.
Dr. McCullough “intends to vigorously defend against Baylor’s unfounded lawsuit,” will seek to dissolve the restraining order, and recover “all payments due him from Baylor under the terms of the settlement agreement,” wrote Mr. Mikel.
The cardiologist’s legal team filed a motion to dismiss the suit on Aug. 9, essentially arguing that Baylor Scott & White’s action restricted Dr. McCullough’s right to free speech under the Texas Citizen’s Participation Act.
COVID-19 vaccines = bioterrorism?
Dr. McCullough accumulated a following in 2020 by promoting early at-home multidrug treatment of COVID-19 in interviews with conservative websites and at a U.S. Senate hearing in November.
Although Dr. McCullough does not appear to have any personal social media accounts, his broadcast and podcast interviews are tweeted by thousands daily around the world and featured on Facebook pages like “Pandemic Debate.”
Some Facebook posts with Dr. McCullough’s pronouncements have been labeled as misinformation or removed. Some of his videos remain on YouTube, where they are posted by the Association of American Physicians and Surgeons, a group that believes Dr. McCullough is “under fierce attack for speaking out about COVID-19 early treatment and vaccine safety.”
Dr. McCullough’s March 2021 testimony to the Texas Senate’s Health and Human Services Committee – in which he claimed that COVID-19 patients are being denied what he called proven treatments like hydroxychloroquine – has been viewed more than 3.7 million times on YouTube. The appearance has also been tweeted repeatedly.
Most of Dr. McCullough’s interviews and presentations are aggregated on Rumble, an alternative to YouTube.
In interviews, Dr. McCullough promotes the use of zinc, hydroxychloroquine, azithromycin, doxycycline, favipiravir, prednisone, and ivermectin as COVID-19 treatments – based on an outpatient treatment algorithm published in August 2020 in the American Journal of Medicine. The cardiologist was the lead author of that paper, which proposed treating people with COVID-like symptoms whether or not they had confirmed infection.
Dr. McCullough and colleagues published a follow-up paper that added colchicine to the mix in Reviews in Cardiovascular Medicine. Dr. McCullough is editor-in-chief of the journal, but this was not noted in the disclosures.
Similarly, Dr. McCullough has not disclosed in his COVID-19 publications or any interviews that he has received consulting fees from a host of pharmaceutical manufacturers that produce COVID-19 drugs and vaccines, including AstraZeneca, Eli Lilly, and Regeneron Pharmaceuticals. According to the Centers for Medicare & Medicaid Services’ Open Payments database, Dr. McCullough was paid about $300,000 annually by drug companies from 2014 to 2019, mostly for consulting on cardiovascular and diabetes medications. His payments dropped to $169,406.06 in 2020.
Dr. McCullough appeared on “The Ingraham Angle” on Fox News in December 2020, claiming that sequential, early treatment with “anti-infectives, corticosteroids, and then antithrombotics” could “reduce [COVID-19] hospitalizations by 85% and cut mortality in half.”
He repeated the claim on the Ingraham show in July and agreed with host Laura Ingraham that the vast majority of healthy people would do fine if they got COVID. He also made the claim that 84% of the COVID-19 cases in Israel were in people who had been vaccinated. “So it’s clear, we can’t vaccinate our way out of this,” he said. An Associated Press “fact check” report has pushed back on similar assertions about vaccine data from Israel.
In a separate interview posted in June, Dr. McCullough called the pandemic the first phase of a bioterrorism event, which was “all about keeping the population in fear and in isolation and preparing them to accept the vaccine, which appears to be phase two of a bioterrorism operation.”
In addition, he said, “good doctors are doing unthinkable things like injecting biologically active messenger RNA that produces this pathogenic spike protein into pregnant women.”
According to the Centers for Disease Control and Prevention, the vaccines teach the body to produce the spike protein, which then triggers an immune response that creates antibodies that will attack the virus.
A PolitiFact review debunks the notion that the mRNA vaccines are toxic, cytotoxic, or introduce live, active virus proteins into the body.
FactCheck.org also disputed Dr. McCullough’s claim in a July 13 Ingraham Angle appearance that the mRNA vaccines are ineffective against the Delta variant.
In the FactCheck article, Frederic Bushman, codirector of the University of Pennsylvania’s Center for Research on Coronaviruses and Other Emerging Pathogens, said that people were much better off being vaccinated than not,” adding, “the Delta variant may reduce the effectiveness [of the vaccines] a little, but still, they’re so effective that you get a lot of benefit.”
“The vaccines are failing,” Dr. McCullough asserted in an Aug. 3 video interview posted on Odysee. “As we sit here today, we have 11,000 Americans that the CDC has certified have died after the vaccine,” he said, citing two analyses – one by Jessica Rose, PhD, and another by British researchers.
Similar figures reportedly based on cases reported to the Food and Drug Administration’s Vaccine Adverse Events Reporting System (VAERS) were forwarded to this news organization by Dr. McCullough.
The CDC website notes that the agency has received reports of 7,653 deaths in people who received a vaccine as of Sept. 13 (0.0020% of vaccine doses given since Dec. 14, 2020), but it cautions that those deaths do not mean the vaccine was the cause.
Dr. McCullough repeatedly claimed in the Aug. 3 interview that the government has not been transparent on vaccine safety. Since June 2020, the CDC’s Advisory Committee on Immunization Practices has held 16 public meetings on the COVID-19 vaccines.
To date, the agency has advised clinicians to monitor for rare side effects including Guillain-Barré syndrome and thrombosis with thrombocytopenia syndrome after the Johnson & Johnson vaccine and myocarditis after mRNA (Pfizer-BioNTech and Moderna) vaccines.
Med schools distance themselves
According to the Baylor Scott & White suit, Dr. McCullough agreed on Feb. 24 in a confidential separation agreement that he would no longer use his academic or leadership titles nor hold himself out to be affiliated with Baylor University Medical Center, Baylor Heart and Vascular Institute, the Baylor Research Institute, or any other related institutions.
However, as of August, according to a Baylor spokesperson, McCullough continued to have privileges at Baylor University Medical Center and Baylor Scott & White Heart and Vascular Hospital, Dallas.
The lawsuit points to three interviews posted in June and July where Dr. McCullough is identified as a “vice chief of medicine” or a “vice chief of internal medicine,” both at Baylor University. It also cites a profile at the Cardiometabolic Health Congress website – which this news organization had also viewed – that was still active in late July with a similar title. The profile was later scrubbed from the site.
Social media posts and other media continue to refer to Dr. McCullough’s Baylor credentials. An episode of the Faith and Freedom podcast posted on Aug. 2 identified McCullough as a “professor of medicine at Baylor University Medical Center.”
As of Sept. 16, Dr. McCullough’s bio page at his current practice, Heart Place, lists him as a professor of medicine at Texas A&M College of Medicine. A spokesperson for Texas A&M told this news organization that McCullough is no longer affiliated with the school.
Dr. McCullough acknowledged in the Aug. 3 interview that his Texas A&M title had been “stripped away” at “around the same time this lawsuit was filed.”
He was still a professor of medicine at the TCU and UNTHSC School of Medicine in Fort Worth, but a school spokesperson notified this news organization on Aug. 19 that Dr. McCullough was no longer with the school.
Dr. McCullough has portrayed himself as both a victim and a truth-teller, a “concerned physician” warning the world about the dangers of COVID-19 vaccines. The Baylor Scott & White lawsuit “is really a strong-armed tactic,” he said in the Aug. 3 interview. “I’m just a little guy, so I have to hire my legal teams, and in a sense be drained dry on legal fees,” he said.
But Dr. McCullough apparently has a plan for helping to defray his legal costs. In the Aug. 3 interview, he said a foundation he helped start, Truth for Health, has a “donation side to it,” adding “some of that may be used for legal expense.”
Cheryl Jones, an attorney with PK Law in Towson, Md., said that might draw interest from the Internal Revenue Service. “I would expect IRS scrutiny if contributions to the Medical Censorship Defense Fund are used to defend Dr McCullough in his personal breach of contract lawsuit,” she told this news organization.
The IRS generally recognizes defending “human and civil rights secured by law” as a legitimate charitable purpose for a legal defense fund, she said, adding that such a fund “must serve only public, rather than private, interests.”
Misinformation from a physician more damaging?
Some in the medical field have refuted Dr. McCullough’s pronouncements on how to treat COVID-19, including two infectious disease specialists with Monash University, Melbourne, who responded to the cardiologist’s original paper in the American Journal of Medicine.
Tony Korman, MBBS, a professor at the Centre for Inflammatory Diseases at Monash, told this news organization, “we had concerns that reputable medical journals would accept and publish papers proposing treatment of COVID-19 which was not supported by evidence.”
The website Healthfeedback.org has also challenged McCullough’s and his supporters’ claims, including that the American Journal of Medicine endorsed the use of hydroxychloroquine and that the COVID-19 vaccines have caused thousands of deaths.
David Broniatowski, PhD, associate director for the Institute for Data, Democracy and Politics at George Washington University, Washington, said in an interview that Dr. McCullough’s casting himself as a “rebel doctor” is a well-known trope in the vaccine misinformation universe.
Although he was not familiar with Dr. McCullough, Dr. Broniatowski said the cardiologist’s claims are not unique – they’ve been circulating among antivaccine and conspiracy-oriented groups for months.
For instance, Dr. McCullough has claimed in interviews that a whistleblower within the CDC knows of 50,000 vaccine-related deaths. Using data from the supposed whistleblower, the group America’s Frontline Doctors sued the federal government in July to stop the administration of COVID-19 vaccines to those under 18, people who have already had COVID, and individuals who the group said have not been adequately informed about the risks.
The idea of a whistleblower inside the CDC is recycled from antivaccine claims from decades ago, Dr. Broniatowski said.
But, he added, “somebody who speaks with the credibility of a major institution will be more likely to be listened to by some people.” That vulnerable group is “being taken advantage of by a relatively small number of disinformation purveyors, who, in some cases, profit from that disinformation,” said Dr. Broniatowski.
“We rely on our doctors because we trust them,” he said. “And we trust them because we believe that as physicians, their value system places the patient’s best interests first. That’s why it’s so much of a disappointment when you have a physician that appears to be exercising this sort of bad judgment.”
Paul Offit, MD, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, also said that he was not familiar with Dr. McCullough. But apprised of his claims, Dr. Offit told this news organization, “Peter McCullough is a friend of the virus.”
“The kind of information he promotes allows the virus to continue to spread, continue to do an enormous amount of harm, and continue to mutate and create variants that have become more contagious and more resistant to vaccine-induced immunity,” said Dr. Offit, the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia.
Dr. Offit added that the war should be against SARS-CoV-2, but “because this virus has so many supporters, the war in essence becomes a war against ourselves, which is much harder.”
Dr. McCullough maintains he is doing a service to his patients. “I’m just giving and trying to help America understand the pandemic,” he told Ms. Ingraham on Fox News on July 29.
But he acknowledged concern about the Federation of State Medical Board’s announcement that physicians who spread COVID-19 vaccine misinformation risk suspension or revocation of their license.
“I have to tell you I’m worried – that no matter what I do and how careful I am to cite the scientific studies, I’m still gonna be hunted down for quote, misinformation,” he said in the Aug. 3 interview.
A version of this article first appeared on Medscape.com.