User login
Multicenter study cites safety of power morcellation within an insufflated isolation bag
A 16-month multicenter study in which 73 patients underwent morcellation of the uterus or myomas within an insufflated isolation bag during minimally invasive (MI) hysterectomy or myomectomy recently has been published in Obstetrics & Gynecology. The researchers conclude that contained power morcellation using this technique is feasible.1
Sarah L. Cohen, MD, MPH, and colleagues at Fairview Ridges Hospital, Burnsville, Minnesota; Johns Hopkins Hospital, Baltimore, Maryland; Massachusetts General Hospital, Boston; and Brigham and Women’s Hospital, Boston, Massachusetts are all high-volume surgeons experienced in advanced MI gynecologic surgical techniques.1
Patients in whom morcellation was planned at the time of MI hysterectomy or myomectomy during the study period (January 2013 through April 2014) were offered in-bag morcellation and included in the study. Exclusion criteria were known or suspected malignancy. Preoperative testing was performed to evaluate risk of genital tract cancer. Perioperative information included mode of access, type of procedure(s) performed, operative time, estimated blood loss, specimen weight, intact status of isolation bag postmorcellation, length of hospital stay, intraoperative complications, postoperative complications, readmission, and reoperation.1
The technique for morcellation within an insufflated isolation bag was developed by one of the authors, Tony Shibley, MD, for use during laparoendoscopic single-site hysterectomy (WATCH Dr. Shibley’s technique video here and listen to an interview with Dr. Shibley here.) The technique adapts to multiport laparoscopic and robot-assisted laparoscopic hysterectomy and myomectomy.1
Based on the results of their study, the authors conclude: “Morcellation within an insufflated isolation bag is a feasible technique. Methods for morcellating uterine tissue in a contained manner may provide an option to minimize the risks of open power morcellation while preserving the benefits of minimally invasive surgery.”1
In response to this study, Charles R. Rardin, MD, Associate Professor of Obstetrics and Gynecology at Brown Medical School and Women and Infants’ Hospital in Providence, Rhode Island, wrote an online editorial in Obstetrics & Gynecology.2 Dr. Rardin pointed out that “Until there are more effective screening tools to detect these unusual cancers [leiomyosarcoma], surgeons and hospitals are required to develop responses to these issues.”
He suggests that one extreme reaction to the morcellation crisis is to ban any method of morcellation entirely, leaving laparotomy as the only option for tissue extraction. Finding that logic faulty—relative value to the few at greater cost to the many—he suggests that one might also question the safety of other strategies to treat leiomyomas, including ablation and embolization.
Institutions have responded in several different ways, he says:
- Some hospitals have completely banned power morcellation (See “FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy.”
- Some allow power morcellation with additional layers of informed consent or case approval.
- One university allows power morcellation only when a uterus is less than 18 weeks’ gestation in size. Morcellation is only permitted when using an endoscopic collection bag.
He finds that Cohen and colleagues’ techniques lack formal investigation of bag integrity or tissue spread (as successful control of tissue spread was judged by a visual assessment by the surgeon). He also indicates that the technique described is better suited to single-port laparoscopy than multi-port, that single-site laparoscopy required additional training and skill, and that the incisions in single-site laparoscopy are fewer in number but larger in diameter, eliciting concern for increased hernia formation. The authors recognize that using the technique in multi-port surgery, because penetration of the bag by one or more trocars may cause a disruption in bag integrity, is in violation of the manufacturer’s recommendations.1,2 Dr. Rardin additionally expresses concern about “the passage of trocars through the peritoneal cavity, out of direct visualization until the trocar pierces the bag”2 where the camera resides. He is concerned about reducing one set of risks while increasing other risks, and suggests that vaginal hysterectomy would reduce the risk of dissemination while preserving the patient’s benefits from minimally invasive surgery.2
1. Cohen SL, Einarsson JI, Wang KC, et al. Contained power morcellation within an insufflated isolation bag [published online ahead of print August 5, 2014]. Obstet Gyncol. doi:10.1097/AOG.0000000000000421. http://journals.lww.com/greenjournal/Abstract/publishahead/Contained_Power_Morcellation_Within_an_Insufflated.99365.aspx. Accessed August 15, 2014.
2. Rardin CR. Mitigating risks of specimen extraction: Is in-bag power morcellation an answer? [published online ahead of print August 5, 2014]. Obstet Gynecol. doi:10.1097/AOG.0000000000000434. http://journals.lww.com/greenjournal/Citation/publishahead/Mitigating_Risks_of_Specimen_Extraction__Is_In_Bag.99352.aspx. Accessed August 15, 2014.
A 16-month multicenter study in which 73 patients underwent morcellation of the uterus or myomas within an insufflated isolation bag during minimally invasive (MI) hysterectomy or myomectomy recently has been published in Obstetrics & Gynecology. The researchers conclude that contained power morcellation using this technique is feasible.1
Sarah L. Cohen, MD, MPH, and colleagues at Fairview Ridges Hospital, Burnsville, Minnesota; Johns Hopkins Hospital, Baltimore, Maryland; Massachusetts General Hospital, Boston; and Brigham and Women’s Hospital, Boston, Massachusetts are all high-volume surgeons experienced in advanced MI gynecologic surgical techniques.1
Patients in whom morcellation was planned at the time of MI hysterectomy or myomectomy during the study period (January 2013 through April 2014) were offered in-bag morcellation and included in the study. Exclusion criteria were known or suspected malignancy. Preoperative testing was performed to evaluate risk of genital tract cancer. Perioperative information included mode of access, type of procedure(s) performed, operative time, estimated blood loss, specimen weight, intact status of isolation bag postmorcellation, length of hospital stay, intraoperative complications, postoperative complications, readmission, and reoperation.1
The technique for morcellation within an insufflated isolation bag was developed by one of the authors, Tony Shibley, MD, for use during laparoendoscopic single-site hysterectomy (WATCH Dr. Shibley’s technique video here and listen to an interview with Dr. Shibley here.) The technique adapts to multiport laparoscopic and robot-assisted laparoscopic hysterectomy and myomectomy.1
Based on the results of their study, the authors conclude: “Morcellation within an insufflated isolation bag is a feasible technique. Methods for morcellating uterine tissue in a contained manner may provide an option to minimize the risks of open power morcellation while preserving the benefits of minimally invasive surgery.”1
In response to this study, Charles R. Rardin, MD, Associate Professor of Obstetrics and Gynecology at Brown Medical School and Women and Infants’ Hospital in Providence, Rhode Island, wrote an online editorial in Obstetrics & Gynecology.2 Dr. Rardin pointed out that “Until there are more effective screening tools to detect these unusual cancers [leiomyosarcoma], surgeons and hospitals are required to develop responses to these issues.”
He suggests that one extreme reaction to the morcellation crisis is to ban any method of morcellation entirely, leaving laparotomy as the only option for tissue extraction. Finding that logic faulty—relative value to the few at greater cost to the many—he suggests that one might also question the safety of other strategies to treat leiomyomas, including ablation and embolization.
Institutions have responded in several different ways, he says:
- Some hospitals have completely banned power morcellation (See “FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy.”
- Some allow power morcellation with additional layers of informed consent or case approval.
- One university allows power morcellation only when a uterus is less than 18 weeks’ gestation in size. Morcellation is only permitted when using an endoscopic collection bag.
He finds that Cohen and colleagues’ techniques lack formal investigation of bag integrity or tissue spread (as successful control of tissue spread was judged by a visual assessment by the surgeon). He also indicates that the technique described is better suited to single-port laparoscopy than multi-port, that single-site laparoscopy required additional training and skill, and that the incisions in single-site laparoscopy are fewer in number but larger in diameter, eliciting concern for increased hernia formation. The authors recognize that using the technique in multi-port surgery, because penetration of the bag by one or more trocars may cause a disruption in bag integrity, is in violation of the manufacturer’s recommendations.1,2 Dr. Rardin additionally expresses concern about “the passage of trocars through the peritoneal cavity, out of direct visualization until the trocar pierces the bag”2 where the camera resides. He is concerned about reducing one set of risks while increasing other risks, and suggests that vaginal hysterectomy would reduce the risk of dissemination while preserving the patient’s benefits from minimally invasive surgery.2
A 16-month multicenter study in which 73 patients underwent morcellation of the uterus or myomas within an insufflated isolation bag during minimally invasive (MI) hysterectomy or myomectomy recently has been published in Obstetrics & Gynecology. The researchers conclude that contained power morcellation using this technique is feasible.1
Sarah L. Cohen, MD, MPH, and colleagues at Fairview Ridges Hospital, Burnsville, Minnesota; Johns Hopkins Hospital, Baltimore, Maryland; Massachusetts General Hospital, Boston; and Brigham and Women’s Hospital, Boston, Massachusetts are all high-volume surgeons experienced in advanced MI gynecologic surgical techniques.1
Patients in whom morcellation was planned at the time of MI hysterectomy or myomectomy during the study period (January 2013 through April 2014) were offered in-bag morcellation and included in the study. Exclusion criteria were known or suspected malignancy. Preoperative testing was performed to evaluate risk of genital tract cancer. Perioperative information included mode of access, type of procedure(s) performed, operative time, estimated blood loss, specimen weight, intact status of isolation bag postmorcellation, length of hospital stay, intraoperative complications, postoperative complications, readmission, and reoperation.1
The technique for morcellation within an insufflated isolation bag was developed by one of the authors, Tony Shibley, MD, for use during laparoendoscopic single-site hysterectomy (WATCH Dr. Shibley’s technique video here and listen to an interview with Dr. Shibley here.) The technique adapts to multiport laparoscopic and robot-assisted laparoscopic hysterectomy and myomectomy.1
Based on the results of their study, the authors conclude: “Morcellation within an insufflated isolation bag is a feasible technique. Methods for morcellating uterine tissue in a contained manner may provide an option to minimize the risks of open power morcellation while preserving the benefits of minimally invasive surgery.”1
In response to this study, Charles R. Rardin, MD, Associate Professor of Obstetrics and Gynecology at Brown Medical School and Women and Infants’ Hospital in Providence, Rhode Island, wrote an online editorial in Obstetrics & Gynecology.2 Dr. Rardin pointed out that “Until there are more effective screening tools to detect these unusual cancers [leiomyosarcoma], surgeons and hospitals are required to develop responses to these issues.”
He suggests that one extreme reaction to the morcellation crisis is to ban any method of morcellation entirely, leaving laparotomy as the only option for tissue extraction. Finding that logic faulty—relative value to the few at greater cost to the many—he suggests that one might also question the safety of other strategies to treat leiomyomas, including ablation and embolization.
Institutions have responded in several different ways, he says:
- Some hospitals have completely banned power morcellation (See “FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy.”
- Some allow power morcellation with additional layers of informed consent or case approval.
- One university allows power morcellation only when a uterus is less than 18 weeks’ gestation in size. Morcellation is only permitted when using an endoscopic collection bag.
He finds that Cohen and colleagues’ techniques lack formal investigation of bag integrity or tissue spread (as successful control of tissue spread was judged by a visual assessment by the surgeon). He also indicates that the technique described is better suited to single-port laparoscopy than multi-port, that single-site laparoscopy required additional training and skill, and that the incisions in single-site laparoscopy are fewer in number but larger in diameter, eliciting concern for increased hernia formation. The authors recognize that using the technique in multi-port surgery, because penetration of the bag by one or more trocars may cause a disruption in bag integrity, is in violation of the manufacturer’s recommendations.1,2 Dr. Rardin additionally expresses concern about “the passage of trocars through the peritoneal cavity, out of direct visualization until the trocar pierces the bag”2 where the camera resides. He is concerned about reducing one set of risks while increasing other risks, and suggests that vaginal hysterectomy would reduce the risk of dissemination while preserving the patient’s benefits from minimally invasive surgery.2
1. Cohen SL, Einarsson JI, Wang KC, et al. Contained power morcellation within an insufflated isolation bag [published online ahead of print August 5, 2014]. Obstet Gyncol. doi:10.1097/AOG.0000000000000421. http://journals.lww.com/greenjournal/Abstract/publishahead/Contained_Power_Morcellation_Within_an_Insufflated.99365.aspx. Accessed August 15, 2014.
2. Rardin CR. Mitigating risks of specimen extraction: Is in-bag power morcellation an answer? [published online ahead of print August 5, 2014]. Obstet Gynecol. doi:10.1097/AOG.0000000000000434. http://journals.lww.com/greenjournal/Citation/publishahead/Mitigating_Risks_of_Specimen_Extraction__Is_In_Bag.99352.aspx. Accessed August 15, 2014.
1. Cohen SL, Einarsson JI, Wang KC, et al. Contained power morcellation within an insufflated isolation bag [published online ahead of print August 5, 2014]. Obstet Gyncol. doi:10.1097/AOG.0000000000000421. http://journals.lww.com/greenjournal/Abstract/publishahead/Contained_Power_Morcellation_Within_an_Insufflated.99365.aspx. Accessed August 15, 2014.
2. Rardin CR. Mitigating risks of specimen extraction: Is in-bag power morcellation an answer? [published online ahead of print August 5, 2014]. Obstet Gynecol. doi:10.1097/AOG.0000000000000434. http://journals.lww.com/greenjournal/Citation/publishahead/Mitigating_Risks_of_Specimen_Extraction__Is_In_Bag.99352.aspx. Accessed August 15, 2014.
Laparoscopic power morcellation coverage will end as of September 1 for Blue Cross Blue Shield affiliate
About 5.2 million people insured by Highmark Inc, a Blue Cross and Blue Shield (BCBS)–affiliated company in Pennsylvania, Delaware, and West Virginia will be denied coverage for laparoscopic power morcellation used in gynecologic surgery. Highmark is the fourth-largest BCBS affiliate.1
On August 2, spokesman Aaron Billger announced by email that, in the best interest of their members, Highmark is halting coverage as of September 1, 2014.2 This decision comes in response to the US Food and Drug Administration (FDA) Safety Communication of April 17, 2014, that discouraged the use of power morcellation during hysterectomy and myomectomy because of the increased risk of dispersion of benign myoma tissue and occult malignant tissue through the abdominal cavity.2,3
University of Pittsburgh Medical Center (UPMC), the largest hospital group in western Pennsylvania, publicized that it will stop performing laparoscopic power morcellation as of September 1. UPMC spokesperson Gloria Kreps said the decision was an “appropriate and prudent course of action,” and that the hospital was “looking to the FDA for further guidance.”4 Other medical centers and hospitals have banned the use of power morcellation, beginning with Brigham and Women’s and Massachusetts General in April.5
In April 2014, Ethicon, a unit of Johnson & Johnson, suspended sales of all its morcellation devices. In an urgent Medical Device Market Withdrawal dated July 30, 2014, Ethicon initiated a “worldwide voluntary market withdrawal of all Ethicon Morcellation Devices that currently remain on the market.”6 Ethicon will issue prorated credit for morcellation devices returned by December 30, 2014, with full credit issued for unopened, unexpired disposable products.6
The FDA Obstetrics and Gynecology Devices Panel Advisory Committee held a 2-day hearing in July 2014 to weigh the risks and benefits of power morcellation. The panel will send recommendations to the FDA, and a final decision on the use of laparoscopic power morcellation will be forthcoming.7
1.
Reuters. U.S. insurer to stop coverage of gynecological procedure. http://in.reuters.com/article/2014/08/02/highmark-procedure-idINL2N0Q80IY20140802. Published August 3, 2014. Accessed August 6, 2014.
2. Kreiter M. Highmark Inc. says it won’t cover laparoscopic power morcellation because of cancer risk. International Business Times. http://www.ibtimes.com/highmark-inc-says-it-wont-cover-laparoscopic-power-morcellation-because-cancer-risk-1647160. Published August 2, 2014. Accessed August 6, 2014.
3. Yates J. FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy. OBG Manag. 2014;26(5):68, 67. http://www.obgmanagement.com/topic-collections/morcellation/article/fda-hospitals-caution-against-laparoscopic-power-morcellation-during-hysterectomy-and-myomectomy.html.
4. Mamula KB. UPMC drops controversial surgical procedure. Pittsburgh Business Times. http://www.bizjournals.com/pittsburgh/news/2014/08/01/upmc-drops-controversial-surgical-procedure.html. Published August 1, 2014. Accessed August 6, 2014.
5. Yates J. Open power morcellation of uterine tumors during hysterectomy banned at two Boston hospitals. OBG Manag. 2014;26(4). http://www.obgmanagement.com/topic-collections/morcellation/article/open-power-morcellation-of-uterine-tumors-during-hysterectomy-banned-at-two-boston-hospitals.html
6. Ethicon. Urgent: Medical device market withdrawal. http://www.ethicon.com/sites/default/files/managed-documents/Ethicon%20Morcellation%20Devices%20Customer%20Letter%20Final.pdf. Published July 30, 2014. Accessed August 6, 2014.
7. Iglesia C, Yates J. Why FDA hearing on morcellation safety could drive innovation [audiocast]. OBG Manag. 2014;26(7). http://www.obgmanagement.com/home/article/why-fda-hearing-on-morcellation-safety-could-drive-innovation/d1071c5e8326e8a2de76a30f0446b1ab.html. Published July 17, 2014. Accessed August 6, 2014.
About 5.2 million people insured by Highmark Inc, a Blue Cross and Blue Shield (BCBS)–affiliated company in Pennsylvania, Delaware, and West Virginia will be denied coverage for laparoscopic power morcellation used in gynecologic surgery. Highmark is the fourth-largest BCBS affiliate.1
On August 2, spokesman Aaron Billger announced by email that, in the best interest of their members, Highmark is halting coverage as of September 1, 2014.2 This decision comes in response to the US Food and Drug Administration (FDA) Safety Communication of April 17, 2014, that discouraged the use of power morcellation during hysterectomy and myomectomy because of the increased risk of dispersion of benign myoma tissue and occult malignant tissue through the abdominal cavity.2,3
University of Pittsburgh Medical Center (UPMC), the largest hospital group in western Pennsylvania, publicized that it will stop performing laparoscopic power morcellation as of September 1. UPMC spokesperson Gloria Kreps said the decision was an “appropriate and prudent course of action,” and that the hospital was “looking to the FDA for further guidance.”4 Other medical centers and hospitals have banned the use of power morcellation, beginning with Brigham and Women’s and Massachusetts General in April.5
In April 2014, Ethicon, a unit of Johnson & Johnson, suspended sales of all its morcellation devices. In an urgent Medical Device Market Withdrawal dated July 30, 2014, Ethicon initiated a “worldwide voluntary market withdrawal of all Ethicon Morcellation Devices that currently remain on the market.”6 Ethicon will issue prorated credit for morcellation devices returned by December 30, 2014, with full credit issued for unopened, unexpired disposable products.6
The FDA Obstetrics and Gynecology Devices Panel Advisory Committee held a 2-day hearing in July 2014 to weigh the risks and benefits of power morcellation. The panel will send recommendations to the FDA, and a final decision on the use of laparoscopic power morcellation will be forthcoming.7
About 5.2 million people insured by Highmark Inc, a Blue Cross and Blue Shield (BCBS)–affiliated company in Pennsylvania, Delaware, and West Virginia will be denied coverage for laparoscopic power morcellation used in gynecologic surgery. Highmark is the fourth-largest BCBS affiliate.1
On August 2, spokesman Aaron Billger announced by email that, in the best interest of their members, Highmark is halting coverage as of September 1, 2014.2 This decision comes in response to the US Food and Drug Administration (FDA) Safety Communication of April 17, 2014, that discouraged the use of power morcellation during hysterectomy and myomectomy because of the increased risk of dispersion of benign myoma tissue and occult malignant tissue through the abdominal cavity.2,3
University of Pittsburgh Medical Center (UPMC), the largest hospital group in western Pennsylvania, publicized that it will stop performing laparoscopic power morcellation as of September 1. UPMC spokesperson Gloria Kreps said the decision was an “appropriate and prudent course of action,” and that the hospital was “looking to the FDA for further guidance.”4 Other medical centers and hospitals have banned the use of power morcellation, beginning with Brigham and Women’s and Massachusetts General in April.5
In April 2014, Ethicon, a unit of Johnson & Johnson, suspended sales of all its morcellation devices. In an urgent Medical Device Market Withdrawal dated July 30, 2014, Ethicon initiated a “worldwide voluntary market withdrawal of all Ethicon Morcellation Devices that currently remain on the market.”6 Ethicon will issue prorated credit for morcellation devices returned by December 30, 2014, with full credit issued for unopened, unexpired disposable products.6
The FDA Obstetrics and Gynecology Devices Panel Advisory Committee held a 2-day hearing in July 2014 to weigh the risks and benefits of power morcellation. The panel will send recommendations to the FDA, and a final decision on the use of laparoscopic power morcellation will be forthcoming.7
1.
Reuters. U.S. insurer to stop coverage of gynecological procedure. http://in.reuters.com/article/2014/08/02/highmark-procedure-idINL2N0Q80IY20140802. Published August 3, 2014. Accessed August 6, 2014.
2. Kreiter M. Highmark Inc. says it won’t cover laparoscopic power morcellation because of cancer risk. International Business Times. http://www.ibtimes.com/highmark-inc-says-it-wont-cover-laparoscopic-power-morcellation-because-cancer-risk-1647160. Published August 2, 2014. Accessed August 6, 2014.
3. Yates J. FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy. OBG Manag. 2014;26(5):68, 67. http://www.obgmanagement.com/topic-collections/morcellation/article/fda-hospitals-caution-against-laparoscopic-power-morcellation-during-hysterectomy-and-myomectomy.html.
4. Mamula KB. UPMC drops controversial surgical procedure. Pittsburgh Business Times. http://www.bizjournals.com/pittsburgh/news/2014/08/01/upmc-drops-controversial-surgical-procedure.html. Published August 1, 2014. Accessed August 6, 2014.
5. Yates J. Open power morcellation of uterine tumors during hysterectomy banned at two Boston hospitals. OBG Manag. 2014;26(4). http://www.obgmanagement.com/topic-collections/morcellation/article/open-power-morcellation-of-uterine-tumors-during-hysterectomy-banned-at-two-boston-hospitals.html
6. Ethicon. Urgent: Medical device market withdrawal. http://www.ethicon.com/sites/default/files/managed-documents/Ethicon%20Morcellation%20Devices%20Customer%20Letter%20Final.pdf. Published July 30, 2014. Accessed August 6, 2014.
7. Iglesia C, Yates J. Why FDA hearing on morcellation safety could drive innovation [audiocast]. OBG Manag. 2014;26(7). http://www.obgmanagement.com/home/article/why-fda-hearing-on-morcellation-safety-could-drive-innovation/d1071c5e8326e8a2de76a30f0446b1ab.html. Published July 17, 2014. Accessed August 6, 2014.
1.
Reuters. U.S. insurer to stop coverage of gynecological procedure. http://in.reuters.com/article/2014/08/02/highmark-procedure-idINL2N0Q80IY20140802. Published August 3, 2014. Accessed August 6, 2014.
2. Kreiter M. Highmark Inc. says it won’t cover laparoscopic power morcellation because of cancer risk. International Business Times. http://www.ibtimes.com/highmark-inc-says-it-wont-cover-laparoscopic-power-morcellation-because-cancer-risk-1647160. Published August 2, 2014. Accessed August 6, 2014.
3. Yates J. FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy. OBG Manag. 2014;26(5):68, 67. http://www.obgmanagement.com/topic-collections/morcellation/article/fda-hospitals-caution-against-laparoscopic-power-morcellation-during-hysterectomy-and-myomectomy.html.
4. Mamula KB. UPMC drops controversial surgical procedure. Pittsburgh Business Times. http://www.bizjournals.com/pittsburgh/news/2014/08/01/upmc-drops-controversial-surgical-procedure.html. Published August 1, 2014. Accessed August 6, 2014.
5. Yates J. Open power morcellation of uterine tumors during hysterectomy banned at two Boston hospitals. OBG Manag. 2014;26(4). http://www.obgmanagement.com/topic-collections/morcellation/article/open-power-morcellation-of-uterine-tumors-during-hysterectomy-banned-at-two-boston-hospitals.html
6. Ethicon. Urgent: Medical device market withdrawal. http://www.ethicon.com/sites/default/files/managed-documents/Ethicon%20Morcellation%20Devices%20Customer%20Letter%20Final.pdf. Published July 30, 2014. Accessed August 6, 2014.
7. Iglesia C, Yates J. Why FDA hearing on morcellation safety could drive innovation [audiocast]. OBG Manag. 2014;26(7). http://www.obgmanagement.com/home/article/why-fda-hearing-on-morcellation-safety-could-drive-innovation/d1071c5e8326e8a2de76a30f0446b1ab.html. Published July 17, 2014. Accessed August 6, 2014.
First large study on the risk of cancer spread using power morcellation pinpoints risk of uterine malignancy
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
Fetal growth restriction may be underestimated in obese patients
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Survey: ObGyns’ salaries rose slightly in 2013
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
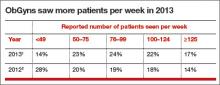
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
Paroxetine mesylate 7.5 mg found to be a safe alternative to hormone therapy for menopausal women with hot flashes
The US Food and Drug Administration (FDA) recently approved paroxetine mesylate 7.5 mg (Brisdelle) for the treatment of moderate to severe menopausal vasomotor symptoms (VMS). Paroxetine, formerly known as low-dose mesylate salt of paroxetine (LDMP), is a nonhormonal agent, which makes it an alternative hot flash therapy for menopausal women who cannot or do not want to use hormones. Paroxetine mesylate (Pexeva, Brisdelle) and paroxetine hydrochloride (Paxil, and generics) are two salts of the same active compound (paroxetine). They may have somewhat different metabolism.
The efficacy and safety of paroxetine mesylate, a selective serotonin-reuptake inhibitor (SSRI), were evaluated individually in three Phase 2 or 3 multicenter, double-blind, randomized, placebo-controlled trials, published by James Simon, MD, from George Washington University School of Medicine, and colleagues,1 and Joffe and colleagues.2 Most treatment-emergent adverse events (TEAEs) in the individual studies were mild or moderate in severity, with minimal acute discontinuation symptoms reported on treatment cessation.
In a study3 presented April 29, at the 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG) in Chicago, Illinois, Simon and colleagues further reported on the overall tolerability and safety profile of paroxetine mesylate 7.5 mg using pooled data from the three randomized trials. In their post-hoc analyses, they specifically examined the emergence of adverse events linked to the use of SSRIs when prescribed for psychiatric disorders at therapeutically higher doses than 7.5 mg. The adverse events focused on included weight gain, decreased libido, and sleep disturbance, as well as suicidality, abnormal bleeding, and bone fracture.
Study details. A total of 1,276 postmenopausal women (approximately 70% white) aged 40 years or older (median age, 54 years) with moderate to severe VMS (7−8 hot flashes/day; 50−60 hot flashes/wk) received either paroxetine mesylate or placebo at bedtime for 8 (Phase 2), 12 (Phase 3), or 24 (Phase 3) weeks. The study was sponsored by Noven Therapeutics, LLC.
Treatment-emergent adverse events and discontinuation
About half (50.4%) of the 635 women in the paroxetine group and 47.0% of the 641 women in the placebo group reported at least one TEAE. Most commonly reported TEAEs in the paroxetine group (reported in ≥2% of patients and with a twofold or higher frequency than in the placebo group) were nausea, fatigue, and dizziness.
TEAEs that were determined to be related to the study drug were reported in 19.5% in the paroxetine group and in 17.6% in the placebo group. These most frequent TEAEs were fatigue, nausea, dizziness, and diarrhea.
Severe AEs were reported in 3.9% and 3.6% of women in the paroxetine and placebo groups, respectively, although the investigator determined that less than 1% were related to paroxetine treatment.
TEAEs that led to discontinuation occurred in 4.7% of paroxetine-treated women and in 3.7% of placebo-treated women, although the incidence of study drug interruptions from TEAEs was similar (0.9%) between treatments. The most frequent adverse reactions leading to discontinuation in the paroxetine arm were abdominal pain (0.3%), attention disturbances (0.3%), headache (0.3%), and suicidal ideation (0.3%).
Of the most common AEs, nausea occurred mainly within the first 4 weeks of treatment; fatigue occurred primarily within the first week of treatment and decreased in frequency with continued therapy. Incidences and types of AEs that began after 12 weeks were similar to those that began during the first 12 weeks of treatment.
AEs related to SSRIs not found to be problematic
No differences were found between groups with regard to TEAEs related to weight, libido, or sleep. No clinically meaningful changes in laboratory values, vital signs, or ECGs were observed with either group. No clinically important findings on abnormal bleeding, bone fracture, or suicidality were evident in the paroxetine arm.
In the Phase 3 studies:
- One suicide attempt was reported in the paroxetine group in the 24-week study, but was determined by investigators to be unrelated to treatment
- Incidence rates of gastrointestinal and other bleeding events were similar between groups
- Five bone fractures were reported: One in the paroxetine group and four among three participants in the placebo group.
One death occurred in the 12-week Phase 3 study due to acute respiratory failure with evidence of hypertension-mediated pulmonary edema and hypertensive cardiovascular disease. The investigator did not consider the death to be related to the study drug.
Study conclusion
The authors concluded that paroxetine 7.5 mg had favorable tolerability in menopausal women with moderate to severe VMS.
“Paroxetine 7.5 mg offers a nonhormonal treatment option for women who seek treatment for moderate to severe hot flashes associated with menopause,” said Dr. Simon.3
Tell us what you think! Send your Letter to the Editor: rbarbieri@frontlinemedcom.com
1. Simon JA, et al. Low dose paroxetine 7.5 mg for menopausal vasomotor symptoms: two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
2. Joffe H et al. Low-dose mesylate salt of paroxetine (LDMP) in treatment of vasomotor symptoms (VMS) in menopause. Presented at: 2012 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists; May 7, 2012; San Diego, CA. Poster 43.
3. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate to severe vasomotor symptoms. Poster presented at: 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG); April 26–30, 2014; Chicago, IL.
The US Food and Drug Administration (FDA) recently approved paroxetine mesylate 7.5 mg (Brisdelle) for the treatment of moderate to severe menopausal vasomotor symptoms (VMS). Paroxetine, formerly known as low-dose mesylate salt of paroxetine (LDMP), is a nonhormonal agent, which makes it an alternative hot flash therapy for menopausal women who cannot or do not want to use hormones. Paroxetine mesylate (Pexeva, Brisdelle) and paroxetine hydrochloride (Paxil, and generics) are two salts of the same active compound (paroxetine). They may have somewhat different metabolism.
The efficacy and safety of paroxetine mesylate, a selective serotonin-reuptake inhibitor (SSRI), were evaluated individually in three Phase 2 or 3 multicenter, double-blind, randomized, placebo-controlled trials, published by James Simon, MD, from George Washington University School of Medicine, and colleagues,1 and Joffe and colleagues.2 Most treatment-emergent adverse events (TEAEs) in the individual studies were mild or moderate in severity, with minimal acute discontinuation symptoms reported on treatment cessation.
In a study3 presented April 29, at the 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG) in Chicago, Illinois, Simon and colleagues further reported on the overall tolerability and safety profile of paroxetine mesylate 7.5 mg using pooled data from the three randomized trials. In their post-hoc analyses, they specifically examined the emergence of adverse events linked to the use of SSRIs when prescribed for psychiatric disorders at therapeutically higher doses than 7.5 mg. The adverse events focused on included weight gain, decreased libido, and sleep disturbance, as well as suicidality, abnormal bleeding, and bone fracture.
Study details. A total of 1,276 postmenopausal women (approximately 70% white) aged 40 years or older (median age, 54 years) with moderate to severe VMS (7−8 hot flashes/day; 50−60 hot flashes/wk) received either paroxetine mesylate or placebo at bedtime for 8 (Phase 2), 12 (Phase 3), or 24 (Phase 3) weeks. The study was sponsored by Noven Therapeutics, LLC.
Treatment-emergent adverse events and discontinuation
About half (50.4%) of the 635 women in the paroxetine group and 47.0% of the 641 women in the placebo group reported at least one TEAE. Most commonly reported TEAEs in the paroxetine group (reported in ≥2% of patients and with a twofold or higher frequency than in the placebo group) were nausea, fatigue, and dizziness.
TEAEs that were determined to be related to the study drug were reported in 19.5% in the paroxetine group and in 17.6% in the placebo group. These most frequent TEAEs were fatigue, nausea, dizziness, and diarrhea.
Severe AEs were reported in 3.9% and 3.6% of women in the paroxetine and placebo groups, respectively, although the investigator determined that less than 1% were related to paroxetine treatment.
TEAEs that led to discontinuation occurred in 4.7% of paroxetine-treated women and in 3.7% of placebo-treated women, although the incidence of study drug interruptions from TEAEs was similar (0.9%) between treatments. The most frequent adverse reactions leading to discontinuation in the paroxetine arm were abdominal pain (0.3%), attention disturbances (0.3%), headache (0.3%), and suicidal ideation (0.3%).
Of the most common AEs, nausea occurred mainly within the first 4 weeks of treatment; fatigue occurred primarily within the first week of treatment and decreased in frequency with continued therapy. Incidences and types of AEs that began after 12 weeks were similar to those that began during the first 12 weeks of treatment.
AEs related to SSRIs not found to be problematic
No differences were found between groups with regard to TEAEs related to weight, libido, or sleep. No clinically meaningful changes in laboratory values, vital signs, or ECGs were observed with either group. No clinically important findings on abnormal bleeding, bone fracture, or suicidality were evident in the paroxetine arm.
In the Phase 3 studies:
- One suicide attempt was reported in the paroxetine group in the 24-week study, but was determined by investigators to be unrelated to treatment
- Incidence rates of gastrointestinal and other bleeding events were similar between groups
- Five bone fractures were reported: One in the paroxetine group and four among three participants in the placebo group.
One death occurred in the 12-week Phase 3 study due to acute respiratory failure with evidence of hypertension-mediated pulmonary edema and hypertensive cardiovascular disease. The investigator did not consider the death to be related to the study drug.
Study conclusion
The authors concluded that paroxetine 7.5 mg had favorable tolerability in menopausal women with moderate to severe VMS.
“Paroxetine 7.5 mg offers a nonhormonal treatment option for women who seek treatment for moderate to severe hot flashes associated with menopause,” said Dr. Simon.3
Tell us what you think! Send your Letter to the Editor: rbarbieri@frontlinemedcom.com
The US Food and Drug Administration (FDA) recently approved paroxetine mesylate 7.5 mg (Brisdelle) for the treatment of moderate to severe menopausal vasomotor symptoms (VMS). Paroxetine, formerly known as low-dose mesylate salt of paroxetine (LDMP), is a nonhormonal agent, which makes it an alternative hot flash therapy for menopausal women who cannot or do not want to use hormones. Paroxetine mesylate (Pexeva, Brisdelle) and paroxetine hydrochloride (Paxil, and generics) are two salts of the same active compound (paroxetine). They may have somewhat different metabolism.
The efficacy and safety of paroxetine mesylate, a selective serotonin-reuptake inhibitor (SSRI), were evaluated individually in three Phase 2 or 3 multicenter, double-blind, randomized, placebo-controlled trials, published by James Simon, MD, from George Washington University School of Medicine, and colleagues,1 and Joffe and colleagues.2 Most treatment-emergent adverse events (TEAEs) in the individual studies were mild or moderate in severity, with minimal acute discontinuation symptoms reported on treatment cessation.
In a study3 presented April 29, at the 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG) in Chicago, Illinois, Simon and colleagues further reported on the overall tolerability and safety profile of paroxetine mesylate 7.5 mg using pooled data from the three randomized trials. In their post-hoc analyses, they specifically examined the emergence of adverse events linked to the use of SSRIs when prescribed for psychiatric disorders at therapeutically higher doses than 7.5 mg. The adverse events focused on included weight gain, decreased libido, and sleep disturbance, as well as suicidality, abnormal bleeding, and bone fracture.
Study details. A total of 1,276 postmenopausal women (approximately 70% white) aged 40 years or older (median age, 54 years) with moderate to severe VMS (7−8 hot flashes/day; 50−60 hot flashes/wk) received either paroxetine mesylate or placebo at bedtime for 8 (Phase 2), 12 (Phase 3), or 24 (Phase 3) weeks. The study was sponsored by Noven Therapeutics, LLC.
Treatment-emergent adverse events and discontinuation
About half (50.4%) of the 635 women in the paroxetine group and 47.0% of the 641 women in the placebo group reported at least one TEAE. Most commonly reported TEAEs in the paroxetine group (reported in ≥2% of patients and with a twofold or higher frequency than in the placebo group) were nausea, fatigue, and dizziness.
TEAEs that were determined to be related to the study drug were reported in 19.5% in the paroxetine group and in 17.6% in the placebo group. These most frequent TEAEs were fatigue, nausea, dizziness, and diarrhea.
Severe AEs were reported in 3.9% and 3.6% of women in the paroxetine and placebo groups, respectively, although the investigator determined that less than 1% were related to paroxetine treatment.
TEAEs that led to discontinuation occurred in 4.7% of paroxetine-treated women and in 3.7% of placebo-treated women, although the incidence of study drug interruptions from TEAEs was similar (0.9%) between treatments. The most frequent adverse reactions leading to discontinuation in the paroxetine arm were abdominal pain (0.3%), attention disturbances (0.3%), headache (0.3%), and suicidal ideation (0.3%).
Of the most common AEs, nausea occurred mainly within the first 4 weeks of treatment; fatigue occurred primarily within the first week of treatment and decreased in frequency with continued therapy. Incidences and types of AEs that began after 12 weeks were similar to those that began during the first 12 weeks of treatment.
AEs related to SSRIs not found to be problematic
No differences were found between groups with regard to TEAEs related to weight, libido, or sleep. No clinically meaningful changes in laboratory values, vital signs, or ECGs were observed with either group. No clinically important findings on abnormal bleeding, bone fracture, or suicidality were evident in the paroxetine arm.
In the Phase 3 studies:
- One suicide attempt was reported in the paroxetine group in the 24-week study, but was determined by investigators to be unrelated to treatment
- Incidence rates of gastrointestinal and other bleeding events were similar between groups
- Five bone fractures were reported: One in the paroxetine group and four among three participants in the placebo group.
One death occurred in the 12-week Phase 3 study due to acute respiratory failure with evidence of hypertension-mediated pulmonary edema and hypertensive cardiovascular disease. The investigator did not consider the death to be related to the study drug.
Study conclusion
The authors concluded that paroxetine 7.5 mg had favorable tolerability in menopausal women with moderate to severe VMS.
“Paroxetine 7.5 mg offers a nonhormonal treatment option for women who seek treatment for moderate to severe hot flashes associated with menopause,” said Dr. Simon.3
Tell us what you think! Send your Letter to the Editor: rbarbieri@frontlinemedcom.com
1. Simon JA, et al. Low dose paroxetine 7.5 mg for menopausal vasomotor symptoms: two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
2. Joffe H et al. Low-dose mesylate salt of paroxetine (LDMP) in treatment of vasomotor symptoms (VMS) in menopause. Presented at: 2012 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists; May 7, 2012; San Diego, CA. Poster 43.
3. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate to severe vasomotor symptoms. Poster presented at: 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG); April 26–30, 2014; Chicago, IL.
1. Simon JA, et al. Low dose paroxetine 7.5 mg for menopausal vasomotor symptoms: two randomized controlled trials. Menopause. 2013;20(10):1027–1035.
2. Joffe H et al. Low-dose mesylate salt of paroxetine (LDMP) in treatment of vasomotor symptoms (VMS) in menopause. Presented at: 2012 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists; May 7, 2012; San Diego, CA. Poster 43.
3. Simon JA, Portman DJ, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Safety profile of paroxetine 7.5 mg in women with moderate to severe vasomotor symptoms. Poster presented at: 2014 Annual Clinical Meeting of The American College of Obstetricians and Gynecologists (ACOG); April 26–30, 2014; Chicago, IL.
Gynecologic cancer patients treated at high-volume hospitals live longer
Women with gynecologic cancers live significantly longer if they’re cared for at hospitals that frequently treat such patients rather than at centers that infrequently care for them. This is according to results from a study of more than 860,000 women.1 The research, which used the National Cancer Database to identify gynecologic cancer cases, was presented at the 2014 Society of Gynecologic Oncology Annual Meeting on Women’s Cancer.
Results of the study
Overall, the median survival for women with all types of gynecologic cancer was 122.7 months at centers with the highest volume (nearly 300 such cases per year) compared with 110 months at the lowest-volume hospitals (<20 per year)—a difference of more than a year. The difference was even greater for cancers that are rare or require particularly complex treatment.
Patients with vaginal cancer, for example, had a median survival of 72.2 months at the highest-volume centers, compared with 38.1 months at the lowest-volume facilities—a difference of close to 3 years. For women with ovarian cancer, the difference in median survival was nearly 17 months (49.4 months for highest-volume versus 32.5 for lowest-volume).
The researchers analyzed data on 863,156 women treated for cervical, ovarian, uterine, vaginal, or vulvar cancer from 1998 to 2011. The patients received treatment at 1666 medical centers, which the researchers divided into quartiles based on the number of reproductive cancer cases treated annually.
Over the 13-year study period, the number of women with gynecologic cancer who received treatment at high-volume facilities rose steadily, said Jeff F. Lin, MD, lead author of the study and a physician in gynecologic oncology at Magee-Womens Hospital at the University of Pittsburgh Medical Center. This rise in treatment at high-volume centers did not benefit elderly patients and those with more advanced cancers, however, as these patients were more likely to receive treatment at lower-volume facilities.
Refer women to high-volume centers, say the authors
The research results did not explain why women treated at high-volume centers live longer, nor the reason more patients with gynecologic cancer are being treated at these facilities. Better coordination of care, better access to cutting-edge clinical trials, and greater likelihood of receiving care from gynecologic oncologists are possible reasons women treated at high-volume centers have better outcomes, said Dr. Lin. He added that, as gynecologic cancer care becomes more complex, physicians may feel more comfortable referring patients to high-volume centers and specialists. “Based on this and other studies, we should be trying to steer even more patients to high-volume hospitals,” he said.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. We will consider publishing your letter in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Reference
1. Women with gynecologic cancers may live longer when treated at high-volume medical centers [press release]. Chicago: Society of Gynecologic Oncology. March 24, 2014. https://www.sgo.org/newsroom/news-releases/women-with-gynecologic-cancers-may-live-longer-when-treated-at-high-volume-medical-centers/. Accessed May 19, 2014.
Women with gynecologic cancers live significantly longer if they’re cared for at hospitals that frequently treat such patients rather than at centers that infrequently care for them. This is according to results from a study of more than 860,000 women.1 The research, which used the National Cancer Database to identify gynecologic cancer cases, was presented at the 2014 Society of Gynecologic Oncology Annual Meeting on Women’s Cancer.
Results of the study
Overall, the median survival for women with all types of gynecologic cancer was 122.7 months at centers with the highest volume (nearly 300 such cases per year) compared with 110 months at the lowest-volume hospitals (<20 per year)—a difference of more than a year. The difference was even greater for cancers that are rare or require particularly complex treatment.
Patients with vaginal cancer, for example, had a median survival of 72.2 months at the highest-volume centers, compared with 38.1 months at the lowest-volume facilities—a difference of close to 3 years. For women with ovarian cancer, the difference in median survival was nearly 17 months (49.4 months for highest-volume versus 32.5 for lowest-volume).
The researchers analyzed data on 863,156 women treated for cervical, ovarian, uterine, vaginal, or vulvar cancer from 1998 to 2011. The patients received treatment at 1666 medical centers, which the researchers divided into quartiles based on the number of reproductive cancer cases treated annually.
Over the 13-year study period, the number of women with gynecologic cancer who received treatment at high-volume facilities rose steadily, said Jeff F. Lin, MD, lead author of the study and a physician in gynecologic oncology at Magee-Womens Hospital at the University of Pittsburgh Medical Center. This rise in treatment at high-volume centers did not benefit elderly patients and those with more advanced cancers, however, as these patients were more likely to receive treatment at lower-volume facilities.
Refer women to high-volume centers, say the authors
The research results did not explain why women treated at high-volume centers live longer, nor the reason more patients with gynecologic cancer are being treated at these facilities. Better coordination of care, better access to cutting-edge clinical trials, and greater likelihood of receiving care from gynecologic oncologists are possible reasons women treated at high-volume centers have better outcomes, said Dr. Lin. He added that, as gynecologic cancer care becomes more complex, physicians may feel more comfortable referring patients to high-volume centers and specialists. “Based on this and other studies, we should be trying to steer even more patients to high-volume hospitals,” he said.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. We will consider publishing your letter in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Women with gynecologic cancers live significantly longer if they’re cared for at hospitals that frequently treat such patients rather than at centers that infrequently care for them. This is according to results from a study of more than 860,000 women.1 The research, which used the National Cancer Database to identify gynecologic cancer cases, was presented at the 2014 Society of Gynecologic Oncology Annual Meeting on Women’s Cancer.
Results of the study
Overall, the median survival for women with all types of gynecologic cancer was 122.7 months at centers with the highest volume (nearly 300 such cases per year) compared with 110 months at the lowest-volume hospitals (<20 per year)—a difference of more than a year. The difference was even greater for cancers that are rare or require particularly complex treatment.
Patients with vaginal cancer, for example, had a median survival of 72.2 months at the highest-volume centers, compared with 38.1 months at the lowest-volume facilities—a difference of close to 3 years. For women with ovarian cancer, the difference in median survival was nearly 17 months (49.4 months for highest-volume versus 32.5 for lowest-volume).
The researchers analyzed data on 863,156 women treated for cervical, ovarian, uterine, vaginal, or vulvar cancer from 1998 to 2011. The patients received treatment at 1666 medical centers, which the researchers divided into quartiles based on the number of reproductive cancer cases treated annually.
Over the 13-year study period, the number of women with gynecologic cancer who received treatment at high-volume facilities rose steadily, said Jeff F. Lin, MD, lead author of the study and a physician in gynecologic oncology at Magee-Womens Hospital at the University of Pittsburgh Medical Center. This rise in treatment at high-volume centers did not benefit elderly patients and those with more advanced cancers, however, as these patients were more likely to receive treatment at lower-volume facilities.
Refer women to high-volume centers, say the authors
The research results did not explain why women treated at high-volume centers live longer, nor the reason more patients with gynecologic cancer are being treated at these facilities. Better coordination of care, better access to cutting-edge clinical trials, and greater likelihood of receiving care from gynecologic oncologists are possible reasons women treated at high-volume centers have better outcomes, said Dr. Lin. He added that, as gynecologic cancer care becomes more complex, physicians may feel more comfortable referring patients to high-volume centers and specialists. “Based on this and other studies, we should be trying to steer even more patients to high-volume hospitals,” he said.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. We will consider publishing your letter in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Reference
1. Women with gynecologic cancers may live longer when treated at high-volume medical centers [press release]. Chicago: Society of Gynecologic Oncology. March 24, 2014. https://www.sgo.org/newsroom/news-releases/women-with-gynecologic-cancers-may-live-longer-when-treated-at-high-volume-medical-centers/. Accessed May 19, 2014.
Reference
1. Women with gynecologic cancers may live longer when treated at high-volume medical centers [press release]. Chicago: Society of Gynecologic Oncology. March 24, 2014. https://www.sgo.org/newsroom/news-releases/women-with-gynecologic-cancers-may-live-longer-when-treated-at-high-volume-medical-centers/. Accessed May 19, 2014.
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
When 95 women from Wright-Patterson Air Force Base in Ohio were surveyed about their views of noninvasive prenatal testing (NIPT) versus invasive screening, more than 60% of respondents said they would choose NIPT or no invasive testing if ultrasound screening, a quad screen, or conventional first-trimester screening revealed an abnormality. One-third of respondents said they would likely undergo invasive testing if NIPT results were abnormal, and more than 50% of women in this group reported that the results might influence their decision to continue the pregnancy.
The survey results were presented as a poster at the 2014 American College of Obstetricians and Gynecologists (ACOG) annual clinical meeting in Chicago.1
All patients attended a group prenatal genetic counseling session led by a single provider in early pregnancy before completing the survey.
The military population surveyed in this study “as a whole is a little bit skewed in race and education,” said Jacqueline Vidosh, MD, a coauthor of the study. That population was predominantly white, with the majority of women having completed at least some college.”
“The nice thing about a military population, however, is that you capture geographical differences, which is a lot harder to do on a small scale,” said Dr. Vidosh.
Andrea Shields, MD, provided the genetic counseling education for the study.
“My class lasted anywhere from 75 minutes to about 90 minutes,” she said, “so it was a considerable time that we took, but it wasn’t specifically devoted to NIPT. That portion took about 10 minutes. But it was introducing them to prenatal diagnosis and screening that took a while, so I think there has to be a large focus on education for any type of prenatal test. Pretest education is extremely important, especially when we’re trying to introduce this technology.”
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Shields A, Vidosh J. Average-risk pregnant patient perspectives on noninvasive prenatal testing. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
When 95 women from Wright-Patterson Air Force Base in Ohio were surveyed about their views of noninvasive prenatal testing (NIPT) versus invasive screening, more than 60% of respondents said they would choose NIPT or no invasive testing if ultrasound screening, a quad screen, or conventional first-trimester screening revealed an abnormality. One-third of respondents said they would likely undergo invasive testing if NIPT results were abnormal, and more than 50% of women in this group reported that the results might influence their decision to continue the pregnancy.
The survey results were presented as a poster at the 2014 American College of Obstetricians and Gynecologists (ACOG) annual clinical meeting in Chicago.1
All patients attended a group prenatal genetic counseling session led by a single provider in early pregnancy before completing the survey.
The military population surveyed in this study “as a whole is a little bit skewed in race and education,” said Jacqueline Vidosh, MD, a coauthor of the study. That population was predominantly white, with the majority of women having completed at least some college.”
“The nice thing about a military population, however, is that you capture geographical differences, which is a lot harder to do on a small scale,” said Dr. Vidosh.
Andrea Shields, MD, provided the genetic counseling education for the study.
“My class lasted anywhere from 75 minutes to about 90 minutes,” she said, “so it was a considerable time that we took, but it wasn’t specifically devoted to NIPT. That portion took about 10 minutes. But it was introducing them to prenatal diagnosis and screening that took a while, so I think there has to be a large focus on education for any type of prenatal test. Pretest education is extremely important, especially when we’re trying to introduce this technology.”
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
When 95 women from Wright-Patterson Air Force Base in Ohio were surveyed about their views of noninvasive prenatal testing (NIPT) versus invasive screening, more than 60% of respondents said they would choose NIPT or no invasive testing if ultrasound screening, a quad screen, or conventional first-trimester screening revealed an abnormality. One-third of respondents said they would likely undergo invasive testing if NIPT results were abnormal, and more than 50% of women in this group reported that the results might influence their decision to continue the pregnancy.
The survey results were presented as a poster at the 2014 American College of Obstetricians and Gynecologists (ACOG) annual clinical meeting in Chicago.1
All patients attended a group prenatal genetic counseling session led by a single provider in early pregnancy before completing the survey.
The military population surveyed in this study “as a whole is a little bit skewed in race and education,” said Jacqueline Vidosh, MD, a coauthor of the study. That population was predominantly white, with the majority of women having completed at least some college.”
“The nice thing about a military population, however, is that you capture geographical differences, which is a lot harder to do on a small scale,” said Dr. Vidosh.
Andrea Shields, MD, provided the genetic counseling education for the study.
“My class lasted anywhere from 75 minutes to about 90 minutes,” she said, “so it was a considerable time that we took, but it wasn’t specifically devoted to NIPT. That portion took about 10 minutes. But it was introducing them to prenatal diagnosis and screening that took a while, so I think there has to be a large focus on education for any type of prenatal test. Pretest education is extremely important, especially when we’re trying to introduce this technology.”
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Shields A, Vidosh J. Average-risk pregnant patient perspectives on noninvasive prenatal testing. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
Reference
Shields A, Vidosh J. Average-risk pregnant patient perspectives on noninvasive prenatal testing. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
Delivery notes after shoulder dystocia often lack critical elements
Shoulder dystocia is a leading cause of litigation in obstetrics, and the delivery note is an indispensable tool in the defense of a case. When investigators from the University of Southern California analyzed 66 delivery notes to determine how many of 20 intrapartum elements were covered, they found that an average of 11 (58%) were documented. No note included all 20 element.
The study was presented as a poster at the 2014 American College of Obstetricians and Gynecologists annual clinical meeting in Chicago.1
The 20 elements and their frequency of documentation were:
- date – 96%
- time – 96%
- maneuvers used to achieve delivery – 91%
- order of maneuvers – 89%
- maternal gravidity and parity – 86%
- mode of delivery – 86%
- Apgar scores – 80%
- type of perineal laceration – 80%
- infant birth weight – 77%
- resident provider – 75%
- head-to-body interval – 58%
- cord gases – 53%
- attending provider – 46%
- whether episiotomy was performed – 39%
- application of gentle downward traction – 31%
- movement of the infant’s extremities after delivery – 30%
- which shoulder was anterior – 21%
- whether the patient was informed of the shoulder dystocia – 4%
- adequacy of maternal pelvis – 2%
- lack of fundal pressure – 1%.
Investigators recommended that providers implement use of a standard form to improve recording of critical elements.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Why it’s important to open the sexual health dialogue
Reference
Stohl HE, Granat A, Ouzounian J, Miller DA, Jaque J. Lack of comprehensiveness of delivery notes for shoulder dystocia. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
Shoulder dystocia is a leading cause of litigation in obstetrics, and the delivery note is an indispensable tool in the defense of a case. When investigators from the University of Southern California analyzed 66 delivery notes to determine how many of 20 intrapartum elements were covered, they found that an average of 11 (58%) were documented. No note included all 20 element.
The study was presented as a poster at the 2014 American College of Obstetricians and Gynecologists annual clinical meeting in Chicago.1
The 20 elements and their frequency of documentation were:
- date – 96%
- time – 96%
- maneuvers used to achieve delivery – 91%
- order of maneuvers – 89%
- maternal gravidity and parity – 86%
- mode of delivery – 86%
- Apgar scores – 80%
- type of perineal laceration – 80%
- infant birth weight – 77%
- resident provider – 75%
- head-to-body interval – 58%
- cord gases – 53%
- attending provider – 46%
- whether episiotomy was performed – 39%
- application of gentle downward traction – 31%
- movement of the infant’s extremities after delivery – 30%
- which shoulder was anterior – 21%
- whether the patient was informed of the shoulder dystocia – 4%
- adequacy of maternal pelvis – 2%
- lack of fundal pressure – 1%.
Investigators recommended that providers implement use of a standard form to improve recording of critical elements.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Why it’s important to open the sexual health dialogue
Shoulder dystocia is a leading cause of litigation in obstetrics, and the delivery note is an indispensable tool in the defense of a case. When investigators from the University of Southern California analyzed 66 delivery notes to determine how many of 20 intrapartum elements were covered, they found that an average of 11 (58%) were documented. No note included all 20 element.
The study was presented as a poster at the 2014 American College of Obstetricians and Gynecologists annual clinical meeting in Chicago.1
The 20 elements and their frequency of documentation were:
- date – 96%
- time – 96%
- maneuvers used to achieve delivery – 91%
- order of maneuvers – 89%
- maternal gravidity and parity – 86%
- mode of delivery – 86%
- Apgar scores – 80%
- type of perineal laceration – 80%
- infant birth weight – 77%
- resident provider – 75%
- head-to-body interval – 58%
- cord gases – 53%
- attending provider – 46%
- whether episiotomy was performed – 39%
- application of gentle downward traction – 31%
- movement of the infant’s extremities after delivery – 30%
- which shoulder was anterior – 21%
- whether the patient was informed of the shoulder dystocia – 4%
- adequacy of maternal pelvis – 2%
- lack of fundal pressure – 1%.
Investigators recommended that providers implement use of a standard form to improve recording of critical elements.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Why it’s important to open the sexual health dialogue
Reference
Stohl HE, Granat A, Ouzounian J, Miller DA, Jaque J. Lack of comprehensiveness of delivery notes for shoulder dystocia. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
Reference
Stohl HE, Granat A, Ouzounian J, Miller DA, Jaque J. Lack of comprehensiveness of delivery notes for shoulder dystocia. Poster presented at the 2014 ACOG Annual Clinical Meeting, April 28, 2014, in Chicago, Illinois.
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.