User login
Technology and the evolution of medical knowledge: What’s happening in the background
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
Electronic health records and the lost power of prose
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
“Don’t tell me the moon is shining; show me the glint of light on broken glass,” Anton Chekhov
In March 2006, four programmers turned entrepreneurs launched Twitter. This revolutionary tool experienced a monumental growth in scale over the next 10 years from a handful of users sharing a few thousand messages (known as “tweets”) each day to a global social network of over 300 million users valued at over $25 billion dollars. In fact, on Election Day 2016, Twitter was the No. 1 source of breaking news1, and it has been used as a launchpad for everything from social activism to national revolutions.
When Twitter was first conceived, it was designed to operate through wireless phone carriers’ SMS messaging functionality (aka “via text message”). SMS messages are limited to just 160 characters, so Twitter’s creators decided to restrict tweets to 140 characters, allowing 20 characters for a username. This decision created a necessity for communication efficiency that harks back to the days of the telegraph. From the liberal use of contractions and abbreviations to the tireless search for the shortest synonyms possible, Twitter users have employed countless techniques to enable them to say more with less. While clever and creative, this extreme verbal austerity has pervaded other media as well, becoming the hallmark literary style of the current generation.
Contemporaneous with the Twitter revolution, the medical field has allowed technology to dramatically change its style of communication as well, but in the opposite way. We have become far less efficient in our use of words, yet we seem to be doing a really poor job of expressing ourselves.
Saying less with more
I was once asked to provide expert testimony in a medical malpractice lawsuit. Working in support of the defense, I endured question after question from the plaintiff’s legal team as they picked apart every aspect of the case. Of particular interest was the physician’s documentation. Sadly – yet perhaps unsurprisingly – it was poor. The defendant had clearly used an EHR template and clicked checkboxes to create his note, documenting history, physical exam, assessment, and plan without having typed a single word. While adequate for billing purposes, the note was missing any narrative that could communicate the story of what had transpired during the patient’s visit. Sure, the presenting symptoms and vital signs were there, but the no description of the patient’s appearance had been recorded? What had the physician been thinking? What unspoken messages had led the physician to make the decisions he had made?
Like Twitter, the dawn of EHRs created an entirely new form of communication, but instead of limiting the content of physicians’ notes it expanded it. Objectively, this has made for more complete notes. Subjectively, this has led to notes packed with data, yet devoid of meaningful narrative. While handwritten notes from the previous generation were brief, they included the most important elements of the patient’s history and often the physician’s thought process in forming the differential. The electronically generated notes of today are quite the opposite; they are dense, yet far from illuminating. A clinician referring back to the record might have tremendous difficulty discerning salient features amidst all of the “note bloat.”This puts the patient (and the provider, as in the case above) at risk. Details may be present, but the diagnosis will be missed without the story that ties them all together.
Writing a new chapter
Physicians hoping to create meaningful notes are often stymied by the technology at their disposal or the demands placed on their time. These issues, combined with an ever-growing number of regulatory requirements, are what led to the decay of narrative in the first place. As a result, doctors are looking for alternative ways to buck the trend and bring patients’ stories back to their medical records. These methods are often expensive or involved, but in many cases they dramatically improve quality and efficiency.
An example of a tool that allows doctors to achieve these goals is speech recognition technology. Instead of typing or clicking, physicians dictate into the EHR, creating notes that are typically richer and more akin to a story than a list of symptoms or data points. When voice-to-text is properly deployed and utilized, documentation improves along with efficiency. Alternately, many providers are now employing scribes to accompany them in the exam room and complete the medical record. Taking this step leads to more descriptive notes, better productivity, and happier providers. The use of scribes also seems to result in happier patients, who report better therapeutic interactions when their doctors aren’t typing or staring at a computer screen.
The above-mentioned methods for recording information about a patient during a visit may be too expensive or complicated for some providers, but there are other simple techniques that can be used without incurring additional cost or resources. Previsit planning is one such possibility. By reviewing patient charts in advance of appointments, physicians can look over results, identify preventive health gaps, and anticipate follow-up needs and medication refills. They can then create skeleton notes and prepopulate orders to reduce the documentation burden during the visit. While time consuming at first, physicians have reported this practice actually saves time in the long run and allows them to focus on recording the patient narrative during the visit.
Another strategy is even more simple in concept, though may seem counter-intuitive at first: get better acquainted with the electronic records system. That is, take the time to really learn and understand the tools designed to improve productivity that are available in your EHR, then use them judiciously; take advantage of templates and macros when they’ll make you more efficient yet won’t inhibit your ability to tell the patient’s story; embrace optimization but don’t compromise on narrative. By carefully choosing your words, you’ll paint a clearer picture of every patient and enable safer and more personalized care.
Reference
1. “For Election Day Influence, Twitter Ruled Social Media” New York Times. Nov. 8, 2016.
Who is in charge here?
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at info@ehrpc.com.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at info@ehrpc.com.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at info@ehrpc.com.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
Breaking down blockchain: How this novel technology will unfetter health care
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
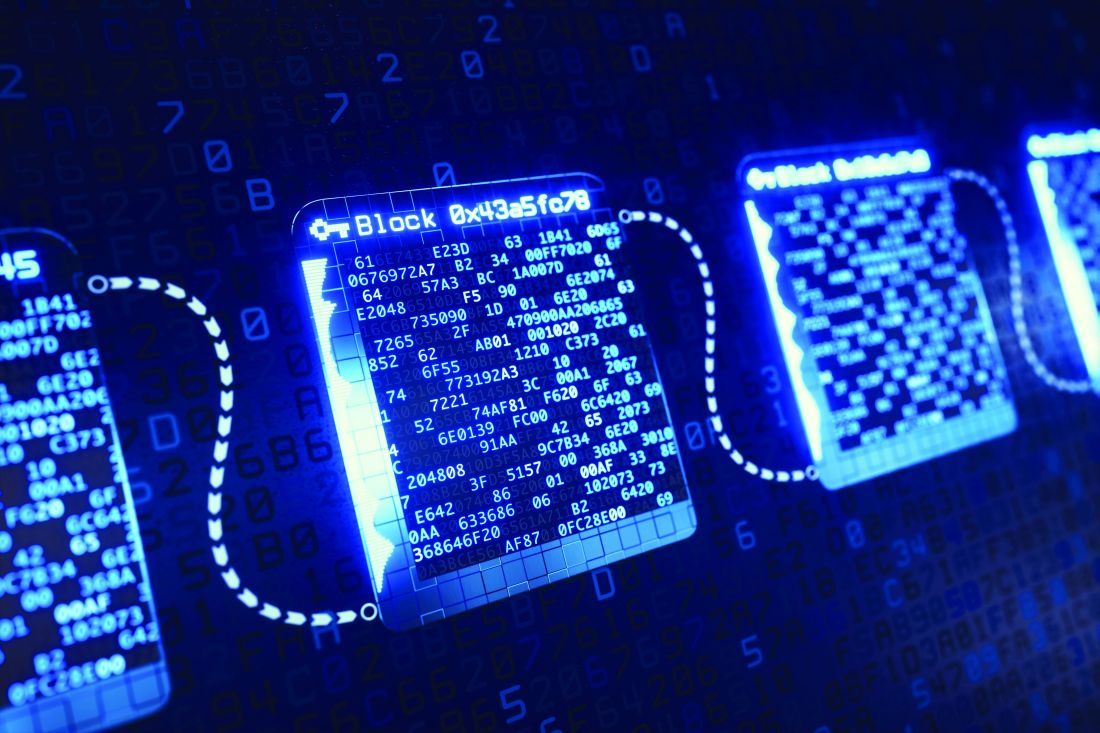
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
One evening in 2016, my 9-year-old son suggested we use Bitcoin to purchase something on the Microsoft Xbox store. Surprised by his suggestion, I was suddenly struck with two thoughts: 1) Microsoft, by accepting Bitcoin, was validating cryptocurrency as a credible form of payment, and 2) I was getting old. My 9-year-old seemed to have a better understanding of a new technology than I did, hardly the first time – or the last time – that happened. In spite of my initial feelings of defeat, I resolved not to cede victory to my son without a fight. I immediately set out to understand cryptocurrencies and, more importantly, the technology underpinning them known as blockchain.
Even just a few years ago, my ignorance of how blockchains work may have been acceptable, but it hardly seems acceptable now. Much more than just cryptocurrency, blockchain technology is beginning to affect every industry that values information sharing and security, and it is about to usher in a revolution in health care. But what are blockchains, and why are they so important?
Explaining blockchains
Blockchains were first conceptualized almost 3 decades ago, but the invention of the first blockchain as we know it today occurred in 2008 by Satoshi Nakomoto, creator of Bitcoin. Blockchains can be thought of as a way to store and communicate information while ensuring its integrity and security. Admittedly, the technology can be a bit confusing, but we’ll attempt to simplify it by focusing on a few fundamental elements.
As the name indicates, the blockchain model relies on a chain of connected blocks. Each block contains some data (which can be financial, medical, legal, or anything else) and bears a unique fingerprint known as a “hash.” Each hash is different and depends entirely on the data stored in the block. In other words, if the contents of the block change, the hash changes, creating an entirely new fingerprint. Each block on the chain also keeps a record of the hash of the previous block. This “links” the chain together, and is the first key to its robust security: If any block is tampered with, its fingerprint will change and it will no longer be linked, thus invalidating all following blocks on the chain.
Ensuring the integrity of the blockchain doesn’t stop there. Just as actual fingerprints can be spoofed by enterprising criminals, hash technology isn’t enough to provide complete security. Thus, several other security features are built into blockchains, with the most noteworthy and important being “decentralization.” This means that blockchains are not stored on any single computer. On the contrary, duplicate copies of every blockchain exist on thousands of computers around the world, creating redundancy and minimizing the vulnerability that any single chain could be tampered with. Before any change in the blockchain can be made and accepted, it must be validated by a majority of the computers storing the chain.
If this all seems perplexing, that’s because it is. Blockchains are complex and difficult to visualize. (But if you’d like a deeper understanding, there are many great YouTube videos that do a great job explaining them.) For now, just remember this: Blockchains are very secure yet highly accessible, and will be essential to how data – especially health data – are stored and communicated in the future.
Blockchains in health care
On Jan. 24, 2019, five major companies (Aetna, Anthem, Health Care Services, IBM, and PNC Bank) “announced a new collaboration to design and create a network using blockchain technology to improve transparency and interoperability in the health care industry.”1 This team of industry leaders is hoping to build the engine that will power the future and impact how health records are created, maintained, and communicated. They’ll achieve this by taking advantage of blockchain’s inclusiveness and decentralization, storing records in a manner that is safe and accessible anywhere a patient seeks care. Because of the redundancy built into blockchains, they can also ensure data integrity. Physicians will benefit from information that is easy to obtain and always accurate; patients will benefit by gaining greater access and ownership of their personal medical records.
The collaboration mentioned above is the latest, but certainly not the first, attempt to exploit the benefits of blockchain for health care. Other major players have already entered the game, and the field is growing quickly. While it’s easy to find their efforts admirable, corporate involvement also means there is money to be saved or made in the space. Chris Ward, head of product for PNC Treasury Management, alluded to this as he commented publicly in the press release: “This collaboration will enable health care–related data and business transactions to occur in way that addresses market demands for transparency and security, while making it easier for the patient, payer, and provider to handle payments. Using this technology, we can remove friction, duplication, and administrative costs that continue to plague the industry.”
Industry executives recognize that interoperability is still the greatest challenge facing the future of health care and are particularly sensitive to the costs of not facing the challenge successfully. Clearly, they see an investment in blockchains as an opportunity to be part of a financially beneficial solution.
Why we should care
As we’ve now covered, there are many advantages of blockchain technology. In fact, we see it as the natural evolution of the patient-centered EHR. Instead of siloed and proprietary information spread across disparate EHRs that can’t communicate, the future of data exchange will be more transparent, yet more secure. Blockchain represents a unique opportunity to democratize the availability of health care information while increasing information quality and lowering costs. It is also shaping up to be the way we’ll exchange sensitive data in the future.
Don’t believe us? Just ask any 9-year-old.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on Twitter, @doctornotte. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
Reference
1. https://newsroom.ibm.com/2019-01-24-Aetna-Anthem-Health-Care-Service-Corporation-PNC-Bank-and-IBM-announce-collaboration-to-establish-blockchain-based-ecosystem-for-the-healthcare-industry
Martin Buber, deep learning, and the still soft voice beyond the screen
Life is short, art long, opportunity fleeting. – Hippocrates
The new year provides an opportunity to reflect on old things: to decide what to keep and what to toss out, to contemplate the habits to which we choose to rededicate ourselves, and those we choose to let wane. Over the last few years, while some older physicians have expressed a yearning for the comfort of paper charts, most of us have come to embrace the benefits of the electronic health record. That is a good thing. The EHR offers many advantages over paper, and, like it or not, it’s here to stay.
The other day I was working with a resident, admitting a patient to a nursing home. I handed her the inch-thick stack of papers that came from the hospital, and she immediately asked what we were supposed to do with it. When I explained that it was the hospital chart, she wondered aloud how she was supposed to navigate to the different sections in order to review the information. I was stupefied but understood the reason behind her question. The way we document has changed so dramatically over just the past decade. Unfortunately, without intention, the way that we chart has affected the way we relate to patients.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other person for all their complexity, in their full humanness. We acknowledge and approach the person as a unique individual who has dreams, goals, fears, and wishes that may be different than ours but to which we can still relate.
While the importance and benefits of the electronic record are clear, we must constantly remind ourselves that the EHR is a tool of care and not the goal of care. While the people we see have health needs that must be diagnosed, treated, and recorded, and their illnesses are an important part of their being, they do not define their being. Nor should they define our relationship with them. Patients agree; when surveyed about the attributes of a good physician, they regularly respond that they want their physicians to have a sense of them as people, not just patients.
Recently, I was reminded of the challenge of keeping this simple task in the forefront of care while on hospital service. I had occasion to sit and talk with one of my patients without a computer in the room. This was unusual for me, as I typically fill out the EHR as I am seeing the patient. As I listened to the individual in his gown, lying on his hospital bed and describing the symptoms that brought him to the hospital, I was reminded of the subtle pauses and nuances that occur during focused conversations, during deep listening.
We have written in previous columns about exciting applications of technology that are in the pipeline. Artificial intelligence with “deep learning” is predicted to change the way we diagnose and treat disease. Deep learning is a term that has been used to describe a type of machine analysis where data are interpreted and analyzed in layers, allowing the computer to detect patterns. In the first layer of learning, the computer may identify the way pixels of the same color form a line or a curve. In the next layer it might detect the way that curve resembles a face. Peeling away layer after layer, the computer might eventually recognize whose face is being represented. This is the type of programing that has allowed computers to interpret mammograms and retina scans, detecting patterns that represent cancer or small retinal hemorrhages. While deep learning will be the subject of much excitement over the next few years, at the start of this new year we think it is equally important be reminded of an essential quality of the excellent physician – deep listening.
Deep listening requires a lifetime of practice. We have all experienced it, both as listeners and as those being listened to. When we are in the presence of someone who is truly interested in what we are saying – in our story and in our life – we feel reaffirmed and refreshed. Regardless of the topic of our discussion, we feel a sense of trust, for we believe that the person with whom we are speaking understands us, and, in that understanding, cares about us. We have a sense that we could trust the listener with our lives.
A lifetime of practice – that is the promise of our jobs as physicians. Every time we enter the exam room we have the opportunity to carry out the sacred skill of hearing others, while trying in some way to improve their lives. With each visit we have the opportunity to perfect our craft. Chaucer, the medieval English poet, observed, “the life so short, the craft so long to learn.” It seems he borrowed that idea from a physician, Hippocrates.
Hippocrates opened his medical text with the words, “Vita brevis, ars longa, occasio praeceps,” which means, “Life is short, the art long, opportunity fleeting.” Hippocrates recognized the challenge involved in learning all that is necessary to take care of our fellow man. This challenge has only become more difficult as the quantity of information required to practice competent medicine has increased. In addition, we now need to record data into the EHR to be used for record keeping, billing, and the further advancement of knowledge. Hippocrates’ medical text continued, “The physician must not only be prepared to do what is right himself, but also to make the patient, the attendants, and externals cooperate.”
On the occasion of this New Year, it is a perfect time to reflect and rededicate ourselves to listening to our patients, to being interested in them and their stories. We just may find that in deep listening, and in the trust that comes from that singular focus, lie solutions to many of the largest problems we face in medicine today: burnout, poor adherence, and regaining the moral authority that comes with truly caring for those in need.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter (@doctornotte).
Life is short, art long, opportunity fleeting. – Hippocrates
The new year provides an opportunity to reflect on old things: to decide what to keep and what to toss out, to contemplate the habits to which we choose to rededicate ourselves, and those we choose to let wane. Over the last few years, while some older physicians have expressed a yearning for the comfort of paper charts, most of us have come to embrace the benefits of the electronic health record. That is a good thing. The EHR offers many advantages over paper, and, like it or not, it’s here to stay.
The other day I was working with a resident, admitting a patient to a nursing home. I handed her the inch-thick stack of papers that came from the hospital, and she immediately asked what we were supposed to do with it. When I explained that it was the hospital chart, she wondered aloud how she was supposed to navigate to the different sections in order to review the information. I was stupefied but understood the reason behind her question. The way we document has changed so dramatically over just the past decade. Unfortunately, without intention, the way that we chart has affected the way we relate to patients.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other person for all their complexity, in their full humanness. We acknowledge and approach the person as a unique individual who has dreams, goals, fears, and wishes that may be different than ours but to which we can still relate.
While the importance and benefits of the electronic record are clear, we must constantly remind ourselves that the EHR is a tool of care and not the goal of care. While the people we see have health needs that must be diagnosed, treated, and recorded, and their illnesses are an important part of their being, they do not define their being. Nor should they define our relationship with them. Patients agree; when surveyed about the attributes of a good physician, they regularly respond that they want their physicians to have a sense of them as people, not just patients.
Recently, I was reminded of the challenge of keeping this simple task in the forefront of care while on hospital service. I had occasion to sit and talk with one of my patients without a computer in the room. This was unusual for me, as I typically fill out the EHR as I am seeing the patient. As I listened to the individual in his gown, lying on his hospital bed and describing the symptoms that brought him to the hospital, I was reminded of the subtle pauses and nuances that occur during focused conversations, during deep listening.
We have written in previous columns about exciting applications of technology that are in the pipeline. Artificial intelligence with “deep learning” is predicted to change the way we diagnose and treat disease. Deep learning is a term that has been used to describe a type of machine analysis where data are interpreted and analyzed in layers, allowing the computer to detect patterns. In the first layer of learning, the computer may identify the way pixels of the same color form a line or a curve. In the next layer it might detect the way that curve resembles a face. Peeling away layer after layer, the computer might eventually recognize whose face is being represented. This is the type of programing that has allowed computers to interpret mammograms and retina scans, detecting patterns that represent cancer or small retinal hemorrhages. While deep learning will be the subject of much excitement over the next few years, at the start of this new year we think it is equally important be reminded of an essential quality of the excellent physician – deep listening.
Deep listening requires a lifetime of practice. We have all experienced it, both as listeners and as those being listened to. When we are in the presence of someone who is truly interested in what we are saying – in our story and in our life – we feel reaffirmed and refreshed. Regardless of the topic of our discussion, we feel a sense of trust, for we believe that the person with whom we are speaking understands us, and, in that understanding, cares about us. We have a sense that we could trust the listener with our lives.
A lifetime of practice – that is the promise of our jobs as physicians. Every time we enter the exam room we have the opportunity to carry out the sacred skill of hearing others, while trying in some way to improve their lives. With each visit we have the opportunity to perfect our craft. Chaucer, the medieval English poet, observed, “the life so short, the craft so long to learn.” It seems he borrowed that idea from a physician, Hippocrates.
Hippocrates opened his medical text with the words, “Vita brevis, ars longa, occasio praeceps,” which means, “Life is short, the art long, opportunity fleeting.” Hippocrates recognized the challenge involved in learning all that is necessary to take care of our fellow man. This challenge has only become more difficult as the quantity of information required to practice competent medicine has increased. In addition, we now need to record data into the EHR to be used for record keeping, billing, and the further advancement of knowledge. Hippocrates’ medical text continued, “The physician must not only be prepared to do what is right himself, but also to make the patient, the attendants, and externals cooperate.”
On the occasion of this New Year, it is a perfect time to reflect and rededicate ourselves to listening to our patients, to being interested in them and their stories. We just may find that in deep listening, and in the trust that comes from that singular focus, lie solutions to many of the largest problems we face in medicine today: burnout, poor adherence, and regaining the moral authority that comes with truly caring for those in need.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter (@doctornotte).
Life is short, art long, opportunity fleeting. – Hippocrates
The new year provides an opportunity to reflect on old things: to decide what to keep and what to toss out, to contemplate the habits to which we choose to rededicate ourselves, and those we choose to let wane. Over the last few years, while some older physicians have expressed a yearning for the comfort of paper charts, most of us have come to embrace the benefits of the electronic health record. That is a good thing. The EHR offers many advantages over paper, and, like it or not, it’s here to stay.
The other day I was working with a resident, admitting a patient to a nursing home. I handed her the inch-thick stack of papers that came from the hospital, and she immediately asked what we were supposed to do with it. When I explained that it was the hospital chart, she wondered aloud how she was supposed to navigate to the different sections in order to review the information. I was stupefied but understood the reason behind her question. The way we document has changed so dramatically over just the past decade. Unfortunately, without intention, the way that we chart has affected the way we relate to patients.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other person for all their complexity, in their full humanness. We acknowledge and approach the person as a unique individual who has dreams, goals, fears, and wishes that may be different than ours but to which we can still relate.
While the importance and benefits of the electronic record are clear, we must constantly remind ourselves that the EHR is a tool of care and not the goal of care. While the people we see have health needs that must be diagnosed, treated, and recorded, and their illnesses are an important part of their being, they do not define their being. Nor should they define our relationship with them. Patients agree; when surveyed about the attributes of a good physician, they regularly respond that they want their physicians to have a sense of them as people, not just patients.
Recently, I was reminded of the challenge of keeping this simple task in the forefront of care while on hospital service. I had occasion to sit and talk with one of my patients without a computer in the room. This was unusual for me, as I typically fill out the EHR as I am seeing the patient. As I listened to the individual in his gown, lying on his hospital bed and describing the symptoms that brought him to the hospital, I was reminded of the subtle pauses and nuances that occur during focused conversations, during deep listening.
We have written in previous columns about exciting applications of technology that are in the pipeline. Artificial intelligence with “deep learning” is predicted to change the way we diagnose and treat disease. Deep learning is a term that has been used to describe a type of machine analysis where data are interpreted and analyzed in layers, allowing the computer to detect patterns. In the first layer of learning, the computer may identify the way pixels of the same color form a line or a curve. In the next layer it might detect the way that curve resembles a face. Peeling away layer after layer, the computer might eventually recognize whose face is being represented. This is the type of programing that has allowed computers to interpret mammograms and retina scans, detecting patterns that represent cancer or small retinal hemorrhages. While deep learning will be the subject of much excitement over the next few years, at the start of this new year we think it is equally important be reminded of an essential quality of the excellent physician – deep listening.
Deep listening requires a lifetime of practice. We have all experienced it, both as listeners and as those being listened to. When we are in the presence of someone who is truly interested in what we are saying – in our story and in our life – we feel reaffirmed and refreshed. Regardless of the topic of our discussion, we feel a sense of trust, for we believe that the person with whom we are speaking understands us, and, in that understanding, cares about us. We have a sense that we could trust the listener with our lives.
A lifetime of practice – that is the promise of our jobs as physicians. Every time we enter the exam room we have the opportunity to carry out the sacred skill of hearing others, while trying in some way to improve their lives. With each visit we have the opportunity to perfect our craft. Chaucer, the medieval English poet, observed, “the life so short, the craft so long to learn.” It seems he borrowed that idea from a physician, Hippocrates.
Hippocrates opened his medical text with the words, “Vita brevis, ars longa, occasio praeceps,” which means, “Life is short, the art long, opportunity fleeting.” Hippocrates recognized the challenge involved in learning all that is necessary to take care of our fellow man. This challenge has only become more difficult as the quantity of information required to practice competent medicine has increased. In addition, we now need to record data into the EHR to be used for record keeping, billing, and the further advancement of knowledge. Hippocrates’ medical text continued, “The physician must not only be prepared to do what is right himself, but also to make the patient, the attendants, and externals cooperate.”
On the occasion of this New Year, it is a perfect time to reflect and rededicate ourselves to listening to our patients, to being interested in them and their stories. We just may find that in deep listening, and in the trust that comes from that singular focus, lie solutions to many of the largest problems we face in medicine today: burnout, poor adherence, and regaining the moral authority that comes with truly caring for those in need.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter (@doctornotte).
Where to go with wearables
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
On Sept. 14 of this year, Apple executives took to the stage to tout the incredible benefits of their new Apple Watch Series 4. While impressively presented in typical Apple fashion, the watch appeared to be only an evolution – not a revolution – in wearable technology. Still, there were a few noteworthy aspects of the new model that seemed to shine a light on the direction of the industry as a whole, and these were all focused on health care.
Like products from FitBit, Garmin, and others, the new Apple Watch can monitor a user’s heart rate and notify if it goes too high or too low. In addition, the watch now includes “fall detection,” and can automatically call for help if its wearer has taken a spill and become unresponsive. Soon it will even be capable of recording a single-lead ECG and detecting atrial fibrillation. While this all sounds fantastic, it also raises an important question in the minds of many physicians (including us): What do we do with all of these new data?
Findings from a Digital Health Study published by the American Medical Association in 20161 reveal that most doctors are aware of growing advances in Mobile Health (mHealth). Interestingly, however, while 85% see potential advantages in mHealth, less than 30% have begun employing it in their practices. This speaks to an adoption divide and highlights the many barriers to overcome before we can bridge it.
First and foremost, providers need confidence in the accuracy of the monitoring equipment, and, thus far, that accuracy has been questionable. Heart rate measurement, for example, is a staple of all currently available fitness wearables, yet is replete with technological pitfalls. This is because most consumer devices rely on optical sensors to measure heart rate. While inexpensive and noninvasive, the accuracy of these sensors can be affected by the interference of sweat, movement, and even the patient’s skin conditions – so much so that FitBit is currently embroiled in a class action lawsuit2 over the issue, in spite of providing disclaimers that a FitBit is “not a medical device.” To improve heart-monitoring capability, Apple has changed to a new sensor technology for this latest generation of Apple Watch. So far its accuracy has yet to be proven, and Apple’s delay in releasing the ECG features until “later this year” suggests there may still be bugs to work out.
Another significant concern raised by the onslaught of wearable health data is how to incorporate it into the electronic health record. Physicians care about efficient data integration, and, when asked in the aforementioned AMA study, physicians named this as their No. 1 functional requirement. EHR vendors have made some strides to allow patients to upload monitoring data directly through an online portal, but the large variety of available consumer devices has made standardizing this process difficult. Doctors have also made it clear that they want it to be straightforward to access and use the information provided by patients, and don’t want it to require special training. These are considerable challenges that will require collaboration between EHR vendors and wearable manufacturers to solve.
The introduction of additional players into the health care space also evokes questions of who owns this new health data set, and who is accountable for its integrity. If history is any indicator, device manufacturers will try their best to eschew any liability, and shift culpability onto patients and physicians. This is causing malpractice insurers to rethink policy coverage and forcing doctors to face a new reality of having “too much information.” While we are excited about the potential for better access to patient monitoring data, we agree that physicians need to understand where their responsibility for these data begins and ends.
Likewise, patients need to understand who has access to their personal health information, and how it’s being used. Privacy concerns will only become more evident as our society becomes ever more connected and as technologies become more invasive. The term “wearable” may soon become antiquated, as more products are coming to market that cross the skin barrier to collect samples directly from the blood or interstitial fluid. Devices such as Abbott’s new FreeStyle Libre continuous blood glucose monitor can be worn for weeks at a time, with its tiny sensor placed just under the skin. It constantly monitors trends in blood sugar and produces enough data points to determine the eating, sleeping, and activity habits of its wearer. This is all uploadable to Abbott’s servers, allowing patients and their providers to review it, thereby further expanding their personal health information footprint.
One encouraging aspect of the expansion mobile health technology is its organic, patient-led adoption. This is quite different from the epoch of electronic health records, which was motivated largely by government financial incentives and resulted in expensive, inefficient software. Patients are expressing a greater desire to take ownership of their health and have a growing interest in personal fitness. Also, the size of the consumer marketplace is forcing vendors to create competitive, high-value, and user-friendly mHealth devices. These products may seem to offer endless possibilities, but patients, vendors, and providers must fully acknowledge existing limitations in order to truly spark a revolution in wearable technology and actually improve patient care.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
References
1. Digital Health Study: Physicians’ motivations and requirements for adopting digital clinical tools. (2016) American Medical Association.
2. Kate Mclellan et al. v. Fitbit Inc. Fitbit Heart Rate Monitors Fraud & Defects Lawsuit.
Real-world data, machine learning, and the reemergence of humanism
As we relentlessly enter information into our EHRs, we typically perceive that we are just recording information about our patients to provide continuity of care and have an accurate representation of what was done. While that is true, the information we record is now increasingly being examined for many additional purposes. A whole new area of study has emerged over the last few years known as “real-world data,” and innovators are beginning to explore how machine learning (currently employed in other areas by such companies as Amazon and Google) may be used to improve the care of patients. The information we are putting into our EHRs is being translated into discrete data and is then combined with data from labs, pharmacies, and claims databases to examine how medications actually work when used in the wide and wild world of practice.
Let’s first talk about why real-world data are important. Traditionally, the evidence we rely upon in medicine has come from randomized trials to give us an unbiased assessment about the safety and the efficacy of the medications that we use. The Achilles’ heel of randomized trials is that, by their nature, they employ a carefully defined group of patients – with specific inclusion and exclusion criteria – who may not be like the patients in our practices. Randomized trials are also conducted in sites that are different than most of our offices. The clinics where randomized trials are conducted have dedicated personnel to follow up on patients, to make sure that patients take their medications, and ensure that patients remember their follow up visits. What this means is that the results in of those studies might not reflect the results seen in the real world.
A nice example of this was reported recently in the area of diabetes management. Randomized trials have shown that the glucagonlike peptide–1 (GLP-1) class of medications have about twice the effectiveness in lowering hemoglobin A1c as do the dipeptidyl peptidase–4 (DPP-4) inhibitor class of medications, but that difference in efficacy is not seen in practice. When looked at in real-world studies, the two classes of medications have about the same glucose-lowering efficacy. Why might that be? In reality, it might be that compliance with GLP-1s is less than that of DPP-4s because of the side effects of nausea and GI intolerance. When patients miss more doses of their GLP-1, they do not achieve the HbA1c lowering seen in trials in which compliance is far better.1
This exploration of real-world outcomes is just a first step in using the information documented in our charts. The exciting next step will be machine learning, also called deep learning.2 In this process, computers look at an enormous number of data points and find relationships that would otherwise not be detected. Imagine a supercomputer analyzing every blood pressure after any medication is changed across thousands, or even millions, of patients, and linking the outcome of that medication choice with the next blood pressure.3 Then imagine the computer meshing millions of data points that include all patients’ weights, ages, sexes, family histories of cardiovascular disease, renal function, etc. and matching those parameters with the specific medication and follow-up blood pressures. While much has been discussed about using genetics to advance personalized medicine, one can imagine these machine-based algorithms discovering connections about which medications work best for individuals with specific characteristics – without the need for additional testing. When the final loop of this cascade is connected, the computer could present recommendations to the clinician about which medication is optimal for the patient and then refine these recommendations, based on outcomes, to optimize safety and efficacy.
Some have argued that there is no way a computer will be able to perform as well as an experienced clinician who utilizes a combination of data and intuition to choose the best medication for his or her patient. This argument is similar to the controversy over autonomous driving cars. Many have asked how you can be assured that the cars will never have an accident. That is, of course, the wrong question. The correct question, as articulated very nicely by one of the innovators in that field, George Holtz, is how we can make a car that is safer than the way that cars are currently being driven (which means fewer deaths than the 15,000 that occur annually with humans behind the wheel).4
Our current method of providing care often leaves patients without appropriate guideline-recommended medications, and many don’t reach their HbA1c, blood pressure, cholesterol, and asthma-control goals. The era of machine learning with machine-generated algorithms may be much closer than we think, which will allow us to spend more time talking with patients, educating them about their disease, and supporting them in their efforts to remain healthy – an attractive future for both us and our patients.
References
1. Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017 Nov;40(11):1469-78.
2. Naylor CD. On the prospects for a (deep) learning health care system. JAMA. 2018 Sep 18;320(11):1099-100.
3. Wang YR et al. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007 Jan 22;167(2):141-7.
4. Super Hacker George Hotz: “I can make your car drive itself for under $1,000.”
As we relentlessly enter information into our EHRs, we typically perceive that we are just recording information about our patients to provide continuity of care and have an accurate representation of what was done. While that is true, the information we record is now increasingly being examined for many additional purposes. A whole new area of study has emerged over the last few years known as “real-world data,” and innovators are beginning to explore how machine learning (currently employed in other areas by such companies as Amazon and Google) may be used to improve the care of patients. The information we are putting into our EHRs is being translated into discrete data and is then combined with data from labs, pharmacies, and claims databases to examine how medications actually work when used in the wide and wild world of practice.
Let’s first talk about why real-world data are important. Traditionally, the evidence we rely upon in medicine has come from randomized trials to give us an unbiased assessment about the safety and the efficacy of the medications that we use. The Achilles’ heel of randomized trials is that, by their nature, they employ a carefully defined group of patients – with specific inclusion and exclusion criteria – who may not be like the patients in our practices. Randomized trials are also conducted in sites that are different than most of our offices. The clinics where randomized trials are conducted have dedicated personnel to follow up on patients, to make sure that patients take their medications, and ensure that patients remember their follow up visits. What this means is that the results in of those studies might not reflect the results seen in the real world.
A nice example of this was reported recently in the area of diabetes management. Randomized trials have shown that the glucagonlike peptide–1 (GLP-1) class of medications have about twice the effectiveness in lowering hemoglobin A1c as do the dipeptidyl peptidase–4 (DPP-4) inhibitor class of medications, but that difference in efficacy is not seen in practice. When looked at in real-world studies, the two classes of medications have about the same glucose-lowering efficacy. Why might that be? In reality, it might be that compliance with GLP-1s is less than that of DPP-4s because of the side effects of nausea and GI intolerance. When patients miss more doses of their GLP-1, they do not achieve the HbA1c lowering seen in trials in which compliance is far better.1
This exploration of real-world outcomes is just a first step in using the information documented in our charts. The exciting next step will be machine learning, also called deep learning.2 In this process, computers look at an enormous number of data points and find relationships that would otherwise not be detected. Imagine a supercomputer analyzing every blood pressure after any medication is changed across thousands, or even millions, of patients, and linking the outcome of that medication choice with the next blood pressure.3 Then imagine the computer meshing millions of data points that include all patients’ weights, ages, sexes, family histories of cardiovascular disease, renal function, etc. and matching those parameters with the specific medication and follow-up blood pressures. While much has been discussed about using genetics to advance personalized medicine, one can imagine these machine-based algorithms discovering connections about which medications work best for individuals with specific characteristics – without the need for additional testing. When the final loop of this cascade is connected, the computer could present recommendations to the clinician about which medication is optimal for the patient and then refine these recommendations, based on outcomes, to optimize safety and efficacy.
Some have argued that there is no way a computer will be able to perform as well as an experienced clinician who utilizes a combination of data and intuition to choose the best medication for his or her patient. This argument is similar to the controversy over autonomous driving cars. Many have asked how you can be assured that the cars will never have an accident. That is, of course, the wrong question. The correct question, as articulated very nicely by one of the innovators in that field, George Holtz, is how we can make a car that is safer than the way that cars are currently being driven (which means fewer deaths than the 15,000 that occur annually with humans behind the wheel).4
Our current method of providing care often leaves patients without appropriate guideline-recommended medications, and many don’t reach their HbA1c, blood pressure, cholesterol, and asthma-control goals. The era of machine learning with machine-generated algorithms may be much closer than we think, which will allow us to spend more time talking with patients, educating them about their disease, and supporting them in their efforts to remain healthy – an attractive future for both us and our patients.
References
1. Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017 Nov;40(11):1469-78.
2. Naylor CD. On the prospects for a (deep) learning health care system. JAMA. 2018 Sep 18;320(11):1099-100.
3. Wang YR et al. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007 Jan 22;167(2):141-7.
4. Super Hacker George Hotz: “I can make your car drive itself for under $1,000.”
As we relentlessly enter information into our EHRs, we typically perceive that we are just recording information about our patients to provide continuity of care and have an accurate representation of what was done. While that is true, the information we record is now increasingly being examined for many additional purposes. A whole new area of study has emerged over the last few years known as “real-world data,” and innovators are beginning to explore how machine learning (currently employed in other areas by such companies as Amazon and Google) may be used to improve the care of patients. The information we are putting into our EHRs is being translated into discrete data and is then combined with data from labs, pharmacies, and claims databases to examine how medications actually work when used in the wide and wild world of practice.
Let’s first talk about why real-world data are important. Traditionally, the evidence we rely upon in medicine has come from randomized trials to give us an unbiased assessment about the safety and the efficacy of the medications that we use. The Achilles’ heel of randomized trials is that, by their nature, they employ a carefully defined group of patients – with specific inclusion and exclusion criteria – who may not be like the patients in our practices. Randomized trials are also conducted in sites that are different than most of our offices. The clinics where randomized trials are conducted have dedicated personnel to follow up on patients, to make sure that patients take their medications, and ensure that patients remember their follow up visits. What this means is that the results in of those studies might not reflect the results seen in the real world.
A nice example of this was reported recently in the area of diabetes management. Randomized trials have shown that the glucagonlike peptide–1 (GLP-1) class of medications have about twice the effectiveness in lowering hemoglobin A1c as do the dipeptidyl peptidase–4 (DPP-4) inhibitor class of medications, but that difference in efficacy is not seen in practice. When looked at in real-world studies, the two classes of medications have about the same glucose-lowering efficacy. Why might that be? In reality, it might be that compliance with GLP-1s is less than that of DPP-4s because of the side effects of nausea and GI intolerance. When patients miss more doses of their GLP-1, they do not achieve the HbA1c lowering seen in trials in which compliance is far better.1
This exploration of real-world outcomes is just a first step in using the information documented in our charts. The exciting next step will be machine learning, also called deep learning.2 In this process, computers look at an enormous number of data points and find relationships that would otherwise not be detected. Imagine a supercomputer analyzing every blood pressure after any medication is changed across thousands, or even millions, of patients, and linking the outcome of that medication choice with the next blood pressure.3 Then imagine the computer meshing millions of data points that include all patients’ weights, ages, sexes, family histories of cardiovascular disease, renal function, etc. and matching those parameters with the specific medication and follow-up blood pressures. While much has been discussed about using genetics to advance personalized medicine, one can imagine these machine-based algorithms discovering connections about which medications work best for individuals with specific characteristics – without the need for additional testing. When the final loop of this cascade is connected, the computer could present recommendations to the clinician about which medication is optimal for the patient and then refine these recommendations, based on outcomes, to optimize safety and efficacy.
Some have argued that there is no way a computer will be able to perform as well as an experienced clinician who utilizes a combination of data and intuition to choose the best medication for his or her patient. This argument is similar to the controversy over autonomous driving cars. Many have asked how you can be assured that the cars will never have an accident. That is, of course, the wrong question. The correct question, as articulated very nicely by one of the innovators in that field, George Holtz, is how we can make a car that is safer than the way that cars are currently being driven (which means fewer deaths than the 15,000 that occur annually with humans behind the wheel).4
Our current method of providing care often leaves patients without appropriate guideline-recommended medications, and many don’t reach their HbA1c, blood pressure, cholesterol, and asthma-control goals. The era of machine learning with machine-generated algorithms may be much closer than we think, which will allow us to spend more time talking with patients, educating them about their disease, and supporting them in their efforts to remain healthy – an attractive future for both us and our patients.
References
1. Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017 Nov;40(11):1469-78.
2. Naylor CD. On the prospects for a (deep) learning health care system. JAMA. 2018 Sep 18;320(11):1099-100.
3. Wang YR et al. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007 Jan 22;167(2):141-7.
4. Super Hacker George Hotz: “I can make your car drive itself for under $1,000.”
Countdown to launch: Health care IT primed for disruption
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
On Friday, June 29, at 5:42 a.m., I stood with my family on a Florida shore overlooking Kennedy Space Center. We had gathered with about a hundred other people to watch a rocket launch and were overwhelmed with excitement as the coastline erupted in fire, and the spacecraft lifted off toward the heavens. Standing there watching the spectacle, I couldn’t help but be caught up in the irony of the moment. Here we were, at the place where NASA sent the first Americans into space – on the very shores where the Apollo astronauts set off for the moon to plant our nation’s flag in the lunar dust in July of 1969. Yet now, almost 50 years later, this launch was profoundly different. The rocket wasn’t built by NASA, and the intention of its builders wasn’t exploration. This was a Falcon 9, built by SpaceX, a for-profit company founded by an enterprising billionaire. Most surprisingly, this relatively routine launch was intended to accomplish something that NASA – the United States’ own space agency – currently can’t do on its own: Launch rockets.
Since retiring the Space Shuttle in 2011, the United States has had to rely on others – including even Roscosmos (the Russian space agency) – to ferry passengers, satellites, and cargo into space. Seeing this opportunity in a multibillion-dollar industry, private enterprise has risen to the challenge, innovating more quickly and at a lower cost than “the establishment” has ever been capable of. As a result, space travel has been disrupted by corporations competing in a new “space race.” Instead of national pride or scientific dominance, this race has been fueled by profit and is quite similar to one being run in another industry: health care.
Just 1 day prior to watching the launch – on June 28 – we learned that Amazon had purchased PillPack, a prescription drug home delivery service. The stock market responded to the news, and the establishment (in this case CVS, Walgreen’s, and WalMart, among others) collectively lost $17.5 billion in one day. This isn’t the first time Amazon has disrupted the health care world; in January of this year, they, along with Berkshire Hathaway and JPMorgan Chase, announced a health care partnership to cut costs and improve care delivery for their employees. This move also sent shivers through the market, as health insurers and providers such as Aetna and United Health lost big on expectations that Amazon et al. wouldn’t stop with their own employees. Those of us watching this play out from the sidelines realized we were witnessing a revolution that would mean the end of health care delivery as we know it – and that’s not necessarily a bad thing, especially in the world of Electronic Health Records.
As you’ve probably noticed, it is quite rare to find physicians nowadays who love computers. Once an exciting novelty in health care, PCs have become a burdensome necessity and providers often feel enslaved to the EHRs that run on them. There are numerous reasons for this, but one primary cause is that the hundreds of disparate EHRs currently available sprouted out of health care – a centuries-old and very provincial industry – prior to the development of technical and regulatory standards to govern them. As they’ve grown larger and larger from their primitive underpinnings, these EHRs have become more cumbersome to navigate, and vendors have simply “bolted-on” additional features without significant changes to their near-obsolete software architecture.
It’s worth noting that a few EHR companies purport to be true innovators in platform usability, such as industry giant, Epic. According to CEO Judy Faulkner, Epic pours 50% of their revenue back into research and development (though, as Epic is a privately held company, this number can’t be verified). If accurate, Epic is truly an exception, as most electronic record companies spend about 10%-30% on improving their products – far less than they spend on recruiting new customers. Regardless, the outcome is this: Physician expectations for user interface and user experience have far outpaced the current state of the art of EHRs, and this has left a gap that new players outside the health care establishment are apt to fill.
Like Amazon, other software giants have made significant investments in health care over the past several years. According to their website, Apple has been working with hospitals, scientists, and developers to “help health care providers streamline their work, deliver better care, and conduct medical research.” Similarly, Google claims to be “making a number of big bets in health care and life sciences,” by leveraging their artificial intelligence technology to assist in clinical diagnosis and scientific discovery. In spite of a few false starts in the past, these companies are poised to do more than simply disrupt health care. As experts in user interface and design, they could truly change the way physicians interact with health care technology, and it seems like it’s no longer a question of if, but when we’ll see that happen.
The effort of SpaceX and others to change the way we launch rockets tells a story that transcends space travel – It’s a story of how new thinking, more efficient processes, and better design can disrupt the establishment. It’s worth pointing out that NASA hasn’t given up – they are continuing to develop the Space Launch System, which, when completed, will be the most powerful rocket in the world and be capable of carrying astronauts into deep space. In the meantime, however, NASA is embracing the efforts of private industry to help pave a better way forward and make space travel safer and more accessible for everyone. We are hopeful that EHR vendors and other establishment health care institutions are taking note, adapting to meet the needs of the current generation of physicians and patients, and innovating a better way to launch health care into the future.
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Jefferson Health.
What is an old doctor to do?
I was in Miami recently to give a talk on diabetes when a physician, Pablo Michel, MD, asked me whether we could address an issue that’s important to him and many of his colleagues. His question was, Do we have any suggestions about how to help “older doctors” such as himself deal with electronic health records?
One of the problems with his question was that he didn’t really look “old”; he looked like he was about 50 years of age and in good shape. This physician had come on a Saturday morning to spend 4 hours learning about diabetes, which made it clear that he cared about his patients, his craft, and staying current with the medical literature.
I was struck by his questions, as well as his concern for both the quality of care for his patients and the issues he and his colleagues were facing. And it is not just him. Increased computerization of practices has been listed among the top five causes of physician burnout.1
A recent article in Annals of Internal Medicine showed that physicians spent only a quarter of their total time directly talking with patients and 50% of their time on EHR and other administrative tasks.2 It is likely that, among older physicians, the EHR takes proportionally more time and is an even larger cause of burnout. Given the importance of EHR, it seems time to revisit both the dilemma of, and propose some solutions for, this common problem.
One of the core issues for many older physicians is an inability to type. If you don’t type well, then entering a patient’s history or documenting the assessment and plan is unduly burdensome. Ten years ago, we might have suggested learning to type, which was an unrealistic recommendation then and, fortunately, is unnecessary now.
Now, solutions ranging from medical scribes to voice recognition have become commonplace. Voice recognition technology has advanced incredibly over the past 10 years, so much so that it is used now in our everyday life. The most well-known voice technology in everyday life might be Siri, Apple’s voice technology. It is easy now to dictate texts and to look up information. Similar voice technologies are available with the Amazon Echo and Google Assistant.
We now also have the advantage of well-developed medical voice recognition technology that can be used with most EHRs. Although some doctors say that the software is expensive, it can cost about $1,500 for the software and another $200-$300 for a good microphone, as well as the time to train on the software. But that expense needs to be weighed against the lost productivity of not using such software. A common complaint we hear from older doctors is that they are spending 1 to 2 hours a night completing charts. If voice recognition software could shave off half that time, decrease stress, and increase satisfaction, then it would pay for itself in 2 weeks.
Another issue is that, because the EHR enables so many things to be done from the EHR platform, many doctors find themselves doing all the work. It is important to work as a team and let each member of the team contribute to making the process more efficient. It turns out that this usually ends up being satisfying for everyone who contributes to patient care. It requires standing back from the process periodically and thinking about areas of inefficiency and how things can be done better.
One clear example is medication reconciliation: A nurse or clinical pharmacist can go over medicines with patients, and while the physician still needs to review the medications, it takes much less time to review medications than it does to enter each medication with the correct dose. Nurses also can help with preventive health initiatives. Performing recommended preventive health activities ranging from hepatitis C screening to colonoscopy can be greatly facilitated by the participation of nursing staff, and their participation will free up doctors so they can have more time to focus on diagnosis and treatment. Teamwork is critical.
Finally, if you don’t know something that is important to your practice – learn it! We are accustomed to going to CME conferences and spending our time learning about diseases like diabetes, asthma, and COPD. Each of these disease accounts for 5%-10% of the patients we see in our practice, and it is critically important to stay current and learn about them. We use our EHR for 100% of the patients we see; therefore, we should allocate time to learning about how to navigate the EHR and work more efficiently with it.
These issues are real, and the processes continue to change, but by standing back and acknowledging the challenges, we can thoughtfully construct an approach to maximize our ability to continue to have productive, gratifying careers while helping our patients.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter @doctornotte.
References
1. Medscape Physician Lifestyle Report 2015. Accessed April 27, 2018. https://www.medscape.com/slideshow/lifestyle-2015-overview-6006535#1.
2. Sinsky C et al. Ann Intern Med. 2016;165(11):753-60.
I was in Miami recently to give a talk on diabetes when a physician, Pablo Michel, MD, asked me whether we could address an issue that’s important to him and many of his colleagues. His question was, Do we have any suggestions about how to help “older doctors” such as himself deal with electronic health records?
One of the problems with his question was that he didn’t really look “old”; he looked like he was about 50 years of age and in good shape. This physician had come on a Saturday morning to spend 4 hours learning about diabetes, which made it clear that he cared about his patients, his craft, and staying current with the medical literature.
I was struck by his questions, as well as his concern for both the quality of care for his patients and the issues he and his colleagues were facing. And it is not just him. Increased computerization of practices has been listed among the top five causes of physician burnout.1
A recent article in Annals of Internal Medicine showed that physicians spent only a quarter of their total time directly talking with patients and 50% of their time on EHR and other administrative tasks.2 It is likely that, among older physicians, the EHR takes proportionally more time and is an even larger cause of burnout. Given the importance of EHR, it seems time to revisit both the dilemma of, and propose some solutions for, this common problem.
One of the core issues for many older physicians is an inability to type. If you don’t type well, then entering a patient’s history or documenting the assessment and plan is unduly burdensome. Ten years ago, we might have suggested learning to type, which was an unrealistic recommendation then and, fortunately, is unnecessary now.
Now, solutions ranging from medical scribes to voice recognition have become commonplace. Voice recognition technology has advanced incredibly over the past 10 years, so much so that it is used now in our everyday life. The most well-known voice technology in everyday life might be Siri, Apple’s voice technology. It is easy now to dictate texts and to look up information. Similar voice technologies are available with the Amazon Echo and Google Assistant.
We now also have the advantage of well-developed medical voice recognition technology that can be used with most EHRs. Although some doctors say that the software is expensive, it can cost about $1,500 for the software and another $200-$300 for a good microphone, as well as the time to train on the software. But that expense needs to be weighed against the lost productivity of not using such software. A common complaint we hear from older doctors is that they are spending 1 to 2 hours a night completing charts. If voice recognition software could shave off half that time, decrease stress, and increase satisfaction, then it would pay for itself in 2 weeks.
Another issue is that, because the EHR enables so many things to be done from the EHR platform, many doctors find themselves doing all the work. It is important to work as a team and let each member of the team contribute to making the process more efficient. It turns out that this usually ends up being satisfying for everyone who contributes to patient care. It requires standing back from the process periodically and thinking about areas of inefficiency and how things can be done better.
One clear example is medication reconciliation: A nurse or clinical pharmacist can go over medicines with patients, and while the physician still needs to review the medications, it takes much less time to review medications than it does to enter each medication with the correct dose. Nurses also can help with preventive health initiatives. Performing recommended preventive health activities ranging from hepatitis C screening to colonoscopy can be greatly facilitated by the participation of nursing staff, and their participation will free up doctors so they can have more time to focus on diagnosis and treatment. Teamwork is critical.
Finally, if you don’t know something that is important to your practice – learn it! We are accustomed to going to CME conferences and spending our time learning about diseases like diabetes, asthma, and COPD. Each of these disease accounts for 5%-10% of the patients we see in our practice, and it is critically important to stay current and learn about them. We use our EHR for 100% of the patients we see; therefore, we should allocate time to learning about how to navigate the EHR and work more efficiently with it.
These issues are real, and the processes continue to change, but by standing back and acknowledging the challenges, we can thoughtfully construct an approach to maximize our ability to continue to have productive, gratifying careers while helping our patients.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter @doctornotte.
References
1. Medscape Physician Lifestyle Report 2015. Accessed April 27, 2018. https://www.medscape.com/slideshow/lifestyle-2015-overview-6006535#1.
2. Sinsky C et al. Ann Intern Med. 2016;165(11):753-60.
I was in Miami recently to give a talk on diabetes when a physician, Pablo Michel, MD, asked me whether we could address an issue that’s important to him and many of his colleagues. His question was, Do we have any suggestions about how to help “older doctors” such as himself deal with electronic health records?
One of the problems with his question was that he didn’t really look “old”; he looked like he was about 50 years of age and in good shape. This physician had come on a Saturday morning to spend 4 hours learning about diabetes, which made it clear that he cared about his patients, his craft, and staying current with the medical literature.
I was struck by his questions, as well as his concern for both the quality of care for his patients and the issues he and his colleagues were facing. And it is not just him. Increased computerization of practices has been listed among the top five causes of physician burnout.1
A recent article in Annals of Internal Medicine showed that physicians spent only a quarter of their total time directly talking with patients and 50% of their time on EHR and other administrative tasks.2 It is likely that, among older physicians, the EHR takes proportionally more time and is an even larger cause of burnout. Given the importance of EHR, it seems time to revisit both the dilemma of, and propose some solutions for, this common problem.
One of the core issues for many older physicians is an inability to type. If you don’t type well, then entering a patient’s history or documenting the assessment and plan is unduly burdensome. Ten years ago, we might have suggested learning to type, which was an unrealistic recommendation then and, fortunately, is unnecessary now.
Now, solutions ranging from medical scribes to voice recognition have become commonplace. Voice recognition technology has advanced incredibly over the past 10 years, so much so that it is used now in our everyday life. The most well-known voice technology in everyday life might be Siri, Apple’s voice technology. It is easy now to dictate texts and to look up information. Similar voice technologies are available with the Amazon Echo and Google Assistant.
We now also have the advantage of well-developed medical voice recognition technology that can be used with most EHRs. Although some doctors say that the software is expensive, it can cost about $1,500 for the software and another $200-$300 for a good microphone, as well as the time to train on the software. But that expense needs to be weighed against the lost productivity of not using such software. A common complaint we hear from older doctors is that they are spending 1 to 2 hours a night completing charts. If voice recognition software could shave off half that time, decrease stress, and increase satisfaction, then it would pay for itself in 2 weeks.
Another issue is that, because the EHR enables so many things to be done from the EHR platform, many doctors find themselves doing all the work. It is important to work as a team and let each member of the team contribute to making the process more efficient. It turns out that this usually ends up being satisfying for everyone who contributes to patient care. It requires standing back from the process periodically and thinking about areas of inefficiency and how things can be done better.
One clear example is medication reconciliation: A nurse or clinical pharmacist can go over medicines with patients, and while the physician still needs to review the medications, it takes much less time to review medications than it does to enter each medication with the correct dose. Nurses also can help with preventive health initiatives. Performing recommended preventive health activities ranging from hepatitis C screening to colonoscopy can be greatly facilitated by the participation of nursing staff, and their participation will free up doctors so they can have more time to focus on diagnosis and treatment. Teamwork is critical.
Finally, if you don’t know something that is important to your practice – learn it! We are accustomed to going to CME conferences and spending our time learning about diseases like diabetes, asthma, and COPD. Each of these disease accounts for 5%-10% of the patients we see in our practice, and it is critically important to stay current and learn about them. We use our EHR for 100% of the patients we see; therefore, we should allocate time to learning about how to navigate the EHR and work more efficiently with it.
These issues are real, and the processes continue to change, but by standing back and acknowledging the challenges, we can thoughtfully construct an approach to maximize our ability to continue to have productive, gratifying careers while helping our patients.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington Jefferson Health. Follow him on twitter @doctornotte.
References
1. Medscape Physician Lifestyle Report 2015. Accessed April 27, 2018. https://www.medscape.com/slideshow/lifestyle-2015-overview-6006535#1.
2. Sinsky C et al. Ann Intern Med. 2016;165(11):753-60.
Risking it all on the miracle of teamwork
On Feb. 4, 2018, with his team narrowly leading the New England Patriots in Super Bowl 52, Philadelphia Eagles head coach Doug Pederson made an audacious 4th-and-goal call. At the suggestion of backup quarterback Nick Foles, Pederson chose to rely on his team’s ability to execute the “Philly Special.” This was a risky trick play that was rehearsed but never tested, and one which could prove disastrous unless executed just right. With 34 seconds left in the first half, the Eagles pulled it off. Foles caught the ball in the end zone, securing his team’s place in football history and becoming the first quarterback to both throw for and catch a touchdown in one Super Bowl. He was named MVP and led the team to its first NFL title in 58 years.
For those of us who call Philadelphia our home, Super Bowl 52 represented so much more than just a victory, it was a miracle. We have long endured the highs and lows of Philadelphia football, watching as year after year our hopes were dashed by coaches and players who showed such promise, yet demonstrated such disappointment. But this year everything changed.
True fans could sense something different in the weeks leading up to that cold February day in Minneapolis. As the Eagle’s chances of competing in the Super Bowl grew more and more possible, the narrative wasn’t about any star player or member of the coaching staff, but instead the story of an incredible team. Even after the injury of starting quarterback and football phenom Carson Wentz in week 14, players and fans never lost hope in the promise of victory. Finally, Philadelphia had the team that could, and would, pull off something that had heretofore seemed like only an impossible dream.
It occurs to us that physicians should find the story of the Philadelphia Eagles not only inspirational, but also aspirational, even more so after reading the original research published by Dr. Richard Young, et al. in the February issue of Family Medicine.1 In this article, Dr. Young and his colleagues observed physicians during 982 patient encounters. The group measured the total visit time, face-to-face time, non-face time, and EHR work time (before, during, and after patient hours). The results weren’t surprising: Physicians spend more time working in the EHR than they spend in face-to-face time with patients.
This study confirmed prior work done by Ardnt et al. published in the fall in Annals of Family Medicine,2 which demonstrated that “primary care physicians spend more than half their workday, nearly 6 hours, interacting with the EHR during and after clinic hours.” Sadly, despite improving technology, the chasm between interacting with computers and interacting with actual patients only seems to be widening. To preserve the sanctity of the physician-patient relationship, we are forced to consider a completely new approach to how we practice: team-based care.
Team-based care isn’t a new idea, but it is being embraced with new fervor in the era of electronic health records. This is because the blessing — and curse — of the EHR is the vast amount of information that can be stored and accessed while caring for patients. To take advantage of this, doctors have been forced to become the primary agents for data entry and retrieval, something that is nearly impossible to do effectively while performing the cognitive work of a highly educated clinician. Rather than allowing us to take better care of patients, EHRs seem to have a paradoxical effect, limiting “face-to-face” time and squelching our efforts to address anything outside the immediate issues at hand. To improve the experience for us and our patients, we need to begin to rely on others.
To start, consider how a team can help support your documentation. As we’ve written about before, scribe services can be a tremendous benefit but aren’t the only way to improve efficiency. Medical assistants and nursing staff need to be encouraged to operate at the top level of their license, documenting where allowable and even queueing up orders, medication refills, and preventative care interventions when appropriate. This can be tremendously useful during previsit planning and can ensure that nothing is missed during the patient encounter.
Team-based care can also extend far beyond the EHR. For example, care coordinators can be employed to focus on specific high- and rising-risk patient populations. These health care professionals (typically nurses) reach out directly to patients and review their care, and even schedule visits with patients independently of the physician. This establishes therapeutic relationships that have been shown to prevent disease exacerbations and hospital readmissions, greatly reducing the cost of care.
Some facilities are now also using scheduling advocates, charged with facilitating referrals, arranging specialist and diagnostic appointments, and following up with patients to make sure they’ve successfully navigated the health care landscape. Behavioral health specialists and clinical pharmacists are also making their way into physician practices to expand the scope of offerings and decompress the burden on physicians. While these all have an associated cost, changes in the way physicians get paid are making the extra support economical and often necessary to satisfy the requirements under risk-based and fee-for-value contracts. We also predict that practices that choose to eschew the team approach to care will lose a competitive advantage in a health care market that is becoming more and more consumer driven. Patients, as well as providers, see the benefits of highly effective care teams.
Following the Eagles’ dramatic Super Bowl victory, coach Doug Pederson addressed his team in the locker room with these words: “This is a team game. As we’ve said before, an individual can make a difference, but a team makes a miracle.” While we as physicians may easily become jaded by the “miracles” of modern medicine, our patients have not yet lost hope in our ability to deliver on the promise of victory. To meet their expectations, we need to acknowledge that we will no longer be able to make it into the end zone alone; instead — in the game of modern medicine — we’ll need a team to take us there.
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era. Fam Med. 2018 February;50(2):91-9.
- Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA, Gilchrist VJ..Ann Fam Med. 2017 September/October;15(5)5:419-26.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and Associate Chief Medical Information Officer for Jefferson Health. Follow him on twitter (@doctornotte).
On Feb. 4, 2018, with his team narrowly leading the New England Patriots in Super Bowl 52, Philadelphia Eagles head coach Doug Pederson made an audacious 4th-and-goal call. At the suggestion of backup quarterback Nick Foles, Pederson chose to rely on his team’s ability to execute the “Philly Special.” This was a risky trick play that was rehearsed but never tested, and one which could prove disastrous unless executed just right. With 34 seconds left in the first half, the Eagles pulled it off. Foles caught the ball in the end zone, securing his team’s place in football history and becoming the first quarterback to both throw for and catch a touchdown in one Super Bowl. He was named MVP and led the team to its first NFL title in 58 years.
For those of us who call Philadelphia our home, Super Bowl 52 represented so much more than just a victory, it was a miracle. We have long endured the highs and lows of Philadelphia football, watching as year after year our hopes were dashed by coaches and players who showed such promise, yet demonstrated such disappointment. But this year everything changed.
True fans could sense something different in the weeks leading up to that cold February day in Minneapolis. As the Eagle’s chances of competing in the Super Bowl grew more and more possible, the narrative wasn’t about any star player or member of the coaching staff, but instead the story of an incredible team. Even after the injury of starting quarterback and football phenom Carson Wentz in week 14, players and fans never lost hope in the promise of victory. Finally, Philadelphia had the team that could, and would, pull off something that had heretofore seemed like only an impossible dream.
It occurs to us that physicians should find the story of the Philadelphia Eagles not only inspirational, but also aspirational, even more so after reading the original research published by Dr. Richard Young, et al. in the February issue of Family Medicine.1 In this article, Dr. Young and his colleagues observed physicians during 982 patient encounters. The group measured the total visit time, face-to-face time, non-face time, and EHR work time (before, during, and after patient hours). The results weren’t surprising: Physicians spend more time working in the EHR than they spend in face-to-face time with patients.
This study confirmed prior work done by Ardnt et al. published in the fall in Annals of Family Medicine,2 which demonstrated that “primary care physicians spend more than half their workday, nearly 6 hours, interacting with the EHR during and after clinic hours.” Sadly, despite improving technology, the chasm between interacting with computers and interacting with actual patients only seems to be widening. To preserve the sanctity of the physician-patient relationship, we are forced to consider a completely new approach to how we practice: team-based care.
Team-based care isn’t a new idea, but it is being embraced with new fervor in the era of electronic health records. This is because the blessing — and curse — of the EHR is the vast amount of information that can be stored and accessed while caring for patients. To take advantage of this, doctors have been forced to become the primary agents for data entry and retrieval, something that is nearly impossible to do effectively while performing the cognitive work of a highly educated clinician. Rather than allowing us to take better care of patients, EHRs seem to have a paradoxical effect, limiting “face-to-face” time and squelching our efforts to address anything outside the immediate issues at hand. To improve the experience for us and our patients, we need to begin to rely on others.
To start, consider how a team can help support your documentation. As we’ve written about before, scribe services can be a tremendous benefit but aren’t the only way to improve efficiency. Medical assistants and nursing staff need to be encouraged to operate at the top level of their license, documenting where allowable and even queueing up orders, medication refills, and preventative care interventions when appropriate. This can be tremendously useful during previsit planning and can ensure that nothing is missed during the patient encounter.
Team-based care can also extend far beyond the EHR. For example, care coordinators can be employed to focus on specific high- and rising-risk patient populations. These health care professionals (typically nurses) reach out directly to patients and review their care, and even schedule visits with patients independently of the physician. This establishes therapeutic relationships that have been shown to prevent disease exacerbations and hospital readmissions, greatly reducing the cost of care.
Some facilities are now also using scheduling advocates, charged with facilitating referrals, arranging specialist and diagnostic appointments, and following up with patients to make sure they’ve successfully navigated the health care landscape. Behavioral health specialists and clinical pharmacists are also making their way into physician practices to expand the scope of offerings and decompress the burden on physicians. While these all have an associated cost, changes in the way physicians get paid are making the extra support economical and often necessary to satisfy the requirements under risk-based and fee-for-value contracts. We also predict that practices that choose to eschew the team approach to care will lose a competitive advantage in a health care market that is becoming more and more consumer driven. Patients, as well as providers, see the benefits of highly effective care teams.
Following the Eagles’ dramatic Super Bowl victory, coach Doug Pederson addressed his team in the locker room with these words: “This is a team game. As we’ve said before, an individual can make a difference, but a team makes a miracle.” While we as physicians may easily become jaded by the “miracles” of modern medicine, our patients have not yet lost hope in our ability to deliver on the promise of victory. To meet their expectations, we need to acknowledge that we will no longer be able to make it into the end zone alone; instead — in the game of modern medicine — we’ll need a team to take us there.
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era. Fam Med. 2018 February;50(2):91-9.
- Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA, Gilchrist VJ..Ann Fam Med. 2017 September/October;15(5)5:419-26.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and Associate Chief Medical Information Officer for Jefferson Health. Follow him on twitter (@doctornotte).
On Feb. 4, 2018, with his team narrowly leading the New England Patriots in Super Bowl 52, Philadelphia Eagles head coach Doug Pederson made an audacious 4th-and-goal call. At the suggestion of backup quarterback Nick Foles, Pederson chose to rely on his team’s ability to execute the “Philly Special.” This was a risky trick play that was rehearsed but never tested, and one which could prove disastrous unless executed just right. With 34 seconds left in the first half, the Eagles pulled it off. Foles caught the ball in the end zone, securing his team’s place in football history and becoming the first quarterback to both throw for and catch a touchdown in one Super Bowl. He was named MVP and led the team to its first NFL title in 58 years.
For those of us who call Philadelphia our home, Super Bowl 52 represented so much more than just a victory, it was a miracle. We have long endured the highs and lows of Philadelphia football, watching as year after year our hopes were dashed by coaches and players who showed such promise, yet demonstrated such disappointment. But this year everything changed.
True fans could sense something different in the weeks leading up to that cold February day in Minneapolis. As the Eagle’s chances of competing in the Super Bowl grew more and more possible, the narrative wasn’t about any star player or member of the coaching staff, but instead the story of an incredible team. Even after the injury of starting quarterback and football phenom Carson Wentz in week 14, players and fans never lost hope in the promise of victory. Finally, Philadelphia had the team that could, and would, pull off something that had heretofore seemed like only an impossible dream.
It occurs to us that physicians should find the story of the Philadelphia Eagles not only inspirational, but also aspirational, even more so after reading the original research published by Dr. Richard Young, et al. in the February issue of Family Medicine.1 In this article, Dr. Young and his colleagues observed physicians during 982 patient encounters. The group measured the total visit time, face-to-face time, non-face time, and EHR work time (before, during, and after patient hours). The results weren’t surprising: Physicians spend more time working in the EHR than they spend in face-to-face time with patients.
This study confirmed prior work done by Ardnt et al. published in the fall in Annals of Family Medicine,2 which demonstrated that “primary care physicians spend more than half their workday, nearly 6 hours, interacting with the EHR during and after clinic hours.” Sadly, despite improving technology, the chasm between interacting with computers and interacting with actual patients only seems to be widening. To preserve the sanctity of the physician-patient relationship, we are forced to consider a completely new approach to how we practice: team-based care.
Team-based care isn’t a new idea, but it is being embraced with new fervor in the era of electronic health records. This is because the blessing — and curse — of the EHR is the vast amount of information that can be stored and accessed while caring for patients. To take advantage of this, doctors have been forced to become the primary agents for data entry and retrieval, something that is nearly impossible to do effectively while performing the cognitive work of a highly educated clinician. Rather than allowing us to take better care of patients, EHRs seem to have a paradoxical effect, limiting “face-to-face” time and squelching our efforts to address anything outside the immediate issues at hand. To improve the experience for us and our patients, we need to begin to rely on others.
To start, consider how a team can help support your documentation. As we’ve written about before, scribe services can be a tremendous benefit but aren’t the only way to improve efficiency. Medical assistants and nursing staff need to be encouraged to operate at the top level of their license, documenting where allowable and even queueing up orders, medication refills, and preventative care interventions when appropriate. This can be tremendously useful during previsit planning and can ensure that nothing is missed during the patient encounter.
Team-based care can also extend far beyond the EHR. For example, care coordinators can be employed to focus on specific high- and rising-risk patient populations. These health care professionals (typically nurses) reach out directly to patients and review their care, and even schedule visits with patients independently of the physician. This establishes therapeutic relationships that have been shown to prevent disease exacerbations and hospital readmissions, greatly reducing the cost of care.
Some facilities are now also using scheduling advocates, charged with facilitating referrals, arranging specialist and diagnostic appointments, and following up with patients to make sure they’ve successfully navigated the health care landscape. Behavioral health specialists and clinical pharmacists are also making their way into physician practices to expand the scope of offerings and decompress the burden on physicians. While these all have an associated cost, changes in the way physicians get paid are making the extra support economical and often necessary to satisfy the requirements under risk-based and fee-for-value contracts. We also predict that practices that choose to eschew the team approach to care will lose a competitive advantage in a health care market that is becoming more and more consumer driven. Patients, as well as providers, see the benefits of highly effective care teams.
Following the Eagles’ dramatic Super Bowl victory, coach Doug Pederson addressed his team in the locker room with these words: “This is a team game. As we’ve said before, an individual can make a difference, but a team makes a miracle.” While we as physicians may easily become jaded by the “miracles” of modern medicine, our patients have not yet lost hope in our ability to deliver on the promise of victory. To meet their expectations, we need to acknowledge that we will no longer be able to make it into the end zone alone; instead — in the game of modern medicine — we’ll need a team to take us there.
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era. Fam Med. 2018 February;50(2):91-9.
- Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA, Gilchrist VJ..Ann Fam Med. 2017 September/October;15(5)5:419-26.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and Associate Chief Medical Information Officer for Jefferson Health. Follow him on twitter (@doctornotte).