User login
HM17 plenaries: Hospital medicine leading health care shift to value, quality
LAS VEGAS – The path to improved health care in the U.S. may never be straight – and it certainly won’t be easy – but the three plenary speakers at HM17 think its destination is pretty clear: a system that increasingly rewards quality care delivered at lower costs.
And the three experts agreed that there may be “no finer group” than hospitalists to continue leading the charge.
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to be the way it always was,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services. “You have been at the forefront of seeing that we’re getting better value out of our health care system.”
Dr. DeSalvo believes HM’s scope of practice must evolve to include a focus on social determinants – such as economic stability, neighborhood and physical environment, education, and access to healthy options for food – because they have “direct relationships with mortality and morbidity and cost.”
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring issues?
“If you listen to the hoof-beats that are coming, there is definitely a financial imprimatur to do this,” Dr. DeSalvo said. “There is going to be an expectation from public and private payers... that we are going to be taking into account and addressing social factors. Just look at the data from the people of this country – they are shouting loudly to you that they need help.”
“I can tell you our system still does not have a highly reliable, whole health system for those children and their families,” he said. “Every weekend, I have a family that I can’t discharge because they don’t have the social and home-based supports for them to go home. So they literally sit in the hospital until Monday. That makes no sense for our overall health system.”
Dr. Conway assured attendees that health system transformation is a bipartisan ideal and that for all the tumult in Washington, the progress of testing new payment- and service-delivery models will move forward.
The work “on value, the work on accountability, the work on bundled payments... will continue and will continue to be important to you and the patients you serve,” he said.
Robert Wachter, MD, MHM, concluded the meeting – as is tradition – by telling hospitalists the field remains positioned to take the lead for hospital transformation. And technology, despite its myriad frustrations, is still the tool that will get the field there.
“Digital is really important here, because it becomes an enabler for those stakeholders who care about what we do to measure what we do, and our ability to change what we do in a far more robust way than we could ever do before, if we get our acts together,” Dr. Wachter said. “We’re well past the time where you can nibble around the edges here, you can get this done with little mini projects. You really have to remake your whole delivery system, the way you do your work in order to succeed in this environment.”
Dr. Wachter agreed that social determinants must be addressed. He said HM might do better to partner with folks handling those issues, rather than tackling them head on. Instead, HM needs to be “focusing on the right things” amid mounting pressures from digitization, consolidation of everything from health systems to insurance companies to HM companies, and the gravitation toward population health.
“We have successfully positioned ourselves as the people who are leaders in this work,” Dr. Wachter said, “and it is increasingly important that we continue to do that as we go forward.”
LAS VEGAS – The path to improved health care in the U.S. may never be straight – and it certainly won’t be easy – but the three plenary speakers at HM17 think its destination is pretty clear: a system that increasingly rewards quality care delivered at lower costs.
And the three experts agreed that there may be “no finer group” than hospitalists to continue leading the charge.
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to be the way it always was,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services. “You have been at the forefront of seeing that we’re getting better value out of our health care system.”
Dr. DeSalvo believes HM’s scope of practice must evolve to include a focus on social determinants – such as economic stability, neighborhood and physical environment, education, and access to healthy options for food – because they have “direct relationships with mortality and morbidity and cost.”
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring issues?
“If you listen to the hoof-beats that are coming, there is definitely a financial imprimatur to do this,” Dr. DeSalvo said. “There is going to be an expectation from public and private payers... that we are going to be taking into account and addressing social factors. Just look at the data from the people of this country – they are shouting loudly to you that they need help.”
“I can tell you our system still does not have a highly reliable, whole health system for those children and their families,” he said. “Every weekend, I have a family that I can’t discharge because they don’t have the social and home-based supports for them to go home. So they literally sit in the hospital until Monday. That makes no sense for our overall health system.”
Dr. Conway assured attendees that health system transformation is a bipartisan ideal and that for all the tumult in Washington, the progress of testing new payment- and service-delivery models will move forward.
The work “on value, the work on accountability, the work on bundled payments... will continue and will continue to be important to you and the patients you serve,” he said.
Robert Wachter, MD, MHM, concluded the meeting – as is tradition – by telling hospitalists the field remains positioned to take the lead for hospital transformation. And technology, despite its myriad frustrations, is still the tool that will get the field there.
“Digital is really important here, because it becomes an enabler for those stakeholders who care about what we do to measure what we do, and our ability to change what we do in a far more robust way than we could ever do before, if we get our acts together,” Dr. Wachter said. “We’re well past the time where you can nibble around the edges here, you can get this done with little mini projects. You really have to remake your whole delivery system, the way you do your work in order to succeed in this environment.”
Dr. Wachter agreed that social determinants must be addressed. He said HM might do better to partner with folks handling those issues, rather than tackling them head on. Instead, HM needs to be “focusing on the right things” amid mounting pressures from digitization, consolidation of everything from health systems to insurance companies to HM companies, and the gravitation toward population health.
“We have successfully positioned ourselves as the people who are leaders in this work,” Dr. Wachter said, “and it is increasingly important that we continue to do that as we go forward.”
LAS VEGAS – The path to improved health care in the U.S. may never be straight – and it certainly won’t be easy – but the three plenary speakers at HM17 think its destination is pretty clear: a system that increasingly rewards quality care delivered at lower costs.
And the three experts agreed that there may be “no finer group” than hospitalists to continue leading the charge.
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to be the way it always was,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services. “You have been at the forefront of seeing that we’re getting better value out of our health care system.”
Dr. DeSalvo believes HM’s scope of practice must evolve to include a focus on social determinants – such as economic stability, neighborhood and physical environment, education, and access to healthy options for food – because they have “direct relationships with mortality and morbidity and cost.”
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring issues?
“If you listen to the hoof-beats that are coming, there is definitely a financial imprimatur to do this,” Dr. DeSalvo said. “There is going to be an expectation from public and private payers... that we are going to be taking into account and addressing social factors. Just look at the data from the people of this country – they are shouting loudly to you that they need help.”
“I can tell you our system still does not have a highly reliable, whole health system for those children and their families,” he said. “Every weekend, I have a family that I can’t discharge because they don’t have the social and home-based supports for them to go home. So they literally sit in the hospital until Monday. That makes no sense for our overall health system.”
Dr. Conway assured attendees that health system transformation is a bipartisan ideal and that for all the tumult in Washington, the progress of testing new payment- and service-delivery models will move forward.
The work “on value, the work on accountability, the work on bundled payments... will continue and will continue to be important to you and the patients you serve,” he said.
Robert Wachter, MD, MHM, concluded the meeting – as is tradition – by telling hospitalists the field remains positioned to take the lead for hospital transformation. And technology, despite its myriad frustrations, is still the tool that will get the field there.
“Digital is really important here, because it becomes an enabler for those stakeholders who care about what we do to measure what we do, and our ability to change what we do in a far more robust way than we could ever do before, if we get our acts together,” Dr. Wachter said. “We’re well past the time where you can nibble around the edges here, you can get this done with little mini projects. You really have to remake your whole delivery system, the way you do your work in order to succeed in this environment.”
Dr. Wachter agreed that social determinants must be addressed. He said HM might do better to partner with folks handling those issues, rather than tackling them head on. Instead, HM needs to be “focusing on the right things” amid mounting pressures from digitization, consolidation of everything from health systems to insurance companies to HM companies, and the gravitation toward population health.
“We have successfully positioned ourselves as the people who are leaders in this work,” Dr. Wachter said, “and it is increasingly important that we continue to do that as we go forward.”
HM17 session summary: Building a practice that people want to be part of
Presenters
Roberta Himebaugh MBA, SHM; John Nelson, MD, FACP, MHM; Jerome Siy, MD, SFHM
Session summary
Creating a “culture of ownership” by recruiting the right people, promoting physician leadership, and improving structural elements such as compensation model and schedule were topics discussed in this practice management precourse at HM17.
The presenters said leaders must reduce hierarchy and promote shared decision making among the group, while instilling a “thank you culture” that recognizes motivations such as autonomy, mastery, and purpose.
Leaders must also consider current changes in health care payment models, such as MIPS (Merit-based Incentive Payment System), bundled payments, and Hospital Value-based Purchasing. Hospitalist groups must be prepared for these changes by learning about them and looking for potential cost reduction opportunities (e.g., reducing the number of patients going to skilled nursing facilities after joint replacement by sending patients home whenever possible).
Promoting a culture of engagement might include the development of interpersonal support strategies (e.g., meditation and mindfulness), innovative staffing (is 7 on/7 off right for everyone?), and comprehensive support for career and leadership development.
Finally, hospitalists should give special attention to the value formula by focusing on improving patient outcomes and experience, but also reducing direct and indirect costs. This is crucial for the sustainability of any hospitalist group.
Key takeaways for HM
• Create a culture of ownership to promote engagement and job satisfaction.
• Make adjustments to schedule and workflow to improve efficiency.
• Prepare for evolving pay-for-performance programs.
• Demonstrate the value of the group by setting expectations with key stakeholders, developing a practice score, and providing effective feedback to providers.
Dr. Villagra is a chief hospitalist in Batesville, Ark., and an editorial board member of The Hospitalist.
Presenters
Roberta Himebaugh MBA, SHM; John Nelson, MD, FACP, MHM; Jerome Siy, MD, SFHM
Session summary
Creating a “culture of ownership” by recruiting the right people, promoting physician leadership, and improving structural elements such as compensation model and schedule were topics discussed in this practice management precourse at HM17.
The presenters said leaders must reduce hierarchy and promote shared decision making among the group, while instilling a “thank you culture” that recognizes motivations such as autonomy, mastery, and purpose.
Leaders must also consider current changes in health care payment models, such as MIPS (Merit-based Incentive Payment System), bundled payments, and Hospital Value-based Purchasing. Hospitalist groups must be prepared for these changes by learning about them and looking for potential cost reduction opportunities (e.g., reducing the number of patients going to skilled nursing facilities after joint replacement by sending patients home whenever possible).
Promoting a culture of engagement might include the development of interpersonal support strategies (e.g., meditation and mindfulness), innovative staffing (is 7 on/7 off right for everyone?), and comprehensive support for career and leadership development.
Finally, hospitalists should give special attention to the value formula by focusing on improving patient outcomes and experience, but also reducing direct and indirect costs. This is crucial for the sustainability of any hospitalist group.
Key takeaways for HM
• Create a culture of ownership to promote engagement and job satisfaction.
• Make adjustments to schedule and workflow to improve efficiency.
• Prepare for evolving pay-for-performance programs.
• Demonstrate the value of the group by setting expectations with key stakeholders, developing a practice score, and providing effective feedback to providers.
Dr. Villagra is a chief hospitalist in Batesville, Ark., and an editorial board member of The Hospitalist.
Presenters
Roberta Himebaugh MBA, SHM; John Nelson, MD, FACP, MHM; Jerome Siy, MD, SFHM
Session summary
Creating a “culture of ownership” by recruiting the right people, promoting physician leadership, and improving structural elements such as compensation model and schedule were topics discussed in this practice management precourse at HM17.
The presenters said leaders must reduce hierarchy and promote shared decision making among the group, while instilling a “thank you culture” that recognizes motivations such as autonomy, mastery, and purpose.
Leaders must also consider current changes in health care payment models, such as MIPS (Merit-based Incentive Payment System), bundled payments, and Hospital Value-based Purchasing. Hospitalist groups must be prepared for these changes by learning about them and looking for potential cost reduction opportunities (e.g., reducing the number of patients going to skilled nursing facilities after joint replacement by sending patients home whenever possible).
Promoting a culture of engagement might include the development of interpersonal support strategies (e.g., meditation and mindfulness), innovative staffing (is 7 on/7 off right for everyone?), and comprehensive support for career and leadership development.
Finally, hospitalists should give special attention to the value formula by focusing on improving patient outcomes and experience, but also reducing direct and indirect costs. This is crucial for the sustainability of any hospitalist group.
Key takeaways for HM
• Create a culture of ownership to promote engagement and job satisfaction.
• Make adjustments to schedule and workflow to improve efficiency.
• Prepare for evolving pay-for-performance programs.
• Demonstrate the value of the group by setting expectations with key stakeholders, developing a practice score, and providing effective feedback to providers.
Dr. Villagra is a chief hospitalist in Batesville, Ark., and an editorial board member of The Hospitalist.
HM17 session summary: Focus on POCUS – Introduction to Point-of-Care Ultrasound for pediatric hospitalists
Presenters
Nilam Soni, MD, FHM; Thomas Conlon, MD; Ria Dancel, MD, FAAP, FHM; Daniel Schnobrich, MD
Summary
Point-of-care ultrasound (POCUS) is rapidly gaining acceptance in the medical community as a goal-directed examination that answers a specific diagnostic question or guides a bedside invasive procedure. Adoption by pediatric hospitalists is increasing, aided by multiple training pathways, opportunities for scholarship, and organization development.
The use of POCUS is increasing among nonradiologist physicians due to the expectation for perfection, desire for improved patient experience, and increased availability of ultrasound machines. POCUS is rapid and safe, and can be used serially to monitor, provide procedural guidance, and lead to initiation of appropriate therapies.
Training in POCUS in limited applications is possible in short periods of time. One recent study showed that approximately 40% of POCUS cases led to new findings or alteration of treatment. However, POCUS requires training, monitoring for competence, transparency of training/competence, and a QA process that supports the training. One solution at Children’s Hospital of Philadelphia was to use American College of Emergency Physician guidelines for POCUS training.
Pediatric applications include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia and associated parapneumonic effusion, and IV placement. More advanced applications include diagnosis of appendicitis, intussusception, and increased intracranial pressure. Novel applications conceived by nonradiologist physicians have included sinus ultrasound.
Initial training can be provided by “in-house experts,” such as pediatric ED physicians and PICU physicians. Alternatively, an on-site commercial course can be arranged for larger groups. Consideration should be given to mentorship, with comparison to formal imaging and/or clinical progression. Relationships with traditional imagers should be cultivated, as POCUS can potentially be misunderstood. In fact, formal US utilization has been found to increase once clinicals begin to use POCUS.
Key takeaways for HM
- Point-of-care ultrasound (POCUS) is rapidly being adopted by pediatric hospitalists.
- Pediatric applications are still being developed, but include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia/associated effusions, and IV placement.
- Initial training can be provided by pediatric ED physicians/PICU physicians or an on-site commercial course can be arranged for larger groups.
- Relationships with radiologists should be established at the outset to avoid misunderstanding of POCUS.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital and is the pediatric editor of The Hospitalist.
Presenters
Nilam Soni, MD, FHM; Thomas Conlon, MD; Ria Dancel, MD, FAAP, FHM; Daniel Schnobrich, MD
Summary
Point-of-care ultrasound (POCUS) is rapidly gaining acceptance in the medical community as a goal-directed examination that answers a specific diagnostic question or guides a bedside invasive procedure. Adoption by pediatric hospitalists is increasing, aided by multiple training pathways, opportunities for scholarship, and organization development.
The use of POCUS is increasing among nonradiologist physicians due to the expectation for perfection, desire for improved patient experience, and increased availability of ultrasound machines. POCUS is rapid and safe, and can be used serially to monitor, provide procedural guidance, and lead to initiation of appropriate therapies.
Training in POCUS in limited applications is possible in short periods of time. One recent study showed that approximately 40% of POCUS cases led to new findings or alteration of treatment. However, POCUS requires training, monitoring for competence, transparency of training/competence, and a QA process that supports the training. One solution at Children’s Hospital of Philadelphia was to use American College of Emergency Physician guidelines for POCUS training.
Pediatric applications include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia and associated parapneumonic effusion, and IV placement. More advanced applications include diagnosis of appendicitis, intussusception, and increased intracranial pressure. Novel applications conceived by nonradiologist physicians have included sinus ultrasound.
Initial training can be provided by “in-house experts,” such as pediatric ED physicians and PICU physicians. Alternatively, an on-site commercial course can be arranged for larger groups. Consideration should be given to mentorship, with comparison to formal imaging and/or clinical progression. Relationships with traditional imagers should be cultivated, as POCUS can potentially be misunderstood. In fact, formal US utilization has been found to increase once clinicals begin to use POCUS.
Key takeaways for HM
- Point-of-care ultrasound (POCUS) is rapidly being adopted by pediatric hospitalists.
- Pediatric applications are still being developed, but include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia/associated effusions, and IV placement.
- Initial training can be provided by pediatric ED physicians/PICU physicians or an on-site commercial course can be arranged for larger groups.
- Relationships with radiologists should be established at the outset to avoid misunderstanding of POCUS.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital and is the pediatric editor of The Hospitalist.
Presenters
Nilam Soni, MD, FHM; Thomas Conlon, MD; Ria Dancel, MD, FAAP, FHM; Daniel Schnobrich, MD
Summary
Point-of-care ultrasound (POCUS) is rapidly gaining acceptance in the medical community as a goal-directed examination that answers a specific diagnostic question or guides a bedside invasive procedure. Adoption by pediatric hospitalists is increasing, aided by multiple training pathways, opportunities for scholarship, and organization development.
The use of POCUS is increasing among nonradiologist physicians due to the expectation for perfection, desire for improved patient experience, and increased availability of ultrasound machines. POCUS is rapid and safe, and can be used serially to monitor, provide procedural guidance, and lead to initiation of appropriate therapies.
Training in POCUS in limited applications is possible in short periods of time. One recent study showed that approximately 40% of POCUS cases led to new findings or alteration of treatment. However, POCUS requires training, monitoring for competence, transparency of training/competence, and a QA process that supports the training. One solution at Children’s Hospital of Philadelphia was to use American College of Emergency Physician guidelines for POCUS training.
Pediatric applications include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia and associated parapneumonic effusion, and IV placement. More advanced applications include diagnosis of appendicitis, intussusception, and increased intracranial pressure. Novel applications conceived by nonradiologist physicians have included sinus ultrasound.
Initial training can be provided by “in-house experts,” such as pediatric ED physicians and PICU physicians. Alternatively, an on-site commercial course can be arranged for larger groups. Consideration should be given to mentorship, with comparison to formal imaging and/or clinical progression. Relationships with traditional imagers should be cultivated, as POCUS can potentially be misunderstood. In fact, formal US utilization has been found to increase once clinicals begin to use POCUS.
Key takeaways for HM
- Point-of-care ultrasound (POCUS) is rapidly being adopted by pediatric hospitalists.
- Pediatric applications are still being developed, but include guidance of bladder catheterization, identifying occult abscesses, diagnosis of pneumonia/associated effusions, and IV placement.
- Initial training can be provided by pediatric ED physicians/PICU physicians or an on-site commercial course can be arranged for larger groups.
- Relationships with radiologists should be established at the outset to avoid misunderstanding of POCUS.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital and is the pediatric editor of The Hospitalist.
Hyponatremia: Watch the water, not the salt
LAS VEGAS – Hyponatremia is not a salt problem, it’s a water problem.
That was the lead message in a well-attended rapid-fire session on hyponatremia at the annual meeting of the Society of Hospital Medicine.
“It’s almost always associated with pathologic elevations of ADH [antidiuretic hormone], and it’s that retention of water that dilutes the serum and drops the sodium, which causes the cerebral edema,” said Thomas Yacovella, MD, assistant professor of medicine at the University of Minnesota, Minneapolis.
“Remember that hyponatremia is a bad actor, especially when associated with a chronic disease,” Dr. Yacovella said. Serum sodium levels are a reliable surrogate for chronic heart failure related to hyponatremia. End-stage disease is when sodium levels are at 125 or less.
A basic work-up for hyponatremia starts with assessing fluid intake, history of medications and of any causes of ADH release, volume status assessment, and laboratory evaluations of blood and urine. The three keys to knowing how quickly hyponatremia can be reversed are severity of symptoms, how long it took for the condition to develop, and the risk of herniation vs. the risk of osmotic demyelination, he said.
In cases of osmotic demyelination, Dr. Yacovella advised monitoring urine osmolality and cases where ADH release could be quickly reversed. “When you don’t know for sure, go slow,” he said.
Exercise-associated hyponatremia is often caused by the perfect storm of sodium loss, high emotion, vomiting, pain, excessive water intake, and high ADH levels. This form of hyponatremia can occur postoperatively, but is more typically associated with the copious water ingestion that can occur during psychosis, extreme exercise, ecstasy ingestion, and “stupid” contests that involve extreme behavior, Dr. Yacovella said. His pearls for acute management of these kinds of hyponatremia were to administer a 100-mL bolus of hypertonic saline, and that a large output of dilute urine indicates corrective aquaresis.
Dr. Yacovella emphasized that in addition to remembering that hyponatremia is a water and not a salt problem, physicians should always look to “the path of physiology of the disease, and how long it took to develop the hyponatremia, and that will inform how quickly you can treat the patient.”
He had nothing to disclose.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
LAS VEGAS – Hyponatremia is not a salt problem, it’s a water problem.
That was the lead message in a well-attended rapid-fire session on hyponatremia at the annual meeting of the Society of Hospital Medicine.
“It’s almost always associated with pathologic elevations of ADH [antidiuretic hormone], and it’s that retention of water that dilutes the serum and drops the sodium, which causes the cerebral edema,” said Thomas Yacovella, MD, assistant professor of medicine at the University of Minnesota, Minneapolis.
“Remember that hyponatremia is a bad actor, especially when associated with a chronic disease,” Dr. Yacovella said. Serum sodium levels are a reliable surrogate for chronic heart failure related to hyponatremia. End-stage disease is when sodium levels are at 125 or less.
A basic work-up for hyponatremia starts with assessing fluid intake, history of medications and of any causes of ADH release, volume status assessment, and laboratory evaluations of blood and urine. The three keys to knowing how quickly hyponatremia can be reversed are severity of symptoms, how long it took for the condition to develop, and the risk of herniation vs. the risk of osmotic demyelination, he said.
In cases of osmotic demyelination, Dr. Yacovella advised monitoring urine osmolality and cases where ADH release could be quickly reversed. “When you don’t know for sure, go slow,” he said.
Exercise-associated hyponatremia is often caused by the perfect storm of sodium loss, high emotion, vomiting, pain, excessive water intake, and high ADH levels. This form of hyponatremia can occur postoperatively, but is more typically associated with the copious water ingestion that can occur during psychosis, extreme exercise, ecstasy ingestion, and “stupid” contests that involve extreme behavior, Dr. Yacovella said. His pearls for acute management of these kinds of hyponatremia were to administer a 100-mL bolus of hypertonic saline, and that a large output of dilute urine indicates corrective aquaresis.
Dr. Yacovella emphasized that in addition to remembering that hyponatremia is a water and not a salt problem, physicians should always look to “the path of physiology of the disease, and how long it took to develop the hyponatremia, and that will inform how quickly you can treat the patient.”
He had nothing to disclose.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
LAS VEGAS – Hyponatremia is not a salt problem, it’s a water problem.
That was the lead message in a well-attended rapid-fire session on hyponatremia at the annual meeting of the Society of Hospital Medicine.
“It’s almost always associated with pathologic elevations of ADH [antidiuretic hormone], and it’s that retention of water that dilutes the serum and drops the sodium, which causes the cerebral edema,” said Thomas Yacovella, MD, assistant professor of medicine at the University of Minnesota, Minneapolis.
“Remember that hyponatremia is a bad actor, especially when associated with a chronic disease,” Dr. Yacovella said. Serum sodium levels are a reliable surrogate for chronic heart failure related to hyponatremia. End-stage disease is when sodium levels are at 125 or less.
A basic work-up for hyponatremia starts with assessing fluid intake, history of medications and of any causes of ADH release, volume status assessment, and laboratory evaluations of blood and urine. The three keys to knowing how quickly hyponatremia can be reversed are severity of symptoms, how long it took for the condition to develop, and the risk of herniation vs. the risk of osmotic demyelination, he said.
In cases of osmotic demyelination, Dr. Yacovella advised monitoring urine osmolality and cases where ADH release could be quickly reversed. “When you don’t know for sure, go slow,” he said.
Exercise-associated hyponatremia is often caused by the perfect storm of sodium loss, high emotion, vomiting, pain, excessive water intake, and high ADH levels. This form of hyponatremia can occur postoperatively, but is more typically associated with the copious water ingestion that can occur during psychosis, extreme exercise, ecstasy ingestion, and “stupid” contests that involve extreme behavior, Dr. Yacovella said. His pearls for acute management of these kinds of hyponatremia were to administer a 100-mL bolus of hypertonic saline, and that a large output of dilute urine indicates corrective aquaresis.
Dr. Yacovella emphasized that in addition to remembering that hyponatremia is a water and not a salt problem, physicians should always look to “the path of physiology of the disease, and how long it took to develop the hyponatremia, and that will inform how quickly you can treat the patient.”
He had nothing to disclose.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
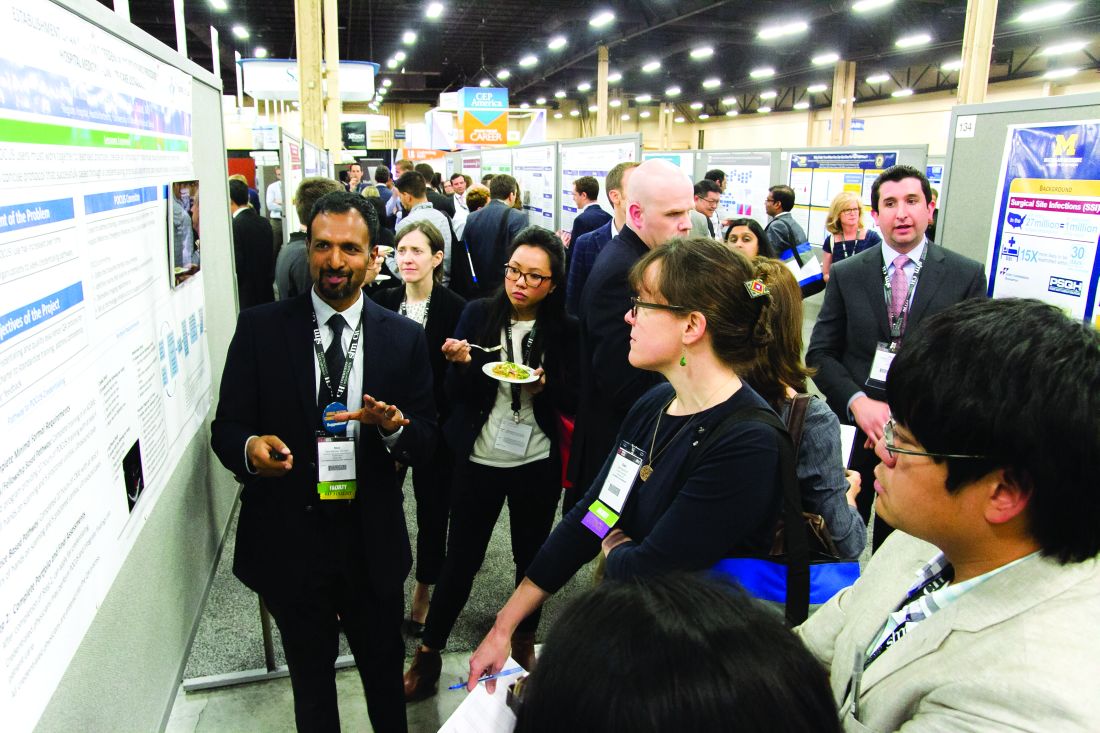
RIV spotlights HM-focused research in real-time
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
Hospitalists share strategies to secure, excel at jobs
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
Hospitalists’ EMR frustrations continue: SHM report
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
Presenters hand out tips for better handoffs
LAS VEGAS – When the resident in the handoff training video approached another resident, she first vented about her “really crazy day” and how she’d been hoping to “get out of here on time for once.” Then, she tore through a case like an auctioneer, leaving out important details. At the end, she got a page and, of course, didn’t finish the handoff.
In Wednesday’s Quality Track session, “Strategies for Implementing a Successful Handoff” – with lessons from SHM’s I-PASS mentored implementation project – some attendees were eager to point out all of the flaws in the handoff. They were, however, slower to point to the good. For instance, the resident in the video made the effort to meet face-to-face and asked whether her colleague had any questions.
The audience had learned an important lesson about how to foster better handoffs, said Glenn Rosenbluth, MD, director of quality and safety programs at the University of California, San Francisco. He noted that it can be difficult to find the positives when the negatives are so glaring.
“This is one of the hard parts about doing feedback,” he said.
It was just one of many lessons taught in the session, also led by Amy Starmer, MD, MPH, a lecturer on pediatrics at Harvard Medical School, and Courtney Edgar-Zarate, MD, a pediatric hospitalist at Arkansas Children’s Hospital who was one of the I-PASS site leaders.
I-PASS was a nine-site study in the United States and Canada that found that using a bundle of interventions while doing handoffs resulted in a 30% reduction in preventable adverse events, meaning less harm to patients. The hallmark is the “I-PASS” mnemonic. It stands for:
- Illness severity – describing the stability level of a patient.
- Patient summary, including general information, such as the events leading to admission.
- Action list – essentially a to-do list for the patient.
- Situation awareness and contingency planning, which involves having a plan for what might happen.
- Synthesis by the receiver, in which the recipient of the information summarizes what was heard and asks questions.
Beyond that, the I-PASS system involves an introductory workshop, simulation exercises, structured observation and feedback, among other elements, Dr. Starmer said.
“This intervention was certainly not just a five-letter mnemonic,” she said.
The I-PASS Mentored Implementation Program, a collaboration with SHM that is funded by the Agency for Healthcare Research and Quality, is an effort to help implement a similar program in 32 hospitals in the United States.
Dr. Edgar-Zarate outlined the steps that worked at her site to make their I-PASS project successful. She said that project managers have to establish institutional support; assess a given center’s needs; gauge where to begin by identifying the most vulnerable transition points; find providers who will champion the project; establish good communication, in part by incorporating I-PASS into previously scheduled meetings; and collect data as time goes on.
Dr. Starmer directed attendees to www.ipassstudygroup.com, where anyone can download the material for free.
“This mentored implementation process,” she said, “has really been a helpful vehicle for disseminating the curriculum and implementation across different areas.”
LAS VEGAS – When the resident in the handoff training video approached another resident, she first vented about her “really crazy day” and how she’d been hoping to “get out of here on time for once.” Then, she tore through a case like an auctioneer, leaving out important details. At the end, she got a page and, of course, didn’t finish the handoff.
In Wednesday’s Quality Track session, “Strategies for Implementing a Successful Handoff” – with lessons from SHM’s I-PASS mentored implementation project – some attendees were eager to point out all of the flaws in the handoff. They were, however, slower to point to the good. For instance, the resident in the video made the effort to meet face-to-face and asked whether her colleague had any questions.
The audience had learned an important lesson about how to foster better handoffs, said Glenn Rosenbluth, MD, director of quality and safety programs at the University of California, San Francisco. He noted that it can be difficult to find the positives when the negatives are so glaring.
“This is one of the hard parts about doing feedback,” he said.
It was just one of many lessons taught in the session, also led by Amy Starmer, MD, MPH, a lecturer on pediatrics at Harvard Medical School, and Courtney Edgar-Zarate, MD, a pediatric hospitalist at Arkansas Children’s Hospital who was one of the I-PASS site leaders.
I-PASS was a nine-site study in the United States and Canada that found that using a bundle of interventions while doing handoffs resulted in a 30% reduction in preventable adverse events, meaning less harm to patients. The hallmark is the “I-PASS” mnemonic. It stands for:
- Illness severity – describing the stability level of a patient.
- Patient summary, including general information, such as the events leading to admission.
- Action list – essentially a to-do list for the patient.
- Situation awareness and contingency planning, which involves having a plan for what might happen.
- Synthesis by the receiver, in which the recipient of the information summarizes what was heard and asks questions.
Beyond that, the I-PASS system involves an introductory workshop, simulation exercises, structured observation and feedback, among other elements, Dr. Starmer said.
“This intervention was certainly not just a five-letter mnemonic,” she said.
The I-PASS Mentored Implementation Program, a collaboration with SHM that is funded by the Agency for Healthcare Research and Quality, is an effort to help implement a similar program in 32 hospitals in the United States.
Dr. Edgar-Zarate outlined the steps that worked at her site to make their I-PASS project successful. She said that project managers have to establish institutional support; assess a given center’s needs; gauge where to begin by identifying the most vulnerable transition points; find providers who will champion the project; establish good communication, in part by incorporating I-PASS into previously scheduled meetings; and collect data as time goes on.
Dr. Starmer directed attendees to www.ipassstudygroup.com, where anyone can download the material for free.
“This mentored implementation process,” she said, “has really been a helpful vehicle for disseminating the curriculum and implementation across different areas.”
LAS VEGAS – When the resident in the handoff training video approached another resident, she first vented about her “really crazy day” and how she’d been hoping to “get out of here on time for once.” Then, she tore through a case like an auctioneer, leaving out important details. At the end, she got a page and, of course, didn’t finish the handoff.
In Wednesday’s Quality Track session, “Strategies for Implementing a Successful Handoff” – with lessons from SHM’s I-PASS mentored implementation project – some attendees were eager to point out all of the flaws in the handoff. They were, however, slower to point to the good. For instance, the resident in the video made the effort to meet face-to-face and asked whether her colleague had any questions.
The audience had learned an important lesson about how to foster better handoffs, said Glenn Rosenbluth, MD, director of quality and safety programs at the University of California, San Francisco. He noted that it can be difficult to find the positives when the negatives are so glaring.
“This is one of the hard parts about doing feedback,” he said.
It was just one of many lessons taught in the session, also led by Amy Starmer, MD, MPH, a lecturer on pediatrics at Harvard Medical School, and Courtney Edgar-Zarate, MD, a pediatric hospitalist at Arkansas Children’s Hospital who was one of the I-PASS site leaders.
I-PASS was a nine-site study in the United States and Canada that found that using a bundle of interventions while doing handoffs resulted in a 30% reduction in preventable adverse events, meaning less harm to patients. The hallmark is the “I-PASS” mnemonic. It stands for:
- Illness severity – describing the stability level of a patient.
- Patient summary, including general information, such as the events leading to admission.
- Action list – essentially a to-do list for the patient.
- Situation awareness and contingency planning, which involves having a plan for what might happen.
- Synthesis by the receiver, in which the recipient of the information summarizes what was heard and asks questions.
Beyond that, the I-PASS system involves an introductory workshop, simulation exercises, structured observation and feedback, among other elements, Dr. Starmer said.
“This intervention was certainly not just a five-letter mnemonic,” she said.
The I-PASS Mentored Implementation Program, a collaboration with SHM that is funded by the Agency for Healthcare Research and Quality, is an effort to help implement a similar program in 32 hospitals in the United States.
Dr. Edgar-Zarate outlined the steps that worked at her site to make their I-PASS project successful. She said that project managers have to establish institutional support; assess a given center’s needs; gauge where to begin by identifying the most vulnerable transition points; find providers who will champion the project; establish good communication, in part by incorporating I-PASS into previously scheduled meetings; and collect data as time goes on.
Dr. Starmer directed attendees to www.ipassstudygroup.com, where anyone can download the material for free.
“This mentored implementation process,” she said, “has really been a helpful vehicle for disseminating the curriculum and implementation across different areas.”
AT HM17
VIDEO: NPs, PAs weigh common issues in hospitalist practice
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Connect: Community hospitalists brainstorm ways to be stronger as a group
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.