User login
Taming or teaching the tiger? Myths and management of childhood aggression
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
How to deal with aggression delivered by a child’s peers is a common concern and social dilemma for both parents and children. How does a child ward off aggressive peers without getting hurt or in trouble while also not looking weak or whiny? What can parents do to stop their child from being hurt or frightened but also not humiliate them or interfere with their learning important life skills by being over protective?
Children do not want to fight, but they do want to be treated fairly. Frustration, with its associated feelings of anger, is the most common reason for aggression. Being a child is certainly full of its frustrations because, while autonomy and desires are increasing, opportunities expand at a slower rate, particularly for children with developmental weaknesses or economic disadvantage. Fear and a lack of coping skills are other major reasons for resorting to aggressive responses.
Physical bullying affects 21% of students in grades 3-12 and is a risk factor for aggression at all ages. A full one-third of 9th-12th graders report having been in a physical fight in the last year. In grade school age and adolescence, factors known to be associated with peer aggression include the humiliation of school failure, substance use, and anger from experiencing parental or sibling aggression.
One would think a universal goal of parents would be to raise their children to get along with others without fighting. Unfortunately, some parents actually espouse childrearing methods that directly or indirectly make fighting more likely.
Essentially all toddlers and preschoolers can be aggressive at times to get things they want (instrumental) or when angry in the beginning of their second year of life; this peaks in the third year and typically declines after age 3 years. But for some 10% of children, aggression remains high. What parent and child factors set children up for such persistent aggression?
Parents have many reasons for how they raise their children, but some myths about parenting that persist promote aggression.
“My child will love me more if I am more permissive.”
Infants and toddlers develop self-regulation skills better when it is gradually expected of them with encouragement and support from their parents. Parents may feel that they are showing love to their toddler by having a “relaxed” home with few limits and no specific bedtime or rules. These parents also may “rescue” their child from frustrating situations by giving in to their demands or removing them from even mildly stressful situations.
These strategies can interfere with the progressive development of frustration tolerance, a key life skill. A lack of routines, inadequate sleep or food, overstimulation by noise, frightening experiences (including fighting in the home or neighborhood), or violent media exposure sets toddlers up to be out of control and thereby increases dysregulation. In addition, the dysregulated child may then act up, which can invoke punishment from that same parent.
Frustrating toddlers with inconsistent expectations and arbitrary punishment, a common result of low structure, makes the child feel insecure and leads to aggression. Instead, children need small doses of frustration appropriate to their age and encouragement from a supportive adult to problem solve. You can praise (or model), cheering on a child with words such as “Are you stuck? You can do it! Try again,” instead of instantly solving problems for them.
“Spare the rod and spoil the child.”
Parents may feel that they are promoting obedience when they use corporal punishment, thinking this will keep the child out of trouble in society. Instead, corporal punishment is associated with increased aggression toward peers, as well as defiance toward parents. These effects are especially strong when mothers are distant emotionally. As pediatricians, we can educate people on the importance of warm parenting, redirection instead of punishment for younger children, and using small, logical consequences or time out when needed for aggression.
“Just ignore bullies.”
It is a rare child who can follow the command to “ignore” a bully without turning red or getting tears in his or her eyes – making them appealing targets. We can coach parents and kids how to disarm bullies by standing tall, putting hands on hips, making eye contact, and asking the peer a question such as “I do not understand what you’re trying to accomplish.” Learning martial arts also teaches children that they are powerful (but not to fight outside the class) so they can present themselves in this way. Programs that encourage children to get together to confront bullies supported by a school administration that uses comprehensive assessment and habilitation strategies for aggressive students are most effective in reducing aggression in schools. Anonymous reporting (for example, by using a cell phone app, such as STOPit) empowers students to report bullying or fights to school staff without risking later retribution from the peer.
“Tough teachers help kids fall in line.”
While peer fights generally increase from 2nd to 4th grade before declining, student fighting progressively increases when teachers use reprimands, rather than praise, to manage their classes. Children look to teachers to learn more than what is in books – how to be respectful and in control without putting others down. The most effective classroom management includes clear, fair rules; any correction should be done privately to avoid shaming students. Students dealt with this way are less likely to be angry and take it out on others. Of course, appropriate services helping every child experience success in learning is the foundation of positive behavior in school.
“Children with ADHD won’t learn self-regulation if they are treated with medicine.”
Children who show “low effortful control” or higher “dysregulation” are both more aggressive and also less likely to decline in aggression in early childhood. ADHD is a neurological condition characterized by such dysregulation and low effortful control. Children with ADHD often have higher and more persistent aggression. These tendencies also result in impulsive behaviors that can irritate peers and adults and can result in correction and criticism, further increasing aggression. Children with ADHD who are better controlled, often with the help of medication, have more positive interactions at school and at home, receive more praise and less correction, and develop more reasoned interaction patterns.
“I am the parent, and my child should do what I say.”
When adults step in to stop a fight, they are rarely in a position to know what actually happened between the kids. Children may quickly learn how to entrap a sibling or peer to look like the perpetrator in order to get them in trouble and/or avoid consequences for themselves, especially if large or harsh punishments are being used.
While it can seem tricky to treat children who are very different in age or development equally, having parents elicit or at least verbalize each child’s point of view is part of how children learn respect and mediation skills. Parents who refrain from taking sides or dictating how disputes should be resolved leave the chance for the children to acquire these component skills of negotiation. This does not mean there are no consequences, just that a brief discussion comes first.
When fighting is a pediatric complaint, you have a great opportunity to educate families in evidence-based ways that can both prevent and reduce their child’s use of aggression.
In one effective 90-minute training program, parents were taught basic mediation principles: to give ground rules and ask their children to agree to them, to ask each child to describe what happened and identify their disagreements and common ground, to encourage the children to discuss their goals in the fight and feelings about the issues, and to encourage the children to come up with suggestions to resolve their disputes and help them assess the practical aspects of their ideas. Praise should be used each time a child uses even some of these skills. Parents in this program also were given communication strategies, such as active listening, reflecting, and reframing, to help children learn to take the others’ perspective. In a follow up survey a month later, children of parents in the intervention group were seen to use these skills in real situations that might otherwise have been fights.
When aggression persists, mindfulness training, cognitive-behavioral techniques, social-emotional approaches, or peer mentoring programs delivered through individual counseling or school programs are all ways of teaching kids important interaction skills to reduce peer aggression. Remember, 40% of severe adult aggression begins before age 8 years, so preventive education or early referral to mental health services is key.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
Anxiety in teens
It seems that every week there is a new headline about the rising rates of anxiety in today’s adolescents. Schools often are asked to address high levels of stress and anxiety in their students, and the pediatrician’s office is often the first place worried parents will call. We will try to help you differentiate between what is normal – even healthy – adolescent stress, and what might represent treatable psychiatric problems. And we will review how to approach stress management with your patients and their parents. For all adolescents, even those with psychiatric diagnoses, learning to manage stress and anxiety is critical to their healthiest development into capable, confident, resilient adults.
Stress is the mental or emotional strain resulting from demanding or adverse circumstances. Anxiety is a feeling of unease about an imminent event with an uncertain outcome. An anxiety disorder is a psychiatric illness characterized by a state of excessive unease leading to functional impairment. These distinctions are critical, as both stress and anxiety are normal-but-uncomfortable parts of the adolescent experience. When all of a teenager’s stress and anxiety is medicalized, it promotes avoidance, which in turn may worsen your patient’s functional impairment rather than improving it.
This is not to suggest that there are not real (and common) psychiatric illnesses that can affect the levels of anxiety in your patients. Anxiety disorders start the earliest, with separation anxiety disorder, specific phobia, and social phobia all having a mean onset before puberty. Anxiety disorders are the most prevalent psychiatric disorders in youth (30% of youth psychiatric illness), and anxiety also may be related to substance use disorders (25%), disruptive behavior disorders (20%), and mood disorders (17%). Despite the excited news coverage, there is no evidence of a statistically significant increase in the incidence of anxiety or mood disorders in young people over the past decade.
It is not difficult to imagine that the challenges facing adolescents are considerable. Of course, adolescence is a time of major change starting with puberty, in which young people actively develop independence, identity, and a rich array of deep relationships beyond their families. Typically, this is a 5- to 10-year process of risk-taking, new experiences, setbacks, delight, heartbreak, and triumphs all alongside growing autonomy.
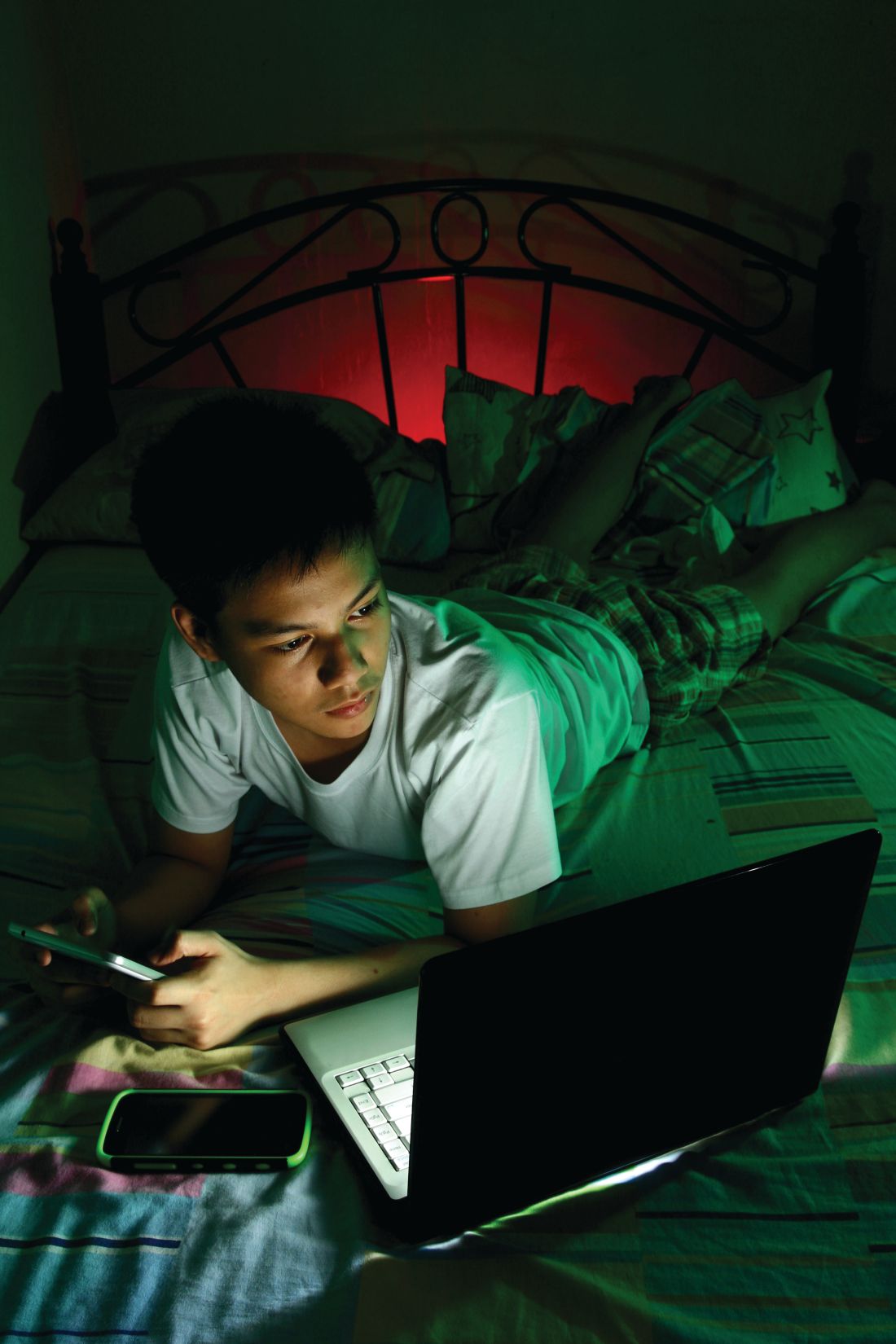
These forces may make their parents even more stressed than the adolescents themselves, but there is one dramatically different feature of adolescent life today: the constant presence of smartphones. While these devices can improve connectedness to school, family, and friends, use of smartphones also means that today’s teenagers often have little downtime cognitively or socially. Use of smartphones can facilitate both supportive affirmation from friends and relentless social pressures, and the feeling of being excluded or bullied. Smartphone use can interfere with restful sleep, and some virtual activities may compete with the genuine experimentation and exploration where teenagers discover their interests and abilities and develop meaningful confidence and independence.
Several factors might impair an adolescent’s ability to cope with challenge and stress. Those teenagers who have not had the opportunity to face and manage modest setbacks, difficulties, and discomforts during their elementary and middle school years may be overwhelmed by starting with the higher-stakes strains of adolescence. This can happen when young children have not explored many new activities, have been shielded from the consequences of failures, or have tried only activities that came easily to them. Certainly, teenagers who are managing a depressive or anxiety disorder as well as those with learning disabilities may have limited ability to cope with routine stress, although those who have a well-treated disorder often have robust coping skills.
Perhaps obvious, but still very important, chronic sleep deprivation can leave adolescents irritable, impatient, and distractible, all of which make coping with a challenge very difficult. Likewise, substance use can directly impair coping skills, and can create the habit of trying to escape stress rather than manage it.
So what does this mean for you? If your patient has an anxiety, depressive, or substance use disorder, refer for appropriate therapy. For both those who screen in and those who do not, your next task is to help them improve their coping skills. What specifically has them so stressed?
Are there family stressors or unrealistic expectations that can be addressed? Can they see their situation as a challenge and focus on what is within their control to do in response? Remind your patients that challenges are uncomfortable. Mastery comes with practice and, inevitably, some setbacks and failures. Have they identified personal goals or a transcendent purpose? This can improve motivation and keep a challenge in perspective. They might focus on learning about their coping style: Do they do better with a slow, steady, methodical approach or intense bursts of effort? Talk with them about self-care. Adequate sleep, regular exercise, putting effort into relaxation as well as work, and spending time with their actual (not just virtual) friends all are essential to keeping their batteries charged while doing the intense work of normal adolescence.
For those patients who do not meet criteria for depression or anxiety disorders, there are circumstances in which a referral for therapy can be helpful. If they are noticeably disconnected from their parents or their parents seem to be more reactive to the stress and pressures than they are, an outside therapist can be a meaningful support as they build skills. Those patients who are socially isolated and stressed, are using substances regularly, are withdrawing from other interests to manage their source of stress, or are having difficulty telling facts from feelings are at risk for failing to adequately manage their stress and for the development of psychiatric problems. Starting early, helping them to build autonomy as preadolescents, experiencing successes and failures, begins the cultivation of resilience and meaningful confidence they will need during adolescence. Your attention and guidance can help all of your adolescent patients improve their coping and lower both their stress and their anxiety.
It seems that every week there is a new headline about the rising rates of anxiety in today’s adolescents. Schools often are asked to address high levels of stress and anxiety in their students, and the pediatrician’s office is often the first place worried parents will call. We will try to help you differentiate between what is normal – even healthy – adolescent stress, and what might represent treatable psychiatric problems. And we will review how to approach stress management with your patients and their parents. For all adolescents, even those with psychiatric diagnoses, learning to manage stress and anxiety is critical to their healthiest development into capable, confident, resilient adults.
Stress is the mental or emotional strain resulting from demanding or adverse circumstances. Anxiety is a feeling of unease about an imminent event with an uncertain outcome. An anxiety disorder is a psychiatric illness characterized by a state of excessive unease leading to functional impairment. These distinctions are critical, as both stress and anxiety are normal-but-uncomfortable parts of the adolescent experience. When all of a teenager’s stress and anxiety is medicalized, it promotes avoidance, which in turn may worsen your patient’s functional impairment rather than improving it.
This is not to suggest that there are not real (and common) psychiatric illnesses that can affect the levels of anxiety in your patients. Anxiety disorders start the earliest, with separation anxiety disorder, specific phobia, and social phobia all having a mean onset before puberty. Anxiety disorders are the most prevalent psychiatric disorders in youth (30% of youth psychiatric illness), and anxiety also may be related to substance use disorders (25%), disruptive behavior disorders (20%), and mood disorders (17%). Despite the excited news coverage, there is no evidence of a statistically significant increase in the incidence of anxiety or mood disorders in young people over the past decade.
It is not difficult to imagine that the challenges facing adolescents are considerable. Of course, adolescence is a time of major change starting with puberty, in which young people actively develop independence, identity, and a rich array of deep relationships beyond their families. Typically, this is a 5- to 10-year process of risk-taking, new experiences, setbacks, delight, heartbreak, and triumphs all alongside growing autonomy.
These forces may make their parents even more stressed than the adolescents themselves, but there is one dramatically different feature of adolescent life today: the constant presence of smartphones. While these devices can improve connectedness to school, family, and friends, use of smartphones also means that today’s teenagers often have little downtime cognitively or socially. Use of smartphones can facilitate both supportive affirmation from friends and relentless social pressures, and the feeling of being excluded or bullied. Smartphone use can interfere with restful sleep, and some virtual activities may compete with the genuine experimentation and exploration where teenagers discover their interests and abilities and develop meaningful confidence and independence.
Several factors might impair an adolescent’s ability to cope with challenge and stress. Those teenagers who have not had the opportunity to face and manage modest setbacks, difficulties, and discomforts during their elementary and middle school years may be overwhelmed by starting with the higher-stakes strains of adolescence. This can happen when young children have not explored many new activities, have been shielded from the consequences of failures, or have tried only activities that came easily to them. Certainly, teenagers who are managing a depressive or anxiety disorder as well as those with learning disabilities may have limited ability to cope with routine stress, although those who have a well-treated disorder often have robust coping skills.
Perhaps obvious, but still very important, chronic sleep deprivation can leave adolescents irritable, impatient, and distractible, all of which make coping with a challenge very difficult. Likewise, substance use can directly impair coping skills, and can create the habit of trying to escape stress rather than manage it.
So what does this mean for you? If your patient has an anxiety, depressive, or substance use disorder, refer for appropriate therapy. For both those who screen in and those who do not, your next task is to help them improve their coping skills. What specifically has them so stressed?
Are there family stressors or unrealistic expectations that can be addressed? Can they see their situation as a challenge and focus on what is within their control to do in response? Remind your patients that challenges are uncomfortable. Mastery comes with practice and, inevitably, some setbacks and failures. Have they identified personal goals or a transcendent purpose? This can improve motivation and keep a challenge in perspective. They might focus on learning about their coping style: Do they do better with a slow, steady, methodical approach or intense bursts of effort? Talk with them about self-care. Adequate sleep, regular exercise, putting effort into relaxation as well as work, and spending time with their actual (not just virtual) friends all are essential to keeping their batteries charged while doing the intense work of normal adolescence.
For those patients who do not meet criteria for depression or anxiety disorders, there are circumstances in which a referral for therapy can be helpful. If they are noticeably disconnected from their parents or their parents seem to be more reactive to the stress and pressures than they are, an outside therapist can be a meaningful support as they build skills. Those patients who are socially isolated and stressed, are using substances regularly, are withdrawing from other interests to manage their source of stress, or are having difficulty telling facts from feelings are at risk for failing to adequately manage their stress and for the development of psychiatric problems. Starting early, helping them to build autonomy as preadolescents, experiencing successes and failures, begins the cultivation of resilience and meaningful confidence they will need during adolescence. Your attention and guidance can help all of your adolescent patients improve their coping and lower both their stress and their anxiety.
It seems that every week there is a new headline about the rising rates of anxiety in today’s adolescents. Schools often are asked to address high levels of stress and anxiety in their students, and the pediatrician’s office is often the first place worried parents will call. We will try to help you differentiate between what is normal – even healthy – adolescent stress, and what might represent treatable psychiatric problems. And we will review how to approach stress management with your patients and their parents. For all adolescents, even those with psychiatric diagnoses, learning to manage stress and anxiety is critical to their healthiest development into capable, confident, resilient adults.
Stress is the mental or emotional strain resulting from demanding or adverse circumstances. Anxiety is a feeling of unease about an imminent event with an uncertain outcome. An anxiety disorder is a psychiatric illness characterized by a state of excessive unease leading to functional impairment. These distinctions are critical, as both stress and anxiety are normal-but-uncomfortable parts of the adolescent experience. When all of a teenager’s stress and anxiety is medicalized, it promotes avoidance, which in turn may worsen your patient’s functional impairment rather than improving it.
This is not to suggest that there are not real (and common) psychiatric illnesses that can affect the levels of anxiety in your patients. Anxiety disorders start the earliest, with separation anxiety disorder, specific phobia, and social phobia all having a mean onset before puberty. Anxiety disorders are the most prevalent psychiatric disorders in youth (30% of youth psychiatric illness), and anxiety also may be related to substance use disorders (25%), disruptive behavior disorders (20%), and mood disorders (17%). Despite the excited news coverage, there is no evidence of a statistically significant increase in the incidence of anxiety or mood disorders in young people over the past decade.
It is not difficult to imagine that the challenges facing adolescents are considerable. Of course, adolescence is a time of major change starting with puberty, in which young people actively develop independence, identity, and a rich array of deep relationships beyond their families. Typically, this is a 5- to 10-year process of risk-taking, new experiences, setbacks, delight, heartbreak, and triumphs all alongside growing autonomy.
These forces may make their parents even more stressed than the adolescents themselves, but there is one dramatically different feature of adolescent life today: the constant presence of smartphones. While these devices can improve connectedness to school, family, and friends, use of smartphones also means that today’s teenagers often have little downtime cognitively or socially. Use of smartphones can facilitate both supportive affirmation from friends and relentless social pressures, and the feeling of being excluded or bullied. Smartphone use can interfere with restful sleep, and some virtual activities may compete with the genuine experimentation and exploration where teenagers discover their interests and abilities and develop meaningful confidence and independence.
Several factors might impair an adolescent’s ability to cope with challenge and stress. Those teenagers who have not had the opportunity to face and manage modest setbacks, difficulties, and discomforts during their elementary and middle school years may be overwhelmed by starting with the higher-stakes strains of adolescence. This can happen when young children have not explored many new activities, have been shielded from the consequences of failures, or have tried only activities that came easily to them. Certainly, teenagers who are managing a depressive or anxiety disorder as well as those with learning disabilities may have limited ability to cope with routine stress, although those who have a well-treated disorder often have robust coping skills.
Perhaps obvious, but still very important, chronic sleep deprivation can leave adolescents irritable, impatient, and distractible, all of which make coping with a challenge very difficult. Likewise, substance use can directly impair coping skills, and can create the habit of trying to escape stress rather than manage it.
So what does this mean for you? If your patient has an anxiety, depressive, or substance use disorder, refer for appropriate therapy. For both those who screen in and those who do not, your next task is to help them improve their coping skills. What specifically has them so stressed?
Are there family stressors or unrealistic expectations that can be addressed? Can they see their situation as a challenge and focus on what is within their control to do in response? Remind your patients that challenges are uncomfortable. Mastery comes with practice and, inevitably, some setbacks and failures. Have they identified personal goals or a transcendent purpose? This can improve motivation and keep a challenge in perspective. They might focus on learning about their coping style: Do they do better with a slow, steady, methodical approach or intense bursts of effort? Talk with them about self-care. Adequate sleep, regular exercise, putting effort into relaxation as well as work, and spending time with their actual (not just virtual) friends all are essential to keeping their batteries charged while doing the intense work of normal adolescence.
For those patients who do not meet criteria for depression or anxiety disorders, there are circumstances in which a referral for therapy can be helpful. If they are noticeably disconnected from their parents or their parents seem to be more reactive to the stress and pressures than they are, an outside therapist can be a meaningful support as they build skills. Those patients who are socially isolated and stressed, are using substances regularly, are withdrawing from other interests to manage their source of stress, or are having difficulty telling facts from feelings are at risk for failing to adequately manage their stress and for the development of psychiatric problems. Starting early, helping them to build autonomy as preadolescents, experiencing successes and failures, begins the cultivation of resilience and meaningful confidence they will need during adolescence. Your attention and guidance can help all of your adolescent patients improve their coping and lower both their stress and their anxiety.
Sleepless in adolescence
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at pdnews@frontlinemedcom.com.
Preventing substance use
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
You can help with behavior of children with autism spectrum disorder
There are lots of reasons you may be eager to refer children with autism spectrum disorder (ASD) to specialty agencies. You want the fastest possible entry for the child into intervention and the families into a support system. , as well as the general health care, of their children.
“Wait!” you say, “I do not have the special knowledge to help with behavior of children with autism! There is much you can and should do, however, as the specialist(s) may not provide such guidance, entry into behavioral services may take months, and behavior issues may feel urgent to families.
So pick an example of a behavior that is concerning to the family. One problem might be lack of cooperation with activities of daily living such as eating. In this case, the A is being asked to stop playing and sit at the table; the B may be refusing to eat what is served or even to sit very long, ending in a tantrum that disrupts the family meal; and the C could be the child being sent from the table to play on their iPad. But what is the G?
Lack of social communication skills, restrictive interests, hypersensitivity, lack of coordination, and ADHD all may be playing a role. Lack of communication skills makes the social aspect of meals uninteresting. Giving verbal reasons for joining the family may not be effective. Hypersensitivity often is associated with extremes of food selectivity. Lack of fine motor coordination makes eating soup a challenge. And ADHD makes sitting for a long time difficult!
But what about that tantrum? Tantrums that are reinforced by allowing the child to leave and play on the iPad easily can turn into a chronic escape mechanism. Instead, parents need to watch for increasing restlessness, and allow the child to signal “all done” and be “excused” before any tantrum begins. Use of the iPad (a reward) should not be allowed until the family meal is over for everyone. Such accommodations are best decided on by all caregivers in advance, ideally also involving the higher-functioning child. A caregiver who persists in thinking that the child “should” be able to behave may be in denial or grief, and deserves counseling on ASD.
But he is so rigid, the parents say! The tendency of children with ASD to like sameness can be an asset to easing behavior. The key is to design and stick to routines as much as possible, 7 days per week. If the meal is at the same time each day, in the same seat, with the same plate, with no iPad, and the child is allowed to leave only after requesting to, the entire sequence is likely to be smoother. While flexibility does not come easily, it is acquired from the natural variability in family life, but only gradually and over time.
Creating and rehearsing “social stories” is an evidence-based way to help children with ASD have acceptable behaviors. Books, storyboards, and visual schedulers can be purchased to help. But even taking photos or a video of the components of a task and posting this online (private YouTube channel) or on the refrigerator, to review before, during, and/or after the activity, builds an internal image for the child. Children with ASD often watch the same YouTube videos over and over again, and even memorize and use chunks of the speech or songs at other times. Families can capitalize on this kind of repetition by using routines and songs to improve skills.
What to do when she only cares about her iPad? It is sometimes difficult to identify reinforcers to use to strengthen desired behaviors in a child with ASD. A smile or a hug or even candy may not be valued. Help parents think about an object, song, or touch the child tends to like. Media are a strong reinforcer, but need to be used sparingly, in specific situations, and kept under parental control, or else removing them can become a major source of upsets.
When a child with ASD gets upset or even violent, the behavior may be interpreted as defiance; it may scare or upset the whole family, and is not conducive to problem solving. Siblings may start screaming or begging for the parents to stop the behavior. While this creates a crisis, you can advise parents to first ensure that everyone is safe, take deep breaths, and then think about which gap is being stressed. A subtle change from what the child expected – new furniture, a guest at the table, a day off from school, or being interrupted mid video – can cause panic, especially for anxious children. Children with ASD also may act up when uncomfortable from a headache, tooth pain, constipation, hunger, or lack of sleep, but often are unable to vocalize the reason, even if they are verbal. Having parents make a few notes about the As, Bs, Cs, and Gs of each event (the essence of a functional behavioral assessment) to review with the child, each other, the teacher, or you is key to understanding the child with ASD and successfully shifting his behavior.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
There are lots of reasons you may be eager to refer children with autism spectrum disorder (ASD) to specialty agencies. You want the fastest possible entry for the child into intervention and the families into a support system. , as well as the general health care, of their children.
“Wait!” you say, “I do not have the special knowledge to help with behavior of children with autism! There is much you can and should do, however, as the specialist(s) may not provide such guidance, entry into behavioral services may take months, and behavior issues may feel urgent to families.
So pick an example of a behavior that is concerning to the family. One problem might be lack of cooperation with activities of daily living such as eating. In this case, the A is being asked to stop playing and sit at the table; the B may be refusing to eat what is served or even to sit very long, ending in a tantrum that disrupts the family meal; and the C could be the child being sent from the table to play on their iPad. But what is the G?
Lack of social communication skills, restrictive interests, hypersensitivity, lack of coordination, and ADHD all may be playing a role. Lack of communication skills makes the social aspect of meals uninteresting. Giving verbal reasons for joining the family may not be effective. Hypersensitivity often is associated with extremes of food selectivity. Lack of fine motor coordination makes eating soup a challenge. And ADHD makes sitting for a long time difficult!
But what about that tantrum? Tantrums that are reinforced by allowing the child to leave and play on the iPad easily can turn into a chronic escape mechanism. Instead, parents need to watch for increasing restlessness, and allow the child to signal “all done” and be “excused” before any tantrum begins. Use of the iPad (a reward) should not be allowed until the family meal is over for everyone. Such accommodations are best decided on by all caregivers in advance, ideally also involving the higher-functioning child. A caregiver who persists in thinking that the child “should” be able to behave may be in denial or grief, and deserves counseling on ASD.
But he is so rigid, the parents say! The tendency of children with ASD to like sameness can be an asset to easing behavior. The key is to design and stick to routines as much as possible, 7 days per week. If the meal is at the same time each day, in the same seat, with the same plate, with no iPad, and the child is allowed to leave only after requesting to, the entire sequence is likely to be smoother. While flexibility does not come easily, it is acquired from the natural variability in family life, but only gradually and over time.
Creating and rehearsing “social stories” is an evidence-based way to help children with ASD have acceptable behaviors. Books, storyboards, and visual schedulers can be purchased to help. But even taking photos or a video of the components of a task and posting this online (private YouTube channel) or on the refrigerator, to review before, during, and/or after the activity, builds an internal image for the child. Children with ASD often watch the same YouTube videos over and over again, and even memorize and use chunks of the speech or songs at other times. Families can capitalize on this kind of repetition by using routines and songs to improve skills.
What to do when she only cares about her iPad? It is sometimes difficult to identify reinforcers to use to strengthen desired behaviors in a child with ASD. A smile or a hug or even candy may not be valued. Help parents think about an object, song, or touch the child tends to like. Media are a strong reinforcer, but need to be used sparingly, in specific situations, and kept under parental control, or else removing them can become a major source of upsets.
When a child with ASD gets upset or even violent, the behavior may be interpreted as defiance; it may scare or upset the whole family, and is not conducive to problem solving. Siblings may start screaming or begging for the parents to stop the behavior. While this creates a crisis, you can advise parents to first ensure that everyone is safe, take deep breaths, and then think about which gap is being stressed. A subtle change from what the child expected – new furniture, a guest at the table, a day off from school, or being interrupted mid video – can cause panic, especially for anxious children. Children with ASD also may act up when uncomfortable from a headache, tooth pain, constipation, hunger, or lack of sleep, but often are unable to vocalize the reason, even if they are verbal. Having parents make a few notes about the As, Bs, Cs, and Gs of each event (the essence of a functional behavioral assessment) to review with the child, each other, the teacher, or you is key to understanding the child with ASD and successfully shifting his behavior.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
There are lots of reasons you may be eager to refer children with autism spectrum disorder (ASD) to specialty agencies. You want the fastest possible entry for the child into intervention and the families into a support system. , as well as the general health care, of their children.
“Wait!” you say, “I do not have the special knowledge to help with behavior of children with autism! There is much you can and should do, however, as the specialist(s) may not provide such guidance, entry into behavioral services may take months, and behavior issues may feel urgent to families.
So pick an example of a behavior that is concerning to the family. One problem might be lack of cooperation with activities of daily living such as eating. In this case, the A is being asked to stop playing and sit at the table; the B may be refusing to eat what is served or even to sit very long, ending in a tantrum that disrupts the family meal; and the C could be the child being sent from the table to play on their iPad. But what is the G?
Lack of social communication skills, restrictive interests, hypersensitivity, lack of coordination, and ADHD all may be playing a role. Lack of communication skills makes the social aspect of meals uninteresting. Giving verbal reasons for joining the family may not be effective. Hypersensitivity often is associated with extremes of food selectivity. Lack of fine motor coordination makes eating soup a challenge. And ADHD makes sitting for a long time difficult!
But what about that tantrum? Tantrums that are reinforced by allowing the child to leave and play on the iPad easily can turn into a chronic escape mechanism. Instead, parents need to watch for increasing restlessness, and allow the child to signal “all done” and be “excused” before any tantrum begins. Use of the iPad (a reward) should not be allowed until the family meal is over for everyone. Such accommodations are best decided on by all caregivers in advance, ideally also involving the higher-functioning child. A caregiver who persists in thinking that the child “should” be able to behave may be in denial or grief, and deserves counseling on ASD.
But he is so rigid, the parents say! The tendency of children with ASD to like sameness can be an asset to easing behavior. The key is to design and stick to routines as much as possible, 7 days per week. If the meal is at the same time each day, in the same seat, with the same plate, with no iPad, and the child is allowed to leave only after requesting to, the entire sequence is likely to be smoother. While flexibility does not come easily, it is acquired from the natural variability in family life, but only gradually and over time.
Creating and rehearsing “social stories” is an evidence-based way to help children with ASD have acceptable behaviors. Books, storyboards, and visual schedulers can be purchased to help. But even taking photos or a video of the components of a task and posting this online (private YouTube channel) or on the refrigerator, to review before, during, and/or after the activity, builds an internal image for the child. Children with ASD often watch the same YouTube videos over and over again, and even memorize and use chunks of the speech or songs at other times. Families can capitalize on this kind of repetition by using routines and songs to improve skills.
What to do when she only cares about her iPad? It is sometimes difficult to identify reinforcers to use to strengthen desired behaviors in a child with ASD. A smile or a hug or even candy may not be valued. Help parents think about an object, song, or touch the child tends to like. Media are a strong reinforcer, but need to be used sparingly, in specific situations, and kept under parental control, or else removing them can become a major source of upsets.
When a child with ASD gets upset or even violent, the behavior may be interpreted as defiance; it may scare or upset the whole family, and is not conducive to problem solving. Siblings may start screaming or begging for the parents to stop the behavior. While this creates a crisis, you can advise parents to first ensure that everyone is safe, take deep breaths, and then think about which gap is being stressed. A subtle change from what the child expected – new furniture, a guest at the table, a day off from school, or being interrupted mid video – can cause panic, especially for anxious children. Children with ASD also may act up when uncomfortable from a headache, tooth pain, constipation, hunger, or lack of sleep, but often are unable to vocalize the reason, even if they are verbal. Having parents make a few notes about the As, Bs, Cs, and Gs of each event (the essence of a functional behavioral assessment) to review with the child, each other, the teacher, or you is key to understanding the child with ASD and successfully shifting his behavior.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
Alternative therapies
Alternative therapies, from vitamins and supplements to meditation and acupuncture, have become increasingly popular treatments in the United States for many medical problems in the past few decades. In 2008, the National Institutes of Health reported that nearly 40% of adults and 12% of children had used “complementary or alternative medicine” (CAM) in the preceding year. Other surveys have suggested that closer to 30% of general pediatric patients and as many as 75% of adolescent patients have used CAM at least once. These treatments are especially popular for chronic conditions that are managed but not usually cured with current evidence-based treatments. Psychiatric conditions in childhood sometimes have a long course, and have effective but controversial treatments, as with stimulants for ADHD. Parents sometimes feel guilty about their child’s problem and want to use “natural” methods or deny the accepted understanding of their child’s illness. So it is not surprising that families may investigate alternative treatments, and such treatments have multiplied.
While there is evidence that parents and patients rarely discuss these treatments with their physicians, it is critical that you know what therapies your patients are using. You should focus on tolerance in the context of protecting the child from harm and improving the child’s functioning. If you have ever recommended chicken soup for a cold, then you have prescribed complementary medicine, so it is not a stretch for you to offer some input about the other alternative therapies your patients may be considering.
It is important to note that rigorous, case-controlled studies of efficacy of most alternative therapies are few in number and usually small in size (so any evidence of efficacy is weaker), and that the products themselves are not regulated by the Food and Drug Administration or other public body. This means that the family (and you) will have to do some homework to ensure that the therapy they purchase comes from a reputable source and is what it purports to be.
Many of the alternative therapies patients are investigating will be herbs or supplements. Omega-3 fatty acids are critical to multiple essential body functions, and are taken in primarily via certain foods, primarily fish and certain seeds and nuts. A deficiency in certain omega-3 fatty acids can cause problems in infant neurological development and put one at risk for heart disease, rheumatologic illness, and depression. Supplementation with Omega-3 fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA], specifically) has a solid evidence base as an effective adjunctive treatment for depression and bipolar disorder in adults. In addition, randomized, placebo-controlled, double-blind studies have demonstrated efficacy in treatment of children with mild to moderate ADHD at doses of 1,200 mg/day. There are some studies that have demonstrated improvement in hyperactivity in children with autism with supplementation at similar doses. These supplements have very low risk of side effects. They are a reasonable recommendation to your patients whose children have mild to moderate ADHD, and they want to manage it without stimulants.
Families also may be considering physical or mechanical treatments. Acupuncture has demonstrated efficacy in the treatment of fatigue and pain, migraines, and addiction, although there are very few studies in children and adolescents. There is some evidence for its efficacy in treatment of mild to moderate depression and anxiety in adults, but again no research has been done in youth. Hypnotherapy has shown modest efficacy in treatment of anticipatory anxiety symptoms, headache, chronic pain, nausea and vomiting, migraines, hair-pulling and skin picking as well as compulsive eating and smoking cessation in adults. There is some clinical evidence for its efficacy in children and adolescents, and its safety is well established. Massage therapy has shown value in improving mood and behavior in children with ADHD, but not efficacy as a first-line treatment for ADHD symptoms. Chiropractic care, which is among the most commonly used alternative therapies, claims to be effective for the treatment of anxiety, depression, ADHD, behavioral problems of autism and even schizophrenia and bipolar disorder, but there is no significant scientific evidence to support these claims. And neurofeedback, which is a variant of biofeedback in which patients practice calming themselves or improving focus while watching an EEG has shown modest efficacy in the treatment of ADHD in children in early studies. It is worth noting that all of these therapies may be costly and not covered by insurance.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Additional readings
1. Child Adolesc Psychiatr Clin N Am. 2013 Jul;22(3):375-80.
2. J Am Acad Child Adolesc Psychiatry. 2008;47(4):364-8.
3. J Am Acad Child Adolesc Psychiatry. 2011;50(10):991-1000.
4. J Am Acad Child Adolesc Psychiatry. 2014 Jun; 53(6):658-66.
5. J Am Acad Child Adolesc Psychiatry. 2016 Oct;55(10):S168-9.
Alternative therapies, from vitamins and supplements to meditation and acupuncture, have become increasingly popular treatments in the United States for many medical problems in the past few decades. In 2008, the National Institutes of Health reported that nearly 40% of adults and 12% of children had used “complementary or alternative medicine” (CAM) in the preceding year. Other surveys have suggested that closer to 30% of general pediatric patients and as many as 75% of adolescent patients have used CAM at least once. These treatments are especially popular for chronic conditions that are managed but not usually cured with current evidence-based treatments. Psychiatric conditions in childhood sometimes have a long course, and have effective but controversial treatments, as with stimulants for ADHD. Parents sometimes feel guilty about their child’s problem and want to use “natural” methods or deny the accepted understanding of their child’s illness. So it is not surprising that families may investigate alternative treatments, and such treatments have multiplied.
While there is evidence that parents and patients rarely discuss these treatments with their physicians, it is critical that you know what therapies your patients are using. You should focus on tolerance in the context of protecting the child from harm and improving the child’s functioning. If you have ever recommended chicken soup for a cold, then you have prescribed complementary medicine, so it is not a stretch for you to offer some input about the other alternative therapies your patients may be considering.
It is important to note that rigorous, case-controlled studies of efficacy of most alternative therapies are few in number and usually small in size (so any evidence of efficacy is weaker), and that the products themselves are not regulated by the Food and Drug Administration or other public body. This means that the family (and you) will have to do some homework to ensure that the therapy they purchase comes from a reputable source and is what it purports to be.
Many of the alternative therapies patients are investigating will be herbs or supplements. Omega-3 fatty acids are critical to multiple essential body functions, and are taken in primarily via certain foods, primarily fish and certain seeds and nuts. A deficiency in certain omega-3 fatty acids can cause problems in infant neurological development and put one at risk for heart disease, rheumatologic illness, and depression. Supplementation with Omega-3 fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA], specifically) has a solid evidence base as an effective adjunctive treatment for depression and bipolar disorder in adults. In addition, randomized, placebo-controlled, double-blind studies have demonstrated efficacy in treatment of children with mild to moderate ADHD at doses of 1,200 mg/day. There are some studies that have demonstrated improvement in hyperactivity in children with autism with supplementation at similar doses. These supplements have very low risk of side effects. They are a reasonable recommendation to your patients whose children have mild to moderate ADHD, and they want to manage it without stimulants.
Families also may be considering physical or mechanical treatments. Acupuncture has demonstrated efficacy in the treatment of fatigue and pain, migraines, and addiction, although there are very few studies in children and adolescents. There is some evidence for its efficacy in treatment of mild to moderate depression and anxiety in adults, but again no research has been done in youth. Hypnotherapy has shown modest efficacy in treatment of anticipatory anxiety symptoms, headache, chronic pain, nausea and vomiting, migraines, hair-pulling and skin picking as well as compulsive eating and smoking cessation in adults. There is some clinical evidence for its efficacy in children and adolescents, and its safety is well established. Massage therapy has shown value in improving mood and behavior in children with ADHD, but not efficacy as a first-line treatment for ADHD symptoms. Chiropractic care, which is among the most commonly used alternative therapies, claims to be effective for the treatment of anxiety, depression, ADHD, behavioral problems of autism and even schizophrenia and bipolar disorder, but there is no significant scientific evidence to support these claims. And neurofeedback, which is a variant of biofeedback in which patients practice calming themselves or improving focus while watching an EEG has shown modest efficacy in the treatment of ADHD in children in early studies. It is worth noting that all of these therapies may be costly and not covered by insurance.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Additional readings
1. Child Adolesc Psychiatr Clin N Am. 2013 Jul;22(3):375-80.
2. J Am Acad Child Adolesc Psychiatry. 2008;47(4):364-8.
3. J Am Acad Child Adolesc Psychiatry. 2011;50(10):991-1000.
4. J Am Acad Child Adolesc Psychiatry. 2014 Jun; 53(6):658-66.
5. J Am Acad Child Adolesc Psychiatry. 2016 Oct;55(10):S168-9.
Alternative therapies, from vitamins and supplements to meditation and acupuncture, have become increasingly popular treatments in the United States for many medical problems in the past few decades. In 2008, the National Institutes of Health reported that nearly 40% of adults and 12% of children had used “complementary or alternative medicine” (CAM) in the preceding year. Other surveys have suggested that closer to 30% of general pediatric patients and as many as 75% of adolescent patients have used CAM at least once. These treatments are especially popular for chronic conditions that are managed but not usually cured with current evidence-based treatments. Psychiatric conditions in childhood sometimes have a long course, and have effective but controversial treatments, as with stimulants for ADHD. Parents sometimes feel guilty about their child’s problem and want to use “natural” methods or deny the accepted understanding of their child’s illness. So it is not surprising that families may investigate alternative treatments, and such treatments have multiplied.
While there is evidence that parents and patients rarely discuss these treatments with their physicians, it is critical that you know what therapies your patients are using. You should focus on tolerance in the context of protecting the child from harm and improving the child’s functioning. If you have ever recommended chicken soup for a cold, then you have prescribed complementary medicine, so it is not a stretch for you to offer some input about the other alternative therapies your patients may be considering.
It is important to note that rigorous, case-controlled studies of efficacy of most alternative therapies are few in number and usually small in size (so any evidence of efficacy is weaker), and that the products themselves are not regulated by the Food and Drug Administration or other public body. This means that the family (and you) will have to do some homework to ensure that the therapy they purchase comes from a reputable source and is what it purports to be.
Many of the alternative therapies patients are investigating will be herbs or supplements. Omega-3 fatty acids are critical to multiple essential body functions, and are taken in primarily via certain foods, primarily fish and certain seeds and nuts. A deficiency in certain omega-3 fatty acids can cause problems in infant neurological development and put one at risk for heart disease, rheumatologic illness, and depression. Supplementation with Omega-3 fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA], specifically) has a solid evidence base as an effective adjunctive treatment for depression and bipolar disorder in adults. In addition, randomized, placebo-controlled, double-blind studies have demonstrated efficacy in treatment of children with mild to moderate ADHD at doses of 1,200 mg/day. There are some studies that have demonstrated improvement in hyperactivity in children with autism with supplementation at similar doses. These supplements have very low risk of side effects. They are a reasonable recommendation to your patients whose children have mild to moderate ADHD, and they want to manage it without stimulants.
Families also may be considering physical or mechanical treatments. Acupuncture has demonstrated efficacy in the treatment of fatigue and pain, migraines, and addiction, although there are very few studies in children and adolescents. There is some evidence for its efficacy in treatment of mild to moderate depression and anxiety in adults, but again no research has been done in youth. Hypnotherapy has shown modest efficacy in treatment of anticipatory anxiety symptoms, headache, chronic pain, nausea and vomiting, migraines, hair-pulling and skin picking as well as compulsive eating and smoking cessation in adults. There is some clinical evidence for its efficacy in children and adolescents, and its safety is well established. Massage therapy has shown value in improving mood and behavior in children with ADHD, but not efficacy as a first-line treatment for ADHD symptoms. Chiropractic care, which is among the most commonly used alternative therapies, claims to be effective for the treatment of anxiety, depression, ADHD, behavioral problems of autism and even schizophrenia and bipolar disorder, but there is no significant scientific evidence to support these claims. And neurofeedback, which is a variant of biofeedback in which patients practice calming themselves or improving focus while watching an EEG has shown modest efficacy in the treatment of ADHD in children in early studies. It is worth noting that all of these therapies may be costly and not covered by insurance.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Additional readings
1. Child Adolesc Psychiatr Clin N Am. 2013 Jul;22(3):375-80.
2. J Am Acad Child Adolesc Psychiatry. 2008;47(4):364-8.
3. J Am Acad Child Adolesc Psychiatry. 2011;50(10):991-1000.
4. J Am Acad Child Adolesc Psychiatry. 2014 Jun; 53(6):658-66.
5. J Am Acad Child Adolesc Psychiatry. 2016 Oct;55(10):S168-9.
Mindfulness and child health
If you are struggling to figure out how you, as an individual pediatrician, can make a significant impact on the most common current issues in child health of anxiety, depression, sleep problems, stress, and even adverse childhood experiences, you are not alone. Many of the problems we see in the office appear to stem so much from the culture in which we live that the medical interventions we have to offer seem paltry. Yet we strive to identify and attempt to ameliorate the child’s and family’s distress.
Real physical danger aside, a lot of personal distress is due to negative thoughts about one’s past or fears for one’s future. These thoughts are very important in restraining us from repeating mistakes and preparing us for action to prevent future harm. But the thoughts themselves can be stressful; they may paralyze us with anxiety, take away pleasure, interrupt our sleep, stimulate physiologic stress responses, and have adverse impacts on health. All these effects can occur without actually changing the course of events! How can we advise our patients and their parents to work to balance the protective function of our thoughts against the cost to our well-being?
One promising method you can confidently recommend to both children and their parents to manage stressful thinking is to learn and practice mindfulness. Mindfulness refers to a state of nonreactivity, awareness, focus, attention, and nonjudgment. Noticing thoughts and feelings passing through us with a neutral mind, as if we were watching a movie, rather than taking them personally, is the goal. Jon Kabat-Zinn, PhD, learned from Buddhists, then developed and disseminated a formal program to teach this skill called mindfulness-based stress reduction; it has yielded significant benefits to the emotions and health of adult participants. While everyone can be mindful at times, the ability to enter this state at will and maintain it for a few minutes can be learned, even by preschool children.
How am I going to refer my patients to mindfulness programs, I can hear you saying, when I can’t even get them to standard therapies? Mindfulness in a less-structured format is often part of yoga or Tai Chi, meditation, art therapy, group therapy, or even religious services. Fortunately, parents and educators also can teach children mindfulness. But the first way you can start making this life skill available to your patients is by recommending it to their parents (“The Family ADHD Solution” by Mark Bertin [New York: Palgrave MacMillan, 2011]).
You know that child emotional or behavior problems can cause adult stress. But adult stress also can cause or exacerbate a child’s emotional or behavior problems. Adult caregivers modeling meltdowns are shaping the minds of their children. Studies of teaching mindfulness to parents of children with developmental disabilities, autism, and ADHD, without touching the underlying disorder, show significant reductions in both adult stress and child behavior problems. Parents who can suspend emotion, take some deep breaths, and be thoughtful about the response they want to make instead of reacting impulsively act more reasonably, appear warmer and more compassionate to their children, and are often rewarded with better behavior. Such parents may feel better about themselves and their parenting, may experience less stress, and may themselves sleep better at night!
For children, having an adult simply declare moments to stop, take deep breaths, and notice the sounds, sights, feelings, and smells around them is a good start. Making a routine of taking an “awareness walk” around the block can be another lesson. Eating a food, such as a strawberry, mindfully – observing and savoring every bite – is another natural opportunity to practice increased awareness. One of my favorite tools, having a child shake a glitter globe (like a snow globe that can be made at home) and silently wait for the chaos to subside, “just like their feelings inside,” is soothing and a great metaphor! Abdominal breathing, part of many relaxation exercises, may be hard for young children to master. A parent might try having the child lie down with a stuffed animal on his or her belly and focus on watching it rise and fall while breathing as a way to learn this. For older children, keeping a “gratitude journal” helps focus on the positive, and also has some proven efficacy in relieving depression. Using the “1 Second Everyday” app to video a special moment daily may have a similar effect on sharpening awareness.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
If you are struggling to figure out how you, as an individual pediatrician, can make a significant impact on the most common current issues in child health of anxiety, depression, sleep problems, stress, and even adverse childhood experiences, you are not alone. Many of the problems we see in the office appear to stem so much from the culture in which we live that the medical interventions we have to offer seem paltry. Yet we strive to identify and attempt to ameliorate the child’s and family’s distress.
Real physical danger aside, a lot of personal distress is due to negative thoughts about one’s past or fears for one’s future. These thoughts are very important in restraining us from repeating mistakes and preparing us for action to prevent future harm. But the thoughts themselves can be stressful; they may paralyze us with anxiety, take away pleasure, interrupt our sleep, stimulate physiologic stress responses, and have adverse impacts on health. All these effects can occur without actually changing the course of events! How can we advise our patients and their parents to work to balance the protective function of our thoughts against the cost to our well-being?
One promising method you can confidently recommend to both children and their parents to manage stressful thinking is to learn and practice mindfulness. Mindfulness refers to a state of nonreactivity, awareness, focus, attention, and nonjudgment. Noticing thoughts and feelings passing through us with a neutral mind, as if we were watching a movie, rather than taking them personally, is the goal. Jon Kabat-Zinn, PhD, learned from Buddhists, then developed and disseminated a formal program to teach this skill called mindfulness-based stress reduction; it has yielded significant benefits to the emotions and health of adult participants. While everyone can be mindful at times, the ability to enter this state at will and maintain it for a few minutes can be learned, even by preschool children.
How am I going to refer my patients to mindfulness programs, I can hear you saying, when I can’t even get them to standard therapies? Mindfulness in a less-structured format is often part of yoga or Tai Chi, meditation, art therapy, group therapy, or even religious services. Fortunately, parents and educators also can teach children mindfulness. But the first way you can start making this life skill available to your patients is by recommending it to their parents (“The Family ADHD Solution” by Mark Bertin [New York: Palgrave MacMillan, 2011]).
You know that child emotional or behavior problems can cause adult stress. But adult stress also can cause or exacerbate a child’s emotional or behavior problems. Adult caregivers modeling meltdowns are shaping the minds of their children. Studies of teaching mindfulness to parents of children with developmental disabilities, autism, and ADHD, without touching the underlying disorder, show significant reductions in both adult stress and child behavior problems. Parents who can suspend emotion, take some deep breaths, and be thoughtful about the response they want to make instead of reacting impulsively act more reasonably, appear warmer and more compassionate to their children, and are often rewarded with better behavior. Such parents may feel better about themselves and their parenting, may experience less stress, and may themselves sleep better at night!
For children, having an adult simply declare moments to stop, take deep breaths, and notice the sounds, sights, feelings, and smells around them is a good start. Making a routine of taking an “awareness walk” around the block can be another lesson. Eating a food, such as a strawberry, mindfully – observing and savoring every bite – is another natural opportunity to practice increased awareness. One of my favorite tools, having a child shake a glitter globe (like a snow globe that can be made at home) and silently wait for the chaos to subside, “just like their feelings inside,” is soothing and a great metaphor! Abdominal breathing, part of many relaxation exercises, may be hard for young children to master. A parent might try having the child lie down with a stuffed animal on his or her belly and focus on watching it rise and fall while breathing as a way to learn this. For older children, keeping a “gratitude journal” helps focus on the positive, and also has some proven efficacy in relieving depression. Using the “1 Second Everyday” app to video a special moment daily may have a similar effect on sharpening awareness.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
If you are struggling to figure out how you, as an individual pediatrician, can make a significant impact on the most common current issues in child health of anxiety, depression, sleep problems, stress, and even adverse childhood experiences, you are not alone. Many of the problems we see in the office appear to stem so much from the culture in which we live that the medical interventions we have to offer seem paltry. Yet we strive to identify and attempt to ameliorate the child’s and family’s distress.
Real physical danger aside, a lot of personal distress is due to negative thoughts about one’s past or fears for one’s future. These thoughts are very important in restraining us from repeating mistakes and preparing us for action to prevent future harm. But the thoughts themselves can be stressful; they may paralyze us with anxiety, take away pleasure, interrupt our sleep, stimulate physiologic stress responses, and have adverse impacts on health. All these effects can occur without actually changing the course of events! How can we advise our patients and their parents to work to balance the protective function of our thoughts against the cost to our well-being?
One promising method you can confidently recommend to both children and their parents to manage stressful thinking is to learn and practice mindfulness. Mindfulness refers to a state of nonreactivity, awareness, focus, attention, and nonjudgment. Noticing thoughts and feelings passing through us with a neutral mind, as if we were watching a movie, rather than taking them personally, is the goal. Jon Kabat-Zinn, PhD, learned from Buddhists, then developed and disseminated a formal program to teach this skill called mindfulness-based stress reduction; it has yielded significant benefits to the emotions and health of adult participants. While everyone can be mindful at times, the ability to enter this state at will and maintain it for a few minutes can be learned, even by preschool children.
How am I going to refer my patients to mindfulness programs, I can hear you saying, when I can’t even get them to standard therapies? Mindfulness in a less-structured format is often part of yoga or Tai Chi, meditation, art therapy, group therapy, or even religious services. Fortunately, parents and educators also can teach children mindfulness. But the first way you can start making this life skill available to your patients is by recommending it to their parents (“The Family ADHD Solution” by Mark Bertin [New York: Palgrave MacMillan, 2011]).
You know that child emotional or behavior problems can cause adult stress. But adult stress also can cause or exacerbate a child’s emotional or behavior problems. Adult caregivers modeling meltdowns are shaping the minds of their children. Studies of teaching mindfulness to parents of children with developmental disabilities, autism, and ADHD, without touching the underlying disorder, show significant reductions in both adult stress and child behavior problems. Parents who can suspend emotion, take some deep breaths, and be thoughtful about the response they want to make instead of reacting impulsively act more reasonably, appear warmer and more compassionate to their children, and are often rewarded with better behavior. Such parents may feel better about themselves and their parenting, may experience less stress, and may themselves sleep better at night!
For children, having an adult simply declare moments to stop, take deep breaths, and notice the sounds, sights, feelings, and smells around them is a good start. Making a routine of taking an “awareness walk” around the block can be another lesson. Eating a food, such as a strawberry, mindfully – observing and savoring every bite – is another natural opportunity to practice increased awareness. One of my favorite tools, having a child shake a glitter globe (like a snow globe that can be made at home) and silently wait for the chaos to subside, “just like their feelings inside,” is soothing and a great metaphor! Abdominal breathing, part of many relaxation exercises, may be hard for young children to master. A parent might try having the child lie down with a stuffed animal on his or her belly and focus on watching it rise and fall while breathing as a way to learn this. For older children, keeping a “gratitude journal” helps focus on the positive, and also has some proven efficacy in relieving depression. Using the “1 Second Everyday” app to video a special moment daily may have a similar effect on sharpening awareness.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News.
Depression in adolescence
As many as 20% of children and adolescents experience a psychiatric disorder, with 50% of all lifetime psychiatric illnesses occurring by the age of 14 years. ADHD and depression are among the most common. The National Institutes of Health estimate that, in 2015, 3 million 12- to 17-year-old American children experienced a major depressive episode. Any illness that affects over 10% of adolescents will present regularly in the primary care provider’s office. It is important to know whom to screen and how to start treatment when your patient appears to be suffering from this serious but treatable condition.
While there are many screening instruments, it is important to be ready to ask patients diagnostic questions when your clinical suspicion of depression is high. In addition to asking about mood, sleep, appetite, energy, and the other DSM5 criteria of a major depressive episode, it is important to remember that teens with depression might present with irritability as much as sadness. While they lose interest in school, sports, or hobbies, they still may be distracted or cheered up by friends. And
Explain to your patient (and their parents) that depression is very treatable, but most effective treatments take time. Psychotherapy usually works over several months, and even effective medications can take 6 weeks or more. But, without treatment, their symptoms may persist for over a year and can disrupt their healthy development.
This is also a good time to ask your patient about suicidal thoughts. Have they been imagining how their death would affect others? Wishing they could just sleep? Do they have a plan? Do they have access to a means of killing themselves? Do they feel attached or connected to family, friends, religion, or a goal? Explain to your patient that these thoughts are common symptoms of depression, and work with their parents to ensure that they are connected and safe when starting treatment.
Psychotherapy is considered the first line treatment for mild to moderate episodes of depression and should be used alongside medications in severe episodes. While structured therapies such as cognitive behavioral therapy or interpersonal therapy have a strong evidence base to support their use, the best predictor of an effective therapy appears to be a strong alliance between therapist and patient. So, help your patient to find a therapist, and explain the importance of finding someone with whom they feel comfortable. Suggest to your patients that they have three visits with a new therapist to see if it feels like a “good match,” before considering trying another.
Finally, antidepressant medications are first-line treatment for more severe episodes of depression and episodes in which significant suicidal ideation or functional impairment are present. If the symptoms are more severe, or if therapy alone has not been effective after 4-6 weeks, you might consider starting antidepressant treatment. Psychiatrists usually start with an selective serotonin reuptake inhibitor, typically of a medium half-life, at a low dose to minimize the chances of side effects. While real efficacy takes up to 6 weeks, there should be some improvement in energy within the first 2 weeks on an effective medication. If there is no change, the dose can be raised gradually as tolerated. It is important to tell patients and their families about common side effects (mild GI upset) and the more rare but dangerous ones (such as hypomania or an increase in the frequency or intensity of suicidal thoughts).
Even when you do not refer your patient to someone else for treatment of depression, it is important that you not be alone in their management. Work closely with their therapist or consider having a psychiatric social worker join your team to offer therapy in close connection with your management. You might also periodically consult with a child psychiatrist to address treatment and medication questions and identify needed resources. Staying in touch with parents or connected adults at school (with the appropriate permission) can be very useful with those patients you are more concerned about. The educated and attuned primary care provider can provide thoughtful first-line treatment of depression in young people and can be an important part of managing this public health challenge. It is always rewarding to help an adolescent overcome depression.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
As many as 20% of children and adolescents experience a psychiatric disorder, with 50% of all lifetime psychiatric illnesses occurring by the age of 14 years. ADHD and depression are among the most common. The National Institutes of Health estimate that, in 2015, 3 million 12- to 17-year-old American children experienced a major depressive episode. Any illness that affects over 10% of adolescents will present regularly in the primary care provider’s office. It is important to know whom to screen and how to start treatment when your patient appears to be suffering from this serious but treatable condition.
While there are many screening instruments, it is important to be ready to ask patients diagnostic questions when your clinical suspicion of depression is high. In addition to asking about mood, sleep, appetite, energy, and the other DSM5 criteria of a major depressive episode, it is important to remember that teens with depression might present with irritability as much as sadness. While they lose interest in school, sports, or hobbies, they still may be distracted or cheered up by friends. And
Explain to your patient (and their parents) that depression is very treatable, but most effective treatments take time. Psychotherapy usually works over several months, and even effective medications can take 6 weeks or more. But, without treatment, their symptoms may persist for over a year and can disrupt their healthy development.
This is also a good time to ask your patient about suicidal thoughts. Have they been imagining how their death would affect others? Wishing they could just sleep? Do they have a plan? Do they have access to a means of killing themselves? Do they feel attached or connected to family, friends, religion, or a goal? Explain to your patient that these thoughts are common symptoms of depression, and work with their parents to ensure that they are connected and safe when starting treatment.
Psychotherapy is considered the first line treatment for mild to moderate episodes of depression and should be used alongside medications in severe episodes. While structured therapies such as cognitive behavioral therapy or interpersonal therapy have a strong evidence base to support their use, the best predictor of an effective therapy appears to be a strong alliance between therapist and patient. So, help your patient to find a therapist, and explain the importance of finding someone with whom they feel comfortable. Suggest to your patients that they have three visits with a new therapist to see if it feels like a “good match,” before considering trying another.
Finally, antidepressant medications are first-line treatment for more severe episodes of depression and episodes in which significant suicidal ideation or functional impairment are present. If the symptoms are more severe, or if therapy alone has not been effective after 4-6 weeks, you might consider starting antidepressant treatment. Psychiatrists usually start with an selective serotonin reuptake inhibitor, typically of a medium half-life, at a low dose to minimize the chances of side effects. While real efficacy takes up to 6 weeks, there should be some improvement in energy within the first 2 weeks on an effective medication. If there is no change, the dose can be raised gradually as tolerated. It is important to tell patients and their families about common side effects (mild GI upset) and the more rare but dangerous ones (such as hypomania or an increase in the frequency or intensity of suicidal thoughts).
Even when you do not refer your patient to someone else for treatment of depression, it is important that you not be alone in their management. Work closely with their therapist or consider having a psychiatric social worker join your team to offer therapy in close connection with your management. You might also periodically consult with a child psychiatrist to address treatment and medication questions and identify needed resources. Staying in touch with parents or connected adults at school (with the appropriate permission) can be very useful with those patients you are more concerned about. The educated and attuned primary care provider can provide thoughtful first-line treatment of depression in young people and can be an important part of managing this public health challenge. It is always rewarding to help an adolescent overcome depression.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
As many as 20% of children and adolescents experience a psychiatric disorder, with 50% of all lifetime psychiatric illnesses occurring by the age of 14 years. ADHD and depression are among the most common. The National Institutes of Health estimate that, in 2015, 3 million 12- to 17-year-old American children experienced a major depressive episode. Any illness that affects over 10% of adolescents will present regularly in the primary care provider’s office. It is important to know whom to screen and how to start treatment when your patient appears to be suffering from this serious but treatable condition.
While there are many screening instruments, it is important to be ready to ask patients diagnostic questions when your clinical suspicion of depression is high. In addition to asking about mood, sleep, appetite, energy, and the other DSM5 criteria of a major depressive episode, it is important to remember that teens with depression might present with irritability as much as sadness. While they lose interest in school, sports, or hobbies, they still may be distracted or cheered up by friends. And
Explain to your patient (and their parents) that depression is very treatable, but most effective treatments take time. Psychotherapy usually works over several months, and even effective medications can take 6 weeks or more. But, without treatment, their symptoms may persist for over a year and can disrupt their healthy development.
This is also a good time to ask your patient about suicidal thoughts. Have they been imagining how their death would affect others? Wishing they could just sleep? Do they have a plan? Do they have access to a means of killing themselves? Do they feel attached or connected to family, friends, religion, or a goal? Explain to your patient that these thoughts are common symptoms of depression, and work with their parents to ensure that they are connected and safe when starting treatment.
Psychotherapy is considered the first line treatment for mild to moderate episodes of depression and should be used alongside medications in severe episodes. While structured therapies such as cognitive behavioral therapy or interpersonal therapy have a strong evidence base to support their use, the best predictor of an effective therapy appears to be a strong alliance between therapist and patient. So, help your patient to find a therapist, and explain the importance of finding someone with whom they feel comfortable. Suggest to your patients that they have three visits with a new therapist to see if it feels like a “good match,” before considering trying another.
Finally, antidepressant medications are first-line treatment for more severe episodes of depression and episodes in which significant suicidal ideation or functional impairment are present. If the symptoms are more severe, or if therapy alone has not been effective after 4-6 weeks, you might consider starting antidepressant treatment. Psychiatrists usually start with an selective serotonin reuptake inhibitor, typically of a medium half-life, at a low dose to minimize the chances of side effects. While real efficacy takes up to 6 weeks, there should be some improvement in energy within the first 2 weeks on an effective medication. If there is no change, the dose can be raised gradually as tolerated. It is important to tell patients and their families about common side effects (mild GI upset) and the more rare but dangerous ones (such as hypomania or an increase in the frequency or intensity of suicidal thoughts).
Even when you do not refer your patient to someone else for treatment of depression, it is important that you not be alone in their management. Work closely with their therapist or consider having a psychiatric social worker join your team to offer therapy in close connection with your management. You might also periodically consult with a child psychiatrist to address treatment and medication questions and identify needed resources. Staying in touch with parents or connected adults at school (with the appropriate permission) can be very useful with those patients you are more concerned about. The educated and attuned primary care provider can provide thoughtful first-line treatment of depression in young people and can be an important part of managing this public health challenge. It is always rewarding to help an adolescent overcome depression.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Solving stool refusal
When parents bring in their delightful, verbal 3-year-old for refusing to poop on the potty, it may seem laughable. But with impending preschool and costs of diapers, stool refusal can be a major aggravation for families! Fortunately,
Commonly a healthy, typically developing boy stands and urinates in the toilet just fine, but sneaks off behind the sofa to poop. Parent gyrations have gone from cajoling, to punishing, to offering trips to Disney! Flaring tempers can set the stage for stool refusal to be a power play.
There are a number of reasons stool refusal may give clues to child and family tendencies and relevant intervention. We always should be alert to rare medical problems such as Hirschsprung disease or traumas (from slammed toilet lids to sexual abuse). But while learning to use the toilet for urination and defecation generally occur around the same time, there are pitfalls making pooping in the potty different. An impending stool provides stronger sensations and more advance warning than urine and tends to come at regular times, making it logical to start toilet learning with sitting on the potty after meals.
But once seated on the potty, stools can require some waiting – not a typical toddler forte! While running to sit has novelty at first and may be reinforced by celebration, this quickly becomes routine and boring. Very active or very intense children especially hate having their play interrupted by a trip to the bathroom. Oppositional children just won’t perform if they think the parent cares! And unlike for urination, everyone can inhibit defecation long enough for the urge to pass. Repeated stool retention from ignoring the urge makes stools dessicated and harder, with resulting pain when finally passed. One painful stool makes many a young child decide “Never again!” and simply refuse the toilet. A rectal fissure can both start
During unclogging and establishing a new stool pattern, the toddler should be matter-of-factly put back in diapers (not pull ups) saying “Oh well, you are just not ready for pants yet.” Dramatically placing the treasured Superhero underwear on the top shelf increases motivation (or promised if none have been acquired). Returning to diapers without shaming the child is key, and all caregivers need to buy in. They need to be good “actors,” conveying that they don’t really care about toileting to reduce the power struggle. If controlling poop is a battle, only the child can win!
When the soft stools are occurring several times per day, I suggest “M&M treatment”: 1 for sitting, 2 for peeing, and 3 for pooping = 6 potential M&Ms per episode. The “1 for sitting” (the easiest part), is not painful and restores the habit of complying. Remember, M&Ms are no match for a game on an iPad! By charting the times of stools, the parent can remove electronics ½ hour before the expected poop and restrict the child to one room of the house with a potty nearby. Parents can interact, but should avoid making this a rewarding playtime. When the child uses the potty rather than their pants, the room restriction is removed until the next window for pooping. If they poop outside the toilet, they remain restricted (and no electronics) until the next window (even the next day).
Some parents are especially sensitive to the smell and mess of stools and pass that attitude along to their child by saying “Ugh, you stink!” or “I can’t stand this mess!” or even handing the child to another caregiver in a gesture of rejection. These messages are not missed by the child, who may then not want to deal with the mess, either. I coach parents to stay at least neutral about stools, reminding them that, “Your child is going to have to poop her whole life!”
Demanding a diaper and then getting the special intimacy of bottom cleaning can be reinforcing. If there is a younger sibling, diaper changes may be a desired opportunity for the toddler to regress and retain some “baby privileges.” Other clues to this dynamic include thumb sucking, baby talk, clinginess, or being rough on the sibling. One part of addressing this issue is to prescribe “babying” the toddler by holding in arms, rocking, talking baby talk, offering a pacifier, and feeding him during daily parent-child one-on-one Special Time. This sounds crazy to parents aiming for grown up toileting, but I promise them the child will not go backwards! It addresses the child’s deep fear that the nurturing of infancy is no longer available.
You may have noticed that boys are much more likely to refuse stools than girls. Some of this difference may be that high activity, but learning to urinate standing up also is fun, a Big Boy feat, and a source of pride to fathers. If regular sitting to poop has not been well established before the fun of standing to pee is offered, the little guys are not so interested in sitting again to poop. Plus the wiping and hand washing after poops are further aggravations delaying return to the Legos. But more! By around age 3 years, both genders make the horrifying discovery that boys have a penis and girls don’t. At this age of confusion about potential transformations, the obvious conclusion is that the girl’s penis was lost! And that turd disappearing down the toilet looks a lot like a dismembered body part! Reassurance and education is in order. I address this with my “Penis Talk”: “Boys are made with a penis and girls are made with a vagina. (For boys:) When you get big like your Dad, your penis will be big, too. No one can ever take your penis away. (For girls, a less common concern.) You have always had a vagina. You did not lose a penis.” I recommend that you practice this in front of a mirror before first use!
Another cognitive milestone concerns what sorts of things can disappear dow
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at pdnews@frontlinemedcom.com.
When parents bring in their delightful, verbal 3-year-old for refusing to poop on the potty, it may seem laughable. But with impending preschool and costs of diapers, stool refusal can be a major aggravation for families! Fortunately,
Commonly a healthy, typically developing boy stands and urinates in the toilet just fine, but sneaks off behind the sofa to poop. Parent gyrations have gone from cajoling, to punishing, to offering trips to Disney! Flaring tempers can set the stage for stool refusal to be a power play.
There are a number of reasons stool refusal may give clues to child and family tendencies and relevant intervention. We always should be alert to rare medical problems such as Hirschsprung disease or traumas (from slammed toilet lids to sexual abuse). But while learning to use the toilet for urination and defecation generally occur around the same time, there are pitfalls making pooping in the potty different. An impending stool provides stronger sensations and more advance warning than urine and tends to come at regular times, making it logical to start toilet learning with sitting on the potty after meals.
But once seated on the potty, stools can require some waiting – not a typical toddler forte! While running to sit has novelty at first and may be reinforced by celebration, this quickly becomes routine and boring. Very active or very intense children especially hate having their play interrupted by a trip to the bathroom. Oppositional children just won’t perform if they think the parent cares! And unlike for urination, everyone can inhibit defecation long enough for the urge to pass. Repeated stool retention from ignoring the urge makes stools dessicated and harder, with resulting pain when finally passed. One painful stool makes many a young child decide “Never again!” and simply refuse the toilet. A rectal fissure can both start
During unclogging and establishing a new stool pattern, the toddler should be matter-of-factly put back in diapers (not pull ups) saying “Oh well, you are just not ready for pants yet.” Dramatically placing the treasured Superhero underwear on the top shelf increases motivation (or promised if none have been acquired). Returning to diapers without shaming the child is key, and all caregivers need to buy in. They need to be good “actors,” conveying that they don’t really care about toileting to reduce the power struggle. If controlling poop is a battle, only the child can win!
When the soft stools are occurring several times per day, I suggest “M&M treatment”: 1 for sitting, 2 for peeing, and 3 for pooping = 6 potential M&Ms per episode. The “1 for sitting” (the easiest part), is not painful and restores the habit of complying. Remember, M&Ms are no match for a game on an iPad! By charting the times of stools, the parent can remove electronics ½ hour before the expected poop and restrict the child to one room of the house with a potty nearby. Parents can interact, but should avoid making this a rewarding playtime. When the child uses the potty rather than their pants, the room restriction is removed until the next window for pooping. If they poop outside the toilet, they remain restricted (and no electronics) until the next window (even the next day).
Some parents are especially sensitive to the smell and mess of stools and pass that attitude along to their child by saying “Ugh, you stink!” or “I can’t stand this mess!” or even handing the child to another caregiver in a gesture of rejection. These messages are not missed by the child, who may then not want to deal with the mess, either. I coach parents to stay at least neutral about stools, reminding them that, “Your child is going to have to poop her whole life!”
Demanding a diaper and then getting the special intimacy of bottom cleaning can be reinforcing. If there is a younger sibling, diaper changes may be a desired opportunity for the toddler to regress and retain some “baby privileges.” Other clues to this dynamic include thumb sucking, baby talk, clinginess, or being rough on the sibling. One part of addressing this issue is to prescribe “babying” the toddler by holding in arms, rocking, talking baby talk, offering a pacifier, and feeding him during daily parent-child one-on-one Special Time. This sounds crazy to parents aiming for grown up toileting, but I promise them the child will not go backwards! It addresses the child’s deep fear that the nurturing of infancy is no longer available.
You may have noticed that boys are much more likely to refuse stools than girls. Some of this difference may be that high activity, but learning to urinate standing up also is fun, a Big Boy feat, and a source of pride to fathers. If regular sitting to poop has not been well established before the fun of standing to pee is offered, the little guys are not so interested in sitting again to poop. Plus the wiping and hand washing after poops are further aggravations delaying return to the Legos. But more! By around age 3 years, both genders make the horrifying discovery that boys have a penis and girls don’t. At this age of confusion about potential transformations, the obvious conclusion is that the girl’s penis was lost! And that turd disappearing down the toilet looks a lot like a dismembered body part! Reassurance and education is in order. I address this with my “Penis Talk”: “Boys are made with a penis and girls are made with a vagina. (For boys:) When you get big like your Dad, your penis will be big, too. No one can ever take your penis away. (For girls, a less common concern.) You have always had a vagina. You did not lose a penis.” I recommend that you practice this in front of a mirror before first use!
Another cognitive milestone concerns what sorts of things can disappear dow
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at pdnews@frontlinemedcom.com.
When parents bring in their delightful, verbal 3-year-old for refusing to poop on the potty, it may seem laughable. But with impending preschool and costs of diapers, stool refusal can be a major aggravation for families! Fortunately,
Commonly a healthy, typically developing boy stands and urinates in the toilet just fine, but sneaks off behind the sofa to poop. Parent gyrations have gone from cajoling, to punishing, to offering trips to Disney! Flaring tempers can set the stage for stool refusal to be a power play.
There are a number of reasons stool refusal may give clues to child and family tendencies and relevant intervention. We always should be alert to rare medical problems such as Hirschsprung disease or traumas (from slammed toilet lids to sexual abuse). But while learning to use the toilet for urination and defecation generally occur around the same time, there are pitfalls making pooping in the potty different. An impending stool provides stronger sensations and more advance warning than urine and tends to come at regular times, making it logical to start toilet learning with sitting on the potty after meals.
But once seated on the potty, stools can require some waiting – not a typical toddler forte! While running to sit has novelty at first and may be reinforced by celebration, this quickly becomes routine and boring. Very active or very intense children especially hate having their play interrupted by a trip to the bathroom. Oppositional children just won’t perform if they think the parent cares! And unlike for urination, everyone can inhibit defecation long enough for the urge to pass. Repeated stool retention from ignoring the urge makes stools dessicated and harder, with resulting pain when finally passed. One painful stool makes many a young child decide “Never again!” and simply refuse the toilet. A rectal fissure can both start
During unclogging and establishing a new stool pattern, the toddler should be matter-of-factly put back in diapers (not pull ups) saying “Oh well, you are just not ready for pants yet.” Dramatically placing the treasured Superhero underwear on the top shelf increases motivation (or promised if none have been acquired). Returning to diapers without shaming the child is key, and all caregivers need to buy in. They need to be good “actors,” conveying that they don’t really care about toileting to reduce the power struggle. If controlling poop is a battle, only the child can win!
When the soft stools are occurring several times per day, I suggest “M&M treatment”: 1 for sitting, 2 for peeing, and 3 for pooping = 6 potential M&Ms per episode. The “1 for sitting” (the easiest part), is not painful and restores the habit of complying. Remember, M&Ms are no match for a game on an iPad! By charting the times of stools, the parent can remove electronics ½ hour before the expected poop and restrict the child to one room of the house with a potty nearby. Parents can interact, but should avoid making this a rewarding playtime. When the child uses the potty rather than their pants, the room restriction is removed until the next window for pooping. If they poop outside the toilet, they remain restricted (and no electronics) until the next window (even the next day).
Some parents are especially sensitive to the smell and mess of stools and pass that attitude along to their child by saying “Ugh, you stink!” or “I can’t stand this mess!” or even handing the child to another caregiver in a gesture of rejection. These messages are not missed by the child, who may then not want to deal with the mess, either. I coach parents to stay at least neutral about stools, reminding them that, “Your child is going to have to poop her whole life!”
Demanding a diaper and then getting the special intimacy of bottom cleaning can be reinforcing. If there is a younger sibling, diaper changes may be a desired opportunity for the toddler to regress and retain some “baby privileges.” Other clues to this dynamic include thumb sucking, baby talk, clinginess, or being rough on the sibling. One part of addressing this issue is to prescribe “babying” the toddler by holding in arms, rocking, talking baby talk, offering a pacifier, and feeding him during daily parent-child one-on-one Special Time. This sounds crazy to parents aiming for grown up toileting, but I promise them the child will not go backwards! It addresses the child’s deep fear that the nurturing of infancy is no longer available.
You may have noticed that boys are much more likely to refuse stools than girls. Some of this difference may be that high activity, but learning to urinate standing up also is fun, a Big Boy feat, and a source of pride to fathers. If regular sitting to poop has not been well established before the fun of standing to pee is offered, the little guys are not so interested in sitting again to poop. Plus the wiping and hand washing after poops are further aggravations delaying return to the Legos. But more! By around age 3 years, both genders make the horrifying discovery that boys have a penis and girls don’t. At this age of confusion about potential transformations, the obvious conclusion is that the girl’s penis was lost! And that turd disappearing down the toilet looks a lot like a dismembered body part! Reassurance and education is in order. I address this with my “Penis Talk”: “Boys are made with a penis and girls are made with a vagina. (For boys:) When you get big like your Dad, your penis will be big, too. No one can ever take your penis away. (For girls, a less common concern.) You have always had a vagina. You did not lose a penis.” I recommend that you practice this in front of a mirror before first use!
Another cognitive milestone concerns what sorts of things can disappear dow
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at pdnews@frontlinemedcom.com.
Adolescents and sleep, or the lack thereof
Every parent will attest that bright-eyed children grow into sleepy adolescents, and the science confirms their observations. There are multiple factors that prevent adolescents from getting the sleep they need, and inadequate sleep has serious consequences – from impaired learning to depressive symptoms, obesity to deadly accidents – all of which are potentially preventable with some practical strategies to promote adequate sleep.
Adolescence is a period of intense growth and development, so it is no surprise that adolescents require a lot of sleep, over 9 hours nightly. But surveys have shown that only 3% of American adolescents get 9 hours of sleep nightly, and the average amount of weeknight sleep is only 6 hours.1 Sleep deprivation is not a problem in childhood, so why can’t adolescents get enough sleep?
Over the last 15 years, a new factor – screen time – has worsened the adolescent sleep situation. Most teens have an electronic device in their bedroom and use it for homework, entertainment, and socializing well into the night. Multiple studies have confirmed that electronic exposure in the evening is associated with less sleep at night and more day time sleepiness,by competing with sleep and suppression of nocturnal melatonin release, which can delay the onset of sleep.2
It is ironic that many teens are staying up late for homework, when their lack of sleep can interfere with consolidation of learning. It also has powerful effects on working memory and reaction time, making both academic and athletic performance suffer. Chronically sleep-deprived teenagers often complain of difficulty with initiating and sustaining attention, which may lead to a mistaken diagnosis of ADHD, and stimulant treatment may further complicate sleep.
Good mental health is not the only casualty of inadequate sleep. A growing body of evidence links short sleep duration with an increased risk of obesity. This appears to be mediated by alterations in neurohormones associated with sleep, leading to higher carbohydrate and fat intake, more snacking and insulin resistance.
Anything that compromises attention and reaction time, including sleep deprivation, adds risk to driving, particularly for inexperienced and impulsive adolescent drivers. The National Highway Transportation Safety Administration estimates that drivers 25 and younger cause more than half of all “fall asleep” crashes.
Teenagers generally know that they are exhausted, but the strategies they might use to manage their fatigue can actually make things worse. Sleepy teenagers often consume large amounts of caffeine to get through their days and their homework at night. Caffeine, in turn, interferes with both the onset and quality of sleep, perpetuating the cycle. Even “catch-up” sleep on weekends is a strategy that can contribute to the problem, as it can lead to more disrupted sleep by pushing the onset of school night sleepiness even later.
While growing autonomy is part of why teenagers are sleep deprived, they will consider the caring and informed guidance of their pediatricians about their health. Ask your teenage patients how much sleep they usually get on a school night. It can be validating to show them how sleep deprived they are, and point out how strategies like caffeine and oversleeping might be making it worse. Explain that people (adults, too!) need to make time for sleep just as they might for exercise or friends. Tell them about “good sleep hygiene,” the practice of having consistent sleep times and routines that are conducive to restful sleep. This can include a hot shower before bed, reading for the last 30 minutes before lights out, and no screen time for at least 1 hour before bed. Indeed, it can be powerful to urge that everyone in the family takes screens out of their bedrooms.
Additionally, while they might sleep in on weekends, it shouldn’t be much more than an hour longer than on weekdays. And no naps after school! It is common for teens to feel overwhelmed by their commitments and that sleep must be the first thing to go. Use their growing sense of autonomy to remind them that they get to choose how to use their time, and balance will pay off much more than sacrificing sleep. A practical conversation about sleep can help them to make informed choices and thoughtfully take care of themselves before they head off to college.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Resources
1. “Adolescent Sleep Needs and Patterns: Research Report and Resource Guide.” (Arlington, Va.: National Sleep Foundation, 2000.)
2. Pediatrics. 2014 Sep;134(3):e921-32.
3. Sleep. 2004 Nov 1;27(7):1351-8.
Every parent will attest that bright-eyed children grow into sleepy adolescents, and the science confirms their observations. There are multiple factors that prevent adolescents from getting the sleep they need, and inadequate sleep has serious consequences – from impaired learning to depressive symptoms, obesity to deadly accidents – all of which are potentially preventable with some practical strategies to promote adequate sleep.
Adolescence is a period of intense growth and development, so it is no surprise that adolescents require a lot of sleep, over 9 hours nightly. But surveys have shown that only 3% of American adolescents get 9 hours of sleep nightly, and the average amount of weeknight sleep is only 6 hours.1 Sleep deprivation is not a problem in childhood, so why can’t adolescents get enough sleep?
Over the last 15 years, a new factor – screen time – has worsened the adolescent sleep situation. Most teens have an electronic device in their bedroom and use it for homework, entertainment, and socializing well into the night. Multiple studies have confirmed that electronic exposure in the evening is associated with less sleep at night and more day time sleepiness,by competing with sleep and suppression of nocturnal melatonin release, which can delay the onset of sleep.2
It is ironic that many teens are staying up late for homework, when their lack of sleep can interfere with consolidation of learning. It also has powerful effects on working memory and reaction time, making both academic and athletic performance suffer. Chronically sleep-deprived teenagers often complain of difficulty with initiating and sustaining attention, which may lead to a mistaken diagnosis of ADHD, and stimulant treatment may further complicate sleep.
Good mental health is not the only casualty of inadequate sleep. A growing body of evidence links short sleep duration with an increased risk of obesity. This appears to be mediated by alterations in neurohormones associated with sleep, leading to higher carbohydrate and fat intake, more snacking and insulin resistance.
Anything that compromises attention and reaction time, including sleep deprivation, adds risk to driving, particularly for inexperienced and impulsive adolescent drivers. The National Highway Transportation Safety Administration estimates that drivers 25 and younger cause more than half of all “fall asleep” crashes.
Teenagers generally know that they are exhausted, but the strategies they might use to manage their fatigue can actually make things worse. Sleepy teenagers often consume large amounts of caffeine to get through their days and their homework at night. Caffeine, in turn, interferes with both the onset and quality of sleep, perpetuating the cycle. Even “catch-up” sleep on weekends is a strategy that can contribute to the problem, as it can lead to more disrupted sleep by pushing the onset of school night sleepiness even later.
While growing autonomy is part of why teenagers are sleep deprived, they will consider the caring and informed guidance of their pediatricians about their health. Ask your teenage patients how much sleep they usually get on a school night. It can be validating to show them how sleep deprived they are, and point out how strategies like caffeine and oversleeping might be making it worse. Explain that people (adults, too!) need to make time for sleep just as they might for exercise or friends. Tell them about “good sleep hygiene,” the practice of having consistent sleep times and routines that are conducive to restful sleep. This can include a hot shower before bed, reading for the last 30 minutes before lights out, and no screen time for at least 1 hour before bed. Indeed, it can be powerful to urge that everyone in the family takes screens out of their bedrooms.
Additionally, while they might sleep in on weekends, it shouldn’t be much more than an hour longer than on weekdays. And no naps after school! It is common for teens to feel overwhelmed by their commitments and that sleep must be the first thing to go. Use their growing sense of autonomy to remind them that they get to choose how to use their time, and balance will pay off much more than sacrificing sleep. A practical conversation about sleep can help them to make informed choices and thoughtfully take care of themselves before they head off to college.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Resources
1. “Adolescent Sleep Needs and Patterns: Research Report and Resource Guide.” (Arlington, Va.: National Sleep Foundation, 2000.)
2. Pediatrics. 2014 Sep;134(3):e921-32.
3. Sleep. 2004 Nov 1;27(7):1351-8.
Every parent will attest that bright-eyed children grow into sleepy adolescents, and the science confirms their observations. There are multiple factors that prevent adolescents from getting the sleep they need, and inadequate sleep has serious consequences – from impaired learning to depressive symptoms, obesity to deadly accidents – all of which are potentially preventable with some practical strategies to promote adequate sleep.
Adolescence is a period of intense growth and development, so it is no surprise that adolescents require a lot of sleep, over 9 hours nightly. But surveys have shown that only 3% of American adolescents get 9 hours of sleep nightly, and the average amount of weeknight sleep is only 6 hours.1 Sleep deprivation is not a problem in childhood, so why can’t adolescents get enough sleep?
Over the last 15 years, a new factor – screen time – has worsened the adolescent sleep situation. Most teens have an electronic device in their bedroom and use it for homework, entertainment, and socializing well into the night. Multiple studies have confirmed that electronic exposure in the evening is associated with less sleep at night and more day time sleepiness,by competing with sleep and suppression of nocturnal melatonin release, which can delay the onset of sleep.2
It is ironic that many teens are staying up late for homework, when their lack of sleep can interfere with consolidation of learning. It also has powerful effects on working memory and reaction time, making both academic and athletic performance suffer. Chronically sleep-deprived teenagers often complain of difficulty with initiating and sustaining attention, which may lead to a mistaken diagnosis of ADHD, and stimulant treatment may further complicate sleep.
Good mental health is not the only casualty of inadequate sleep. A growing body of evidence links short sleep duration with an increased risk of obesity. This appears to be mediated by alterations in neurohormones associated with sleep, leading to higher carbohydrate and fat intake, more snacking and insulin resistance.
Anything that compromises attention and reaction time, including sleep deprivation, adds risk to driving, particularly for inexperienced and impulsive adolescent drivers. The National Highway Transportation Safety Administration estimates that drivers 25 and younger cause more than half of all “fall asleep” crashes.
Teenagers generally know that they are exhausted, but the strategies they might use to manage their fatigue can actually make things worse. Sleepy teenagers often consume large amounts of caffeine to get through their days and their homework at night. Caffeine, in turn, interferes with both the onset and quality of sleep, perpetuating the cycle. Even “catch-up” sleep on weekends is a strategy that can contribute to the problem, as it can lead to more disrupted sleep by pushing the onset of school night sleepiness even later.
While growing autonomy is part of why teenagers are sleep deprived, they will consider the caring and informed guidance of their pediatricians about their health. Ask your teenage patients how much sleep they usually get on a school night. It can be validating to show them how sleep deprived they are, and point out how strategies like caffeine and oversleeping might be making it worse. Explain that people (adults, too!) need to make time for sleep just as they might for exercise or friends. Tell them about “good sleep hygiene,” the practice of having consistent sleep times and routines that are conducive to restful sleep. This can include a hot shower before bed, reading for the last 30 minutes before lights out, and no screen time for at least 1 hour before bed. Indeed, it can be powerful to urge that everyone in the family takes screens out of their bedrooms.
Additionally, while they might sleep in on weekends, it shouldn’t be much more than an hour longer than on weekdays. And no naps after school! It is common for teens to feel overwhelmed by their commitments and that sleep must be the first thing to go. Use their growing sense of autonomy to remind them that they get to choose how to use their time, and balance will pay off much more than sacrificing sleep. A practical conversation about sleep can help them to make informed choices and thoughtfully take care of themselves before they head off to college.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@frontlinemedcom.com.
Resources
1. “Adolescent Sleep Needs and Patterns: Research Report and Resource Guide.” (Arlington, Va.: National Sleep Foundation, 2000.)
2. Pediatrics. 2014 Sep;134(3):e921-32.
3. Sleep. 2004 Nov 1;27(7):1351-8.