User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Why Residents Are Joining Unions in Droves
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Before the 350 residents finalized their union contract at the University of Vermont (UVM) Medical Center, Burlington, in 2022, Jesse Mostoller, DO, now a third-year pathology resident, recalls hearing about another resident at the hospital who resorted to moonlighting as an Uber driver to make ends meet.
“In Vermont, rent and childcare are expensive,” said Dr. Mostoller, adding that, thanks to union bargaining, first-year residents at UVM are now paid $71,000 per year instead of $61,000. In addition, residents now receive $1800 per year for food (up from $200-$300 annually) and a $1800 annual fund to help pay for board exams that can be carried over for 2 years. “When we were negotiating, the biggest item on our list of demands was to help alleviate the financial pressure residents have been facing for years.”
The UVM residents’ collective bargaining also includes a cap on working hours so that residents don’t work 80 hours a week, paid parental leave, affordable housing, and funds for education and wellness.
These are some of the most common challenges that are faced by residents all over the country, said A. Taylor Walker, MD, MPH, family medicine chief physician at Tufts University School of Medicine/Cambridge Health Alliance in Boston, Massachusetts, and national president of the Committee of Interns and Residents (CIR), which is part of the Service Employees International Union.
For these reasons, residents at Montefiore Medical Center, Stanford Health Care, George Washington University, and the University of Pennsylvania have recently voted to unionize, according to Dr. Walker.
And while there are several small local unions that have picked up residents at local hospitals, CIR is the largest union of physicians in the United States, with a total of 33,000 residents and fellows across the country (15% of the staff at more than 60 hospitals nationwide).
“We’ve doubled in size in the last 4 years,” said Dr. Walker. “The reason is that we’re in a national reckoning on the corporatization of American medicine and the way in which graduate medical education is rooted in a cycle of exploitation that doesn’t center on the health, well-being, or safety of our doctors and ultimately negatively affects our patients.”
Here’s what residents are fighting for — right now.
Adequate Parental Leave
Christopher Domanski, MD, a first-year resident in psychiatry at California Pacific Medical Center (CPMC) in San Francisco, is also a new dad to a 5-month-old son and is currently in the sixth week of parental leave. One goal of CPMC’s union, started a year and a half ago, is to expand parental leave to 8 weeks.
“I started as a resident here in mid-June, but the fight with CPMC leaders has been going on for a year and a half,” Dr. Domanski said. “It can feel very frustrating because many times there’s no budge in the conversations we want to have.”
Contract negotiations here continue to be slow — and arduous.
“It goes back and forth,” said Dr. Domanski, who makes about $75,000 a year. “Sometimes they listen to our proposals, but they deny the vast majority or make a paltry increase in salary or time off. It goes like this: We’ll have a negotiation; we’ll talk about it, and then they say, ‘we’re not comfortable doing this’ and it stalls again.”
If a resident hasn’t started a family yet, access to fertility benefits and reproductive healthcare is paramount because most residents are in their 20s and 30s, Dr. Walker said.
“Our reproductive futures are really hindered by what care we have access to and what care is covered,” she added. “We don’t make enough money to pay for reproductive care out of pocket.”
Fair Pay
In Boston, the residents at Mass General Brigham certified their union in June 2023, but they still don’t have a contract.
“When I applied for a residency in September 2023, I spoke to the folks here, and I was basically under the impression that we would have a contract by the time I matched,” said Madison Masters, MD, a resident in internal medicine. “We are not there.”
This timeline isn’t unusual — the 1400 Penn Medicine residents who unionized in 2023 only recently secured a tentative union contract at the end of September, and at Stanford, the process to ratify their first contract took 13 months.
Still, the salary issue remains frustrating as resident compensation doesn’t line up with the cost of living or the amount of work residents do, said Dr. Masters, who says starting salaries at Mass General Brigham are $78,500 plus a $10,000 stipend for housing.
“There’s been a long tradition of underpaying residents — we’re treated like trainees, but we’re also a primary labor force,” Dr. Masters said, adding that nurse practitioners and physician assistants are paid almost twice as much as residents — some make $120,000 per year or more, while the salary range for residents nationwide is $49,000-$65,000 per year.
“Every time we discuss the contract and talk about a financial package, they offer a 1.5% raise for the next 3 years while we had asked for closer to 8%,” Dr. Masters said. “Then, when they come back for the next bargaining session, they go up a quarter of a percent each time. Recently, they said we will need to go to a mediator to try and resolve this.”
Adequate Healthcare
The biggest — and perhaps the most shocking — ask is for robust health insurance coverage.
“At my hospital, they’re telling us to get Amazon One Medical for health insurance,” Dr. Masters said. “They’re saying it’s hard for anyone to get primary care coverage here.”
Inadequate health insurance is a big issue, as burnout among residents and fellows remains a problem. At UVM, a $10,000 annual wellness stipend has helped address some of these issues. Even so, union members at UVM are planning to return to the table within 18 months to continue their collective bargaining.
The ability to access mental health services anywhere you want is also critical for residents, Dr. Walker said.
“If you can only go to a therapist at your own institution, there is a hesitation to utilize that specialist if that’s even offered,” Dr. Walker said. “Do you want to go to therapy with a colleague? Probably not.”
Ultimately, the residents we spoke to are committed to fighting for their workplace rights — no matter how time-consuming or difficult this has been.
“No administration wants us to have to have a union, but it’s necessary,” Dr. Mostoller said. “As an individual, you don’t have leverage to get a seat at the table, but now we have a seat at the table. We have a wonderful contract, but we’re going to keep fighting to make it even better.”
Paving the way for future residents is a key motivator, too.
“There’s this idea of leaving the campsite cleaner than you found it,” Dr. Mostoller told this news organization. “It’s the same thing here — we’re trying to fix this so that the next generation of residents won’t have to.”
A version of this article first appeared on Medscape.com.
Nonalcoholic Beer and Underage Drinking
Several months ago in a letter about healthcare providers and the decision to use alcohol and other mind-altering substances on the job, I waxed enthusiastically about the new wave of no alcohol (NA) and zero (00) alcohol beers that have come on the market. In the last 2 years our local grocery store’s cooler space for nonalcoholic beer has grown from less than 24 inches to something approaching the height of the average sixth grader.
In a bold act of chivalry at the beginning of the pandemic I accepted the mantle of designated grocery shopper and over the last 3 years have become uncommonly proud of my ability to bring home the groceries efficiently and cost effectively, without catching COVID in the process. I have developed a sixth sense of choosing which human checker/bagger combination is fastest or whether the self-checkout is the way to go.
For obvious reasons the human checkers don’t ask for my ID when I am buying adult beverages. However, the self-check register freezes up instantly when I scan my 12-pack of Run Wild nonalcoholic. This necessitates a search for the MIA store person assigned to patrol the self-check corral, ever on the lookout for shoplifters, underage drinkers, and other generally shifty looking characters.
When I find one of the grocery store detectives (who is likely to have been a former patient), I say: “You know, this doesn’t have any alcohol in it.” They invariably reply with a shrug. “I know. But, the rules are the rules.” Occasionally, they may add: “It doesn’t make sense, does it?”
At first blush checking IDs for a nonalcoholic beverage may sound dumb, certainly to someone who is just a few years on either side of the legal drinking age. Why are we trying to protect some crazy teenager from the futility of getting high on a six-pack of something that at worst will make him spend most of the next couple of hours peeing?
But, there is concern in some corners that nonalcoholic drinks pose a significant threat to teenagers. Two PhDs at Stanford University have recently published a paper in which they worry that the dramatic rise in US sales of nonalcoholic drinks from 15% to 30% since 2018 may be socializing “users of alcohol drinking experiences by exposing them to the taste, look, and even brands of alcoholic beverages”.
Is there evidence to support their concern? I could only find one brief report in the Japanese literature that states that among young people “who experienced the nonalcoholic beverage intake, interest in or motivation for drinking alcoholic beverages, and/or smoking is higher than [among] those who did not.” The study didn’t appear to clearly separate the exposure in a family setting from the actual intake.
Beer is an acquired taste. If someone offered you your first taste of beer after a hot-weather set of tennis most of you would reject it and ask for water or lemonade. I can recall my first taste of beer. For some reason my father thought at age 11 or 12 I might like to try some from his glass. I’m not sure of his motivation, but he tried the same thing with oysters. I didn’t drink beer again until I was 16, motivated at that time by a group dynamic. The oyster trial, however, backfired on him and from then on he had to share his coveted dozen with me. Alcohol, unless heavily disguised by a mixer, is also not a taste that most young people find appealing.
It is unlikely that the average thrill-seeking teenager is going to ask his older-appearing buddy with a fake ID to buy him some nonalcoholic beer. Nor would he go to the effort or risk of acquiring his own fake ID just to see how it tastes. It just doesn’t compute, especially to a self-check corral patroller.
I guess one could envision a scenario in which a teenager wanting to fit in with the fast crowd would ask a trusted adult (or clueless parent) to buy him some nonalcoholic beer to bring to a party. He is running a serious risk of being laughed at by his friends if they find he’s drinking the fake stuff. It also seems unlikely that a parent would buy nonalcoholic beer to introduce his teenager to the taste of beer.
So,
Although it runs counter to my usual commitment to evidence-based decisions, making it difficult for adolescents to buy nonalcoholic beverages feels like the right think to do. As long as alcoholic and nonalcoholic beverages share the same display space and are packaged in nearly identical containers, there is ample opportunity for confusion. Recent evidence suggesting that even small amounts of alcohol increases some health risks should strengthen our resolve to minimize that confusion.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Several months ago in a letter about healthcare providers and the decision to use alcohol and other mind-altering substances on the job, I waxed enthusiastically about the new wave of no alcohol (NA) and zero (00) alcohol beers that have come on the market. In the last 2 years our local grocery store’s cooler space for nonalcoholic beer has grown from less than 24 inches to something approaching the height of the average sixth grader.
In a bold act of chivalry at the beginning of the pandemic I accepted the mantle of designated grocery shopper and over the last 3 years have become uncommonly proud of my ability to bring home the groceries efficiently and cost effectively, without catching COVID in the process. I have developed a sixth sense of choosing which human checker/bagger combination is fastest or whether the self-checkout is the way to go.
For obvious reasons the human checkers don’t ask for my ID when I am buying adult beverages. However, the self-check register freezes up instantly when I scan my 12-pack of Run Wild nonalcoholic. This necessitates a search for the MIA store person assigned to patrol the self-check corral, ever on the lookout for shoplifters, underage drinkers, and other generally shifty looking characters.
When I find one of the grocery store detectives (who is likely to have been a former patient), I say: “You know, this doesn’t have any alcohol in it.” They invariably reply with a shrug. “I know. But, the rules are the rules.” Occasionally, they may add: “It doesn’t make sense, does it?”
At first blush checking IDs for a nonalcoholic beverage may sound dumb, certainly to someone who is just a few years on either side of the legal drinking age. Why are we trying to protect some crazy teenager from the futility of getting high on a six-pack of something that at worst will make him spend most of the next couple of hours peeing?
But, there is concern in some corners that nonalcoholic drinks pose a significant threat to teenagers. Two PhDs at Stanford University have recently published a paper in which they worry that the dramatic rise in US sales of nonalcoholic drinks from 15% to 30% since 2018 may be socializing “users of alcohol drinking experiences by exposing them to the taste, look, and even brands of alcoholic beverages”.
Is there evidence to support their concern? I could only find one brief report in the Japanese literature that states that among young people “who experienced the nonalcoholic beverage intake, interest in or motivation for drinking alcoholic beverages, and/or smoking is higher than [among] those who did not.” The study didn’t appear to clearly separate the exposure in a family setting from the actual intake.
Beer is an acquired taste. If someone offered you your first taste of beer after a hot-weather set of tennis most of you would reject it and ask for water or lemonade. I can recall my first taste of beer. For some reason my father thought at age 11 or 12 I might like to try some from his glass. I’m not sure of his motivation, but he tried the same thing with oysters. I didn’t drink beer again until I was 16, motivated at that time by a group dynamic. The oyster trial, however, backfired on him and from then on he had to share his coveted dozen with me. Alcohol, unless heavily disguised by a mixer, is also not a taste that most young people find appealing.
It is unlikely that the average thrill-seeking teenager is going to ask his older-appearing buddy with a fake ID to buy him some nonalcoholic beer. Nor would he go to the effort or risk of acquiring his own fake ID just to see how it tastes. It just doesn’t compute, especially to a self-check corral patroller.
I guess one could envision a scenario in which a teenager wanting to fit in with the fast crowd would ask a trusted adult (or clueless parent) to buy him some nonalcoholic beer to bring to a party. He is running a serious risk of being laughed at by his friends if they find he’s drinking the fake stuff. It also seems unlikely that a parent would buy nonalcoholic beer to introduce his teenager to the taste of beer.
So,
Although it runs counter to my usual commitment to evidence-based decisions, making it difficult for adolescents to buy nonalcoholic beverages feels like the right think to do. As long as alcoholic and nonalcoholic beverages share the same display space and are packaged in nearly identical containers, there is ample opportunity for confusion. Recent evidence suggesting that even small amounts of alcohol increases some health risks should strengthen our resolve to minimize that confusion.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Several months ago in a letter about healthcare providers and the decision to use alcohol and other mind-altering substances on the job, I waxed enthusiastically about the new wave of no alcohol (NA) and zero (00) alcohol beers that have come on the market. In the last 2 years our local grocery store’s cooler space for nonalcoholic beer has grown from less than 24 inches to something approaching the height of the average sixth grader.
In a bold act of chivalry at the beginning of the pandemic I accepted the mantle of designated grocery shopper and over the last 3 years have become uncommonly proud of my ability to bring home the groceries efficiently and cost effectively, without catching COVID in the process. I have developed a sixth sense of choosing which human checker/bagger combination is fastest or whether the self-checkout is the way to go.
For obvious reasons the human checkers don’t ask for my ID when I am buying adult beverages. However, the self-check register freezes up instantly when I scan my 12-pack of Run Wild nonalcoholic. This necessitates a search for the MIA store person assigned to patrol the self-check corral, ever on the lookout for shoplifters, underage drinkers, and other generally shifty looking characters.
When I find one of the grocery store detectives (who is likely to have been a former patient), I say: “You know, this doesn’t have any alcohol in it.” They invariably reply with a shrug. “I know. But, the rules are the rules.” Occasionally, they may add: “It doesn’t make sense, does it?”
At first blush checking IDs for a nonalcoholic beverage may sound dumb, certainly to someone who is just a few years on either side of the legal drinking age. Why are we trying to protect some crazy teenager from the futility of getting high on a six-pack of something that at worst will make him spend most of the next couple of hours peeing?
But, there is concern in some corners that nonalcoholic drinks pose a significant threat to teenagers. Two PhDs at Stanford University have recently published a paper in which they worry that the dramatic rise in US sales of nonalcoholic drinks from 15% to 30% since 2018 may be socializing “users of alcohol drinking experiences by exposing them to the taste, look, and even brands of alcoholic beverages”.
Is there evidence to support their concern? I could only find one brief report in the Japanese literature that states that among young people “who experienced the nonalcoholic beverage intake, interest in or motivation for drinking alcoholic beverages, and/or smoking is higher than [among] those who did not.” The study didn’t appear to clearly separate the exposure in a family setting from the actual intake.
Beer is an acquired taste. If someone offered you your first taste of beer after a hot-weather set of tennis most of you would reject it and ask for water or lemonade. I can recall my first taste of beer. For some reason my father thought at age 11 or 12 I might like to try some from his glass. I’m not sure of his motivation, but he tried the same thing with oysters. I didn’t drink beer again until I was 16, motivated at that time by a group dynamic. The oyster trial, however, backfired on him and from then on he had to share his coveted dozen with me. Alcohol, unless heavily disguised by a mixer, is also not a taste that most young people find appealing.
It is unlikely that the average thrill-seeking teenager is going to ask his older-appearing buddy with a fake ID to buy him some nonalcoholic beer. Nor would he go to the effort or risk of acquiring his own fake ID just to see how it tastes. It just doesn’t compute, especially to a self-check corral patroller.
I guess one could envision a scenario in which a teenager wanting to fit in with the fast crowd would ask a trusted adult (or clueless parent) to buy him some nonalcoholic beer to bring to a party. He is running a serious risk of being laughed at by his friends if they find he’s drinking the fake stuff. It also seems unlikely that a parent would buy nonalcoholic beer to introduce his teenager to the taste of beer.
So,
Although it runs counter to my usual commitment to evidence-based decisions, making it difficult for adolescents to buy nonalcoholic beverages feels like the right think to do. As long as alcoholic and nonalcoholic beverages share the same display space and are packaged in nearly identical containers, there is ample opportunity for confusion. Recent evidence suggesting that even small amounts of alcohol increases some health risks should strengthen our resolve to minimize that confusion.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Anticipated Effects of Pneumococcal Vaccines on Otitis
Acute otitis media (AOM) is caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Since the introduction of pneumococcal conjugate vaccines (PCVs) shifts in the proportion of these three bacteria as causes of AOM and their antibiotic susceptibility profiles and strain diversity have occurred due to multiple factors including the PCVs and antibiotic selection pressure.
The 7-valent PCV (PCV7) was introduced in 2000 and was proven to be efficacious in preventing AOM, but no subsequent PCV has received an indication for prevention of AOM because the FDA required a tympanocentesis study to prove efficacy and that approval was not achieved for PCV13, PCV15, or PCV20. This is a little known fact. After introduction of PCV7, replacement pneumococcal strains expressing serotypes not in PCV7 emerged and antibiotic non-susceptible strains became predominant causes of AOM, especially antibiotic-resistant serotype 19A. To address the phenomena of pneumococcal serotype replacement, PCV13 was introduced in 2010. But serotype replacement continued to occur under PCV13 pressure, replacement serotypes increasingly caused AOM, and antibiotic-resistant serotype 35B emerged. Now we have two new higher valency PCVs: PCV15 (Merck) where serotypes 22F and 33F were added to the PCV13 serotypes and PCV20 (Pfizer) where 22F, 33F, 8, 10A, 11A, 12F, 15B were added to PCV13. Note that neither PCV15 nor PCV20 includes the most common serotype causing AOM – serotype 35B.1
While PCV15 and PCV20 should provide protection against more pneumococcal serotypes, increasing serotypes in both vaccines decreased immunogenicity of certain shared serotypes, more so with the addition of seven more in PCV20 than two more in PCV15, compared with PCV13. Whether lower antibody concentrations will make a difference clinically in terms of vaccine failure to prevent nasopharyngeal colonization, AOM, and/or invasive pneumococcal infections is currently unknown.
Our group from greater Rochester, New York, is the only one in the United States performing tympanocentesis to determine the etiology of AOM infections. Children between ages 6 and 36 months are studied. We recently reported our results for the time span September 2021 to September 2023, the immediate 2 years prior to recommendations for use of PCV15 and PCV20 in young children.2 Tympanocentesis was performed in 139 (78%) of 179 episodes of AOM, yielding 216 middle ear fluid samples (the higher number of middle ear fluids was due to bilateral tympanocentesis in some children). H. influenzae (40%) was the most common bacterial isolate, followed by S. pneumonia (19%) and M. catarrhalis (17%), with the remainder no growth. Polymerase chain reactions (PCR) was positive in many of those culture negative samples, suggesting prior use of antibiotics before tympanocentesis was performed. Among the pneumococcal isolates, 46% were oxacillin non-susceptible. Among the H. influenzae isolates, 27% were beta-lactamase producing and all M. catarrhalis were beta-lactamase-producing.
As we previously reported,1 we once again found that serotype 35B was the most frequent non-PCV15, non-PCV20, serotype. Other frequently detected non-PCV20 pneumococcal serotypes were 23A, 23B, 35D, 35F and 15C.2
Projected Pneumococcal Serotype Coverage by PCV15 and PCV20
PCV13 serotypes were identified in 9% of middle ear fluids, consistent with vaccine failure. Assuming 100% vaccine-type effectiveness, PCV15 will provide about 11% coverage of pneumococci causing AOM, the same PCV13 and PCV20 will provide 30% coverage, leaving 70% of pneumococci causing AOM in young children uncovered (Figure).
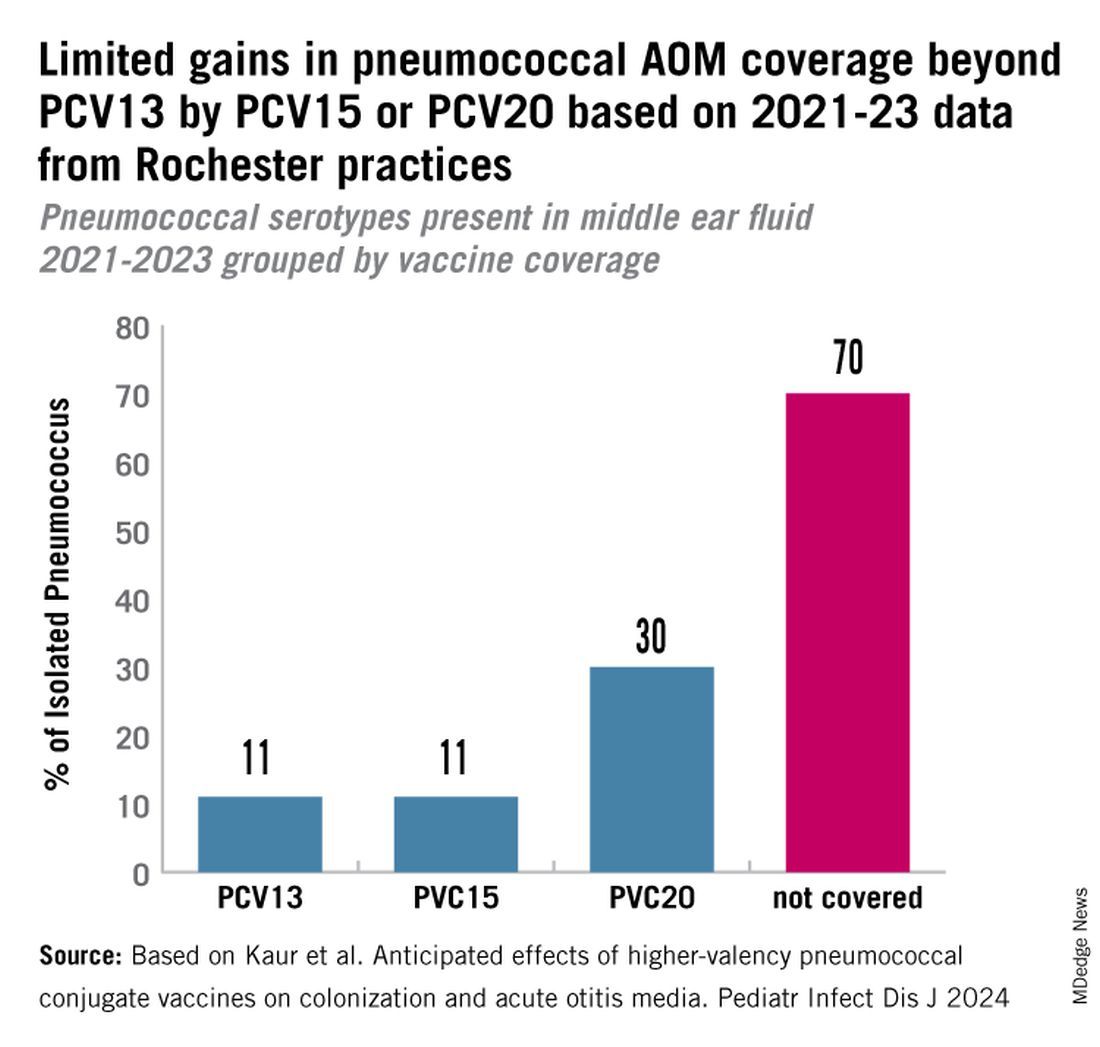
Thus, the high proportion of pneumococcal serotype 35B and other non-PCV15 or non-PCV20 serotypes will result in a relatively small incremental benefit over PCV13 in young children for AOM.
AOM is the most common cause of pediatric outpatient visits and antibiotic prescriptions in the United States that contributes to selection of antibiotic-resistant microbes.3 The economic burden of AOM is high, estimated at about $3 billion annually in the United States, when direct and indirect costs are calculated,4 thereby making AOM a major factor in calculations of cost effectiveness analyses of PCV immunizations in children.
While PCV15 and PCV20 include common serotypes associated with invasive pneumococcal diseases, their effectiveness in preventing AOM, acute sinusitis, and non-bacteremic community-acquired pneumonia is currently unknown because these vaccines were licensed based on safety and immunogenicity data, not proven efficacy.
The data on antibiotic susceptibility of pneumococci and H. influenza and M. catarrhalis isolated in the late post PCV13 era from young children in a pediatric primary-care setting raise a question about empiric antibiotic choice for AOM today. For penicillin non-susceptible pneumococcal strains, higher dosages of amoxicillin can improve eradication. However, higher dosages of amoxicillin cannot overcome beta-lactamase production by H. influenza and M. catarrhalis. Based on the mix of pathogens causing AOM and the antibiotic susceptibility of those bacteria, high-dose amoxicillin/clavulanate or alternative cephalosporin drugs active against pneumococci and beta-lactamase producing H. influenza and M. catarrhalis would be a better empiric choice over high-dose amoxicillin.
Limitations of our study include that it occurred in one center in New York, although we have previously shown results of tympanocentesis at our center are similar to those in Virginia and Pennsylvania5 and our study population was composed of children living in urban, suburban, and rural households of all economic levels. Because this study was conducted during a relatively short time frame (2021-2023), the numbers of subjects and samples were sometimes insufficient to identify statistically significant differences in some comparisons. Some children were lost to follow-up, and not every participant was consented for tympanocentesis. Some participants received antibiotics prior to middle ear fluid specimen collection.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Dynamic Changes in Otopathogens Colonizing the Nasopharynx and Causing Acute Otitis Media in Children After 13-Valent (PCV13) Pneumococcal Conjugate Vaccination During 2015-2019. Eur J Clin Microbiol Infect Dis. 2022 Jan;41(1):37-44. doi: 10.1007/s10096-021-04324-0.
2. Kaur R et al. Anticipated Effects of Higher-valency Pneumococcal Conjugate Vaccines on Colonization and Acute Otitis Media. Pediatr Infect Dis J. 2024 Oct 1;43(10):1004-1010. doi: 10.1097/INF.0000000000004413.
3. King LM et al. Pediatric Outpatient Visits and Antibiotic Use Attributable to Higher Valency Pneumococcal Conjugate Vaccine Serotypes. medRxiv [Preprint]. 2023 Aug 25:2023.08.24.23294570. doi: 10.1101/2023.08.24.23294570.
4. Ahmed S et al. Incremental Health Care Utilization and Costs for Acute Otitis Media in Children. Laryngoscope. 2014 Jan;124(1):301-5. doi: 10.1002/lary.24190.
5. Pichichero ME et al. Pathogens Causing Recurrent and Difficult-to-Treat Acute Otitis Media, 2003-2006. Clin Pediatr (Phila). 2008 Nov;47(9):901-6. doi: 10.1177/0009922808319966.
Acute otitis media (AOM) is caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Since the introduction of pneumococcal conjugate vaccines (PCVs) shifts in the proportion of these three bacteria as causes of AOM and their antibiotic susceptibility profiles and strain diversity have occurred due to multiple factors including the PCVs and antibiotic selection pressure.
The 7-valent PCV (PCV7) was introduced in 2000 and was proven to be efficacious in preventing AOM, but no subsequent PCV has received an indication for prevention of AOM because the FDA required a tympanocentesis study to prove efficacy and that approval was not achieved for PCV13, PCV15, or PCV20. This is a little known fact. After introduction of PCV7, replacement pneumococcal strains expressing serotypes not in PCV7 emerged and antibiotic non-susceptible strains became predominant causes of AOM, especially antibiotic-resistant serotype 19A. To address the phenomena of pneumococcal serotype replacement, PCV13 was introduced in 2010. But serotype replacement continued to occur under PCV13 pressure, replacement serotypes increasingly caused AOM, and antibiotic-resistant serotype 35B emerged. Now we have two new higher valency PCVs: PCV15 (Merck) where serotypes 22F and 33F were added to the PCV13 serotypes and PCV20 (Pfizer) where 22F, 33F, 8, 10A, 11A, 12F, 15B were added to PCV13. Note that neither PCV15 nor PCV20 includes the most common serotype causing AOM – serotype 35B.1
While PCV15 and PCV20 should provide protection against more pneumococcal serotypes, increasing serotypes in both vaccines decreased immunogenicity of certain shared serotypes, more so with the addition of seven more in PCV20 than two more in PCV15, compared with PCV13. Whether lower antibody concentrations will make a difference clinically in terms of vaccine failure to prevent nasopharyngeal colonization, AOM, and/or invasive pneumococcal infections is currently unknown.
Our group from greater Rochester, New York, is the only one in the United States performing tympanocentesis to determine the etiology of AOM infections. Children between ages 6 and 36 months are studied. We recently reported our results for the time span September 2021 to September 2023, the immediate 2 years prior to recommendations for use of PCV15 and PCV20 in young children.2 Tympanocentesis was performed in 139 (78%) of 179 episodes of AOM, yielding 216 middle ear fluid samples (the higher number of middle ear fluids was due to bilateral tympanocentesis in some children). H. influenzae (40%) was the most common bacterial isolate, followed by S. pneumonia (19%) and M. catarrhalis (17%), with the remainder no growth. Polymerase chain reactions (PCR) was positive in many of those culture negative samples, suggesting prior use of antibiotics before tympanocentesis was performed. Among the pneumococcal isolates, 46% were oxacillin non-susceptible. Among the H. influenzae isolates, 27% were beta-lactamase producing and all M. catarrhalis were beta-lactamase-producing.
As we previously reported,1 we once again found that serotype 35B was the most frequent non-PCV15, non-PCV20, serotype. Other frequently detected non-PCV20 pneumococcal serotypes were 23A, 23B, 35D, 35F and 15C.2
Projected Pneumococcal Serotype Coverage by PCV15 and PCV20
PCV13 serotypes were identified in 9% of middle ear fluids, consistent with vaccine failure. Assuming 100% vaccine-type effectiveness, PCV15 will provide about 11% coverage of pneumococci causing AOM, the same PCV13 and PCV20 will provide 30% coverage, leaving 70% of pneumococci causing AOM in young children uncovered (Figure).
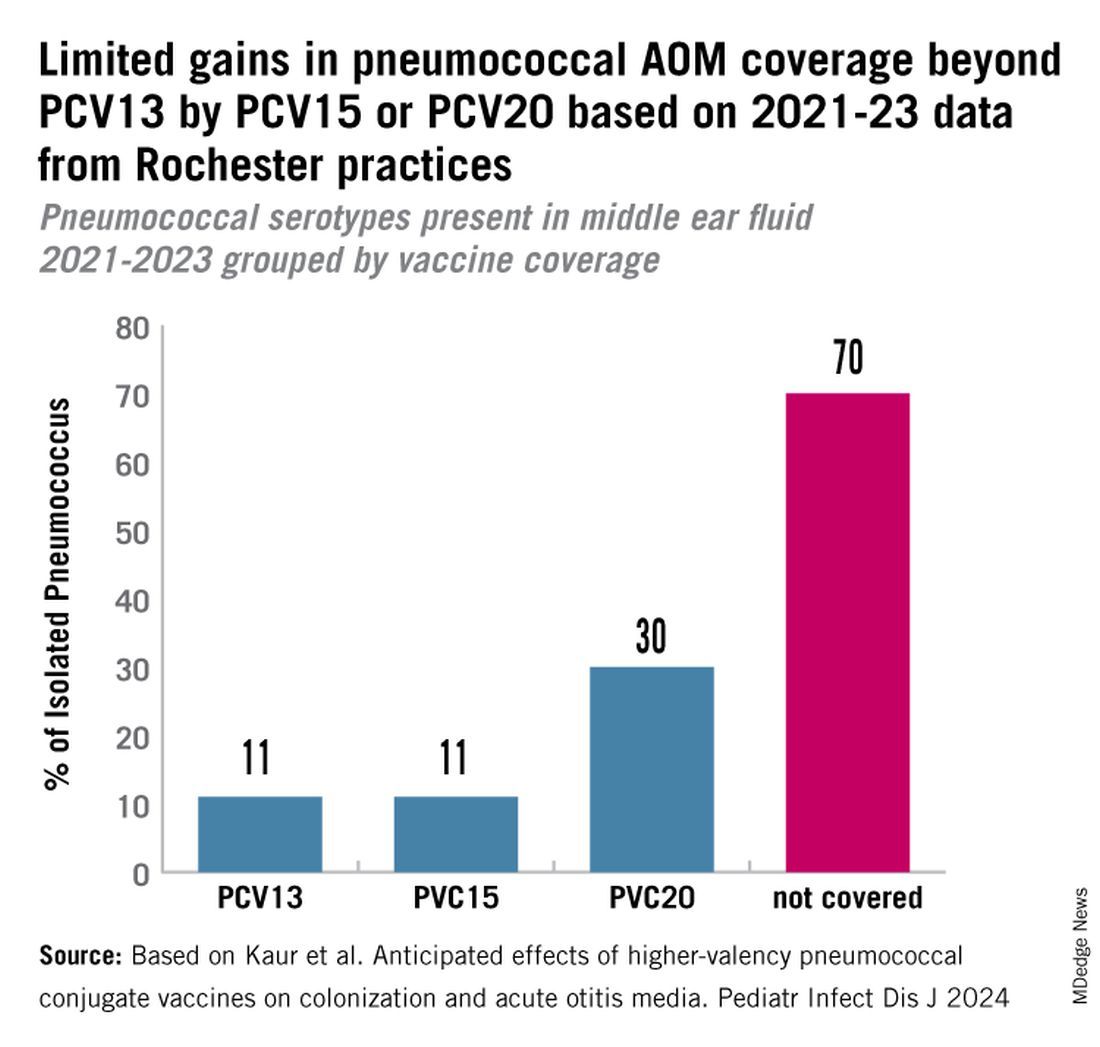
Thus, the high proportion of pneumococcal serotype 35B and other non-PCV15 or non-PCV20 serotypes will result in a relatively small incremental benefit over PCV13 in young children for AOM.
AOM is the most common cause of pediatric outpatient visits and antibiotic prescriptions in the United States that contributes to selection of antibiotic-resistant microbes.3 The economic burden of AOM is high, estimated at about $3 billion annually in the United States, when direct and indirect costs are calculated,4 thereby making AOM a major factor in calculations of cost effectiveness analyses of PCV immunizations in children.
While PCV15 and PCV20 include common serotypes associated with invasive pneumococcal diseases, their effectiveness in preventing AOM, acute sinusitis, and non-bacteremic community-acquired pneumonia is currently unknown because these vaccines were licensed based on safety and immunogenicity data, not proven efficacy.
The data on antibiotic susceptibility of pneumococci and H. influenza and M. catarrhalis isolated in the late post PCV13 era from young children in a pediatric primary-care setting raise a question about empiric antibiotic choice for AOM today. For penicillin non-susceptible pneumococcal strains, higher dosages of amoxicillin can improve eradication. However, higher dosages of amoxicillin cannot overcome beta-lactamase production by H. influenza and M. catarrhalis. Based on the mix of pathogens causing AOM and the antibiotic susceptibility of those bacteria, high-dose amoxicillin/clavulanate or alternative cephalosporin drugs active against pneumococci and beta-lactamase producing H. influenza and M. catarrhalis would be a better empiric choice over high-dose amoxicillin.
Limitations of our study include that it occurred in one center in New York, although we have previously shown results of tympanocentesis at our center are similar to those in Virginia and Pennsylvania5 and our study population was composed of children living in urban, suburban, and rural households of all economic levels. Because this study was conducted during a relatively short time frame (2021-2023), the numbers of subjects and samples were sometimes insufficient to identify statistically significant differences in some comparisons. Some children were lost to follow-up, and not every participant was consented for tympanocentesis. Some participants received antibiotics prior to middle ear fluid specimen collection.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Dynamic Changes in Otopathogens Colonizing the Nasopharynx and Causing Acute Otitis Media in Children After 13-Valent (PCV13) Pneumococcal Conjugate Vaccination During 2015-2019. Eur J Clin Microbiol Infect Dis. 2022 Jan;41(1):37-44. doi: 10.1007/s10096-021-04324-0.
2. Kaur R et al. Anticipated Effects of Higher-valency Pneumococcal Conjugate Vaccines on Colonization and Acute Otitis Media. Pediatr Infect Dis J. 2024 Oct 1;43(10):1004-1010. doi: 10.1097/INF.0000000000004413.
3. King LM et al. Pediatric Outpatient Visits and Antibiotic Use Attributable to Higher Valency Pneumococcal Conjugate Vaccine Serotypes. medRxiv [Preprint]. 2023 Aug 25:2023.08.24.23294570. doi: 10.1101/2023.08.24.23294570.
4. Ahmed S et al. Incremental Health Care Utilization and Costs for Acute Otitis Media in Children. Laryngoscope. 2014 Jan;124(1):301-5. doi: 10.1002/lary.24190.
5. Pichichero ME et al. Pathogens Causing Recurrent and Difficult-to-Treat Acute Otitis Media, 2003-2006. Clin Pediatr (Phila). 2008 Nov;47(9):901-6. doi: 10.1177/0009922808319966.
Acute otitis media (AOM) is caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Since the introduction of pneumococcal conjugate vaccines (PCVs) shifts in the proportion of these three bacteria as causes of AOM and their antibiotic susceptibility profiles and strain diversity have occurred due to multiple factors including the PCVs and antibiotic selection pressure.
The 7-valent PCV (PCV7) was introduced in 2000 and was proven to be efficacious in preventing AOM, but no subsequent PCV has received an indication for prevention of AOM because the FDA required a tympanocentesis study to prove efficacy and that approval was not achieved for PCV13, PCV15, or PCV20. This is a little known fact. After introduction of PCV7, replacement pneumococcal strains expressing serotypes not in PCV7 emerged and antibiotic non-susceptible strains became predominant causes of AOM, especially antibiotic-resistant serotype 19A. To address the phenomena of pneumococcal serotype replacement, PCV13 was introduced in 2010. But serotype replacement continued to occur under PCV13 pressure, replacement serotypes increasingly caused AOM, and antibiotic-resistant serotype 35B emerged. Now we have two new higher valency PCVs: PCV15 (Merck) where serotypes 22F and 33F were added to the PCV13 serotypes and PCV20 (Pfizer) where 22F, 33F, 8, 10A, 11A, 12F, 15B were added to PCV13. Note that neither PCV15 nor PCV20 includes the most common serotype causing AOM – serotype 35B.1
While PCV15 and PCV20 should provide protection against more pneumococcal serotypes, increasing serotypes in both vaccines decreased immunogenicity of certain shared serotypes, more so with the addition of seven more in PCV20 than two more in PCV15, compared with PCV13. Whether lower antibody concentrations will make a difference clinically in terms of vaccine failure to prevent nasopharyngeal colonization, AOM, and/or invasive pneumococcal infections is currently unknown.
Our group from greater Rochester, New York, is the only one in the United States performing tympanocentesis to determine the etiology of AOM infections. Children between ages 6 and 36 months are studied. We recently reported our results for the time span September 2021 to September 2023, the immediate 2 years prior to recommendations for use of PCV15 and PCV20 in young children.2 Tympanocentesis was performed in 139 (78%) of 179 episodes of AOM, yielding 216 middle ear fluid samples (the higher number of middle ear fluids was due to bilateral tympanocentesis in some children). H. influenzae (40%) was the most common bacterial isolate, followed by S. pneumonia (19%) and M. catarrhalis (17%), with the remainder no growth. Polymerase chain reactions (PCR) was positive in many of those culture negative samples, suggesting prior use of antibiotics before tympanocentesis was performed. Among the pneumococcal isolates, 46% were oxacillin non-susceptible. Among the H. influenzae isolates, 27% were beta-lactamase producing and all M. catarrhalis were beta-lactamase-producing.
As we previously reported,1 we once again found that serotype 35B was the most frequent non-PCV15, non-PCV20, serotype. Other frequently detected non-PCV20 pneumococcal serotypes were 23A, 23B, 35D, 35F and 15C.2
Projected Pneumococcal Serotype Coverage by PCV15 and PCV20
PCV13 serotypes were identified in 9% of middle ear fluids, consistent with vaccine failure. Assuming 100% vaccine-type effectiveness, PCV15 will provide about 11% coverage of pneumococci causing AOM, the same PCV13 and PCV20 will provide 30% coverage, leaving 70% of pneumococci causing AOM in young children uncovered (Figure).
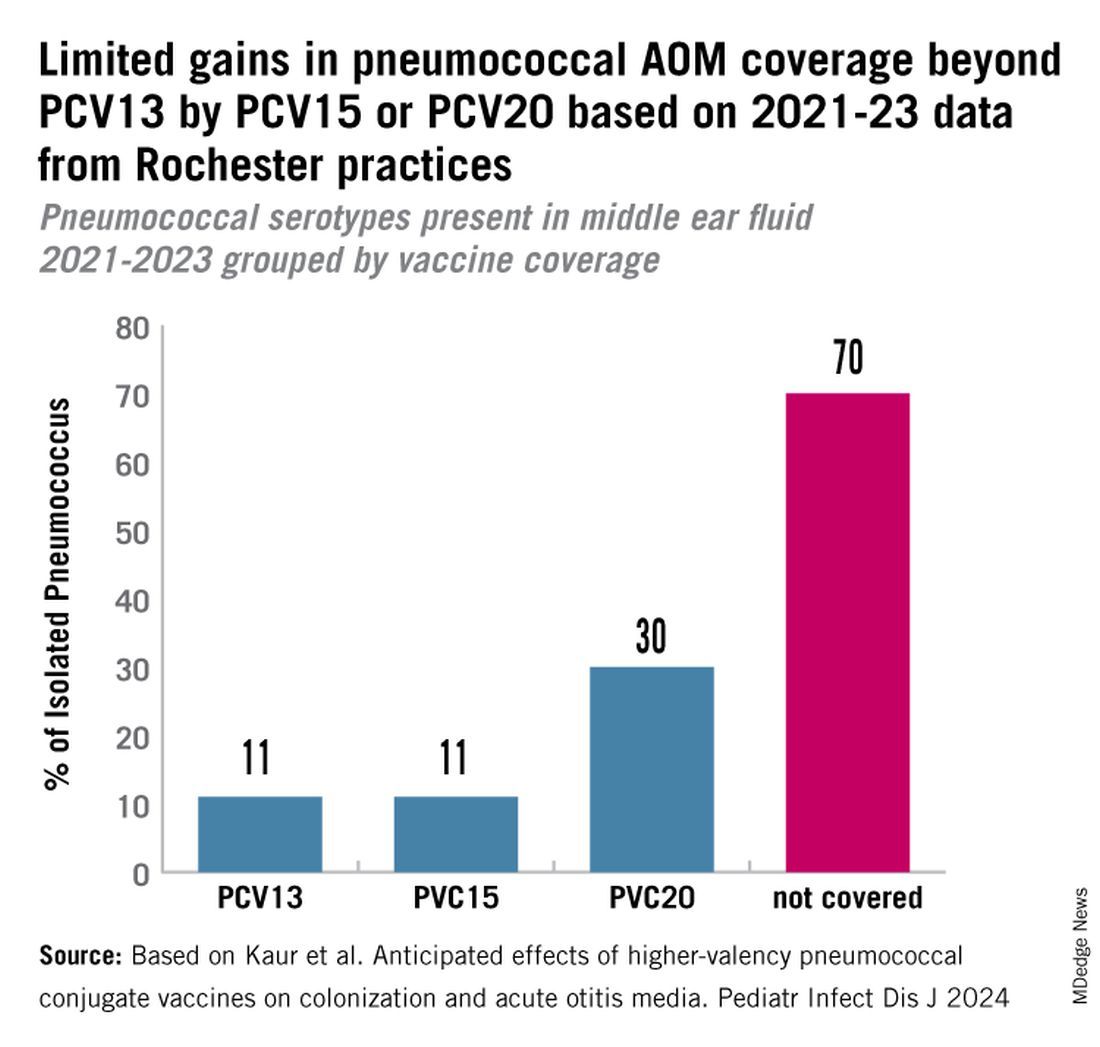
Thus, the high proportion of pneumococcal serotype 35B and other non-PCV15 or non-PCV20 serotypes will result in a relatively small incremental benefit over PCV13 in young children for AOM.
AOM is the most common cause of pediatric outpatient visits and antibiotic prescriptions in the United States that contributes to selection of antibiotic-resistant microbes.3 The economic burden of AOM is high, estimated at about $3 billion annually in the United States, when direct and indirect costs are calculated,4 thereby making AOM a major factor in calculations of cost effectiveness analyses of PCV immunizations in children.
While PCV15 and PCV20 include common serotypes associated with invasive pneumococcal diseases, their effectiveness in preventing AOM, acute sinusitis, and non-bacteremic community-acquired pneumonia is currently unknown because these vaccines were licensed based on safety and immunogenicity data, not proven efficacy.
The data on antibiotic susceptibility of pneumococci and H. influenza and M. catarrhalis isolated in the late post PCV13 era from young children in a pediatric primary-care setting raise a question about empiric antibiotic choice for AOM today. For penicillin non-susceptible pneumococcal strains, higher dosages of amoxicillin can improve eradication. However, higher dosages of amoxicillin cannot overcome beta-lactamase production by H. influenza and M. catarrhalis. Based on the mix of pathogens causing AOM and the antibiotic susceptibility of those bacteria, high-dose amoxicillin/clavulanate or alternative cephalosporin drugs active against pneumococci and beta-lactamase producing H. influenza and M. catarrhalis would be a better empiric choice over high-dose amoxicillin.
Limitations of our study include that it occurred in one center in New York, although we have previously shown results of tympanocentesis at our center are similar to those in Virginia and Pennsylvania5 and our study population was composed of children living in urban, suburban, and rural households of all economic levels. Because this study was conducted during a relatively short time frame (2021-2023), the numbers of subjects and samples were sometimes insufficient to identify statistically significant differences in some comparisons. Some children were lost to follow-up, and not every participant was consented for tympanocentesis. Some participants received antibiotics prior to middle ear fluid specimen collection.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Dynamic Changes in Otopathogens Colonizing the Nasopharynx and Causing Acute Otitis Media in Children After 13-Valent (PCV13) Pneumococcal Conjugate Vaccination During 2015-2019. Eur J Clin Microbiol Infect Dis. 2022 Jan;41(1):37-44. doi: 10.1007/s10096-021-04324-0.
2. Kaur R et al. Anticipated Effects of Higher-valency Pneumococcal Conjugate Vaccines on Colonization and Acute Otitis Media. Pediatr Infect Dis J. 2024 Oct 1;43(10):1004-1010. doi: 10.1097/INF.0000000000004413.
3. King LM et al. Pediatric Outpatient Visits and Antibiotic Use Attributable to Higher Valency Pneumococcal Conjugate Vaccine Serotypes. medRxiv [Preprint]. 2023 Aug 25:2023.08.24.23294570. doi: 10.1101/2023.08.24.23294570.
4. Ahmed S et al. Incremental Health Care Utilization and Costs for Acute Otitis Media in Children. Laryngoscope. 2014 Jan;124(1):301-5. doi: 10.1002/lary.24190.
5. Pichichero ME et al. Pathogens Causing Recurrent and Difficult-to-Treat Acute Otitis Media, 2003-2006. Clin Pediatr (Phila). 2008 Nov;47(9):901-6. doi: 10.1177/0009922808319966.
ART Linked With Congenital Heart Defects in Newborns
The rate of congenital heart defects is higher in newborns conceived using assisted reproductive technologies (ART) than in newborns conceived without assistance. This finding comes from a population-based cohort study led by Dr. Nona Sargisian, a gynecologist at the University of Gothenburg, Sweden, and colleagues, which was published in the European Heart Journal.
The researchers analyzed more than 7 million results of all live-born children in Denmark, Finland, Sweden, and Norway between 1984 and 2015. They found that congenital heart defects occurred more frequently in the ART newborn group (1.85%) than in naturally conceived newborns (1.15%).
The study also revealed that the risk for congenital heart defects in multiple births is higher than in single births, with and without the use of ART. However, the result that congenital heart defects occur more often in ART newborns remained significant when comparing single births from both groups (1.62% vs 1.11%).
Relatively Low Prevalence
Barbara Sonntag, MD, PhD, a gynecologist at Amedes Fertility Center in Hamburg, Germany, referred to a “clinically relevant risk increase” with a relatively low prevalence of the condition.
“When 1000 children are born, an abnormality occurs in 18 children after ART, compared with 11 children born after natural conception,” she told the Science Media Center.
Dr. Sonntag emphasized that the risk is particularly increased by a multiple pregnancy. A statement about causality is not possible based on the study, but multiple pregnancies are generally associated with increased risks during pregnancy and for the children.
The large and robust dataset confirms long-known findings, said Georg Griesinger, MD, PhD, medical director of the fertility centers of the University Medical Center Schleswig-Holstein in Lübeck and Manhagen, Germany.
The key figures can be found in single births, he explained. “Among single births conceived by ART, the rate of severe congenital heart defects was 1.62% compared with 1.11% in spontaneously conceived single births, an increase in risk by 1.19 times. For severe heart defects, the rate was 0.31% in ART single births, compared with 0.25% in spontaneously conceived single births.”
The increased risks are consistent with existing literature. Therefore, the current study does not reveal any new risk signals, said Dr. Griesinger.
Single Embryo Transfer
The “risks are small but present,” according to Michael von Wolff, MD, head of gynecological endocrinology and reproductive medicine at Bern University Hospital in Switzerland. “Therefore, ART therapy should only be carried out after exhausting conservative treatments,” he recommended. For example, ovarian stimulation with low-dose hormone preparations could be an option.
Dr. Griesinger pointed out that, in absolute numbers, all maternal and fetal or neonatal risks are significantly increased in twins and higher-order multiples, compared with the estimated risk association within the actual ART treatment.
“For this reason, reproductive medicine specialists have been advocating for single-embryo transfer for years to promote the occurrence of single pregnancies through ART,” said Dr. Griesinger.
The study “emphasizes the importance of single embryo transfer to avoid the higher risks associated with multiple pregnancies,” according to Rocío Núñez Calonge, PhD, scientific director of the International Reproduction Unit in Alicante, Spain.
Dr. Sonntag also sees a “strong additional call to avoid multiple pregnancies through a predominant strategy of single-embryo transfer in the data. The increased rate of childhood birth defects is already part of the information provided before assisted reproduction.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The rate of congenital heart defects is higher in newborns conceived using assisted reproductive technologies (ART) than in newborns conceived without assistance. This finding comes from a population-based cohort study led by Dr. Nona Sargisian, a gynecologist at the University of Gothenburg, Sweden, and colleagues, which was published in the European Heart Journal.
The researchers analyzed more than 7 million results of all live-born children in Denmark, Finland, Sweden, and Norway between 1984 and 2015. They found that congenital heart defects occurred more frequently in the ART newborn group (1.85%) than in naturally conceived newborns (1.15%).
The study also revealed that the risk for congenital heart defects in multiple births is higher than in single births, with and without the use of ART. However, the result that congenital heart defects occur more often in ART newborns remained significant when comparing single births from both groups (1.62% vs 1.11%).
Relatively Low Prevalence
Barbara Sonntag, MD, PhD, a gynecologist at Amedes Fertility Center in Hamburg, Germany, referred to a “clinically relevant risk increase” with a relatively low prevalence of the condition.
“When 1000 children are born, an abnormality occurs in 18 children after ART, compared with 11 children born after natural conception,” she told the Science Media Center.
Dr. Sonntag emphasized that the risk is particularly increased by a multiple pregnancy. A statement about causality is not possible based on the study, but multiple pregnancies are generally associated with increased risks during pregnancy and for the children.
The large and robust dataset confirms long-known findings, said Georg Griesinger, MD, PhD, medical director of the fertility centers of the University Medical Center Schleswig-Holstein in Lübeck and Manhagen, Germany.
The key figures can be found in single births, he explained. “Among single births conceived by ART, the rate of severe congenital heart defects was 1.62% compared with 1.11% in spontaneously conceived single births, an increase in risk by 1.19 times. For severe heart defects, the rate was 0.31% in ART single births, compared with 0.25% in spontaneously conceived single births.”
The increased risks are consistent with existing literature. Therefore, the current study does not reveal any new risk signals, said Dr. Griesinger.
Single Embryo Transfer
The “risks are small but present,” according to Michael von Wolff, MD, head of gynecological endocrinology and reproductive medicine at Bern University Hospital in Switzerland. “Therefore, ART therapy should only be carried out after exhausting conservative treatments,” he recommended. For example, ovarian stimulation with low-dose hormone preparations could be an option.
Dr. Griesinger pointed out that, in absolute numbers, all maternal and fetal or neonatal risks are significantly increased in twins and higher-order multiples, compared with the estimated risk association within the actual ART treatment.
“For this reason, reproductive medicine specialists have been advocating for single-embryo transfer for years to promote the occurrence of single pregnancies through ART,” said Dr. Griesinger.
The study “emphasizes the importance of single embryo transfer to avoid the higher risks associated with multiple pregnancies,” according to Rocío Núñez Calonge, PhD, scientific director of the International Reproduction Unit in Alicante, Spain.
Dr. Sonntag also sees a “strong additional call to avoid multiple pregnancies through a predominant strategy of single-embryo transfer in the data. The increased rate of childhood birth defects is already part of the information provided before assisted reproduction.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The rate of congenital heart defects is higher in newborns conceived using assisted reproductive technologies (ART) than in newborns conceived without assistance. This finding comes from a population-based cohort study led by Dr. Nona Sargisian, a gynecologist at the University of Gothenburg, Sweden, and colleagues, which was published in the European Heart Journal.
The researchers analyzed more than 7 million results of all live-born children in Denmark, Finland, Sweden, and Norway between 1984 and 2015. They found that congenital heart defects occurred more frequently in the ART newborn group (1.85%) than in naturally conceived newborns (1.15%).
The study also revealed that the risk for congenital heart defects in multiple births is higher than in single births, with and without the use of ART. However, the result that congenital heart defects occur more often in ART newborns remained significant when comparing single births from both groups (1.62% vs 1.11%).
Relatively Low Prevalence
Barbara Sonntag, MD, PhD, a gynecologist at Amedes Fertility Center in Hamburg, Germany, referred to a “clinically relevant risk increase” with a relatively low prevalence of the condition.
“When 1000 children are born, an abnormality occurs in 18 children after ART, compared with 11 children born after natural conception,” she told the Science Media Center.
Dr. Sonntag emphasized that the risk is particularly increased by a multiple pregnancy. A statement about causality is not possible based on the study, but multiple pregnancies are generally associated with increased risks during pregnancy and for the children.
The large and robust dataset confirms long-known findings, said Georg Griesinger, MD, PhD, medical director of the fertility centers of the University Medical Center Schleswig-Holstein in Lübeck and Manhagen, Germany.
The key figures can be found in single births, he explained. “Among single births conceived by ART, the rate of severe congenital heart defects was 1.62% compared with 1.11% in spontaneously conceived single births, an increase in risk by 1.19 times. For severe heart defects, the rate was 0.31% in ART single births, compared with 0.25% in spontaneously conceived single births.”
The increased risks are consistent with existing literature. Therefore, the current study does not reveal any new risk signals, said Dr. Griesinger.
Single Embryo Transfer
The “risks are small but present,” according to Michael von Wolff, MD, head of gynecological endocrinology and reproductive medicine at Bern University Hospital in Switzerland. “Therefore, ART therapy should only be carried out after exhausting conservative treatments,” he recommended. For example, ovarian stimulation with low-dose hormone preparations could be an option.
Dr. Griesinger pointed out that, in absolute numbers, all maternal and fetal or neonatal risks are significantly increased in twins and higher-order multiples, compared with the estimated risk association within the actual ART treatment.
“For this reason, reproductive medicine specialists have been advocating for single-embryo transfer for years to promote the occurrence of single pregnancies through ART,” said Dr. Griesinger.
The study “emphasizes the importance of single embryo transfer to avoid the higher risks associated with multiple pregnancies,” according to Rocío Núñez Calonge, PhD, scientific director of the International Reproduction Unit in Alicante, Spain.
Dr. Sonntag also sees a “strong additional call to avoid multiple pregnancies through a predominant strategy of single-embryo transfer in the data. The increased rate of childhood birth defects is already part of the information provided before assisted reproduction.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL
How Doctors Can Overcome Vaccine Hesitancy Through Empathy, Storytelling, and Patient-Centered Communication
When Kimberly Fisher, MD, was a junior doctor, she got fired up when patients showed hesitancy about vaccines. She responded by providing numbers, data, and facts that proved vaccines were safe and effective in preventing life-threatening diseases. But she soon realized that regurgitating scientific evidence wasn’t a winning strategy. “I’ve made the mistake of launching into a let me tell you all the things that I know that you don’t know kind of lecture,” Dr. Fisher, now an associate professor of medicine at UMass Chan Medical School, Worcester, Massachusetts, a pulmonary physician, and a researcher interested in patient-provider communication, told this news organization. “Through experience and research, I have learned that when you do that, they stop listening.”
She said when patients give reasons for not getting vaccinated that are factually wrong and rooted in misinformation, the most common reaction is to correct that information and not let it stand. “That is important; it just can’t be the first thing you do,” she said.
Diane Arnaout, MD, a pediatrician at Cook Children’s Pediatrics in Fort Worth, Texas, said listening to some patients explaining why vaccine injections are poisonous or a conspiracy can be exhausting and frustrating, but she agrees that presenting scientific facts alone won’t change people’s minds. “Even in my worst days, I take the time to stop talking for a moment and let the parents talk about what concerns them because if you just get mad and put a wall up, then that trust is gone, possibly forever, not just about vaccines.”
The Default Option
Since the start of the COVID-19 pandemic, Dr. Fisher has dedicated much of her time researching vaccine hesitancy. One of the most “fascinating and unexpected” findings of her work was that people are more likely to get vaccinated if a healthcare provider recommends that they get vaccinated in a “presumptive style,” which means that the provider uses language that presupposes that the person’s going to get vaccinated. “Rather than asking whether they wanted to get the vaccine conveying that the option of not getting it is just as valid, you make vaccination the default option,” she suggested.
The strategy wins many undecided, but it might not work on the most reluctant. “The presumptive recommendation is very directive, and if that works, great, but if it doesn’t, you need to shift to almost the opposite strategy, showing empathy and understanding about the person’s reasons for not wanting to be vaccinated,” Dr. Fisher said.
Find One Thing to Agree On
During a focus group on COVID-19 vaccine hesitancy that Dr. Fisher conducted in December 2021, most physicians expressed frustration that some patients remained resistant despite their best efforts. However, one participant shared an approach she found effective with even the most hesitant patients. The physician would listen carefully and express understanding, and even if what the patient said wasn’t accurate, she would find a kernel of truth to agree with and align herself with the patient. By doing this, she made patients feel like they were a team.
The example she gave was if a patient said, “I don’t know. I’ve heard different things and don’t feel comfortable taking the vaccine,” she might respond with something like, “I think it’s great that you’re thinking critically about this before making a decision. I was the same way — I wanted to fully understand the data before getting vaccinated. I also wouldn’t want to take something if I thought it wasn’t safe. It’s good that you’re being thorough.” Acknowledging their careful thought process, the physician helped patients feel seen and understood only after she introduced additional information to guide them toward understanding why the vaccine might be beneficial.
Focus on the Disease
Dr. Arnaout’s frustration grows when at the end of an appointment some parents object to vaccines with irrational and misguided concerns. “You’ve trusted me with everything else we’ve discussed today — whether it’s a diaper rash or an ear infection — so why wouldn’t you trust me on this? Sometimes it feels almost offensive — why trust my medical expertise on everything else but not vaccines?” she said.
The answer, she believes, is that vaccines are preventive, and when the threat of disease feels distant, it’s hard to see the necessity of a painful shot for your healthy child. “But if your baby were dying from meningitis, the needles we use to deliver life-saving medications in the hospital would feel absolutely necessary. It’s hard as a parent to inflict pain for something you’ve never personally seen.”
Dr. Arnaout thinks it is important to bring the focus on the disease the vaccine prevents. “Let’s talk about measles — how if a baby in my waiting room has measles and coughs, the virus can stay suspended in the air for 2 hours, and 100% of unvaccinated people in that room will get measles.”
She said sharing personal stories can also help physicians connect with their patients. “I talk to parents every day about their vaccine concerns, and I’ve found that if I take the time to explain why we vaccinate, they start to understand. I also tell them, ‘I vaccinated my children for everything on time and give them the flu shot every year. Why would I offer your child something I wouldn’t give my own?’ That personal decision, made without hesitation, resonates with parents.”
Wired for Stories
Medical professionals have a professional necessity to think and speak with precision. Their training is based on analyzing studies and data, and they develop a specialized vocabulary to describe their findings accurately.
But the human brain is naturally inclined to process and make sense of information through the structure and narrative of stories. We instinctively organize reality into a “shape of a story” rather than just isolated facts, explained Ben Riggs, senior communications specialist at Kettering Health, Dayton, Ohio, a nonfiction writing coach and author. Storytelling also taps into the emotional, rather than just the rational, parts of the brain. This emotional connection helps make the information more memorable and impactful for the listener.
Mr. Riggs said that moving from this world of precision and accuracy to one that also requires effective communication with those who haven’t had that same training is much like learning a new language. “If they can’t speak in a way that non-scientists understand, it’s like the old saying: If a tree falls in the woods and no one hears it, does it make a sound?”
Metaphors can help doctors translate scientific facts into language that meets people where they are, allowing patients to make informed decisions about their health. They can help physicians transform abstract concepts into vivid, tangible mental images that are easier for people to understand and relate to, Mr. Riggs explained. “We are predominantly concrete thinkers. Metaphors can create concrete scenes and do much of the heavy lifting when communicating complex ideas.”
“It’s important to align yourself with the other person by showing that you care, that you’re truly listening, and understand their perspective,” concluded Dr. Fisher. “Acknowledge their point of view and emphasize that they have autonomy in the decision-making process. This can open people up to hearing your perspective. You also need to know when to let go don’t cause a rift in the relationship.”
Dr. Fisher, Dr. Arnaout, and Mr. Riggs reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When Kimberly Fisher, MD, was a junior doctor, she got fired up when patients showed hesitancy about vaccines. She responded by providing numbers, data, and facts that proved vaccines were safe and effective in preventing life-threatening diseases. But she soon realized that regurgitating scientific evidence wasn’t a winning strategy. “I’ve made the mistake of launching into a let me tell you all the things that I know that you don’t know kind of lecture,” Dr. Fisher, now an associate professor of medicine at UMass Chan Medical School, Worcester, Massachusetts, a pulmonary physician, and a researcher interested in patient-provider communication, told this news organization. “Through experience and research, I have learned that when you do that, they stop listening.”
She said when patients give reasons for not getting vaccinated that are factually wrong and rooted in misinformation, the most common reaction is to correct that information and not let it stand. “That is important; it just can’t be the first thing you do,” she said.
Diane Arnaout, MD, a pediatrician at Cook Children’s Pediatrics in Fort Worth, Texas, said listening to some patients explaining why vaccine injections are poisonous or a conspiracy can be exhausting and frustrating, but she agrees that presenting scientific facts alone won’t change people’s minds. “Even in my worst days, I take the time to stop talking for a moment and let the parents talk about what concerns them because if you just get mad and put a wall up, then that trust is gone, possibly forever, not just about vaccines.”
The Default Option
Since the start of the COVID-19 pandemic, Dr. Fisher has dedicated much of her time researching vaccine hesitancy. One of the most “fascinating and unexpected” findings of her work was that people are more likely to get vaccinated if a healthcare provider recommends that they get vaccinated in a “presumptive style,” which means that the provider uses language that presupposes that the person’s going to get vaccinated. “Rather than asking whether they wanted to get the vaccine conveying that the option of not getting it is just as valid, you make vaccination the default option,” she suggested.
The strategy wins many undecided, but it might not work on the most reluctant. “The presumptive recommendation is very directive, and if that works, great, but if it doesn’t, you need to shift to almost the opposite strategy, showing empathy and understanding about the person’s reasons for not wanting to be vaccinated,” Dr. Fisher said.
Find One Thing to Agree On
During a focus group on COVID-19 vaccine hesitancy that Dr. Fisher conducted in December 2021, most physicians expressed frustration that some patients remained resistant despite their best efforts. However, one participant shared an approach she found effective with even the most hesitant patients. The physician would listen carefully and express understanding, and even if what the patient said wasn’t accurate, she would find a kernel of truth to agree with and align herself with the patient. By doing this, she made patients feel like they were a team.
The example she gave was if a patient said, “I don’t know. I’ve heard different things and don’t feel comfortable taking the vaccine,” she might respond with something like, “I think it’s great that you’re thinking critically about this before making a decision. I was the same way — I wanted to fully understand the data before getting vaccinated. I also wouldn’t want to take something if I thought it wasn’t safe. It’s good that you’re being thorough.” Acknowledging their careful thought process, the physician helped patients feel seen and understood only after she introduced additional information to guide them toward understanding why the vaccine might be beneficial.
Focus on the Disease
Dr. Arnaout’s frustration grows when at the end of an appointment some parents object to vaccines with irrational and misguided concerns. “You’ve trusted me with everything else we’ve discussed today — whether it’s a diaper rash or an ear infection — so why wouldn’t you trust me on this? Sometimes it feels almost offensive — why trust my medical expertise on everything else but not vaccines?” she said.
The answer, she believes, is that vaccines are preventive, and when the threat of disease feels distant, it’s hard to see the necessity of a painful shot for your healthy child. “But if your baby were dying from meningitis, the needles we use to deliver life-saving medications in the hospital would feel absolutely necessary. It’s hard as a parent to inflict pain for something you’ve never personally seen.”
Dr. Arnaout thinks it is important to bring the focus on the disease the vaccine prevents. “Let’s talk about measles — how if a baby in my waiting room has measles and coughs, the virus can stay suspended in the air for 2 hours, and 100% of unvaccinated people in that room will get measles.”
She said sharing personal stories can also help physicians connect with their patients. “I talk to parents every day about their vaccine concerns, and I’ve found that if I take the time to explain why we vaccinate, they start to understand. I also tell them, ‘I vaccinated my children for everything on time and give them the flu shot every year. Why would I offer your child something I wouldn’t give my own?’ That personal decision, made without hesitation, resonates with parents.”
Wired for Stories
Medical professionals have a professional necessity to think and speak with precision. Their training is based on analyzing studies and data, and they develop a specialized vocabulary to describe their findings accurately.
But the human brain is naturally inclined to process and make sense of information through the structure and narrative of stories. We instinctively organize reality into a “shape of a story” rather than just isolated facts, explained Ben Riggs, senior communications specialist at Kettering Health, Dayton, Ohio, a nonfiction writing coach and author. Storytelling also taps into the emotional, rather than just the rational, parts of the brain. This emotional connection helps make the information more memorable and impactful for the listener.
Mr. Riggs said that moving from this world of precision and accuracy to one that also requires effective communication with those who haven’t had that same training is much like learning a new language. “If they can’t speak in a way that non-scientists understand, it’s like the old saying: If a tree falls in the woods and no one hears it, does it make a sound?”
Metaphors can help doctors translate scientific facts into language that meets people where they are, allowing patients to make informed decisions about their health. They can help physicians transform abstract concepts into vivid, tangible mental images that are easier for people to understand and relate to, Mr. Riggs explained. “We are predominantly concrete thinkers. Metaphors can create concrete scenes and do much of the heavy lifting when communicating complex ideas.”
“It’s important to align yourself with the other person by showing that you care, that you’re truly listening, and understand their perspective,” concluded Dr. Fisher. “Acknowledge their point of view and emphasize that they have autonomy in the decision-making process. This can open people up to hearing your perspective. You also need to know when to let go don’t cause a rift in the relationship.”
Dr. Fisher, Dr. Arnaout, and Mr. Riggs reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When Kimberly Fisher, MD, was a junior doctor, she got fired up when patients showed hesitancy about vaccines. She responded by providing numbers, data, and facts that proved vaccines were safe and effective in preventing life-threatening diseases. But she soon realized that regurgitating scientific evidence wasn’t a winning strategy. “I’ve made the mistake of launching into a let me tell you all the things that I know that you don’t know kind of lecture,” Dr. Fisher, now an associate professor of medicine at UMass Chan Medical School, Worcester, Massachusetts, a pulmonary physician, and a researcher interested in patient-provider communication, told this news organization. “Through experience and research, I have learned that when you do that, they stop listening.”
She said when patients give reasons for not getting vaccinated that are factually wrong and rooted in misinformation, the most common reaction is to correct that information and not let it stand. “That is important; it just can’t be the first thing you do,” she said.
Diane Arnaout, MD, a pediatrician at Cook Children’s Pediatrics in Fort Worth, Texas, said listening to some patients explaining why vaccine injections are poisonous or a conspiracy can be exhausting and frustrating, but she agrees that presenting scientific facts alone won’t change people’s minds. “Even in my worst days, I take the time to stop talking for a moment and let the parents talk about what concerns them because if you just get mad and put a wall up, then that trust is gone, possibly forever, not just about vaccines.”
The Default Option
Since the start of the COVID-19 pandemic, Dr. Fisher has dedicated much of her time researching vaccine hesitancy. One of the most “fascinating and unexpected” findings of her work was that people are more likely to get vaccinated if a healthcare provider recommends that they get vaccinated in a “presumptive style,” which means that the provider uses language that presupposes that the person’s going to get vaccinated. “Rather than asking whether they wanted to get the vaccine conveying that the option of not getting it is just as valid, you make vaccination the default option,” she suggested.
The strategy wins many undecided, but it might not work on the most reluctant. “The presumptive recommendation is very directive, and if that works, great, but if it doesn’t, you need to shift to almost the opposite strategy, showing empathy and understanding about the person’s reasons for not wanting to be vaccinated,” Dr. Fisher said.
Find One Thing to Agree On
During a focus group on COVID-19 vaccine hesitancy that Dr. Fisher conducted in December 2021, most physicians expressed frustration that some patients remained resistant despite their best efforts. However, one participant shared an approach she found effective with even the most hesitant patients. The physician would listen carefully and express understanding, and even if what the patient said wasn’t accurate, she would find a kernel of truth to agree with and align herself with the patient. By doing this, she made patients feel like they were a team.
The example she gave was if a patient said, “I don’t know. I’ve heard different things and don’t feel comfortable taking the vaccine,” she might respond with something like, “I think it’s great that you’re thinking critically about this before making a decision. I was the same way — I wanted to fully understand the data before getting vaccinated. I also wouldn’t want to take something if I thought it wasn’t safe. It’s good that you’re being thorough.” Acknowledging their careful thought process, the physician helped patients feel seen and understood only after she introduced additional information to guide them toward understanding why the vaccine might be beneficial.
Focus on the Disease
Dr. Arnaout’s frustration grows when at the end of an appointment some parents object to vaccines with irrational and misguided concerns. “You’ve trusted me with everything else we’ve discussed today — whether it’s a diaper rash or an ear infection — so why wouldn’t you trust me on this? Sometimes it feels almost offensive — why trust my medical expertise on everything else but not vaccines?” she said.
The answer, she believes, is that vaccines are preventive, and when the threat of disease feels distant, it’s hard to see the necessity of a painful shot for your healthy child. “But if your baby were dying from meningitis, the needles we use to deliver life-saving medications in the hospital would feel absolutely necessary. It’s hard as a parent to inflict pain for something you’ve never personally seen.”
Dr. Arnaout thinks it is important to bring the focus on the disease the vaccine prevents. “Let’s talk about measles — how if a baby in my waiting room has measles and coughs, the virus can stay suspended in the air for 2 hours, and 100% of unvaccinated people in that room will get measles.”
She said sharing personal stories can also help physicians connect with their patients. “I talk to parents every day about their vaccine concerns, and I’ve found that if I take the time to explain why we vaccinate, they start to understand. I also tell them, ‘I vaccinated my children for everything on time and give them the flu shot every year. Why would I offer your child something I wouldn’t give my own?’ That personal decision, made without hesitation, resonates with parents.”
Wired for Stories
Medical professionals have a professional necessity to think and speak with precision. Their training is based on analyzing studies and data, and they develop a specialized vocabulary to describe their findings accurately.
But the human brain is naturally inclined to process and make sense of information through the structure and narrative of stories. We instinctively organize reality into a “shape of a story” rather than just isolated facts, explained Ben Riggs, senior communications specialist at Kettering Health, Dayton, Ohio, a nonfiction writing coach and author. Storytelling also taps into the emotional, rather than just the rational, parts of the brain. This emotional connection helps make the information more memorable and impactful for the listener.
Mr. Riggs said that moving from this world of precision and accuracy to one that also requires effective communication with those who haven’t had that same training is much like learning a new language. “If they can’t speak in a way that non-scientists understand, it’s like the old saying: If a tree falls in the woods and no one hears it, does it make a sound?”
Metaphors can help doctors translate scientific facts into language that meets people where they are, allowing patients to make informed decisions about their health. They can help physicians transform abstract concepts into vivid, tangible mental images that are easier for people to understand and relate to, Mr. Riggs explained. “We are predominantly concrete thinkers. Metaphors can create concrete scenes and do much of the heavy lifting when communicating complex ideas.”
“It’s important to align yourself with the other person by showing that you care, that you’re truly listening, and understand their perspective,” concluded Dr. Fisher. “Acknowledge their point of view and emphasize that they have autonomy in the decision-making process. This can open people up to hearing your perspective. You also need to know when to let go don’t cause a rift in the relationship.”
Dr. Fisher, Dr. Arnaout, and Mr. Riggs reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Down Syndrome: Several Cutaneous Conditions Common, Study Finds
TOPLINE:
(DS) in a 10-year retrospective study.
METHODOLOGY:
- Researchers conducted a multicenter retrospective study of 1529 patients with DS from eight outpatient dermatology clinics in the United States and Canada between 2011 and 2021.
- In total, 50.8% of patients were children (0-12 years), 25.2% were adolescents (13-17 years), and 24% were adults (≥ 18 years).
- The researchers evaluated skin conditions in the patients.
TAKEAWAY:
- Eczematous dermatitis was the most common diagnosis, affecting 26% of patients, followed by folliculitis (19.3%) and seborrheic dermatitis (15.6%). Dermatophyte infections were diagnosed in 13%.
- Alopecia areata was the most common autoimmune skin condition, diagnosed in 178 patients (11.6%); 135 (75.8%) were children. Vitiligo was diagnosed in 66 patients (4.3%).
- The most common cutaneous infections were onychomycosis (5.9%), tinea pedis (5%), and verruca vulgaris/other viral warts (5%).
- High-risk medication use was reported in 4.3% of patients; acne vulgaris, hidradenitis suppurativa, and eczematous dermatitis were the most common associated conditions with such medications.
IN PRACTICE:
“Children, adolescents, and adults with DS are most often found to have eczematous, adnexal, and autoimmune skin conditions at outpatient dermatology visits,” the authors wrote. Their findings, they added, “offer valuable insights for clinicians and researchers, aiding in the improved prioritization of screening, diagnosis, and management, as well as facilitating both basic science and clinical research into prevalent skin conditions in individuals with DS.”
SOURCE:
The study was led by Tasya Rakasiwi, of the Department of Dermatology, Dartmouth Health, Manchester, New Hampshire, and was published online in Pediatric Dermatology.
LIMITATIONS:
Over 50% of the patients were children, potentially resulting in bias toward pediatric diagnoses and younger ages of presentation. Race, ethnicity, and sociodemographic factors were not captured, limiting the generalizability of the findings. Medical codes often do not capture disease phenotype or severity, and the manual conversion of International Classification of Diseases (ICD) 9 to ICD-10 codes may introduce potential conversion errors.
DISCLOSURES:
The study was supported by the Pediatric Dermatology Research Alliance. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
(DS) in a 10-year retrospective study.
METHODOLOGY:
- Researchers conducted a multicenter retrospective study of 1529 patients with DS from eight outpatient dermatology clinics in the United States and Canada between 2011 and 2021.
- In total, 50.8% of patients were children (0-12 years), 25.2% were adolescents (13-17 years), and 24% were adults (≥ 18 years).
- The researchers evaluated skin conditions in the patients.
TAKEAWAY:
- Eczematous dermatitis was the most common diagnosis, affecting 26% of patients, followed by folliculitis (19.3%) and seborrheic dermatitis (15.6%). Dermatophyte infections were diagnosed in 13%.
- Alopecia areata was the most common autoimmune skin condition, diagnosed in 178 patients (11.6%); 135 (75.8%) were children. Vitiligo was diagnosed in 66 patients (4.3%).
- The most common cutaneous infections were onychomycosis (5.9%), tinea pedis (5%), and verruca vulgaris/other viral warts (5%).
- High-risk medication use was reported in 4.3% of patients; acne vulgaris, hidradenitis suppurativa, and eczematous dermatitis were the most common associated conditions with such medications.
IN PRACTICE:
“Children, adolescents, and adults with DS are most often found to have eczematous, adnexal, and autoimmune skin conditions at outpatient dermatology visits,” the authors wrote. Their findings, they added, “offer valuable insights for clinicians and researchers, aiding in the improved prioritization of screening, diagnosis, and management, as well as facilitating both basic science and clinical research into prevalent skin conditions in individuals with DS.”
SOURCE:
The study was led by Tasya Rakasiwi, of the Department of Dermatology, Dartmouth Health, Manchester, New Hampshire, and was published online in Pediatric Dermatology.
LIMITATIONS:
Over 50% of the patients were children, potentially resulting in bias toward pediatric diagnoses and younger ages of presentation. Race, ethnicity, and sociodemographic factors were not captured, limiting the generalizability of the findings. Medical codes often do not capture disease phenotype or severity, and the manual conversion of International Classification of Diseases (ICD) 9 to ICD-10 codes may introduce potential conversion errors.
DISCLOSURES:
The study was supported by the Pediatric Dermatology Research Alliance. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
(DS) in a 10-year retrospective study.
METHODOLOGY:
- Researchers conducted a multicenter retrospective study of 1529 patients with DS from eight outpatient dermatology clinics in the United States and Canada between 2011 and 2021.
- In total, 50.8% of patients were children (0-12 years), 25.2% were adolescents (13-17 years), and 24% were adults (≥ 18 years).
- The researchers evaluated skin conditions in the patients.
TAKEAWAY:
- Eczematous dermatitis was the most common diagnosis, affecting 26% of patients, followed by folliculitis (19.3%) and seborrheic dermatitis (15.6%). Dermatophyte infections were diagnosed in 13%.
- Alopecia areata was the most common autoimmune skin condition, diagnosed in 178 patients (11.6%); 135 (75.8%) were children. Vitiligo was diagnosed in 66 patients (4.3%).
- The most common cutaneous infections were onychomycosis (5.9%), tinea pedis (5%), and verruca vulgaris/other viral warts (5%).
- High-risk medication use was reported in 4.3% of patients; acne vulgaris, hidradenitis suppurativa, and eczematous dermatitis were the most common associated conditions with such medications.
IN PRACTICE:
“Children, adolescents, and adults with DS are most often found to have eczematous, adnexal, and autoimmune skin conditions at outpatient dermatology visits,” the authors wrote. Their findings, they added, “offer valuable insights for clinicians and researchers, aiding in the improved prioritization of screening, diagnosis, and management, as well as facilitating both basic science and clinical research into prevalent skin conditions in individuals with DS.”
SOURCE:
The study was led by Tasya Rakasiwi, of the Department of Dermatology, Dartmouth Health, Manchester, New Hampshire, and was published online in Pediatric Dermatology.
LIMITATIONS:
Over 50% of the patients were children, potentially resulting in bias toward pediatric diagnoses and younger ages of presentation. Race, ethnicity, and sociodemographic factors were not captured, limiting the generalizability of the findings. Medical codes often do not capture disease phenotype or severity, and the manual conversion of International Classification of Diseases (ICD) 9 to ICD-10 codes may introduce potential conversion errors.
DISCLOSURES:
The study was supported by the Pediatric Dermatology Research Alliance. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Reduced Vaccination Rates Contribute to Rising Pertussis Numbers
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Caregiver Surveys on Firearms, Suicide Offer Pediatricians Prevention Opportunities
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
From AAP 2024
FDA Approves Ustekinumab Biosimilar Otulfi
This is the fourth ustekinumab biosimilar approved in the United States. Like the reference product, ustekinumab-aauz is indicated for:
- Patients 6 years or older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy
- Patients 6 years or older with active psoriatic arthritis
- Adult patients with moderately to severely active Crohn’s disease
- Adult patients with moderately to severely active ulcerative colitis
Ustekinumab-aauz, produced by a partnership between Fresenius Kabi and Formycon, has two formulations: subcutaneous injection (45 mg/0.5 mL or 90 mg/mL solution in a single-dose prefilled syringe) or intravenous infusion (130 mg/26 mL solution in a single-dose vial).
The biosimilar will launch in the United States “no later than February 22, 2025,” according to the press release, “in accordance with the patent settlement between Fresenius Kabi, Formycon, and Johnson & Johnson.”
Ustekinumab-aauz is Fresenius Kabi’s fourth biosimilar granted US approval, behind adalimumab-aacf (Idacio), tocilizumab-aazg (Tyenne), and pegfilgrastim-fpgk (Stimufend).
A version of this article first appeared on Medscape.com.
This is the fourth ustekinumab biosimilar approved in the United States. Like the reference product, ustekinumab-aauz is indicated for:
- Patients 6 years or older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy
- Patients 6 years or older with active psoriatic arthritis
- Adult patients with moderately to severely active Crohn’s disease
- Adult patients with moderately to severely active ulcerative colitis
Ustekinumab-aauz, produced by a partnership between Fresenius Kabi and Formycon, has two formulations: subcutaneous injection (45 mg/0.5 mL or 90 mg/mL solution in a single-dose prefilled syringe) or intravenous infusion (130 mg/26 mL solution in a single-dose vial).
The biosimilar will launch in the United States “no later than February 22, 2025,” according to the press release, “in accordance with the patent settlement between Fresenius Kabi, Formycon, and Johnson & Johnson.”
Ustekinumab-aauz is Fresenius Kabi’s fourth biosimilar granted US approval, behind adalimumab-aacf (Idacio), tocilizumab-aazg (Tyenne), and pegfilgrastim-fpgk (Stimufend).
A version of this article first appeared on Medscape.com.
This is the fourth ustekinumab biosimilar approved in the United States. Like the reference product, ustekinumab-aauz is indicated for:
- Patients 6 years or older with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy
- Patients 6 years or older with active psoriatic arthritis
- Adult patients with moderately to severely active Crohn’s disease
- Adult patients with moderately to severely active ulcerative colitis
Ustekinumab-aauz, produced by a partnership between Fresenius Kabi and Formycon, has two formulations: subcutaneous injection (45 mg/0.5 mL or 90 mg/mL solution in a single-dose prefilled syringe) or intravenous infusion (130 mg/26 mL solution in a single-dose vial).
The biosimilar will launch in the United States “no later than February 22, 2025,” according to the press release, “in accordance with the patent settlement between Fresenius Kabi, Formycon, and Johnson & Johnson.”
Ustekinumab-aauz is Fresenius Kabi’s fourth biosimilar granted US approval, behind adalimumab-aacf (Idacio), tocilizumab-aazg (Tyenne), and pegfilgrastim-fpgk (Stimufend).
A version of this article first appeared on Medscape.com.
Study Supports Efficacy of Home-Based Phototherapy for Psoriasis
TOPLINE:
study.
METHODOLOGY:
- The pragmatic, investigator-initiated, open-label, noninferiority, randomized trial compared the effectiveness of 12 weeks of treatment with narrow-band ultraviolet B phototherapy administered at home (n = 393) vs at the doctor’s office (n = 390).
- Overall, 783 patients with plaque or guttate psoriasis (mean age, 48 years; 48% women) were enrolled at 42 academic and private clinical dermatology practices in the United States from March 1, 2019, to December 4, 2023, and were followed up through June 2024. At baseline, the mean Physician Global Assessment (PGA) and the mean Dermatology Life Quality Index (DLQI) scores were 2.7 and 12.2, respectively.
- The two co-primary endpoints were a PGA score ≤ 1 indicating clear or almost clear skin and a DLQI score ≤ 5.
TAKEAWAY:
- At 12 weeks, a PGA score ≤ 1 was achieved in 32.8% of patients using home-based phototherapy and in 25.6% of those who received office-based phototherapy (P < .001).
- At 12 weeks, a DLQI score ≤ 5 was achieved in 52.4% and 33.6% of home- and office-treated patients, respectively (P < .001).
- Similar benefits were seen across all Fitzpatrick skin types.
- A higher percentage of patients were adherent to home-based (51.4%) vs office-based (15.9%) phototherapy (P < .001).
IN PRACTICE:
“These data support the use of home phototherapy as a first-line treatment option for psoriasis,” and “efforts are needed to make home and office phototherapy more available to patients,” said the study’s lead author.
SOURCE:
Joel M. Gelfand, MD, director of the Psoriasis and Phototherapy Treatment Center at the University of Pennsylvania, Philadelphia, presented the findings at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis meeting during the annual meeting of the European Academy of Dermatology and Venereology, with simultaneous publication in JAMA Dermatology.
LIMITATIONS:
This was an open-label trial and because of its pragmatic design, outcome data were missing. The cost of the home-based phototherapy equipment used in the study was $6040.88, which was mostly covered by Medicare, but direct costs to patients may have varied depending on their insurance plan.
DISCLOSURES:
The Patient-Centered Outcomes Research Institute funded the study. Daavlin provided and shipped machines for home-based phototherapy to patients at no cost. Dr. Gelfand disclosed serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, Boehringer Ingelheim, Celldex, and other companies. The full list of author disclosures can be found in the published study.
A version of this article first appeared on Medscape.com.
TOPLINE:
study.
METHODOLOGY:
- The pragmatic, investigator-initiated, open-label, noninferiority, randomized trial compared the effectiveness of 12 weeks of treatment with narrow-band ultraviolet B phototherapy administered at home (n = 393) vs at the doctor’s office (n = 390).
- Overall, 783 patients with plaque or guttate psoriasis (mean age, 48 years; 48% women) were enrolled at 42 academic and private clinical dermatology practices in the United States from March 1, 2019, to December 4, 2023, and were followed up through June 2024. At baseline, the mean Physician Global Assessment (PGA) and the mean Dermatology Life Quality Index (DLQI) scores were 2.7 and 12.2, respectively.
- The two co-primary endpoints were a PGA score ≤ 1 indicating clear or almost clear skin and a DLQI score ≤ 5.
TAKEAWAY:
- At 12 weeks, a PGA score ≤ 1 was achieved in 32.8% of patients using home-based phototherapy and in 25.6% of those who received office-based phototherapy (P < .001).
- At 12 weeks, a DLQI score ≤ 5 was achieved in 52.4% and 33.6% of home- and office-treated patients, respectively (P < .001).
- Similar benefits were seen across all Fitzpatrick skin types.
- A higher percentage of patients were adherent to home-based (51.4%) vs office-based (15.9%) phototherapy (P < .001).
IN PRACTICE:
“These data support the use of home phototherapy as a first-line treatment option for psoriasis,” and “efforts are needed to make home and office phototherapy more available to patients,” said the study’s lead author.
SOURCE:
Joel M. Gelfand, MD, director of the Psoriasis and Phototherapy Treatment Center at the University of Pennsylvania, Philadelphia, presented the findings at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis meeting during the annual meeting of the European Academy of Dermatology and Venereology, with simultaneous publication in JAMA Dermatology.
LIMITATIONS:
This was an open-label trial and because of its pragmatic design, outcome data were missing. The cost of the home-based phototherapy equipment used in the study was $6040.88, which was mostly covered by Medicare, but direct costs to patients may have varied depending on their insurance plan.
DISCLOSURES:
The Patient-Centered Outcomes Research Institute funded the study. Daavlin provided and shipped machines for home-based phototherapy to patients at no cost. Dr. Gelfand disclosed serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, Boehringer Ingelheim, Celldex, and other companies. The full list of author disclosures can be found in the published study.
A version of this article first appeared on Medscape.com.
TOPLINE:
study.
METHODOLOGY:
- The pragmatic, investigator-initiated, open-label, noninferiority, randomized trial compared the effectiveness of 12 weeks of treatment with narrow-band ultraviolet B phototherapy administered at home (n = 393) vs at the doctor’s office (n = 390).
- Overall, 783 patients with plaque or guttate psoriasis (mean age, 48 years; 48% women) were enrolled at 42 academic and private clinical dermatology practices in the United States from March 1, 2019, to December 4, 2023, and were followed up through June 2024. At baseline, the mean Physician Global Assessment (PGA) and the mean Dermatology Life Quality Index (DLQI) scores were 2.7 and 12.2, respectively.
- The two co-primary endpoints were a PGA score ≤ 1 indicating clear or almost clear skin and a DLQI score ≤ 5.
TAKEAWAY:
- At 12 weeks, a PGA score ≤ 1 was achieved in 32.8% of patients using home-based phototherapy and in 25.6% of those who received office-based phototherapy (P < .001).
- At 12 weeks, a DLQI score ≤ 5 was achieved in 52.4% and 33.6% of home- and office-treated patients, respectively (P < .001).
- Similar benefits were seen across all Fitzpatrick skin types.
- A higher percentage of patients were adherent to home-based (51.4%) vs office-based (15.9%) phototherapy (P < .001).
IN PRACTICE:
“These data support the use of home phototherapy as a first-line treatment option for psoriasis,” and “efforts are needed to make home and office phototherapy more available to patients,” said the study’s lead author.
SOURCE:
Joel M. Gelfand, MD, director of the Psoriasis and Phototherapy Treatment Center at the University of Pennsylvania, Philadelphia, presented the findings at the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis meeting during the annual meeting of the European Academy of Dermatology and Venereology, with simultaneous publication in JAMA Dermatology.
LIMITATIONS:
This was an open-label trial and because of its pragmatic design, outcome data were missing. The cost of the home-based phototherapy equipment used in the study was $6040.88, which was mostly covered by Medicare, but direct costs to patients may have varied depending on their insurance plan.
DISCLOSURES:
The Patient-Centered Outcomes Research Institute funded the study. Daavlin provided and shipped machines for home-based phototherapy to patients at no cost. Dr. Gelfand disclosed serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, Boehringer Ingelheim, Celldex, and other companies. The full list of author disclosures can be found in the published study.
A version of this article first appeared on Medscape.com.






