User login
Wounded Warriors Fight Invasive Fungal Infections
DALLAS – Deadly invasive fungal infections are increasingly being identified in soft-tissue and intra-abdominal wounds in troops deployed to Iraq and Afghanistan, prompting the creation of hospital-based clinical practice guidelines.
When the first case emerged in July 2009, the medical team initially suspected significant bacterial infection in a young, previously healthy Marine with extensive soft-tissue injuries. By the time appropriate antifungal therapies were initiated in week 3, it was too late. An autopsy revealed that the 22-year-old soldier’s death was from systemic angioinvasive Aspergillus terreus (Surg. Infect. [Larchmt.] 2011;12:397-400).
"We were not expecting the degree of mold infestation early on," Col. Debra Malone, MC, USAF, trauma research director of the Walter Reed National Military Medical Center (NMMC) in Bethesda, Md., said in an interview. "It’s not necessarily that things were missed – it’s that the disease itself didn’t present early on.
"Sometimes it can take 2, 3, 6 weeks for certain molds to actually grow. Now we don’t wait for them to grow. If we have the clinical suspicion, we treat right away with very powerful antimold medications."
The NMMC has also developed a 24-hour invasive fungal infection (IFI) pathology protocol and hospital-based clinical practice guidelines to improve outcomes for trauma-related IFI, which has a reported mortality rate of 25% in previously immunocompetent patients.
From July 2009 to November 2011, IFI was suspected or identified on pathology in 75 of 2,755 trauma patients admitted to the NMMC, Dr. Malone reported at the annual meeting of the Surgical Infection Society.
Although the index case occurred in the heavily agricultural Helmand Province in Afghanistan, IFI cases are cropping up throughout Iraq and Afghanistan, particularly in troops with injuries caused by improvised explosive devices (IEDs).
"It’s not uncommon for the bomb to cause a big crater in the ground, and all that dirt or whatever has been displaced," she said. "We think it’s been driven up into the body, deep into the open wounds, and that the mold spores are sitting up there, just percolating."
The typical patient is an 18-year-old with devastating soft-tissue IED blast injuries who is resuscitated and has wounds debrided to normal tissue. However, 5-7 days later, there is evidence of infected tissue on successive washouts, and the patient is hypertensive and in shock.
Frozen-section histopathology was initially used for diagnosis because of its quick turnaround, but resulted in a 33% negative predictive value in their lab and is no longer used, Dr. Malone said. This led to the 24-hour IFI protocol utilizing permanent sections. Periodic acid-Schiff and Gomori methenamine silver staining have proved efficacious for Aspergillus species, but not as efficacious for identifying Mucorales species. Calcofluor white staining is also used and may allow morphology-based speciation.
In all, 42 (56%) of the 75 patients met histologic criteria for IFI. Notably, IFI was suspected clinically in the remaining patients but never proved by histologic criteria. More than a fourth (28%) of wounds infected with Mucor were coinfected with non-Mucor species. In addition, the vast majority of wounds will be coinfected with bacteria, according to the investigators, led by Dr. Carlos Rodriguez, an attending trauma and critical care surgeon at NMMC.
Therapy should include aggressive debridement, with minimization of blood loss. Surgery should be repeated every 24-48 hours until the wounds are clean, with compromised tissue sent from every surgery for histopathology and culture. Changes in surgical practice as related to the treatment of nonnecrotic tissue abnormalities may have led to improvement in tissue salvage.
Broad-spectrum antifungal medications should be tailored based on serial tissue specimen culture results. Focused antifungal therapies should be continued for 2-3 weeks after wound closure. Liposomal amphotericin B and the triazoles – voriconazole (Vfend) and posaconazole (Noxafil) – have been used as initial therapies. Vancomycin (Vancocin) and meropenem (Merrem IV) also should be considered because of the high risk of coinfection with bacteria.
Adjunctive therapies include minimization of immunosuppression, antimicrobial beads in open wounds, and negative-pressure wound therapy with a 0.025% Dakin’s solution (sodium hypochlorite). Intra-abdominal washings with amphotericin B, voriconazole, or bacitracin plus gentamicin can be utilized on a case-by-case basis.
Among the 75 patients, the time from injury to IFI diagnosis decreased from 10 days (range 7-12) in 2009 to 3 days (range 2-6 days) in 2011. The mortality rate was 4%; mean ICU length of stay, 13 days; and mean hospital stay, 48 days. All IFI patients were male; their mean age was 24 years, and their mean Injury Severity Score was 23.
Although the authors acknowledged that significant diagnostic challenges persist and that weaknesses still exist in their guidelines, progress has been made.
"We’re saving these guys now because the guideline that we developed is allowing us to do a better job," Dr. Malone said. "They’re losing less tissue with surgical debridements, and they’re surviving. So we’ve come a long way since we identified the problem."
"This observation is important not only for military patients but also for patients with contaminated civilian wounds," said Dr. Grace Rozycki, who was asked to comment on the findings. "As the authors point out, the diagnosis is difficult to make and cultures, although helpful, may take several weeks. A presumptive diagnosis is helpful so that antifungal and antibiotic therapy can be started early," said Dr. Rozycki, chief of the division of trauma/surgical critical care, department of surgery, Emory University, Atlanta.
The project was funded by the National Institute of Allergy and Infectious Diseases and the Department of the Navy under the Wounded, Ill, and Injured program.
DALLAS – Deadly invasive fungal infections are increasingly being identified in soft-tissue and intra-abdominal wounds in troops deployed to Iraq and Afghanistan, prompting the creation of hospital-based clinical practice guidelines.
When the first case emerged in July 2009, the medical team initially suspected significant bacterial infection in a young, previously healthy Marine with extensive soft-tissue injuries. By the time appropriate antifungal therapies were initiated in week 3, it was too late. An autopsy revealed that the 22-year-old soldier’s death was from systemic angioinvasive Aspergillus terreus (Surg. Infect. [Larchmt.] 2011;12:397-400).
"We were not expecting the degree of mold infestation early on," Col. Debra Malone, MC, USAF, trauma research director of the Walter Reed National Military Medical Center (NMMC) in Bethesda, Md., said in an interview. "It’s not necessarily that things were missed – it’s that the disease itself didn’t present early on.
"Sometimes it can take 2, 3, 6 weeks for certain molds to actually grow. Now we don’t wait for them to grow. If we have the clinical suspicion, we treat right away with very powerful antimold medications."
The NMMC has also developed a 24-hour invasive fungal infection (IFI) pathology protocol and hospital-based clinical practice guidelines to improve outcomes for trauma-related IFI, which has a reported mortality rate of 25% in previously immunocompetent patients.
From July 2009 to November 2011, IFI was suspected or identified on pathology in 75 of 2,755 trauma patients admitted to the NMMC, Dr. Malone reported at the annual meeting of the Surgical Infection Society.
Although the index case occurred in the heavily agricultural Helmand Province in Afghanistan, IFI cases are cropping up throughout Iraq and Afghanistan, particularly in troops with injuries caused by improvised explosive devices (IEDs).
"It’s not uncommon for the bomb to cause a big crater in the ground, and all that dirt or whatever has been displaced," she said. "We think it’s been driven up into the body, deep into the open wounds, and that the mold spores are sitting up there, just percolating."
The typical patient is an 18-year-old with devastating soft-tissue IED blast injuries who is resuscitated and has wounds debrided to normal tissue. However, 5-7 days later, there is evidence of infected tissue on successive washouts, and the patient is hypertensive and in shock.
Frozen-section histopathology was initially used for diagnosis because of its quick turnaround, but resulted in a 33% negative predictive value in their lab and is no longer used, Dr. Malone said. This led to the 24-hour IFI protocol utilizing permanent sections. Periodic acid-Schiff and Gomori methenamine silver staining have proved efficacious for Aspergillus species, but not as efficacious for identifying Mucorales species. Calcofluor white staining is also used and may allow morphology-based speciation.
In all, 42 (56%) of the 75 patients met histologic criteria for IFI. Notably, IFI was suspected clinically in the remaining patients but never proved by histologic criteria. More than a fourth (28%) of wounds infected with Mucor were coinfected with non-Mucor species. In addition, the vast majority of wounds will be coinfected with bacteria, according to the investigators, led by Dr. Carlos Rodriguez, an attending trauma and critical care surgeon at NMMC.
Therapy should include aggressive debridement, with minimization of blood loss. Surgery should be repeated every 24-48 hours until the wounds are clean, with compromised tissue sent from every surgery for histopathology and culture. Changes in surgical practice as related to the treatment of nonnecrotic tissue abnormalities may have led to improvement in tissue salvage.
Broad-spectrum antifungal medications should be tailored based on serial tissue specimen culture results. Focused antifungal therapies should be continued for 2-3 weeks after wound closure. Liposomal amphotericin B and the triazoles – voriconazole (Vfend) and posaconazole (Noxafil) – have been used as initial therapies. Vancomycin (Vancocin) and meropenem (Merrem IV) also should be considered because of the high risk of coinfection with bacteria.
Adjunctive therapies include minimization of immunosuppression, antimicrobial beads in open wounds, and negative-pressure wound therapy with a 0.025% Dakin’s solution (sodium hypochlorite). Intra-abdominal washings with amphotericin B, voriconazole, or bacitracin plus gentamicin can be utilized on a case-by-case basis.
Among the 75 patients, the time from injury to IFI diagnosis decreased from 10 days (range 7-12) in 2009 to 3 days (range 2-6 days) in 2011. The mortality rate was 4%; mean ICU length of stay, 13 days; and mean hospital stay, 48 days. All IFI patients were male; their mean age was 24 years, and their mean Injury Severity Score was 23.
Although the authors acknowledged that significant diagnostic challenges persist and that weaknesses still exist in their guidelines, progress has been made.
"We’re saving these guys now because the guideline that we developed is allowing us to do a better job," Dr. Malone said. "They’re losing less tissue with surgical debridements, and they’re surviving. So we’ve come a long way since we identified the problem."
"This observation is important not only for military patients but also for patients with contaminated civilian wounds," said Dr. Grace Rozycki, who was asked to comment on the findings. "As the authors point out, the diagnosis is difficult to make and cultures, although helpful, may take several weeks. A presumptive diagnosis is helpful so that antifungal and antibiotic therapy can be started early," said Dr. Rozycki, chief of the division of trauma/surgical critical care, department of surgery, Emory University, Atlanta.
The project was funded by the National Institute of Allergy and Infectious Diseases and the Department of the Navy under the Wounded, Ill, and Injured program.
DALLAS – Deadly invasive fungal infections are increasingly being identified in soft-tissue and intra-abdominal wounds in troops deployed to Iraq and Afghanistan, prompting the creation of hospital-based clinical practice guidelines.
When the first case emerged in July 2009, the medical team initially suspected significant bacterial infection in a young, previously healthy Marine with extensive soft-tissue injuries. By the time appropriate antifungal therapies were initiated in week 3, it was too late. An autopsy revealed that the 22-year-old soldier’s death was from systemic angioinvasive Aspergillus terreus (Surg. Infect. [Larchmt.] 2011;12:397-400).
"We were not expecting the degree of mold infestation early on," Col. Debra Malone, MC, USAF, trauma research director of the Walter Reed National Military Medical Center (NMMC) in Bethesda, Md., said in an interview. "It’s not necessarily that things were missed – it’s that the disease itself didn’t present early on.
"Sometimes it can take 2, 3, 6 weeks for certain molds to actually grow. Now we don’t wait for them to grow. If we have the clinical suspicion, we treat right away with very powerful antimold medications."
The NMMC has also developed a 24-hour invasive fungal infection (IFI) pathology protocol and hospital-based clinical practice guidelines to improve outcomes for trauma-related IFI, which has a reported mortality rate of 25% in previously immunocompetent patients.
From July 2009 to November 2011, IFI was suspected or identified on pathology in 75 of 2,755 trauma patients admitted to the NMMC, Dr. Malone reported at the annual meeting of the Surgical Infection Society.
Although the index case occurred in the heavily agricultural Helmand Province in Afghanistan, IFI cases are cropping up throughout Iraq and Afghanistan, particularly in troops with injuries caused by improvised explosive devices (IEDs).
"It’s not uncommon for the bomb to cause a big crater in the ground, and all that dirt or whatever has been displaced," she said. "We think it’s been driven up into the body, deep into the open wounds, and that the mold spores are sitting up there, just percolating."
The typical patient is an 18-year-old with devastating soft-tissue IED blast injuries who is resuscitated and has wounds debrided to normal tissue. However, 5-7 days later, there is evidence of infected tissue on successive washouts, and the patient is hypertensive and in shock.
Frozen-section histopathology was initially used for diagnosis because of its quick turnaround, but resulted in a 33% negative predictive value in their lab and is no longer used, Dr. Malone said. This led to the 24-hour IFI protocol utilizing permanent sections. Periodic acid-Schiff and Gomori methenamine silver staining have proved efficacious for Aspergillus species, but not as efficacious for identifying Mucorales species. Calcofluor white staining is also used and may allow morphology-based speciation.
In all, 42 (56%) of the 75 patients met histologic criteria for IFI. Notably, IFI was suspected clinically in the remaining patients but never proved by histologic criteria. More than a fourth (28%) of wounds infected with Mucor were coinfected with non-Mucor species. In addition, the vast majority of wounds will be coinfected with bacteria, according to the investigators, led by Dr. Carlos Rodriguez, an attending trauma and critical care surgeon at NMMC.
Therapy should include aggressive debridement, with minimization of blood loss. Surgery should be repeated every 24-48 hours until the wounds are clean, with compromised tissue sent from every surgery for histopathology and culture. Changes in surgical practice as related to the treatment of nonnecrotic tissue abnormalities may have led to improvement in tissue salvage.
Broad-spectrum antifungal medications should be tailored based on serial tissue specimen culture results. Focused antifungal therapies should be continued for 2-3 weeks after wound closure. Liposomal amphotericin B and the triazoles – voriconazole (Vfend) and posaconazole (Noxafil) – have been used as initial therapies. Vancomycin (Vancocin) and meropenem (Merrem IV) also should be considered because of the high risk of coinfection with bacteria.
Adjunctive therapies include minimization of immunosuppression, antimicrobial beads in open wounds, and negative-pressure wound therapy with a 0.025% Dakin’s solution (sodium hypochlorite). Intra-abdominal washings with amphotericin B, voriconazole, or bacitracin plus gentamicin can be utilized on a case-by-case basis.
Among the 75 patients, the time from injury to IFI diagnosis decreased from 10 days (range 7-12) in 2009 to 3 days (range 2-6 days) in 2011. The mortality rate was 4%; mean ICU length of stay, 13 days; and mean hospital stay, 48 days. All IFI patients were male; their mean age was 24 years, and their mean Injury Severity Score was 23.
Although the authors acknowledged that significant diagnostic challenges persist and that weaknesses still exist in their guidelines, progress has been made.
"We’re saving these guys now because the guideline that we developed is allowing us to do a better job," Dr. Malone said. "They’re losing less tissue with surgical debridements, and they’re surviving. So we’ve come a long way since we identified the problem."
"This observation is important not only for military patients but also for patients with contaminated civilian wounds," said Dr. Grace Rozycki, who was asked to comment on the findings. "As the authors point out, the diagnosis is difficult to make and cultures, although helpful, may take several weeks. A presumptive diagnosis is helpful so that antifungal and antibiotic therapy can be started early," said Dr. Rozycki, chief of the division of trauma/surgical critical care, department of surgery, Emory University, Atlanta.
The project was funded by the National Institute of Allergy and Infectious Diseases and the Department of the Navy under the Wounded, Ill, and Injured program.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY
Major Finding: Invasive fungal infection was suspected or identified on pathology in 75 of 2,755 trauma patients admitted to the NNMC.
Data Source: The study was a retrospective analysis of 2,755 hospitalized troops with traumatic injuries.
Disclosures: The project was funded by the National Institute of Allergy and Infectious Diseases and the Department of the Navy under the Wounded, Ill, and Injured Program.
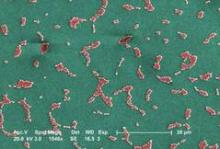
Multidrug Resistance Not Linked to Acinetobacter-Related Deaths
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
DALLAS – In a surprising twist, multidrug resistance and antibiotic appropriateness were not correlated with mortality in a retrospective analysis of critically ill patients infected with Acinetobacter bacillus.
Acinetobacter infections among critically ill patients are increasing and have been associated with mortality rates of 26%-68%. The mortality rates are thought to be driven by high rates of multidrug resistance and subsequent delays in appropriate antimicrobial therapy, Claire Murphy, Pharm.D., explained at the annual meeting of the Surgical Infection Society.
She presented data on 156 surgical and medical ICU patients with at least one positive Acinetobacter culture and associated clinical symptoms who were admitted to an ICU between January 2006 and December 2009. In-hospital mortality was 35%.
Patients who died had significantly higher APACHE II (Acute Physiology and Chronic Health Evaluation II) II scores than did survivors (22.3 vs. 19.5; P = .02), and were more likely to be surgical patients (50% vs. 33.3%; P = .04) and to be in an immunosuppressed state (33.3% vs. 16.7%; P = .02).
Survivors were significantly younger (53 years vs. 59 years; P = .006), and – inexplicably – more likely to have prior colonization or infection with methicillin-resistant Staphylococcus aureus (4% vs. 2%; P = .04), said Dr. Murphy of the department of surgery at the Ohio State University, Columbus.
Respiratory infections were the most common source of Acinetobacter for all patients. Survivors were more likely to have respiratory sources of infection (82.5% vs. 67%; P = .02), whereas nonsurvivors had a higher incidence of Acinetobacter bacteremia, including both secondary and catheter-related bacteremias (43% vs. 8%; P less than .001).
Multidrug resistance rates were similar among survivors and nonsurvivors at 64% and 70.4%, respectively, although there was a slight trend toward increased resistance among nonsurvivors for cefepime (Maxipime), impinem (Primaxin IV/Primaxin IM), and tigecycline (Tygacil), she said.
Rates of appropriate empirical antibiotic coverage were not significantly different, at 18.5% among nonsurvivors and 28.4% among survivors, although survivors were more likely to receive a broad-spectrum carbapenem as empirical therapy (33% vs. 17%; P = .02).
ICU stay, hospital length of stay, and duration of mechanical ventilation were also similar.
In a multivariate analysis that was adjusted for potential confounders, the independent predictors of mortality were bacteremia (odds ratio, 14.1; P less than .001), immunosuppression (OR, 2.76; P = .04), and higher severity of illness by APACHE II score (OR, 1.1; P = .002).
The use of the carbapenem antibiotic imipenem as directed therapy was protective (OR, 0.29; P = .012).
"A carbapenem should be considered for [empirical] therapy in ICU patients at risk for Acinetobacter infection," Dr. Murphy said.
Invited discussant Dr. Nicholas Namias, chief of trauma and professor of surgery at the University of Miami Health System, observed that the 35% mortality rate was disturbingly high, but not unexpected. He asked whether the use of carbapenems was forced, in a sense, by the susceptibility pattern of the isolate, and whether patients might have done better if they had been given an antibiotic like colistin.
Dr. Murphy agreed that the choice of carbapenem was directed by susceptibility patterns, and remarked that clinicians tend to lean toward a carbapenem because they’re more comfortable administering and dosing a carbapenem (particularly in complex cases, such as obese patients or those on renal replacement therapy) than colistin.
Dr. Namias also asked how empirical therapy is selected, and how the results might look if only carbapenem-resistant patients were included in the analysis. Dr. Murphy replied that the hospital does not have a fixed rotation, but reviews its ICU-specific antibiograms on an annual basis to determine its standard empirical therapy.
The investigators plan to study outcomes in carbapenem-resistant patients, said Dr. Murphy, but she pointed out that more than half of the patients in the current study were carbapenem resistant. She suggested that a carbapenem may still be beneficial in this setting because there are in vitro data showing synergy between carbapenems and other antibiotics, including colistin, tigecycline, and amikacin. Extended infusions of impinem were not used during the study period, although the hospital recently began using 4-hour infusions of doripenem (Doribax).
The authors reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY
Active Surveillance in ICU Cut Acinetobacter Contamination
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY
Chest X-Rays Incongruous With Lavage Results in VAP
DALLAS – Clinicians frequently perform bronchoalveolar lavage in ventilated trauma patients without radiologic evidence of pneumonia, according to a retrospective analysis.
Among 1,343 chest x-ray reports from 344 patients who all underwent bronchoalveolar lavage (BAL), there was no mention of infiltrates in 11% and no suspicion of pneumonia in 64%, according to a review that used natural language processing to sift through the reports.
"Our indication for BAL includes chest x-ray infiltrates or a change in chest x-rays, so I was very surprised to see that there were so many BALs done without an infiltrate mentioned in the chest x-ray report," said lead author Dr. Heather L. Evans, a trauma and acute care surgeon and surgical intensivist at the University of Washington in Seattle. "I think that this may be something of a soft call when providers are concerned that the patient has increasing secretions, increasing oxygenation, and worsening sepsis of unknown etiology. Perhaps the chest x-ray is not as firm and fast a rule as we are led to believe."
Indeed, the Centers for Disease Control and Prevention removed the chest x-ray from its new surveillance definition for what is now termed adult ventilator-associated events. The new definition, expected to be implemented in 2013, is not intended for clinical management, leaving physicians in a quandary when making a clinical diagnosis of VAP. Enter natural language processing, a tool that is increasingly being applied in radiology as part of machine learning to aid in-text analysis of radiology reports (Med. Image Anal. 2012 [doi:10.1016/j.media.2012.02.005]).
The investigators used natural language processing coding methods to code 1,343 chest x-ray reports from the day prior, day of, and day after BAL among 344 trauma patients ventilated for more than 48 hours at a level 1 trauma center. Two specially trained reviewers coded the reports using the chest x-ray element from the Clinical Pulmonary Infection Score (CPIS) as "no infiltrate," "diffuse infiltrate or atelectasis," or "focal infiltrate" and scored the reports on a three-point scale for suspicion of pneumonia as "no suspicion," "suspicion," or "probable pneumonia."
The CPIS classifier had a 90% overall accuracy, 93% specificity, 86% sensitivity, and 85% positive predictive value. The suspicion classifier achieved comparable results of 85%, 89%, 78%, and 78%, respectively.
As expected, localized infiltrate was significantly more common in reports from BAL-positive than BAL-negative patients (13% vs. 9%), while no infiltrate was significantly more common in those from BAL-negative patients (15.3% vs. 11.5%). However, 1,013 chest x-ray reports, or 75.4% of the data, fell in-between with diffuse infiltrate or atelectasis and had a 50-50 chance of being diagnosed as VAP, Dr. Evans said at the annual meeting of the Surgical Infection Society.
"Failure to discriminate diffuse infiltrate defines the group where culture data is most useful," she observed.
Radiology reports noting any suspicion of pneumonia were significantly more common in positive-BAL than in negative-BAL patients (45.6% vs. 28%), while reports with no suspicion of pneumonia were significantly more common in BAL-negative patients (68% vs. 60%).
Still, 430 (50%) of the 856 chest x-ray reports with no suspicion of VAP were in patients with BAL-positive results, Dr. Evans pointed out.
To sort out the implications of this finding, the investigators stratified the CPIS data by time and discovered that differences between the BAL-positive and -negative groups regarding the presence or absence of infiltrates were statistically significant only on chest x-ray reports from the day after BAL (P = .004).
"Considering the timing of this chest x-ray report information is absolutely crucial and something we will definitely incorporate in the future," she said, adding that future work will involve evaluation of coded chest x-ray report content in VAP risk assessment.
Invited discussant Dr. Addison K. May, chief of trauma and surgical critical care at Vanderbilt University in Nashville, Tenn., questioned whether the authors were surprised by the findings given that chest x-ray readings and BAL results correlate only about 40% of the time, and asked why the authors chose to include the radiology report from the day after BAL. Dr. Evans said the lack of correlation wasn’t surprising and that chest x-ray report language will be incorporated, along with other available clinical values, into their VAP risk assessment model.
"To exclude the chest x-ray information is to ignore a fundamental piece of diagnostic data that clinicians use all the time," she added. "As much as we don’t like to rely on the chest x-ray, I’m currently doing a qualitative study of the diagnosis of ventilator-associated pneumonia at my institution, and I can tell you in the 15 interviews I’ve done, every single person says the chest x-ray is a fundamental piece that they rely on to make the diagnosis.
"So I think if we’re going to remove the chest x-ray from our definition, whether it’s from surveillance or from the definition that we use clinically, we have to have data to support that it shouldn’t be there."
Dr. Evans said the chest x-ray report from the day after BAL was included to help train the classifier to be accurate, and that the finding of statistical significance only for that day’s chest x-ray report data was unexpected and provocative.
Dr. Pamela Lipsett, immediate past president of the Surgical Infection Society, was involved in the CDC’s redefinition of what is now termed ventilator-associated events. She argued against the use of chest x-rays for VAP diagnosis and said they were removed from the CDC definition because they are unreliable.
Some attendees questioned why the authors didn’t just use a structured method for reading the radiographs. Dr. E. Patchen Dellinger, also a past president of the Society, simply asked, "Haven’t you just proved that we don’t know how to diagnosis VAP and that we should stop taking chest x-rays unless we’re worried about a pneumothorax?"
Dr. Evans replied that there are many other indications for chest x-ray in the ICU, but added that "the days of getting a chest x-ray every morning just because the patient is ventilated are a gross overuse of that imaging modality."
The authors reported no relevant conflicts of interest.
DALLAS – Clinicians frequently perform bronchoalveolar lavage in ventilated trauma patients without radiologic evidence of pneumonia, according to a retrospective analysis.
Among 1,343 chest x-ray reports from 344 patients who all underwent bronchoalveolar lavage (BAL), there was no mention of infiltrates in 11% and no suspicion of pneumonia in 64%, according to a review that used natural language processing to sift through the reports.
"Our indication for BAL includes chest x-ray infiltrates or a change in chest x-rays, so I was very surprised to see that there were so many BALs done without an infiltrate mentioned in the chest x-ray report," said lead author Dr. Heather L. Evans, a trauma and acute care surgeon and surgical intensivist at the University of Washington in Seattle. "I think that this may be something of a soft call when providers are concerned that the patient has increasing secretions, increasing oxygenation, and worsening sepsis of unknown etiology. Perhaps the chest x-ray is not as firm and fast a rule as we are led to believe."
Indeed, the Centers for Disease Control and Prevention removed the chest x-ray from its new surveillance definition for what is now termed adult ventilator-associated events. The new definition, expected to be implemented in 2013, is not intended for clinical management, leaving physicians in a quandary when making a clinical diagnosis of VAP. Enter natural language processing, a tool that is increasingly being applied in radiology as part of machine learning to aid in-text analysis of radiology reports (Med. Image Anal. 2012 [doi:10.1016/j.media.2012.02.005]).
The investigators used natural language processing coding methods to code 1,343 chest x-ray reports from the day prior, day of, and day after BAL among 344 trauma patients ventilated for more than 48 hours at a level 1 trauma center. Two specially trained reviewers coded the reports using the chest x-ray element from the Clinical Pulmonary Infection Score (CPIS) as "no infiltrate," "diffuse infiltrate or atelectasis," or "focal infiltrate" and scored the reports on a three-point scale for suspicion of pneumonia as "no suspicion," "suspicion," or "probable pneumonia."
The CPIS classifier had a 90% overall accuracy, 93% specificity, 86% sensitivity, and 85% positive predictive value. The suspicion classifier achieved comparable results of 85%, 89%, 78%, and 78%, respectively.
As expected, localized infiltrate was significantly more common in reports from BAL-positive than BAL-negative patients (13% vs. 9%), while no infiltrate was significantly more common in those from BAL-negative patients (15.3% vs. 11.5%). However, 1,013 chest x-ray reports, or 75.4% of the data, fell in-between with diffuse infiltrate or atelectasis and had a 50-50 chance of being diagnosed as VAP, Dr. Evans said at the annual meeting of the Surgical Infection Society.
"Failure to discriminate diffuse infiltrate defines the group where culture data is most useful," she observed.
Radiology reports noting any suspicion of pneumonia were significantly more common in positive-BAL than in negative-BAL patients (45.6% vs. 28%), while reports with no suspicion of pneumonia were significantly more common in BAL-negative patients (68% vs. 60%).
Still, 430 (50%) of the 856 chest x-ray reports with no suspicion of VAP were in patients with BAL-positive results, Dr. Evans pointed out.
To sort out the implications of this finding, the investigators stratified the CPIS data by time and discovered that differences between the BAL-positive and -negative groups regarding the presence or absence of infiltrates were statistically significant only on chest x-ray reports from the day after BAL (P = .004).
"Considering the timing of this chest x-ray report information is absolutely crucial and something we will definitely incorporate in the future," she said, adding that future work will involve evaluation of coded chest x-ray report content in VAP risk assessment.
Invited discussant Dr. Addison K. May, chief of trauma and surgical critical care at Vanderbilt University in Nashville, Tenn., questioned whether the authors were surprised by the findings given that chest x-ray readings and BAL results correlate only about 40% of the time, and asked why the authors chose to include the radiology report from the day after BAL. Dr. Evans said the lack of correlation wasn’t surprising and that chest x-ray report language will be incorporated, along with other available clinical values, into their VAP risk assessment model.
"To exclude the chest x-ray information is to ignore a fundamental piece of diagnostic data that clinicians use all the time," she added. "As much as we don’t like to rely on the chest x-ray, I’m currently doing a qualitative study of the diagnosis of ventilator-associated pneumonia at my institution, and I can tell you in the 15 interviews I’ve done, every single person says the chest x-ray is a fundamental piece that they rely on to make the diagnosis.
"So I think if we’re going to remove the chest x-ray from our definition, whether it’s from surveillance or from the definition that we use clinically, we have to have data to support that it shouldn’t be there."
Dr. Evans said the chest x-ray report from the day after BAL was included to help train the classifier to be accurate, and that the finding of statistical significance only for that day’s chest x-ray report data was unexpected and provocative.
Dr. Pamela Lipsett, immediate past president of the Surgical Infection Society, was involved in the CDC’s redefinition of what is now termed ventilator-associated events. She argued against the use of chest x-rays for VAP diagnosis and said they were removed from the CDC definition because they are unreliable.
Some attendees questioned why the authors didn’t just use a structured method for reading the radiographs. Dr. E. Patchen Dellinger, also a past president of the Society, simply asked, "Haven’t you just proved that we don’t know how to diagnosis VAP and that we should stop taking chest x-rays unless we’re worried about a pneumothorax?"
Dr. Evans replied that there are many other indications for chest x-ray in the ICU, but added that "the days of getting a chest x-ray every morning just because the patient is ventilated are a gross overuse of that imaging modality."
The authors reported no relevant conflicts of interest.
DALLAS – Clinicians frequently perform bronchoalveolar lavage in ventilated trauma patients without radiologic evidence of pneumonia, according to a retrospective analysis.
Among 1,343 chest x-ray reports from 344 patients who all underwent bronchoalveolar lavage (BAL), there was no mention of infiltrates in 11% and no suspicion of pneumonia in 64%, according to a review that used natural language processing to sift through the reports.
"Our indication for BAL includes chest x-ray infiltrates or a change in chest x-rays, so I was very surprised to see that there were so many BALs done without an infiltrate mentioned in the chest x-ray report," said lead author Dr. Heather L. Evans, a trauma and acute care surgeon and surgical intensivist at the University of Washington in Seattle. "I think that this may be something of a soft call when providers are concerned that the patient has increasing secretions, increasing oxygenation, and worsening sepsis of unknown etiology. Perhaps the chest x-ray is not as firm and fast a rule as we are led to believe."
Indeed, the Centers for Disease Control and Prevention removed the chest x-ray from its new surveillance definition for what is now termed adult ventilator-associated events. The new definition, expected to be implemented in 2013, is not intended for clinical management, leaving physicians in a quandary when making a clinical diagnosis of VAP. Enter natural language processing, a tool that is increasingly being applied in radiology as part of machine learning to aid in-text analysis of radiology reports (Med. Image Anal. 2012 [doi:10.1016/j.media.2012.02.005]).
The investigators used natural language processing coding methods to code 1,343 chest x-ray reports from the day prior, day of, and day after BAL among 344 trauma patients ventilated for more than 48 hours at a level 1 trauma center. Two specially trained reviewers coded the reports using the chest x-ray element from the Clinical Pulmonary Infection Score (CPIS) as "no infiltrate," "diffuse infiltrate or atelectasis," or "focal infiltrate" and scored the reports on a three-point scale for suspicion of pneumonia as "no suspicion," "suspicion," or "probable pneumonia."
The CPIS classifier had a 90% overall accuracy, 93% specificity, 86% sensitivity, and 85% positive predictive value. The suspicion classifier achieved comparable results of 85%, 89%, 78%, and 78%, respectively.
As expected, localized infiltrate was significantly more common in reports from BAL-positive than BAL-negative patients (13% vs. 9%), while no infiltrate was significantly more common in those from BAL-negative patients (15.3% vs. 11.5%). However, 1,013 chest x-ray reports, or 75.4% of the data, fell in-between with diffuse infiltrate or atelectasis and had a 50-50 chance of being diagnosed as VAP, Dr. Evans said at the annual meeting of the Surgical Infection Society.
"Failure to discriminate diffuse infiltrate defines the group where culture data is most useful," she observed.
Radiology reports noting any suspicion of pneumonia were significantly more common in positive-BAL than in negative-BAL patients (45.6% vs. 28%), while reports with no suspicion of pneumonia were significantly more common in BAL-negative patients (68% vs. 60%).
Still, 430 (50%) of the 856 chest x-ray reports with no suspicion of VAP were in patients with BAL-positive results, Dr. Evans pointed out.
To sort out the implications of this finding, the investigators stratified the CPIS data by time and discovered that differences between the BAL-positive and -negative groups regarding the presence or absence of infiltrates were statistically significant only on chest x-ray reports from the day after BAL (P = .004).
"Considering the timing of this chest x-ray report information is absolutely crucial and something we will definitely incorporate in the future," she said, adding that future work will involve evaluation of coded chest x-ray report content in VAP risk assessment.
Invited discussant Dr. Addison K. May, chief of trauma and surgical critical care at Vanderbilt University in Nashville, Tenn., questioned whether the authors were surprised by the findings given that chest x-ray readings and BAL results correlate only about 40% of the time, and asked why the authors chose to include the radiology report from the day after BAL. Dr. Evans said the lack of correlation wasn’t surprising and that chest x-ray report language will be incorporated, along with other available clinical values, into their VAP risk assessment model.
"To exclude the chest x-ray information is to ignore a fundamental piece of diagnostic data that clinicians use all the time," she added. "As much as we don’t like to rely on the chest x-ray, I’m currently doing a qualitative study of the diagnosis of ventilator-associated pneumonia at my institution, and I can tell you in the 15 interviews I’ve done, every single person says the chest x-ray is a fundamental piece that they rely on to make the diagnosis.
"So I think if we’re going to remove the chest x-ray from our definition, whether it’s from surveillance or from the definition that we use clinically, we have to have data to support that it shouldn’t be there."
Dr. Evans said the chest x-ray report from the day after BAL was included to help train the classifier to be accurate, and that the finding of statistical significance only for that day’s chest x-ray report data was unexpected and provocative.
Dr. Pamela Lipsett, immediate past president of the Surgical Infection Society, was involved in the CDC’s redefinition of what is now termed ventilator-associated events. She argued against the use of chest x-rays for VAP diagnosis and said they were removed from the CDC definition because they are unreliable.
Some attendees questioned why the authors didn’t just use a structured method for reading the radiographs. Dr. E. Patchen Dellinger, also a past president of the Society, simply asked, "Haven’t you just proved that we don’t know how to diagnosis VAP and that we should stop taking chest x-rays unless we’re worried about a pneumothorax?"
Dr. Evans replied that there are many other indications for chest x-ray in the ICU, but added that "the days of getting a chest x-ray every morning just because the patient is ventilated are a gross overuse of that imaging modality."
The authors reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY
Major Finding: Differences between the BAL-positive and -negative groups regarding the presence or absence of infiltrates were significant only on chest x-ray reports from the day after BAL (P = .004).
Data Source: This study was a retrospective analysis of 1,343 chest x-ray reports and bronchoalveolar lavage results from 344 ventilated trauma patients.
Disclosures: The authors reported no relevant conflicts of interest.