User login
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
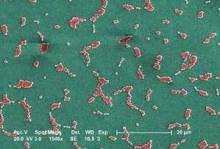
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
DALLAS – Unannounced surveillance detected Acinetobacter contamination in more than one-fourth of burn/trauma intensive care unit rooms tested at a Miami hospital.
Although 58% of rooms housed an Acinetobacter-positive patient, 42% had patients who were negative for the aerobic gram-negative bacillus.
"That’s a worrisome number because those patients are now at risk of picking up Acinetobacter from their environment," senior author Dr. Nicholas Namias said at the annual meeting of the Surgical Infection Society.
Acinetobacter has become one of the preeminent ICU pathogens and is resistant to simple cleaning and many commonly prescribed antibiotics.
New acquisitions of carbapenem-resistant Acinetobacter at the University of Miami’s Jackson Memorial Hospital, where the study was conducted, were high in early 2011 at up to 13/week, but leveled off to zero in some weeks after a bundle intervention was put in place. The bundle included grouping a positive patient cohort, active surveillance of patients using rectal swab cultures, hand hygiene education, operating room interventions, and weekly environmental cleaning feedback.
The 25-bed ICU was cultured weekly and the cultures subjected to pulsed field gel electrophoresis. Ultraviolet powder, invisible to the naked eye, was also placed on surfaces throughout the ICU and checked 48 hours later with ultraviolet light to see if they were cleaned.
"We even went so far as to place plates on high surfaces where nobody reaches to see if Acinetobacter could grow out of thin air," said Dr. Namias, chief of trauma and professor of surgery at the University of Miami Health System.
Of the 213 rooms cultured over 15 weeks, 57 (27%) were positive for Acinetobacter. More than 90% of samples were identified as Acinetobacter baumannii. Contaminated sites included 38 bed rails (67%), 21 intravenous pumps (37%), 6 bedside tables (11%), and 3 ventilator control panels (5%).
"This actually turned out to be a major issue, because once you discover they’re dirty, it becomes a big question of who’s supposed to clean them," he said. "Understandably, environmental staff was kind of hesitant to touch IV pumps and ventilator control panels, and the nurses are probably overtrained to be cleaning bed rails and bedside tables. So you end up having to use techs, the people who go around doing urimeters and finger-prick glucose, but you have to make sure they’re trained in proper hand hygiene."
At baseline, only slightly more than 40% of surfaces had been cleaned at 48 hours – a percentage that Dr. Namias described as alarming, but typical in surveillance studies. Once the ultraviolet "spying" began, and environmental services was told that surfaces were unclean, there was a very quick response. Within 1 week, the percentage of surfaces cleaned at 48 hours rose to nearly 100%, where it has remained.
"Once they know they are being watched, you can have them do the right thing," he said.
In a separate analysis, similar results were achieved in the operating room, where the percentage of surfaces cleaned at 48 hours increased from 47% to 82% after the educational and cleaning intervention.
Importantly, the number of new acquisitions of Acinetobacter decreased concomitantly from 1.40 patients/week to 0.37; and from 9.2/month during the first 6 months of 2011 to 3.3/month during the last 6 months (P = .003).
Invited discussant Dr. Heather Evans, a trauma and acute care surgeon and surgical intensivist with the University of Washington in Seattle, thanked the program committee for selecting the abstract for oral discussion, citing the relevance of infection-control data to the practicing clinician and to prevention efforts. She went on to ask whether the hospital regularly uses active surveillance for Acinetobacter and contact precautions when a patient is colonized and whether the hospital would presumptively put a patient on contact precautions if they reach a certain level.
Dr. Evans also asked whether cleaning personnel can game the system, citing a recent paper by lead study author Dr. L. Silvia Munoz-Price that identified preferential cleaning of white UV powder targets among units with high levels of experience with UV powder (Infect. Control Hosp. Epidemiol. 2012;33:92-5). Dr. Namias said it’s entirely possible that personnel are gaming the system, but noted that Acinetobacter is also airborne.
Finally, an audience member remarked that the open-air design of the trauma ICU, as shown in an illustration, may be contributing to the unusually high rates of contamination. Dr. Namias agreed that the unit is due for an update and said it was designed before it was known that closed units are best.
Dr. Munoz-Price, medical director of infection control at Jackson Memorial, said they are currently performing multivariable analyses to better understand the factors associated with higher environmental contamination.
"The control of Acinetobacter within a hospital setting deals with the interaction of patient’s bioburden, health care worker hands/uniforms, and contaminated objects in the environment," she said in an interview. "This cycle of contamination needs to be tackled at different levels in order to sustain good outcomes."
The authors reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SURGICAL INFECTION SOCIETY