User login
Endocrine Society: Annual Meeting (ENDO 2015)
High testosterone, no growth benefit for boys treated with letrozole
SAN DIEGO – The aromatase inhibitor letrozole didn’t help boys with short stature grow taller, but it did boost their testosterone to concerning levels in a small study at Children’s Hospital Los Angeles.
Estrogens are thought to help close epiphyseal growth plates; the idea of giving aromatase inhibitors (AIs) is to block aromatase from converting androgens to estrogens in boys so that their growth plates stay open a bit longer and they grow taller. In the United States, the drugs are frequently prescribed off label for that purpose in boys with short-stature or rapid-tempo puberty.
It didn’t seem to work, however, in the 16 boys in the study, who were an average of about 12.5 years old when they were started on letrozole.
The seven boys who started out at Tanner stages 1-3 were on the drug for an average of 2.7 years; their Bayley-Pinneau predicted adult height (PAH) fell from 66.9 inches to 66.5 inches. The nine boys who started out at Tanner stages 4-5 went from a PAH of 65.3 inches to 65.4 inches. The changes were not statistically significant.
Meanwhile, testosterone increased from 155 ng/dL to 728 ng/dL in stage 1-3 boys and from 417 ng/dL to 1,192 ng/dL in stage 4-5 boys. Those changes were statistically significant, and testosterone levels were significantly above the upper limit of normal in six (67%) of the later Tanner stage boys. There was a corresponding increase from no or mild acne to moderate acne in later stage boys, and a significant increase in hematocrit, from 43% to 47.5%. Seven (78%) of the later Tanner stage boys had hematocrit levels above the upper limit of normal.
“Short-term AIs were not effective in increasing PAH, regardless of pubertal age. [The] potential consequences of these findings are of concern and require careful long-term study, especially when AIs are started in late puberty,” the team concluded.
The findings “will change my practice with regard to” letrozole, said senior author Dr. Mitchell Geffner, professor of pediatrics at the hospital and president of the Pediatric Endocrine Society. Dr. Geffner treated all but one of the children in the study.
“I might still use” anastrozole, a less-potent AI, “but I have to get a better sense of all the parameters we measured here, a number of which are potentially unhealthy. These drugs are used to treat” boys with short stature and rapid-tempo puberty “very frequently in the United States,” but “I think we’re entering uncharted territory” with them. “We don’t really have a lot of data with use as single agents. We have to be very careful because we are giving a drug that alters, at least in the short term, reproductive hormones. Reproductive health in the future is completely unknown,” he said.
Despite having elevated testosterone levels, all the children had significant change in estradiol levels; in fact, there was a trend toward higher levels in the Tanner stage 4-5 boys, who also had significant increases in follicle-stimulating hormone and luteinizing-hormone levels that were often above the upper limit of normal.
“I was surprised by the results, and how high testosterone went in some of these boys. There’s conflicting data on whether these drugs help gain extra height, but we have to be very careful because we are causing very high testosterone levels,” which – although not seen in the study – could affect bone health and even cause stroke if hematocrit is pushed high enough, said lead investigator Dr. Jessica Ferris of Children’s Hospital Los Angeles.
There was no outside funding for the work. Dr. Ferris had no disclosures. Dr. Geffner is an investigator, consultant, or adviser for several companies, including Eli Lilly, Endo Pharmaceuticals, Genentech, Ipsen, Novo Nordisk, and Pfizer.
SAN DIEGO – The aromatase inhibitor letrozole didn’t help boys with short stature grow taller, but it did boost their testosterone to concerning levels in a small study at Children’s Hospital Los Angeles.
Estrogens are thought to help close epiphyseal growth plates; the idea of giving aromatase inhibitors (AIs) is to block aromatase from converting androgens to estrogens in boys so that their growth plates stay open a bit longer and they grow taller. In the United States, the drugs are frequently prescribed off label for that purpose in boys with short-stature or rapid-tempo puberty.
It didn’t seem to work, however, in the 16 boys in the study, who were an average of about 12.5 years old when they were started on letrozole.
The seven boys who started out at Tanner stages 1-3 were on the drug for an average of 2.7 years; their Bayley-Pinneau predicted adult height (PAH) fell from 66.9 inches to 66.5 inches. The nine boys who started out at Tanner stages 4-5 went from a PAH of 65.3 inches to 65.4 inches. The changes were not statistically significant.
Meanwhile, testosterone increased from 155 ng/dL to 728 ng/dL in stage 1-3 boys and from 417 ng/dL to 1,192 ng/dL in stage 4-5 boys. Those changes were statistically significant, and testosterone levels were significantly above the upper limit of normal in six (67%) of the later Tanner stage boys. There was a corresponding increase from no or mild acne to moderate acne in later stage boys, and a significant increase in hematocrit, from 43% to 47.5%. Seven (78%) of the later Tanner stage boys had hematocrit levels above the upper limit of normal.
“Short-term AIs were not effective in increasing PAH, regardless of pubertal age. [The] potential consequences of these findings are of concern and require careful long-term study, especially when AIs are started in late puberty,” the team concluded.
The findings “will change my practice with regard to” letrozole, said senior author Dr. Mitchell Geffner, professor of pediatrics at the hospital and president of the Pediatric Endocrine Society. Dr. Geffner treated all but one of the children in the study.
“I might still use” anastrozole, a less-potent AI, “but I have to get a better sense of all the parameters we measured here, a number of which are potentially unhealthy. These drugs are used to treat” boys with short stature and rapid-tempo puberty “very frequently in the United States,” but “I think we’re entering uncharted territory” with them. “We don’t really have a lot of data with use as single agents. We have to be very careful because we are giving a drug that alters, at least in the short term, reproductive hormones. Reproductive health in the future is completely unknown,” he said.
Despite having elevated testosterone levels, all the children had significant change in estradiol levels; in fact, there was a trend toward higher levels in the Tanner stage 4-5 boys, who also had significant increases in follicle-stimulating hormone and luteinizing-hormone levels that were often above the upper limit of normal.
“I was surprised by the results, and how high testosterone went in some of these boys. There’s conflicting data on whether these drugs help gain extra height, but we have to be very careful because we are causing very high testosterone levels,” which – although not seen in the study – could affect bone health and even cause stroke if hematocrit is pushed high enough, said lead investigator Dr. Jessica Ferris of Children’s Hospital Los Angeles.
There was no outside funding for the work. Dr. Ferris had no disclosures. Dr. Geffner is an investigator, consultant, or adviser for several companies, including Eli Lilly, Endo Pharmaceuticals, Genentech, Ipsen, Novo Nordisk, and Pfizer.
SAN DIEGO – The aromatase inhibitor letrozole didn’t help boys with short stature grow taller, but it did boost their testosterone to concerning levels in a small study at Children’s Hospital Los Angeles.
Estrogens are thought to help close epiphyseal growth plates; the idea of giving aromatase inhibitors (AIs) is to block aromatase from converting androgens to estrogens in boys so that their growth plates stay open a bit longer and they grow taller. In the United States, the drugs are frequently prescribed off label for that purpose in boys with short-stature or rapid-tempo puberty.
It didn’t seem to work, however, in the 16 boys in the study, who were an average of about 12.5 years old when they were started on letrozole.
The seven boys who started out at Tanner stages 1-3 were on the drug for an average of 2.7 years; their Bayley-Pinneau predicted adult height (PAH) fell from 66.9 inches to 66.5 inches. The nine boys who started out at Tanner stages 4-5 went from a PAH of 65.3 inches to 65.4 inches. The changes were not statistically significant.
Meanwhile, testosterone increased from 155 ng/dL to 728 ng/dL in stage 1-3 boys and from 417 ng/dL to 1,192 ng/dL in stage 4-5 boys. Those changes were statistically significant, and testosterone levels were significantly above the upper limit of normal in six (67%) of the later Tanner stage boys. There was a corresponding increase from no or mild acne to moderate acne in later stage boys, and a significant increase in hematocrit, from 43% to 47.5%. Seven (78%) of the later Tanner stage boys had hematocrit levels above the upper limit of normal.
“Short-term AIs were not effective in increasing PAH, regardless of pubertal age. [The] potential consequences of these findings are of concern and require careful long-term study, especially when AIs are started in late puberty,” the team concluded.
The findings “will change my practice with regard to” letrozole, said senior author Dr. Mitchell Geffner, professor of pediatrics at the hospital and president of the Pediatric Endocrine Society. Dr. Geffner treated all but one of the children in the study.
“I might still use” anastrozole, a less-potent AI, “but I have to get a better sense of all the parameters we measured here, a number of which are potentially unhealthy. These drugs are used to treat” boys with short stature and rapid-tempo puberty “very frequently in the United States,” but “I think we’re entering uncharted territory” with them. “We don’t really have a lot of data with use as single agents. We have to be very careful because we are giving a drug that alters, at least in the short term, reproductive hormones. Reproductive health in the future is completely unknown,” he said.
Despite having elevated testosterone levels, all the children had significant change in estradiol levels; in fact, there was a trend toward higher levels in the Tanner stage 4-5 boys, who also had significant increases in follicle-stimulating hormone and luteinizing-hormone levels that were often above the upper limit of normal.
“I was surprised by the results, and how high testosterone went in some of these boys. There’s conflicting data on whether these drugs help gain extra height, but we have to be very careful because we are causing very high testosterone levels,” which – although not seen in the study – could affect bone health and even cause stroke if hematocrit is pushed high enough, said lead investigator Dr. Jessica Ferris of Children’s Hospital Los Angeles.
There was no outside funding for the work. Dr. Ferris had no disclosures. Dr. Geffner is an investigator, consultant, or adviser for several companies, including Eli Lilly, Endo Pharmaceuticals, Genentech, Ipsen, Novo Nordisk, and Pfizer.
AT ENDO 2015
Key clinical point: Aromatase inhibitors don’t help shorter boys grow taller.
Major finding: The seven boys who started out at Tanner stages 1-3 were on letrozole for an average of 2.7 years; their Bayley-Pinneau predicted adult height fell from 66.9 inches to 66.5 inches. The nine boys who started out at Tanner stages 4-5 went from a PAH of 65.3 inches to 65.4 inches.
Data source: A review of outcomes for 16 boys treated at Children’s Hospital Los Angeles.
Disclosures: There was no outside funding for the work. The senior investigator is a consultant, adviser, or researcher for several companies, including Eli Lilly, Endo Pharmaceuticals, Genentech, Ipsen, Novo Nordisk, and Pfizer.
HT not linked with increased mortality
AT ENDO 2015
SAN DIEGO – Hormone therapy in postmenopausal women does not seem to affect risk of mortality, results from a meta-analysis demonstrated.
“Most menopausal women suffer from a lot of bothersome symptoms, like hot flashes, sleep problems, and night sweats,” Dr. Khalid Benkhadra said during a press briefing at the meeting of the Endocrine Society. “Hormone therapy is usually very effective in alleviating these symptoms. However, women are usually concerned about the long-term safety [of HT].”
To assess all-cause and specific mortality associated with hormone therapy in postmenopausal women, Dr. Benkhadra and his associates searched databases for randomized trials published before August 2013 that compared hormone therapy with placebo or no treatment, with a follow-up of at least 6 months. The databases included MEDLINE and the Cochrane Central Register of Controlled Trials.
The outcome of interest was death from any cause, death from cardiac events, and death from breast cancer, lung cancer, ovarian cancer, colorectal cancer, and stroke.
The final meta-analysis included 43 clinical trials involving more than 52,000 women, mean age 62 years. Dr. Benkhadra, a research fellow at Mayo Clinic, Rochester, Minn., reported that no statistically significant association was observed between the use of hormone therapy and all-cause mortality (risk ratio, 0.99), with no significant interaction based on hormone type or preexisting heart disease. In addition, no association was observed between use of hormone therapy and death from myocardial infarction (RR, 1.04), stroke (RR, 1.49), and breast cancer (RR, 0.93), nor lung cancer, ovarian cancer, and colorectal cancer. “In each of these categories, there was no significant effect of HR on the risk of dying,” Dr. Benkhadra said. “Results were similar for estrogen only versus combined estrogen and progesterone therapy.”
He acknowledged certain limitations of the study, including the fact that the evidence in the 43 trials was rated as “low to moderate” and the length of follow-up was limited to 5 years.
Based on the findings, he concluded that postmenopausal women with bothersome symptoms “can engage with their physician in shared decision making to discuss treatment [with HT].”
Dr. Benkhadra reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Hormone therapy in postmenopausal women does not seem to affect risk of mortality, results from a meta-analysis demonstrated.
“Most menopausal women suffer from a lot of bothersome symptoms, like hot flashes, sleep problems, and night sweats,” Dr. Khalid Benkhadra said during a press briefing at the meeting of the Endocrine Society. “Hormone therapy is usually very effective in alleviating these symptoms. However, women are usually concerned about the long-term safety [of HT].”
To assess all-cause and specific mortality associated with hormone therapy in postmenopausal women, Dr. Benkhadra and his associates searched databases for randomized trials published before August 2013 that compared hormone therapy with placebo or no treatment, with a follow-up of at least 6 months. The databases included MEDLINE and the Cochrane Central Register of Controlled Trials.
The outcome of interest was death from any cause, death from cardiac events, and death from breast cancer, lung cancer, ovarian cancer, colorectal cancer, and stroke.
The final meta-analysis included 43 clinical trials involving more than 52,000 women, mean age 62 years. Dr. Benkhadra, a research fellow at Mayo Clinic, Rochester, Minn., reported that no statistically significant association was observed between the use of hormone therapy and all-cause mortality (risk ratio, 0.99), with no significant interaction based on hormone type or preexisting heart disease. In addition, no association was observed between use of hormone therapy and death from myocardial infarction (RR, 1.04), stroke (RR, 1.49), and breast cancer (RR, 0.93), nor lung cancer, ovarian cancer, and colorectal cancer. “In each of these categories, there was no significant effect of HR on the risk of dying,” Dr. Benkhadra said. “Results were similar for estrogen only versus combined estrogen and progesterone therapy.”
He acknowledged certain limitations of the study, including the fact that the evidence in the 43 trials was rated as “low to moderate” and the length of follow-up was limited to 5 years.
Based on the findings, he concluded that postmenopausal women with bothersome symptoms “can engage with their physician in shared decision making to discuss treatment [with HT].”
Dr. Benkhadra reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Hormone therapy in postmenopausal women does not seem to affect risk of mortality, results from a meta-analysis demonstrated.
“Most menopausal women suffer from a lot of bothersome symptoms, like hot flashes, sleep problems, and night sweats,” Dr. Khalid Benkhadra said during a press briefing at the meeting of the Endocrine Society. “Hormone therapy is usually very effective in alleviating these symptoms. However, women are usually concerned about the long-term safety [of HT].”
To assess all-cause and specific mortality associated with hormone therapy in postmenopausal women, Dr. Benkhadra and his associates searched databases for randomized trials published before August 2013 that compared hormone therapy with placebo or no treatment, with a follow-up of at least 6 months. The databases included MEDLINE and the Cochrane Central Register of Controlled Trials.
The outcome of interest was death from any cause, death from cardiac events, and death from breast cancer, lung cancer, ovarian cancer, colorectal cancer, and stroke.
The final meta-analysis included 43 clinical trials involving more than 52,000 women, mean age 62 years. Dr. Benkhadra, a research fellow at Mayo Clinic, Rochester, Minn., reported that no statistically significant association was observed between the use of hormone therapy and all-cause mortality (risk ratio, 0.99), with no significant interaction based on hormone type or preexisting heart disease. In addition, no association was observed between use of hormone therapy and death from myocardial infarction (RR, 1.04), stroke (RR, 1.49), and breast cancer (RR, 0.93), nor lung cancer, ovarian cancer, and colorectal cancer. “In each of these categories, there was no significant effect of HR on the risk of dying,” Dr. Benkhadra said. “Results were similar for estrogen only versus combined estrogen and progesterone therapy.”
He acknowledged certain limitations of the study, including the fact that the evidence in the 43 trials was rated as “low to moderate” and the length of follow-up was limited to 5 years.
Based on the findings, he concluded that postmenopausal women with bothersome symptoms “can engage with their physician in shared decision making to discuss treatment [with HT].”
Dr. Benkhadra reported having no relevant financial conflicts.
On Twitter @dougbrunk
Key clinical point: Use of hormone therapy by postmenopausal women was not associated with an increased risk of mortality.
Major finding: No statistically significant association was observed between the use of hormone therapy and all-cause mortality (risk ratio, 0.99).
Data source: A meta-analysis of 43 clinical trials involving more than 52,000 women, mean age 62 years.
Disclosures: Dr. Benkhadra reported having no relevant financial conflicts.
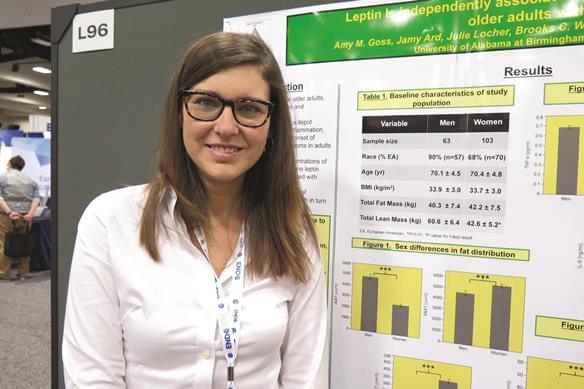
Elevated leptin linked to depression in obese older adults
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Elevated leptin may play a role in the relationship between excess adiposity and depressive symptoms in older adults, judging from the results of a cross-sectional survey.
While depression is common among older adults, particularly among those who are obese, “what’s not known is the underlying physiological mechanisms of what’s linking depression with excess fat mass,” Amy M. Goss, Ph.D., a postdoctoral research fellow in the department of nutrition sciences at the University of Alabama at Birmingham, said in an interview at the meeting of the Endocrine Society. “There’s a lot of work showing that visceral fat in particular is linked to depression. It’s thought that inflammation that emanates from visceral fat can lead to depressive symptoms. This is a particular problem in older adults, because they tend to have a lot of visceral adiposity.”
In an effort to investigate the independent relationships among depressive symptoms, total fat mass, intra-abdominal adipose tissue, markers of inflammation, and leptin in aging men and women, Dr. Goss and her associates evaluated 164 obese adults older than 65 years. The researchers used the Center for Epidemiologic Studies Depression (CES-D) 20-item scale to assess depressive symptoms, DXA to assess body composition, MRI to assess fat distribution, and a fasting blood sample to assess leptin, high-sensitivity C-reactive protein (hsCRP), interleukin-6, and tumor necrosis factor–alpha.
Compared with men, women had significantly greater levels of leptin (+100%; P less than .001), hsCRP (+63.9%; P less than .01), and CES-D scores (+52.7%; P less than .001). At the same time, men had significantly greater intra-abdominal adipose tissue (+82%; P less than .001) and lean mass (+42%; P less than .001), compared with women.
Multiple linear regression analysis revealed that only leptin was positively associated with CES-D scores, independent of gender and of all other markers studied (P less than .05).
In their abstract, the researchers concluded that elevated leptin “may, in part, mediate the observed relationship between excess adiposity and onset of depressive symptoms in aging, obese adults. Higher leptin and hsCRP concentration in women, compared to men may indicate greater proinflammatory state and explain sex differences in depressive symptoms in this population.”
Dr. Goss said that a key limitation of the study is its cross-sectional design. “We can’t determine the cause and effect based on this study, but it does lead the way to design randomized, clinical trials to test how we can improve depression in older adults with obesity,” she said.
She reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
Key clinical point: Leptin may play a role in the onset of depressive symptoms in aging, obese adults.
Major finding: Only leptin was positively associated with Center for Epidemiologic Studies Depression (CES-D) scores, independent of gender and of all other markers studied (P less than .05).
Data source: A cross-sectional study of 164 obese adults over the age of 65 years.
Disclosures: Dr. Goss reported having no relevant financial conflicts.
Add baseline DHEAS when screening adrenal incidentalomas for subclinical hypercortisolism
SAN DIEGO – A single baseline measurement of dehydroepiandrosterone sulfate (DHEAS) outperforms overnight dexamethasone suppression and other standard tests for the detection of subclinical hypercortisolism in patients with adrenal incidentalomas, according to a prospective, blinded study of 185 consecutive patients at Cambridge University in England.
It’s an important finding because 1-mg overnight dexamethasone suppression testing is the current screening standard for detection of the condition, said Dr. Michael Dennedy, a former endocrinology fellow at Cambridge and now a senior lecturer at the National University of Ireland (NUI), Galway.
“On the basis of these data, we advocate the use of a single measurement of DHEAS as a convenient, reliable, and robust test for screening of SH [subclinical hypercortisolism] in the context of adrenal incidentalomas,” Dr. Dennedy said at the meeting of the Endocrine Society.
DHEAS avoids the sampling problems and high false positives of older tests and “reliably differentiates between SH and non-SH etiologies of adrenal nodules. We use it now as a standard test for patients who have adrenal nodules” at Cambridge and NUI Galway, he said.
The theory for checking DHEAS is straightforward. Like DHEA, it’s regulated by pituitary ACTH; sustained suppression of central ACTH leads to reductions in both. However, DHEA does not work for screening because it has a short half-life – about 25 minutes – and has circadian secretion patterns similar to ACTH. The half-life of DHEAS, on the other hand, is 10-16 hours and levels stay relatively stable throughout the day, which makes it a more attractive marker for detecting chronically suppressed ACTH.
At baseline, the team measured DHEAS by immunoassay and then put their 185 subjects through standard workups for newly diagnosed adrenal incidentalomas, including plasma metanephrines, 1-mg overnight dexamethasone suppression, 24-hour urinary free cortisol, and paired renin and aldosterone measurements. They then unblinded their DHEAS measurements to see how they fared against the standard approaches.
Because DHEAS levels are determined by a person’s age and gender, the investigators used a ratio of the actual baseline measurement divided by the lower limit of the appropriate reference range; for instance, 1.2 mmol/L in younger patients and 0.4 mmol/L in older patients.
A baseline DHEAS ratio at or below 1.12 was 100% sensitive and 92% specific for the diagnosis of SH in patients with adrenal incidentalomas. In contrast, a cortisol cutoff of 1.9 mcg/dL following 1-mg dexamethasone suppression was 100% sensitive but 82.9% specific and 24-hour urinary free cortisol was 69% sensitive and 68% specific.
The patients were aged 25 years to over 85, with an average age of about 65 years; 29 (16%) were diagnosed with SH. Most had nonfunctional adenomas, and a few had adrenal cortical carcinomas.
“Once upon a time, if there was a positive overnight dexamethasone or a positive urinary free cortisol, or both, we would send” patients on for a full inpatient Cushing’s workup. “Now we have a third criterion,” he said: suppressed DHEAS. Also, “in the presence of a high DHEAS with a failed dexamethasone suppression test, you would worry about adrenal corticocarcinoma, pituitary Cushing’s, or adrenal metastasis,” Dr. Dennedy said.
The investigators had no relevant disclosures, and there was no outside funding for the research.
SAN DIEGO – A single baseline measurement of dehydroepiandrosterone sulfate (DHEAS) outperforms overnight dexamethasone suppression and other standard tests for the detection of subclinical hypercortisolism in patients with adrenal incidentalomas, according to a prospective, blinded study of 185 consecutive patients at Cambridge University in England.
It’s an important finding because 1-mg overnight dexamethasone suppression testing is the current screening standard for detection of the condition, said Dr. Michael Dennedy, a former endocrinology fellow at Cambridge and now a senior lecturer at the National University of Ireland (NUI), Galway.
“On the basis of these data, we advocate the use of a single measurement of DHEAS as a convenient, reliable, and robust test for screening of SH [subclinical hypercortisolism] in the context of adrenal incidentalomas,” Dr. Dennedy said at the meeting of the Endocrine Society.
DHEAS avoids the sampling problems and high false positives of older tests and “reliably differentiates between SH and non-SH etiologies of adrenal nodules. We use it now as a standard test for patients who have adrenal nodules” at Cambridge and NUI Galway, he said.
The theory for checking DHEAS is straightforward. Like DHEA, it’s regulated by pituitary ACTH; sustained suppression of central ACTH leads to reductions in both. However, DHEA does not work for screening because it has a short half-life – about 25 minutes – and has circadian secretion patterns similar to ACTH. The half-life of DHEAS, on the other hand, is 10-16 hours and levels stay relatively stable throughout the day, which makes it a more attractive marker for detecting chronically suppressed ACTH.
At baseline, the team measured DHEAS by immunoassay and then put their 185 subjects through standard workups for newly diagnosed adrenal incidentalomas, including plasma metanephrines, 1-mg overnight dexamethasone suppression, 24-hour urinary free cortisol, and paired renin and aldosterone measurements. They then unblinded their DHEAS measurements to see how they fared against the standard approaches.
Because DHEAS levels are determined by a person’s age and gender, the investigators used a ratio of the actual baseline measurement divided by the lower limit of the appropriate reference range; for instance, 1.2 mmol/L in younger patients and 0.4 mmol/L in older patients.
A baseline DHEAS ratio at or below 1.12 was 100% sensitive and 92% specific for the diagnosis of SH in patients with adrenal incidentalomas. In contrast, a cortisol cutoff of 1.9 mcg/dL following 1-mg dexamethasone suppression was 100% sensitive but 82.9% specific and 24-hour urinary free cortisol was 69% sensitive and 68% specific.
The patients were aged 25 years to over 85, with an average age of about 65 years; 29 (16%) were diagnosed with SH. Most had nonfunctional adenomas, and a few had adrenal cortical carcinomas.
“Once upon a time, if there was a positive overnight dexamethasone or a positive urinary free cortisol, or both, we would send” patients on for a full inpatient Cushing’s workup. “Now we have a third criterion,” he said: suppressed DHEAS. Also, “in the presence of a high DHEAS with a failed dexamethasone suppression test, you would worry about adrenal corticocarcinoma, pituitary Cushing’s, or adrenal metastasis,” Dr. Dennedy said.
The investigators had no relevant disclosures, and there was no outside funding for the research.
SAN DIEGO – A single baseline measurement of dehydroepiandrosterone sulfate (DHEAS) outperforms overnight dexamethasone suppression and other standard tests for the detection of subclinical hypercortisolism in patients with adrenal incidentalomas, according to a prospective, blinded study of 185 consecutive patients at Cambridge University in England.
It’s an important finding because 1-mg overnight dexamethasone suppression testing is the current screening standard for detection of the condition, said Dr. Michael Dennedy, a former endocrinology fellow at Cambridge and now a senior lecturer at the National University of Ireland (NUI), Galway.
“On the basis of these data, we advocate the use of a single measurement of DHEAS as a convenient, reliable, and robust test for screening of SH [subclinical hypercortisolism] in the context of adrenal incidentalomas,” Dr. Dennedy said at the meeting of the Endocrine Society.
DHEAS avoids the sampling problems and high false positives of older tests and “reliably differentiates between SH and non-SH etiologies of adrenal nodules. We use it now as a standard test for patients who have adrenal nodules” at Cambridge and NUI Galway, he said.
The theory for checking DHEAS is straightforward. Like DHEA, it’s regulated by pituitary ACTH; sustained suppression of central ACTH leads to reductions in both. However, DHEA does not work for screening because it has a short half-life – about 25 minutes – and has circadian secretion patterns similar to ACTH. The half-life of DHEAS, on the other hand, is 10-16 hours and levels stay relatively stable throughout the day, which makes it a more attractive marker for detecting chronically suppressed ACTH.
At baseline, the team measured DHEAS by immunoassay and then put their 185 subjects through standard workups for newly diagnosed adrenal incidentalomas, including plasma metanephrines, 1-mg overnight dexamethasone suppression, 24-hour urinary free cortisol, and paired renin and aldosterone measurements. They then unblinded their DHEAS measurements to see how they fared against the standard approaches.
Because DHEAS levels are determined by a person’s age and gender, the investigators used a ratio of the actual baseline measurement divided by the lower limit of the appropriate reference range; for instance, 1.2 mmol/L in younger patients and 0.4 mmol/L in older patients.
A baseline DHEAS ratio at or below 1.12 was 100% sensitive and 92% specific for the diagnosis of SH in patients with adrenal incidentalomas. In contrast, a cortisol cutoff of 1.9 mcg/dL following 1-mg dexamethasone suppression was 100% sensitive but 82.9% specific and 24-hour urinary free cortisol was 69% sensitive and 68% specific.
The patients were aged 25 years to over 85, with an average age of about 65 years; 29 (16%) were diagnosed with SH. Most had nonfunctional adenomas, and a few had adrenal cortical carcinomas.
“Once upon a time, if there was a positive overnight dexamethasone or a positive urinary free cortisol, or both, we would send” patients on for a full inpatient Cushing’s workup. “Now we have a third criterion,” he said: suppressed DHEAS. Also, “in the presence of a high DHEAS with a failed dexamethasone suppression test, you would worry about adrenal corticocarcinoma, pituitary Cushing’s, or adrenal metastasis,” Dr. Dennedy said.
The investigators had no relevant disclosures, and there was no outside funding for the research.
AT ENDO 2015
Key clinical point: A single baseline measurement of dehydroepiandrosterone sulfate (DHEAS) beats 1-mg overnight dexamethasone suppression testing for detecting subclinical hypercortisolism.
Major finding: A baseline DHEAS ratio at or below 1.12 was 100% sensitive and 92% specific for the diagnosis of SH in patients with adrenal incidentalomas. In contrast, 1-mg dexamethasone suppression testing was 100% sensitive but 82.9% specific and 24-hour urinary free cortisol was 69% sensitive and 68% specific.
Data source: Prospective, blinded study of 185 patients worked up for adrenal incidentalomas.
Disclosures: The investigators had no relevant disclosures, and there was no outside funding for the work.
Lowering dietary fat, not carbs, led to greater body fat loss
SAN DIEGO – In adults with obesity, lowering intake of dietary fat may lead to greater body fat loss than lowering intake of dietary carbohydrates, results from a small federally funded study showed.
“A lot of focus has been placed on the idea of the competing importance of dietary carbohydrate versus dietary fat in the treatment and prevention of obesity,” lead study author Kevin D. Hall, Ph.D., said during a press briefing at the meeting of the Endocrine Society. “The fashion of which is the evil macronutrient of choice at one time or another is vacillating back and forth. More recently I would say that dietary carbohydrate has been the one demonized, with sugars and refined carbohydrates being the main culprit.”
Dr. Hall, a senior investigator at the National Institute of Diabetes and Digestive and Kidney Diseases, went on to note that at the level of the whole body, “you can think of fat balance as a balance between the intake of fat and how much fat is being burned. So if you’re eating a certain amount of fat and burning that same amount of fat, your body fat will be stable. The only way to perturb that fat balance at the whole-body level is to induce an imbalance between intake of fat and the amount of fat that is being burned.” The low carbohydrate advocates will suggest that an obese adult should decrease carbohydrate intake in the diet, thereby lowering insulin. This in turn has the effect of releasing fat from the fat cells, thereby leading to an imbalance that will eventually rebalance at a lower level of body fat. Alternatively, another way an obese adult could potentially achieve the same results is to cut dietary fat. The resulting state of fat imbalance would promote loss of body fat, according to Dr. Hall.
In an effort to investigate the whole-body energy expenditure and metabolic fat balance from selective restriction of dietary carbohydrate versus dietary fat, the researchers enrolled 19 nondiabetic volunteers with a mean age of 34 years and a mean body mass index of 36 mg/m2. Of the 19 volunteers, 10 were men. The volunteers were housed in a metabolic ward at the National Institutes of Health for a pair of 2-week inpatient visits. For 5 days, everyone was fed a eucaloric baseline diet of 50% carbohydrate, 35% fat, and 15% protein that was designed to provide them with the number of calories they needed to maintain their body weight. Next, the volunteers were randomized to one of two groups where they received a 30% reduced energy diet by restriction of their intake of either fat or carbohydrate. “We provided all of their food; they had no choice in what they ate,” Dr. Hall said.
After a 2-4-week washout period the volunteers returned to the ward and received the alternative diet after the same 5-day baseline run-in phase. “The idea here was [that] we knew exactly how much they ate, and during the time they spent in metabolic chambers we could measure how much fat they burned,” he explained. “So we could calculate how fat oxidation changed as well as the fat imbalance in the body. The low-carb diet selectively reduced carbohydrates, keeping fat and protein at the constant levels, whereas the low-fat diet selectively reduced fat, keeping carbohydrate and protein at baseline levels.”
During the 6-day diet phase the researchers cut 30% of participants’ calories, selectively from either carbohydrates or fat. This translated into about 800 calories per day being cut from both diets.
Dr. Hall reported that reduction of dietary carbohydrates led to a significant increase in whole-body 24-hour fat oxidation (P< .0001), while isocaloric reduction of dietary fat in the same subjects had no significant effect on 24-hour fat oxidation (P = .15). However, the cumulative metabolic fat balance (adding up the daily imbalance between intake and expenditure of fat) indicated that the reduced fat diet resulted in about 80% greater body fat loss, compared with the reduced carbohydrate diet (P = .0003).
Dr. Hall acknowledged certain limitations of the study, including the fact that it did not address the long-term efficacy of low-carbohydrate or low-fat diets. One remaining key unanswered question is whether “the low fat diet continue to outpace the low carbohydrate diet with respect to body fat?” he asked. “This is a short-term study, a small number of people with obesity under metabolic ward conditions. We can’t extrapolate about what might happen to their health with respect to these diets, if they were able to adhere to them for long periods of time.”
The study was funded by the Intramural Research Program of the NIDDK. Dr. Hall reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – In adults with obesity, lowering intake of dietary fat may lead to greater body fat loss than lowering intake of dietary carbohydrates, results from a small federally funded study showed.
“A lot of focus has been placed on the idea of the competing importance of dietary carbohydrate versus dietary fat in the treatment and prevention of obesity,” lead study author Kevin D. Hall, Ph.D., said during a press briefing at the meeting of the Endocrine Society. “The fashion of which is the evil macronutrient of choice at one time or another is vacillating back and forth. More recently I would say that dietary carbohydrate has been the one demonized, with sugars and refined carbohydrates being the main culprit.”
Dr. Hall, a senior investigator at the National Institute of Diabetes and Digestive and Kidney Diseases, went on to note that at the level of the whole body, “you can think of fat balance as a balance between the intake of fat and how much fat is being burned. So if you’re eating a certain amount of fat and burning that same amount of fat, your body fat will be stable. The only way to perturb that fat balance at the whole-body level is to induce an imbalance between intake of fat and the amount of fat that is being burned.” The low carbohydrate advocates will suggest that an obese adult should decrease carbohydrate intake in the diet, thereby lowering insulin. This in turn has the effect of releasing fat from the fat cells, thereby leading to an imbalance that will eventually rebalance at a lower level of body fat. Alternatively, another way an obese adult could potentially achieve the same results is to cut dietary fat. The resulting state of fat imbalance would promote loss of body fat, according to Dr. Hall.
In an effort to investigate the whole-body energy expenditure and metabolic fat balance from selective restriction of dietary carbohydrate versus dietary fat, the researchers enrolled 19 nondiabetic volunteers with a mean age of 34 years and a mean body mass index of 36 mg/m2. Of the 19 volunteers, 10 were men. The volunteers were housed in a metabolic ward at the National Institutes of Health for a pair of 2-week inpatient visits. For 5 days, everyone was fed a eucaloric baseline diet of 50% carbohydrate, 35% fat, and 15% protein that was designed to provide them with the number of calories they needed to maintain their body weight. Next, the volunteers were randomized to one of two groups where they received a 30% reduced energy diet by restriction of their intake of either fat or carbohydrate. “We provided all of their food; they had no choice in what they ate,” Dr. Hall said.
After a 2-4-week washout period the volunteers returned to the ward and received the alternative diet after the same 5-day baseline run-in phase. “The idea here was [that] we knew exactly how much they ate, and during the time they spent in metabolic chambers we could measure how much fat they burned,” he explained. “So we could calculate how fat oxidation changed as well as the fat imbalance in the body. The low-carb diet selectively reduced carbohydrates, keeping fat and protein at the constant levels, whereas the low-fat diet selectively reduced fat, keeping carbohydrate and protein at baseline levels.”
During the 6-day diet phase the researchers cut 30% of participants’ calories, selectively from either carbohydrates or fat. This translated into about 800 calories per day being cut from both diets.
Dr. Hall reported that reduction of dietary carbohydrates led to a significant increase in whole-body 24-hour fat oxidation (P< .0001), while isocaloric reduction of dietary fat in the same subjects had no significant effect on 24-hour fat oxidation (P = .15). However, the cumulative metabolic fat balance (adding up the daily imbalance between intake and expenditure of fat) indicated that the reduced fat diet resulted in about 80% greater body fat loss, compared with the reduced carbohydrate diet (P = .0003).
Dr. Hall acknowledged certain limitations of the study, including the fact that it did not address the long-term efficacy of low-carbohydrate or low-fat diets. One remaining key unanswered question is whether “the low fat diet continue to outpace the low carbohydrate diet with respect to body fat?” he asked. “This is a short-term study, a small number of people with obesity under metabolic ward conditions. We can’t extrapolate about what might happen to their health with respect to these diets, if they were able to adhere to them for long periods of time.”
The study was funded by the Intramural Research Program of the NIDDK. Dr. Hall reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – In adults with obesity, lowering intake of dietary fat may lead to greater body fat loss than lowering intake of dietary carbohydrates, results from a small federally funded study showed.
“A lot of focus has been placed on the idea of the competing importance of dietary carbohydrate versus dietary fat in the treatment and prevention of obesity,” lead study author Kevin D. Hall, Ph.D., said during a press briefing at the meeting of the Endocrine Society. “The fashion of which is the evil macronutrient of choice at one time or another is vacillating back and forth. More recently I would say that dietary carbohydrate has been the one demonized, with sugars and refined carbohydrates being the main culprit.”
Dr. Hall, a senior investigator at the National Institute of Diabetes and Digestive and Kidney Diseases, went on to note that at the level of the whole body, “you can think of fat balance as a balance between the intake of fat and how much fat is being burned. So if you’re eating a certain amount of fat and burning that same amount of fat, your body fat will be stable. The only way to perturb that fat balance at the whole-body level is to induce an imbalance between intake of fat and the amount of fat that is being burned.” The low carbohydrate advocates will suggest that an obese adult should decrease carbohydrate intake in the diet, thereby lowering insulin. This in turn has the effect of releasing fat from the fat cells, thereby leading to an imbalance that will eventually rebalance at a lower level of body fat. Alternatively, another way an obese adult could potentially achieve the same results is to cut dietary fat. The resulting state of fat imbalance would promote loss of body fat, according to Dr. Hall.
In an effort to investigate the whole-body energy expenditure and metabolic fat balance from selective restriction of dietary carbohydrate versus dietary fat, the researchers enrolled 19 nondiabetic volunteers with a mean age of 34 years and a mean body mass index of 36 mg/m2. Of the 19 volunteers, 10 were men. The volunteers were housed in a metabolic ward at the National Institutes of Health for a pair of 2-week inpatient visits. For 5 days, everyone was fed a eucaloric baseline diet of 50% carbohydrate, 35% fat, and 15% protein that was designed to provide them with the number of calories they needed to maintain their body weight. Next, the volunteers were randomized to one of two groups where they received a 30% reduced energy diet by restriction of their intake of either fat or carbohydrate. “We provided all of their food; they had no choice in what they ate,” Dr. Hall said.
After a 2-4-week washout period the volunteers returned to the ward and received the alternative diet after the same 5-day baseline run-in phase. “The idea here was [that] we knew exactly how much they ate, and during the time they spent in metabolic chambers we could measure how much fat they burned,” he explained. “So we could calculate how fat oxidation changed as well as the fat imbalance in the body. The low-carb diet selectively reduced carbohydrates, keeping fat and protein at the constant levels, whereas the low-fat diet selectively reduced fat, keeping carbohydrate and protein at baseline levels.”
During the 6-day diet phase the researchers cut 30% of participants’ calories, selectively from either carbohydrates or fat. This translated into about 800 calories per day being cut from both diets.
Dr. Hall reported that reduction of dietary carbohydrates led to a significant increase in whole-body 24-hour fat oxidation (P< .0001), while isocaloric reduction of dietary fat in the same subjects had no significant effect on 24-hour fat oxidation (P = .15). However, the cumulative metabolic fat balance (adding up the daily imbalance between intake and expenditure of fat) indicated that the reduced fat diet resulted in about 80% greater body fat loss, compared with the reduced carbohydrate diet (P = .0003).
Dr. Hall acknowledged certain limitations of the study, including the fact that it did not address the long-term efficacy of low-carbohydrate or low-fat diets. One remaining key unanswered question is whether “the low fat diet continue to outpace the low carbohydrate diet with respect to body fat?” he asked. “This is a short-term study, a small number of people with obesity under metabolic ward conditions. We can’t extrapolate about what might happen to their health with respect to these diets, if they were able to adhere to them for long periods of time.”
The study was funded by the Intramural Research Program of the NIDDK. Dr. Hall reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
Key clinical point: To reduce body fat, consuming less fat may be more effective than consuming fewer carbohydrates.
Major finding: Reduction of dietary carbohydrates led to a significant increase in whole-body 24-hour fat oxidation (P < .0001), while isocaloric reduction of dietary fat in the same subjects had no significant effect on 24-hour fat oxidation (P = .15).
Data source: An inpatient study of 19 obese adults, which set out to evaluate the selective effect of restricting carbohydrate versus fat on energy and macronutrient balance.
Disclosures: The study was funded by the Intramural Research Program of the NIDDK. Dr. Hall reported having no relevant financial conflicts.
Pamphlet helped Graves’ patients find peace with treatment choices
San Diego – Graves’ disease patients are more comfortable with their treatment decisions when doctors walk them through the options with a short pamphlet being developed at the Mayo Clinic in Rochester, Minn.
None of the three treatment options for Graves’ – thyroidectomy, radioactive iodine, and antithyroid drugs – is clearly superior to the others. That usually means that patients end up getting whatever treatment their institution prefers, and not so much making the choice themselves, said lead investigator Dr. Juan Brito, an assistant endocrinology professor at the Mayo Clinic.
That approach isn’t going to work much longer as patient involvement and satisfaction come online as quality metrics, Dr. Brito noted.
Shared decision making has been a theme at Mayo for a while now, he said, and the institution has developed and validated a range of “decision-making tools” for patients with various diseases. The Graves’ diseasepamphlet is among its latest efforts.
“We don’t really care if patients make a decision for surgery, medicine, or radioactive iodine,” said Dr. Brito. “What we care about is that patients know what they are doing, are more involved in the process, and more satisfied with their decisions.
“We want patients to decide, not the institution,” added Dr. Brito, who noted that Mayo has traditionally been a radioactive iodine institution.
The Graves’ decision pamphlet lays out the pros and cons of all three options – effectiveness, costs, number of follow-up visits, likelihood of thyroid replacement, eye complications, and the like – using five easy-to-understand graphics. The goal is for doctors to use the pamphlet during consultations to ensure that all the bases are covered and patients understand what they hear. The pamphlet doesn’t make consults longer, Dr. Brito noted – if anything, it shortens them a bit.
To assess the pamphlet’s effectiveness, Dr. Brito and his team surveyed patients after their encounters.
The 19 patients guided through their options with the “Graves’ Disease Treatment Choice” pamphlet were more involved with decisions than the 33 patients who were not, as measured by the OPTION [observing patient involvement in decision making] scale (mean score 38.5 points versus 30.8, with 100 points indicating the greatest involvement, P = 0.02).
Pamphlet patients also were more certain of their decisions, as assessed by the Decisional Conflict Scale (19 points versus 31 points, with 0 points being complete certainty, P = 0.19). The length of the discussion was slightly shorter with the pamphlet (37 minutes versus 39 minutes), but the difference was not significant.
Pamphlet patients also seemed more knowledgeable about treatment side effects, and were more likely to choose radioactive iodine and less likely to choose antithyroid drugs; but the differences in what they opted for were also not significant.
On average, patients were in their early 40s, and three-quarters were women.
The decision tool “improves patient involvement in decision making about treatment options without increasing the length of the consultation,” Dr. Brito explained. “This tool helps the patient and clinician navigate through the options and enhances the quality of the process.”
The investigators have no disclosures and no outside funding for their work.
San Diego – Graves’ disease patients are more comfortable with their treatment decisions when doctors walk them through the options with a short pamphlet being developed at the Mayo Clinic in Rochester, Minn.
None of the three treatment options for Graves’ – thyroidectomy, radioactive iodine, and antithyroid drugs – is clearly superior to the others. That usually means that patients end up getting whatever treatment their institution prefers, and not so much making the choice themselves, said lead investigator Dr. Juan Brito, an assistant endocrinology professor at the Mayo Clinic.
That approach isn’t going to work much longer as patient involvement and satisfaction come online as quality metrics, Dr. Brito noted.
Shared decision making has been a theme at Mayo for a while now, he said, and the institution has developed and validated a range of “decision-making tools” for patients with various diseases. The Graves’ diseasepamphlet is among its latest efforts.
“We don’t really care if patients make a decision for surgery, medicine, or radioactive iodine,” said Dr. Brito. “What we care about is that patients know what they are doing, are more involved in the process, and more satisfied with their decisions.
“We want patients to decide, not the institution,” added Dr. Brito, who noted that Mayo has traditionally been a radioactive iodine institution.
The Graves’ decision pamphlet lays out the pros and cons of all three options – effectiveness, costs, number of follow-up visits, likelihood of thyroid replacement, eye complications, and the like – using five easy-to-understand graphics. The goal is for doctors to use the pamphlet during consultations to ensure that all the bases are covered and patients understand what they hear. The pamphlet doesn’t make consults longer, Dr. Brito noted – if anything, it shortens them a bit.
To assess the pamphlet’s effectiveness, Dr. Brito and his team surveyed patients after their encounters.
The 19 patients guided through their options with the “Graves’ Disease Treatment Choice” pamphlet were more involved with decisions than the 33 patients who were not, as measured by the OPTION [observing patient involvement in decision making] scale (mean score 38.5 points versus 30.8, with 100 points indicating the greatest involvement, P = 0.02).
Pamphlet patients also were more certain of their decisions, as assessed by the Decisional Conflict Scale (19 points versus 31 points, with 0 points being complete certainty, P = 0.19). The length of the discussion was slightly shorter with the pamphlet (37 minutes versus 39 minutes), but the difference was not significant.
Pamphlet patients also seemed more knowledgeable about treatment side effects, and were more likely to choose radioactive iodine and less likely to choose antithyroid drugs; but the differences in what they opted for were also not significant.
On average, patients were in their early 40s, and three-quarters were women.
The decision tool “improves patient involvement in decision making about treatment options without increasing the length of the consultation,” Dr. Brito explained. “This tool helps the patient and clinician navigate through the options and enhances the quality of the process.”
The investigators have no disclosures and no outside funding for their work.
San Diego – Graves’ disease patients are more comfortable with their treatment decisions when doctors walk them through the options with a short pamphlet being developed at the Mayo Clinic in Rochester, Minn.
None of the three treatment options for Graves’ – thyroidectomy, radioactive iodine, and antithyroid drugs – is clearly superior to the others. That usually means that patients end up getting whatever treatment their institution prefers, and not so much making the choice themselves, said lead investigator Dr. Juan Brito, an assistant endocrinology professor at the Mayo Clinic.
That approach isn’t going to work much longer as patient involvement and satisfaction come online as quality metrics, Dr. Brito noted.
Shared decision making has been a theme at Mayo for a while now, he said, and the institution has developed and validated a range of “decision-making tools” for patients with various diseases. The Graves’ diseasepamphlet is among its latest efforts.
“We don’t really care if patients make a decision for surgery, medicine, or radioactive iodine,” said Dr. Brito. “What we care about is that patients know what they are doing, are more involved in the process, and more satisfied with their decisions.
“We want patients to decide, not the institution,” added Dr. Brito, who noted that Mayo has traditionally been a radioactive iodine institution.
The Graves’ decision pamphlet lays out the pros and cons of all three options – effectiveness, costs, number of follow-up visits, likelihood of thyroid replacement, eye complications, and the like – using five easy-to-understand graphics. The goal is for doctors to use the pamphlet during consultations to ensure that all the bases are covered and patients understand what they hear. The pamphlet doesn’t make consults longer, Dr. Brito noted – if anything, it shortens them a bit.
To assess the pamphlet’s effectiveness, Dr. Brito and his team surveyed patients after their encounters.
The 19 patients guided through their options with the “Graves’ Disease Treatment Choice” pamphlet were more involved with decisions than the 33 patients who were not, as measured by the OPTION [observing patient involvement in decision making] scale (mean score 38.5 points versus 30.8, with 100 points indicating the greatest involvement, P = 0.02).
Pamphlet patients also were more certain of their decisions, as assessed by the Decisional Conflict Scale (19 points versus 31 points, with 0 points being complete certainty, P = 0.19). The length of the discussion was slightly shorter with the pamphlet (37 minutes versus 39 minutes), but the difference was not significant.
Pamphlet patients also seemed more knowledgeable about treatment side effects, and were more likely to choose radioactive iodine and less likely to choose antithyroid drugs; but the differences in what they opted for were also not significant.
On average, patients were in their early 40s, and three-quarters were women.
The decision tool “improves patient involvement in decision making about treatment options without increasing the length of the consultation,” Dr. Brito explained. “This tool helps the patient and clinician navigate through the options and enhances the quality of the process.”
The investigators have no disclosures and no outside funding for their work.
AT ENDO 2015
Key clinical point: It’s possible to increase patient involvement in treatment decisions without increasing length of consultations.
Major finding: The 19 Graves’ patients guided through treatment options with a Mayo Clinic Graves’ pamphlet were more involved with decision making than the 33 who were not, as measured by the OPTION scale (mean score 38.5 points versus 30.8, with 100 points indicating the greatest involvement, P = 0.02).
Data source: Surveys of 55 Graves’ disease patients.
Disclosures: The investigators have no disclosures and no outside funding for their work.
Long-term endocrine effects common after reduced-intensity chemotherapy in children
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
SAN DIEGO – Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Traditionally, hematopoietic stem cell transplants (HSCT) for leukemia and other malignancies are preceded by myeloablation with high-dose chemotherapy and radiation. Over the past decade, however, that approach has been supplanted by reduced-intensity conditioning (RIC), a gentler method for less aggressive diseases that don’t require a cancer to be wiped out before HSCT. RIC usually involves low-dose chemotherapy without radiation.
The hope is to reduce side effects with the gentler approach, but that’s not always how it works, according to a retrospective study of 120 children followed for a mean of 3.2 years at the Cincinnati Children’s Hospital Medical Center, which was presented at a poster session at the meeting of the Endocrine Society.
The children had RIC with campath, fludarabine, and melphalan – but no radiation – prior to one HSCT for hemophagocytic lymphohistiocytosis/X-linked lymphoproliferative syndrome (HLH/XLP), primary immune deficiency, or other generally nonmalignant conditions.
During follow-up, almost a quarter had thyroid problems and nearly three-fourths were vitamin-D deficient. Children less than 2 years old when transplanted started to catch up to their peers on growth charts, but children over 2 years old fell further behind. Hypogonadism might be a problem, too; the investigators plan to follow the children to see how they fare during puberty.
“We were surprised” by the results, said senior investigator Dr. Susan Rose, professor of endocrinology at the University of Cincinnati.
“We really thought that, with [RIC], not as many of them would have problems after their transplants, and they would grow better. [Many] were coming off steroids” after the procedure, “which usually leads children to have catch-up growth. Instead, we are seeing their growth is slower than normal. The occurrence of endocrinopathy after [RIC] is probably lower than with high-dose chemotherapy combined with radiation, but we still have to monitor [these children] and not be cavalier” about follow-up, she said.
“We can’t expect there to be no or fewer endocrine complications just because there was a less intensive [conditioning] regimen. We must, as endocrinologists, be vigilant about monitoring and screening” these patients, said endocrinologist and lead author Dr. Jonathan Howell, assistant professor of pediatrics at the university.
The children were an average of 6 years old when transplanted. They were shorter than average both before (height-for-age Z-score [HAZ] = –1.33) and after (HAZ = –1.35).
Children with HLH/XLP who were under 2 years old at transplant improved from an HAZ of –3.36 to –1.35 afterwards, but older children fell from an HAZ of –0.61 to –0.99.
Older children with HLH/XLP lost weight after transplant (body mass index Z-score [BMI-Z], 1.29 vs. 0.61), as did those transplanted for metabolic or genetic disorders (BMI-Z, 0.56 vs. –0.77). There was a trend towards increased BMI-Z in toddlers.
Seventy-seven children had their thyroids checked after HSCT: 11 had primary hypothyroidism, five had central hypothyroidism, and two were hyperthyroid. Also, 48 of the 68 children assessed for 25-OH vitamin D had levels below 30 ng/mL.
Fourteen children broke bones after their transplants and six were diagnosed with avascular necrosis. The team is looking into whether it had something to do with endocrine dysfunction.
The investigators had no disclosures and no external funding for their work.
AT ENDO 2015
Key clinical point: Remain vigilant for endocrine side effects after reduced-intensity conditioning for hematopoietic stem cell transplants in children.
Major finding: Of the 77 children assessed for thyroid function after HSCT with reduced-intensity conditioning, 11 had evidence of primary hypothyroidism, five had central hypothyroidism, and two had evidence of primary hyperthyroidism.
Data source: Review of 120 pediatric hematopoietic stem cell transplants at the Cincinnati Children’s Hospital Medical Center.
Disclosures: The investigators had no disclosures and no external funding for their work.
Gastric bypass patients on calcium had higher rates of kidney stone growth
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
SAN DIEGO – Patients taking calcium supplementation after gastric bypass surgery had higher rates of kidney stone growth, compared with those who received no calcium supplementation, results from a single-center retrospective study showed.
In addition, the majority of stones in patients taking calcium supplementation were comprised of calcium oxalate monohydrate, which is less amenable to extracorporeal shockwave therapy. “You need more invasive procedures to break up these kinds of stones,” lead author Christopher Loftus said in an interview at the meeting of the Endocrine Society, where the study was presented during a late-breaking abstract session.
Though it has been demonstrated that bariatric surgery is associated with an increased risk of kidney stone formation (Kidney Int. 2014 [doi:10.1038/ki.2014.352]), Mr. Loftus, a fourth-year medical student at Cleveland Clinic Lerner College of Medicine, and his associates set out to determine whether calcium supplementation increases the risk of nephrolithiasis in 60 stone-forming patients after gastric bypass surgery performed at the Cleveland Clinic. For each patient, two unenhanced CT scans at least 1 month apart and less than 2 years apart were selected at the start of the supplementation date and after the gastric bypass surgery date. The researchers calculated the rate of stone growth by the change in consecutive stone burden (the sum of maximum diameters of stones) divided by the elapsed time between scans.
Of the 60 patients, 31 received postoperative calcium supplementation (an average of 500 mg/day) and 29 did not. Compared with patients who did not take calcium supplementation, those who did were younger (a mean of 53 years vs. 58 years, respectively), more likely to be female (81% vs. 69%), and had a higher body mass index (34.5 kg/m2 vs. 32.7 kg/m2). In addition, a greater proportion of patients taking calcium supplements underwent Roux-en-Y bypass (83% vs. 64%; P = .19), had stones comprised of calcium oxalate (81% vs. 67%; P = .56), and a higher rate of stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004). “We weren’t expecting such a pronounced effect,” Mr. Loftus said.
In their abstract, the researchers said that further studies are required to elucidate the exact role of calcium supplementation on stone disease in this patient population.
The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
Key clinical point: Calcium supplementation for post-gastric bypass surgery patients may increase the risk of kidney stone growth.
Major finding: Compared with patients who did not take calcium supplementation, those who did had a higher rate of kidney stone growth (more than 10 mm/year vs. less than 5 mm/year; P = .0004).
Data source: An analysis of 60 stone-forming patients who underwent gastric bypass surgery at the Cleveland Clinic.
Disclosures: The study was funded in part by a grant from the American Society of Nephrology. Mr. Loftus reported having no relevant financial conflicts.
Racial differences in birth outcomes noted in women using ART
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
AT ENDO 2015
SAN DIEGO – Compared to white women undergoing assisted reproductive technology, black women were more likely to have preterm births and deliver small-for-gestational-age infants, a large prospective cohort study demonstrated.
“What this means in the long-term outcomes and what this means as far as counseling [ART patients] is a tricky subject, but I think it does warrant more study,” Dr. Snigdha Alur, the study’s lead author, said in an interview at the meeting of the Endocrine Society.
Assisted reproductive technology “is an increasingly employed form of treatment, prompting interest in which factors could predict or influence its success. Despite black women having the highest prevalence of infertility and ample investigation on racial disparities influencing pregnancy outcomes, few have evaluated whether race also affects ART outcomes,” Dr. Alur of the department of obstetrics and gynecology at the University of Rochester (N.Y.) Medical Center, and her associates wrote in a late-breaking abstract.
In an effort to explore whether adverse pregnancy outcomes differ between white and black women using ART, the researchers evaluated data from 1,871 singleton births to women resulting from ART delivered in the Central and Finger Lakes regions of New York state between 2005 and 2013.
The women completed the state’s perinatal data system questionnaire pertaining to their and their partners’ background and their prenatal care, labor course, and birth outcome. These data were combined with obstetric records including birth size and gestational age. A preterm birth was defined as one delivered at less than 37 weeks’ gestational age, while a very preterm birth was defined as one delivered at less than 34 weeks’ gestational age. A small-for-gestational-age (SGA) infant and a very SGA infant were defined as gender-adjusted weight less than 10% and less than 5%, respectively.
Of the 1,871 singleton births studied, 47 were to black women and 1,824 were to white women. After the researchers adjusted for maternal age, smoking status, highest level of education, and other covariates, black women were significantly more likely to have preterm births (odds ratio, 2.63) but not very preterm births (OR, 2.17), compared with their white counterparts. They also had significantly increased odds of having a SGA (OR, 2.71) or a very SGA infant (OR, 3.01), compared with white women.
“It could be that we have to alter some of our counseling and education based on some of these findings,” Dr. Alur said. “Maybe it’s not just the ART, but there could be other factors playing a role [in poorer outcomes for black ART pregnancies] that need further research.”
Dr. Alur reported having no relevant financial conflicts.
On Twitter @dougbrunk
Key clinical point: Black women with singleton births from assisted reproductive technology were more likely to have preterm births and deliver SGA infants when compared with white women who also used ART.
Major finding: Black women were significantly more likely to have preterm births (OR 2.63) but not very preterm births (OR 2.17), when compared with their white counterparts. They also had significantly increased odds of having a SGA (OR 2.71) or a very SGA infant (OR 3.01).
Data source: A prospective analysis of 1,871 births to women resulting from ART delivered in the Central and Finger Lakes regions of New York State between 2005 and 2013.
Disclosures: Dr. Alur reported having no relevant financial conflicts.
VIDEO: Following breast cancer diagnosis, risk of thyroid cancer rises
SAN DIEGO – Women who survive breast cancer face an increased risk of developing thyroid cancer, especially within 5 years of their breast cancer diagnosis, according to a large analysis of the National Cancer Institute’s Surveillance, Epidemiology, and End Results 9 database, covering 1973-2011.
In an interview at the meeting of the Endocrine Society, the study’s lead author, Dr. Jennifer H. Kuo, thyroid biopsy program director in the division of GI/endocrine surgery at Columbia University, New York, said that compared with patients with breast cancer alone, women who had breast cancer followed by thyroid cancer were younger on average when diagnosed with their breast cancer. They also were more likely to have had invasive ductal carcinoma, a smaller focus of cancer, and to have received radiation therapy as part of their breast cancer treatment.
Dr. Kuo concluded that recognition of the association should prompt vigilant screening for thyroid cancer among breast cancer survivors. She reported having no relevant financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @dougbrunk
SAN DIEGO – Women who survive breast cancer face an increased risk of developing thyroid cancer, especially within 5 years of their breast cancer diagnosis, according to a large analysis of the National Cancer Institute’s Surveillance, Epidemiology, and End Results 9 database, covering 1973-2011.
In an interview at the meeting of the Endocrine Society, the study’s lead author, Dr. Jennifer H. Kuo, thyroid biopsy program director in the division of GI/endocrine surgery at Columbia University, New York, said that compared with patients with breast cancer alone, women who had breast cancer followed by thyroid cancer were younger on average when diagnosed with their breast cancer. They also were more likely to have had invasive ductal carcinoma, a smaller focus of cancer, and to have received radiation therapy as part of their breast cancer treatment.
Dr. Kuo concluded that recognition of the association should prompt vigilant screening for thyroid cancer among breast cancer survivors. She reported having no relevant financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @dougbrunk
SAN DIEGO – Women who survive breast cancer face an increased risk of developing thyroid cancer, especially within 5 years of their breast cancer diagnosis, according to a large analysis of the National Cancer Institute’s Surveillance, Epidemiology, and End Results 9 database, covering 1973-2011.
In an interview at the meeting of the Endocrine Society, the study’s lead author, Dr. Jennifer H. Kuo, thyroid biopsy program director in the division of GI/endocrine surgery at Columbia University, New York, said that compared with patients with breast cancer alone, women who had breast cancer followed by thyroid cancer were younger on average when diagnosed with their breast cancer. They also were more likely to have had invasive ductal carcinoma, a smaller focus of cancer, and to have received radiation therapy as part of their breast cancer treatment.
Dr. Kuo concluded that recognition of the association should prompt vigilant screening for thyroid cancer among breast cancer survivors. She reported having no relevant financial conflicts to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @dougbrunk
AT ENDO 2015