User login
Digestive Disease Week (DDW 2015)
VIDEO: Stroop app predicts hepatic encephalopathy
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT DDW 2015
DDW: Scheduled for a colonoscopy? Pass the pretzels!
WASHINGTON – A novel, edible colon preparation could make obsolete the fasting and large volume of salty liquid cleansing that keep many a patient from completing their colonoscopies.
A pilot study showed that all 10 patients who ate a series of nutritionally balanced meals, drinks, and snacks such as pretzels and pudding had a successful colon cleansing according to the endoscopist at the time of the procedure, Dr. L. Campbell Levy of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., reported at the annual Digestive Disease Week.
The preparation, which is blended with polyethylene glycol 3350, sorbitol, and ascorbic acid, did not produce any significant changes in electrolytes or creatinine.
There were no adverse events and, equally important, all 10 patients said that they would follow the edible bowel regimen again for a subsequent procedure.
In a video interview, he discussed the small study’s results and the plans for larger, randomized studies.
Dr. Levy reported no relevant conflicts. The inventor of the diet and the founder of Colonary Concepts were involved in the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
WASHINGTON – A novel, edible colon preparation could make obsolete the fasting and large volume of salty liquid cleansing that keep many a patient from completing their colonoscopies.
A pilot study showed that all 10 patients who ate a series of nutritionally balanced meals, drinks, and snacks such as pretzels and pudding had a successful colon cleansing according to the endoscopist at the time of the procedure, Dr. L. Campbell Levy of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., reported at the annual Digestive Disease Week.
The preparation, which is blended with polyethylene glycol 3350, sorbitol, and ascorbic acid, did not produce any significant changes in electrolytes or creatinine.
There were no adverse events and, equally important, all 10 patients said that they would follow the edible bowel regimen again for a subsequent procedure.
In a video interview, he discussed the small study’s results and the plans for larger, randomized studies.
Dr. Levy reported no relevant conflicts. The inventor of the diet and the founder of Colonary Concepts were involved in the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
WASHINGTON – A novel, edible colon preparation could make obsolete the fasting and large volume of salty liquid cleansing that keep many a patient from completing their colonoscopies.
A pilot study showed that all 10 patients who ate a series of nutritionally balanced meals, drinks, and snacks such as pretzels and pudding had a successful colon cleansing according to the endoscopist at the time of the procedure, Dr. L. Campbell Levy of Dartmouth-Hitchcock Medical Center in Lebanon, N.H., reported at the annual Digestive Disease Week.
The preparation, which is blended with polyethylene glycol 3350, sorbitol, and ascorbic acid, did not produce any significant changes in electrolytes or creatinine.
There were no adverse events and, equally important, all 10 patients said that they would follow the edible bowel regimen again for a subsequent procedure.
In a video interview, he discussed the small study’s results and the plans for larger, randomized studies.
Dr. Levy reported no relevant conflicts. The inventor of the diet and the founder of Colonary Concepts were involved in the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
AT DDW® 2015
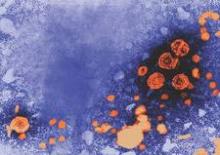
DDW: HBV, tuberculosis reactivations rare in IBD patients on biologic therapy
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
AT DDW 2015
Key clinical point: Significant clinical events related to tuberculosis and hepatitis B virus reactivation after initiating anti–tumor necrosis factor therapy in a screened population are rare.
Major finding: Rates of tuberculosis and HBV were estimated at 2.8 and less than 1.4 cases per 10,000 patient-years of exposure to treatment, respectively, in a large, fairly well screened national cohort of veterans with IBD treated with an anti-TNF drug.
Data source: A retrospective cohort study evaluated the rates of tuberculosis and HBV reactivation, identifying cases of IBD treated with anti-TNF therapy in a Veterans Health Administration database during 2003-2011, confirming cases, treatment, and HBV and TB screening status with electronic medical record review.
Disclosures: Dr. Hou’s financial disclosure includes receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and Abbvie.
The GLUTOX Trial: Getting closer to identifying nonceliac gluten sensitivity
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
AT DDW 2015
Key clinical point: A randomized, double-blind dietary challenge may be useful in identifying nonceliac gluten sensitivity.
Major finding: More than 30% of patients with functional gastrointestinal disorders were classified as possibly having nonceliac gluten sensitivity.
Data source: Randomized, double-blind study in 100 patients with suspected nonceliac gluten sensitivity.
Disclosures: The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
DDW: VIDEO: What we don’t know in the management of liver disease and coagulopathy
WASHINGTON – Your patient has cirrhosis, platelets 60,000 mm3, an INR of 2.0, serum creatinine of 1.2 mg/dL, and requires an endoscopic retrograde cholangiopancreatography with sphincterotomy.
What do you do next?
Management of a patient such as this is challenging, but not just because of the long-perceived risk for bleeding, Dr. Patrick S. Kamath of the Mayo Clinic in Rochester, Minn., said during a clinical symposium at the annual Digestive Disease Week.
Several other factors must be considered, including the clotting risk in patients with liver disease and the fact that procedure-related bleeding risk cannot be adequately determined preprocedure. Transfusions also carry their own dangers in this patient population and should be approached with caution, he said.
To hear more from this world-renowned liver expert, check out our interview as we sat down with Dr. Kamath at this year’s DDW.
Dr. Kamath reported no relevant financial conflicts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
WASHINGTON – Your patient has cirrhosis, platelets 60,000 mm3, an INR of 2.0, serum creatinine of 1.2 mg/dL, and requires an endoscopic retrograde cholangiopancreatography with sphincterotomy.
What do you do next?
Management of a patient such as this is challenging, but not just because of the long-perceived risk for bleeding, Dr. Patrick S. Kamath of the Mayo Clinic in Rochester, Minn., said during a clinical symposium at the annual Digestive Disease Week.
Several other factors must be considered, including the clotting risk in patients with liver disease and the fact that procedure-related bleeding risk cannot be adequately determined preprocedure. Transfusions also carry their own dangers in this patient population and should be approached with caution, he said.
To hear more from this world-renowned liver expert, check out our interview as we sat down with Dr. Kamath at this year’s DDW.
Dr. Kamath reported no relevant financial conflicts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
WASHINGTON – Your patient has cirrhosis, platelets 60,000 mm3, an INR of 2.0, serum creatinine of 1.2 mg/dL, and requires an endoscopic retrograde cholangiopancreatography with sphincterotomy.
What do you do next?
Management of a patient such as this is challenging, but not just because of the long-perceived risk for bleeding, Dr. Patrick S. Kamath of the Mayo Clinic in Rochester, Minn., said during a clinical symposium at the annual Digestive Disease Week.
Several other factors must be considered, including the clotting risk in patients with liver disease and the fact that procedure-related bleeding risk cannot be adequately determined preprocedure. Transfusions also carry their own dangers in this patient population and should be approached with caution, he said.
To hear more from this world-renowned liver expert, check out our interview as we sat down with Dr. Kamath at this year’s DDW.
Dr. Kamath reported no relevant financial conflicts.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @pwendl
AT DDW 2015
DDW: Barrett’s ‘indefinite for dysplasia’ may be cancer harbinger
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
AT DDW 2015
Key clinical point: Barrett’s esophagus indefinite for dysplasia may progress to dysplasia or adenocarcinoma within a year of diagnosis.
Major finding: Seven of 87 patients with a diagnosis of Barrett’s indefinite for dysplasia (IND) had disease progression within 1 year.
Data source: Retrospective case series of 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s IND.
Disclosures: The study was internally funded. The authors reported no conflicts of interest.
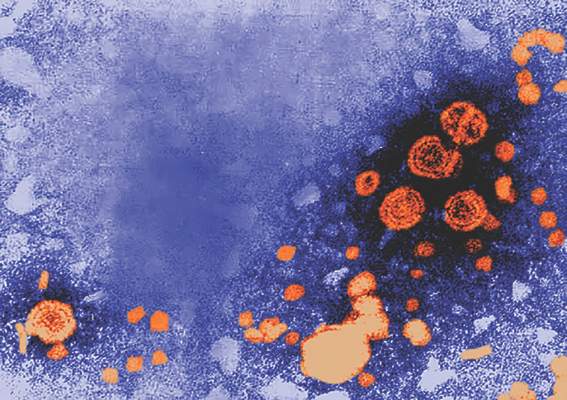
Significant Worker Productivity Gains With Newer Hepatitis C Drugs
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
FROM DDW 2015
DDW: Significant worker productivity gains with newer hepatitis C drugs
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
Achieving a cure in hepatitis C infection could result in significant economic gains, with a study estimating that the beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Researchers used data on work productivity and activity scores from patients enrolled in clinical trials of the all-oral sofosbuvir and lepidasvir combo to estimate the impact of achieving sustained virologic response at 12 weeks (SVR-12) on workers’ productivity.
They calculated an average work productivity loss of $4,954 for each employed patient with chronic hepatitis C infection per year in the United States and $1,129 per year for the five European Union countries included in the mix.
“These new all-oral combinations such as lepidasvir and sofosbuvir have cure rates between 95% and 99% with minimum side effects, [so] treating patients with these combinations results in improved work productivity, improved quality of life, and patient-reported outcomes that can translate into economic benefit,” Dr. Zobair M. Younossi of the Inova Fairfax Medical Campus, Falls Church, Va., said at the annual Digestive Disease Week.
No conflicts of interest were disclosed.
FROM DDW 2015
Key clinical point: Achieving a cure in hepatitis C infection could result in significant economic gains from improved worker productivity.
Major finding: The beneficial effects in terms of improved worker productivity could total around $3.23 billion per year for the United States alone.
Data source: Economic model using data from hepatitis C clinical trials in the United States and Europe.
Disclosures: No conflicts of interest were disclosed.
DDW: Biologic agents improve Crohn’s disease picture
WASHINGTON – The course of Crohn’s disease has changed for the better since the introduction of biological therapies and other treatments in the late 1990s.
“In an era of novel treatment options and strategies for Crohn’s disease, we are seeing that the hospitalization and surgery rates have declined, but progression to a complicated phenotype is unfortunately still common nowadays,” said Dr. Steven Jeuring from Maastricht (the Netherlands) University Medical Center.
A community-based study comparing outcomes for patients with Crohn’s Disease (CD) before and after the introduction of infliximab (Remicade) in the Netherlands in 1999 showed the risk of hospitalization was 55% lower for patients treated after 1999, and the risk for hospitalization during the course of the disease was 35% lower. Similarly, the risk for requiring surgery was 77% lower for patients treated in the modern era, and the risk for surgery at any time in the disease course was 54% lower, Dr. Jeuring said at the annual Digestive Disease Week.
The prevalence of a complicated CD phenotype, marked by the presence of bowel stricturing and/or penetration, was also 48% lower at the time of diagnosis among patients treated within the last two decades, but the rate of progression from an inflammatory to complicated phenotype remained unchanged from the pre-biologics era, Dr. Jeuring said.
He and his colleagues conducted a retrospective study with a population-based cohort of adults with incident inflammatory bowel disease diagnosed from 1991 through 1998 (342 patients) and from 1999 through 2011 (820 patients). The cohort represented 93% of all patients in the IBD registry of the South Limburg region of the Netherlands.
They found that the distribution of disease phenotypes was significantly different between the two time periods, with 45% of patients having complicated disease in the pre-biologics era, compared with 37% during the biologics era, translating into a 23% reduction over time. However, in both cohorts, a fairly large proportion of patients already had complicated disease at the time of diagnosis, Dr. Jeuring noted.
When the investigators looked at the risk of developing stricturing or penetrating disease during 8 years of follow-up, however, they found that there was no difference between the groups, with 30% of patients in the earlier cohort having disease progression, compared with 28% of patients in the later cohort, translating into a non-significant hazard ratio (HR) of 0.95.
Dr. Jeuring said that this finding was “very, very disappointing.”
More encouraging, however was the finding that hospitalization rates in the modern era were significantly lower than in the pre-biologics period. For example, the likelihood of being hospitalized at any time during 8 years of follow-up was 72% in the earlier cohort, compared with 52% in the later cohort.
The HR for being hospitalized at the time of diagnosis among the later vs. earlier cohorts was 0.45, and was statistically significant. Similarly, the HR for being hospitalized at any time over 8 years was 0.65 for patients in the modern era (also significant, with a 95% confidence interval that did not cross 1).
Even more dramatically, more modern therapies were associated with a significant reduction in the risk of being rehospitalized, with a significant HR of 0.29.
The risk for surgical resection either at diagnosis or during the 8-year follow-up period was 52% among patients diagnosed and started on treatment in the 1990s, compared with 25% for patients treated in the new millennium. For the latter cohort, the HRs for surgery at the time of diagnosis and for surgery during follow-up were 0.23 and 0.46, respectively. Both were statistically significant.
The lower risk for surgery for patients in the modern era is primarily driven by decreased risk for surgery for inflammatory disease, Dr, Jeuring said.
The study was supported by Maastricht University Medical Center. Dr. Jeuring reported having no conflicts of interest.
WASHINGTON – The course of Crohn’s disease has changed for the better since the introduction of biological therapies and other treatments in the late 1990s.
“In an era of novel treatment options and strategies for Crohn’s disease, we are seeing that the hospitalization and surgery rates have declined, but progression to a complicated phenotype is unfortunately still common nowadays,” said Dr. Steven Jeuring from Maastricht (the Netherlands) University Medical Center.
A community-based study comparing outcomes for patients with Crohn’s Disease (CD) before and after the introduction of infliximab (Remicade) in the Netherlands in 1999 showed the risk of hospitalization was 55% lower for patients treated after 1999, and the risk for hospitalization during the course of the disease was 35% lower. Similarly, the risk for requiring surgery was 77% lower for patients treated in the modern era, and the risk for surgery at any time in the disease course was 54% lower, Dr. Jeuring said at the annual Digestive Disease Week.
The prevalence of a complicated CD phenotype, marked by the presence of bowel stricturing and/or penetration, was also 48% lower at the time of diagnosis among patients treated within the last two decades, but the rate of progression from an inflammatory to complicated phenotype remained unchanged from the pre-biologics era, Dr. Jeuring said.
He and his colleagues conducted a retrospective study with a population-based cohort of adults with incident inflammatory bowel disease diagnosed from 1991 through 1998 (342 patients) and from 1999 through 2011 (820 patients). The cohort represented 93% of all patients in the IBD registry of the South Limburg region of the Netherlands.
They found that the distribution of disease phenotypes was significantly different between the two time periods, with 45% of patients having complicated disease in the pre-biologics era, compared with 37% during the biologics era, translating into a 23% reduction over time. However, in both cohorts, a fairly large proportion of patients already had complicated disease at the time of diagnosis, Dr. Jeuring noted.
When the investigators looked at the risk of developing stricturing or penetrating disease during 8 years of follow-up, however, they found that there was no difference between the groups, with 30% of patients in the earlier cohort having disease progression, compared with 28% of patients in the later cohort, translating into a non-significant hazard ratio (HR) of 0.95.
Dr. Jeuring said that this finding was “very, very disappointing.”
More encouraging, however was the finding that hospitalization rates in the modern era were significantly lower than in the pre-biologics period. For example, the likelihood of being hospitalized at any time during 8 years of follow-up was 72% in the earlier cohort, compared with 52% in the later cohort.
The HR for being hospitalized at the time of diagnosis among the later vs. earlier cohorts was 0.45, and was statistically significant. Similarly, the HR for being hospitalized at any time over 8 years was 0.65 for patients in the modern era (also significant, with a 95% confidence interval that did not cross 1).
Even more dramatically, more modern therapies were associated with a significant reduction in the risk of being rehospitalized, with a significant HR of 0.29.
The risk for surgical resection either at diagnosis or during the 8-year follow-up period was 52% among patients diagnosed and started on treatment in the 1990s, compared with 25% for patients treated in the new millennium. For the latter cohort, the HRs for surgery at the time of diagnosis and for surgery during follow-up were 0.23 and 0.46, respectively. Both were statistically significant.
The lower risk for surgery for patients in the modern era is primarily driven by decreased risk for surgery for inflammatory disease, Dr, Jeuring said.
The study was supported by Maastricht University Medical Center. Dr. Jeuring reported having no conflicts of interest.
WASHINGTON – The course of Crohn’s disease has changed for the better since the introduction of biological therapies and other treatments in the late 1990s.
“In an era of novel treatment options and strategies for Crohn’s disease, we are seeing that the hospitalization and surgery rates have declined, but progression to a complicated phenotype is unfortunately still common nowadays,” said Dr. Steven Jeuring from Maastricht (the Netherlands) University Medical Center.
A community-based study comparing outcomes for patients with Crohn’s Disease (CD) before and after the introduction of infliximab (Remicade) in the Netherlands in 1999 showed the risk of hospitalization was 55% lower for patients treated after 1999, and the risk for hospitalization during the course of the disease was 35% lower. Similarly, the risk for requiring surgery was 77% lower for patients treated in the modern era, and the risk for surgery at any time in the disease course was 54% lower, Dr. Jeuring said at the annual Digestive Disease Week.
The prevalence of a complicated CD phenotype, marked by the presence of bowel stricturing and/or penetration, was also 48% lower at the time of diagnosis among patients treated within the last two decades, but the rate of progression from an inflammatory to complicated phenotype remained unchanged from the pre-biologics era, Dr. Jeuring said.
He and his colleagues conducted a retrospective study with a population-based cohort of adults with incident inflammatory bowel disease diagnosed from 1991 through 1998 (342 patients) and from 1999 through 2011 (820 patients). The cohort represented 93% of all patients in the IBD registry of the South Limburg region of the Netherlands.
They found that the distribution of disease phenotypes was significantly different between the two time periods, with 45% of patients having complicated disease in the pre-biologics era, compared with 37% during the biologics era, translating into a 23% reduction over time. However, in both cohorts, a fairly large proportion of patients already had complicated disease at the time of diagnosis, Dr. Jeuring noted.
When the investigators looked at the risk of developing stricturing or penetrating disease during 8 years of follow-up, however, they found that there was no difference between the groups, with 30% of patients in the earlier cohort having disease progression, compared with 28% of patients in the later cohort, translating into a non-significant hazard ratio (HR) of 0.95.
Dr. Jeuring said that this finding was “very, very disappointing.”
More encouraging, however was the finding that hospitalization rates in the modern era were significantly lower than in the pre-biologics period. For example, the likelihood of being hospitalized at any time during 8 years of follow-up was 72% in the earlier cohort, compared with 52% in the later cohort.
The HR for being hospitalized at the time of diagnosis among the later vs. earlier cohorts was 0.45, and was statistically significant. Similarly, the HR for being hospitalized at any time over 8 years was 0.65 for patients in the modern era (also significant, with a 95% confidence interval that did not cross 1).
Even more dramatically, more modern therapies were associated with a significant reduction in the risk of being rehospitalized, with a significant HR of 0.29.
The risk for surgical resection either at diagnosis or during the 8-year follow-up period was 52% among patients diagnosed and started on treatment in the 1990s, compared with 25% for patients treated in the new millennium. For the latter cohort, the HRs for surgery at the time of diagnosis and for surgery during follow-up were 0.23 and 0.46, respectively. Both were statistically significant.
The lower risk for surgery for patients in the modern era is primarily driven by decreased risk for surgery for inflammatory disease, Dr, Jeuring said.
The study was supported by Maastricht University Medical Center. Dr. Jeuring reported having no conflicts of interest.
AT DDW 2015
Key clinical point: The advent of biologic agents has improved hospitalization and surgery rates for patients with Crohn’s disease.
Major finding: The risk of hospitalization for patients treated after 1999 or for hospitalization during the course of the disease was 55% and 35% lower, respectively. and the risks for requiring surgery in the modern era or at any time in the disease course was 77% and 54% lower.
Data source: Population-based cohort study of 1,162 patients with inflammatory bowel disease in the South Limburg region of the Netherlands.
Disclosures: The study was supported by Maastricht University Medical Center. Dr. Jeuring reported having no conflicts of interest.
DDW: Statin use associated with significantly lower risk of new-onset IBD
WASHINGTON – A prescription for a statin was associated with about a 40% lower risk of new-onset inflammatory bowel disease in a study that evaluated data from a large U.S. health claims database over a 5-year period, Dr. Ryan Ungaro said at the annual Digestive Disease Week.
The protective effect was seen with different statins and was not associated with the intensity of statin treatment, said Dr. Ungaro, a gastroenterologist at Mount Sinai Hospital, New York.
He and his associates conducted a case-control study by using a national medical claims and pharmacy database, identifying 87,579 patients aged 18 and older with an ICD-9 code for a diagnosis of ulcerative colitis (UC) or Crohn’s disease (CD) from January 2008 through December 2012, and 189,526 controls (each case was matched with up to 10 controls, matched for age, gender, race, and state of residence). The median age of cases and controls was about 51 years, and about 41% were male. About 47% were diagnosed with CD, and about 44% were diagnosed with UC. A smaller group of patients who were new-onset cases were included who had at least 1 year with no IBD-related diagnostic code or prescription before the index diagnosis.
Statin use was associated with about a 40% reduced risk of new-onset IBD (odds ratio, 0.59), with similar trends for UC and CD, Dr. Ungaro reported. Separately, the risks of new-onset CD (OR, 0.55) and new-onset UC (OR, 0.62) associated with having a prescription for a statin were also significantly lower.
This association was maintained “regardless of which specific statin a patient was exposed to,” he noted. There was no significant difference in risk of IBD based on the intensity of statin treatment, according to American Heart Association guidelines for low-, moderate-, and high-intensity treatment.
Another finding was that the strongest protective effect was seen in older people, with an OR of 0.55 among those aged 60 years and older. There was no significant effect among those aged 18-30 years, but there were a limited number of statin prescriptions for younger patients, Dr. Ungaro noted.
Limitations of the study include the retrospective design, the inability to directly validate cases, and the reliance on a prescription as a surrogate for the patient actually taking the medication, he said.
Based on the results, “we think that future studies should confirm this protective effect, as well as continue to investigate statins in established IBD,” he concluded.
He referred to recent research demonstrating that statins have immunomodulatory effects “and may actually potentially be beneficial in established IBD.” In addition, a few clinical studies that have looked at the effects of statins in people with established IBD have found that statins are associated with a decreased need for oral steroids and may be associated with improvements in clinical indices and disease and inflammatory markers. Basic science studies indicate that statins are associated with amelioration of disease in mouse models of IBD, may decrease mediators of inflammation, such as tumor necrosis factor-alpha, and may also suppress antigen presentation and T-cell proliferation, he noted.
Dr. Ungaro and his coauthors had no relevant financial disclosures.
WASHINGTON – A prescription for a statin was associated with about a 40% lower risk of new-onset inflammatory bowel disease in a study that evaluated data from a large U.S. health claims database over a 5-year period, Dr. Ryan Ungaro said at the annual Digestive Disease Week.
The protective effect was seen with different statins and was not associated with the intensity of statin treatment, said Dr. Ungaro, a gastroenterologist at Mount Sinai Hospital, New York.
He and his associates conducted a case-control study by using a national medical claims and pharmacy database, identifying 87,579 patients aged 18 and older with an ICD-9 code for a diagnosis of ulcerative colitis (UC) or Crohn’s disease (CD) from January 2008 through December 2012, and 189,526 controls (each case was matched with up to 10 controls, matched for age, gender, race, and state of residence). The median age of cases and controls was about 51 years, and about 41% were male. About 47% were diagnosed with CD, and about 44% were diagnosed with UC. A smaller group of patients who were new-onset cases were included who had at least 1 year with no IBD-related diagnostic code or prescription before the index diagnosis.
Statin use was associated with about a 40% reduced risk of new-onset IBD (odds ratio, 0.59), with similar trends for UC and CD, Dr. Ungaro reported. Separately, the risks of new-onset CD (OR, 0.55) and new-onset UC (OR, 0.62) associated with having a prescription for a statin were also significantly lower.
This association was maintained “regardless of which specific statin a patient was exposed to,” he noted. There was no significant difference in risk of IBD based on the intensity of statin treatment, according to American Heart Association guidelines for low-, moderate-, and high-intensity treatment.
Another finding was that the strongest protective effect was seen in older people, with an OR of 0.55 among those aged 60 years and older. There was no significant effect among those aged 18-30 years, but there were a limited number of statin prescriptions for younger patients, Dr. Ungaro noted.
Limitations of the study include the retrospective design, the inability to directly validate cases, and the reliance on a prescription as a surrogate for the patient actually taking the medication, he said.
Based on the results, “we think that future studies should confirm this protective effect, as well as continue to investigate statins in established IBD,” he concluded.
He referred to recent research demonstrating that statins have immunomodulatory effects “and may actually potentially be beneficial in established IBD.” In addition, a few clinical studies that have looked at the effects of statins in people with established IBD have found that statins are associated with a decreased need for oral steroids and may be associated with improvements in clinical indices and disease and inflammatory markers. Basic science studies indicate that statins are associated with amelioration of disease in mouse models of IBD, may decrease mediators of inflammation, such as tumor necrosis factor-alpha, and may also suppress antigen presentation and T-cell proliferation, he noted.
Dr. Ungaro and his coauthors had no relevant financial disclosures.
WASHINGTON – A prescription for a statin was associated with about a 40% lower risk of new-onset inflammatory bowel disease in a study that evaluated data from a large U.S. health claims database over a 5-year period, Dr. Ryan Ungaro said at the annual Digestive Disease Week.
The protective effect was seen with different statins and was not associated with the intensity of statin treatment, said Dr. Ungaro, a gastroenterologist at Mount Sinai Hospital, New York.
He and his associates conducted a case-control study by using a national medical claims and pharmacy database, identifying 87,579 patients aged 18 and older with an ICD-9 code for a diagnosis of ulcerative colitis (UC) or Crohn’s disease (CD) from January 2008 through December 2012, and 189,526 controls (each case was matched with up to 10 controls, matched for age, gender, race, and state of residence). The median age of cases and controls was about 51 years, and about 41% were male. About 47% were diagnosed with CD, and about 44% were diagnosed with UC. A smaller group of patients who were new-onset cases were included who had at least 1 year with no IBD-related diagnostic code or prescription before the index diagnosis.
Statin use was associated with about a 40% reduced risk of new-onset IBD (odds ratio, 0.59), with similar trends for UC and CD, Dr. Ungaro reported. Separately, the risks of new-onset CD (OR, 0.55) and new-onset UC (OR, 0.62) associated with having a prescription for a statin were also significantly lower.
This association was maintained “regardless of which specific statin a patient was exposed to,” he noted. There was no significant difference in risk of IBD based on the intensity of statin treatment, according to American Heart Association guidelines for low-, moderate-, and high-intensity treatment.
Another finding was that the strongest protective effect was seen in older people, with an OR of 0.55 among those aged 60 years and older. There was no significant effect among those aged 18-30 years, but there were a limited number of statin prescriptions for younger patients, Dr. Ungaro noted.
Limitations of the study include the retrospective design, the inability to directly validate cases, and the reliance on a prescription as a surrogate for the patient actually taking the medication, he said.
Based on the results, “we think that future studies should confirm this protective effect, as well as continue to investigate statins in established IBD,” he concluded.
He referred to recent research demonstrating that statins have immunomodulatory effects “and may actually potentially be beneficial in established IBD.” In addition, a few clinical studies that have looked at the effects of statins in people with established IBD have found that statins are associated with a decreased need for oral steroids and may be associated with improvements in clinical indices and disease and inflammatory markers. Basic science studies indicate that statins are associated with amelioration of disease in mouse models of IBD, may decrease mediators of inflammation, such as tumor necrosis factor-alpha, and may also suppress antigen presentation and T-cell proliferation, he noted.
Dr. Ungaro and his coauthors had no relevant financial disclosures.
AT DDW 2015
Key clinical point: A reduced risk of new onset inflammatory bowel disease (IBD) may be another benefit of statin therapy.
Major finding: A prescription for a statin was associated with about a 40% lower risk of new-onset IBD, an effect that was seen with different statins and only in older people, in a large case-control study.
Data source: The retrospective study evaluated the risk of new-onset Crohn’s disease (CD) and new-onset ulcerative colitis (UC), in about 87,500 patients with a diagnostic code for UC or CD, and controls using a US national medical claims and pharmacy database from 2008-2012.
Disclosures: Dr. Ungaro and his coauthors had no relevant disclosures.