User login
Extended maraviroc helps prevent graft-versus-host disease
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: The 180-day rates of grade 2-4 and grade 3-4 acute GVHD were 27% and 5%, respectively.
Data source: A phase II study of 37 patients.
Disclosures: Dr. Reshef reported receiving research funding from Pfizer.
Biomarker algorithm sharpens GVHD treatment outcomes prediction
ORLANDO – A biomarker algorithm was better than was clinical response at predicting outcomes after 1 week of systemic steroid treatment for graft-versus-host disease, according to findings from a multicenter study.
The findings have implications for early decision making regarding treatment course, Hannah Major-Monfried reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“The same GVHD algorithm that stratifies patients at day 7 after transplant, at [GVHD] diagnosis, also stratifies them after 1 week of steroid treatment into two groups with distinct risks for treatment failure, 6-month nonrelapse mortality, and overall survival,” she said.
The biomarker algorithm, which includes measures of ST2 and REG3-alpha, was previously shown to predict day-28 treatment response and 6-month non-relapse mortality (NRM) when applied at day 7 post transplant before the onset of GVHD and at the time of diagnosis, said Ms. Major-Monfried, a third-year medical student at Icahn School of Medicine at Mount Sinai, New York.
For the current analysis, levels of the biomarkers were measured after 1 week of treatment in 378 patients with acute GVHD from 11 centers in the Mount Sinai Acute GVHD International Consortium.
In a test cohort that included 236 of the patients, the measurements were used to generate a new predicted probability, or treatment score, for 6-month NRM, which had a value between 0 and 1.
Of the 236 patients, 93 (39%) were considered to have high posttreatment probability of NRM, and the remaining patients (61%) had low posttreatment probability of NRM, based on their treatment scores.
“High-risk patients were significantly less likely to respond to treatment than low-risk patients,” she said, noting that very similar results were found in a validation cohort of the remaining 142 patients, which had a similar proportion of high- and low-risk patients as did the test cohort.
The overall 6-month NRM for patients treated for GVHD was 27% in the test cohort. When the biomarker algorithm was used to separate the cohort into high- and low-risk groups, the NRM rate was found to be approximately 4 times higher among the high-risk patients than among the low-risk patients.
Overall survival was also significantly worse among high- vs. low-risk patients in both the test and validation cohorts.
“We can conclude that the increased NRM seen in the high-risk groups can explain these large differences in overall survival,” Ms. Major-Monfried said.
Because treatment decisions are often made after 1 week based on early clinical response, she and her colleagues also explored whether treatment response after 1 week could similarly predict NRM.
In the test cohort, early response – which includes complete or partial response in GVHD symptoms after 1 week of steroids – was observed in 48% of patients, while 52% were early nonresponders. NRM occurred in 17% of the early responders, compared with 36% of the nonresponders in the test cohort, and similar results were found in the validation cohort.
“These differences are independent of biomarkers,” she noted. “These are solely based on observed clinical response.”
When the biomarker algorithm was applied, prediction of NRM was more precise.
“We started with the early responders,” she explained. “When we used the biomarker algorithm to stratify these patients into high- and low-risk groups, we found that 28% of early responders were actually high risk, and that they experienced 38% NRM – significantly higher than the 8% observed in low-risk patients. Similar results were found again in the validation cohort.”
When the biomarker algorithm was used to stratify patients who were nonresponders at 7 days into high- and low-risk groups, 50% were found to be low risk, and those patients experienced 17% NRM, significantly lower than the 57% seen in the high-risk patients. Similar results were again seen in the validation cohort.
“Early responders with high posttreatment probability have high NRM, and perhaps should not be tapered despite the improvement of their clinical symptoms, while early nonresponders with low posttreatment probability have lower NRM and may not need treatment escalation,” Ms. Major-Monfried said.
“In data not shown, many of these patients are actually what we could call ‘slow responders’ who ultimately fare well,” she noted.
Ms. Major-Monfried reported having no disclosures.
ORLANDO – A biomarker algorithm was better than was clinical response at predicting outcomes after 1 week of systemic steroid treatment for graft-versus-host disease, according to findings from a multicenter study.
The findings have implications for early decision making regarding treatment course, Hannah Major-Monfried reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“The same GVHD algorithm that stratifies patients at day 7 after transplant, at [GVHD] diagnosis, also stratifies them after 1 week of steroid treatment into two groups with distinct risks for treatment failure, 6-month nonrelapse mortality, and overall survival,” she said.
The biomarker algorithm, which includes measures of ST2 and REG3-alpha, was previously shown to predict day-28 treatment response and 6-month non-relapse mortality (NRM) when applied at day 7 post transplant before the onset of GVHD and at the time of diagnosis, said Ms. Major-Monfried, a third-year medical student at Icahn School of Medicine at Mount Sinai, New York.
For the current analysis, levels of the biomarkers were measured after 1 week of treatment in 378 patients with acute GVHD from 11 centers in the Mount Sinai Acute GVHD International Consortium.
In a test cohort that included 236 of the patients, the measurements were used to generate a new predicted probability, or treatment score, for 6-month NRM, which had a value between 0 and 1.
Of the 236 patients, 93 (39%) were considered to have high posttreatment probability of NRM, and the remaining patients (61%) had low posttreatment probability of NRM, based on their treatment scores.
“High-risk patients were significantly less likely to respond to treatment than low-risk patients,” she said, noting that very similar results were found in a validation cohort of the remaining 142 patients, which had a similar proportion of high- and low-risk patients as did the test cohort.
The overall 6-month NRM for patients treated for GVHD was 27% in the test cohort. When the biomarker algorithm was used to separate the cohort into high- and low-risk groups, the NRM rate was found to be approximately 4 times higher among the high-risk patients than among the low-risk patients.
Overall survival was also significantly worse among high- vs. low-risk patients in both the test and validation cohorts.
“We can conclude that the increased NRM seen in the high-risk groups can explain these large differences in overall survival,” Ms. Major-Monfried said.
Because treatment decisions are often made after 1 week based on early clinical response, she and her colleagues also explored whether treatment response after 1 week could similarly predict NRM.
In the test cohort, early response – which includes complete or partial response in GVHD symptoms after 1 week of steroids – was observed in 48% of patients, while 52% were early nonresponders. NRM occurred in 17% of the early responders, compared with 36% of the nonresponders in the test cohort, and similar results were found in the validation cohort.
“These differences are independent of biomarkers,” she noted. “These are solely based on observed clinical response.”
When the biomarker algorithm was applied, prediction of NRM was more precise.
“We started with the early responders,” she explained. “When we used the biomarker algorithm to stratify these patients into high- and low-risk groups, we found that 28% of early responders were actually high risk, and that they experienced 38% NRM – significantly higher than the 8% observed in low-risk patients. Similar results were found again in the validation cohort.”
When the biomarker algorithm was used to stratify patients who were nonresponders at 7 days into high- and low-risk groups, 50% were found to be low risk, and those patients experienced 17% NRM, significantly lower than the 57% seen in the high-risk patients. Similar results were again seen in the validation cohort.
“Early responders with high posttreatment probability have high NRM, and perhaps should not be tapered despite the improvement of their clinical symptoms, while early nonresponders with low posttreatment probability have lower NRM and may not need treatment escalation,” Ms. Major-Monfried said.
“In data not shown, many of these patients are actually what we could call ‘slow responders’ who ultimately fare well,” she noted.
Ms. Major-Monfried reported having no disclosures.
ORLANDO – A biomarker algorithm was better than was clinical response at predicting outcomes after 1 week of systemic steroid treatment for graft-versus-host disease, according to findings from a multicenter study.
The findings have implications for early decision making regarding treatment course, Hannah Major-Monfried reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“The same GVHD algorithm that stratifies patients at day 7 after transplant, at [GVHD] diagnosis, also stratifies them after 1 week of steroid treatment into two groups with distinct risks for treatment failure, 6-month nonrelapse mortality, and overall survival,” she said.
The biomarker algorithm, which includes measures of ST2 and REG3-alpha, was previously shown to predict day-28 treatment response and 6-month non-relapse mortality (NRM) when applied at day 7 post transplant before the onset of GVHD and at the time of diagnosis, said Ms. Major-Monfried, a third-year medical student at Icahn School of Medicine at Mount Sinai, New York.
For the current analysis, levels of the biomarkers were measured after 1 week of treatment in 378 patients with acute GVHD from 11 centers in the Mount Sinai Acute GVHD International Consortium.
In a test cohort that included 236 of the patients, the measurements were used to generate a new predicted probability, or treatment score, for 6-month NRM, which had a value between 0 and 1.
Of the 236 patients, 93 (39%) were considered to have high posttreatment probability of NRM, and the remaining patients (61%) had low posttreatment probability of NRM, based on their treatment scores.
“High-risk patients were significantly less likely to respond to treatment than low-risk patients,” she said, noting that very similar results were found in a validation cohort of the remaining 142 patients, which had a similar proportion of high- and low-risk patients as did the test cohort.
The overall 6-month NRM for patients treated for GVHD was 27% in the test cohort. When the biomarker algorithm was used to separate the cohort into high- and low-risk groups, the NRM rate was found to be approximately 4 times higher among the high-risk patients than among the low-risk patients.
Overall survival was also significantly worse among high- vs. low-risk patients in both the test and validation cohorts.
“We can conclude that the increased NRM seen in the high-risk groups can explain these large differences in overall survival,” Ms. Major-Monfried said.
Because treatment decisions are often made after 1 week based on early clinical response, she and her colleagues also explored whether treatment response after 1 week could similarly predict NRM.
In the test cohort, early response – which includes complete or partial response in GVHD symptoms after 1 week of steroids – was observed in 48% of patients, while 52% were early nonresponders. NRM occurred in 17% of the early responders, compared with 36% of the nonresponders in the test cohort, and similar results were found in the validation cohort.
“These differences are independent of biomarkers,” she noted. “These are solely based on observed clinical response.”
When the biomarker algorithm was applied, prediction of NRM was more precise.
“We started with the early responders,” she explained. “When we used the biomarker algorithm to stratify these patients into high- and low-risk groups, we found that 28% of early responders were actually high risk, and that they experienced 38% NRM – significantly higher than the 8% observed in low-risk patients. Similar results were found again in the validation cohort.”
When the biomarker algorithm was used to stratify patients who were nonresponders at 7 days into high- and low-risk groups, 50% were found to be low risk, and those patients experienced 17% NRM, significantly lower than the 57% seen in the high-risk patients. Similar results were again seen in the validation cohort.
“Early responders with high posttreatment probability have high NRM, and perhaps should not be tapered despite the improvement of their clinical symptoms, while early nonresponders with low posttreatment probability have lower NRM and may not need treatment escalation,” Ms. Major-Monfried said.
“In data not shown, many of these patients are actually what we could call ‘slow responders’ who ultimately fare well,” she noted.
Ms. Major-Monfried reported having no disclosures.
Key clinical point:
Major finding: High- vs. low-risk patients, based on the biomarker algorithm, had a fourfold higher rate of nonrelapse mortality.
Data source: A multicenter study of 378 patients.
Disclosures: Ms. Major-Monfried reported having no disclosures.
Three factors linked to rhinovirus pneumonia in HCT patients
ORLANDO – For patients who have received hematopoietic cell transplants, a rhinovirus infection can become much more than a cold.
“It holds true that rhinovirus is just as likely to be associated with mortality as are other respiratory viruses” among HCT recipients, Alpana Waghmare, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In a new retrospective study, Dr. Waghmare and her coinvestigators found that the median time for a rhinovirus infection to progress from an upper to a lower respiratory tract infection was about 2 weeks among post-HCT patients.
Clinical and demographic risk factors for progression to lower respiratory tract infection included higher levels of steroid use (2 mg/kg per day or more) before developing the upper respiratory infection, a low white blood cell count, and a low monocyte count, said Dr. Waghmare, an infectious disease specialist and professor of pediatrics at the University of Washington, Seattle.
Of 3,445 HCT patients treated at the university center during the 6-year study, 732 patients (21%) were positive for human rhinovirus. Patients were classified as having upper respiratory infections if they had a PCR-positive nasal swab.
Patients were classed in one of three categories for potential lower respiratory infections: Proven lower respiratory infections were those detected by bronchoalveolar lavage or biopsy in patients who had a new radiographic abnormality. Probable lower respiratory infections were those with positive findings on bronchoalveolar lavage or biopsy but without radiographic changes. In possible lower respiratory infections, patients had upper tract virus detected on nasal swabs but did have a new radiographic abnormality.
Among the patients positive for human rhinovirus, 85% (665 patients) presented with upper respiratory infections and 15% (117 patients) with lower respiratory tract infections. By day 90, 16% of patients progressed from upper to lower respiratory tract infections. The median time to progression was 13.5 days. Progression to proven lower respiratory tract infection affected 5% of the HCT recipients.
In multivariable analytic models, a minimum white blood cell count of 1,000 or less was associated with a hazard ratio (HR) of 2.21 for progression to lower respiratory tract infection. A minimum monocyte count of 1,000 or less was associated with a HR of 3.66 for progression to lower respiratory tract infection.
The model also found a HR of 3.37 for lower respiratory tract infection with steroid use of 2 mg/kg per day or more. The patient’s conditioning regimen and donor type were not significantly associated with risk of progression to lower respiratory infection.
Viral copathogens, prior respiratory virus episodes, and the duration of time since HCT were not associated with risk of progress to lower respiratory infections. Neither were patient age, baseline lung function, and the year the transplant occurred.
“These data provide an initial framework for patient risk stratification and the development of rational prevention and treatment strategies in HCT recipients,” she said.
Dr. Waghmare reported receiving research funding from Aviragen, the maker of vapendavir, an investigational drug for human rhinovirus infection, and Gilead Sciences.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – For patients who have received hematopoietic cell transplants, a rhinovirus infection can become much more than a cold.
“It holds true that rhinovirus is just as likely to be associated with mortality as are other respiratory viruses” among HCT recipients, Alpana Waghmare, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In a new retrospective study, Dr. Waghmare and her coinvestigators found that the median time for a rhinovirus infection to progress from an upper to a lower respiratory tract infection was about 2 weeks among post-HCT patients.
Clinical and demographic risk factors for progression to lower respiratory tract infection included higher levels of steroid use (2 mg/kg per day or more) before developing the upper respiratory infection, a low white blood cell count, and a low monocyte count, said Dr. Waghmare, an infectious disease specialist and professor of pediatrics at the University of Washington, Seattle.
Of 3,445 HCT patients treated at the university center during the 6-year study, 732 patients (21%) were positive for human rhinovirus. Patients were classified as having upper respiratory infections if they had a PCR-positive nasal swab.
Patients were classed in one of three categories for potential lower respiratory infections: Proven lower respiratory infections were those detected by bronchoalveolar lavage or biopsy in patients who had a new radiographic abnormality. Probable lower respiratory infections were those with positive findings on bronchoalveolar lavage or biopsy but without radiographic changes. In possible lower respiratory infections, patients had upper tract virus detected on nasal swabs but did have a new radiographic abnormality.
Among the patients positive for human rhinovirus, 85% (665 patients) presented with upper respiratory infections and 15% (117 patients) with lower respiratory tract infections. By day 90, 16% of patients progressed from upper to lower respiratory tract infections. The median time to progression was 13.5 days. Progression to proven lower respiratory tract infection affected 5% of the HCT recipients.
In multivariable analytic models, a minimum white blood cell count of 1,000 or less was associated with a hazard ratio (HR) of 2.21 for progression to lower respiratory tract infection. A minimum monocyte count of 1,000 or less was associated with a HR of 3.66 for progression to lower respiratory tract infection.
The model also found a HR of 3.37 for lower respiratory tract infection with steroid use of 2 mg/kg per day or more. The patient’s conditioning regimen and donor type were not significantly associated with risk of progression to lower respiratory infection.
Viral copathogens, prior respiratory virus episodes, and the duration of time since HCT were not associated with risk of progress to lower respiratory infections. Neither were patient age, baseline lung function, and the year the transplant occurred.
“These data provide an initial framework for patient risk stratification and the development of rational prevention and treatment strategies in HCT recipients,” she said.
Dr. Waghmare reported receiving research funding from Aviragen, the maker of vapendavir, an investigational drug for human rhinovirus infection, and Gilead Sciences.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – For patients who have received hematopoietic cell transplants, a rhinovirus infection can become much more than a cold.
“It holds true that rhinovirus is just as likely to be associated with mortality as are other respiratory viruses” among HCT recipients, Alpana Waghmare, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In a new retrospective study, Dr. Waghmare and her coinvestigators found that the median time for a rhinovirus infection to progress from an upper to a lower respiratory tract infection was about 2 weeks among post-HCT patients.
Clinical and demographic risk factors for progression to lower respiratory tract infection included higher levels of steroid use (2 mg/kg per day or more) before developing the upper respiratory infection, a low white blood cell count, and a low monocyte count, said Dr. Waghmare, an infectious disease specialist and professor of pediatrics at the University of Washington, Seattle.
Of 3,445 HCT patients treated at the university center during the 6-year study, 732 patients (21%) were positive for human rhinovirus. Patients were classified as having upper respiratory infections if they had a PCR-positive nasal swab.
Patients were classed in one of three categories for potential lower respiratory infections: Proven lower respiratory infections were those detected by bronchoalveolar lavage or biopsy in patients who had a new radiographic abnormality. Probable lower respiratory infections were those with positive findings on bronchoalveolar lavage or biopsy but without radiographic changes. In possible lower respiratory infections, patients had upper tract virus detected on nasal swabs but did have a new radiographic abnormality.
Among the patients positive for human rhinovirus, 85% (665 patients) presented with upper respiratory infections and 15% (117 patients) with lower respiratory tract infections. By day 90, 16% of patients progressed from upper to lower respiratory tract infections. The median time to progression was 13.5 days. Progression to proven lower respiratory tract infection affected 5% of the HCT recipients.
In multivariable analytic models, a minimum white blood cell count of 1,000 or less was associated with a hazard ratio (HR) of 2.21 for progression to lower respiratory tract infection. A minimum monocyte count of 1,000 or less was associated with a HR of 3.66 for progression to lower respiratory tract infection.
The model also found a HR of 3.37 for lower respiratory tract infection with steroid use of 2 mg/kg per day or more. The patient’s conditioning regimen and donor type were not significantly associated with risk of progression to lower respiratory infection.
Viral copathogens, prior respiratory virus episodes, and the duration of time since HCT were not associated with risk of progress to lower respiratory infections. Neither were patient age, baseline lung function, and the year the transplant occurred.
“These data provide an initial framework for patient risk stratification and the development of rational prevention and treatment strategies in HCT recipients,” she said.
Dr. Waghmare reported receiving research funding from Aviragen, the maker of vapendavir, an investigational drug for human rhinovirus infection, and Gilead Sciences.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT THE BMT TANDEM MEETINGS
Key clinical point:
Major finding: Of 3,445 HCT patients, 732 patients (21%) were positive for human rhinovirus.
Data source: Single-center, 6-year retrospective study of 732 HCT patients with human rhinovirus infection.
Disclosures: Dr. Waghmare reported receiving research funding from Aviragen, the maker of vapendavir, an investigational drug for human rhinovirus infection, and Gilead Sciences.
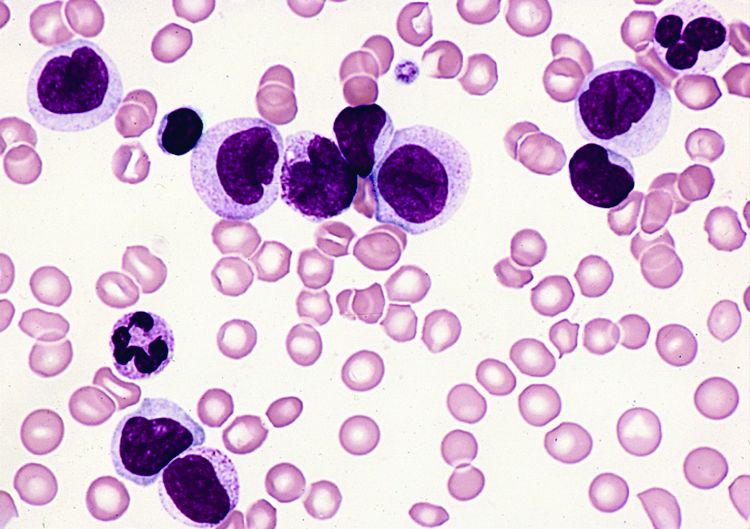
Off-the-shelf T cells an option for post-HCT viral infections
ORLANDO – Infusions of banked multivirus-specific T lymphocytes were associated with complete or partial responses in 93% of 42 patients who had undergone hematopoietic cell transplants and had drug-refractory viral illnesses. Further, these patients experienced minimal new or reactivated graft-versus-host disease (GVHD).
Viral infections cause nearly 40% of deaths after alternative donor hematopoietic cell transfer (HCT), Ifigeneia Tzannou, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation. Banked, “off-the-shelf” donor virus-resistant T cells can be an alternative to antiviral drugs, which are far from universally effective and may have serious side effects.
“Traditionally, we have generated T cells for infusion from the stem cell donor” by isolating and then stimulating and expanding the peripheral blood mononuclear cells for about 10 days ex vivo, said Dr. Tzannou. At that point, the clonal multivirus-resistant T cells can then be transferred to the recipient.
Donor-derived T cells have been used to prevent and treat Epstein-Barr virus (EBV), cytomegalovirus (CMV), adenovirus (AdV), BK virus (BKV), and human herpes virus 6 (HHV6) infections. The approach has been safe, reconstituting antiviral immunity and clearing disease effectively, with a 94% response rate reported in one recent study. However, said Dr. Tzannou, donor-derived virus-specific T cells (VSTs) have their limitations. Donors are increasingly younger and cord blood is being used more commonly, so there are growing numbers of donors who are seronegative for pathogenic viruses. In addition, the 10 days of production time and the additional week or 10 days required for release means that donor-derived VSTs can’t be urgently used.
The concept of banked third party VST therapy came about to address those limitations, said Dr. Tzannou of Baylor College of Medicine, Houston.
In a banked VST scenario, donor T cells with specific multiviral immunity are human leukocyte antigen (HLA) typed, expanded, and cryopreserved. A post-HCT patient with drug-refractory viral illness can receive T cells that are partially matched at HLA –A, HLA-B, or HLA-DR. Dr. Tzannou said that her group has now generated a bank of 59 VST lines to use in clinical testing of the third party approach.
In the study, Dr. Tzannou and her colleagues included both pediatric and adult post-allo-HCT patients with refractory EBV, CMV, AdV, BKV, and/or HHV6 infections. All had either failed a 14-day trial of antiviral therapy or could not tolerate antivirals. Patients could not be on more than 0.5 mg/kg per day of prednisone; they had to have an absolute neutrophil count above 500 per microliter and hemoglobin greater than 8 g/dL. Patients were excluded if they had acute GVHD of grade 2 or higher. There had to be a compatible VST line available that matched both the patient’s illness and HLA typing.
Patients initially received 20,000,000 VST cells per square meter of body surface area. If the investigators saw a partial response, patients could receive additional VST doses every 2 weeks.
Of the 42 patients infused, 23 received one infusion and 19 required two or more infusions. Seven study participants had two viral infections; 18 had CMV, 2 had EBV, 9 had AdV, 17 had BKV, and 3 had HHV6.
Dr. Tzannou and her colleagues tracked the virus-specific T cells and viral load for particular viruses. Virus-specific peripheral T cell counts also rose measurably and viral load plummeted within 2 weeks of VST infusions for most patients.
Overall, 93% of patients met the primary outcome measure of achieving complete or partial response; a partial response was defined as a 50% or better decrease in the viral load and/or clinical improvement.
All of the 17 BKV patients treated to date had tissue disease; 15 had hemorrhagic cystitis and 2 had nephritis. All responded to VSTs, and all of those with hemorrhagic cystitis had symptomatic improvement or resolution.
Overall, the safety profile for VST was good, said Dr. Tzannou. Four patients developed grade 1 acute cutaneous GVHD within 45 days of infusion; one of these developed de novo, but resolved with topical steroids. Another patient had a flare of gastrointestinal GVHD when immunosuppresion was being tapered. One more patient had a transient fever post infusion that resolved spontaneously, said Dr. Tzannou.
Next steps include a multicenter registration study, said Dr. Tzannou, who reports being a consultant for ViraCyte, which helped fund the study.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – Infusions of banked multivirus-specific T lymphocytes were associated with complete or partial responses in 93% of 42 patients who had undergone hematopoietic cell transplants and had drug-refractory viral illnesses. Further, these patients experienced minimal new or reactivated graft-versus-host disease (GVHD).
Viral infections cause nearly 40% of deaths after alternative donor hematopoietic cell transfer (HCT), Ifigeneia Tzannou, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation. Banked, “off-the-shelf” donor virus-resistant T cells can be an alternative to antiviral drugs, which are far from universally effective and may have serious side effects.
“Traditionally, we have generated T cells for infusion from the stem cell donor” by isolating and then stimulating and expanding the peripheral blood mononuclear cells for about 10 days ex vivo, said Dr. Tzannou. At that point, the clonal multivirus-resistant T cells can then be transferred to the recipient.
Donor-derived T cells have been used to prevent and treat Epstein-Barr virus (EBV), cytomegalovirus (CMV), adenovirus (AdV), BK virus (BKV), and human herpes virus 6 (HHV6) infections. The approach has been safe, reconstituting antiviral immunity and clearing disease effectively, with a 94% response rate reported in one recent study. However, said Dr. Tzannou, donor-derived virus-specific T cells (VSTs) have their limitations. Donors are increasingly younger and cord blood is being used more commonly, so there are growing numbers of donors who are seronegative for pathogenic viruses. In addition, the 10 days of production time and the additional week or 10 days required for release means that donor-derived VSTs can’t be urgently used.
The concept of banked third party VST therapy came about to address those limitations, said Dr. Tzannou of Baylor College of Medicine, Houston.
In a banked VST scenario, donor T cells with specific multiviral immunity are human leukocyte antigen (HLA) typed, expanded, and cryopreserved. A post-HCT patient with drug-refractory viral illness can receive T cells that are partially matched at HLA –A, HLA-B, or HLA-DR. Dr. Tzannou said that her group has now generated a bank of 59 VST lines to use in clinical testing of the third party approach.
In the study, Dr. Tzannou and her colleagues included both pediatric and adult post-allo-HCT patients with refractory EBV, CMV, AdV, BKV, and/or HHV6 infections. All had either failed a 14-day trial of antiviral therapy or could not tolerate antivirals. Patients could not be on more than 0.5 mg/kg per day of prednisone; they had to have an absolute neutrophil count above 500 per microliter and hemoglobin greater than 8 g/dL. Patients were excluded if they had acute GVHD of grade 2 or higher. There had to be a compatible VST line available that matched both the patient’s illness and HLA typing.
Patients initially received 20,000,000 VST cells per square meter of body surface area. If the investigators saw a partial response, patients could receive additional VST doses every 2 weeks.
Of the 42 patients infused, 23 received one infusion and 19 required two or more infusions. Seven study participants had two viral infections; 18 had CMV, 2 had EBV, 9 had AdV, 17 had BKV, and 3 had HHV6.
Dr. Tzannou and her colleagues tracked the virus-specific T cells and viral load for particular viruses. Virus-specific peripheral T cell counts also rose measurably and viral load plummeted within 2 weeks of VST infusions for most patients.
Overall, 93% of patients met the primary outcome measure of achieving complete or partial response; a partial response was defined as a 50% or better decrease in the viral load and/or clinical improvement.
All of the 17 BKV patients treated to date had tissue disease; 15 had hemorrhagic cystitis and 2 had nephritis. All responded to VSTs, and all of those with hemorrhagic cystitis had symptomatic improvement or resolution.
Overall, the safety profile for VST was good, said Dr. Tzannou. Four patients developed grade 1 acute cutaneous GVHD within 45 days of infusion; one of these developed de novo, but resolved with topical steroids. Another patient had a flare of gastrointestinal GVHD when immunosuppresion was being tapered. One more patient had a transient fever post infusion that resolved spontaneously, said Dr. Tzannou.
Next steps include a multicenter registration study, said Dr. Tzannou, who reports being a consultant for ViraCyte, which helped fund the study.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – Infusions of banked multivirus-specific T lymphocytes were associated with complete or partial responses in 93% of 42 patients who had undergone hematopoietic cell transplants and had drug-refractory viral illnesses. Further, these patients experienced minimal new or reactivated graft-versus-host disease (GVHD).
Viral infections cause nearly 40% of deaths after alternative donor hematopoietic cell transfer (HCT), Ifigeneia Tzannou, MD, said at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation. Banked, “off-the-shelf” donor virus-resistant T cells can be an alternative to antiviral drugs, which are far from universally effective and may have serious side effects.
“Traditionally, we have generated T cells for infusion from the stem cell donor” by isolating and then stimulating and expanding the peripheral blood mononuclear cells for about 10 days ex vivo, said Dr. Tzannou. At that point, the clonal multivirus-resistant T cells can then be transferred to the recipient.
Donor-derived T cells have been used to prevent and treat Epstein-Barr virus (EBV), cytomegalovirus (CMV), adenovirus (AdV), BK virus (BKV), and human herpes virus 6 (HHV6) infections. The approach has been safe, reconstituting antiviral immunity and clearing disease effectively, with a 94% response rate reported in one recent study. However, said Dr. Tzannou, donor-derived virus-specific T cells (VSTs) have their limitations. Donors are increasingly younger and cord blood is being used more commonly, so there are growing numbers of donors who are seronegative for pathogenic viruses. In addition, the 10 days of production time and the additional week or 10 days required for release means that donor-derived VSTs can’t be urgently used.
The concept of banked third party VST therapy came about to address those limitations, said Dr. Tzannou of Baylor College of Medicine, Houston.
In a banked VST scenario, donor T cells with specific multiviral immunity are human leukocyte antigen (HLA) typed, expanded, and cryopreserved. A post-HCT patient with drug-refractory viral illness can receive T cells that are partially matched at HLA –A, HLA-B, or HLA-DR. Dr. Tzannou said that her group has now generated a bank of 59 VST lines to use in clinical testing of the third party approach.
In the study, Dr. Tzannou and her colleagues included both pediatric and adult post-allo-HCT patients with refractory EBV, CMV, AdV, BKV, and/or HHV6 infections. All had either failed a 14-day trial of antiviral therapy or could not tolerate antivirals. Patients could not be on more than 0.5 mg/kg per day of prednisone; they had to have an absolute neutrophil count above 500 per microliter and hemoglobin greater than 8 g/dL. Patients were excluded if they had acute GVHD of grade 2 or higher. There had to be a compatible VST line available that matched both the patient’s illness and HLA typing.
Patients initially received 20,000,000 VST cells per square meter of body surface area. If the investigators saw a partial response, patients could receive additional VST doses every 2 weeks.
Of the 42 patients infused, 23 received one infusion and 19 required two or more infusions. Seven study participants had two viral infections; 18 had CMV, 2 had EBV, 9 had AdV, 17 had BKV, and 3 had HHV6.
Dr. Tzannou and her colleagues tracked the virus-specific T cells and viral load for particular viruses. Virus-specific peripheral T cell counts also rose measurably and viral load plummeted within 2 weeks of VST infusions for most patients.
Overall, 93% of patients met the primary outcome measure of achieving complete or partial response; a partial response was defined as a 50% or better decrease in the viral load and/or clinical improvement.
All of the 17 BKV patients treated to date had tissue disease; 15 had hemorrhagic cystitis and 2 had nephritis. All responded to VSTs, and all of those with hemorrhagic cystitis had symptomatic improvement or resolution.
Overall, the safety profile for VST was good, said Dr. Tzannou. Four patients developed grade 1 acute cutaneous GVHD within 45 days of infusion; one of these developed de novo, but resolved with topical steroids. Another patient had a flare of gastrointestinal GVHD when immunosuppresion was being tapered. One more patient had a transient fever post infusion that resolved spontaneously, said Dr. Tzannou.
Next steps include a multicenter registration study, said Dr. Tzannou, who reports being a consultant for ViraCyte, which helped fund the study.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: With banked multivirus-specific T cells, viral illnesses either improved or resolved in 93% of 42 patients.
Data source: Clinical trial of 42 postallogeneic hematopoietic cell transfer patients who had any of five viral illnesses and had either failed a 14-day trial of antiviral therapy or could not tolerate antivirals.
Disclosures: Dr. Tzannou is a consultant for Incyte, which partially funded the trial and is developing third-party VSTs.
Tocilizumab shows promise for GVHD prevention
ORLANDO – Tocilizumab plus standard immune suppression appears to drive down the risk for graft-versus-host disease (GVHD), according to results from a phase II study of 35 adults undergoing allogeneic stem cell transplants.
The effect was particularly pronounced for prevention of GVHD in the colon, William Drobyski, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The incidence rate of grades II-IV and III-IV acute GVHD was 12% at day 100 in patients given standard prophylaxis of tacrolimus/methotrexate (Tac/MTX) and 3% in patients given Tac/MTX plus 8 mg/kg of tocilizumab (Toc, capped at 800 mg), said Dr. Drobyski of the Medical College of Wisconsin, Milwaukee.
To provide further context to the results, Dr. Drobyski and his colleagues performed a matched case-control analysis using contemporary controls in the Center for International Blood & Marrow Transplant Research from 2000 to 2014. The same eligibility criteria used for the trial were applied to the matched controls except for the use of Tac/MTX as GVHD prophylaxis. Patients were otherwise matched based on age, performance score, disease, and donor type.
The incidence of grades II-IV acute GVHD at day 100 was significantly lower in the Toc/Tac/MTX group than in the Tac/MTX control population (12% vs. 41%). The incidence of grades III-IV acute GVHD was slightly lower with tocilizumab, but the difference between the groups was not statistically significant, Dr. Drobyski said.
The probability of grade II-IV acute GVHD–free survival, which was the primary endpoint of the study, was significantly higher in the Toc/Tac/MTX group (79% vs 52%), he said.
Five patients developed grade 2 acute GVHD of the skin or upper GI tract, and one patient died of grade 4 acute GVHD of the skin in the first 100 days. Notably, there were no cases of acute GVHD of the lower GI tract during that time, although two cases did occur between days 130 and 180, he said.
“There was no difference in transplant-related mortality, relapse, disease-free survival, or overall survival,” he said, adding that preliminary data suggest there were no differences in chronic GVHD between the groups.
Causes of death also were similar between the two cohorts with respect to disease- and transplant-related complications.
Patients in the tocilizumab study were enrolled between January 2015 and June 2016; the median age was 66 years. Diseases represented in the cohort included de novo acute myeloid leukemia (13 patients), AML (6 patients), chronic myelomonocytic leukemia (6 patients), acute lymphoblastic leukemia (4 patients), myelodysplastic syndrome (3 patients), and T-cell lymphoma, chronic myeloid leukemia, and NK/T cell lymphoma (in 1 patient each). Most patients were classified as high risk (9 patients) or intermediate risk (22 patients) by the disease risk index.
Conditioning was entirely busulfan based. Myeloablative conditioning was with busulfan and cyclophosphamide (Cytoxan) in 5 patients, or fludarabine and 4 days of busulfan in 10 patients, and reduced-intensity conditioning was with fludarabine and 2 days of busulfan in 18 patients. Transplants were with either HLA-matched related or unrelated donor grafts. Most patients (29 of 35) received peripheral stem cell grafts.
Tocilizumab, an interleuken-6 receptor blocker that is approved for treatment of rheumatoid arthritis, was administered after completion of conditioning and on the day prior to stem cell infusion.
In a pilot clinical trial of tocilizumab for the treatment of steroid-resistant acute GVHD in patients who had primarily had lower GI tract disease, “we were able to demonstrate responses in a majority of these patients,” Dr. Drobyski said, noting that a recent study presented at the 2016 annual meeting of the American Society of Hematology also showed efficacy in the treatment of lower tract GI GVHD, “providing evidence that tocilizumab had activity in acute GVHD, and perhaps in the treatment of steroid-refractory lower GI GVHD.”
Elevated IL-6 levels in the peripheral blood are correlated with an increased incidence and severity of GVHD; administration of an anti-IL-6 receptor antibody has been shown in preclinical studies to protect mice from lethal GVHD. The current open-label study was performed to “try to advance this concept” by assessing whether inhibition of IL-6 signaling could also prevent acute GVHD.
The findings confirm those of a 2014 study by Kennedy et al. in Lancet Oncology (2014;15:1451-9), and imply that tocilizumab warrants a randomized trial as prophylaxis for acute GVHD, he concluded.
Dr. Drobyski reported having no disclosures.
ORLANDO – Tocilizumab plus standard immune suppression appears to drive down the risk for graft-versus-host disease (GVHD), according to results from a phase II study of 35 adults undergoing allogeneic stem cell transplants.
The effect was particularly pronounced for prevention of GVHD in the colon, William Drobyski, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The incidence rate of grades II-IV and III-IV acute GVHD was 12% at day 100 in patients given standard prophylaxis of tacrolimus/methotrexate (Tac/MTX) and 3% in patients given Tac/MTX plus 8 mg/kg of tocilizumab (Toc, capped at 800 mg), said Dr. Drobyski of the Medical College of Wisconsin, Milwaukee.
To provide further context to the results, Dr. Drobyski and his colleagues performed a matched case-control analysis using contemporary controls in the Center for International Blood & Marrow Transplant Research from 2000 to 2014. The same eligibility criteria used for the trial were applied to the matched controls except for the use of Tac/MTX as GVHD prophylaxis. Patients were otherwise matched based on age, performance score, disease, and donor type.
The incidence of grades II-IV acute GVHD at day 100 was significantly lower in the Toc/Tac/MTX group than in the Tac/MTX control population (12% vs. 41%). The incidence of grades III-IV acute GVHD was slightly lower with tocilizumab, but the difference between the groups was not statistically significant, Dr. Drobyski said.
The probability of grade II-IV acute GVHD–free survival, which was the primary endpoint of the study, was significantly higher in the Toc/Tac/MTX group (79% vs 52%), he said.
Five patients developed grade 2 acute GVHD of the skin or upper GI tract, and one patient died of grade 4 acute GVHD of the skin in the first 100 days. Notably, there were no cases of acute GVHD of the lower GI tract during that time, although two cases did occur between days 130 and 180, he said.
“There was no difference in transplant-related mortality, relapse, disease-free survival, or overall survival,” he said, adding that preliminary data suggest there were no differences in chronic GVHD between the groups.
Causes of death also were similar between the two cohorts with respect to disease- and transplant-related complications.
Patients in the tocilizumab study were enrolled between January 2015 and June 2016; the median age was 66 years. Diseases represented in the cohort included de novo acute myeloid leukemia (13 patients), AML (6 patients), chronic myelomonocytic leukemia (6 patients), acute lymphoblastic leukemia (4 patients), myelodysplastic syndrome (3 patients), and T-cell lymphoma, chronic myeloid leukemia, and NK/T cell lymphoma (in 1 patient each). Most patients were classified as high risk (9 patients) or intermediate risk (22 patients) by the disease risk index.
Conditioning was entirely busulfan based. Myeloablative conditioning was with busulfan and cyclophosphamide (Cytoxan) in 5 patients, or fludarabine and 4 days of busulfan in 10 patients, and reduced-intensity conditioning was with fludarabine and 2 days of busulfan in 18 patients. Transplants were with either HLA-matched related or unrelated donor grafts. Most patients (29 of 35) received peripheral stem cell grafts.
Tocilizumab, an interleuken-6 receptor blocker that is approved for treatment of rheumatoid arthritis, was administered after completion of conditioning and on the day prior to stem cell infusion.
In a pilot clinical trial of tocilizumab for the treatment of steroid-resistant acute GVHD in patients who had primarily had lower GI tract disease, “we were able to demonstrate responses in a majority of these patients,” Dr. Drobyski said, noting that a recent study presented at the 2016 annual meeting of the American Society of Hematology also showed efficacy in the treatment of lower tract GI GVHD, “providing evidence that tocilizumab had activity in acute GVHD, and perhaps in the treatment of steroid-refractory lower GI GVHD.”
Elevated IL-6 levels in the peripheral blood are correlated with an increased incidence and severity of GVHD; administration of an anti-IL-6 receptor antibody has been shown in preclinical studies to protect mice from lethal GVHD. The current open-label study was performed to “try to advance this concept” by assessing whether inhibition of IL-6 signaling could also prevent acute GVHD.
The findings confirm those of a 2014 study by Kennedy et al. in Lancet Oncology (2014;15:1451-9), and imply that tocilizumab warrants a randomized trial as prophylaxis for acute GVHD, he concluded.
Dr. Drobyski reported having no disclosures.
ORLANDO – Tocilizumab plus standard immune suppression appears to drive down the risk for graft-versus-host disease (GVHD), according to results from a phase II study of 35 adults undergoing allogeneic stem cell transplants.
The effect was particularly pronounced for prevention of GVHD in the colon, William Drobyski, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The incidence rate of grades II-IV and III-IV acute GVHD was 12% at day 100 in patients given standard prophylaxis of tacrolimus/methotrexate (Tac/MTX) and 3% in patients given Tac/MTX plus 8 mg/kg of tocilizumab (Toc, capped at 800 mg), said Dr. Drobyski of the Medical College of Wisconsin, Milwaukee.
To provide further context to the results, Dr. Drobyski and his colleagues performed a matched case-control analysis using contemporary controls in the Center for International Blood & Marrow Transplant Research from 2000 to 2014. The same eligibility criteria used for the trial were applied to the matched controls except for the use of Tac/MTX as GVHD prophylaxis. Patients were otherwise matched based on age, performance score, disease, and donor type.
The incidence of grades II-IV acute GVHD at day 100 was significantly lower in the Toc/Tac/MTX group than in the Tac/MTX control population (12% vs. 41%). The incidence of grades III-IV acute GVHD was slightly lower with tocilizumab, but the difference between the groups was not statistically significant, Dr. Drobyski said.
The probability of grade II-IV acute GVHD–free survival, which was the primary endpoint of the study, was significantly higher in the Toc/Tac/MTX group (79% vs 52%), he said.
Five patients developed grade 2 acute GVHD of the skin or upper GI tract, and one patient died of grade 4 acute GVHD of the skin in the first 100 days. Notably, there were no cases of acute GVHD of the lower GI tract during that time, although two cases did occur between days 130 and 180, he said.
“There was no difference in transplant-related mortality, relapse, disease-free survival, or overall survival,” he said, adding that preliminary data suggest there were no differences in chronic GVHD between the groups.
Causes of death also were similar between the two cohorts with respect to disease- and transplant-related complications.
Patients in the tocilizumab study were enrolled between January 2015 and June 2016; the median age was 66 years. Diseases represented in the cohort included de novo acute myeloid leukemia (13 patients), AML (6 patients), chronic myelomonocytic leukemia (6 patients), acute lymphoblastic leukemia (4 patients), myelodysplastic syndrome (3 patients), and T-cell lymphoma, chronic myeloid leukemia, and NK/T cell lymphoma (in 1 patient each). Most patients were classified as high risk (9 patients) or intermediate risk (22 patients) by the disease risk index.
Conditioning was entirely busulfan based. Myeloablative conditioning was with busulfan and cyclophosphamide (Cytoxan) in 5 patients, or fludarabine and 4 days of busulfan in 10 patients, and reduced-intensity conditioning was with fludarabine and 2 days of busulfan in 18 patients. Transplants were with either HLA-matched related or unrelated donor grafts. Most patients (29 of 35) received peripheral stem cell grafts.
Tocilizumab, an interleuken-6 receptor blocker that is approved for treatment of rheumatoid arthritis, was administered after completion of conditioning and on the day prior to stem cell infusion.
In a pilot clinical trial of tocilizumab for the treatment of steroid-resistant acute GVHD in patients who had primarily had lower GI tract disease, “we were able to demonstrate responses in a majority of these patients,” Dr. Drobyski said, noting that a recent study presented at the 2016 annual meeting of the American Society of Hematology also showed efficacy in the treatment of lower tract GI GVHD, “providing evidence that tocilizumab had activity in acute GVHD, and perhaps in the treatment of steroid-refractory lower GI GVHD.”
Elevated IL-6 levels in the peripheral blood are correlated with an increased incidence and severity of GVHD; administration of an anti-IL-6 receptor antibody has been shown in preclinical studies to protect mice from lethal GVHD. The current open-label study was performed to “try to advance this concept” by assessing whether inhibition of IL-6 signaling could also prevent acute GVHD.
The findings confirm those of a 2014 study by Kennedy et al. in Lancet Oncology (2014;15:1451-9), and imply that tocilizumab warrants a randomized trial as prophylaxis for acute GVHD, he concluded.
Dr. Drobyski reported having no disclosures.
Key clinical point:
Major finding: The probability of grade II-IV acute GVHD-free survival was 79% vs. 52% in the tocilizumab group vs. age-matched controls.
Data source: An open-label phase II study of 35 patients.
Disclosures: Dr. Drobyski reported having no disclosures.
Auto-HCT patients run high risks for myeloid neoplasms
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT THE BMT TANDEM MEETINGS
Key clinical point:
Major finding: The 10-year cumulative risk for auto-HCT patients with Hodgkin or non-Hodgkin lymphoma or multiple myeloma was as high at 6%.
Data source: Review of 9,108 patients from an international transplant database.
Disclosures: Dr. Hashmi reported no conflicts of interest.
MRD predicts outcome of HSCT in ALL, study suggests
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
ORLANDO, FL—Minimal residual disease (MRD) measurements before and after hematopoietic stem cell transplant (HSCT) can help predict outcomes in patients with childhood acute lymphoblastic leukemia (ALL), according to researchers.
Their work also suggests several other factors can be used to predict event-free survival (EFS) in this patient population, and the team developed risk scores incorporating these factors.
Michael A. Pulsipher, MD, of Children’s Hospital Los Angeles in California, presented this work as one of the “Best Abstracts” at the 2017 BMT Tandem Meetings (abstract 4*).
“The new risk scores that we were able to develop very nicely predict outcomes post-transplant and can guide study planning,” Dr Pulsipher said.
“MRD pre-transplant was a very powerful predictor of outcome, and MRD post-transplant highlights individual patients at risk.”
For this study, Dr Pulsipher and his colleagues retrospectively analyzed 747 patients treated in Europe, North America, and Australia. The patients received transplants between September 1999 and May 2015.
Most patients had pre-B ALL (78%, n=586), 19% (n=145) had T-cell ALL, 2% had “other” ALLs (n=8) or no data on ALL type (n=8). Sixty-two percent (n=466) were male.
Nearly half of patients were between the ages of 2 and 10 (49%, n=365), 47% (n=351) were older than 10, and 4% (n=31) were younger than 2.
Transplant details
Patients received grafts from matched unrelated donors (42%, n=314), matched sibling donors (30%, n=227), mismatched donors (10%, n=75), and cord blood from unrelated donors (17%, n=128). There was no data on donor type for 3 patients.
Most patients received bone marrow transplants (61%, n=458), 20% (n=147) received cord blood, and 18% (n=131) received peripheral blood stem cells. Eight patients received “other” types of transplants, and 3 patients had no data on stem cell source.
More than half of the patients (55%, n=410) were in their second complete remission (CR) at transplant. Thirty-seven percent were in their first CR (n=275), 7% were in their third or greater CR (n=53), and 1% were not in remission (n=7). Two patients had no data on remission status.
MRD
MRD was assessed before HSCT as well as after—on or near days 30, 60, 90, 180, 365, and beyond.
There were 4 MRD categories:
- MRD negative: No signal
- MRD low: >0 to <10-4 (<0.01%)
- MRD high: ≥10-4 to <10-3 (0.01 to 0.1%)
- MRD very high: ≥10-3 to <10-2 (>0.1%).
Dr Pulsipher noted that, when analyzing MRD pre-HSCT or at 30 days after HSCT, the estimated 5-year EFS was similar for patients in the MRD-negative and MRD-low groups. However, as time went on (at days 90, 180, and 365), any detectable level of MRD was associated with a poor prognosis.
“And patients arriving at day 365 with no detectable MRD had an exceptional prognosis, with survival approaching 90%,” Dr Pulsipher said.
He also pointed out an interaction between acute graft-vs-host disease (aGVHD) and MRD post-HSCT. He and his colleagues observed better survival for MRD-positive patients with aGVHD (grade 1-2) than for MRD-positive patients without aGVHD.
Pre-HSCT risk score
Via an adjusted Cox regression analysis, the researchers identified several pre-transplant factors that predicted EFS at 18 months.
These included remission status, donor type, immunophenotype, and MRD. The researchers assigned points to each of these factors to create a risk score.
Compared to patients in first CR, the hazard ratio (HR) for patients in early second CR was 2.53, and the score was 3. For patients in third CR or greater, the HR was 1.95, and the score was 2.
Compared to patients with a matched sibling donor, the HR for patients with a mismatched donor was 1.41, and the score was 1. For patients who received cord blood from an unrelated donor, the HR was 1.48, and the score was 1.
Compared to patients with T-cell ALL, the HR for patients with pre-B ALL was 1.35, and the score was 1.
Compared to patients with MRD <10-4, the HR for patients with MRD ≥10-4 was 2.32, and the score was 2.
The probability of EFS at 18 months was 78% ± 2% for patients with 0 to 1 points, 54% ± 3% for those with 2 to 3 points, and 46% ± 5% for patients with 4 or more points.
Day 30 post-HSCT risk score
When considering patients at day 30 post-HSCT, factors that predicted 18-month EFS included remission status, donor type, immunophenotype, aGVHD status, and MRD.
The HR for patients in early second CR was 2.51, and the score was 3. For patients in third CR or greater, the HR was 2.09, and the score was 2.
The HR for patients with a mismatched donor was 1.75, and the score was 2. The HR for patients with pre-B ALL was 1.40, and the score was 1.
Compared to patients with grade 1-2 aGVHD, the HR was 2.02 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 3 aGVHD, the HR was 1.44, and the score was 1. For patients with grade 4 aGVHD, the HR was 7.12, and the score was 7.
The researchers evaluated MRD prior to HSCT and MRD at day 30, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 30, the HR was 2.29, and the score was 2.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 30, the HR was 3.17, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 30, the HR was 3.63, and the score was 4.
The probability of EFS at 18 months was 80% ± 2% for patients with 0 to 3 points, 54% ± 4% for those with 4 to 6 points, and 25% ± 6% for those with 7 or more points.
Day 90 post-HSCT risk score
When considering patients at day 90 post-HSCT, factors that predicted 18-month EFS included remission status, aGVHD status, and MRD.
For patients in early second CR, the HR was 2.81, and the score was 3. For those in third CR or greater, the HR was 1.85, and the score was 2.
Compared to patients with grade 1-2 aGVHD, the HR was 1.60 for patients with grade 0 aGVHD, and the score was 2. For patients with grade 4 aGVHD, the HR was 2.49, and the score was 2.
The researchers assessed MRD prior to HSCT and MRD at day 90, using a reference of MRD <10-4 at both time points. For patients with MRD <10-4 pre-HSCT and ≥10-4 at day 90, the HR was 6.03, and the score was 6.
For patients with MRD ≥10-4 pre-HSCT and <10-4 at day 90, the HR was 3.11, and the score was 3. For patients with MRD ≥10-4 pre-HSCT and at day 90, the HR was 4.59, and the score was 5.
The probability of EFS at 18 months was 83% ± 2% for patients with 0 to 2 points, 60% ± 4% for those with 3 to 5 points, and 17% ± 11 for those with 6 or more points. ![]()
*Information in the abstract differs from the presentation.
Study confirms increased adiposity in HSCT survivors
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
ORLANDO, FL—A recently conducted study confirms that survivors of hematopoietic stem cell transplant (HSCT) have increased body fat mass and lower lean mass compared to normal controls. And this is despite having a comparable body mass index (BMI).
Researchers say the abnormalities in adipokine levels—leptin and adiponectin—could provide insight into the mechanisms that contribute to the metabolic syndrome and cardiovascular complications that often develop in HSCT survivors.
Leptin and adiponectin are associated with obesity, insulin secretion, insulin resistance, endothelial function, vascular homeostasis, and atherosclerosis.
“So knowing that there is a dynamic interplay between obesity and insulin resistance and cytokine and adipokine profiles and, ultimately, insulin-resistance syndrome, we sought to evaluate, as part of a larger study, how treatment effects, including high-dose chemotherapy and radiation, alter cytokine profiles as well as obesity and body composition,” said Tyler G. Ketterl, MD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington.
Dr Ketterl presented the findings at the 2017 BMT Tandem Meetings as abstract 52.*
Study design
The research team compared 151 HSCT recipients who had survived more than 2 years after transplant with 92 sibling controls.
HSCT survivors were randomly recruited from 2 centers—Fred Hutchinson Cancer Research Center and University of Minnesota Masonic Children’s Hospital—and were younger than 21 years when diagnosed.
The researchers evaluated all participants for body composition, cardiovascular risk factors, and adipokines using anthropomorphic measurements, DXA scans for muscle and fat mass, and laboratory bloodwork.
The team stratified the HSCT survivors by the preparative regimen they had received—total body irradiation (TBI) alone, TBI plus cranial radiation (CRT), and chemotherapy alone.
Study population
Males comprised more than half the study population in each arm, 58% of HSCT survivors and 54% of siblings.
Nine percent and 8% in the HSCT and sibling arms, respectively, were non-white and/or Hispanic, and the mean current ages were 24.0 (range, 10-51) for HSCT survivors and 24.2 (range, 10-48) for siblings.
The survivors’ mean age at diagnosis was 9.1 years (range, 0.4–20.6), their mean age at transplant was 11.2 years (range, 0.6–32.6), and the mean time from transplant to study participation was 13.5 years (range, 2.6–32).
Most patients received a transplant for leukemia—54 (36%) for acute myeloid leukemia, 46 (31%) for acute lymphoblastic leukemia, and 15 (10%) for chronic myeloid leukemia. Thirteen (9%) received transplants for myelodysplastic syndromes, 12 (8%) for Hodgkin lymphoma, and 10 (6%) for non-Hodgkin lymphoma.
A little more than half had TBI (85, 56%) as the preparative regimen, 31 (21%) had TBI plus CRT, and 35 (23%) had chemotherapy only.
About three-quarters (116, 77%) had an allogeneic transplant, and 35 (23%) had an autologous transplant.
Results
Overall, HSCT survivors had significantly lower adiponectin levels than siblings (P<0.001).
Survivors who received TBI with or without CRT had significantly lower adiponectin levels than siblings (P<0.001), while survivors who received chemotherapy alone did not (P=0.42).
Adiponectin is involved in insulin sensitization, hepatoprotective action, antiatherogenic action, protection against the development of diabetes, and regulation of lipid metabolism.
Overall, survivors had significantly higher leptin levels than siblings (P<0.001).
This held true regardless of conditioning regimen, although levels for patients who received chemotherapy only were not as significantly high (P=0.02) as for survivors who received TBI (P<0.001).
Leptin helps increase energy expenditure, decrease appetite and food uptake, modify insulin sensitivity on muscles and liver, prevent ectopic lipid deposition, and regulate immune function.
BMI adjusted for age, sex, and Tanner stage was not significantly different between survivors and siblings, but percent fat mass was significantly higher across all conditioning regimens for survivors compared to siblings (P<0.001).
“And this goes along with previous data,” Dr Ketterl said, “that shows sarcopenic obesity is common amongst transplant survivors.”
The researchers believe these significant differences may provide insight into the underlying risk of developing metabolic syndrome and cardiovascular complications in transplant survivors. ![]()
*Some details in the abstract differ from the presentation.
Post-transplant drug combo eyed for high-risk AML
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
ORLANDO – Azacitadine and valproic acid can be safely coadministered as maintenance therapy after allogeneic stem cell transplantation in patients with high-risk acute myelogenous leukemia (AML), according to interim findings from an investigator-initiated phase II study.
One-year relapse-free and overall survival rates were about 80%, and no significant toxicities were reported in 28 such patients who began the treatment at least 40 days after transplant and were treated for 4 months, Patrick A. Hagen, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
“As we all know, relapse after allogeneic transplant for AML is a huge and ongoing problem. It’s the primary cause of death following transplant, and unfortunately it really hasn’t decreased over the past couple decades,” Dr. Hagen said, adding that relapse is of increasing concern for biologically high-risk patients and is a “pretty ripe area for improved methodologies or approaches.” The decision to pursue maintenance therapy after transplant is complicated: It’s a good opportunity to improve outcomes, but there are many challenges, including problems with drug interactions and myelosuppression, he said.
The study was undertaken based in part on previously reported findings of synergism of a demethylating agent and a histone dacetylase inhibitor in patients with AML, he said.
The maintenance therapy included up to four 28-day cycles of azacitadine at 40 mg/m2 daily on days 1-5, along with oral valproic acid daily throughout the cycle at a 15-mg/kg dose adjusted to achieve a 100-mcg/mL trough level of bound valproic acid as tolerated. Nineteen patients completed all four cycles of treatment.
“The regimen was pretty well tolerated. The vast majority of the toxicities were grade I/II – 70%. The only grade-4 toxicities were cytopenia related and did not lead to a delay in treatment,” he said.
No patients developed acute graft-versus-host disease after therapy, although 11 (39%) developed chronic GVHD, which was extensive in 8, Dr. Hagen said.
Study participants were adults with high-risk AML with no grade 3-4 acute GVHD. All had adequate organ function after allogeneic stem cell transplantation (allo-SCT) performed 40-60 days prior to the start of maintenance therapy. Those with active or uncontrolled infections, low-risk AML in first relapse, neutrophil counts below 1,500, and platelets below 50,000 were excluded, he said.
The patients’ median age was 44 years, they had a median of two prior chemotherapy regimens, and their median Sorror Comorbidity Index was 2.5. Cytogenetics were mostly intermediate and adverse; only one patient had favorable cytogenetics.
Graft type was mixed, with most patients having matched unrelated donors. Conditioning regimens also were mixed, although they “skewed toward myeloablative,” he said. GVHD prophylaxis was standard for the institution and included tacrolimus and methotrexate.
The promising 1-year overall survival and relapse rate without significant dose-limiting toxicities warrants further evaluation in a phase III trial, Dr. Hagen concluded.
He reported having no disclosures.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: 1-year relapse-free survival and 1-year overall survival were about 80%.
Data source: An interim analysis of data from 28 patients in a phase II study.
Disclosures: Dr. Hagen reported having no disclosures.
Genetic variants linked to HSCT outcomes in ALL
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.” ![]()
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.” ![]()
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.” ![]()