User login
Flumazenil effective in refractory hypersomnolence
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
AT SLEEP 2016
Key clinical point: Flumazenil offers a new option for refractory hypersomnolence.
Major finding: Sixty-three percent of patients with highly refractory hypersomnolence derived symptomatic benefit from flumazenil, and 39% of treated patients remained on the drug at a mean 6.8 months of follow-up.
Data source: This was a retrospective chart review of 153 consecutive patients with severe hypersomnolence refractory to all standard therapies who were treated with sublingual or topical flumazenil.
Disclosures: The presenter reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
GERD and Sleep Disorders Often Go Hand in Glove
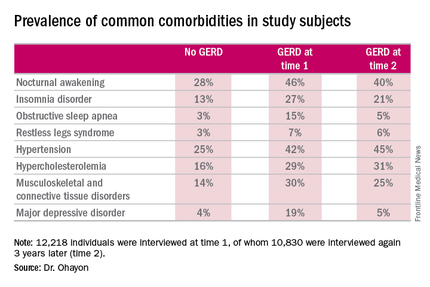
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
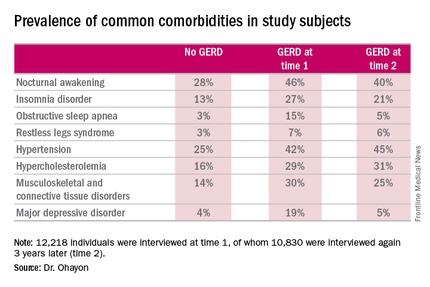
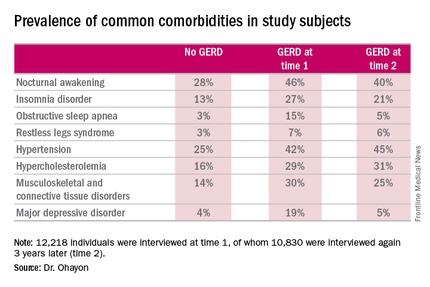
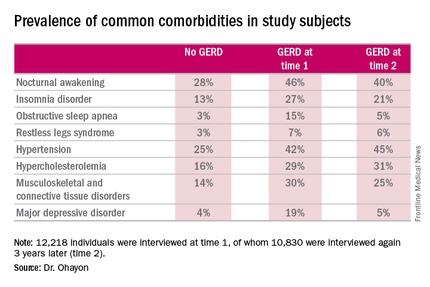
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
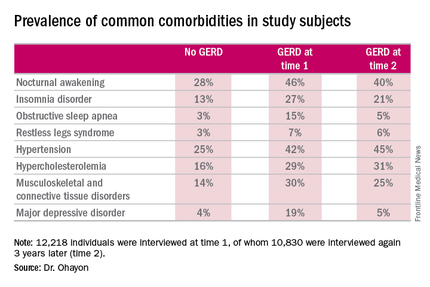
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
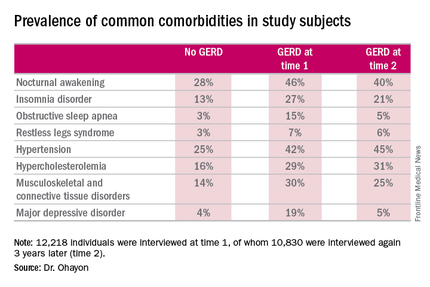
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
AT SLEEP 2016
GERD and sleep disorders often go hand in glove
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
AT SLEEP 2016
Key clinical point: Inquire about potentially treatable sleep disturbances in patients with GERD.
Major finding: Nocturnal awakenings were reported to be a problem in 28% of subjects with no history of gastroesophageal reflux disease, but in up to 46% of those with the digestive disease.
Data source: A longitudinal, population-based study of 12,218 nationally representative adults interviewed regarding the prevalence of GERD as well as comorbid sleep, medical, and psychiatric conditions.
Disclosures: The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. The presenter reported having no financial conflicts of interest.
Expert: Screen military spouses for sleep problems
DENVER – Sleep problems and their host of deleterious physical and psychosocial consequences are pervasive among the civilian female spouses of U.S. military service members, according to the first large study to examine the issue.
“Our findings suggest that if we’re trying to promote the resilience and adjustment of military spouses and their families – particularly in light of 14 years of protracted overseas combat, where many families are experiencing deployment – sleep might be a really important target,” Wendy M. Troxel, PhD, said while presenting the study results at the annual meeting of the Associated Professional Sleep Societies.
The study population consisted of a nationally representative group of 1,805 female civilian spouses of military service members. Forty-four percent reported short sleep duration, meaning 6 hours or less per night. Another 18% got 5 hours or less. The Centers for Disease Control and Prevention and the American Academy of Sleep Medicine recommend 7 hours or more, noted Dr. Troxel, senior behavioral and social scientist at RAND Corporation in Pittsburgh.
More than half (54%) of military spouses reported that their sleep problems contributed to daytime impairment, such as intolerance of their spouse or children, frequent crying, or suboptimal performance at work or chores. One-third of the spouses reported feeling daytime fatigue three or more times per week, and another 29% experienced daytime fatigue one or two days per week.
As has been observed in other studies, sleep problems in military spouses were associated with psychosocial impairment. In linear regression analyses, the spouses with poor sleep quality, daytime impairment, and/or fatigue had significantly more depressive symptoms on the Patient Health Questionnaire–8, lower marital satisfaction, and poor self-rated health. Women with shorter sleep duration had more depressive symptoms and poorer self-rated health, but not lower marital satisfaction.
The spouses of services members currently deployed in combat zones had significantly worse sleep quality as measured on the Pittsburgh Sleep Quality Index compared with spouses of previously or never-deployed service members. But for the other outcomes of interest – sleep duration, daytime impairment, and fatigue – there were no differences based upon deployment status.
“This shows that it’s not just about the stress of combat deployment, it’s also about the stresses of everyday military life. Military families experience a great deal of stress that could lead to sleep disturbances whether or not a service member has been deployed: frequent residential moves, very long and unpredictable work hours, demanding jobs, threatening training environments,” Dr. Troxel said. “I think we need to be thinking about sleep as an important health indicator of military families in general across the deployment cycle.”
The study results are a call to action, she added.
“These findings highlight the importance of targeted screening, prevention, and intervention methods for military spouses. And primary care is where most people present with sleep problems,” Dr. Troxel said.
There are formal screening instruments for sleep problems, but in her view they really need to be better validated for use in primary care before widespread adoption.
“Simply having providers ask three quick questions about their patients’ sleep and daytime function is a good, practical approach: How’s the quality of your sleep? How much do you sleep on average? Do you have enough energy during the daytime to get through your day-to-day functioning? That’s informative enough to indicate the utility of moving on to longer screening tools or to referral for evidence-based treatments,” she said.
Dr. Troxel noted successful intervention in sleep problems in civilian spouses is a priority for reasons beyond their personal well-being. “Civilian spouses are most often the primary caretakers for service members who return from war with either invisible mental health wounds or physical health wounds,” she said. “And we’re expecting to have need for a lot of caretakers.”
The RAND National Defense Research Institute, the Office of the Surgeon General, the U.S. Army, and the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury funded the study.
DENVER – Sleep problems and their host of deleterious physical and psychosocial consequences are pervasive among the civilian female spouses of U.S. military service members, according to the first large study to examine the issue.
“Our findings suggest that if we’re trying to promote the resilience and adjustment of military spouses and their families – particularly in light of 14 years of protracted overseas combat, where many families are experiencing deployment – sleep might be a really important target,” Wendy M. Troxel, PhD, said while presenting the study results at the annual meeting of the Associated Professional Sleep Societies.
The study population consisted of a nationally representative group of 1,805 female civilian spouses of military service members. Forty-four percent reported short sleep duration, meaning 6 hours or less per night. Another 18% got 5 hours or less. The Centers for Disease Control and Prevention and the American Academy of Sleep Medicine recommend 7 hours or more, noted Dr. Troxel, senior behavioral and social scientist at RAND Corporation in Pittsburgh.
More than half (54%) of military spouses reported that their sleep problems contributed to daytime impairment, such as intolerance of their spouse or children, frequent crying, or suboptimal performance at work or chores. One-third of the spouses reported feeling daytime fatigue three or more times per week, and another 29% experienced daytime fatigue one or two days per week.
As has been observed in other studies, sleep problems in military spouses were associated with psychosocial impairment. In linear regression analyses, the spouses with poor sleep quality, daytime impairment, and/or fatigue had significantly more depressive symptoms on the Patient Health Questionnaire–8, lower marital satisfaction, and poor self-rated health. Women with shorter sleep duration had more depressive symptoms and poorer self-rated health, but not lower marital satisfaction.
The spouses of services members currently deployed in combat zones had significantly worse sleep quality as measured on the Pittsburgh Sleep Quality Index compared with spouses of previously or never-deployed service members. But for the other outcomes of interest – sleep duration, daytime impairment, and fatigue – there were no differences based upon deployment status.
“This shows that it’s not just about the stress of combat deployment, it’s also about the stresses of everyday military life. Military families experience a great deal of stress that could lead to sleep disturbances whether or not a service member has been deployed: frequent residential moves, very long and unpredictable work hours, demanding jobs, threatening training environments,” Dr. Troxel said. “I think we need to be thinking about sleep as an important health indicator of military families in general across the deployment cycle.”
The study results are a call to action, she added.
“These findings highlight the importance of targeted screening, prevention, and intervention methods for military spouses. And primary care is where most people present with sleep problems,” Dr. Troxel said.
There are formal screening instruments for sleep problems, but in her view they really need to be better validated for use in primary care before widespread adoption.
“Simply having providers ask three quick questions about their patients’ sleep and daytime function is a good, practical approach: How’s the quality of your sleep? How much do you sleep on average? Do you have enough energy during the daytime to get through your day-to-day functioning? That’s informative enough to indicate the utility of moving on to longer screening tools or to referral for evidence-based treatments,” she said.
Dr. Troxel noted successful intervention in sleep problems in civilian spouses is a priority for reasons beyond their personal well-being. “Civilian spouses are most often the primary caretakers for service members who return from war with either invisible mental health wounds or physical health wounds,” she said. “And we’re expecting to have need for a lot of caretakers.”
The RAND National Defense Research Institute, the Office of the Surgeon General, the U.S. Army, and the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury funded the study.
DENVER – Sleep problems and their host of deleterious physical and psychosocial consequences are pervasive among the civilian female spouses of U.S. military service members, according to the first large study to examine the issue.
“Our findings suggest that if we’re trying to promote the resilience and adjustment of military spouses and their families – particularly in light of 14 years of protracted overseas combat, where many families are experiencing deployment – sleep might be a really important target,” Wendy M. Troxel, PhD, said while presenting the study results at the annual meeting of the Associated Professional Sleep Societies.
The study population consisted of a nationally representative group of 1,805 female civilian spouses of military service members. Forty-four percent reported short sleep duration, meaning 6 hours or less per night. Another 18% got 5 hours or less. The Centers for Disease Control and Prevention and the American Academy of Sleep Medicine recommend 7 hours or more, noted Dr. Troxel, senior behavioral and social scientist at RAND Corporation in Pittsburgh.
More than half (54%) of military spouses reported that their sleep problems contributed to daytime impairment, such as intolerance of their spouse or children, frequent crying, or suboptimal performance at work or chores. One-third of the spouses reported feeling daytime fatigue three or more times per week, and another 29% experienced daytime fatigue one or two days per week.
As has been observed in other studies, sleep problems in military spouses were associated with psychosocial impairment. In linear regression analyses, the spouses with poor sleep quality, daytime impairment, and/or fatigue had significantly more depressive symptoms on the Patient Health Questionnaire–8, lower marital satisfaction, and poor self-rated health. Women with shorter sleep duration had more depressive symptoms and poorer self-rated health, but not lower marital satisfaction.
The spouses of services members currently deployed in combat zones had significantly worse sleep quality as measured on the Pittsburgh Sleep Quality Index compared with spouses of previously or never-deployed service members. But for the other outcomes of interest – sleep duration, daytime impairment, and fatigue – there were no differences based upon deployment status.
“This shows that it’s not just about the stress of combat deployment, it’s also about the stresses of everyday military life. Military families experience a great deal of stress that could lead to sleep disturbances whether or not a service member has been deployed: frequent residential moves, very long and unpredictable work hours, demanding jobs, threatening training environments,” Dr. Troxel said. “I think we need to be thinking about sleep as an important health indicator of military families in general across the deployment cycle.”
The study results are a call to action, she added.
“These findings highlight the importance of targeted screening, prevention, and intervention methods for military spouses. And primary care is where most people present with sleep problems,” Dr. Troxel said.
There are formal screening instruments for sleep problems, but in her view they really need to be better validated for use in primary care before widespread adoption.
“Simply having providers ask three quick questions about their patients’ sleep and daytime function is a good, practical approach: How’s the quality of your sleep? How much do you sleep on average? Do you have enough energy during the daytime to get through your day-to-day functioning? That’s informative enough to indicate the utility of moving on to longer screening tools or to referral for evidence-based treatments,” she said.
Dr. Troxel noted successful intervention in sleep problems in civilian spouses is a priority for reasons beyond their personal well-being. “Civilian spouses are most often the primary caretakers for service members who return from war with either invisible mental health wounds or physical health wounds,” she said. “And we’re expecting to have need for a lot of caretakers.”
The RAND National Defense Research Institute, the Office of the Surgeon General, the U.S. Army, and the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury funded the study.
AT SLEEP 2016
Key clinical point: A significant portion of civilian female spouses of U.S. military members report short sleep duration and daytime impairment due to sleep problems.
Major finding: Fifty-four percent of a large group of civilian spouses of U.S. military service members reported daytime impairment due to sleep problems.
Data source: A cross-sectional study of the prevalence and consequences of sleep problems in 1,805 civilian female military spouses.
Disclosures: The RAND National Defense Research Institute, the Office of the Surgeon General, the U.S. Army, and the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury funded the study. Dr. Troxel is employed by RAND Corporation.
Sleep apnea in pregnancy linked to preterm birth
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
DENVER – Pregnant women with sleep apnea are more likely to have planned obstetric interventions, results of an Australian population-based cohort study suggest.
The study included all 636,227 in-hospital births during 2002-2012 in New South Wales, Australia’s most populous state. Maternal sleep apnea was also associated with increased rates of planned preterm birth, even though preterm birth is widely considered the greatest contributor to neonatal morbidity and mortality, Yu Sun Bin, PhD, said at the annual meeting of the Associated Professional Sleep Societies.
“Somewhere along the line, clinicians decided that the risks of preterm birth to the baby were outweighed by the risks to the mother of delivering at term,” said Dr. Bin of the University of Sydney.
She and her coinvestigators undertook this study because even though previous studies have linked maternal sleep apnea to increased risks of gestational diabetes and gestational hypertension, most of the prior studies were small, cross-sectional, and/or relied upon snoring as a proxy for sleep apnea, which many sleep specialists consider invalid.
The investigators compared maternal and infant outcomes for mothers with a documented diagnosis of sleep apnea – either central or obstructive – in the year before or during pregnancy with outcomes for mothers without that diagnosis.
There were 519 mothers with diagnosed sleep apnea, for a prevalence of 0.08%. That figure is low in light of other evidence, making it likely that the 635,708 women in the no-sleep-apnea group actually included a substantial number of mothers with undiagnosed sleep apnea. Thus, the investigators’ estimates of the adverse impacts of sleep apnea in pregnancy are “rather conservative,” according to Dr. Bin.
Australian women with sleep apnea were older and less healthy than mothers without sleep apnea were. They had higher baseline rates of obesity, preexisting diabetes, chronic hypertension, and were more likely to be smokers.
The incidence of pregnancy hypertension was 19.7% in the sleep apnea group and 8.7% in controls. In a multivariate regression analysis adjusted for potential confounders, the maternal sleep apnea group had a 40% greater risk of developing hypertension than did controls. However, contrary to previous smaller studies, they did not have a significantly increased rate of gestational diabetes.
Even after controlling for both pregnancy hypertension and gestational diabetes, the sleep apnea group still had a significant 15% increase in the relative likelihood of a planned delivery.
The rate of preterm birth at 36 weeks or earlier was 14.5% in the maternal sleep apnea group, compared with 6.9% in controls, for an adjusted 1.5-fold increased relative risk.
Perinatal death occurred in 1.9% of the sleep apnea group and 0.9% of controls; however, the resultant adjusted 1.73-fold increased risk didn’t attain statistical significance because of the small number of deaths in the study. Dr. Bin said she and her colleagues plan to further investigate this signal to learn whether it is real or an artifact of small numbers.
The incidence of 5-minute Apgar scores below 7 was 4.6% in the sleep apnea group, compared with 2.4% in controls, for an adjusted 1.6-fold increased risk. The rate of neonatal intensive care unit admission in the sleep apnea group was 27.9%, versus 16% in controls, for a 1.61-fold increased relative risk.
The NICU admission rate for preterm infants didn’t differ between the two groups. The difference occurred in term babies, whose NICU admission rate was 20.3% if they were in the sleep apnea group, but just 12.1% in the control group.
“This suggests that maternal sleep apnea is contributing to some condition in the baby that requires additional support,” Dr. Bin observed.
The nature of that condition, however, remains unclear, since all patient data available to the investigators was deidentified.
The incidence of small-for-gestational-age babies was similar in the sleep apnea and control groups. In contrast, the large-for-gestational-age rate was 15.2% in the sleep apnea group, compared with 9.1% in controls, for an adjusted 1.27-fold increased risk.
The two main limitations of the Australian study were the likely underdiagnosis of sleep apnea and the lack of any information on treatment of affected patients, according to Dr. Bin. A key unresolved question, she added, is whether interventions for maternal sleep apnea reduce the risks identified in the New South Wales study. She noted that one 16-patient randomized study of nasal continuous positive airway pressure suggests the answer is yes (Sleep Med. 2007 Dec;9:15-21).
The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
AT SLEEP 2016
Key clinical point: Maternal sleep apnea is associated with increased rates of obstetric intervention and preterm birth.
Major finding: The rate of preterm birth at 36 weeks or earlier was 14.5% in the group with maternal sleep apnea, compared with 6.9% in controls.
Data source: A population-based cohort study of 636,227 women who gave birth in a New South Wales, Australia, hospital during 2002-2012.
Disclosures: The Australian National Health and Medical Research Council supported the study. Dr. Bin reported having no financial conflicts.
Insomnia in Young Men Boosts Cardiovascular and Cerebrovascular Risk
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
AT SLEEP 2016
Insomnia in young men boosts cardiovascular and cerebrovascular risk
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
DENVER – Young to early middle-aged men with insomnia symptoms are at increased risk for cardiovascular and cerebrovascular events, according to an analysis from the landmark CARDIA study.
“We found that younger to mid-life men with difficulty initiating sleep or with more than one insomnia symptom were at greater risk for incident cardiovascular disease events. And despite the fact that women in general seemed to be more prone to report those sleep difficulties, those that did were not at increased risk,” Megan E. Petrov, PhD, reported at the annual meeting of the Associated Professional Sleep Societies.
It is well established that insomnia in older adults is associated with increased cardiovascular risk. For example, a meta-analysis of 13 prospective studies with more than 123,000 subjects concluded that insomnia was associated with a 45% increased risk of fatal and nonfatal cardiovascular events (Eur J Prev Cardiol. 2014 Jan;21[1]:57-64). But those studies typically involved older individuals, which makes cause and effect more difficult to determine because so many chronic conditions become more prevalent with advancing age, noted Dr. Petrov of Arizona State University in Phoenix.
“We wanted to see if insomnia is truly an early risk factor in the pathogenesis of cardiovascular disease and stroke,” she said.
To do so, she and her coinvestigators turned to the CARDIA database. CARDIA (the Coronary Artery Risk Development in Young Adults study), is a National Heart, Lung, and Blood Institute–sponsored prospective, epidemiologic study.
She reported on 2,950 non-Hispanic black or white participants aged 33-45 and free of any history of cardiovascular disease in 2000-2001, when they answered questions about insomnia symptoms. Difficulty in initiating sleep was reported by 16.3% of men and 20.7% of women. Difficulty maintaining sleep was a problem for 9.3% of men and 14.5% of women. And 20.6% of men and 20.1% of women reported frequent early morning awakening.
During a mean 11.5 years of prospective follow-up, 4.1% of men and 2.3% of women had a fatal or nonfatal MI, stroke, transient ischemic attack, heart failure, peripheral vascular disease, or hospitalization for an acute coronary syndrome.
In a multivariate logistic regression analysis fully adjusted for demographics, socioeconomic status, body mass index, blood pressure, diabetes, depression, health behaviors, medications, thyroid disease, and kidney problems, men who reported difficulty in getting to sleep had a 2.64-fold increased risk of one of these adverse outcomes. That was the only insomnia symptom associated with significantly increased risk. However, men but not women who reported having more than one insomnia symptom had a 39% increased risk of a cardiovascular event for each additional symptom.
Prior studies have shown that insomnia is associated with cardiac sympathetic hyperactivation. That observation suggests a plausible mechanism for increased cardiovascular and cerebrovascular risk, but it doesn’t explain why that risk was confined to young men in CARDIA. One possibility is that because of gender-related differences in perception, men tend to report having insomnia symptoms only when the insomnia is more severe, Dr. Petrov suggested.
The strengths of the CARDIA study are that all cardiovascular endpoints had to be physician certified, and the study includes a large black population. A study limitation is the relatively small number of cardiovascular events, as to be expected in a younger population. Thus, confirmation of the new findings in another large data set will be important, she noted.
As a next step in her research, Dr. Petrov said she plans to drill down in the CARDIA data to see if race modified the impact of insomnia symptoms on cardiovascular outcomes. Black participants reported all insomnia symptoms more frequently than did whites. For example, difficulty initiating sleep was reported by 25.7% of blacks, compared with just 13.5% of whites, and early morning awakening was twice as prevalent among the black participants.
Also, CARDIA participants provided self-reported sleep duration data. It will be illuminating to see if sleep duration had a modifying effect upon the insomnia/cardiovascular risk association observed in men, she said.
Dr. Petrov reported having no relevant financial conflicts.
AT SLEEP 2016
Key clinical point: Insomnia symptoms are associated with increased cardiovascular and cerebrovascular event rates in young to middle-aged men.
Major finding: Men aged 33-45 who reported frequent difficulty in falling asleep were at an adjusted 2.64-fold increased risk of a major cardiovascular or cerebrovascular event during subsequent follow-up.
Data source: The prospective, epidemiologic CARDIA study including 2,950 black or white subjects aged 33-45 at enrollment who were followed for a mean of 11.5 years.
Disclosures: The CARDIA study is supported by the National Institutes of Health. The presenter reported having no relevant financial conflicts.
Restless Sleep in 11-year-olds Predicts Earlier Substance Use
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
AT SLEEP 2016
Restless sleep in 11-year-olds predicts earlier substance use
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
DENVER – Poor sleep quality and shorter sleep duration in boys at age 11 years is associated with subsequent accelerated use and misuse of alcohol and cannabis during adolescence and emerging adulthood, Thomas B. Mike reported at the annual meeting of the Associated Professional Sleep Societies.
This association has been reported before in cross-sectional studies. But Mr. Mike presented new findings from the longitudinal prospective Pitt Mother and Child Project.
The study comprised 170 boys aged 11 years whose mothers filled out the Child Sleep Questionnaire, modified for pediatric use from the well known Pittsburgh Sleep Quality Index. At that time, the boys also were assessed for internalizing and externalizing behaviors, neighborhood dangerousness, and socioeconomic status – all of which are factors known to influence teen substance use.
When participants reached ages 20 and 22 years, they underwent detailed interviews including assessment via the validated Lifetime Drinking History and Lifetime Drug History questionnaires.
In a multivariate Cox regression analysis controlling for a history of child internalizing and externalizing problem behavior as well as socioeconomic factors, every hour of sleep duration less than 9.5 hours at age 11 years was associated with a 21% acceleration in the time to first use of alcohol and a 22% acceleration in first use of cannabis, reported Mr. Mike, a medical student at the University of Pittsburgh.
Moreover, every 1 point worse score for sleep quality on the Child Sleep Questionnaire, scored from 0 (best) to 21 (worst), was associated with a 9% acceleration in time to alcohol use and an 8% acceleration to cannabis use.
Subjects with poor sleep duration and quality as 11-year-olds by parental report also experienced intoxication at a younger age than did those who had been better sleepers at that age. And they reported more frequent use of alcohol and cannabis during adolescence.
In an interview, Mr. Mike, who is planning a career in pediatrics, said the study findings contain an important message for pediatricians and family physicians when they meet with the parents of young boys entering adolescence.
“Probably the biggest take-home message is, ‘sleep more, sleep better.’ We don’t have a lot of ways to intervene right now for kids who have poor sleep, but we know based on this and other studies that kids who don’t sleep enough are more likely to use drugs and more likely to engage in other risky behaviors. So any way the parents can intervene will help, perhaps by getting them to bed earlier or trying to get them on a more regular schedule. At a social policy level, having school start later would probably be the most effective measure, but that probably won’t happen for a very long time,” he said.
“The vast majority of people who end up addicted to drugs later in life started when they were kids, so any way we can reduce adolescent substance use should have a downstream effect, including a decreased total substance use burden,” Mr. Mike added.
Possible mechanisms for the observed longitudinal association between poor quality and duration of sleep at age 11 years and earlier and heavier use of alcohol and cannabis later in adolescence include attempted self-medication for sleep problems, reward regulation, and alterations in brain chemistry, making the boys more susceptible to using drugs later in life, perhaps because they obtain a bigger high than their peers do. The investigators plan to delve deeper into the role of self-regulation and mental health as possible mechanisms linking childhood sleep and later substance use, he said.
The Pitt Mother and Child Project is supported by the National Institutes of Health. Mr. Mike reported having no financial conflicts.
AT SLEEP 2016
Key clinical point: Boys with poor sleep quality and quantity start using alcohol and cannabis earlier as teens.
Major finding: Every hour less of sleep duration at age 11 years was associated with a 21% acceleration in time to first use of alcohol and a 22% acceleration in first use of cannabis.
Data source: An analysis from the Pitt Mother and Child Project of 170 boys with sleep data recorded at age 11 and lifetime alcohol and cannabis use recalled at ages 20 and 22.
Disclosures: The Pitt Mother and Child Project is supported by the National Institutes of Health. The presenter reported having no financial conflicts.
Upper airway stimulation for obstructive sleep apnea shows continued benefit at 42 months
DENVER – The surgically implanted Inspire system for controlled upper airway stimulation as therapy for moderate to severe obstructive sleep apnea demonstrated sustained benefit at 42 months of prospective follow-up in the STAR trial, Dr. Patrick J. Strollo Jr. reported at the annual meeting of the Associated Professional Sleep Societies.
STAR was the pivotal trial whose previously reported 12-month outcomes led to Food and Drug Administration clearance of the device. Dr. Strollo was first author of that paper (N Engl J Med. 2014 Jan 9;370:139-49). At SLEEP 2016, he presented patient- and partner-reported outcomes at 42 months. Bottom line: The device had continued safety and no loss in efficacy.
“So far it seems to be a useful option for people who frequently didn’t have an option. And the technology is improving and will only get better,” said Dr. Strollo, professor of medicine and clinical and translational science, director of the Sleep Medicine Center, and codirector of the Sleep Medicine Institute at the University of Pittsburgh.
The Inspire system consists of three parts implanted by an otolaryngologist in an outpatient procedure: a small impulse generator, a breathing sensor lead inserted in the intercostal muscle, and a stimulator lead attached to the distal branch of the 10th cranial nerve, the hypoglossal nerve controlling the tongue muscles.
The device is programmed to discharge at the end of expiration and continue through the inspiratory phase, causing the tongue to move forward and the retrolingual and retropalatal airways to open, he explained in an interview.
Upper airway stimulation is approved for commercial use in patients such as those enrolled in the STAR trial on the basis of pilot studies that identified most likely responders. The key selection criteria include moderate to severe obstructive sleep apnea as defined by an apnea-hypopnea index of 20-50, nonadherence to continuous positive airway pressure (CPAP), a body mass index of 32 kg/m2 or less, and absence of concentric collapse of the airway at the level of the palate during sedated endoscopy.
STAR included 126 participants who received the upper airway stimulation device. There have been two explants: one from septic arthritis, the other elective.
A total of 97 STAR participants had 42-month follow-up data available. Among the key findings were that:
• Mean scores on the Epworth Sleepiness Scale decreased from 11.6 at baseline to 7 at 12 months and 7.1 at 42 months.
• Scores on the Functional Outcomes of Sleep Questionnaire improved from 14.3 at baseline to 17.3 at 12 months and 17.5 at 42 months.
• The scores on both the Epworth Sleepiness Scale and Functional Outcomes of Sleep Questionnaire were abnormal at baseline and converted to normal range at both 12 and 42 months of follow-up.
• At baseline, 29% of the patients’ sleeping partners characterized the snoring as loud, 24% rated it ‘very intense,’ and 30% left the bedroom. At 32 months, 11% of partners called the snoring loud, 3% deemed it very intense, and only 4% left the room.
• At 42 months, 81% of patients reported using the device nightly. That’s consistent with the objective evidence of adherence Dr. Strollo and his coinvestigators obtained in a study of postmarketing device implants in which they found device usage averaged about 7 hours per night.
“That’s much better than we see with CPAP in patients who can tolerate that therapy,” Dr. Strollo observed.
The planned 5-year follow-up of STAR participants includes a full laboratory polysomnography study to obtain objective apnea-hypopnea index figures.
The other major development is the launch of a comprehensive registry of patients who receive a post-marketing commercial implant. Roughly 1,000 implants have been done worldwide to date, but now that the device is approved, that number will quickly grow. The registry should prove a rich source for research.
“The goal is to try to refine the selection criteria,” according to Dr. Strollo.
Given that only about 50% of patients with moderate to severe sleep apnea are able to tolerate CPAP long term, where does the Inspire system fit into today’s practice of sleep medicine?
“Upper airway stimulation is another tool, another option for patients,” he said. “In my practice, normally I’d let patients try positive pressure first. I want to make sure they’ve tried CPAP, and they’ve tried more advanced therapy like autotitrating bilevel positive airway pressure, which is more comfortable than CPAP. Bilevel positive airway pressure allows you to salvage a fair number of patients who can’t tolerate CPAP. And I also offer an oral appliance, although the robustness of an oral appliance is not great as apnea becomes more severe.”
The STAR trial is supported by Inspire Medical Systems. Dr. Strollo reported receiving a research grant from the company.
DENVER – The surgically implanted Inspire system for controlled upper airway stimulation as therapy for moderate to severe obstructive sleep apnea demonstrated sustained benefit at 42 months of prospective follow-up in the STAR trial, Dr. Patrick J. Strollo Jr. reported at the annual meeting of the Associated Professional Sleep Societies.
STAR was the pivotal trial whose previously reported 12-month outcomes led to Food and Drug Administration clearance of the device. Dr. Strollo was first author of that paper (N Engl J Med. 2014 Jan 9;370:139-49). At SLEEP 2016, he presented patient- and partner-reported outcomes at 42 months. Bottom line: The device had continued safety and no loss in efficacy.
“So far it seems to be a useful option for people who frequently didn’t have an option. And the technology is improving and will only get better,” said Dr. Strollo, professor of medicine and clinical and translational science, director of the Sleep Medicine Center, and codirector of the Sleep Medicine Institute at the University of Pittsburgh.
The Inspire system consists of three parts implanted by an otolaryngologist in an outpatient procedure: a small impulse generator, a breathing sensor lead inserted in the intercostal muscle, and a stimulator lead attached to the distal branch of the 10th cranial nerve, the hypoglossal nerve controlling the tongue muscles.
The device is programmed to discharge at the end of expiration and continue through the inspiratory phase, causing the tongue to move forward and the retrolingual and retropalatal airways to open, he explained in an interview.
Upper airway stimulation is approved for commercial use in patients such as those enrolled in the STAR trial on the basis of pilot studies that identified most likely responders. The key selection criteria include moderate to severe obstructive sleep apnea as defined by an apnea-hypopnea index of 20-50, nonadherence to continuous positive airway pressure (CPAP), a body mass index of 32 kg/m2 or less, and absence of concentric collapse of the airway at the level of the palate during sedated endoscopy.
STAR included 126 participants who received the upper airway stimulation device. There have been two explants: one from septic arthritis, the other elective.
A total of 97 STAR participants had 42-month follow-up data available. Among the key findings were that:
• Mean scores on the Epworth Sleepiness Scale decreased from 11.6 at baseline to 7 at 12 months and 7.1 at 42 months.
• Scores on the Functional Outcomes of Sleep Questionnaire improved from 14.3 at baseline to 17.3 at 12 months and 17.5 at 42 months.
• The scores on both the Epworth Sleepiness Scale and Functional Outcomes of Sleep Questionnaire were abnormal at baseline and converted to normal range at both 12 and 42 months of follow-up.
• At baseline, 29% of the patients’ sleeping partners characterized the snoring as loud, 24% rated it ‘very intense,’ and 30% left the bedroom. At 32 months, 11% of partners called the snoring loud, 3% deemed it very intense, and only 4% left the room.
• At 42 months, 81% of patients reported using the device nightly. That’s consistent with the objective evidence of adherence Dr. Strollo and his coinvestigators obtained in a study of postmarketing device implants in which they found device usage averaged about 7 hours per night.
“That’s much better than we see with CPAP in patients who can tolerate that therapy,” Dr. Strollo observed.
The planned 5-year follow-up of STAR participants includes a full laboratory polysomnography study to obtain objective apnea-hypopnea index figures.
The other major development is the launch of a comprehensive registry of patients who receive a post-marketing commercial implant. Roughly 1,000 implants have been done worldwide to date, but now that the device is approved, that number will quickly grow. The registry should prove a rich source for research.
“The goal is to try to refine the selection criteria,” according to Dr. Strollo.
Given that only about 50% of patients with moderate to severe sleep apnea are able to tolerate CPAP long term, where does the Inspire system fit into today’s practice of sleep medicine?
“Upper airway stimulation is another tool, another option for patients,” he said. “In my practice, normally I’d let patients try positive pressure first. I want to make sure they’ve tried CPAP, and they’ve tried more advanced therapy like autotitrating bilevel positive airway pressure, which is more comfortable than CPAP. Bilevel positive airway pressure allows you to salvage a fair number of patients who can’t tolerate CPAP. And I also offer an oral appliance, although the robustness of an oral appliance is not great as apnea becomes more severe.”
The STAR trial is supported by Inspire Medical Systems. Dr. Strollo reported receiving a research grant from the company.
DENVER – The surgically implanted Inspire system for controlled upper airway stimulation as therapy for moderate to severe obstructive sleep apnea demonstrated sustained benefit at 42 months of prospective follow-up in the STAR trial, Dr. Patrick J. Strollo Jr. reported at the annual meeting of the Associated Professional Sleep Societies.
STAR was the pivotal trial whose previously reported 12-month outcomes led to Food and Drug Administration clearance of the device. Dr. Strollo was first author of that paper (N Engl J Med. 2014 Jan 9;370:139-49). At SLEEP 2016, he presented patient- and partner-reported outcomes at 42 months. Bottom line: The device had continued safety and no loss in efficacy.
“So far it seems to be a useful option for people who frequently didn’t have an option. And the technology is improving and will only get better,” said Dr. Strollo, professor of medicine and clinical and translational science, director of the Sleep Medicine Center, and codirector of the Sleep Medicine Institute at the University of Pittsburgh.
The Inspire system consists of three parts implanted by an otolaryngologist in an outpatient procedure: a small impulse generator, a breathing sensor lead inserted in the intercostal muscle, and a stimulator lead attached to the distal branch of the 10th cranial nerve, the hypoglossal nerve controlling the tongue muscles.
The device is programmed to discharge at the end of expiration and continue through the inspiratory phase, causing the tongue to move forward and the retrolingual and retropalatal airways to open, he explained in an interview.
Upper airway stimulation is approved for commercial use in patients such as those enrolled in the STAR trial on the basis of pilot studies that identified most likely responders. The key selection criteria include moderate to severe obstructive sleep apnea as defined by an apnea-hypopnea index of 20-50, nonadherence to continuous positive airway pressure (CPAP), a body mass index of 32 kg/m2 or less, and absence of concentric collapse of the airway at the level of the palate during sedated endoscopy.
STAR included 126 participants who received the upper airway stimulation device. There have been two explants: one from septic arthritis, the other elective.
A total of 97 STAR participants had 42-month follow-up data available. Among the key findings were that:
• Mean scores on the Epworth Sleepiness Scale decreased from 11.6 at baseline to 7 at 12 months and 7.1 at 42 months.
• Scores on the Functional Outcomes of Sleep Questionnaire improved from 14.3 at baseline to 17.3 at 12 months and 17.5 at 42 months.
• The scores on both the Epworth Sleepiness Scale and Functional Outcomes of Sleep Questionnaire were abnormal at baseline and converted to normal range at both 12 and 42 months of follow-up.
• At baseline, 29% of the patients’ sleeping partners characterized the snoring as loud, 24% rated it ‘very intense,’ and 30% left the bedroom. At 32 months, 11% of partners called the snoring loud, 3% deemed it very intense, and only 4% left the room.
• At 42 months, 81% of patients reported using the device nightly. That’s consistent with the objective evidence of adherence Dr. Strollo and his coinvestigators obtained in a study of postmarketing device implants in which they found device usage averaged about 7 hours per night.
“That’s much better than we see with CPAP in patients who can tolerate that therapy,” Dr. Strollo observed.
The planned 5-year follow-up of STAR participants includes a full laboratory polysomnography study to obtain objective apnea-hypopnea index figures.
The other major development is the launch of a comprehensive registry of patients who receive a post-marketing commercial implant. Roughly 1,000 implants have been done worldwide to date, but now that the device is approved, that number will quickly grow. The registry should prove a rich source for research.
“The goal is to try to refine the selection criteria,” according to Dr. Strollo.
Given that only about 50% of patients with moderate to severe sleep apnea are able to tolerate CPAP long term, where does the Inspire system fit into today’s practice of sleep medicine?
“Upper airway stimulation is another tool, another option for patients,” he said. “In my practice, normally I’d let patients try positive pressure first. I want to make sure they’ve tried CPAP, and they’ve tried more advanced therapy like autotitrating bilevel positive airway pressure, which is more comfortable than CPAP. Bilevel positive airway pressure allows you to salvage a fair number of patients who can’t tolerate CPAP. And I also offer an oral appliance, although the robustness of an oral appliance is not great as apnea becomes more severe.”
The STAR trial is supported by Inspire Medical Systems. Dr. Strollo reported receiving a research grant from the company.
AT SLEEP 2016
Key clinical point: Device therapy for stimulation of the hyperglossal nerve as treatment for obstructive sleep apnea showed continued strong results at 42 months of follow-up.
Major finding: Scores on the Epworth Sleepiness Scale went from 11.6 at baseline to 7.0 at 12 months follow-up following implantation of the Inspire upper airway stimulation device and 7.1 at 42 months.
Data source: This presentation features the prospective 42-month follow-up of 97 participants in the pivotal STAR trial, whose 12-month data earned Food and Drug Administration clearance of the Inspire device.
Disclosures: The study was supported by Inspire Medical Systems. The presenter reported receiving a research grant from the company.