User login
American Academy of Pediatrics (AAP): 2017 National Conference and Exhibition
Duke’s Criteria help guide echocardiography decision in suspected infective endocarditis
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
AT AAP 2017
Key clinical point: Duke’s Criteria should be used to establish whether echocardiograms is needed to screen for infective endocarditis.
Major finding: A total 3% of echocardiograms were positive for mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis.
Data source: Review of 300 patients who had an echocardiogram for suspected infective endocarditis between 2005 and 2015.
Disclosures: Dr. Hua reported having no financial disclosures.
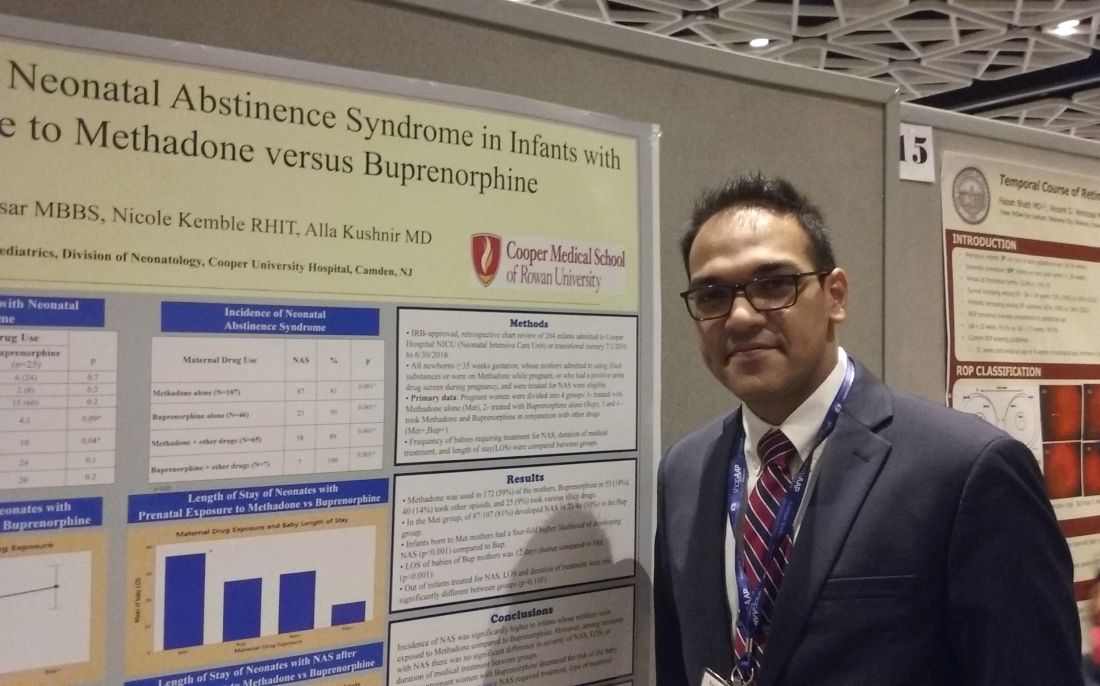
Buprenorphine linked to less neonatal abstinence syndrome than methadone
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
AT AAP 2017
Key clinical point: .
Major finding: 81% of infants in the methadone group developed NAS, compared with 50% of the buprenorphine group.
Data source: Retrospective study of 204 babies admitted to a NICU between July 2010 to June 2016 whose mothers admitted or tested positive for opioid maintenance therapy.
Disclosures: Dr. Kushnir and Dr. Bhaysar reported having no relevant financial disclosures.
AAP annual meeting sessions you won’t want to miss
- “The preconference program ‘Pediatricians Leading Change in Physician Health and Wellness’ will be something you don’t want to miss. Speakers will address topics such as burnout among physicians and residents, compassion fatigue, and approaches to wellness that target individuals, practices, organizations, and medical education. Physician wellness is essential if we want to provide excellent medical care.” Friday, Sept. 15, 11:30 a.m. – 5:30 p.m. at McCormick Place West, W375 E.
- “Monday’s plenary session, ‘The Heat Is On: Why Climate Change Advocacy Is Essential to Child Health’ by Jonathan Patz, MD, MPH, will be particularly relevant, given recent extreme weather events. Children also are affected by climate change, because infectious diseases patterns are altered and because of changes in plant growth and pollen production. Dr. Patz will discuss how pediatricians and physicians from other specialties need to join together to protect patients from further harm, through education and advocacy.” Monday, Sept. 18, at 12:10 p.m. – 12:30 p.m. at Skyline Ballroom.
- “Tics, CANS, PANS, and Other Movement Disorders” by Joanna Blackburn, MD. “When I was in training, these diagnoses were not really recognized; but from what I have seen in practice, they exist and require support from specialists who are hard to find. Having more knowledge of the disorders would benefit any primary care physician.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 C, and Sunday, Sept. 17, at 8:30 a.m. – 9:15 a.m. at McCormick Place West, W185D.
- “Are Vaccines Safe?” by Paul Offit, MD. “As physicians, we know that vaccines are safe; but our patients are very skeptical about this and don’t believe us. I hope this lecture will give us statistics and studies to bring back to our patients.” Saturday, Sept. 16, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 B, and Sunday, Sept. 17, at 2 p.m. – 2:45 p.m. at McCormick Place West, W183 B.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, is always a good guide.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Integrating Mental Health Services in the Primary Care Office” by Jay Rabinowitz, MD. “Pediatricians are increasingly involved in dealing with children and adolescents who have mental health problems. Enhancing their ability to do so in their office can be very beneficial.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5:00 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
- “2017 AAP Guidelines for Childhood Hypertension: Highlights” by Joseph Flynn, MD, MS. “New guidelines for diagnosis, evaluation, and management of abnormal blood pressures in the ambulatory setting were issued by the AAP in September. Pediatricians need to be updated on this important disease and incorporate these into their practices.” Tuesday, Sept. 19, at 10:30 a.m. – 10:50 a.m. at Skyline Ballroom.
- “Meet the Redbook Committee.” “This session will include discussions of issues germane to infectious diseases in children. It always includes new information on important topics for practice, including immunizations.” Monday, Sept. 18, at 8 a.m. – 10 a.m. at McCormick Place West, W190 A.
- “Vaccine Update, What’s New and What’s Changed” by Mary Anne Jackson, MD. “Recommendations change yearly, so this session is always important.” Sunday, Sept. 17, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 A, and Sunday, Sept. 17, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 A.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, highlights the new recommendations for the new guidelines published this year. There are important changes for all who use Bright Futures for their preventive child health visits (well-child visits).” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health – What’s at Stake in the New Administration” by Lynda Young, MD. “Dr. Young has significant experience in the advocacy area, which started for her when she was a young practitioner in Massachusetts and became interested in learning about how to promote the health of her patients through legislative connections and actions. Lynda is now chair of the AAP Committee on Federal Government Affairs, and with the changes in Washington adversely affecting millions of children in our country, it will be crucial for individual pediatricians to advocate in their communities and beyond. This session will share key concepts and tools for child health advocacy.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “AAP President’s Address.” “The AAP is our voice, our tool to improve the lives of children. I want to know what the AAP thinks is important today, and AAP President Fernando Stein, MD, will provide an update on efforts by the academy to advance the Agenda for Children.” Saturday, Sept. 16, at 10:30 a.m. – 11:15 a.m. at Skyline Ballroom.
- “Antimicrobial Update.” “Infectious diseases is a big part of pediatrics. I need to stay current on the latest antibiotic tools.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W179, and Monday, Sept. 18, at 8:30 a.m. – 10 a.m. at McCormick Place West, W180.
- “Teens Gone Wild: Advising Families on Parenting Adolescents.” “Working with parenting issues with teens is fun but complicated. I look forward to the refresher.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W183 A.
- “Social Determinants of Health: Practical and Sensitive Identification and Strategies.” “Yes, but what is our responsibility as pediatricians? Hopefully, I can find out at this session.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Council on Community Pediatrics Program. The Intersection of Housing, Neighborhood, and Child Health.” “We must never forget that the factors that impact the health and development of our patients often are not medical, but social and environmental. This should be an interesting session.” Monday, Sept. 18, at 8 a.m. – 12 p.m. at McCormick Place West, S105 A.
- “Bright Futures Update: What Has Changed and Why.” “There is nothing more complicated or important than the well-child care we provide. Bright Futures has come out with new changes, and I need to take advantage of having the editor, Joe Hagan, guide me through the changes.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health: What’s at Stake in the New Administration.” “These are scary times for children, especially for those who come from disadvantaged backgrounds. I need to prioritize where to take action.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Integrating Mental Health Services in the Primary Care Office.” “We see more and more children coming in the office with mental health issues, and I need new skill development to take care of them.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
- “The preconference program ‘Pediatricians Leading Change in Physician Health and Wellness’ will be something you don’t want to miss. Speakers will address topics such as burnout among physicians and residents, compassion fatigue, and approaches to wellness that target individuals, practices, organizations, and medical education. Physician wellness is essential if we want to provide excellent medical care.” Friday, Sept. 15, 11:30 a.m. – 5:30 p.m. at McCormick Place West, W375 E.
- “Monday’s plenary session, ‘The Heat Is On: Why Climate Change Advocacy Is Essential to Child Health’ by Jonathan Patz, MD, MPH, will be particularly relevant, given recent extreme weather events. Children also are affected by climate change, because infectious diseases patterns are altered and because of changes in plant growth and pollen production. Dr. Patz will discuss how pediatricians and physicians from other specialties need to join together to protect patients from further harm, through education and advocacy.” Monday, Sept. 18, at 12:10 p.m. – 12:30 p.m. at Skyline Ballroom.
- “Tics, CANS, PANS, and Other Movement Disorders” by Joanna Blackburn, MD. “When I was in training, these diagnoses were not really recognized; but from what I have seen in practice, they exist and require support from specialists who are hard to find. Having more knowledge of the disorders would benefit any primary care physician.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 C, and Sunday, Sept. 17, at 8:30 a.m. – 9:15 a.m. at McCormick Place West, W185D.
- “Are Vaccines Safe?” by Paul Offit, MD. “As physicians, we know that vaccines are safe; but our patients are very skeptical about this and don’t believe us. I hope this lecture will give us statistics and studies to bring back to our patients.” Saturday, Sept. 16, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 B, and Sunday, Sept. 17, at 2 p.m. – 2:45 p.m. at McCormick Place West, W183 B.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, is always a good guide.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Integrating Mental Health Services in the Primary Care Office” by Jay Rabinowitz, MD. “Pediatricians are increasingly involved in dealing with children and adolescents who have mental health problems. Enhancing their ability to do so in their office can be very beneficial.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5:00 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
- “2017 AAP Guidelines for Childhood Hypertension: Highlights” by Joseph Flynn, MD, MS. “New guidelines for diagnosis, evaluation, and management of abnormal blood pressures in the ambulatory setting were issued by the AAP in September. Pediatricians need to be updated on this important disease and incorporate these into their practices.” Tuesday, Sept. 19, at 10:30 a.m. – 10:50 a.m. at Skyline Ballroom.
- “Meet the Redbook Committee.” “This session will include discussions of issues germane to infectious diseases in children. It always includes new information on important topics for practice, including immunizations.” Monday, Sept. 18, at 8 a.m. – 10 a.m. at McCormick Place West, W190 A.
- “Vaccine Update, What’s New and What’s Changed” by Mary Anne Jackson, MD. “Recommendations change yearly, so this session is always important.” Sunday, Sept. 17, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 A, and Sunday, Sept. 17, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 A.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, highlights the new recommendations for the new guidelines published this year. There are important changes for all who use Bright Futures for their preventive child health visits (well-child visits).” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health – What’s at Stake in the New Administration” by Lynda Young, MD. “Dr. Young has significant experience in the advocacy area, which started for her when she was a young practitioner in Massachusetts and became interested in learning about how to promote the health of her patients through legislative connections and actions. Lynda is now chair of the AAP Committee on Federal Government Affairs, and with the changes in Washington adversely affecting millions of children in our country, it will be crucial for individual pediatricians to advocate in their communities and beyond. This session will share key concepts and tools for child health advocacy.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “AAP President’s Address.” “The AAP is our voice, our tool to improve the lives of children. I want to know what the AAP thinks is important today, and AAP President Fernando Stein, MD, will provide an update on efforts by the academy to advance the Agenda for Children.” Saturday, Sept. 16, at 10:30 a.m. – 11:15 a.m. at Skyline Ballroom.
- “Antimicrobial Update.” “Infectious diseases is a big part of pediatrics. I need to stay current on the latest antibiotic tools.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W179, and Monday, Sept. 18, at 8:30 a.m. – 10 a.m. at McCormick Place West, W180.
- “Teens Gone Wild: Advising Families on Parenting Adolescents.” “Working with parenting issues with teens is fun but complicated. I look forward to the refresher.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W183 A.
- “Social Determinants of Health: Practical and Sensitive Identification and Strategies.” “Yes, but what is our responsibility as pediatricians? Hopefully, I can find out at this session.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Council on Community Pediatrics Program. The Intersection of Housing, Neighborhood, and Child Health.” “We must never forget that the factors that impact the health and development of our patients often are not medical, but social and environmental. This should be an interesting session.” Monday, Sept. 18, at 8 a.m. – 12 p.m. at McCormick Place West, S105 A.
- “Bright Futures Update: What Has Changed and Why.” “There is nothing more complicated or important than the well-child care we provide. Bright Futures has come out with new changes, and I need to take advantage of having the editor, Joe Hagan, guide me through the changes.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health: What’s at Stake in the New Administration.” “These are scary times for children, especially for those who come from disadvantaged backgrounds. I need to prioritize where to take action.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Integrating Mental Health Services in the Primary Care Office.” “We see more and more children coming in the office with mental health issues, and I need new skill development to take care of them.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
- “The preconference program ‘Pediatricians Leading Change in Physician Health and Wellness’ will be something you don’t want to miss. Speakers will address topics such as burnout among physicians and residents, compassion fatigue, and approaches to wellness that target individuals, practices, organizations, and medical education. Physician wellness is essential if we want to provide excellent medical care.” Friday, Sept. 15, 11:30 a.m. – 5:30 p.m. at McCormick Place West, W375 E.
- “Monday’s plenary session, ‘The Heat Is On: Why Climate Change Advocacy Is Essential to Child Health’ by Jonathan Patz, MD, MPH, will be particularly relevant, given recent extreme weather events. Children also are affected by climate change, because infectious diseases patterns are altered and because of changes in plant growth and pollen production. Dr. Patz will discuss how pediatricians and physicians from other specialties need to join together to protect patients from further harm, through education and advocacy.” Monday, Sept. 18, at 12:10 p.m. – 12:30 p.m. at Skyline Ballroom.
- “Tics, CANS, PANS, and Other Movement Disorders” by Joanna Blackburn, MD. “When I was in training, these diagnoses were not really recognized; but from what I have seen in practice, they exist and require support from specialists who are hard to find. Having more knowledge of the disorders would benefit any primary care physician.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 C, and Sunday, Sept. 17, at 8:30 a.m. – 9:15 a.m. at McCormick Place West, W185D.
- “Are Vaccines Safe?” by Paul Offit, MD. “As physicians, we know that vaccines are safe; but our patients are very skeptical about this and don’t believe us. I hope this lecture will give us statistics and studies to bring back to our patients.” Saturday, Sept. 16, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 B, and Sunday, Sept. 17, at 2 p.m. – 2:45 p.m. at McCormick Place West, W183 B.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, is always a good guide.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Integrating Mental Health Services in the Primary Care Office” by Jay Rabinowitz, MD. “Pediatricians are increasingly involved in dealing with children and adolescents who have mental health problems. Enhancing their ability to do so in their office can be very beneficial.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5:00 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
- “2017 AAP Guidelines for Childhood Hypertension: Highlights” by Joseph Flynn, MD, MS. “New guidelines for diagnosis, evaluation, and management of abnormal blood pressures in the ambulatory setting were issued by the AAP in September. Pediatricians need to be updated on this important disease and incorporate these into their practices.” Tuesday, Sept. 19, at 10:30 a.m. – 10:50 a.m. at Skyline Ballroom.
- “Meet the Redbook Committee.” “This session will include discussions of issues germane to infectious diseases in children. It always includes new information on important topics for practice, including immunizations.” Monday, Sept. 18, at 8 a.m. – 10 a.m. at McCormick Place West, W190 A.
- “Vaccine Update, What’s New and What’s Changed” by Mary Anne Jackson, MD. “Recommendations change yearly, so this session is always important.” Sunday, Sept. 17, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W183 A, and Sunday, Sept. 17, at 4 p.m. – 4:45 p.m. at McCormick Place West, W183 A.
- “The presentation ‘Bright Futures Update: What Has Changed and Why’ by Joseph Hagan Jr., MD, highlights the new recommendations for the new guidelines published this year. There are important changes for all who use Bright Futures for their preventive child health visits (well-child visits).” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health – What’s at Stake in the New Administration” by Lynda Young, MD. “Dr. Young has significant experience in the advocacy area, which started for her when she was a young practitioner in Massachusetts and became interested in learning about how to promote the health of her patients through legislative connections and actions. Lynda is now chair of the AAP Committee on Federal Government Affairs, and with the changes in Washington adversely affecting millions of children in our country, it will be crucial for individual pediatricians to advocate in their communities and beyond. This session will share key concepts and tools for child health advocacy.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “AAP President’s Address.” “The AAP is our voice, our tool to improve the lives of children. I want to know what the AAP thinks is important today, and AAP President Fernando Stein, MD, will provide an update on efforts by the academy to advance the Agenda for Children.” Saturday, Sept. 16, at 10:30 a.m. – 11:15 a.m. at Skyline Ballroom.
- “Antimicrobial Update.” “Infectious diseases is a big part of pediatrics. I need to stay current on the latest antibiotic tools.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W179, and Monday, Sept. 18, at 8:30 a.m. – 10 a.m. at McCormick Place West, W180.
- “Teens Gone Wild: Advising Families on Parenting Adolescents.” “Working with parenting issues with teens is fun but complicated. I look forward to the refresher.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W183 A.
- “Social Determinants of Health: Practical and Sensitive Identification and Strategies.” “Yes, but what is our responsibility as pediatricians? Hopefully, I can find out at this session.” Sunday, Sept. 17, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Council on Community Pediatrics Program. The Intersection of Housing, Neighborhood, and Child Health.” “We must never forget that the factors that impact the health and development of our patients often are not medical, but social and environmental. This should be an interesting session.” Monday, Sept. 18, at 8 a.m. – 12 p.m. at McCormick Place West, S105 A.
- “Bright Futures Update: What Has Changed and Why.” “There is nothing more complicated or important than the well-child care we provide. Bright Futures has come out with new changes, and I need to take advantage of having the editor, Joe Hagan, guide me through the changes.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W179, and Sunday, Sept. 17, at 9:30 a.m. – 10:15 a.m. at McCormick Place West, W187 A.
- “Children’s Health: What’s at Stake in the New Administration.” “These are scary times for children, especially for those who come from disadvantaged backgrounds. I need to prioritize where to take action.” Saturday, Sept. 16, at 8:30 a.m. – 10 a.m. at McCormick Place West, W181 A.
- “Integrating Mental Health Services in the Primary Care Office.” “We see more and more children coming in the office with mental health issues, and I need new skill development to take care of them.” Saturday, Sept. 16, at 7:30 a.m. – 8:15 a.m. at McCormick Place West, W178 B, and Saturday, Sept. 16, at 5 p.m. – 5:45 p.m. at McCormick Place West, W176 C.
Your job: Provide oral health promotion, fluoride varnish
Learn the “Nuts and Bolts of Office-Based Oral Health Promotion and Fluoride Varnish” from Melinda Clark, MD, and Rocio Quiñonez, DMD.
Caries affect 50% of 5- to 9-year-olds and 78% of 17-year-olds, yet 25% of poor children don’t see a dentist by age 5. You are in an excellent position to provide “timely preventive oral health interventions” in your office, the United States Preventive Services Task Force recommends that “primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption,” and fluoride varnish was added to the Bright Futures Periodicity Schedule in 2015.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Clark and Dr. Quiñonez will address the importance of dealing with early childhood caries (ECC), defined as one or more decayed, missing from dental caries, or filled tooth surfaces in any primary tooth in a preschool-age child between birth and younger than 6 years of age. ECC can result in missed school, inappropriate use of over-the-counter pain medication, disturbed sleep, eating dysfunction, infection, and even death.
Dr. Clark is an associate professor of pediatrics at Albany (N.Y.) Medical College, and Dr. Quiñonez is an associate professor of pediatric dentistry and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Clark and Dr. Quiñonez will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!
Learn the “Nuts and Bolts of Office-Based Oral Health Promotion and Fluoride Varnish” from Melinda Clark, MD, and Rocio Quiñonez, DMD.
Caries affect 50% of 5- to 9-year-olds and 78% of 17-year-olds, yet 25% of poor children don’t see a dentist by age 5. You are in an excellent position to provide “timely preventive oral health interventions” in your office, the United States Preventive Services Task Force recommends that “primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption,” and fluoride varnish was added to the Bright Futures Periodicity Schedule in 2015.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Clark and Dr. Quiñonez will address the importance of dealing with early childhood caries (ECC), defined as one or more decayed, missing from dental caries, or filled tooth surfaces in any primary tooth in a preschool-age child between birth and younger than 6 years of age. ECC can result in missed school, inappropriate use of over-the-counter pain medication, disturbed sleep, eating dysfunction, infection, and even death.
Dr. Clark is an associate professor of pediatrics at Albany (N.Y.) Medical College, and Dr. Quiñonez is an associate professor of pediatric dentistry and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Clark and Dr. Quiñonez will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!
Learn the “Nuts and Bolts of Office-Based Oral Health Promotion and Fluoride Varnish” from Melinda Clark, MD, and Rocio Quiñonez, DMD.
Caries affect 50% of 5- to 9-year-olds and 78% of 17-year-olds, yet 25% of poor children don’t see a dentist by age 5. You are in an excellent position to provide “timely preventive oral health interventions” in your office, the United States Preventive Services Task Force recommends that “primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption,” and fluoride varnish was added to the Bright Futures Periodicity Schedule in 2015.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Clark and Dr. Quiñonez will address the importance of dealing with early childhood caries (ECC), defined as one or more decayed, missing from dental caries, or filled tooth surfaces in any primary tooth in a preschool-age child between birth and younger than 6 years of age. ECC can result in missed school, inappropriate use of over-the-counter pain medication, disturbed sleep, eating dysfunction, infection, and even death.
Dr. Clark is an associate professor of pediatrics at Albany (N.Y.) Medical College, and Dr. Quiñonez is an associate professor of pediatric dentistry and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Clark and Dr. Quiñonez will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!
Learn how to manage your patients’ behavior problems
One of the presentations you’ll definitely want to attend is Dr. Barbara J. Howard’s “As Easy as A-B-C-G: Office Management of Behavior Problems in Children.”
She’ll teach you the A, B, C, and G of managing behavior problems:
- A = Antecedents/meaning
- B = Behavior
- C = Consequences
- G = Gap in skills
Dr. Howard, an assistant professor of pediatrics at the Johns Hopkins University, Baltimore, will use case presentations to show you how this model works in detail. She’ll describe how best to organize a session with a patient, how to engage the family, and how to approach the objectives of family interviewing.

Dr. Howard goes into much more detail, giving examples in each case, explaining how to assist the parent-child relationship, providing parents with bypass strategies for various issues, and teaching behavior modification for dysfunctional patterns.
That is just one case presentation. Others detail how to handle a toddler who refuses to go to bed, an aggressive 5-year-old, a clingy 9-year-old suffering from anxiety, and a 12-year-old who has recently begun wetting the bed and stealing from her mother.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Howard will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!
One of the presentations you’ll definitely want to attend is Dr. Barbara J. Howard’s “As Easy as A-B-C-G: Office Management of Behavior Problems in Children.”
She’ll teach you the A, B, C, and G of managing behavior problems:
- A = Antecedents/meaning
- B = Behavior
- C = Consequences
- G = Gap in skills
Dr. Howard, an assistant professor of pediatrics at the Johns Hopkins University, Baltimore, will use case presentations to show you how this model works in detail. She’ll describe how best to organize a session with a patient, how to engage the family, and how to approach the objectives of family interviewing.

Dr. Howard goes into much more detail, giving examples in each case, explaining how to assist the parent-child relationship, providing parents with bypass strategies for various issues, and teaching behavior modification for dysfunctional patterns.
That is just one case presentation. Others detail how to handle a toddler who refuses to go to bed, an aggressive 5-year-old, a clingy 9-year-old suffering from anxiety, and a 12-year-old who has recently begun wetting the bed and stealing from her mother.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Howard will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!
One of the presentations you’ll definitely want to attend is Dr. Barbara J. Howard’s “As Easy as A-B-C-G: Office Management of Behavior Problems in Children.”
She’ll teach you the A, B, C, and G of managing behavior problems:
- A = Antecedents/meaning
- B = Behavior
- C = Consequences
- G = Gap in skills
Dr. Howard, an assistant professor of pediatrics at the Johns Hopkins University, Baltimore, will use case presentations to show you how this model works in detail. She’ll describe how best to organize a session with a patient, how to engage the family, and how to approach the objectives of family interviewing.

Dr. Howard goes into much more detail, giving examples in each case, explaining how to assist the parent-child relationship, providing parents with bypass strategies for various issues, and teaching behavior modification for dysfunctional patterns.
That is just one case presentation. Others detail how to handle a toddler who refuses to go to bed, an aggressive 5-year-old, a clingy 9-year-old suffering from anxiety, and a 12-year-old who has recently begun wetting the bed and stealing from her mother.
At the American Academy of Pediatrics’ annual meeting in Chicago, Dr. Howard will be presenting Sunday, Sept. 17, from 4 p.m. to 5:30 p.m., and Monday, Sept. 18, from 8:30 a.m. to 10 a.m. You don’t want to miss it!