User login
American Academy of Pediatrics (AAP): 2017 National Conference and Exhibition
Evidence-backed questions can guide a GERD vs. NERD differential diagnosis
CHICAGO – when doing a differential diagnosis. Fortunately, five questions backed by increasing evidence can help you make the call.
“Everyone in the room knows babies puke, and babies can puke a lot,” Barry K. Wershil, MD, said at the annual meeting of the American Academy of Pediatrics. The approach to diagnosing GERD is age specific. “Kids who puke tend to outgrow it over time. With development, 95% or more are no longer refluxing at 18 months of age.”
“So generally there is no reason to initially refer older children and teenagers to a gastroenterologist,” Dr. Wershil said. “One of the essential things [you] do is consider all the causes of vomiting that are not GERD. If your first go-to is GERD, you’re going to miss other issues.”
Dr. Wershil reviewed the definitions: Gastroesophageal reflux is passage of gastric contents into the esophagus. GERD, on the other hand, is defined by the troublesome symptoms or complications associated with reflux of gastric material into the esophagus. In contrast, NERD is the presence of reflux symptoms with no evidence of mucosal erosion or mucosal breaks.
Considerations backed by evidence
Unfortunately, symptoms alone do not always differentiate erosive versus nonerosive esophagitis, Dr. Wershil said, although recurrent vomiting, poor weight gain, anemia, feeding problems, and respiratory problems can be signs of complicated GERD.
He recommended the following five considerations to distinguish GERD from NERD:
- Is the patient exhibiting normal weight gain? If not, ask questions about how the child is being fed. Have the parents started diluting the formula because they think that will take care of the vomiting? Have they begun limiting the amount of formula after observing that the child throws up at 4 ounces but not at 2 ounces?
- Is the patient bleeding or anemic? Hematemesis is rarely the presentation of infants with GERD, but anemia may be.
- Does the patient have respiratory problems (for example, a history of aspiration, recurring wheezing, or cough)?
- Is the patient neurologically normal? If so, that can present a special class of patients in which vomiting may not be just normal infant vomiting.
- Is the patient older than 2 years? We expect 95% of children to outgrow reflux by 18 months, and most children who have physiological reflux will outgrow it by 2 years.
“Those five questions in 1983 had little evidence, but in 2017 there is more evidence that these are the questions to focus on,” Dr. Wershil said.
The role of diagnostic testing
Diagnostic testing, such as pH monitoring, impedance testing, and endoscopy, can be useful in specific situations but carry limitations for widespread use, Dr. Wershil said. “Each test has reasons and limitations.”
An upper GI tract series looks only for anatomic anomalies, for example. pH monitoring is still used in many centers, but in general, impedance monitoring has become more common because it can detect both acid and nonacid reflux: “You can get a very detailed analysis of events happening in the esophagus over time.” One caveat Dr. Wershil added is that, “in some instances, we’re unsure how to define this in the pediatric age ranges we treat.”
Endoscopy has a limited role for the rare patients with mucosal changes or erosive esophagitis, he added. Endoscopy is ordered to detect mucosal changes that confirm esophageal erosion. “In all the kids we scope with positive pH, we rarely find erosive esophagitis,” Dr. Wershil said. “What we find more often is NERD. That really represents more of what we see in our patient population.”
“I hope this information is a good starting point to understand the algorithms that get generated,” Dr. Wershil said.
He recommended an algorithm for gastroesophageal reflux prepared by the American Academy of Pediatrics’ Section on Gastroenterology, Hepatology, and Nutrition (Pediatrics. 2013 May. doi: 10.1542/peds.2013-0421). “I think this information is really solidly grounded in evidence.”
Dr. Wershil is a consultant for Alexion Pharmaceuticals; is a member of the speakers bureau for Abbott Nutrition, Mead Johnson Nutrition, and Nutricia; and receives funding from the National Institutes of Health Consortium of Eosinophilic Gastrointestinal Disease Researchers.
CHICAGO – when doing a differential diagnosis. Fortunately, five questions backed by increasing evidence can help you make the call.
“Everyone in the room knows babies puke, and babies can puke a lot,” Barry K. Wershil, MD, said at the annual meeting of the American Academy of Pediatrics. The approach to diagnosing GERD is age specific. “Kids who puke tend to outgrow it over time. With development, 95% or more are no longer refluxing at 18 months of age.”
“So generally there is no reason to initially refer older children and teenagers to a gastroenterologist,” Dr. Wershil said. “One of the essential things [you] do is consider all the causes of vomiting that are not GERD. If your first go-to is GERD, you’re going to miss other issues.”
Dr. Wershil reviewed the definitions: Gastroesophageal reflux is passage of gastric contents into the esophagus. GERD, on the other hand, is defined by the troublesome symptoms or complications associated with reflux of gastric material into the esophagus. In contrast, NERD is the presence of reflux symptoms with no evidence of mucosal erosion or mucosal breaks.
Considerations backed by evidence
Unfortunately, symptoms alone do not always differentiate erosive versus nonerosive esophagitis, Dr. Wershil said, although recurrent vomiting, poor weight gain, anemia, feeding problems, and respiratory problems can be signs of complicated GERD.
He recommended the following five considerations to distinguish GERD from NERD:
- Is the patient exhibiting normal weight gain? If not, ask questions about how the child is being fed. Have the parents started diluting the formula because they think that will take care of the vomiting? Have they begun limiting the amount of formula after observing that the child throws up at 4 ounces but not at 2 ounces?
- Is the patient bleeding or anemic? Hematemesis is rarely the presentation of infants with GERD, but anemia may be.
- Does the patient have respiratory problems (for example, a history of aspiration, recurring wheezing, or cough)?
- Is the patient neurologically normal? If so, that can present a special class of patients in which vomiting may not be just normal infant vomiting.
- Is the patient older than 2 years? We expect 95% of children to outgrow reflux by 18 months, and most children who have physiological reflux will outgrow it by 2 years.
“Those five questions in 1983 had little evidence, but in 2017 there is more evidence that these are the questions to focus on,” Dr. Wershil said.
The role of diagnostic testing
Diagnostic testing, such as pH monitoring, impedance testing, and endoscopy, can be useful in specific situations but carry limitations for widespread use, Dr. Wershil said. “Each test has reasons and limitations.”
An upper GI tract series looks only for anatomic anomalies, for example. pH monitoring is still used in many centers, but in general, impedance monitoring has become more common because it can detect both acid and nonacid reflux: “You can get a very detailed analysis of events happening in the esophagus over time.” One caveat Dr. Wershil added is that, “in some instances, we’re unsure how to define this in the pediatric age ranges we treat.”
Endoscopy has a limited role for the rare patients with mucosal changes or erosive esophagitis, he added. Endoscopy is ordered to detect mucosal changes that confirm esophageal erosion. “In all the kids we scope with positive pH, we rarely find erosive esophagitis,” Dr. Wershil said. “What we find more often is NERD. That really represents more of what we see in our patient population.”
“I hope this information is a good starting point to understand the algorithms that get generated,” Dr. Wershil said.
He recommended an algorithm for gastroesophageal reflux prepared by the American Academy of Pediatrics’ Section on Gastroenterology, Hepatology, and Nutrition (Pediatrics. 2013 May. doi: 10.1542/peds.2013-0421). “I think this information is really solidly grounded in evidence.”
Dr. Wershil is a consultant for Alexion Pharmaceuticals; is a member of the speakers bureau for Abbott Nutrition, Mead Johnson Nutrition, and Nutricia; and receives funding from the National Institutes of Health Consortium of Eosinophilic Gastrointestinal Disease Researchers.
CHICAGO – when doing a differential diagnosis. Fortunately, five questions backed by increasing evidence can help you make the call.
“Everyone in the room knows babies puke, and babies can puke a lot,” Barry K. Wershil, MD, said at the annual meeting of the American Academy of Pediatrics. The approach to diagnosing GERD is age specific. “Kids who puke tend to outgrow it over time. With development, 95% or more are no longer refluxing at 18 months of age.”
“So generally there is no reason to initially refer older children and teenagers to a gastroenterologist,” Dr. Wershil said. “One of the essential things [you] do is consider all the causes of vomiting that are not GERD. If your first go-to is GERD, you’re going to miss other issues.”
Dr. Wershil reviewed the definitions: Gastroesophageal reflux is passage of gastric contents into the esophagus. GERD, on the other hand, is defined by the troublesome symptoms or complications associated with reflux of gastric material into the esophagus. In contrast, NERD is the presence of reflux symptoms with no evidence of mucosal erosion or mucosal breaks.
Considerations backed by evidence
Unfortunately, symptoms alone do not always differentiate erosive versus nonerosive esophagitis, Dr. Wershil said, although recurrent vomiting, poor weight gain, anemia, feeding problems, and respiratory problems can be signs of complicated GERD.
He recommended the following five considerations to distinguish GERD from NERD:
- Is the patient exhibiting normal weight gain? If not, ask questions about how the child is being fed. Have the parents started diluting the formula because they think that will take care of the vomiting? Have they begun limiting the amount of formula after observing that the child throws up at 4 ounces but not at 2 ounces?
- Is the patient bleeding or anemic? Hematemesis is rarely the presentation of infants with GERD, but anemia may be.
- Does the patient have respiratory problems (for example, a history of aspiration, recurring wheezing, or cough)?
- Is the patient neurologically normal? If so, that can present a special class of patients in which vomiting may not be just normal infant vomiting.
- Is the patient older than 2 years? We expect 95% of children to outgrow reflux by 18 months, and most children who have physiological reflux will outgrow it by 2 years.
“Those five questions in 1983 had little evidence, but in 2017 there is more evidence that these are the questions to focus on,” Dr. Wershil said.
The role of diagnostic testing
Diagnostic testing, such as pH monitoring, impedance testing, and endoscopy, can be useful in specific situations but carry limitations for widespread use, Dr. Wershil said. “Each test has reasons and limitations.”
An upper GI tract series looks only for anatomic anomalies, for example. pH monitoring is still used in many centers, but in general, impedance monitoring has become more common because it can detect both acid and nonacid reflux: “You can get a very detailed analysis of events happening in the esophagus over time.” One caveat Dr. Wershil added is that, “in some instances, we’re unsure how to define this in the pediatric age ranges we treat.”
Endoscopy has a limited role for the rare patients with mucosal changes or erosive esophagitis, he added. Endoscopy is ordered to detect mucosal changes that confirm esophageal erosion. “In all the kids we scope with positive pH, we rarely find erosive esophagitis,” Dr. Wershil said. “What we find more often is NERD. That really represents more of what we see in our patient population.”
“I hope this information is a good starting point to understand the algorithms that get generated,” Dr. Wershil said.
He recommended an algorithm for gastroesophageal reflux prepared by the American Academy of Pediatrics’ Section on Gastroenterology, Hepatology, and Nutrition (Pediatrics. 2013 May. doi: 10.1542/peds.2013-0421). “I think this information is really solidly grounded in evidence.”
Dr. Wershil is a consultant for Alexion Pharmaceuticals; is a member of the speakers bureau for Abbott Nutrition, Mead Johnson Nutrition, and Nutricia; and receives funding from the National Institutes of Health Consortium of Eosinophilic Gastrointestinal Disease Researchers.
EXPERT ANALYSIS FROM AAP 2017
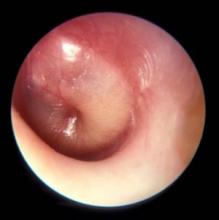
Localized wheezing differs from asthmatic, viral wheezing
CHICAGO – , explained Erik Hysinger, MD, MS, of the division of pulmonary medicine at Cincinnati Children’s Hospital.
Localized wheezing is not consistent with asthmatic or viral wheezing, which is typically diffuse and polyphonic, Dr. Hysinger emphasized at the annual meeting of the American Academy of Pediatrics.
“Localized wheezing is less common than diffuse wheezing and typically has a homophonous sound,” Dr. Hysinger said. It also usually arises from a central airway pathology. “High flow rates create loud amplitude sounds.”
Dr. Hysinger also covered management strategies for focal wheezing, starting with an initial trial of bronchodilators. Any wheezing resulting from a central airway problem, however, isn’t likely to respond to bronchodilators. Standard work-up for any of these causes is usually a chest x-ray, often paired with a bronchoscopy. Persistent wheezing likely needs a chest CT, and many of these conditions will require referral to a subspecialist.
Airway occlusion diagnoses
Four potential causes of an airway blockage are a foreign body, a bronchial cast, mucous plugs, or airway tumors.
A foreign body typically occurs with a cough, wheezing, stridor, and respiratory distress. It is most common in children under age 4 years, usually in those without a history of aspiration, yet providers initially misdiagnose more than 20% of patients with a foreign body. The foreign object – often coins, food, or batteries – frequently ends up in the right main bronchus and may go undetected up to a month, potentially leading to pneumonia, abscess, atelectasis, bronchiectasis, or airway erosion.
An endobronchial cast is rarer than a foreign body, but can be large enough to completely fill a lung with branching mucin, fibrin, and inflammatory cells. The wheezing sounds homophonous, with a barky or brassy cough accompanied by atelectasis. Dr. Hysinger recommended ordering chest x-ray, echocardiogram, and bronchoscopy. Although often idiopathic, these casts also can result from asthma or another disease: neutrophilic inflammation typically indicates a heart condition whereas asthma or influenza leads to eosinophilic inflammation.
Treatment should involve clearing the airway, followed by hypertonic saline, an inhaled tissue plasminogen activator, and a bronchoscopy for extraction.
Although distinct from endobronchial casts, a mucus plug also presents with wheezing, a cough, and atelectasis, and potentially respiratory distress or failure, and hypoxemia. Mucus plugs are diagnosed with a chest x-ray and flexible bronchoscopy, and then treated by removing the plug and clearing the airway, hypertonic saline, and mucolytics.
The rarest cause of an airway blockage is an airway tumor, often mistaken for asthma. Benign causes include papillomatosis, hemangioma, and hamartomas, while potentially malignant causes include a carcinoid, mucoepidermoid carcinoma, inflammatory myofibromas, and granular cell tumors.
In addition to a chest x-ray and bronchoscopy, a chest CT scan plus a biopsy and resection are necessary to diagnose airway tumors. Treatment will depend on the specific type of tumor identified.
“Overall survival is excellent,” Dr. Hysinger said of children with airway tumors.
Airway narrowing diagnoses
Two possible diagnoses for an intrinsic airway narrowing include bronchomalacia, occurring in only 1 of 2,100 children, and bronchial stenosis.
In bronchomalacia – diagnosed primarily with bronchoscopy – the airway collapses from weakening of the cartilage and posterior membrane. Bronchomalacia sounds like homophonous wheezing with a barky or brassy cough, and it’s frequently accompanied by recurrent bronchitis and/or pneumonia. Intervention is rarely necessary when occurring on its own, but severe cases may require endobronchial stents. Dr. Hysinger also recommended considering ipratroprium instead of albuterol.
Bronchial stenosis involves a fixed narrowing of the bronchi and can be congenital – typically occurring with heart disease – or acquired after an intubation and suction trauma or bronchiolitis obliterans (“popcorn lung”). A chest x-ray and bronchoscopy again are standard, but MRI may be necessary as well. Aside from helping the patient clear the airway, bronchial stenosis typically needs limited management unless the patient is symptomatic. In that case, options include balloon dilation, endobronchial stents, or a slide bronchoplasty.
Airway compression diagnoses
An extrinsic airway compression could have a vascular cause or could result from pressure by an extrinsic mass or the axial skeleton.
Vascular compression usually occurs due to abnormal vasculature development, particularly with vascular stents, Dr. Hysinger said. The wheezing presents with stridor, feeding intolerance, recurrent infections, and cyanotic episodes. The work-up should include a chest x-ray, bronchoscopy, and a chest CT and/or MRI. A variety of interventions may be necessary to treat it, including an aortopexy, pulmonary artery trunk–pexy, arterioplasty, vessel implantation, or endobronchial stent. Residual malacia may remain after treatment, however.
The most common reasons for airway compression by some kind of mass is a reactive lymphadenopathy, a tumor, or an infection, including tuberculosis or histoplasmosis. Severe narrowing of the airway can lead to respiratory failure, but because the compression can develop slowly, the wheezing can be mistaken for asthma. In addition to a chest CT and bronchoscopy, a patient will need other work-ups depending on the cause. Possibilities include a biopsy, a gastric aspirate (for tuberculosis), a bronchoalveolar lavage, or antibody titers.
Similarly, because therapeutic intervention requires treating the underlying infection, specific treatments will vary. Tumors typically will need resection, chemotherapy, and/or radiation – and, until the airway is fully cleared, the patient may need chronic mechanical ventilation.
Children with severe scoliosis or kyphosis are those most likely to experience airway compression resulting from pressure by the axial skeleton, in which the spine’s curvature directly presses on the airway. In addition to the wheeze, these patients may have respiratory distress or recurrent focal pneumonia, Dr. Hysinger said. The standard work-up involves a chest x-ray, chest CT, spinal MRI, and bronchoscopy.
Consider using spinal rods, but they can both help the condition or potentially exacerbate the compression, Dr. Hysinger said. Either way, children also will need help with airway clearance and coughing.
Dr. Hysinger concluded by reviewing what you may consider changing in your current practice, including the initial trial of bronchodilators, a chest x-ray, and a subspecialist referral.
No funding was used for this presentation, and Dr. Hysinger reported having no relevant financial disclosures.
CHICAGO – , explained Erik Hysinger, MD, MS, of the division of pulmonary medicine at Cincinnati Children’s Hospital.
Localized wheezing is not consistent with asthmatic or viral wheezing, which is typically diffuse and polyphonic, Dr. Hysinger emphasized at the annual meeting of the American Academy of Pediatrics.
“Localized wheezing is less common than diffuse wheezing and typically has a homophonous sound,” Dr. Hysinger said. It also usually arises from a central airway pathology. “High flow rates create loud amplitude sounds.”
Dr. Hysinger also covered management strategies for focal wheezing, starting with an initial trial of bronchodilators. Any wheezing resulting from a central airway problem, however, isn’t likely to respond to bronchodilators. Standard work-up for any of these causes is usually a chest x-ray, often paired with a bronchoscopy. Persistent wheezing likely needs a chest CT, and many of these conditions will require referral to a subspecialist.
Airway occlusion diagnoses
Four potential causes of an airway blockage are a foreign body, a bronchial cast, mucous plugs, or airway tumors.
A foreign body typically occurs with a cough, wheezing, stridor, and respiratory distress. It is most common in children under age 4 years, usually in those without a history of aspiration, yet providers initially misdiagnose more than 20% of patients with a foreign body. The foreign object – often coins, food, or batteries – frequently ends up in the right main bronchus and may go undetected up to a month, potentially leading to pneumonia, abscess, atelectasis, bronchiectasis, or airway erosion.
An endobronchial cast is rarer than a foreign body, but can be large enough to completely fill a lung with branching mucin, fibrin, and inflammatory cells. The wheezing sounds homophonous, with a barky or brassy cough accompanied by atelectasis. Dr. Hysinger recommended ordering chest x-ray, echocardiogram, and bronchoscopy. Although often idiopathic, these casts also can result from asthma or another disease: neutrophilic inflammation typically indicates a heart condition whereas asthma or influenza leads to eosinophilic inflammation.
Treatment should involve clearing the airway, followed by hypertonic saline, an inhaled tissue plasminogen activator, and a bronchoscopy for extraction.
Although distinct from endobronchial casts, a mucus plug also presents with wheezing, a cough, and atelectasis, and potentially respiratory distress or failure, and hypoxemia. Mucus plugs are diagnosed with a chest x-ray and flexible bronchoscopy, and then treated by removing the plug and clearing the airway, hypertonic saline, and mucolytics.
The rarest cause of an airway blockage is an airway tumor, often mistaken for asthma. Benign causes include papillomatosis, hemangioma, and hamartomas, while potentially malignant causes include a carcinoid, mucoepidermoid carcinoma, inflammatory myofibromas, and granular cell tumors.
In addition to a chest x-ray and bronchoscopy, a chest CT scan plus a biopsy and resection are necessary to diagnose airway tumors. Treatment will depend on the specific type of tumor identified.
“Overall survival is excellent,” Dr. Hysinger said of children with airway tumors.
Airway narrowing diagnoses
Two possible diagnoses for an intrinsic airway narrowing include bronchomalacia, occurring in only 1 of 2,100 children, and bronchial stenosis.
In bronchomalacia – diagnosed primarily with bronchoscopy – the airway collapses from weakening of the cartilage and posterior membrane. Bronchomalacia sounds like homophonous wheezing with a barky or brassy cough, and it’s frequently accompanied by recurrent bronchitis and/or pneumonia. Intervention is rarely necessary when occurring on its own, but severe cases may require endobronchial stents. Dr. Hysinger also recommended considering ipratroprium instead of albuterol.
Bronchial stenosis involves a fixed narrowing of the bronchi and can be congenital – typically occurring with heart disease – or acquired after an intubation and suction trauma or bronchiolitis obliterans (“popcorn lung”). A chest x-ray and bronchoscopy again are standard, but MRI may be necessary as well. Aside from helping the patient clear the airway, bronchial stenosis typically needs limited management unless the patient is symptomatic. In that case, options include balloon dilation, endobronchial stents, or a slide bronchoplasty.
Airway compression diagnoses
An extrinsic airway compression could have a vascular cause or could result from pressure by an extrinsic mass or the axial skeleton.
Vascular compression usually occurs due to abnormal vasculature development, particularly with vascular stents, Dr. Hysinger said. The wheezing presents with stridor, feeding intolerance, recurrent infections, and cyanotic episodes. The work-up should include a chest x-ray, bronchoscopy, and a chest CT and/or MRI. A variety of interventions may be necessary to treat it, including an aortopexy, pulmonary artery trunk–pexy, arterioplasty, vessel implantation, or endobronchial stent. Residual malacia may remain after treatment, however.
The most common reasons for airway compression by some kind of mass is a reactive lymphadenopathy, a tumor, or an infection, including tuberculosis or histoplasmosis. Severe narrowing of the airway can lead to respiratory failure, but because the compression can develop slowly, the wheezing can be mistaken for asthma. In addition to a chest CT and bronchoscopy, a patient will need other work-ups depending on the cause. Possibilities include a biopsy, a gastric aspirate (for tuberculosis), a bronchoalveolar lavage, or antibody titers.
Similarly, because therapeutic intervention requires treating the underlying infection, specific treatments will vary. Tumors typically will need resection, chemotherapy, and/or radiation – and, until the airway is fully cleared, the patient may need chronic mechanical ventilation.
Children with severe scoliosis or kyphosis are those most likely to experience airway compression resulting from pressure by the axial skeleton, in which the spine’s curvature directly presses on the airway. In addition to the wheeze, these patients may have respiratory distress or recurrent focal pneumonia, Dr. Hysinger said. The standard work-up involves a chest x-ray, chest CT, spinal MRI, and bronchoscopy.
Consider using spinal rods, but they can both help the condition or potentially exacerbate the compression, Dr. Hysinger said. Either way, children also will need help with airway clearance and coughing.
Dr. Hysinger concluded by reviewing what you may consider changing in your current practice, including the initial trial of bronchodilators, a chest x-ray, and a subspecialist referral.
No funding was used for this presentation, and Dr. Hysinger reported having no relevant financial disclosures.
CHICAGO – , explained Erik Hysinger, MD, MS, of the division of pulmonary medicine at Cincinnati Children’s Hospital.
Localized wheezing is not consistent with asthmatic or viral wheezing, which is typically diffuse and polyphonic, Dr. Hysinger emphasized at the annual meeting of the American Academy of Pediatrics.
“Localized wheezing is less common than diffuse wheezing and typically has a homophonous sound,” Dr. Hysinger said. It also usually arises from a central airway pathology. “High flow rates create loud amplitude sounds.”
Dr. Hysinger also covered management strategies for focal wheezing, starting with an initial trial of bronchodilators. Any wheezing resulting from a central airway problem, however, isn’t likely to respond to bronchodilators. Standard work-up for any of these causes is usually a chest x-ray, often paired with a bronchoscopy. Persistent wheezing likely needs a chest CT, and many of these conditions will require referral to a subspecialist.
Airway occlusion diagnoses
Four potential causes of an airway blockage are a foreign body, a bronchial cast, mucous plugs, or airway tumors.
A foreign body typically occurs with a cough, wheezing, stridor, and respiratory distress. It is most common in children under age 4 years, usually in those without a history of aspiration, yet providers initially misdiagnose more than 20% of patients with a foreign body. The foreign object – often coins, food, or batteries – frequently ends up in the right main bronchus and may go undetected up to a month, potentially leading to pneumonia, abscess, atelectasis, bronchiectasis, or airway erosion.
An endobronchial cast is rarer than a foreign body, but can be large enough to completely fill a lung with branching mucin, fibrin, and inflammatory cells. The wheezing sounds homophonous, with a barky or brassy cough accompanied by atelectasis. Dr. Hysinger recommended ordering chest x-ray, echocardiogram, and bronchoscopy. Although often idiopathic, these casts also can result from asthma or another disease: neutrophilic inflammation typically indicates a heart condition whereas asthma or influenza leads to eosinophilic inflammation.
Treatment should involve clearing the airway, followed by hypertonic saline, an inhaled tissue plasminogen activator, and a bronchoscopy for extraction.
Although distinct from endobronchial casts, a mucus plug also presents with wheezing, a cough, and atelectasis, and potentially respiratory distress or failure, and hypoxemia. Mucus plugs are diagnosed with a chest x-ray and flexible bronchoscopy, and then treated by removing the plug and clearing the airway, hypertonic saline, and mucolytics.
The rarest cause of an airway blockage is an airway tumor, often mistaken for asthma. Benign causes include papillomatosis, hemangioma, and hamartomas, while potentially malignant causes include a carcinoid, mucoepidermoid carcinoma, inflammatory myofibromas, and granular cell tumors.
In addition to a chest x-ray and bronchoscopy, a chest CT scan plus a biopsy and resection are necessary to diagnose airway tumors. Treatment will depend on the specific type of tumor identified.
“Overall survival is excellent,” Dr. Hysinger said of children with airway tumors.
Airway narrowing diagnoses
Two possible diagnoses for an intrinsic airway narrowing include bronchomalacia, occurring in only 1 of 2,100 children, and bronchial stenosis.
In bronchomalacia – diagnosed primarily with bronchoscopy – the airway collapses from weakening of the cartilage and posterior membrane. Bronchomalacia sounds like homophonous wheezing with a barky or brassy cough, and it’s frequently accompanied by recurrent bronchitis and/or pneumonia. Intervention is rarely necessary when occurring on its own, but severe cases may require endobronchial stents. Dr. Hysinger also recommended considering ipratroprium instead of albuterol.
Bronchial stenosis involves a fixed narrowing of the bronchi and can be congenital – typically occurring with heart disease – or acquired after an intubation and suction trauma or bronchiolitis obliterans (“popcorn lung”). A chest x-ray and bronchoscopy again are standard, but MRI may be necessary as well. Aside from helping the patient clear the airway, bronchial stenosis typically needs limited management unless the patient is symptomatic. In that case, options include balloon dilation, endobronchial stents, or a slide bronchoplasty.
Airway compression diagnoses
An extrinsic airway compression could have a vascular cause or could result from pressure by an extrinsic mass or the axial skeleton.
Vascular compression usually occurs due to abnormal vasculature development, particularly with vascular stents, Dr. Hysinger said. The wheezing presents with stridor, feeding intolerance, recurrent infections, and cyanotic episodes. The work-up should include a chest x-ray, bronchoscopy, and a chest CT and/or MRI. A variety of interventions may be necessary to treat it, including an aortopexy, pulmonary artery trunk–pexy, arterioplasty, vessel implantation, or endobronchial stent. Residual malacia may remain after treatment, however.
The most common reasons for airway compression by some kind of mass is a reactive lymphadenopathy, a tumor, or an infection, including tuberculosis or histoplasmosis. Severe narrowing of the airway can lead to respiratory failure, but because the compression can develop slowly, the wheezing can be mistaken for asthma. In addition to a chest CT and bronchoscopy, a patient will need other work-ups depending on the cause. Possibilities include a biopsy, a gastric aspirate (for tuberculosis), a bronchoalveolar lavage, or antibody titers.
Similarly, because therapeutic intervention requires treating the underlying infection, specific treatments will vary. Tumors typically will need resection, chemotherapy, and/or radiation – and, until the airway is fully cleared, the patient may need chronic mechanical ventilation.
Children with severe scoliosis or kyphosis are those most likely to experience airway compression resulting from pressure by the axial skeleton, in which the spine’s curvature directly presses on the airway. In addition to the wheeze, these patients may have respiratory distress or recurrent focal pneumonia, Dr. Hysinger said. The standard work-up involves a chest x-ray, chest CT, spinal MRI, and bronchoscopy.
Consider using spinal rods, but they can both help the condition or potentially exacerbate the compression, Dr. Hysinger said. Either way, children also will need help with airway clearance and coughing.
Dr. Hysinger concluded by reviewing what you may consider changing in your current practice, including the initial trial of bronchodilators, a chest x-ray, and a subspecialist referral.
No funding was used for this presentation, and Dr. Hysinger reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 2017
Sorting out syncope signs and symptoms in kids remains essential
CHICAGO – Syncope often is misdiagnosed in pediatric patients complaining of chest pain, and a new guideline released in 2017 could guide clinicians toward a more accurate differential diagnosis and help them know when immediate referral to cardiology or the emergency department is warranted.
“There are recent guidelines published this year which are helpful,” said Dr. Barbara Deal, the Getz Professor of Cardiology at Northwestern University in Chicago. “,” which is defined as transient loss of consciousness.
“Once you establish it is a simple vasovagal [cause], you need to educate patients on conditions that would promote this and the need to be anticipatory,” Dr. Deal said at the annual meeting of the American Academy of Pediatrics. “Further testing with an echo[cardiogram] should be done if you suspect heart disease or a rhythm disorder.”
Chest pain and syncope are common complaints that can lead to significant anxiety for patients, parents, and pediatric providers. The greatest cause of this anxiety is the prospect of a fatal or near-fatal event. An abnormal cardiac examination, any associated palpitations, and a history of urinary incontinence or traumatic injury are reasons to worry, she said. “Any of these should prompt an urgent consult to cardiology or the emergency department.”
Cardiac causes of chest pain include reflex or vasovagal syncope or even a more serious cardiac cause, such as arrhythmic or structural issues, Dr. Deal said. Symptoms that appear with exertion or stress also are very worrisome. “You would know if they have a heart murmur or stenosis – it’s these other things that don’t present with a cardiac abnormality: hypertrophic cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy,” she said. “If they have symptoms on exertion, pay attention. This is not good.”
Syncope often is misdiagnosed, Dr. Deal said. Approximately 35%-48% of patients classified as having syncope do not have actual syncope;rather they experience dizziness rather than a loss of consciousness. In a study of 194 children, for example, the leading etiologies diagnosed after evaluation for syncope included simple fainting in 49%, a vasopressor/vasovagal response in 14%, and possible seizure in 14% (J Am Coll Cardiol. 1997;29[6]:1039-45). Seven percent were diagnosed with syncope not otherwise specified in this series. Some other causes included psychogenic or orthostatic ones, hyperventilation, dysmenorrhea, vertigo, dehydration, trauma, stress, exhaustion, or an infectious condition.*
“When should you be thinking life-threatening syncope?” Dr. Deal asked. Arrhythmic disorders that are heritable, such as an ion channelopathy, are an example. “They don’t always feel the racing heartbeat, but they feel something is not right; they feel a sense of impending doom. Some families report signs during exercise like swimming, seizures, gargling noises, or unusual symptoms on awakening.”
Dr. Deal noted that ages 3-24 years are “the problem territory for cardiac arrest.” In this age group, 43%-55% of cardiac arrests are associated with hypertrophic cardiomyopathy or arrhythmias; about one in three will have prior syncope. “These causes are not detectable on physical examination and often are not detectable with ECG only,” adding to the differential diagnosis challenges.*
Refer to a pediatric cardiologist
For this reason and others, referral to a pediatric cardiologist is indicated instead of a consult with an adult cardiologist, Dr. Deal said. “You know how your kids will start with ‘no offense.’ Like, ‘no offense, Mom, but your hair looks awful.’ With moderate offense intended, having an adult cardiologist read a pediatric ECG and clear them is not adequate. They will be looking for ischemia or A-fib [atrial fibrillation]; they’re not looking for long QT syndrome, arrhythmogenic cardiomyopathy, or abnormal T waves.”
Early detection of long QT syndrome is optimal, Dr. Deal said, because symptom onset often is between infancy and age 7 years. In addition, mortality is highest in the first 2 decades of life. “I think this could be why adult cardiologists are not as concerned as we are,” Dr. Deal said. “The bad ones die before they reach adulthood.”
Ruling out a cardiac cause
The 2017 joint guideline defined syncope as a transient loss of consciousness. “By definition, you pass out, you’re not aware of where you are, and you cannot hear,” Dr. Deal said. If a patient reports they could hear people talking, they may have lost postural tone, but they did not have syncope, she added.
“Sometimes, we see teenagers who are said to pass out and are unresponsive for 5 minutes, 10 minutes, or 20 minutes. I’m usually relieved to hear that because that gets cardiac off the hook,” Dr. Deal said. “There is nothing cardiac that makes you pass out for 20 minutes, unless people are resuscitating you.” She added, “I’m not suggesting it’s not a significant problem that you need to get to the bottom of.”
Noncardiac etiologies can be neurologic, metabolic, drug-induced, or psychogenic. “This is where the detective work comes in.”
Keep clinical suspicion high for psychogenic syncope, Dr. Deal said. Psychogenic episodes stem from significant psychological stress, often something so profoundly bothersome that they cannot cope, such as sexual abuse.
A helpful tip for diagnosing the less worrisome vasovagal syncope is asking whether a patient was sitting to standing or standing a long time before an episode, Dr. Deal said. “A common complaint is that the family went to airport, got up early, didn’t eat, and ended up standing for a long time. Kids will say they don’t feel well, they fall down, and all hell breaks loose.” Other causes of vasovagal syncope include stress, pain, or a situational trigger, for example, when a person faints during a blood draw or immunization.
The 2017 guideline also set forth the evidence behind various medications used to lower the risk of syncope. However, Dr. Deal said, “If syncope only happens every 3 years when you go to an airport, it’s probably not worth daily therapy to prevent that.”
‘The world’s most boring test’
For the most part, lifestyle measures should work to address vasovagal syncope. A tilt table test can be useful to aid the differential diagnosis, but it’s recommended only when the etiology is unclear, Dr. Deal said. On the plus side, the tilt table test allows clinicians to reproduce symptoms in a controlled environment. On the downside, she added, “It’s the world’s most boring test. It’s a challenge for the cardiologist to stay awake. It’s very boring, until all hell breaks loose.”
“I find this helpful in the setting of kids with seizures and for kids with this atypical syncope where you just cannot convince the family that these 20-minute episodes of loss of consciousness are not near-death episodes.”
Dr. Deal had no relevant financial disclosures.
*This article was updated on 10/25/2017.
CHICAGO – Syncope often is misdiagnosed in pediatric patients complaining of chest pain, and a new guideline released in 2017 could guide clinicians toward a more accurate differential diagnosis and help them know when immediate referral to cardiology or the emergency department is warranted.
“There are recent guidelines published this year which are helpful,” said Dr. Barbara Deal, the Getz Professor of Cardiology at Northwestern University in Chicago. “,” which is defined as transient loss of consciousness.
“Once you establish it is a simple vasovagal [cause], you need to educate patients on conditions that would promote this and the need to be anticipatory,” Dr. Deal said at the annual meeting of the American Academy of Pediatrics. “Further testing with an echo[cardiogram] should be done if you suspect heart disease or a rhythm disorder.”
Chest pain and syncope are common complaints that can lead to significant anxiety for patients, parents, and pediatric providers. The greatest cause of this anxiety is the prospect of a fatal or near-fatal event. An abnormal cardiac examination, any associated palpitations, and a history of urinary incontinence or traumatic injury are reasons to worry, she said. “Any of these should prompt an urgent consult to cardiology or the emergency department.”
Cardiac causes of chest pain include reflex or vasovagal syncope or even a more serious cardiac cause, such as arrhythmic or structural issues, Dr. Deal said. Symptoms that appear with exertion or stress also are very worrisome. “You would know if they have a heart murmur or stenosis – it’s these other things that don’t present with a cardiac abnormality: hypertrophic cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy,” she said. “If they have symptoms on exertion, pay attention. This is not good.”
Syncope often is misdiagnosed, Dr. Deal said. Approximately 35%-48% of patients classified as having syncope do not have actual syncope;rather they experience dizziness rather than a loss of consciousness. In a study of 194 children, for example, the leading etiologies diagnosed after evaluation for syncope included simple fainting in 49%, a vasopressor/vasovagal response in 14%, and possible seizure in 14% (J Am Coll Cardiol. 1997;29[6]:1039-45). Seven percent were diagnosed with syncope not otherwise specified in this series. Some other causes included psychogenic or orthostatic ones, hyperventilation, dysmenorrhea, vertigo, dehydration, trauma, stress, exhaustion, or an infectious condition.*
“When should you be thinking life-threatening syncope?” Dr. Deal asked. Arrhythmic disorders that are heritable, such as an ion channelopathy, are an example. “They don’t always feel the racing heartbeat, but they feel something is not right; they feel a sense of impending doom. Some families report signs during exercise like swimming, seizures, gargling noises, or unusual symptoms on awakening.”
Dr. Deal noted that ages 3-24 years are “the problem territory for cardiac arrest.” In this age group, 43%-55% of cardiac arrests are associated with hypertrophic cardiomyopathy or arrhythmias; about one in three will have prior syncope. “These causes are not detectable on physical examination and often are not detectable with ECG only,” adding to the differential diagnosis challenges.*
Refer to a pediatric cardiologist
For this reason and others, referral to a pediatric cardiologist is indicated instead of a consult with an adult cardiologist, Dr. Deal said. “You know how your kids will start with ‘no offense.’ Like, ‘no offense, Mom, but your hair looks awful.’ With moderate offense intended, having an adult cardiologist read a pediatric ECG and clear them is not adequate. They will be looking for ischemia or A-fib [atrial fibrillation]; they’re not looking for long QT syndrome, arrhythmogenic cardiomyopathy, or abnormal T waves.”
Early detection of long QT syndrome is optimal, Dr. Deal said, because symptom onset often is between infancy and age 7 years. In addition, mortality is highest in the first 2 decades of life. “I think this could be why adult cardiologists are not as concerned as we are,” Dr. Deal said. “The bad ones die before they reach adulthood.”
Ruling out a cardiac cause
The 2017 joint guideline defined syncope as a transient loss of consciousness. “By definition, you pass out, you’re not aware of where you are, and you cannot hear,” Dr. Deal said. If a patient reports they could hear people talking, they may have lost postural tone, but they did not have syncope, she added.
“Sometimes, we see teenagers who are said to pass out and are unresponsive for 5 minutes, 10 minutes, or 20 minutes. I’m usually relieved to hear that because that gets cardiac off the hook,” Dr. Deal said. “There is nothing cardiac that makes you pass out for 20 minutes, unless people are resuscitating you.” She added, “I’m not suggesting it’s not a significant problem that you need to get to the bottom of.”
Noncardiac etiologies can be neurologic, metabolic, drug-induced, or psychogenic. “This is where the detective work comes in.”
Keep clinical suspicion high for psychogenic syncope, Dr. Deal said. Psychogenic episodes stem from significant psychological stress, often something so profoundly bothersome that they cannot cope, such as sexual abuse.
A helpful tip for diagnosing the less worrisome vasovagal syncope is asking whether a patient was sitting to standing or standing a long time before an episode, Dr. Deal said. “A common complaint is that the family went to airport, got up early, didn’t eat, and ended up standing for a long time. Kids will say they don’t feel well, they fall down, and all hell breaks loose.” Other causes of vasovagal syncope include stress, pain, or a situational trigger, for example, when a person faints during a blood draw or immunization.
The 2017 guideline also set forth the evidence behind various medications used to lower the risk of syncope. However, Dr. Deal said, “If syncope only happens every 3 years when you go to an airport, it’s probably not worth daily therapy to prevent that.”
‘The world’s most boring test’
For the most part, lifestyle measures should work to address vasovagal syncope. A tilt table test can be useful to aid the differential diagnosis, but it’s recommended only when the etiology is unclear, Dr. Deal said. On the plus side, the tilt table test allows clinicians to reproduce symptoms in a controlled environment. On the downside, she added, “It’s the world’s most boring test. It’s a challenge for the cardiologist to stay awake. It’s very boring, until all hell breaks loose.”
“I find this helpful in the setting of kids with seizures and for kids with this atypical syncope where you just cannot convince the family that these 20-minute episodes of loss of consciousness are not near-death episodes.”
Dr. Deal had no relevant financial disclosures.
*This article was updated on 10/25/2017.
CHICAGO – Syncope often is misdiagnosed in pediatric patients complaining of chest pain, and a new guideline released in 2017 could guide clinicians toward a more accurate differential diagnosis and help them know when immediate referral to cardiology or the emergency department is warranted.
“There are recent guidelines published this year which are helpful,” said Dr. Barbara Deal, the Getz Professor of Cardiology at Northwestern University in Chicago. “,” which is defined as transient loss of consciousness.
“Once you establish it is a simple vasovagal [cause], you need to educate patients on conditions that would promote this and the need to be anticipatory,” Dr. Deal said at the annual meeting of the American Academy of Pediatrics. “Further testing with an echo[cardiogram] should be done if you suspect heart disease or a rhythm disorder.”
Chest pain and syncope are common complaints that can lead to significant anxiety for patients, parents, and pediatric providers. The greatest cause of this anxiety is the prospect of a fatal or near-fatal event. An abnormal cardiac examination, any associated palpitations, and a history of urinary incontinence or traumatic injury are reasons to worry, she said. “Any of these should prompt an urgent consult to cardiology or the emergency department.”
Cardiac causes of chest pain include reflex or vasovagal syncope or even a more serious cardiac cause, such as arrhythmic or structural issues, Dr. Deal said. Symptoms that appear with exertion or stress also are very worrisome. “You would know if they have a heart murmur or stenosis – it’s these other things that don’t present with a cardiac abnormality: hypertrophic cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy,” she said. “If they have symptoms on exertion, pay attention. This is not good.”
Syncope often is misdiagnosed, Dr. Deal said. Approximately 35%-48% of patients classified as having syncope do not have actual syncope;rather they experience dizziness rather than a loss of consciousness. In a study of 194 children, for example, the leading etiologies diagnosed after evaluation for syncope included simple fainting in 49%, a vasopressor/vasovagal response in 14%, and possible seizure in 14% (J Am Coll Cardiol. 1997;29[6]:1039-45). Seven percent were diagnosed with syncope not otherwise specified in this series. Some other causes included psychogenic or orthostatic ones, hyperventilation, dysmenorrhea, vertigo, dehydration, trauma, stress, exhaustion, or an infectious condition.*
“When should you be thinking life-threatening syncope?” Dr. Deal asked. Arrhythmic disorders that are heritable, such as an ion channelopathy, are an example. “They don’t always feel the racing heartbeat, but they feel something is not right; they feel a sense of impending doom. Some families report signs during exercise like swimming, seizures, gargling noises, or unusual symptoms on awakening.”
Dr. Deal noted that ages 3-24 years are “the problem territory for cardiac arrest.” In this age group, 43%-55% of cardiac arrests are associated with hypertrophic cardiomyopathy or arrhythmias; about one in three will have prior syncope. “These causes are not detectable on physical examination and often are not detectable with ECG only,” adding to the differential diagnosis challenges.*
Refer to a pediatric cardiologist
For this reason and others, referral to a pediatric cardiologist is indicated instead of a consult with an adult cardiologist, Dr. Deal said. “You know how your kids will start with ‘no offense.’ Like, ‘no offense, Mom, but your hair looks awful.’ With moderate offense intended, having an adult cardiologist read a pediatric ECG and clear them is not adequate. They will be looking for ischemia or A-fib [atrial fibrillation]; they’re not looking for long QT syndrome, arrhythmogenic cardiomyopathy, or abnormal T waves.”
Early detection of long QT syndrome is optimal, Dr. Deal said, because symptom onset often is between infancy and age 7 years. In addition, mortality is highest in the first 2 decades of life. “I think this could be why adult cardiologists are not as concerned as we are,” Dr. Deal said. “The bad ones die before they reach adulthood.”
Ruling out a cardiac cause
The 2017 joint guideline defined syncope as a transient loss of consciousness. “By definition, you pass out, you’re not aware of where you are, and you cannot hear,” Dr. Deal said. If a patient reports they could hear people talking, they may have lost postural tone, but they did not have syncope, she added.
“Sometimes, we see teenagers who are said to pass out and are unresponsive for 5 minutes, 10 minutes, or 20 minutes. I’m usually relieved to hear that because that gets cardiac off the hook,” Dr. Deal said. “There is nothing cardiac that makes you pass out for 20 minutes, unless people are resuscitating you.” She added, “I’m not suggesting it’s not a significant problem that you need to get to the bottom of.”
Noncardiac etiologies can be neurologic, metabolic, drug-induced, or psychogenic. “This is where the detective work comes in.”
Keep clinical suspicion high for psychogenic syncope, Dr. Deal said. Psychogenic episodes stem from significant psychological stress, often something so profoundly bothersome that they cannot cope, such as sexual abuse.
A helpful tip for diagnosing the less worrisome vasovagal syncope is asking whether a patient was sitting to standing or standing a long time before an episode, Dr. Deal said. “A common complaint is that the family went to airport, got up early, didn’t eat, and ended up standing for a long time. Kids will say they don’t feel well, they fall down, and all hell breaks loose.” Other causes of vasovagal syncope include stress, pain, or a situational trigger, for example, when a person faints during a blood draw or immunization.
The 2017 guideline also set forth the evidence behind various medications used to lower the risk of syncope. However, Dr. Deal said, “If syncope only happens every 3 years when you go to an airport, it’s probably not worth daily therapy to prevent that.”
‘The world’s most boring test’
For the most part, lifestyle measures should work to address vasovagal syncope. A tilt table test can be useful to aid the differential diagnosis, but it’s recommended only when the etiology is unclear, Dr. Deal said. On the plus side, the tilt table test allows clinicians to reproduce symptoms in a controlled environment. On the downside, she added, “It’s the world’s most boring test. It’s a challenge for the cardiologist to stay awake. It’s very boring, until all hell breaks loose.”
“I find this helpful in the setting of kids with seizures and for kids with this atypical syncope where you just cannot convince the family that these 20-minute episodes of loss of consciousness are not near-death episodes.”
Dr. Deal had no relevant financial disclosures.
*This article was updated on 10/25/2017.
EXPERT ANALYSIS FROM AAP 2017
Evidence is mixed on probiotics in pediatric patients
CHICAGO – Outside of that, things are less clear.
“In terms of diarrhea, the evidence is positive, but probiotics only provide about 25 hours of benefit. And treatment of antibiotic-associated diarrhea is really dependent on patient adherence,” said Michael D. Cabana, MD. When it comes to treating colic, there is a particular probiotic that looks promising, he added, but the research so far demonstrating effectiveness is limited to breastfed babies. Also, the probiotic therapy appears to work best when started relatively early.
You are very likely to be asked your take on probiotics for a wide range of conditions, Dr. Cabana said, Overall, however, skepticism is warranted. Advise patients and families to be aware of advertising that promotes many different products as “probiotic,” especially around claims of improved “gut health” or “balanced microbiota.” He emphasized: “Make sure what your patients are using has some evidence behind it.”
Knowing the particular probiotic strain is essential to researching the evidence around its use, said Dr. Cabana, professor of pediatrics at the University of California, San Francisco. “I used the Canis familiaris example. All dogs are C. familiaris. But there are different breeds. You want to make sure you match the right breed to the task. If you were in an avalanche in the Swiss Alps, you would want a St. Bernard to rescue you, not a Chihuahua,” he said. “Similarly, when you are using probiotics you want to make sure you have the right strain, not just the genus and species.” For example, if a product label states it contains Bifidobacterium breve C50, the “C50” is the strain.
Another tip is to look for labeling that lists probiotic concentrations in colony-forming units or CFUs, Dr. Cabana said. He’s seen concentrations listed in mg, a red flag that a product is not legitimate.
Families also might ask if it’s better to take a probiotic supplement or choose food that contains probiotics. “Food products offer additional nutritional benefits, but you can give a relatively higher dose with supplements with a much lower volume ingested,” Dr. Cabana said. “And supplements theoretically provide a more consistent dose.” Speaking of dose, it’s difficult to counsel patients on dosing and frequency in general because probiotics really vary by the indication and formulation.
“As a pediatrician, I also get this question: Should kids get a lower dose of probiotic?” Dr. Cabana said. There are no known reports of toxicity associated with probiotic use in either adults or children, he said. “Unless a dose modification has been documented in a clinical trial, it is not clear that this is necessary. You’re just giving less of the probiotic.”
Treating diarrhea and antibiotic-associated diarrhea
When it comes to probiotics for treating acute diarrhea in children, “the literature is actually fairly good here,” Dr. Cabana said. More than 60 studies with an excess of 8,000 participants, the majority with rotavirus infection, suggests probiotics are not associated with any adverse effects and generally shorten duration of diarrhea.
In fact, Dr. Cabana added, multiple meta-analyses support a shorter course of diarrhea. He added, “Look at the units here – it’s hours, not days. You can treat, but on average it’s only 25 hours.” He added that a day less of diarrhea can be significant for patients and parents, however.
In another meta-analysis probiotics, particularly Lactobacillus strains, were analyzed for prevention of antibiotic-associated diarrhea (JAMA. 2012 May 9;307[18]:1959-69). Researchers assessed 63 randomized controlled trials with nearly 12,000 participants. The pooled results showed a statistically significant positive reduction in antibiotic-associated diarrhea (relative risk, 0.58; P less than .001). “Note the number needed to treat to see the effect is 13, so it won’t work in every patient,” Dr. Cabana said.
“So prevention of antibiotic-associated diarrhea is well documented. However, it’s also highly dependent on patent adherence,” he emphasized.
The clinical evidence on colic
For treating babies with colic, the best evidence is behind use of Lactobacilus reuteri DSM 17938, Dr. Cabana said. It tends to work best in breastfed infants, babies not on any gastrointestinal meds, and babies that start therapy early in the course of symptoms. “Use in formula-fed infants is unknown, because there are not enough data so far,” he said.
In some cases, during a prenatal visit, soon-to-be-parents will ask if they should start a probiotic to prevent colic. Dr. Cabana has seen only one prophylaxis study for this indication (JAMA Pediatr. 2014 Mar;168[3]:228-33). In the study, 589 infants were randomly allocated to take L. reuteri DSM 17938 or placebo daily for 90 days. At 3 months of age, the researchers discovered a significantly shorter mean duration of daily crying in the probiotic group (38 vs. 71 minutes; P less than .01).
What’s known about efficacy for eczema
The evidence for treating a child who presents with eczema with probiotics does not support efficacy in general, Dr. Cabana said. And the evidence on prevention of atopic eczema is mixed.
For example, in a randomized, controlled study from Finland, investigators randomized mothers to receive Lactobacillus GG or placebo during the prenatal period (Lancet. 2001;357:1076-9). Of 132 of the children, 35% were later diagnosed with atopic eczema, and the rate in the probiotic group, 23%, was half the 46% rate in the placebo group.
In contrast, researchers found no benefit regarding prevention of atopic dermatitis when 105 pregnant women were randomized to Lactobacillus GG or placebo. At the age of 2 years, atopic dermatitis was diagnosed in 28% of the 50 children in the probiotic group and 27.3% of the 44 in the placebo group (Pediatrics. 2008;121:e850-6).
The region of Germany where the study was conducted was rural/agricultural, so the diet could be different, Dr. Cabana said. Also, the median duration of breastfeeding differed between the Finnish and German study population, 6.8 months versus 9.2 months, respectively. “So that could potentially explain it, or there are just differences that cannot be explained.”
For more information, Dr. Cabana recommended information provided by the International Scientific Association of Prebiotics & Probiotics (https://isappscience.org/infographics/). The association’s website has easy to understand infographics including: What are probiotics and what can they do for you?; What’s so special about fermented foods?; and How do you read a probiotic label?
Dr. Cabana reported he receives research support from the National Institutes of Health, Wyeth Nutrition, and Nestle; is on the speakers bureau for Merck; owns stocks or bonds in Abbot and AbbVie; and is a consultant for Mead Johnson, Abbott, Genentech, Biogaia, General Mills, and Nestle.
CHICAGO – Outside of that, things are less clear.
“In terms of diarrhea, the evidence is positive, but probiotics only provide about 25 hours of benefit. And treatment of antibiotic-associated diarrhea is really dependent on patient adherence,” said Michael D. Cabana, MD. When it comes to treating colic, there is a particular probiotic that looks promising, he added, but the research so far demonstrating effectiveness is limited to breastfed babies. Also, the probiotic therapy appears to work best when started relatively early.
You are very likely to be asked your take on probiotics for a wide range of conditions, Dr. Cabana said, Overall, however, skepticism is warranted. Advise patients and families to be aware of advertising that promotes many different products as “probiotic,” especially around claims of improved “gut health” or “balanced microbiota.” He emphasized: “Make sure what your patients are using has some evidence behind it.”
Knowing the particular probiotic strain is essential to researching the evidence around its use, said Dr. Cabana, professor of pediatrics at the University of California, San Francisco. “I used the Canis familiaris example. All dogs are C. familiaris. But there are different breeds. You want to make sure you match the right breed to the task. If you were in an avalanche in the Swiss Alps, you would want a St. Bernard to rescue you, not a Chihuahua,” he said. “Similarly, when you are using probiotics you want to make sure you have the right strain, not just the genus and species.” For example, if a product label states it contains Bifidobacterium breve C50, the “C50” is the strain.
Another tip is to look for labeling that lists probiotic concentrations in colony-forming units or CFUs, Dr. Cabana said. He’s seen concentrations listed in mg, a red flag that a product is not legitimate.
Families also might ask if it’s better to take a probiotic supplement or choose food that contains probiotics. “Food products offer additional nutritional benefits, but you can give a relatively higher dose with supplements with a much lower volume ingested,” Dr. Cabana said. “And supplements theoretically provide a more consistent dose.” Speaking of dose, it’s difficult to counsel patients on dosing and frequency in general because probiotics really vary by the indication and formulation.
“As a pediatrician, I also get this question: Should kids get a lower dose of probiotic?” Dr. Cabana said. There are no known reports of toxicity associated with probiotic use in either adults or children, he said. “Unless a dose modification has been documented in a clinical trial, it is not clear that this is necessary. You’re just giving less of the probiotic.”
Treating diarrhea and antibiotic-associated diarrhea
When it comes to probiotics for treating acute diarrhea in children, “the literature is actually fairly good here,” Dr. Cabana said. More than 60 studies with an excess of 8,000 participants, the majority with rotavirus infection, suggests probiotics are not associated with any adverse effects and generally shorten duration of diarrhea.
In fact, Dr. Cabana added, multiple meta-analyses support a shorter course of diarrhea. He added, “Look at the units here – it’s hours, not days. You can treat, but on average it’s only 25 hours.” He added that a day less of diarrhea can be significant for patients and parents, however.
In another meta-analysis probiotics, particularly Lactobacillus strains, were analyzed for prevention of antibiotic-associated diarrhea (JAMA. 2012 May 9;307[18]:1959-69). Researchers assessed 63 randomized controlled trials with nearly 12,000 participants. The pooled results showed a statistically significant positive reduction in antibiotic-associated diarrhea (relative risk, 0.58; P less than .001). “Note the number needed to treat to see the effect is 13, so it won’t work in every patient,” Dr. Cabana said.
“So prevention of antibiotic-associated diarrhea is well documented. However, it’s also highly dependent on patent adherence,” he emphasized.
The clinical evidence on colic
For treating babies with colic, the best evidence is behind use of Lactobacilus reuteri DSM 17938, Dr. Cabana said. It tends to work best in breastfed infants, babies not on any gastrointestinal meds, and babies that start therapy early in the course of symptoms. “Use in formula-fed infants is unknown, because there are not enough data so far,” he said.
In some cases, during a prenatal visit, soon-to-be-parents will ask if they should start a probiotic to prevent colic. Dr. Cabana has seen only one prophylaxis study for this indication (JAMA Pediatr. 2014 Mar;168[3]:228-33). In the study, 589 infants were randomly allocated to take L. reuteri DSM 17938 or placebo daily for 90 days. At 3 months of age, the researchers discovered a significantly shorter mean duration of daily crying in the probiotic group (38 vs. 71 minutes; P less than .01).
What’s known about efficacy for eczema
The evidence for treating a child who presents with eczema with probiotics does not support efficacy in general, Dr. Cabana said. And the evidence on prevention of atopic eczema is mixed.
For example, in a randomized, controlled study from Finland, investigators randomized mothers to receive Lactobacillus GG or placebo during the prenatal period (Lancet. 2001;357:1076-9). Of 132 of the children, 35% were later diagnosed with atopic eczema, and the rate in the probiotic group, 23%, was half the 46% rate in the placebo group.
In contrast, researchers found no benefit regarding prevention of atopic dermatitis when 105 pregnant women were randomized to Lactobacillus GG or placebo. At the age of 2 years, atopic dermatitis was diagnosed in 28% of the 50 children in the probiotic group and 27.3% of the 44 in the placebo group (Pediatrics. 2008;121:e850-6).
The region of Germany where the study was conducted was rural/agricultural, so the diet could be different, Dr. Cabana said. Also, the median duration of breastfeeding differed between the Finnish and German study population, 6.8 months versus 9.2 months, respectively. “So that could potentially explain it, or there are just differences that cannot be explained.”
For more information, Dr. Cabana recommended information provided by the International Scientific Association of Prebiotics & Probiotics (https://isappscience.org/infographics/). The association’s website has easy to understand infographics including: What are probiotics and what can they do for you?; What’s so special about fermented foods?; and How do you read a probiotic label?
Dr. Cabana reported he receives research support from the National Institutes of Health, Wyeth Nutrition, and Nestle; is on the speakers bureau for Merck; owns stocks or bonds in Abbot and AbbVie; and is a consultant for Mead Johnson, Abbott, Genentech, Biogaia, General Mills, and Nestle.
CHICAGO – Outside of that, things are less clear.
“In terms of diarrhea, the evidence is positive, but probiotics only provide about 25 hours of benefit. And treatment of antibiotic-associated diarrhea is really dependent on patient adherence,” said Michael D. Cabana, MD. When it comes to treating colic, there is a particular probiotic that looks promising, he added, but the research so far demonstrating effectiveness is limited to breastfed babies. Also, the probiotic therapy appears to work best when started relatively early.
You are very likely to be asked your take on probiotics for a wide range of conditions, Dr. Cabana said, Overall, however, skepticism is warranted. Advise patients and families to be aware of advertising that promotes many different products as “probiotic,” especially around claims of improved “gut health” or “balanced microbiota.” He emphasized: “Make sure what your patients are using has some evidence behind it.”
Knowing the particular probiotic strain is essential to researching the evidence around its use, said Dr. Cabana, professor of pediatrics at the University of California, San Francisco. “I used the Canis familiaris example. All dogs are C. familiaris. But there are different breeds. You want to make sure you match the right breed to the task. If you were in an avalanche in the Swiss Alps, you would want a St. Bernard to rescue you, not a Chihuahua,” he said. “Similarly, when you are using probiotics you want to make sure you have the right strain, not just the genus and species.” For example, if a product label states it contains Bifidobacterium breve C50, the “C50” is the strain.
Another tip is to look for labeling that lists probiotic concentrations in colony-forming units or CFUs, Dr. Cabana said. He’s seen concentrations listed in mg, a red flag that a product is not legitimate.
Families also might ask if it’s better to take a probiotic supplement or choose food that contains probiotics. “Food products offer additional nutritional benefits, but you can give a relatively higher dose with supplements with a much lower volume ingested,” Dr. Cabana said. “And supplements theoretically provide a more consistent dose.” Speaking of dose, it’s difficult to counsel patients on dosing and frequency in general because probiotics really vary by the indication and formulation.
“As a pediatrician, I also get this question: Should kids get a lower dose of probiotic?” Dr. Cabana said. There are no known reports of toxicity associated with probiotic use in either adults or children, he said. “Unless a dose modification has been documented in a clinical trial, it is not clear that this is necessary. You’re just giving less of the probiotic.”
Treating diarrhea and antibiotic-associated diarrhea
When it comes to probiotics for treating acute diarrhea in children, “the literature is actually fairly good here,” Dr. Cabana said. More than 60 studies with an excess of 8,000 participants, the majority with rotavirus infection, suggests probiotics are not associated with any adverse effects and generally shorten duration of diarrhea.
In fact, Dr. Cabana added, multiple meta-analyses support a shorter course of diarrhea. He added, “Look at the units here – it’s hours, not days. You can treat, but on average it’s only 25 hours.” He added that a day less of diarrhea can be significant for patients and parents, however.
In another meta-analysis probiotics, particularly Lactobacillus strains, were analyzed for prevention of antibiotic-associated diarrhea (JAMA. 2012 May 9;307[18]:1959-69). Researchers assessed 63 randomized controlled trials with nearly 12,000 participants. The pooled results showed a statistically significant positive reduction in antibiotic-associated diarrhea (relative risk, 0.58; P less than .001). “Note the number needed to treat to see the effect is 13, so it won’t work in every patient,” Dr. Cabana said.
“So prevention of antibiotic-associated diarrhea is well documented. However, it’s also highly dependent on patent adherence,” he emphasized.
The clinical evidence on colic
For treating babies with colic, the best evidence is behind use of Lactobacilus reuteri DSM 17938, Dr. Cabana said. It tends to work best in breastfed infants, babies not on any gastrointestinal meds, and babies that start therapy early in the course of symptoms. “Use in formula-fed infants is unknown, because there are not enough data so far,” he said.
In some cases, during a prenatal visit, soon-to-be-parents will ask if they should start a probiotic to prevent colic. Dr. Cabana has seen only one prophylaxis study for this indication (JAMA Pediatr. 2014 Mar;168[3]:228-33). In the study, 589 infants were randomly allocated to take L. reuteri DSM 17938 or placebo daily for 90 days. At 3 months of age, the researchers discovered a significantly shorter mean duration of daily crying in the probiotic group (38 vs. 71 minutes; P less than .01).
What’s known about efficacy for eczema
The evidence for treating a child who presents with eczema with probiotics does not support efficacy in general, Dr. Cabana said. And the evidence on prevention of atopic eczema is mixed.
For example, in a randomized, controlled study from Finland, investigators randomized mothers to receive Lactobacillus GG or placebo during the prenatal period (Lancet. 2001;357:1076-9). Of 132 of the children, 35% were later diagnosed with atopic eczema, and the rate in the probiotic group, 23%, was half the 46% rate in the placebo group.
In contrast, researchers found no benefit regarding prevention of atopic dermatitis when 105 pregnant women were randomized to Lactobacillus GG or placebo. At the age of 2 years, atopic dermatitis was diagnosed in 28% of the 50 children in the probiotic group and 27.3% of the 44 in the placebo group (Pediatrics. 2008;121:e850-6).
The region of Germany where the study was conducted was rural/agricultural, so the diet could be different, Dr. Cabana said. Also, the median duration of breastfeeding differed between the Finnish and German study population, 6.8 months versus 9.2 months, respectively. “So that could potentially explain it, or there are just differences that cannot be explained.”
For more information, Dr. Cabana recommended information provided by the International Scientific Association of Prebiotics & Probiotics (https://isappscience.org/infographics/). The association’s website has easy to understand infographics including: What are probiotics and what can they do for you?; What’s so special about fermented foods?; and How do you read a probiotic label?
Dr. Cabana reported he receives research support from the National Institutes of Health, Wyeth Nutrition, and Nestle; is on the speakers bureau for Merck; owns stocks or bonds in Abbot and AbbVie; and is a consultant for Mead Johnson, Abbott, Genentech, Biogaia, General Mills, and Nestle.
EXPERT ANALYSIS FROM AAP 2017
Treatment of hemangioma with brand-name propranolol tied to fewer dosing errors
CHICAGO – Among physicians using generic propranolol to treat infantile hemangioma, 30% reported at least one patient experienced a miscalculation dosing error, a new survey showed. Among respondents who prescribed Hemangeol (Pierre Fabre Pharmaceuticals), 10% reported a similar error. The errors were made by either a provider or caregiver.
Confusion may have contributed to a second source of errors, said Elaine Siegfried, MD, professor of pediatrics and dermatology at St. Louis University in Missouri. Generic propranolol is supplied as a 20-mg/5-mL oral solution and a 40-mg/5-mL oral solution. “Any time you have more than one formulation, it’s a nidus for dispensing error by the pharmacy.”
“So if a doctor prescribes [the lower dose], which is what we always do for safety, and they get 40 [mg], the [patient] can become hypoglycemic, hypotensive, or bradycardic,” Dr. Siegfried said. “That’s not good.”
Dr. Siegfried and colleagues assessed survey responses from 223 physicians. The majority, 90%, reported prescribing generic propranolol to treat infantile hemangioma in the past. Sixty-percent reported also prescribing the brand name formulation approved by the Food and Drug Administration in 2014. Most of those who completed the survey, 70%, were pediatric dermatologists; general dermatologists, pediatric otolaryngologists, and other specialists also participated.
A total of 18% of physicians surveyed reported a dispensing error associated with use of generic propranolol. Dr. Siegfried said such errors are not possible with the branded formulation because it is available only in a single concentration, a 4.28 mg/mL oral solution. She added that one central specialty pharmacy dispenses Hemangeol, further reducing the likelihood of errors.
Addressing cost concerns
“When this [branded] drug became available, I wondered why everyone was not prescribing it,” Dr. Siegfried said.
“One of the pushbacks with this drug is that people didn’t want to prescribe it because they thought it was too expensive.” She acknowledged the higher cost, but added the manufacturer has a program to provide the agent free-of-charge to families without health insurance who cannot afford the medicine. She added, “People with private insurance do have higher copays, but insurance generally pays for most of it, depending on the plan.”
Dr. Siegfried also emphasized that the manufacturer invested considerable time and money to bring the agent and its specific pediatric indication to market, generating scientific data on its safety and efficacy along the way. In contrast, generic propranolol has been available in the United States for decades as a beta-blocker. The discovery that the agent also could effectively treat infantile hemangioma was serendipitous, not based on preclinical efficacy, safety, or dosing studies.
An additional benefit of the single-concentration branded formulation is pediatric clinicians might be more comfortable using this agent, Dr. Siegfried said. She described the package insert instructions as straightforward and easy to follow. Also, given a sometimes longer wait to see a pediatric dermatologist because of their shortage in certain parts of the country, having general pediatricians or family physicians gain proficiency in administering the medication could mean earlier treatment of hemangioma. “If you have to wait to get into a specialist, that can delay treatment. The caveat about hemangiomas is the earlier you treat them, the more effective the treatment is.”
“Using propranolol to treat hemangiomas is probably one of the biggest positive changes in my practice. It was very difficult to treat hemangiomas with steroids, vincristine, or other alternatives. Now treatment is ‘cookbook’ and well-tolerated. It’s amazing,” Dr. Siegfried said. “I only prescribe the branded propranolol because of the specialty pharmacy issue, because of the formulation issue, and because we have data that Pierre Fabre paid for,” she added.
Dr. Siegfried is a consultant for Pierre Fabre and served as a principle investigator on phase 3 research. The company did not sponsor the current study, but a coauthor and employee of Pierre Fabre assisted with the logistics of the survey.
CHICAGO – Among physicians using generic propranolol to treat infantile hemangioma, 30% reported at least one patient experienced a miscalculation dosing error, a new survey showed. Among respondents who prescribed Hemangeol (Pierre Fabre Pharmaceuticals), 10% reported a similar error. The errors were made by either a provider or caregiver.
Confusion may have contributed to a second source of errors, said Elaine Siegfried, MD, professor of pediatrics and dermatology at St. Louis University in Missouri. Generic propranolol is supplied as a 20-mg/5-mL oral solution and a 40-mg/5-mL oral solution. “Any time you have more than one formulation, it’s a nidus for dispensing error by the pharmacy.”
“So if a doctor prescribes [the lower dose], which is what we always do for safety, and they get 40 [mg], the [patient] can become hypoglycemic, hypotensive, or bradycardic,” Dr. Siegfried said. “That’s not good.”
Dr. Siegfried and colleagues assessed survey responses from 223 physicians. The majority, 90%, reported prescribing generic propranolol to treat infantile hemangioma in the past. Sixty-percent reported also prescribing the brand name formulation approved by the Food and Drug Administration in 2014. Most of those who completed the survey, 70%, were pediatric dermatologists; general dermatologists, pediatric otolaryngologists, and other specialists also participated.
A total of 18% of physicians surveyed reported a dispensing error associated with use of generic propranolol. Dr. Siegfried said such errors are not possible with the branded formulation because it is available only in a single concentration, a 4.28 mg/mL oral solution. She added that one central specialty pharmacy dispenses Hemangeol, further reducing the likelihood of errors.
Addressing cost concerns
“When this [branded] drug became available, I wondered why everyone was not prescribing it,” Dr. Siegfried said.
“One of the pushbacks with this drug is that people didn’t want to prescribe it because they thought it was too expensive.” She acknowledged the higher cost, but added the manufacturer has a program to provide the agent free-of-charge to families without health insurance who cannot afford the medicine. She added, “People with private insurance do have higher copays, but insurance generally pays for most of it, depending on the plan.”
Dr. Siegfried also emphasized that the manufacturer invested considerable time and money to bring the agent and its specific pediatric indication to market, generating scientific data on its safety and efficacy along the way. In contrast, generic propranolol has been available in the United States for decades as a beta-blocker. The discovery that the agent also could effectively treat infantile hemangioma was serendipitous, not based on preclinical efficacy, safety, or dosing studies.
An additional benefit of the single-concentration branded formulation is pediatric clinicians might be more comfortable using this agent, Dr. Siegfried said. She described the package insert instructions as straightforward and easy to follow. Also, given a sometimes longer wait to see a pediatric dermatologist because of their shortage in certain parts of the country, having general pediatricians or family physicians gain proficiency in administering the medication could mean earlier treatment of hemangioma. “If you have to wait to get into a specialist, that can delay treatment. The caveat about hemangiomas is the earlier you treat them, the more effective the treatment is.”
“Using propranolol to treat hemangiomas is probably one of the biggest positive changes in my practice. It was very difficult to treat hemangiomas with steroids, vincristine, or other alternatives. Now treatment is ‘cookbook’ and well-tolerated. It’s amazing,” Dr. Siegfried said. “I only prescribe the branded propranolol because of the specialty pharmacy issue, because of the formulation issue, and because we have data that Pierre Fabre paid for,” she added.
Dr. Siegfried is a consultant for Pierre Fabre and served as a principle investigator on phase 3 research. The company did not sponsor the current study, but a coauthor and employee of Pierre Fabre assisted with the logistics of the survey.
CHICAGO – Among physicians using generic propranolol to treat infantile hemangioma, 30% reported at least one patient experienced a miscalculation dosing error, a new survey showed. Among respondents who prescribed Hemangeol (Pierre Fabre Pharmaceuticals), 10% reported a similar error. The errors were made by either a provider or caregiver.
Confusion may have contributed to a second source of errors, said Elaine Siegfried, MD, professor of pediatrics and dermatology at St. Louis University in Missouri. Generic propranolol is supplied as a 20-mg/5-mL oral solution and a 40-mg/5-mL oral solution. “Any time you have more than one formulation, it’s a nidus for dispensing error by the pharmacy.”
“So if a doctor prescribes [the lower dose], which is what we always do for safety, and they get 40 [mg], the [patient] can become hypoglycemic, hypotensive, or bradycardic,” Dr. Siegfried said. “That’s not good.”
Dr. Siegfried and colleagues assessed survey responses from 223 physicians. The majority, 90%, reported prescribing generic propranolol to treat infantile hemangioma in the past. Sixty-percent reported also prescribing the brand name formulation approved by the Food and Drug Administration in 2014. Most of those who completed the survey, 70%, were pediatric dermatologists; general dermatologists, pediatric otolaryngologists, and other specialists also participated.
A total of 18% of physicians surveyed reported a dispensing error associated with use of generic propranolol. Dr. Siegfried said such errors are not possible with the branded formulation because it is available only in a single concentration, a 4.28 mg/mL oral solution. She added that one central specialty pharmacy dispenses Hemangeol, further reducing the likelihood of errors.
Addressing cost concerns
“When this [branded] drug became available, I wondered why everyone was not prescribing it,” Dr. Siegfried said.
“One of the pushbacks with this drug is that people didn’t want to prescribe it because they thought it was too expensive.” She acknowledged the higher cost, but added the manufacturer has a program to provide the agent free-of-charge to families without health insurance who cannot afford the medicine. She added, “People with private insurance do have higher copays, but insurance generally pays for most of it, depending on the plan.”
Dr. Siegfried also emphasized that the manufacturer invested considerable time and money to bring the agent and its specific pediatric indication to market, generating scientific data on its safety and efficacy along the way. In contrast, generic propranolol has been available in the United States for decades as a beta-blocker. The discovery that the agent also could effectively treat infantile hemangioma was serendipitous, not based on preclinical efficacy, safety, or dosing studies.
An additional benefit of the single-concentration branded formulation is pediatric clinicians might be more comfortable using this agent, Dr. Siegfried said. She described the package insert instructions as straightforward and easy to follow. Also, given a sometimes longer wait to see a pediatric dermatologist because of their shortage in certain parts of the country, having general pediatricians or family physicians gain proficiency in administering the medication could mean earlier treatment of hemangioma. “If you have to wait to get into a specialist, that can delay treatment. The caveat about hemangiomas is the earlier you treat them, the more effective the treatment is.”
“Using propranolol to treat hemangiomas is probably one of the biggest positive changes in my practice. It was very difficult to treat hemangiomas with steroids, vincristine, or other alternatives. Now treatment is ‘cookbook’ and well-tolerated. It’s amazing,” Dr. Siegfried said. “I only prescribe the branded propranolol because of the specialty pharmacy issue, because of the formulation issue, and because we have data that Pierre Fabre paid for,” she added.
Dr. Siegfried is a consultant for Pierre Fabre and served as a principle investigator on phase 3 research. The company did not sponsor the current study, but a coauthor and employee of Pierre Fabre assisted with the logistics of the survey.
AT AAP 2017
Key clinical point: Although more costly than generics, Hemangeol (Pierre Fabre) could reduce safety concerns for treating infantile hemangioma.
Major finding:
Data source: Based on survey responses from 223 physicians, 70% of whom were pediatric dermatologists.
Disclosures: Dr. Siegfried is a consultant for Pierre Fabre and served as a principle investigator on phase 3 research. The company did not sponsor the current study, but a coauthor and employee of Pierre Fabre assisted with the logistics of the survey.
Mental health services can be successfully integrated in primary care
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2017
How to have a rational approach to the FUO work-up
CHICAGO – When a child’s worried parents bring him back to be rechecked on his 8th day of fever, what’s next? If the initial work-up is unrevealing, when is it time to consider hospitalization? And which children can safely be managed as outpatients?
These tough scenarios are part of why “most pediatricians really don’t enjoy fever of unknown origin (FUO),” said Brian Williams, MD, speaking at a pediatric infectious disease update at the annual meeting of the American Academy of Pediatrics. “It can be really time consuming and frustrating to tease all of this out.”
Dr. Williams comes into the picture when, for the pediatrician, “something about that history, that physical exam, and that lab work has them concerned that the child needs to be hospitalized for closer monitoring and a more extensive work-up.”
“There’s lots of variability for inclusion criteria in the studies for pediatrics,” said Dr. Williams, but most characterize FUO as a fever of at least 100.4° F for 8 days or longer with no clear diagnosis.
he said. “I think it’s one of those diagnoses where a thorough history and exam can oftentimes give you some clues that can help lead to your diagnosis.”
“It’s a diagnosis that always gets my full attention because sometimes you can find some pretty significant infections – an osteomyelitis or a severe pelvic abscess,” he said. “And there’s always the concern of some of these more serious underlying diseases, like rheumatologic diseases; there’s plenty of case reports of [inflammatory bowel disease] presenting with FUO.” Of course, he said, even more dire diagnoses like Hodgkin’s lymphoma and leukemia have to remain in the differential as well.
Although the broad diagnostic differential includes noninfectious causes, they are rarer by far than infections. When the etiology of FUO has been studied in the United States, said Dr. Williams, “infections pretty consistently dominate as the most common cause of FUO … as general pediatricians, it’s our job to really do a good evaluation for infection before we start going after some of these less common diagnoses – the rheumatologic and cancer diagnoses.”
A systematic approach is important, he said. “A really good fever history can, a lot of times, provide important and valuable information.” Take the time to get granular detail: Find out how often the fever is being checked and by whom, what symptoms accompany the fever, and how the fever is being measured.
And don’t forget to ask if there are fever-free days, he said. In an otherwise well-appearing child, a few days’ respite from fever can increase the likelihood that you’re really seeing back-to-back viral illnesses rather than a protracted unexplained fever.
A thorough head-to-toe review of symptoms and history is critical, too. Dr. Williams related the story of a well-appearing 9-year-old boy who’d had many days of high fever with accompanying elevated inflammatory markers. His exam was unremarkable, and the only untoward symptom he could recall was a few days’ worth of left upper quadrant tenderness when running in gym class. The child, said Dr. Williams, turned out to have nephronia. “Sometimes, really subtle clues from the history can guide you.”
Ask about exposures, including travel, animals, foods, insects, and sick contacts. “Obviously, children can get into just about anything,” said Dr. Williams. A detailed family and social history also may turn up clues.
An infection-focused musculoskeletal exam, to include the spine, is a must, as is a top-to-bottom search for lymphadenopathy as part of a complete physical exam.
At this point in the pediatrics office, said Dr. Williams, you’ve come to a decision point: “Does this work-up need to be initiated in the inpatient setting, or is this something that can be started in the outpatient setting?”
“There’s a lot of data to support that, initially, a lot of these patients can be worked up in the outpatient setting with close follow-up,” he said. The outpatient FUO work-up begins with some basic screening labs. In addition to a complete blood count, chemistries, and a urinalysis, labs should include blood and urine cultures, erythrocyte sedimentation rate, and C-reactive protein levels.
“I’ll actually rely pretty heavily on my ESR and CRP,” said Dr. Williams. “If I have an otherwise well-appearing child with a normal CRP and an unremarkable exam, I think it’s a pretty tough argument to keep that child hospitalized and do a more invasive work-up.”
The advent of the viral polymerase chain reaction panel has helped streamline the FUO work-up as well. In the setting of a well-appearing child with an unremarkable initial work-up, “a positive adenovirus can provide a lot of reassurance to the families.”
Dr. Williams usually also gets a chest radiograph at this point, knowing that pneumonia is in the differential for FUO. He said he’s seen mediastinal masses, as well as picked up dense right upper lobe infiltrates that were missed on exam.
If the answer is still unclear at this point, exam and laboratory findings from the first-tier inquiry can help guide the next steps.
Some less common infectious etiologies can be considered now, said Dr. Williams. These can include Epstein-Barr virus, cytomegalovirus, and cat scratch fever; the latter, he’s found, is the third-most-common cause of FUO in some case series. For the real mystery cases, next-generation sequencing is an option: A blood sample is used to search for DNA fragments from a huge variety of microorganisms. “It’s a little overwhelming,” and very expensive, he said.
If an oncologic process is suspected, second-tier labs can include lactate dehydrogenase, uric acid, ferritin levels, and a peripheral smear. A rheumatologic work-up can be started, with antinuclear antibody and complement levels. At this point, though, a general pediatrician would be considering consults, he said.
Empiric antibiotics can be a tempting diagnostic strategy in some cases. “Is a trial of antibiotics warranted? Usually we advise against it,” but a case can be made for a time-limited trial in certain circumstances, said Dr. Williams.
Dr. Williams is a consultant for Zavante Therapeutics, which markets fosfomycin.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – When a child’s worried parents bring him back to be rechecked on his 8th day of fever, what’s next? If the initial work-up is unrevealing, when is it time to consider hospitalization? And which children can safely be managed as outpatients?
These tough scenarios are part of why “most pediatricians really don’t enjoy fever of unknown origin (FUO),” said Brian Williams, MD, speaking at a pediatric infectious disease update at the annual meeting of the American Academy of Pediatrics. “It can be really time consuming and frustrating to tease all of this out.”
Dr. Williams comes into the picture when, for the pediatrician, “something about that history, that physical exam, and that lab work has them concerned that the child needs to be hospitalized for closer monitoring and a more extensive work-up.”
“There’s lots of variability for inclusion criteria in the studies for pediatrics,” said Dr. Williams, but most characterize FUO as a fever of at least 100.4° F for 8 days or longer with no clear diagnosis.
he said. “I think it’s one of those diagnoses where a thorough history and exam can oftentimes give you some clues that can help lead to your diagnosis.”
“It’s a diagnosis that always gets my full attention because sometimes you can find some pretty significant infections – an osteomyelitis or a severe pelvic abscess,” he said. “And there’s always the concern of some of these more serious underlying diseases, like rheumatologic diseases; there’s plenty of case reports of [inflammatory bowel disease] presenting with FUO.” Of course, he said, even more dire diagnoses like Hodgkin’s lymphoma and leukemia have to remain in the differential as well.
Although the broad diagnostic differential includes noninfectious causes, they are rarer by far than infections. When the etiology of FUO has been studied in the United States, said Dr. Williams, “infections pretty consistently dominate as the most common cause of FUO … as general pediatricians, it’s our job to really do a good evaluation for infection before we start going after some of these less common diagnoses – the rheumatologic and cancer diagnoses.”
A systematic approach is important, he said. “A really good fever history can, a lot of times, provide important and valuable information.” Take the time to get granular detail: Find out how often the fever is being checked and by whom, what symptoms accompany the fever, and how the fever is being measured.
And don’t forget to ask if there are fever-free days, he said. In an otherwise well-appearing child, a few days’ respite from fever can increase the likelihood that you’re really seeing back-to-back viral illnesses rather than a protracted unexplained fever.
A thorough head-to-toe review of symptoms and history is critical, too. Dr. Williams related the story of a well-appearing 9-year-old boy who’d had many days of high fever with accompanying elevated inflammatory markers. His exam was unremarkable, and the only untoward symptom he could recall was a few days’ worth of left upper quadrant tenderness when running in gym class. The child, said Dr. Williams, turned out to have nephronia. “Sometimes, really subtle clues from the history can guide you.”
Ask about exposures, including travel, animals, foods, insects, and sick contacts. “Obviously, children can get into just about anything,” said Dr. Williams. A detailed family and social history also may turn up clues.
An infection-focused musculoskeletal exam, to include the spine, is a must, as is a top-to-bottom search for lymphadenopathy as part of a complete physical exam.
At this point in the pediatrics office, said Dr. Williams, you’ve come to a decision point: “Does this work-up need to be initiated in the inpatient setting, or is this something that can be started in the outpatient setting?”
“There’s a lot of data to support that, initially, a lot of these patients can be worked up in the outpatient setting with close follow-up,” he said. The outpatient FUO work-up begins with some basic screening labs. In addition to a complete blood count, chemistries, and a urinalysis, labs should include blood and urine cultures, erythrocyte sedimentation rate, and C-reactive protein levels.
“I’ll actually rely pretty heavily on my ESR and CRP,” said Dr. Williams. “If I have an otherwise well-appearing child with a normal CRP and an unremarkable exam, I think it’s a pretty tough argument to keep that child hospitalized and do a more invasive work-up.”
The advent of the viral polymerase chain reaction panel has helped streamline the FUO work-up as well. In the setting of a well-appearing child with an unremarkable initial work-up, “a positive adenovirus can provide a lot of reassurance to the families.”
Dr. Williams usually also gets a chest radiograph at this point, knowing that pneumonia is in the differential for FUO. He said he’s seen mediastinal masses, as well as picked up dense right upper lobe infiltrates that were missed on exam.
If the answer is still unclear at this point, exam and laboratory findings from the first-tier inquiry can help guide the next steps.
Some less common infectious etiologies can be considered now, said Dr. Williams. These can include Epstein-Barr virus, cytomegalovirus, and cat scratch fever; the latter, he’s found, is the third-most-common cause of FUO in some case series. For the real mystery cases, next-generation sequencing is an option: A blood sample is used to search for DNA fragments from a huge variety of microorganisms. “It’s a little overwhelming,” and very expensive, he said.
If an oncologic process is suspected, second-tier labs can include lactate dehydrogenase, uric acid, ferritin levels, and a peripheral smear. A rheumatologic work-up can be started, with antinuclear antibody and complement levels. At this point, though, a general pediatrician would be considering consults, he said.
Empiric antibiotics can be a tempting diagnostic strategy in some cases. “Is a trial of antibiotics warranted? Usually we advise against it,” but a case can be made for a time-limited trial in certain circumstances, said Dr. Williams.
Dr. Williams is a consultant for Zavante Therapeutics, which markets fosfomycin.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – When a child’s worried parents bring him back to be rechecked on his 8th day of fever, what’s next? If the initial work-up is unrevealing, when is it time to consider hospitalization? And which children can safely be managed as outpatients?
These tough scenarios are part of why “most pediatricians really don’t enjoy fever of unknown origin (FUO),” said Brian Williams, MD, speaking at a pediatric infectious disease update at the annual meeting of the American Academy of Pediatrics. “It can be really time consuming and frustrating to tease all of this out.”
Dr. Williams comes into the picture when, for the pediatrician, “something about that history, that physical exam, and that lab work has them concerned that the child needs to be hospitalized for closer monitoring and a more extensive work-up.”
“There’s lots of variability for inclusion criteria in the studies for pediatrics,” said Dr. Williams, but most characterize FUO as a fever of at least 100.4° F for 8 days or longer with no clear diagnosis.
he said. “I think it’s one of those diagnoses where a thorough history and exam can oftentimes give you some clues that can help lead to your diagnosis.”
“It’s a diagnosis that always gets my full attention because sometimes you can find some pretty significant infections – an osteomyelitis or a severe pelvic abscess,” he said. “And there’s always the concern of some of these more serious underlying diseases, like rheumatologic diseases; there’s plenty of case reports of [inflammatory bowel disease] presenting with FUO.” Of course, he said, even more dire diagnoses like Hodgkin’s lymphoma and leukemia have to remain in the differential as well.
Although the broad diagnostic differential includes noninfectious causes, they are rarer by far than infections. When the etiology of FUO has been studied in the United States, said Dr. Williams, “infections pretty consistently dominate as the most common cause of FUO … as general pediatricians, it’s our job to really do a good evaluation for infection before we start going after some of these less common diagnoses – the rheumatologic and cancer diagnoses.”
A systematic approach is important, he said. “A really good fever history can, a lot of times, provide important and valuable information.” Take the time to get granular detail: Find out how often the fever is being checked and by whom, what symptoms accompany the fever, and how the fever is being measured.
And don’t forget to ask if there are fever-free days, he said. In an otherwise well-appearing child, a few days’ respite from fever can increase the likelihood that you’re really seeing back-to-back viral illnesses rather than a protracted unexplained fever.
A thorough head-to-toe review of symptoms and history is critical, too. Dr. Williams related the story of a well-appearing 9-year-old boy who’d had many days of high fever with accompanying elevated inflammatory markers. His exam was unremarkable, and the only untoward symptom he could recall was a few days’ worth of left upper quadrant tenderness when running in gym class. The child, said Dr. Williams, turned out to have nephronia. “Sometimes, really subtle clues from the history can guide you.”
Ask about exposures, including travel, animals, foods, insects, and sick contacts. “Obviously, children can get into just about anything,” said Dr. Williams. A detailed family and social history also may turn up clues.
An infection-focused musculoskeletal exam, to include the spine, is a must, as is a top-to-bottom search for lymphadenopathy as part of a complete physical exam.
At this point in the pediatrics office, said Dr. Williams, you’ve come to a decision point: “Does this work-up need to be initiated in the inpatient setting, or is this something that can be started in the outpatient setting?”
“There’s a lot of data to support that, initially, a lot of these patients can be worked up in the outpatient setting with close follow-up,” he said. The outpatient FUO work-up begins with some basic screening labs. In addition to a complete blood count, chemistries, and a urinalysis, labs should include blood and urine cultures, erythrocyte sedimentation rate, and C-reactive protein levels.
“I’ll actually rely pretty heavily on my ESR and CRP,” said Dr. Williams. “If I have an otherwise well-appearing child with a normal CRP and an unremarkable exam, I think it’s a pretty tough argument to keep that child hospitalized and do a more invasive work-up.”
The advent of the viral polymerase chain reaction panel has helped streamline the FUO work-up as well. In the setting of a well-appearing child with an unremarkable initial work-up, “a positive adenovirus can provide a lot of reassurance to the families.”
Dr. Williams usually also gets a chest radiograph at this point, knowing that pneumonia is in the differential for FUO. He said he’s seen mediastinal masses, as well as picked up dense right upper lobe infiltrates that were missed on exam.
If the answer is still unclear at this point, exam and laboratory findings from the first-tier inquiry can help guide the next steps.
Some less common infectious etiologies can be considered now, said Dr. Williams. These can include Epstein-Barr virus, cytomegalovirus, and cat scratch fever; the latter, he’s found, is the third-most-common cause of FUO in some case series. For the real mystery cases, next-generation sequencing is an option: A blood sample is used to search for DNA fragments from a huge variety of microorganisms. “It’s a little overwhelming,” and very expensive, he said.
If an oncologic process is suspected, second-tier labs can include lactate dehydrogenase, uric acid, ferritin levels, and a peripheral smear. A rheumatologic work-up can be started, with antinuclear antibody and complement levels. At this point, though, a general pediatrician would be considering consults, he said.
Empiric antibiotics can be a tempting diagnostic strategy in some cases. “Is a trial of antibiotics warranted? Usually we advise against it,” but a case can be made for a time-limited trial in certain circumstances, said Dr. Williams.
Dr. Williams is a consultant for Zavante Therapeutics, which markets fosfomycin.
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM AAP 2017
Thinking may be shifting about first-line AOM treatment
CHICAGO – Treating even uncomplicated acute otitis media (AOM) in 2017 may not be as simple as writing an amoxicillin prescription. Changes in pathogens may mean a shift in prescribing practices, Ellen Wald, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wald, speaking to an audience that filled the lecture hall and an overflow room, said that there has long been good reason to turn to amoxicillin for AOM. “The reason that pediatricians and others like to reserve the use of amoxicillin as first-line therapy for children with AOM is that it is generally effective, it’s safe, it’s narrow in spectrum, and it’s relatively inexpensive. Those are all very desirable characteristics.”
However, the high-dose amoxicillin strategy is predicated on S. pneumoniae being the most likely cause of bacterial AOM. Since the seven-valent pneumococcal conjugate vaccine (PCV7), and then its successor PCV13, became part of the standard series of childhood immunizations, said Dr. Wald, the microbiology of AOM has shifted.
In 1990, S. pneumoniae was estimated to cause 35%-45% of AOM cases, with Haemophilus influenzae responsible for 25%-30% of cases. Moraxella catarrhalis was thought to cause 12%-15% of cases, with Streptococcus pyogenes–related AOM falling into the single digits.
In 2017, the balance has shifted, with S. pneumoniae only responsible for about a quarter of cases of AOM, and H. influenzae causing about half. The prevalence of M. catarrhalis and S. pyogenes cases hasn’t changed. This, said Dr. Wald, should prompt a shift in thinking about antibiotic strategy for AOM.
“The real problem with amoxicillin is that it’s not active against beta-lactamase–producing H. influenzae and M. catarrhalis. So my recommendation would be, rather than using amoxicillin, to use amoxicillin potassium clavulanate.”
Dr. Wald said she can’t currently recommend using azithromycin to treat AOM. “Azithromycin and the other macrolides have almost no activity against H. influenzae,” she said. “So given the current situation with the high prevalence of H. influenzae, azithromycin really should be avoided in the management of AOM.”
For children with non–type 1 penicillin hypersensitivity or mild type 1 hypersensitivity, a second- or third-generation cephalosporin, such as cefuroxime, cefpodoxime, or cefdinir, can be considered, she said.
“For life-threatening type 1 hypersensitivity reactions, we like to choose a drug of an entirely different class. For that reason, levofloxacin might be something you’d consider,” in those cases, said Dr. Wald, making clear that this is not a Food and Drug Administration–approved indication. Levofloxacin does have the antimicrobial spectrum to cover AOM pathogens, she said.
When parenteral therapy is indicated, as when a child isn’t tolerating oral medications or when nonadherence is likely, a single dose of ceftriaxone IM or IV, dosed at 50 mg/kg, remains a good option. “It’s a suitable agent because all middle ear pathogens are susceptible to ceftriaxone,” said Dr. Wald.
When oral antibiotics are used, how long should they be given? Some experts, she said, recommend a 5-day course for older children who have had infrequent previous episodes of AOM. In this age group, the shorter course can still yield an excellent response, she said.
However, a 2016 study that tried a shortened course of amoxicillin/clavulanate for children 6-23 months of age found that clinical failure occurred in 34% of the patients who received 5 days of antibiotics, compared with 16% of those who got the full 10-day course. “The recommendation is pretty clear that, for children under 2 years of age, a 10-day course of therapy is best,” said Dr. Wald.
Dr. Wald reported that she had no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – Treating even uncomplicated acute otitis media (AOM) in 2017 may not be as simple as writing an amoxicillin prescription. Changes in pathogens may mean a shift in prescribing practices, Ellen Wald, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wald, speaking to an audience that filled the lecture hall and an overflow room, said that there has long been good reason to turn to amoxicillin for AOM. “The reason that pediatricians and others like to reserve the use of amoxicillin as first-line therapy for children with AOM is that it is generally effective, it’s safe, it’s narrow in spectrum, and it’s relatively inexpensive. Those are all very desirable characteristics.”
However, the high-dose amoxicillin strategy is predicated on S. pneumoniae being the most likely cause of bacterial AOM. Since the seven-valent pneumococcal conjugate vaccine (PCV7), and then its successor PCV13, became part of the standard series of childhood immunizations, said Dr. Wald, the microbiology of AOM has shifted.
In 1990, S. pneumoniae was estimated to cause 35%-45% of AOM cases, with Haemophilus influenzae responsible for 25%-30% of cases. Moraxella catarrhalis was thought to cause 12%-15% of cases, with Streptococcus pyogenes–related AOM falling into the single digits.
In 2017, the balance has shifted, with S. pneumoniae only responsible for about a quarter of cases of AOM, and H. influenzae causing about half. The prevalence of M. catarrhalis and S. pyogenes cases hasn’t changed. This, said Dr. Wald, should prompt a shift in thinking about antibiotic strategy for AOM.
“The real problem with amoxicillin is that it’s not active against beta-lactamase–producing H. influenzae and M. catarrhalis. So my recommendation would be, rather than using amoxicillin, to use amoxicillin potassium clavulanate.”
Dr. Wald said she can’t currently recommend using azithromycin to treat AOM. “Azithromycin and the other macrolides have almost no activity against H. influenzae,” she said. “So given the current situation with the high prevalence of H. influenzae, azithromycin really should be avoided in the management of AOM.”
For children with non–type 1 penicillin hypersensitivity or mild type 1 hypersensitivity, a second- or third-generation cephalosporin, such as cefuroxime, cefpodoxime, or cefdinir, can be considered, she said.
“For life-threatening type 1 hypersensitivity reactions, we like to choose a drug of an entirely different class. For that reason, levofloxacin might be something you’d consider,” in those cases, said Dr. Wald, making clear that this is not a Food and Drug Administration–approved indication. Levofloxacin does have the antimicrobial spectrum to cover AOM pathogens, she said.
When parenteral therapy is indicated, as when a child isn’t tolerating oral medications or when nonadherence is likely, a single dose of ceftriaxone IM or IV, dosed at 50 mg/kg, remains a good option. “It’s a suitable agent because all middle ear pathogens are susceptible to ceftriaxone,” said Dr. Wald.
When oral antibiotics are used, how long should they be given? Some experts, she said, recommend a 5-day course for older children who have had infrequent previous episodes of AOM. In this age group, the shorter course can still yield an excellent response, she said.
However, a 2016 study that tried a shortened course of amoxicillin/clavulanate for children 6-23 months of age found that clinical failure occurred in 34% of the patients who received 5 days of antibiotics, compared with 16% of those who got the full 10-day course. “The recommendation is pretty clear that, for children under 2 years of age, a 10-day course of therapy is best,” said Dr. Wald.
Dr. Wald reported that she had no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO – Treating even uncomplicated acute otitis media (AOM) in 2017 may not be as simple as writing an amoxicillin prescription. Changes in pathogens may mean a shift in prescribing practices, Ellen Wald, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Wald, speaking to an audience that filled the lecture hall and an overflow room, said that there has long been good reason to turn to amoxicillin for AOM. “The reason that pediatricians and others like to reserve the use of amoxicillin as first-line therapy for children with AOM is that it is generally effective, it’s safe, it’s narrow in spectrum, and it’s relatively inexpensive. Those are all very desirable characteristics.”
However, the high-dose amoxicillin strategy is predicated on S. pneumoniae being the most likely cause of bacterial AOM. Since the seven-valent pneumococcal conjugate vaccine (PCV7), and then its successor PCV13, became part of the standard series of childhood immunizations, said Dr. Wald, the microbiology of AOM has shifted.
In 1990, S. pneumoniae was estimated to cause 35%-45% of AOM cases, with Haemophilus influenzae responsible for 25%-30% of cases. Moraxella catarrhalis was thought to cause 12%-15% of cases, with Streptococcus pyogenes–related AOM falling into the single digits.
In 2017, the balance has shifted, with S. pneumoniae only responsible for about a quarter of cases of AOM, and H. influenzae causing about half. The prevalence of M. catarrhalis and S. pyogenes cases hasn’t changed. This, said Dr. Wald, should prompt a shift in thinking about antibiotic strategy for AOM.
“The real problem with amoxicillin is that it’s not active against beta-lactamase–producing H. influenzae and M. catarrhalis. So my recommendation would be, rather than using amoxicillin, to use amoxicillin potassium clavulanate.”
Dr. Wald said she can’t currently recommend using azithromycin to treat AOM. “Azithromycin and the other macrolides have almost no activity against H. influenzae,” she said. “So given the current situation with the high prevalence of H. influenzae, azithromycin really should be avoided in the management of AOM.”
For children with non–type 1 penicillin hypersensitivity or mild type 1 hypersensitivity, a second- or third-generation cephalosporin, such as cefuroxime, cefpodoxime, or cefdinir, can be considered, she said.
“For life-threatening type 1 hypersensitivity reactions, we like to choose a drug of an entirely different class. For that reason, levofloxacin might be something you’d consider,” in those cases, said Dr. Wald, making clear that this is not a Food and Drug Administration–approved indication. Levofloxacin does have the antimicrobial spectrum to cover AOM pathogens, she said.
When parenteral therapy is indicated, as when a child isn’t tolerating oral medications or when nonadherence is likely, a single dose of ceftriaxone IM or IV, dosed at 50 mg/kg, remains a good option. “It’s a suitable agent because all middle ear pathogens are susceptible to ceftriaxone,” said Dr. Wald.
When oral antibiotics are used, how long should they be given? Some experts, she said, recommend a 5-day course for older children who have had infrequent previous episodes of AOM. In this age group, the shorter course can still yield an excellent response, she said.
However, a 2016 study that tried a shortened course of amoxicillin/clavulanate for children 6-23 months of age found that clinical failure occurred in 34% of the patients who received 5 days of antibiotics, compared with 16% of those who got the full 10-day course. “The recommendation is pretty clear that, for children under 2 years of age, a 10-day course of therapy is best,” said Dr. Wald.
Dr. Wald reported that she had no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM AAP 2017
Healthy youth sports participation excludes early specialization
CHICAGO – When a boy receives five college football scholarship offers and a girl commits to playing soccer for a university before either of them starts ninth grade, it’s time to take several steps back in youth sports.
, including the risk of potentially discouraging a lifetime of healthy athletic participation, according to Joel S. Brenner, MD, MPH, a sports medicine expert at the Children’s Hospital of The King’s Daughters and Eastern Virginia Medical School, both in Norfolk.
“This paradigm should be discouraged by society,” Dr. Brenner told attendees at the American Academy of Pediatrics annual meeting. “Sports specialization refers to focusing on one sport to the exclusion of all others, often playing that single sport year-round. Dr. Brenner authored the AAP’s 2016 clinical report on sports specialization and intensive training in young athletes.
Dr. Brenner emphasized the benefits of delaying sports specialization until after puberty, the risks of specializing sooner, and the importance of rest to prevent burnout and injuries.
This is not a new problem, he noted, showing the attendees two Time Magazine covers, from 1999 and 2017, that featured the concern of “Sports Crazed Kids.” But it is so far-reaching that it will requires more than just physicians to change.
“This is not just an athlete problem, a parent problem, a coach problem, or even a physician problem,” Dr. Brenner said. “It’s a societal problem, a youth sports culture problem, and one that all of us as stakeholders need to attack and try to change the culture.”
Youth sports offer a broad range of benefits, such as developing physical activity, and leadership skills, and promoting self-esteem, socialization, and teamwork, Dr. Brenner said.
“But one benefit that often gets forgotten by people, including the coaches, the parents, and the athletes, is that sports is supposed to be about having fun,” he said.
The old model of kids’ sports was loosely organized fun, with kids playing multiple sports throughout the year and less direct involvement from adults, such as street hockey games and pick-up basketball. But those bygone days, Dr. Brenner noted wistfully, have been replaced with a different paradigm today: Children specialize in a single sport very early, and parents and coaches are the driving forces behind their involvement.
Today’s culture of very early sports specialization and college recruitment increases pressure on parents and young athletes to play year-round on multiple teams to stay on the radar of scouts and colleges. And this specialization has expanded to younger and younger ages, with 7-year-olds participating in travel leagues and national rankings of children in their sport as early as sixth grade.
“We should not be ranking kids in middle school or even in early high school,” Dr. Brenner said to wide applause. “We should allow kids to develop in a low-pressure, healthy system before we do that.”
The effects of high pressure have potentially lifelong ramifications. By the time children are 13 years old, 70% have dropped out of organized sports, Dr. Brenner said, and injuries from overuse account for more than half of all sports-related injuries in youth.
Yet the alternative – early diversification and late specialization – can really benefit kids, he said. The early specialization paradigm of playing just one sport focuses on deliberate practice and performance from the start. By contrast, early diversification with multiple sports focuses on deliberate play, during which children develop foundational athletic skills. Children who play a variety of sports are more likely to participate for more years – and it meets youth’s more realistic, long-term needs for lifelong physical activity through “fun, variety, and play,” he said.
Dr. Brenner said that just 1% of high school athletes receive any athletic scholarships, and only 3%-11% of high school athletes compete at the college level. The numbers for high school athletes that go on to play at the professional level is, of course, even smaller: 0.03% to 0.5%, depending on the sport.
And the irony is that the goal of early specialization – producing such elite level athletes – is actually better accomplished through playing multiple sports, Dr. Brenner said. Most Division 1 National Collegiate Athletic Association (NCAA) athletes and 90% of National Football League (NFL) first-round picks played multiple sports in high school. So the benefits of waiting until late adolescence to specialize are twofold: a greater likelihood of athletic success, even at elite levels, and minimizing the risks of injury.
Overuse injuries pose serious risks
More than half of sports injuries are from overuse, and a number of factors contribute to those injuries, such as muscle imbalance, playing surfaces, and training errors, Dr. Brenner said. But the biggest contributors are early specialization, playing year-round sports, and playing on multiple teams.
“This is a problem we see daily,” Dr. Brenner said. “We can see the young dancer, who’s dancing 6-7 days a week, who develops back pain and continues to dance, and develops a stress fracture in her lumbar spine known spondylosis.
“Or we see the young soccer player who plays on multiple teams and develops heel pain, who starts limping with activities of daily living, continues to play soccer despite limping, and develops calcaneal apophysitis, known as Sever’s disease. Or the young baseball pitcher, who pitches for two teams, who develops arm pain and weakness, who has a stress fracture through the proximal humeral epiphysis, known as Little League shoulder.” 
Two broad pieces of guidance can help reduce the risk of injuries, particularly from overuse. First, young athletes should take off at least 1 month from a specific sport at least three times a year to give them adequate time for physical and psychological recovery. Second, ensuring young athletes take at least 1 or 2 days off of practice each week further reduces the likelihood of injury.
In addition to the physical problems these young athletes may develop, they also risk anxiety, depression, burnout, early retirement, and social isolation from peers who don’t play their sport, Dr. Brenner said. Family members also may experience greater stress, he added. And then there’s the risk of missing out on learning other sports they may excel in that offer a lifetime of enjoyment, such as tennis or swimming.
It is not clear where the threshold of involvement is for reducing overuse injury, burnout, and attrition, but Dr. Brenner provided some guidelines as a starting place. High school athletes should not train more 16 hours a week, and organized sports should not exceed free play time by a greater ratio than 2:1. Another guideline is not to exceed more hours per week in organized sports than a child’s age in years.
The primary focus of sports should be learning lifelong physical activity skills and having fun, Dr. Brenner said. Pediatricians should encourage patients to play in a wide variety of sports at least until puberty, thereby decreasing the chance of injuries, stress, and burnout, he said. That can include sports that are not necessarily an official part of school or club competition. Waiting until later to specialize may lead to a higher likelihood of athletic success.
Dr. Brenner said he had no relevant financial disclosures.
CHICAGO – When a boy receives five college football scholarship offers and a girl commits to playing soccer for a university before either of them starts ninth grade, it’s time to take several steps back in youth sports.
, including the risk of potentially discouraging a lifetime of healthy athletic participation, according to Joel S. Brenner, MD, MPH, a sports medicine expert at the Children’s Hospital of The King’s Daughters and Eastern Virginia Medical School, both in Norfolk.
“This paradigm should be discouraged by society,” Dr. Brenner told attendees at the American Academy of Pediatrics annual meeting. “Sports specialization refers to focusing on one sport to the exclusion of all others, often playing that single sport year-round. Dr. Brenner authored the AAP’s 2016 clinical report on sports specialization and intensive training in young athletes.
Dr. Brenner emphasized the benefits of delaying sports specialization until after puberty, the risks of specializing sooner, and the importance of rest to prevent burnout and injuries.
This is not a new problem, he noted, showing the attendees two Time Magazine covers, from 1999 and 2017, that featured the concern of “Sports Crazed Kids.” But it is so far-reaching that it will requires more than just physicians to change.
“This is not just an athlete problem, a parent problem, a coach problem, or even a physician problem,” Dr. Brenner said. “It’s a societal problem, a youth sports culture problem, and one that all of us as stakeholders need to attack and try to change the culture.”
Youth sports offer a broad range of benefits, such as developing physical activity, and leadership skills, and promoting self-esteem, socialization, and teamwork, Dr. Brenner said.
“But one benefit that often gets forgotten by people, including the coaches, the parents, and the athletes, is that sports is supposed to be about having fun,” he said.
The old model of kids’ sports was loosely organized fun, with kids playing multiple sports throughout the year and less direct involvement from adults, such as street hockey games and pick-up basketball. But those bygone days, Dr. Brenner noted wistfully, have been replaced with a different paradigm today: Children specialize in a single sport very early, and parents and coaches are the driving forces behind their involvement.
Today’s culture of very early sports specialization and college recruitment increases pressure on parents and young athletes to play year-round on multiple teams to stay on the radar of scouts and colleges. And this specialization has expanded to younger and younger ages, with 7-year-olds participating in travel leagues and national rankings of children in their sport as early as sixth grade.
“We should not be ranking kids in middle school or even in early high school,” Dr. Brenner said to wide applause. “We should allow kids to develop in a low-pressure, healthy system before we do that.”
The effects of high pressure have potentially lifelong ramifications. By the time children are 13 years old, 70% have dropped out of organized sports, Dr. Brenner said, and injuries from overuse account for more than half of all sports-related injuries in youth.
Yet the alternative – early diversification and late specialization – can really benefit kids, he said. The early specialization paradigm of playing just one sport focuses on deliberate practice and performance from the start. By contrast, early diversification with multiple sports focuses on deliberate play, during which children develop foundational athletic skills. Children who play a variety of sports are more likely to participate for more years – and it meets youth’s more realistic, long-term needs for lifelong physical activity through “fun, variety, and play,” he said.
Dr. Brenner said that just 1% of high school athletes receive any athletic scholarships, and only 3%-11% of high school athletes compete at the college level. The numbers for high school athletes that go on to play at the professional level is, of course, even smaller: 0.03% to 0.5%, depending on the sport.
And the irony is that the goal of early specialization – producing such elite level athletes – is actually better accomplished through playing multiple sports, Dr. Brenner said. Most Division 1 National Collegiate Athletic Association (NCAA) athletes and 90% of National Football League (NFL) first-round picks played multiple sports in high school. So the benefits of waiting until late adolescence to specialize are twofold: a greater likelihood of athletic success, even at elite levels, and minimizing the risks of injury.
Overuse injuries pose serious risks
More than half of sports injuries are from overuse, and a number of factors contribute to those injuries, such as muscle imbalance, playing surfaces, and training errors, Dr. Brenner said. But the biggest contributors are early specialization, playing year-round sports, and playing on multiple teams.
“This is a problem we see daily,” Dr. Brenner said. “We can see the young dancer, who’s dancing 6-7 days a week, who develops back pain and continues to dance, and develops a stress fracture in her lumbar spine known spondylosis.
“Or we see the young soccer player who plays on multiple teams and develops heel pain, who starts limping with activities of daily living, continues to play soccer despite limping, and develops calcaneal apophysitis, known as Sever’s disease. Or the young baseball pitcher, who pitches for two teams, who develops arm pain and weakness, who has a stress fracture through the proximal humeral epiphysis, known as Little League shoulder.” 
Two broad pieces of guidance can help reduce the risk of injuries, particularly from overuse. First, young athletes should take off at least 1 month from a specific sport at least three times a year to give them adequate time for physical and psychological recovery. Second, ensuring young athletes take at least 1 or 2 days off of practice each week further reduces the likelihood of injury.
In addition to the physical problems these young athletes may develop, they also risk anxiety, depression, burnout, early retirement, and social isolation from peers who don’t play their sport, Dr. Brenner said. Family members also may experience greater stress, he added. And then there’s the risk of missing out on learning other sports they may excel in that offer a lifetime of enjoyment, such as tennis or swimming.
It is not clear where the threshold of involvement is for reducing overuse injury, burnout, and attrition, but Dr. Brenner provided some guidelines as a starting place. High school athletes should not train more 16 hours a week, and organized sports should not exceed free play time by a greater ratio than 2:1. Another guideline is not to exceed more hours per week in organized sports than a child’s age in years.
The primary focus of sports should be learning lifelong physical activity skills and having fun, Dr. Brenner said. Pediatricians should encourage patients to play in a wide variety of sports at least until puberty, thereby decreasing the chance of injuries, stress, and burnout, he said. That can include sports that are not necessarily an official part of school or club competition. Waiting until later to specialize may lead to a higher likelihood of athletic success.
Dr. Brenner said he had no relevant financial disclosures.
CHICAGO – When a boy receives five college football scholarship offers and a girl commits to playing soccer for a university before either of them starts ninth grade, it’s time to take several steps back in youth sports.
, including the risk of potentially discouraging a lifetime of healthy athletic participation, according to Joel S. Brenner, MD, MPH, a sports medicine expert at the Children’s Hospital of The King’s Daughters and Eastern Virginia Medical School, both in Norfolk.
“This paradigm should be discouraged by society,” Dr. Brenner told attendees at the American Academy of Pediatrics annual meeting. “Sports specialization refers to focusing on one sport to the exclusion of all others, often playing that single sport year-round. Dr. Brenner authored the AAP’s 2016 clinical report on sports specialization and intensive training in young athletes.
Dr. Brenner emphasized the benefits of delaying sports specialization until after puberty, the risks of specializing sooner, and the importance of rest to prevent burnout and injuries.
This is not a new problem, he noted, showing the attendees two Time Magazine covers, from 1999 and 2017, that featured the concern of “Sports Crazed Kids.” But it is so far-reaching that it will requires more than just physicians to change.
“This is not just an athlete problem, a parent problem, a coach problem, or even a physician problem,” Dr. Brenner said. “It’s a societal problem, a youth sports culture problem, and one that all of us as stakeholders need to attack and try to change the culture.”
Youth sports offer a broad range of benefits, such as developing physical activity, and leadership skills, and promoting self-esteem, socialization, and teamwork, Dr. Brenner said.
“But one benefit that often gets forgotten by people, including the coaches, the parents, and the athletes, is that sports is supposed to be about having fun,” he said.
The old model of kids’ sports was loosely organized fun, with kids playing multiple sports throughout the year and less direct involvement from adults, such as street hockey games and pick-up basketball. But those bygone days, Dr. Brenner noted wistfully, have been replaced with a different paradigm today: Children specialize in a single sport very early, and parents and coaches are the driving forces behind their involvement.
Today’s culture of very early sports specialization and college recruitment increases pressure on parents and young athletes to play year-round on multiple teams to stay on the radar of scouts and colleges. And this specialization has expanded to younger and younger ages, with 7-year-olds participating in travel leagues and national rankings of children in their sport as early as sixth grade.
“We should not be ranking kids in middle school or even in early high school,” Dr. Brenner said to wide applause. “We should allow kids to develop in a low-pressure, healthy system before we do that.”
The effects of high pressure have potentially lifelong ramifications. By the time children are 13 years old, 70% have dropped out of organized sports, Dr. Brenner said, and injuries from overuse account for more than half of all sports-related injuries in youth.
Yet the alternative – early diversification and late specialization – can really benefit kids, he said. The early specialization paradigm of playing just one sport focuses on deliberate practice and performance from the start. By contrast, early diversification with multiple sports focuses on deliberate play, during which children develop foundational athletic skills. Children who play a variety of sports are more likely to participate for more years – and it meets youth’s more realistic, long-term needs for lifelong physical activity through “fun, variety, and play,” he said.
Dr. Brenner said that just 1% of high school athletes receive any athletic scholarships, and only 3%-11% of high school athletes compete at the college level. The numbers for high school athletes that go on to play at the professional level is, of course, even smaller: 0.03% to 0.5%, depending on the sport.
And the irony is that the goal of early specialization – producing such elite level athletes – is actually better accomplished through playing multiple sports, Dr. Brenner said. Most Division 1 National Collegiate Athletic Association (NCAA) athletes and 90% of National Football League (NFL) first-round picks played multiple sports in high school. So the benefits of waiting until late adolescence to specialize are twofold: a greater likelihood of athletic success, even at elite levels, and minimizing the risks of injury.
Overuse injuries pose serious risks
More than half of sports injuries are from overuse, and a number of factors contribute to those injuries, such as muscle imbalance, playing surfaces, and training errors, Dr. Brenner said. But the biggest contributors are early specialization, playing year-round sports, and playing on multiple teams.
“This is a problem we see daily,” Dr. Brenner said. “We can see the young dancer, who’s dancing 6-7 days a week, who develops back pain and continues to dance, and develops a stress fracture in her lumbar spine known spondylosis.
“Or we see the young soccer player who plays on multiple teams and develops heel pain, who starts limping with activities of daily living, continues to play soccer despite limping, and develops calcaneal apophysitis, known as Sever’s disease. Or the young baseball pitcher, who pitches for two teams, who develops arm pain and weakness, who has a stress fracture through the proximal humeral epiphysis, known as Little League shoulder.” 
Two broad pieces of guidance can help reduce the risk of injuries, particularly from overuse. First, young athletes should take off at least 1 month from a specific sport at least three times a year to give them adequate time for physical and psychological recovery. Second, ensuring young athletes take at least 1 or 2 days off of practice each week further reduces the likelihood of injury.
In addition to the physical problems these young athletes may develop, they also risk anxiety, depression, burnout, early retirement, and social isolation from peers who don’t play their sport, Dr. Brenner said. Family members also may experience greater stress, he added. And then there’s the risk of missing out on learning other sports they may excel in that offer a lifetime of enjoyment, such as tennis or swimming.
It is not clear where the threshold of involvement is for reducing overuse injury, burnout, and attrition, but Dr. Brenner provided some guidelines as a starting place. High school athletes should not train more 16 hours a week, and organized sports should not exceed free play time by a greater ratio than 2:1. Another guideline is not to exceed more hours per week in organized sports than a child’s age in years.
The primary focus of sports should be learning lifelong physical activity skills and having fun, Dr. Brenner said. Pediatricians should encourage patients to play in a wide variety of sports at least until puberty, thereby decreasing the chance of injuries, stress, and burnout, he said. That can include sports that are not necessarily an official part of school or club competition. Waiting until later to specialize may lead to a higher likelihood of athletic success.
Dr. Brenner said he had no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 2017
Talking with vaccine-hesitant parents takes training and finesse
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Pediatricians can use tactics to help reduce the anxiety of discussing the importance of immunization with vaccine-hesitant parents.
Major finding: The CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent, but pediatricians perceived motivational interviewing as useful for the more strongly resistant parent.
Data source: Pilot study of five pediatric providers who received comprehensive training and ongoing support using different communication techniques.
Disclosures: Ms. Dybsand and Dr. Carson had no relevant financial disclosures.