User login
American Academy of Pediatrics (AAP): 2016 National Conference and Exhibition
Challenges of influenza, measles, pertussis guide outbreak management
SAN FRANCISCO – Recent U.S. outbreaks of pertussis, influenza, and measles have revealed shifts in the diseases’ epidemiology, shifts that pose new prevention and management challenges, explained Yvonne Maldonado, MD, at the annual meeting of the American Academy of Pediatrics.
Routine immunizations prevent 33,000 child deaths a year in the United States, having reduced vaccine-preventable diseases by more than 90%, but outbreaks still occur, she said. The recent announcement that measles was eliminated from the Western Hemisphere, for example, doesn’t mean we won’t see cases, said Dr. Maldonado, vice chair of the AAP Committee on Infectious Diseases and chief of the division of pediatric infectious diseases at Stanford (Calif.) University.
Dr. Maldonado reviewed specific challenges for flu, pertussis, and measles.
Influenza
The biggest challenges with controlling influenza are the failure to vaccinate children and the variable circulating strains each season, which can impact the performance of that year’s vaccine. Those changing strains and other factors also mean that the populations most at risk for serious complications also vary each season.
The two new mechanisms of change in influenza strains are antigenic drift and antigenic shift. Antigenic drift involves mutations that occur during repeated replications in the RNA strains of the virus, shifting its configuration over time so that it may not respond to the same antigens that the original strain responded to. Antigenic shift, however, is responsible for the periodic pandemics, when a complete genetic reassortment abruptly occurs because a new major protein from a strain jumps from an animal population into the human population, forming a new hybrid strain in humans.
Pertussis
Unlike flu, pertussis did become very uncommon because of widespread vaccination up until the early 2000s. But rates have begun to climb again, largely because of problems with the vaccine over time. Until the 1990s, the DTP vaccine, which includes a whole pertussis bacterium, was highly effective at preventing pertussis but could cause febrile seizures, an adverse event that proved too intolerable for many families.
It was replaced with the acellular pertussis vaccine DTaP, but research in the past 5-10 years has revealed that the effectiveness of DTaP and Tdap vaccines wanes much more quickly than anticipated. Subsequently, pertussis rates have almost continuously climbed from the early 2000s through the present, reaching an incidence of more than 100 cases per 100,000 among children younger than 1 year.
One of the biggest challenges now is improving vaccination rates among pregnant women, who were recommended in 2015 to get the Tdap vaccine in every pregnancy so that the newborn would have some passively acquired protection during the first few months of life.
Ongoing outbreaks then become exacerbated by pockets of lower vaccination rates among children in general.
Measles
The only chink in the armor against measles is failure to vaccinate against it, Dr. Maldonado said. Though the disease was eliminated from the United States in 2000, measles cases peaked recently in 2014, when 31 outbreaks involving 667 cases occurred because of imported cases from the Philippines. The next year, 60% of the 189 cases in 2015 resulted from the multistate measles outbreak starting at Disneyland in California.
Most of the individuals in both those years’ outbreaks were not vaccinated or had an unknown vaccination status. Of the 110 individuals with measles in California from the Disneyland outbreak, 45% were not immunized. Twelve were too young for vaccination, but 37 were eligible to have been vaccinated, and 67% of these were not vaccinated because of personal beliefs.
Vaccination rates for measles must be considerably higher, around 92%-94% of the population, to prevent outbreaks than for most other diseases, because the virus is so incredibly contagious.
“Measles is so infectious because it can exist in tiny microdroplets less than 5 mcg that can sit in the air up to 2 hours,” Dr. Maldonado explained. Yet only 92.6% of kindergartners had had both their MMR doses in 2014, compared with the peak of 97% between 2002 to 2007.
When children across all ages who have not received both doses of the vaccine are taken into account, 12.5% of all U.S. children and adolescents are currently susceptible to measles – and a quarter of those aged 3 years and younger are, Maldonado said.
The keys to preventing measles are high national coverage rates, an aggressive public health response (because early diagnosis can limit transmission), and improved implementation of health care worker recommendations.
“We have to keep measles in mind whenever we see fevers and rashes,” Dr. Maldonado cautioned. “Unfortunately, we see fevers and rashes all the time, so what really helps is a history of international travel or a parent with international travel.”
For families planning overseas travel, parents are recommended to give their infants the MMR as young as 6 months. But that dose does not count toward the child’s two doses recommended by the Centers for Disease Control and Prevention schedule.
“It’s a very tough call with measles, because we never know when it might pop up,” Dr. Maldonado said. “Measles will be sporadic, but when it happens, it’s a really big deal. You basically have to reach out to your entire patient log for several days before the child came in.”
Managing suspected/confirmed outbreaks
To prepare for and manage suspected outbreaks of an infectious disease, Dr. Maldonado advised taking the following steps:
• Establish a plan for evaluating suspected or confirmed infectious disease outbreaks in your office setting.
• Identify and eliminate the source of the infection, such as providing a separate waiting room for coughing children.
• Prevent additional cases using screening questions at the front desk.
• Provide prompt and consistent ongoing evaluation to prevent or minimize transmission to others.
• Track disease trends and advice from the AAP, CDC, and local county public health officials and disease experts to engage in ongoing surveillance and communication.
• Identify the initial source and route of exposure to understand why an outbreak occurred and how to prevent similar ones in the future.
Dr. Maldonado reporting being a member of a data safety monitoring board for Pfizer.
SAN FRANCISCO – Recent U.S. outbreaks of pertussis, influenza, and measles have revealed shifts in the diseases’ epidemiology, shifts that pose new prevention and management challenges, explained Yvonne Maldonado, MD, at the annual meeting of the American Academy of Pediatrics.
Routine immunizations prevent 33,000 child deaths a year in the United States, having reduced vaccine-preventable diseases by more than 90%, but outbreaks still occur, she said. The recent announcement that measles was eliminated from the Western Hemisphere, for example, doesn’t mean we won’t see cases, said Dr. Maldonado, vice chair of the AAP Committee on Infectious Diseases and chief of the division of pediatric infectious diseases at Stanford (Calif.) University.
Dr. Maldonado reviewed specific challenges for flu, pertussis, and measles.
Influenza
The biggest challenges with controlling influenza are the failure to vaccinate children and the variable circulating strains each season, which can impact the performance of that year’s vaccine. Those changing strains and other factors also mean that the populations most at risk for serious complications also vary each season.
The two new mechanisms of change in influenza strains are antigenic drift and antigenic shift. Antigenic drift involves mutations that occur during repeated replications in the RNA strains of the virus, shifting its configuration over time so that it may not respond to the same antigens that the original strain responded to. Antigenic shift, however, is responsible for the periodic pandemics, when a complete genetic reassortment abruptly occurs because a new major protein from a strain jumps from an animal population into the human population, forming a new hybrid strain in humans.
Pertussis
Unlike flu, pertussis did become very uncommon because of widespread vaccination up until the early 2000s. But rates have begun to climb again, largely because of problems with the vaccine over time. Until the 1990s, the DTP vaccine, which includes a whole pertussis bacterium, was highly effective at preventing pertussis but could cause febrile seizures, an adverse event that proved too intolerable for many families.
It was replaced with the acellular pertussis vaccine DTaP, but research in the past 5-10 years has revealed that the effectiveness of DTaP and Tdap vaccines wanes much more quickly than anticipated. Subsequently, pertussis rates have almost continuously climbed from the early 2000s through the present, reaching an incidence of more than 100 cases per 100,000 among children younger than 1 year.
One of the biggest challenges now is improving vaccination rates among pregnant women, who were recommended in 2015 to get the Tdap vaccine in every pregnancy so that the newborn would have some passively acquired protection during the first few months of life.
Ongoing outbreaks then become exacerbated by pockets of lower vaccination rates among children in general.
Measles
The only chink in the armor against measles is failure to vaccinate against it, Dr. Maldonado said. Though the disease was eliminated from the United States in 2000, measles cases peaked recently in 2014, when 31 outbreaks involving 667 cases occurred because of imported cases from the Philippines. The next year, 60% of the 189 cases in 2015 resulted from the multistate measles outbreak starting at Disneyland in California.
Most of the individuals in both those years’ outbreaks were not vaccinated or had an unknown vaccination status. Of the 110 individuals with measles in California from the Disneyland outbreak, 45% were not immunized. Twelve were too young for vaccination, but 37 were eligible to have been vaccinated, and 67% of these were not vaccinated because of personal beliefs.
Vaccination rates for measles must be considerably higher, around 92%-94% of the population, to prevent outbreaks than for most other diseases, because the virus is so incredibly contagious.
“Measles is so infectious because it can exist in tiny microdroplets less than 5 mcg that can sit in the air up to 2 hours,” Dr. Maldonado explained. Yet only 92.6% of kindergartners had had both their MMR doses in 2014, compared with the peak of 97% between 2002 to 2007.
When children across all ages who have not received both doses of the vaccine are taken into account, 12.5% of all U.S. children and adolescents are currently susceptible to measles – and a quarter of those aged 3 years and younger are, Maldonado said.
The keys to preventing measles are high national coverage rates, an aggressive public health response (because early diagnosis can limit transmission), and improved implementation of health care worker recommendations.
“We have to keep measles in mind whenever we see fevers and rashes,” Dr. Maldonado cautioned. “Unfortunately, we see fevers and rashes all the time, so what really helps is a history of international travel or a parent with international travel.”
For families planning overseas travel, parents are recommended to give their infants the MMR as young as 6 months. But that dose does not count toward the child’s two doses recommended by the Centers for Disease Control and Prevention schedule.
“It’s a very tough call with measles, because we never know when it might pop up,” Dr. Maldonado said. “Measles will be sporadic, but when it happens, it’s a really big deal. You basically have to reach out to your entire patient log for several days before the child came in.”
Managing suspected/confirmed outbreaks
To prepare for and manage suspected outbreaks of an infectious disease, Dr. Maldonado advised taking the following steps:
• Establish a plan for evaluating suspected or confirmed infectious disease outbreaks in your office setting.
• Identify and eliminate the source of the infection, such as providing a separate waiting room for coughing children.
• Prevent additional cases using screening questions at the front desk.
• Provide prompt and consistent ongoing evaluation to prevent or minimize transmission to others.
• Track disease trends and advice from the AAP, CDC, and local county public health officials and disease experts to engage in ongoing surveillance and communication.
• Identify the initial source and route of exposure to understand why an outbreak occurred and how to prevent similar ones in the future.
Dr. Maldonado reporting being a member of a data safety monitoring board for Pfizer.
SAN FRANCISCO – Recent U.S. outbreaks of pertussis, influenza, and measles have revealed shifts in the diseases’ epidemiology, shifts that pose new prevention and management challenges, explained Yvonne Maldonado, MD, at the annual meeting of the American Academy of Pediatrics.
Routine immunizations prevent 33,000 child deaths a year in the United States, having reduced vaccine-preventable diseases by more than 90%, but outbreaks still occur, she said. The recent announcement that measles was eliminated from the Western Hemisphere, for example, doesn’t mean we won’t see cases, said Dr. Maldonado, vice chair of the AAP Committee on Infectious Diseases and chief of the division of pediatric infectious diseases at Stanford (Calif.) University.
Dr. Maldonado reviewed specific challenges for flu, pertussis, and measles.
Influenza
The biggest challenges with controlling influenza are the failure to vaccinate children and the variable circulating strains each season, which can impact the performance of that year’s vaccine. Those changing strains and other factors also mean that the populations most at risk for serious complications also vary each season.
The two new mechanisms of change in influenza strains are antigenic drift and antigenic shift. Antigenic drift involves mutations that occur during repeated replications in the RNA strains of the virus, shifting its configuration over time so that it may not respond to the same antigens that the original strain responded to. Antigenic shift, however, is responsible for the periodic pandemics, when a complete genetic reassortment abruptly occurs because a new major protein from a strain jumps from an animal population into the human population, forming a new hybrid strain in humans.
Pertussis
Unlike flu, pertussis did become very uncommon because of widespread vaccination up until the early 2000s. But rates have begun to climb again, largely because of problems with the vaccine over time. Until the 1990s, the DTP vaccine, which includes a whole pertussis bacterium, was highly effective at preventing pertussis but could cause febrile seizures, an adverse event that proved too intolerable for many families.
It was replaced with the acellular pertussis vaccine DTaP, but research in the past 5-10 years has revealed that the effectiveness of DTaP and Tdap vaccines wanes much more quickly than anticipated. Subsequently, pertussis rates have almost continuously climbed from the early 2000s through the present, reaching an incidence of more than 100 cases per 100,000 among children younger than 1 year.
One of the biggest challenges now is improving vaccination rates among pregnant women, who were recommended in 2015 to get the Tdap vaccine in every pregnancy so that the newborn would have some passively acquired protection during the first few months of life.
Ongoing outbreaks then become exacerbated by pockets of lower vaccination rates among children in general.
Measles
The only chink in the armor against measles is failure to vaccinate against it, Dr. Maldonado said. Though the disease was eliminated from the United States in 2000, measles cases peaked recently in 2014, when 31 outbreaks involving 667 cases occurred because of imported cases from the Philippines. The next year, 60% of the 189 cases in 2015 resulted from the multistate measles outbreak starting at Disneyland in California.
Most of the individuals in both those years’ outbreaks were not vaccinated or had an unknown vaccination status. Of the 110 individuals with measles in California from the Disneyland outbreak, 45% were not immunized. Twelve were too young for vaccination, but 37 were eligible to have been vaccinated, and 67% of these were not vaccinated because of personal beliefs.
Vaccination rates for measles must be considerably higher, around 92%-94% of the population, to prevent outbreaks than for most other diseases, because the virus is so incredibly contagious.
“Measles is so infectious because it can exist in tiny microdroplets less than 5 mcg that can sit in the air up to 2 hours,” Dr. Maldonado explained. Yet only 92.6% of kindergartners had had both their MMR doses in 2014, compared with the peak of 97% between 2002 to 2007.
When children across all ages who have not received both doses of the vaccine are taken into account, 12.5% of all U.S. children and adolescents are currently susceptible to measles – and a quarter of those aged 3 years and younger are, Maldonado said.
The keys to preventing measles are high national coverage rates, an aggressive public health response (because early diagnosis can limit transmission), and improved implementation of health care worker recommendations.
“We have to keep measles in mind whenever we see fevers and rashes,” Dr. Maldonado cautioned. “Unfortunately, we see fevers and rashes all the time, so what really helps is a history of international travel or a parent with international travel.”
For families planning overseas travel, parents are recommended to give their infants the MMR as young as 6 months. But that dose does not count toward the child’s two doses recommended by the Centers for Disease Control and Prevention schedule.
“It’s a very tough call with measles, because we never know when it might pop up,” Dr. Maldonado said. “Measles will be sporadic, but when it happens, it’s a really big deal. You basically have to reach out to your entire patient log for several days before the child came in.”
Managing suspected/confirmed outbreaks
To prepare for and manage suspected outbreaks of an infectious disease, Dr. Maldonado advised taking the following steps:
• Establish a plan for evaluating suspected or confirmed infectious disease outbreaks in your office setting.
• Identify and eliminate the source of the infection, such as providing a separate waiting room for coughing children.
• Prevent additional cases using screening questions at the front desk.
• Provide prompt and consistent ongoing evaluation to prevent or minimize transmission to others.
• Track disease trends and advice from the AAP, CDC, and local county public health officials and disease experts to engage in ongoing surveillance and communication.
• Identify the initial source and route of exposure to understand why an outbreak occurred and how to prevent similar ones in the future.
Dr. Maldonado reporting being a member of a data safety monitoring board for Pfizer.
FROM AAP 16
New research in otitis media means new controversies
SAN FRANCISCO – As researchers have learned more about otitis media in the past decade, the guidelines have shifted accordingly for one of the most common conditions of childhood.
Yet some controversies remain, and the condition remains a challenge to properly identify, David Conrad, MD, of the University of California, San Francisco, said at the annual meeting of the American Academy of Pediatrics.
Pediatricians already know it’s the most common reason young children come into their offices and the most common reason they prescribe antibiotics. But they may know less about recognizing complications and long-term effects.
Complications and treatment
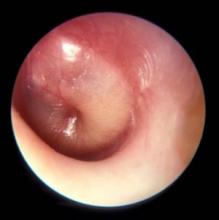
Ossicular erosion or tympanic membrane perforation are two complications; the latter’s rate is 5%-29% for untreated acute otitis media. It typically closes within hours to days, however, with a 95% closure rate within 4 weeks.
“The ear drum is pretty forgiving, pretty resilient, really,” Dr. Conrad said. The perforation occurs when pressure builds up and takes the path of least resistance through the drum, but that release of pressure also typically relieves the pain.
“Mastoiditis is one of the most feared complications, obviously,” Dr. Conrad noted, and it’s a clinical diagnosis that’s important to distinguish from mastoid effusion.
“Any child who has acute otitis media, and the middle ear fills up with fluid, which is under pressure, it will then migrate up the mastoid cavity; so, if you have an ear infection, you will have mastoid fluid – but that doesn’t necessarily mean you have mastoiditis,” he explained. “Mastoiditis is a very aggressive inflammatory process that destroys bone in the mastoid cavity. It’s often due to strep, and it’s usually a pyogenic organism that’s particularly virulent.”
Pus will then leak out from the mastoid cavity and form an abscess. If there is bone destruction, that is mastoiditis, which is treated with an ear tube or sometimes a mastoidectomy, in which a drill drains all the pus and other tissue.
Speech development and other controversies
Aside from the child’s pain, parental anxiety, and the other potential complications, researchers have learned more recently about speech delay with otitis media. The average child with recurrent otitis media or with otitis media with effusion will experience decreased hearing for about 3 or 4 months, which can affect speech, educational, and cognitive outcomes.
“If that process repeats itself, they could lose out on an entire year of not hearing well. It’s like walking around with an ear plug in,” Dr. Conrad said. It’s about a 25-35 dB hearing loss, he said, which can lead to trouble with speech discrimination, particularly with background noise, and can interfere with relationships with family, peers, and other adults.
Emerging data suggest educational difficulties, such as problems with reading comprehension, could result, and research is pivoting to look at potential cognitive development concerns, Dr. Conrad said.
“It has been noted that earlier onset of otitis media has a greater impact on educational and attention outcomes,” he said. Central auditory processing drives the development of the auditory cortex, and if that is impaired during a critical window of opportunity while synapses are forming, it could also have effects on speech.
“Otitis media and speech development is an area of controversy,” Dr. Conrad explained. Otitis media has been found to impact auditory processing skills, speech discrimination, auditory pattern recognition, and auditory temporal processing, “but there’s little evidence to support long-term language impairment,” he said.
But that’s being challenged now. Research in rats and cats in particular, however, has shown changes in the auditory cortex from ear infections.
“Most of the data are from animal models, and I think that will morph into more studies into educational outcomes in children who had a lot of ear infections when they were younger,” Dr. Conrad predicted.
Other areas of controversy relate to whether the use of the pneumococcal conjugate vaccine (PCV13), which has reduced ear infections, may have led to the rise of infections from Haemophilus influenzae and Moraxella catarrhalis, and what the duration of therapy should be for antibiotics.
If not doing watchful waiting, first-line treatment is amoxicillin or amoxicillin-clavulanate unless the child has a penicillin allergy, in which case cefdinir, cefuroxime, or cefpodoxime can be prescribed. After 48-72 hours of failed therapy, amoxicillin-clavulanate can be considered, or clindamycin or ceftriaxone, “obviously a popular option if the child has had multiple ear infections in the past month or so,” he said.
“If the child is older, we don’t treat as long,” Dr. Conrad noted. Current guidelines recommend a 10-day course if the infection resulted from strep, a 7-day or 10-day course in children aged 2-5 years, and a 5-7 day course for children older than 6 years.
Dr. Conrad reported no disclosures.
SAN FRANCISCO – As researchers have learned more about otitis media in the past decade, the guidelines have shifted accordingly for one of the most common conditions of childhood.
Yet some controversies remain, and the condition remains a challenge to properly identify, David Conrad, MD, of the University of California, San Francisco, said at the annual meeting of the American Academy of Pediatrics.
Pediatricians already know it’s the most common reason young children come into their offices and the most common reason they prescribe antibiotics. But they may know less about recognizing complications and long-term effects.
Complications and treatment
Ossicular erosion or tympanic membrane perforation are two complications; the latter’s rate is 5%-29% for untreated acute otitis media. It typically closes within hours to days, however, with a 95% closure rate within 4 weeks.
“The ear drum is pretty forgiving, pretty resilient, really,” Dr. Conrad said. The perforation occurs when pressure builds up and takes the path of least resistance through the drum, but that release of pressure also typically relieves the pain.
“Mastoiditis is one of the most feared complications, obviously,” Dr. Conrad noted, and it’s a clinical diagnosis that’s important to distinguish from mastoid effusion.
“Any child who has acute otitis media, and the middle ear fills up with fluid, which is under pressure, it will then migrate up the mastoid cavity; so, if you have an ear infection, you will have mastoid fluid – but that doesn’t necessarily mean you have mastoiditis,” he explained. “Mastoiditis is a very aggressive inflammatory process that destroys bone in the mastoid cavity. It’s often due to strep, and it’s usually a pyogenic organism that’s particularly virulent.”
Pus will then leak out from the mastoid cavity and form an abscess. If there is bone destruction, that is mastoiditis, which is treated with an ear tube or sometimes a mastoidectomy, in which a drill drains all the pus and other tissue.
Speech development and other controversies
Aside from the child’s pain, parental anxiety, and the other potential complications, researchers have learned more recently about speech delay with otitis media. The average child with recurrent otitis media or with otitis media with effusion will experience decreased hearing for about 3 or 4 months, which can affect speech, educational, and cognitive outcomes.
“If that process repeats itself, they could lose out on an entire year of not hearing well. It’s like walking around with an ear plug in,” Dr. Conrad said. It’s about a 25-35 dB hearing loss, he said, which can lead to trouble with speech discrimination, particularly with background noise, and can interfere with relationships with family, peers, and other adults.
Emerging data suggest educational difficulties, such as problems with reading comprehension, could result, and research is pivoting to look at potential cognitive development concerns, Dr. Conrad said.
“It has been noted that earlier onset of otitis media has a greater impact on educational and attention outcomes,” he said. Central auditory processing drives the development of the auditory cortex, and if that is impaired during a critical window of opportunity while synapses are forming, it could also have effects on speech.
“Otitis media and speech development is an area of controversy,” Dr. Conrad explained. Otitis media has been found to impact auditory processing skills, speech discrimination, auditory pattern recognition, and auditory temporal processing, “but there’s little evidence to support long-term language impairment,” he said.
But that’s being challenged now. Research in rats and cats in particular, however, has shown changes in the auditory cortex from ear infections.
“Most of the data are from animal models, and I think that will morph into more studies into educational outcomes in children who had a lot of ear infections when they were younger,” Dr. Conrad predicted.
Other areas of controversy relate to whether the use of the pneumococcal conjugate vaccine (PCV13), which has reduced ear infections, may have led to the rise of infections from Haemophilus influenzae and Moraxella catarrhalis, and what the duration of therapy should be for antibiotics.
If not doing watchful waiting, first-line treatment is amoxicillin or amoxicillin-clavulanate unless the child has a penicillin allergy, in which case cefdinir, cefuroxime, or cefpodoxime can be prescribed. After 48-72 hours of failed therapy, amoxicillin-clavulanate can be considered, or clindamycin or ceftriaxone, “obviously a popular option if the child has had multiple ear infections in the past month or so,” he said.
“If the child is older, we don’t treat as long,” Dr. Conrad noted. Current guidelines recommend a 10-day course if the infection resulted from strep, a 7-day or 10-day course in children aged 2-5 years, and a 5-7 day course for children older than 6 years.
Dr. Conrad reported no disclosures.
SAN FRANCISCO – As researchers have learned more about otitis media in the past decade, the guidelines have shifted accordingly for one of the most common conditions of childhood.
Yet some controversies remain, and the condition remains a challenge to properly identify, David Conrad, MD, of the University of California, San Francisco, said at the annual meeting of the American Academy of Pediatrics.
Pediatricians already know it’s the most common reason young children come into their offices and the most common reason they prescribe antibiotics. But they may know less about recognizing complications and long-term effects.
Complications and treatment
Ossicular erosion or tympanic membrane perforation are two complications; the latter’s rate is 5%-29% for untreated acute otitis media. It typically closes within hours to days, however, with a 95% closure rate within 4 weeks.
“The ear drum is pretty forgiving, pretty resilient, really,” Dr. Conrad said. The perforation occurs when pressure builds up and takes the path of least resistance through the drum, but that release of pressure also typically relieves the pain.
“Mastoiditis is one of the most feared complications, obviously,” Dr. Conrad noted, and it’s a clinical diagnosis that’s important to distinguish from mastoid effusion.
“Any child who has acute otitis media, and the middle ear fills up with fluid, which is under pressure, it will then migrate up the mastoid cavity; so, if you have an ear infection, you will have mastoid fluid – but that doesn’t necessarily mean you have mastoiditis,” he explained. “Mastoiditis is a very aggressive inflammatory process that destroys bone in the mastoid cavity. It’s often due to strep, and it’s usually a pyogenic organism that’s particularly virulent.”
Pus will then leak out from the mastoid cavity and form an abscess. If there is bone destruction, that is mastoiditis, which is treated with an ear tube or sometimes a mastoidectomy, in which a drill drains all the pus and other tissue.
Speech development and other controversies
Aside from the child’s pain, parental anxiety, and the other potential complications, researchers have learned more recently about speech delay with otitis media. The average child with recurrent otitis media or with otitis media with effusion will experience decreased hearing for about 3 or 4 months, which can affect speech, educational, and cognitive outcomes.
“If that process repeats itself, they could lose out on an entire year of not hearing well. It’s like walking around with an ear plug in,” Dr. Conrad said. It’s about a 25-35 dB hearing loss, he said, which can lead to trouble with speech discrimination, particularly with background noise, and can interfere with relationships with family, peers, and other adults.
Emerging data suggest educational difficulties, such as problems with reading comprehension, could result, and research is pivoting to look at potential cognitive development concerns, Dr. Conrad said.
“It has been noted that earlier onset of otitis media has a greater impact on educational and attention outcomes,” he said. Central auditory processing drives the development of the auditory cortex, and if that is impaired during a critical window of opportunity while synapses are forming, it could also have effects on speech.
“Otitis media and speech development is an area of controversy,” Dr. Conrad explained. Otitis media has been found to impact auditory processing skills, speech discrimination, auditory pattern recognition, and auditory temporal processing, “but there’s little evidence to support long-term language impairment,” he said.
But that’s being challenged now. Research in rats and cats in particular, however, has shown changes in the auditory cortex from ear infections.
“Most of the data are from animal models, and I think that will morph into more studies into educational outcomes in children who had a lot of ear infections when they were younger,” Dr. Conrad predicted.
Other areas of controversy relate to whether the use of the pneumococcal conjugate vaccine (PCV13), which has reduced ear infections, may have led to the rise of infections from Haemophilus influenzae and Moraxella catarrhalis, and what the duration of therapy should be for antibiotics.
If not doing watchful waiting, first-line treatment is amoxicillin or amoxicillin-clavulanate unless the child has a penicillin allergy, in which case cefdinir, cefuroxime, or cefpodoxime can be prescribed. After 48-72 hours of failed therapy, amoxicillin-clavulanate can be considered, or clindamycin or ceftriaxone, “obviously a popular option if the child has had multiple ear infections in the past month or so,” he said.
“If the child is older, we don’t treat as long,” Dr. Conrad noted. Current guidelines recommend a 10-day course if the infection resulted from strep, a 7-day or 10-day course in children aged 2-5 years, and a 5-7 day course for children older than 6 years.
Dr. Conrad reported no disclosures.
Wide spectrum of feeding problems poses challenge for clinicians
SAN FRANCISCO – Clinicians are likely to encounter diverse feeding problems in daily practice that will challenge their diagnostic and treatment acumen, Dr. Irene Chatoor told attendees of the annual meeting of the American Academy of Pediatrics.
These problems run the gamut from the most prevalent but least serious picky eating, to the least prevalent but most serious feeding disorders, she noted. Correspondingly, management will range from simple reassurance of parents to more intensive behavioral and medical interventions.
Assessment
“When you assess a feeding problem, you have to look at both the mother and father, and the child,” she advised. The parents are evaluated for their feeding style, while the child is evaluated for three feeding problems: limited appetite, selective intake, and fear of feeding (Pediatrics. 2015;135[2]:344-53).
Clinicians must be alert for organic red flags, such as dysphagia, aspiration, and vomiting, and for behavioral red flags, such as food fixation, abrupt cessation of feeding after a trigger event, and anticipatory gagging. An overarching red flag is failure to thrive.
Sometimes, a child will have both an organic condition and a behavioral feeding disorder at the same time. “It’s very important that you don’t think one excludes the other,” she cautioned.
Diagnosis
“To delineate milder feeding difficulties from feeding disorders, there must be some form of impairment caused by the feeding problem,” Dr. Chatoor commented. “Why is this important? For two reasons. One is for the insurance companies, because they don’t pay unless there is a disorder. And then there is research: you cannot do research unless you clearly define what you are studying.”
Children are considered to have impairment if they have weight loss or growth faltering, considerable nutritional deficiency, or a marked interference with psychosocial functioning.
“When we diagnose feeding problems, it is best done with a multidisciplinary team,” Dr. Chatoor maintained. “I have learned many years ago that I’m not effective in helping parents deal with the feeding disorder if they are still in the back of their mind worried that the child has something organically wrong and that’s why the child does not want to eat.”
Accordingly, various team members perform a medical examination, a nutritional assessment, an oral motor and sensory evaluation, and a psychiatric or psychological assessment to identify the root cause or causes of the problem.
When it comes to behavioral etiologies, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) now groups all feeding and eating disorders together in one section, reflecting the fact that disorders starting early in life can and often do track into adolescence and adulthood, according to Dr. Chatoor.
The manual also features a new diagnosis, avoidant/restrictive food intake disorder (ARFID). Key criteria include the presence of an eating or feeding disturbance that cannot be better explained by lack of available food, culturally sanctioned practices, or a concurrent medical condition or another mental disorder.
The child must have a persistent failure to meet appropriate nutritional and/or energy needs, associated with any of four findings: significant weight loss or failure to achieve expected weight gain or growth, significant nutritional deficiencies, dependence on enteral feeding or oral nutritional supplements, and marked interference with psychosocial functioning.
“You need to have at least one but often you have a combination of nutritional and emotional impairment in the same child,” she commented.
ARFID and its treatment
There are three subtypes of ARFID having different features, treatments, and prognosis, although they all share in common food refusal, according to Dr. Chatoor.
The first subtype – apparent lack of interest in eating or food – emerges by 3 years of age, most often during the transition to self-feeding between 9 and 18 months. Affected children refuse to eat an adequate amount of food for at least 1 month, rarely communicate hunger, lack interest in food, and prefer to play or talk. They typically present with growth deficiency.
“If you have a child who refuses to eat, it generates anxiety in the mother. The mother does things she would not normally do with the child who is eating well. She starts to distract, to cajole, to sometimes even force-feed the child,” Dr. Chatoor explained. “And the more she engages in these behaviors, the more resistant the child becomes. So they become trapped in this vicious cycle.”
Treatment is aimed at removing this conflict with three approaches: explaining to parents the infant’s special temperament (notably, high arousal and difficulty turning off excitement); addressing their background, including any eating issues of their own, and difficulty with setting limits; and providing specific feeding guidelines and a time-out procedure.
The guidelines stress regular feeding, withholding of all snacks, keeping the child at the table for 20 to 30 minutes, and not using any distractions or pressure. Also, importantly, the parents should have dinner with their child. “I always tell the parents what is good for the child is good for you. It’s good for your whole family,” she said. “If they have other children, these rules apply to everybody. Young children learn to eat by watching their parents eating.”
With early and consistent use of these interventions, about two-thirds of children outgrow this eating/feeding disturbance by mid-childhood, according to Dr. Chatoor.
Children with the second subtype of ARFID – avoidance based on the sensory characteristics of food – consistently refuse to eat certain foods having specific tastes, textures, temperatures, smells, and/or appearances. Onset occurs during the toddler years, when a new or different food is introduced.
“Not only do they refuse the same foods that were aversive, but they also generalize it. So these children are afraid to try other foods and they may end up limiting food groups – they don’t eat any vegetables and some of them don’t eat any meats,” she explained. “They are a challenge because this always causes a nutritional deficiency and they also have problems socially as they get older.”
Treatment varies by age, with gradual desensitization for infants and parent modeling of eating new foods for toddlers. A multifaceted approach is used for preschoolers, combining modeling, giving foods attractive shapes and names, having the child participate in food preparation, and using focused play therapy, such as feeding dolls who are “brave” and try new foods.
Clinicians can explain to affected school-aged children that they are “supertasters,” having more taste buds and therefore experiencing food more intensely, and that they can help their taste buds not react so strongly by starting to eat small amounts of new foods and gradually increasing over time. Parents can let the child make a list of 10 foods they would like to eat, and award them points for “courage” for every bite of a new food they try.
Prognosis of this type of ARFID varies, according to Dr. Chatoor. “Through gradual exposure, young children can expand the variety of foods they eat,” she elaborated. However, “some children become very rigid and brand sensitive in regard to the food they are willing to eat and begin to experience social problems during mid-childhood and adolescence. Some children grow up eating a limited diet, but finding ways to compensate nutritionally and socially.”
Children with the third subtype of ARFID – concern about aversive consequences of eating – have an acute onset of consistent food refusal at any age, from infancy onward, after experiencing a traumatic event or repeated traumatic insults to the oropharynx or gastrointestinal tract that trigger distress in the child. These children often have comorbidities such as gastroesophageal reflux, eosinophilic gastroenteritis, or anxiety disorder.
“Treatment involves gradual desensitization to feared objects: the highchair, bib, bottle, or spoon,” Dr. Chatoor explained. “It also involves training of the mother in behavioral techniques to feed the child in spite of the child’s fear and distress.”
Any underlying medical condition causing pain or distress should be treated. Additional measures may include, for example, use of a graduated approach, starting with liquids and progressing to purees, if the child fears solid foods, and prescribing anxiolytic medication in cases of severe anxiety.
Dr. Chatoor disclosed that she has lectured internationally at conferences on feeding disorders that were organized by Abbott Nutrition International and that the company provided a research grant for a study on feeding.
SAN FRANCISCO – Clinicians are likely to encounter diverse feeding problems in daily practice that will challenge their diagnostic and treatment acumen, Dr. Irene Chatoor told attendees of the annual meeting of the American Academy of Pediatrics.
These problems run the gamut from the most prevalent but least serious picky eating, to the least prevalent but most serious feeding disorders, she noted. Correspondingly, management will range from simple reassurance of parents to more intensive behavioral and medical interventions.
Assessment
“When you assess a feeding problem, you have to look at both the mother and father, and the child,” she advised. The parents are evaluated for their feeding style, while the child is evaluated for three feeding problems: limited appetite, selective intake, and fear of feeding (Pediatrics. 2015;135[2]:344-53).
Clinicians must be alert for organic red flags, such as dysphagia, aspiration, and vomiting, and for behavioral red flags, such as food fixation, abrupt cessation of feeding after a trigger event, and anticipatory gagging. An overarching red flag is failure to thrive.
Sometimes, a child will have both an organic condition and a behavioral feeding disorder at the same time. “It’s very important that you don’t think one excludes the other,” she cautioned.
Diagnosis
“To delineate milder feeding difficulties from feeding disorders, there must be some form of impairment caused by the feeding problem,” Dr. Chatoor commented. “Why is this important? For two reasons. One is for the insurance companies, because they don’t pay unless there is a disorder. And then there is research: you cannot do research unless you clearly define what you are studying.”
Children are considered to have impairment if they have weight loss or growth faltering, considerable nutritional deficiency, or a marked interference with psychosocial functioning.
“When we diagnose feeding problems, it is best done with a multidisciplinary team,” Dr. Chatoor maintained. “I have learned many years ago that I’m not effective in helping parents deal with the feeding disorder if they are still in the back of their mind worried that the child has something organically wrong and that’s why the child does not want to eat.”
Accordingly, various team members perform a medical examination, a nutritional assessment, an oral motor and sensory evaluation, and a psychiatric or psychological assessment to identify the root cause or causes of the problem.
When it comes to behavioral etiologies, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) now groups all feeding and eating disorders together in one section, reflecting the fact that disorders starting early in life can and often do track into adolescence and adulthood, according to Dr. Chatoor.
The manual also features a new diagnosis, avoidant/restrictive food intake disorder (ARFID). Key criteria include the presence of an eating or feeding disturbance that cannot be better explained by lack of available food, culturally sanctioned practices, or a concurrent medical condition or another mental disorder.
The child must have a persistent failure to meet appropriate nutritional and/or energy needs, associated with any of four findings: significant weight loss or failure to achieve expected weight gain or growth, significant nutritional deficiencies, dependence on enteral feeding or oral nutritional supplements, and marked interference with psychosocial functioning.
“You need to have at least one but often you have a combination of nutritional and emotional impairment in the same child,” she commented.
ARFID and its treatment
There are three subtypes of ARFID having different features, treatments, and prognosis, although they all share in common food refusal, according to Dr. Chatoor.
The first subtype – apparent lack of interest in eating or food – emerges by 3 years of age, most often during the transition to self-feeding between 9 and 18 months. Affected children refuse to eat an adequate amount of food for at least 1 month, rarely communicate hunger, lack interest in food, and prefer to play or talk. They typically present with growth deficiency.
“If you have a child who refuses to eat, it generates anxiety in the mother. The mother does things she would not normally do with the child who is eating well. She starts to distract, to cajole, to sometimes even force-feed the child,” Dr. Chatoor explained. “And the more she engages in these behaviors, the more resistant the child becomes. So they become trapped in this vicious cycle.”
Treatment is aimed at removing this conflict with three approaches: explaining to parents the infant’s special temperament (notably, high arousal and difficulty turning off excitement); addressing their background, including any eating issues of their own, and difficulty with setting limits; and providing specific feeding guidelines and a time-out procedure.
The guidelines stress regular feeding, withholding of all snacks, keeping the child at the table for 20 to 30 minutes, and not using any distractions or pressure. Also, importantly, the parents should have dinner with their child. “I always tell the parents what is good for the child is good for you. It’s good for your whole family,” she said. “If they have other children, these rules apply to everybody. Young children learn to eat by watching their parents eating.”
With early and consistent use of these interventions, about two-thirds of children outgrow this eating/feeding disturbance by mid-childhood, according to Dr. Chatoor.
Children with the second subtype of ARFID – avoidance based on the sensory characteristics of food – consistently refuse to eat certain foods having specific tastes, textures, temperatures, smells, and/or appearances. Onset occurs during the toddler years, when a new or different food is introduced.
“Not only do they refuse the same foods that were aversive, but they also generalize it. So these children are afraid to try other foods and they may end up limiting food groups – they don’t eat any vegetables and some of them don’t eat any meats,” she explained. “They are a challenge because this always causes a nutritional deficiency and they also have problems socially as they get older.”
Treatment varies by age, with gradual desensitization for infants and parent modeling of eating new foods for toddlers. A multifaceted approach is used for preschoolers, combining modeling, giving foods attractive shapes and names, having the child participate in food preparation, and using focused play therapy, such as feeding dolls who are “brave” and try new foods.
Clinicians can explain to affected school-aged children that they are “supertasters,” having more taste buds and therefore experiencing food more intensely, and that they can help their taste buds not react so strongly by starting to eat small amounts of new foods and gradually increasing over time. Parents can let the child make a list of 10 foods they would like to eat, and award them points for “courage” for every bite of a new food they try.
Prognosis of this type of ARFID varies, according to Dr. Chatoor. “Through gradual exposure, young children can expand the variety of foods they eat,” she elaborated. However, “some children become very rigid and brand sensitive in regard to the food they are willing to eat and begin to experience social problems during mid-childhood and adolescence. Some children grow up eating a limited diet, but finding ways to compensate nutritionally and socially.”
Children with the third subtype of ARFID – concern about aversive consequences of eating – have an acute onset of consistent food refusal at any age, from infancy onward, after experiencing a traumatic event or repeated traumatic insults to the oropharynx or gastrointestinal tract that trigger distress in the child. These children often have comorbidities such as gastroesophageal reflux, eosinophilic gastroenteritis, or anxiety disorder.
“Treatment involves gradual desensitization to feared objects: the highchair, bib, bottle, or spoon,” Dr. Chatoor explained. “It also involves training of the mother in behavioral techniques to feed the child in spite of the child’s fear and distress.”
Any underlying medical condition causing pain or distress should be treated. Additional measures may include, for example, use of a graduated approach, starting with liquids and progressing to purees, if the child fears solid foods, and prescribing anxiolytic medication in cases of severe anxiety.
Dr. Chatoor disclosed that she has lectured internationally at conferences on feeding disorders that were organized by Abbott Nutrition International and that the company provided a research grant for a study on feeding.
SAN FRANCISCO – Clinicians are likely to encounter diverse feeding problems in daily practice that will challenge their diagnostic and treatment acumen, Dr. Irene Chatoor told attendees of the annual meeting of the American Academy of Pediatrics.
These problems run the gamut from the most prevalent but least serious picky eating, to the least prevalent but most serious feeding disorders, she noted. Correspondingly, management will range from simple reassurance of parents to more intensive behavioral and medical interventions.
Assessment
“When you assess a feeding problem, you have to look at both the mother and father, and the child,” she advised. The parents are evaluated for their feeding style, while the child is evaluated for three feeding problems: limited appetite, selective intake, and fear of feeding (Pediatrics. 2015;135[2]:344-53).
Clinicians must be alert for organic red flags, such as dysphagia, aspiration, and vomiting, and for behavioral red flags, such as food fixation, abrupt cessation of feeding after a trigger event, and anticipatory gagging. An overarching red flag is failure to thrive.
Sometimes, a child will have both an organic condition and a behavioral feeding disorder at the same time. “It’s very important that you don’t think one excludes the other,” she cautioned.
Diagnosis
“To delineate milder feeding difficulties from feeding disorders, there must be some form of impairment caused by the feeding problem,” Dr. Chatoor commented. “Why is this important? For two reasons. One is for the insurance companies, because they don’t pay unless there is a disorder. And then there is research: you cannot do research unless you clearly define what you are studying.”
Children are considered to have impairment if they have weight loss or growth faltering, considerable nutritional deficiency, or a marked interference with psychosocial functioning.
“When we diagnose feeding problems, it is best done with a multidisciplinary team,” Dr. Chatoor maintained. “I have learned many years ago that I’m not effective in helping parents deal with the feeding disorder if they are still in the back of their mind worried that the child has something organically wrong and that’s why the child does not want to eat.”
Accordingly, various team members perform a medical examination, a nutritional assessment, an oral motor and sensory evaluation, and a psychiatric or psychological assessment to identify the root cause or causes of the problem.
When it comes to behavioral etiologies, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) now groups all feeding and eating disorders together in one section, reflecting the fact that disorders starting early in life can and often do track into adolescence and adulthood, according to Dr. Chatoor.
The manual also features a new diagnosis, avoidant/restrictive food intake disorder (ARFID). Key criteria include the presence of an eating or feeding disturbance that cannot be better explained by lack of available food, culturally sanctioned practices, or a concurrent medical condition or another mental disorder.
The child must have a persistent failure to meet appropriate nutritional and/or energy needs, associated with any of four findings: significant weight loss or failure to achieve expected weight gain or growth, significant nutritional deficiencies, dependence on enteral feeding or oral nutritional supplements, and marked interference with psychosocial functioning.
“You need to have at least one but often you have a combination of nutritional and emotional impairment in the same child,” she commented.
ARFID and its treatment
There are three subtypes of ARFID having different features, treatments, and prognosis, although they all share in common food refusal, according to Dr. Chatoor.
The first subtype – apparent lack of interest in eating or food – emerges by 3 years of age, most often during the transition to self-feeding between 9 and 18 months. Affected children refuse to eat an adequate amount of food for at least 1 month, rarely communicate hunger, lack interest in food, and prefer to play or talk. They typically present with growth deficiency.
“If you have a child who refuses to eat, it generates anxiety in the mother. The mother does things she would not normally do with the child who is eating well. She starts to distract, to cajole, to sometimes even force-feed the child,” Dr. Chatoor explained. “And the more she engages in these behaviors, the more resistant the child becomes. So they become trapped in this vicious cycle.”
Treatment is aimed at removing this conflict with three approaches: explaining to parents the infant’s special temperament (notably, high arousal and difficulty turning off excitement); addressing their background, including any eating issues of their own, and difficulty with setting limits; and providing specific feeding guidelines and a time-out procedure.
The guidelines stress regular feeding, withholding of all snacks, keeping the child at the table for 20 to 30 minutes, and not using any distractions or pressure. Also, importantly, the parents should have dinner with their child. “I always tell the parents what is good for the child is good for you. It’s good for your whole family,” she said. “If they have other children, these rules apply to everybody. Young children learn to eat by watching their parents eating.”
With early and consistent use of these interventions, about two-thirds of children outgrow this eating/feeding disturbance by mid-childhood, according to Dr. Chatoor.
Children with the second subtype of ARFID – avoidance based on the sensory characteristics of food – consistently refuse to eat certain foods having specific tastes, textures, temperatures, smells, and/or appearances. Onset occurs during the toddler years, when a new or different food is introduced.
“Not only do they refuse the same foods that were aversive, but they also generalize it. So these children are afraid to try other foods and they may end up limiting food groups – they don’t eat any vegetables and some of them don’t eat any meats,” she explained. “They are a challenge because this always causes a nutritional deficiency and they also have problems socially as they get older.”
Treatment varies by age, with gradual desensitization for infants and parent modeling of eating new foods for toddlers. A multifaceted approach is used for preschoolers, combining modeling, giving foods attractive shapes and names, having the child participate in food preparation, and using focused play therapy, such as feeding dolls who are “brave” and try new foods.
Clinicians can explain to affected school-aged children that they are “supertasters,” having more taste buds and therefore experiencing food more intensely, and that they can help their taste buds not react so strongly by starting to eat small amounts of new foods and gradually increasing over time. Parents can let the child make a list of 10 foods they would like to eat, and award them points for “courage” for every bite of a new food they try.
Prognosis of this type of ARFID varies, according to Dr. Chatoor. “Through gradual exposure, young children can expand the variety of foods they eat,” she elaborated. However, “some children become very rigid and brand sensitive in regard to the food they are willing to eat and begin to experience social problems during mid-childhood and adolescence. Some children grow up eating a limited diet, but finding ways to compensate nutritionally and socially.”
Children with the third subtype of ARFID – concern about aversive consequences of eating – have an acute onset of consistent food refusal at any age, from infancy onward, after experiencing a traumatic event or repeated traumatic insults to the oropharynx or gastrointestinal tract that trigger distress in the child. These children often have comorbidities such as gastroesophageal reflux, eosinophilic gastroenteritis, or anxiety disorder.
“Treatment involves gradual desensitization to feared objects: the highchair, bib, bottle, or spoon,” Dr. Chatoor explained. “It also involves training of the mother in behavioral techniques to feed the child in spite of the child’s fear and distress.”
Any underlying medical condition causing pain or distress should be treated. Additional measures may include, for example, use of a graduated approach, starting with liquids and progressing to purees, if the child fears solid foods, and prescribing anxiolytic medication in cases of severe anxiety.
Dr. Chatoor disclosed that she has lectured internationally at conferences on feeding disorders that were organized by Abbott Nutrition International and that the company provided a research grant for a study on feeding.
EXPERT ANALYSIS FROM AAP 16
Pornography warps children’s concept of sex, sexual identity
SAN FRANCISCO – The pornography industry has taken over children’s sense of self and sexuality and warped their concept of what sex and a sexual identity is, said Gail Dines, PhD.
She challenged pediatricians to shape policy and help parents in wrangling back that control in a presentation at the annual meeting of the American Academy of Pediatrics.
The culprit, Dr. Dines charged, is the multibillion-dollar porn industry that exploded around the year 2000 with the Internet. Then, in 2011, the business model shifted to free pornography to hook young boys in their adolescence and hopefully maintain them as customers after age 18 when they could get their own credit cards.
The average age of a boy’s first encounter with pornography is age 11, explained Dr. Dines, a professor of sociology and women’s studies at Wheelock College in Chestnut Hill, Mass.
Instead of a father’s Playboy featuring a naked woman in a cornfield, as many male pediatricians in the room might have been introduced to pornography or sexuality, today’s youth are introduced via the brutalization and dehumanization of women, she said. Such experiences traumatize the children viewing them, who become confused about who they are if they are masturbating to images and video of sexual violence, and then they enter a cycle of retraumatization that engenders shame while bringing children back to those sites again and again.
“Hence, in the business model of free porn, you are building in trauma, which is building in addiction,” Dr. Dines said. The effects of this exposure and addiction, based on decades of research, include limited capacity for intimacy, a greater likelihood of using coercive tactics for sex, decreased empathy for rape victims, increased depression and anxiety, and, most recently, rates of erectile dysfunction in males aged 15-27 that mirror the rates in those aged 27-35.
“We have never brought up boys with access to hard core pornography 24-7,” Dr. Dines said. The best way to tackle hard-core pornography is a public health model that educates parents and pediatricians who can band together to raise awareness. Her organization, Culture Reframed, is attempting to do precisely that.
Dr. Dines founded the nonprofit Culture Reframed, which attempts to counter the effects of the pornography industry and media sexuality. Her presentation used no external funding.
SAN FRANCISCO – The pornography industry has taken over children’s sense of self and sexuality and warped their concept of what sex and a sexual identity is, said Gail Dines, PhD.
She challenged pediatricians to shape policy and help parents in wrangling back that control in a presentation at the annual meeting of the American Academy of Pediatrics.
The culprit, Dr. Dines charged, is the multibillion-dollar porn industry that exploded around the year 2000 with the Internet. Then, in 2011, the business model shifted to free pornography to hook young boys in their adolescence and hopefully maintain them as customers after age 18 when they could get their own credit cards.
The average age of a boy’s first encounter with pornography is age 11, explained Dr. Dines, a professor of sociology and women’s studies at Wheelock College in Chestnut Hill, Mass.
Instead of a father’s Playboy featuring a naked woman in a cornfield, as many male pediatricians in the room might have been introduced to pornography or sexuality, today’s youth are introduced via the brutalization and dehumanization of women, she said. Such experiences traumatize the children viewing them, who become confused about who they are if they are masturbating to images and video of sexual violence, and then they enter a cycle of retraumatization that engenders shame while bringing children back to those sites again and again.
“Hence, in the business model of free porn, you are building in trauma, which is building in addiction,” Dr. Dines said. The effects of this exposure and addiction, based on decades of research, include limited capacity for intimacy, a greater likelihood of using coercive tactics for sex, decreased empathy for rape victims, increased depression and anxiety, and, most recently, rates of erectile dysfunction in males aged 15-27 that mirror the rates in those aged 27-35.
“We have never brought up boys with access to hard core pornography 24-7,” Dr. Dines said. The best way to tackle hard-core pornography is a public health model that educates parents and pediatricians who can band together to raise awareness. Her organization, Culture Reframed, is attempting to do precisely that.
Dr. Dines founded the nonprofit Culture Reframed, which attempts to counter the effects of the pornography industry and media sexuality. Her presentation used no external funding.
SAN FRANCISCO – The pornography industry has taken over children’s sense of self and sexuality and warped their concept of what sex and a sexual identity is, said Gail Dines, PhD.
She challenged pediatricians to shape policy and help parents in wrangling back that control in a presentation at the annual meeting of the American Academy of Pediatrics.
The culprit, Dr. Dines charged, is the multibillion-dollar porn industry that exploded around the year 2000 with the Internet. Then, in 2011, the business model shifted to free pornography to hook young boys in their adolescence and hopefully maintain them as customers after age 18 when they could get their own credit cards.
The average age of a boy’s first encounter with pornography is age 11, explained Dr. Dines, a professor of sociology and women’s studies at Wheelock College in Chestnut Hill, Mass.
Instead of a father’s Playboy featuring a naked woman in a cornfield, as many male pediatricians in the room might have been introduced to pornography or sexuality, today’s youth are introduced via the brutalization and dehumanization of women, she said. Such experiences traumatize the children viewing them, who become confused about who they are if they are masturbating to images and video of sexual violence, and then they enter a cycle of retraumatization that engenders shame while bringing children back to those sites again and again.
“Hence, in the business model of free porn, you are building in trauma, which is building in addiction,” Dr. Dines said. The effects of this exposure and addiction, based on decades of research, include limited capacity for intimacy, a greater likelihood of using coercive tactics for sex, decreased empathy for rape victims, increased depression and anxiety, and, most recently, rates of erectile dysfunction in males aged 15-27 that mirror the rates in those aged 27-35.
“We have never brought up boys with access to hard core pornography 24-7,” Dr. Dines said. The best way to tackle hard-core pornography is a public health model that educates parents and pediatricians who can band together to raise awareness. Her organization, Culture Reframed, is attempting to do precisely that.
Dr. Dines founded the nonprofit Culture Reframed, which attempts to counter the effects of the pornography industry and media sexuality. Her presentation used no external funding.
EXPERT ANALYSIS FROM AAP 16
Mental health integration into pediatric primary care offers multiple benefits
SAN FRANCISCO – Integrating pediatric mental health care into your primary care office can be an effective way to ensure your patients get the care they really need – and it’s easier than you think.
That’s the message Jay Rabinowitz, MD, MPH, a clinical professor of pediatrics at the University of Colorado at Denver, Aurora, delivered to a packed room at the annual meeting of the American Academy of Pediatrics.
He noted that depression and anxiety are among the top five conditions driving overall health costs in the United States, and a 1999 Surgeon General’s Report found that one in five children have a diagnosable mental disorder – but only a fifth to a quarter of these children receive treatment. The rub is that treatment is highly successful; it’s just difficult to access for many families, so making it a part of a child’s medical home just makes sense, Dr. Rabinowitz said.
To drive home his point, he described a case of a depressed adolescent with cutting and suicidal ideation, and the steps he would need to take without integration: find out their insurance, get a list of covered mental health professionals, refer to someone he may or may not heard of, and then rarely receive follow-up reports, much less confirmation the patient had gone to the appointment. With integrated care, parents can make appointments on their way out, he can read the psychologist’s report immediately after the visit, and he can drop in to say hello during the child’s mental health appointment.
“Sometimes there’s a question abut a medication or something, and sometimes it’s an inopportune moment if the child is sad or crying, but generally it seems to be pretty popular,” he said.
Taking steps toward integration
If providers are interesting in exploring the possibility of integration, they need to consider and decide on several issues before taking any concrete steps, Dr. Rabinowitz said. One is the type of arrangement that would work best for your practice: hiring on mental health professionals as employees of the practice, hiring independent contractors, coordinating a space share agreement or creating an out-of-office agreement.
“In our practice, psychologists are employees of the practice, but there are other arrangements,” he said, and some may depend on what is easiest based on state law or billing procedures.
The next question is what kind of provider(s) you would hire. His office has child psychologists with a PhD and postdoctorate fellowships working with children, but other possibilities include social workers, licensed counselors, psychiatric nurse practitioners, or psychiatrists.
Another consideration is what diagnoses your office will handle because it’s not possible to see everything. His practice sees patients in-house for attention deficit/hyperactivity disorder (ADHD), depression, anxiety, drug counseling, and behavioral and adjustment disorders. They choose to refer out educational testing, autism, difficult divorce cases, and complex cases that require more than 20 sessions. They refer out divorce cases because they frequently require specialized knowledge and a lot of court time and phone calls. Aside from ADHD evaluations, his office does not see the staff’s children.
Providers also should consider options for adapting their physical space to accommodate integration. His practice converted an exam room into a consultation room, making it homier with a throw rug, soft chairs, a painted wall, and office decor.
Establishing effective protocols with integration
The next step after providers decide to integrate is to determine the office protocols that govern what forms get used, who can schedule appointments and how long they last, billing, and similar procedures.
“You need to have certain protocols, and some of these things you don’t think about it until you start doing it,” Dr. Rabinowitz said. Should mental health appointments be 50 minutes, for example, or 20 to 25 minutes? His office has gradually shrunk these appointments from 50 to 30 minutes, but they give psychologists an hour of time each day for follow-up phone calls.
Forms to consider developing include a disclosure form, notice of privacy practices, late cancel/no show policy, financial policy, and a summary of parent concerns. His office’s charting includes an extensive intake form with medical, treatment, family, and social history, an intake summary, and a progress note.
It’s with reimbursement, of course, that providers will need to do the most research, particularly with regard to their state’s laws and in looking for grants to provide funding – which is more available than many realize.
“Money is often out there if you look for it,” Dr. Rabinowitz said.” Mental health is an area where no one is really against it: You get together the NRA (National Rifle Association) and the anti-gun movement, and they are both for it.”
Planning for reimbursement challenges
Reimbursement barriers can include lack of payment if mental health codes are used instead of pediatrics ones (depending on the practice arrangement), lack of “incident to” payments, same day billing of physical and mental health appointments, reimbursement for screening, and lack of payment for non–face-to-face services. Although a concierge or fee-for-service option solves many of these, it excludes Medicaid patients and is an economic barrier for many families.
Mental health networks offer a different route, but they can involve poor reimbursement and an additional layer of administration, which makes financial integration more viable as long as providers investigate their options.
“It’s going to be a regional variation, and you need to look at state rules and regulations,” Dr. Rabinowitz said, explaining that his office then sought insurance contracts to include mental health care reimbursement through their office and then sought the same from Medicaid.
“We weren’t about to see Medicaid patients for fear of an audit unless we got written permission, but we got that,” he said. His office simply asked for it and received in writing a letter starting as follows: “Under Department policy, they (our psychologists) may submit E&M claims to Medicaid under a supervising physician’s billing ID. It is not mandatory they be credentialed into a BHO (Behavioral Healthcare Options) network…”
He also noted that his state allows inclusion of psychologists on medical malpractice insurance policies, which is far less expensive for mental health professionals, compared with medical doctors.
Ultimately, the result of mental health integration into primary care practices is greater satisfaction among patients and pediatricians as well as potentially better health outcomes, Dr. Rabinowitz said. An in-house patient satisfaction survey his office conducted found that 91% of parents felt it was convenient for their child to receive mental health services at the same location as medical care, and 90% were satisfied with their care. Only 9% cited barriers to their child seeing a psychologist at their office, and 89% found the services beneficial for their child. Similarly, providers find integration more convenient, easier for follow-up, less stressful, and more efficient while improving communication, confidence, and follow-up.
Dr. Rabinowitz reported no disclosures. No external funding was used for the presentation.
SAN FRANCISCO – Integrating pediatric mental health care into your primary care office can be an effective way to ensure your patients get the care they really need – and it’s easier than you think.
That’s the message Jay Rabinowitz, MD, MPH, a clinical professor of pediatrics at the University of Colorado at Denver, Aurora, delivered to a packed room at the annual meeting of the American Academy of Pediatrics.
He noted that depression and anxiety are among the top five conditions driving overall health costs in the United States, and a 1999 Surgeon General’s Report found that one in five children have a diagnosable mental disorder – but only a fifth to a quarter of these children receive treatment. The rub is that treatment is highly successful; it’s just difficult to access for many families, so making it a part of a child’s medical home just makes sense, Dr. Rabinowitz said.
To drive home his point, he described a case of a depressed adolescent with cutting and suicidal ideation, and the steps he would need to take without integration: find out their insurance, get a list of covered mental health professionals, refer to someone he may or may not heard of, and then rarely receive follow-up reports, much less confirmation the patient had gone to the appointment. With integrated care, parents can make appointments on their way out, he can read the psychologist’s report immediately after the visit, and he can drop in to say hello during the child’s mental health appointment.
“Sometimes there’s a question abut a medication or something, and sometimes it’s an inopportune moment if the child is sad or crying, but generally it seems to be pretty popular,” he said.
Taking steps toward integration
If providers are interesting in exploring the possibility of integration, they need to consider and decide on several issues before taking any concrete steps, Dr. Rabinowitz said. One is the type of arrangement that would work best for your practice: hiring on mental health professionals as employees of the practice, hiring independent contractors, coordinating a space share agreement or creating an out-of-office agreement.
“In our practice, psychologists are employees of the practice, but there are other arrangements,” he said, and some may depend on what is easiest based on state law or billing procedures.
The next question is what kind of provider(s) you would hire. His office has child psychologists with a PhD and postdoctorate fellowships working with children, but other possibilities include social workers, licensed counselors, psychiatric nurse practitioners, or psychiatrists.
Another consideration is what diagnoses your office will handle because it’s not possible to see everything. His practice sees patients in-house for attention deficit/hyperactivity disorder (ADHD), depression, anxiety, drug counseling, and behavioral and adjustment disorders. They choose to refer out educational testing, autism, difficult divorce cases, and complex cases that require more than 20 sessions. They refer out divorce cases because they frequently require specialized knowledge and a lot of court time and phone calls. Aside from ADHD evaluations, his office does not see the staff’s children.
Providers also should consider options for adapting their physical space to accommodate integration. His practice converted an exam room into a consultation room, making it homier with a throw rug, soft chairs, a painted wall, and office decor.
Establishing effective protocols with integration
The next step after providers decide to integrate is to determine the office protocols that govern what forms get used, who can schedule appointments and how long they last, billing, and similar procedures.
“You need to have certain protocols, and some of these things you don’t think about it until you start doing it,” Dr. Rabinowitz said. Should mental health appointments be 50 minutes, for example, or 20 to 25 minutes? His office has gradually shrunk these appointments from 50 to 30 minutes, but they give psychologists an hour of time each day for follow-up phone calls.
Forms to consider developing include a disclosure form, notice of privacy practices, late cancel/no show policy, financial policy, and a summary of parent concerns. His office’s charting includes an extensive intake form with medical, treatment, family, and social history, an intake summary, and a progress note.
It’s with reimbursement, of course, that providers will need to do the most research, particularly with regard to their state’s laws and in looking for grants to provide funding – which is more available than many realize.
“Money is often out there if you look for it,” Dr. Rabinowitz said.” Mental health is an area where no one is really against it: You get together the NRA (National Rifle Association) and the anti-gun movement, and they are both for it.”
Planning for reimbursement challenges
Reimbursement barriers can include lack of payment if mental health codes are used instead of pediatrics ones (depending on the practice arrangement), lack of “incident to” payments, same day billing of physical and mental health appointments, reimbursement for screening, and lack of payment for non–face-to-face services. Although a concierge or fee-for-service option solves many of these, it excludes Medicaid patients and is an economic barrier for many families.
Mental health networks offer a different route, but they can involve poor reimbursement and an additional layer of administration, which makes financial integration more viable as long as providers investigate their options.
“It’s going to be a regional variation, and you need to look at state rules and regulations,” Dr. Rabinowitz said, explaining that his office then sought insurance contracts to include mental health care reimbursement through their office and then sought the same from Medicaid.
“We weren’t about to see Medicaid patients for fear of an audit unless we got written permission, but we got that,” he said. His office simply asked for it and received in writing a letter starting as follows: “Under Department policy, they (our psychologists) may submit E&M claims to Medicaid under a supervising physician’s billing ID. It is not mandatory they be credentialed into a BHO (Behavioral Healthcare Options) network…”
He also noted that his state allows inclusion of psychologists on medical malpractice insurance policies, which is far less expensive for mental health professionals, compared with medical doctors.
Ultimately, the result of mental health integration into primary care practices is greater satisfaction among patients and pediatricians as well as potentially better health outcomes, Dr. Rabinowitz said. An in-house patient satisfaction survey his office conducted found that 91% of parents felt it was convenient for their child to receive mental health services at the same location as medical care, and 90% were satisfied with their care. Only 9% cited barriers to their child seeing a psychologist at their office, and 89% found the services beneficial for their child. Similarly, providers find integration more convenient, easier for follow-up, less stressful, and more efficient while improving communication, confidence, and follow-up.
Dr. Rabinowitz reported no disclosures. No external funding was used for the presentation.
SAN FRANCISCO – Integrating pediatric mental health care into your primary care office can be an effective way to ensure your patients get the care they really need – and it’s easier than you think.
That’s the message Jay Rabinowitz, MD, MPH, a clinical professor of pediatrics at the University of Colorado at Denver, Aurora, delivered to a packed room at the annual meeting of the American Academy of Pediatrics.
He noted that depression and anxiety are among the top five conditions driving overall health costs in the United States, and a 1999 Surgeon General’s Report found that one in five children have a diagnosable mental disorder – but only a fifth to a quarter of these children receive treatment. The rub is that treatment is highly successful; it’s just difficult to access for many families, so making it a part of a child’s medical home just makes sense, Dr. Rabinowitz said.
To drive home his point, he described a case of a depressed adolescent with cutting and suicidal ideation, and the steps he would need to take without integration: find out their insurance, get a list of covered mental health professionals, refer to someone he may or may not heard of, and then rarely receive follow-up reports, much less confirmation the patient had gone to the appointment. With integrated care, parents can make appointments on their way out, he can read the psychologist’s report immediately after the visit, and he can drop in to say hello during the child’s mental health appointment.
“Sometimes there’s a question abut a medication or something, and sometimes it’s an inopportune moment if the child is sad or crying, but generally it seems to be pretty popular,” he said.
Taking steps toward integration
If providers are interesting in exploring the possibility of integration, they need to consider and decide on several issues before taking any concrete steps, Dr. Rabinowitz said. One is the type of arrangement that would work best for your practice: hiring on mental health professionals as employees of the practice, hiring independent contractors, coordinating a space share agreement or creating an out-of-office agreement.
“In our practice, psychologists are employees of the practice, but there are other arrangements,” he said, and some may depend on what is easiest based on state law or billing procedures.
The next question is what kind of provider(s) you would hire. His office has child psychologists with a PhD and postdoctorate fellowships working with children, but other possibilities include social workers, licensed counselors, psychiatric nurse practitioners, or psychiatrists.
Another consideration is what diagnoses your office will handle because it’s not possible to see everything. His practice sees patients in-house for attention deficit/hyperactivity disorder (ADHD), depression, anxiety, drug counseling, and behavioral and adjustment disorders. They choose to refer out educational testing, autism, difficult divorce cases, and complex cases that require more than 20 sessions. They refer out divorce cases because they frequently require specialized knowledge and a lot of court time and phone calls. Aside from ADHD evaluations, his office does not see the staff’s children.
Providers also should consider options for adapting their physical space to accommodate integration. His practice converted an exam room into a consultation room, making it homier with a throw rug, soft chairs, a painted wall, and office decor.
Establishing effective protocols with integration
The next step after providers decide to integrate is to determine the office protocols that govern what forms get used, who can schedule appointments and how long they last, billing, and similar procedures.
“You need to have certain protocols, and some of these things you don’t think about it until you start doing it,” Dr. Rabinowitz said. Should mental health appointments be 50 minutes, for example, or 20 to 25 minutes? His office has gradually shrunk these appointments from 50 to 30 minutes, but they give psychologists an hour of time each day for follow-up phone calls.
Forms to consider developing include a disclosure form, notice of privacy practices, late cancel/no show policy, financial policy, and a summary of parent concerns. His office’s charting includes an extensive intake form with medical, treatment, family, and social history, an intake summary, and a progress note.
It’s with reimbursement, of course, that providers will need to do the most research, particularly with regard to their state’s laws and in looking for grants to provide funding – which is more available than many realize.
“Money is often out there if you look for it,” Dr. Rabinowitz said.” Mental health is an area where no one is really against it: You get together the NRA (National Rifle Association) and the anti-gun movement, and they are both for it.”
Planning for reimbursement challenges
Reimbursement barriers can include lack of payment if mental health codes are used instead of pediatrics ones (depending on the practice arrangement), lack of “incident to” payments, same day billing of physical and mental health appointments, reimbursement for screening, and lack of payment for non–face-to-face services. Although a concierge or fee-for-service option solves many of these, it excludes Medicaid patients and is an economic barrier for many families.
Mental health networks offer a different route, but they can involve poor reimbursement and an additional layer of administration, which makes financial integration more viable as long as providers investigate their options.
“It’s going to be a regional variation, and you need to look at state rules and regulations,” Dr. Rabinowitz said, explaining that his office then sought insurance contracts to include mental health care reimbursement through their office and then sought the same from Medicaid.
“We weren’t about to see Medicaid patients for fear of an audit unless we got written permission, but we got that,” he said. His office simply asked for it and received in writing a letter starting as follows: “Under Department policy, they (our psychologists) may submit E&M claims to Medicaid under a supervising physician’s billing ID. It is not mandatory they be credentialed into a BHO (Behavioral Healthcare Options) network…”
He also noted that his state allows inclusion of psychologists on medical malpractice insurance policies, which is far less expensive for mental health professionals, compared with medical doctors.
Ultimately, the result of mental health integration into primary care practices is greater satisfaction among patients and pediatricians as well as potentially better health outcomes, Dr. Rabinowitz said. An in-house patient satisfaction survey his office conducted found that 91% of parents felt it was convenient for their child to receive mental health services at the same location as medical care, and 90% were satisfied with their care. Only 9% cited barriers to their child seeing a psychologist at their office, and 89% found the services beneficial for their child. Similarly, providers find integration more convenient, easier for follow-up, less stressful, and more efficient while improving communication, confidence, and follow-up.
Dr. Rabinowitz reported no disclosures. No external funding was used for the presentation.
EXPERT ANALYSIS FROM AAP 16
Yes, pediatric practices can provide immunizations without going broke
SAN FRANCISCO – With a little number crunching and strategizing, pediatric practices can provide immunizations to their patients without getting financially soaked, according to Chip Hart, a pediatric practice management consultant.
He discussed various pitfalls and challenges when it comes to the business aspects of providing immunizations, and offered some solutions at the annual meeting of the American Academy of Pediatrics.
His company has collected data suggesting that as of 2015, revenue from vaccine products made up fully 21% of all revenue in private pediatric practices, a near doubling from the value in 2003. As a consultant today, “I try to find out how practices manage the vaccines because, after staff, it’s your biggest expense,” he noted.
Spotting hidden costs
In its business case, the AAP determined that direct and indirect expenses for vaccine product total to 17% to 28% of the cost. In other words, “if you buy a vaccine for $100, you need to collect somewhere between $117 and $128, on average, just to break even,” Mr. Hart explained.
What accounts for that extra expense? Carrying costs that are commonly overlooked, namely, those myriad costs of providing immunizations that accrue before a child is given any vaccine and that can add up quickly.
They include the costs of the refrigerator and examination table; the sharps and waste management; insurance to cover vaccine loss; vaccine wastage and denials; and opportunity cost, that is, the cost of not being able to invest the funds tied up in vaccine sitting in the fridge – some $75,000 to $100,000 for the average practice – elsewhere.
Add to those personnel costs; costs related to activities such as ordering, inventory and storage management, registry input, and temperature monitoring; and malpractice coverage. And not to be forgotten is the inability to collect payment for some vaccines.
“You’re not paid for carrying costs. Unfortunately, society or the American health care system has given pediatricians this burden,” Mr. Hart commented.
Doing the math
Pediatricians can get a handle on the true costs to their practice of providing immunizations by spending just an hour or two crunching some key numbers, according to Mr. Hart.
They should start by ascertaining those carrying costs. For example, assuming hazardous waste costs run $3,500 per year, vaccines account for 50% of the waste, and the practice gives 13,000 vaccines annually, it averages out to $0.13 per vaccine.
Similar calculations are done to determine the costs of administering the shot (preparing, administering, counseling, billing, recording, putting it in the registry, and so on), arriving at about $12 per vaccine. The largest share here comes from clinicians, so calculations focus on their hourly wages and the percent of their time spent on vaccines.
Next is a calculation of the cost of the vaccine product. This calculation starts with the hypothetical invoiced amount of $100, factors in units that are wasted or go unpaid (at least 5%, according to AAP data), and tacks on the distributed carrying costs, arriving finally at an actual cost to the practice of about $120.
Last, all of these data are loaded into a payer-specific spreadsheet. Commonly, payers go by Red Book values and will therefore cover, for example, only $98 of that $100 invoice cost of the vaccine. But they will pay roughly $27 for its administration.
Taken together, the math suggests the practice bears a total cost of $132 for this vaccine ($120 for the product and $12 for its administration) but will collect only $125 from this payer ($98 for the product and $27 for its administration).
“You see over and over again that the payers underpay for the vaccines and pay you well for the administration, and it very often makes up the difference,” Mr. Hart noted. “But even with that boost on the admin side, this practice is losing money on this vaccine – they get $125 for something that costs them $132.”
Practices strapped for time can use some estimates in their spreadsheets instead, he said. “If you use an assumption of 25% over your invoice” – roughly the midpoint between the AAP’s 17% and 28% – “and $12 to $15 on your administration” – based on the value found in a study using time-motion analysis (Pediatrics. 2009 Dec;124 Suppl 5:S492-8) – “for your costs, all you need is your fee schedule, and you can make a spreadsheet to find out whether it makes sense to continue giving immunizations to this payer’s kids.”
Striving for profitability
“In all honesty, from what I see nationally, pediatricians break even on vaccines. It’s a break-even situation, on average,” Mr. Hart commented. “But who wants to be average? No one. We want you to actually be profitable with vaccines because it’s the only way you can continue to give them.”
Practices can take a variety of steps toward that goal. First, they should negotiate payments with payers, using the AAP’s business case and other literature. “Don’t listen to anybody” who says you can’t negotiate, he stressed. “You can negotiate. I don’t care if you’re a solo practice or you’ve just opened. If a payer says they can’t negotiate, they are fibbing to you. The only payers who don’t negotiate are the state Medicaid and Medicare. Everyone else can and does.”
Second, practices should ensure that they are using proper Current Procedural Terminology codes when submitting claims to payers to maximize payment.
“I still see too many practices who don’t bill for these properly,” Mr. Hart commented. “If you have a typical pediatric practice and you use more 90471s and 90472s than 90460s and 90461s, and frankly, if [the latter] aren’t two to three to four to five times more common… you are losing a lot of money.”
Third, practices should join or confirm that they belong to an effective group purchasing organization (GPO) to reduce their vaccine costs, with data suggesting that doing so will save the practice $10,000 to $15,000 per physician each year.
“If you are solo, out on the furthest edge of Alaska, you can see Russia from your house, and you have no leverage whatsoever, you can sign up with one of these GPOs and you are as strong as any hospital,” he said. The AAP helps here as well, by maintaining a list of GPOs on its website.
Fourth, practices should review their vaccine delivery work flow to look for money leaks, Mr. Hart advised. For example, physicians who get caught up in tasks such as ordering and inventorying are losing revenue that could come in from seeing patients.
“This is the sort of thing that affects your bottom line substantially. And it’s exactly the sort of thing that is an invisible expense: the business owners don’t consider their time as part of the expense of doing this administration,” he said.
Additionally, legacy procedures should be re-evaluated to see if they can be streamlined. Gains also may be made here from investing in better technology, such as a refrigerator with a glass door that saves time by allowing ready identification of vaccines.
Finally, practices should join the AAP’s Section on Administration and Practice Management (SOAPM) as it’s an invaluable, interactive resource in this area when questions or challenges arise, Mr. Hart recommended.
pdnews@frontlinemedcom.com
SAN FRANCISCO – With a little number crunching and strategizing, pediatric practices can provide immunizations to their patients without getting financially soaked, according to Chip Hart, a pediatric practice management consultant.
He discussed various pitfalls and challenges when it comes to the business aspects of providing immunizations, and offered some solutions at the annual meeting of the American Academy of Pediatrics.
His company has collected data suggesting that as of 2015, revenue from vaccine products made up fully 21% of all revenue in private pediatric practices, a near doubling from the value in 2003. As a consultant today, “I try to find out how practices manage the vaccines because, after staff, it’s your biggest expense,” he noted.
Spotting hidden costs
In its business case, the AAP determined that direct and indirect expenses for vaccine product total to 17% to 28% of the cost. In other words, “if you buy a vaccine for $100, you need to collect somewhere between $117 and $128, on average, just to break even,” Mr. Hart explained.
What accounts for that extra expense? Carrying costs that are commonly overlooked, namely, those myriad costs of providing immunizations that accrue before a child is given any vaccine and that can add up quickly.
They include the costs of the refrigerator and examination table; the sharps and waste management; insurance to cover vaccine loss; vaccine wastage and denials; and opportunity cost, that is, the cost of not being able to invest the funds tied up in vaccine sitting in the fridge – some $75,000 to $100,000 for the average practice – elsewhere.
Add to those personnel costs; costs related to activities such as ordering, inventory and storage management, registry input, and temperature monitoring; and malpractice coverage. And not to be forgotten is the inability to collect payment for some vaccines.
“You’re not paid for carrying costs. Unfortunately, society or the American health care system has given pediatricians this burden,” Mr. Hart commented.
Doing the math
Pediatricians can get a handle on the true costs to their practice of providing immunizations by spending just an hour or two crunching some key numbers, according to Mr. Hart.
They should start by ascertaining those carrying costs. For example, assuming hazardous waste costs run $3,500 per year, vaccines account for 50% of the waste, and the practice gives 13,000 vaccines annually, it averages out to $0.13 per vaccine.
Similar calculations are done to determine the costs of administering the shot (preparing, administering, counseling, billing, recording, putting it in the registry, and so on), arriving at about $12 per vaccine. The largest share here comes from clinicians, so calculations focus on their hourly wages and the percent of their time spent on vaccines.
Next is a calculation of the cost of the vaccine product. This calculation starts with the hypothetical invoiced amount of $100, factors in units that are wasted or go unpaid (at least 5%, according to AAP data), and tacks on the distributed carrying costs, arriving finally at an actual cost to the practice of about $120.
Last, all of these data are loaded into a payer-specific spreadsheet. Commonly, payers go by Red Book values and will therefore cover, for example, only $98 of that $100 invoice cost of the vaccine. But they will pay roughly $27 for its administration.
Taken together, the math suggests the practice bears a total cost of $132 for this vaccine ($120 for the product and $12 for its administration) but will collect only $125 from this payer ($98 for the product and $27 for its administration).
“You see over and over again that the payers underpay for the vaccines and pay you well for the administration, and it very often makes up the difference,” Mr. Hart noted. “But even with that boost on the admin side, this practice is losing money on this vaccine – they get $125 for something that costs them $132.”
Practices strapped for time can use some estimates in their spreadsheets instead, he said. “If you use an assumption of 25% over your invoice” – roughly the midpoint between the AAP’s 17% and 28% – “and $12 to $15 on your administration” – based on the value found in a study using time-motion analysis (Pediatrics. 2009 Dec;124 Suppl 5:S492-8) – “for your costs, all you need is your fee schedule, and you can make a spreadsheet to find out whether it makes sense to continue giving immunizations to this payer’s kids.”
Striving for profitability
“In all honesty, from what I see nationally, pediatricians break even on vaccines. It’s a break-even situation, on average,” Mr. Hart commented. “But who wants to be average? No one. We want you to actually be profitable with vaccines because it’s the only way you can continue to give them.”
Practices can take a variety of steps toward that goal. First, they should negotiate payments with payers, using the AAP’s business case and other literature. “Don’t listen to anybody” who says you can’t negotiate, he stressed. “You can negotiate. I don’t care if you’re a solo practice or you’ve just opened. If a payer says they can’t negotiate, they are fibbing to you. The only payers who don’t negotiate are the state Medicaid and Medicare. Everyone else can and does.”
Second, practices should ensure that they are using proper Current Procedural Terminology codes when submitting claims to payers to maximize payment.
“I still see too many practices who don’t bill for these properly,” Mr. Hart commented. “If you have a typical pediatric practice and you use more 90471s and 90472s than 90460s and 90461s, and frankly, if [the latter] aren’t two to three to four to five times more common… you are losing a lot of money.”
Third, practices should join or confirm that they belong to an effective group purchasing organization (GPO) to reduce their vaccine costs, with data suggesting that doing so will save the practice $10,000 to $15,000 per physician each year.
“If you are solo, out on the furthest edge of Alaska, you can see Russia from your house, and you have no leverage whatsoever, you can sign up with one of these GPOs and you are as strong as any hospital,” he said. The AAP helps here as well, by maintaining a list of GPOs on its website.
Fourth, practices should review their vaccine delivery work flow to look for money leaks, Mr. Hart advised. For example, physicians who get caught up in tasks such as ordering and inventorying are losing revenue that could come in from seeing patients.
“This is the sort of thing that affects your bottom line substantially. And it’s exactly the sort of thing that is an invisible expense: the business owners don’t consider their time as part of the expense of doing this administration,” he said.
Additionally, legacy procedures should be re-evaluated to see if they can be streamlined. Gains also may be made here from investing in better technology, such as a refrigerator with a glass door that saves time by allowing ready identification of vaccines.
Finally, practices should join the AAP’s Section on Administration and Practice Management (SOAPM) as it’s an invaluable, interactive resource in this area when questions or challenges arise, Mr. Hart recommended.
pdnews@frontlinemedcom.com
SAN FRANCISCO – With a little number crunching and strategizing, pediatric practices can provide immunizations to their patients without getting financially soaked, according to Chip Hart, a pediatric practice management consultant.
He discussed various pitfalls and challenges when it comes to the business aspects of providing immunizations, and offered some solutions at the annual meeting of the American Academy of Pediatrics.
His company has collected data suggesting that as of 2015, revenue from vaccine products made up fully 21% of all revenue in private pediatric practices, a near doubling from the value in 2003. As a consultant today, “I try to find out how practices manage the vaccines because, after staff, it’s your biggest expense,” he noted.
Spotting hidden costs
In its business case, the AAP determined that direct and indirect expenses for vaccine product total to 17% to 28% of the cost. In other words, “if you buy a vaccine for $100, you need to collect somewhere between $117 and $128, on average, just to break even,” Mr. Hart explained.
What accounts for that extra expense? Carrying costs that are commonly overlooked, namely, those myriad costs of providing immunizations that accrue before a child is given any vaccine and that can add up quickly.
They include the costs of the refrigerator and examination table; the sharps and waste management; insurance to cover vaccine loss; vaccine wastage and denials; and opportunity cost, that is, the cost of not being able to invest the funds tied up in vaccine sitting in the fridge – some $75,000 to $100,000 for the average practice – elsewhere.
Add to those personnel costs; costs related to activities such as ordering, inventory and storage management, registry input, and temperature monitoring; and malpractice coverage. And not to be forgotten is the inability to collect payment for some vaccines.
“You’re not paid for carrying costs. Unfortunately, society or the American health care system has given pediatricians this burden,” Mr. Hart commented.
Doing the math
Pediatricians can get a handle on the true costs to their practice of providing immunizations by spending just an hour or two crunching some key numbers, according to Mr. Hart.
They should start by ascertaining those carrying costs. For example, assuming hazardous waste costs run $3,500 per year, vaccines account for 50% of the waste, and the practice gives 13,000 vaccines annually, it averages out to $0.13 per vaccine.
Similar calculations are done to determine the costs of administering the shot (preparing, administering, counseling, billing, recording, putting it in the registry, and so on), arriving at about $12 per vaccine. The largest share here comes from clinicians, so calculations focus on their hourly wages and the percent of their time spent on vaccines.
Next is a calculation of the cost of the vaccine product. This calculation starts with the hypothetical invoiced amount of $100, factors in units that are wasted or go unpaid (at least 5%, according to AAP data), and tacks on the distributed carrying costs, arriving finally at an actual cost to the practice of about $120.
Last, all of these data are loaded into a payer-specific spreadsheet. Commonly, payers go by Red Book values and will therefore cover, for example, only $98 of that $100 invoice cost of the vaccine. But they will pay roughly $27 for its administration.
Taken together, the math suggests the practice bears a total cost of $132 for this vaccine ($120 for the product and $12 for its administration) but will collect only $125 from this payer ($98 for the product and $27 for its administration).
“You see over and over again that the payers underpay for the vaccines and pay you well for the administration, and it very often makes up the difference,” Mr. Hart noted. “But even with that boost on the admin side, this practice is losing money on this vaccine – they get $125 for something that costs them $132.”
Practices strapped for time can use some estimates in their spreadsheets instead, he said. “If you use an assumption of 25% over your invoice” – roughly the midpoint between the AAP’s 17% and 28% – “and $12 to $15 on your administration” – based on the value found in a study using time-motion analysis (Pediatrics. 2009 Dec;124 Suppl 5:S492-8) – “for your costs, all you need is your fee schedule, and you can make a spreadsheet to find out whether it makes sense to continue giving immunizations to this payer’s kids.”
Striving for profitability
“In all honesty, from what I see nationally, pediatricians break even on vaccines. It’s a break-even situation, on average,” Mr. Hart commented. “But who wants to be average? No one. We want you to actually be profitable with vaccines because it’s the only way you can continue to give them.”
Practices can take a variety of steps toward that goal. First, they should negotiate payments with payers, using the AAP’s business case and other literature. “Don’t listen to anybody” who says you can’t negotiate, he stressed. “You can negotiate. I don’t care if you’re a solo practice or you’ve just opened. If a payer says they can’t negotiate, they are fibbing to you. The only payers who don’t negotiate are the state Medicaid and Medicare. Everyone else can and does.”
Second, practices should ensure that they are using proper Current Procedural Terminology codes when submitting claims to payers to maximize payment.
“I still see too many practices who don’t bill for these properly,” Mr. Hart commented. “If you have a typical pediatric practice and you use more 90471s and 90472s than 90460s and 90461s, and frankly, if [the latter] aren’t two to three to four to five times more common… you are losing a lot of money.”
Third, practices should join or confirm that they belong to an effective group purchasing organization (GPO) to reduce their vaccine costs, with data suggesting that doing so will save the practice $10,000 to $15,000 per physician each year.
“If you are solo, out on the furthest edge of Alaska, you can see Russia from your house, and you have no leverage whatsoever, you can sign up with one of these GPOs and you are as strong as any hospital,” he said. The AAP helps here as well, by maintaining a list of GPOs on its website.
Fourth, practices should review their vaccine delivery work flow to look for money leaks, Mr. Hart advised. For example, physicians who get caught up in tasks such as ordering and inventorying are losing revenue that could come in from seeing patients.
“This is the sort of thing that affects your bottom line substantially. And it’s exactly the sort of thing that is an invisible expense: the business owners don’t consider their time as part of the expense of doing this administration,” he said.
Additionally, legacy procedures should be re-evaluated to see if they can be streamlined. Gains also may be made here from investing in better technology, such as a refrigerator with a glass door that saves time by allowing ready identification of vaccines.
Finally, practices should join the AAP’s Section on Administration and Practice Management (SOAPM) as it’s an invaluable, interactive resource in this area when questions or challenges arise, Mr. Hart recommended.
pdnews@frontlinemedcom.com
AT AAP 16
Body-size awareness linked with BMI decrease in obese children, teens
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
SAN FRANCISCO – Body-size awareness was associated with a decrease in BMI among Latino children and teens, said Grace Lim, MD, a pediatrician in King City, Calif.
Awareness of body size, as a proxy for motivation to change behavior, was based on choices of sex-specific body silhouettes in comparison to actual body mass index (BMI) z-scores. Dr. Lim and her coauthor, Dr. Nazrat Mirza, conducted a study at Children’s National Medical Center in Washington of 80 overweight or obese Latino youths aged 7-15 years who were taking part in a 12-week, community-based weight management program: 68% of study participants demonstrated awareness of overweight or obese body sizes. They were more likely to be older (P less than .001) and with higher maternal age (P = .02). Body-size awareness in the child was positively associated with a decrease in BMI during the intervention period (P less than .001).
Dr. Lim said that she had no relevant financial disclosures.
AT AAP 16
Key clinical point:
Major finding: 68% of 80 the children demonstrated awareness of overweight or obese body sizes and were more likely to drop their BMI.
Data source: A study of 80 overweight or obese Latino youths aged 7-15 years taking part in a 12-week, community-based weight management program.
Disclosures: Dr. Lim said she that had no relevant financial disclosures.
New screen time guidelines address rapid changes in media environment
SAN FRANCISCO – A new set of policy statements on children’s media use from the American Academy of Pediatrics brings the recommendations into the 21st century.
The new guidance, released at the annual meeting of the AAP, synthesizes the most current evidence on mobile devices, interactivity, educational technology, sleep, obesity, cognitive development, and other aspects of the pervasive digital environment children now grow up in.
“I think our policy statement reflects the changes in the media landscape because not all media use is the same,” Megan A. Moreno, MD, lead author of the policy statement, “Media Use in School-Aged Children and Adolescents,” said during a press conference (Pediatrics. 2016, Oct. doi: 10.1542/peds.2016-2592).
The new statement both lowers the overall age at which parents can feel comfortable introducing their children to media and decreases the amount of screen time exposure per day. One key component of the new guidelines includes the unveiling of a new tool parents can use to create a Family Media Plan. The tool, available at https://www.healthychildren.org/English/media/Pages/default.aspx, enables parents to create a plan for each child in the household and reflects the individuality of each child’s use and age-appropriate guidelines.
After parents enter children’s names, the plan provides an editable template for each child that lays out screen-free zones, screen-free times, device curfews, recreational screen-time choices, alternative activities during non-screen time, media manners, digital citizenship, personal safety, sleep, and exercise.
Previous policy statements from the AAP relied primarily on research about television, a passive screen experience. In an age where many children and teens have interactive screens in their pockets and visit grandparents via video conferencing, however, the AAP Council on Communications and Media has likewise broadened its definition of media and noted the problems with applying research about television to other totally different types of screens.
“When we’re using media to connect, this is not what we’re traditionally calling screen time. These are tools,” Jenny S. Radesky, MD, lead author of the policy statement “Media and Young Minds,” said at the press conference (Pediatrics. 2016 Oct. doi: 10.1542/peds.2016-2592). She referred to the fact that many families who are spread across great distances, such as parents deployed overseas or grandparents in another state, use Skype, FaceTime, Google Hangouts, and similar programs to communicate and remain connected.
“We’re making sure our relationships are staying strong and not something to be discouraged with infants and toddlers, even though infants and toddlers will need their parent’s help to understand what they’re seeing on the screen,” said Dr. Radesky, a developmental-behavioral pediatrician at C.S. Mott Children’s Hospital at the University of Michigan in Ann Arbor.
The policy statement further notes that some emerging evidence has suggested children aged 2 and older can learn words from live video chatting with a responsive adult or by using an interactive touch screen that scaffolds learning.
An earlier introduction to screens
Among the most significant changes to the recommendations for children up to 5 years old is an allowance for introducing media before age 2, the previous policy’s age recommendation.
“If you want to introduce media, 18 months is the age when kids are cognitively ready to start, but we’re not saying parents need to introduce media then,” Dr. Radesky said, adding that more research is needed regarding devices such as tablets before it’s possible to know whether apps can be beneficial in toddlers that young. “There’s not enough evidence to know if interactivity helps or not right now,” she said.
The “Media and Young Minds” policy statement notes that children under age 2 years develop their cognitive, language, motor, and social-emotional skills through hands-on exploration and social interaction with trusted adults.
“Apps can’t do the things that parents’ minds can do or children’s minds can do on their own,” Dr. Radesky said. The policy notes that digital books, or eBooks, can be beneficial when used like a traditional physical book, but interactive elements to these eBooks could be distracting and decrease children’s comprehension.
When parents do choose to introduce media to their children, it’s “crucial that media be a shared experience” between the caregiving adult and the child, she said. “Think of media as a teaching tool, a way to connect and to create, not just to consume,” Dr. Radesky said.
What can preschoolers learn?
Although some laboratory research shows toddlers as young as 15 months can learn new words from touch screens, they have difficulty transferring that knowledge to the three-dimensional world. For children aged 3-5 years, however, both well-designed television programming and high-quality learning apps from Public Broadcasting Service (PBS) and the Sesame Workshop have shown benefits. In addition to early literacy, math, and personal and social development skills learned from shows such as Sesame Street, preschoolers have learned literacy skills from those programs’ apps.
But those apps are unfortunately in the minority.
“Most apps parents find under the ‘educational’ category in app stores have no such evidence of efficacy, target only rote academic skills, are not based on established curricula, and use little or no input from developmental specialists and educators,” the “Media and Young Minds” policy states. “The higher-order thinking skills and executive functions essential for school success, such as task persistence, impulse control, emotion regulation, and creative, flexible thinking, are best taught through unstructured and social (not digital) play, as well as responsive parent-child interactions.”
Risks and recommendations for preschoolers
Heavy media use among preschoolers, meanwhile, carries risks of increased weight – primarily as a result of food advertising and eating while watching TV – as well as reduced sleep and cognitive, language, and social/emotional delays.
“Content is crucial,” the “Media and Young Minds” policy notes. “Experimental evidence shows that switching from violent content to educational/prosocial content results in significant improvement in behavioral symptoms, particularly for low-income boys.”
The key points of the new statement therefore include the following recommendations:
• Limit media use to 1 hour a day in children ages 2 years and older.
• Do not use screens during mealtimes and for 1 hour before bedtime.
• Start discussing family and child media use with parents early in children’s lives.
• Educate parents about early brain development and help families develop a Family Media Use Plan.
• Discourage screen use besides video-chatting in children under 18 months old.
• Encourage caregiving adults to use screen media with children aged 18-24 months, who should not use it on their own.
• Encourage parents to rely on high-quality programming products such as PBS Kids, Sesame Workshop, and Common Sense Media.
• Help parents with challenges such as setting limits, finding alternatives to screen time, and calming children without using media.
• Avoid using screens or media to calm children except during rare extenuating circumstances, such as painful medical procedures and airplane flights.
• Encourage parents to avoid fast-paced programs, apps with distracting content, any media with violent content, and any background television, which can stunt children’s early language development.
Understanding older youth’s media use
As children move into school age and adolescence, the opportunities and utilities for media use expand – and so do the risks. Children and teens can benefit from media through gaining social support, learning about healthy behaviors, and discovering new ideas and knowledge, but youth remain at risk for obesity, sleep problems, cyberbullying, compromised privacy, and exposure to inaccurate, inappropriate or unsafe content, the “Media Use in School-Aged Children and Adolescents” policy statement reports.
Despite the wide range of media types available, TV remains the most commonly used media type among school-aged children and teens and is watched an average of 2 hours a day. Still, 91% of boys have access to a video game console, and 84% report playing games online or on a mobile phone. Further, three-quarters of teens own a smartphone and 76% use at least one social media site, with more than 70% maintaining a “social media portfolio” across several platforms.
Such social media use can provide teens with helpful support networks, particularly for those with ongoing illnesses or disabilities or those needing community support as lesbian, gay, bisexual, transgender, questioning, or intersex individuals. Social media can also promote wellness and healthy behaviors such as eating well and not smoking.
Risks for school-aged children and adolescents using media
Yet social media also can open the door to cyberbullying, leading to short-term and long-term social, academic, and health problems. It carries the risk of exploitation of youth or their images, or predation from pornographers and pedophiles. Children and teens must be made aware that the “Internet is forever” and should be taught to consider privacy and confidentiality concerns in their use of social and other media.
Another concern is teens’ “sexting,” in which they share sexually explicit messages and/or partly or fully nude photos. Exposures to unhealthy behaviors, such as substance abuse, sexual behaviors, self-injury, or disordered eating are likewise among the risks of social media, as they are with television and cinema.
In fact, TV/movie content showing alcohol use, smoking, and sexual activity is linked to earlier experimentation among children and adolescents. In addition, each extra hour of television watching is associated with increase in body mass index, as is having a TV set in the bedroom. Enjoying entertainment media while doing school work is linked to poor learning and academics.
Excessive media use may lead to problematic Internet use and Internet gaming disorder as described in the DSM-5, occurring among 4%-8.5% of children and adolescents.
“Symptoms can include a preoccupation with the activity, decreased interest in offline or ‘real life’ relationships, unsuccessful attempts to decrease use and withdrawal symptoms,” the “Media Use in School-Aged Children and Adolescents” policy statement notes.
Recommendations for older children
The policy statement advises pediatricians to help families and schools promote understanding of media’s risks and benefits, including awareness of tools to screen for sexting, cyberbullying, problematic Internet use, and Internet gaming disorder. Pediatricians should advocate for training in media literacy in the community and encourage parents to follow the media, sleep, and physical activity guidelines included in the Family Media Plan.
The research was supported by the American Academy of Pediatrics. The authors reported no disclosures.
SAN FRANCISCO – A new set of policy statements on children’s media use from the American Academy of Pediatrics brings the recommendations into the 21st century.
The new guidance, released at the annual meeting of the AAP, synthesizes the most current evidence on mobile devices, interactivity, educational technology, sleep, obesity, cognitive development, and other aspects of the pervasive digital environment children now grow up in.
“I think our policy statement reflects the changes in the media landscape because not all media use is the same,” Megan A. Moreno, MD, lead author of the policy statement, “Media Use in School-Aged Children and Adolescents,” said during a press conference (Pediatrics. 2016, Oct. doi: 10.1542/peds.2016-2592).
The new statement both lowers the overall age at which parents can feel comfortable introducing their children to media and decreases the amount of screen time exposure per day. One key component of the new guidelines includes the unveiling of a new tool parents can use to create a Family Media Plan. The tool, available at https://www.healthychildren.org/English/media/Pages/default.aspx, enables parents to create a plan for each child in the household and reflects the individuality of each child’s use and age-appropriate guidelines.
After parents enter children’s names, the plan provides an editable template for each child that lays out screen-free zones, screen-free times, device curfews, recreational screen-time choices, alternative activities during non-screen time, media manners, digital citizenship, personal safety, sleep, and exercise.
Previous policy statements from the AAP relied primarily on research about television, a passive screen experience. In an age where many children and teens have interactive screens in their pockets and visit grandparents via video conferencing, however, the AAP Council on Communications and Media has likewise broadened its definition of media and noted the problems with applying research about television to other totally different types of screens.
“When we’re using media to connect, this is not what we’re traditionally calling screen time. These are tools,” Jenny S. Radesky, MD, lead author of the policy statement “Media and Young Minds,” said at the press conference (Pediatrics. 2016 Oct. doi: 10.1542/peds.2016-2592). She referred to the fact that many families who are spread across great distances, such as parents deployed overseas or grandparents in another state, use Skype, FaceTime, Google Hangouts, and similar programs to communicate and remain connected.
“We’re making sure our relationships are staying strong and not something to be discouraged with infants and toddlers, even though infants and toddlers will need their parent’s help to understand what they’re seeing on the screen,” said Dr. Radesky, a developmental-behavioral pediatrician at C.S. Mott Children’s Hospital at the University of Michigan in Ann Arbor.
The policy statement further notes that some emerging evidence has suggested children aged 2 and older can learn words from live video chatting with a responsive adult or by using an interactive touch screen that scaffolds learning.
An earlier introduction to screens
Among the most significant changes to the recommendations for children up to 5 years old is an allowance for introducing media before age 2, the previous policy’s age recommendation.
“If you want to introduce media, 18 months is the age when kids are cognitively ready to start, but we’re not saying parents need to introduce media then,” Dr. Radesky said, adding that more research is needed regarding devices such as tablets before it’s possible to know whether apps can be beneficial in toddlers that young. “There’s not enough evidence to know if interactivity helps or not right now,” she said.
The “Media and Young Minds” policy statement notes that children under age 2 years develop their cognitive, language, motor, and social-emotional skills through hands-on exploration and social interaction with trusted adults.
“Apps can’t do the things that parents’ minds can do or children’s minds can do on their own,” Dr. Radesky said. The policy notes that digital books, or eBooks, can be beneficial when used like a traditional physical book, but interactive elements to these eBooks could be distracting and decrease children’s comprehension.
When parents do choose to introduce media to their children, it’s “crucial that media be a shared experience” between the caregiving adult and the child, she said. “Think of media as a teaching tool, a way to connect and to create, not just to consume,” Dr. Radesky said.
What can preschoolers learn?
Although some laboratory research shows toddlers as young as 15 months can learn new words from touch screens, they have difficulty transferring that knowledge to the three-dimensional world. For children aged 3-5 years, however, both well-designed television programming and high-quality learning apps from Public Broadcasting Service (PBS) and the Sesame Workshop have shown benefits. In addition to early literacy, math, and personal and social development skills learned from shows such as Sesame Street, preschoolers have learned literacy skills from those programs’ apps.
But those apps are unfortunately in the minority.
“Most apps parents find under the ‘educational’ category in app stores have no such evidence of efficacy, target only rote academic skills, are not based on established curricula, and use little or no input from developmental specialists and educators,” the “Media and Young Minds” policy states. “The higher-order thinking skills and executive functions essential for school success, such as task persistence, impulse control, emotion regulation, and creative, flexible thinking, are best taught through unstructured and social (not digital) play, as well as responsive parent-child interactions.”
Risks and recommendations for preschoolers
Heavy media use among preschoolers, meanwhile, carries risks of increased weight – primarily as a result of food advertising and eating while watching TV – as well as reduced sleep and cognitive, language, and social/emotional delays.
“Content is crucial,” the “Media and Young Minds” policy notes. “Experimental evidence shows that switching from violent content to educational/prosocial content results in significant improvement in behavioral symptoms, particularly for low-income boys.”
The key points of the new statement therefore include the following recommendations:
• Limit media use to 1 hour a day in children ages 2 years and older.
• Do not use screens during mealtimes and for 1 hour before bedtime.
• Start discussing family and child media use with parents early in children’s lives.
• Educate parents about early brain development and help families develop a Family Media Use Plan.
• Discourage screen use besides video-chatting in children under 18 months old.
• Encourage caregiving adults to use screen media with children aged 18-24 months, who should not use it on their own.
• Encourage parents to rely on high-quality programming products such as PBS Kids, Sesame Workshop, and Common Sense Media.
• Help parents with challenges such as setting limits, finding alternatives to screen time, and calming children without using media.
• Avoid using screens or media to calm children except during rare extenuating circumstances, such as painful medical procedures and airplane flights.
• Encourage parents to avoid fast-paced programs, apps with distracting content, any media with violent content, and any background television, which can stunt children’s early language development.
Understanding older youth’s media use
As children move into school age and adolescence, the opportunities and utilities for media use expand – and so do the risks. Children and teens can benefit from media through gaining social support, learning about healthy behaviors, and discovering new ideas and knowledge, but youth remain at risk for obesity, sleep problems, cyberbullying, compromised privacy, and exposure to inaccurate, inappropriate or unsafe content, the “Media Use in School-Aged Children and Adolescents” policy statement reports.
Despite the wide range of media types available, TV remains the most commonly used media type among school-aged children and teens and is watched an average of 2 hours a day. Still, 91% of boys have access to a video game console, and 84% report playing games online or on a mobile phone. Further, three-quarters of teens own a smartphone and 76% use at least one social media site, with more than 70% maintaining a “social media portfolio” across several platforms.
Such social media use can provide teens with helpful support networks, particularly for those with ongoing illnesses or disabilities or those needing community support as lesbian, gay, bisexual, transgender, questioning, or intersex individuals. Social media can also promote wellness and healthy behaviors such as eating well and not smoking.
Risks for school-aged children and adolescents using media
Yet social media also can open the door to cyberbullying, leading to short-term and long-term social, academic, and health problems. It carries the risk of exploitation of youth or their images, or predation from pornographers and pedophiles. Children and teens must be made aware that the “Internet is forever” and should be taught to consider privacy and confidentiality concerns in their use of social and other media.
Another concern is teens’ “sexting,” in which they share sexually explicit messages and/or partly or fully nude photos. Exposures to unhealthy behaviors, such as substance abuse, sexual behaviors, self-injury, or disordered eating are likewise among the risks of social media, as they are with television and cinema.
In fact, TV/movie content showing alcohol use, smoking, and sexual activity is linked to earlier experimentation among children and adolescents. In addition, each extra hour of television watching is associated with increase in body mass index, as is having a TV set in the bedroom. Enjoying entertainment media while doing school work is linked to poor learning and academics.
Excessive media use may lead to problematic Internet use and Internet gaming disorder as described in the DSM-5, occurring among 4%-8.5% of children and adolescents.
“Symptoms can include a preoccupation with the activity, decreased interest in offline or ‘real life’ relationships, unsuccessful attempts to decrease use and withdrawal symptoms,” the “Media Use in School-Aged Children and Adolescents” policy statement notes.
Recommendations for older children
The policy statement advises pediatricians to help families and schools promote understanding of media’s risks and benefits, including awareness of tools to screen for sexting, cyberbullying, problematic Internet use, and Internet gaming disorder. Pediatricians should advocate for training in media literacy in the community and encourage parents to follow the media, sleep, and physical activity guidelines included in the Family Media Plan.
The research was supported by the American Academy of Pediatrics. The authors reported no disclosures.
SAN FRANCISCO – A new set of policy statements on children’s media use from the American Academy of Pediatrics brings the recommendations into the 21st century.
The new guidance, released at the annual meeting of the AAP, synthesizes the most current evidence on mobile devices, interactivity, educational technology, sleep, obesity, cognitive development, and other aspects of the pervasive digital environment children now grow up in.
“I think our policy statement reflects the changes in the media landscape because not all media use is the same,” Megan A. Moreno, MD, lead author of the policy statement, “Media Use in School-Aged Children and Adolescents,” said during a press conference (Pediatrics. 2016, Oct. doi: 10.1542/peds.2016-2592).
The new statement both lowers the overall age at which parents can feel comfortable introducing their children to media and decreases the amount of screen time exposure per day. One key component of the new guidelines includes the unveiling of a new tool parents can use to create a Family Media Plan. The tool, available at https://www.healthychildren.org/English/media/Pages/default.aspx, enables parents to create a plan for each child in the household and reflects the individuality of each child’s use and age-appropriate guidelines.
After parents enter children’s names, the plan provides an editable template for each child that lays out screen-free zones, screen-free times, device curfews, recreational screen-time choices, alternative activities during non-screen time, media manners, digital citizenship, personal safety, sleep, and exercise.
Previous policy statements from the AAP relied primarily on research about television, a passive screen experience. In an age where many children and teens have interactive screens in their pockets and visit grandparents via video conferencing, however, the AAP Council on Communications and Media has likewise broadened its definition of media and noted the problems with applying research about television to other totally different types of screens.
“When we’re using media to connect, this is not what we’re traditionally calling screen time. These are tools,” Jenny S. Radesky, MD, lead author of the policy statement “Media and Young Minds,” said at the press conference (Pediatrics. 2016 Oct. doi: 10.1542/peds.2016-2592). She referred to the fact that many families who are spread across great distances, such as parents deployed overseas or grandparents in another state, use Skype, FaceTime, Google Hangouts, and similar programs to communicate and remain connected.
“We’re making sure our relationships are staying strong and not something to be discouraged with infants and toddlers, even though infants and toddlers will need their parent’s help to understand what they’re seeing on the screen,” said Dr. Radesky, a developmental-behavioral pediatrician at C.S. Mott Children’s Hospital at the University of Michigan in Ann Arbor.
The policy statement further notes that some emerging evidence has suggested children aged 2 and older can learn words from live video chatting with a responsive adult or by using an interactive touch screen that scaffolds learning.
An earlier introduction to screens
Among the most significant changes to the recommendations for children up to 5 years old is an allowance for introducing media before age 2, the previous policy’s age recommendation.
“If you want to introduce media, 18 months is the age when kids are cognitively ready to start, but we’re not saying parents need to introduce media then,” Dr. Radesky said, adding that more research is needed regarding devices such as tablets before it’s possible to know whether apps can be beneficial in toddlers that young. “There’s not enough evidence to know if interactivity helps or not right now,” she said.
The “Media and Young Minds” policy statement notes that children under age 2 years develop their cognitive, language, motor, and social-emotional skills through hands-on exploration and social interaction with trusted adults.
“Apps can’t do the things that parents’ minds can do or children’s minds can do on their own,” Dr. Radesky said. The policy notes that digital books, or eBooks, can be beneficial when used like a traditional physical book, but interactive elements to these eBooks could be distracting and decrease children’s comprehension.
When parents do choose to introduce media to their children, it’s “crucial that media be a shared experience” between the caregiving adult and the child, she said. “Think of media as a teaching tool, a way to connect and to create, not just to consume,” Dr. Radesky said.
What can preschoolers learn?
Although some laboratory research shows toddlers as young as 15 months can learn new words from touch screens, they have difficulty transferring that knowledge to the three-dimensional world. For children aged 3-5 years, however, both well-designed television programming and high-quality learning apps from Public Broadcasting Service (PBS) and the Sesame Workshop have shown benefits. In addition to early literacy, math, and personal and social development skills learned from shows such as Sesame Street, preschoolers have learned literacy skills from those programs’ apps.
But those apps are unfortunately in the minority.
“Most apps parents find under the ‘educational’ category in app stores have no such evidence of efficacy, target only rote academic skills, are not based on established curricula, and use little or no input from developmental specialists and educators,” the “Media and Young Minds” policy states. “The higher-order thinking skills and executive functions essential for school success, such as task persistence, impulse control, emotion regulation, and creative, flexible thinking, are best taught through unstructured and social (not digital) play, as well as responsive parent-child interactions.”
Risks and recommendations for preschoolers
Heavy media use among preschoolers, meanwhile, carries risks of increased weight – primarily as a result of food advertising and eating while watching TV – as well as reduced sleep and cognitive, language, and social/emotional delays.
“Content is crucial,” the “Media and Young Minds” policy notes. “Experimental evidence shows that switching from violent content to educational/prosocial content results in significant improvement in behavioral symptoms, particularly for low-income boys.”
The key points of the new statement therefore include the following recommendations:
• Limit media use to 1 hour a day in children ages 2 years and older.
• Do not use screens during mealtimes and for 1 hour before bedtime.
• Start discussing family and child media use with parents early in children’s lives.
• Educate parents about early brain development and help families develop a Family Media Use Plan.
• Discourage screen use besides video-chatting in children under 18 months old.
• Encourage caregiving adults to use screen media with children aged 18-24 months, who should not use it on their own.
• Encourage parents to rely on high-quality programming products such as PBS Kids, Sesame Workshop, and Common Sense Media.
• Help parents with challenges such as setting limits, finding alternatives to screen time, and calming children without using media.
• Avoid using screens or media to calm children except during rare extenuating circumstances, such as painful medical procedures and airplane flights.
• Encourage parents to avoid fast-paced programs, apps with distracting content, any media with violent content, and any background television, which can stunt children’s early language development.
Understanding older youth’s media use
As children move into school age and adolescence, the opportunities and utilities for media use expand – and so do the risks. Children and teens can benefit from media through gaining social support, learning about healthy behaviors, and discovering new ideas and knowledge, but youth remain at risk for obesity, sleep problems, cyberbullying, compromised privacy, and exposure to inaccurate, inappropriate or unsafe content, the “Media Use in School-Aged Children and Adolescents” policy statement reports.
Despite the wide range of media types available, TV remains the most commonly used media type among school-aged children and teens and is watched an average of 2 hours a day. Still, 91% of boys have access to a video game console, and 84% report playing games online or on a mobile phone. Further, three-quarters of teens own a smartphone and 76% use at least one social media site, with more than 70% maintaining a “social media portfolio” across several platforms.
Such social media use can provide teens with helpful support networks, particularly for those with ongoing illnesses or disabilities or those needing community support as lesbian, gay, bisexual, transgender, questioning, or intersex individuals. Social media can also promote wellness and healthy behaviors such as eating well and not smoking.
Risks for school-aged children and adolescents using media
Yet social media also can open the door to cyberbullying, leading to short-term and long-term social, academic, and health problems. It carries the risk of exploitation of youth or their images, or predation from pornographers and pedophiles. Children and teens must be made aware that the “Internet is forever” and should be taught to consider privacy and confidentiality concerns in their use of social and other media.
Another concern is teens’ “sexting,” in which they share sexually explicit messages and/or partly or fully nude photos. Exposures to unhealthy behaviors, such as substance abuse, sexual behaviors, self-injury, or disordered eating are likewise among the risks of social media, as they are with television and cinema.
In fact, TV/movie content showing alcohol use, smoking, and sexual activity is linked to earlier experimentation among children and adolescents. In addition, each extra hour of television watching is associated with increase in body mass index, as is having a TV set in the bedroom. Enjoying entertainment media while doing school work is linked to poor learning and academics.
Excessive media use may lead to problematic Internet use and Internet gaming disorder as described in the DSM-5, occurring among 4%-8.5% of children and adolescents.
“Symptoms can include a preoccupation with the activity, decreased interest in offline or ‘real life’ relationships, unsuccessful attempts to decrease use and withdrawal symptoms,” the “Media Use in School-Aged Children and Adolescents” policy statement notes.
Recommendations for older children
The policy statement advises pediatricians to help families and schools promote understanding of media’s risks and benefits, including awareness of tools to screen for sexting, cyberbullying, problematic Internet use, and Internet gaming disorder. Pediatricians should advocate for training in media literacy in the community and encourage parents to follow the media, sleep, and physical activity guidelines included in the Family Media Plan.
The research was supported by the American Academy of Pediatrics. The authors reported no disclosures.
Obesity risk rises when kids aren’t active 1 hour a day
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
SAN FRANCISCO – The behavioral characteristic that correlated the most with obesity in school-age children was being active less than 1 hour per day, according to findings from a prospective study.
Meredith Johnston, DO, of Eau Claire Cooperative in Columbia, S.C., performed the study with Nirupma Sharma, MD, at Children’s Hospital of Georgia in Augusta. The prospective, questionnaire-based study was conducted with 103 children, aged 5-18 years, over a 6-month period. Dr. Johnston reported the results in a poster presentation at the annual meeting of the American Academy of Pediatrics.
“Giving a child one modifiable lifestyle factor to incorporate into their lifestyle instead of overwhelming them with multiple changes is more likely to produce significant change to prevent obesity,” Dr. Johnston said in an interview. “And finding an activity that the child enjoys will produce the best adherence and greatest long-term effects.”
Considering the findings of the study, “children should exercise 30 minutes to 1 hour a day to prevent childhood obesity,” she explained.
A recent review in the Annual Review of Public Health has shown a change in teen physical activity patterns due to an increase in screen time and a decrease in opportunities for physical activities at school and in the community. Giving patients tools for exercise such as dancing to YouTube videos or playing active video games might be a good idea, Dr. Johnston said.
Drinking more than five cans of soda in a day also was significantly associated with a higher BMI (P = .001). That lifestyle factor could be addressed at subsequent well-child visits.
Such efforts are critical, she noted, because an estimated 17% of 2- to 19-year-olds are obese, and 15% are overweight.
Dr. Johnston said she had no relevant financial disclosures.
AT AAP 2016
Key clinical point:
Major finding: Being active less than 1 hour per day was significantly associated with a higher body mass index in children (P = .006 for 30 minutes to 1 hour, and P = .017 for less than 30 minutes).
Data source: A prospective, questionnaire-based study involving 103 children, aged 5-18 years, over a 6-month period.
Disclosures: Dr. Johnston said she had no relevant financial disclosures.
Updated AAP safe sleep recs for infants reinforce life-saving messages
SAN FRANCISCO – At sleep time, infants should share their parents’ bedroom on a separate sleep surface without bed sharing, should be placed on their backs on a firm surface, and should have a sleep area free of blankets and soft objects, according to updated guidelines from the American Academy of Pediatrics aimed at reducing the risk of sudden infant death syndrome (SIDS) and other sleep-related infant deaths.
Drafted by a multidisciplinary task force, the set of 19 evidence-based recommendations largely reiterate messages that the academy has promoted for years such as “back to sleep for every sleep,” according to task force member Fern R. Hauck, MD, the Spencer P. Bass, MD, Twenty-First Century Professor of Family Medicine at the University of Virginia, Charlottesville. They were unveiled in a press briefing at the academy’s annual meeting and simultaneously published (Pediatrics. 2016;138[5]:e20162938).
Progress, but still a ways to go
Education campaigns that convey these and related messages to new parents and other caregivers have led to a more than halving of the rate of SIDS in recent decades. Yet, 3,500 infants are still lost each year to this syndrome and other sleep-related causes of infant death, such as unintentional suffocation, collectively called sudden unexpected infant death (SUID).
New is a recommendation for skin-to-skin care for at least the first hour of life for healthy newborns, as soon as the mother is alert enough to respond to her infant, according to Dr. Hauck. The aims here are to optimize neurodevelopment and promote temperature regulation.
There is no evidence that swaddling reduces the risk of SIDS, but parents can still use this technique if they wish as long as infants are placed on their back and it is discontinued as soon as they start to show signs of rolling over, she said. Evidence is also lacking for new technologies marketed as protective, for example, crib mattresses designed to reduce re-breathing of carbon dioxide should an infant become prone.
Sleeping in the parents’ room but on a separate surface decreases the risk of SIDS by as much as 50%, according to several studies. Bed sharing is not recommended because of the risk of suffocation, strangulation, and entrapment, the policy states.
The updated recommendations should be followed for every sleep and by every caregiver, until the child reaches 1 year of age, Dr. Hauck stressed. “This includes nap time and bedtime sleep, at home, in day care, or in any other locations where the baby is sleeping.”
“We feel that these messages need to start while the mom’s pregnant because some of the decisions that are made that are not always the best decisions, when the mother is exhausted, can occur spur of the moment,” she added. “As pediatricians, you can set up a prebirth visit to start talking about this, and obstetricians should be doing more as well to bring this up during their prenatal visits.”
Other recommendations include offering a pacifier at nap time and bedtime; avoiding smoke exposure during pregnancy and after birth; and avoiding alcohol and illicit drug use during pregnancy and after birth.
Breastfeeding issues
Although breastfeeding protects against SIDS, it can pose some problems for safe sleep practices, acknowledged Lori B. Feldman-Winter, MD, a liaison from the AAP section on breastfeeding to the task force, as well as head of the division of adolescent medicine and professor of pediatrics at Cooper University Health Care in Camden, N.J.
Bedside sleepers (also called sidecar sleepers) that attach to the parents’ bed may help facilitate the dual aims of breastfeeding and safe sleep, but they have not been formally studied to assess their impact on SIDS risk.
Raising awareness
“As a father and pediatrician, I want parents to know that their baby is safest following the AAP safe sleep recommendations, and spreading this message has become my life’s mission,” said Dr. Samuel P. Hanke, a pediatric cardiologist at the University of Cincinnati, who knows the heartbreak of SIDS firsthand.
“We know practicing safe sleep is hard. We have to be vigilant. We need to start adopting a mentality that safe sleep is not negotiable,” Dr. Hanke asserted. “We cannot emphasize enough that practicing safe sleep for every sleep is as important as buckling your child into a car seat for every drive. And just like car seats, this change won’t occur overnight.”
Federal commitment
Since the 1970s, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) in Bethesda, Md., has been supporting and performing much of the research on which the updated recommendations are based. This research continues to help identify areas where greater efforts are needed, according to acting director Catherine Y. Spong, MD.
NICHD also conducts and collaborates on related education campaigns, such as Safe to Sleep, to disseminate messages such as those in the updated AAP recommendations as widely as possible.
“I encourage all physicians, pediatricians, nurses, and other health care and child care providers to lend their authoritative voices to the Safe to Sleep effort,” Dr. Spong said. “Join us all in sharing safe infant sleep recommendations and in supporting parents and caregivers to make informed decisions that will help keep their baby safe during sleep.”
A closer look at setting
Published in conjunction with the guidelines is a study on risk factors that looked at the role of the setting in which sleep-related infant deaths occur (Pediatrics. 2016 Oct 24:e20161124).
The analysis of nearly 12,000 such deaths found that, relative to counterparts who died in their home, infants who died outside of their home were more likely to be in a stroller or car seat at the time (adjusted odds ratio, 2.6) and in other locations, such as on the floor or a futon (1.9), and to have been placed prone (1.1). They were less likely to have been sharing a bed (0.7).
The groups did not differ in terms of whether the infant was sleeping in an adult bed or on a person, on a couch or chair, or with any objects in their sleep environment.
“Caregivers should be educated on the importance of placing infants to sleep supine in cribs/bassinets to protect against sleep-related deaths, both in and out of the home,” conclude the investigators, one of whom disclosed serving as a paid expert witness in cases of sleep-related infant death.
SAN FRANCISCO – At sleep time, infants should share their parents’ bedroom on a separate sleep surface without bed sharing, should be placed on their backs on a firm surface, and should have a sleep area free of blankets and soft objects, according to updated guidelines from the American Academy of Pediatrics aimed at reducing the risk of sudden infant death syndrome (SIDS) and other sleep-related infant deaths.
Drafted by a multidisciplinary task force, the set of 19 evidence-based recommendations largely reiterate messages that the academy has promoted for years such as “back to sleep for every sleep,” according to task force member Fern R. Hauck, MD, the Spencer P. Bass, MD, Twenty-First Century Professor of Family Medicine at the University of Virginia, Charlottesville. They were unveiled in a press briefing at the academy’s annual meeting and simultaneously published (Pediatrics. 2016;138[5]:e20162938).
Progress, but still a ways to go
Education campaigns that convey these and related messages to new parents and other caregivers have led to a more than halving of the rate of SIDS in recent decades. Yet, 3,500 infants are still lost each year to this syndrome and other sleep-related causes of infant death, such as unintentional suffocation, collectively called sudden unexpected infant death (SUID).
New is a recommendation for skin-to-skin care for at least the first hour of life for healthy newborns, as soon as the mother is alert enough to respond to her infant, according to Dr. Hauck. The aims here are to optimize neurodevelopment and promote temperature regulation.
There is no evidence that swaddling reduces the risk of SIDS, but parents can still use this technique if they wish as long as infants are placed on their back and it is discontinued as soon as they start to show signs of rolling over, she said. Evidence is also lacking for new technologies marketed as protective, for example, crib mattresses designed to reduce re-breathing of carbon dioxide should an infant become prone.
Sleeping in the parents’ room but on a separate surface decreases the risk of SIDS by as much as 50%, according to several studies. Bed sharing is not recommended because of the risk of suffocation, strangulation, and entrapment, the policy states.
The updated recommendations should be followed for every sleep and by every caregiver, until the child reaches 1 year of age, Dr. Hauck stressed. “This includes nap time and bedtime sleep, at home, in day care, or in any other locations where the baby is sleeping.”
“We feel that these messages need to start while the mom’s pregnant because some of the decisions that are made that are not always the best decisions, when the mother is exhausted, can occur spur of the moment,” she added. “As pediatricians, you can set up a prebirth visit to start talking about this, and obstetricians should be doing more as well to bring this up during their prenatal visits.”
Other recommendations include offering a pacifier at nap time and bedtime; avoiding smoke exposure during pregnancy and after birth; and avoiding alcohol and illicit drug use during pregnancy and after birth.
Breastfeeding issues
Although breastfeeding protects against SIDS, it can pose some problems for safe sleep practices, acknowledged Lori B. Feldman-Winter, MD, a liaison from the AAP section on breastfeeding to the task force, as well as head of the division of adolescent medicine and professor of pediatrics at Cooper University Health Care in Camden, N.J.
Bedside sleepers (also called sidecar sleepers) that attach to the parents’ bed may help facilitate the dual aims of breastfeeding and safe sleep, but they have not been formally studied to assess their impact on SIDS risk.
Raising awareness
“As a father and pediatrician, I want parents to know that their baby is safest following the AAP safe sleep recommendations, and spreading this message has become my life’s mission,” said Dr. Samuel P. Hanke, a pediatric cardiologist at the University of Cincinnati, who knows the heartbreak of SIDS firsthand.
“We know practicing safe sleep is hard. We have to be vigilant. We need to start adopting a mentality that safe sleep is not negotiable,” Dr. Hanke asserted. “We cannot emphasize enough that practicing safe sleep for every sleep is as important as buckling your child into a car seat for every drive. And just like car seats, this change won’t occur overnight.”
Federal commitment
Since the 1970s, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) in Bethesda, Md., has been supporting and performing much of the research on which the updated recommendations are based. This research continues to help identify areas where greater efforts are needed, according to acting director Catherine Y. Spong, MD.
NICHD also conducts and collaborates on related education campaigns, such as Safe to Sleep, to disseminate messages such as those in the updated AAP recommendations as widely as possible.
“I encourage all physicians, pediatricians, nurses, and other health care and child care providers to lend their authoritative voices to the Safe to Sleep effort,” Dr. Spong said. “Join us all in sharing safe infant sleep recommendations and in supporting parents and caregivers to make informed decisions that will help keep their baby safe during sleep.”
A closer look at setting
Published in conjunction with the guidelines is a study on risk factors that looked at the role of the setting in which sleep-related infant deaths occur (Pediatrics. 2016 Oct 24:e20161124).
The analysis of nearly 12,000 such deaths found that, relative to counterparts who died in their home, infants who died outside of their home were more likely to be in a stroller or car seat at the time (adjusted odds ratio, 2.6) and in other locations, such as on the floor or a futon (1.9), and to have been placed prone (1.1). They were less likely to have been sharing a bed (0.7).
The groups did not differ in terms of whether the infant was sleeping in an adult bed or on a person, on a couch or chair, or with any objects in their sleep environment.
“Caregivers should be educated on the importance of placing infants to sleep supine in cribs/bassinets to protect against sleep-related deaths, both in and out of the home,” conclude the investigators, one of whom disclosed serving as a paid expert witness in cases of sleep-related infant death.
SAN FRANCISCO – At sleep time, infants should share their parents’ bedroom on a separate sleep surface without bed sharing, should be placed on their backs on a firm surface, and should have a sleep area free of blankets and soft objects, according to updated guidelines from the American Academy of Pediatrics aimed at reducing the risk of sudden infant death syndrome (SIDS) and other sleep-related infant deaths.
Drafted by a multidisciplinary task force, the set of 19 evidence-based recommendations largely reiterate messages that the academy has promoted for years such as “back to sleep for every sleep,” according to task force member Fern R. Hauck, MD, the Spencer P. Bass, MD, Twenty-First Century Professor of Family Medicine at the University of Virginia, Charlottesville. They were unveiled in a press briefing at the academy’s annual meeting and simultaneously published (Pediatrics. 2016;138[5]:e20162938).
Progress, but still a ways to go
Education campaigns that convey these and related messages to new parents and other caregivers have led to a more than halving of the rate of SIDS in recent decades. Yet, 3,500 infants are still lost each year to this syndrome and other sleep-related causes of infant death, such as unintentional suffocation, collectively called sudden unexpected infant death (SUID).
New is a recommendation for skin-to-skin care for at least the first hour of life for healthy newborns, as soon as the mother is alert enough to respond to her infant, according to Dr. Hauck. The aims here are to optimize neurodevelopment and promote temperature regulation.
There is no evidence that swaddling reduces the risk of SIDS, but parents can still use this technique if they wish as long as infants are placed on their back and it is discontinued as soon as they start to show signs of rolling over, she said. Evidence is also lacking for new technologies marketed as protective, for example, crib mattresses designed to reduce re-breathing of carbon dioxide should an infant become prone.
Sleeping in the parents’ room but on a separate surface decreases the risk of SIDS by as much as 50%, according to several studies. Bed sharing is not recommended because of the risk of suffocation, strangulation, and entrapment, the policy states.
The updated recommendations should be followed for every sleep and by every caregiver, until the child reaches 1 year of age, Dr. Hauck stressed. “This includes nap time and bedtime sleep, at home, in day care, or in any other locations where the baby is sleeping.”
“We feel that these messages need to start while the mom’s pregnant because some of the decisions that are made that are not always the best decisions, when the mother is exhausted, can occur spur of the moment,” she added. “As pediatricians, you can set up a prebirth visit to start talking about this, and obstetricians should be doing more as well to bring this up during their prenatal visits.”
Other recommendations include offering a pacifier at nap time and bedtime; avoiding smoke exposure during pregnancy and after birth; and avoiding alcohol and illicit drug use during pregnancy and after birth.
Breastfeeding issues
Although breastfeeding protects against SIDS, it can pose some problems for safe sleep practices, acknowledged Lori B. Feldman-Winter, MD, a liaison from the AAP section on breastfeeding to the task force, as well as head of the division of adolescent medicine and professor of pediatrics at Cooper University Health Care in Camden, N.J.
Bedside sleepers (also called sidecar sleepers) that attach to the parents’ bed may help facilitate the dual aims of breastfeeding and safe sleep, but they have not been formally studied to assess their impact on SIDS risk.
Raising awareness
“As a father and pediatrician, I want parents to know that their baby is safest following the AAP safe sleep recommendations, and spreading this message has become my life’s mission,” said Dr. Samuel P. Hanke, a pediatric cardiologist at the University of Cincinnati, who knows the heartbreak of SIDS firsthand.
“We know practicing safe sleep is hard. We have to be vigilant. We need to start adopting a mentality that safe sleep is not negotiable,” Dr. Hanke asserted. “We cannot emphasize enough that practicing safe sleep for every sleep is as important as buckling your child into a car seat for every drive. And just like car seats, this change won’t occur overnight.”
Federal commitment
Since the 1970s, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) in Bethesda, Md., has been supporting and performing much of the research on which the updated recommendations are based. This research continues to help identify areas where greater efforts are needed, according to acting director Catherine Y. Spong, MD.
NICHD also conducts and collaborates on related education campaigns, such as Safe to Sleep, to disseminate messages such as those in the updated AAP recommendations as widely as possible.
“I encourage all physicians, pediatricians, nurses, and other health care and child care providers to lend their authoritative voices to the Safe to Sleep effort,” Dr. Spong said. “Join us all in sharing safe infant sleep recommendations and in supporting parents and caregivers to make informed decisions that will help keep their baby safe during sleep.”
A closer look at setting
Published in conjunction with the guidelines is a study on risk factors that looked at the role of the setting in which sleep-related infant deaths occur (Pediatrics. 2016 Oct 24:e20161124).
The analysis of nearly 12,000 such deaths found that, relative to counterparts who died in their home, infants who died outside of their home were more likely to be in a stroller or car seat at the time (adjusted odds ratio, 2.6) and in other locations, such as on the floor or a futon (1.9), and to have been placed prone (1.1). They were less likely to have been sharing a bed (0.7).
The groups did not differ in terms of whether the infant was sleeping in an adult bed or on a person, on a couch or chair, or with any objects in their sleep environment.
“Caregivers should be educated on the importance of placing infants to sleep supine in cribs/bassinets to protect against sleep-related deaths, both in and out of the home,” conclude the investigators, one of whom disclosed serving as a paid expert witness in cases of sleep-related infant death.
EXPERT ANALYSIS FROM AAP 16