User login
DEET and picaridin safely protect against insect bites
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
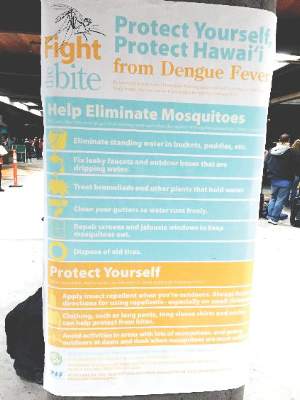
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
EXPERT ANALYSIS FROM AAD SUMMER ACADEMY 2016
Distinguish between autoinflammatory, autoimmune disorders in children
Boston – Autoinflammatory and autoimmune disorders in children have many overlapping features, but the former represents a malfunction of the innate immune system, and the latter a malfunction of the adaptive immune system. Fevers, skin eruptions, joint pain and swelling, fatigue, and growth failure can occur in both, but it is important to identify the underlying problem, according to Raegan Hunt, MD.
Autoinflammatory disorders can be difficult to detect, so it is important to maintain a high index of suspicion for them, Dr. Hunt of Baylor College of Medicine and Texas Children’s Hospital, Houston, said at the American Academy of Dermatology annual summer meeting.
She discussed five signs of possible autoinflammatory disease in children, as described in a recent report by Hal M. Hoffman, MD, and Lori Broderick, MD, of Children’s Hospital of San Diego, La Jolla, Calif. (J Allergy Clin Immunol. July 2016; 138:3-14)*:
1. More than three episodes of fever over 101 degrees Farenheit with no explained infectious etiology.
2. Having predictable patterns of characteristic course of each episode.
3. Having specific symptoms during episodes, including nonpruritic skin eruptions, joint or bone pain, severe abdominal pain, and conjunctivitis, with no upper respiratory infection symptoms.
4. Episodes may be triggered by specific stimuli, such as cold exposure or vaccines.
5. A family history of autoinflammatory disease or amyloidosis.
The authors “propose that two or more of these might suggest that an autoinflammatory disorder is possible and should be investigated,” Dr. Hunt said.
Dr. Hunt reported having no relevant disclosures.
sworcester@frontlinemedcom.com
*Correction, 8/16/16: An earlier version of this article failed to note that Dr. Lori Broderick was a co-investigator in the cited report.
Boston – Autoinflammatory and autoimmune disorders in children have many overlapping features, but the former represents a malfunction of the innate immune system, and the latter a malfunction of the adaptive immune system. Fevers, skin eruptions, joint pain and swelling, fatigue, and growth failure can occur in both, but it is important to identify the underlying problem, according to Raegan Hunt, MD.
Autoinflammatory disorders can be difficult to detect, so it is important to maintain a high index of suspicion for them, Dr. Hunt of Baylor College of Medicine and Texas Children’s Hospital, Houston, said at the American Academy of Dermatology annual summer meeting.
She discussed five signs of possible autoinflammatory disease in children, as described in a recent report by Hal M. Hoffman, MD, and Lori Broderick, MD, of Children’s Hospital of San Diego, La Jolla, Calif. (J Allergy Clin Immunol. July 2016; 138:3-14)*:
1. More than three episodes of fever over 101 degrees Farenheit with no explained infectious etiology.
2. Having predictable patterns of characteristic course of each episode.
3. Having specific symptoms during episodes, including nonpruritic skin eruptions, joint or bone pain, severe abdominal pain, and conjunctivitis, with no upper respiratory infection symptoms.
4. Episodes may be triggered by specific stimuli, such as cold exposure or vaccines.
5. A family history of autoinflammatory disease or amyloidosis.
The authors “propose that two or more of these might suggest that an autoinflammatory disorder is possible and should be investigated,” Dr. Hunt said.
Dr. Hunt reported having no relevant disclosures.
sworcester@frontlinemedcom.com
*Correction, 8/16/16: An earlier version of this article failed to note that Dr. Lori Broderick was a co-investigator in the cited report.
Boston – Autoinflammatory and autoimmune disorders in children have many overlapping features, but the former represents a malfunction of the innate immune system, and the latter a malfunction of the adaptive immune system. Fevers, skin eruptions, joint pain and swelling, fatigue, and growth failure can occur in both, but it is important to identify the underlying problem, according to Raegan Hunt, MD.
Autoinflammatory disorders can be difficult to detect, so it is important to maintain a high index of suspicion for them, Dr. Hunt of Baylor College of Medicine and Texas Children’s Hospital, Houston, said at the American Academy of Dermatology annual summer meeting.
She discussed five signs of possible autoinflammatory disease in children, as described in a recent report by Hal M. Hoffman, MD, and Lori Broderick, MD, of Children’s Hospital of San Diego, La Jolla, Calif. (J Allergy Clin Immunol. July 2016; 138:3-14)*:
1. More than three episodes of fever over 101 degrees Farenheit with no explained infectious etiology.
2. Having predictable patterns of characteristic course of each episode.
3. Having specific symptoms during episodes, including nonpruritic skin eruptions, joint or bone pain, severe abdominal pain, and conjunctivitis, with no upper respiratory infection symptoms.
4. Episodes may be triggered by specific stimuli, such as cold exposure or vaccines.
5. A family history of autoinflammatory disease or amyloidosis.
The authors “propose that two or more of these might suggest that an autoinflammatory disorder is possible and should be investigated,” Dr. Hunt said.
Dr. Hunt reported having no relevant disclosures.
sworcester@frontlinemedcom.com
*Correction, 8/16/16: An earlier version of this article failed to note that Dr. Lori Broderick was a co-investigator in the cited report.
Expert Analysis from the AAD Summer Academy 2016
Sunscreens safe in babies, children
BOSTON – Despite what some popular online media outlets report, sunscreens are safe in children and can even be used on infants under 6 months of age when sun avoidance – the best approach to protecting babies from the damaging effects of the sun – is not possible, according to Mercedes E. Gonzalez, MD.
A quick Google search reveals numerous, widely-shared articles about the dangers lurking in one’s beach bag, and while many product labels recommend asking a doctor about whether the product is safe for babies under age 6 months, that’s only because most product safety studies didn’t include that age group, Dr. Gonzalez of the University of Miami said at the American Academy of Dermatology summer meeting.
In fact, there is “nothing magical that happens” in infant skin after 6 months that makes sunscreen use safer, she said, explaining that infant skin is structurally and functionally different from adult skin, and that while gradual maturation takes place over time, thereby reducing susceptibility to percutaneous absorption of topically applied products, the risk is minimal even in babies younger than age 6 months.
The skin characteristics that make younger skin more susceptible to percutaneous absorption also make babies and children unusually susceptible to ultraviolet radiation and ultraviolet radiation–induced immunosuppression, for which the consequences are not fully understood, she said.
Among the more commonly cited sunscreen ingredients of concern are oxybenzone, or benzonephenone-3, and nanoparticles, she noted.
However, the overall consensus based on studies of oxybenzone is that aside from causing some cases of allergic and irritant contact dermatitis, the compound is safe; no harmful cause and effect relationship with oxybenzone and systemic side effects in humans have been reported, and periodic reviews by European, Australian and U.S. safety panels all conclude that it is safe.
Numerous studies of nanoparticles – such as nanosized zinc oxide and titanium dioxide – have shown that absorption is confined to the level of stratum corneum – even when skin barrier function has been altered, she said, noting that most are coated with aluminum oxide and SiO2 to minimize contact.
However, the safety of sunscreen shouldn’t be seen as license to ignore sun-exposure recommendations; sunscreen in infants should be considered “the last layer of protection,” used only on exposed areas when adequate clothing and shade are not available, according to a 2011 American Academy of Pediatrics statement (Pediatrics. 2011 Feb. doi: 10.1542/peds.2010-3501).
Efforts should be made to keep babies in the shade when outdoors whenever possible, especially during peak sun hours. Use sun-protective clothing, including hats, sunglasses, and long-sleeved shirts, Dr. Gonzalez advised.
When sunscreen is required, a broad-spectrum water-resistant product with an SPF of more than 30 is preferable.
“But the best sunscreen is the one you and your child will use,” she said.
Mineral-based products are less irritating and thus may be a preferred option for children with atopic dermatitis, she added.
Advise parents to apply sunscreen to all areas not protected by their child’s clothing, paying particular attention to vulnerable areas, including the back of the neck, ears, and dorsal feet. Reapply before going outdoors, and then again every 2 hours, she advised.
“So the overall answer to the parents’ question, ‘Are sunscreens safe?’ ... the overwhelming answer here is yes, and the weight of the evidence shows there is no proven harm from sunscreen use especially when used properly,” she said.
Provide specific guidance for pediatric sunscreen use
In the face of conflicting information about sunscreen safety and efficacy, parents with questions about sunscreen are looking for specific direction, Dr. Gonzalez said.
She said she finds it helpful to teach them about the importance of reading labels. That is, looking at the ingredients, and looking for SPF above 30, broad-spectrum coverage, and water resistance. She also recommends providing a list or images of good options, and circling the specific preferred products.
For babies, she finds stick sunscreens most useful for application.
“I generally don’t recommend sprays, but if they’re going to use a spray – and parents love sprays because they are easy to apply – I recommend the ones that have some zinc oxide in them, so that when they apply them they can see where they’re going on the skin,” Dr. Gonzalez said.
Tell patients to apply sunscreen before leaving the house, she advised, adding that making sunscreen application part of a daily routine helps encourage healthy behaviors, as does allowing children, at the right age, to participate in sunscreen application.
For adolescents, avoid scare tactics such as warning about skin cancer. Rather, focus on benefits of avoiding the sun, help them find a product they like by finding out why they don’t like a particular product and recommending an alternative, then following up on that when they come back in, she suggested.
“I really try to address it at every visit,” Dr. Gonzalez said.
“Finally, the most important message is that sunscreen is really just one part of complete sun protection,” she said, noting that specific information about where to buy sun-protective clothing and hats is also important.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Despite what some popular online media outlets report, sunscreens are safe in children and can even be used on infants under 6 months of age when sun avoidance – the best approach to protecting babies from the damaging effects of the sun – is not possible, according to Mercedes E. Gonzalez, MD.
A quick Google search reveals numerous, widely-shared articles about the dangers lurking in one’s beach bag, and while many product labels recommend asking a doctor about whether the product is safe for babies under age 6 months, that’s only because most product safety studies didn’t include that age group, Dr. Gonzalez of the University of Miami said at the American Academy of Dermatology summer meeting.
In fact, there is “nothing magical that happens” in infant skin after 6 months that makes sunscreen use safer, she said, explaining that infant skin is structurally and functionally different from adult skin, and that while gradual maturation takes place over time, thereby reducing susceptibility to percutaneous absorption of topically applied products, the risk is minimal even in babies younger than age 6 months.
The skin characteristics that make younger skin more susceptible to percutaneous absorption also make babies and children unusually susceptible to ultraviolet radiation and ultraviolet radiation–induced immunosuppression, for which the consequences are not fully understood, she said.
Among the more commonly cited sunscreen ingredients of concern are oxybenzone, or benzonephenone-3, and nanoparticles, she noted.
However, the overall consensus based on studies of oxybenzone is that aside from causing some cases of allergic and irritant contact dermatitis, the compound is safe; no harmful cause and effect relationship with oxybenzone and systemic side effects in humans have been reported, and periodic reviews by European, Australian and U.S. safety panels all conclude that it is safe.
Numerous studies of nanoparticles – such as nanosized zinc oxide and titanium dioxide – have shown that absorption is confined to the level of stratum corneum – even when skin barrier function has been altered, she said, noting that most are coated with aluminum oxide and SiO2 to minimize contact.
However, the safety of sunscreen shouldn’t be seen as license to ignore sun-exposure recommendations; sunscreen in infants should be considered “the last layer of protection,” used only on exposed areas when adequate clothing and shade are not available, according to a 2011 American Academy of Pediatrics statement (Pediatrics. 2011 Feb. doi: 10.1542/peds.2010-3501).
Efforts should be made to keep babies in the shade when outdoors whenever possible, especially during peak sun hours. Use sun-protective clothing, including hats, sunglasses, and long-sleeved shirts, Dr. Gonzalez advised.
When sunscreen is required, a broad-spectrum water-resistant product with an SPF of more than 30 is preferable.
“But the best sunscreen is the one you and your child will use,” she said.
Mineral-based products are less irritating and thus may be a preferred option for children with atopic dermatitis, she added.
Advise parents to apply sunscreen to all areas not protected by their child’s clothing, paying particular attention to vulnerable areas, including the back of the neck, ears, and dorsal feet. Reapply before going outdoors, and then again every 2 hours, she advised.
“So the overall answer to the parents’ question, ‘Are sunscreens safe?’ ... the overwhelming answer here is yes, and the weight of the evidence shows there is no proven harm from sunscreen use especially when used properly,” she said.
Provide specific guidance for pediatric sunscreen use
In the face of conflicting information about sunscreen safety and efficacy, parents with questions about sunscreen are looking for specific direction, Dr. Gonzalez said.
She said she finds it helpful to teach them about the importance of reading labels. That is, looking at the ingredients, and looking for SPF above 30, broad-spectrum coverage, and water resistance. She also recommends providing a list or images of good options, and circling the specific preferred products.
For babies, she finds stick sunscreens most useful for application.
“I generally don’t recommend sprays, but if they’re going to use a spray – and parents love sprays because they are easy to apply – I recommend the ones that have some zinc oxide in them, so that when they apply them they can see where they’re going on the skin,” Dr. Gonzalez said.
Tell patients to apply sunscreen before leaving the house, she advised, adding that making sunscreen application part of a daily routine helps encourage healthy behaviors, as does allowing children, at the right age, to participate in sunscreen application.
For adolescents, avoid scare tactics such as warning about skin cancer. Rather, focus on benefits of avoiding the sun, help them find a product they like by finding out why they don’t like a particular product and recommending an alternative, then following up on that when they come back in, she suggested.
“I really try to address it at every visit,” Dr. Gonzalez said.
“Finally, the most important message is that sunscreen is really just one part of complete sun protection,” she said, noting that specific information about where to buy sun-protective clothing and hats is also important.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Despite what some popular online media outlets report, sunscreens are safe in children and can even be used on infants under 6 months of age when sun avoidance – the best approach to protecting babies from the damaging effects of the sun – is not possible, according to Mercedes E. Gonzalez, MD.
A quick Google search reveals numerous, widely-shared articles about the dangers lurking in one’s beach bag, and while many product labels recommend asking a doctor about whether the product is safe for babies under age 6 months, that’s only because most product safety studies didn’t include that age group, Dr. Gonzalez of the University of Miami said at the American Academy of Dermatology summer meeting.
In fact, there is “nothing magical that happens” in infant skin after 6 months that makes sunscreen use safer, she said, explaining that infant skin is structurally and functionally different from adult skin, and that while gradual maturation takes place over time, thereby reducing susceptibility to percutaneous absorption of topically applied products, the risk is minimal even in babies younger than age 6 months.
The skin characteristics that make younger skin more susceptible to percutaneous absorption also make babies and children unusually susceptible to ultraviolet radiation and ultraviolet radiation–induced immunosuppression, for which the consequences are not fully understood, she said.
Among the more commonly cited sunscreen ingredients of concern are oxybenzone, or benzonephenone-3, and nanoparticles, she noted.
However, the overall consensus based on studies of oxybenzone is that aside from causing some cases of allergic and irritant contact dermatitis, the compound is safe; no harmful cause and effect relationship with oxybenzone and systemic side effects in humans have been reported, and periodic reviews by European, Australian and U.S. safety panels all conclude that it is safe.
Numerous studies of nanoparticles – such as nanosized zinc oxide and titanium dioxide – have shown that absorption is confined to the level of stratum corneum – even when skin barrier function has been altered, she said, noting that most are coated with aluminum oxide and SiO2 to minimize contact.
However, the safety of sunscreen shouldn’t be seen as license to ignore sun-exposure recommendations; sunscreen in infants should be considered “the last layer of protection,” used only on exposed areas when adequate clothing and shade are not available, according to a 2011 American Academy of Pediatrics statement (Pediatrics. 2011 Feb. doi: 10.1542/peds.2010-3501).
Efforts should be made to keep babies in the shade when outdoors whenever possible, especially during peak sun hours. Use sun-protective clothing, including hats, sunglasses, and long-sleeved shirts, Dr. Gonzalez advised.
When sunscreen is required, a broad-spectrum water-resistant product with an SPF of more than 30 is preferable.
“But the best sunscreen is the one you and your child will use,” she said.
Mineral-based products are less irritating and thus may be a preferred option for children with atopic dermatitis, she added.
Advise parents to apply sunscreen to all areas not protected by their child’s clothing, paying particular attention to vulnerable areas, including the back of the neck, ears, and dorsal feet. Reapply before going outdoors, and then again every 2 hours, she advised.
“So the overall answer to the parents’ question, ‘Are sunscreens safe?’ ... the overwhelming answer here is yes, and the weight of the evidence shows there is no proven harm from sunscreen use especially when used properly,” she said.
Provide specific guidance for pediatric sunscreen use
In the face of conflicting information about sunscreen safety and efficacy, parents with questions about sunscreen are looking for specific direction, Dr. Gonzalez said.
She said she finds it helpful to teach them about the importance of reading labels. That is, looking at the ingredients, and looking for SPF above 30, broad-spectrum coverage, and water resistance. She also recommends providing a list or images of good options, and circling the specific preferred products.
For babies, she finds stick sunscreens most useful for application.
“I generally don’t recommend sprays, but if they’re going to use a spray – and parents love sprays because they are easy to apply – I recommend the ones that have some zinc oxide in them, so that when they apply them they can see where they’re going on the skin,” Dr. Gonzalez said.
Tell patients to apply sunscreen before leaving the house, she advised, adding that making sunscreen application part of a daily routine helps encourage healthy behaviors, as does allowing children, at the right age, to participate in sunscreen application.
For adolescents, avoid scare tactics such as warning about skin cancer. Rather, focus on benefits of avoiding the sun, help them find a product they like by finding out why they don’t like a particular product and recommending an alternative, then following up on that when they come back in, she suggested.
“I really try to address it at every visit,” Dr. Gonzalez said.
“Finally, the most important message is that sunscreen is really just one part of complete sun protection,” she said, noting that specific information about where to buy sun-protective clothing and hats is also important.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
Rosacea responds well to laser, IPL therapies
BOSTON – Patients with rosacea, particularly the erythrotelangiectatic form, are considered good candidates for treatment with lasers and light therapies, but for acne, treatments with these therapies are still in the development stage.
For acne, treatments that are being studied include those that target the sebaceous glands, according to Mathew M. Avram, MD, who spoke about laser and light therapies for acne and rosacea at the American Academy of Dermatology summer meeting.
Light therapies for rosacea
Oxyhemoglobin in the blood absorbs light from lasers at wavelengths of about 595 nm (pulsed dye laser) and 532 nm (KTP laser), creating heat that helps destroy capillaries that contribute to the appearance of rosacea. Over a period of 3-4 weeks, the vessels are resorbed, and facial redness diminishes.
Patients with rosacea that are expected to do best with laser therapy are those with telangiectasia. Laser therapy is also effective for background redness but will be less effective for people with the papules associated with rosacea and “almost not effective at all for preventing flushing,” Dr. Avram said in an interview at the meeting.
Intense pulsed light (IPL) is another modality for treating rosacea. As with lasers, the mode of action is heating of certain structures and chromophores, causing their destruction and resorption, but unlike lasers, IPL output is broad spectrum and can be modified using filters.
With IPL, “basically, the endpoint that you want to see is transient purpural change, just a fleeting period of some black and blue, or if you’re treating vessels, you want to see vessel clearance when you’re firing the laser or the intense pulsed light,” said Dr. Avram, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, Boston.
On-screen settings of laser or IPL devices are essential, “but ultimately, if you want to have an effective treatment you really have to see what’s happening to your target … you need to pay attention to clinical endpoints, which is seeing that black and blue or that vessel clearance, not just paying attention to what’s on the screen.”
With IPL, too much pressure can compress vessels and blanch the skin, resulting in a less effective treatment, he added. He noted that tissue graying, whitening, or contraction indicates overly aggressive treatment, with the risk of scarring.
Certain factors can reduce the efficacy of IPL treatments of rosacea. Dr. Avram recommended against treating tanned skin and pointed out that anemic patients may benefit less from this approach since less hemoglobin presents a less-absorptive target for the treatments. He also advised particular caution when treating darker skin phototypes. But the most common factor that may make these treatments less effective is when a patient is on any type of anticoagulant, including NSAIDs or warfarin (Coumadin), because the mechanism of action is immediate microvascular hemorrhage, thrombosis, and eventual resorption.
For best results, Dr. Avram advises “appropriate overlap with the laser” to get an even and uniform improvement in the redness, with about a 15% overlap. Spacing laser spots too far apart can result in “foot printing,” the appearance of clearance in the areas of the laser pulse, but not in areas immediately around it “so it looks almost polka dotted.” After treatments, all patients should avoid the sun, he added.
What’s ahead for acne treatment
Until now, laser and light-based treatments for acne, “have provided inconsistent benefits for patients and all too often disappointing results,” Dr. Avram said in the interview. But several developments on the horizon may offer more effective therapies based on completely different technologies than are currently available. “Each of these therapies will be targeting the sebaceous glands in order to provide improved treatment for acne.”
One is a cryolysis device that uses cooling to selectively target lipids in the sebaceous glands. (Cryolysis is similar to cryolipolysis, which uses cooling to target fat cells.) The lipid-filled adipocytes are more sensitive to cold than is the water-rich dermis, thereby preserving the surrounding structures. There are also laser wavelengths that are absorbed by lipids, one of which is at about 1720 nm. In this case, heating rather than cooling targets the lipids.
Another technology in development is the use of nanoparticles coated with elements such as gold that are massaged through the skin into the sebaceous glands. Laser treatment with multiple different wavelengths targets the nanoparticles, heating them within the sebaceous glands, resulting in improvements in acne. In this case, treatment does not depend on the absorption spectrum of lipids. Clinical trials of this approach are now underway.
It is too early to tell which of these technologies is going to be effective or what potential side effects may occur. “However, the exciting news is that there will be multiple different technologies” designed to improve acne by targeting the sebaceous gland, and there is “the promise of potentially more effective noninvasive treatments that don’t require topical medications or oral medications,” Dr. Avram said.
For these potential new treatments, some objective outcome measure is needed to judge their efficacy. Right now, all that can be said is that they target the sebaceous gland, and clinical work still needs to be done to determine whether they will be effective, the degree of effectiveness, and how to optimize treatment, he noted.
Dr. Avram reported financial relationships with Cytrellis Biosystems, Invasix, Kythera, Masters of Aesthetics, Sciton, Zalea, and Zeltiq Aesthetics.
BOSTON – Patients with rosacea, particularly the erythrotelangiectatic form, are considered good candidates for treatment with lasers and light therapies, but for acne, treatments with these therapies are still in the development stage.
For acne, treatments that are being studied include those that target the sebaceous glands, according to Mathew M. Avram, MD, who spoke about laser and light therapies for acne and rosacea at the American Academy of Dermatology summer meeting.
Light therapies for rosacea
Oxyhemoglobin in the blood absorbs light from lasers at wavelengths of about 595 nm (pulsed dye laser) and 532 nm (KTP laser), creating heat that helps destroy capillaries that contribute to the appearance of rosacea. Over a period of 3-4 weeks, the vessels are resorbed, and facial redness diminishes.
Patients with rosacea that are expected to do best with laser therapy are those with telangiectasia. Laser therapy is also effective for background redness but will be less effective for people with the papules associated with rosacea and “almost not effective at all for preventing flushing,” Dr. Avram said in an interview at the meeting.
Intense pulsed light (IPL) is another modality for treating rosacea. As with lasers, the mode of action is heating of certain structures and chromophores, causing their destruction and resorption, but unlike lasers, IPL output is broad spectrum and can be modified using filters.
With IPL, “basically, the endpoint that you want to see is transient purpural change, just a fleeting period of some black and blue, or if you’re treating vessels, you want to see vessel clearance when you’re firing the laser or the intense pulsed light,” said Dr. Avram, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, Boston.
On-screen settings of laser or IPL devices are essential, “but ultimately, if you want to have an effective treatment you really have to see what’s happening to your target … you need to pay attention to clinical endpoints, which is seeing that black and blue or that vessel clearance, not just paying attention to what’s on the screen.”
With IPL, too much pressure can compress vessels and blanch the skin, resulting in a less effective treatment, he added. He noted that tissue graying, whitening, or contraction indicates overly aggressive treatment, with the risk of scarring.
Certain factors can reduce the efficacy of IPL treatments of rosacea. Dr. Avram recommended against treating tanned skin and pointed out that anemic patients may benefit less from this approach since less hemoglobin presents a less-absorptive target for the treatments. He also advised particular caution when treating darker skin phototypes. But the most common factor that may make these treatments less effective is when a patient is on any type of anticoagulant, including NSAIDs or warfarin (Coumadin), because the mechanism of action is immediate microvascular hemorrhage, thrombosis, and eventual resorption.
For best results, Dr. Avram advises “appropriate overlap with the laser” to get an even and uniform improvement in the redness, with about a 15% overlap. Spacing laser spots too far apart can result in “foot printing,” the appearance of clearance in the areas of the laser pulse, but not in areas immediately around it “so it looks almost polka dotted.” After treatments, all patients should avoid the sun, he added.
What’s ahead for acne treatment
Until now, laser and light-based treatments for acne, “have provided inconsistent benefits for patients and all too often disappointing results,” Dr. Avram said in the interview. But several developments on the horizon may offer more effective therapies based on completely different technologies than are currently available. “Each of these therapies will be targeting the sebaceous glands in order to provide improved treatment for acne.”
One is a cryolysis device that uses cooling to selectively target lipids in the sebaceous glands. (Cryolysis is similar to cryolipolysis, which uses cooling to target fat cells.) The lipid-filled adipocytes are more sensitive to cold than is the water-rich dermis, thereby preserving the surrounding structures. There are also laser wavelengths that are absorbed by lipids, one of which is at about 1720 nm. In this case, heating rather than cooling targets the lipids.
Another technology in development is the use of nanoparticles coated with elements such as gold that are massaged through the skin into the sebaceous glands. Laser treatment with multiple different wavelengths targets the nanoparticles, heating them within the sebaceous glands, resulting in improvements in acne. In this case, treatment does not depend on the absorption spectrum of lipids. Clinical trials of this approach are now underway.
It is too early to tell which of these technologies is going to be effective or what potential side effects may occur. “However, the exciting news is that there will be multiple different technologies” designed to improve acne by targeting the sebaceous gland, and there is “the promise of potentially more effective noninvasive treatments that don’t require topical medications or oral medications,” Dr. Avram said.
For these potential new treatments, some objective outcome measure is needed to judge their efficacy. Right now, all that can be said is that they target the sebaceous gland, and clinical work still needs to be done to determine whether they will be effective, the degree of effectiveness, and how to optimize treatment, he noted.
Dr. Avram reported financial relationships with Cytrellis Biosystems, Invasix, Kythera, Masters of Aesthetics, Sciton, Zalea, and Zeltiq Aesthetics.
BOSTON – Patients with rosacea, particularly the erythrotelangiectatic form, are considered good candidates for treatment with lasers and light therapies, but for acne, treatments with these therapies are still in the development stage.
For acne, treatments that are being studied include those that target the sebaceous glands, according to Mathew M. Avram, MD, who spoke about laser and light therapies for acne and rosacea at the American Academy of Dermatology summer meeting.
Light therapies for rosacea
Oxyhemoglobin in the blood absorbs light from lasers at wavelengths of about 595 nm (pulsed dye laser) and 532 nm (KTP laser), creating heat that helps destroy capillaries that contribute to the appearance of rosacea. Over a period of 3-4 weeks, the vessels are resorbed, and facial redness diminishes.
Patients with rosacea that are expected to do best with laser therapy are those with telangiectasia. Laser therapy is also effective for background redness but will be less effective for people with the papules associated with rosacea and “almost not effective at all for preventing flushing,” Dr. Avram said in an interview at the meeting.
Intense pulsed light (IPL) is another modality for treating rosacea. As with lasers, the mode of action is heating of certain structures and chromophores, causing their destruction and resorption, but unlike lasers, IPL output is broad spectrum and can be modified using filters.
With IPL, “basically, the endpoint that you want to see is transient purpural change, just a fleeting period of some black and blue, or if you’re treating vessels, you want to see vessel clearance when you’re firing the laser or the intense pulsed light,” said Dr. Avram, director of the Massachusetts General Hospital Dermatology Laser & Cosmetic Center, Boston.
On-screen settings of laser or IPL devices are essential, “but ultimately, if you want to have an effective treatment you really have to see what’s happening to your target … you need to pay attention to clinical endpoints, which is seeing that black and blue or that vessel clearance, not just paying attention to what’s on the screen.”
With IPL, too much pressure can compress vessels and blanch the skin, resulting in a less effective treatment, he added. He noted that tissue graying, whitening, or contraction indicates overly aggressive treatment, with the risk of scarring.
Certain factors can reduce the efficacy of IPL treatments of rosacea. Dr. Avram recommended against treating tanned skin and pointed out that anemic patients may benefit less from this approach since less hemoglobin presents a less-absorptive target for the treatments. He also advised particular caution when treating darker skin phototypes. But the most common factor that may make these treatments less effective is when a patient is on any type of anticoagulant, including NSAIDs or warfarin (Coumadin), because the mechanism of action is immediate microvascular hemorrhage, thrombosis, and eventual resorption.
For best results, Dr. Avram advises “appropriate overlap with the laser” to get an even and uniform improvement in the redness, with about a 15% overlap. Spacing laser spots too far apart can result in “foot printing,” the appearance of clearance in the areas of the laser pulse, but not in areas immediately around it “so it looks almost polka dotted.” After treatments, all patients should avoid the sun, he added.
What’s ahead for acne treatment
Until now, laser and light-based treatments for acne, “have provided inconsistent benefits for patients and all too often disappointing results,” Dr. Avram said in the interview. But several developments on the horizon may offer more effective therapies based on completely different technologies than are currently available. “Each of these therapies will be targeting the sebaceous glands in order to provide improved treatment for acne.”
One is a cryolysis device that uses cooling to selectively target lipids in the sebaceous glands. (Cryolysis is similar to cryolipolysis, which uses cooling to target fat cells.) The lipid-filled adipocytes are more sensitive to cold than is the water-rich dermis, thereby preserving the surrounding structures. There are also laser wavelengths that are absorbed by lipids, one of which is at about 1720 nm. In this case, heating rather than cooling targets the lipids.
Another technology in development is the use of nanoparticles coated with elements such as gold that are massaged through the skin into the sebaceous glands. Laser treatment with multiple different wavelengths targets the nanoparticles, heating them within the sebaceous glands, resulting in improvements in acne. In this case, treatment does not depend on the absorption spectrum of lipids. Clinical trials of this approach are now underway.
It is too early to tell which of these technologies is going to be effective or what potential side effects may occur. “However, the exciting news is that there will be multiple different technologies” designed to improve acne by targeting the sebaceous gland, and there is “the promise of potentially more effective noninvasive treatments that don’t require topical medications or oral medications,” Dr. Avram said.
For these potential new treatments, some objective outcome measure is needed to judge their efficacy. Right now, all that can be said is that they target the sebaceous gland, and clinical work still needs to be done to determine whether they will be effective, the degree of effectiveness, and how to optimize treatment, he noted.
Dr. Avram reported financial relationships with Cytrellis Biosystems, Invasix, Kythera, Masters of Aesthetics, Sciton, Zalea, and Zeltiq Aesthetics.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
COMFORT mnemonic can help guide malignant wound care
BOSTON – Malignancy in a chronic leg wound can be very aggressive, and multidisciplinary care is a must – particularly in those who oppose amputation, according to Tania J. Phillips, MD.
“When you get a more advanced, malignant, ulcerated wound, this is really a complex situation that requires multidisciplinary care,” she said at the American Academy of Dermatology summer meeting.
In addition to dermatologic care, patients may need medical oncology, surgery, radiation, and good nursing care, she explained.
For patients with malignancy who oppose amputation, a palliative care team may also be a necessity, said Dr. Phillips, professor of dermatology at Boston University. She described one patient she cared for who had an ulcerated wound with squamous cell carcinoma. The patient was treated daily 5 days per week for 2 months. The wound did not heal.
“In these kinds of patients you may not heal the wound; you may just have to try to keep the wound clean, free of pain, and free of infection, she said.
COMFORT is a valuable mnemonic device for caring for such patients, she said: Care for pain and itching, use Odor control, Manage exudate and bleeding, Fight infection, Optimize peri-wound skin integrity, use Reparative and aesthetic wound dressings, Treat the cancer.
Pain is a major issue in patients with such wounds. It is important assess the wound etiology and treat the underlying disease, but it is also important to assess the pain and try to manage it, Dr. Phillips said. Often, addressing local wound management will help with the pain. Appropriate dressing selection is particularly important, as dressing changes can be very painful, she said, recommending the use of non-stick dressings that keep the wound moist. Local and systemic treatment may also be necessary to control pain and itching, she said.
Odor control is another concern. Necrotic tissue has a lot of odor, so debridement can help.
“Use a 19-guage needle to cleanse the wound,” she suggested, noting that this provides higher pressure that can be effective for cleansing.
Dressings that contain nanocrystalline silver or activated charcoal can also help.
As for managing exudate and bleeding, dressing choice is again an important consideration. More absorbent dressings like alginates are useful and have hemostatic properties that can also help with bleeding. Frequent dressing changes are also important.
“And obviously, you want to treat infection,” Dr. Phillips added. Metronidazole gel or powder can help with both infection and odor, she noted.
Peri-wound skin can be very fragile, so it is important to provide protection. In some cases, this can be addressed simply with zinc oxide or petrolatum. Various skin sealants are also available, and can be used to form a barrier to dressings that can be damaging to the skin.
Silicone dressings are very powerful because they don’t stick to the skin, and are not painful or damaging when removed, she said.
The use of a window with hydrocolloid dressing, which allows for changing only the inside of the dressing, is another useful approach, and using mesh rather than tape to hold the dressing in place can help to protect peri-wound skin.
Dr. Phillips reported a financial relationship with Hygeia.
BOSTON – Malignancy in a chronic leg wound can be very aggressive, and multidisciplinary care is a must – particularly in those who oppose amputation, according to Tania J. Phillips, MD.
“When you get a more advanced, malignant, ulcerated wound, this is really a complex situation that requires multidisciplinary care,” she said at the American Academy of Dermatology summer meeting.
In addition to dermatologic care, patients may need medical oncology, surgery, radiation, and good nursing care, she explained.
For patients with malignancy who oppose amputation, a palliative care team may also be a necessity, said Dr. Phillips, professor of dermatology at Boston University. She described one patient she cared for who had an ulcerated wound with squamous cell carcinoma. The patient was treated daily 5 days per week for 2 months. The wound did not heal.
“In these kinds of patients you may not heal the wound; you may just have to try to keep the wound clean, free of pain, and free of infection, she said.
COMFORT is a valuable mnemonic device for caring for such patients, she said: Care for pain and itching, use Odor control, Manage exudate and bleeding, Fight infection, Optimize peri-wound skin integrity, use Reparative and aesthetic wound dressings, Treat the cancer.
Pain is a major issue in patients with such wounds. It is important assess the wound etiology and treat the underlying disease, but it is also important to assess the pain and try to manage it, Dr. Phillips said. Often, addressing local wound management will help with the pain. Appropriate dressing selection is particularly important, as dressing changes can be very painful, she said, recommending the use of non-stick dressings that keep the wound moist. Local and systemic treatment may also be necessary to control pain and itching, she said.
Odor control is another concern. Necrotic tissue has a lot of odor, so debridement can help.
“Use a 19-guage needle to cleanse the wound,” she suggested, noting that this provides higher pressure that can be effective for cleansing.
Dressings that contain nanocrystalline silver or activated charcoal can also help.
As for managing exudate and bleeding, dressing choice is again an important consideration. More absorbent dressings like alginates are useful and have hemostatic properties that can also help with bleeding. Frequent dressing changes are also important.
“And obviously, you want to treat infection,” Dr. Phillips added. Metronidazole gel or powder can help with both infection and odor, she noted.
Peri-wound skin can be very fragile, so it is important to provide protection. In some cases, this can be addressed simply with zinc oxide or petrolatum. Various skin sealants are also available, and can be used to form a barrier to dressings that can be damaging to the skin.
Silicone dressings are very powerful because they don’t stick to the skin, and are not painful or damaging when removed, she said.
The use of a window with hydrocolloid dressing, which allows for changing only the inside of the dressing, is another useful approach, and using mesh rather than tape to hold the dressing in place can help to protect peri-wound skin.
Dr. Phillips reported a financial relationship with Hygeia.
BOSTON – Malignancy in a chronic leg wound can be very aggressive, and multidisciplinary care is a must – particularly in those who oppose amputation, according to Tania J. Phillips, MD.
“When you get a more advanced, malignant, ulcerated wound, this is really a complex situation that requires multidisciplinary care,” she said at the American Academy of Dermatology summer meeting.
In addition to dermatologic care, patients may need medical oncology, surgery, radiation, and good nursing care, she explained.
For patients with malignancy who oppose amputation, a palliative care team may also be a necessity, said Dr. Phillips, professor of dermatology at Boston University. She described one patient she cared for who had an ulcerated wound with squamous cell carcinoma. The patient was treated daily 5 days per week for 2 months. The wound did not heal.
“In these kinds of patients you may not heal the wound; you may just have to try to keep the wound clean, free of pain, and free of infection, she said.
COMFORT is a valuable mnemonic device for caring for such patients, she said: Care for pain and itching, use Odor control, Manage exudate and bleeding, Fight infection, Optimize peri-wound skin integrity, use Reparative and aesthetic wound dressings, Treat the cancer.
Pain is a major issue in patients with such wounds. It is important assess the wound etiology and treat the underlying disease, but it is also important to assess the pain and try to manage it, Dr. Phillips said. Often, addressing local wound management will help with the pain. Appropriate dressing selection is particularly important, as dressing changes can be very painful, she said, recommending the use of non-stick dressings that keep the wound moist. Local and systemic treatment may also be necessary to control pain and itching, she said.
Odor control is another concern. Necrotic tissue has a lot of odor, so debridement can help.
“Use a 19-guage needle to cleanse the wound,” she suggested, noting that this provides higher pressure that can be effective for cleansing.
Dressings that contain nanocrystalline silver or activated charcoal can also help.
As for managing exudate and bleeding, dressing choice is again an important consideration. More absorbent dressings like alginates are useful and have hemostatic properties that can also help with bleeding. Frequent dressing changes are also important.
“And obviously, you want to treat infection,” Dr. Phillips added. Metronidazole gel or powder can help with both infection and odor, she noted.
Peri-wound skin can be very fragile, so it is important to provide protection. In some cases, this can be addressed simply with zinc oxide or petrolatum. Various skin sealants are also available, and can be used to form a barrier to dressings that can be damaging to the skin.
Silicone dressings are very powerful because they don’t stick to the skin, and are not painful or damaging when removed, she said.
The use of a window with hydrocolloid dressing, which allows for changing only the inside of the dressing, is another useful approach, and using mesh rather than tape to hold the dressing in place can help to protect peri-wound skin.
Dr. Phillips reported a financial relationship with Hygeia.
EXPERT ANALYSIS FROM AAD SUMMER ACADEMY 2016
Certain skin cancers respond to nonsurgical treatments
BOSTON – Surgery is the standard of care for most skin cancers, but nonsurgical and adjuvant treatments can be good options for certain skin cancers when surgery would be neither curative nor feasible, according to Anthony Rossi, MD.
“Whether you’re treating a superficial basal cell or superficial squamous cell carcinoma, I think first and foremost, if you’re going to use nonsurgical treatment options, it’s important to have a good biopsy diagnosis,” Dr. Rossi said at the American Academy of Dermatology summer meeting. He also advised that the biopsy capture the entire lesion or a good portion of it to get a good representation. “You don’t want to be surprised by any hiding, high-risk subtypes,” said Dr. Rossi, of the Memorial Sloan Kettering Cancer Center in New York.
Deciding on a nonsurgical treatment option should be based on knowing the patient. For example, know the patient’s concerns about cosmetic deformities, willingness to undergo surgery or not, and ability and willingness to do follow-up self-care.
For superficial basal cell or squamous cell carcinomas in situ and even lentigo maligna in situ not amenable to surgery, imiquimod may be an appropriate treatment. Dr. Rossi said his practice is to use it in an incremental fashion, starting with application five times per week, going to every day if there is no response after 1 to 2 weeks. If the response remains inadequate, he recommended adding a topical retinoid, such as tazarotene, in an effort to increase penetration.
For basal cell carcinomas and squamous cell carcinoma in situ, he uses imiquimod for a total of 6 to 8 weeks, starting from the time of the first reaction. For melanoma in situ, he uses it for more than 60 applications (12 weeks).
To show patients where they should be applying any topical treatment, Dr. Rossi marks the skin, photographs it, and prints out a picture for the patient. Sometimes he uses the patient’s phone to take the picture. For a basal cell or squamous cell carcinoma in situ, he indicates an area at least 5 to 10 mm beyond the margin of the tumor. The area is even larger for melanomas.
Dr. Rossi studies confocal microscopy to detect skin cancers. He uses it before treating a lesion to define the clinical boundaries of the lesion and the boundaries for the nonsurgical treatments, and then he uses it on follow up to look for any recurrences.
New anti-tumor agents
Two oral inhibitors of the sonic hedgehog pathway have been approved within the past 5 years for locally advanced or metastatic basal cell carcinomas. “In the right person, they can be quite beneficial if surgery would leave them with a very large cosmetic deformity or if surgery would be not curative,” Dr. Rossi said. “We’re seeing good results” with acceptable adverse events, specifically taste disturbances, muscle cramps, and hair loss. The first such drug, vismodegib (Erivedge), was approved in 2012, and sonidegib (Odomzo) came on the market about 1 year ago.
Besides oral agents, photodynamic therapy (PDT) with photosensitizers are another option for certain skin tumors. Dr. Rossi said his practice is to keep the treatment room fairly warm to assure good blood flow to the skin and thus good penetration of the drug. Because PDT acts by generating singlet oxygen to kill tumors, good blood flow to the tumor is necessary. To minimize discomfort, he uses pretreatment acetaminophen if patients can take it. After a skin reaction occurs, cool compresses are used, along with dilute acetic acid soaks on crusted or scaling lesions in an effort to prevent infection.
And while these treatments can produce quite angry-looking lesions in the short term, very good healing usually occurs if patients are diligent about wound care. However, Dr. Rossi cautioned that they may need “more hand holding with these nonsurgical treatments, because it is a longer duration of treatment.”
In general for counseling patients on nonsurgical treatments, Dr. Rossi said it is advisable to have good pretreatment and post-treatment plans. “They have to know that they will need to be following up to make sure that there is no recurrence,” he said. “We don’t have clear surgical margins if we’re using these topical treatments, so we have to make sure that they have good, constant follow-up.”
Dr. Rossi reported consulting relationships with Merz, DynaMed, and Novartis.
BOSTON – Surgery is the standard of care for most skin cancers, but nonsurgical and adjuvant treatments can be good options for certain skin cancers when surgery would be neither curative nor feasible, according to Anthony Rossi, MD.
“Whether you’re treating a superficial basal cell or superficial squamous cell carcinoma, I think first and foremost, if you’re going to use nonsurgical treatment options, it’s important to have a good biopsy diagnosis,” Dr. Rossi said at the American Academy of Dermatology summer meeting. He also advised that the biopsy capture the entire lesion or a good portion of it to get a good representation. “You don’t want to be surprised by any hiding, high-risk subtypes,” said Dr. Rossi, of the Memorial Sloan Kettering Cancer Center in New York.
Deciding on a nonsurgical treatment option should be based on knowing the patient. For example, know the patient’s concerns about cosmetic deformities, willingness to undergo surgery or not, and ability and willingness to do follow-up self-care.
For superficial basal cell or squamous cell carcinomas in situ and even lentigo maligna in situ not amenable to surgery, imiquimod may be an appropriate treatment. Dr. Rossi said his practice is to use it in an incremental fashion, starting with application five times per week, going to every day if there is no response after 1 to 2 weeks. If the response remains inadequate, he recommended adding a topical retinoid, such as tazarotene, in an effort to increase penetration.
For basal cell carcinomas and squamous cell carcinoma in situ, he uses imiquimod for a total of 6 to 8 weeks, starting from the time of the first reaction. For melanoma in situ, he uses it for more than 60 applications (12 weeks).
To show patients where they should be applying any topical treatment, Dr. Rossi marks the skin, photographs it, and prints out a picture for the patient. Sometimes he uses the patient’s phone to take the picture. For a basal cell or squamous cell carcinoma in situ, he indicates an area at least 5 to 10 mm beyond the margin of the tumor. The area is even larger for melanomas.
Dr. Rossi studies confocal microscopy to detect skin cancers. He uses it before treating a lesion to define the clinical boundaries of the lesion and the boundaries for the nonsurgical treatments, and then he uses it on follow up to look for any recurrences.
New anti-tumor agents
Two oral inhibitors of the sonic hedgehog pathway have been approved within the past 5 years for locally advanced or metastatic basal cell carcinomas. “In the right person, they can be quite beneficial if surgery would leave them with a very large cosmetic deformity or if surgery would be not curative,” Dr. Rossi said. “We’re seeing good results” with acceptable adverse events, specifically taste disturbances, muscle cramps, and hair loss. The first such drug, vismodegib (Erivedge), was approved in 2012, and sonidegib (Odomzo) came on the market about 1 year ago.
Besides oral agents, photodynamic therapy (PDT) with photosensitizers are another option for certain skin tumors. Dr. Rossi said his practice is to keep the treatment room fairly warm to assure good blood flow to the skin and thus good penetration of the drug. Because PDT acts by generating singlet oxygen to kill tumors, good blood flow to the tumor is necessary. To minimize discomfort, he uses pretreatment acetaminophen if patients can take it. After a skin reaction occurs, cool compresses are used, along with dilute acetic acid soaks on crusted or scaling lesions in an effort to prevent infection.
And while these treatments can produce quite angry-looking lesions in the short term, very good healing usually occurs if patients are diligent about wound care. However, Dr. Rossi cautioned that they may need “more hand holding with these nonsurgical treatments, because it is a longer duration of treatment.”
In general for counseling patients on nonsurgical treatments, Dr. Rossi said it is advisable to have good pretreatment and post-treatment plans. “They have to know that they will need to be following up to make sure that there is no recurrence,” he said. “We don’t have clear surgical margins if we’re using these topical treatments, so we have to make sure that they have good, constant follow-up.”
Dr. Rossi reported consulting relationships with Merz, DynaMed, and Novartis.
BOSTON – Surgery is the standard of care for most skin cancers, but nonsurgical and adjuvant treatments can be good options for certain skin cancers when surgery would be neither curative nor feasible, according to Anthony Rossi, MD.
“Whether you’re treating a superficial basal cell or superficial squamous cell carcinoma, I think first and foremost, if you’re going to use nonsurgical treatment options, it’s important to have a good biopsy diagnosis,” Dr. Rossi said at the American Academy of Dermatology summer meeting. He also advised that the biopsy capture the entire lesion or a good portion of it to get a good representation. “You don’t want to be surprised by any hiding, high-risk subtypes,” said Dr. Rossi, of the Memorial Sloan Kettering Cancer Center in New York.
Deciding on a nonsurgical treatment option should be based on knowing the patient. For example, know the patient’s concerns about cosmetic deformities, willingness to undergo surgery or not, and ability and willingness to do follow-up self-care.
For superficial basal cell or squamous cell carcinomas in situ and even lentigo maligna in situ not amenable to surgery, imiquimod may be an appropriate treatment. Dr. Rossi said his practice is to use it in an incremental fashion, starting with application five times per week, going to every day if there is no response after 1 to 2 weeks. If the response remains inadequate, he recommended adding a topical retinoid, such as tazarotene, in an effort to increase penetration.
For basal cell carcinomas and squamous cell carcinoma in situ, he uses imiquimod for a total of 6 to 8 weeks, starting from the time of the first reaction. For melanoma in situ, he uses it for more than 60 applications (12 weeks).
To show patients where they should be applying any topical treatment, Dr. Rossi marks the skin, photographs it, and prints out a picture for the patient. Sometimes he uses the patient’s phone to take the picture. For a basal cell or squamous cell carcinoma in situ, he indicates an area at least 5 to 10 mm beyond the margin of the tumor. The area is even larger for melanomas.
Dr. Rossi studies confocal microscopy to detect skin cancers. He uses it before treating a lesion to define the clinical boundaries of the lesion and the boundaries for the nonsurgical treatments, and then he uses it on follow up to look for any recurrences.
New anti-tumor agents
Two oral inhibitors of the sonic hedgehog pathway have been approved within the past 5 years for locally advanced or metastatic basal cell carcinomas. “In the right person, they can be quite beneficial if surgery would leave them with a very large cosmetic deformity or if surgery would be not curative,” Dr. Rossi said. “We’re seeing good results” with acceptable adverse events, specifically taste disturbances, muscle cramps, and hair loss. The first such drug, vismodegib (Erivedge), was approved in 2012, and sonidegib (Odomzo) came on the market about 1 year ago.
Besides oral agents, photodynamic therapy (PDT) with photosensitizers are another option for certain skin tumors. Dr. Rossi said his practice is to keep the treatment room fairly warm to assure good blood flow to the skin and thus good penetration of the drug. Because PDT acts by generating singlet oxygen to kill tumors, good blood flow to the tumor is necessary. To minimize discomfort, he uses pretreatment acetaminophen if patients can take it. After a skin reaction occurs, cool compresses are used, along with dilute acetic acid soaks on crusted or scaling lesions in an effort to prevent infection.
And while these treatments can produce quite angry-looking lesions in the short term, very good healing usually occurs if patients are diligent about wound care. However, Dr. Rossi cautioned that they may need “more hand holding with these nonsurgical treatments, because it is a longer duration of treatment.”
In general for counseling patients on nonsurgical treatments, Dr. Rossi said it is advisable to have good pretreatment and post-treatment plans. “They have to know that they will need to be following up to make sure that there is no recurrence,” he said. “We don’t have clear surgical margins if we’re using these topical treatments, so we have to make sure that they have good, constant follow-up.”
Dr. Rossi reported consulting relationships with Merz, DynaMed, and Novartis.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
Perform biopsy in non-healing ulcers
BOSTON – Most ulcers seen in the clinic setting are venous, arterial, or neuropathic, but about 10% are tied to “more unusual causes” and require biopsy, according to Tania J. Phillips, MD.
A particular concern is malignancy, Dr. Phillips, professor of dermatology at Boston University, said at the American Academy of Dermatology summer meeting.
“We do need to have a low threshold for biopsying wounds – particularly if they are wounds of long duration and are not healing,”
A rule of thumb for performing biopsy is 3 months of non-healing, she said.
“If you have a non-healing wound and you’re doing good wound care, you have to re-evaluate. Do you have the right diagnosis? You may need several biopsies on several different occasions to get the right diagnosis,” she said.
Other reasons to biopsy include suspected infection – whether bacterial, fungal, or mycobacterial; atypical appearance; suspected vasculitis; and recent travel history.
Ideally, the biopsy will include a deep wedge containing wound margin and the wound bed.
“Failing that, [take] multiple punch biopsies from the wound bed and the margins,” she said.
While many people are nervous about biopsying an ulcer, most biopsy sites heal very well with no complications, she noted.
As for what to do with the tissue, it can be sent in formalin.
“But if you’re going to do immunofluorescence, you will need Michel’s medium. And if you want to culture, just check with your microbiology lab, because often they will take your piece of tissue and they’ll mix it up, and they’ll divide it and will send it out for bacterial, fungal, mycobacterial culture and you won’t have to do that yourself,” she said.
Dr. Phillips noted that she doesn’t usually suture an ulcer biopsy site.
“The skin around ulcers is usually very friable, the sutures often pull out, and you can usually just pack the biopsy site with gel foam or with an alginate, and then just apply firm compression like a wrap over the biopsy site and you’ll do just fine,” she said.
Dr. Phillips reported a financial relationship with Hygeia.
BOSTON – Most ulcers seen in the clinic setting are venous, arterial, or neuropathic, but about 10% are tied to “more unusual causes” and require biopsy, according to Tania J. Phillips, MD.
A particular concern is malignancy, Dr. Phillips, professor of dermatology at Boston University, said at the American Academy of Dermatology summer meeting.
“We do need to have a low threshold for biopsying wounds – particularly if they are wounds of long duration and are not healing,”
A rule of thumb for performing biopsy is 3 months of non-healing, she said.
“If you have a non-healing wound and you’re doing good wound care, you have to re-evaluate. Do you have the right diagnosis? You may need several biopsies on several different occasions to get the right diagnosis,” she said.
Other reasons to biopsy include suspected infection – whether bacterial, fungal, or mycobacterial; atypical appearance; suspected vasculitis; and recent travel history.
Ideally, the biopsy will include a deep wedge containing wound margin and the wound bed.
“Failing that, [take] multiple punch biopsies from the wound bed and the margins,” she said.
While many people are nervous about biopsying an ulcer, most biopsy sites heal very well with no complications, she noted.
As for what to do with the tissue, it can be sent in formalin.
“But if you’re going to do immunofluorescence, you will need Michel’s medium. And if you want to culture, just check with your microbiology lab, because often they will take your piece of tissue and they’ll mix it up, and they’ll divide it and will send it out for bacterial, fungal, mycobacterial culture and you won’t have to do that yourself,” she said.
Dr. Phillips noted that she doesn’t usually suture an ulcer biopsy site.
“The skin around ulcers is usually very friable, the sutures often pull out, and you can usually just pack the biopsy site with gel foam or with an alginate, and then just apply firm compression like a wrap over the biopsy site and you’ll do just fine,” she said.
Dr. Phillips reported a financial relationship with Hygeia.
BOSTON – Most ulcers seen in the clinic setting are venous, arterial, or neuropathic, but about 10% are tied to “more unusual causes” and require biopsy, according to Tania J. Phillips, MD.
A particular concern is malignancy, Dr. Phillips, professor of dermatology at Boston University, said at the American Academy of Dermatology summer meeting.
“We do need to have a low threshold for biopsying wounds – particularly if they are wounds of long duration and are not healing,”
A rule of thumb for performing biopsy is 3 months of non-healing, she said.
“If you have a non-healing wound and you’re doing good wound care, you have to re-evaluate. Do you have the right diagnosis? You may need several biopsies on several different occasions to get the right diagnosis,” she said.
Other reasons to biopsy include suspected infection – whether bacterial, fungal, or mycobacterial; atypical appearance; suspected vasculitis; and recent travel history.
Ideally, the biopsy will include a deep wedge containing wound margin and the wound bed.
“Failing that, [take] multiple punch biopsies from the wound bed and the margins,” she said.
While many people are nervous about biopsying an ulcer, most biopsy sites heal very well with no complications, she noted.
As for what to do with the tissue, it can be sent in formalin.
“But if you’re going to do immunofluorescence, you will need Michel’s medium. And if you want to culture, just check with your microbiology lab, because often they will take your piece of tissue and they’ll mix it up, and they’ll divide it and will send it out for bacterial, fungal, mycobacterial culture and you won’t have to do that yourself,” she said.
Dr. Phillips noted that she doesn’t usually suture an ulcer biopsy site.
“The skin around ulcers is usually very friable, the sutures often pull out, and you can usually just pack the biopsy site with gel foam or with an alginate, and then just apply firm compression like a wrap over the biopsy site and you’ll do just fine,” she said.
Dr. Phillips reported a financial relationship with Hygeia.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
Skin rash in recent traveler? Think dengue fever
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
Aluminum chloride still helps control hyperhidrosis
BOSTON – Aluminum chloride, a chemical found in rocks and as ancient as the earth itself, still can control hyperhidrosis for many people when used correctly. It is the active ingredient in over-the-counter antiperspirants as well as prescription products.
At the American Academy of Dermatology summer meeting, Louis Kuchnir, MD, who is a physical chemist by training as well as a dermatologist, described the chemical properties of aluminum chloride and how it works, based on those properties.
Just as no dermatologist would prescribe isotretinoin for acne without understanding its mechanism of action, so should physicians know how aluminum chloride works to be able to use it effectively, he said. Each aluminum chloride molecule can covalently bind six water molecules and tightly bind another shell or two of 12-20 molecules, with a further third shell, all “making the water very viscous such that the weak muscles that push sweat out of our sweat glands are unable to move the sweat to the surface of our skin,” he said.
“When aluminum chloride gets close to water, it soaks it up and thickens it,” said Dr. Kuchnir, who is in private practice in Marlborough, Mass. “By spreading it over the areas that perspire, it thickens the water in the top of the duct where the sweat’s coming out, and that thickening, like a gel, will block it.” Most people get satisfactory results for a full day from one application of an antiperspirant containing aluminum chloride. A failure to control sweating results from such excessive sweat gland activity that the moisture pushes the gel away from the top of the sweat gland.
Diagnosis of hyperhidrosis
A diagnosis of primary hyperhidrosis requires focal, visible sweating present for at least 6 months with no apparent secondary causes and at least two of the following criteria:
• It is bilateral and symmetric.
• It impairs activities of daily life.
• There is at least one episode per week.
• The age of onset is less than 25 years.
• There is a positive family history.
• There is cessation during sleep.
Patients whose sweating is not controlled with regular antiperspirant deodorants may find relief using an aluminum chloride–containing liquid that is not a classic deodorant. These products are available over the counter. Beyond that, primary care doctors often prescribe a 20% aluminum chloride liquid, which can be very effective.
If a patient still has hyperhidrosis, often of the axillae or the palms of the hand, a dermatologist may recommend injections of botulinum toxin A “to disable sweat glands up to 10 months at a time ... which is a costly procedure that has been heavily marketed over the past 5-10 years,” Dr. Kuchnir said. By asking patients what they have been using and what the problem is, and understanding why aluminum chloride failed them in the past, he has found that he could get “four out of five of these patients to be happy and not perspiring with topical antiperspirants, often prescription strength, even though virtually all of them are ready to go for neurotoxins when I first meet them.” The remaining 20% will need botulinum toxin A to block nerve endings from communicating with the smooth muscle in the eccrine gland, which is required to push sweat out of the gland.
Botulinum toxin for hyperhidrosis is covered by prescription drug benefit plans, and prior authorization is routine. Patients should obtain the drug at the best price they can find and then bring it to the physician for injection. The duration of action is often 8-10 months, so dosing can be done yearly in the springtime. Aluminum chloride preparations can be retried once botulinum toxin wears off.
Countering common problems with aluminum chloride preparations
The two most common complaints about topical aluminum chloride preparations are that they sting or do not work. Stinging is often from alcohol in the liquids, so letting it evaporate from the armpits before patients put their arms down can solve this problem. As for the problem of not controlling sweating, Dr. Kuchnir said the most common reason is that patients apply the products while they are actively sweating, “so the aluminum chloride doesn’t have time to gel in the eccrine gland.” Another reason is that the preparation has too much moisture in it and will fail to block sweating.
To be able to apply an antiperspirant to dry skin, patients should minimize the causes of sweating by being in a cool, calm environment. The temporary use of anticholinergic drugs may help. Once control of sweating is achieved, the aluminum chloride–containing preparation should be reapplied before it wears off.
Dr. Kuchnir says he encourages dermatologists to bring the same level of care, understanding, and communication to patients suffering from hyperhidrosis that they do to patients whom they see for acne. Just as clinicians do not always use the strongest medicines but choose the safest ones, especially ones that can be self-administered and self-guided, teaching patients how to use antiperspirants when they will work “is as important as being able to effectively and safely inject neurotoxins,” Dr. Kuchnir advised.
While many patients have heard reports of an association between the use of aluminum chloride–containing antiperspirants and a risk of breast cancer or of aluminum in general being associated with Alzheimer’s disease, he says he tells his patients that “aluminum chloride is completely safe, and I don’t say that about a lot of prescription medicines.”
Dr. Kuchnir reported having no financial disclosures.
BOSTON – Aluminum chloride, a chemical found in rocks and as ancient as the earth itself, still can control hyperhidrosis for many people when used correctly. It is the active ingredient in over-the-counter antiperspirants as well as prescription products.
At the American Academy of Dermatology summer meeting, Louis Kuchnir, MD, who is a physical chemist by training as well as a dermatologist, described the chemical properties of aluminum chloride and how it works, based on those properties.
Just as no dermatologist would prescribe isotretinoin for acne without understanding its mechanism of action, so should physicians know how aluminum chloride works to be able to use it effectively, he said. Each aluminum chloride molecule can covalently bind six water molecules and tightly bind another shell or two of 12-20 molecules, with a further third shell, all “making the water very viscous such that the weak muscles that push sweat out of our sweat glands are unable to move the sweat to the surface of our skin,” he said.
“When aluminum chloride gets close to water, it soaks it up and thickens it,” said Dr. Kuchnir, who is in private practice in Marlborough, Mass. “By spreading it over the areas that perspire, it thickens the water in the top of the duct where the sweat’s coming out, and that thickening, like a gel, will block it.” Most people get satisfactory results for a full day from one application of an antiperspirant containing aluminum chloride. A failure to control sweating results from such excessive sweat gland activity that the moisture pushes the gel away from the top of the sweat gland.
Diagnosis of hyperhidrosis
A diagnosis of primary hyperhidrosis requires focal, visible sweating present for at least 6 months with no apparent secondary causes and at least two of the following criteria:
• It is bilateral and symmetric.
• It impairs activities of daily life.
• There is at least one episode per week.
• The age of onset is less than 25 years.
• There is a positive family history.
• There is cessation during sleep.
Patients whose sweating is not controlled with regular antiperspirant deodorants may find relief using an aluminum chloride–containing liquid that is not a classic deodorant. These products are available over the counter. Beyond that, primary care doctors often prescribe a 20% aluminum chloride liquid, which can be very effective.
If a patient still has hyperhidrosis, often of the axillae or the palms of the hand, a dermatologist may recommend injections of botulinum toxin A “to disable sweat glands up to 10 months at a time ... which is a costly procedure that has been heavily marketed over the past 5-10 years,” Dr. Kuchnir said. By asking patients what they have been using and what the problem is, and understanding why aluminum chloride failed them in the past, he has found that he could get “four out of five of these patients to be happy and not perspiring with topical antiperspirants, often prescription strength, even though virtually all of them are ready to go for neurotoxins when I first meet them.” The remaining 20% will need botulinum toxin A to block nerve endings from communicating with the smooth muscle in the eccrine gland, which is required to push sweat out of the gland.
Botulinum toxin for hyperhidrosis is covered by prescription drug benefit plans, and prior authorization is routine. Patients should obtain the drug at the best price they can find and then bring it to the physician for injection. The duration of action is often 8-10 months, so dosing can be done yearly in the springtime. Aluminum chloride preparations can be retried once botulinum toxin wears off.
Countering common problems with aluminum chloride preparations
The two most common complaints about topical aluminum chloride preparations are that they sting or do not work. Stinging is often from alcohol in the liquids, so letting it evaporate from the armpits before patients put their arms down can solve this problem. As for the problem of not controlling sweating, Dr. Kuchnir said the most common reason is that patients apply the products while they are actively sweating, “so the aluminum chloride doesn’t have time to gel in the eccrine gland.” Another reason is that the preparation has too much moisture in it and will fail to block sweating.
To be able to apply an antiperspirant to dry skin, patients should minimize the causes of sweating by being in a cool, calm environment. The temporary use of anticholinergic drugs may help. Once control of sweating is achieved, the aluminum chloride–containing preparation should be reapplied before it wears off.
Dr. Kuchnir says he encourages dermatologists to bring the same level of care, understanding, and communication to patients suffering from hyperhidrosis that they do to patients whom they see for acne. Just as clinicians do not always use the strongest medicines but choose the safest ones, especially ones that can be self-administered and self-guided, teaching patients how to use antiperspirants when they will work “is as important as being able to effectively and safely inject neurotoxins,” Dr. Kuchnir advised.
While many patients have heard reports of an association between the use of aluminum chloride–containing antiperspirants and a risk of breast cancer or of aluminum in general being associated with Alzheimer’s disease, he says he tells his patients that “aluminum chloride is completely safe, and I don’t say that about a lot of prescription medicines.”
Dr. Kuchnir reported having no financial disclosures.
BOSTON – Aluminum chloride, a chemical found in rocks and as ancient as the earth itself, still can control hyperhidrosis for many people when used correctly. It is the active ingredient in over-the-counter antiperspirants as well as prescription products.
At the American Academy of Dermatology summer meeting, Louis Kuchnir, MD, who is a physical chemist by training as well as a dermatologist, described the chemical properties of aluminum chloride and how it works, based on those properties.
Just as no dermatologist would prescribe isotretinoin for acne without understanding its mechanism of action, so should physicians know how aluminum chloride works to be able to use it effectively, he said. Each aluminum chloride molecule can covalently bind six water molecules and tightly bind another shell or two of 12-20 molecules, with a further third shell, all “making the water very viscous such that the weak muscles that push sweat out of our sweat glands are unable to move the sweat to the surface of our skin,” he said.
“When aluminum chloride gets close to water, it soaks it up and thickens it,” said Dr. Kuchnir, who is in private practice in Marlborough, Mass. “By spreading it over the areas that perspire, it thickens the water in the top of the duct where the sweat’s coming out, and that thickening, like a gel, will block it.” Most people get satisfactory results for a full day from one application of an antiperspirant containing aluminum chloride. A failure to control sweating results from such excessive sweat gland activity that the moisture pushes the gel away from the top of the sweat gland.
Diagnosis of hyperhidrosis
A diagnosis of primary hyperhidrosis requires focal, visible sweating present for at least 6 months with no apparent secondary causes and at least two of the following criteria:
• It is bilateral and symmetric.
• It impairs activities of daily life.
• There is at least one episode per week.
• The age of onset is less than 25 years.
• There is a positive family history.
• There is cessation during sleep.
Patients whose sweating is not controlled with regular antiperspirant deodorants may find relief using an aluminum chloride–containing liquid that is not a classic deodorant. These products are available over the counter. Beyond that, primary care doctors often prescribe a 20% aluminum chloride liquid, which can be very effective.
If a patient still has hyperhidrosis, often of the axillae or the palms of the hand, a dermatologist may recommend injections of botulinum toxin A “to disable sweat glands up to 10 months at a time ... which is a costly procedure that has been heavily marketed over the past 5-10 years,” Dr. Kuchnir said. By asking patients what they have been using and what the problem is, and understanding why aluminum chloride failed them in the past, he has found that he could get “four out of five of these patients to be happy and not perspiring with topical antiperspirants, often prescription strength, even though virtually all of them are ready to go for neurotoxins when I first meet them.” The remaining 20% will need botulinum toxin A to block nerve endings from communicating with the smooth muscle in the eccrine gland, which is required to push sweat out of the gland.
Botulinum toxin for hyperhidrosis is covered by prescription drug benefit plans, and prior authorization is routine. Patients should obtain the drug at the best price they can find and then bring it to the physician for injection. The duration of action is often 8-10 months, so dosing can be done yearly in the springtime. Aluminum chloride preparations can be retried once botulinum toxin wears off.
Countering common problems with aluminum chloride preparations
The two most common complaints about topical aluminum chloride preparations are that they sting or do not work. Stinging is often from alcohol in the liquids, so letting it evaporate from the armpits before patients put their arms down can solve this problem. As for the problem of not controlling sweating, Dr. Kuchnir said the most common reason is that patients apply the products while they are actively sweating, “so the aluminum chloride doesn’t have time to gel in the eccrine gland.” Another reason is that the preparation has too much moisture in it and will fail to block sweating.
To be able to apply an antiperspirant to dry skin, patients should minimize the causes of sweating by being in a cool, calm environment. The temporary use of anticholinergic drugs may help. Once control of sweating is achieved, the aluminum chloride–containing preparation should be reapplied before it wears off.
Dr. Kuchnir says he encourages dermatologists to bring the same level of care, understanding, and communication to patients suffering from hyperhidrosis that they do to patients whom they see for acne. Just as clinicians do not always use the strongest medicines but choose the safest ones, especially ones that can be self-administered and self-guided, teaching patients how to use antiperspirants when they will work “is as important as being able to effectively and safely inject neurotoxins,” Dr. Kuchnir advised.
While many patients have heard reports of an association between the use of aluminum chloride–containing antiperspirants and a risk of breast cancer or of aluminum in general being associated with Alzheimer’s disease, he says he tells his patients that “aluminum chloride is completely safe, and I don’t say that about a lot of prescription medicines.”
Dr. Kuchnir reported having no financial disclosures.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016