User login
COLUMBUS, OHIO – Carotid endarterectomy is an effective treatment for people with asymptomatic carotid artery disease when stroke rates are low and they survive long enough to benefit from the treatment. But determining who those patients are can be a challenge for vascular surgeons. A team of vascular specialists from around the country have developed risk prediction models to help surgeons better select asymptomatic patients for the procedure, Randall DeMartino, MD, said at the annual meeting of the Midwestern Vascular Surgical Society.
“These models will be used for mobile apps and web-based applications for point of care patient risk assessment,” said Dr. DeMartino of the Mayo Clinic in Rochester, Minn. He is the lead researcher for the study, which uses data from the Vascular Quality Initiative (VQI).
In developing the models, the researchers sampled asymptomatic patients in the VQI who had first-time elective CEA. There were 31,939 patients in the stroke analysis who had CEA from 2010-2015, and 24,086 patients in the mortality analysis who had procedures from 2010-2014. Dr. DeMartino and his colleagues evaluated all preoperative patient and surgeon characteristics, then used an algorithm to optimize the variables that were selected for the final logistic model.
The researchers also evaluated 30-day stroke rates and 1-year mortality at participating centers and found wide variability: an average of 0.9% for stroke, with a range of 0-8.3%; and 3.2% for mortality, with a range of 0-20%. “Actually, 22% of centers had a 1-year mortality rate that exceeded 5%,” Dr. DeMartino said.
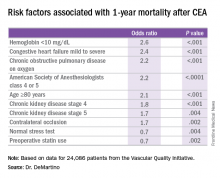
The model for 1-year mortality identified the following variables associated with the highest risk of death 1 year after CEA: age greater than or equal to 80 years; a preoperative hemoglobin less than 10 mg/dL; oxygen-dependent chronic obstructive pulmonary disease; mild to severe congestive heart failure; American Society of Anesthesiologists classification of IV or V; stage 4 or 5 chronic kidney disease; and a contralateral occlusion.
“Conversely, a normal stress test, when performed, and preoperative statin use were associated with reduced risk of death over a year,” Dr. DeMartino said.
“These data have been used to provide Center Opportunity for Improvement reports through VQI where centers can identify if they are selecting patients with risk factors for stroke or mortality more often compared to other centers,” Dr. DeMartino said. “This allows centers to see where opportunities for improvement exist.”
Also, physicians can see the proportion of patients they select with a predicted mortality risk over 5% at one year – “a group of patients who may gain little benefit from prophylactic CEA,” he said. “Physicians can compare their patient selection to those in their region or nationally.”
Dr. DeMartino had no relationships to disclose.
COLUMBUS, OHIO – Carotid endarterectomy is an effective treatment for people with asymptomatic carotid artery disease when stroke rates are low and they survive long enough to benefit from the treatment. But determining who those patients are can be a challenge for vascular surgeons. A team of vascular specialists from around the country have developed risk prediction models to help surgeons better select asymptomatic patients for the procedure, Randall DeMartino, MD, said at the annual meeting of the Midwestern Vascular Surgical Society.
“These models will be used for mobile apps and web-based applications for point of care patient risk assessment,” said Dr. DeMartino of the Mayo Clinic in Rochester, Minn. He is the lead researcher for the study, which uses data from the Vascular Quality Initiative (VQI).
In developing the models, the researchers sampled asymptomatic patients in the VQI who had first-time elective CEA. There were 31,939 patients in the stroke analysis who had CEA from 2010-2015, and 24,086 patients in the mortality analysis who had procedures from 2010-2014. Dr. DeMartino and his colleagues evaluated all preoperative patient and surgeon characteristics, then used an algorithm to optimize the variables that were selected for the final logistic model.
The researchers also evaluated 30-day stroke rates and 1-year mortality at participating centers and found wide variability: an average of 0.9% for stroke, with a range of 0-8.3%; and 3.2% for mortality, with a range of 0-20%. “Actually, 22% of centers had a 1-year mortality rate that exceeded 5%,” Dr. DeMartino said.
The model for 1-year mortality identified the following variables associated with the highest risk of death 1 year after CEA: age greater than or equal to 80 years; a preoperative hemoglobin less than 10 mg/dL; oxygen-dependent chronic obstructive pulmonary disease; mild to severe congestive heart failure; American Society of Anesthesiologists classification of IV or V; stage 4 or 5 chronic kidney disease; and a contralateral occlusion.
“Conversely, a normal stress test, when performed, and preoperative statin use were associated with reduced risk of death over a year,” Dr. DeMartino said.
“These data have been used to provide Center Opportunity for Improvement reports through VQI where centers can identify if they are selecting patients with risk factors for stroke or mortality more often compared to other centers,” Dr. DeMartino said. “This allows centers to see where opportunities for improvement exist.”
Also, physicians can see the proportion of patients they select with a predicted mortality risk over 5% at one year – “a group of patients who may gain little benefit from prophylactic CEA,” he said. “Physicians can compare their patient selection to those in their region or nationally.”
Dr. DeMartino had no relationships to disclose.
COLUMBUS, OHIO – Carotid endarterectomy is an effective treatment for people with asymptomatic carotid artery disease when stroke rates are low and they survive long enough to benefit from the treatment. But determining who those patients are can be a challenge for vascular surgeons. A team of vascular specialists from around the country have developed risk prediction models to help surgeons better select asymptomatic patients for the procedure, Randall DeMartino, MD, said at the annual meeting of the Midwestern Vascular Surgical Society.
“These models will be used for mobile apps and web-based applications for point of care patient risk assessment,” said Dr. DeMartino of the Mayo Clinic in Rochester, Minn. He is the lead researcher for the study, which uses data from the Vascular Quality Initiative (VQI).
In developing the models, the researchers sampled asymptomatic patients in the VQI who had first-time elective CEA. There were 31,939 patients in the stroke analysis who had CEA from 2010-2015, and 24,086 patients in the mortality analysis who had procedures from 2010-2014. Dr. DeMartino and his colleagues evaluated all preoperative patient and surgeon characteristics, then used an algorithm to optimize the variables that were selected for the final logistic model.
The researchers also evaluated 30-day stroke rates and 1-year mortality at participating centers and found wide variability: an average of 0.9% for stroke, with a range of 0-8.3%; and 3.2% for mortality, with a range of 0-20%. “Actually, 22% of centers had a 1-year mortality rate that exceeded 5%,” Dr. DeMartino said.
The model for 1-year mortality identified the following variables associated with the highest risk of death 1 year after CEA: age greater than or equal to 80 years; a preoperative hemoglobin less than 10 mg/dL; oxygen-dependent chronic obstructive pulmonary disease; mild to severe congestive heart failure; American Society of Anesthesiologists classification of IV or V; stage 4 or 5 chronic kidney disease; and a contralateral occlusion.
“Conversely, a normal stress test, when performed, and preoperative statin use were associated with reduced risk of death over a year,” Dr. DeMartino said.
“These data have been used to provide Center Opportunity for Improvement reports through VQI where centers can identify if they are selecting patients with risk factors for stroke or mortality more often compared to other centers,” Dr. DeMartino said. “This allows centers to see where opportunities for improvement exist.”
Also, physicians can see the proportion of patients they select with a predicted mortality risk over 5% at one year – “a group of patients who may gain little benefit from prophylactic CEA,” he said. “Physicians can compare their patient selection to those in their region or nationally.”
Dr. DeMartino had no relationships to disclose.
AT MIDWESTERN VASCULAR 2016
Key clinical point: Risk-prediction models may identify patients at greatest risk of stroke and 1-year death after carotid endarterectomy (CEA).
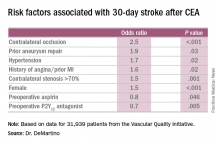
Major finding: Contralateral occlusion has odds ratios of 2.5 for 30-day stroke after CEA and 1.7 for death at 1 year.
Data source: Sampling of patients from the Vascular Quality Initiative who had first-time CEA: 31,939 in the stroke analysis and 24,086 in the mortality analysis.
Disclosures: Dr. DeMartino reported having no financial disclosures.