User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Physicians wearing white coats rated more experienced
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
FROM JAMA NETWORK OPEN
Modest calorie reduction plus exercise linked with improved vascular health
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
Finding applies to seniors with obesity, who were part of a new study
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
FROM CIRCULATION
Even 10 minutes of daily exercise beneficial after ICD implantation
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.
FDA’s fast-track approval process exposed as lax, in need of reform
an in-depth investigation published in The BMJ has determined.
“Despite the pathway’s good intentions to accelerate ‘the availability of drugs that treat serious diseases,’ experts are concerned that it is now being exploited – to the detriment of patients, who may be prescribed a drug that offers little benefit and possible harm, and to taxpayers,” writes Elisabeth Mahase, clinical reporter at The BMJ, who carried out the analysis.
The FDA’s accelerated approval pathway is intended to provide earlier access to drugs for serious diseases when there is lingering uncertainty at the time of approval regarding the drug’s ultimate clinical benefit.
Required studies rarely completed
As part of this fast-track pathway, drug manufacturers must conduct postapproval, phase 4 confirmatory trials to verify the anticipated clinical benefit. If these trials indicate no benefit, FDA approval can be withdrawn.
However, the analysis of FDA data shows once they are approved drugs are rarely taken off the market.
The BMJ investigation that analyzed data up to the end of 2020 shows that 112 of the 253 (44%) medications granted accelerated approval have not been confirmed to be effective.
In addition, 24 (21%) of these questionable drugs have been on the market for more than 5 years and some have been on the market for more than 20 years – often with a hefty price tag.
Furthermore, only 16 drugs approved through the accelerated approval process have ever been withdrawn, and most were shown to be ineffective, but in some cases the confirmatory trials were never done, Ms. Mahase reports.
For example, the COX-2 inhibitor celecoxib (Celebrex), which was granted accelerated approval in 1999 for the treatment of familial adenomatous polyposis, was on the market for 12 years before the FDA finally asked Pfizer to voluntarily withdraw it for this indication because efficacy trials were never completed.
As part of The BMJ’s investigation, Ms. Mahase asked manufacturers of the 24 drugs that have remained on the market for more than 5 years whether they had conducted the required phase 4 confirmatory trials. Six of the drugs had been withdrawn, approved, or postponed.
Of the remaining 18 drugs, the manufacturers provided the relevant trial information for only six. Only four drugmakers had started to recruit patients; two said they were still in discussion with the FDA over the final trial design.
“These products routinely have side effects, but the benefit information is a lot less certain. That’s what we’re concerned about – that we may have drugs on the market that don’t have any benefits, but certainly predictably have harms associated with them,” Huseyin Naci, PhD, MHS, with the London School of Economics, comments in the report.
Call for reform
As reported by this news organization, a 2015 report by the General Accountability Office (GAO) concluded that the FDA does not do an effective job of tracking the clinical efficacy or the safety of drugs with expedited approval after they hit the market.
In April of this year, the Institute for Clinical and Economic Review (ICER) cited a lack of “credible threats” to withdraw approval if companies don’t do confirmatory trials – meaning drugmakers have little incentive to do the trials.
“There are some instances where the companies really do seem to be taking advantage of the accelerated approval pathway and are using it in a way that makes it harder to get at the truth about whether these products really are safe and effective,” Rachel Sachs, JD, MPH, Washington University, St. Louis, said in The BMJ article.
In addition, the authors of a recent viewpoint article in JAMA Internal Medicine assert the recent approval of the controversial anti-amyloid drug aducanumab (Aduhelm, Biogen) shows that the accelerated approval pathway needs to be reformed.
Despite the concerns, Ms. Mahase said all experts who spoke to The BMJ believe the accelerated approval pathway is still useful and can be beneficial to patients, although some changes are needed.
One effective reform might be to have confirmatory trials designed, and even started, as part of accelerated approval.
“One important piece of the puzzle is for the FDA itself to be tougher on these companies, to hold them to the bargain that they have agreed to, and to take action when the company has not met their obligations,” Ms. Sachs told the journal.
An FDA spokesperson told the BMJ that the agency is “committed to working with sponsors to ensure that confirmatory studies are completed in a timely manner.”
“We expect sponsors to commit all resources needed to move trials forward as effectively as possible, with the aim of completing trials as soon as is feasible, while assuring the quality of the data and the robustness of the results,” the agency said.
A version of this article first appeared on Medscape.com.
an in-depth investigation published in The BMJ has determined.
“Despite the pathway’s good intentions to accelerate ‘the availability of drugs that treat serious diseases,’ experts are concerned that it is now being exploited – to the detriment of patients, who may be prescribed a drug that offers little benefit and possible harm, and to taxpayers,” writes Elisabeth Mahase, clinical reporter at The BMJ, who carried out the analysis.
The FDA’s accelerated approval pathway is intended to provide earlier access to drugs for serious diseases when there is lingering uncertainty at the time of approval regarding the drug’s ultimate clinical benefit.
Required studies rarely completed
As part of this fast-track pathway, drug manufacturers must conduct postapproval, phase 4 confirmatory trials to verify the anticipated clinical benefit. If these trials indicate no benefit, FDA approval can be withdrawn.
However, the analysis of FDA data shows once they are approved drugs are rarely taken off the market.
The BMJ investigation that analyzed data up to the end of 2020 shows that 112 of the 253 (44%) medications granted accelerated approval have not been confirmed to be effective.
In addition, 24 (21%) of these questionable drugs have been on the market for more than 5 years and some have been on the market for more than 20 years – often with a hefty price tag.
Furthermore, only 16 drugs approved through the accelerated approval process have ever been withdrawn, and most were shown to be ineffective, but in some cases the confirmatory trials were never done, Ms. Mahase reports.
For example, the COX-2 inhibitor celecoxib (Celebrex), which was granted accelerated approval in 1999 for the treatment of familial adenomatous polyposis, was on the market for 12 years before the FDA finally asked Pfizer to voluntarily withdraw it for this indication because efficacy trials were never completed.
As part of The BMJ’s investigation, Ms. Mahase asked manufacturers of the 24 drugs that have remained on the market for more than 5 years whether they had conducted the required phase 4 confirmatory trials. Six of the drugs had been withdrawn, approved, or postponed.
Of the remaining 18 drugs, the manufacturers provided the relevant trial information for only six. Only four drugmakers had started to recruit patients; two said they were still in discussion with the FDA over the final trial design.
“These products routinely have side effects, but the benefit information is a lot less certain. That’s what we’re concerned about – that we may have drugs on the market that don’t have any benefits, but certainly predictably have harms associated with them,” Huseyin Naci, PhD, MHS, with the London School of Economics, comments in the report.
Call for reform
As reported by this news organization, a 2015 report by the General Accountability Office (GAO) concluded that the FDA does not do an effective job of tracking the clinical efficacy or the safety of drugs with expedited approval after they hit the market.
In April of this year, the Institute for Clinical and Economic Review (ICER) cited a lack of “credible threats” to withdraw approval if companies don’t do confirmatory trials – meaning drugmakers have little incentive to do the trials.
“There are some instances where the companies really do seem to be taking advantage of the accelerated approval pathway and are using it in a way that makes it harder to get at the truth about whether these products really are safe and effective,” Rachel Sachs, JD, MPH, Washington University, St. Louis, said in The BMJ article.
In addition, the authors of a recent viewpoint article in JAMA Internal Medicine assert the recent approval of the controversial anti-amyloid drug aducanumab (Aduhelm, Biogen) shows that the accelerated approval pathway needs to be reformed.
Despite the concerns, Ms. Mahase said all experts who spoke to The BMJ believe the accelerated approval pathway is still useful and can be beneficial to patients, although some changes are needed.
One effective reform might be to have confirmatory trials designed, and even started, as part of accelerated approval.
“One important piece of the puzzle is for the FDA itself to be tougher on these companies, to hold them to the bargain that they have agreed to, and to take action when the company has not met their obligations,” Ms. Sachs told the journal.
An FDA spokesperson told the BMJ that the agency is “committed to working with sponsors to ensure that confirmatory studies are completed in a timely manner.”
“We expect sponsors to commit all resources needed to move trials forward as effectively as possible, with the aim of completing trials as soon as is feasible, while assuring the quality of the data and the robustness of the results,” the agency said.
A version of this article first appeared on Medscape.com.
an in-depth investigation published in The BMJ has determined.
“Despite the pathway’s good intentions to accelerate ‘the availability of drugs that treat serious diseases,’ experts are concerned that it is now being exploited – to the detriment of patients, who may be prescribed a drug that offers little benefit and possible harm, and to taxpayers,” writes Elisabeth Mahase, clinical reporter at The BMJ, who carried out the analysis.
The FDA’s accelerated approval pathway is intended to provide earlier access to drugs for serious diseases when there is lingering uncertainty at the time of approval regarding the drug’s ultimate clinical benefit.
Required studies rarely completed
As part of this fast-track pathway, drug manufacturers must conduct postapproval, phase 4 confirmatory trials to verify the anticipated clinical benefit. If these trials indicate no benefit, FDA approval can be withdrawn.
However, the analysis of FDA data shows once they are approved drugs are rarely taken off the market.
The BMJ investigation that analyzed data up to the end of 2020 shows that 112 of the 253 (44%) medications granted accelerated approval have not been confirmed to be effective.
In addition, 24 (21%) of these questionable drugs have been on the market for more than 5 years and some have been on the market for more than 20 years – often with a hefty price tag.
Furthermore, only 16 drugs approved through the accelerated approval process have ever been withdrawn, and most were shown to be ineffective, but in some cases the confirmatory trials were never done, Ms. Mahase reports.
For example, the COX-2 inhibitor celecoxib (Celebrex), which was granted accelerated approval in 1999 for the treatment of familial adenomatous polyposis, was on the market for 12 years before the FDA finally asked Pfizer to voluntarily withdraw it for this indication because efficacy trials were never completed.
As part of The BMJ’s investigation, Ms. Mahase asked manufacturers of the 24 drugs that have remained on the market for more than 5 years whether they had conducted the required phase 4 confirmatory trials. Six of the drugs had been withdrawn, approved, or postponed.
Of the remaining 18 drugs, the manufacturers provided the relevant trial information for only six. Only four drugmakers had started to recruit patients; two said they were still in discussion with the FDA over the final trial design.
“These products routinely have side effects, but the benefit information is a lot less certain. That’s what we’re concerned about – that we may have drugs on the market that don’t have any benefits, but certainly predictably have harms associated with them,” Huseyin Naci, PhD, MHS, with the London School of Economics, comments in the report.
Call for reform
As reported by this news organization, a 2015 report by the General Accountability Office (GAO) concluded that the FDA does not do an effective job of tracking the clinical efficacy or the safety of drugs with expedited approval after they hit the market.
In April of this year, the Institute for Clinical and Economic Review (ICER) cited a lack of “credible threats” to withdraw approval if companies don’t do confirmatory trials – meaning drugmakers have little incentive to do the trials.
“There are some instances where the companies really do seem to be taking advantage of the accelerated approval pathway and are using it in a way that makes it harder to get at the truth about whether these products really are safe and effective,” Rachel Sachs, JD, MPH, Washington University, St. Louis, said in The BMJ article.
In addition, the authors of a recent viewpoint article in JAMA Internal Medicine assert the recent approval of the controversial anti-amyloid drug aducanumab (Aduhelm, Biogen) shows that the accelerated approval pathway needs to be reformed.
Despite the concerns, Ms. Mahase said all experts who spoke to The BMJ believe the accelerated approval pathway is still useful and can be beneficial to patients, although some changes are needed.
One effective reform might be to have confirmatory trials designed, and even started, as part of accelerated approval.
“One important piece of the puzzle is for the FDA itself to be tougher on these companies, to hold them to the bargain that they have agreed to, and to take action when the company has not met their obligations,” Ms. Sachs told the journal.
An FDA spokesperson told the BMJ that the agency is “committed to working with sponsors to ensure that confirmatory studies are completed in a timely manner.”
“We expect sponsors to commit all resources needed to move trials forward as effectively as possible, with the aim of completing trials as soon as is feasible, while assuring the quality of the data and the robustness of the results,” the agency said.
A version of this article first appeared on Medscape.com.
‘Shocking’ early complications from teen-onset type 2 diabetes
Newly published data show alarmingly high rates and severity of early diabetes-specific complications in individuals who develop type 2 diabetes at a young age. This suggests intervention should be early and aggressive among these youngsters, said the researchers.
The results for the 500 young adult participants in the Treatment Options for Type 2 Diabetes in Adolescents and Youth 2 (TODAY 2) study were published online July 29 in the New England Journal of Medicine by the TODAY study group.
At follow-up – after originally participating in the TODAY trial when they were young teenagers – they had a mean age of 26.4 years.
At this time, more than two thirds had hypertension and half had dyslipidemia.
Overall, 60% had at least one diabetic microvascular complication (retinal disease, neuropathy, or diabetic kidney disease), and more than a quarter had two or more such complications.
“These data illustrate the serious personal and public health consequences of youth-onset type 2 diabetes in the transition to adulthood,” the researchers noted.
Don’t tread lightly just because they are young
“The fact that these youth are accumulating complications at a rapid rate and are broadly affected early in adulthood certainly suggests that aggressive therapy is needed, both for glycemic control and treatment of risk factors like hypertension and dyslipidemia,” study coauthor Philip S. Zeitler, MD, PhD, said in an interview.
“In the absence of studies specifically addressing this, we need to take a more aggressive approach than people might be inclined to, given that the age at diagnosis is young, around 14 years,” he added.
“Contrary to the inclination to be ‘gentle’ in treating them because they are kids, these data suggest that we can’t let these initial years go by without strong intervention, and we need to be prepared for polypharmacy.”
Unfortunately, as Dr. Zeitler and coauthors explained, youth-onset type 2 diabetes is characterized by a suboptimal response to currently approved diabetes medications.
New pediatric indications in the United States for drugs used to treat type 2 diabetes in adults, including the recent Food and Drug Administration approval of extended-release exenatide for children as young as 10 years of age, “helps, but only marginally,” said Dr. Zeitler, of the Clinical & Translational Research Center, Children’s Hospital Colorado, Aurora.
“In some cases, it will help get them covered by carriers, which is always good. But this is still a very limited set of medications. It doesn’t include more recently approved more potent glucagon-like peptide-1 (GLP-1) agonists, like semaglutide, and doesn’t include the sodium-glucose cotransporter 2 (SGLT2) inhibitors. Pediatricians are used to using medications off label and that is necessary here while we await further approvals,” he said.
And he noted that most individuals with youth-onset type 2 diabetes in the United States are covered by public insurance or are uninsured, depending on which state they live in. While the two major Medicaid programs in Colorado allow full access to adult formularies, that’s not the case everywhere. Moreover, patients often face further access barriers in states without expanded Medicaid.
Follow-up shows all metrics worsening over time
In TODAY 2, patients participated in an observational follow-up in their usual care settings in 2011-2020. At the start, they were receiving metformin with or without insulin for diabetes, but whether this continued and whether they were treated for other risk factors was down to individual circumstances.
Participants’ median A1c increased over time, and the percentage with A1c < 6% (< 48 mmol/mol) declined from 75% at the time of TODAY entry to just 19% at the 15-year end of follow-up.
The proportion with an A1c ≤ 10% (≤ 86 mmol/mol) rose from 0% at baseline to 34% at 15 years.
At that time, nearly 50% were taking both metformin and insulin, while more than a quarter were taking no medications.
The prevalence of hypertension increased from 19.2% at baseline to 67.5% at 15 years, while dyslipidemia rose from 20.8% to 51.6%.
Kidney disease prevalence increased from 8.0% at baseline to 54.8% at 15 years. Nerve disease rose from 1.0% to 32.4%. Retinal disease jumped from 13.7% with milder nonproliferative retinopathy in 2010-2011 to 51.0% with any eye disease in 2017-2018, including 8.8% with moderate to severe retinal changes and 3.5% with macular edema.
Overall, at the time of the last visit, 39.9% had no diabetes complications, 31.8% had one, 21.3% had two, and 7.1% had three complications.
Serious cardiovascular events in mid-20s
There were 17 adjudicated serious cardiovascular events, including four myocardial infarctions, six heart failure events, three diagnoses of coronary artery disease, and four strokes.
Six participants died, one each from myocardial infarction, kidney failure, and drug overdose, and three from sepsis.
Dr. Zeitler called the macrovascular events “shocking,” noting that although the numbers are small, for people in their mid-20s “they should be zero ... While we don’t yet know if the rates are the same or faster than in adults, even if they are the same, these kids are only in their late 20s, as opposed to adults experiencing these problems in their 50s, 60s, and 70s.
“The fact that these complications are occurring when these individuals should be in the prime of their life for both family and work has huge implications,” he stressed.
Findings have multiple causes
The reasons for the findings are both biologic and socioeconomic, Dr. Zeitler said.
“We know already that many kids with type 2 have rapid [deterioration of] beta-cell [function], which is probably very biologic. It stands to reason that an individual who can get diabetes as an adolescent probably has more fragile beta cells in some way,” he noted.
“But we also know that many other things contribute: stress, social determinants, access to quality care and medications, access to healthy foods and physical activity, availability of family supervision given the realities of families’ economic status and jobs, etc.”
It’s also known that youth with type 2 diabetes have much more severe insulin resistance than that of adults with the condition, and that “once the kids left ... the [TODAY] study, risk factor treatment in the community was less than ideal, and a lot of kids who met criteria for treatment of their blood pressure or lipids were not being treated. This is likely at least partly sociologic and partly the general pediatric hesitancy to use medications.”
He said the TODAY team will soon have some new data to show that “glycemia during the early years makes a difference, again supporting intensive intervention early on.”
The TODAY study was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Zeitler had no further disclosures.
A version of this article first appeared on Medscape.com.
Newly published data show alarmingly high rates and severity of early diabetes-specific complications in individuals who develop type 2 diabetes at a young age. This suggests intervention should be early and aggressive among these youngsters, said the researchers.
The results for the 500 young adult participants in the Treatment Options for Type 2 Diabetes in Adolescents and Youth 2 (TODAY 2) study were published online July 29 in the New England Journal of Medicine by the TODAY study group.
At follow-up – after originally participating in the TODAY trial when they were young teenagers – they had a mean age of 26.4 years.
At this time, more than two thirds had hypertension and half had dyslipidemia.
Overall, 60% had at least one diabetic microvascular complication (retinal disease, neuropathy, or diabetic kidney disease), and more than a quarter had two or more such complications.
“These data illustrate the serious personal and public health consequences of youth-onset type 2 diabetes in the transition to adulthood,” the researchers noted.
Don’t tread lightly just because they are young
“The fact that these youth are accumulating complications at a rapid rate and are broadly affected early in adulthood certainly suggests that aggressive therapy is needed, both for glycemic control and treatment of risk factors like hypertension and dyslipidemia,” study coauthor Philip S. Zeitler, MD, PhD, said in an interview.
“In the absence of studies specifically addressing this, we need to take a more aggressive approach than people might be inclined to, given that the age at diagnosis is young, around 14 years,” he added.
“Contrary to the inclination to be ‘gentle’ in treating them because they are kids, these data suggest that we can’t let these initial years go by without strong intervention, and we need to be prepared for polypharmacy.”
Unfortunately, as Dr. Zeitler and coauthors explained, youth-onset type 2 diabetes is characterized by a suboptimal response to currently approved diabetes medications.
New pediatric indications in the United States for drugs used to treat type 2 diabetes in adults, including the recent Food and Drug Administration approval of extended-release exenatide for children as young as 10 years of age, “helps, but only marginally,” said Dr. Zeitler, of the Clinical & Translational Research Center, Children’s Hospital Colorado, Aurora.
“In some cases, it will help get them covered by carriers, which is always good. But this is still a very limited set of medications. It doesn’t include more recently approved more potent glucagon-like peptide-1 (GLP-1) agonists, like semaglutide, and doesn’t include the sodium-glucose cotransporter 2 (SGLT2) inhibitors. Pediatricians are used to using medications off label and that is necessary here while we await further approvals,” he said.
And he noted that most individuals with youth-onset type 2 diabetes in the United States are covered by public insurance or are uninsured, depending on which state they live in. While the two major Medicaid programs in Colorado allow full access to adult formularies, that’s not the case everywhere. Moreover, patients often face further access barriers in states without expanded Medicaid.
Follow-up shows all metrics worsening over time
In TODAY 2, patients participated in an observational follow-up in their usual care settings in 2011-2020. At the start, they were receiving metformin with or without insulin for diabetes, but whether this continued and whether they were treated for other risk factors was down to individual circumstances.
Participants’ median A1c increased over time, and the percentage with A1c < 6% (< 48 mmol/mol) declined from 75% at the time of TODAY entry to just 19% at the 15-year end of follow-up.
The proportion with an A1c ≤ 10% (≤ 86 mmol/mol) rose from 0% at baseline to 34% at 15 years.
At that time, nearly 50% were taking both metformin and insulin, while more than a quarter were taking no medications.
The prevalence of hypertension increased from 19.2% at baseline to 67.5% at 15 years, while dyslipidemia rose from 20.8% to 51.6%.
Kidney disease prevalence increased from 8.0% at baseline to 54.8% at 15 years. Nerve disease rose from 1.0% to 32.4%. Retinal disease jumped from 13.7% with milder nonproliferative retinopathy in 2010-2011 to 51.0% with any eye disease in 2017-2018, including 8.8% with moderate to severe retinal changes and 3.5% with macular edema.
Overall, at the time of the last visit, 39.9% had no diabetes complications, 31.8% had one, 21.3% had two, and 7.1% had three complications.
Serious cardiovascular events in mid-20s
There were 17 adjudicated serious cardiovascular events, including four myocardial infarctions, six heart failure events, three diagnoses of coronary artery disease, and four strokes.
Six participants died, one each from myocardial infarction, kidney failure, and drug overdose, and three from sepsis.
Dr. Zeitler called the macrovascular events “shocking,” noting that although the numbers are small, for people in their mid-20s “they should be zero ... While we don’t yet know if the rates are the same or faster than in adults, even if they are the same, these kids are only in their late 20s, as opposed to adults experiencing these problems in their 50s, 60s, and 70s.
“The fact that these complications are occurring when these individuals should be in the prime of their life for both family and work has huge implications,” he stressed.
Findings have multiple causes
The reasons for the findings are both biologic and socioeconomic, Dr. Zeitler said.
“We know already that many kids with type 2 have rapid [deterioration of] beta-cell [function], which is probably very biologic. It stands to reason that an individual who can get diabetes as an adolescent probably has more fragile beta cells in some way,” he noted.
“But we also know that many other things contribute: stress, social determinants, access to quality care and medications, access to healthy foods and physical activity, availability of family supervision given the realities of families’ economic status and jobs, etc.”
It’s also known that youth with type 2 diabetes have much more severe insulin resistance than that of adults with the condition, and that “once the kids left ... the [TODAY] study, risk factor treatment in the community was less than ideal, and a lot of kids who met criteria for treatment of their blood pressure or lipids were not being treated. This is likely at least partly sociologic and partly the general pediatric hesitancy to use medications.”
He said the TODAY team will soon have some new data to show that “glycemia during the early years makes a difference, again supporting intensive intervention early on.”
The TODAY study was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Zeitler had no further disclosures.
A version of this article first appeared on Medscape.com.
Newly published data show alarmingly high rates and severity of early diabetes-specific complications in individuals who develop type 2 diabetes at a young age. This suggests intervention should be early and aggressive among these youngsters, said the researchers.
The results for the 500 young adult participants in the Treatment Options for Type 2 Diabetes in Adolescents and Youth 2 (TODAY 2) study were published online July 29 in the New England Journal of Medicine by the TODAY study group.
At follow-up – after originally participating in the TODAY trial when they were young teenagers – they had a mean age of 26.4 years.
At this time, more than two thirds had hypertension and half had dyslipidemia.
Overall, 60% had at least one diabetic microvascular complication (retinal disease, neuropathy, or diabetic kidney disease), and more than a quarter had two or more such complications.
“These data illustrate the serious personal and public health consequences of youth-onset type 2 diabetes in the transition to adulthood,” the researchers noted.
Don’t tread lightly just because they are young
“The fact that these youth are accumulating complications at a rapid rate and are broadly affected early in adulthood certainly suggests that aggressive therapy is needed, both for glycemic control and treatment of risk factors like hypertension and dyslipidemia,” study coauthor Philip S. Zeitler, MD, PhD, said in an interview.
“In the absence of studies specifically addressing this, we need to take a more aggressive approach than people might be inclined to, given that the age at diagnosis is young, around 14 years,” he added.
“Contrary to the inclination to be ‘gentle’ in treating them because they are kids, these data suggest that we can’t let these initial years go by without strong intervention, and we need to be prepared for polypharmacy.”
Unfortunately, as Dr. Zeitler and coauthors explained, youth-onset type 2 diabetes is characterized by a suboptimal response to currently approved diabetes medications.
New pediatric indications in the United States for drugs used to treat type 2 diabetes in adults, including the recent Food and Drug Administration approval of extended-release exenatide for children as young as 10 years of age, “helps, but only marginally,” said Dr. Zeitler, of the Clinical & Translational Research Center, Children’s Hospital Colorado, Aurora.
“In some cases, it will help get them covered by carriers, which is always good. But this is still a very limited set of medications. It doesn’t include more recently approved more potent glucagon-like peptide-1 (GLP-1) agonists, like semaglutide, and doesn’t include the sodium-glucose cotransporter 2 (SGLT2) inhibitors. Pediatricians are used to using medications off label and that is necessary here while we await further approvals,” he said.
And he noted that most individuals with youth-onset type 2 diabetes in the United States are covered by public insurance or are uninsured, depending on which state they live in. While the two major Medicaid programs in Colorado allow full access to adult formularies, that’s not the case everywhere. Moreover, patients often face further access barriers in states without expanded Medicaid.
Follow-up shows all metrics worsening over time
In TODAY 2, patients participated in an observational follow-up in their usual care settings in 2011-2020. At the start, they were receiving metformin with or without insulin for diabetes, but whether this continued and whether they were treated for other risk factors was down to individual circumstances.
Participants’ median A1c increased over time, and the percentage with A1c < 6% (< 48 mmol/mol) declined from 75% at the time of TODAY entry to just 19% at the 15-year end of follow-up.
The proportion with an A1c ≤ 10% (≤ 86 mmol/mol) rose from 0% at baseline to 34% at 15 years.
At that time, nearly 50% were taking both metformin and insulin, while more than a quarter were taking no medications.
The prevalence of hypertension increased from 19.2% at baseline to 67.5% at 15 years, while dyslipidemia rose from 20.8% to 51.6%.
Kidney disease prevalence increased from 8.0% at baseline to 54.8% at 15 years. Nerve disease rose from 1.0% to 32.4%. Retinal disease jumped from 13.7% with milder nonproliferative retinopathy in 2010-2011 to 51.0% with any eye disease in 2017-2018, including 8.8% with moderate to severe retinal changes and 3.5% with macular edema.
Overall, at the time of the last visit, 39.9% had no diabetes complications, 31.8% had one, 21.3% had two, and 7.1% had three complications.
Serious cardiovascular events in mid-20s
There were 17 adjudicated serious cardiovascular events, including four myocardial infarctions, six heart failure events, three diagnoses of coronary artery disease, and four strokes.
Six participants died, one each from myocardial infarction, kidney failure, and drug overdose, and three from sepsis.
Dr. Zeitler called the macrovascular events “shocking,” noting that although the numbers are small, for people in their mid-20s “they should be zero ... While we don’t yet know if the rates are the same or faster than in adults, even if they are the same, these kids are only in their late 20s, as opposed to adults experiencing these problems in their 50s, 60s, and 70s.
“The fact that these complications are occurring when these individuals should be in the prime of their life for both family and work has huge implications,” he stressed.
Findings have multiple causes
The reasons for the findings are both biologic and socioeconomic, Dr. Zeitler said.
“We know already that many kids with type 2 have rapid [deterioration of] beta-cell [function], which is probably very biologic. It stands to reason that an individual who can get diabetes as an adolescent probably has more fragile beta cells in some way,” he noted.
“But we also know that many other things contribute: stress, social determinants, access to quality care and medications, access to healthy foods and physical activity, availability of family supervision given the realities of families’ economic status and jobs, etc.”
It’s also known that youth with type 2 diabetes have much more severe insulin resistance than that of adults with the condition, and that “once the kids left ... the [TODAY] study, risk factor treatment in the community was less than ideal, and a lot of kids who met criteria for treatment of their blood pressure or lipids were not being treated. This is likely at least partly sociologic and partly the general pediatric hesitancy to use medications.”
He said the TODAY team will soon have some new data to show that “glycemia during the early years makes a difference, again supporting intensive intervention early on.”
The TODAY study was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Zeitler had no further disclosures.
A version of this article first appeared on Medscape.com.
COVID-19 leaves wake of medical debt among U.S. adults
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
ESC heart failure guideline to integrate bounty of new meds
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.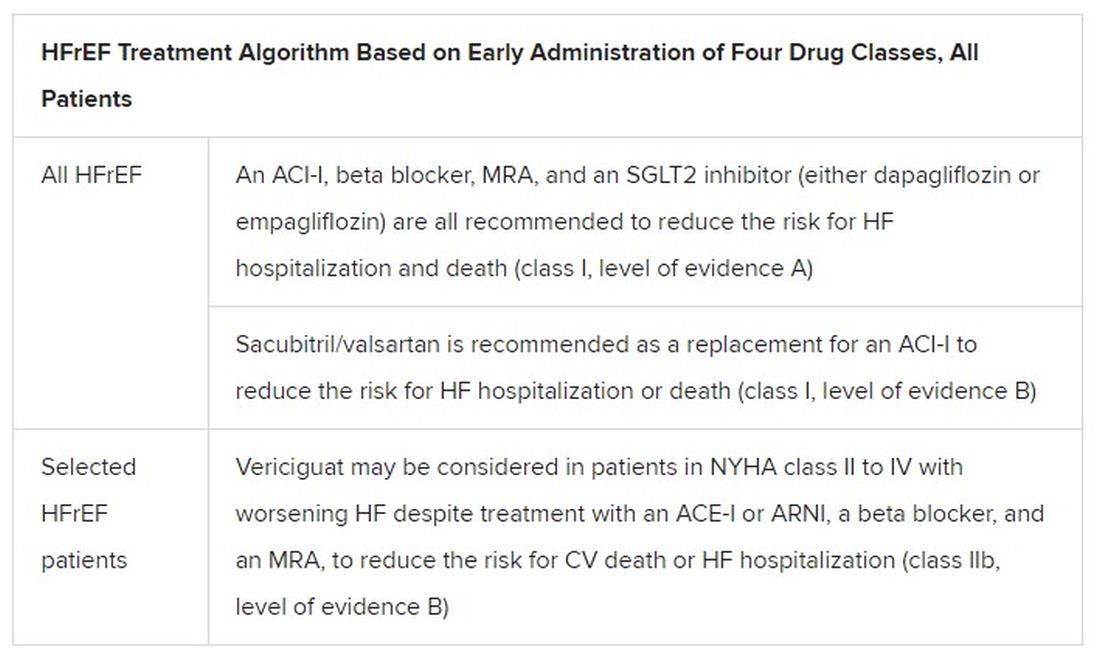
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
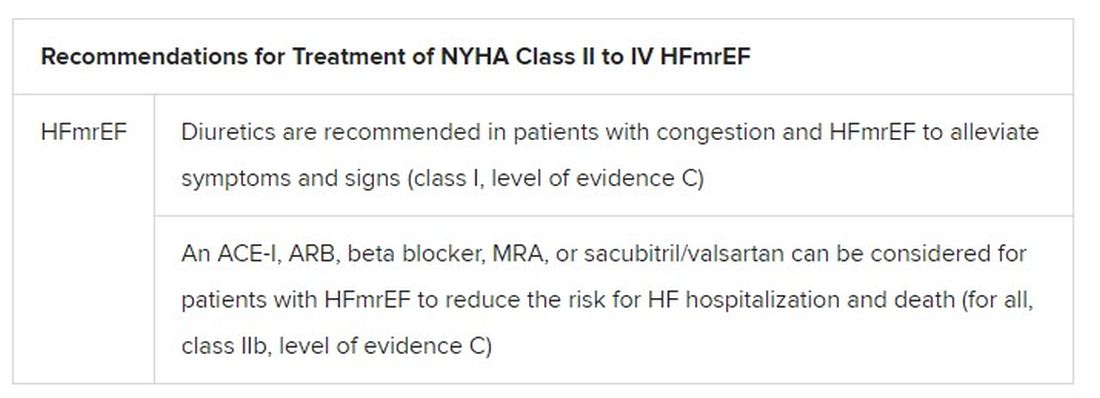
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.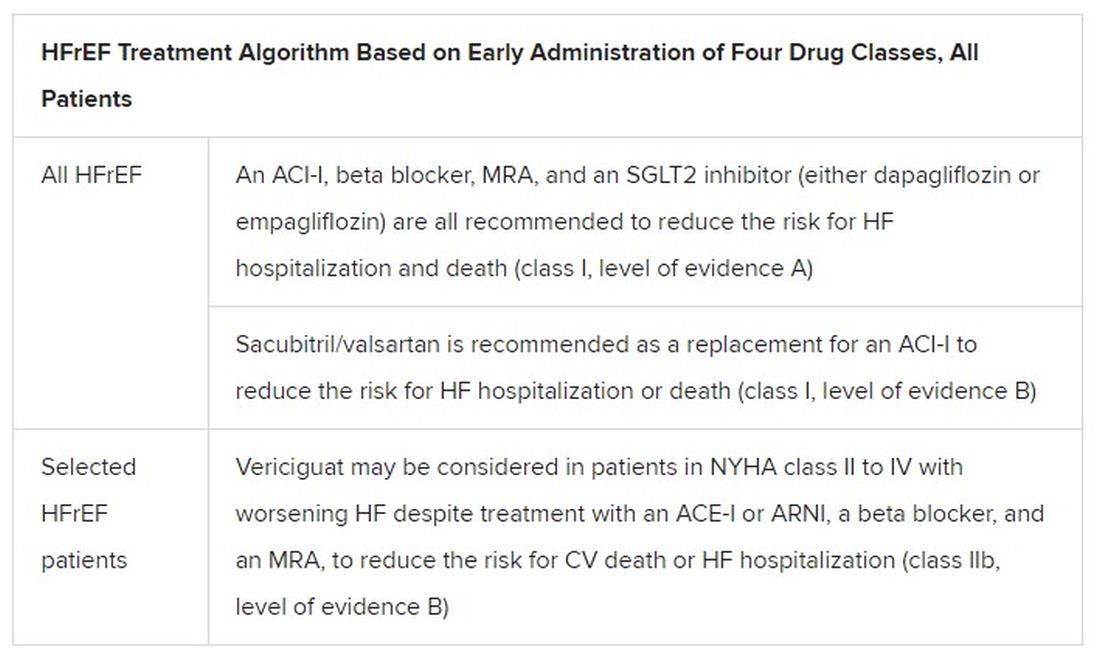
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
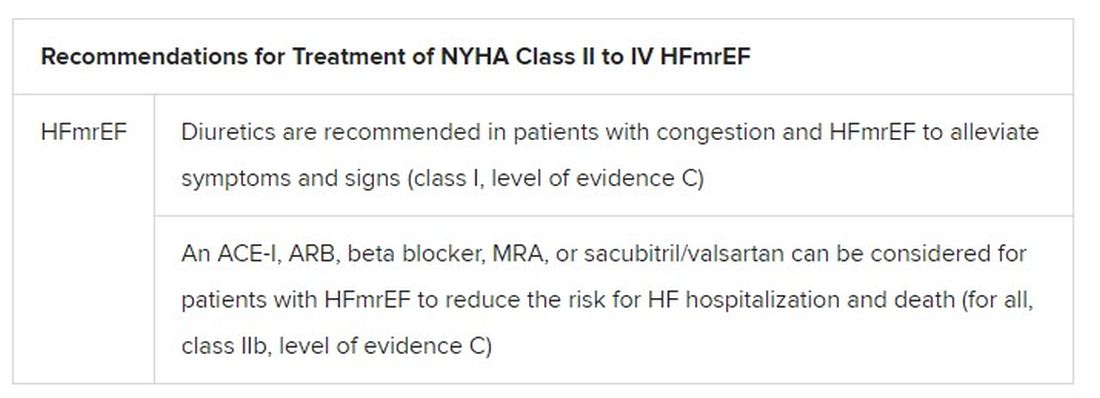
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.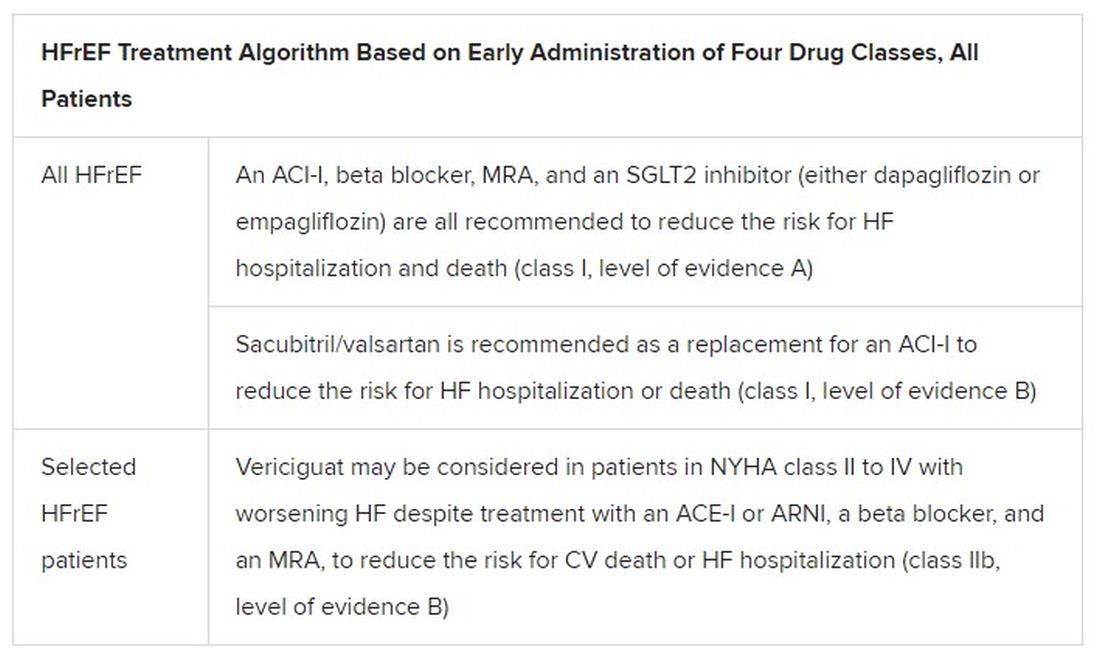
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
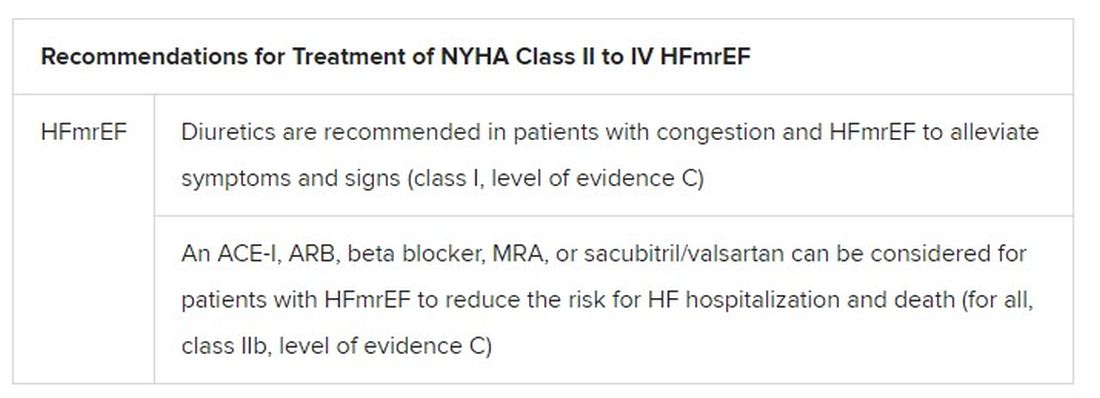
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
FDA approves first interchangeable biosimilar insulin
The
The approval will allow Semglee to function like a generic drug in the market and may reduce insulin costs.
It is indicated to improve glycemic control in adults and pediatric patients with type 1 diabetes and in adults with type 2 diabetes.
Originally approved in June 2020 as a biosimilar to glargine, Semglee is now an “interchangeable biosimilar,” meaning that it has no clinically meaningful difference from the reference product and also may be substituted for that product – in this case, glargine (Lantus) – without prescriber intervention, just as generic drugs typically are, subject to state pharmacy laws.
For approval as an interchangeable biosimilar, manufacturers are required to provide additional data reflecting how the interchangeable biosimilar may be used in the marketplace with patients.
“Biosimilar and interchangeable biosimilar products have the potential to reduce health care costs, similar to how generic drugs have reduced costs. Biosimilars marketed in the U.S. typically have launched with initial list prices 15% to 35% lower than comparative list prices of the reference products,” the FDA said in a statement.
Semglee comes in 10-mL and 3-mL prefilled pens, and is administered subcutaneously once daily, with individualized doses. The most common side effects are hypoglycemia, edema, lipodystrophy, weight gain, and allergic reactions.
The FDA released new materials for health care providers regarding biosimilar and interchangeable biosimilar products, including a fact sheet about interchangeable biosimilar products.
A version of this article first appeared on Medscape.com.
The
The approval will allow Semglee to function like a generic drug in the market and may reduce insulin costs.
It is indicated to improve glycemic control in adults and pediatric patients with type 1 diabetes and in adults with type 2 diabetes.
Originally approved in June 2020 as a biosimilar to glargine, Semglee is now an “interchangeable biosimilar,” meaning that it has no clinically meaningful difference from the reference product and also may be substituted for that product – in this case, glargine (Lantus) – without prescriber intervention, just as generic drugs typically are, subject to state pharmacy laws.
For approval as an interchangeable biosimilar, manufacturers are required to provide additional data reflecting how the interchangeable biosimilar may be used in the marketplace with patients.
“Biosimilar and interchangeable biosimilar products have the potential to reduce health care costs, similar to how generic drugs have reduced costs. Biosimilars marketed in the U.S. typically have launched with initial list prices 15% to 35% lower than comparative list prices of the reference products,” the FDA said in a statement.
Semglee comes in 10-mL and 3-mL prefilled pens, and is administered subcutaneously once daily, with individualized doses. The most common side effects are hypoglycemia, edema, lipodystrophy, weight gain, and allergic reactions.
The FDA released new materials for health care providers regarding biosimilar and interchangeable biosimilar products, including a fact sheet about interchangeable biosimilar products.
A version of this article first appeared on Medscape.com.
The
The approval will allow Semglee to function like a generic drug in the market and may reduce insulin costs.
It is indicated to improve glycemic control in adults and pediatric patients with type 1 diabetes and in adults with type 2 diabetes.
Originally approved in June 2020 as a biosimilar to glargine, Semglee is now an “interchangeable biosimilar,” meaning that it has no clinically meaningful difference from the reference product and also may be substituted for that product – in this case, glargine (Lantus) – without prescriber intervention, just as generic drugs typically are, subject to state pharmacy laws.
For approval as an interchangeable biosimilar, manufacturers are required to provide additional data reflecting how the interchangeable biosimilar may be used in the marketplace with patients.
“Biosimilar and interchangeable biosimilar products have the potential to reduce health care costs, similar to how generic drugs have reduced costs. Biosimilars marketed in the U.S. typically have launched with initial list prices 15% to 35% lower than comparative list prices of the reference products,” the FDA said in a statement.
Semglee comes in 10-mL and 3-mL prefilled pens, and is administered subcutaneously once daily, with individualized doses. The most common side effects are hypoglycemia, edema, lipodystrophy, weight gain, and allergic reactions.
The FDA released new materials for health care providers regarding biosimilar and interchangeable biosimilar products, including a fact sheet about interchangeable biosimilar products.
A version of this article first appeared on Medscape.com.
PCPs lag on albuminuria tests in patients with type 2 diabetes
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
FROM DIABETES CARE
Money buys life, and a cigarette maker wants to ‘unsmoke the world’
With COVID, the fun never ends
Welcome to America’s favorite pandemic-themed game show! Let’s play Covidiot Proof! And now, here’s your host, the lovely and talented Anthony Grouchy!
Tony: Hello everyone! Our first category today is America or [blank], and the first clue is for you, Don. This country requires “individuals to use a health pass to patronize indoor establishments such as restaurants, bars, nightclubs and cinemas.”
Don: Freedom-loving Americans would never stand for that, Tony, so I’m going to say Greece.
Tony: That’s correct, Don. One hundred points for you. Okay Joe, here’s your clue: In this country, some people wear disguises to get a COVID vaccination so their friends and families won’t find out.
Joe: Sounds like communism to me, Tony. I’ll say Cuba.
Tony: Sorry Joe, that’s incorrect. Don?
Don: The friends and families sound like freedom-loving Americans, so it must be America.
Tony: It is America. Missouri, to be exact. And now, one last question for both of you to win the game. True or false? Did the pastor of a church in Tennessee say that mask-wearers would be kicked out of the building because “I am not playing these Democrat games up in this church”?
Joe: That’s fake news, Tony. It’s gotta be false.
Tony: Incorrect! It’s absolutely true. That means today’s winner is … Joe? Yes, I’m being told that Tennessee goes to Joe.
Don: That’s bulls#&@! I won this thing! I’ll see you in court!
More money, more life
Does it seem to you that the wealthy live forever, while the less financially comfortable live shorter lives? If you answered, yes, it turns out that you’re right.
Researchers analyzed the effect of net worth at midlife with mortality. To take out genetic differences among the sample of 5,400 adults aged 46 years, the investigators also studied a subset of 2,490 twin and sibling pairs.
“The within-family association provides strong evidence that an association between wealth accumulation and life expectancy exists, because comparing siblings within the same family to each other controls for all of the life experience and biology that they share,” said coauthor Eric Finegood of Northwestern University, Chicago.
But what if one sibling has a history of cancer, heart disease, or other health conditions? The cost of treatment and employment limitations could affect someone’s ability to stack their wealth, right? Absolutely. The researchers took that into account and looked at only healthy individuals and found the same results. More money, longer life.
We have the policies and programs in place for heart health, diabetes prevention, and smoking cessation, as they are seen as major threats to public health. So why not do the same for financial security? A low bank account may just be more harmful.
Holding the ‘health care and wellness’ gun
Cigarettes are not good for us. We know this.
It’s, therefore, not surprising to learn that a business has requested for a U.K. ban on the sale of cigarettes by 2030. However, when that someone turns out to be the CEO of Philip Morris International, tobacco company and maker of Marlboro cigarettes, things get a little confusing.
Banning cigarettes, according to Jacek Olczak, would reduce confusion among consumers, many of whom feel that the alternatives are worse for their health. His company can “see the world without cigarettes ... and actually, the sooner it happens, the better it is for everyone.” A truly noble sentiment from the CEO of a large tobacco company. Nothing nefarious going on here.
And if those aren’t egregious business euphemisms, we don’t know what is.
Of course, for all the completely believable and sincere rhetoric, the fact is that Marlboros are still on the shelves. Philip Morris is still making and advertising them. If their concern was genuine, why wouldn’t they just stop manufacturing them now?
So, we ask ourselves if this a selfless act of kindness or is it an unscrupulous corporate act to get a leg up on their competitors? We’ll leave it up to the readers to decide.
Okay, we lied, it’s the second one.
Autopsy of the living dead
Imagine the absolute terror you’d feel if you opened your eyes to bright, blinding white lights only to see a bone saw 3 inches from your forehead and getting closer by the second. Horrifying for you, certainly, but think about the poor pathologist behind the saw who probably thought a zombie apocalypse was coming. This was close to being a reality for a 29-year-old prisoner at the Asturias Central Penitentiary in Spain.
Gonzalo Montoya Jiménez was discovered in his cell unresponsive. Three physicians examined him and found he was showing signs of death, such as cyanosis and rigor mortis. Mr. Jiménez was processed like any other body and was sent, in a body bag, to a hospital mortuary, where he spent time in a freezer for body preservation. Just before he was due for his autopsy, he began showing signs of life.
It’s not completely clear why this happened to poor Mr. Jiménez, but it was reported that he wasn’t feeling well the day before and that he has epilepsy. Hospital officials suggested he may have been cataleptic, possibly because he had trouble adhering to his medication schedule.
Mr. Jiménez was moved to another hospital under armed guard after coming back to life and regained consciousness after a day or so. Talk about cheating death.
With COVID, the fun never ends
Welcome to America’s favorite pandemic-themed game show! Let’s play Covidiot Proof! And now, here’s your host, the lovely and talented Anthony Grouchy!
Tony: Hello everyone! Our first category today is America or [blank], and the first clue is for you, Don. This country requires “individuals to use a health pass to patronize indoor establishments such as restaurants, bars, nightclubs and cinemas.”
Don: Freedom-loving Americans would never stand for that, Tony, so I’m going to say Greece.
Tony: That’s correct, Don. One hundred points for you. Okay Joe, here’s your clue: In this country, some people wear disguises to get a COVID vaccination so their friends and families won’t find out.
Joe: Sounds like communism to me, Tony. I’ll say Cuba.
Tony: Sorry Joe, that’s incorrect. Don?
Don: The friends and families sound like freedom-loving Americans, so it must be America.
Tony: It is America. Missouri, to be exact. And now, one last question for both of you to win the game. True or false? Did the pastor of a church in Tennessee say that mask-wearers would be kicked out of the building because “I am not playing these Democrat games up in this church”?
Joe: That’s fake news, Tony. It’s gotta be false.
Tony: Incorrect! It’s absolutely true. That means today’s winner is … Joe? Yes, I’m being told that Tennessee goes to Joe.
Don: That’s bulls#&@! I won this thing! I’ll see you in court!
More money, more life
Does it seem to you that the wealthy live forever, while the less financially comfortable live shorter lives? If you answered, yes, it turns out that you’re right.
Researchers analyzed the effect of net worth at midlife with mortality. To take out genetic differences among the sample of 5,400 adults aged 46 years, the investigators also studied a subset of 2,490 twin and sibling pairs.
“The within-family association provides strong evidence that an association between wealth accumulation and life expectancy exists, because comparing siblings within the same family to each other controls for all of the life experience and biology that they share,” said coauthor Eric Finegood of Northwestern University, Chicago.
But what if one sibling has a history of cancer, heart disease, or other health conditions? The cost of treatment and employment limitations could affect someone’s ability to stack their wealth, right? Absolutely. The researchers took that into account and looked at only healthy individuals and found the same results. More money, longer life.
We have the policies and programs in place for heart health, diabetes prevention, and smoking cessation, as they are seen as major threats to public health. So why not do the same for financial security? A low bank account may just be more harmful.
Holding the ‘health care and wellness’ gun
Cigarettes are not good for us. We know this.
It’s, therefore, not surprising to learn that a business has requested for a U.K. ban on the sale of cigarettes by 2030. However, when that someone turns out to be the CEO of Philip Morris International, tobacco company and maker of Marlboro cigarettes, things get a little confusing.
Banning cigarettes, according to Jacek Olczak, would reduce confusion among consumers, many of whom feel that the alternatives are worse for their health. His company can “see the world without cigarettes ... and actually, the sooner it happens, the better it is for everyone.” A truly noble sentiment from the CEO of a large tobacco company. Nothing nefarious going on here.
And if those aren’t egregious business euphemisms, we don’t know what is.
Of course, for all the completely believable and sincere rhetoric, the fact is that Marlboros are still on the shelves. Philip Morris is still making and advertising them. If their concern was genuine, why wouldn’t they just stop manufacturing them now?
So, we ask ourselves if this a selfless act of kindness or is it an unscrupulous corporate act to get a leg up on their competitors? We’ll leave it up to the readers to decide.
Okay, we lied, it’s the second one.
Autopsy of the living dead
Imagine the absolute terror you’d feel if you opened your eyes to bright, blinding white lights only to see a bone saw 3 inches from your forehead and getting closer by the second. Horrifying for you, certainly, but think about the poor pathologist behind the saw who probably thought a zombie apocalypse was coming. This was close to being a reality for a 29-year-old prisoner at the Asturias Central Penitentiary in Spain.
Gonzalo Montoya Jiménez was discovered in his cell unresponsive. Three physicians examined him and found he was showing signs of death, such as cyanosis and rigor mortis. Mr. Jiménez was processed like any other body and was sent, in a body bag, to a hospital mortuary, where he spent time in a freezer for body preservation. Just before he was due for his autopsy, he began showing signs of life.
It’s not completely clear why this happened to poor Mr. Jiménez, but it was reported that he wasn’t feeling well the day before and that he has epilepsy. Hospital officials suggested he may have been cataleptic, possibly because he had trouble adhering to his medication schedule.
Mr. Jiménez was moved to another hospital under armed guard after coming back to life and regained consciousness after a day or so. Talk about cheating death.
With COVID, the fun never ends
Welcome to America’s favorite pandemic-themed game show! Let’s play Covidiot Proof! And now, here’s your host, the lovely and talented Anthony Grouchy!
Tony: Hello everyone! Our first category today is America or [blank], and the first clue is for you, Don. This country requires “individuals to use a health pass to patronize indoor establishments such as restaurants, bars, nightclubs and cinemas.”
Don: Freedom-loving Americans would never stand for that, Tony, so I’m going to say Greece.
Tony: That’s correct, Don. One hundred points for you. Okay Joe, here’s your clue: In this country, some people wear disguises to get a COVID vaccination so their friends and families won’t find out.
Joe: Sounds like communism to me, Tony. I’ll say Cuba.
Tony: Sorry Joe, that’s incorrect. Don?
Don: The friends and families sound like freedom-loving Americans, so it must be America.
Tony: It is America. Missouri, to be exact. And now, one last question for both of you to win the game. True or false? Did the pastor of a church in Tennessee say that mask-wearers would be kicked out of the building because “I am not playing these Democrat games up in this church”?
Joe: That’s fake news, Tony. It’s gotta be false.
Tony: Incorrect! It’s absolutely true. That means today’s winner is … Joe? Yes, I’m being told that Tennessee goes to Joe.
Don: That’s bulls#&@! I won this thing! I’ll see you in court!
More money, more life
Does it seem to you that the wealthy live forever, while the less financially comfortable live shorter lives? If you answered, yes, it turns out that you’re right.
Researchers analyzed the effect of net worth at midlife with mortality. To take out genetic differences among the sample of 5,400 adults aged 46 years, the investigators also studied a subset of 2,490 twin and sibling pairs.
“The within-family association provides strong evidence that an association between wealth accumulation and life expectancy exists, because comparing siblings within the same family to each other controls for all of the life experience and biology that they share,” said coauthor Eric Finegood of Northwestern University, Chicago.
But what if one sibling has a history of cancer, heart disease, or other health conditions? The cost of treatment and employment limitations could affect someone’s ability to stack their wealth, right? Absolutely. The researchers took that into account and looked at only healthy individuals and found the same results. More money, longer life.
We have the policies and programs in place for heart health, diabetes prevention, and smoking cessation, as they are seen as major threats to public health. So why not do the same for financial security? A low bank account may just be more harmful.
Holding the ‘health care and wellness’ gun
Cigarettes are not good for us. We know this.
It’s, therefore, not surprising to learn that a business has requested for a U.K. ban on the sale of cigarettes by 2030. However, when that someone turns out to be the CEO of Philip Morris International, tobacco company and maker of Marlboro cigarettes, things get a little confusing.
Banning cigarettes, according to Jacek Olczak, would reduce confusion among consumers, many of whom feel that the alternatives are worse for their health. His company can “see the world without cigarettes ... and actually, the sooner it happens, the better it is for everyone.” A truly noble sentiment from the CEO of a large tobacco company. Nothing nefarious going on here.
And if those aren’t egregious business euphemisms, we don’t know what is.
Of course, for all the completely believable and sincere rhetoric, the fact is that Marlboros are still on the shelves. Philip Morris is still making and advertising them. If their concern was genuine, why wouldn’t they just stop manufacturing them now?
So, we ask ourselves if this a selfless act of kindness or is it an unscrupulous corporate act to get a leg up on their competitors? We’ll leave it up to the readers to decide.
Okay, we lied, it’s the second one.
Autopsy of the living dead
Imagine the absolute terror you’d feel if you opened your eyes to bright, blinding white lights only to see a bone saw 3 inches from your forehead and getting closer by the second. Horrifying for you, certainly, but think about the poor pathologist behind the saw who probably thought a zombie apocalypse was coming. This was close to being a reality for a 29-year-old prisoner at the Asturias Central Penitentiary in Spain.
Gonzalo Montoya Jiménez was discovered in his cell unresponsive. Three physicians examined him and found he was showing signs of death, such as cyanosis and rigor mortis. Mr. Jiménez was processed like any other body and was sent, in a body bag, to a hospital mortuary, where he spent time in a freezer for body preservation. Just before he was due for his autopsy, he began showing signs of life.
It’s not completely clear why this happened to poor Mr. Jiménez, but it was reported that he wasn’t feeling well the day before and that he has epilepsy. Hospital officials suggested he may have been cataleptic, possibly because he had trouble adhering to his medication schedule.
Mr. Jiménez was moved to another hospital under armed guard after coming back to life and regained consciousness after a day or so. Talk about cheating death.












