User login
AGA issues position statements on reducing CRC burden
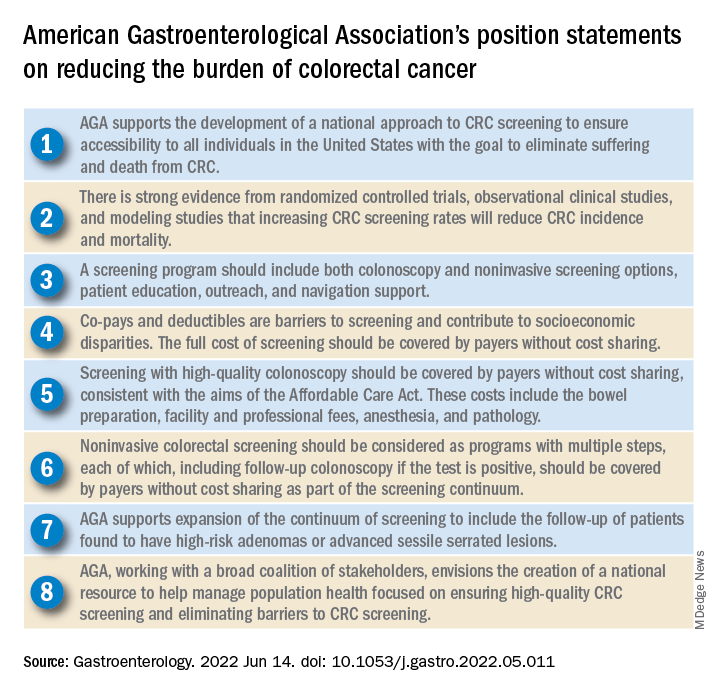
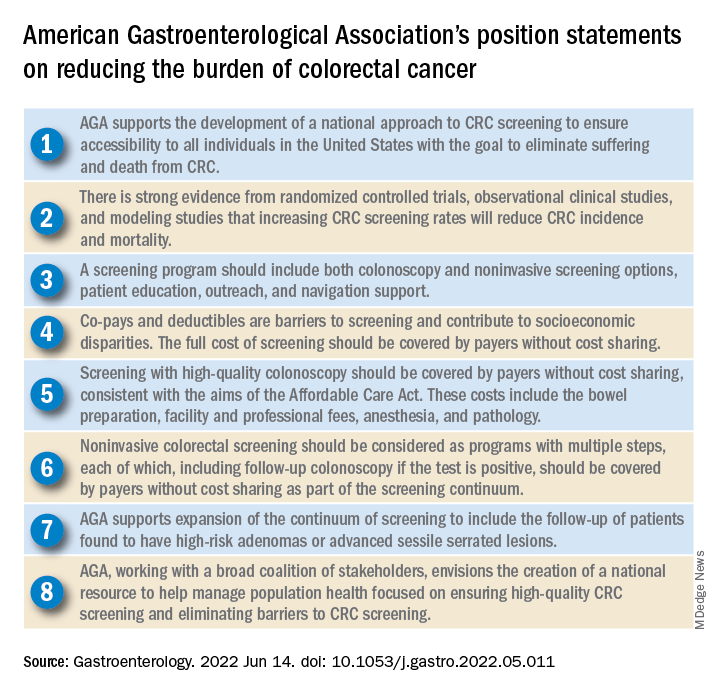
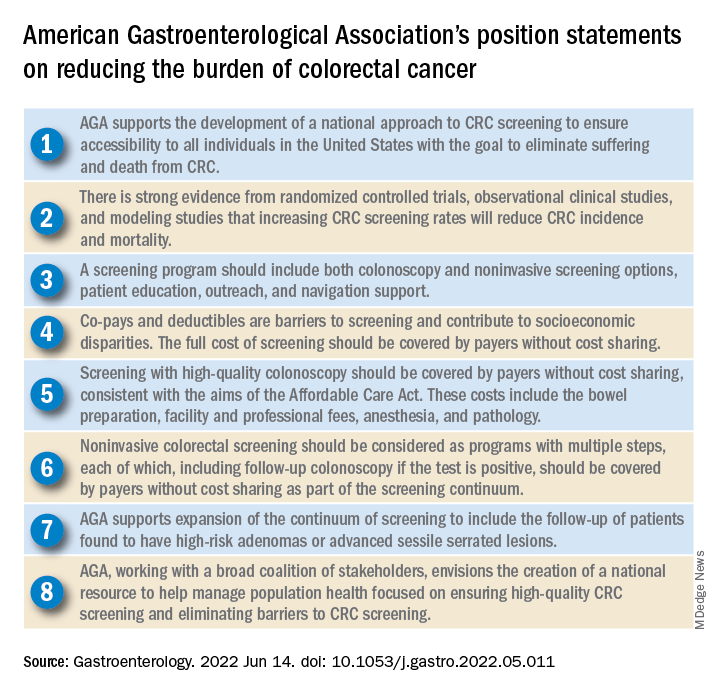
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
The American Gastroenterological Association has published eight position statements aimed at reducing the burden of colorectal cancer (CRC).
The evidence-based statements, published in Gastroenterology, call for a national approach to CRC screening, outline the elements of a high-quality screening program, and make clear that payers should cover all costs, from bowel prep through pathology, plus follow-up for high-risk patients.
“There is strong evidence that CRC screening is effective [at reducing CRC incidence and mortality] ... but less than 70% of eligible individuals have been screened,” wrote authors led by David Lieberman, MD, who is on the AGA Executive Committee on the Screening Continuum and affiliated with Oregon Health and Science University, Portland, noting the recent expansion of eligibility to include individuals in the 45- to 49-year age group.
“CRC screening saves lives, but only if people get screened,” Dr. Lieberman said in a press release from the AGA. “Cost sharing is an important barrier to screening, which contributes to racial, ethnic and socioeconomic inequities in colorectal cancer outcomes. The full cost of screening – including noninvasive tests and follow-up colonoscopies – should be covered without cost to patients.”
He added: “AGA wishes to collaborate with stakeholders to eliminate obstacles to screening, which disproportionately impact those with low income and lack of insurance.”
Eliminating disparities in screening
Among the position statements, Dr. Lieberman and colleagues first called for “development of a national approach to CRC screening” to patch gaps in access across the United States.
“Systematic outreach occurs infrequently,” they noted. “CRC screening prevalence is much lower among individuals who do not have access to health care due to lack of insurance, do not have a primary care provider, or are part of a medically underserved community.”
According to Dr. Lieberman and colleagues, the AGA is also “working with a broad coalition of stakeholders,” such as the American Cancer Society, payers, patient advocacy groups, and others, to create a “national resource ... focused on ensuring high-quality CRC screening and eliminating barriers to CRC screening.”
Specifically, the coalition will work to collectively tackle “disparities created by social determinants of health, which includes lack of access to screening, transportation, and even work hours and child care.
“The AGA recognizes that moving the needle to achieve a CRC screening participation goal of 80% will take a village,” they wrote.
Elements of high-quality CRC screening
The investigators went on to describe the key features of a high-quality CRC screening program, including “colonoscopy and noninvasive screening options, patient education, outreach, and navigation support.”
Dr. Lieberman and colleagues pointed out that offering more than one type of screening test “acknowledges patient preferences and improves participation.”
Certain noninvasive methods, such as fecal immunochemical testing (FIT), eliminate “important barriers” to screening, they noted, such as the need for special preparation, time off work, and transportation to a medical facility.
For individuals who have high-risk adenomas (HRAs) or advanced sessile serrated lesions (SSLs), screening should be expanded to include follow-up, the investigators added.
“Evidence from a systematic review demonstrates that individuals with HRAs at baseline have a 3- to 4-fold higher risk of incident CRC during follow-up compared with individuals with no adenoma or low-risk adenomas,” they wrote. “There is also evidence that individuals with advanced SSLs have a three= to fourfold higher risk of CRC, compared with individuals with nonadvanced SSLs.”
Payers should cover costs
To further improve access to care, payers should cover the full costs of CRC screening because “copays and deductibles are barriers to screening and contribute to socioeconomic disparities,” that “disproportionately impact those with low income and lack of insurance,” according to Dr. Lieberman and colleagues.
They noted that the Affordable Care Act “eliminated copayments for preventive services,” yet a recent study showed that almost half of patients with commercial insurance and more than three-quarters of patients with Medicare still share some cost of CRC screening.
The investigators made clear that payers need to cover costs from start to finish, including “bowel preparation, facility and professional fees, anesthesia, and pathology,” as well as follow-up screening for high-risk patients identified by noninvasive methods.
“Noninvasive colorectal screening should be considered as programs with multiple steps, each of which, including follow-up colonoscopy if the test is positive, should be covered by payers without cost sharing as part of the screening continuum,” Dr. Lieberman and colleagues wrote.
Changes underway
According to Steven Itzkowitz, MD, professor of medicine and oncological sciences and director of the gastroenterology fellowship training program at the Icahn School of Medicine at Mount Sinai, New York, the AGA publication is important because it “consolidates many of the critical issues related to decreasing the burden of colorectal cancer in the United States.”
Dr. Itzkowitz noted that changes are already underway to eliminate cost as a barrier to screening.
“The good news is that, in the past year, the Departments of Health & Human Services, Labor, and Treasury declared that cost sharing should not be imposed, and plans are required to cover screening colonoscopy with polyp removal and colonoscopy that is performed to follow-up after an abnormal noninvasive CRC screening test,” Dr. Itzkowitz said in an interview. “Many plans are following suit, but it will take time for this coverage to take effect across all plans.”
For individual gastroenterologists who would like to do their part in reducing screening inequity, Dr. Itzkowitz suggested leveraging noninvasive testing, as the AGA recommends.
“This publication is the latest to call for using noninvasive, stool-based testing in addition to colonoscopy,” Dr. Itzkowitz said. “FIT and multitarget stool DNA tests all have proven efficacy in this regard, so gastroenterologists should have those conversations with their patients. GIs can also make it easier for patients to complete colonoscopy by developing patient navigation programs, direct access referrals, and systems for communicating with primary care providers for easier referrals and communicating colonoscopy results.”
Many practices are already instituting such improvements in response to the restrictions imposed by the COVID-19 pandemic, according to Dr. Itzkowitz.“These changes, plus better coverage by payers, will make a huge impact on health equity when it comes to colorectal cancer screening.”
The publication was supported by the AGA. The investigators disclosed relationships with Geneoscopy, ColoWrap, UniversalDx, and others. Dr. Itzkowitz disclosed no relevant conflicts of interest.
FROM GASTROENTEROLOGY
Cannabis may relieve pain as effectively as opioids, but more research is needed
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
Several other systematic reviews have recently evaluated cannabinoids for treating chronic pain, but the new study’s methodology was “distinct” in “important ways,” leading to “conclusions that differ from other reviews,” according to the authors of the paper published in the Annals of Internal Medicine.
In the new systematic review, synthetic products with high THC:CBD ratios were associated with moderate improvements in pain, whereas plant-based products with comparable THC:CBD ratios offered less relief, said study author Marian S. McDonagh, PharmD, professor of medical informatics and clinical epidemiology, and codirector of the Evidence-based Practice Center at Oregon Health & Science University, Portland, and colleagues.
Specifically, the investigators stratified cannabis-based interventions according to relative content of two key cannabinoids: THC and CBD. Products were sorted into five categories: high THC:CBD ratio (at least 2:1), comparable THC:CBD ratio (less than 2:1 but more than 1:2), low THC:CBD ratio (no more than 1:2), whole-plant cannabis products, and other cannabinoids.
“In preclinical studies, THC and related compounds have demonstrated analgesic properties, although its psychoactive effects and addiction potential may limit its suitability as an analgesic,” the investigators wrote. “CBD and other cannabinoids may also have some analgesic or anti-inflammatory properties and are not believed to be psychoactive or addictive. Given the variation in analgesic effect with THC and CBD, response may differ according to the ratio of THC to CBD in products used to treat pain.”
The final analysis included 18 randomized placebo-controlled trials involving 1,740 individuals and 7 cohort studies involving 13,095 individuals. Most of the studies were short-term, lasting 1-6 months.
Pain was scored on a ten-point scale, with improvements reported as the mean difference from baseline to post treatment. A mean difference in pain score of 0.5-1.0 was considered a “small effect,” an improvement of 1-2 points was considered a “moderate effect,” and an improvement greater than 2 points was considered a “large effect.”
Cannabis-based products with relatively high THC:CBD ratios showed efficacy
Synthetic products with high THC:CBD ratios offered moderate pain relief, based on a mean difference in pain score of –1.15 (95% confidence interval, –1.99 to –0.54), whereas products with comparable THC:CBD ratios were associated with a small effect on pain, with a mean difference of –0.52 (95% CI, –0.95 to –0.19).
According to Dr. McDonagh, treatment response rates were on par with response rates for more conventional treatments, “such as opioids or specific antidepressant drugs,” but data for the cannabis-based products are weaker.
“The amount of evidence available for cannabis-related products is very limited for [response rates], and therefore less certain,” Dr. McDonagh said in an interview. “The average reduction in pain severity is also similar to some other treatments, but we do not have studies directly comparing these treatments to draw conclusions.”
Although the cannabis-based products with relatively high and comparable THC:CBD ratios showed efficacy, they were also associated with “moderate to large increased risk for dizziness, sedation, and nausea,” the investigators wrote, noting that evidence was insufficient to characterize other “key adverse event outcomes” that may occur with long-term use, such as “psychosis, cannabis use disorder, and cognitive deficits.”
For products with low THC:CBD ratios, or without reported THC:CBD ratios, data were too scarce to reach any conclusions at all about safety or efficacy, highlighting the sizable knowledge gaps that remain in the area, the authors said.
“The current evidence on cannabis-related products for chronic pain is quite limited,” Dr. McDonagh said in an interview. “Patients with chronic pain should consult with their doctor to discuss which of the many options for treating chronic pain is best for them to start with.”
Patients may face resistance when asking about cannabis
According to Kevin F. Boehnke, PhD, and Daniel J. Clauw, MD, of the anesthesiology department and Chronic Pain and Fatigue Research Center at the University of Michigan, Ann Arbor, patients with chronic pain may face resistance, or even risk of being reported, when asking about cannabis-based products.
“Some physicians cite lack of data as rationale for not engaging with patients who wish to use or currently use cannabis,” Dr. Boehnke and Dr. Clauw wrote in an accompanying editorial. “Such practices may reflect consideration of cannabis solely as a drug of misuse (even in the 37 states where medical cannabis is legal) and requirements to refer patients who disclose or test positive for cannabis use to addiction services or decline to refill opioid prescriptions.”
Instead of shutting patients out, Dr. Boehnke and Dr. Clauw suggested clinicians engage in an “open information exchange” with their patients that focuses on “pragmatism, patient experience, known cannabinoid effects, and harm reduction.” In these conversations, the editorialists recommend noting that, “as with other analgesics, some persons will benefit, and others will not.”
They also offered some practical guidance: “Clinicians could suggest using tinctures (effect onset, 15-45 minutes) for breakthrough pain and edibles or capsules (which last about 6-8 hours) for extended relief. ... The scientific literature suggests that CBD doses could start at 5-10 mg twice daily and increase to 40-50 mg daily, whereas THC doses could start at 0.5-3 mg (initially at night) and increase to 30-40 mg/day.”
David Copenhaver, MD, MPH, clinical professor and chief of the division of pain medicine at UC Davis Health, Sacramento, shared a similar clinical mindset for patients choosing between opioids and cannabis-based products, specifically, CBD.
Compared with opioids, “the side-effect profile for CBD is less and the risk of mortality is less,” Dr. Copenhaver said in an interview, pointing out that nobody, to his knowledge, has ever died from an overdose of cannabis alone, and that CBD doses up to 1,000 mg/kg have been safely tolerated in people. “You present that, and most patients will say, ‘You know, I’d like to give this a try.’”
If so, Dr. Copenhaver makes sure patients know about a nonmedical risk: “The risk to the pocketbook.” Unlike opioids, which are covered under most insurance policies, most cannabis-based therapies are self-pay.
Buyers may get what they pay for, Dr. Copenhaver said, since products vary in quality, as do the dispensaries, from “very modest,” to highly sophisticated, with some even using chromatographic datasets to support the purity of their products.
Dr. Copenhaver steers his patients toward these more sophisticated retailers. Their expertise appears to be paying off, he said, not only in relief for patients, but also in market share. “Survival of the most fit will occur in the marketplace based on the results,” he said. “Unfortunately, some of that information doesn’t get percolated out into the literature.”
For investigators to fully uncover what cannabis-based products can do for chronic pain, Dr. Copenhaver said they need to get as “granular” as the leading dispensaries, which may first require recognition of the “very expansive opportunity” that less-studied cannabinoids may provide.
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators, Dr. Boehnke, Dr. Clauw, and Dr. Copenhaver, disclosed no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Blood-based assay may offer new way of diagnosing Parkinson’s disease
A novel blood-based assay could one day be used to diagnose Parkinson’s disease and possibly other chronic inflammatory conditions, according to investigators. In addition to being highly accurate, the assay, which detects changes in expression of cytochrome P450s, is faster and easier to perform than other Parkinson’s disease assays under investigation, reported lead author Kohei Ihara, PhD, of Kobe University, Japan, and colleagues.
“Effective diagnostic systems and biomarkers for patients without subjective motor symptoms have not yet been established,” the investigators wrote in Nature Scientific Reports. “Consequently, the poor diagnostic options for Parkinson’s disease delay the development of therapeutic approaches and medication. Therefore, the development of efficient diagnostic systems and biomarkers is crucial for overcoming Parkinson’s disease.”
According to Dr. Ihara and colleagues, various cytochrome P450 expression patterns and associated serum metabolites correlate with chronic conditions, making them possible markers of disease. To detect these changes, they developed the present assay. It relies upon recombinant P450s expressed on the surface of Escherichia coli. By mixing the E. coli with serum and Vivid, a fluorescent substrate, the investigators can measure “the inhibition rate of the Vivid decomposition reaction” that was driven by “serum metabolites associated with P450s,” revealing underlying expression and, if present, disease.
After some promising initial experiments with mouse models of ulcerative colitis and diabetes, Dr. Ihara and colleagues focused on a rat model of Parkinson’s disease. Evaluating inhibition rates associated with four P450s revealed area-under-the-curve (AUC) values of 0.814-0.914. Two of those P450s were also associated with progression of disease symptoms.
“Therefore, we concluded that the P450 inhibition assay could discriminate between Parkinson’s disease model rats and control rats,” the investigators wrote.
Next, the investigators tested the approach with a case-control study involving 20 patients with Parkinson’s disease and 20 healthy volunteers. Twelve P450s were analyzed, three of which revealed significant differences between patients with Parkinson’s disease and controls, with AUCs ranging from 0.740-0.775. Each of the three P450 enzymes also correlated significantly with stage of disease on the Hoehn & Yahr scale, although severity and frequency of symptoms were not reported.
To increase accuracy of the technique, the investigators developed a logistic regression model using two of the three P450s, generating an AUC of 0.910. Further testing showed that the P450 inhibition assay could distinguish between patients with Parkinson’s disease and Alzheimer’s disease, as well as other chronic inflammatory diseases.
“The P450 inhibition assay is easier to perform and is faster than other assays because this assay does not require pretreatment, such as purification of exosomes, and it involves a single enzymatic reaction,” the investigators wrote, suggesting that the assay may be suitable for real-world diagnosis.
‘Promising’ findings need replication
According to Douglas Galasko, MD, a neurologist and professor of neurosciences at UC San Diego Health, the reported accuracy of the assay “seems spectacular,” and the findings are “promising,” but they need to be replicated, “particularly in early-stage patients where the diagnosis [of Parkinson’s disease] is more difficult and important to make.” In practice, the assay would likely see greatest usage for “early diagnosis or diagnosis of unusual or challenging cases,” so accuracy testing needs to be conducted in this setting, he said.
Dr. Galasko, who was not involved in the study, predicted that liquid biopsy for detecting Parkinson’s disease is unlikely to hit the clinic floor anytime soon. “We’re not really close with blood-based biomarkers for Parkinson’s disease,” he said, “unlike the situation for Alzheimer’s disease, where there are several promising blood-based biomarkers.”
For diagnosing Parkinson’s disease, Dr. Galasko suggested that assays using skin biopsies to measure alpha-synuclein accumulation may be closer to approval.
The study was supported by JSPS KAKENHI Grant Number 20K20223 and the Sumitomo Electric Industries Group Corporate Social Responsibility Foundation. The investigators disclosed no conflicts of interest.
A novel blood-based assay could one day be used to diagnose Parkinson’s disease and possibly other chronic inflammatory conditions, according to investigators. In addition to being highly accurate, the assay, which detects changes in expression of cytochrome P450s, is faster and easier to perform than other Parkinson’s disease assays under investigation, reported lead author Kohei Ihara, PhD, of Kobe University, Japan, and colleagues.
“Effective diagnostic systems and biomarkers for patients without subjective motor symptoms have not yet been established,” the investigators wrote in Nature Scientific Reports. “Consequently, the poor diagnostic options for Parkinson’s disease delay the development of therapeutic approaches and medication. Therefore, the development of efficient diagnostic systems and biomarkers is crucial for overcoming Parkinson’s disease.”
According to Dr. Ihara and colleagues, various cytochrome P450 expression patterns and associated serum metabolites correlate with chronic conditions, making them possible markers of disease. To detect these changes, they developed the present assay. It relies upon recombinant P450s expressed on the surface of Escherichia coli. By mixing the E. coli with serum and Vivid, a fluorescent substrate, the investigators can measure “the inhibition rate of the Vivid decomposition reaction” that was driven by “serum metabolites associated with P450s,” revealing underlying expression and, if present, disease.
After some promising initial experiments with mouse models of ulcerative colitis and diabetes, Dr. Ihara and colleagues focused on a rat model of Parkinson’s disease. Evaluating inhibition rates associated with four P450s revealed area-under-the-curve (AUC) values of 0.814-0.914. Two of those P450s were also associated with progression of disease symptoms.
“Therefore, we concluded that the P450 inhibition assay could discriminate between Parkinson’s disease model rats and control rats,” the investigators wrote.
Next, the investigators tested the approach with a case-control study involving 20 patients with Parkinson’s disease and 20 healthy volunteers. Twelve P450s were analyzed, three of which revealed significant differences between patients with Parkinson’s disease and controls, with AUCs ranging from 0.740-0.775. Each of the three P450 enzymes also correlated significantly with stage of disease on the Hoehn & Yahr scale, although severity and frequency of symptoms were not reported.
To increase accuracy of the technique, the investigators developed a logistic regression model using two of the three P450s, generating an AUC of 0.910. Further testing showed that the P450 inhibition assay could distinguish between patients with Parkinson’s disease and Alzheimer’s disease, as well as other chronic inflammatory diseases.
“The P450 inhibition assay is easier to perform and is faster than other assays because this assay does not require pretreatment, such as purification of exosomes, and it involves a single enzymatic reaction,” the investigators wrote, suggesting that the assay may be suitable for real-world diagnosis.
‘Promising’ findings need replication
According to Douglas Galasko, MD, a neurologist and professor of neurosciences at UC San Diego Health, the reported accuracy of the assay “seems spectacular,” and the findings are “promising,” but they need to be replicated, “particularly in early-stage patients where the diagnosis [of Parkinson’s disease] is more difficult and important to make.” In practice, the assay would likely see greatest usage for “early diagnosis or diagnosis of unusual or challenging cases,” so accuracy testing needs to be conducted in this setting, he said.
Dr. Galasko, who was not involved in the study, predicted that liquid biopsy for detecting Parkinson’s disease is unlikely to hit the clinic floor anytime soon. “We’re not really close with blood-based biomarkers for Parkinson’s disease,” he said, “unlike the situation for Alzheimer’s disease, where there are several promising blood-based biomarkers.”
For diagnosing Parkinson’s disease, Dr. Galasko suggested that assays using skin biopsies to measure alpha-synuclein accumulation may be closer to approval.
The study was supported by JSPS KAKENHI Grant Number 20K20223 and the Sumitomo Electric Industries Group Corporate Social Responsibility Foundation. The investigators disclosed no conflicts of interest.
A novel blood-based assay could one day be used to diagnose Parkinson’s disease and possibly other chronic inflammatory conditions, according to investigators. In addition to being highly accurate, the assay, which detects changes in expression of cytochrome P450s, is faster and easier to perform than other Parkinson’s disease assays under investigation, reported lead author Kohei Ihara, PhD, of Kobe University, Japan, and colleagues.
“Effective diagnostic systems and biomarkers for patients without subjective motor symptoms have not yet been established,” the investigators wrote in Nature Scientific Reports. “Consequently, the poor diagnostic options for Parkinson’s disease delay the development of therapeutic approaches and medication. Therefore, the development of efficient diagnostic systems and biomarkers is crucial for overcoming Parkinson’s disease.”
According to Dr. Ihara and colleagues, various cytochrome P450 expression patterns and associated serum metabolites correlate with chronic conditions, making them possible markers of disease. To detect these changes, they developed the present assay. It relies upon recombinant P450s expressed on the surface of Escherichia coli. By mixing the E. coli with serum and Vivid, a fluorescent substrate, the investigators can measure “the inhibition rate of the Vivid decomposition reaction” that was driven by “serum metabolites associated with P450s,” revealing underlying expression and, if present, disease.
After some promising initial experiments with mouse models of ulcerative colitis and diabetes, Dr. Ihara and colleagues focused on a rat model of Parkinson’s disease. Evaluating inhibition rates associated with four P450s revealed area-under-the-curve (AUC) values of 0.814-0.914. Two of those P450s were also associated with progression of disease symptoms.
“Therefore, we concluded that the P450 inhibition assay could discriminate between Parkinson’s disease model rats and control rats,” the investigators wrote.
Next, the investigators tested the approach with a case-control study involving 20 patients with Parkinson’s disease and 20 healthy volunteers. Twelve P450s were analyzed, three of which revealed significant differences between patients with Parkinson’s disease and controls, with AUCs ranging from 0.740-0.775. Each of the three P450 enzymes also correlated significantly with stage of disease on the Hoehn & Yahr scale, although severity and frequency of symptoms were not reported.
To increase accuracy of the technique, the investigators developed a logistic regression model using two of the three P450s, generating an AUC of 0.910. Further testing showed that the P450 inhibition assay could distinguish between patients with Parkinson’s disease and Alzheimer’s disease, as well as other chronic inflammatory diseases.
“The P450 inhibition assay is easier to perform and is faster than other assays because this assay does not require pretreatment, such as purification of exosomes, and it involves a single enzymatic reaction,” the investigators wrote, suggesting that the assay may be suitable for real-world diagnosis.
‘Promising’ findings need replication
According to Douglas Galasko, MD, a neurologist and professor of neurosciences at UC San Diego Health, the reported accuracy of the assay “seems spectacular,” and the findings are “promising,” but they need to be replicated, “particularly in early-stage patients where the diagnosis [of Parkinson’s disease] is more difficult and important to make.” In practice, the assay would likely see greatest usage for “early diagnosis or diagnosis of unusual or challenging cases,” so accuracy testing needs to be conducted in this setting, he said.
Dr. Galasko, who was not involved in the study, predicted that liquid biopsy for detecting Parkinson’s disease is unlikely to hit the clinic floor anytime soon. “We’re not really close with blood-based biomarkers for Parkinson’s disease,” he said, “unlike the situation for Alzheimer’s disease, where there are several promising blood-based biomarkers.”
For diagnosing Parkinson’s disease, Dr. Galasko suggested that assays using skin biopsies to measure alpha-synuclein accumulation may be closer to approval.
The study was supported by JSPS KAKENHI Grant Number 20K20223 and the Sumitomo Electric Industries Group Corporate Social Responsibility Foundation. The investigators disclosed no conflicts of interest.
FROM NATURE SCIENTIFIC REPORTS
Two years after UCNS switch to continuous certification, major frustrations remain
Headache medicine expert Joel Saper, MD once saw the formation of the United Council for Neurologic Subspecialties as a sign of progress in the field. In 2005, he even helped write their first certification exam for headache medicine.
Now he’s calling fraud.
After Dr. Saper’s initial 10-year certification expired, he paid $1,800 to take a recertification test. Passing this, he earned another decade of diplomate status; or so he thought, until a couple years later, when he received word from the UCNS.
“They were changing the rules,” Dr. Saper said in an interview. “The 10-year certificate was no longer valid. You had to go through another process.”
That process, known as continuous certification, has become the new standard among medical boards. In contrast with a more conventional recertification process that depends upon high-fee, high-stakes exams taken years apart, continuous certification typically involves a relatively small annual fee coupled with online reading and assessments designed to ensure familiarity with advances in the field.
It’s not just the physicians that need to study up. Medical boards are under pressure to ensure that they are maintaining retention, a potentially challenging task with approximately 200 medical certifying boards in the United States competing for attention, and in some cases, credibility.
Pivots to new systems of recertification have been a particular flash point among physicians. In 2015, a Newsweek article described how a group of “nationally known physicians revolted against the American Board of Internal Medicine” after the board “attempted to expand its program for recertifying doctors, adding boatloads of requirements and fees to be paid by physicians.”
In response, ABIM attacked both the journalist and Newsweek, citing a conflict of interest (the journalist was married to a doctor). The journalist went on to uncover some uncomfortable statistics, including the fact that, over a 5-year period, the ABIM Foundation lost $39.8 million while paying senior administrators $125.7 million. Such revelations have likely added to a collective skepticism about medical boards and their motives.
The changing landscape of recertification
According to Brenda Riggott, executive director of the UCNS, the switch to continuous certification was driven by a need to keep up with new standards.
“We really found the landscape of maintaining medical certifications in general was changing,” Ms. Riggott said, highlighting how the UCNS “evaluated 13 different continuous certification models being administered by medical boards” before settling upon the present model.
Continuous certification with the UCNS now requires a $175 annual fee. Each year, diplomates read 10 journal articles, then take a 25-question online quiz to demonstrate their understanding.
“It’s really about patient care,” Ms. Riggott said in an interview. “Medicine changes rapidly. And there are a lot of advances. Evaluating that once a decade is really not enough to verify that somebody is maintaining their skills, their knowledge.”
Dr. Saper, a clinical professor of neurology at Michigan State University, East Lansing, and founder-director of the Michigan Head Pain and Neurological Institute, Ann Arbor, had no inherent qualm with transitioning to this newer process, but he did take umbrage at its execution, since his UCNS certificate still had about 7 years until expiry.
He said the UCNS should have honored existing certificates through their stated duration, citing precedent set by the American Academy of Neurology. When the AAN transitioned from lifetime board certification to a periodic recertification process, they honored the lifetime status of those who already held it, according to Dr. Saper.
“[The AAN] looked at those of us who had been boarded under the premise that we were going to be lifetime boarded ... and they said: ‘We’re going to grandfather you ... because that was the rule under which you took your initial exams.’ ... That’s what UCNS should have done,” Dr. Saper said.
A compromise
Under pressure from Dr. Saper and others, UCNS compromised by endorsing 10-year diplomates until the 5-year mark.
Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, and the editor-in-chief of Neurology Reviews, was among those who spoke up, only to see the duration of his certification cut in half.
“UCNS obviously realized that they had been wrong,” Dr. Rapoport said, referring to the compromise they made.
At the 5-year mark, physicians who didn’t adopt the new system were deleted from the UCNS online database, eliminating “the only way the public would know whether or not we were certified. This was after UCNS told us we would stay on the list with a note next to our name suggesting our certification was incomplete. They did not care that this might have hurt our reputations,” Dr. Rapoport said.
“To this day, no refunds, partial or full, have been given for the $1,800 we paid for the privilege of sitting for the exam, or for our time studying, or for the expenses accrued from canceling a day in the office and traveling to a testing center,” Dr. Rapoport said. “I did not want the money back; I wanted the certification promised to me. Since they have removed my name from this list, they do owe me the $1,800. They say they do not return their fees if you fail. How about if you pass and they remove you from their list?”
Yet he went on to make clear that the real issue is the principle of the matter. “This is not about money,” Dr. Rapoport said. “This is about what is fair and right.”
“The UCNS issued me a certificate for 10 years of certification in headache medicine; it is unethical and unlawful to break that contract and grant me only 5 years. Worse, they removed my name as though I do not exist. Along with Dr. Saper, I was one of the doctors that spent time and effort to advance headache medicine from October 1979, when I became a headache specialist, to today. I supported the principles of UCNS and took the first exam. I became the President of the International Headache Society and traveled the world promoting headache medicine; and this is how I am treated. Who can respect this type of certification, or this organization?”
Dr. Saper agreed: “It’s not about the money. It’s about the commitment. It’s very fraudulent.”
After the UCNS decision, Dr. Rapoport and Dr. Saper sought legal counsel, but ultimately decided not to sue the UCNS because of the lengthy process it would entail and the cost, estimated to be over $100,000.
“Our lawyers said: ‘It’s going to be years to get through it. You’ll probably win in the end, because it was fraudulent behavior,’ ” Dr. Saper said.
A different viewpoint
Ms. Riggott offered a different viewpoint: Nobody was guaranteed 10 years of certification.
“People do not pay for certification [from the UCNS],” Ms. Riggott said. “They pay to sit for an exam. It’s an exam administration fee. That can be construed as: ‘They paid for 10 years.’ They did not. They paid to sit for an exam. There are people who pay for an exam, and they don’t pass it, and they’re not certified. They don’t get a refund. That’s just the way high-stakes certification exams go.”
Dr. Saper and Dr. Rapoport see it differently. “The inherent reason any of us sit for an exam is to get certified.” Dr. Rapoport added. “Ms. Riggott is not being honest. There was an implied contract that if we passed, we would be granted a 10-year certification because that was what we did previously and that is what they told us would happen. Why would they have sent me this nice certificate for 10 more years of certification if she were telling the truth?”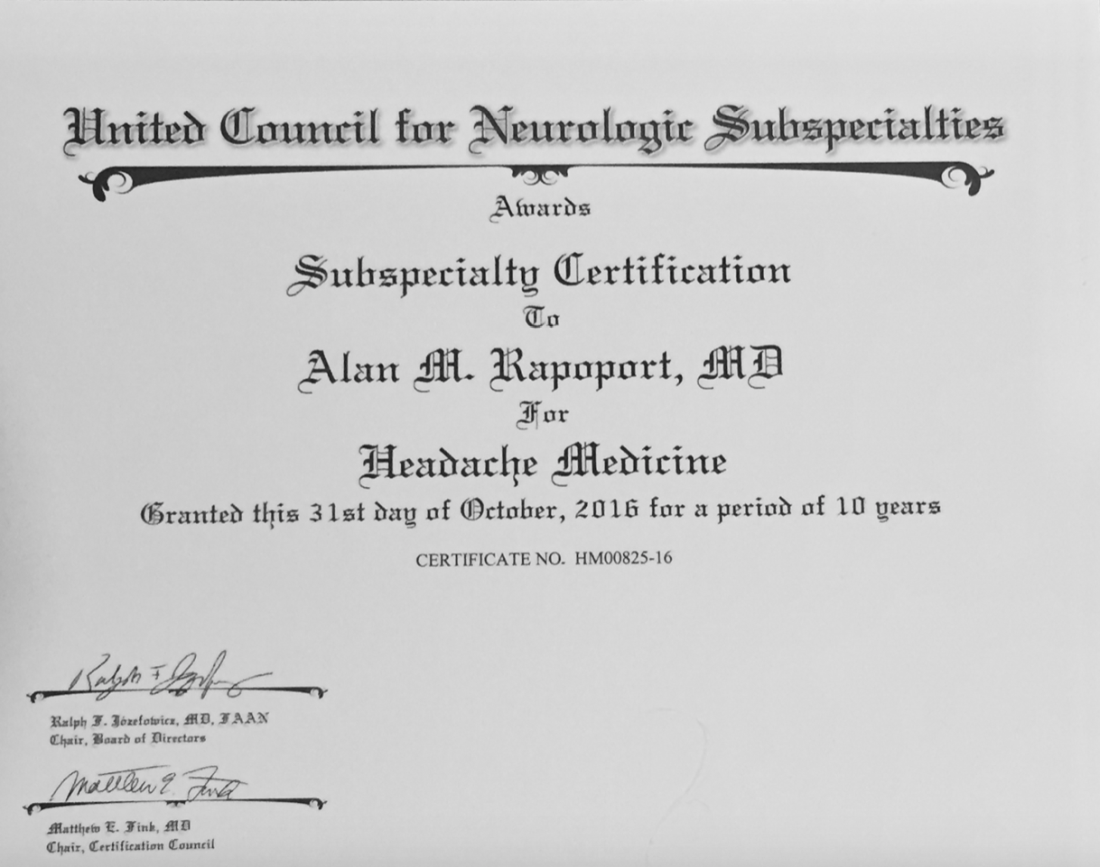
Profits over promises
Dr. Rapoport estimates that many other neurologists had their certificates cut short and were dropped from this official list, some of them eminent members of the field, including David Watson, MD, professor and chair of neurology at West Virginia University Rockefeller Neuroscience Institute, Morgantown, and Robert Cowan, MD, professor of neurology and chief of the division of headache medicine at Stanford (Calif.) University.
“It is troubling when the organizations charged with maintaining the integrity of our specialization do not act with integrity,” Dr. Watson said. “The UCNS chose profits over promises and has refused to meaningfully engage with those of us whom they have wronged. What was once a point of pride for me (being in the second class of certified headache medicine diplomates) has become a meaningless piece of paper. This makes me sad.”
Dr. Cowan said the UCNS actions angered him while affirming his lifelong skepticism of clubs. “I was very sorry, but not surprised, to see the UCNS change the rules when the opportunity to make more money presented itself, and not surprised they did not honor their contracts. UCNS is just another scam like Best Doctors in the US and similar hypes. Neither are worth another dime of my money nor the time spent discussing them. One thing more: I have no quarrel with efforts to encourage keeping up with the field, although no one I know needs codification or direction as to which articles should be read. My outrage comes when responsible behavior is used as an excuse to line the pockets of dishonest, immoral individuals. I’m done.”
According to Ms. Riggott, the UCNS continuous certification process continues to evolve based on feedback from diplomates. She noted that “change is hard,” although the challenges of the transition appear to be paying off. “Initial retention for continuing certification is much higher than we would have expected from a high-stakes recertification exam,” she said. “So we are very, very happy about that.”
Proprietary tests drive revenue
According to Katie Collins, executive director of the National Board of Physicians and Surgeons, proprietary tests are a key revenue driver for medical boards, casting doubt on their educational motives.
“This isn’t really about maintaining their education, it’s really about having control over what they learn,” Ms. Collins said. “And unfortunately, physicians no longer have control over what they learn.”
NBPAS was formed largely in response to physicians dissatisfied with this situation. For $189 every 2 years, plus $25 for a paper certificate, NBPAS recertifies doctors originally credentialed by the American Board of Medical Specialties or the American Osteopathic Association.
Instead of making physicians take proprietary tests, NBPAS requires them to earn 50 hours of Accreditation Council for Continuing Medical Education–accredited CME every 2 years. Physicians can select where they seek this credit, giving them the agency to “pick and choose where they want to learn more,” Ms. Collins said, noting that this allows physicians to address personal knowledge gaps, instead of mastering the prescriptive lessons issued by other boards.
While this benefits physicians, Ms. Collins added, it also reduces the bottom line.
NBPAS is a “true 501(c)(3),” she said. “We have money for rainy days, but certainly not millions. We don’t have anything close to a million in savings.” Most medical boards are making millions on top of their services, she said. “That’s not for me to rein in, but it’s for me to point out.”
Noah Rosen, MD, associate professor of neurology and psychiatry at Northwell Health, Great Neck, N.Y., and former UCNS board member, said the UCNS was not motivated by money when they decided to switch to continuous recertification.
“The UCNS budget is publicly available,” Dr. Rosen said in an interview. “This is not a money-making organization,” he added, noting that the UCNS has “been basically operating on a breakeven budget,” and that certification “is not really a money-making proposition.”
Public IRS filings from 2019 and 2020 suggest a slightly different picture. In 2019, the UCNS reported net income of $72,256. In 2020, the inaugural year of the continuous certification program, net income jumped almost fivefold to $349,108. Over the same period, total assets held by the UCNS rose from $1.97 million to $2.37 million.
For comparison, NBPAS controls approximately $500,000 in total assets. The ABIM? Just shy of $72 million.
Recertification highlights a generational gap
Dr. Rosen, who was not a voting board member when the UCNS decided to switch to continuous certification, suggested that the transition could have been handled more effectively.
“I think Dr. Rapoport speaks to the frustration of how they made the transition, and that it could have been done in a way that recognizes people that held the certificate in a better way,” Dr. Rosen said.
He said that the departure of Dr. Rapoport and other neurologists from the UCNS points to another trend in the certification space. “I do think it brings up a deeper issue: What’s the value of certification? Dr. Rapoport and other people have brought up the question: What actually does this certificate bring you, if it’s not recognized by the federal government, and actually is not recognized by a lot of state governments, as well, as an official certification?”
He said the answer could depend on age.
“There seems to be a difference between younger people entering into the field and people that are more established in the field already,” Dr. Rosen said. “Younger people entering the field, they see certification as a distinction, something that separates them from the experiences and maybe every other neurologist.”
Ms. Collins independently pointed out the same generational gap. She noted that when the ABMS changed their maintenance model from lifelong to periodic in 2000, approximately 60% of their physicians had to change with the times, while the remainder did not.
“They grandfathered the other 40% – the older, probably more Caucasian male physicians,” she said. “It’s just the field. It’s evolved, it’s become more diverse. They created a divide in the physician community about what is the best means to maintain your board.”
In response to these comments, and despite his negative experiences with the UCNS, Dr. Rapoport emphasized that he still places high value on subspecialty certification.
“I care a lot about certification and that is why I decided to study for and take the only exam offered at the time,” he said, “I do not need it to continue my practice in headache medicine. No one asks me if I am certified in headache medicine. My patients are referred to me because of my reputation. But I have always sought the highest level of certification I could get. What UCNS has done is to cheapen the value of their certification.”
Dr. Rosen and Ms. Collins highlighted the other side of the same conclusion: For younger physicians, board certifications are more of a career consideration than they are for older physicians, as they could mean the difference between landing or losing a job.
“The American Board of Medical Specialties and [their] 24 member boards have really woven board certification into a requirement for employment for hospital privileges and for reimbursement,” Ms. Collins said.
And so, the practical value of board certification may depend most on the tenure of the person holding paper.
“I have not gone back to get any further certification [from the UCNS],” Dr. Saper said.
Even if his name has been removed from the UCNS register, he pointed out that his printed certificate still shows it’s valid until October 31st, 2026: “If anybody asks: ‘Are you certified?’ I say: ‘Here’s my certificate.’ ”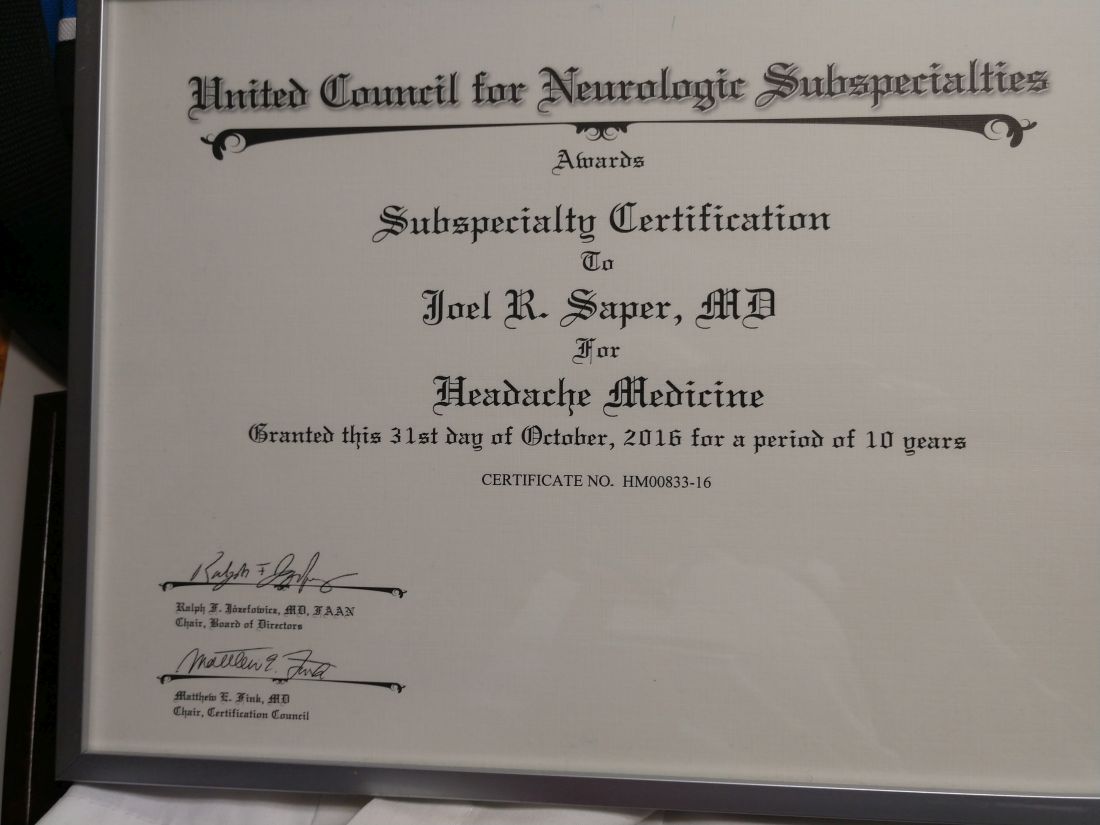
Headache medicine expert Joel Saper, MD once saw the formation of the United Council for Neurologic Subspecialties as a sign of progress in the field. In 2005, he even helped write their first certification exam for headache medicine.
Now he’s calling fraud.
After Dr. Saper’s initial 10-year certification expired, he paid $1,800 to take a recertification test. Passing this, he earned another decade of diplomate status; or so he thought, until a couple years later, when he received word from the UCNS.
“They were changing the rules,” Dr. Saper said in an interview. “The 10-year certificate was no longer valid. You had to go through another process.”
That process, known as continuous certification, has become the new standard among medical boards. In contrast with a more conventional recertification process that depends upon high-fee, high-stakes exams taken years apart, continuous certification typically involves a relatively small annual fee coupled with online reading and assessments designed to ensure familiarity with advances in the field.
It’s not just the physicians that need to study up. Medical boards are under pressure to ensure that they are maintaining retention, a potentially challenging task with approximately 200 medical certifying boards in the United States competing for attention, and in some cases, credibility.
Pivots to new systems of recertification have been a particular flash point among physicians. In 2015, a Newsweek article described how a group of “nationally known physicians revolted against the American Board of Internal Medicine” after the board “attempted to expand its program for recertifying doctors, adding boatloads of requirements and fees to be paid by physicians.”
In response, ABIM attacked both the journalist and Newsweek, citing a conflict of interest (the journalist was married to a doctor). The journalist went on to uncover some uncomfortable statistics, including the fact that, over a 5-year period, the ABIM Foundation lost $39.8 million while paying senior administrators $125.7 million. Such revelations have likely added to a collective skepticism about medical boards and their motives.
The changing landscape of recertification
According to Brenda Riggott, executive director of the UCNS, the switch to continuous certification was driven by a need to keep up with new standards.
“We really found the landscape of maintaining medical certifications in general was changing,” Ms. Riggott said, highlighting how the UCNS “evaluated 13 different continuous certification models being administered by medical boards” before settling upon the present model.
Continuous certification with the UCNS now requires a $175 annual fee. Each year, diplomates read 10 journal articles, then take a 25-question online quiz to demonstrate their understanding.
“It’s really about patient care,” Ms. Riggott said in an interview. “Medicine changes rapidly. And there are a lot of advances. Evaluating that once a decade is really not enough to verify that somebody is maintaining their skills, their knowledge.”
Dr. Saper, a clinical professor of neurology at Michigan State University, East Lansing, and founder-director of the Michigan Head Pain and Neurological Institute, Ann Arbor, had no inherent qualm with transitioning to this newer process, but he did take umbrage at its execution, since his UCNS certificate still had about 7 years until expiry.
He said the UCNS should have honored existing certificates through their stated duration, citing precedent set by the American Academy of Neurology. When the AAN transitioned from lifetime board certification to a periodic recertification process, they honored the lifetime status of those who already held it, according to Dr. Saper.
“[The AAN] looked at those of us who had been boarded under the premise that we were going to be lifetime boarded ... and they said: ‘We’re going to grandfather you ... because that was the rule under which you took your initial exams.’ ... That’s what UCNS should have done,” Dr. Saper said.
A compromise
Under pressure from Dr. Saper and others, UCNS compromised by endorsing 10-year diplomates until the 5-year mark.
Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, and the editor-in-chief of Neurology Reviews, was among those who spoke up, only to see the duration of his certification cut in half.
“UCNS obviously realized that they had been wrong,” Dr. Rapoport said, referring to the compromise they made.
At the 5-year mark, physicians who didn’t adopt the new system were deleted from the UCNS online database, eliminating “the only way the public would know whether or not we were certified. This was after UCNS told us we would stay on the list with a note next to our name suggesting our certification was incomplete. They did not care that this might have hurt our reputations,” Dr. Rapoport said.
“To this day, no refunds, partial or full, have been given for the $1,800 we paid for the privilege of sitting for the exam, or for our time studying, or for the expenses accrued from canceling a day in the office and traveling to a testing center,” Dr. Rapoport said. “I did not want the money back; I wanted the certification promised to me. Since they have removed my name from this list, they do owe me the $1,800. They say they do not return their fees if you fail. How about if you pass and they remove you from their list?”
Yet he went on to make clear that the real issue is the principle of the matter. “This is not about money,” Dr. Rapoport said. “This is about what is fair and right.”
“The UCNS issued me a certificate for 10 years of certification in headache medicine; it is unethical and unlawful to break that contract and grant me only 5 years. Worse, they removed my name as though I do not exist. Along with Dr. Saper, I was one of the doctors that spent time and effort to advance headache medicine from October 1979, when I became a headache specialist, to today. I supported the principles of UCNS and took the first exam. I became the President of the International Headache Society and traveled the world promoting headache medicine; and this is how I am treated. Who can respect this type of certification, or this organization?”
Dr. Saper agreed: “It’s not about the money. It’s about the commitment. It’s very fraudulent.”
After the UCNS decision, Dr. Rapoport and Dr. Saper sought legal counsel, but ultimately decided not to sue the UCNS because of the lengthy process it would entail and the cost, estimated to be over $100,000.
“Our lawyers said: ‘It’s going to be years to get through it. You’ll probably win in the end, because it was fraudulent behavior,’ ” Dr. Saper said.
A different viewpoint
Ms. Riggott offered a different viewpoint: Nobody was guaranteed 10 years of certification.
“People do not pay for certification [from the UCNS],” Ms. Riggott said. “They pay to sit for an exam. It’s an exam administration fee. That can be construed as: ‘They paid for 10 years.’ They did not. They paid to sit for an exam. There are people who pay for an exam, and they don’t pass it, and they’re not certified. They don’t get a refund. That’s just the way high-stakes certification exams go.”
Dr. Saper and Dr. Rapoport see it differently. “The inherent reason any of us sit for an exam is to get certified.” Dr. Rapoport added. “Ms. Riggott is not being honest. There was an implied contract that if we passed, we would be granted a 10-year certification because that was what we did previously and that is what they told us would happen. Why would they have sent me this nice certificate for 10 more years of certification if she were telling the truth?”
Profits over promises
Dr. Rapoport estimates that many other neurologists had their certificates cut short and were dropped from this official list, some of them eminent members of the field, including David Watson, MD, professor and chair of neurology at West Virginia University Rockefeller Neuroscience Institute, Morgantown, and Robert Cowan, MD, professor of neurology and chief of the division of headache medicine at Stanford (Calif.) University.
“It is troubling when the organizations charged with maintaining the integrity of our specialization do not act with integrity,” Dr. Watson said. “The UCNS chose profits over promises and has refused to meaningfully engage with those of us whom they have wronged. What was once a point of pride for me (being in the second class of certified headache medicine diplomates) has become a meaningless piece of paper. This makes me sad.”
Dr. Cowan said the UCNS actions angered him while affirming his lifelong skepticism of clubs. “I was very sorry, but not surprised, to see the UCNS change the rules when the opportunity to make more money presented itself, and not surprised they did not honor their contracts. UCNS is just another scam like Best Doctors in the US and similar hypes. Neither are worth another dime of my money nor the time spent discussing them. One thing more: I have no quarrel with efforts to encourage keeping up with the field, although no one I know needs codification or direction as to which articles should be read. My outrage comes when responsible behavior is used as an excuse to line the pockets of dishonest, immoral individuals. I’m done.”
According to Ms. Riggott, the UCNS continuous certification process continues to evolve based on feedback from diplomates. She noted that “change is hard,” although the challenges of the transition appear to be paying off. “Initial retention for continuing certification is much higher than we would have expected from a high-stakes recertification exam,” she said. “So we are very, very happy about that.”
Proprietary tests drive revenue
According to Katie Collins, executive director of the National Board of Physicians and Surgeons, proprietary tests are a key revenue driver for medical boards, casting doubt on their educational motives.
“This isn’t really about maintaining their education, it’s really about having control over what they learn,” Ms. Collins said. “And unfortunately, physicians no longer have control over what they learn.”
NBPAS was formed largely in response to physicians dissatisfied with this situation. For $189 every 2 years, plus $25 for a paper certificate, NBPAS recertifies doctors originally credentialed by the American Board of Medical Specialties or the American Osteopathic Association.
Instead of making physicians take proprietary tests, NBPAS requires them to earn 50 hours of Accreditation Council for Continuing Medical Education–accredited CME every 2 years. Physicians can select where they seek this credit, giving them the agency to “pick and choose where they want to learn more,” Ms. Collins said, noting that this allows physicians to address personal knowledge gaps, instead of mastering the prescriptive lessons issued by other boards.
While this benefits physicians, Ms. Collins added, it also reduces the bottom line.
NBPAS is a “true 501(c)(3),” she said. “We have money for rainy days, but certainly not millions. We don’t have anything close to a million in savings.” Most medical boards are making millions on top of their services, she said. “That’s not for me to rein in, but it’s for me to point out.”
Noah Rosen, MD, associate professor of neurology and psychiatry at Northwell Health, Great Neck, N.Y., and former UCNS board member, said the UCNS was not motivated by money when they decided to switch to continuous recertification.
“The UCNS budget is publicly available,” Dr. Rosen said in an interview. “This is not a money-making organization,” he added, noting that the UCNS has “been basically operating on a breakeven budget,” and that certification “is not really a money-making proposition.”
Public IRS filings from 2019 and 2020 suggest a slightly different picture. In 2019, the UCNS reported net income of $72,256. In 2020, the inaugural year of the continuous certification program, net income jumped almost fivefold to $349,108. Over the same period, total assets held by the UCNS rose from $1.97 million to $2.37 million.
For comparison, NBPAS controls approximately $500,000 in total assets. The ABIM? Just shy of $72 million.
Recertification highlights a generational gap
Dr. Rosen, who was not a voting board member when the UCNS decided to switch to continuous certification, suggested that the transition could have been handled more effectively.
“I think Dr. Rapoport speaks to the frustration of how they made the transition, and that it could have been done in a way that recognizes people that held the certificate in a better way,” Dr. Rosen said.
He said that the departure of Dr. Rapoport and other neurologists from the UCNS points to another trend in the certification space. “I do think it brings up a deeper issue: What’s the value of certification? Dr. Rapoport and other people have brought up the question: What actually does this certificate bring you, if it’s not recognized by the federal government, and actually is not recognized by a lot of state governments, as well, as an official certification?”
He said the answer could depend on age.
“There seems to be a difference between younger people entering into the field and people that are more established in the field already,” Dr. Rosen said. “Younger people entering the field, they see certification as a distinction, something that separates them from the experiences and maybe every other neurologist.”
Ms. Collins independently pointed out the same generational gap. She noted that when the ABMS changed their maintenance model from lifelong to periodic in 2000, approximately 60% of their physicians had to change with the times, while the remainder did not.
“They grandfathered the other 40% – the older, probably more Caucasian male physicians,” she said. “It’s just the field. It’s evolved, it’s become more diverse. They created a divide in the physician community about what is the best means to maintain your board.”
In response to these comments, and despite his negative experiences with the UCNS, Dr. Rapoport emphasized that he still places high value on subspecialty certification.
“I care a lot about certification and that is why I decided to study for and take the only exam offered at the time,” he said, “I do not need it to continue my practice in headache medicine. No one asks me if I am certified in headache medicine. My patients are referred to me because of my reputation. But I have always sought the highest level of certification I could get. What UCNS has done is to cheapen the value of their certification.”
Dr. Rosen and Ms. Collins highlighted the other side of the same conclusion: For younger physicians, board certifications are more of a career consideration than they are for older physicians, as they could mean the difference between landing or losing a job.
“The American Board of Medical Specialties and [their] 24 member boards have really woven board certification into a requirement for employment for hospital privileges and for reimbursement,” Ms. Collins said.
And so, the practical value of board certification may depend most on the tenure of the person holding paper.
“I have not gone back to get any further certification [from the UCNS],” Dr. Saper said.
Even if his name has been removed from the UCNS register, he pointed out that his printed certificate still shows it’s valid until October 31st, 2026: “If anybody asks: ‘Are you certified?’ I say: ‘Here’s my certificate.’ ”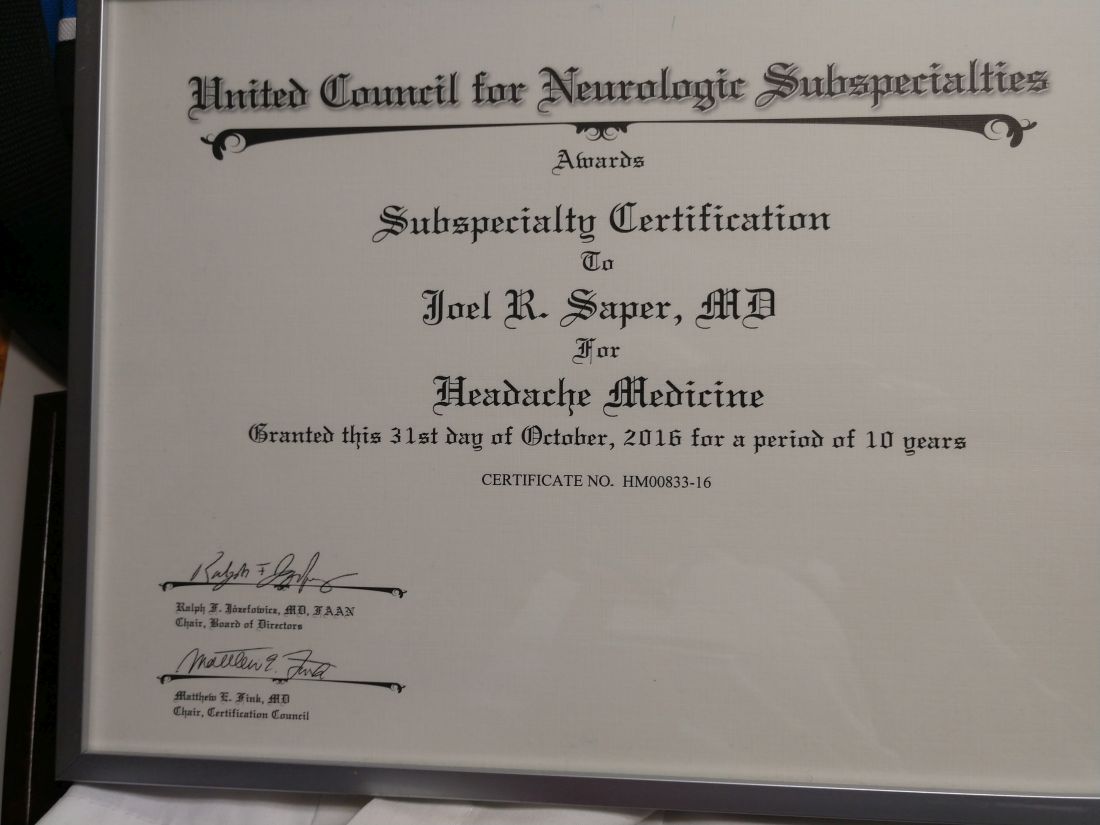
Headache medicine expert Joel Saper, MD once saw the formation of the United Council for Neurologic Subspecialties as a sign of progress in the field. In 2005, he even helped write their first certification exam for headache medicine.
Now he’s calling fraud.
After Dr. Saper’s initial 10-year certification expired, he paid $1,800 to take a recertification test. Passing this, he earned another decade of diplomate status; or so he thought, until a couple years later, when he received word from the UCNS.
“They were changing the rules,” Dr. Saper said in an interview. “The 10-year certificate was no longer valid. You had to go through another process.”
That process, known as continuous certification, has become the new standard among medical boards. In contrast with a more conventional recertification process that depends upon high-fee, high-stakes exams taken years apart, continuous certification typically involves a relatively small annual fee coupled with online reading and assessments designed to ensure familiarity with advances in the field.
It’s not just the physicians that need to study up. Medical boards are under pressure to ensure that they are maintaining retention, a potentially challenging task with approximately 200 medical certifying boards in the United States competing for attention, and in some cases, credibility.
Pivots to new systems of recertification have been a particular flash point among physicians. In 2015, a Newsweek article described how a group of “nationally known physicians revolted against the American Board of Internal Medicine” after the board “attempted to expand its program for recertifying doctors, adding boatloads of requirements and fees to be paid by physicians.”
In response, ABIM attacked both the journalist and Newsweek, citing a conflict of interest (the journalist was married to a doctor). The journalist went on to uncover some uncomfortable statistics, including the fact that, over a 5-year period, the ABIM Foundation lost $39.8 million while paying senior administrators $125.7 million. Such revelations have likely added to a collective skepticism about medical boards and their motives.
The changing landscape of recertification
According to Brenda Riggott, executive director of the UCNS, the switch to continuous certification was driven by a need to keep up with new standards.
“We really found the landscape of maintaining medical certifications in general was changing,” Ms. Riggott said, highlighting how the UCNS “evaluated 13 different continuous certification models being administered by medical boards” before settling upon the present model.
Continuous certification with the UCNS now requires a $175 annual fee. Each year, diplomates read 10 journal articles, then take a 25-question online quiz to demonstrate their understanding.
“It’s really about patient care,” Ms. Riggott said in an interview. “Medicine changes rapidly. And there are a lot of advances. Evaluating that once a decade is really not enough to verify that somebody is maintaining their skills, their knowledge.”
Dr. Saper, a clinical professor of neurology at Michigan State University, East Lansing, and founder-director of the Michigan Head Pain and Neurological Institute, Ann Arbor, had no inherent qualm with transitioning to this newer process, but he did take umbrage at its execution, since his UCNS certificate still had about 7 years until expiry.
He said the UCNS should have honored existing certificates through their stated duration, citing precedent set by the American Academy of Neurology. When the AAN transitioned from lifetime board certification to a periodic recertification process, they honored the lifetime status of those who already held it, according to Dr. Saper.
“[The AAN] looked at those of us who had been boarded under the premise that we were going to be lifetime boarded ... and they said: ‘We’re going to grandfather you ... because that was the rule under which you took your initial exams.’ ... That’s what UCNS should have done,” Dr. Saper said.
A compromise
Under pressure from Dr. Saper and others, UCNS compromised by endorsing 10-year diplomates until the 5-year mark.
Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, and the editor-in-chief of Neurology Reviews, was among those who spoke up, only to see the duration of his certification cut in half.
“UCNS obviously realized that they had been wrong,” Dr. Rapoport said, referring to the compromise they made.
At the 5-year mark, physicians who didn’t adopt the new system were deleted from the UCNS online database, eliminating “the only way the public would know whether or not we were certified. This was after UCNS told us we would stay on the list with a note next to our name suggesting our certification was incomplete. They did not care that this might have hurt our reputations,” Dr. Rapoport said.
“To this day, no refunds, partial or full, have been given for the $1,800 we paid for the privilege of sitting for the exam, or for our time studying, or for the expenses accrued from canceling a day in the office and traveling to a testing center,” Dr. Rapoport said. “I did not want the money back; I wanted the certification promised to me. Since they have removed my name from this list, they do owe me the $1,800. They say they do not return their fees if you fail. How about if you pass and they remove you from their list?”
Yet he went on to make clear that the real issue is the principle of the matter. “This is not about money,” Dr. Rapoport said. “This is about what is fair and right.”
“The UCNS issued me a certificate for 10 years of certification in headache medicine; it is unethical and unlawful to break that contract and grant me only 5 years. Worse, they removed my name as though I do not exist. Along with Dr. Saper, I was one of the doctors that spent time and effort to advance headache medicine from October 1979, when I became a headache specialist, to today. I supported the principles of UCNS and took the first exam. I became the President of the International Headache Society and traveled the world promoting headache medicine; and this is how I am treated. Who can respect this type of certification, or this organization?”
Dr. Saper agreed: “It’s not about the money. It’s about the commitment. It’s very fraudulent.”
After the UCNS decision, Dr. Rapoport and Dr. Saper sought legal counsel, but ultimately decided not to sue the UCNS because of the lengthy process it would entail and the cost, estimated to be over $100,000.
“Our lawyers said: ‘It’s going to be years to get through it. You’ll probably win in the end, because it was fraudulent behavior,’ ” Dr. Saper said.
A different viewpoint
Ms. Riggott offered a different viewpoint: Nobody was guaranteed 10 years of certification.
“People do not pay for certification [from the UCNS],” Ms. Riggott said. “They pay to sit for an exam. It’s an exam administration fee. That can be construed as: ‘They paid for 10 years.’ They did not. They paid to sit for an exam. There are people who pay for an exam, and they don’t pass it, and they’re not certified. They don’t get a refund. That’s just the way high-stakes certification exams go.”
Dr. Saper and Dr. Rapoport see it differently. “The inherent reason any of us sit for an exam is to get certified.” Dr. Rapoport added. “Ms. Riggott is not being honest. There was an implied contract that if we passed, we would be granted a 10-year certification because that was what we did previously and that is what they told us would happen. Why would they have sent me this nice certificate for 10 more years of certification if she were telling the truth?”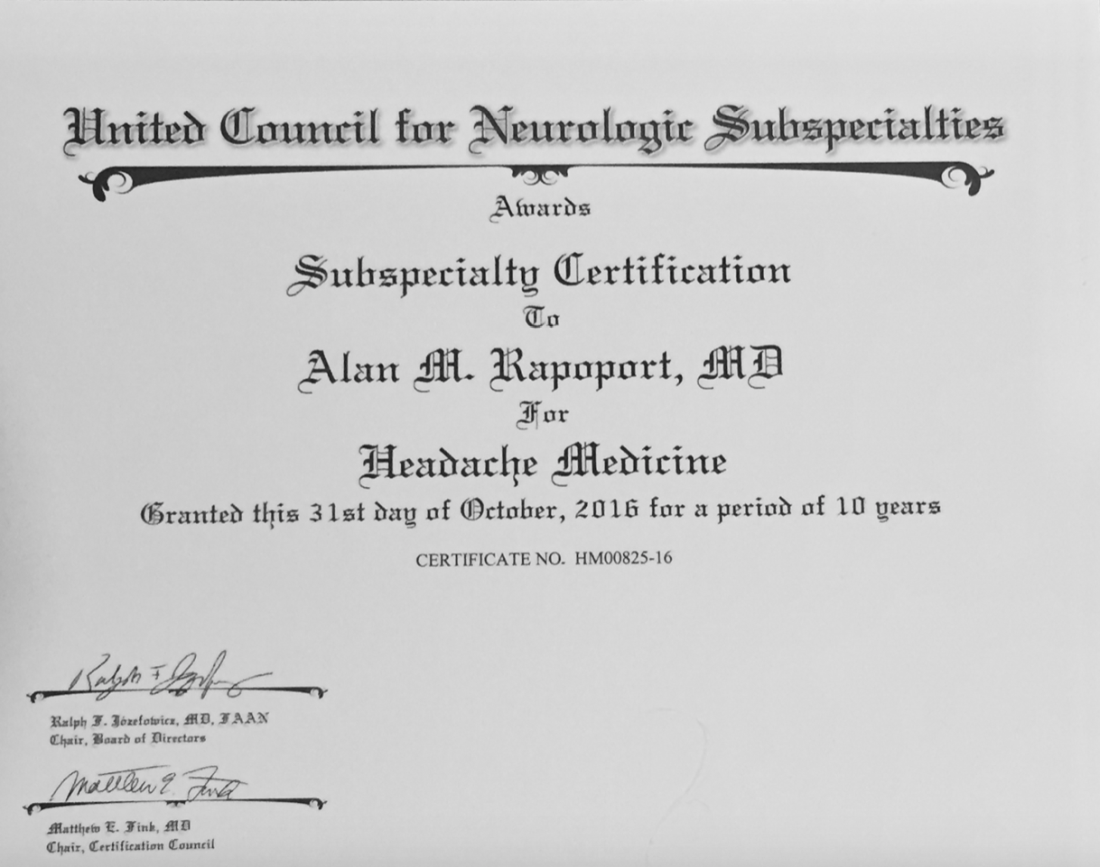
Profits over promises
Dr. Rapoport estimates that many other neurologists had their certificates cut short and were dropped from this official list, some of them eminent members of the field, including David Watson, MD, professor and chair of neurology at West Virginia University Rockefeller Neuroscience Institute, Morgantown, and Robert Cowan, MD, professor of neurology and chief of the division of headache medicine at Stanford (Calif.) University.
“It is troubling when the organizations charged with maintaining the integrity of our specialization do not act with integrity,” Dr. Watson said. “The UCNS chose profits over promises and has refused to meaningfully engage with those of us whom they have wronged. What was once a point of pride for me (being in the second class of certified headache medicine diplomates) has become a meaningless piece of paper. This makes me sad.”
Dr. Cowan said the UCNS actions angered him while affirming his lifelong skepticism of clubs. “I was very sorry, but not surprised, to see the UCNS change the rules when the opportunity to make more money presented itself, and not surprised they did not honor their contracts. UCNS is just another scam like Best Doctors in the US and similar hypes. Neither are worth another dime of my money nor the time spent discussing them. One thing more: I have no quarrel with efforts to encourage keeping up with the field, although no one I know needs codification or direction as to which articles should be read. My outrage comes when responsible behavior is used as an excuse to line the pockets of dishonest, immoral individuals. I’m done.”
According to Ms. Riggott, the UCNS continuous certification process continues to evolve based on feedback from diplomates. She noted that “change is hard,” although the challenges of the transition appear to be paying off. “Initial retention for continuing certification is much higher than we would have expected from a high-stakes recertification exam,” she said. “So we are very, very happy about that.”
Proprietary tests drive revenue
According to Katie Collins, executive director of the National Board of Physicians and Surgeons, proprietary tests are a key revenue driver for medical boards, casting doubt on their educational motives.
“This isn’t really about maintaining their education, it’s really about having control over what they learn,” Ms. Collins said. “And unfortunately, physicians no longer have control over what they learn.”
NBPAS was formed largely in response to physicians dissatisfied with this situation. For $189 every 2 years, plus $25 for a paper certificate, NBPAS recertifies doctors originally credentialed by the American Board of Medical Specialties or the American Osteopathic Association.
Instead of making physicians take proprietary tests, NBPAS requires them to earn 50 hours of Accreditation Council for Continuing Medical Education–accredited CME every 2 years. Physicians can select where they seek this credit, giving them the agency to “pick and choose where they want to learn more,” Ms. Collins said, noting that this allows physicians to address personal knowledge gaps, instead of mastering the prescriptive lessons issued by other boards.
While this benefits physicians, Ms. Collins added, it also reduces the bottom line.
NBPAS is a “true 501(c)(3),” she said. “We have money for rainy days, but certainly not millions. We don’t have anything close to a million in savings.” Most medical boards are making millions on top of their services, she said. “That’s not for me to rein in, but it’s for me to point out.”
Noah Rosen, MD, associate professor of neurology and psychiatry at Northwell Health, Great Neck, N.Y., and former UCNS board member, said the UCNS was not motivated by money when they decided to switch to continuous recertification.
“The UCNS budget is publicly available,” Dr. Rosen said in an interview. “This is not a money-making organization,” he added, noting that the UCNS has “been basically operating on a breakeven budget,” and that certification “is not really a money-making proposition.”
Public IRS filings from 2019 and 2020 suggest a slightly different picture. In 2019, the UCNS reported net income of $72,256. In 2020, the inaugural year of the continuous certification program, net income jumped almost fivefold to $349,108. Over the same period, total assets held by the UCNS rose from $1.97 million to $2.37 million.
For comparison, NBPAS controls approximately $500,000 in total assets. The ABIM? Just shy of $72 million.
Recertification highlights a generational gap
Dr. Rosen, who was not a voting board member when the UCNS decided to switch to continuous certification, suggested that the transition could have been handled more effectively.
“I think Dr. Rapoport speaks to the frustration of how they made the transition, and that it could have been done in a way that recognizes people that held the certificate in a better way,” Dr. Rosen said.
He said that the departure of Dr. Rapoport and other neurologists from the UCNS points to another trend in the certification space. “I do think it brings up a deeper issue: What’s the value of certification? Dr. Rapoport and other people have brought up the question: What actually does this certificate bring you, if it’s not recognized by the federal government, and actually is not recognized by a lot of state governments, as well, as an official certification?”
He said the answer could depend on age.
“There seems to be a difference between younger people entering into the field and people that are more established in the field already,” Dr. Rosen said. “Younger people entering the field, they see certification as a distinction, something that separates them from the experiences and maybe every other neurologist.”
Ms. Collins independently pointed out the same generational gap. She noted that when the ABMS changed their maintenance model from lifelong to periodic in 2000, approximately 60% of their physicians had to change with the times, while the remainder did not.
“They grandfathered the other 40% – the older, probably more Caucasian male physicians,” she said. “It’s just the field. It’s evolved, it’s become more diverse. They created a divide in the physician community about what is the best means to maintain your board.”
In response to these comments, and despite his negative experiences with the UCNS, Dr. Rapoport emphasized that he still places high value on subspecialty certification.
“I care a lot about certification and that is why I decided to study for and take the only exam offered at the time,” he said, “I do not need it to continue my practice in headache medicine. No one asks me if I am certified in headache medicine. My patients are referred to me because of my reputation. But I have always sought the highest level of certification I could get. What UCNS has done is to cheapen the value of their certification.”
Dr. Rosen and Ms. Collins highlighted the other side of the same conclusion: For younger physicians, board certifications are more of a career consideration than they are for older physicians, as they could mean the difference between landing or losing a job.
“The American Board of Medical Specialties and [their] 24 member boards have really woven board certification into a requirement for employment for hospital privileges and for reimbursement,” Ms. Collins said.
And so, the practical value of board certification may depend most on the tenure of the person holding paper.
“I have not gone back to get any further certification [from the UCNS],” Dr. Saper said.
Even if his name has been removed from the UCNS register, he pointed out that his printed certificate still shows it’s valid until October 31st, 2026: “If anybody asks: ‘Are you certified?’ I say: ‘Here’s my certificate.’ ”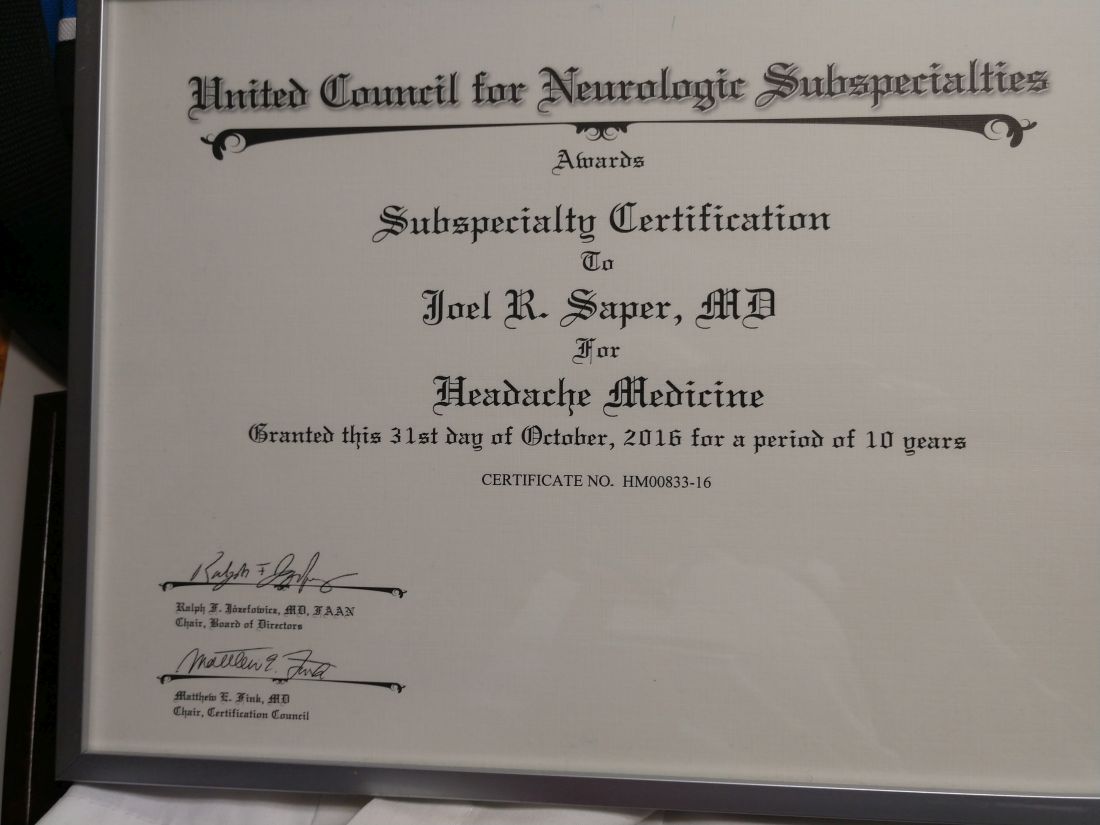
Coffee drinkers – even those with a sweet tooth – live longer
Among more than 170,000 people in the United Kingdom, those who drank about two to four cups of coffee a day, with or without sugar, had a lower rate of death than those who didn’t drink coffee, reported lead author Dan Liu, MD, of the department of epidemiology at Southern Medical University, Guangzhou, China.
“Previous observational studies have suggested an association between coffee intake and reduced risk for death, but they did not distinguish between coffee consumed with sugar or artificial sweeteners and coffee consumed without,” Dr. Liu, who is also of the department of public health and preventive medicine, Jinan University, Guangzhou, China, and colleagues wrote in Annals of Internal Medicine.
To learn more, the investigators turned to the UK Biobank, which recruited approximately half a million participants in the United Kingdom between 2006 and 2010 to undergo a variety of questionnaires, interviews, physical measurements, and medical tests. Out of this group, 171,616 participants completed at least one dietary questionnaire and met the criteria for the present study, including lack of cancer or cardiovascular disease upon enrollment.
Results from these questionnaires showed that 55.4% of participants drank coffee without any sweetener, 14.3% drank coffee with sugar, 6.1% drank coffee with artificial sweetener, and 24.2% did not drink coffee at all. Coffee drinkers were further sorted into groups based on how many cups of coffee they drank per day.
Coffee drinkers were significantly less likely to die from any cause
Over the course of about 7 years, 3,177 of the participants died, including 1,725 who died from cancer and 628 who died from cardiovascular disease.
After accounting for other factors that might impact risk of death, like lifestyle choices, the investigators found that coffee drinkers were significantly less likely to die from any cause, cardiovascular disease, or cancer, than those who didn’t drink coffee at all. This benefit was observed across types of coffee, including ground, instant, and decaffeinated varieties. The protective effects of coffee were most apparent in people who drank about two to four cups a day, among whom death was about 30% less likely, regardless of whether they added sugar to their coffee or not. Individuals who drank coffee with artificial sweetener did not live significantly longer than those who drank no coffee at all; however, the investigators suggested that this result may have been skewed by higher rates of negative health factors, such as obesity and hypertension, in the artificial sweetener group.
Dr. Liu and colleagues noted that their findings align with previous studies linking coffee consumption with survival. Like those other studies, the present data revealed a “U-shaped” benefit curve, in which moderate coffee consumption was associated with longer life, whereas low or no consumption and high consumption were not.
Experts caution against drinking sweetened beverages despite new findings
Although the present findings suggested that adding sugar did not eliminate the health benefits of coffee, Dr. Liu and colleagues still cautioned against sweetened beverages, citing widely known associations between sugar consumption and poor health.
In an accompanying editorial, Christina C. Wee, MD, MPH, deputy editor of Annals of Internal Medicine, pointed out a key detail from the data: the amount of sugar added to coffee in the U.K. study may be dwarfed by the amount consumed by some coffee drinkers across the pond.
“The average dose of added sugar per cup of sweetened coffee [in the study] was only a little over a teaspoon, or about 4 grams,” Dr. Wee wrote. “This is a far cry from the 15 grams of sugar in an 8-ounce cup of caramel macchiato at a popular U.S. coffee chain.”
Still, Dr. Wee, an associate professor of medicine at Harvard Medical School, Boston, and director of the obesity research program in the division of general medicine at Beth Israel Deaconess Medical Center, Boston, suggested that your typical coffee drinker can feel safe in their daily habit.
“The evidence does not suggest a need for most coffee drinkers – particularly those who drink it with no or modest amounts of sugar – to eliminate coffee,” she wrote. “So drink up – but it would be prudent to avoid too many caramel macchiatos while more evidence brews.”
Estefanía Toledo, MD, MPH, PhD, of the department of preventive medicine and public health at the University of Navarra, Pamplona, Spain, offered a similar takeaway.
“For those who enjoy drinking coffee, are not pregnant or lactating, and do not have special health conditions, coffee consumption could be considered part of a healthy lifestyle,” Dr. Toledo said in a written comment. “I would recommend adding as little sugar as possible to coffee until more evidence has been accrued.”
Dr. Toledo, who previously published a study showing a link between coffee and extended survival, noted that moderate coffee consumption has “repeatedly” been associated with lower rates of “several chronic diseases” and death, but there still isn’t enough evidence to recommend coffee for those who don’t already drink it.
More long-term research is needed, Dr. Toledo said, ideally with studies comparing changes in coffee consumption and health outcomes over time. These may not be forthcoming, however, as such trials are “not easy and feasible to conduct.”
David Kao, MD, assistant professor of medicine-cardiology and medical director of the school of medicine at the University of Colorado at Denver, Aurora, said that the study conducted by Dr. Liu and colleagues is a “very well-executed analysis” that strengthens our confidence in the safety of long-term coffee consumption, even for patients with heart disease.
Dr. Kao, who recently published an analysis showing that higher coffee intake is associated with a lower risk of heart failure, refrained from advising anyone to up their coffee quota.
“I remain cautious about stating too strongly that people should increase coffee intake purely to improve survival,” Dr. Kao said in a written comment. “That said, it does not appear harmful to increase it some, until you drink consistently more than six to seven cups per day.”
The study was supported by the National Natural Science Foundation of China, the Young Elite Scientist Sponsorship Program by CAST, the Guangdong Basic and Applied Basic Research Foundation, and others. Dr. Toledo and Dr. Kao disclosed no relevant conflicts of interest.
Among more than 170,000 people in the United Kingdom, those who drank about two to four cups of coffee a day, with or without sugar, had a lower rate of death than those who didn’t drink coffee, reported lead author Dan Liu, MD, of the department of epidemiology at Southern Medical University, Guangzhou, China.
“Previous observational studies have suggested an association between coffee intake and reduced risk for death, but they did not distinguish between coffee consumed with sugar or artificial sweeteners and coffee consumed without,” Dr. Liu, who is also of the department of public health and preventive medicine, Jinan University, Guangzhou, China, and colleagues wrote in Annals of Internal Medicine.
To learn more, the investigators turned to the UK Biobank, which recruited approximately half a million participants in the United Kingdom between 2006 and 2010 to undergo a variety of questionnaires, interviews, physical measurements, and medical tests. Out of this group, 171,616 participants completed at least one dietary questionnaire and met the criteria for the present study, including lack of cancer or cardiovascular disease upon enrollment.
Results from these questionnaires showed that 55.4% of participants drank coffee without any sweetener, 14.3% drank coffee with sugar, 6.1% drank coffee with artificial sweetener, and 24.2% did not drink coffee at all. Coffee drinkers were further sorted into groups based on how many cups of coffee they drank per day.
Coffee drinkers were significantly less likely to die from any cause
Over the course of about 7 years, 3,177 of the participants died, including 1,725 who died from cancer and 628 who died from cardiovascular disease.
After accounting for other factors that might impact risk of death, like lifestyle choices, the investigators found that coffee drinkers were significantly less likely to die from any cause, cardiovascular disease, or cancer, than those who didn’t drink coffee at all. This benefit was observed across types of coffee, including ground, instant, and decaffeinated varieties. The protective effects of coffee were most apparent in people who drank about two to four cups a day, among whom death was about 30% less likely, regardless of whether they added sugar to their coffee or not. Individuals who drank coffee with artificial sweetener did not live significantly longer than those who drank no coffee at all; however, the investigators suggested that this result may have been skewed by higher rates of negative health factors, such as obesity and hypertension, in the artificial sweetener group.
Dr. Liu and colleagues noted that their findings align with previous studies linking coffee consumption with survival. Like those other studies, the present data revealed a “U-shaped” benefit curve, in which moderate coffee consumption was associated with longer life, whereas low or no consumption and high consumption were not.
Experts caution against drinking sweetened beverages despite new findings
Although the present findings suggested that adding sugar did not eliminate the health benefits of coffee, Dr. Liu and colleagues still cautioned against sweetened beverages, citing widely known associations between sugar consumption and poor health.
In an accompanying editorial, Christina C. Wee, MD, MPH, deputy editor of Annals of Internal Medicine, pointed out a key detail from the data: the amount of sugar added to coffee in the U.K. study may be dwarfed by the amount consumed by some coffee drinkers across the pond.
“The average dose of added sugar per cup of sweetened coffee [in the study] was only a little over a teaspoon, or about 4 grams,” Dr. Wee wrote. “This is a far cry from the 15 grams of sugar in an 8-ounce cup of caramel macchiato at a popular U.S. coffee chain.”
Still, Dr. Wee, an associate professor of medicine at Harvard Medical School, Boston, and director of the obesity research program in the division of general medicine at Beth Israel Deaconess Medical Center, Boston, suggested that your typical coffee drinker can feel safe in their daily habit.
“The evidence does not suggest a need for most coffee drinkers – particularly those who drink it with no or modest amounts of sugar – to eliminate coffee,” she wrote. “So drink up – but it would be prudent to avoid too many caramel macchiatos while more evidence brews.”
Estefanía Toledo, MD, MPH, PhD, of the department of preventive medicine and public health at the University of Navarra, Pamplona, Spain, offered a similar takeaway.
“For those who enjoy drinking coffee, are not pregnant or lactating, and do not have special health conditions, coffee consumption could be considered part of a healthy lifestyle,” Dr. Toledo said in a written comment. “I would recommend adding as little sugar as possible to coffee until more evidence has been accrued.”
Dr. Toledo, who previously published a study showing a link between coffee and extended survival, noted that moderate coffee consumption has “repeatedly” been associated with lower rates of “several chronic diseases” and death, but there still isn’t enough evidence to recommend coffee for those who don’t already drink it.
More long-term research is needed, Dr. Toledo said, ideally with studies comparing changes in coffee consumption and health outcomes over time. These may not be forthcoming, however, as such trials are “not easy and feasible to conduct.”
David Kao, MD, assistant professor of medicine-cardiology and medical director of the school of medicine at the University of Colorado at Denver, Aurora, said that the study conducted by Dr. Liu and colleagues is a “very well-executed analysis” that strengthens our confidence in the safety of long-term coffee consumption, even for patients with heart disease.
Dr. Kao, who recently published an analysis showing that higher coffee intake is associated with a lower risk of heart failure, refrained from advising anyone to up their coffee quota.
“I remain cautious about stating too strongly that people should increase coffee intake purely to improve survival,” Dr. Kao said in a written comment. “That said, it does not appear harmful to increase it some, until you drink consistently more than six to seven cups per day.”
The study was supported by the National Natural Science Foundation of China, the Young Elite Scientist Sponsorship Program by CAST, the Guangdong Basic and Applied Basic Research Foundation, and others. Dr. Toledo and Dr. Kao disclosed no relevant conflicts of interest.
Among more than 170,000 people in the United Kingdom, those who drank about two to four cups of coffee a day, with or without sugar, had a lower rate of death than those who didn’t drink coffee, reported lead author Dan Liu, MD, of the department of epidemiology at Southern Medical University, Guangzhou, China.
“Previous observational studies have suggested an association between coffee intake and reduced risk for death, but they did not distinguish between coffee consumed with sugar or artificial sweeteners and coffee consumed without,” Dr. Liu, who is also of the department of public health and preventive medicine, Jinan University, Guangzhou, China, and colleagues wrote in Annals of Internal Medicine.
To learn more, the investigators turned to the UK Biobank, which recruited approximately half a million participants in the United Kingdom between 2006 and 2010 to undergo a variety of questionnaires, interviews, physical measurements, and medical tests. Out of this group, 171,616 participants completed at least one dietary questionnaire and met the criteria for the present study, including lack of cancer or cardiovascular disease upon enrollment.
Results from these questionnaires showed that 55.4% of participants drank coffee without any sweetener, 14.3% drank coffee with sugar, 6.1% drank coffee with artificial sweetener, and 24.2% did not drink coffee at all. Coffee drinkers were further sorted into groups based on how many cups of coffee they drank per day.
Coffee drinkers were significantly less likely to die from any cause
Over the course of about 7 years, 3,177 of the participants died, including 1,725 who died from cancer and 628 who died from cardiovascular disease.
After accounting for other factors that might impact risk of death, like lifestyle choices, the investigators found that coffee drinkers were significantly less likely to die from any cause, cardiovascular disease, or cancer, than those who didn’t drink coffee at all. This benefit was observed across types of coffee, including ground, instant, and decaffeinated varieties. The protective effects of coffee were most apparent in people who drank about two to four cups a day, among whom death was about 30% less likely, regardless of whether they added sugar to their coffee or not. Individuals who drank coffee with artificial sweetener did not live significantly longer than those who drank no coffee at all; however, the investigators suggested that this result may have been skewed by higher rates of negative health factors, such as obesity and hypertension, in the artificial sweetener group.
Dr. Liu and colleagues noted that their findings align with previous studies linking coffee consumption with survival. Like those other studies, the present data revealed a “U-shaped” benefit curve, in which moderate coffee consumption was associated with longer life, whereas low or no consumption and high consumption were not.
Experts caution against drinking sweetened beverages despite new findings
Although the present findings suggested that adding sugar did not eliminate the health benefits of coffee, Dr. Liu and colleagues still cautioned against sweetened beverages, citing widely known associations between sugar consumption and poor health.
In an accompanying editorial, Christina C. Wee, MD, MPH, deputy editor of Annals of Internal Medicine, pointed out a key detail from the data: the amount of sugar added to coffee in the U.K. study may be dwarfed by the amount consumed by some coffee drinkers across the pond.
“The average dose of added sugar per cup of sweetened coffee [in the study] was only a little over a teaspoon, or about 4 grams,” Dr. Wee wrote. “This is a far cry from the 15 grams of sugar in an 8-ounce cup of caramel macchiato at a popular U.S. coffee chain.”
Still, Dr. Wee, an associate professor of medicine at Harvard Medical School, Boston, and director of the obesity research program in the division of general medicine at Beth Israel Deaconess Medical Center, Boston, suggested that your typical coffee drinker can feel safe in their daily habit.
“The evidence does not suggest a need for most coffee drinkers – particularly those who drink it with no or modest amounts of sugar – to eliminate coffee,” she wrote. “So drink up – but it would be prudent to avoid too many caramel macchiatos while more evidence brews.”
Estefanía Toledo, MD, MPH, PhD, of the department of preventive medicine and public health at the University of Navarra, Pamplona, Spain, offered a similar takeaway.
“For those who enjoy drinking coffee, are not pregnant or lactating, and do not have special health conditions, coffee consumption could be considered part of a healthy lifestyle,” Dr. Toledo said in a written comment. “I would recommend adding as little sugar as possible to coffee until more evidence has been accrued.”
Dr. Toledo, who previously published a study showing a link between coffee and extended survival, noted that moderate coffee consumption has “repeatedly” been associated with lower rates of “several chronic diseases” and death, but there still isn’t enough evidence to recommend coffee for those who don’t already drink it.
More long-term research is needed, Dr. Toledo said, ideally with studies comparing changes in coffee consumption and health outcomes over time. These may not be forthcoming, however, as such trials are “not easy and feasible to conduct.”
David Kao, MD, assistant professor of medicine-cardiology and medical director of the school of medicine at the University of Colorado at Denver, Aurora, said that the study conducted by Dr. Liu and colleagues is a “very well-executed analysis” that strengthens our confidence in the safety of long-term coffee consumption, even for patients with heart disease.
Dr. Kao, who recently published an analysis showing that higher coffee intake is associated with a lower risk of heart failure, refrained from advising anyone to up their coffee quota.
“I remain cautious about stating too strongly that people should increase coffee intake purely to improve survival,” Dr. Kao said in a written comment. “That said, it does not appear harmful to increase it some, until you drink consistently more than six to seven cups per day.”
The study was supported by the National Natural Science Foundation of China, the Young Elite Scientist Sponsorship Program by CAST, the Guangdong Basic and Applied Basic Research Foundation, and others. Dr. Toledo and Dr. Kao disclosed no relevant conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
AGA Clinical Practice Guideline: Diagnosis, treatment of rare hamartomatous polyposis
which is comprised of experts representing the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy.
Gastrointestinal hamartomatous polyposis syndromes are rare, autosomal dominant disorders associated with intestinal and extraintestinal tumors. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,” lead author C. Richard Boland, MD, of the University of California, San Diego, and colleagues reported.
According to the investigators, “there are essentially no long-term prospective controlled studies of comparative effectiveness of management strategies for these syndromes.” As a result, their recommendations are based on “low-quality” evidence according to GRADE criteria.
Still, Dr. Boland and colleagues highlighted that “there has been tremendous progress in recent years, both in understanding the underlying genetics that underpin these disorders and in elucidating the biology of associated premalignant and malignant conditions.”
The guideline was published online in Gastroenterology .
Four syndromes reviewed
The investigators gathered these data to provide an overview of genetic and clinical features for each syndrome, as well as management strategies. Four disorders are included: juvenile polyposis syndrome; Peutz-Jeghers syndrome; hereditary mixed polyposis syndrome; and PTEN-hamartoma tumor syndrome, encompassing Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome.
Although all gastrointestinal hamartomatous polyposis syndromes are caused by germline alterations, Dr. Boland and colleagues pointed out that diagnoses are typically made based on clinical criteria, with germline results serving as confirmatory evidence.
The guideline recommends that any patient with a family history of hamartomatous polyps, or with a history of at least two hamartomatous polyps, should undergo genetic testing. The guideline also provides more nuanced genetic testing algorithms for each syndrome.
Among all the hamartomatous polyp disorders, Peutz-Jeghers syndrome is most understood, according to the investigators. It is caused by aberrations in the STK11 gene, and is characterized by polyps with “branching bands of smooth muscle covered by hyperplastic glandular mucosa” that may occur in the stomach, small intestine, and colon. Patients are also at risk of extraintestinal neoplasia.
For management of Peutz-Jeghers syndrome, the guideline advises frequent endoscopic surveillance to prevent mechanical obstruction and bleeding, as well as multidisciplinary surveillance of the breasts, pancreas, ovaries, testes, and lungs.
Juvenile polyposis syndrome is most often characterized by solitary, sporadic polyps in the colorectum (98% of patients affected), followed distantly by polyps in the stomach (14%), ileum (7%), jejunum (7%), and duodenum (7%). The condition is linked with abnormalities in BMPR1A or SMAD4 genes, with SMAD4 germline abnormalities more often leading to “massive” gastric polyps, gastrointestinal bleeding, protein-losing enteropathy, and a higher incidence of gastric cancer in adulthood. Most patients with SMAD4 mutations also have hereditary hemorrhagic telangiectasia, characterized by gastrointestinal bleeding from mucocutaneous telangiectasias, arteriovenous malformations, and epistaxis.
Management of juvenile polyposis syndrome depends on frequent colonoscopies with polypectomies beginning at 12-15 years.
“The goal of surveillance in juvenile polyposis syndrome is to mitigate symptoms related to the disorder and decrease the risk of complications from the manifestations, including cancer,” Dr. Boland and colleagues wrote.
PTEN-hamartoma tumor syndrome, which includes both Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome, is caused by abnormalities in the eponymous PTEN gene. Patients with the condition have an increased risk of colon cancer and polyposis, as well as extraintestinal cancers.
Diagnosis of PTEN-hamartoma tumor syndrome may be complex, involving “clinical examination, mammography and breast MRI, thyroid ultrasound, transvaginal ultrasound, upper gastrointestinal endoscopy, colonoscopy, and renal ultrasound,” according to the guideline.
After diagnosis, frequent colonoscopies are recommended, typically starting at age 35 years, as well as continued surveillance of other organs.
Hereditary mixed polyposis syndrome, which involves attenuated colonic polyposis, is the rarest of the four disorders, having been reported in only “a few families,” according to the guideline. The condition has been linked with “large duplications of the promoter region or entire GREM1 gene.”
Onset is typically in the late 20s, “which is when colonoscopic surveillance should begin,” the investigators wrote. More data are needed to determine appropriate surveillance intervals and if the condition is associated with increased risk of extraintestinal neoplasia.
This call for more research into gastrointestinal hamartomatous polyposis syndromes carried through to the conclusion of the guideline.
“Long-term prospective studies of mutation carriers are still needed to further clarify the risk of cancer and the role of surveillance in these syndromes,” Dr. Boland and colleagues wrote. “With increases in genetic testing and evaluation, future studies will be conducted with more robust cohorts of genetically characterized, less heterogeneous populations. However, there is also a need to study patients and families with unusual phenotypes where no genotype can be found.”
The investigators disclosed no conflicts of interest with the current guideline; however, they provided a list of industry relationships, including Salix Pharmaceuticals, Ferring Pharmaceuticals, and Pfizer, among others.
which is comprised of experts representing the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy.
Gastrointestinal hamartomatous polyposis syndromes are rare, autosomal dominant disorders associated with intestinal and extraintestinal tumors. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,” lead author C. Richard Boland, MD, of the University of California, San Diego, and colleagues reported.
According to the investigators, “there are essentially no long-term prospective controlled studies of comparative effectiveness of management strategies for these syndromes.” As a result, their recommendations are based on “low-quality” evidence according to GRADE criteria.
Still, Dr. Boland and colleagues highlighted that “there has been tremendous progress in recent years, both in understanding the underlying genetics that underpin these disorders and in elucidating the biology of associated premalignant and malignant conditions.”
The guideline was published online in Gastroenterology .
Four syndromes reviewed
The investigators gathered these data to provide an overview of genetic and clinical features for each syndrome, as well as management strategies. Four disorders are included: juvenile polyposis syndrome; Peutz-Jeghers syndrome; hereditary mixed polyposis syndrome; and PTEN-hamartoma tumor syndrome, encompassing Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome.
Although all gastrointestinal hamartomatous polyposis syndromes are caused by germline alterations, Dr. Boland and colleagues pointed out that diagnoses are typically made based on clinical criteria, with germline results serving as confirmatory evidence.
The guideline recommends that any patient with a family history of hamartomatous polyps, or with a history of at least two hamartomatous polyps, should undergo genetic testing. The guideline also provides more nuanced genetic testing algorithms for each syndrome.
Among all the hamartomatous polyp disorders, Peutz-Jeghers syndrome is most understood, according to the investigators. It is caused by aberrations in the STK11 gene, and is characterized by polyps with “branching bands of smooth muscle covered by hyperplastic glandular mucosa” that may occur in the stomach, small intestine, and colon. Patients are also at risk of extraintestinal neoplasia.
For management of Peutz-Jeghers syndrome, the guideline advises frequent endoscopic surveillance to prevent mechanical obstruction and bleeding, as well as multidisciplinary surveillance of the breasts, pancreas, ovaries, testes, and lungs.
Juvenile polyposis syndrome is most often characterized by solitary, sporadic polyps in the colorectum (98% of patients affected), followed distantly by polyps in the stomach (14%), ileum (7%), jejunum (7%), and duodenum (7%). The condition is linked with abnormalities in BMPR1A or SMAD4 genes, with SMAD4 germline abnormalities more often leading to “massive” gastric polyps, gastrointestinal bleeding, protein-losing enteropathy, and a higher incidence of gastric cancer in adulthood. Most patients with SMAD4 mutations also have hereditary hemorrhagic telangiectasia, characterized by gastrointestinal bleeding from mucocutaneous telangiectasias, arteriovenous malformations, and epistaxis.
Management of juvenile polyposis syndrome depends on frequent colonoscopies with polypectomies beginning at 12-15 years.
“The goal of surveillance in juvenile polyposis syndrome is to mitigate symptoms related to the disorder and decrease the risk of complications from the manifestations, including cancer,” Dr. Boland and colleagues wrote.
PTEN-hamartoma tumor syndrome, which includes both Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome, is caused by abnormalities in the eponymous PTEN gene. Patients with the condition have an increased risk of colon cancer and polyposis, as well as extraintestinal cancers.
Diagnosis of PTEN-hamartoma tumor syndrome may be complex, involving “clinical examination, mammography and breast MRI, thyroid ultrasound, transvaginal ultrasound, upper gastrointestinal endoscopy, colonoscopy, and renal ultrasound,” according to the guideline.
After diagnosis, frequent colonoscopies are recommended, typically starting at age 35 years, as well as continued surveillance of other organs.
Hereditary mixed polyposis syndrome, which involves attenuated colonic polyposis, is the rarest of the four disorders, having been reported in only “a few families,” according to the guideline. The condition has been linked with “large duplications of the promoter region or entire GREM1 gene.”
Onset is typically in the late 20s, “which is when colonoscopic surveillance should begin,” the investigators wrote. More data are needed to determine appropriate surveillance intervals and if the condition is associated with increased risk of extraintestinal neoplasia.
This call for more research into gastrointestinal hamartomatous polyposis syndromes carried through to the conclusion of the guideline.
“Long-term prospective studies of mutation carriers are still needed to further clarify the risk of cancer and the role of surveillance in these syndromes,” Dr. Boland and colleagues wrote. “With increases in genetic testing and evaluation, future studies will be conducted with more robust cohorts of genetically characterized, less heterogeneous populations. However, there is also a need to study patients and families with unusual phenotypes where no genotype can be found.”
The investigators disclosed no conflicts of interest with the current guideline; however, they provided a list of industry relationships, including Salix Pharmaceuticals, Ferring Pharmaceuticals, and Pfizer, among others.
which is comprised of experts representing the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy.
Gastrointestinal hamartomatous polyposis syndromes are rare, autosomal dominant disorders associated with intestinal and extraintestinal tumors. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,” lead author C. Richard Boland, MD, of the University of California, San Diego, and colleagues reported.
According to the investigators, “there are essentially no long-term prospective controlled studies of comparative effectiveness of management strategies for these syndromes.” As a result, their recommendations are based on “low-quality” evidence according to GRADE criteria.
Still, Dr. Boland and colleagues highlighted that “there has been tremendous progress in recent years, both in understanding the underlying genetics that underpin these disorders and in elucidating the biology of associated premalignant and malignant conditions.”
The guideline was published online in Gastroenterology .
Four syndromes reviewed
The investigators gathered these data to provide an overview of genetic and clinical features for each syndrome, as well as management strategies. Four disorders are included: juvenile polyposis syndrome; Peutz-Jeghers syndrome; hereditary mixed polyposis syndrome; and PTEN-hamartoma tumor syndrome, encompassing Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome.
Although all gastrointestinal hamartomatous polyposis syndromes are caused by germline alterations, Dr. Boland and colleagues pointed out that diagnoses are typically made based on clinical criteria, with germline results serving as confirmatory evidence.
The guideline recommends that any patient with a family history of hamartomatous polyps, or with a history of at least two hamartomatous polyps, should undergo genetic testing. The guideline also provides more nuanced genetic testing algorithms for each syndrome.
Among all the hamartomatous polyp disorders, Peutz-Jeghers syndrome is most understood, according to the investigators. It is caused by aberrations in the STK11 gene, and is characterized by polyps with “branching bands of smooth muscle covered by hyperplastic glandular mucosa” that may occur in the stomach, small intestine, and colon. Patients are also at risk of extraintestinal neoplasia.
For management of Peutz-Jeghers syndrome, the guideline advises frequent endoscopic surveillance to prevent mechanical obstruction and bleeding, as well as multidisciplinary surveillance of the breasts, pancreas, ovaries, testes, and lungs.
Juvenile polyposis syndrome is most often characterized by solitary, sporadic polyps in the colorectum (98% of patients affected), followed distantly by polyps in the stomach (14%), ileum (7%), jejunum (7%), and duodenum (7%). The condition is linked with abnormalities in BMPR1A or SMAD4 genes, with SMAD4 germline abnormalities more often leading to “massive” gastric polyps, gastrointestinal bleeding, protein-losing enteropathy, and a higher incidence of gastric cancer in adulthood. Most patients with SMAD4 mutations also have hereditary hemorrhagic telangiectasia, characterized by gastrointestinal bleeding from mucocutaneous telangiectasias, arteriovenous malformations, and epistaxis.
Management of juvenile polyposis syndrome depends on frequent colonoscopies with polypectomies beginning at 12-15 years.
“The goal of surveillance in juvenile polyposis syndrome is to mitigate symptoms related to the disorder and decrease the risk of complications from the manifestations, including cancer,” Dr. Boland and colleagues wrote.
PTEN-hamartoma tumor syndrome, which includes both Bannayan-Riley-Ruvalcaba syndrome and Cowden’s syndrome, is caused by abnormalities in the eponymous PTEN gene. Patients with the condition have an increased risk of colon cancer and polyposis, as well as extraintestinal cancers.
Diagnosis of PTEN-hamartoma tumor syndrome may be complex, involving “clinical examination, mammography and breast MRI, thyroid ultrasound, transvaginal ultrasound, upper gastrointestinal endoscopy, colonoscopy, and renal ultrasound,” according to the guideline.
After diagnosis, frequent colonoscopies are recommended, typically starting at age 35 years, as well as continued surveillance of other organs.
Hereditary mixed polyposis syndrome, which involves attenuated colonic polyposis, is the rarest of the four disorders, having been reported in only “a few families,” according to the guideline. The condition has been linked with “large duplications of the promoter region or entire GREM1 gene.”
Onset is typically in the late 20s, “which is when colonoscopic surveillance should begin,” the investigators wrote. More data are needed to determine appropriate surveillance intervals and if the condition is associated with increased risk of extraintestinal neoplasia.
This call for more research into gastrointestinal hamartomatous polyposis syndromes carried through to the conclusion of the guideline.
“Long-term prospective studies of mutation carriers are still needed to further clarify the risk of cancer and the role of surveillance in these syndromes,” Dr. Boland and colleagues wrote. “With increases in genetic testing and evaluation, future studies will be conducted with more robust cohorts of genetically characterized, less heterogeneous populations. However, there is also a need to study patients and families with unusual phenotypes where no genotype can be found.”
The investigators disclosed no conflicts of interest with the current guideline; however, they provided a list of industry relationships, including Salix Pharmaceuticals, Ferring Pharmaceuticals, and Pfizer, among others.
FROM GASTROENTEROLOGY
Creatinine variability linked to liver transplant outcomes
Patients with greater changes in serum creatinine are more likely to have worse pre- and post–liver transplant outcomes. Moreover, underserved patients may be most frequently affected, according to a retrospective analysis of UNOS (United Network for Organ Sharing) data.
These results should drive further development of serum creatinine coefficient of variation (sCr CoV) as an independent predictor of renal-related mortality risk, according to lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
“Intra-individual clinical and laboratory parameter dynamics often provide additional prognostic information – added information that goes beyond what can be found with cross-sectional data,” the researchers wrote in Hepatology. “This finding has been seen in several scenarios in the general population – intra-individual variability in blood pressure, weight, hemoglobin, and kidney function, have all been associated with worse clinical outcomes. However, in cirrhosis patients, and more specifically in patients awaiting a liver transplant, kidney function dynamics as a predictor of clinical outcomes has yet to be investigated.”
To gauge the predictive power of shifting kidney values, Dr. Cullaro and colleagues analyzed UNOS/OPTN (Organ Procurement and Transplantation Network) registry data from 2011 through 2019. Exclusion criteria included patients who were aged younger than 18 years, were listed as status 1, received a living donor liver transplantation, were on hemodialysis, or had fewer than three updates. The final dataset included 25,204 patients.
After the researchers sorted patients into low, intermediate, and high sCr CoV tertiles, they used logistic regression to determine relationships between higher sCr and a variety of covariates, such as age, sex, diagnosis, presence of acute kidney injury, or chronic kidney disease. A competing risk regression was then done to look for associations between wait list mortality and the covariables, with liver transplant used as the competing risk.
The median sCr CoV was 17.4% (interquartile range [IQR], 10.8%-29.5%). Patients in the bottom sCr CoV tertile had a median value of 8.8% (IQR, 6.6%-10.8%), compared with 17.4% (IQR, 14.8%-20.4%) in the intermediate variability group and 36.8% (IQR, 29.5%-48.8%) in the high variability group. High variability was associated with female sex, Hispanic ethnicity, ascites, and hepatic encephalopathy as well as higher body mass index, MELDNa score, and serum creatinine.
Of note, each decreasing serum creatinine variability tertile was associated with a significantly lower rate of wait list mortality (34.7% vs. 19.6% vs. 11.7%; P < .001). The creatinine variability profiles were similarly associated with the likelihood of receiving a liver transplant (52.3% vs. 48.9% vs. 43.7%; P < .001) and posttransplant mortality (7.5% vs. 5.5% vs. 3.9%; P < .001).
A multivariate model showed that each 10% increase in sCr CoV predicted an 8% increased risk of a combined outcome comprising post–liver transplant death or post–liver transplant kidney transplant (KALT), independently of other variables (adjusted hazard ratio, 1.08; 95% confidence interval, 1.05-1.11).
“These data highlight that all fluctuations in sCr are associated with worse pre- and post–liver transplant outcomes,” the investigators concluded. “Moreover, the groups that are most underserved by sCr, specifically women, were most likely to have greater sCr CoVs. We believe our work lays the foundation for implementing the sCr CoV as an independent metric of renal-related mortality risk and may be most beneficial for those groups most underserved by sCr values alone.”
According to Brian P. Lee, MD, a hepatologist with Keck Medicine of USC and assistant professor of clinical medicine with the Keck School of Medicine of USC in Los Angeles, “this is a great study ... in an area of high need” that used “high quality data.”
Current liver allocation strategies depend on a snapshot of kidney function, but these new findings suggest that a more dynamic approach may be needed. “As a practicing liver specialist I see that creatinine numbers can fluctuate a lot. ... So which number do you use when you’re trying to calculate what a patient’s risk of death is on the wait list? This study gets toward that answer. If there is a lot of variability, these might be higher risk patients; these might be patients that we should put higher on the transplant waiting list,” said Dr. Lee.
He suggested that clinicians should account for creatinine fluctuations when considering mortality risk; however, the evidence is “not quite there yet ... in terms of changing transplant policy and allocation.” He pointed out three unanswered questions: Why are creatinine values fluctuating? How should fluctuations be scored for risk modeling? And, what impact would those risk scores have on transplant waitlist prioritization?
“I think that that’s the work that you would need to do before you could really change national transplant policy,” Dr. Lee concluded.
The study was supported by the National Institutes of Health and the UCSF Liver Center. Dr. Cullaro and another author have disclosed relationships with Mallinckrodt Pharmaceuticals and Axcella Health, respectively. Dr. Lee reported no conflicts of interest.
Patients with greater changes in serum creatinine are more likely to have worse pre- and post–liver transplant outcomes. Moreover, underserved patients may be most frequently affected, according to a retrospective analysis of UNOS (United Network for Organ Sharing) data.
These results should drive further development of serum creatinine coefficient of variation (sCr CoV) as an independent predictor of renal-related mortality risk, according to lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
“Intra-individual clinical and laboratory parameter dynamics often provide additional prognostic information – added information that goes beyond what can be found with cross-sectional data,” the researchers wrote in Hepatology. “This finding has been seen in several scenarios in the general population – intra-individual variability in blood pressure, weight, hemoglobin, and kidney function, have all been associated with worse clinical outcomes. However, in cirrhosis patients, and more specifically in patients awaiting a liver transplant, kidney function dynamics as a predictor of clinical outcomes has yet to be investigated.”
To gauge the predictive power of shifting kidney values, Dr. Cullaro and colleagues analyzed UNOS/OPTN (Organ Procurement and Transplantation Network) registry data from 2011 through 2019. Exclusion criteria included patients who were aged younger than 18 years, were listed as status 1, received a living donor liver transplantation, were on hemodialysis, or had fewer than three updates. The final dataset included 25,204 patients.
After the researchers sorted patients into low, intermediate, and high sCr CoV tertiles, they used logistic regression to determine relationships between higher sCr and a variety of covariates, such as age, sex, diagnosis, presence of acute kidney injury, or chronic kidney disease. A competing risk regression was then done to look for associations between wait list mortality and the covariables, with liver transplant used as the competing risk.
The median sCr CoV was 17.4% (interquartile range [IQR], 10.8%-29.5%). Patients in the bottom sCr CoV tertile had a median value of 8.8% (IQR, 6.6%-10.8%), compared with 17.4% (IQR, 14.8%-20.4%) in the intermediate variability group and 36.8% (IQR, 29.5%-48.8%) in the high variability group. High variability was associated with female sex, Hispanic ethnicity, ascites, and hepatic encephalopathy as well as higher body mass index, MELDNa score, and serum creatinine.
Of note, each decreasing serum creatinine variability tertile was associated with a significantly lower rate of wait list mortality (34.7% vs. 19.6% vs. 11.7%; P < .001). The creatinine variability profiles were similarly associated with the likelihood of receiving a liver transplant (52.3% vs. 48.9% vs. 43.7%; P < .001) and posttransplant mortality (7.5% vs. 5.5% vs. 3.9%; P < .001).
A multivariate model showed that each 10% increase in sCr CoV predicted an 8% increased risk of a combined outcome comprising post–liver transplant death or post–liver transplant kidney transplant (KALT), independently of other variables (adjusted hazard ratio, 1.08; 95% confidence interval, 1.05-1.11).
“These data highlight that all fluctuations in sCr are associated with worse pre- and post–liver transplant outcomes,” the investigators concluded. “Moreover, the groups that are most underserved by sCr, specifically women, were most likely to have greater sCr CoVs. We believe our work lays the foundation for implementing the sCr CoV as an independent metric of renal-related mortality risk and may be most beneficial for those groups most underserved by sCr values alone.”
According to Brian P. Lee, MD, a hepatologist with Keck Medicine of USC and assistant professor of clinical medicine with the Keck School of Medicine of USC in Los Angeles, “this is a great study ... in an area of high need” that used “high quality data.”
Current liver allocation strategies depend on a snapshot of kidney function, but these new findings suggest that a more dynamic approach may be needed. “As a practicing liver specialist I see that creatinine numbers can fluctuate a lot. ... So which number do you use when you’re trying to calculate what a patient’s risk of death is on the wait list? This study gets toward that answer. If there is a lot of variability, these might be higher risk patients; these might be patients that we should put higher on the transplant waiting list,” said Dr. Lee.
He suggested that clinicians should account for creatinine fluctuations when considering mortality risk; however, the evidence is “not quite there yet ... in terms of changing transplant policy and allocation.” He pointed out three unanswered questions: Why are creatinine values fluctuating? How should fluctuations be scored for risk modeling? And, what impact would those risk scores have on transplant waitlist prioritization?
“I think that that’s the work that you would need to do before you could really change national transplant policy,” Dr. Lee concluded.
The study was supported by the National Institutes of Health and the UCSF Liver Center. Dr. Cullaro and another author have disclosed relationships with Mallinckrodt Pharmaceuticals and Axcella Health, respectively. Dr. Lee reported no conflicts of interest.
Patients with greater changes in serum creatinine are more likely to have worse pre- and post–liver transplant outcomes. Moreover, underserved patients may be most frequently affected, according to a retrospective analysis of UNOS (United Network for Organ Sharing) data.
These results should drive further development of serum creatinine coefficient of variation (sCr CoV) as an independent predictor of renal-related mortality risk, according to lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
“Intra-individual clinical and laboratory parameter dynamics often provide additional prognostic information – added information that goes beyond what can be found with cross-sectional data,” the researchers wrote in Hepatology. “This finding has been seen in several scenarios in the general population – intra-individual variability in blood pressure, weight, hemoglobin, and kidney function, have all been associated with worse clinical outcomes. However, in cirrhosis patients, and more specifically in patients awaiting a liver transplant, kidney function dynamics as a predictor of clinical outcomes has yet to be investigated.”
To gauge the predictive power of shifting kidney values, Dr. Cullaro and colleagues analyzed UNOS/OPTN (Organ Procurement and Transplantation Network) registry data from 2011 through 2019. Exclusion criteria included patients who were aged younger than 18 years, were listed as status 1, received a living donor liver transplantation, were on hemodialysis, or had fewer than three updates. The final dataset included 25,204 patients.
After the researchers sorted patients into low, intermediate, and high sCr CoV tertiles, they used logistic regression to determine relationships between higher sCr and a variety of covariates, such as age, sex, diagnosis, presence of acute kidney injury, or chronic kidney disease. A competing risk regression was then done to look for associations between wait list mortality and the covariables, with liver transplant used as the competing risk.
The median sCr CoV was 17.4% (interquartile range [IQR], 10.8%-29.5%). Patients in the bottom sCr CoV tertile had a median value of 8.8% (IQR, 6.6%-10.8%), compared with 17.4% (IQR, 14.8%-20.4%) in the intermediate variability group and 36.8% (IQR, 29.5%-48.8%) in the high variability group. High variability was associated with female sex, Hispanic ethnicity, ascites, and hepatic encephalopathy as well as higher body mass index, MELDNa score, and serum creatinine.
Of note, each decreasing serum creatinine variability tertile was associated with a significantly lower rate of wait list mortality (34.7% vs. 19.6% vs. 11.7%; P < .001). The creatinine variability profiles were similarly associated with the likelihood of receiving a liver transplant (52.3% vs. 48.9% vs. 43.7%; P < .001) and posttransplant mortality (7.5% vs. 5.5% vs. 3.9%; P < .001).
A multivariate model showed that each 10% increase in sCr CoV predicted an 8% increased risk of a combined outcome comprising post–liver transplant death or post–liver transplant kidney transplant (KALT), independently of other variables (adjusted hazard ratio, 1.08; 95% confidence interval, 1.05-1.11).
“These data highlight that all fluctuations in sCr are associated with worse pre- and post–liver transplant outcomes,” the investigators concluded. “Moreover, the groups that are most underserved by sCr, specifically women, were most likely to have greater sCr CoVs. We believe our work lays the foundation for implementing the sCr CoV as an independent metric of renal-related mortality risk and may be most beneficial for those groups most underserved by sCr values alone.”
According to Brian P. Lee, MD, a hepatologist with Keck Medicine of USC and assistant professor of clinical medicine with the Keck School of Medicine of USC in Los Angeles, “this is a great study ... in an area of high need” that used “high quality data.”
Current liver allocation strategies depend on a snapshot of kidney function, but these new findings suggest that a more dynamic approach may be needed. “As a practicing liver specialist I see that creatinine numbers can fluctuate a lot. ... So which number do you use when you’re trying to calculate what a patient’s risk of death is on the wait list? This study gets toward that answer. If there is a lot of variability, these might be higher risk patients; these might be patients that we should put higher on the transplant waiting list,” said Dr. Lee.
He suggested that clinicians should account for creatinine fluctuations when considering mortality risk; however, the evidence is “not quite there yet ... in terms of changing transplant policy and allocation.” He pointed out three unanswered questions: Why are creatinine values fluctuating? How should fluctuations be scored for risk modeling? And, what impact would those risk scores have on transplant waitlist prioritization?
“I think that that’s the work that you would need to do before you could really change national transplant policy,” Dr. Lee concluded.
The study was supported by the National Institutes of Health and the UCSF Liver Center. Dr. Cullaro and another author have disclosed relationships with Mallinckrodt Pharmaceuticals and Axcella Health, respectively. Dr. Lee reported no conflicts of interest.
FROM HEPATOLOGY
NAFLD vs. MAFLD: What’s in a name?
Non-alcoholic fatty liver disease (NAFLD) and metabolic associated fatty liver disease (MAFLD) demonstrate highly similar clinical courses and mortality rates, and a name change may not be clinically beneficial, based on data from more than 17,000 patients.
Instead, etiologic subcategorization of fatty liver disease (FLD) should be considered, reported lead author Zobair M. Younossi, MD, of Betty and Guy Beatty Center for Integrated Research, Inova Health System, Falls Church, Va., and colleagues.
“There is debate about whether NAFLD is an appropriate name as the term ‘non-alcoholic’ overemphasizes the absence of alcohol use and underemphasizes the importance of the metabolic risk factors which are the main drivers of disease progression,” the investigators wrote in Hepatology. “It has been suggested that MAFLD may better reflect these risk factors. However, such a recommendation is made despite a lack of a general consensus on the definition of ‘metabolic health’ and disagreements in endocrinology circles about the term ‘metabolic syndrome.’ Nevertheless, a few investigators have suggested that MAFLD but not NAFLD is associated with increased fibrosis and mortality.”
To look for clinical differences between the two disease entities, Dr. Younossi and colleagues turned to the National Health and Nutrition Examination Survey (NHANES). Specifically, the NHANES III and NHANES 2017-2018 cohorts were employed, including 12,878 and 4,328 participants, respectively.
MAFLD was defined as FLD with overweight/obesity, evidence of metabolic dysregulation, or type 2 diabetes mellitus. NAFLD was defined as FLD without excessive alcohol consumption or other causes of chronic liver disease. Patients were sorted into four groups: NAFLD, MAFLD, both disease types, or neither disease type. Since the categories were not mutually exclusive, the investigators compared clinical characteristics based on 95% confidence intervals. If no overlap was found, then differences were deemed statistically significant.
Diagnoses of NAFLD and MAFLD were highly concordant (kappa coefficient = 0.83-0.94). After a median of 22.8 years follow-up, no significant differences were found between groups for cause-specific mortality, all-cause mortality, or major clinical characteristics except those inherent to the disease definitions (for example, lack of alcohol use in NAFLD). Greatest risk factors for advanced fibrosis in both groups were obesity, high-risk fibrosis, and type 2 diabetes mellitus.
As anticipated, by definition, alcoholic liver disease and excess alcohol use were documented in approximately 15% of patients with MAFLD, but in no patients with NAFLD. As such, alcoholic liver disease predicted liver-specific mortality for MAFLD (hazard ratio, 4.50; 95% confidence interval, 1.89-10.75) but not NAFLD. Conversely, insulin resistance predicted liver-specific mortality in NAFLD (HR, 3.57; 95% CI, 1.35-9.42) but not MAFLD (HR, 0.84; 95% CI, 0.36-1.95).
“These data do not support the notion that a name change from NAFLD to MAFLD will better capture the risk for long-term outcomes of these patients or better define metabolically at-risk patients who present with FLD,” the investigators concluded. “On the other hand, enlarging the definition to FLD with subcategories of ‘alcoholic,’ ‘non-alcoholic,’ ‘drug-induced,’ etc. has merit and needs to be further considered. In this context, a true international consensus group of experts supported by liver and non-liver scientific societies must undertake an evidence-based and comprehensive approach to this issue and assess both the benefits and risks of changing the name.”
According to Rohit Loomba, MD, director of the NAFLD research center and professor of medicine in the division of gastroenterology and hepatology at University of California, San Diego, the study offers a preview of the consequences if NAFLD were changed to MAFLD, most notably by making alcohol a key driver of outcomes.
“If we change the name of a disease entity ... how does that impact natural history?” Dr. Loomba asked in an interview. “This paper gives you an idea. If you start calling it MAFLD, then people are dying from alcohol use, and they’re not dying from what we are currently seeing patients with NAFLD die of.”
He also noted that the name change could disrupt drug development and outcome measures since most drugs currently in development are directed at nonalcoholic steatohepatitis (NASH).
“Is it worth the headache?” Dr. Loomba asked. “How are we going to define NASH-related fibrosis? That probably will remain the same because the therapies that we will use to address that will remain consistent with what we are currently pursuing. ... It’s probably premature to change the nomenclature before assessing the impact on finding new treatment.”
Dr. Younossi disclosed relationships with BMS, Novartis, Gilead, and others. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myer Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals, and Viking Therapeutics.
Non-alcoholic fatty liver disease (NAFLD) and metabolic associated fatty liver disease (MAFLD) demonstrate highly similar clinical courses and mortality rates, and a name change may not be clinically beneficial, based on data from more than 17,000 patients.
Instead, etiologic subcategorization of fatty liver disease (FLD) should be considered, reported lead author Zobair M. Younossi, MD, of Betty and Guy Beatty Center for Integrated Research, Inova Health System, Falls Church, Va., and colleagues.
“There is debate about whether NAFLD is an appropriate name as the term ‘non-alcoholic’ overemphasizes the absence of alcohol use and underemphasizes the importance of the metabolic risk factors which are the main drivers of disease progression,” the investigators wrote in Hepatology. “It has been suggested that MAFLD may better reflect these risk factors. However, such a recommendation is made despite a lack of a general consensus on the definition of ‘metabolic health’ and disagreements in endocrinology circles about the term ‘metabolic syndrome.’ Nevertheless, a few investigators have suggested that MAFLD but not NAFLD is associated with increased fibrosis and mortality.”
To look for clinical differences between the two disease entities, Dr. Younossi and colleagues turned to the National Health and Nutrition Examination Survey (NHANES). Specifically, the NHANES III and NHANES 2017-2018 cohorts were employed, including 12,878 and 4,328 participants, respectively.
MAFLD was defined as FLD with overweight/obesity, evidence of metabolic dysregulation, or type 2 diabetes mellitus. NAFLD was defined as FLD without excessive alcohol consumption or other causes of chronic liver disease. Patients were sorted into four groups: NAFLD, MAFLD, both disease types, or neither disease type. Since the categories were not mutually exclusive, the investigators compared clinical characteristics based on 95% confidence intervals. If no overlap was found, then differences were deemed statistically significant.
Diagnoses of NAFLD and MAFLD were highly concordant (kappa coefficient = 0.83-0.94). After a median of 22.8 years follow-up, no significant differences were found between groups for cause-specific mortality, all-cause mortality, or major clinical characteristics except those inherent to the disease definitions (for example, lack of alcohol use in NAFLD). Greatest risk factors for advanced fibrosis in both groups were obesity, high-risk fibrosis, and type 2 diabetes mellitus.
As anticipated, by definition, alcoholic liver disease and excess alcohol use were documented in approximately 15% of patients with MAFLD, but in no patients with NAFLD. As such, alcoholic liver disease predicted liver-specific mortality for MAFLD (hazard ratio, 4.50; 95% confidence interval, 1.89-10.75) but not NAFLD. Conversely, insulin resistance predicted liver-specific mortality in NAFLD (HR, 3.57; 95% CI, 1.35-9.42) but not MAFLD (HR, 0.84; 95% CI, 0.36-1.95).
“These data do not support the notion that a name change from NAFLD to MAFLD will better capture the risk for long-term outcomes of these patients or better define metabolically at-risk patients who present with FLD,” the investigators concluded. “On the other hand, enlarging the definition to FLD with subcategories of ‘alcoholic,’ ‘non-alcoholic,’ ‘drug-induced,’ etc. has merit and needs to be further considered. In this context, a true international consensus group of experts supported by liver and non-liver scientific societies must undertake an evidence-based and comprehensive approach to this issue and assess both the benefits and risks of changing the name.”
According to Rohit Loomba, MD, director of the NAFLD research center and professor of medicine in the division of gastroenterology and hepatology at University of California, San Diego, the study offers a preview of the consequences if NAFLD were changed to MAFLD, most notably by making alcohol a key driver of outcomes.
“If we change the name of a disease entity ... how does that impact natural history?” Dr. Loomba asked in an interview. “This paper gives you an idea. If you start calling it MAFLD, then people are dying from alcohol use, and they’re not dying from what we are currently seeing patients with NAFLD die of.”
He also noted that the name change could disrupt drug development and outcome measures since most drugs currently in development are directed at nonalcoholic steatohepatitis (NASH).
“Is it worth the headache?” Dr. Loomba asked. “How are we going to define NASH-related fibrosis? That probably will remain the same because the therapies that we will use to address that will remain consistent with what we are currently pursuing. ... It’s probably premature to change the nomenclature before assessing the impact on finding new treatment.”
Dr. Younossi disclosed relationships with BMS, Novartis, Gilead, and others. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myer Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals, and Viking Therapeutics.
Non-alcoholic fatty liver disease (NAFLD) and metabolic associated fatty liver disease (MAFLD) demonstrate highly similar clinical courses and mortality rates, and a name change may not be clinically beneficial, based on data from more than 17,000 patients.
Instead, etiologic subcategorization of fatty liver disease (FLD) should be considered, reported lead author Zobair M. Younossi, MD, of Betty and Guy Beatty Center for Integrated Research, Inova Health System, Falls Church, Va., and colleagues.
“There is debate about whether NAFLD is an appropriate name as the term ‘non-alcoholic’ overemphasizes the absence of alcohol use and underemphasizes the importance of the metabolic risk factors which are the main drivers of disease progression,” the investigators wrote in Hepatology. “It has been suggested that MAFLD may better reflect these risk factors. However, such a recommendation is made despite a lack of a general consensus on the definition of ‘metabolic health’ and disagreements in endocrinology circles about the term ‘metabolic syndrome.’ Nevertheless, a few investigators have suggested that MAFLD but not NAFLD is associated with increased fibrosis and mortality.”
To look for clinical differences between the two disease entities, Dr. Younossi and colleagues turned to the National Health and Nutrition Examination Survey (NHANES). Specifically, the NHANES III and NHANES 2017-2018 cohorts were employed, including 12,878 and 4,328 participants, respectively.
MAFLD was defined as FLD with overweight/obesity, evidence of metabolic dysregulation, or type 2 diabetes mellitus. NAFLD was defined as FLD without excessive alcohol consumption or other causes of chronic liver disease. Patients were sorted into four groups: NAFLD, MAFLD, both disease types, or neither disease type. Since the categories were not mutually exclusive, the investigators compared clinical characteristics based on 95% confidence intervals. If no overlap was found, then differences were deemed statistically significant.
Diagnoses of NAFLD and MAFLD were highly concordant (kappa coefficient = 0.83-0.94). After a median of 22.8 years follow-up, no significant differences were found between groups for cause-specific mortality, all-cause mortality, or major clinical characteristics except those inherent to the disease definitions (for example, lack of alcohol use in NAFLD). Greatest risk factors for advanced fibrosis in both groups were obesity, high-risk fibrosis, and type 2 diabetes mellitus.
As anticipated, by definition, alcoholic liver disease and excess alcohol use were documented in approximately 15% of patients with MAFLD, but in no patients with NAFLD. As such, alcoholic liver disease predicted liver-specific mortality for MAFLD (hazard ratio, 4.50; 95% confidence interval, 1.89-10.75) but not NAFLD. Conversely, insulin resistance predicted liver-specific mortality in NAFLD (HR, 3.57; 95% CI, 1.35-9.42) but not MAFLD (HR, 0.84; 95% CI, 0.36-1.95).
“These data do not support the notion that a name change from NAFLD to MAFLD will better capture the risk for long-term outcomes of these patients or better define metabolically at-risk patients who present with FLD,” the investigators concluded. “On the other hand, enlarging the definition to FLD with subcategories of ‘alcoholic,’ ‘non-alcoholic,’ ‘drug-induced,’ etc. has merit and needs to be further considered. In this context, a true international consensus group of experts supported by liver and non-liver scientific societies must undertake an evidence-based and comprehensive approach to this issue and assess both the benefits and risks of changing the name.”
According to Rohit Loomba, MD, director of the NAFLD research center and professor of medicine in the division of gastroenterology and hepatology at University of California, San Diego, the study offers a preview of the consequences if NAFLD were changed to MAFLD, most notably by making alcohol a key driver of outcomes.
“If we change the name of a disease entity ... how does that impact natural history?” Dr. Loomba asked in an interview. “This paper gives you an idea. If you start calling it MAFLD, then people are dying from alcohol use, and they’re not dying from what we are currently seeing patients with NAFLD die of.”
He also noted that the name change could disrupt drug development and outcome measures since most drugs currently in development are directed at nonalcoholic steatohepatitis (NASH).
“Is it worth the headache?” Dr. Loomba asked. “How are we going to define NASH-related fibrosis? That probably will remain the same because the therapies that we will use to address that will remain consistent with what we are currently pursuing. ... It’s probably premature to change the nomenclature before assessing the impact on finding new treatment.”
Dr. Younossi disclosed relationships with BMS, Novartis, Gilead, and others. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myer Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89 bio, Terns Pharmaceuticals, and Viking Therapeutics.
FROM HEPATOLOGY
AGA Clinical Practice Update: Expert review of dietary options for IBS
The American Gastroenterological Association has published a clinical practice update on dietary interventions for patients with irritable bowel syndrome (IBS). The topics range from identification of suitable candidates for dietary interventions, to levels of evidence for specific diets, which are becoming increasingly recognized for their key role in managing patients with IBS, according to lead author William D. Chey, MD, of the University of Michigan, Ann Arbor, and colleagues.
“Most medical therapies for IBS improve global symptoms in fewer than one-half of patients, with a therapeutic gain of 7%-15% over placebo,” the researchers wrote in Gastroenterology. “Most patients with IBS associate their GI symptoms with eating food.”
According to Dr. Chey and colleagues, clinicians who are considering dietary modifications for treating IBS should first recognize the inherent challenges presented by this process and be aware that new diets won’t work for everyone.
“Specialty diets require planning and preparation, which may be impractical for some patients,” they wrote, noting that individuals with “decreased cognitive abilities and significant psychiatric disease” may be unable to follow diets or interpret their own responses to specific foods. Special diets may also be inappropriate for patients with financial constraints, and “should be avoided in patients with an eating disorder.”
Because of the challenges involved in dietary interventions, Dr. Chey and colleagues advised clinical support from a registered dietitian nutritionist or other resource.
Patients who are suitable candidates for intervention and willing to try a new diet should first provide information about their current eating habits. A food trial can then be personalized and implemented for a predetermined amount of time. If the patient does not respond, then the diet should be stopped and changed to a new diet or another intervention.
Dr. Chey and colleagues discussed three specific dietary interventions and their corresponding levels of evidence: soluble fiber; the low-fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) diet; and a gluten-free diet.
“Soluble fiber is efficacious in treating global symptoms of IBS,” they wrote, citing 15 randomized controlled trials. Soluble fiber is most suitable for patients with constipation-predominant IBS, and different soluble fibers may yield different outcomes based on characteristics such as rate of fermentation and viscosity. In contrast, insoluble fiber is unlikely to help with IBS, and may worsen abdominal pain and bloating.
The low-FODMAP diet is “currently the most evidence-based diet intervention for IBS,” especially for patients with diarrhea-predominant IBS. Dr. Chey and colleagues offered a clear roadmap for employing the diet. First, patients should eat only low-FODMAP foods for 4-6 weeks. If symptoms don’t improve, the diet should be stopped. If symptoms do improve, foods containing a single FODMAP should be reintroduced one at a time, each in increasing quantities over 3 days, alongside documentation of symptom responses. Finally, the diet should be personalized based on these responses. The majority of patients (close to 80%) “can liberalize” a low-FODMAP diet based on their responses.
In contrast with the low-FODMAP diet, which has a relatively solid body of supporting evidence, efficacy data are still limited for treating IBS with a gluten-free diet. “Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results,” Dr. Chey and colleagues explained.
Their report cited a recent monograph on the topic that concluded that gluten-free eating offered no significant benefit over placebo (relative risk, 0.46; 95% confidence interval, 0.16-1.28). While some studies have documented positive results with a gluten-free diet, Dr. Chey and colleagues suggested that confounding variables such as the nocebo effect and the impact of other dietary factors have yet to be ruled out. “At present, it remains unclear whether a gluten-free diet is of benefit to patients with IBS.”
Dr. Chey and colleagues also explored IBS biomarkers. While some early data have shown that biomarkers may predict dietary responses, “there is insufficient evidence to support their routine use in clinical practice. ... Further efforts to identify and validate biomarkers that predict response to dietary interventions are needed to deliver ‘personalized nutrition.’ ”
The clinical practice update was commissioned and approved by the AGA CPU Committee and the AGA Governing Board. The researchers disclosed relationships with Biomerica, Salix, Mauna Kea Technologies, and others.
This article was updated May 19, 2022.
The American Gastroenterological Association has published a clinical practice update on dietary interventions for patients with irritable bowel syndrome (IBS). The topics range from identification of suitable candidates for dietary interventions, to levels of evidence for specific diets, which are becoming increasingly recognized for their key role in managing patients with IBS, according to lead author William D. Chey, MD, of the University of Michigan, Ann Arbor, and colleagues.
“Most medical therapies for IBS improve global symptoms in fewer than one-half of patients, with a therapeutic gain of 7%-15% over placebo,” the researchers wrote in Gastroenterology. “Most patients with IBS associate their GI symptoms with eating food.”
According to Dr. Chey and colleagues, clinicians who are considering dietary modifications for treating IBS should first recognize the inherent challenges presented by this process and be aware that new diets won’t work for everyone.
“Specialty diets require planning and preparation, which may be impractical for some patients,” they wrote, noting that individuals with “decreased cognitive abilities and significant psychiatric disease” may be unable to follow diets or interpret their own responses to specific foods. Special diets may also be inappropriate for patients with financial constraints, and “should be avoided in patients with an eating disorder.”
Because of the challenges involved in dietary interventions, Dr. Chey and colleagues advised clinical support from a registered dietitian nutritionist or other resource.
Patients who are suitable candidates for intervention and willing to try a new diet should first provide information about their current eating habits. A food trial can then be personalized and implemented for a predetermined amount of time. If the patient does not respond, then the diet should be stopped and changed to a new diet or another intervention.
Dr. Chey and colleagues discussed three specific dietary interventions and their corresponding levels of evidence: soluble fiber; the low-fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) diet; and a gluten-free diet.
“Soluble fiber is efficacious in treating global symptoms of IBS,” they wrote, citing 15 randomized controlled trials. Soluble fiber is most suitable for patients with constipation-predominant IBS, and different soluble fibers may yield different outcomes based on characteristics such as rate of fermentation and viscosity. In contrast, insoluble fiber is unlikely to help with IBS, and may worsen abdominal pain and bloating.
The low-FODMAP diet is “currently the most evidence-based diet intervention for IBS,” especially for patients with diarrhea-predominant IBS. Dr. Chey and colleagues offered a clear roadmap for employing the diet. First, patients should eat only low-FODMAP foods for 4-6 weeks. If symptoms don’t improve, the diet should be stopped. If symptoms do improve, foods containing a single FODMAP should be reintroduced one at a time, each in increasing quantities over 3 days, alongside documentation of symptom responses. Finally, the diet should be personalized based on these responses. The majority of patients (close to 80%) “can liberalize” a low-FODMAP diet based on their responses.
In contrast with the low-FODMAP diet, which has a relatively solid body of supporting evidence, efficacy data are still limited for treating IBS with a gluten-free diet. “Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results,” Dr. Chey and colleagues explained.
Their report cited a recent monograph on the topic that concluded that gluten-free eating offered no significant benefit over placebo (relative risk, 0.46; 95% confidence interval, 0.16-1.28). While some studies have documented positive results with a gluten-free diet, Dr. Chey and colleagues suggested that confounding variables such as the nocebo effect and the impact of other dietary factors have yet to be ruled out. “At present, it remains unclear whether a gluten-free diet is of benefit to patients with IBS.”
Dr. Chey and colleagues also explored IBS biomarkers. While some early data have shown that biomarkers may predict dietary responses, “there is insufficient evidence to support their routine use in clinical practice. ... Further efforts to identify and validate biomarkers that predict response to dietary interventions are needed to deliver ‘personalized nutrition.’ ”
The clinical practice update was commissioned and approved by the AGA CPU Committee and the AGA Governing Board. The researchers disclosed relationships with Biomerica, Salix, Mauna Kea Technologies, and others.
This article was updated May 19, 2022.
The American Gastroenterological Association has published a clinical practice update on dietary interventions for patients with irritable bowel syndrome (IBS). The topics range from identification of suitable candidates for dietary interventions, to levels of evidence for specific diets, which are becoming increasingly recognized for their key role in managing patients with IBS, according to lead author William D. Chey, MD, of the University of Michigan, Ann Arbor, and colleagues.
“Most medical therapies for IBS improve global symptoms in fewer than one-half of patients, with a therapeutic gain of 7%-15% over placebo,” the researchers wrote in Gastroenterology. “Most patients with IBS associate their GI symptoms with eating food.”
According to Dr. Chey and colleagues, clinicians who are considering dietary modifications for treating IBS should first recognize the inherent challenges presented by this process and be aware that new diets won’t work for everyone.
“Specialty diets require planning and preparation, which may be impractical for some patients,” they wrote, noting that individuals with “decreased cognitive abilities and significant psychiatric disease” may be unable to follow diets or interpret their own responses to specific foods. Special diets may also be inappropriate for patients with financial constraints, and “should be avoided in patients with an eating disorder.”
Because of the challenges involved in dietary interventions, Dr. Chey and colleagues advised clinical support from a registered dietitian nutritionist or other resource.
Patients who are suitable candidates for intervention and willing to try a new diet should first provide information about their current eating habits. A food trial can then be personalized and implemented for a predetermined amount of time. If the patient does not respond, then the diet should be stopped and changed to a new diet or another intervention.
Dr. Chey and colleagues discussed three specific dietary interventions and their corresponding levels of evidence: soluble fiber; the low-fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) diet; and a gluten-free diet.
“Soluble fiber is efficacious in treating global symptoms of IBS,” they wrote, citing 15 randomized controlled trials. Soluble fiber is most suitable for patients with constipation-predominant IBS, and different soluble fibers may yield different outcomes based on characteristics such as rate of fermentation and viscosity. In contrast, insoluble fiber is unlikely to help with IBS, and may worsen abdominal pain and bloating.
The low-FODMAP diet is “currently the most evidence-based diet intervention for IBS,” especially for patients with diarrhea-predominant IBS. Dr. Chey and colleagues offered a clear roadmap for employing the diet. First, patients should eat only low-FODMAP foods for 4-6 weeks. If symptoms don’t improve, the diet should be stopped. If symptoms do improve, foods containing a single FODMAP should be reintroduced one at a time, each in increasing quantities over 3 days, alongside documentation of symptom responses. Finally, the diet should be personalized based on these responses. The majority of patients (close to 80%) “can liberalize” a low-FODMAP diet based on their responses.
In contrast with the low-FODMAP diet, which has a relatively solid body of supporting evidence, efficacy data are still limited for treating IBS with a gluten-free diet. “Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results,” Dr. Chey and colleagues explained.
Their report cited a recent monograph on the topic that concluded that gluten-free eating offered no significant benefit over placebo (relative risk, 0.46; 95% confidence interval, 0.16-1.28). While some studies have documented positive results with a gluten-free diet, Dr. Chey and colleagues suggested that confounding variables such as the nocebo effect and the impact of other dietary factors have yet to be ruled out. “At present, it remains unclear whether a gluten-free diet is of benefit to patients with IBS.”
Dr. Chey and colleagues also explored IBS biomarkers. While some early data have shown that biomarkers may predict dietary responses, “there is insufficient evidence to support their routine use in clinical practice. ... Further efforts to identify and validate biomarkers that predict response to dietary interventions are needed to deliver ‘personalized nutrition.’ ”
The clinical practice update was commissioned and approved by the AGA CPU Committee and the AGA Governing Board. The researchers disclosed relationships with Biomerica, Salix, Mauna Kea Technologies, and others.
This article was updated May 19, 2022.
FROM GASTROENTEROLOGY
Study casts doubt on safety, efficacy of L-serine supplementation for AD
When given to patients with AD, L-serine supplements could be driving abnormally increased serine levels in the brain even higher, potentially accelerating neuronal death, according to study author Xu Chen, PhD, of the University of California, San Diego, and colleagues.
This conclusion conflicts with a 2020 study by Juliette Le Douce, PhD, and colleagues, who reported that oral L-serine supplementation may act as a “ready-to-use therapy” for AD, based on their findings that patients with AD had low levels of PHGDH, an enzyme necessary for synthesizing serine, and AD-like mice had low levels of serine.
Writing in Cell Metabolism, Dr. Chen and colleagues framed the present study, and their findings, in this context.
“In contrast to the work of Le Douce et al., here we report that PHGDH mRNA and protein levels are increased in the brains of two mouse models of AD and/or tauopathy, and are also progressively increased in human brains with no, early, and late AD pathology, as well as in people with no, asymptomatic, and symptomatic AD,” they wrote.
They suggested adjusting clinical recommendations for L-serine, the form of the amino acid commonly found in supplements. In the body, L-serine is converted to D-serine, which acts on the NMDA receptor (NMDAR).
‘Long-term use of D-serine contributes to neuronal death’ suggests research
“We feel oral L-serine as a ready-to-use therapy to AD warrants precaution,” Dr. Chen and colleagues wrote. “This is because despite being a cognitive enhancer, some [research] suggests that long-term use of D-serine contributes to neuronal death in AD through excitotoxicity. Furthermore, D-serine, as a co-agonist of NMDAR, would be expected to oppose NMDAR antagonists, which have proven clinical benefits in treating AD.”
According to principal author Sheng Zhong, PhD, of the University of California, San Diego, “Research is needed to test if targeting PHGDH can ameliorate cognitive decline in AD.”
Dr. Zhong also noted that the present findings support the “promise of using a specific RNA in blood as a biomarker for early detection of Alzheimer’s disease.” This approach is currently being validated at UCSD Shiley-Marcos Alzheimer’s Disease Research Center, he added.
Roles of PHGDH and serine in Alzheimer’s disease require further study
Commenting on both studies, Steve W. Barger, PhD, of the University of Arkansas for Medical Sciences, Little Rock, suggested that more work is needed to better understand the roles of PHGDH and serine in AD before clinical applications can be considered.
“In the end, these two studies fail to provide the clarity we need in designing evidence-based therapeutic hypotheses,” Dr. Barger said in an interview. “We still do not have a firm grasp on the role that D-serine plays in AD. Indeed, the evidence regarding even a single enzyme contributing to its levels is ambiguous.”
Dr. Barger, who has published extensively on the topic of neuronal death, with a particular focus on Alzheimer’s disease, noted that “determination of what happens to D-serine levels in AD has been of interest for decades,” but levels of the amino acid have been notoriously challenging to measure because “D-serine can disappear rapidly from the brain and its fluids after death.”
While Dr. Le Douce and colleagues did measure levels of serine in mice, Dr. Barger noted that the study by Dr. Chen and colleagues was conducted with more “quantitatively rigorous methods.” Even though Dr. Chen and colleagues “did not assay the levels of D-serine itself ... the implication of their findings is that PHGDH is poised to elevate this critical neurotransmitter,” leading to their conclusion that serine supplementation is “potentially dangerous.”
At this point, it may be too early to tell, according to Dr. Barger.
He suggested that conclusions drawn from PHGDH levels alone are “always limited,” and conclusions based on serine levels may be equally dubious, considering that the activities and effects of serine “are quite complex,” and may be influenced by other physiologic processes, including the effects of gut bacteria.
Instead, Dr. Barger suggested that changes in PHGDH and serine may be interpreted as signals coming from a more relevant process upstream: glucose metabolism.
“What we can say confidently is that the glucose metabolism that PHGDH connects to D-serine is most definitely a factor in AD,” he said. “Countless studies have documented what now appears to be a universal decline in glucose delivery to the cerebral cortex, even before frank dementia sets in.”
Dr. Barger noted that declining glucose delivery coincides with some of the earliest events in the development of AD, perhaps “linking accumulation of amyloid β-peptide to subsequent neurofibrillary tangles and tissue atrophy.”
Dr. Barger’s own work recently demonstrated that AD is associated with “an irregularity in the insertion of a specific glucose transporter (GLUT1) into the cell surface” of astrocytes.
“It could be more effective to direct therapeutic interventions at these events lying upstream of PHGDH or serine,” he concluded.
The study was partly supported by a Kreuger v. Wyeth research award. The investigators and Dr. Barger reported no conflicts of interest.
When given to patients with AD, L-serine supplements could be driving abnormally increased serine levels in the brain even higher, potentially accelerating neuronal death, according to study author Xu Chen, PhD, of the University of California, San Diego, and colleagues.
This conclusion conflicts with a 2020 study by Juliette Le Douce, PhD, and colleagues, who reported that oral L-serine supplementation may act as a “ready-to-use therapy” for AD, based on their findings that patients with AD had low levels of PHGDH, an enzyme necessary for synthesizing serine, and AD-like mice had low levels of serine.
Writing in Cell Metabolism, Dr. Chen and colleagues framed the present study, and their findings, in this context.
“In contrast to the work of Le Douce et al., here we report that PHGDH mRNA and protein levels are increased in the brains of two mouse models of AD and/or tauopathy, and are also progressively increased in human brains with no, early, and late AD pathology, as well as in people with no, asymptomatic, and symptomatic AD,” they wrote.
They suggested adjusting clinical recommendations for L-serine, the form of the amino acid commonly found in supplements. In the body, L-serine is converted to D-serine, which acts on the NMDA receptor (NMDAR).
‘Long-term use of D-serine contributes to neuronal death’ suggests research
“We feel oral L-serine as a ready-to-use therapy to AD warrants precaution,” Dr. Chen and colleagues wrote. “This is because despite being a cognitive enhancer, some [research] suggests that long-term use of D-serine contributes to neuronal death in AD through excitotoxicity. Furthermore, D-serine, as a co-agonist of NMDAR, would be expected to oppose NMDAR antagonists, which have proven clinical benefits in treating AD.”
According to principal author Sheng Zhong, PhD, of the University of California, San Diego, “Research is needed to test if targeting PHGDH can ameliorate cognitive decline in AD.”
Dr. Zhong also noted that the present findings support the “promise of using a specific RNA in blood as a biomarker for early detection of Alzheimer’s disease.” This approach is currently being validated at UCSD Shiley-Marcos Alzheimer’s Disease Research Center, he added.
Roles of PHGDH and serine in Alzheimer’s disease require further study
Commenting on both studies, Steve W. Barger, PhD, of the University of Arkansas for Medical Sciences, Little Rock, suggested that more work is needed to better understand the roles of PHGDH and serine in AD before clinical applications can be considered.
“In the end, these two studies fail to provide the clarity we need in designing evidence-based therapeutic hypotheses,” Dr. Barger said in an interview. “We still do not have a firm grasp on the role that D-serine plays in AD. Indeed, the evidence regarding even a single enzyme contributing to its levels is ambiguous.”
Dr. Barger, who has published extensively on the topic of neuronal death, with a particular focus on Alzheimer’s disease, noted that “determination of what happens to D-serine levels in AD has been of interest for decades,” but levels of the amino acid have been notoriously challenging to measure because “D-serine can disappear rapidly from the brain and its fluids after death.”
While Dr. Le Douce and colleagues did measure levels of serine in mice, Dr. Barger noted that the study by Dr. Chen and colleagues was conducted with more “quantitatively rigorous methods.” Even though Dr. Chen and colleagues “did not assay the levels of D-serine itself ... the implication of their findings is that PHGDH is poised to elevate this critical neurotransmitter,” leading to their conclusion that serine supplementation is “potentially dangerous.”
At this point, it may be too early to tell, according to Dr. Barger.
He suggested that conclusions drawn from PHGDH levels alone are “always limited,” and conclusions based on serine levels may be equally dubious, considering that the activities and effects of serine “are quite complex,” and may be influenced by other physiologic processes, including the effects of gut bacteria.
Instead, Dr. Barger suggested that changes in PHGDH and serine may be interpreted as signals coming from a more relevant process upstream: glucose metabolism.
“What we can say confidently is that the glucose metabolism that PHGDH connects to D-serine is most definitely a factor in AD,” he said. “Countless studies have documented what now appears to be a universal decline in glucose delivery to the cerebral cortex, even before frank dementia sets in.”
Dr. Barger noted that declining glucose delivery coincides with some of the earliest events in the development of AD, perhaps “linking accumulation of amyloid β-peptide to subsequent neurofibrillary tangles and tissue atrophy.”
Dr. Barger’s own work recently demonstrated that AD is associated with “an irregularity in the insertion of a specific glucose transporter (GLUT1) into the cell surface” of astrocytes.
“It could be more effective to direct therapeutic interventions at these events lying upstream of PHGDH or serine,” he concluded.
The study was partly supported by a Kreuger v. Wyeth research award. The investigators and Dr. Barger reported no conflicts of interest.
When given to patients with AD, L-serine supplements could be driving abnormally increased serine levels in the brain even higher, potentially accelerating neuronal death, according to study author Xu Chen, PhD, of the University of California, San Diego, and colleagues.
This conclusion conflicts with a 2020 study by Juliette Le Douce, PhD, and colleagues, who reported that oral L-serine supplementation may act as a “ready-to-use therapy” for AD, based on their findings that patients with AD had low levels of PHGDH, an enzyme necessary for synthesizing serine, and AD-like mice had low levels of serine.
Writing in Cell Metabolism, Dr. Chen and colleagues framed the present study, and their findings, in this context.
“In contrast to the work of Le Douce et al., here we report that PHGDH mRNA and protein levels are increased in the brains of two mouse models of AD and/or tauopathy, and are also progressively increased in human brains with no, early, and late AD pathology, as well as in people with no, asymptomatic, and symptomatic AD,” they wrote.
They suggested adjusting clinical recommendations for L-serine, the form of the amino acid commonly found in supplements. In the body, L-serine is converted to D-serine, which acts on the NMDA receptor (NMDAR).
‘Long-term use of D-serine contributes to neuronal death’ suggests research
“We feel oral L-serine as a ready-to-use therapy to AD warrants precaution,” Dr. Chen and colleagues wrote. “This is because despite being a cognitive enhancer, some [research] suggests that long-term use of D-serine contributes to neuronal death in AD through excitotoxicity. Furthermore, D-serine, as a co-agonist of NMDAR, would be expected to oppose NMDAR antagonists, which have proven clinical benefits in treating AD.”
According to principal author Sheng Zhong, PhD, of the University of California, San Diego, “Research is needed to test if targeting PHGDH can ameliorate cognitive decline in AD.”
Dr. Zhong also noted that the present findings support the “promise of using a specific RNA in blood as a biomarker for early detection of Alzheimer’s disease.” This approach is currently being validated at UCSD Shiley-Marcos Alzheimer’s Disease Research Center, he added.
Roles of PHGDH and serine in Alzheimer’s disease require further study
Commenting on both studies, Steve W. Barger, PhD, of the University of Arkansas for Medical Sciences, Little Rock, suggested that more work is needed to better understand the roles of PHGDH and serine in AD before clinical applications can be considered.
“In the end, these two studies fail to provide the clarity we need in designing evidence-based therapeutic hypotheses,” Dr. Barger said in an interview. “We still do not have a firm grasp on the role that D-serine plays in AD. Indeed, the evidence regarding even a single enzyme contributing to its levels is ambiguous.”
Dr. Barger, who has published extensively on the topic of neuronal death, with a particular focus on Alzheimer’s disease, noted that “determination of what happens to D-serine levels in AD has been of interest for decades,” but levels of the amino acid have been notoriously challenging to measure because “D-serine can disappear rapidly from the brain and its fluids after death.”
While Dr. Le Douce and colleagues did measure levels of serine in mice, Dr. Barger noted that the study by Dr. Chen and colleagues was conducted with more “quantitatively rigorous methods.” Even though Dr. Chen and colleagues “did not assay the levels of D-serine itself ... the implication of their findings is that PHGDH is poised to elevate this critical neurotransmitter,” leading to their conclusion that serine supplementation is “potentially dangerous.”
At this point, it may be too early to tell, according to Dr. Barger.
He suggested that conclusions drawn from PHGDH levels alone are “always limited,” and conclusions based on serine levels may be equally dubious, considering that the activities and effects of serine “are quite complex,” and may be influenced by other physiologic processes, including the effects of gut bacteria.
Instead, Dr. Barger suggested that changes in PHGDH and serine may be interpreted as signals coming from a more relevant process upstream: glucose metabolism.
“What we can say confidently is that the glucose metabolism that PHGDH connects to D-serine is most definitely a factor in AD,” he said. “Countless studies have documented what now appears to be a universal decline in glucose delivery to the cerebral cortex, even before frank dementia sets in.”
Dr. Barger noted that declining glucose delivery coincides with some of the earliest events in the development of AD, perhaps “linking accumulation of amyloid β-peptide to subsequent neurofibrillary tangles and tissue atrophy.”
Dr. Barger’s own work recently demonstrated that AD is associated with “an irregularity in the insertion of a specific glucose transporter (GLUT1) into the cell surface” of astrocytes.
“It could be more effective to direct therapeutic interventions at these events lying upstream of PHGDH or serine,” he concluded.
The study was partly supported by a Kreuger v. Wyeth research award. The investigators and Dr. Barger reported no conflicts of interest.
FROM CELL METABOLISM