User login
Richard Pizzi is editor of The Hospitalist. He has been an editor at Frontline Medical Communications since 2015, and previously served as editor of MDedge publications Hospitalist News and ID Practitioner. He has also worked as an editor and in editorial management roles for HIMSS Media, MedTech Media, and the American Association for Clinical Chemistry. Follow him on Twitter @richpizzi
HIV research update: Early May 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Viral load measurements can be used to predict if an HIV-infected patient will be suppressed by 6-months after starting combination antiretroviral therapy, according to a study in the journal AIDS. The investigators said graphical presentations of this information could help clinicians decide the optimum time to switch treatment regimen during the first months of cART.
A study in The Lancet HIV shows the first application of an automated phylogenetic system monitoring a clinical database to detect a recent HIV outbreak and support the ensuing public health response. The authors said that by making secondary use of routinely collected HIV genotypes, such an approach is cost-effective, attains near real-time monitoring of new cases, and can be implemented in all settings in which HIV genotyping is the standard of care.
According to a study in Epidemiology & Infection, statistical models of risk for skin and soft tissue infection (SSTIs) in HIV patients may yield biased results if they do not account for how HIV viral load may be a marker of adherence to trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis. TMP-SMX is prescribed to many severely immunocompromised HIV patients and is potentially protective against SSTIs.
The treatment failure misclassification rate in HIV-infected Kenyan children was 21% for the 2006 World Health Organization treatment guidelines and 46% for the 2010/2013 guidelines, according to a recent analysis. Investigators said the findings support current WHO recommendations for routine viral load monitoring but not necessarily the proposed CD4 thresholds.
Doravirine, a new non-nucleoside reverse transcriptase inhibitor in phase III clinical trials, is susceptible to a number of well-known NNRTI resistance mutations, reports a study in JAIDS. The authors said an understanding of the mutational susceptibilities and binding interactions of NNRTIs with reverse transcriptase could be used to develop pairs of compounds with nonoverlapping mutational susceptibilities.
The pharmacokinetics of the antiretroviral drug abacavir, prescribed at 600 mg once daily, in pregnant HIV-infected women are equivalent to those post partum, according to a study in the journal AIDS. No dose adjustments are required during pregnancy and similar antiviral activity is expected, researchers said.
A recent study describes the processes by which the SMILE Program, with Connect-to-Protect community coalitions – which are affiliated with the Adolescent Trials Network for HIV/AIDS Interventions – addressed structural barriers that prevented HIV testing, linkage, and engagement in HIV health care among young people.
Serial HIV viral load measures are a valid source for estimating antiretroviral initiation, a study published in JAIDS confirmed. The investigators said a definition that includes a >=1-log viral load decline or a change from detectable to undetectable viral load performed best.
The acceptability of the HPV vaccine was high among HIV-negative men who have sex with men in Ireland, based on no cost vaccine and on stated vaccine efficacy (78%). Higher cost was negatively associated with vaccine acceptability, researchers reported.
Most HIV-infected people discontinuing therapy release a diverse population of virus, and this released virus has entry features of virus selected for replication in CD4+ T cells rather than myeloid cells, according to a report in the Journal of Infectious Diseases.
The majority of new HIV-infected patients in a Ugandan study who screened positive for suspected TB did not have a sputum order, and those who did were more likely to have more advanced HIV disease and symptoms. The authors said improved evaluation of provider behavior in the management of TB screen positive patients could improve active TB case detection rates.
Researchers writing in JAIDS said etravirine 200 mg twice daily, as part of individualized combination antiretroviral therapy, may be a treatment option for HIV-1-infected pregnant women.
Offering single-visit antiretroviral therapy initiation to adult patients in South Africa increased uptake of ART by 36% and viral suppression by 26%, a study in PLOS Medicine revealed. The authors said this intervention should be considered for adoption in the public sector in Africa.
Elevated levels of invariant natural killer T (iNKT) cell and natural killer (NK) cell activation are associated with viremia and disease progression markers in both HIV-1 and HIV-2 infections, according to a study in AIDS.
A study of 22 German HIV clinics demonstrated the noninferiority of ritonavir-boosted darunavir (DRV/r) therapy to standard of care, and said DRV/r should be included as a standard component of recommended regimens in postexposure prophylaxis guidelines.
A study in a large pediatric HIV care setting in Botswana found that children “lost to follow-up” (LTFU) were more likely than were controls to have advanced disease and greater immunosuppression, and to not be receiving antiretroviral therapy. Socioeconomic and psychosocial factors were listed as characteristic of children LTFU but not of controls.
A study published in JAIDS showed that psychosocial conditions such as intimate partner violence fuel HIV incidence among Latino men who have sex with men, and psychosocial interventions should be considered to reduce HIV disparities in this population.
Virologic failure is uncommon in individuals who initiate antiretroviral therapy during acute HIV infection, according to a study in Thailand. The authors said this shows that ART initiation during acute HIV infection is efficacious and clinicians can monitor for virologic failure after 24 weeks of therapy.
In children with slow-progressing HIV, there is a substantial burden of chronic morbidity even when CD4 count is relatively preserved, researchers reported in JAIDS. They said timely HIV testing and prompt antiretroviral initiation are urgently needed to prevent development of chronic complications.
A better understanding of patient-level HIV-related outcomes across different staffing models, and among different patient populations and geographic locations, is urgently needed to improve HIV disease management, according to a study in AIDS Care.
A study in the journal AIDS found that short treatment interruption did not compromise 18-month CD4%, viral control, growth, or morbidity compared to continued antiretroviral therapy among infants who started ART in early HIV infection.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Viral load measurements can be used to predict if an HIV-infected patient will be suppressed by 6-months after starting combination antiretroviral therapy, according to a study in the journal AIDS. The investigators said graphical presentations of this information could help clinicians decide the optimum time to switch treatment regimen during the first months of cART.
A study in The Lancet HIV shows the first application of an automated phylogenetic system monitoring a clinical database to detect a recent HIV outbreak and support the ensuing public health response. The authors said that by making secondary use of routinely collected HIV genotypes, such an approach is cost-effective, attains near real-time monitoring of new cases, and can be implemented in all settings in which HIV genotyping is the standard of care.
According to a study in Epidemiology & Infection, statistical models of risk for skin and soft tissue infection (SSTIs) in HIV patients may yield biased results if they do not account for how HIV viral load may be a marker of adherence to trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis. TMP-SMX is prescribed to many severely immunocompromised HIV patients and is potentially protective against SSTIs.
The treatment failure misclassification rate in HIV-infected Kenyan children was 21% for the 2006 World Health Organization treatment guidelines and 46% for the 2010/2013 guidelines, according to a recent analysis. Investigators said the findings support current WHO recommendations for routine viral load monitoring but not necessarily the proposed CD4 thresholds.
Doravirine, a new non-nucleoside reverse transcriptase inhibitor in phase III clinical trials, is susceptible to a number of well-known NNRTI resistance mutations, reports a study in JAIDS. The authors said an understanding of the mutational susceptibilities and binding interactions of NNRTIs with reverse transcriptase could be used to develop pairs of compounds with nonoverlapping mutational susceptibilities.
The pharmacokinetics of the antiretroviral drug abacavir, prescribed at 600 mg once daily, in pregnant HIV-infected women are equivalent to those post partum, according to a study in the journal AIDS. No dose adjustments are required during pregnancy and similar antiviral activity is expected, researchers said.
A recent study describes the processes by which the SMILE Program, with Connect-to-Protect community coalitions – which are affiliated with the Adolescent Trials Network for HIV/AIDS Interventions – addressed structural barriers that prevented HIV testing, linkage, and engagement in HIV health care among young people.
Serial HIV viral load measures are a valid source for estimating antiretroviral initiation, a study published in JAIDS confirmed. The investigators said a definition that includes a >=1-log viral load decline or a change from detectable to undetectable viral load performed best.
The acceptability of the HPV vaccine was high among HIV-negative men who have sex with men in Ireland, based on no cost vaccine and on stated vaccine efficacy (78%). Higher cost was negatively associated with vaccine acceptability, researchers reported.
Most HIV-infected people discontinuing therapy release a diverse population of virus, and this released virus has entry features of virus selected for replication in CD4+ T cells rather than myeloid cells, according to a report in the Journal of Infectious Diseases.
The majority of new HIV-infected patients in a Ugandan study who screened positive for suspected TB did not have a sputum order, and those who did were more likely to have more advanced HIV disease and symptoms. The authors said improved evaluation of provider behavior in the management of TB screen positive patients could improve active TB case detection rates.
Researchers writing in JAIDS said etravirine 200 mg twice daily, as part of individualized combination antiretroviral therapy, may be a treatment option for HIV-1-infected pregnant women.
Offering single-visit antiretroviral therapy initiation to adult patients in South Africa increased uptake of ART by 36% and viral suppression by 26%, a study in PLOS Medicine revealed. The authors said this intervention should be considered for adoption in the public sector in Africa.
Elevated levels of invariant natural killer T (iNKT) cell and natural killer (NK) cell activation are associated with viremia and disease progression markers in both HIV-1 and HIV-2 infections, according to a study in AIDS.
A study of 22 German HIV clinics demonstrated the noninferiority of ritonavir-boosted darunavir (DRV/r) therapy to standard of care, and said DRV/r should be included as a standard component of recommended regimens in postexposure prophylaxis guidelines.
A study in a large pediatric HIV care setting in Botswana found that children “lost to follow-up” (LTFU) were more likely than were controls to have advanced disease and greater immunosuppression, and to not be receiving antiretroviral therapy. Socioeconomic and psychosocial factors were listed as characteristic of children LTFU but not of controls.
A study published in JAIDS showed that psychosocial conditions such as intimate partner violence fuel HIV incidence among Latino men who have sex with men, and psychosocial interventions should be considered to reduce HIV disparities in this population.
Virologic failure is uncommon in individuals who initiate antiretroviral therapy during acute HIV infection, according to a study in Thailand. The authors said this shows that ART initiation during acute HIV infection is efficacious and clinicians can monitor for virologic failure after 24 weeks of therapy.
In children with slow-progressing HIV, there is a substantial burden of chronic morbidity even when CD4 count is relatively preserved, researchers reported in JAIDS. They said timely HIV testing and prompt antiretroviral initiation are urgently needed to prevent development of chronic complications.
A better understanding of patient-level HIV-related outcomes across different staffing models, and among different patient populations and geographic locations, is urgently needed to improve HIV disease management, according to a study in AIDS Care.
A study in the journal AIDS found that short treatment interruption did not compromise 18-month CD4%, viral control, growth, or morbidity compared to continued antiretroviral therapy among infants who started ART in early HIV infection.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Viral load measurements can be used to predict if an HIV-infected patient will be suppressed by 6-months after starting combination antiretroviral therapy, according to a study in the journal AIDS. The investigators said graphical presentations of this information could help clinicians decide the optimum time to switch treatment regimen during the first months of cART.
A study in The Lancet HIV shows the first application of an automated phylogenetic system monitoring a clinical database to detect a recent HIV outbreak and support the ensuing public health response. The authors said that by making secondary use of routinely collected HIV genotypes, such an approach is cost-effective, attains near real-time monitoring of new cases, and can be implemented in all settings in which HIV genotyping is the standard of care.
According to a study in Epidemiology & Infection, statistical models of risk for skin and soft tissue infection (SSTIs) in HIV patients may yield biased results if they do not account for how HIV viral load may be a marker of adherence to trimethoprim-sulfamethoxazole (TMP-SMX) prophylaxis. TMP-SMX is prescribed to many severely immunocompromised HIV patients and is potentially protective against SSTIs.
The treatment failure misclassification rate in HIV-infected Kenyan children was 21% for the 2006 World Health Organization treatment guidelines and 46% for the 2010/2013 guidelines, according to a recent analysis. Investigators said the findings support current WHO recommendations for routine viral load monitoring but not necessarily the proposed CD4 thresholds.
Doravirine, a new non-nucleoside reverse transcriptase inhibitor in phase III clinical trials, is susceptible to a number of well-known NNRTI resistance mutations, reports a study in JAIDS. The authors said an understanding of the mutational susceptibilities and binding interactions of NNRTIs with reverse transcriptase could be used to develop pairs of compounds with nonoverlapping mutational susceptibilities.
The pharmacokinetics of the antiretroviral drug abacavir, prescribed at 600 mg once daily, in pregnant HIV-infected women are equivalent to those post partum, according to a study in the journal AIDS. No dose adjustments are required during pregnancy and similar antiviral activity is expected, researchers said.
A recent study describes the processes by which the SMILE Program, with Connect-to-Protect community coalitions – which are affiliated with the Adolescent Trials Network for HIV/AIDS Interventions – addressed structural barriers that prevented HIV testing, linkage, and engagement in HIV health care among young people.
Serial HIV viral load measures are a valid source for estimating antiretroviral initiation, a study published in JAIDS confirmed. The investigators said a definition that includes a >=1-log viral load decline or a change from detectable to undetectable viral load performed best.
The acceptability of the HPV vaccine was high among HIV-negative men who have sex with men in Ireland, based on no cost vaccine and on stated vaccine efficacy (78%). Higher cost was negatively associated with vaccine acceptability, researchers reported.
Most HIV-infected people discontinuing therapy release a diverse population of virus, and this released virus has entry features of virus selected for replication in CD4+ T cells rather than myeloid cells, according to a report in the Journal of Infectious Diseases.
The majority of new HIV-infected patients in a Ugandan study who screened positive for suspected TB did not have a sputum order, and those who did were more likely to have more advanced HIV disease and symptoms. The authors said improved evaluation of provider behavior in the management of TB screen positive patients could improve active TB case detection rates.
Researchers writing in JAIDS said etravirine 200 mg twice daily, as part of individualized combination antiretroviral therapy, may be a treatment option for HIV-1-infected pregnant women.
Offering single-visit antiretroviral therapy initiation to adult patients in South Africa increased uptake of ART by 36% and viral suppression by 26%, a study in PLOS Medicine revealed. The authors said this intervention should be considered for adoption in the public sector in Africa.
Elevated levels of invariant natural killer T (iNKT) cell and natural killer (NK) cell activation are associated with viremia and disease progression markers in both HIV-1 and HIV-2 infections, according to a study in AIDS.
A study of 22 German HIV clinics demonstrated the noninferiority of ritonavir-boosted darunavir (DRV/r) therapy to standard of care, and said DRV/r should be included as a standard component of recommended regimens in postexposure prophylaxis guidelines.
A study in a large pediatric HIV care setting in Botswana found that children “lost to follow-up” (LTFU) were more likely than were controls to have advanced disease and greater immunosuppression, and to not be receiving antiretroviral therapy. Socioeconomic and psychosocial factors were listed as characteristic of children LTFU but not of controls.
A study published in JAIDS showed that psychosocial conditions such as intimate partner violence fuel HIV incidence among Latino men who have sex with men, and psychosocial interventions should be considered to reduce HIV disparities in this population.
Virologic failure is uncommon in individuals who initiate antiretroviral therapy during acute HIV infection, according to a study in Thailand. The authors said this shows that ART initiation during acute HIV infection is efficacious and clinicians can monitor for virologic failure after 24 weeks of therapy.
In children with slow-progressing HIV, there is a substantial burden of chronic morbidity even when CD4 count is relatively preserved, researchers reported in JAIDS. They said timely HIV testing and prompt antiretroviral initiation are urgently needed to prevent development of chronic complications.
A better understanding of patient-level HIV-related outcomes across different staffing models, and among different patient populations and geographic locations, is urgently needed to improve HIV disease management, according to a study in AIDS Care.
A study in the journal AIDS found that short treatment interruption did not compromise 18-month CD4%, viral control, growth, or morbidity compared to continued antiretroviral therapy among infants who started ART in early HIV infection.
On Twitter @richpizzi
VIDEO: Cardiothoracic surgeon shortage requires action
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Wedge resection beats SBRT for stage I lung cancer treatment
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT AATS 2016
FDA publishes draft guidance for developing HCV antivirals
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued revised draft guidance intended to foster the development of direct-acting antiviral drugs to treat chronic hepatitis C virus infection.
The guidance, developed by the FDA’s Center for Drug Evaluation and Research, delineates the drug development process from the preinvestigational new drug application through the new drug application and postmarketing stages.
According to the FDA, the draft guidance, when finalized, will represent the current thinking of the agency on development of direct-acting antivirals and clinical trial designs, but is not binding on the FDA or the public. It explicitly states that industry may use an alternative approach to drug development if it “satisfies the requirements of the applicable statutes and regulations.” For the purposes of drug development, the FDA defines direct-acting HCV antivirals as drugs that “interfere with specific steps in the HCV replication cycle through a direct interaction with the HCV genome, polyprotein, or its polyprotein cleavage products.”
The guidance does not address the development of drugs that target host functions necessary for viral replication or immune-based drugs for the treatment of HCV infection, including new interferon drugs or therapeutics “without antiviral mechanisms intended to mitigate or reverse clinical or pathophysiological outcomes” of chronic HCV infection, such as prevention of hepatocellular carcinoma or reversal of fibrosis.
Once the draft guidance has been published in the Federal Register, the FDA will accept comments and suggestions at www.regulations.gov for 60 days.
On Twitter @richpizzi
VIDEO: Del Nido cardioplegic solution receives high grade
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Sutureless Heart Valve: A Critical Innovation
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
FDA warns against routine fluoroquinolone use
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
The U.S. Food and Drug Administration has issued a warning to health care providers against the routine prescribing of fluoroquinolone antibiotics to those patients with sinusitis, bronchitis, and uncomplicated urinary tract infections who have other treatment options.
After conducting a safety review of the drugs, the FDA concluded that fluoroquinolone should be reserved for those patients who do not have alternative treatment options, in light of the findings that the antibiotics – when used systemically in either tablet, capsule, or injectable form – are associated with “disabling and potentially permanent serious side effects” that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system, according to the agency.
The FDA says health care providers should stop systemic fluoroquinolone treatment immediately in patients reporting serious side effects and switch to a non-fluoroquinolone antibacterial drug to complete the patient’s treatment course. The drug labels and medication guides for all fluoroquinolone antibiotics will be updated to reflect the new safety information.
The FDA had previously communicated safety information associated with systemic fluoroquinolone antibacterial drugs in August 2013 and July 2008, and the safety issues described in the current warning were discussed at an FDA Advisory Committee meeting in November 2015.
On Twitter @richpizzi
HIV research update: Late April 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to keep track of everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
CD4 cell count monitoring can be safely performed annually in HIV-monoinfected patients with CD4 cell counts greater than 300 cells/mcL and HIV/hepatitis C virus–coinfected patients with counts greater than 350 cells/mcL, according to a study in Clinical Infectious Diseases.
A three-pill trial of generic antiretroviral therapy is more likely to lead to post-trial treatment changes and to provide more value than a two-pill trial if policy decisions are based on cost-effectiveness, reports a study in HIV Clinical Trials. The authors said value of information analysis can identify trials likely to confer the greatest impact and value for HIV care.
Researchers reported the first case of Alzheimer’s disease (AD) diagnosed in an HIV-positive individual, in a case study published in the journal Alzheimer’s & Dementia. The authors say progressive dementia in older HIV-positive individuals may be due to HIV-associated neurocognitive disorder (HAND), AD, or both, and that amyloid PET imaging may be of value in distinguishing HAND from AD pathologies.
Despite expanded treatment, attrition along the continuum of HIV care is slowing prevention progress in South Africa, according to a study in JAIDS. Investigators said improved detection is critically needed, particularly among men.
A commentary in Lancet Infectious Diseases concluded that plasma concentrations of efavirenz are difficult to predict in HIV-infected children because of immaturity of and genetic variation in metabolic enzymes, and that efavirenz exerts a lysergide (LSD)-like effect on brain serotonergic pathways and affects CNS metabolic pathways. The authors say these uncertainties underline the imminent need for better monitoring of mental health and neurocognitive development in children given and exposed to efavirenz.
A study in the journal AIDS found that HIV infection was independently associated with higher FIB-4 scores, indicating more advanced liver fibrosis, though the difference in FIB-4 score between HIV-infected and uninfected was small. Researchers said higher levels of immune activation were associated with liver fibrosis in HIV-infected, even in the absence of hepatitis B or C virus infection, but not in HIV-uninfected individuals.
The results of a case study of a patient who developed a peripheral facial palsy and a trigeminal neuralgia during an acute HIV infection strongly suggested the HIV primary infection as the etiology of these neuropathies, according to researchers, who assessed laboratory and microbiological findings, including the HIV viral load in cerebrospinal fluid.
A study in the International Journal of Infectious Diseases found that concurrent sexual partnerships may increase the HIV infection risk for black South African women, and in particular, for younger women.
A study of prolonged breastfeeding in Zambia found that the practice increased the risk of human cytomegalovirus (HCMV) infection in infants generally, but children of HIV-positive women were at increased risk of infection. Women who were HIV-positive secreted higher HCMV levels, and for longer duration, than HIV-negative women.
Both chronic and recent HIV infection lead to an average aging advancement of 4.9 years, increasing expected mortality risk by 19%, according to a study in Molecular Cell. In addition, the authors say that decreased human leukocyte antigen methylation is predictive of lower CD4 / CD8 T cell ratio, linking molecular aging, epigenetic regulation, and disease progression.
Lipid-based nutrient supplements given during the first 4 months of antiretroviral therapy improve the quality of life of people living with HIV, according to a study published in Tropical Medicine & International Health.
Because HIV-related immunosuppression and ongoing viral replication may contribute to an increased hypertension risk, a new study recommends aggressive cardiovascular disease risk factor management, early HIV diagnosis, linkage to care, antiretroviral therapy initiation, and durable viral suppression as important components of a comprehensive primary cardiovascular disease prevention strategy in HIV-infected persons.
A study in the Journal of Infectious Diseases reports that for HIV-infected persons in care during 2000-2010 in the U.S. and Canada, rates of first opportunistic infection were relatively low and generally declined over time.
Single viral load measurements overestimated the percent of HIV patients with stable suppressed viral load by 16% (relative difference), according to a study in JAIDS. The authors said targeted clinical interventions are needed to increase the percent of patients with stable suppression.
An Italian population-based study of 5,285 people with AIDS documented extremely elevated risks of death for non-AIDS defining cancers among this population. The authors say the findings stress the need for preventive interventions for both virus-related and non virus-related cancers among HIV-infected individuals.
The mortality risk in HIV-exposed, uninfected (HEU) children was about double that of HIV-unexposed, uninfected (HUU) children, according to a meta-analysis of studies reporting mortality of HEU children to age 60 months and associated factors. The authors said further research is needed to characterize the impact of maternal death and breastfeeding on the survival of HEU infants in the context of maternal antiretroviral therapy, where current evidence is limited.
A study published in Nature showed the efficacy of a single injection of four anti–HIV-1 neutralizing monoclonal antibodies (VRC01, VRC01-LS, 3BNC117, and 10-1074) in blocking repeated weekly low-dose virus challenges of the clade B simian/human chimeric virus AD8.
A systematic review of recent medical literature found that persons of low socioeconomic status in South Africa had a more than 50% higher risk of dying from HIV/AIDS. The authors reported increased relative risk for low-income people when analyzing for income, assets score, and employment status, although relative risk for education was not significant.
A study in HIV Clinical Trials concluded that the use of fosamprenavir/ritonavir therapy (FPV/r) is tolerated in HIV-infected patients with viral hepatitis coinfection. The investigators found the FPV/r discontinuation rate due to adverse events or alanine aminotransferase elevation was similar across all European-approved FPV/r doses and to that of patients on lopinavir/ritonavir therapy.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to keep track of everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
CD4 cell count monitoring can be safely performed annually in HIV-monoinfected patients with CD4 cell counts greater than 300 cells/mcL and HIV/hepatitis C virus–coinfected patients with counts greater than 350 cells/mcL, according to a study in Clinical Infectious Diseases.
A three-pill trial of generic antiretroviral therapy is more likely to lead to post-trial treatment changes and to provide more value than a two-pill trial if policy decisions are based on cost-effectiveness, reports a study in HIV Clinical Trials. The authors said value of information analysis can identify trials likely to confer the greatest impact and value for HIV care.
Researchers reported the first case of Alzheimer’s disease (AD) diagnosed in an HIV-positive individual, in a case study published in the journal Alzheimer’s & Dementia. The authors say progressive dementia in older HIV-positive individuals may be due to HIV-associated neurocognitive disorder (HAND), AD, or both, and that amyloid PET imaging may be of value in distinguishing HAND from AD pathologies.
Despite expanded treatment, attrition along the continuum of HIV care is slowing prevention progress in South Africa, according to a study in JAIDS. Investigators said improved detection is critically needed, particularly among men.
A commentary in Lancet Infectious Diseases concluded that plasma concentrations of efavirenz are difficult to predict in HIV-infected children because of immaturity of and genetic variation in metabolic enzymes, and that efavirenz exerts a lysergide (LSD)-like effect on brain serotonergic pathways and affects CNS metabolic pathways. The authors say these uncertainties underline the imminent need for better monitoring of mental health and neurocognitive development in children given and exposed to efavirenz.
A study in the journal AIDS found that HIV infection was independently associated with higher FIB-4 scores, indicating more advanced liver fibrosis, though the difference in FIB-4 score between HIV-infected and uninfected was small. Researchers said higher levels of immune activation were associated with liver fibrosis in HIV-infected, even in the absence of hepatitis B or C virus infection, but not in HIV-uninfected individuals.
The results of a case study of a patient who developed a peripheral facial palsy and a trigeminal neuralgia during an acute HIV infection strongly suggested the HIV primary infection as the etiology of these neuropathies, according to researchers, who assessed laboratory and microbiological findings, including the HIV viral load in cerebrospinal fluid.
A study in the International Journal of Infectious Diseases found that concurrent sexual partnerships may increase the HIV infection risk for black South African women, and in particular, for younger women.
A study of prolonged breastfeeding in Zambia found that the practice increased the risk of human cytomegalovirus (HCMV) infection in infants generally, but children of HIV-positive women were at increased risk of infection. Women who were HIV-positive secreted higher HCMV levels, and for longer duration, than HIV-negative women.
Both chronic and recent HIV infection lead to an average aging advancement of 4.9 years, increasing expected mortality risk by 19%, according to a study in Molecular Cell. In addition, the authors say that decreased human leukocyte antigen methylation is predictive of lower CD4 / CD8 T cell ratio, linking molecular aging, epigenetic regulation, and disease progression.
Lipid-based nutrient supplements given during the first 4 months of antiretroviral therapy improve the quality of life of people living with HIV, according to a study published in Tropical Medicine & International Health.
Because HIV-related immunosuppression and ongoing viral replication may contribute to an increased hypertension risk, a new study recommends aggressive cardiovascular disease risk factor management, early HIV diagnosis, linkage to care, antiretroviral therapy initiation, and durable viral suppression as important components of a comprehensive primary cardiovascular disease prevention strategy in HIV-infected persons.
A study in the Journal of Infectious Diseases reports that for HIV-infected persons in care during 2000-2010 in the U.S. and Canada, rates of first opportunistic infection were relatively low and generally declined over time.
Single viral load measurements overestimated the percent of HIV patients with stable suppressed viral load by 16% (relative difference), according to a study in JAIDS. The authors said targeted clinical interventions are needed to increase the percent of patients with stable suppression.
An Italian population-based study of 5,285 people with AIDS documented extremely elevated risks of death for non-AIDS defining cancers among this population. The authors say the findings stress the need for preventive interventions for both virus-related and non virus-related cancers among HIV-infected individuals.
The mortality risk in HIV-exposed, uninfected (HEU) children was about double that of HIV-unexposed, uninfected (HUU) children, according to a meta-analysis of studies reporting mortality of HEU children to age 60 months and associated factors. The authors said further research is needed to characterize the impact of maternal death and breastfeeding on the survival of HEU infants in the context of maternal antiretroviral therapy, where current evidence is limited.
A study published in Nature showed the efficacy of a single injection of four anti–HIV-1 neutralizing monoclonal antibodies (VRC01, VRC01-LS, 3BNC117, and 10-1074) in blocking repeated weekly low-dose virus challenges of the clade B simian/human chimeric virus AD8.
A systematic review of recent medical literature found that persons of low socioeconomic status in South Africa had a more than 50% higher risk of dying from HIV/AIDS. The authors reported increased relative risk for low-income people when analyzing for income, assets score, and employment status, although relative risk for education was not significant.
A study in HIV Clinical Trials concluded that the use of fosamprenavir/ritonavir therapy (FPV/r) is tolerated in HIV-infected patients with viral hepatitis coinfection. The investigators found the FPV/r discontinuation rate due to adverse events or alanine aminotransferase elevation was similar across all European-approved FPV/r doses and to that of patients on lopinavir/ritonavir therapy.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to keep track of everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
CD4 cell count monitoring can be safely performed annually in HIV-monoinfected patients with CD4 cell counts greater than 300 cells/mcL and HIV/hepatitis C virus–coinfected patients with counts greater than 350 cells/mcL, according to a study in Clinical Infectious Diseases.
A three-pill trial of generic antiretroviral therapy is more likely to lead to post-trial treatment changes and to provide more value than a two-pill trial if policy decisions are based on cost-effectiveness, reports a study in HIV Clinical Trials. The authors said value of information analysis can identify trials likely to confer the greatest impact and value for HIV care.
Researchers reported the first case of Alzheimer’s disease (AD) diagnosed in an HIV-positive individual, in a case study published in the journal Alzheimer’s & Dementia. The authors say progressive dementia in older HIV-positive individuals may be due to HIV-associated neurocognitive disorder (HAND), AD, or both, and that amyloid PET imaging may be of value in distinguishing HAND from AD pathologies.
Despite expanded treatment, attrition along the continuum of HIV care is slowing prevention progress in South Africa, according to a study in JAIDS. Investigators said improved detection is critically needed, particularly among men.
A commentary in Lancet Infectious Diseases concluded that plasma concentrations of efavirenz are difficult to predict in HIV-infected children because of immaturity of and genetic variation in metabolic enzymes, and that efavirenz exerts a lysergide (LSD)-like effect on brain serotonergic pathways and affects CNS metabolic pathways. The authors say these uncertainties underline the imminent need for better monitoring of mental health and neurocognitive development in children given and exposed to efavirenz.
A study in the journal AIDS found that HIV infection was independently associated with higher FIB-4 scores, indicating more advanced liver fibrosis, though the difference in FIB-4 score between HIV-infected and uninfected was small. Researchers said higher levels of immune activation were associated with liver fibrosis in HIV-infected, even in the absence of hepatitis B or C virus infection, but not in HIV-uninfected individuals.
The results of a case study of a patient who developed a peripheral facial palsy and a trigeminal neuralgia during an acute HIV infection strongly suggested the HIV primary infection as the etiology of these neuropathies, according to researchers, who assessed laboratory and microbiological findings, including the HIV viral load in cerebrospinal fluid.
A study in the International Journal of Infectious Diseases found that concurrent sexual partnerships may increase the HIV infection risk for black South African women, and in particular, for younger women.
A study of prolonged breastfeeding in Zambia found that the practice increased the risk of human cytomegalovirus (HCMV) infection in infants generally, but children of HIV-positive women were at increased risk of infection. Women who were HIV-positive secreted higher HCMV levels, and for longer duration, than HIV-negative women.
Both chronic and recent HIV infection lead to an average aging advancement of 4.9 years, increasing expected mortality risk by 19%, according to a study in Molecular Cell. In addition, the authors say that decreased human leukocyte antigen methylation is predictive of lower CD4 / CD8 T cell ratio, linking molecular aging, epigenetic regulation, and disease progression.
Lipid-based nutrient supplements given during the first 4 months of antiretroviral therapy improve the quality of life of people living with HIV, according to a study published in Tropical Medicine & International Health.
Because HIV-related immunosuppression and ongoing viral replication may contribute to an increased hypertension risk, a new study recommends aggressive cardiovascular disease risk factor management, early HIV diagnosis, linkage to care, antiretroviral therapy initiation, and durable viral suppression as important components of a comprehensive primary cardiovascular disease prevention strategy in HIV-infected persons.
A study in the Journal of Infectious Diseases reports that for HIV-infected persons in care during 2000-2010 in the U.S. and Canada, rates of first opportunistic infection were relatively low and generally declined over time.
Single viral load measurements overestimated the percent of HIV patients with stable suppressed viral load by 16% (relative difference), according to a study in JAIDS. The authors said targeted clinical interventions are needed to increase the percent of patients with stable suppression.
An Italian population-based study of 5,285 people with AIDS documented extremely elevated risks of death for non-AIDS defining cancers among this population. The authors say the findings stress the need for preventive interventions for both virus-related and non virus-related cancers among HIV-infected individuals.
The mortality risk in HIV-exposed, uninfected (HEU) children was about double that of HIV-unexposed, uninfected (HUU) children, according to a meta-analysis of studies reporting mortality of HEU children to age 60 months and associated factors. The authors said further research is needed to characterize the impact of maternal death and breastfeeding on the survival of HEU infants in the context of maternal antiretroviral therapy, where current evidence is limited.
A study published in Nature showed the efficacy of a single injection of four anti–HIV-1 neutralizing monoclonal antibodies (VRC01, VRC01-LS, 3BNC117, and 10-1074) in blocking repeated weekly low-dose virus challenges of the clade B simian/human chimeric virus AD8.
A systematic review of recent medical literature found that persons of low socioeconomic status in South Africa had a more than 50% higher risk of dying from HIV/AIDS. The authors reported increased relative risk for low-income people when analyzing for income, assets score, and employment status, although relative risk for education was not significant.
A study in HIV Clinical Trials concluded that the use of fosamprenavir/ritonavir therapy (FPV/r) is tolerated in HIV-infected patients with viral hepatitis coinfection. The investigators found the FPV/r discontinuation rate due to adverse events or alanine aminotransferase elevation was similar across all European-approved FPV/r doses and to that of patients on lopinavir/ritonavir therapy.
On Twitter @richpizzi
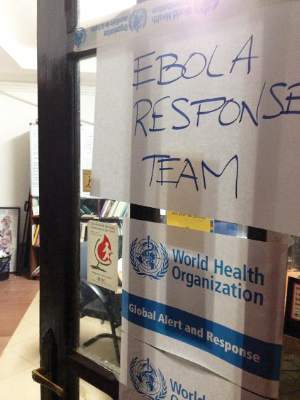
Ebola research update: April 2016
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
A research letter to Annals of Internal Medicine described a case study involving a patient with severe Ebola virus disease, complicated by meningoencephalitis and multiorgan failure, who was managed with supportive care alone until he recovered.
Investigators at the National Institute of Allergy and Infectious Diseases compared in vitro and in vivo approaches to the inactivation of Ebola virus specimens before removal from high-level biocontainment, to evaluate the efficacy of methods of chemical inactivation. The study establishes inactivation procedures for Ebola virus that the authors say can be safely applied to distinct specimen types and research purposes; it might also apply to other enveloped, single-strand, negative-sense RNA viruses.
Researchers from the University of Cambridge (England) evaluated the effect of presymptomatic infection on predictions of major epidemics, and found that precise estimates of the current number of infected individuals – and consequently the chance of a major outbreak in the future – cannot be inferred from data on symptomatic cases alone. They say accurate prediction is impossible without additional data from which the number of currently infected but as yet presymptomatic individuals can be deduced.
A year on from the Ebola outbreaks in West Africa, many Ebola survivors are now suffering symptoms of post-Ebola syndrome, including vision complications, joint and muscle pain, and psychiatric and neurologic problems, according to a presentation at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
A study of the impact of the 2014 Ebola virus outbreak on health care attendance in the Guinean prefecture of Guéckédou found only modest decreases in nonhospital health care visits. Investigators reported a drop in visits in Guéckédou’s outpatient health care facilities during the outbreak of 4.8% and 7.4%, compared with 2013 and 2012, respectively.
TKM-130803, a small interfering RNA lipid nanoparticle product, has been developed for the treatment of Ebola virus disease (EVD). A phase II study found that administration of TKM-130803 at an IV dose of 0.3 mg/kg per day to adult patients with severe EVD was not shown to improve survival, compared with historic controls.
A phase I study of two Ebola vaccines, Ad26.ZEBOV and MVA-BN-Filo, did not result in any vaccine-related serious adverse events in healthy volunteers. Investigators said an immune response was observed after primary immunization with Ad26.ZEBOV, while boosting by MVA-BN-Filo resulted in “sustained elevation of specific immunity.” These vaccines will be further studied in phase II and III studies.
A research brief in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report revealed that a managed contact tracing program in Kambia, Sierra Leone, was effective in identifying 13 Ebola cases that might previously have been missed. The program introduced clear accountability for daily follow-up and patient status recording by contact tracers. The authors said that, based on the findings from the program, recommendations and training materials for improvements in data management and quality control to increase the effectiveness of Ebola contact tracing were subsequently developed for widespread use in Sierra Leone.
A study in Analytical Chemistry demonstrated the utilization of a recently developed cell phone–sized real-time polymerase chain reaction (PCR) device to detect Ebola virus RNA using single-step reverse transcription PCR (RT-PCR). The entire process, which consisted of reverse transcription, PCR amplification, and melting curve analysis, was conducted in less than 37 minutes, and the investigators will next attempt to form an “integrated sample-to-answer system for point-of-care infectious disease diagnostics.”
A personal protective equipment supervision protocol can reduce error rates when health care workers treating Ebola patients take off personal protective equipment, a study showed. Investigators said a video monitoring process can be an effective complement to conventional supervision methods by wardens.
The June 2015 Ebola virus disease “flare-up” in Liberia was due to a reemergence of a Liberian transmission chain originating from a persistently infected source, rather than a reintroduction from a reservoir or a neighboring country with active transmission, according to a report in Science Advances. The authors said the findings highlight the risk of EVD flare-ups even after an outbreak is declared over.
On Twitter @richpizzi
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
A research letter to Annals of Internal Medicine described a case study involving a patient with severe Ebola virus disease, complicated by meningoencephalitis and multiorgan failure, who was managed with supportive care alone until he recovered.
Investigators at the National Institute of Allergy and Infectious Diseases compared in vitro and in vivo approaches to the inactivation of Ebola virus specimens before removal from high-level biocontainment, to evaluate the efficacy of methods of chemical inactivation. The study establishes inactivation procedures for Ebola virus that the authors say can be safely applied to distinct specimen types and research purposes; it might also apply to other enveloped, single-strand, negative-sense RNA viruses.
Researchers from the University of Cambridge (England) evaluated the effect of presymptomatic infection on predictions of major epidemics, and found that precise estimates of the current number of infected individuals – and consequently the chance of a major outbreak in the future – cannot be inferred from data on symptomatic cases alone. They say accurate prediction is impossible without additional data from which the number of currently infected but as yet presymptomatic individuals can be deduced.
A year on from the Ebola outbreaks in West Africa, many Ebola survivors are now suffering symptoms of post-Ebola syndrome, including vision complications, joint and muscle pain, and psychiatric and neurologic problems, according to a presentation at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
A study of the impact of the 2014 Ebola virus outbreak on health care attendance in the Guinean prefecture of Guéckédou found only modest decreases in nonhospital health care visits. Investigators reported a drop in visits in Guéckédou’s outpatient health care facilities during the outbreak of 4.8% and 7.4%, compared with 2013 and 2012, respectively.
TKM-130803, a small interfering RNA lipid nanoparticle product, has been developed for the treatment of Ebola virus disease (EVD). A phase II study found that administration of TKM-130803 at an IV dose of 0.3 mg/kg per day to adult patients with severe EVD was not shown to improve survival, compared with historic controls.
A phase I study of two Ebola vaccines, Ad26.ZEBOV and MVA-BN-Filo, did not result in any vaccine-related serious adverse events in healthy volunteers. Investigators said an immune response was observed after primary immunization with Ad26.ZEBOV, while boosting by MVA-BN-Filo resulted in “sustained elevation of specific immunity.” These vaccines will be further studied in phase II and III studies.
A research brief in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report revealed that a managed contact tracing program in Kambia, Sierra Leone, was effective in identifying 13 Ebola cases that might previously have been missed. The program introduced clear accountability for daily follow-up and patient status recording by contact tracers. The authors said that, based on the findings from the program, recommendations and training materials for improvements in data management and quality control to increase the effectiveness of Ebola contact tracing were subsequently developed for widespread use in Sierra Leone.
A study in Analytical Chemistry demonstrated the utilization of a recently developed cell phone–sized real-time polymerase chain reaction (PCR) device to detect Ebola virus RNA using single-step reverse transcription PCR (RT-PCR). The entire process, which consisted of reverse transcription, PCR amplification, and melting curve analysis, was conducted in less than 37 minutes, and the investigators will next attempt to form an “integrated sample-to-answer system for point-of-care infectious disease diagnostics.”
A personal protective equipment supervision protocol can reduce error rates when health care workers treating Ebola patients take off personal protective equipment, a study showed. Investigators said a video monitoring process can be an effective complement to conventional supervision methods by wardens.
The June 2015 Ebola virus disease “flare-up” in Liberia was due to a reemergence of a Liberian transmission chain originating from a persistently infected source, rather than a reintroduction from a reservoir or a neighboring country with active transmission, according to a report in Science Advances. The authors said the findings highlight the risk of EVD flare-ups even after an outbreak is declared over.
On Twitter @richpizzi
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
A research letter to Annals of Internal Medicine described a case study involving a patient with severe Ebola virus disease, complicated by meningoencephalitis and multiorgan failure, who was managed with supportive care alone until he recovered.
Investigators at the National Institute of Allergy and Infectious Diseases compared in vitro and in vivo approaches to the inactivation of Ebola virus specimens before removal from high-level biocontainment, to evaluate the efficacy of methods of chemical inactivation. The study establishes inactivation procedures for Ebola virus that the authors say can be safely applied to distinct specimen types and research purposes; it might also apply to other enveloped, single-strand, negative-sense RNA viruses.
Researchers from the University of Cambridge (England) evaluated the effect of presymptomatic infection on predictions of major epidemics, and found that precise estimates of the current number of infected individuals – and consequently the chance of a major outbreak in the future – cannot be inferred from data on symptomatic cases alone. They say accurate prediction is impossible without additional data from which the number of currently infected but as yet presymptomatic individuals can be deduced.
A year on from the Ebola outbreaks in West Africa, many Ebola survivors are now suffering symptoms of post-Ebola syndrome, including vision complications, joint and muscle pain, and psychiatric and neurologic problems, according to a presentation at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
A study of the impact of the 2014 Ebola virus outbreak on health care attendance in the Guinean prefecture of Guéckédou found only modest decreases in nonhospital health care visits. Investigators reported a drop in visits in Guéckédou’s outpatient health care facilities during the outbreak of 4.8% and 7.4%, compared with 2013 and 2012, respectively.
TKM-130803, a small interfering RNA lipid nanoparticle product, has been developed for the treatment of Ebola virus disease (EVD). A phase II study found that administration of TKM-130803 at an IV dose of 0.3 mg/kg per day to adult patients with severe EVD was not shown to improve survival, compared with historic controls.
A phase I study of two Ebola vaccines, Ad26.ZEBOV and MVA-BN-Filo, did not result in any vaccine-related serious adverse events in healthy volunteers. Investigators said an immune response was observed after primary immunization with Ad26.ZEBOV, while boosting by MVA-BN-Filo resulted in “sustained elevation of specific immunity.” These vaccines will be further studied in phase II and III studies.
A research brief in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report revealed that a managed contact tracing program in Kambia, Sierra Leone, was effective in identifying 13 Ebola cases that might previously have been missed. The program introduced clear accountability for daily follow-up and patient status recording by contact tracers. The authors said that, based on the findings from the program, recommendations and training materials for improvements in data management and quality control to increase the effectiveness of Ebola contact tracing were subsequently developed for widespread use in Sierra Leone.
A study in Analytical Chemistry demonstrated the utilization of a recently developed cell phone–sized real-time polymerase chain reaction (PCR) device to detect Ebola virus RNA using single-step reverse transcription PCR (RT-PCR). The entire process, which consisted of reverse transcription, PCR amplification, and melting curve analysis, was conducted in less than 37 minutes, and the investigators will next attempt to form an “integrated sample-to-answer system for point-of-care infectious disease diagnostics.”
A personal protective equipment supervision protocol can reduce error rates when health care workers treating Ebola patients take off personal protective equipment, a study showed. Investigators said a video monitoring process can be an effective complement to conventional supervision methods by wardens.
The June 2015 Ebola virus disease “flare-up” in Liberia was due to a reemergence of a Liberian transmission chain originating from a persistently infected source, rather than a reintroduction from a reservoir or a neighboring country with active transmission, according to a report in Science Advances. The authors said the findings highlight the risk of EVD flare-ups even after an outbreak is declared over.
On Twitter @richpizzi
CDC: Zika virus urine testing preferable to serum
New data showing that Zika virus can be found at higher levels or for longer duration in urine than serum, has prompted the Centers for Disease Control and Prevention to update its interim diagnostic testing guidance for the virus in public health laboratories.
The CDC now recommends that Zika virus real-time reverse transcription–polymerase chain reaction (rRT-PCR) be performed on urine collected less than 14 days after the onset of symptoms in patients with suspected Zika virus disease. The rRT-PCR is the preferred test for Zika infection because it can be performed rapidly and is highly specific, the CDC notes, and currently, the CDC Trioplex rRT-PCR assay is the only diagnostic tool authorized by the Food and Drug Administration for Zika virus testing of urine (MMWR. 2016 May 10. doi:10.15585/mmwr.mm6518e1).
In most patients, Zika virus RNA is unlikely to be detected in serum after the first week of illness, the CDC said, but adaptations of previously published diagnostic methods suggest that Zika virus RNA can be detected in urine for at least 2 weeks after onset of symptoms. However, the CDC affirmed that Zika virus rRT-PCR testing of urine should be performed in conjunction with serum testing if using specimens collected less than 7 days after symptom onset, and a positive result in either specimen type provides evidence of Zika virus infection.
The CDC added that, because viremia decreases over time and dates of illness onset may not be accurately reported, a negative rRT-PCR does not exclude Zika virus infection, and IgM antibody testing should be performed. The agency also said other laboratory-developed tests will need in-house validations to adequately characterize the performance of the assay and meet Clinical Laboratory Improvement Amendments requirements.
Read the full report here.
On Twitter @richpizzi
New data showing that Zika virus can be found at higher levels or for longer duration in urine than serum, has prompted the Centers for Disease Control and Prevention to update its interim diagnostic testing guidance for the virus in public health laboratories.
The CDC now recommends that Zika virus real-time reverse transcription–polymerase chain reaction (rRT-PCR) be performed on urine collected less than 14 days after the onset of symptoms in patients with suspected Zika virus disease. The rRT-PCR is the preferred test for Zika infection because it can be performed rapidly and is highly specific, the CDC notes, and currently, the CDC Trioplex rRT-PCR assay is the only diagnostic tool authorized by the Food and Drug Administration for Zika virus testing of urine (MMWR. 2016 May 10. doi:10.15585/mmwr.mm6518e1).
In most patients, Zika virus RNA is unlikely to be detected in serum after the first week of illness, the CDC said, but adaptations of previously published diagnostic methods suggest that Zika virus RNA can be detected in urine for at least 2 weeks after onset of symptoms. However, the CDC affirmed that Zika virus rRT-PCR testing of urine should be performed in conjunction with serum testing if using specimens collected less than 7 days after symptom onset, and a positive result in either specimen type provides evidence of Zika virus infection.
The CDC added that, because viremia decreases over time and dates of illness onset may not be accurately reported, a negative rRT-PCR does not exclude Zika virus infection, and IgM antibody testing should be performed. The agency also said other laboratory-developed tests will need in-house validations to adequately characterize the performance of the assay and meet Clinical Laboratory Improvement Amendments requirements.
Read the full report here.
On Twitter @richpizzi
New data showing that Zika virus can be found at higher levels or for longer duration in urine than serum, has prompted the Centers for Disease Control and Prevention to update its interim diagnostic testing guidance for the virus in public health laboratories.
The CDC now recommends that Zika virus real-time reverse transcription–polymerase chain reaction (rRT-PCR) be performed on urine collected less than 14 days after the onset of symptoms in patients with suspected Zika virus disease. The rRT-PCR is the preferred test for Zika infection because it can be performed rapidly and is highly specific, the CDC notes, and currently, the CDC Trioplex rRT-PCR assay is the only diagnostic tool authorized by the Food and Drug Administration for Zika virus testing of urine (MMWR. 2016 May 10. doi:10.15585/mmwr.mm6518e1).
In most patients, Zika virus RNA is unlikely to be detected in serum after the first week of illness, the CDC said, but adaptations of previously published diagnostic methods suggest that Zika virus RNA can be detected in urine for at least 2 weeks after onset of symptoms. However, the CDC affirmed that Zika virus rRT-PCR testing of urine should be performed in conjunction with serum testing if using specimens collected less than 7 days after symptom onset, and a positive result in either specimen type provides evidence of Zika virus infection.
The CDC added that, because viremia decreases over time and dates of illness onset may not be accurately reported, a negative rRT-PCR does not exclude Zika virus infection, and IgM antibody testing should be performed. The agency also said other laboratory-developed tests will need in-house validations to adequately characterize the performance of the assay and meet Clinical Laboratory Improvement Amendments requirements.
Read the full report here.
On Twitter @richpizzi
FROM MORBIDITY AND MORTALITY WEEKLY REPORT