User login
Biopsy bests HCRT for lung fibrosis, has risks
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
The role of surgical biopsy in the high-risk population with interstitial lung disease is well suited for surgical review because thoracic surgeons must weigh the risks, including potential mortality, and benefits when discussion options with patients and families, Dr. Katie S. Nason noted in her invited editorial commentary.

|
Dr. Katie S. Nason |
Current guidelines suggest that SLB is no longer essential for diagnosis of idiopathic pulmonary fibrosis and they now consider an HRCT scan showing unusual interstitial pneumonia (UIP) sufficient for diagnosis. “However, in the absence of diagnostic imaging criteria for UIP, specifically honeycombing, surgical lung biopsy with interpretation by an expert pathologist is necessary and should be performed to further define patients with possible UIP,” Dr. Nason wrote. “Comprehensive application of this approach will delineate circumstances in which a surgical biopsy will be more informative than an HRCT scan as well as when a surgical biopsy is not necessary.”
She called for a multi-institutional, international registry to collect and better understand data on the diagnostic yield and mortality after SLB for interstitial lung disease.
Dr. Nason is an assistant professor of cardiothoracic surgery at the University of Pittsburgh.
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
Surgical lung biopsy performs well and is relatively safe for evaluating suspected interstitial lung diseases, but may be especially helpful in confirming the diagnosis and directing the treatment of patients with idiopathic pulmonary fibrosis with atypical signs and symptoms, researchers have found.
In patients with immune disorders or severe respiratory dysfunction, or on mechanical ventilation, clinicians should weigh the diagnostic benefits of surgical lung biopsy (SLB) against its potential risks, according to a systematic review and meta-analysis of 23 studies published between 2000 and 2014, comprising 2,148 patients. Dr. Qian Han of the Guangzhou Institute of Respiratory Disease in China led the investigative team. The findings were published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
The meta-analysis focused on diagnostic yield of biopsy samples and postbiopsy mortality within 90 days of surgery (J. Thorac. Cardiovasc. Surg. 2014 [doi:10.1016/j.jtcvs.2014.12.057). The mean age of patients across the studies ranged from 36 to 62 years. The population of the meta-analysis included 1,632 (76%) who had undergone video-assisted thoracic surgery (VATS) and 268 (12.5%) who had open-lung biopsy.
Slightly more than one third (33.5%) of diagnoses involved idiopathic pulmonary fibrosis, followed by nonspecific interstitial pneumonia (12%), hypersensitivity pneumonitis (9.6%), cryptogenic organizing pneumonia (7.5%), sarcoidosis (6.8%), and connective tissue disease related to interstitial lung disease (4%).
The median diagnostic yield across all studies was 95%, ranging from 42% to 100% depending on the study. One study showed a diagnostic yield below 70%. Eight studies showed that the biopsy influenced a change in the treatment plan 42%-90% of the time. In the entire meta-analysis, treatment plans were altered for 59.5% of patients who received a specific diagnosis and in 55.2% of those without a definitive diagnosis.
“These results suggested that an alteration in treatment may not be directed by a definitive histological diagnosis and nonspecific histological results could also be useful in clinical practice,” Dr. Han said.
Eleven of the studies used CT guidance to obtain biopsies without a preference to lobe, but two studies predisposed to the right lobes had diagnostic yields of 84% and 94%. One study avoided the lingual or middle lobe, with a diagnostic yield of 97%, and another focused on the lingular lobe only, with a 100% yield. Two studies showed that biopsy samples from lingual or middle lobes had the same diagnostic yield as did those from other lobes.
With regard to diagnostic performance based on biopsy numbers, one study showed that multiple biopsies may increase the diagnostic yield. Twelve studies obtained one to three samples, and among them eight studies suggested one sample containing both lesion and normal tissue was sufficient to represent pathological changes. One study showed that multiple biopsies may increase diagnostic yield.
Of the 16 studies that provided sufficient data on mortality rates, the pooled 30- and 90-day mortality rates were 2.2% (95% CI 1.0-4.0%) and 3.4% (95% CI 1.8-5.5%), respectively. The composite postoperative mortality rate was 3.6% (95% CI 2.1%-5.5%).
In their discussion, Dr. Han and colleagues addressed the controversy surrounding lingual vs. middle lobe biopsy by noting that high-resolution CT (HRCT) can be valuable in identifying the appropriate biopsy location. While multiple studies supported the effectiveness of only one biopsy as long as it contained both normal and abnormal tissue, the researchers pointed out that future studies evaluating biopsy samples would do well to evaluate biopsy number combined with sample size.
HRCT, while highly specific, may be less sensitive than SLB in the diagnosis of idiopathic pulmonary fibrosis, they found. Two studies the meta-analysis looked at compared the diagnostic yield between SLB and HRCT; SLB finally diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease. “These findings suggested that HRCT, albeit highly specific, is less sensitive in the diagnosis of IPF, therefore necessitating the utility of SLB in the diagnosis of these HRCT-omitted cases,” Dr. Han said.
On the safety issue, while studies that excluded patients on mechanical ventilation reported lower mortality rates and two studies identified ventilator dependence as an independent risk factor for mortality, the investigators reported that the higher mortality rates were probably the result of a sicker patient population rather than the SLB procedure itself. They wrote that to “indiscreetly refuse” to perform SLB in these patients is “overcautious and inappropriate” given the benefits of SLB in validating diagnoses and influencing treatment plans.
Dr. Han and his colleagues reported having no relevant disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Surgical lung biopsy is helpful to confirm interstitial lung disease in patients with unique signs and symptoms, but the benefit of SLB should be balanced against the risks in patients with more severe disease.
Major finding: In two studies that compared the diagnostic yield between SLB and HRCT; SLB diagnosed idiopathic pulmonary fibrosis in 75%-91% of suspected cases and in 19%-74% of cases when HRCT did not raise suspicion of the disease.
Data source: Meta-analysis of 23 studies published between 2000 and 2014 and involving 2,148 patients.
Disclosures: The National Natural Science Foundation of China Young Investigator Funding supported the work. The investigators reported having no conflicts of interest.
Why cardiac surgeons must adopt percutaneous skills
With the widespread adoption of transcatheter aortic valve replacement and the public’s embrace of minimally invasive procedures, cardiac surgeons must adapt to stay relevant in the future, and that means acquiring skills to perform percutaneous procedures, Dr. Tom C. Nguyen and Dr. Isaac George wrote in the Young Surgeon column in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Drawing upon their own year in a structural heart endovascular fellowship, Dr. Nguyen and Dr. George called for a new approach to surgical training that encompasses percutaneous technology and procedures, “with a caveat that failure to do so will exclude surgeons from treating valve disease altogether in the future” (J. Thorac. Cardiovasc. Surg. 2015;149:675-77 [doi: 10.1016/j.jtcvs.2014.11.091]).
In making their case, Dr. Nguyen and Dr. George invoked psychologist Abraham Maslow’s “law of the instrument”: “I suppose it is tempting, if the only tool you have is a hammer, to treat everything as if it were a nail.” Dr. Nguyen is with the University of Texas and Memorial Hermann Heart and Vascular Institute in Houston. Dr. George is with New York-Presbyterian Hospital and Columbia University in New York.
Cardiac surgeons must break out of that mindset and learn from the evolution of vascular surgery, which was once the domain of general surgery but then evolved into its own specialty. Patients with peripheral vascular disease who were once surgical candidates instead opted for less-invasive endovascular procedures as interventional radiology techniques advanced. “This direction may have had devastating consequences for vascular surgeons if it were not for their ability and willingness to learn new skills so that they could also perform catheter-based interventions,” Dr. Nguyen and Dr. George wrote.
Catheter-based treatment for heart valve disease is following a similar path, but that doesn’t mean cardiac surgeons should vacate this field to cardiologists. “In fact, in order to provide the best comprehensive care for patients, a collaborative heart team including cardiologists and surgeons who all are equally proficient in endovascular techniques is essential,” they wrote. Further, if surgeons can work independently of cardiologists by learning and adopting percutaneous techniques, new technologies will advance even faster. “Surgeons have an intimate knowledge of the heart that is unmatched by any specialty; translation of this knowledge into structural heart valve technology is logical and needed,” Dr. Nguyen and Dr. George said.
Also, surgeons well versed in all techniques – endovascular, minimally invasive surgery, and conventional surgery – will be equipped to objectively offer the procedure that’s best suited for the patient rather than their own skill set.
Acquiring percutaneous skills, however, poses a high hurdle for cardiac surgeons. They must be able to perform the entire transapical and transaortic transcatheter aortic valve replacement (TAVR) procedure and seize the lead for the procedure from the cardiologist, Dr. Nguyen and Dr. George said. “To do this, surgeons will have to change their mindset regarding their role in the procedure and be willing to learn the technology.”
The minimum time commitment to learn these procedures is 6 months; for residents, a dedicated structural heart fellowship can take up to a year. The 20 interventional procedures that graduates are now required to perform “is not nearly enough,” they wrote.
Because percutaneous skills also apply to all future structural heart interventions, such as percutaneous mitral valve repair and replacement, percutaneous tricuspid valve repair and replacement, and pulmonic valve replacement, they can help the cardiac surgeon get past seeing valvular heart disease as something other than a nail.
The authors reported having no disclosures.
Dr. Nguyen and Dr. George address an important current topic regarding the need for cardiothoracic surgeons to quickly adopt and become experts in nontraditional techniques (percutaneous, minimally invasive interventions). Alluding to the historic failure of cardiac surgeons to adopt early angiography (and subsequently lose a valuable share of the market to interventional cardiology) and citing vascular surgeons who aggressively avoided this fate (by being early adopters of endovascular techniques), the authors propose an alternate schema moving forward.
As is clear, TAVR is here to stay. There is a growing emphasis on percutaneous and minimally invasive cardiac interventions that require an elaborate set of nontraditional skills (access, wires, fluoroscopy, angiography, endostenting, and percutaneous closure, to name a few) that take time and experience to develop. Programs are currently mandated by the Centers for Medicare & Medicaid Services to team a cardiologist and a cardiac surgeon for reimbursement, although this limitation may eventually be eased. When that happens, will cardiac surgeons have the market share, hospital privileges, and experience to be able to independently handle a TAVR case? If not, will the cardiac surgeon play second fiddle to an experienced interventional cardiologist as valvular disease will become increasingly better managed without a traditional sternotomy?
This issue is critical to the young cardiothoracic trainee. How do “the cardiac surgeons of the past … transform into the surgeons of the future?” Dr. Nguyen and Dr. George propose a three-pronged approach: early clinical adoption (mainly by attendings, departments, and institutions); appropriate training; and innovation to move technology forward. The discussed training arm is critical and requires dedicated time. Both authors spent 1 year as advanced fellows in structural heart disease, and only after a high-volume, multidisciplinary experience did they become more facile with catheter-based techniques. I agree with the authors’ conclusion that advanced fellowship training in percutaneous and endovascular techniques (which includes intimate collaboration with cardiology) is critical. This advanced training needs to be regulated and restricted to centers of high volume excellence, where the surgeon is capable of being the team leader, thus making it a much more robust learning experience.
Dr. David D. Shersher is one of the resident editors for Thoracic Surgery News.
Dr. Nguyen and Dr. George address an important current topic regarding the need for cardiothoracic surgeons to quickly adopt and become experts in nontraditional techniques (percutaneous, minimally invasive interventions). Alluding to the historic failure of cardiac surgeons to adopt early angiography (and subsequently lose a valuable share of the market to interventional cardiology) and citing vascular surgeons who aggressively avoided this fate (by being early adopters of endovascular techniques), the authors propose an alternate schema moving forward.
As is clear, TAVR is here to stay. There is a growing emphasis on percutaneous and minimally invasive cardiac interventions that require an elaborate set of nontraditional skills (access, wires, fluoroscopy, angiography, endostenting, and percutaneous closure, to name a few) that take time and experience to develop. Programs are currently mandated by the Centers for Medicare & Medicaid Services to team a cardiologist and a cardiac surgeon for reimbursement, although this limitation may eventually be eased. When that happens, will cardiac surgeons have the market share, hospital privileges, and experience to be able to independently handle a TAVR case? If not, will the cardiac surgeon play second fiddle to an experienced interventional cardiologist as valvular disease will become increasingly better managed without a traditional sternotomy?
This issue is critical to the young cardiothoracic trainee. How do “the cardiac surgeons of the past … transform into the surgeons of the future?” Dr. Nguyen and Dr. George propose a three-pronged approach: early clinical adoption (mainly by attendings, departments, and institutions); appropriate training; and innovation to move technology forward. The discussed training arm is critical and requires dedicated time. Both authors spent 1 year as advanced fellows in structural heart disease, and only after a high-volume, multidisciplinary experience did they become more facile with catheter-based techniques. I agree with the authors’ conclusion that advanced fellowship training in percutaneous and endovascular techniques (which includes intimate collaboration with cardiology) is critical. This advanced training needs to be regulated and restricted to centers of high volume excellence, where the surgeon is capable of being the team leader, thus making it a much more robust learning experience.
Dr. David D. Shersher is one of the resident editors for Thoracic Surgery News.
Dr. Nguyen and Dr. George address an important current topic regarding the need for cardiothoracic surgeons to quickly adopt and become experts in nontraditional techniques (percutaneous, minimally invasive interventions). Alluding to the historic failure of cardiac surgeons to adopt early angiography (and subsequently lose a valuable share of the market to interventional cardiology) and citing vascular surgeons who aggressively avoided this fate (by being early adopters of endovascular techniques), the authors propose an alternate schema moving forward.
As is clear, TAVR is here to stay. There is a growing emphasis on percutaneous and minimally invasive cardiac interventions that require an elaborate set of nontraditional skills (access, wires, fluoroscopy, angiography, endostenting, and percutaneous closure, to name a few) that take time and experience to develop. Programs are currently mandated by the Centers for Medicare & Medicaid Services to team a cardiologist and a cardiac surgeon for reimbursement, although this limitation may eventually be eased. When that happens, will cardiac surgeons have the market share, hospital privileges, and experience to be able to independently handle a TAVR case? If not, will the cardiac surgeon play second fiddle to an experienced interventional cardiologist as valvular disease will become increasingly better managed without a traditional sternotomy?
This issue is critical to the young cardiothoracic trainee. How do “the cardiac surgeons of the past … transform into the surgeons of the future?” Dr. Nguyen and Dr. George propose a three-pronged approach: early clinical adoption (mainly by attendings, departments, and institutions); appropriate training; and innovation to move technology forward. The discussed training arm is critical and requires dedicated time. Both authors spent 1 year as advanced fellows in structural heart disease, and only after a high-volume, multidisciplinary experience did they become more facile with catheter-based techniques. I agree with the authors’ conclusion that advanced fellowship training in percutaneous and endovascular techniques (which includes intimate collaboration with cardiology) is critical. This advanced training needs to be regulated and restricted to centers of high volume excellence, where the surgeon is capable of being the team leader, thus making it a much more robust learning experience.
Dr. David D. Shersher is one of the resident editors for Thoracic Surgery News.
With the widespread adoption of transcatheter aortic valve replacement and the public’s embrace of minimally invasive procedures, cardiac surgeons must adapt to stay relevant in the future, and that means acquiring skills to perform percutaneous procedures, Dr. Tom C. Nguyen and Dr. Isaac George wrote in the Young Surgeon column in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Drawing upon their own year in a structural heart endovascular fellowship, Dr. Nguyen and Dr. George called for a new approach to surgical training that encompasses percutaneous technology and procedures, “with a caveat that failure to do so will exclude surgeons from treating valve disease altogether in the future” (J. Thorac. Cardiovasc. Surg. 2015;149:675-77 [doi: 10.1016/j.jtcvs.2014.11.091]).
In making their case, Dr. Nguyen and Dr. George invoked psychologist Abraham Maslow’s “law of the instrument”: “I suppose it is tempting, if the only tool you have is a hammer, to treat everything as if it were a nail.” Dr. Nguyen is with the University of Texas and Memorial Hermann Heart and Vascular Institute in Houston. Dr. George is with New York-Presbyterian Hospital and Columbia University in New York.
Cardiac surgeons must break out of that mindset and learn from the evolution of vascular surgery, which was once the domain of general surgery but then evolved into its own specialty. Patients with peripheral vascular disease who were once surgical candidates instead opted for less-invasive endovascular procedures as interventional radiology techniques advanced. “This direction may have had devastating consequences for vascular surgeons if it were not for their ability and willingness to learn new skills so that they could also perform catheter-based interventions,” Dr. Nguyen and Dr. George wrote.
Catheter-based treatment for heart valve disease is following a similar path, but that doesn’t mean cardiac surgeons should vacate this field to cardiologists. “In fact, in order to provide the best comprehensive care for patients, a collaborative heart team including cardiologists and surgeons who all are equally proficient in endovascular techniques is essential,” they wrote. Further, if surgeons can work independently of cardiologists by learning and adopting percutaneous techniques, new technologies will advance even faster. “Surgeons have an intimate knowledge of the heart that is unmatched by any specialty; translation of this knowledge into structural heart valve technology is logical and needed,” Dr. Nguyen and Dr. George said.
Also, surgeons well versed in all techniques – endovascular, minimally invasive surgery, and conventional surgery – will be equipped to objectively offer the procedure that’s best suited for the patient rather than their own skill set.
Acquiring percutaneous skills, however, poses a high hurdle for cardiac surgeons. They must be able to perform the entire transapical and transaortic transcatheter aortic valve replacement (TAVR) procedure and seize the lead for the procedure from the cardiologist, Dr. Nguyen and Dr. George said. “To do this, surgeons will have to change their mindset regarding their role in the procedure and be willing to learn the technology.”
The minimum time commitment to learn these procedures is 6 months; for residents, a dedicated structural heart fellowship can take up to a year. The 20 interventional procedures that graduates are now required to perform “is not nearly enough,” they wrote.
Because percutaneous skills also apply to all future structural heart interventions, such as percutaneous mitral valve repair and replacement, percutaneous tricuspid valve repair and replacement, and pulmonic valve replacement, they can help the cardiac surgeon get past seeing valvular heart disease as something other than a nail.
The authors reported having no disclosures.
With the widespread adoption of transcatheter aortic valve replacement and the public’s embrace of minimally invasive procedures, cardiac surgeons must adapt to stay relevant in the future, and that means acquiring skills to perform percutaneous procedures, Dr. Tom C. Nguyen and Dr. Isaac George wrote in the Young Surgeon column in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Drawing upon their own year in a structural heart endovascular fellowship, Dr. Nguyen and Dr. George called for a new approach to surgical training that encompasses percutaneous technology and procedures, “with a caveat that failure to do so will exclude surgeons from treating valve disease altogether in the future” (J. Thorac. Cardiovasc. Surg. 2015;149:675-77 [doi: 10.1016/j.jtcvs.2014.11.091]).
In making their case, Dr. Nguyen and Dr. George invoked psychologist Abraham Maslow’s “law of the instrument”: “I suppose it is tempting, if the only tool you have is a hammer, to treat everything as if it were a nail.” Dr. Nguyen is with the University of Texas and Memorial Hermann Heart and Vascular Institute in Houston. Dr. George is with New York-Presbyterian Hospital and Columbia University in New York.
Cardiac surgeons must break out of that mindset and learn from the evolution of vascular surgery, which was once the domain of general surgery but then evolved into its own specialty. Patients with peripheral vascular disease who were once surgical candidates instead opted for less-invasive endovascular procedures as interventional radiology techniques advanced. “This direction may have had devastating consequences for vascular surgeons if it were not for their ability and willingness to learn new skills so that they could also perform catheter-based interventions,” Dr. Nguyen and Dr. George wrote.
Catheter-based treatment for heart valve disease is following a similar path, but that doesn’t mean cardiac surgeons should vacate this field to cardiologists. “In fact, in order to provide the best comprehensive care for patients, a collaborative heart team including cardiologists and surgeons who all are equally proficient in endovascular techniques is essential,” they wrote. Further, if surgeons can work independently of cardiologists by learning and adopting percutaneous techniques, new technologies will advance even faster. “Surgeons have an intimate knowledge of the heart that is unmatched by any specialty; translation of this knowledge into structural heart valve technology is logical and needed,” Dr. Nguyen and Dr. George said.
Also, surgeons well versed in all techniques – endovascular, minimally invasive surgery, and conventional surgery – will be equipped to objectively offer the procedure that’s best suited for the patient rather than their own skill set.
Acquiring percutaneous skills, however, poses a high hurdle for cardiac surgeons. They must be able to perform the entire transapical and transaortic transcatheter aortic valve replacement (TAVR) procedure and seize the lead for the procedure from the cardiologist, Dr. Nguyen and Dr. George said. “To do this, surgeons will have to change their mindset regarding their role in the procedure and be willing to learn the technology.”
The minimum time commitment to learn these procedures is 6 months; for residents, a dedicated structural heart fellowship can take up to a year. The 20 interventional procedures that graduates are now required to perform “is not nearly enough,” they wrote.
Because percutaneous skills also apply to all future structural heart interventions, such as percutaneous mitral valve repair and replacement, percutaneous tricuspid valve repair and replacement, and pulmonic valve replacement, they can help the cardiac surgeon get past seeing valvular heart disease as something other than a nail.
The authors reported having no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Pneumonia most deadly emergency surgery complication
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
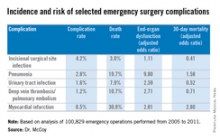
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
Key clinical point: Target pneumonia for prevention after emergency general surgery.
Major finding: Emergency operations account for only 15% of all operations but more than half of postoperative deaths. Of the studied complications, pneumonia was associated with the greatest number of deaths after emergency general surgery.
Data source: Analysis of 100,829 emergency surgery cases in the American College of Surgeons National Surgical Quality Improvement Program database.
Disclosures: Dr. McCoy had no financial conflicts to disclose.
Splenectomy rare after first 24 hours in trauma, early trial results show
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
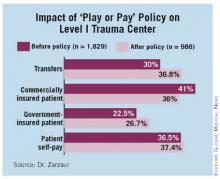
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Follow-up angiography and CT may not be necessary for trauma patients with blunt spleen injury because of the low rates of splenectomy after 24 hours.
Major finding: Only 3.6% of trauma patients required in-hospital splenectomy between 24 hours and 9 days after surgery; the vast majority were discharged with spleen intact.
Data source: Splenic Injury Outcomes Trial, a prospective study involving 383 patients at 11 level 1 trauma centers.
Disclosures: Dr. Zarzaur reported having no relevant financial disclosures.
PROOVIT registry results make case for expansion
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Gathering previously uncollected information on management of trauma-related vascular injuries can inform treatment and may improve outcomes.
Major finding: The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
Data source: The AAST PROOVIT registry involving 13 Level 1 and 1 Level 2 trauma centers with data on 542 injuries.
Disclosures: Dr. DuBose reported having no relevant financial disclosures.
Antihypertension drugs may have clotting protection in obese trauma patients
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
FROM AATS ANNUAL MEETING
Key clinical point: ACE-I and ARB medications may help obese trauma patients maintain trauma scores similar to nonobese patients.
Major finding: Obese patients who took ACE inhibitors or ARB drugs before their injuries had trauma scores similar to nonobese trauma patients, while obese patients in a prospective study displayed hypercoagulability, compared with that of normal weight patients.
Data source: Analysis of data from Inflammation and the Host Response to Injury database, and prospective analysis of demographic, outcomes and laboratory measures of 377 patients of varying BMI.
Disclosures: Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
Same-day combined ERCP and cholecystectomy: achievable and cost effective
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
FROM THE AAST ANNUAL MEETING
Key clinical point: Scheduling both ERCP and cholecystectomy on the same day reduces hospital stays and saves money.
Major finding: Patients who had preoperative endoscopic retrograde cholangiopancreatography (ERCP) on the same day as cholecystectomy had 3-day hospital stays compared to 5 days for patients who had the procedures on separate days.
Data source: Single-center retrospective study of 240 patients from 2010 to 2014.
Disclosures: Dr. Wild reported having no relevant financial disclosures.
CTA before visceral arteriography improves bleed identification, localization
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
AT THE AAST ANNUAL MEETING
Key clinical point: In patients with lower GI hemorrhage, performing CT angiography before visceral arteriography can improve diagnostic accuracy and reduce radiation exposure.
Major finding: CTA before VA vs. VA alone was more than twice as likely to find bleeds and reduce fluoroscopy times without affecting kidney function, and without subjecting patients to the radiation of a nuclear bleeding scan. The ability of CTA before VA to find bleeding was comparable to that of an NBS, with an ability to localize bleeding about 60% better than that of an NBS.
Data source: Single-center review of an interventional radiology database of 161 patients after implementation of institutional policy.
Disclosures: Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
Acute Kidney Injury Implicated in Multiple Organ Failure
CHICAGO – Early kidney failure was associated with a 19-fold increased risk of multiple organ failure and a sixfold higher risk of death in a retrospective analysis of 1,273 trauma cases.
The study was done at the Rocky Mountain Regional Trauma Center of the University of Colorado at Denver to learn more about the epidemiology of acute kidney injury and its role in acute respiratory distress syndrome (ARDS) and subsequent multiple organ failure (MOF).
"Of the four major organ systems involved, the kidneys are often overlooked as MOF development has been thought to occur sequentially, being initiated by the lungs," Dr. Max V. Wohlauer said at the annual meeting of the American Association for the Surgery of Trauma.
He noted that postinjury MOF death rates remain high at 60%, "despite widespread availability [of] renal replacement therapy," and that therefore the prevention of early acute kidney injury could help to reduce complications and death rates in the critically ill.
Conceptually, MOF occurs as patients are resuscitated into a state of early systemic hyperinflammation, explained Dr. Wohlauer, who is now at the University of Washington Medical Center, Seattle. Although a mild response may be beneficial and will resolve in most patients as they recover, a massive traumatic insult can overwhelm a patient’s response to resuscitation, precipitating early organ failure.
"As neutrophil mediated ischemia-reperfusion injury is thought to be the driving factor in the development of ARDS, recent investigation highlights the critical function of the neutrophils in acute kidney injury as well," Dr. Wohlauer said. "Indeed, emerging evidence indicates that there is a direct contribution of the inflamed, injured kidney in the development of ARDS and MOF. Recent research has shown that acute kidney injury leads to increased vascular permeability and both cellular and soluble inflammation in the lungs, and that acute kidney injury–mediated lung dysfunction begins within hours."
Of the 1,273 patients the study evaluated, 21% went on to develop MOF with an overall mortality of 8%. Early acute kidney injury was detected in only 2% of the patients, but was associated with a 78% MOF rate and a 27% death rate, higher rates than isolated cardiac, liver, or lung dysfunction, Dr. Wohlauer reported. (See box.) The study defined acute kidney injury as an acute increase in creatinine greater than 1.8 mg/dL. Renal replacement therapy was mostly ineffective in these patients, he said.
The most important independent predictors of early acute kidney failure were shock, day 1 crystalloid count, day 2 base deficit, and a need for blood transfusion in the first 12 hours, according to Dr. Wohlauer. "Most patients who developed early kidney injury culminated in full-blown MOF, whereas only 34% of the lung failure cases evolved to ... full MOF," he said.
Dr. Mitchell Jay Cohen of San Francisco General Hospital noted that no consensus exists in the hospital on the definition of acute kidney injury, and that nephrology uses different definitions. "Can you identify a group of patients with acute kidney failure [who] don’t go on to develop multiple organ failure, and what distinguishes these two groups?"
Dr. Wohlauer noted that the renal component of the Denver Postinjury MOF Scale score (creatinine greater than 1.8 mg/dL) correlated strongly with the development of MOF, but that patients with acute kidney injury using the RIFLE (Risk, Injury, Failure, Loss, End-Stage Renal Disease) criteria did not go on to develop subsequent MOF.
"We’re suggesting that a creatinine of 1.8 is a severe insult to the kidney, and by the time that occurs [on day 2], a lot of the injury and inflammation has already occurred and we’re pedaling backwards to catch up," he said.
"When it comes to postinjury acute kidney injury, an ounce of prevention is worth a pound of cure," Dr. Wohlauer said. He noted that conservative strategies, including judicious use of IV contrast and rational use of hypotensive resuscitation, may help prevent early acute kidney injury and ensuing MOF.
"Once acute kidney injury had reared its ugly head, renal replacement therapy did very little to alter the progression of disease," he said.
Dr. Wohlauer said he had no conflicts to disclose. The study received funding from the National Institutes of Health.
CHICAGO – Early kidney failure was associated with a 19-fold increased risk of multiple organ failure and a sixfold higher risk of death in a retrospective analysis of 1,273 trauma cases.
The study was done at the Rocky Mountain Regional Trauma Center of the University of Colorado at Denver to learn more about the epidemiology of acute kidney injury and its role in acute respiratory distress syndrome (ARDS) and subsequent multiple organ failure (MOF).
"Of the four major organ systems involved, the kidneys are often overlooked as MOF development has been thought to occur sequentially, being initiated by the lungs," Dr. Max V. Wohlauer said at the annual meeting of the American Association for the Surgery of Trauma.
He noted that postinjury MOF death rates remain high at 60%, "despite widespread availability [of] renal replacement therapy," and that therefore the prevention of early acute kidney injury could help to reduce complications and death rates in the critically ill.
Conceptually, MOF occurs as patients are resuscitated into a state of early systemic hyperinflammation, explained Dr. Wohlauer, who is now at the University of Washington Medical Center, Seattle. Although a mild response may be beneficial and will resolve in most patients as they recover, a massive traumatic insult can overwhelm a patient’s response to resuscitation, precipitating early organ failure.
"As neutrophil mediated ischemia-reperfusion injury is thought to be the driving factor in the development of ARDS, recent investigation highlights the critical function of the neutrophils in acute kidney injury as well," Dr. Wohlauer said. "Indeed, emerging evidence indicates that there is a direct contribution of the inflamed, injured kidney in the development of ARDS and MOF. Recent research has shown that acute kidney injury leads to increased vascular permeability and both cellular and soluble inflammation in the lungs, and that acute kidney injury–mediated lung dysfunction begins within hours."
Of the 1,273 patients the study evaluated, 21% went on to develop MOF with an overall mortality of 8%. Early acute kidney injury was detected in only 2% of the patients, but was associated with a 78% MOF rate and a 27% death rate, higher rates than isolated cardiac, liver, or lung dysfunction, Dr. Wohlauer reported. (See box.) The study defined acute kidney injury as an acute increase in creatinine greater than 1.8 mg/dL. Renal replacement therapy was mostly ineffective in these patients, he said.
The most important independent predictors of early acute kidney failure were shock, day 1 crystalloid count, day 2 base deficit, and a need for blood transfusion in the first 12 hours, according to Dr. Wohlauer. "Most patients who developed early kidney injury culminated in full-blown MOF, whereas only 34% of the lung failure cases evolved to ... full MOF," he said.
Dr. Mitchell Jay Cohen of San Francisco General Hospital noted that no consensus exists in the hospital on the definition of acute kidney injury, and that nephrology uses different definitions. "Can you identify a group of patients with acute kidney failure [who] don’t go on to develop multiple organ failure, and what distinguishes these two groups?"
Dr. Wohlauer noted that the renal component of the Denver Postinjury MOF Scale score (creatinine greater than 1.8 mg/dL) correlated strongly with the development of MOF, but that patients with acute kidney injury using the RIFLE (Risk, Injury, Failure, Loss, End-Stage Renal Disease) criteria did not go on to develop subsequent MOF.
"We’re suggesting that a creatinine of 1.8 is a severe insult to the kidney, and by the time that occurs [on day 2], a lot of the injury and inflammation has already occurred and we’re pedaling backwards to catch up," he said.
"When it comes to postinjury acute kidney injury, an ounce of prevention is worth a pound of cure," Dr. Wohlauer said. He noted that conservative strategies, including judicious use of IV contrast and rational use of hypotensive resuscitation, may help prevent early acute kidney injury and ensuing MOF.
"Once acute kidney injury had reared its ugly head, renal replacement therapy did very little to alter the progression of disease," he said.
Dr. Wohlauer said he had no conflicts to disclose. The study received funding from the National Institutes of Health.
CHICAGO – Early kidney failure was associated with a 19-fold increased risk of multiple organ failure and a sixfold higher risk of death in a retrospective analysis of 1,273 trauma cases.
The study was done at the Rocky Mountain Regional Trauma Center of the University of Colorado at Denver to learn more about the epidemiology of acute kidney injury and its role in acute respiratory distress syndrome (ARDS) and subsequent multiple organ failure (MOF).
"Of the four major organ systems involved, the kidneys are often overlooked as MOF development has been thought to occur sequentially, being initiated by the lungs," Dr. Max V. Wohlauer said at the annual meeting of the American Association for the Surgery of Trauma.
He noted that postinjury MOF death rates remain high at 60%, "despite widespread availability [of] renal replacement therapy," and that therefore the prevention of early acute kidney injury could help to reduce complications and death rates in the critically ill.
Conceptually, MOF occurs as patients are resuscitated into a state of early systemic hyperinflammation, explained Dr. Wohlauer, who is now at the University of Washington Medical Center, Seattle. Although a mild response may be beneficial and will resolve in most patients as they recover, a massive traumatic insult can overwhelm a patient’s response to resuscitation, precipitating early organ failure.
"As neutrophil mediated ischemia-reperfusion injury is thought to be the driving factor in the development of ARDS, recent investigation highlights the critical function of the neutrophils in acute kidney injury as well," Dr. Wohlauer said. "Indeed, emerging evidence indicates that there is a direct contribution of the inflamed, injured kidney in the development of ARDS and MOF. Recent research has shown that acute kidney injury leads to increased vascular permeability and both cellular and soluble inflammation in the lungs, and that acute kidney injury–mediated lung dysfunction begins within hours."
Of the 1,273 patients the study evaluated, 21% went on to develop MOF with an overall mortality of 8%. Early acute kidney injury was detected in only 2% of the patients, but was associated with a 78% MOF rate and a 27% death rate, higher rates than isolated cardiac, liver, or lung dysfunction, Dr. Wohlauer reported. (See box.) The study defined acute kidney injury as an acute increase in creatinine greater than 1.8 mg/dL. Renal replacement therapy was mostly ineffective in these patients, he said.
The most important independent predictors of early acute kidney failure were shock, day 1 crystalloid count, day 2 base deficit, and a need for blood transfusion in the first 12 hours, according to Dr. Wohlauer. "Most patients who developed early kidney injury culminated in full-blown MOF, whereas only 34% of the lung failure cases evolved to ... full MOF," he said.
Dr. Mitchell Jay Cohen of San Francisco General Hospital noted that no consensus exists in the hospital on the definition of acute kidney injury, and that nephrology uses different definitions. "Can you identify a group of patients with acute kidney failure [who] don’t go on to develop multiple organ failure, and what distinguishes these two groups?"
Dr. Wohlauer noted that the renal component of the Denver Postinjury MOF Scale score (creatinine greater than 1.8 mg/dL) correlated strongly with the development of MOF, but that patients with acute kidney injury using the RIFLE (Risk, Injury, Failure, Loss, End-Stage Renal Disease) criteria did not go on to develop subsequent MOF.
"We’re suggesting that a creatinine of 1.8 is a severe insult to the kidney, and by the time that occurs [on day 2], a lot of the injury and inflammation has already occurred and we’re pedaling backwards to catch up," he said.
"When it comes to postinjury acute kidney injury, an ounce of prevention is worth a pound of cure," Dr. Wohlauer said. He noted that conservative strategies, including judicious use of IV contrast and rational use of hypotensive resuscitation, may help prevent early acute kidney injury and ensuing MOF.
"Once acute kidney injury had reared its ugly head, renal replacement therapy did very little to alter the progression of disease," he said.
Dr. Wohlauer said he had no conflicts to disclose. The study received funding from the National Institutes of Health.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
'Play or Pay' Underwrites Trauma Costs in Mississippi
CHICAGO – With reimbursements declining, finding the money to sustain trauma centers is becoming even more crucial for hospitals and the trauma surgeons who staff them, but a Mississippi "play or pay" policy for trauma centers could be a model for other states, according to a recent study.
"The ‘play or pay’ policy in Mississippi was associated with an increase in trauma system participation, and it created increased access for Mississippians, particularly in the southern part of the state," Dr. Ben L. Zarzaur said at the annual meeting of the American Association for the Surgery of Trauma.
Dr. Zarzaur presented an analysis of the state’s "play or pay" program based on 2,815 trauma admissions to the Presley Memorial Trauma Center in Memphis, a level I trauma center that covers southwestern Tennessee and northern Mississippi. Although Mississippi has had a fund for trauma centers for most of the last decade, the Mississippi Trauma Care System Fund underwent a major change in 2008 when the state implemented a "play or pay" policy.
He noted that readiness costs for level I trauma centers were about $2.7 million a year in 2004 (Am. J. Surg. 2004;187:7-13). Under "play or pay," hospitals now either establish a trauma center at a level that the state deems sufficient, or they pay into the fund.
"Fundamentally, 'play or pay' is a social contract with citizens and patients of the most important type."
For example, a hospital with a level III center that the state says should be a level II facility would pay $423,500, and fees can range up to $1.5 million, according to Dr. Zarzaur, a surgeon at the University of Tennessee Health Science Center, Memphis, and the Presley Memorial Trauma Center. Out-of-state trauma centers may participate if an independent review team determines that they comply with Mississippi regulations.
About 15% of the Trauma Care System Fund comes from these hospital fees, said Dr. John Porter of Jackson, Miss., an attendee at the paper presentation and a policy author and trauma surgeon at the University of Mississippi, Oxford, which has the only in-state level I center. The fund had accumulated more than $24 million through 2010, Dr. Zarzaur said. Funding also comes from motor vehicle fees and fines.
Before the policy was enacted in July 2008, 70 of 107 hospitals had trauma centers and two level I centers served the state, Dr. Zarzaur said. Today, 85 of 106 hospitals have trauma centers and a third level I center (the University of South Alabama in neighboring Mobile) has joined the program. "There was also an increase in level II centers in the southern part of the state, which had previously been underserved," Dr. Zarzaur noted.
The study found a shift in the payer mix after the policy was put in place, despite similar patient demographics, injury severity, and mortality. Associated with this change in payer mix was an increase in transfers from referring facilities, Dr. Zarzaur said. Among residents of Mississippi, "there was a decrease in the number of commercially insured patients and an increase in government-insured as well as self-pay patients, but there was no similar change in the Tennessee cohort," he said.
Overall, commercially insured patients made up 41% of patients admitted from Mississippi before the policy, compared with 36% since. The ratio of reimbursements to charges declined under the policy to 0.22, compared with 0.26 previously, with a ratio of 1 indicating profit, Dr. Zarzaur said.
At Presley, reimbursements for all patients decreased slightly for the entire cohort, Dr. Zarzaur said. Although that was more pronounced for Mississippians, "play or pay" made up for it. "Funds received from the Trauma Care System Fund almost completely offset this unfavorable change in payer mix," Dr. Zarzaur said.
Discussion leader Dr. David B. Hoyt, professor emeritus of surgery at the University of California, Irvine, and executive director of the American College of Surgeons, applauded the concept. "Fundamentally, ‘play or pay’ is a social contract with citizens and patients of the most important type: It legislates our responsibility to a safety net and allows hospitals to participate either directly or through financial support," he said.
He also noted that California tried to employ a similar funding scheme but abandoned it. "There’s a lesson in this about the persistence and the timing of a policy development that has implications for the AAST and the ACS Committee on Trauma," he said. "This is probably one of best ideas that will come forth as we consider ideas for refinancing our health system."
Dr. Zarzaur said he had no financial conflicts to disclose.
CHICAGO – With reimbursements declining, finding the money to sustain trauma centers is becoming even more crucial for hospitals and the trauma surgeons who staff them, but a Mississippi "play or pay" policy for trauma centers could be a model for other states, according to a recent study.
"The ‘play or pay’ policy in Mississippi was associated with an increase in trauma system participation, and it created increased access for Mississippians, particularly in the southern part of the state," Dr. Ben L. Zarzaur said at the annual meeting of the American Association for the Surgery of Trauma.
Dr. Zarzaur presented an analysis of the state’s "play or pay" program based on 2,815 trauma admissions to the Presley Memorial Trauma Center in Memphis, a level I trauma center that covers southwestern Tennessee and northern Mississippi. Although Mississippi has had a fund for trauma centers for most of the last decade, the Mississippi Trauma Care System Fund underwent a major change in 2008 when the state implemented a "play or pay" policy.
He noted that readiness costs for level I trauma centers were about $2.7 million a year in 2004 (Am. J. Surg. 2004;187:7-13). Under "play or pay," hospitals now either establish a trauma center at a level that the state deems sufficient, or they pay into the fund.
"Fundamentally, 'play or pay' is a social contract with citizens and patients of the most important type."
For example, a hospital with a level III center that the state says should be a level II facility would pay $423,500, and fees can range up to $1.5 million, according to Dr. Zarzaur, a surgeon at the University of Tennessee Health Science Center, Memphis, and the Presley Memorial Trauma Center. Out-of-state trauma centers may participate if an independent review team determines that they comply with Mississippi regulations.
About 15% of the Trauma Care System Fund comes from these hospital fees, said Dr. John Porter of Jackson, Miss., an attendee at the paper presentation and a policy author and trauma surgeon at the University of Mississippi, Oxford, which has the only in-state level I center. The fund had accumulated more than $24 million through 2010, Dr. Zarzaur said. Funding also comes from motor vehicle fees and fines.
Before the policy was enacted in July 2008, 70 of 107 hospitals had trauma centers and two level I centers served the state, Dr. Zarzaur said. Today, 85 of 106 hospitals have trauma centers and a third level I center (the University of South Alabama in neighboring Mobile) has joined the program. "There was also an increase in level II centers in the southern part of the state, which had previously been underserved," Dr. Zarzaur noted.
The study found a shift in the payer mix after the policy was put in place, despite similar patient demographics, injury severity, and mortality. Associated with this change in payer mix was an increase in transfers from referring facilities, Dr. Zarzaur said. Among residents of Mississippi, "there was a decrease in the number of commercially insured patients and an increase in government-insured as well as self-pay patients, but there was no similar change in the Tennessee cohort," he said.
Overall, commercially insured patients made up 41% of patients admitted from Mississippi before the policy, compared with 36% since. The ratio of reimbursements to charges declined under the policy to 0.22, compared with 0.26 previously, with a ratio of 1 indicating profit, Dr. Zarzaur said.
At Presley, reimbursements for all patients decreased slightly for the entire cohort, Dr. Zarzaur said. Although that was more pronounced for Mississippians, "play or pay" made up for it. "Funds received from the Trauma Care System Fund almost completely offset this unfavorable change in payer mix," Dr. Zarzaur said.
Discussion leader Dr. David B. Hoyt, professor emeritus of surgery at the University of California, Irvine, and executive director of the American College of Surgeons, applauded the concept. "Fundamentally, ‘play or pay’ is a social contract with citizens and patients of the most important type: It legislates our responsibility to a safety net and allows hospitals to participate either directly or through financial support," he said.
He also noted that California tried to employ a similar funding scheme but abandoned it. "There’s a lesson in this about the persistence and the timing of a policy development that has implications for the AAST and the ACS Committee on Trauma," he said. "This is probably one of best ideas that will come forth as we consider ideas for refinancing our health system."
Dr. Zarzaur said he had no financial conflicts to disclose.
CHICAGO – With reimbursements declining, finding the money to sustain trauma centers is becoming even more crucial for hospitals and the trauma surgeons who staff them, but a Mississippi "play or pay" policy for trauma centers could be a model for other states, according to a recent study.
"The ‘play or pay’ policy in Mississippi was associated with an increase in trauma system participation, and it created increased access for Mississippians, particularly in the southern part of the state," Dr. Ben L. Zarzaur said at the annual meeting of the American Association for the Surgery of Trauma.
Dr. Zarzaur presented an analysis of the state’s "play or pay" program based on 2,815 trauma admissions to the Presley Memorial Trauma Center in Memphis, a level I trauma center that covers southwestern Tennessee and northern Mississippi. Although Mississippi has had a fund for trauma centers for most of the last decade, the Mississippi Trauma Care System Fund underwent a major change in 2008 when the state implemented a "play or pay" policy.
He noted that readiness costs for level I trauma centers were about $2.7 million a year in 2004 (Am. J. Surg. 2004;187:7-13). Under "play or pay," hospitals now either establish a trauma center at a level that the state deems sufficient, or they pay into the fund.
"Fundamentally, 'play or pay' is a social contract with citizens and patients of the most important type."
For example, a hospital with a level III center that the state says should be a level II facility would pay $423,500, and fees can range up to $1.5 million, according to Dr. Zarzaur, a surgeon at the University of Tennessee Health Science Center, Memphis, and the Presley Memorial Trauma Center. Out-of-state trauma centers may participate if an independent review team determines that they comply with Mississippi regulations.
About 15% of the Trauma Care System Fund comes from these hospital fees, said Dr. John Porter of Jackson, Miss., an attendee at the paper presentation and a policy author and trauma surgeon at the University of Mississippi, Oxford, which has the only in-state level I center. The fund had accumulated more than $24 million through 2010, Dr. Zarzaur said. Funding also comes from motor vehicle fees and fines.
Before the policy was enacted in July 2008, 70 of 107 hospitals had trauma centers and two level I centers served the state, Dr. Zarzaur said. Today, 85 of 106 hospitals have trauma centers and a third level I center (the University of South Alabama in neighboring Mobile) has joined the program. "There was also an increase in level II centers in the southern part of the state, which had previously been underserved," Dr. Zarzaur noted.
The study found a shift in the payer mix after the policy was put in place, despite similar patient demographics, injury severity, and mortality. Associated with this change in payer mix was an increase in transfers from referring facilities, Dr. Zarzaur said. Among residents of Mississippi, "there was a decrease in the number of commercially insured patients and an increase in government-insured as well as self-pay patients, but there was no similar change in the Tennessee cohort," he said.
Overall, commercially insured patients made up 41% of patients admitted from Mississippi before the policy, compared with 36% since. The ratio of reimbursements to charges declined under the policy to 0.22, compared with 0.26 previously, with a ratio of 1 indicating profit, Dr. Zarzaur said.
At Presley, reimbursements for all patients decreased slightly for the entire cohort, Dr. Zarzaur said. Although that was more pronounced for Mississippians, "play or pay" made up for it. "Funds received from the Trauma Care System Fund almost completely offset this unfavorable change in payer mix," Dr. Zarzaur said.
Discussion leader Dr. David B. Hoyt, professor emeritus of surgery at the University of California, Irvine, and executive director of the American College of Surgeons, applauded the concept. "Fundamentally, ‘play or pay’ is a social contract with citizens and patients of the most important type: It legislates our responsibility to a safety net and allows hospitals to participate either directly or through financial support," he said.
He also noted that California tried to employ a similar funding scheme but abandoned it. "There’s a lesson in this about the persistence and the timing of a policy development that has implications for the AAST and the ACS Committee on Trauma," he said. "This is probably one of best ideas that will come forth as we consider ideas for refinancing our health system."
Dr. Zarzaur said he had no financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA