User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Children and COVID: Vaccines now available to all ages
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.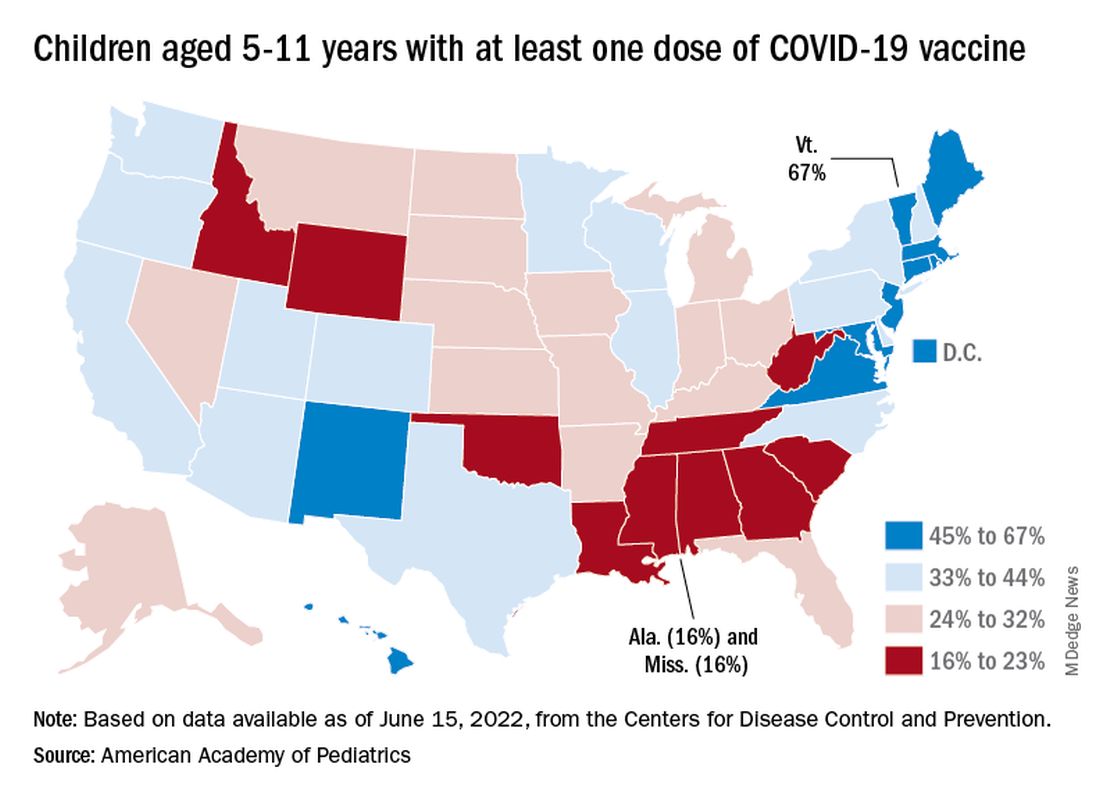
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.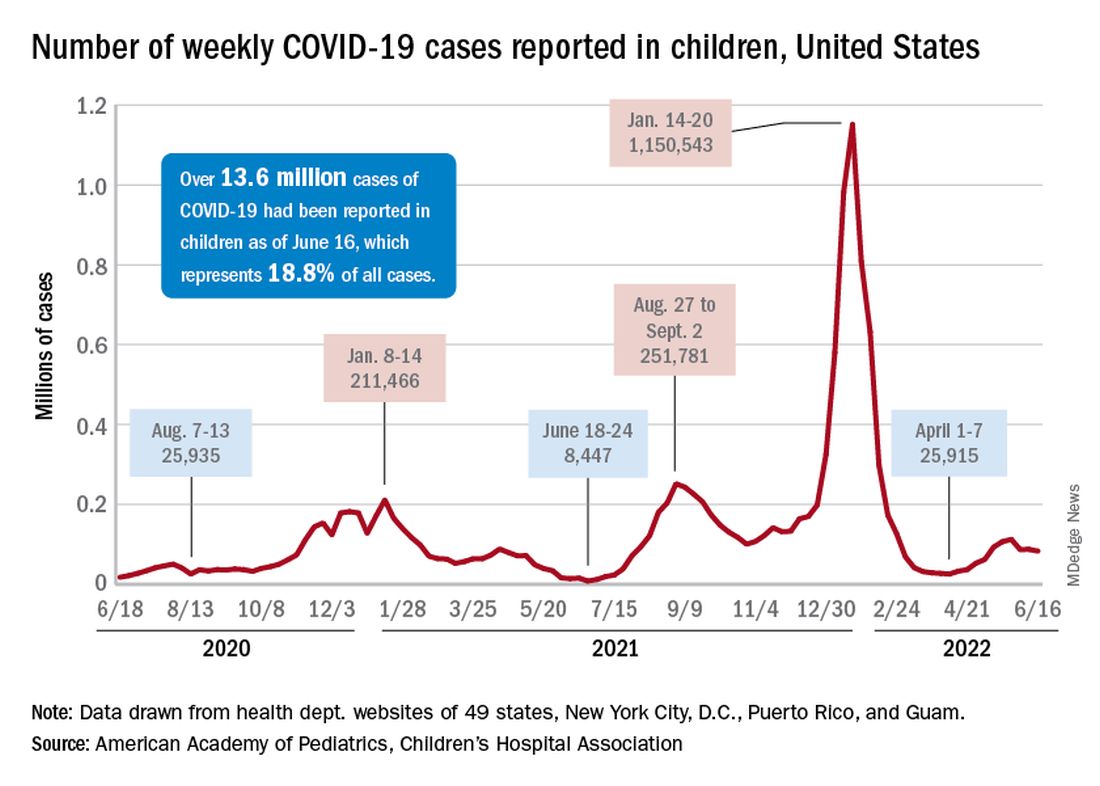
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.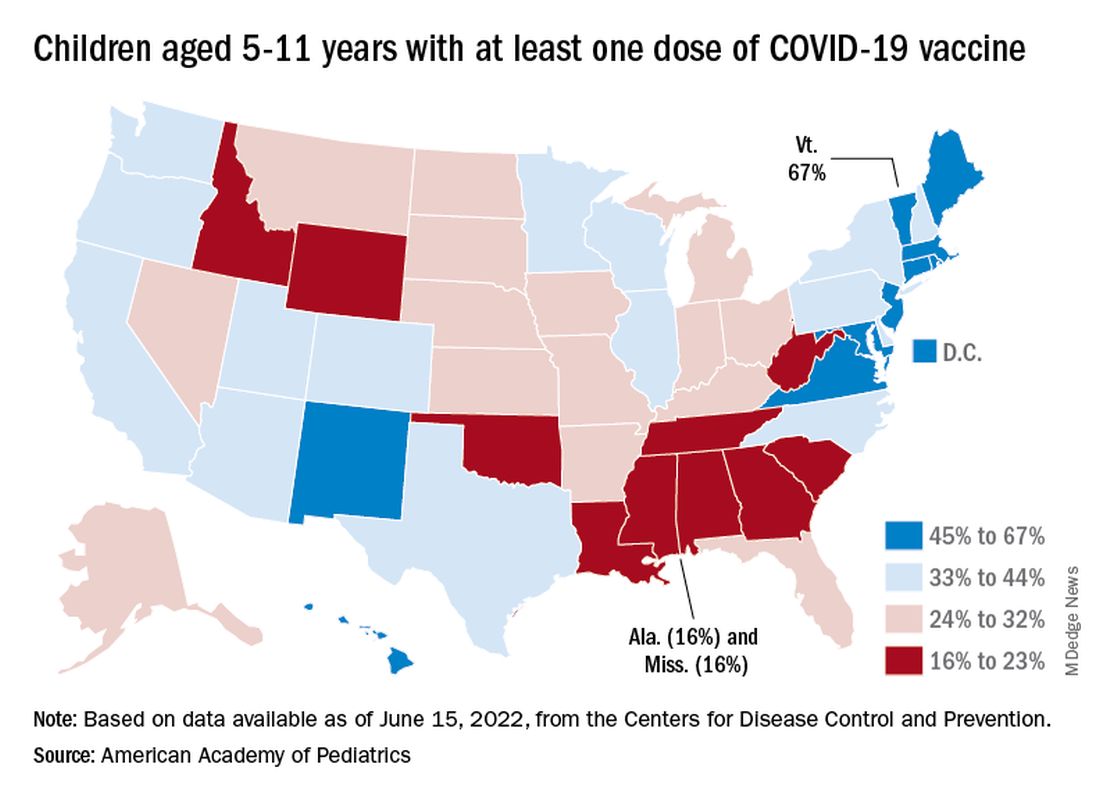
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.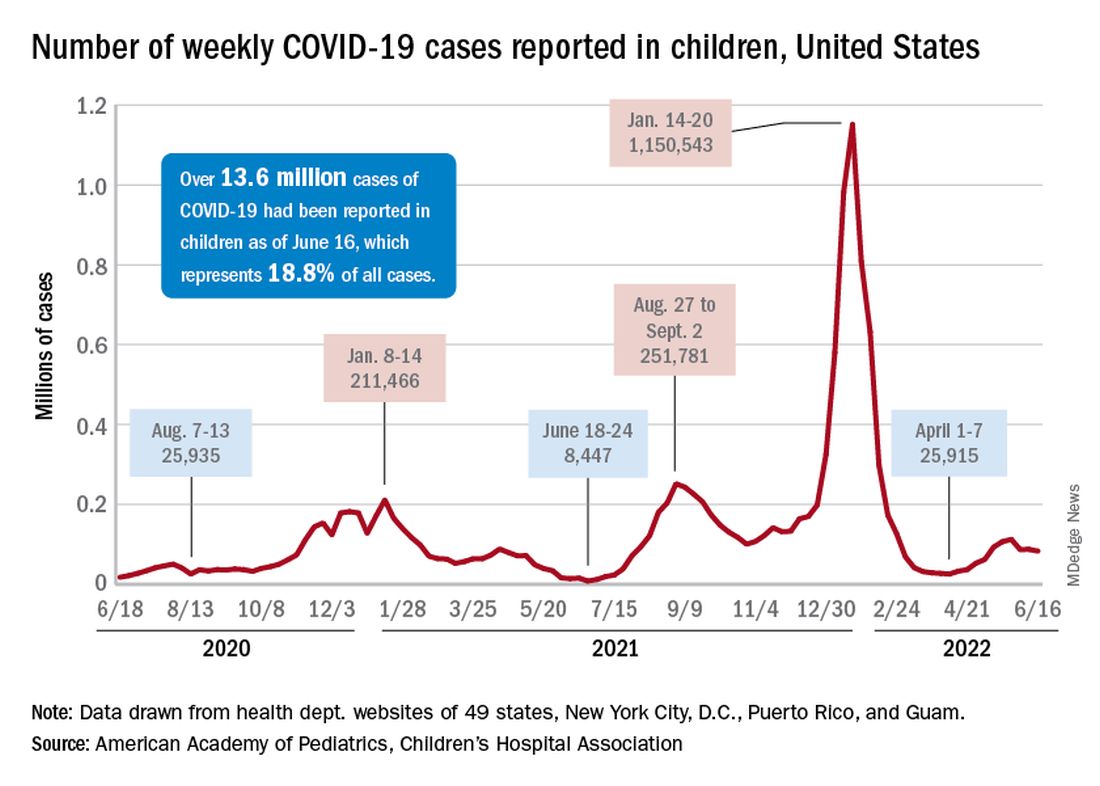
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.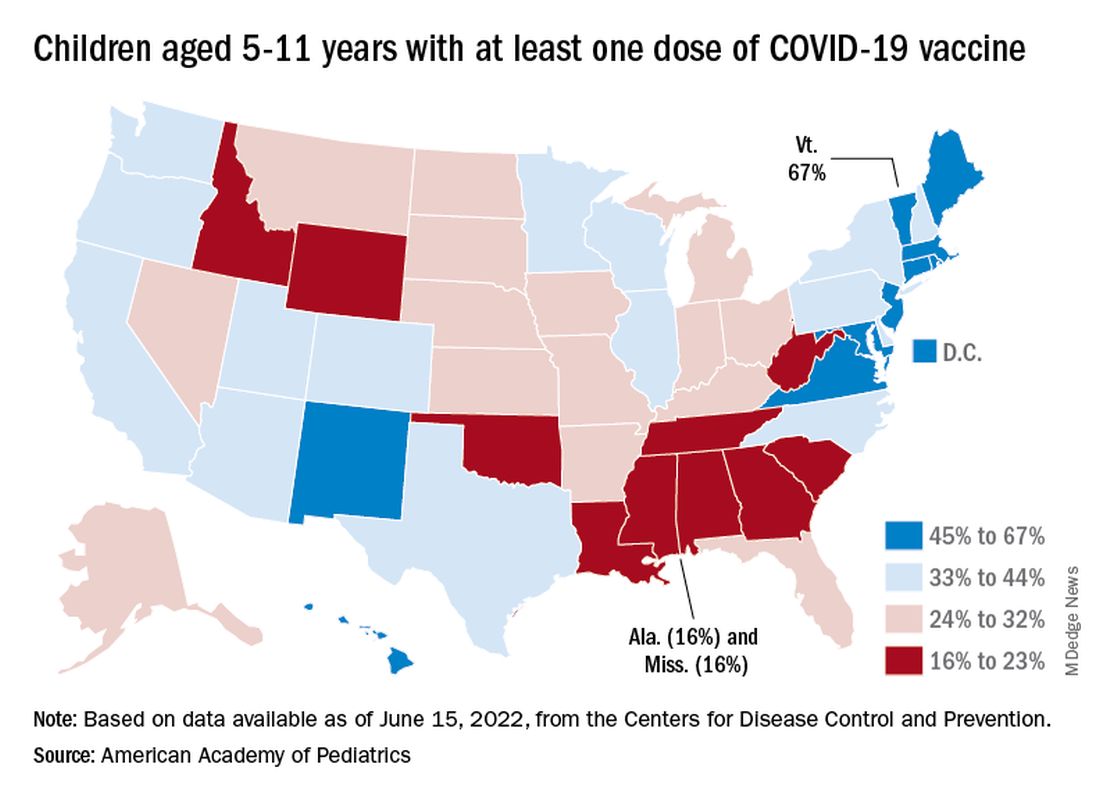
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.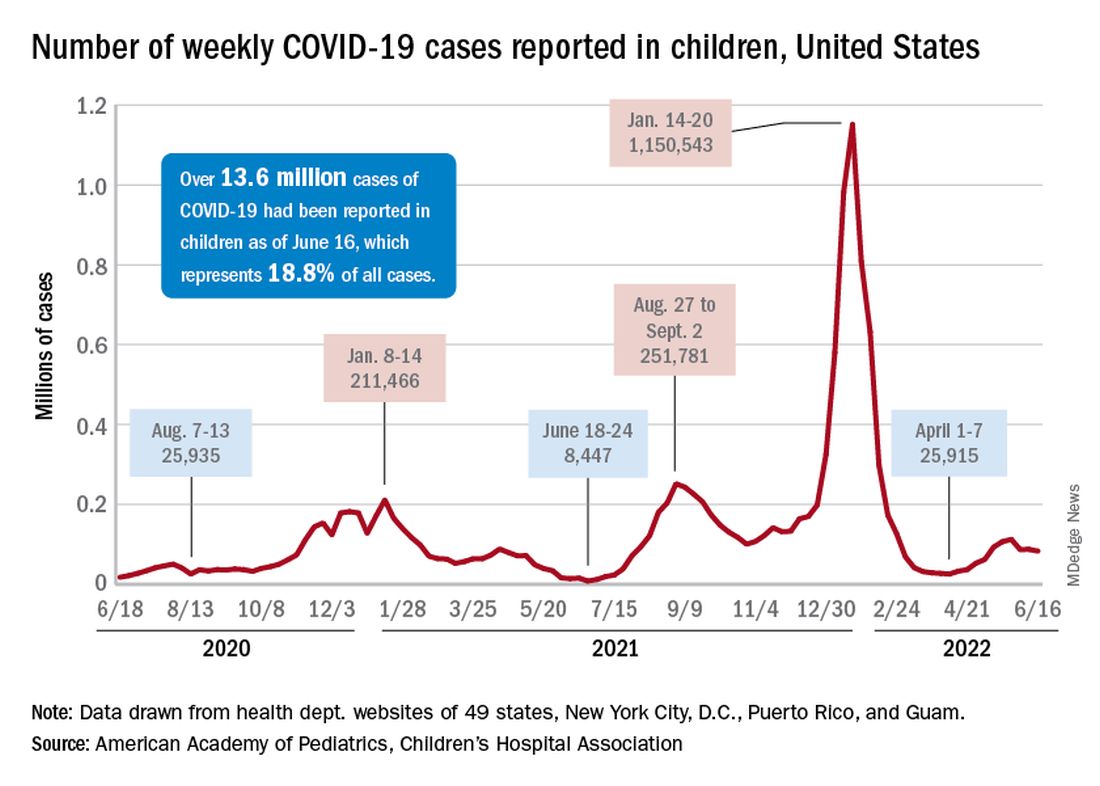
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
Heart failure: Medicare cost sharing may put quadruple therapy out of reach
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.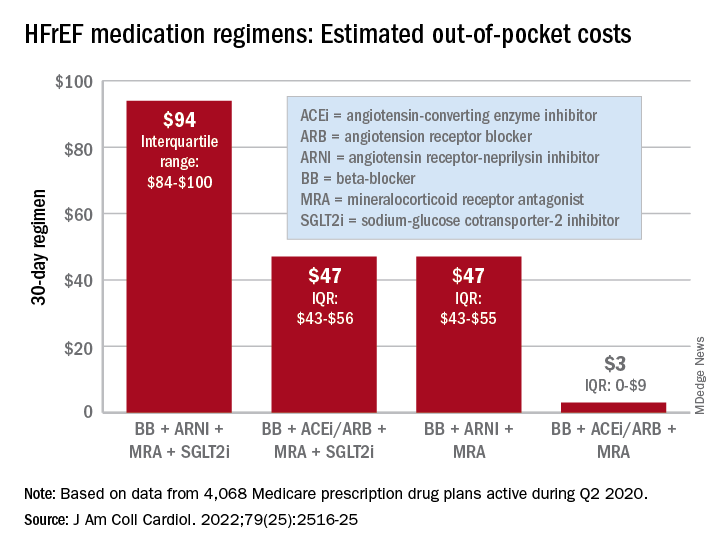
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
Out-of-pocket (OOP) costs for Medicare enrollees receiving quadruple drug therapy for heart failure with reduced ejection fraction were “substantially higher than regimens limited to generically available medications,” according to a new analysis of prescription drug plans.
“Despite the clinical benefit of quadruple therapy” consisting of beta-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs), mineralocorticoid receptor antagonists (MRAs), and sodium-glucose cotransporter-2 (SGLT2) inhibitors, “coverage was restricted primarily through cost sharing, and estimated annual OOP costs for beneficiaries were [over $2,000] per year under most plans,” wrote Kamil F. Faridi, MD, and associates. The findings were published in the Journal of the American College of Cardiology.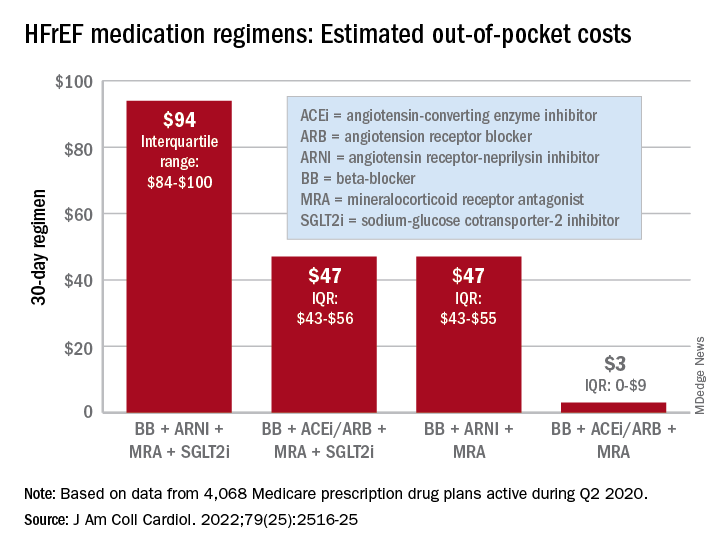
For just 1 month of quadruple drug therapy for heart failure with reduced ejection fraction (HFrEF), the estimated median OOP cost was $94 for individuals covered by a Medicare prescription drug plan during the second quarter of 2020, with the majority coming from the ARNI (median, $47) and the SGLT2 inhibitor (median, $45). Alternative HFrEF regimens were significantly less costly, ranging from $3 to $47 OOP, the investigators reported.
Almost all of the 4,068 plans participating in Medicare at that time covered quadruple therapy for HFrEF, but more than 99% restricted coverage by instituting cost sharing for medications at tier level 3 and above on the drug formularies. Such restrictions for ARNIs and SGLT2 inhibitors “might not be readily apparent to prescribing physicians,” wrote Dr. Faridi of Yale University, New Haven, Conn., and associates.
Other methods of regulating coverage were less common. Prior authorization of ARNIs was invoked by about a quarter of the plans, but none required authorization for any of the other drugs involved, and few plans used step therapy-requirements involving lower-cost alternatives, they noted.
“The use of cost sharing restricts access through high OOP costs for patients. Furthermore, these policies likely disadvantage relatively poorer patients (although the poorest Medicare patients will tend to be dual-enrolled in Medicaid and protected from cost sharing),” Jason H. Wasfy, MD, and Anna C. O’Kelly, MD, said in an accompanying editorial comment .
Since acceptable cost-effectiveness has been demonstrated for dapagliflozin, an SGLT1 inhibitor, and for the ARNIs, and because these medications have no generic equivalents, health plans should “use the discretion they have under Medicare Part D to reduce cost sharing for patients with HFrEF,” Dr. Wasfy and Dr. O’Kelly wrote, adding that the current study “demonstrates that without consensus on cost effectiveness from the societal perspective, costs can be imposed directly on patients in ways that slow uptake of cost-effective drugs.”
Data for all Medicare Advantage plans (n = 3,167) and standalone Part D plans (n = 901) came from the Medicare Prescription Drug Plan Formulary and Pricing Information Files. Annual OOP costs were estimated “using each phase of a 2020 Medicare part D standard benefit,” including deductible, standard coverage, coverage gap, and catastrophic coverage, the investigators explained.
Dr. Faridi and associates did not report any direct funding sources for their study. Dr Faridi received a grant from the National Institutes of Health outside the scope of the present work, and other investigators disclosed ties to the Food and Drug Administration, the Centers for Medicare and Medicaid Services, Johnson & Johnson, AstraZeneca, Boehringer Ingelheim, Amgen, Cytokinetics, and the Institute for Clinical and Economic Review.
Dr. Wasfy is supported by the American Heart Association and has received consulting fees from Pfizer and honoraria from the Institute for Clinical and Economic Review. Dr. O’Kelly has no relevant disclosures.
FROM THE JOURNAL Of the AMERICAN COLLEGE OF CARDIOLOGY
Microbiome’s new happy place: The beer gut
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Children and COVID: New cases hold steady in nonholiday week
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
Parkinson’s disease could be hiding behind those nightmares
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
Children and COVID: Cases down, start of vaccinations near
The first decline in COVID-19 cases among children since early April may have been holiday related, but the shortened week also brought news about vaccination for the youngest children.
The Food and Drug Administration has accepted Pfizer’s application for a COVID-19 vaccine for children under age 5, so vaccination could begin as early as June 21, according to White House COVID-19 response coordinator Ashish Jha, MD.
“We know that many, many parents are eager to vaccinate their youngest kids and it’s important to do this right,” Dr. Jha said at a White House press briefing June 2. “We expect that vaccinations will begin in earnest as early as June 21 and really roll on throughout that week.”
Decline may just be underreporting
Over on the incidence side of the pandemic, “Testing and reporting may have been affected by the holiday weekend [since] states may change their reporting schedules, which may cause irregularities in trends,” the American Academy of Pediatrics and the Children’s Hospital association said in their latest COVID report.
The decline in new cases was not spread uniformly across the four major regions of the United States. The count actually went up in the West for the week of May 27 to June 2, while the South saw the largest decline. The Midwest and Northeast, meanwhile, saw new cases drop for the second straight week, the AAP and CHA said.
The cumulative number of COVID-19 cases in children was up to 13.45 million as of June 2, with children representing 18.9% of all cases since the start of the pandemic, according to the two organizations. The Centers for Disease Control and Prevention reported figures of 13.14 million and 17.5% on June 6.
The AAP/CHA estimates, however, are based on state data that have become increasingly hard to obtain and subject to inconsistency. “Shortages of COVID-19 tests during surges and the increasing use of COVID-19 home tests likely affect the undercounting of COVID-19 cases,” they noted, and “at times when COVID-19 transmission is low, states might reduce the frequency information is updated.”
Vaccinations held steady over the holiday
The ongoing vaccination effort in children aged 5 years and older did not show a Memorial Day drop-off, as initial vaccinations held at 43,000 in 5- to 11-year-olds and at 27,000 in 12- to 17-year-olds for a second consecutive week. That number has ranged from 34,000 to 70,000 for the younger children and from 25,000 to 47,000 for the older group since mid-March, the AAP said in a separate weekly report.
Despite weekly vaccine initiations that have been roughly double those of the older children for months, the 5- to 11-year-olds are still only at 36.0% coverage with at least one dose, compared with 69.5% for the 12- to-17-year-olds. Full vaccination for the two age groups comes in at 29.3% and 59.6%, respectively, as of June 6, according to the CDC’s COVID Data Tracker.
The first decline in COVID-19 cases among children since early April may have been holiday related, but the shortened week also brought news about vaccination for the youngest children.
The Food and Drug Administration has accepted Pfizer’s application for a COVID-19 vaccine for children under age 5, so vaccination could begin as early as June 21, according to White House COVID-19 response coordinator Ashish Jha, MD.
“We know that many, many parents are eager to vaccinate their youngest kids and it’s important to do this right,” Dr. Jha said at a White House press briefing June 2. “We expect that vaccinations will begin in earnest as early as June 21 and really roll on throughout that week.”
Decline may just be underreporting
Over on the incidence side of the pandemic, “Testing and reporting may have been affected by the holiday weekend [since] states may change their reporting schedules, which may cause irregularities in trends,” the American Academy of Pediatrics and the Children’s Hospital association said in their latest COVID report.
The decline in new cases was not spread uniformly across the four major regions of the United States. The count actually went up in the West for the week of May 27 to June 2, while the South saw the largest decline. The Midwest and Northeast, meanwhile, saw new cases drop for the second straight week, the AAP and CHA said.
The cumulative number of COVID-19 cases in children was up to 13.45 million as of June 2, with children representing 18.9% of all cases since the start of the pandemic, according to the two organizations. The Centers for Disease Control and Prevention reported figures of 13.14 million and 17.5% on June 6.
The AAP/CHA estimates, however, are based on state data that have become increasingly hard to obtain and subject to inconsistency. “Shortages of COVID-19 tests during surges and the increasing use of COVID-19 home tests likely affect the undercounting of COVID-19 cases,” they noted, and “at times when COVID-19 transmission is low, states might reduce the frequency information is updated.”
Vaccinations held steady over the holiday
The ongoing vaccination effort in children aged 5 years and older did not show a Memorial Day drop-off, as initial vaccinations held at 43,000 in 5- to 11-year-olds and at 27,000 in 12- to 17-year-olds for a second consecutive week. That number has ranged from 34,000 to 70,000 for the younger children and from 25,000 to 47,000 for the older group since mid-March, the AAP said in a separate weekly report.
Despite weekly vaccine initiations that have been roughly double those of the older children for months, the 5- to 11-year-olds are still only at 36.0% coverage with at least one dose, compared with 69.5% for the 12- to-17-year-olds. Full vaccination for the two age groups comes in at 29.3% and 59.6%, respectively, as of June 6, according to the CDC’s COVID Data Tracker.
The first decline in COVID-19 cases among children since early April may have been holiday related, but the shortened week also brought news about vaccination for the youngest children.
The Food and Drug Administration has accepted Pfizer’s application for a COVID-19 vaccine for children under age 5, so vaccination could begin as early as June 21, according to White House COVID-19 response coordinator Ashish Jha, MD.
“We know that many, many parents are eager to vaccinate their youngest kids and it’s important to do this right,” Dr. Jha said at a White House press briefing June 2. “We expect that vaccinations will begin in earnest as early as June 21 and really roll on throughout that week.”
Decline may just be underreporting
Over on the incidence side of the pandemic, “Testing and reporting may have been affected by the holiday weekend [since] states may change their reporting schedules, which may cause irregularities in trends,” the American Academy of Pediatrics and the Children’s Hospital association said in their latest COVID report.
The decline in new cases was not spread uniformly across the four major regions of the United States. The count actually went up in the West for the week of May 27 to June 2, while the South saw the largest decline. The Midwest and Northeast, meanwhile, saw new cases drop for the second straight week, the AAP and CHA said.
The cumulative number of COVID-19 cases in children was up to 13.45 million as of June 2, with children representing 18.9% of all cases since the start of the pandemic, according to the two organizations. The Centers for Disease Control and Prevention reported figures of 13.14 million and 17.5% on June 6.
The AAP/CHA estimates, however, are based on state data that have become increasingly hard to obtain and subject to inconsistency. “Shortages of COVID-19 tests during surges and the increasing use of COVID-19 home tests likely affect the undercounting of COVID-19 cases,” they noted, and “at times when COVID-19 transmission is low, states might reduce the frequency information is updated.”
Vaccinations held steady over the holiday
The ongoing vaccination effort in children aged 5 years and older did not show a Memorial Day drop-off, as initial vaccinations held at 43,000 in 5- to 11-year-olds and at 27,000 in 12- to 17-year-olds for a second consecutive week. That number has ranged from 34,000 to 70,000 for the younger children and from 25,000 to 47,000 for the older group since mid-March, the AAP said in a separate weekly report.
Despite weekly vaccine initiations that have been roughly double those of the older children for months, the 5- to 11-year-olds are still only at 36.0% coverage with at least one dose, compared with 69.5% for the 12- to-17-year-olds. Full vaccination for the two age groups comes in at 29.3% and 59.6%, respectively, as of June 6, according to the CDC’s COVID Data Tracker.
Today’s medical oxymoron: Healthy overconfidence
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
Children & COVID: Rise in new cases slows
New cases of COVID-19 in children climbed for the seventh consecutive week, but the latest increase was the smallest of the seven, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Since the weekly total bottomed out at just under 26,000 in early April, the new-case count has risen by 28.0%, 11.8%, 43.5%, 17.4%, 50%, 14.6%, and 5.0%, based on data from the AAP/CHA weekly COVID-19 report.
The cumulative number of pediatric cases is almost 13.4 million since the pandemic began, and those infected children represent 18.9% of all cases, the AAP and CHA said based on data from 49 states, New York City, the District of Columbia, Puerto Rico, and Guam.
That 18.9% is noteworthy because it marks the first decline in that particular measure since the AAP and CHA started keeping track in April of 2020. Children’s share of the overall COVID burden had been holding at 19.0% for 14 straight weeks, the AAP/CHA data show.
Regionally, new cases were up in the South and the West, where recent rising trends continued, and down in the Midwest and Northeast, where the recent rising trends were reversed for the first time. At the state/territory level, Puerto Rico had the largest percent increase over the last 2 weeks, followed by Maryland and Delaware, the organizations noted in their joint report.
Hospital admissions in children aged 0-17 have changed little in the last week, with the Centers for Disease Control and Prevention reporting rates of 0.25 per 100,000 population on May 23 and 0.25 per 100,000 on May 29, the latest date available. There was, however, a move up to 0.26 per 100,000 from May 24 to May 28, and the CDC acknowledges a possible reporting delay over the most recent 7-day period.
Emergency department visits have dipped slightly in recent days, with children aged 0-11 years at a 7-day average of 2.0% of ED visits with diagnosed COVID on May 28, down from a 5-day stretch at 2.2% from May 19 to May 23. Children aged 12-15 years were at 1.8% on May 28, compared with 2.0% on May 23-24, and 15- to 17-year-olds were at 2.0% on May 28, down from the 2.1% reached over the previous 2 days, the CDC reported on its COVID Data Tracker.
New cases of COVID-19 in children climbed for the seventh consecutive week, but the latest increase was the smallest of the seven, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Since the weekly total bottomed out at just under 26,000 in early April, the new-case count has risen by 28.0%, 11.8%, 43.5%, 17.4%, 50%, 14.6%, and 5.0%, based on data from the AAP/CHA weekly COVID-19 report.
The cumulative number of pediatric cases is almost 13.4 million since the pandemic began, and those infected children represent 18.9% of all cases, the AAP and CHA said based on data from 49 states, New York City, the District of Columbia, Puerto Rico, and Guam.
That 18.9% is noteworthy because it marks the first decline in that particular measure since the AAP and CHA started keeping track in April of 2020. Children’s share of the overall COVID burden had been holding at 19.0% for 14 straight weeks, the AAP/CHA data show.
Regionally, new cases were up in the South and the West, where recent rising trends continued, and down in the Midwest and Northeast, where the recent rising trends were reversed for the first time. At the state/territory level, Puerto Rico had the largest percent increase over the last 2 weeks, followed by Maryland and Delaware, the organizations noted in their joint report.
Hospital admissions in children aged 0-17 have changed little in the last week, with the Centers for Disease Control and Prevention reporting rates of 0.25 per 100,000 population on May 23 and 0.25 per 100,000 on May 29, the latest date available. There was, however, a move up to 0.26 per 100,000 from May 24 to May 28, and the CDC acknowledges a possible reporting delay over the most recent 7-day period.
Emergency department visits have dipped slightly in recent days, with children aged 0-11 years at a 7-day average of 2.0% of ED visits with diagnosed COVID on May 28, down from a 5-day stretch at 2.2% from May 19 to May 23. Children aged 12-15 years were at 1.8% on May 28, compared with 2.0% on May 23-24, and 15- to 17-year-olds were at 2.0% on May 28, down from the 2.1% reached over the previous 2 days, the CDC reported on its COVID Data Tracker.
New cases of COVID-19 in children climbed for the seventh consecutive week, but the latest increase was the smallest of the seven, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Since the weekly total bottomed out at just under 26,000 in early April, the new-case count has risen by 28.0%, 11.8%, 43.5%, 17.4%, 50%, 14.6%, and 5.0%, based on data from the AAP/CHA weekly COVID-19 report.
The cumulative number of pediatric cases is almost 13.4 million since the pandemic began, and those infected children represent 18.9% of all cases, the AAP and CHA said based on data from 49 states, New York City, the District of Columbia, Puerto Rico, and Guam.
That 18.9% is noteworthy because it marks the first decline in that particular measure since the AAP and CHA started keeping track in April of 2020. Children’s share of the overall COVID burden had been holding at 19.0% for 14 straight weeks, the AAP/CHA data show.
Regionally, new cases were up in the South and the West, where recent rising trends continued, and down in the Midwest and Northeast, where the recent rising trends were reversed for the first time. At the state/territory level, Puerto Rico had the largest percent increase over the last 2 weeks, followed by Maryland and Delaware, the organizations noted in their joint report.
Hospital admissions in children aged 0-17 have changed little in the last week, with the Centers for Disease Control and Prevention reporting rates of 0.25 per 100,000 population on May 23 and 0.25 per 100,000 on May 29, the latest date available. There was, however, a move up to 0.26 per 100,000 from May 24 to May 28, and the CDC acknowledges a possible reporting delay over the most recent 7-day period.
Emergency department visits have dipped slightly in recent days, with children aged 0-11 years at a 7-day average of 2.0% of ED visits with diagnosed COVID on May 28, down from a 5-day stretch at 2.2% from May 19 to May 23. Children aged 12-15 years were at 1.8% on May 28, compared with 2.0% on May 23-24, and 15- to 17-year-olds were at 2.0% on May 28, down from the 2.1% reached over the previous 2 days, the CDC reported on its COVID Data Tracker.
Crohn’s disease research goes to the dogs
Why it might be better to be a dog person
Here’s that old debate again: Dogs or cats? You probably have your own opinion, but research presented at this year’s Digestive Disease Week may have tipped the scale by showing that children who lived with dogs may be less likely to have Crohn’s disease as adults.
The research was done by having approximately 4,300 people closely related to patients with Crohn’s disease fill out an environmental questionnaire. Using these data, the research team looked into environmental factors such as size of the families, where the home was, how many bathrooms the homes had, and quality of drinking water.
The researchers found that those who had or were exposed to dogs between the ages of 5 and 15 years were more likely to have healthy gut permeability and balanced microbes, which increased their protection against Crohn’s disease.
“Our study seems to add to others that have explored the ‘hygiene hypothesis’ which suggests that the lack of exposure to microbes early in life may lead to lack of immune regulation toward environmental microbes,” senior author Williams Turpin, PhD, said in the written statement.
The researchers aren’t sure why they didn’t get the same findings with cats, but Dr. Turpin theorized that dog owners tend to be outside more with their dogs or live in places with more green space, which are good protectors against Crohn’s disease.
It’s all good for dog owners, but do their pets’ parasites make you more attractive? Just more fuel for the ongoing debate.
Come for the history, stay for the fossilized parasites
Another week, another analysis of old British poop. LOTME really is your one-stop shop for all the important, hard-hitting news about historic parasites. You’re welcome, Internet.
The news this week is from Stonehenge, which is apparently kind of a big deal. Rocks in a circle, celestial calendar, cultural significance, whatever. We’re not here to talk about rocks. We’re here to talk about, uh, rocks. Smaller rocks. Specifically, coprolites, which are essentially poop turned into a rock. (Though now we’re imagining Stonehenge made out of fossilized poop rocks. Would it still be a big tourist destination? We can see both sides of the argument on that one.)
Archaeologists from the University of Cambridge have conducted an analysis of coprolites from Durrington Walls, a Neolithic settlement just a few kilometers from Stonehenge. The town dates to the same time that Stonehenge was constructed, and it’s believed that the residents were responsible for building the landmark. These coprolites, depending on what’s inside, can tell us a lot about how the builders of Stonehenge lived and, more specifically, how they ate.
In this case, the coprolites of one human and three dogs contained capillariid worm eggs. These worms come from cows, and when a human is typically infected, the eggs embed in the liver and do not pass through the body. Finding them in excrement indicates that the people were eating raw cow organs and feeding leftovers to their dogs. This is interesting, because a preponderance of pottery and cooking implements also found at the site indicates that the residents of Durrington Walls were spit-roasting or boiling their beef and pork. So the meat was cooked, but not the organs. That is an interesting dietary decision, ancient British people. Then again, modern British cuisine exists. At least now we know where they got it from.
This new research raises one other very important question: When are we going to get a full-on guided tour of all the important coprolite sites in Britain? They’ve clearly got plenty of them, and the tourist demand for ancient parasites must be sky-high. Come on, capitalism, follow through on this. We’d go.
Everyone lies: Food intake edition
Do you have any patients on special diets? Do you ask them if they are following those diets? Don’t bother, because they’re lying. Everyone lies about the food they eat. Everyone. Obese people lie, and nonobese people lie.
Investigators at the University of Essex in England asked 221 adults to keep food diaries, and then they checked on energy consumption by analyzing radioactive water levels in the participants’ urine over a 10-day period.
Underreporting of food consumption was rampant, even among those who were not obese. The obese subjects did underreport by a greater extent (1,200 calories per day) than did those who were not obese, who were off by only 800 calories, but the obese participants burned about 400 calories more each day than did the nonobese, so the difference was a wash.
Everyone ended up underreporting their calorie consumption by an average of about 900 calories, and the investigators were good enough to provide some food equivalents, tops on the list being three MacDonald’s cheeseburgers.
“Public health recommendations have historically relied heavily on self-reported energy intake values,” senior author Gavin Sandercock, PhD, said in a EurekAlert statement, and “recognising that the measures of energy intake are incorrect might result in the setting of more realistic targets.”
Maybe you can be more realistic with your patients, too. Go ahead and ask Mr. Smith about the burger sticking out of his coat pocket, because there are probably two more you can’t see. We’ve each got 900 calories hiding on us somewhere. Ours is usually pizza.
The art of the gallbladder
Ever thought you would see a portrait of a gallbladder hanging up in a gallery? Not just an artist’s rendition, but an actual photo from an actual patient? Well, you can at the Soloway Gallery in Brooklyn, N.Y., at least until June 12.
The artist? K.C. Joseph, MD, a general surgeon from St. Marie, Pa., who died in 2015. His daughter Melissa is the curator of the show and told ARTnews about the interesting connection her father had with art and surgery.
In 2010, Dr. Joseph gave his daughter a box of photos and said “Make me a famous artist,” she recalled. At first, “I was like, ‘These are weird,’ and then I put them under my bed for 10 years.”
Apparently he had been making art with his patients’ organs for about 15 years and had a system in which he put each one together. Before a surgery Dr. Joseph would make a note card with the patient’s name handwritten in calligraphy with a couple of pages taken out of the magazine from the waiting room as the backdrop. Afterward, when the patient was in recovery, the removed organ would be placed among the pages and the name card. A photo was taken with the same endoscope that was used for the procedure.
After the show’s debut, people reached out expressing their love for their photos. “I wish, before he died, I had asked him more questions about it,” Ms. Joseph told ARTnews. “I’m regretting it so much now, kicking myself.”
Who gets to take home an artsy photo of their gallbladder after getting it removed? Not us, that’s who. Each collage is a one-of-a-kind piece. They definitely should be framed and shown in an art gallery. Oh, right. Never mind.
Why it might be better to be a dog person
Here’s that old debate again: Dogs or cats? You probably have your own opinion, but research presented at this year’s Digestive Disease Week may have tipped the scale by showing that children who lived with dogs may be less likely to have Crohn’s disease as adults.
The research was done by having approximately 4,300 people closely related to patients with Crohn’s disease fill out an environmental questionnaire. Using these data, the research team looked into environmental factors such as size of the families, where the home was, how many bathrooms the homes had, and quality of drinking water.
The researchers found that those who had or were exposed to dogs between the ages of 5 and 15 years were more likely to have healthy gut permeability and balanced microbes, which increased their protection against Crohn’s disease.
“Our study seems to add to others that have explored the ‘hygiene hypothesis’ which suggests that the lack of exposure to microbes early in life may lead to lack of immune regulation toward environmental microbes,” senior author Williams Turpin, PhD, said in the written statement.
The researchers aren’t sure why they didn’t get the same findings with cats, but Dr. Turpin theorized that dog owners tend to be outside more with their dogs or live in places with more green space, which are good protectors against Crohn’s disease.
It’s all good for dog owners, but do their pets’ parasites make you more attractive? Just more fuel for the ongoing debate.
Come for the history, stay for the fossilized parasites
Another week, another analysis of old British poop. LOTME really is your one-stop shop for all the important, hard-hitting news about historic parasites. You’re welcome, Internet.
The news this week is from Stonehenge, which is apparently kind of a big deal. Rocks in a circle, celestial calendar, cultural significance, whatever. We’re not here to talk about rocks. We’re here to talk about, uh, rocks. Smaller rocks. Specifically, coprolites, which are essentially poop turned into a rock. (Though now we’re imagining Stonehenge made out of fossilized poop rocks. Would it still be a big tourist destination? We can see both sides of the argument on that one.)
Archaeologists from the University of Cambridge have conducted an analysis of coprolites from Durrington Walls, a Neolithic settlement just a few kilometers from Stonehenge. The town dates to the same time that Stonehenge was constructed, and it’s believed that the residents were responsible for building the landmark. These coprolites, depending on what’s inside, can tell us a lot about how the builders of Stonehenge lived and, more specifically, how they ate.
In this case, the coprolites of one human and three dogs contained capillariid worm eggs. These worms come from cows, and when a human is typically infected, the eggs embed in the liver and do not pass through the body. Finding them in excrement indicates that the people were eating raw cow organs and feeding leftovers to their dogs. This is interesting, because a preponderance of pottery and cooking implements also found at the site indicates that the residents of Durrington Walls were spit-roasting or boiling their beef and pork. So the meat was cooked, but not the organs. That is an interesting dietary decision, ancient British people. Then again, modern British cuisine exists. At least now we know where they got it from.
This new research raises one other very important question: When are we going to get a full-on guided tour of all the important coprolite sites in Britain? They’ve clearly got plenty of them, and the tourist demand for ancient parasites must be sky-high. Come on, capitalism, follow through on this. We’d go.
Everyone lies: Food intake edition
Do you have any patients on special diets? Do you ask them if they are following those diets? Don’t bother, because they’re lying. Everyone lies about the food they eat. Everyone. Obese people lie, and nonobese people lie.
Investigators at the University of Essex in England asked 221 adults to keep food diaries, and then they checked on energy consumption by analyzing radioactive water levels in the participants’ urine over a 10-day period.
Underreporting of food consumption was rampant, even among those who were not obese. The obese subjects did underreport by a greater extent (1,200 calories per day) than did those who were not obese, who were off by only 800 calories, but the obese participants burned about 400 calories more each day than did the nonobese, so the difference was a wash.
Everyone ended up underreporting their calorie consumption by an average of about 900 calories, and the investigators were good enough to provide some food equivalents, tops on the list being three MacDonald’s cheeseburgers.
“Public health recommendations have historically relied heavily on self-reported energy intake values,” senior author Gavin Sandercock, PhD, said in a EurekAlert statement, and “recognising that the measures of energy intake are incorrect might result in the setting of more realistic targets.”
Maybe you can be more realistic with your patients, too. Go ahead and ask Mr. Smith about the burger sticking out of his coat pocket, because there are probably two more you can’t see. We’ve each got 900 calories hiding on us somewhere. Ours is usually pizza.
The art of the gallbladder
Ever thought you would see a portrait of a gallbladder hanging up in a gallery? Not just an artist’s rendition, but an actual photo from an actual patient? Well, you can at the Soloway Gallery in Brooklyn, N.Y., at least until June 12.
The artist? K.C. Joseph, MD, a general surgeon from St. Marie, Pa., who died in 2015. His daughter Melissa is the curator of the show and told ARTnews about the interesting connection her father had with art and surgery.
In 2010, Dr. Joseph gave his daughter a box of photos and said “Make me a famous artist,” she recalled. At first, “I was like, ‘These are weird,’ and then I put them under my bed for 10 years.”
Apparently he had been making art with his patients’ organs for about 15 years and had a system in which he put each one together. Before a surgery Dr. Joseph would make a note card with the patient’s name handwritten in calligraphy with a couple of pages taken out of the magazine from the waiting room as the backdrop. Afterward, when the patient was in recovery, the removed organ would be placed among the pages and the name card. A photo was taken with the same endoscope that was used for the procedure.
After the show’s debut, people reached out expressing their love for their photos. “I wish, before he died, I had asked him more questions about it,” Ms. Joseph told ARTnews. “I’m regretting it so much now, kicking myself.”
Who gets to take home an artsy photo of their gallbladder after getting it removed? Not us, that’s who. Each collage is a one-of-a-kind piece. They definitely should be framed and shown in an art gallery. Oh, right. Never mind.
Why it might be better to be a dog person
Here’s that old debate again: Dogs or cats? You probably have your own opinion, but research presented at this year’s Digestive Disease Week may have tipped the scale by showing that children who lived with dogs may be less likely to have Crohn’s disease as adults.
The research was done by having approximately 4,300 people closely related to patients with Crohn’s disease fill out an environmental questionnaire. Using these data, the research team looked into environmental factors such as size of the families, where the home was, how many bathrooms the homes had, and quality of drinking water.
The researchers found that those who had or were exposed to dogs between the ages of 5 and 15 years were more likely to have healthy gut permeability and balanced microbes, which increased their protection against Crohn’s disease.
“Our study seems to add to others that have explored the ‘hygiene hypothesis’ which suggests that the lack of exposure to microbes early in life may lead to lack of immune regulation toward environmental microbes,” senior author Williams Turpin, PhD, said in the written statement.
The researchers aren’t sure why they didn’t get the same findings with cats, but Dr. Turpin theorized that dog owners tend to be outside more with their dogs or live in places with more green space, which are good protectors against Crohn’s disease.
It’s all good for dog owners, but do their pets’ parasites make you more attractive? Just more fuel for the ongoing debate.
Come for the history, stay for the fossilized parasites
Another week, another analysis of old British poop. LOTME really is your one-stop shop for all the important, hard-hitting news about historic parasites. You’re welcome, Internet.
The news this week is from Stonehenge, which is apparently kind of a big deal. Rocks in a circle, celestial calendar, cultural significance, whatever. We’re not here to talk about rocks. We’re here to talk about, uh, rocks. Smaller rocks. Specifically, coprolites, which are essentially poop turned into a rock. (Though now we’re imagining Stonehenge made out of fossilized poop rocks. Would it still be a big tourist destination? We can see both sides of the argument on that one.)
Archaeologists from the University of Cambridge have conducted an analysis of coprolites from Durrington Walls, a Neolithic settlement just a few kilometers from Stonehenge. The town dates to the same time that Stonehenge was constructed, and it’s believed that the residents were responsible for building the landmark. These coprolites, depending on what’s inside, can tell us a lot about how the builders of Stonehenge lived and, more specifically, how they ate.
In this case, the coprolites of one human and three dogs contained capillariid worm eggs. These worms come from cows, and when a human is typically infected, the eggs embed in the liver and do not pass through the body. Finding them in excrement indicates that the people were eating raw cow organs and feeding leftovers to their dogs. This is interesting, because a preponderance of pottery and cooking implements also found at the site indicates that the residents of Durrington Walls were spit-roasting or boiling their beef and pork. So the meat was cooked, but not the organs. That is an interesting dietary decision, ancient British people. Then again, modern British cuisine exists. At least now we know where they got it from.
This new research raises one other very important question: When are we going to get a full-on guided tour of all the important coprolite sites in Britain? They’ve clearly got plenty of them, and the tourist demand for ancient parasites must be sky-high. Come on, capitalism, follow through on this. We’d go.
Everyone lies: Food intake edition
Do you have any patients on special diets? Do you ask them if they are following those diets? Don’t bother, because they’re lying. Everyone lies about the food they eat. Everyone. Obese people lie, and nonobese people lie.
Investigators at the University of Essex in England asked 221 adults to keep food diaries, and then they checked on energy consumption by analyzing radioactive water levels in the participants’ urine over a 10-day period.
Underreporting of food consumption was rampant, even among those who were not obese. The obese subjects did underreport by a greater extent (1,200 calories per day) than did those who were not obese, who were off by only 800 calories, but the obese participants burned about 400 calories more each day than did the nonobese, so the difference was a wash.
Everyone ended up underreporting their calorie consumption by an average of about 900 calories, and the investigators were good enough to provide some food equivalents, tops on the list being three MacDonald’s cheeseburgers.
“Public health recommendations have historically relied heavily on self-reported energy intake values,” senior author Gavin Sandercock, PhD, said in a EurekAlert statement, and “recognising that the measures of energy intake are incorrect might result in the setting of more realistic targets.”
Maybe you can be more realistic with your patients, too. Go ahead and ask Mr. Smith about the burger sticking out of his coat pocket, because there are probably two more you can’t see. We’ve each got 900 calories hiding on us somewhere. Ours is usually pizza.
The art of the gallbladder
Ever thought you would see a portrait of a gallbladder hanging up in a gallery? Not just an artist’s rendition, but an actual photo from an actual patient? Well, you can at the Soloway Gallery in Brooklyn, N.Y., at least until June 12.
The artist? K.C. Joseph, MD, a general surgeon from St. Marie, Pa., who died in 2015. His daughter Melissa is the curator of the show and told ARTnews about the interesting connection her father had with art and surgery.
In 2010, Dr. Joseph gave his daughter a box of photos and said “Make me a famous artist,” she recalled. At first, “I was like, ‘These are weird,’ and then I put them under my bed for 10 years.”
Apparently he had been making art with his patients’ organs for about 15 years and had a system in which he put each one together. Before a surgery Dr. Joseph would make a note card with the patient’s name handwritten in calligraphy with a couple of pages taken out of the magazine from the waiting room as the backdrop. Afterward, when the patient was in recovery, the removed organ would be placed among the pages and the name card. A photo was taken with the same endoscope that was used for the procedure.
After the show’s debut, people reached out expressing their love for their photos. “I wish, before he died, I had asked him more questions about it,” Ms. Joseph told ARTnews. “I’m regretting it so much now, kicking myself.”
Who gets to take home an artsy photo of their gallbladder after getting it removed? Not us, that’s who. Each collage is a one-of-a-kind piece. They definitely should be framed and shown in an art gallery. Oh, right. Never mind.
Children and COVID: Weekly cases keep rising past 100,000
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.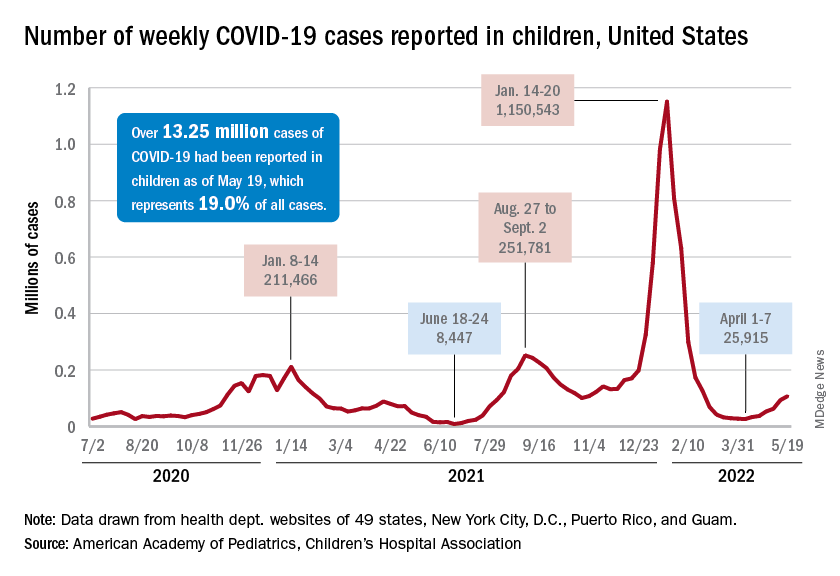
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”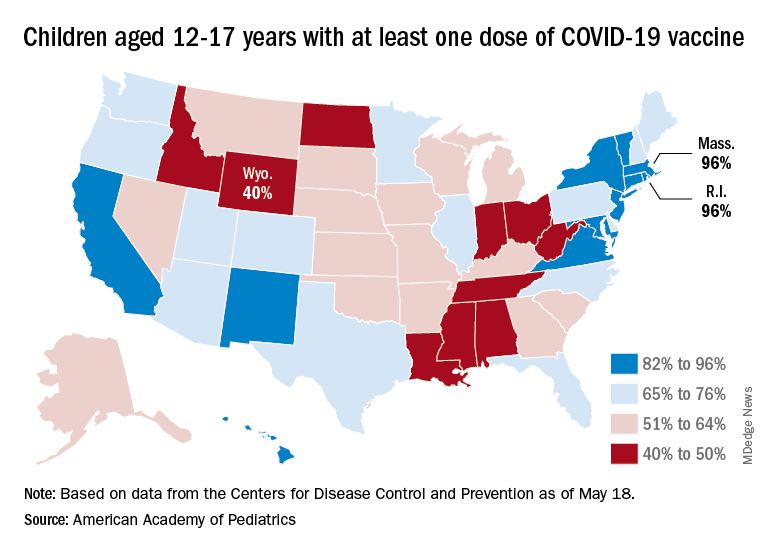
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.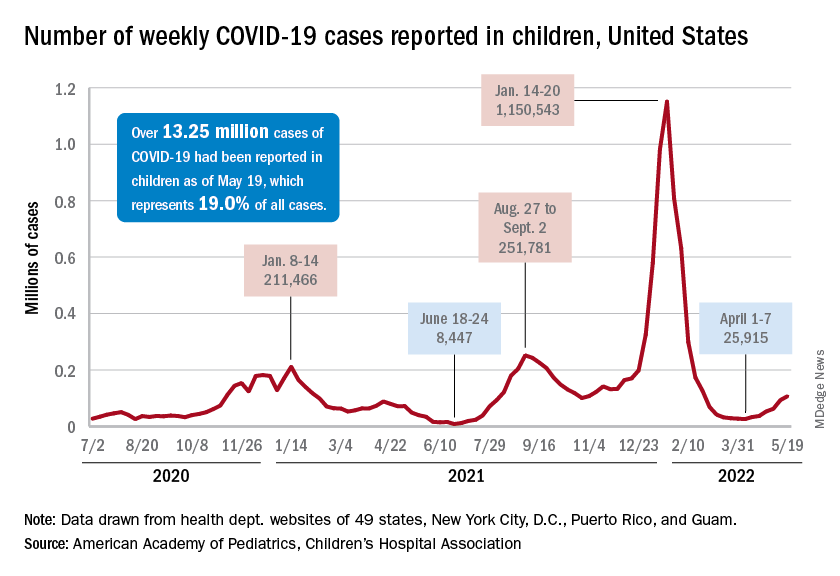
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”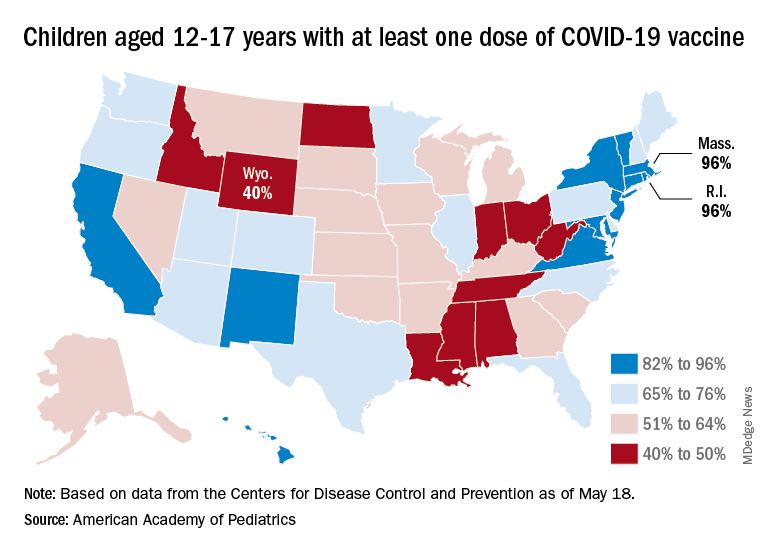
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
New cases were up by 14.6% over the previous week to just over 107,000 reported during May 13-16, marking the sixth straight increase since April 1-7, when the count was almost 26,000. Over that period, weekly cases rose 313%, based on data in the latest weekly COVID report from the AAP and CHA.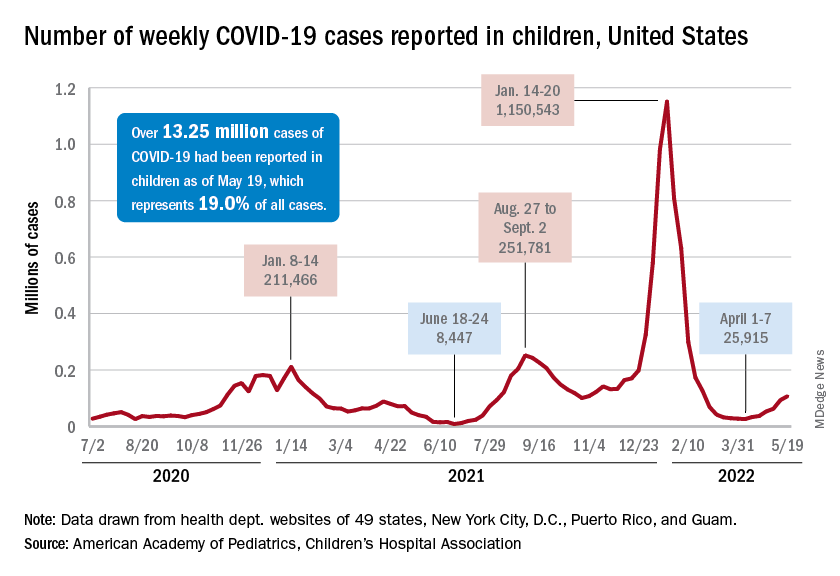
Rates reported by the Centers for Disease Control and Prevention show the same trend. Weekly cases per 100,000 population, which were down to 34.9 in children aged 0-4 years and 43.1 for those aged 5-11 on March 26, were up to 49.5 and 52.2, respectively, by April 16. The pace picked up right after that, and as of May 14, the rates of new cases were 125.4 per 100,000 in children aged 0-4 years and 143.1 in those aged 5-11, the CDC said.
Hospital admissions continue to rise as well. The rate of new admissions in children aged 0-17 was up to 0.25 per 100,000 population on May 18, nearly double the 0.13 per 100,000 recorded as late as April 13. The latest 7-day average count for new admissions, 163 per day from May 15-21, is down from the previous week’s 175 per day, but the CDC also acknowledges potential reporting delays in the most recent 7-day period.
Both of those weekly averages, however, are far below the peak rate for the pandemic, 914 per day, which occurred Jan. 10-16, 2022, during the Omicron surge. Since the CDC began keeping count at the beginning of August 2020, more than 125,000 children aged 0-17 years have been admitted with confirmed COVID-19, which is about 2.7% of all admissions over that period, the CDC’s data show.
Booster gets the green light
The week brought some positive news on the prevention side, though, as the CDC officially approved a COVID vaccine booster dose for children aged 5-11 years.
Even that good news came with a caveat, however. The vote by the CDC’s Advisory Committee on Immunization Practices was 11:1 in favor, with the negative vote cast by Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., who said that “boosters are great once we’ve gotten everyone their first round. That needs to be our priority in this.”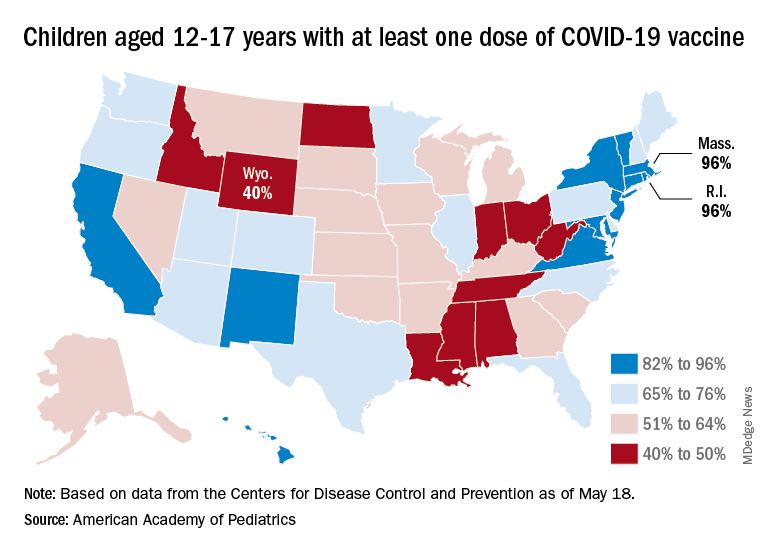
Nationally, in fact, just 35.7% of children aged 5-11 years have received at least one dose of the vaccine and only 29.0% are fully vaccinated. Those figures are nearly doubled among 12- to 17-year-olds: 69.3% have received at least one dose and 59.4% are fully vaccinated, the CDC said on its COVID Data Tracker.
Some states, meanwhile, are well below those national rates. In Wyoming, only 40% of children aged 12-17 have received an initial vaccine dose, and eight other states are below 50%. Among children aged 5-12, there are still five states below 20% in that measure, while the states on the other end of the spectrum – Vermont and Massachusetts – are above 60%, the AAP said in its separate vaccination report.



















