User login
Jury still out on mortality benefits of knee replacement in OA
People with osteoarthritis who go on to have a total or partial knee replacement do not appear to have an increased risk of all-cause mortality, but the jury is still out on whether they gain any improvement, a study showed.
In their research published in the Annals of the Rheumatic Diseases [2016 May 17. doi: 10.1136/annrheumdis-2016-209167], Dr. Devyani Misra of Boston University and colleagues noted that knee replacement (KR) was thought to decrease long-term mortality risk because of the relief from pain and improvement in function that typically comes with surgery. However, studies on the topic had been conflicting, largely because of the challenges associated with studying mortality with KR surgery in observational settings.
In the current study the research team sought to evaluate the relation of KR to the risk of all-cause mortality among subjects with knee OA, while at the same time giving particular attention to “potential sources of confounding bias that may account for [the] effect of KR on mortality.”
Using patient data from the U.K. primary care electronic database THIN, the investigators compared the risk of mortality among 14,042 subjects who had OA, were aged 50-89 years old, and had had or had not had KR.
They discovered a strong protective effect of KR on all-cause long-term mortality risk, particularly among the adults over 63 years of age.
For example, people who had undergone KR had a 28% lower risk of mortality than did non-KR subjects (hazard ratio, 0.72; 95% confidence interval, 0.66-0.78).
In the overall propensity score–matched study sample, crude mortality per 1,000 person-years (total person-years) for the KR and non-KR cohorts were 19 (61,015) and 25 (58,294), respectively.
However, despite their best efforts, the researchers said the results showed evidence of residual confounding.
“For example, the observation of improved survival immediately after KR, despite the expectation of potential short-term increased postoperative mortality risk supports the presence of residual confounding,” they wrote.
Another finding suggestive of confounding was that the protective effect was seen only in older patients (over 63) when the authors stratified study participants by age.
“While it is possible that survival benefit seen in older patients with KR is a true effect because it is in this group that greater physical activity is particularly important to survival, more likely it is a result of residual confounding because subject selection is rigorous in this age group due to vulnerability,” the authors wrote.
They concluded that knee replacement “did not appear to be associated with an increased risk of all-cause mortality.”
“While we cannot rule out that KR may potentially reduce the risk of mortality over the long term, the true extent of that potential benefit is difficult to discern due to confounding by indication in observational studies using administrative data or electronic health records,” they added.
This study was funded by the Arthritis Foundation Postdoctoral Fellowship Award, the ACR Rheumatology Research Foundation Investigator Award, and a Boston University scholarship grant.
People with osteoarthritis who go on to have a total or partial knee replacement do not appear to have an increased risk of all-cause mortality, but the jury is still out on whether they gain any improvement, a study showed.
In their research published in the Annals of the Rheumatic Diseases [2016 May 17. doi: 10.1136/annrheumdis-2016-209167], Dr. Devyani Misra of Boston University and colleagues noted that knee replacement (KR) was thought to decrease long-term mortality risk because of the relief from pain and improvement in function that typically comes with surgery. However, studies on the topic had been conflicting, largely because of the challenges associated with studying mortality with KR surgery in observational settings.
In the current study the research team sought to evaluate the relation of KR to the risk of all-cause mortality among subjects with knee OA, while at the same time giving particular attention to “potential sources of confounding bias that may account for [the] effect of KR on mortality.”
Using patient data from the U.K. primary care electronic database THIN, the investigators compared the risk of mortality among 14,042 subjects who had OA, were aged 50-89 years old, and had had or had not had KR.
They discovered a strong protective effect of KR on all-cause long-term mortality risk, particularly among the adults over 63 years of age.
For example, people who had undergone KR had a 28% lower risk of mortality than did non-KR subjects (hazard ratio, 0.72; 95% confidence interval, 0.66-0.78).
In the overall propensity score–matched study sample, crude mortality per 1,000 person-years (total person-years) for the KR and non-KR cohorts were 19 (61,015) and 25 (58,294), respectively.
However, despite their best efforts, the researchers said the results showed evidence of residual confounding.
“For example, the observation of improved survival immediately after KR, despite the expectation of potential short-term increased postoperative mortality risk supports the presence of residual confounding,” they wrote.
Another finding suggestive of confounding was that the protective effect was seen only in older patients (over 63) when the authors stratified study participants by age.
“While it is possible that survival benefit seen in older patients with KR is a true effect because it is in this group that greater physical activity is particularly important to survival, more likely it is a result of residual confounding because subject selection is rigorous in this age group due to vulnerability,” the authors wrote.
They concluded that knee replacement “did not appear to be associated with an increased risk of all-cause mortality.”
“While we cannot rule out that KR may potentially reduce the risk of mortality over the long term, the true extent of that potential benefit is difficult to discern due to confounding by indication in observational studies using administrative data or electronic health records,” they added.
This study was funded by the Arthritis Foundation Postdoctoral Fellowship Award, the ACR Rheumatology Research Foundation Investigator Award, and a Boston University scholarship grant.
People with osteoarthritis who go on to have a total or partial knee replacement do not appear to have an increased risk of all-cause mortality, but the jury is still out on whether they gain any improvement, a study showed.
In their research published in the Annals of the Rheumatic Diseases [2016 May 17. doi: 10.1136/annrheumdis-2016-209167], Dr. Devyani Misra of Boston University and colleagues noted that knee replacement (KR) was thought to decrease long-term mortality risk because of the relief from pain and improvement in function that typically comes with surgery. However, studies on the topic had been conflicting, largely because of the challenges associated with studying mortality with KR surgery in observational settings.
In the current study the research team sought to evaluate the relation of KR to the risk of all-cause mortality among subjects with knee OA, while at the same time giving particular attention to “potential sources of confounding bias that may account for [the] effect of KR on mortality.”
Using patient data from the U.K. primary care electronic database THIN, the investigators compared the risk of mortality among 14,042 subjects who had OA, were aged 50-89 years old, and had had or had not had KR.
They discovered a strong protective effect of KR on all-cause long-term mortality risk, particularly among the adults over 63 years of age.
For example, people who had undergone KR had a 28% lower risk of mortality than did non-KR subjects (hazard ratio, 0.72; 95% confidence interval, 0.66-0.78).
In the overall propensity score–matched study sample, crude mortality per 1,000 person-years (total person-years) for the KR and non-KR cohorts were 19 (61,015) and 25 (58,294), respectively.
However, despite their best efforts, the researchers said the results showed evidence of residual confounding.
“For example, the observation of improved survival immediately after KR, despite the expectation of potential short-term increased postoperative mortality risk supports the presence of residual confounding,” they wrote.
Another finding suggestive of confounding was that the protective effect was seen only in older patients (over 63) when the authors stratified study participants by age.
“While it is possible that survival benefit seen in older patients with KR is a true effect because it is in this group that greater physical activity is particularly important to survival, more likely it is a result of residual confounding because subject selection is rigorous in this age group due to vulnerability,” the authors wrote.
They concluded that knee replacement “did not appear to be associated with an increased risk of all-cause mortality.”
“While we cannot rule out that KR may potentially reduce the risk of mortality over the long term, the true extent of that potential benefit is difficult to discern due to confounding by indication in observational studies using administrative data or electronic health records,” they added.
This study was funded by the Arthritis Foundation Postdoctoral Fellowship Award, the ACR Rheumatology Research Foundation Investigator Award, and a Boston University scholarship grant.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:Knee replacement surgery in people with OA showed a protective effect on mortality, but residual confounding in the study makes it challenging to definitively conclude whether the surgery conferred a long-term mortality benefit.
Major finding: Subjects who had undergone a knee replacement had a 28% lower risk of mortality than non-KR subjects (HR, 0.72; 95% CI, 0.66-0.78).
Data source: Population-based time-varying propensity score–matched cohort of 14,042 subjects with OA aged 50-89 years with and without knee replacement.
Disclosures: This study was funded by the Arthritis Foundation Postdoctoral Fellowship Award, the ACR Rheumatology Research Foundation Investigator Award, and a Boston University scholarship grant.
Early RA remission more unstable in the presence of foot synovitis
Clinicians should consider escalating therapy in patients with early rheumatoid arthritis who have persistent foot synovitis regardless of disease activity status, Australian rheumatologists have suggested.
The advice comes after the team of doctors from several hospitals in Adelaide, South Australia, found that patients who were in remission according to disease activity (DA) standard measures but had foot synovitis were almost twice as likely to relapse, compared with patients in remission without foot synovitis.
These patients also were more likely to have worse long-term radiographic and functional outcomes, Dr. Mihir D. Wechalekar of Flinders University, Adelaide, and his colleagues reported (Arthritis Care Res. 2016. doi: 10.1002/acr.22887).
The research team assessed the disease activity in 266 patients attending the Early Arthritis Clinic at Royal Adelaide Hospital using the Disease Activity Score 28 (DAS28), clinical disease activity index (CDAI), and the simplified disease activity index (SDAI).
Patients also received yearly hand and foot radiographs and their quality of life was measured via the Medical Outcome Study Short–Form 36 (SF-36) questionnaire.
Patients were treated initially with triple-DMARD therapy and were escalated to achieve DAS28(ESR) remission by increasing methotrexate or adding a further DMARD or biologic DMARD according to a predefined treatment algorithm.
The researchers discovered that DA scores captured less than 50% of the variation in foot swollen joint count/tender joint count scores, “indicating that assessment of disease activity using these criteria is likely to be insufficient for detecting disease flares in the feet.”
Furthermore, the authors noted that despite the SDAI and CDAI being considered “more stringent” remission criteria, 24% of patients in SDAI remission and 25% of patients in CDAI remission had ongoing foot synovitis.
The sustainability of remission influenced the progression of erosion scores (P = .006); foot synovitis was linked to worse SF-36 physical functioning (P = 0.025).
“Our findings emphasize the importance of examining the ankle and foot as a part of the routine management of patients with RA,” the research team concluded.
“Given the impact of foot synovitis on stability of remission, radiological progression, and independent impact on quality of life, decisions should not be made solely on the basis of DA scores that omit foot joints,” they wrote.
“Presence of foot synovitis despite apparent remission should prompt escalation of therapy to prevent long-term joint damage and improve functional outcomes,” they added.
Clinicians should consider escalating therapy in patients with early rheumatoid arthritis who have persistent foot synovitis regardless of disease activity status, Australian rheumatologists have suggested.
The advice comes after the team of doctors from several hospitals in Adelaide, South Australia, found that patients who were in remission according to disease activity (DA) standard measures but had foot synovitis were almost twice as likely to relapse, compared with patients in remission without foot synovitis.
These patients also were more likely to have worse long-term radiographic and functional outcomes, Dr. Mihir D. Wechalekar of Flinders University, Adelaide, and his colleagues reported (Arthritis Care Res. 2016. doi: 10.1002/acr.22887).
The research team assessed the disease activity in 266 patients attending the Early Arthritis Clinic at Royal Adelaide Hospital using the Disease Activity Score 28 (DAS28), clinical disease activity index (CDAI), and the simplified disease activity index (SDAI).
Patients also received yearly hand and foot radiographs and their quality of life was measured via the Medical Outcome Study Short–Form 36 (SF-36) questionnaire.
Patients were treated initially with triple-DMARD therapy and were escalated to achieve DAS28(ESR) remission by increasing methotrexate or adding a further DMARD or biologic DMARD according to a predefined treatment algorithm.
The researchers discovered that DA scores captured less than 50% of the variation in foot swollen joint count/tender joint count scores, “indicating that assessment of disease activity using these criteria is likely to be insufficient for detecting disease flares in the feet.”
Furthermore, the authors noted that despite the SDAI and CDAI being considered “more stringent” remission criteria, 24% of patients in SDAI remission and 25% of patients in CDAI remission had ongoing foot synovitis.
The sustainability of remission influenced the progression of erosion scores (P = .006); foot synovitis was linked to worse SF-36 physical functioning (P = 0.025).
“Our findings emphasize the importance of examining the ankle and foot as a part of the routine management of patients with RA,” the research team concluded.
“Given the impact of foot synovitis on stability of remission, radiological progression, and independent impact on quality of life, decisions should not be made solely on the basis of DA scores that omit foot joints,” they wrote.
“Presence of foot synovitis despite apparent remission should prompt escalation of therapy to prevent long-term joint damage and improve functional outcomes,” they added.
Clinicians should consider escalating therapy in patients with early rheumatoid arthritis who have persistent foot synovitis regardless of disease activity status, Australian rheumatologists have suggested.
The advice comes after the team of doctors from several hospitals in Adelaide, South Australia, found that patients who were in remission according to disease activity (DA) standard measures but had foot synovitis were almost twice as likely to relapse, compared with patients in remission without foot synovitis.
These patients also were more likely to have worse long-term radiographic and functional outcomes, Dr. Mihir D. Wechalekar of Flinders University, Adelaide, and his colleagues reported (Arthritis Care Res. 2016. doi: 10.1002/acr.22887).
The research team assessed the disease activity in 266 patients attending the Early Arthritis Clinic at Royal Adelaide Hospital using the Disease Activity Score 28 (DAS28), clinical disease activity index (CDAI), and the simplified disease activity index (SDAI).
Patients also received yearly hand and foot radiographs and their quality of life was measured via the Medical Outcome Study Short–Form 36 (SF-36) questionnaire.
Patients were treated initially with triple-DMARD therapy and were escalated to achieve DAS28(ESR) remission by increasing methotrexate or adding a further DMARD or biologic DMARD according to a predefined treatment algorithm.
The researchers discovered that DA scores captured less than 50% of the variation in foot swollen joint count/tender joint count scores, “indicating that assessment of disease activity using these criteria is likely to be insufficient for detecting disease flares in the feet.”
Furthermore, the authors noted that despite the SDAI and CDAI being considered “more stringent” remission criteria, 24% of patients in SDAI remission and 25% of patients in CDAI remission had ongoing foot synovitis.
The sustainability of remission influenced the progression of erosion scores (P = .006); foot synovitis was linked to worse SF-36 physical functioning (P = 0.025).
“Our findings emphasize the importance of examining the ankle and foot as a part of the routine management of patients with RA,” the research team concluded.
“Given the impact of foot synovitis on stability of remission, radiological progression, and independent impact on quality of life, decisions should not be made solely on the basis of DA scores that omit foot joints,” they wrote.
“Presence of foot synovitis despite apparent remission should prompt escalation of therapy to prevent long-term joint damage and improve functional outcomes,” they added.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: The presence of foot synovitis despite apparent remission should prompt escalation of therapy to prevent long-term joint damage and improve functional outcomes.
Major finding: Patients who were in remission according to DA standard measures but had foot synovitis were almost twice as likely to relapse, compared with patients in remission without foot synovitis.
Data source: A study of 266 consecutive patients with early RA attending the Early Arthritis Clinic at Royal Adelaide Hospital.
Disclosures: The study was funded through a National Health and Medical Research Council of Australia postgraduate scholarship.
New gout drug under investigation has dual benefit
The novel uricosuric drug arhalofenate significantly reduced the incidence of gout flares, compared with allopurinol alone and placebo, and also modestly lowered serum urate levels in a phase IIb trial.
However, arhalofenate alone did not lower serum uric acid levels as much as did allopurinol plus colchicine, potentially making it “better suited for a combination regimen with a xanthine-oxidase inhibitor,” first author Dr. Jeffrey Poiley of Arthritis Associates in Orlando, and his coauthors at CymaBay Therapeutics in Newark, Calif.
The double-blind, randomized, placebo- and active-drug controlled trial of 239 gout patients showed that arhalofenate at a dose of 800 mg daily significantly reduced gout flares over 12 weeks by 46% versus allopurinol at a dose of 300 mg daily (0.66 flares vs. 1.24; P = .0056) and by 41% versus placebo (0.66 vs. 1.13; P = .049).
The 12-week incidence of flares with the 800-mg dose was no better than the combination of allopurinol 300 mg with 0.6 mg colchicine a day (0.40), but the study was not powered to detect this comparison. “The clinical utility of arhalofenate 800 mg will have to be judged in the context of the respective risk/benefit ratio of each flare treatment,” the study authors said (Arthritis Rheumatol. 2016 Mar 18. doi: 101002/art.39684).
The flare rate for arhalofenate at a lower daily dose of 600 mg was not significantly different from allopurinol 300 mg without flare prophylaxis (1.04 vs. 1.24, respectively).
Secondary outcomes of the study revealed that arhalofenate had modest effects on serum urate levels, compared with allopurinol on its own and in combination with colchicine. The average percentage change in serum uric acid levels from baseline to week 12 were –12.5% with 600 mg of arhalofenate; –16.5% with 800 mg; –28.8% with allopurinol 300 mg, and –24.9% for allopurinol plus colchicine, and –0.9% with placebo.
Arhalofenate lowers serum urate by blocking its reabsorption by the proximal tubules of the kidney via inhibition of the urate transporter 1. In animal studies of urate crystal–induced inflammation, arhalofenate suppressed the release of proinflammatory cytokines and prevented the movement of neutrophils to the site of inflammation. Prior studies of arhalofenate in gout patients treated with colchicine suggested that the drug could prevent flares, but this was impossible to prove definitively because of the simultaneous use of colchicine, the authors wrote.
The study authors will now confirm their findings in a phase III trial with a treatment regimen that combines arhalofenate with febuxostat.
Patients involved in the study had more than three flares in the previous year, had discontinued urate-lowering therapy and colchicine, and had a serum urate level of 7.5-12 mg/dL.
They were randomized in a 2:2:2:2:1 fashion to one of five treatment groups: daily arhalofenate 600 mg or 800 mg, allopurinol 300 mg, allopurinol 300 mg together with 0.6 mg of colchicine, or placebo.
The researchers said there were no meaningful differences in adverse events between treatment groups. There were no significant changes in estimated creatinine clearance in any treatment group, including no declines in any group receiving arhalofenate.
The study was sponsored by CymaBay Therapeutics. Dr. Poiley was an investigator in the study, and five other authors are employees of CymaBay.
 |
Dr. Tuhina Neogi |
Arhalofenate provided a reduction in gout attack risk and serum urate level that appears to be clinically meaningful, particularly for patients who cannot use colchicine or nonsteroidal anti-inflammatory drugs for flare prophylaxis. It could potentially be the first in a new urate-lowering, antiflare therapy (ULAFT) class of drug.
However, the trial used of lower-than-recommended doses of the comparator drug allopurinol. If the allopurinol dose had been up-titrated from 300 mg to 400 mg per day, an even greater proportion of patients in this arm would have likely reached the serum urate target of less than 6 mg/dL.
Starting the patients at 100 mg allopurinol before titrating upward as current recommendations advise, instead of initiating treatment at 300 mg without flare prophylaxis, could have lowered the flare rate.
 |
Dr. Hyon K. Choi |
It would also have been useful to see the effect of the drug in patients with renal impairment (subjects with a creatinine clearance less than 60 mL/min were excluded from the study), as well as explore further the potential metabolic effects first seen when the agent was first investigated as an insulin sensitizer.
Dr. Tuhina Neogi is with the department of medicine at Boston University, and Dr. Hyon Choi is a professor of medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. Their comments are derived from an editorial accompanying Dr. Poiley and his colleagues’ report (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39687). No conflicts of interest were disclosed.
 |
Dr. Tuhina Neogi |
Arhalofenate provided a reduction in gout attack risk and serum urate level that appears to be clinically meaningful, particularly for patients who cannot use colchicine or nonsteroidal anti-inflammatory drugs for flare prophylaxis. It could potentially be the first in a new urate-lowering, antiflare therapy (ULAFT) class of drug.
However, the trial used of lower-than-recommended doses of the comparator drug allopurinol. If the allopurinol dose had been up-titrated from 300 mg to 400 mg per day, an even greater proportion of patients in this arm would have likely reached the serum urate target of less than 6 mg/dL.
Starting the patients at 100 mg allopurinol before titrating upward as current recommendations advise, instead of initiating treatment at 300 mg without flare prophylaxis, could have lowered the flare rate.
 |
Dr. Hyon K. Choi |
It would also have been useful to see the effect of the drug in patients with renal impairment (subjects with a creatinine clearance less than 60 mL/min were excluded from the study), as well as explore further the potential metabolic effects first seen when the agent was first investigated as an insulin sensitizer.
Dr. Tuhina Neogi is with the department of medicine at Boston University, and Dr. Hyon Choi is a professor of medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. Their comments are derived from an editorial accompanying Dr. Poiley and his colleagues’ report (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39687). No conflicts of interest were disclosed.
 |
Dr. Tuhina Neogi |
Arhalofenate provided a reduction in gout attack risk and serum urate level that appears to be clinically meaningful, particularly for patients who cannot use colchicine or nonsteroidal anti-inflammatory drugs for flare prophylaxis. It could potentially be the first in a new urate-lowering, antiflare therapy (ULAFT) class of drug.
However, the trial used of lower-than-recommended doses of the comparator drug allopurinol. If the allopurinol dose had been up-titrated from 300 mg to 400 mg per day, an even greater proportion of patients in this arm would have likely reached the serum urate target of less than 6 mg/dL.
Starting the patients at 100 mg allopurinol before titrating upward as current recommendations advise, instead of initiating treatment at 300 mg without flare prophylaxis, could have lowered the flare rate.
 |
Dr. Hyon K. Choi |
It would also have been useful to see the effect of the drug in patients with renal impairment (subjects with a creatinine clearance less than 60 mL/min were excluded from the study), as well as explore further the potential metabolic effects first seen when the agent was first investigated as an insulin sensitizer.
Dr. Tuhina Neogi is with the department of medicine at Boston University, and Dr. Hyon Choi is a professor of medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. Their comments are derived from an editorial accompanying Dr. Poiley and his colleagues’ report (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39687). No conflicts of interest were disclosed.
The novel uricosuric drug arhalofenate significantly reduced the incidence of gout flares, compared with allopurinol alone and placebo, and also modestly lowered serum urate levels in a phase IIb trial.
However, arhalofenate alone did not lower serum uric acid levels as much as did allopurinol plus colchicine, potentially making it “better suited for a combination regimen with a xanthine-oxidase inhibitor,” first author Dr. Jeffrey Poiley of Arthritis Associates in Orlando, and his coauthors at CymaBay Therapeutics in Newark, Calif.
The double-blind, randomized, placebo- and active-drug controlled trial of 239 gout patients showed that arhalofenate at a dose of 800 mg daily significantly reduced gout flares over 12 weeks by 46% versus allopurinol at a dose of 300 mg daily (0.66 flares vs. 1.24; P = .0056) and by 41% versus placebo (0.66 vs. 1.13; P = .049).
The 12-week incidence of flares with the 800-mg dose was no better than the combination of allopurinol 300 mg with 0.6 mg colchicine a day (0.40), but the study was not powered to detect this comparison. “The clinical utility of arhalofenate 800 mg will have to be judged in the context of the respective risk/benefit ratio of each flare treatment,” the study authors said (Arthritis Rheumatol. 2016 Mar 18. doi: 101002/art.39684).
The flare rate for arhalofenate at a lower daily dose of 600 mg was not significantly different from allopurinol 300 mg without flare prophylaxis (1.04 vs. 1.24, respectively).
Secondary outcomes of the study revealed that arhalofenate had modest effects on serum urate levels, compared with allopurinol on its own and in combination with colchicine. The average percentage change in serum uric acid levels from baseline to week 12 were –12.5% with 600 mg of arhalofenate; –16.5% with 800 mg; –28.8% with allopurinol 300 mg, and –24.9% for allopurinol plus colchicine, and –0.9% with placebo.
Arhalofenate lowers serum urate by blocking its reabsorption by the proximal tubules of the kidney via inhibition of the urate transporter 1. In animal studies of urate crystal–induced inflammation, arhalofenate suppressed the release of proinflammatory cytokines and prevented the movement of neutrophils to the site of inflammation. Prior studies of arhalofenate in gout patients treated with colchicine suggested that the drug could prevent flares, but this was impossible to prove definitively because of the simultaneous use of colchicine, the authors wrote.
The study authors will now confirm their findings in a phase III trial with a treatment regimen that combines arhalofenate with febuxostat.
Patients involved in the study had more than three flares in the previous year, had discontinued urate-lowering therapy and colchicine, and had a serum urate level of 7.5-12 mg/dL.
They were randomized in a 2:2:2:2:1 fashion to one of five treatment groups: daily arhalofenate 600 mg or 800 mg, allopurinol 300 mg, allopurinol 300 mg together with 0.6 mg of colchicine, or placebo.
The researchers said there were no meaningful differences in adverse events between treatment groups. There were no significant changes in estimated creatinine clearance in any treatment group, including no declines in any group receiving arhalofenate.
The study was sponsored by CymaBay Therapeutics. Dr. Poiley was an investigator in the study, and five other authors are employees of CymaBay.
The novel uricosuric drug arhalofenate significantly reduced the incidence of gout flares, compared with allopurinol alone and placebo, and also modestly lowered serum urate levels in a phase IIb trial.
However, arhalofenate alone did not lower serum uric acid levels as much as did allopurinol plus colchicine, potentially making it “better suited for a combination regimen with a xanthine-oxidase inhibitor,” first author Dr. Jeffrey Poiley of Arthritis Associates in Orlando, and his coauthors at CymaBay Therapeutics in Newark, Calif.
The double-blind, randomized, placebo- and active-drug controlled trial of 239 gout patients showed that arhalofenate at a dose of 800 mg daily significantly reduced gout flares over 12 weeks by 46% versus allopurinol at a dose of 300 mg daily (0.66 flares vs. 1.24; P = .0056) and by 41% versus placebo (0.66 vs. 1.13; P = .049).
The 12-week incidence of flares with the 800-mg dose was no better than the combination of allopurinol 300 mg with 0.6 mg colchicine a day (0.40), but the study was not powered to detect this comparison. “The clinical utility of arhalofenate 800 mg will have to be judged in the context of the respective risk/benefit ratio of each flare treatment,” the study authors said (Arthritis Rheumatol. 2016 Mar 18. doi: 101002/art.39684).
The flare rate for arhalofenate at a lower daily dose of 600 mg was not significantly different from allopurinol 300 mg without flare prophylaxis (1.04 vs. 1.24, respectively).
Secondary outcomes of the study revealed that arhalofenate had modest effects on serum urate levels, compared with allopurinol on its own and in combination with colchicine. The average percentage change in serum uric acid levels from baseline to week 12 were –12.5% with 600 mg of arhalofenate; –16.5% with 800 mg; –28.8% with allopurinol 300 mg, and –24.9% for allopurinol plus colchicine, and –0.9% with placebo.
Arhalofenate lowers serum urate by blocking its reabsorption by the proximal tubules of the kidney via inhibition of the urate transporter 1. In animal studies of urate crystal–induced inflammation, arhalofenate suppressed the release of proinflammatory cytokines and prevented the movement of neutrophils to the site of inflammation. Prior studies of arhalofenate in gout patients treated with colchicine suggested that the drug could prevent flares, but this was impossible to prove definitively because of the simultaneous use of colchicine, the authors wrote.
The study authors will now confirm their findings in a phase III trial with a treatment regimen that combines arhalofenate with febuxostat.
Patients involved in the study had more than three flares in the previous year, had discontinued urate-lowering therapy and colchicine, and had a serum urate level of 7.5-12 mg/dL.
They were randomized in a 2:2:2:2:1 fashion to one of five treatment groups: daily arhalofenate 600 mg or 800 mg, allopurinol 300 mg, allopurinol 300 mg together with 0.6 mg of colchicine, or placebo.
The researchers said there were no meaningful differences in adverse events between treatment groups. There were no significant changes in estimated creatinine clearance in any treatment group, including no declines in any group receiving arhalofenate.
The study was sponsored by CymaBay Therapeutics. Dr. Poiley was an investigator in the study, and five other authors are employees of CymaBay.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: The investigational uricosuric drug arhalofenate significantly reduced the incidence of flares in gout patients and also modestly reduced serum uric acid.Major finding: Arhalofenate at an 800-mg daily dose significantly reduced gout flares over 12 weeks by 46% versus allopurinol at a dose of 300 mg daily (0.66 flares vs. 1.24; P = .0056).
Data source: A 12-week, phase IIb, double-blind, randomized, placebo- and active-drug controlled trial involving 239 gout patients.
Disclosures: The study was sponsored by CymaBay Therapeutics. Dr. Poiley was an investigator in the study, and five other authors are employees of CymaBay.
Genetics, smoking, and inflammation on MRI predict progression in axial SpA
Progression to structural damage occurs slowly among patients with early axial spondyloarthritis and more often takes place in current smokers, HLAB27 carriers, and those with signs of inflammation on MRI, according to new observations from the French DESIR cohort study.
The findings help to establish risk factors for early progression of nonradiographic axial spondyloarthritis (nr-axSpA) to radiographic disease, said Dr. Maxime Dougados of the department of rheumatology at Cochin Hospital, Paris, and his colleagues (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39666).
The study involved 449 patients with recent-onset inflammatory back pain who were participating in the multicenter, longitudinal DESIR study and had x-rays available at baseline and 2-year follow-up.
A total of 16 (4.9%) out of 326 patients who did not fulfill the modified New York criteria (mNY) at baseline progressed from nonradiographic to radiographic axSpA over the 2-year study period.
Of the 123 patients who met the mNY criteria at baseline, 7 (5.7%) no longer met the criteria at follow-up.
Independent factors found to influence the odds of progressing to radiographic axSpA were smoking status (odds ratio, 3.3; 95% confidence interval, 1.0-11.5), HLAB27 positivity (OR, 12.6; 95% CI, 2.3-274), and the presence of inflammation at MRI in the sacroiliac joints (SIJs) at baseline (OR, 48.8; 95% CI, 9.3-904), a multivariate analysis showed.
However, when the authors defined radiographic progression as “a worsening of at least one grade in at least one SIJ,” HLAB27 positivity (OR, 1.68; 95% CI, 0.8-3.71, P = .02), MRI positivity (OR, 5.85; 95% CI, 2.38-15.37, P less than .001), and baseline structural damage at SIJs on pelvic x-rays (OR, 6.35; 95% CI, 2.14-18.88; P less than .001) were predictors of radiographic disease progression. Another analysis confirmed those as risk factors even when the definition of progression also required a final absolute grade of at least 2 in the worsened SIJs.
When the authors considered the change in total score (based on the mean of two readers), only HLAB27 positivity and baseline MRI positivity were highlighted as independent predictors of disease progression. In this analysis, HLAB27 positivity and inflammation on MRI had grading score increases of 0.41 (P = .014) and 1.03 (P less than .001), respectively.
Unlike other studies, the researchers did not see a clear relationship between abnormal C-reactive protein at baseline and radiographic progression.
The findings suggest that, in early SpA, “structural progression does exist but is quite small and observed in a small number of patients,” the study authors wrote.
The authors noted that their findings should be “interpreted with caution” because they were based on a small number of patients, and additional studies with a longer-follow-up period are needed to confirm the findings.
The DESIR cohort was sponsored by the Department de la recherché Clinique et du Development de l’Assistance Publique-Hopitaux de Paris. An unrestricted grant from Pfizer was allocated for the 10 years of follow-up.
Progression to structural damage occurs slowly among patients with early axial spondyloarthritis and more often takes place in current smokers, HLAB27 carriers, and those with signs of inflammation on MRI, according to new observations from the French DESIR cohort study.
The findings help to establish risk factors for early progression of nonradiographic axial spondyloarthritis (nr-axSpA) to radiographic disease, said Dr. Maxime Dougados of the department of rheumatology at Cochin Hospital, Paris, and his colleagues (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39666).
The study involved 449 patients with recent-onset inflammatory back pain who were participating in the multicenter, longitudinal DESIR study and had x-rays available at baseline and 2-year follow-up.
A total of 16 (4.9%) out of 326 patients who did not fulfill the modified New York criteria (mNY) at baseline progressed from nonradiographic to radiographic axSpA over the 2-year study period.
Of the 123 patients who met the mNY criteria at baseline, 7 (5.7%) no longer met the criteria at follow-up.
Independent factors found to influence the odds of progressing to radiographic axSpA were smoking status (odds ratio, 3.3; 95% confidence interval, 1.0-11.5), HLAB27 positivity (OR, 12.6; 95% CI, 2.3-274), and the presence of inflammation at MRI in the sacroiliac joints (SIJs) at baseline (OR, 48.8; 95% CI, 9.3-904), a multivariate analysis showed.
However, when the authors defined radiographic progression as “a worsening of at least one grade in at least one SIJ,” HLAB27 positivity (OR, 1.68; 95% CI, 0.8-3.71, P = .02), MRI positivity (OR, 5.85; 95% CI, 2.38-15.37, P less than .001), and baseline structural damage at SIJs on pelvic x-rays (OR, 6.35; 95% CI, 2.14-18.88; P less than .001) were predictors of radiographic disease progression. Another analysis confirmed those as risk factors even when the definition of progression also required a final absolute grade of at least 2 in the worsened SIJs.
When the authors considered the change in total score (based on the mean of two readers), only HLAB27 positivity and baseline MRI positivity were highlighted as independent predictors of disease progression. In this analysis, HLAB27 positivity and inflammation on MRI had grading score increases of 0.41 (P = .014) and 1.03 (P less than .001), respectively.
Unlike other studies, the researchers did not see a clear relationship between abnormal C-reactive protein at baseline and radiographic progression.
The findings suggest that, in early SpA, “structural progression does exist but is quite small and observed in a small number of patients,” the study authors wrote.
The authors noted that their findings should be “interpreted with caution” because they were based on a small number of patients, and additional studies with a longer-follow-up period are needed to confirm the findings.
The DESIR cohort was sponsored by the Department de la recherché Clinique et du Development de l’Assistance Publique-Hopitaux de Paris. An unrestricted grant from Pfizer was allocated for the 10 years of follow-up.
Progression to structural damage occurs slowly among patients with early axial spondyloarthritis and more often takes place in current smokers, HLAB27 carriers, and those with signs of inflammation on MRI, according to new observations from the French DESIR cohort study.
The findings help to establish risk factors for early progression of nonradiographic axial spondyloarthritis (nr-axSpA) to radiographic disease, said Dr. Maxime Dougados of the department of rheumatology at Cochin Hospital, Paris, and his colleagues (Arthritis Rheumatol. 2016 Mar 18. doi: 10.1002/art.39666).
The study involved 449 patients with recent-onset inflammatory back pain who were participating in the multicenter, longitudinal DESIR study and had x-rays available at baseline and 2-year follow-up.
A total of 16 (4.9%) out of 326 patients who did not fulfill the modified New York criteria (mNY) at baseline progressed from nonradiographic to radiographic axSpA over the 2-year study period.
Of the 123 patients who met the mNY criteria at baseline, 7 (5.7%) no longer met the criteria at follow-up.
Independent factors found to influence the odds of progressing to radiographic axSpA were smoking status (odds ratio, 3.3; 95% confidence interval, 1.0-11.5), HLAB27 positivity (OR, 12.6; 95% CI, 2.3-274), and the presence of inflammation at MRI in the sacroiliac joints (SIJs) at baseline (OR, 48.8; 95% CI, 9.3-904), a multivariate analysis showed.
However, when the authors defined radiographic progression as “a worsening of at least one grade in at least one SIJ,” HLAB27 positivity (OR, 1.68; 95% CI, 0.8-3.71, P = .02), MRI positivity (OR, 5.85; 95% CI, 2.38-15.37, P less than .001), and baseline structural damage at SIJs on pelvic x-rays (OR, 6.35; 95% CI, 2.14-18.88; P less than .001) were predictors of radiographic disease progression. Another analysis confirmed those as risk factors even when the definition of progression also required a final absolute grade of at least 2 in the worsened SIJs.
When the authors considered the change in total score (based on the mean of two readers), only HLAB27 positivity and baseline MRI positivity were highlighted as independent predictors of disease progression. In this analysis, HLAB27 positivity and inflammation on MRI had grading score increases of 0.41 (P = .014) and 1.03 (P less than .001), respectively.
Unlike other studies, the researchers did not see a clear relationship between abnormal C-reactive protein at baseline and radiographic progression.
The findings suggest that, in early SpA, “structural progression does exist but is quite small and observed in a small number of patients,” the study authors wrote.
The authors noted that their findings should be “interpreted with caution” because they were based on a small number of patients, and additional studies with a longer-follow-up period are needed to confirm the findings.
The DESIR cohort was sponsored by the Department de la recherché Clinique et du Development de l’Assistance Publique-Hopitaux de Paris. An unrestricted grant from Pfizer was allocated for the 10 years of follow-up.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: The switch from nonradiographic to radiographic axSpA, made by about 5% of patients over the 2-year study period, was influenced by HLAB27 positivity, smoking status, and inflammatory sacroiliac joint lesions on MRI.
Major finding: Multivariate analysis showed smoking status (OR, 3.3; 95% CI, 1.0-11.5), HLAB27 positivity (OR, 12.6; 95% CI, 2.3-274), and the presence of inflammation at MRI in the sacroiliac joints (SIJ) at baseline (OR, 48.8; 95% CI, 9.3-904) predicted progression.
Data source: An analysis of 2-year data from 449 patients with recent-onset inflammatory back pain participating in the multicenter, longitudinal DESIR study.
Disclosures: The DESIR cohort was sponsored by the Department de la recherché Clinique et du Development de l’Assistance Publique-Hopitaux de Paris. An unrestricted grant from Pfizer was allocated for the 10 years of follow-up.
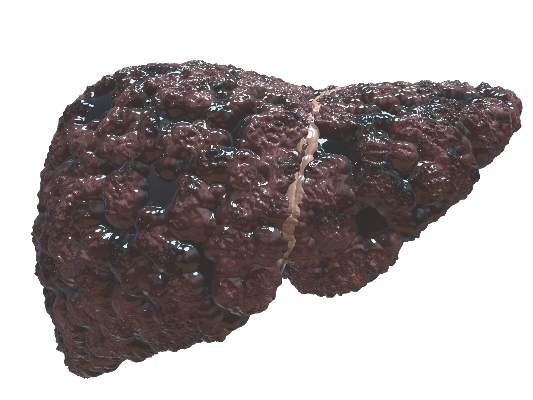
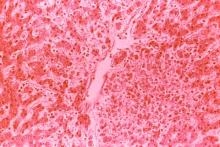
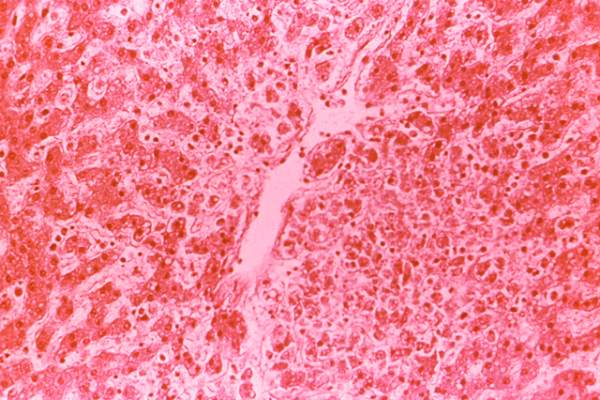
Gut microbiota plays undefined role in liver disease
The development and progression of fatty liver, and alcoholic and nonalcoholic diseases appear to be influenced by gut microbiota but it is too early to say whether microbial therapy could be used to treat patients, experts have concluded in a review of the literature.
In a study published in Gastroenterology (2016. doi: 10.1053/j.gastro.2016.02.073), Ph.D. student Naga S. Betrapally and Patrick M. Gillevet, Ph.D., of the microbiome analysis center at George Mason University in Fairfax, Va., together with colleague Dr. Jasmohan S. Bajaj of the Virginia Commonwealth University in Richmond looked at whether changes in the intestinal microbiome and alcoholic and nonalcoholic liver diseases were causes of the disease or effects.
Researchers had found that intestinal microbiota affected precirrhotic and cirrhotic stages of liver disease, the review authors said.
For example, one way in which gut microbiota might influence the severity of nonalcoholic fatty liver disease (NAFLD) was by “increasing production of ethanol, activating TLR [toll-like receptor] signaling and TNF [tumor necrosis factor] production in the liver, or altering the bile acid profile,” they said.
Researchers had also found that changes to intestinal microbiota could have an impact on the development of nonalcoholic steatohepatitis by affecting processes like digestion, immune response, and the production of gut hormones.
Microbial therapies such as antibiotics, synbiotics, probiotics, and prebiotics could be developed to treat patients with NAFLD and alcoholic liver disease (ALD), they noted.
For instance, short-term use of Bifidobacterium bifidum and Lactobacillus plantarum 8PA3 in alcoholic patients was shown to lower plasma levels of alanine aminotransferase and aspartate aminotransferase, restore intestinal microbiota, and reduce alcohol-related liver injuries.
However, they cautioned that NAFLD and ALD were “multiorgan diseases that also involve metabolic syndrome and the widespread effects of alcohol.”
Furthermore, the composition of the intestinal microbiome varies widely among individuals and different ethnic groups, and “its effects on the development of liver disease involve additional environmental, dietary, genetic, social, and behavioral factors,” they said.
“Although substantial progress has been made in increasing our understanding of the gut microbiota in patients with alcoholic and nonalcoholic steatohepatitis, many important questions remain,” they concluded.
“Large multicenter studies of many patients, over long time periods, are needed to determine how the microbiota might cause liver disease and how liver disease alters the microbiota,” they added.
The development and progression of fatty liver, and alcoholic and nonalcoholic diseases appear to be influenced by gut microbiota but it is too early to say whether microbial therapy could be used to treat patients, experts have concluded in a review of the literature.
In a study published in Gastroenterology (2016. doi: 10.1053/j.gastro.2016.02.073), Ph.D. student Naga S. Betrapally and Patrick M. Gillevet, Ph.D., of the microbiome analysis center at George Mason University in Fairfax, Va., together with colleague Dr. Jasmohan S. Bajaj of the Virginia Commonwealth University in Richmond looked at whether changes in the intestinal microbiome and alcoholic and nonalcoholic liver diseases were causes of the disease or effects.
Researchers had found that intestinal microbiota affected precirrhotic and cirrhotic stages of liver disease, the review authors said.
For example, one way in which gut microbiota might influence the severity of nonalcoholic fatty liver disease (NAFLD) was by “increasing production of ethanol, activating TLR [toll-like receptor] signaling and TNF [tumor necrosis factor] production in the liver, or altering the bile acid profile,” they said.
Researchers had also found that changes to intestinal microbiota could have an impact on the development of nonalcoholic steatohepatitis by affecting processes like digestion, immune response, and the production of gut hormones.
Microbial therapies such as antibiotics, synbiotics, probiotics, and prebiotics could be developed to treat patients with NAFLD and alcoholic liver disease (ALD), they noted.
For instance, short-term use of Bifidobacterium bifidum and Lactobacillus plantarum 8PA3 in alcoholic patients was shown to lower plasma levels of alanine aminotransferase and aspartate aminotransferase, restore intestinal microbiota, and reduce alcohol-related liver injuries.
However, they cautioned that NAFLD and ALD were “multiorgan diseases that also involve metabolic syndrome and the widespread effects of alcohol.”
Furthermore, the composition of the intestinal microbiome varies widely among individuals and different ethnic groups, and “its effects on the development of liver disease involve additional environmental, dietary, genetic, social, and behavioral factors,” they said.
“Although substantial progress has been made in increasing our understanding of the gut microbiota in patients with alcoholic and nonalcoholic steatohepatitis, many important questions remain,” they concluded.
“Large multicenter studies of many patients, over long time periods, are needed to determine how the microbiota might cause liver disease and how liver disease alters the microbiota,” they added.
The development and progression of fatty liver, and alcoholic and nonalcoholic diseases appear to be influenced by gut microbiota but it is too early to say whether microbial therapy could be used to treat patients, experts have concluded in a review of the literature.
In a study published in Gastroenterology (2016. doi: 10.1053/j.gastro.2016.02.073), Ph.D. student Naga S. Betrapally and Patrick M. Gillevet, Ph.D., of the microbiome analysis center at George Mason University in Fairfax, Va., together with colleague Dr. Jasmohan S. Bajaj of the Virginia Commonwealth University in Richmond looked at whether changes in the intestinal microbiome and alcoholic and nonalcoholic liver diseases were causes of the disease or effects.
Researchers had found that intestinal microbiota affected precirrhotic and cirrhotic stages of liver disease, the review authors said.
For example, one way in which gut microbiota might influence the severity of nonalcoholic fatty liver disease (NAFLD) was by “increasing production of ethanol, activating TLR [toll-like receptor] signaling and TNF [tumor necrosis factor] production in the liver, or altering the bile acid profile,” they said.
Researchers had also found that changes to intestinal microbiota could have an impact on the development of nonalcoholic steatohepatitis by affecting processes like digestion, immune response, and the production of gut hormones.
Microbial therapies such as antibiotics, synbiotics, probiotics, and prebiotics could be developed to treat patients with NAFLD and alcoholic liver disease (ALD), they noted.
For instance, short-term use of Bifidobacterium bifidum and Lactobacillus plantarum 8PA3 in alcoholic patients was shown to lower plasma levels of alanine aminotransferase and aspartate aminotransferase, restore intestinal microbiota, and reduce alcohol-related liver injuries.
However, they cautioned that NAFLD and ALD were “multiorgan diseases that also involve metabolic syndrome and the widespread effects of alcohol.”
Furthermore, the composition of the intestinal microbiome varies widely among individuals and different ethnic groups, and “its effects on the development of liver disease involve additional environmental, dietary, genetic, social, and behavioral factors,” they said.
“Although substantial progress has been made in increasing our understanding of the gut microbiota in patients with alcoholic and nonalcoholic steatohepatitis, many important questions remain,” they concluded.
“Large multicenter studies of many patients, over long time periods, are needed to determine how the microbiota might cause liver disease and how liver disease alters the microbiota,” they added.
FROM GASTROENTEROLOGY
Key clinical point: Although substantial progress has been made in the understanding of the gut microbiota in patients with alcoholic and nonalcoholic steatohepatitis many important questions remain.
Major finding: Large multicenter studies involving many patients over long time periods are needed to determine how the microbiota might cause liver disease and how liver disease alters the microbiota.
Data source: A review of the literature on the differences and similarities in the cirrhotic and precirrhotic stages of NAFLD and ALD and the role of intestinal microbiota.
Disclosures: No conflicts of interest were declared.
Terlipressin does not reverse hepatorenal syndrome but improves survival
Treating patients with hepatorenal syndrome type 1 (HRS-1) with the synthetic vasopressin analogue terlipressin (Lucassin) and albumin does not improve the chances of reversal of hepatorenal syndrome compared with albumin alone, but could improve survival, the results of a multicenter, randomized, double-blind, placebo-controlled trial suggest.
Reporting the latest findings from the REVERSE trial, Dr. Thomas D. Boyer of the Liver Research Institute at the University of Arizona, Tucson, and colleagues said previous studies, including one by their team, had shown that terlipressin together with albumin was more effective at reversing hepatorenal syndrome type 1 (HRS-1) and improving serum creatinine compared with placebo.
However, they noted that while terlipressin was approved for treating HRS-1 in several countries, it was not approved in the United States or Canada. European guidelines also recommended terlipressin plus albumin as a first-line treatment in these patients.
In the current phase III, randomized double-blind, placebo-controlled trial, 196 patients with cirrhosis, ascites, and HRS-1 were enrolled from 50 centers in the United States and two centers in Canada (Gastroenterology 2016. doi: 10.1053/j.gastro.2016.02.026). Study participants were randomly assigned to terlipressin 1 mg (n = 97) or placebo (n = 99) with albumin every 6 hours.
Treatment continued for 14 days unless the patient had met the study primary endpoint of a confirmed HRS reversal defined by the authors as two serum creatinine levels less than 1.5 mg/dL at least 40 hours apart on treatment without renal replacement therapy or transplant, or serum creatinine (sCr) levels at or above baseline on day 4.
Results showed that confirmed HRS reversal occurred in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%) (P = .22), a difference that was not statistically significant.
The secondary outcome of reversal of HRS-1 (defined as at least 1 sCr value less than or equal to 1.5 mg/dL while on treatment) was reached by 23 patients on terlipressin and 15 patients on albumin alone (23.7 vs. 15.2%, P = .13), a finding that again was not statistically significant.
However, the research team observed significant improvements in serum creatinine in the patients treated with terlipressin that correlated with survival. For example, sCr decreased by 1.1 mg/dL in patients receiving terlipressin compared to 0.6 mg/dL in patients receiving placebo.
“While all patients with [confirmed HRS reversal] had a more than 20% decrease in sCr from baseline, the majority with a greater than 20% decrease in sCr did not achieve [confirmed HRS reversal] and yet appeared to have an improved survival compared with patients with less than or equal to 20% improvement,” the study authors wrote.
There were no significant differences in adverse events or overall survival and transplant-free survival rates between the groups.
According to the researchers, the reasons for a “lower than expected treatment effect of terlipressin” were likely due to a combination of factors.
For example, the response rate to active treatment was lower in females (15.6%) than in males and significantly more female patients had been randomized to terlipressin.
Three patients treated with terlipressin who had HRS reversal were also discharged before obtaining the second serum creatinine measurement required to confirm they had met the study’s primary endpoint.
Furthermore, one-third of patients had received less than 3 days of active treatment, which could have also contributed to the lower response rate.
“Overall, the safety profile observed in the study reflects the known pharmacodynamic properties of terlipressin and is consistent with the scientific literature. Terlipressin is an effective therapy for the treatment of HRS-1, with a favorable benefit-risk profile,” the researchers concluded.
Several of the authors are consultants of Ikaria Therapeutics LLC/a Mallinckrodt Company, which sponsored the study and participated in its design, interpretation of data, and writing.
Treating patients with hepatorenal syndrome type 1 (HRS-1) with the synthetic vasopressin analogue terlipressin (Lucassin) and albumin does not improve the chances of reversal of hepatorenal syndrome compared with albumin alone, but could improve survival, the results of a multicenter, randomized, double-blind, placebo-controlled trial suggest.
Reporting the latest findings from the REVERSE trial, Dr. Thomas D. Boyer of the Liver Research Institute at the University of Arizona, Tucson, and colleagues said previous studies, including one by their team, had shown that terlipressin together with albumin was more effective at reversing hepatorenal syndrome type 1 (HRS-1) and improving serum creatinine compared with placebo.
However, they noted that while terlipressin was approved for treating HRS-1 in several countries, it was not approved in the United States or Canada. European guidelines also recommended terlipressin plus albumin as a first-line treatment in these patients.
In the current phase III, randomized double-blind, placebo-controlled trial, 196 patients with cirrhosis, ascites, and HRS-1 were enrolled from 50 centers in the United States and two centers in Canada (Gastroenterology 2016. doi: 10.1053/j.gastro.2016.02.026). Study participants were randomly assigned to terlipressin 1 mg (n = 97) or placebo (n = 99) with albumin every 6 hours.
Treatment continued for 14 days unless the patient had met the study primary endpoint of a confirmed HRS reversal defined by the authors as two serum creatinine levels less than 1.5 mg/dL at least 40 hours apart on treatment without renal replacement therapy or transplant, or serum creatinine (sCr) levels at or above baseline on day 4.
Results showed that confirmed HRS reversal occurred in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%) (P = .22), a difference that was not statistically significant.
The secondary outcome of reversal of HRS-1 (defined as at least 1 sCr value less than or equal to 1.5 mg/dL while on treatment) was reached by 23 patients on terlipressin and 15 patients on albumin alone (23.7 vs. 15.2%, P = .13), a finding that again was not statistically significant.
However, the research team observed significant improvements in serum creatinine in the patients treated with terlipressin that correlated with survival. For example, sCr decreased by 1.1 mg/dL in patients receiving terlipressin compared to 0.6 mg/dL in patients receiving placebo.
“While all patients with [confirmed HRS reversal] had a more than 20% decrease in sCr from baseline, the majority with a greater than 20% decrease in sCr did not achieve [confirmed HRS reversal] and yet appeared to have an improved survival compared with patients with less than or equal to 20% improvement,” the study authors wrote.
There were no significant differences in adverse events or overall survival and transplant-free survival rates between the groups.
According to the researchers, the reasons for a “lower than expected treatment effect of terlipressin” were likely due to a combination of factors.
For example, the response rate to active treatment was lower in females (15.6%) than in males and significantly more female patients had been randomized to terlipressin.
Three patients treated with terlipressin who had HRS reversal were also discharged before obtaining the second serum creatinine measurement required to confirm they had met the study’s primary endpoint.
Furthermore, one-third of patients had received less than 3 days of active treatment, which could have also contributed to the lower response rate.
“Overall, the safety profile observed in the study reflects the known pharmacodynamic properties of terlipressin and is consistent with the scientific literature. Terlipressin is an effective therapy for the treatment of HRS-1, with a favorable benefit-risk profile,” the researchers concluded.
Several of the authors are consultants of Ikaria Therapeutics LLC/a Mallinckrodt Company, which sponsored the study and participated in its design, interpretation of data, and writing.
Treating patients with hepatorenal syndrome type 1 (HRS-1) with the synthetic vasopressin analogue terlipressin (Lucassin) and albumin does not improve the chances of reversal of hepatorenal syndrome compared with albumin alone, but could improve survival, the results of a multicenter, randomized, double-blind, placebo-controlled trial suggest.
Reporting the latest findings from the REVERSE trial, Dr. Thomas D. Boyer of the Liver Research Institute at the University of Arizona, Tucson, and colleagues said previous studies, including one by their team, had shown that terlipressin together with albumin was more effective at reversing hepatorenal syndrome type 1 (HRS-1) and improving serum creatinine compared with placebo.
However, they noted that while terlipressin was approved for treating HRS-1 in several countries, it was not approved in the United States or Canada. European guidelines also recommended terlipressin plus albumin as a first-line treatment in these patients.
In the current phase III, randomized double-blind, placebo-controlled trial, 196 patients with cirrhosis, ascites, and HRS-1 were enrolled from 50 centers in the United States and two centers in Canada (Gastroenterology 2016. doi: 10.1053/j.gastro.2016.02.026). Study participants were randomly assigned to terlipressin 1 mg (n = 97) or placebo (n = 99) with albumin every 6 hours.
Treatment continued for 14 days unless the patient had met the study primary endpoint of a confirmed HRS reversal defined by the authors as two serum creatinine levels less than 1.5 mg/dL at least 40 hours apart on treatment without renal replacement therapy or transplant, or serum creatinine (sCr) levels at or above baseline on day 4.
Results showed that confirmed HRS reversal occurred in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%) (P = .22), a difference that was not statistically significant.
The secondary outcome of reversal of HRS-1 (defined as at least 1 sCr value less than or equal to 1.5 mg/dL while on treatment) was reached by 23 patients on terlipressin and 15 patients on albumin alone (23.7 vs. 15.2%, P = .13), a finding that again was not statistically significant.
However, the research team observed significant improvements in serum creatinine in the patients treated with terlipressin that correlated with survival. For example, sCr decreased by 1.1 mg/dL in patients receiving terlipressin compared to 0.6 mg/dL in patients receiving placebo.
“While all patients with [confirmed HRS reversal] had a more than 20% decrease in sCr from baseline, the majority with a greater than 20% decrease in sCr did not achieve [confirmed HRS reversal] and yet appeared to have an improved survival compared with patients with less than or equal to 20% improvement,” the study authors wrote.
There were no significant differences in adverse events or overall survival and transplant-free survival rates between the groups.
According to the researchers, the reasons for a “lower than expected treatment effect of terlipressin” were likely due to a combination of factors.
For example, the response rate to active treatment was lower in females (15.6%) than in males and significantly more female patients had been randomized to terlipressin.
Three patients treated with terlipressin who had HRS reversal were also discharged before obtaining the second serum creatinine measurement required to confirm they had met the study’s primary endpoint.
Furthermore, one-third of patients had received less than 3 days of active treatment, which could have also contributed to the lower response rate.
“Overall, the safety profile observed in the study reflects the known pharmacodynamic properties of terlipressin and is consistent with the scientific literature. Terlipressin is an effective therapy for the treatment of HRS-1, with a favorable benefit-risk profile,” the researchers concluded.
Several of the authors are consultants of Ikaria Therapeutics LLC/a Mallinckrodt Company, which sponsored the study and participated in its design, interpretation of data, and writing.
FROM GASTROENTEROLOGY
Key clinical point: Treating patients with hepatorenal syndrome type 1 with terlipressin and albumin does not improve the chances of reversal of hepatorenal syndrome compared to albumin alone but could improve survival.
Major finding: Hepatorenal syndrome reversal occurred in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%), a difference that was not statistically significant.
Data source: A phase III randomized, double-blind placebo-controlled trial of 196 patients with cirrhosis, ascites, and HRS-1.
Disclosures: Several of the authors are consultants of Ikaria Therapeutics LLC/a Mallinckrodt Company, which sponsored the study and participated in its design, interpretation of data, and writing.
Anti-Remicade antibodies also cross-react with infliximab biosimilar
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Rheumatology patients with positive antibodies to Remicade should not be switched to infliximab biosimilar (Remsima, Inflectra).
Major finding: Antibodies to infliximab in Remicade-treated rheumatology patients showed identical reactivity towards the biosimilar CT-P13.
Data source: A retrospective study of 250 consecutive patients with RA and SpA taking Remicade and 77 infliximab-naive controls.
Disclosures: Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Severe dengue fever outcomes predicted via metabolomics
The progression of dengue fever into life-threatening dengue hemorrhagic fever or dengue shock syndrome can be predicted by analyzing patient serum for metabolites associated with dengue virus infection, a proof of concept study suggests.
Researchers led by Natalia V. Voge, Ph.D., of Colorado State University, Fort Collins, said that because dengue fever had the potential to develop into life-threatening dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS), “the ability to predict these severe outcomes using acute phase clinical specimens would be of enormous value to physicians and health care workers for appropriate triaging of patients for clinical management” (PLOS Negl Trop Dis. 2016. doi: 10.1371/journal.pntd.0004449).
Advances in the field of metabolomics provided new opportunities to identify host small molecule biomarkers (SMBs) in acute phase clinical specimens that differentiate dengue disease outcomes, they said.
Collaborating with colleagues from the University of California, Berkeley, the Nicaraguan Ministry of Health, and the University of Yucatan, Mexico, the researchers used liquid chromatography and mass spectrometry to analyze 88 serum samples from Nicaraguan pediatric patients with diagnosed DHF/DSS or ND, and 101 serum samples from pediatric and adult Mexican patients.
In the Nicaraguan samples, the researchers identified metabolites that were associated with and differentiated DHF/DSS, DF, and non-dengue febrile illness outcomes, primary and secondary virus infections, and infections with different dengue virus serotypes.
“These metabolites provide insights into metabolic pathways that play roles in dengue virus infection, replication, and pathogenesis,” they wrote.
For instance, some were associated with “lipid metabolism and regulation of inflammatory processes controlled by signaling fatty acids and phospholipids, and others with endothelial cell homeostasis and vascular barrier function.”
The findings were not seen in the Mexican samples, which Dr. Voge and her associates said could reflect the diversity of the disease and the Mexican patients, who had a larger age distribution, compared with the pediatric Nicaraguan population.
Nevertheless, their results provided a proof of concept that “differential perturbation of the serum metabolome” is associated with different dengue infections and disease outcomes, they said.
Dr. Voge and her associates cautioned that while the results were encouraging, they were based on a small sample size and additional studies would be needed to confirm the results.
The findings were restricted to pediatric Nicaraguan patients and the same metabolites may not be predictive of progression to DHF/DSS in adult Nicaraguan patients or in patients from other geographic, genetic, and environmental backgrounds, they added.
The research was supported by National Institutes of Health grants.
The progression of dengue fever into life-threatening dengue hemorrhagic fever or dengue shock syndrome can be predicted by analyzing patient serum for metabolites associated with dengue virus infection, a proof of concept study suggests.
Researchers led by Natalia V. Voge, Ph.D., of Colorado State University, Fort Collins, said that because dengue fever had the potential to develop into life-threatening dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS), “the ability to predict these severe outcomes using acute phase clinical specimens would be of enormous value to physicians and health care workers for appropriate triaging of patients for clinical management” (PLOS Negl Trop Dis. 2016. doi: 10.1371/journal.pntd.0004449).
Advances in the field of metabolomics provided new opportunities to identify host small molecule biomarkers (SMBs) in acute phase clinical specimens that differentiate dengue disease outcomes, they said.
Collaborating with colleagues from the University of California, Berkeley, the Nicaraguan Ministry of Health, and the University of Yucatan, Mexico, the researchers used liquid chromatography and mass spectrometry to analyze 88 serum samples from Nicaraguan pediatric patients with diagnosed DHF/DSS or ND, and 101 serum samples from pediatric and adult Mexican patients.
In the Nicaraguan samples, the researchers identified metabolites that were associated with and differentiated DHF/DSS, DF, and non-dengue febrile illness outcomes, primary and secondary virus infections, and infections with different dengue virus serotypes.
“These metabolites provide insights into metabolic pathways that play roles in dengue virus infection, replication, and pathogenesis,” they wrote.
For instance, some were associated with “lipid metabolism and regulation of inflammatory processes controlled by signaling fatty acids and phospholipids, and others with endothelial cell homeostasis and vascular barrier function.”
The findings were not seen in the Mexican samples, which Dr. Voge and her associates said could reflect the diversity of the disease and the Mexican patients, who had a larger age distribution, compared with the pediatric Nicaraguan population.
Nevertheless, their results provided a proof of concept that “differential perturbation of the serum metabolome” is associated with different dengue infections and disease outcomes, they said.
Dr. Voge and her associates cautioned that while the results were encouraging, they were based on a small sample size and additional studies would be needed to confirm the results.
The findings were restricted to pediatric Nicaraguan patients and the same metabolites may not be predictive of progression to DHF/DSS in adult Nicaraguan patients or in patients from other geographic, genetic, and environmental backgrounds, they added.
The research was supported by National Institutes of Health grants.
The progression of dengue fever into life-threatening dengue hemorrhagic fever or dengue shock syndrome can be predicted by analyzing patient serum for metabolites associated with dengue virus infection, a proof of concept study suggests.
Researchers led by Natalia V. Voge, Ph.D., of Colorado State University, Fort Collins, said that because dengue fever had the potential to develop into life-threatening dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS), “the ability to predict these severe outcomes using acute phase clinical specimens would be of enormous value to physicians and health care workers for appropriate triaging of patients for clinical management” (PLOS Negl Trop Dis. 2016. doi: 10.1371/journal.pntd.0004449).
Advances in the field of metabolomics provided new opportunities to identify host small molecule biomarkers (SMBs) in acute phase clinical specimens that differentiate dengue disease outcomes, they said.
Collaborating with colleagues from the University of California, Berkeley, the Nicaraguan Ministry of Health, and the University of Yucatan, Mexico, the researchers used liquid chromatography and mass spectrometry to analyze 88 serum samples from Nicaraguan pediatric patients with diagnosed DHF/DSS or ND, and 101 serum samples from pediatric and adult Mexican patients.
In the Nicaraguan samples, the researchers identified metabolites that were associated with and differentiated DHF/DSS, DF, and non-dengue febrile illness outcomes, primary and secondary virus infections, and infections with different dengue virus serotypes.
“These metabolites provide insights into metabolic pathways that play roles in dengue virus infection, replication, and pathogenesis,” they wrote.
For instance, some were associated with “lipid metabolism and regulation of inflammatory processes controlled by signaling fatty acids and phospholipids, and others with endothelial cell homeostasis and vascular barrier function.”
The findings were not seen in the Mexican samples, which Dr. Voge and her associates said could reflect the diversity of the disease and the Mexican patients, who had a larger age distribution, compared with the pediatric Nicaraguan population.
Nevertheless, their results provided a proof of concept that “differential perturbation of the serum metabolome” is associated with different dengue infections and disease outcomes, they said.
Dr. Voge and her associates cautioned that while the results were encouraging, they were based on a small sample size and additional studies would be needed to confirm the results.
The findings were restricted to pediatric Nicaraguan patients and the same metabolites may not be predictive of progression to DHF/DSS in adult Nicaraguan patients or in patients from other geographic, genetic, and environmental backgrounds, they added.
The research was supported by National Institutes of Health grants.
FROM PLOS NEGLECTED TROPICAL DISEASES
Key clinical point: The life-threatening outcomes of dengue fever could be predicted by identifying host small biomarkers in patient serum.
Major finding: The researchers identified metabolites that were associated with and differentiated dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS), dengue fever (DF), and non-dengue febrile illness (ND) outcomes, primary and secondary virus infections, and infections with different dengue virus serotypes.
Data source: A total of 88 serum samples from Nicaraguan pediatric patients with diagnosed DHF/DSS or ND, and 101 serum samples from pediatric and adult Mexican patients.
Disclosures: The research was supported by National Institute of Health grants.
Minimal disease activity criteria in PsA fall short
The minimal disease activity criteria used to identify low disease activity in psoriatic arthritis (PsA) may not be useful as a treatment target in patients with extended skin involvement, according to the results of a small study.
Minimal disease activity (MDA) for PsA is a composite measure encompassing clinically important aspects of the disease: arthritis, psoriasis, enthesitis, pain, patient-assessed global disease activity, and physical function and provides an objective target for therapy in clinical trials, Dr. Josefina Marin of the Hospital Italiano de Buenos Aires and her associates wrote in the Journal of Rheumatology.
To evaluate components of the MDA criteria, the research team enrolled 83 consecutive patients with PsA aged over 18 years who were attending their clinic. Patients needed to fulfill five out of the seven criteria to be classified as having MDA.
An assessment by a single experienced rheumatologist revealed that 41 patients met MDA criteria, with only 7.4% of these patients not satisfying the tender/swollen joint–count criteria.
However, only 51% (n = 21) of patients fulfilling MDA fulfilled the skin criteria (Psoriasis Area and Severity Index [PASI] and body surface area [BSA]), a percentage not statistically different from the 36% of patients not in MDA (n = 15; P = .154). “This is important because MDA may therefore not be useful as a treatment target in patients with extended skin involvement,” the investigators wrote (J Rheum. 2016 Mar 1. doi: 10.3899/jrheum.151101).
The investigators noted that the selection of the target was of crucial importance when implementing a treat-to-target and tight control strategy. “In this sense our study provides reassurance that almost all patients at MDA will have no swollen/tender joints but also raises some concerns that the skin might not be well controlled if the MDA is used as the only target to treat patients with both joint and skin involvement,” they wrote. One explanation could be that the cutoff values selected in the MDA criteria for skin involvement are too stringent for therapies currently available, they suggested.
MDA seems to be a valuable tool to define low disease activity in patients with PsA, but the skin component requires further evaluation, they concluded.
The research was partially supported by the PANLAR/Abbvie Rheumatology prize 2012.
The minimal disease activity criteria used to identify low disease activity in psoriatic arthritis (PsA) may not be useful as a treatment target in patients with extended skin involvement, according to the results of a small study.
Minimal disease activity (MDA) for PsA is a composite measure encompassing clinically important aspects of the disease: arthritis, psoriasis, enthesitis, pain, patient-assessed global disease activity, and physical function and provides an objective target for therapy in clinical trials, Dr. Josefina Marin of the Hospital Italiano de Buenos Aires and her associates wrote in the Journal of Rheumatology.
To evaluate components of the MDA criteria, the research team enrolled 83 consecutive patients with PsA aged over 18 years who were attending their clinic. Patients needed to fulfill five out of the seven criteria to be classified as having MDA.
An assessment by a single experienced rheumatologist revealed that 41 patients met MDA criteria, with only 7.4% of these patients not satisfying the tender/swollen joint–count criteria.
However, only 51% (n = 21) of patients fulfilling MDA fulfilled the skin criteria (Psoriasis Area and Severity Index [PASI] and body surface area [BSA]), a percentage not statistically different from the 36% of patients not in MDA (n = 15; P = .154). “This is important because MDA may therefore not be useful as a treatment target in patients with extended skin involvement,” the investigators wrote (J Rheum. 2016 Mar 1. doi: 10.3899/jrheum.151101).
The investigators noted that the selection of the target was of crucial importance when implementing a treat-to-target and tight control strategy. “In this sense our study provides reassurance that almost all patients at MDA will have no swollen/tender joints but also raises some concerns that the skin might not be well controlled if the MDA is used as the only target to treat patients with both joint and skin involvement,” they wrote. One explanation could be that the cutoff values selected in the MDA criteria for skin involvement are too stringent for therapies currently available, they suggested.
MDA seems to be a valuable tool to define low disease activity in patients with PsA, but the skin component requires further evaluation, they concluded.
The research was partially supported by the PANLAR/Abbvie Rheumatology prize 2012.
The minimal disease activity criteria used to identify low disease activity in psoriatic arthritis (PsA) may not be useful as a treatment target in patients with extended skin involvement, according to the results of a small study.
Minimal disease activity (MDA) for PsA is a composite measure encompassing clinically important aspects of the disease: arthritis, psoriasis, enthesitis, pain, patient-assessed global disease activity, and physical function and provides an objective target for therapy in clinical trials, Dr. Josefina Marin of the Hospital Italiano de Buenos Aires and her associates wrote in the Journal of Rheumatology.
To evaluate components of the MDA criteria, the research team enrolled 83 consecutive patients with PsA aged over 18 years who were attending their clinic. Patients needed to fulfill five out of the seven criteria to be classified as having MDA.
An assessment by a single experienced rheumatologist revealed that 41 patients met MDA criteria, with only 7.4% of these patients not satisfying the tender/swollen joint–count criteria.
However, only 51% (n = 21) of patients fulfilling MDA fulfilled the skin criteria (Psoriasis Area and Severity Index [PASI] and body surface area [BSA]), a percentage not statistically different from the 36% of patients not in MDA (n = 15; P = .154). “This is important because MDA may therefore not be useful as a treatment target in patients with extended skin involvement,” the investigators wrote (J Rheum. 2016 Mar 1. doi: 10.3899/jrheum.151101).
The investigators noted that the selection of the target was of crucial importance when implementing a treat-to-target and tight control strategy. “In this sense our study provides reassurance that almost all patients at MDA will have no swollen/tender joints but also raises some concerns that the skin might not be well controlled if the MDA is used as the only target to treat patients with both joint and skin involvement,” they wrote. One explanation could be that the cutoff values selected in the MDA criteria for skin involvement are too stringent for therapies currently available, they suggested.
MDA seems to be a valuable tool to define low disease activity in patients with PsA, but the skin component requires further evaluation, they concluded.
The research was partially supported by the PANLAR/Abbvie Rheumatology prize 2012.
FROM THE JOURNAL OF RHEUMATOLOGY
Key clinical point: Minimal disease activity criteria in PsA may not be stringent enough for people with extended skin involvement.
Major finding: Only half of the PsA patients classified as having minimal disease activity met PASI and body surface area criteria.
Data source: A single-center study of 83 consecutive PsA patients aged over 18 years.
Disclosures: The research was partially supported by the PANLAR/Abbvie Rheumatology prize 2012.
Subtle radiographic progression in axial SpA cannot be reliably distinguished from error
Sacroiliitis observed in patients with axial spondyloarthritis more often regressed rather than progressed on radiography over nearly 5 years of follow-up of the Assessment of SpondyloArthritis international Society (ASAS) cohort, which lead author Dr. Alexandre Sepriano and his colleagues called “strange” and “sobering.”
The findings call into question the reliability of plain pelvic radiographs for detecting subtle change in sacroiliitis and should prompt the evaluation of alternative imaging modalities such as MRI and low-dose CT, according to Dr. Sepriano of Leiden (the Netherlands) University Medical Center and his associates.
Determining the presence of radiographic sacroiliitis is prognostically relevant and can pave the way for treatment with biologics, but ambiguity in making this decision and in tracking progression has been revealed in the large inter-and intrareader variability found in previous studies. Furthermore, previous studies tracking progression of nonradiographic axial spondyloarthritis (axSpA) to radiographic axSpA have addressed only disease progression and ignored regression. While regression is likely to be rare, it cannot be ignored from a methodologic standpoint, the investigators wrote.
The researchers therefore set out in the current study to assess positive and negative changes in sacroiliitis on plain pelvic radiographs over time in 975 patients from the ASAS cohort who had chronic back pain of unknown origin or undiagnosed peripheral symptoms (Ann Rheum Dis. 2016 Feb 22. doi: 10.1136/annrheumdis-2015-208964).
Of the 357 of the patients who had paired plain pelvic radiographs available at baseline and follow-up, 17.4% (62/357) fulfilled the criteria for radiographic axSpA at baseline, as defined by modified New York criteria (mNY). At a mean follow-up of 4.4 years, this figure had risen to 22.4% (80/357), suggesting a net progression of 5%.
However, when the authors cross-tabulated their figures, more than half (36/62) of the patients considered mNY positive at baseline were assessed as mNY negative at follow-up. This would mean that radiographic sacroiliitis would have regressed in 58% of the cases; conversely, only 54 of 295 patients (18.3%) became mNY positive at follow-up.
“If only positive change (progression) is valued and negative change is ignored, one would disregard measurement error and spuriously attribute part of the observed positive change to real progression,” the research team explained. “The most likely explanation of our strange and extreme observation is that subtle radiographic progression (the signal) – if truly present – cannot be reliably distinguished from measurement error (the noise). These sobering data clearly illustrate that more research is needed in visualising progression in axSpA.”
ASAS funded the study. The authors had no competing interests to declare.
Sacroiliitis observed in patients with axial spondyloarthritis more often regressed rather than progressed on radiography over nearly 5 years of follow-up of the Assessment of SpondyloArthritis international Society (ASAS) cohort, which lead author Dr. Alexandre Sepriano and his colleagues called “strange” and “sobering.”
The findings call into question the reliability of plain pelvic radiographs for detecting subtle change in sacroiliitis and should prompt the evaluation of alternative imaging modalities such as MRI and low-dose CT, according to Dr. Sepriano of Leiden (the Netherlands) University Medical Center and his associates.
Determining the presence of radiographic sacroiliitis is prognostically relevant and can pave the way for treatment with biologics, but ambiguity in making this decision and in tracking progression has been revealed in the large inter-and intrareader variability found in previous studies. Furthermore, previous studies tracking progression of nonradiographic axial spondyloarthritis (axSpA) to radiographic axSpA have addressed only disease progression and ignored regression. While regression is likely to be rare, it cannot be ignored from a methodologic standpoint, the investigators wrote.
The researchers therefore set out in the current study to assess positive and negative changes in sacroiliitis on plain pelvic radiographs over time in 975 patients from the ASAS cohort who had chronic back pain of unknown origin or undiagnosed peripheral symptoms (Ann Rheum Dis. 2016 Feb 22. doi: 10.1136/annrheumdis-2015-208964).
Of the 357 of the patients who had paired plain pelvic radiographs available at baseline and follow-up, 17.4% (62/357) fulfilled the criteria for radiographic axSpA at baseline, as defined by modified New York criteria (mNY). At a mean follow-up of 4.4 years, this figure had risen to 22.4% (80/357), suggesting a net progression of 5%.
However, when the authors cross-tabulated their figures, more than half (36/62) of the patients considered mNY positive at baseline were assessed as mNY negative at follow-up. This would mean that radiographic sacroiliitis would have regressed in 58% of the cases; conversely, only 54 of 295 patients (18.3%) became mNY positive at follow-up.
“If only positive change (progression) is valued and negative change is ignored, one would disregard measurement error and spuriously attribute part of the observed positive change to real progression,” the research team explained. “The most likely explanation of our strange and extreme observation is that subtle radiographic progression (the signal) – if truly present – cannot be reliably distinguished from measurement error (the noise). These sobering data clearly illustrate that more research is needed in visualising progression in axSpA.”
ASAS funded the study. The authors had no competing interests to declare.
Sacroiliitis observed in patients with axial spondyloarthritis more often regressed rather than progressed on radiography over nearly 5 years of follow-up of the Assessment of SpondyloArthritis international Society (ASAS) cohort, which lead author Dr. Alexandre Sepriano and his colleagues called “strange” and “sobering.”
The findings call into question the reliability of plain pelvic radiographs for detecting subtle change in sacroiliitis and should prompt the evaluation of alternative imaging modalities such as MRI and low-dose CT, according to Dr. Sepriano of Leiden (the Netherlands) University Medical Center and his associates.
Determining the presence of radiographic sacroiliitis is prognostically relevant and can pave the way for treatment with biologics, but ambiguity in making this decision and in tracking progression has been revealed in the large inter-and intrareader variability found in previous studies. Furthermore, previous studies tracking progression of nonradiographic axial spondyloarthritis (axSpA) to radiographic axSpA have addressed only disease progression and ignored regression. While regression is likely to be rare, it cannot be ignored from a methodologic standpoint, the investigators wrote.
The researchers therefore set out in the current study to assess positive and negative changes in sacroiliitis on plain pelvic radiographs over time in 975 patients from the ASAS cohort who had chronic back pain of unknown origin or undiagnosed peripheral symptoms (Ann Rheum Dis. 2016 Feb 22. doi: 10.1136/annrheumdis-2015-208964).
Of the 357 of the patients who had paired plain pelvic radiographs available at baseline and follow-up, 17.4% (62/357) fulfilled the criteria for radiographic axSpA at baseline, as defined by modified New York criteria (mNY). At a mean follow-up of 4.4 years, this figure had risen to 22.4% (80/357), suggesting a net progression of 5%.
However, when the authors cross-tabulated their figures, more than half (36/62) of the patients considered mNY positive at baseline were assessed as mNY negative at follow-up. This would mean that radiographic sacroiliitis would have regressed in 58% of the cases; conversely, only 54 of 295 patients (18.3%) became mNY positive at follow-up.
“If only positive change (progression) is valued and negative change is ignored, one would disregard measurement error and spuriously attribute part of the observed positive change to real progression,” the research team explained. “The most likely explanation of our strange and extreme observation is that subtle radiographic progression (the signal) – if truly present – cannot be reliably distinguished from measurement error (the noise). These sobering data clearly illustrate that more research is needed in visualising progression in axSpA.”
ASAS funded the study. The authors had no competing interests to declare.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Subtle radiographic progression in axSpA cannot be reliably distinguished from measurement error.
Major finding: Using plain radiographs, more than half of the patients identified as mNY positive for axSpA at baseline were assessed as mNY negative at a mean follow-up of 4.4 years.
Data source: 975 patients with chronic back pain of unknown origin or undiagnosed peripheral symptoms taking part in the Assessment of SpondyloArthritis international Society (ASAS) cohort.
Disclosures: ASAS funded the study. The authors had no competing interests to declare.