User login
A Novel Technique for the Treatment of Jersey Fingers
ABSTRACT
The avulsion of the flexor digitorum profundus from its insertion, or “jersey finger,” is a relatively common injury. Numerous modifications have been made to the classification and treatment of this injury since its initial description. We describe a novel variation of the surgical management of jersey finger.
The avulsion-type injury of the flexor digitorum profundus (FDP) from its insertion on the distal phalanx is relatively common. FDP avulsions are seen in athletes and nonathletes, and are the result of the sudden hyperextension of the distal interphalangeal joint during active flexion. These injuries usually occur while grasping the jersey of an opposing player and are thus commonly referred to as “jersey finger.” Initially described in 1977 by Leddy and Packer1, FDP avulsions are classified on the basis of the proximal extent of the retraction of the FDP and the presence or absence of a bony avulsion fracture fragment. Type I injuries are defined by tendon retraction to the level of the palm, where it is tethered by the lumbricals. At this level, the vinculum longus profundus (VLP) and vinculum brevis profundus (VBP) are ruptured, resulting in the substantial loss of intrinsic and extrinsic vascular supply to the tendon. In type II injuries, which are the most common type of FDP avulsions, the FDP tendon retracts to the level of the proximal interphalangeal (PIP) joint. Although the VBP is disrupted in this scenario, the VLP remains preserved because it arises at the level of the volar plate of the PIP joint. Type III lesions involve tendon avulsions with an associated bony fragment that is typically sufficiently large to not pass through the flexor sheath, thus limiting retraction to the level of the A4 pulley. Both vincula remain intact, given that the VBP originates at the distal portion of the middle phalanx. The Leddy and Packer classification was later expanded to include type IV and V injury patterns, which are less common than other injury patterns. Similar to type III injuries, type IV injuries involve a bony avulsion; however, the FDP subsequently ruptures from this fragment and the tendon subsequently retracts into the finger or palm.2,3 Type V injuries are more complex than other injury types because they involve a concomitant distal phalanx fracture with the FDP avulsion.4 Al-Qattan5 subclassified type V injuries into extra-articular (type Va) and intra-articular (type Vb) distal phalanx fractures on the basis of the distinct management of these 2 entities.
Numerous techniques have been proposed and described for the repair of FDP avulsion injuries. The pullout suture-dorsal button combination is the most widely described technique and was initially described by Bunnell.6 Unfortunately, this technique is accompanied by numerous potential postoperative complications.6 Nail plate deformity is the most commonly described complication. Other complications include local wound irritation, pain, button snagging, and repair failure. Additionally, the presence of external sutures creates a potential route of ingress for bacterial infection.
Continue to: Bone suture anchor techniques...
Bone suture anchor techniques were later utilized to repair FDP avulsions in an attempt to decrease complications associated with the external suture-button construct.7 The use of a transosseous suture without external button fixation has also been proposed. Sood and Elliot8 described a technique where the suture is passed through a hole, drilled transversely through the tuft of the distal phalanx, and affixed to the other limb. In 1999, Schultz and colleagues9 described a technique where transosseous tunnels are placed in the distal phalanx in a dorsal-to-volar direction. The suture is then passed through and tied on the dorsal surface. In this article, we propose a transosseous suture technique that may provide advantages over previously described methods.
SURGICAL TECHNIQUE
TYPES I, II, AND III
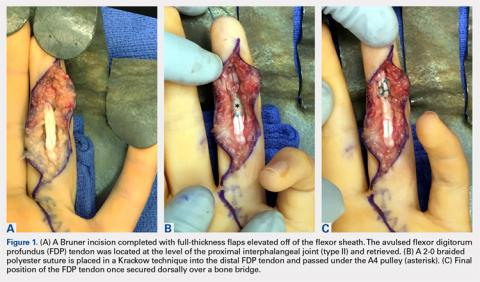
A Bruner incision is performed on the volar aspect of the affected finger, and full thickness flaps are elevated off the flexor sheath (Figures 1A-1C).
TYPES IV AND V
In cases of type IV or V injury (Figure 4A), a screw or plate construct is first used to allow for the successful reduction and fixation of the fracture (Figure 4B).
DISCUSSION
The avulsion of the FDP tendon from its insertion (zone I) on the distal phalanx is commonly called “jersey finger” and is a well-described injury that occurs most commonly in the ring finger.10 These injuries can be difficult to treat and are associated with a complication rate of as high as 60%.11,12 Bunnell’s initial description of a suture passed through the fingernail and then tied over a polypropylene button has been associated with multiple complications. Kang and colleagues13 reported abnormal nail growth, nail fold necrosis, fingertip deformity, stiffness, infection, and amputation, 43% of all complications were directly related to the button. As an alternative to the button, sutures may be tied directly over the nail plate itself via 2 separate holes.14 While this technique eliminates the complications directly associated with the button, the potential for infection remains. Additionally, increased direct pressure is placed on the nail plate and nail bed, thus potentially increasing the risk of nail deformity.
In 1994, Hallock7 initially described the use of bone anchors as an “internal fixation” alternative and cited the “expense of the apparatus” as the major drawback of this technique. McCallister and colleagues15 compared the clinical outcome of suture anchor fixation with that of the button-over-nail technique. Although they ultimately demonstrated that the clinical outcomes of the 2 techniques are not significantly different, they noted that suture anchor fixation is associated with decreased infection rate (7% vs 0%) and time to return to work. Poor bone mineral density and low cortical thickness are correlated with anchor pull-out, thus limiting its universal use.16 Furthermore, the universal use of many commonly available anchors is limited given that they are too large to be accommodated within many phalanges, particularly in women and in the small and ring fingers.17 The use of microanchors rather than mini anchors not only decreases this risk but also decreases construct strength, thus necessitating the use of 2 anchors to restore adequate fixation strength. Anchor use is associated with specific risks, including the dorsal migration of the anchor, the osteolysis of the surrounding bone, as well as the perforation of the dorsal cortex and the possible extrusion of the anchor through the phalanx and into the nail bed.18,19 Additionally, in the wake of a changing healthcare system, the cost of suture anchors, as initially noted by Hallock,7 must be considered. This consideration is particularly relevant to the use of a 2 microanchor construct, which has been advocated given its biomechanical advantage.20,21
Continue to: Transosseous tendon repair...
Transosseous tendon repair is a cost-effective option that obviates many complications commonly observed with other fixation methods. By keeping the suture within the body, the complications inherent in external sutures and buttons are eliminated, including the loss of fixation as a result of button or suture damage and facilitating hand hygiene maintenance. The rate of infection is also reduced. Moreover, the risk of nail deformities is decreased because the suture is not passed through the nail bed and nail plate in the described technique. Occasionally, some patients do note irritation from the dorsal suture knot under the thin skin proximal to the germinal matrix. This can be easily addressed in the clinic by removing the knot under local anesthesia following sufficient tendon healing. Additionally, the described technique can be used safely in pediatric patients with open physes because the needles can be placed to prevent violating the physis. This technique can be performed in conjunction with the skeletal fixation of type III, IV, and V jersey fingers. In our experience, the transosseous suture repair is more secure than the limited screw fixation, which can be accomplished in many type III jersey fingers, and in at least 1 case, has maintained flexor function when the skeletal fixation of the jersey finger has failed (Figures 5A, 5B).
All internal fixation techniques have been described previously by Sood and Elliot8 and, later, by Schultz and colleagues.9 In contrast to Sood and Elliott’s8 technique, which requires the creation of transverse tunnels, a volar-to-dorsal tunnel is technically easy to create and creates a direct repair to tendon insertion. Our technique is similar to that of Schultz and colleagues'9 but has the following differences and potential improvements:
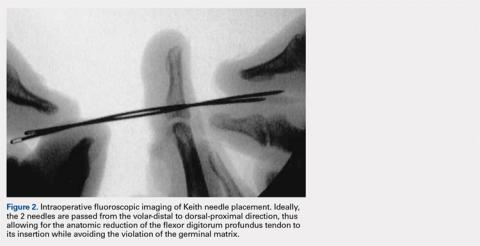
- Keith needles are passed in a volar-to-dorsal fashion, thus allowing for the direct visualization of the transosseous tunnel origin, minimizing the size of the transosseous tunnels, and allowing for the anatomic reduction of the tendon.
- Fluoroscopy is used to confirm wire placement prior to skin incision, thus enabling precise placement and potentially allowing the needles to be placed so as to avoid physeal injury in pediatric jersey fingers.
- By using Keith needles, sutures can be passed with the same instrument that created the tunnel, thus simplifying surgical technique.
- A Krakow suture technique is used. This technique results in less gapping and higher load-to-failure than other suturing techniques.22
- A 2-0 braided suture is used, therefore strengthening repair.
This paper will be judged for the Resident Writer’s Award.
1. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2(1):66-69. doi:https://doi.org/10.1016/S0363-5023(77)80012-9.
2. Langa V, Posner MA. Unusual rupture of a flexor profundus tendon. J Hand Surg Am. 1986;11(2):227-229. doi:https://doi.org/10.1016/S0363-5023(86)80056-9.
3. Ehlert KJ, Gould JS, Black KP. A simultaneous distal phalanx avulsion fracture with profundus tendon avulsion: A case report and review of the literature. Clin Orthop Relat Res. 1992;(283):265-269.
4. Smith JH. Avulsion of a profundus tendon with simultaneous intraarticular fracture of the distal phalanx–case report. J Hand Surg Am. 1981;6(6):600-601. doi:10.1097/00006534-198305000-00081.
5. Al-Qattan MM. Type 5 avulsion of the insertion of the flexor digitorum profundus tendon. J Hand Surg Br. 2001;26(5):427-431. doi:10.1054/jhsb.2001.0619.
6. Bunnell S. Surgery of the hand, 2nd edition. Philadelphia, PA: JB Lippincott; 1948:381-466.
7. Hallock GG. The Mitek Mini GII anchor introduced for tendon reinsertion in the hand. Ann Plast Surg. 1994;33(2):211-213.
8. Sood MK, Elliot D. A new technique of attachment of flexor tendons to the distal phalanx without a button tie-over. J Hand Surg Br. 1996;21(5):629-632. doi:https://doi.org/10.1016/S0266-7681(96)80146-X.
9. Schultz RO, Drake DB, Morgan RF. A new technique for the treatment of flexor digitorum profundus tendon avulsion. Ann Plast Surg. 1999;42(1):46-48. doi:10.1097/00000637-199901000-00008.
10. Manske PR, Lesker PA. Avulsion of the ring finger flexor digitorum profundus tendon: An experimental study. Hand 1978;10(1):52-55. doi:https://doi.org/10.1016/S0072-968X(78)80025-4.
11. Gerbino PG, Saldana MJ, Westerbeck P, Schacherer TG. Complications experienced in the rehabilitation of zone I flexor tendon injuries with dynamic traction splinting. J Hand Surg Am. 1991;16(4):680-686. doi:https://doi.org/10.1016/0363-5023(91)90194-G
12. Evans RB. Zone I flexor tendon rehabilitation with limited extension and active flexion. J Hand Ther. 2005;18(2):128-140. doi:10.1197/j.jht.2005.02.001
13. Kang N, Marsh D, Dewar D. The morbidity of the button-over-nail technique for zone 1 flexor tendon repairs. Should we still be using this technique? J Hand Surg Eur Vol. 2008;33(5):566-570. doi:10.1177/1753193408090118
14. Taras JS. Flexor tendon reconstruction: Single stage flexor tendon grafting: FDP, FDS disrupted. In: Green DP, Hotchkiss RN, Pederson WL, Wolfe SW, eds. Green’s Operative Hand Surgery. 5th ed. Philadelphia, PA: Elsevier Health Sciences; 2005:248-249.
15. McCallister WV, Ambrose HC, Katolik LI, Trumble TE. Comparison of pullout button versus suture anchor for zone I flexor tendon repair. J Hand Surg Am. 2006;31:246-251. doi:10.1016/j.jhsa.2005.10.020
16. Matzsuzaki H, Zaegel MA, Gelberman RH, Silva MJ. Effect of suture material and bone quality on the mechanical properties of zone 1 flexor tendon-bone reattachment with bone anchors. J Hand Surg Am. 2008;33(5):709-717. doi:10.1016/j.jhsa.2008.01.025
17. Singh R, Kakarala G, Persaud I, Roberts M, Strandring S, Compson J. The optimal length of tissue anchors for distal phalanges. A study in 395 cadaver digits. J Bone Joint Surg Br. 2006;88-B(SUPP I):37.
18. Giannikas D, Athanaselis E, Matzaroglou C, Saridis A, Tyllianakis M. An unusual complication of Mitek suture anchor use in primary treatment of flexor digitorum profundus tendon laceration: a case report. Cases J. 2009;2:9319. doi:10.1186/1757-1626-2-9319
19. Tiong WH, O'Sullivan ST. Extrusion of bone anchor suture following flexor digitorum profundus tendon avulsion injury repair. J Plast Reconstr Aesthet Surg. 2011;64(9):1242-1244. doi:10.1016/j.bjps.2011.01.016
20. Silva MJ, Hollstien SB, Brodt MD, Boyer MI, Tetro AM, Gelberman RH. Flexor digitorum profundus tendon-to-bone repair: An ex vivo biomechanical analysis of 3 pullout suture techniques. J Hand Surg Am. 1998;23(1):120-126. doi:10.1016/S0363-5023(98)80099-3
21. Latendresse K, Dona E, Scougall PJ, Schreuder FB, Puchert E, Walsh WR. Cyclic testing of pullout sutures and micro-mitek suture anchors in flexor digitorum profundus tendon distal fixation. J Hand Surg Am. 2005;30(3):471-478. doi:10.1016/j.jhsa.2004.10.014
22. Lee SK, Fajardo M, Kardashian G, Klein J, Tsai P, Christoforou D. Repair of flexor digitorum profundus to distal phalanx: a biomechanical evaluation of four techniques. J Hand Surg Am. 2011;36(10):1604-1609. doi:10.1016/j.jhsa.2011.07.017
ABSTRACT
The avulsion of the flexor digitorum profundus from its insertion, or “jersey finger,” is a relatively common injury. Numerous modifications have been made to the classification and treatment of this injury since its initial description. We describe a novel variation of the surgical management of jersey finger.
The avulsion-type injury of the flexor digitorum profundus (FDP) from its insertion on the distal phalanx is relatively common. FDP avulsions are seen in athletes and nonathletes, and are the result of the sudden hyperextension of the distal interphalangeal joint during active flexion. These injuries usually occur while grasping the jersey of an opposing player and are thus commonly referred to as “jersey finger.” Initially described in 1977 by Leddy and Packer1, FDP avulsions are classified on the basis of the proximal extent of the retraction of the FDP and the presence or absence of a bony avulsion fracture fragment. Type I injuries are defined by tendon retraction to the level of the palm, where it is tethered by the lumbricals. At this level, the vinculum longus profundus (VLP) and vinculum brevis profundus (VBP) are ruptured, resulting in the substantial loss of intrinsic and extrinsic vascular supply to the tendon. In type II injuries, which are the most common type of FDP avulsions, the FDP tendon retracts to the level of the proximal interphalangeal (PIP) joint. Although the VBP is disrupted in this scenario, the VLP remains preserved because it arises at the level of the volar plate of the PIP joint. Type III lesions involve tendon avulsions with an associated bony fragment that is typically sufficiently large to not pass through the flexor sheath, thus limiting retraction to the level of the A4 pulley. Both vincula remain intact, given that the VBP originates at the distal portion of the middle phalanx. The Leddy and Packer classification was later expanded to include type IV and V injury patterns, which are less common than other injury patterns. Similar to type III injuries, type IV injuries involve a bony avulsion; however, the FDP subsequently ruptures from this fragment and the tendon subsequently retracts into the finger or palm.2,3 Type V injuries are more complex than other injury types because they involve a concomitant distal phalanx fracture with the FDP avulsion.4 Al-Qattan5 subclassified type V injuries into extra-articular (type Va) and intra-articular (type Vb) distal phalanx fractures on the basis of the distinct management of these 2 entities.
Numerous techniques have been proposed and described for the repair of FDP avulsion injuries. The pullout suture-dorsal button combination is the most widely described technique and was initially described by Bunnell.6 Unfortunately, this technique is accompanied by numerous potential postoperative complications.6 Nail plate deformity is the most commonly described complication. Other complications include local wound irritation, pain, button snagging, and repair failure. Additionally, the presence of external sutures creates a potential route of ingress for bacterial infection.
Continue to: Bone suture anchor techniques...
Bone suture anchor techniques were later utilized to repair FDP avulsions in an attempt to decrease complications associated with the external suture-button construct.7 The use of a transosseous suture without external button fixation has also been proposed. Sood and Elliot8 described a technique where the suture is passed through a hole, drilled transversely through the tuft of the distal phalanx, and affixed to the other limb. In 1999, Schultz and colleagues9 described a technique where transosseous tunnels are placed in the distal phalanx in a dorsal-to-volar direction. The suture is then passed through and tied on the dorsal surface. In this article, we propose a transosseous suture technique that may provide advantages over previously described methods.
SURGICAL TECHNIQUE
TYPES I, II, AND III
A Bruner incision is performed on the volar aspect of the affected finger, and full thickness flaps are elevated off the flexor sheath (Figures 1A-1C).
TYPES IV AND V
In cases of type IV or V injury (Figure 4A), a screw or plate construct is first used to allow for the successful reduction and fixation of the fracture (Figure 4B).
DISCUSSION
The avulsion of the FDP tendon from its insertion (zone I) on the distal phalanx is commonly called “jersey finger” and is a well-described injury that occurs most commonly in the ring finger.10 These injuries can be difficult to treat and are associated with a complication rate of as high as 60%.11,12 Bunnell’s initial description of a suture passed through the fingernail and then tied over a polypropylene button has been associated with multiple complications. Kang and colleagues13 reported abnormal nail growth, nail fold necrosis, fingertip deformity, stiffness, infection, and amputation, 43% of all complications were directly related to the button. As an alternative to the button, sutures may be tied directly over the nail plate itself via 2 separate holes.14 While this technique eliminates the complications directly associated with the button, the potential for infection remains. Additionally, increased direct pressure is placed on the nail plate and nail bed, thus potentially increasing the risk of nail deformity.
In 1994, Hallock7 initially described the use of bone anchors as an “internal fixation” alternative and cited the “expense of the apparatus” as the major drawback of this technique. McCallister and colleagues15 compared the clinical outcome of suture anchor fixation with that of the button-over-nail technique. Although they ultimately demonstrated that the clinical outcomes of the 2 techniques are not significantly different, they noted that suture anchor fixation is associated with decreased infection rate (7% vs 0%) and time to return to work. Poor bone mineral density and low cortical thickness are correlated with anchor pull-out, thus limiting its universal use.16 Furthermore, the universal use of many commonly available anchors is limited given that they are too large to be accommodated within many phalanges, particularly in women and in the small and ring fingers.17 The use of microanchors rather than mini anchors not only decreases this risk but also decreases construct strength, thus necessitating the use of 2 anchors to restore adequate fixation strength. Anchor use is associated with specific risks, including the dorsal migration of the anchor, the osteolysis of the surrounding bone, as well as the perforation of the dorsal cortex and the possible extrusion of the anchor through the phalanx and into the nail bed.18,19 Additionally, in the wake of a changing healthcare system, the cost of suture anchors, as initially noted by Hallock,7 must be considered. This consideration is particularly relevant to the use of a 2 microanchor construct, which has been advocated given its biomechanical advantage.20,21
Continue to: Transosseous tendon repair...
Transosseous tendon repair is a cost-effective option that obviates many complications commonly observed with other fixation methods. By keeping the suture within the body, the complications inherent in external sutures and buttons are eliminated, including the loss of fixation as a result of button or suture damage and facilitating hand hygiene maintenance. The rate of infection is also reduced. Moreover, the risk of nail deformities is decreased because the suture is not passed through the nail bed and nail plate in the described technique. Occasionally, some patients do note irritation from the dorsal suture knot under the thin skin proximal to the germinal matrix. This can be easily addressed in the clinic by removing the knot under local anesthesia following sufficient tendon healing. Additionally, the described technique can be used safely in pediatric patients with open physes because the needles can be placed to prevent violating the physis. This technique can be performed in conjunction with the skeletal fixation of type III, IV, and V jersey fingers. In our experience, the transosseous suture repair is more secure than the limited screw fixation, which can be accomplished in many type III jersey fingers, and in at least 1 case, has maintained flexor function when the skeletal fixation of the jersey finger has failed (Figures 5A, 5B).
All internal fixation techniques have been described previously by Sood and Elliot8 and, later, by Schultz and colleagues.9 In contrast to Sood and Elliott’s8 technique, which requires the creation of transverse tunnels, a volar-to-dorsal tunnel is technically easy to create and creates a direct repair to tendon insertion. Our technique is similar to that of Schultz and colleagues'9 but has the following differences and potential improvements:
- Keith needles are passed in a volar-to-dorsal fashion, thus allowing for the direct visualization of the transosseous tunnel origin, minimizing the size of the transosseous tunnels, and allowing for the anatomic reduction of the tendon.
- Fluoroscopy is used to confirm wire placement prior to skin incision, thus enabling precise placement and potentially allowing the needles to be placed so as to avoid physeal injury in pediatric jersey fingers.
- By using Keith needles, sutures can be passed with the same instrument that created the tunnel, thus simplifying surgical technique.
- A Krakow suture technique is used. This technique results in less gapping and higher load-to-failure than other suturing techniques.22
- A 2-0 braided suture is used, therefore strengthening repair.
This paper will be judged for the Resident Writer’s Award.
ABSTRACT
The avulsion of the flexor digitorum profundus from its insertion, or “jersey finger,” is a relatively common injury. Numerous modifications have been made to the classification and treatment of this injury since its initial description. We describe a novel variation of the surgical management of jersey finger.
The avulsion-type injury of the flexor digitorum profundus (FDP) from its insertion on the distal phalanx is relatively common. FDP avulsions are seen in athletes and nonathletes, and are the result of the sudden hyperextension of the distal interphalangeal joint during active flexion. These injuries usually occur while grasping the jersey of an opposing player and are thus commonly referred to as “jersey finger.” Initially described in 1977 by Leddy and Packer1, FDP avulsions are classified on the basis of the proximal extent of the retraction of the FDP and the presence or absence of a bony avulsion fracture fragment. Type I injuries are defined by tendon retraction to the level of the palm, where it is tethered by the lumbricals. At this level, the vinculum longus profundus (VLP) and vinculum brevis profundus (VBP) are ruptured, resulting in the substantial loss of intrinsic and extrinsic vascular supply to the tendon. In type II injuries, which are the most common type of FDP avulsions, the FDP tendon retracts to the level of the proximal interphalangeal (PIP) joint. Although the VBP is disrupted in this scenario, the VLP remains preserved because it arises at the level of the volar plate of the PIP joint. Type III lesions involve tendon avulsions with an associated bony fragment that is typically sufficiently large to not pass through the flexor sheath, thus limiting retraction to the level of the A4 pulley. Both vincula remain intact, given that the VBP originates at the distal portion of the middle phalanx. The Leddy and Packer classification was later expanded to include type IV and V injury patterns, which are less common than other injury patterns. Similar to type III injuries, type IV injuries involve a bony avulsion; however, the FDP subsequently ruptures from this fragment and the tendon subsequently retracts into the finger or palm.2,3 Type V injuries are more complex than other injury types because they involve a concomitant distal phalanx fracture with the FDP avulsion.4 Al-Qattan5 subclassified type V injuries into extra-articular (type Va) and intra-articular (type Vb) distal phalanx fractures on the basis of the distinct management of these 2 entities.
Numerous techniques have been proposed and described for the repair of FDP avulsion injuries. The pullout suture-dorsal button combination is the most widely described technique and was initially described by Bunnell.6 Unfortunately, this technique is accompanied by numerous potential postoperative complications.6 Nail plate deformity is the most commonly described complication. Other complications include local wound irritation, pain, button snagging, and repair failure. Additionally, the presence of external sutures creates a potential route of ingress for bacterial infection.
Continue to: Bone suture anchor techniques...
Bone suture anchor techniques were later utilized to repair FDP avulsions in an attempt to decrease complications associated with the external suture-button construct.7 The use of a transosseous suture without external button fixation has also been proposed. Sood and Elliot8 described a technique where the suture is passed through a hole, drilled transversely through the tuft of the distal phalanx, and affixed to the other limb. In 1999, Schultz and colleagues9 described a technique where transosseous tunnels are placed in the distal phalanx in a dorsal-to-volar direction. The suture is then passed through and tied on the dorsal surface. In this article, we propose a transosseous suture technique that may provide advantages over previously described methods.
SURGICAL TECHNIQUE
TYPES I, II, AND III
A Bruner incision is performed on the volar aspect of the affected finger, and full thickness flaps are elevated off the flexor sheath (Figures 1A-1C).
TYPES IV AND V
In cases of type IV or V injury (Figure 4A), a screw or plate construct is first used to allow for the successful reduction and fixation of the fracture (Figure 4B).
DISCUSSION
The avulsion of the FDP tendon from its insertion (zone I) on the distal phalanx is commonly called “jersey finger” and is a well-described injury that occurs most commonly in the ring finger.10 These injuries can be difficult to treat and are associated with a complication rate of as high as 60%.11,12 Bunnell’s initial description of a suture passed through the fingernail and then tied over a polypropylene button has been associated with multiple complications. Kang and colleagues13 reported abnormal nail growth, nail fold necrosis, fingertip deformity, stiffness, infection, and amputation, 43% of all complications were directly related to the button. As an alternative to the button, sutures may be tied directly over the nail plate itself via 2 separate holes.14 While this technique eliminates the complications directly associated with the button, the potential for infection remains. Additionally, increased direct pressure is placed on the nail plate and nail bed, thus potentially increasing the risk of nail deformity.
In 1994, Hallock7 initially described the use of bone anchors as an “internal fixation” alternative and cited the “expense of the apparatus” as the major drawback of this technique. McCallister and colleagues15 compared the clinical outcome of suture anchor fixation with that of the button-over-nail technique. Although they ultimately demonstrated that the clinical outcomes of the 2 techniques are not significantly different, they noted that suture anchor fixation is associated with decreased infection rate (7% vs 0%) and time to return to work. Poor bone mineral density and low cortical thickness are correlated with anchor pull-out, thus limiting its universal use.16 Furthermore, the universal use of many commonly available anchors is limited given that they are too large to be accommodated within many phalanges, particularly in women and in the small and ring fingers.17 The use of microanchors rather than mini anchors not only decreases this risk but also decreases construct strength, thus necessitating the use of 2 anchors to restore adequate fixation strength. Anchor use is associated with specific risks, including the dorsal migration of the anchor, the osteolysis of the surrounding bone, as well as the perforation of the dorsal cortex and the possible extrusion of the anchor through the phalanx and into the nail bed.18,19 Additionally, in the wake of a changing healthcare system, the cost of suture anchors, as initially noted by Hallock,7 must be considered. This consideration is particularly relevant to the use of a 2 microanchor construct, which has been advocated given its biomechanical advantage.20,21
Continue to: Transosseous tendon repair...
Transosseous tendon repair is a cost-effective option that obviates many complications commonly observed with other fixation methods. By keeping the suture within the body, the complications inherent in external sutures and buttons are eliminated, including the loss of fixation as a result of button or suture damage and facilitating hand hygiene maintenance. The rate of infection is also reduced. Moreover, the risk of nail deformities is decreased because the suture is not passed through the nail bed and nail plate in the described technique. Occasionally, some patients do note irritation from the dorsal suture knot under the thin skin proximal to the germinal matrix. This can be easily addressed in the clinic by removing the knot under local anesthesia following sufficient tendon healing. Additionally, the described technique can be used safely in pediatric patients with open physes because the needles can be placed to prevent violating the physis. This technique can be performed in conjunction with the skeletal fixation of type III, IV, and V jersey fingers. In our experience, the transosseous suture repair is more secure than the limited screw fixation, which can be accomplished in many type III jersey fingers, and in at least 1 case, has maintained flexor function when the skeletal fixation of the jersey finger has failed (Figures 5A, 5B).
All internal fixation techniques have been described previously by Sood and Elliot8 and, later, by Schultz and colleagues.9 In contrast to Sood and Elliott’s8 technique, which requires the creation of transverse tunnels, a volar-to-dorsal tunnel is technically easy to create and creates a direct repair to tendon insertion. Our technique is similar to that of Schultz and colleagues'9 but has the following differences and potential improvements:
- Keith needles are passed in a volar-to-dorsal fashion, thus allowing for the direct visualization of the transosseous tunnel origin, minimizing the size of the transosseous tunnels, and allowing for the anatomic reduction of the tendon.
- Fluoroscopy is used to confirm wire placement prior to skin incision, thus enabling precise placement and potentially allowing the needles to be placed so as to avoid physeal injury in pediatric jersey fingers.
- By using Keith needles, sutures can be passed with the same instrument that created the tunnel, thus simplifying surgical technique.
- A Krakow suture technique is used. This technique results in less gapping and higher load-to-failure than other suturing techniques.22
- A 2-0 braided suture is used, therefore strengthening repair.
This paper will be judged for the Resident Writer’s Award.
1. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2(1):66-69. doi:https://doi.org/10.1016/S0363-5023(77)80012-9.
2. Langa V, Posner MA. Unusual rupture of a flexor profundus tendon. J Hand Surg Am. 1986;11(2):227-229. doi:https://doi.org/10.1016/S0363-5023(86)80056-9.
3. Ehlert KJ, Gould JS, Black KP. A simultaneous distal phalanx avulsion fracture with profundus tendon avulsion: A case report and review of the literature. Clin Orthop Relat Res. 1992;(283):265-269.
4. Smith JH. Avulsion of a profundus tendon with simultaneous intraarticular fracture of the distal phalanx–case report. J Hand Surg Am. 1981;6(6):600-601. doi:10.1097/00006534-198305000-00081.
5. Al-Qattan MM. Type 5 avulsion of the insertion of the flexor digitorum profundus tendon. J Hand Surg Br. 2001;26(5):427-431. doi:10.1054/jhsb.2001.0619.
6. Bunnell S. Surgery of the hand, 2nd edition. Philadelphia, PA: JB Lippincott; 1948:381-466.
7. Hallock GG. The Mitek Mini GII anchor introduced for tendon reinsertion in the hand. Ann Plast Surg. 1994;33(2):211-213.
8. Sood MK, Elliot D. A new technique of attachment of flexor tendons to the distal phalanx without a button tie-over. J Hand Surg Br. 1996;21(5):629-632. doi:https://doi.org/10.1016/S0266-7681(96)80146-X.
9. Schultz RO, Drake DB, Morgan RF. A new technique for the treatment of flexor digitorum profundus tendon avulsion. Ann Plast Surg. 1999;42(1):46-48. doi:10.1097/00000637-199901000-00008.
10. Manske PR, Lesker PA. Avulsion of the ring finger flexor digitorum profundus tendon: An experimental study. Hand 1978;10(1):52-55. doi:https://doi.org/10.1016/S0072-968X(78)80025-4.
11. Gerbino PG, Saldana MJ, Westerbeck P, Schacherer TG. Complications experienced in the rehabilitation of zone I flexor tendon injuries with dynamic traction splinting. J Hand Surg Am. 1991;16(4):680-686. doi:https://doi.org/10.1016/0363-5023(91)90194-G
12. Evans RB. Zone I flexor tendon rehabilitation with limited extension and active flexion. J Hand Ther. 2005;18(2):128-140. doi:10.1197/j.jht.2005.02.001
13. Kang N, Marsh D, Dewar D. The morbidity of the button-over-nail technique for zone 1 flexor tendon repairs. Should we still be using this technique? J Hand Surg Eur Vol. 2008;33(5):566-570. doi:10.1177/1753193408090118
14. Taras JS. Flexor tendon reconstruction: Single stage flexor tendon grafting: FDP, FDS disrupted. In: Green DP, Hotchkiss RN, Pederson WL, Wolfe SW, eds. Green’s Operative Hand Surgery. 5th ed. Philadelphia, PA: Elsevier Health Sciences; 2005:248-249.
15. McCallister WV, Ambrose HC, Katolik LI, Trumble TE. Comparison of pullout button versus suture anchor for zone I flexor tendon repair. J Hand Surg Am. 2006;31:246-251. doi:10.1016/j.jhsa.2005.10.020
16. Matzsuzaki H, Zaegel MA, Gelberman RH, Silva MJ. Effect of suture material and bone quality on the mechanical properties of zone 1 flexor tendon-bone reattachment with bone anchors. J Hand Surg Am. 2008;33(5):709-717. doi:10.1016/j.jhsa.2008.01.025
17. Singh R, Kakarala G, Persaud I, Roberts M, Strandring S, Compson J. The optimal length of tissue anchors for distal phalanges. A study in 395 cadaver digits. J Bone Joint Surg Br. 2006;88-B(SUPP I):37.
18. Giannikas D, Athanaselis E, Matzaroglou C, Saridis A, Tyllianakis M. An unusual complication of Mitek suture anchor use in primary treatment of flexor digitorum profundus tendon laceration: a case report. Cases J. 2009;2:9319. doi:10.1186/1757-1626-2-9319
19. Tiong WH, O'Sullivan ST. Extrusion of bone anchor suture following flexor digitorum profundus tendon avulsion injury repair. J Plast Reconstr Aesthet Surg. 2011;64(9):1242-1244. doi:10.1016/j.bjps.2011.01.016
20. Silva MJ, Hollstien SB, Brodt MD, Boyer MI, Tetro AM, Gelberman RH. Flexor digitorum profundus tendon-to-bone repair: An ex vivo biomechanical analysis of 3 pullout suture techniques. J Hand Surg Am. 1998;23(1):120-126. doi:10.1016/S0363-5023(98)80099-3
21. Latendresse K, Dona E, Scougall PJ, Schreuder FB, Puchert E, Walsh WR. Cyclic testing of pullout sutures and micro-mitek suture anchors in flexor digitorum profundus tendon distal fixation. J Hand Surg Am. 2005;30(3):471-478. doi:10.1016/j.jhsa.2004.10.014
22. Lee SK, Fajardo M, Kardashian G, Klein J, Tsai P, Christoforou D. Repair of flexor digitorum profundus to distal phalanx: a biomechanical evaluation of four techniques. J Hand Surg Am. 2011;36(10):1604-1609. doi:10.1016/j.jhsa.2011.07.017
1. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2(1):66-69. doi:https://doi.org/10.1016/S0363-5023(77)80012-9.
2. Langa V, Posner MA. Unusual rupture of a flexor profundus tendon. J Hand Surg Am. 1986;11(2):227-229. doi:https://doi.org/10.1016/S0363-5023(86)80056-9.
3. Ehlert KJ, Gould JS, Black KP. A simultaneous distal phalanx avulsion fracture with profundus tendon avulsion: A case report and review of the literature. Clin Orthop Relat Res. 1992;(283):265-269.
4. Smith JH. Avulsion of a profundus tendon with simultaneous intraarticular fracture of the distal phalanx–case report. J Hand Surg Am. 1981;6(6):600-601. doi:10.1097/00006534-198305000-00081.
5. Al-Qattan MM. Type 5 avulsion of the insertion of the flexor digitorum profundus tendon. J Hand Surg Br. 2001;26(5):427-431. doi:10.1054/jhsb.2001.0619.
6. Bunnell S. Surgery of the hand, 2nd edition. Philadelphia, PA: JB Lippincott; 1948:381-466.
7. Hallock GG. The Mitek Mini GII anchor introduced for tendon reinsertion in the hand. Ann Plast Surg. 1994;33(2):211-213.
8. Sood MK, Elliot D. A new technique of attachment of flexor tendons to the distal phalanx without a button tie-over. J Hand Surg Br. 1996;21(5):629-632. doi:https://doi.org/10.1016/S0266-7681(96)80146-X.
9. Schultz RO, Drake DB, Morgan RF. A new technique for the treatment of flexor digitorum profundus tendon avulsion. Ann Plast Surg. 1999;42(1):46-48. doi:10.1097/00000637-199901000-00008.
10. Manske PR, Lesker PA. Avulsion of the ring finger flexor digitorum profundus tendon: An experimental study. Hand 1978;10(1):52-55. doi:https://doi.org/10.1016/S0072-968X(78)80025-4.
11. Gerbino PG, Saldana MJ, Westerbeck P, Schacherer TG. Complications experienced in the rehabilitation of zone I flexor tendon injuries with dynamic traction splinting. J Hand Surg Am. 1991;16(4):680-686. doi:https://doi.org/10.1016/0363-5023(91)90194-G
12. Evans RB. Zone I flexor tendon rehabilitation with limited extension and active flexion. J Hand Ther. 2005;18(2):128-140. doi:10.1197/j.jht.2005.02.001
13. Kang N, Marsh D, Dewar D. The morbidity of the button-over-nail technique for zone 1 flexor tendon repairs. Should we still be using this technique? J Hand Surg Eur Vol. 2008;33(5):566-570. doi:10.1177/1753193408090118
14. Taras JS. Flexor tendon reconstruction: Single stage flexor tendon grafting: FDP, FDS disrupted. In: Green DP, Hotchkiss RN, Pederson WL, Wolfe SW, eds. Green’s Operative Hand Surgery. 5th ed. Philadelphia, PA: Elsevier Health Sciences; 2005:248-249.
15. McCallister WV, Ambrose HC, Katolik LI, Trumble TE. Comparison of pullout button versus suture anchor for zone I flexor tendon repair. J Hand Surg Am. 2006;31:246-251. doi:10.1016/j.jhsa.2005.10.020
16. Matzsuzaki H, Zaegel MA, Gelberman RH, Silva MJ. Effect of suture material and bone quality on the mechanical properties of zone 1 flexor tendon-bone reattachment with bone anchors. J Hand Surg Am. 2008;33(5):709-717. doi:10.1016/j.jhsa.2008.01.025
17. Singh R, Kakarala G, Persaud I, Roberts M, Strandring S, Compson J. The optimal length of tissue anchors for distal phalanges. A study in 395 cadaver digits. J Bone Joint Surg Br. 2006;88-B(SUPP I):37.
18. Giannikas D, Athanaselis E, Matzaroglou C, Saridis A, Tyllianakis M. An unusual complication of Mitek suture anchor use in primary treatment of flexor digitorum profundus tendon laceration: a case report. Cases J. 2009;2:9319. doi:10.1186/1757-1626-2-9319
19. Tiong WH, O'Sullivan ST. Extrusion of bone anchor suture following flexor digitorum profundus tendon avulsion injury repair. J Plast Reconstr Aesthet Surg. 2011;64(9):1242-1244. doi:10.1016/j.bjps.2011.01.016
20. Silva MJ, Hollstien SB, Brodt MD, Boyer MI, Tetro AM, Gelberman RH. Flexor digitorum profundus tendon-to-bone repair: An ex vivo biomechanical analysis of 3 pullout suture techniques. J Hand Surg Am. 1998;23(1):120-126. doi:10.1016/S0363-5023(98)80099-3
21. Latendresse K, Dona E, Scougall PJ, Schreuder FB, Puchert E, Walsh WR. Cyclic testing of pullout sutures and micro-mitek suture anchors in flexor digitorum profundus tendon distal fixation. J Hand Surg Am. 2005;30(3):471-478. doi:10.1016/j.jhsa.2004.10.014
22. Lee SK, Fajardo M, Kardashian G, Klein J, Tsai P, Christoforou D. Repair of flexor digitorum profundus to distal phalanx: a biomechanical evaluation of four techniques. J Hand Surg Am. 2011;36(10):1604-1609. doi:10.1016/j.jhsa.2011.07.017
TAKE-HOME POINTS
- Transosseous repair of FDP has been long utilized, tying the sutures over a polyethylene button at the nail plate, which is associated with significant complications.
- Avoiding use of a button decreases these complications, eliminating damage to the nailbed and eliminating external sutures, thus decreasing infection risk.
- Keith needles can be utilized to pass the sutures from volar to dorsal, and can be inserted using a wire drive; their position can be checked fluoroscopically prior to suture passage.
- This technique can be used in conjunction with skeletal fixation of associated fractures.
- This technique can be utilized in pediatric patients, placing the sutures distal to the physis.
What is cell phone elbow, and what should we tell our patients?
With prolonged cellular telephone use, people may note the onset of aching, burning, numbness, or tingling in the ulnar forearm and hand. This constellation of symptoms, termed “cell phone elbow” by the lay press, is known medically as cubital tunnel syndrome—the second most common nerve compression syndrome in the upper extremities after carpal tunnel syndrome.
In most cases, treatment consists simply of modifying the activity and avoiding activities that aggravate the symptoms. Switching hands frequently while talking on the phone or using a hands-free headset can help. Other daily activities that produce cubital tunnel syndrome include leaning on an elbow while driving or working, and sitting at a computer workstation that requires elbow flexion greater than 90 degrees. Making ergonomic adjustments to these activities is beneficial.
For patients who have nocturnal symptoms, a simple elbow pad worn anteriorly or a towel wrapped around the elbow to prevent flexion while sleeping can be very efficacious. Occasionally, anti-inflammatory injections can be given to quiet an inflamed ulnar nerve and reduce symptoms.1 Surgical interventions, discussed below, are available for patients with severe, persistent symptoms.
WHAT IS CUBITAL TUNNEL SYNDROME?
Cellular telephone use has increased exponentially, with 3.3 billion service contracts active worldwide—or about one for every two people on the planet. The exact incidence of cell phone elbow is not known, but anecdotal reports and our own clinical experience indicate that its incidence parallels the rise in the use of cell phones and computer workstations.
Cubital tunnel syndrome is caused by compression of the ulnar nerve as it traverses the posterior elbow, wrapping around the medial condyle of the humerus. When people hold their elbow flexed for a prolonged period, such as when speaking on the phone or sleeping at night, the ulnar nerve is placed in tension; the nerve itself can elongate 4.5 to 8 mm with elbow flexion.2 Additionally, flexion of the elbow narrows the space available for the nerve2 and can cause a sevenfold to 20-fold increase in the pressure within the cubital tunnel, depending on muscle contraction.3 This can be compounded by compression on the nerve, either from various fascial bands surrounding the nerve or from extrinsic sources of compression, such as leaning on one’s elbow while driving or talking. This increased pressure on the nerve leads to decreased blood flow and nerve ischemia; this in turn causes increased permeability of the epineurial vessels and nerve edema, enlarging the nerve and continuing the cycle. Less frequently, cubital tunnel symptoms can be caused by the ulnar nerve subluxing in and out of its groove in the posterior elbow, leading to nerve inflammation and swelling from the repetitive friction.
THE CLINICAL PRESENTATION
The clinical picture of cubital tunnel syndrome consists of numbness or paresthesias in the small and ring fingers. Dorsal ulnar hand numbness, which is not present if the ulnar nerve is compressed at Guyon’s canal, helps the clinician differentiate cubital tunnel nerve compression from distal ulnar nerve compression.
If ulnar nerve compression persists, symptoms may progress to hand fatigue and weakness, including difficulty opening bottles or jars. Chronic and severe compression may lead to permanent motor deficits, including an inability to adduct the small finger (Wartenberg sign) and severe clawing of the ring and small fingers (a hand posture of metacarpophalangeal extension and flexion of the proximal and distal interphalangeal joints due to dysfunction of the ulnar-innervated intrinsic hand musculature). Patients may be unable to grasp things in a key-pinch grip, using a fingertip grip instead (Froment sign).
THE DIAGNOSIS IS USUALLY CLINICAL
The diagnosis of cubital tunnel syndrome is first and foremost a clinical one based on a thorough history, including symptoms, duration, and aggravating activities and factors.
The physical examination should include evaluation of sensibility of the hand, including the Semmes-Weinstein monofilament test and vibratory perception test, which will be affected before the Weber two-point discrimination test. Sensibility of the entire hand should be assessed to differentiate focal ulnar deficits from more widespread peripheral neuropathies.
Motor function can be evaluated by asking the patient to hold the fingers abducted, testing key-pinch grip, or asking the patient to cross the middle finger over the index finger. This crossed-finger test is quite reliable, as it is difficult to “fake out” with other muscles.4
The examination should also evaluate the cervical spine and vascularity. Provocative maneuvers can be performed to elicit symptoms, including the Hoffman-Tinel test (tapping the ulnar nerve in its groove at the posterior medial elbow, eliciting electric shocks or tingling radiating into the small finger). The equivalent of the Phalen maneuver for carpal tunnel syndrome can be performed by having the patient sit with the elbow fully flexed for 30 seconds to see if symptoms are reproduced; this may be positive in 10% of normal individuals. 5 One can combine elbow flexion with compression over the proximal ulnar nerve; this maneuver has good sensitivity and specificity. 6 Early in the disease, these provocative maneuvers may be the only examination findings, since sensation and motor function are usually normal.
Ruling out other entities that can cause numbness in the distribution of the medial hand and forearm is also important. These entities include cervical spine conditions such as herniated disk impinging on the C8 nerve root, or a space-occupying lesion of the cervical spine such as a tumor or syrinx.
The neck should be examined for loss of motion. Also, a Spurling test of the cervical spine checks for foraminal nerve impingement: with the patient seated, the clinician extends the patient’s neck and rotates it toward the involved side, then presses down on the top of the patient’s head and asks if this reproduces or worsens the symptoms in the patient’s arm. Hyperreflexia of the upper extremities or the presence of a Hoffman sign should alert the clinician to a more central process. In unclear cases or in patients with known cervical disease, electromyography should be able to differentiate ulnar neuropathy from a C8 nerveroot impingement or confirm the presence of both conditions (a so-called “double crush” phenomenon).
Other less common entities that can present with hand tingling include an apical lung tumor compressing the lower brachial plexus, thoracic outlet syndrome, or peripheral neuropathy (diabetes, vitamin B12 deficiency, hypothyroidism, alcoholism). Other conditions that can cause medial-sided elbow pain include elbow instability or medial epicondylitis (golfer’s elbow); however, these are not associated with numbness or tingling by themselves.
DIAGNOSTIC TESTS
Advanced diagnostic studies may help in certain cases, although they are not essential if the diagnosis is obvious on clinical examination.
Imaging studies may include plain radiography to look for osteophytes or bone fragments, which may impinge on the ulnar nerve, particularly in an arthritic or previously traumatized elbow. Magnetic resonance imaging is only indicated if a space-occupying lesion is suspected. Electrodiagnostic studies may help when findings are equivocal, when the site of compression is unclear, or when coexisting conditions such as diabetes or cervical spine disease make the diagnosis unclear. Nerve conduction studies may be unreliable early in cubital tunnel syndrome, as nondiseased nerve fibers may be tested, creating a false-negative result. Performing the study with the patient’s elbow flexed may increase the sensitivity of the test. Electromyography generally does not become positive until later in the disease, when more profound changes have occurred.
TREATMENT OF CELL PHONE ELBOW
As mentioned, changing how one uses a cell phone often helps, as does avoiding activities that require the elbow to remain flexed more than 90 degrees for extended periods. But when nonoperative means fail to reduce symptoms, surgery may be warranted.
Operative interventions include simple decompression or transposing the nerve from its usual course around the posterior elbow to a path anterior to the elbow, thus decreasing the tension on the nerve. This can be done either subcutaneously or by embedding the nerve in or under the muscles of the forearm.
In patients with coexisting medial epicondylitis or a subluxing nerve, the medial epicondyle can be excised. Techniques for minimally invasive or endoscopic ulnar nerve decompression have been recently introduced, but the long-term results with these are not yet known.
Overall, treatment for persistent paresthesias is successful even when patients present late, but those who present early have a better chance of full sensory and motor recovery.
- Pechan J, Kredba J. Treatment of cubital tunnel syndrome by means of local administration of cortisonoids. Acta Univ Carol [Med] (Praha) 1980; 26:125–133.
- Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg 1973; 51:79–81.
- Werner CO, Ohlin P, Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand 1985; 56:404–406.
- Earle AS, Vlastou C. Crossed fingers and other tests of ulnar nerve motor function. J Hand Surg [Am] 1980; 5:560–565.
- Rayann GM, Jensen C, Duke J. Elbow flexion test in the normal population. J Hand Surg [Am] 1992; 17:86–89.
- Novak CB, Lee GW, Mackinnon SE, Lay L. Provocative testing for cubital tunnel syndrome. J Hand Surg [Am] 1994; 19:817–820.
With prolonged cellular telephone use, people may note the onset of aching, burning, numbness, or tingling in the ulnar forearm and hand. This constellation of symptoms, termed “cell phone elbow” by the lay press, is known medically as cubital tunnel syndrome—the second most common nerve compression syndrome in the upper extremities after carpal tunnel syndrome.
In most cases, treatment consists simply of modifying the activity and avoiding activities that aggravate the symptoms. Switching hands frequently while talking on the phone or using a hands-free headset can help. Other daily activities that produce cubital tunnel syndrome include leaning on an elbow while driving or working, and sitting at a computer workstation that requires elbow flexion greater than 90 degrees. Making ergonomic adjustments to these activities is beneficial.
For patients who have nocturnal symptoms, a simple elbow pad worn anteriorly or a towel wrapped around the elbow to prevent flexion while sleeping can be very efficacious. Occasionally, anti-inflammatory injections can be given to quiet an inflamed ulnar nerve and reduce symptoms.1 Surgical interventions, discussed below, are available for patients with severe, persistent symptoms.
WHAT IS CUBITAL TUNNEL SYNDROME?
Cellular telephone use has increased exponentially, with 3.3 billion service contracts active worldwide—or about one for every two people on the planet. The exact incidence of cell phone elbow is not known, but anecdotal reports and our own clinical experience indicate that its incidence parallels the rise in the use of cell phones and computer workstations.
Cubital tunnel syndrome is caused by compression of the ulnar nerve as it traverses the posterior elbow, wrapping around the medial condyle of the humerus. When people hold their elbow flexed for a prolonged period, such as when speaking on the phone or sleeping at night, the ulnar nerve is placed in tension; the nerve itself can elongate 4.5 to 8 mm with elbow flexion.2 Additionally, flexion of the elbow narrows the space available for the nerve2 and can cause a sevenfold to 20-fold increase in the pressure within the cubital tunnel, depending on muscle contraction.3 This can be compounded by compression on the nerve, either from various fascial bands surrounding the nerve or from extrinsic sources of compression, such as leaning on one’s elbow while driving or talking. This increased pressure on the nerve leads to decreased blood flow and nerve ischemia; this in turn causes increased permeability of the epineurial vessels and nerve edema, enlarging the nerve and continuing the cycle. Less frequently, cubital tunnel symptoms can be caused by the ulnar nerve subluxing in and out of its groove in the posterior elbow, leading to nerve inflammation and swelling from the repetitive friction.
THE CLINICAL PRESENTATION
The clinical picture of cubital tunnel syndrome consists of numbness or paresthesias in the small and ring fingers. Dorsal ulnar hand numbness, which is not present if the ulnar nerve is compressed at Guyon’s canal, helps the clinician differentiate cubital tunnel nerve compression from distal ulnar nerve compression.
If ulnar nerve compression persists, symptoms may progress to hand fatigue and weakness, including difficulty opening bottles or jars. Chronic and severe compression may lead to permanent motor deficits, including an inability to adduct the small finger (Wartenberg sign) and severe clawing of the ring and small fingers (a hand posture of metacarpophalangeal extension and flexion of the proximal and distal interphalangeal joints due to dysfunction of the ulnar-innervated intrinsic hand musculature). Patients may be unable to grasp things in a key-pinch grip, using a fingertip grip instead (Froment sign).
THE DIAGNOSIS IS USUALLY CLINICAL
The diagnosis of cubital tunnel syndrome is first and foremost a clinical one based on a thorough history, including symptoms, duration, and aggravating activities and factors.
The physical examination should include evaluation of sensibility of the hand, including the Semmes-Weinstein monofilament test and vibratory perception test, which will be affected before the Weber two-point discrimination test. Sensibility of the entire hand should be assessed to differentiate focal ulnar deficits from more widespread peripheral neuropathies.
Motor function can be evaluated by asking the patient to hold the fingers abducted, testing key-pinch grip, or asking the patient to cross the middle finger over the index finger. This crossed-finger test is quite reliable, as it is difficult to “fake out” with other muscles.4
The examination should also evaluate the cervical spine and vascularity. Provocative maneuvers can be performed to elicit symptoms, including the Hoffman-Tinel test (tapping the ulnar nerve in its groove at the posterior medial elbow, eliciting electric shocks or tingling radiating into the small finger). The equivalent of the Phalen maneuver for carpal tunnel syndrome can be performed by having the patient sit with the elbow fully flexed for 30 seconds to see if symptoms are reproduced; this may be positive in 10% of normal individuals. 5 One can combine elbow flexion with compression over the proximal ulnar nerve; this maneuver has good sensitivity and specificity. 6 Early in the disease, these provocative maneuvers may be the only examination findings, since sensation and motor function are usually normal.
Ruling out other entities that can cause numbness in the distribution of the medial hand and forearm is also important. These entities include cervical spine conditions such as herniated disk impinging on the C8 nerve root, or a space-occupying lesion of the cervical spine such as a tumor or syrinx.
The neck should be examined for loss of motion. Also, a Spurling test of the cervical spine checks for foraminal nerve impingement: with the patient seated, the clinician extends the patient’s neck and rotates it toward the involved side, then presses down on the top of the patient’s head and asks if this reproduces or worsens the symptoms in the patient’s arm. Hyperreflexia of the upper extremities or the presence of a Hoffman sign should alert the clinician to a more central process. In unclear cases or in patients with known cervical disease, electromyography should be able to differentiate ulnar neuropathy from a C8 nerveroot impingement or confirm the presence of both conditions (a so-called “double crush” phenomenon).
Other less common entities that can present with hand tingling include an apical lung tumor compressing the lower brachial plexus, thoracic outlet syndrome, or peripheral neuropathy (diabetes, vitamin B12 deficiency, hypothyroidism, alcoholism). Other conditions that can cause medial-sided elbow pain include elbow instability or medial epicondylitis (golfer’s elbow); however, these are not associated with numbness or tingling by themselves.
DIAGNOSTIC TESTS
Advanced diagnostic studies may help in certain cases, although they are not essential if the diagnosis is obvious on clinical examination.
Imaging studies may include plain radiography to look for osteophytes or bone fragments, which may impinge on the ulnar nerve, particularly in an arthritic or previously traumatized elbow. Magnetic resonance imaging is only indicated if a space-occupying lesion is suspected. Electrodiagnostic studies may help when findings are equivocal, when the site of compression is unclear, or when coexisting conditions such as diabetes or cervical spine disease make the diagnosis unclear. Nerve conduction studies may be unreliable early in cubital tunnel syndrome, as nondiseased nerve fibers may be tested, creating a false-negative result. Performing the study with the patient’s elbow flexed may increase the sensitivity of the test. Electromyography generally does not become positive until later in the disease, when more profound changes have occurred.
TREATMENT OF CELL PHONE ELBOW
As mentioned, changing how one uses a cell phone often helps, as does avoiding activities that require the elbow to remain flexed more than 90 degrees for extended periods. But when nonoperative means fail to reduce symptoms, surgery may be warranted.
Operative interventions include simple decompression or transposing the nerve from its usual course around the posterior elbow to a path anterior to the elbow, thus decreasing the tension on the nerve. This can be done either subcutaneously or by embedding the nerve in or under the muscles of the forearm.
In patients with coexisting medial epicondylitis or a subluxing nerve, the medial epicondyle can be excised. Techniques for minimally invasive or endoscopic ulnar nerve decompression have been recently introduced, but the long-term results with these are not yet known.
Overall, treatment for persistent paresthesias is successful even when patients present late, but those who present early have a better chance of full sensory and motor recovery.
With prolonged cellular telephone use, people may note the onset of aching, burning, numbness, or tingling in the ulnar forearm and hand. This constellation of symptoms, termed “cell phone elbow” by the lay press, is known medically as cubital tunnel syndrome—the second most common nerve compression syndrome in the upper extremities after carpal tunnel syndrome.
In most cases, treatment consists simply of modifying the activity and avoiding activities that aggravate the symptoms. Switching hands frequently while talking on the phone or using a hands-free headset can help. Other daily activities that produce cubital tunnel syndrome include leaning on an elbow while driving or working, and sitting at a computer workstation that requires elbow flexion greater than 90 degrees. Making ergonomic adjustments to these activities is beneficial.
For patients who have nocturnal symptoms, a simple elbow pad worn anteriorly or a towel wrapped around the elbow to prevent flexion while sleeping can be very efficacious. Occasionally, anti-inflammatory injections can be given to quiet an inflamed ulnar nerve and reduce symptoms.1 Surgical interventions, discussed below, are available for patients with severe, persistent symptoms.
WHAT IS CUBITAL TUNNEL SYNDROME?
Cellular telephone use has increased exponentially, with 3.3 billion service contracts active worldwide—or about one for every two people on the planet. The exact incidence of cell phone elbow is not known, but anecdotal reports and our own clinical experience indicate that its incidence parallels the rise in the use of cell phones and computer workstations.
Cubital tunnel syndrome is caused by compression of the ulnar nerve as it traverses the posterior elbow, wrapping around the medial condyle of the humerus. When people hold their elbow flexed for a prolonged period, such as when speaking on the phone or sleeping at night, the ulnar nerve is placed in tension; the nerve itself can elongate 4.5 to 8 mm with elbow flexion.2 Additionally, flexion of the elbow narrows the space available for the nerve2 and can cause a sevenfold to 20-fold increase in the pressure within the cubital tunnel, depending on muscle contraction.3 This can be compounded by compression on the nerve, either from various fascial bands surrounding the nerve or from extrinsic sources of compression, such as leaning on one’s elbow while driving or talking. This increased pressure on the nerve leads to decreased blood flow and nerve ischemia; this in turn causes increased permeability of the epineurial vessels and nerve edema, enlarging the nerve and continuing the cycle. Less frequently, cubital tunnel symptoms can be caused by the ulnar nerve subluxing in and out of its groove in the posterior elbow, leading to nerve inflammation and swelling from the repetitive friction.
THE CLINICAL PRESENTATION
The clinical picture of cubital tunnel syndrome consists of numbness or paresthesias in the small and ring fingers. Dorsal ulnar hand numbness, which is not present if the ulnar nerve is compressed at Guyon’s canal, helps the clinician differentiate cubital tunnel nerve compression from distal ulnar nerve compression.
If ulnar nerve compression persists, symptoms may progress to hand fatigue and weakness, including difficulty opening bottles or jars. Chronic and severe compression may lead to permanent motor deficits, including an inability to adduct the small finger (Wartenberg sign) and severe clawing of the ring and small fingers (a hand posture of metacarpophalangeal extension and flexion of the proximal and distal interphalangeal joints due to dysfunction of the ulnar-innervated intrinsic hand musculature). Patients may be unable to grasp things in a key-pinch grip, using a fingertip grip instead (Froment sign).
THE DIAGNOSIS IS USUALLY CLINICAL
The diagnosis of cubital tunnel syndrome is first and foremost a clinical one based on a thorough history, including symptoms, duration, and aggravating activities and factors.
The physical examination should include evaluation of sensibility of the hand, including the Semmes-Weinstein monofilament test and vibratory perception test, which will be affected before the Weber two-point discrimination test. Sensibility of the entire hand should be assessed to differentiate focal ulnar deficits from more widespread peripheral neuropathies.
Motor function can be evaluated by asking the patient to hold the fingers abducted, testing key-pinch grip, or asking the patient to cross the middle finger over the index finger. This crossed-finger test is quite reliable, as it is difficult to “fake out” with other muscles.4
The examination should also evaluate the cervical spine and vascularity. Provocative maneuvers can be performed to elicit symptoms, including the Hoffman-Tinel test (tapping the ulnar nerve in its groove at the posterior medial elbow, eliciting electric shocks or tingling radiating into the small finger). The equivalent of the Phalen maneuver for carpal tunnel syndrome can be performed by having the patient sit with the elbow fully flexed for 30 seconds to see if symptoms are reproduced; this may be positive in 10% of normal individuals. 5 One can combine elbow flexion with compression over the proximal ulnar nerve; this maneuver has good sensitivity and specificity. 6 Early in the disease, these provocative maneuvers may be the only examination findings, since sensation and motor function are usually normal.
Ruling out other entities that can cause numbness in the distribution of the medial hand and forearm is also important. These entities include cervical spine conditions such as herniated disk impinging on the C8 nerve root, or a space-occupying lesion of the cervical spine such as a tumor or syrinx.
The neck should be examined for loss of motion. Also, a Spurling test of the cervical spine checks for foraminal nerve impingement: with the patient seated, the clinician extends the patient’s neck and rotates it toward the involved side, then presses down on the top of the patient’s head and asks if this reproduces or worsens the symptoms in the patient’s arm. Hyperreflexia of the upper extremities or the presence of a Hoffman sign should alert the clinician to a more central process. In unclear cases or in patients with known cervical disease, electromyography should be able to differentiate ulnar neuropathy from a C8 nerveroot impingement or confirm the presence of both conditions (a so-called “double crush” phenomenon).
Other less common entities that can present with hand tingling include an apical lung tumor compressing the lower brachial plexus, thoracic outlet syndrome, or peripheral neuropathy (diabetes, vitamin B12 deficiency, hypothyroidism, alcoholism). Other conditions that can cause medial-sided elbow pain include elbow instability or medial epicondylitis (golfer’s elbow); however, these are not associated with numbness or tingling by themselves.
DIAGNOSTIC TESTS
Advanced diagnostic studies may help in certain cases, although they are not essential if the diagnosis is obvious on clinical examination.
Imaging studies may include plain radiography to look for osteophytes or bone fragments, which may impinge on the ulnar nerve, particularly in an arthritic or previously traumatized elbow. Magnetic resonance imaging is only indicated if a space-occupying lesion is suspected. Electrodiagnostic studies may help when findings are equivocal, when the site of compression is unclear, or when coexisting conditions such as diabetes or cervical spine disease make the diagnosis unclear. Nerve conduction studies may be unreliable early in cubital tunnel syndrome, as nondiseased nerve fibers may be tested, creating a false-negative result. Performing the study with the patient’s elbow flexed may increase the sensitivity of the test. Electromyography generally does not become positive until later in the disease, when more profound changes have occurred.
TREATMENT OF CELL PHONE ELBOW
As mentioned, changing how one uses a cell phone often helps, as does avoiding activities that require the elbow to remain flexed more than 90 degrees for extended periods. But when nonoperative means fail to reduce symptoms, surgery may be warranted.
Operative interventions include simple decompression or transposing the nerve from its usual course around the posterior elbow to a path anterior to the elbow, thus decreasing the tension on the nerve. This can be done either subcutaneously or by embedding the nerve in or under the muscles of the forearm.
In patients with coexisting medial epicondylitis or a subluxing nerve, the medial epicondyle can be excised. Techniques for minimally invasive or endoscopic ulnar nerve decompression have been recently introduced, but the long-term results with these are not yet known.
Overall, treatment for persistent paresthesias is successful even when patients present late, but those who present early have a better chance of full sensory and motor recovery.
- Pechan J, Kredba J. Treatment of cubital tunnel syndrome by means of local administration of cortisonoids. Acta Univ Carol [Med] (Praha) 1980; 26:125–133.
- Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg 1973; 51:79–81.
- Werner CO, Ohlin P, Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand 1985; 56:404–406.
- Earle AS, Vlastou C. Crossed fingers and other tests of ulnar nerve motor function. J Hand Surg [Am] 1980; 5:560–565.
- Rayann GM, Jensen C, Duke J. Elbow flexion test in the normal population. J Hand Surg [Am] 1992; 17:86–89.
- Novak CB, Lee GW, Mackinnon SE, Lay L. Provocative testing for cubital tunnel syndrome. J Hand Surg [Am] 1994; 19:817–820.
- Pechan J, Kredba J. Treatment of cubital tunnel syndrome by means of local administration of cortisonoids. Acta Univ Carol [Med] (Praha) 1980; 26:125–133.
- Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg 1973; 51:79–81.
- Werner CO, Ohlin P, Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand 1985; 56:404–406.
- Earle AS, Vlastou C. Crossed fingers and other tests of ulnar nerve motor function. J Hand Surg [Am] 1980; 5:560–565.
- Rayann GM, Jensen C, Duke J. Elbow flexion test in the normal population. J Hand Surg [Am] 1992; 17:86–89.
- Novak CB, Lee GW, Mackinnon SE, Lay L. Provocative testing for cubital tunnel syndrome. J Hand Surg [Am] 1994; 19:817–820.