User login
The Use of Secure Messaging in Medical Specialty Care
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
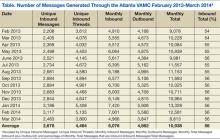
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Secure messaging (SM) is an encrypted, web-based mode of communication within the My HealtheVet (MHV) website. It was developed for the nonurgent, nonemergency communication of test results and other health information as well as for scheduling appointments and renewing medication prescriptions. Secure messaging is asynchronous, which means that communication between parties is not done at the same time. It was designed to address the need for a secure means of communication between patient and provider.1 Messages can be triaged across teams and saved to the Computerized Patient Record System (CPRS).
The VA patients who use MHV can upgrade their account through an in-person authentication process (IPA), which takes about 10 minutes. Any health care provider (HCP) team or administrator can use SM if set up in the system. Health care providers can only receive messages from patients who have been associated with their triage care group. Patients may only message an HCP with which they are associated. In general, this group would comprise their HCP and 1 or more specialty clinics where they have already been seen. Patients can choose an HCP from a limited drop-down menu.
Patients using SM choose a subject, such as appointments, medications, tests, or general. Patients are then able to type a message, and they are also able to see the threads of previous messages. They may access test results or attachments sent to them by the HCPs. Patients are notified of messages through their previously registered e-mail account, which displays a message asking them to log on to MHV.
Health care providers may access MHV either through the CPRS on the tools menu or as a link in an e-mail. Once HCPs log on, they will see their inbox and messages listed by sender and type of inquiry (ie, prescription refill, test question, and so forth). The HCPs can view escalated messages (those that have not been answered within 3 days), drafts, and sent and completed messages. Health care providers can also create special folders to store their messages.
The health care team can personalize how and to whom messages appear. There are 2 main models used by Specialty Care. The first involves a staff member designated to triage messages for the team. This staff member will see all incoming messages and forward them appropriately. For example, in one clinic model, the program assistant reviews all messages and then forwards them to the appropriate provider. The team pharmacist receives prescription requests, the HCP receives general or test inquiries from patients, and the program assistant retains and answers all communication related to appointments and cancellations. Another model involves employing a staff person or administrator as a co-user with each HCP. The HCP can then forward messages that may need administrative action.
The HCPs receive an e-mail notification with a link when a message has been received. Clicking on the link takes them directly to SM within MHV, where they can sign in to see all their messages. Users can also add a signature block, which will appear on all correspondence. They may also designate a surrogate to answer messages when they are unavailable, such as during administrative or personal leave. The HCPs also have the ability to create a SM even if the patient has not yet messaged them. Users can also send copies of messages to other staff members. Providers and staff have the ability to attach a file, which can be a test result, letter, records, etc. Messages can then be saved in the CPRS if desired.
Patients, however, cannot send attachments to their HCP. Only those HCPs who have seen the patient will be available for communication. This system eliminates the possibility of patients self-referring to a specialist and asking questions of HCPs who have never seen them. The HCPs and staff may also forward messages to the appropriate person.
Secure messaging can provide unique opportunities for communication and improvement in outcome measures in certain specialties. For example, in endocrinology patients may be asked to send home blood sugar or blood pressure (BP) readings in between visits, to allow for more rapid medication titration and achievement of treatment goals. A study by Harris and colleagues showed that the frequent use of electronic SM was associated with improved glycemic control.2
At the Atlanta VAMC, SM was implemented in the Primary Care Service Line prior to the Medicine Specialty Care Service Line. The implementation was a natural fit for the organized Primary Care teams. Implementation within the specialties brought forth a new set of issues. Many specialties were not formally organized with a team leader. There were often multiple HCPs in a division, some full time, some part time, in addition to subspecialty pharmacists, physician assistants, and nurse practitioners. Because the Atlanta VAMC is also a training hospital for the Emory University School of Medicine, new residents and fellows are included in the teams each month. It was, therefore, necessary for each specialty to design a message flow that would best fit its needs. Initially, there was concern that SM would add yet another layer of responsibilities to the already stretched HCPs.
The reality has been the opposite. Secure messaging was found to be an additional type of communication, which could be completed more rapidly than a phone call or generating a results letter. The HCPs were also concerned that patients would attempt to use them as primary care providers (PCPs). However, as patients were able to view both their PCP and their specialty care provider in the drop-down menu, they were generally able to direct their questions appropriately.
At the Atlanta VAMC, 60% of the messages were completed by the provider, 29% by a clinical team member, and 11% by the triage staff from 2013 to 2014 (Figure 1). Some HCPs were concerned that once SM was in place, they would be inundated with messages. The reality seems to be that most patients use SM judiciously, and although they are comfortable in the knowledge that they can communicate directly with their HCP, the need is infrequent. The number of messages has slowly increased over the past year as more patients join MHV and SM (Table). Surprisingly, as the number of inbound messages increased, the percentage of escalated messages (messages not answered within 3 days) declined, indicating a learning curve as HCPs begin using SM.
There are 3 steps to patient enrollment in SM. The first is enrollment in MHV, which can be done either online or at the VAMC. The second step requires the patient to go to the VAMC and present identification to complete the IPA. Finally, the enrolled patients must opt-in to the program. Enrollment in MHV has steadily increased through advertising campaigns on the VAMC website, within the VAMC, and through HCPs and staff (Figure 2).
However, barriers still exist. Some patients do not have an Internet connection and are not computer savvy. Other patients express interest but put it off to another visit. Some patients have been confused about the additional step of IPA that is required for SM and stop at enrollment in MHV only.
Therefore the key challenges for implementing SM are facilitating MHV enrollment, IPA, and completion of the opt-in feature. To encourage participation, VISN 7 mailed postcards to all 33,000 patients who had undergone IPA but had not yet opted-in. The number of patients who opted-in quadrupled, demonstrating that this type of promotion is an effective recruitment tool.
Another ongoing challenge is developing a method to easily generate workload credit for the HCPs’ time spent using SM for patient care. This will be an important parameter to track, as the time spent on SM per provider is expected to increase. It has also been suggested that there be an out-of-office response for nonemergent messages and the assignment of a surrogate to handle incoming messages for HCPs who are on leave. An unforeseen example of a nonemergent message occurs when a patient replies “Thank you” to a message from an HCP. That message is then counted as a new message and must be viewed and completed like any other message. It can also become an escalated message, even though there is no important information being transmitted.
Conclusions
Secure messaging provides a simple means of rapid communication and feedback between HCPs and their patients. An e-mail notification is generated, HCPs access SM through the link, the reply is sent, and a CPRS note is automatically generated. That same communication would require a far more time-consuming and complicated process without SM: The patient must contact the service, usually the program assistant, and leave a message; that message would be passed on via voicemail or e-mail to the appropriate HCP; the provider would need to access the CPRS, phone the patient, discuss the issue if the patient is available, and then document the contact with a note in the CPRS. If the patient was unavailable, this process would require multiple phone calls.
With respect to patients, the benefits of SM are significant and include easy access to prescription refills and a quick response to questions about medications, dosages, or tests. Patients are able to change or cancel appointments, thereby avoiding no-shows. Frustration concerning the inability to reach the correct party or to speak with staff directly is reduced with SM, and overall communication between HCP and patient is streamlined.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.
1. Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. New Engl J Med. 2004;350(17):1705-1707.
2. Harris LT, Haneuse SJ, Martin DP, Ralston JD. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: A cross-sectional analysis. Diabetes Care. 2009;32(7):1182-1187.