User login
Maternal mortality: Critical next steps in addressing the crisis
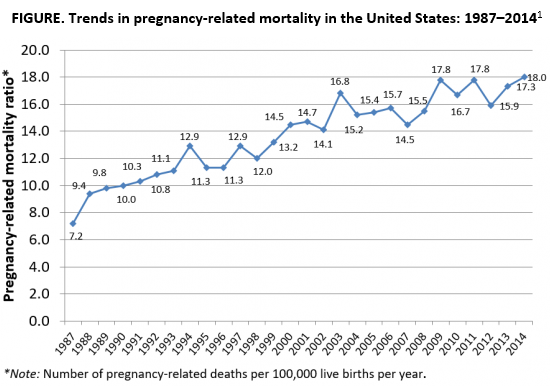
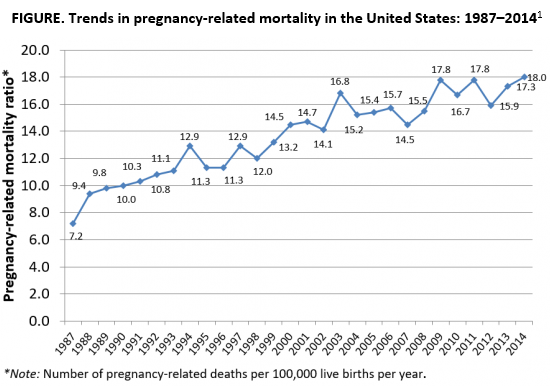
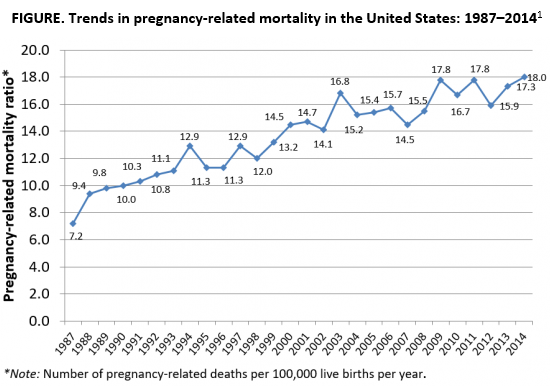
As the rest of the industrialized world has seen a decline in maternal mortality, the United States has seen a substantial rise over the last 30 years (FIGURE).1 It is estimated that more than 60% of these pregnancy-related deaths are preventable. Additionally, substantial disparities exist, with African-American women 3 to 4 times more likely to die of pregnancy-related complications than white women.1
A good first step
The Preventing Maternal Deaths Act was passed by the 115th Congress and signed into law December 2018 in an effort to support and expand maternal mortality review committees (MMRCs) on a state level while allowing the Centers for Disease Control and Prevention (CDC) to further study disparities within maternal mortality. Although these efforts are a good first step to help reduce maternal mortality, more needs to be done to quell this growing epidemic.
We must now improve care access
One strategy to aid in decreasing maternal morbidity and mortality is to improve affordable access to medical care. Medicaid is the largest single payer of maternity care in the United States, covering 42.6% of births. Currently, in many states, Medicaid coverage only lasts until a woman is 60 days postpartum.2 Although 31 states, including the District of Columbia, have adopted Medicaid expansion programs to allow women to extend coverage beyond those 60 days, offering these programs is not a federal law. In the 19 remaining states with no extension options, the vast majority of women will lose their Medicaid coverage just after they are 2 months postpartum and will have no alternative health insurance coverage.2
Why does this coverage cutoff matter? Pregnancy-related deaths are defined as up to 12 months postpartum. A report reviewing 9 MMRCs found that 38% of pregnancy-related deaths occurred while a woman was pregnant, 45% of deaths occurred within 42 days of delivery, and 18% from 43 days to 1 year after delivery.3 Additionally, nearly half of women with Medicaid do not come to their 6-week postpartum visit (for a variety of reasons), missing a critical opportunity to address health concerns.2 Of the deaths that occurred in this later postpartum period, leading causes were cardiomyopathy (32%), mental health conditions (16%), and embolism (11%).3 Prevention and management of these conditions require regular follow-up with an ObGyn, as well as potentially from subspecialists in cardiology, psychiatry, hematology, and other subspecialties. Women not having access to affordable health care during the critical postpartum period greatly increases their risk of death or severe morbidity.
An important next step beyond the Preventing Maternal Deaths Act is to extend Medicaid coverage to 12 months postpartum for all women everywhere. MMRCs have concluded that extending coverage would ensure that “medical and behavioral health conditions [could be] managed and treated before becoming progressively severe.”3 This would presumably help decrease the risk of pregnancy-related death and address worsening morbidity. Additionally, the postpartum period is a well-established time of increased stress and can be an overwhelming and emotional time for many new mothers, especially for those with limited resources for childcare, transportation, stable housing, etc.6 Providing and ensuring ongoing medical care would substantially improve the lives and health of women and the health of their families.
We, as a country, need to make changes
Every step of the way, a woman faces challenges to safely and affordably access health care. Providing access to insurance coverage for 12 months postpartum can help to decrease our country’s rising maternal mortality and morbidity rates.
Take action
Congresswoman Robin Kelly (D-IL) and Senator Dick Durbin (D-IL) have introduced the MOMMA Act (H.R. 1897/S. 916) to help address the rising maternal mortality rate.
This Act would:
- Expand Medicaid coverage to 1 year postpartum.
- Work with the CDC to uniformly collect data to accurately assess maternal mortality and morbidity.
- Ensure the sharing of best practices of care across hospital systems.
- Focus on culturally-competent care to address implicit bias among health care workers.
- Support and expand the Alliance for Innovation on Maternal Health (AIM)—a data-driven initiative to implement safety protocols in hospitals across the country.
To call or contact your representative to co-sponsor this bill, click here. To review if your Congressperson is a co-sponsor, click here. To review if your Senator is a co-sponsor, click here.
- The Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System, Trends in Pregnancy-Related Deaths. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm. Accessed May 29, 2019.
- Stuebe A, Moore JE, Mittal P, et al. Extending medicaid coverage for postpartum moms. May 6, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190501.254675/full/. Accessed May 29, 2019.
- Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018. Color/Word_R17_G85_B204http://reviewtoaction.org/Report_from_Nine_MMRCs. Accessed May 29, 2019.
- MacDorman MF, Declercq E, Cabral H, et al. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447-455.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1-55.
- Vestal C. For addicted women, the year after childbirth is the deadliest. August 14, 2018. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2018/08/14/for-addicted-women-the-year-after-childbirth-is-the-deadliest. Accessed May 29, 2019.
As the rest of the industrialized world has seen a decline in maternal mortality, the United States has seen a substantial rise over the last 30 years (FIGURE).1 It is estimated that more than 60% of these pregnancy-related deaths are preventable. Additionally, substantial disparities exist, with African-American women 3 to 4 times more likely to die of pregnancy-related complications than white women.1
A good first step
The Preventing Maternal Deaths Act was passed by the 115th Congress and signed into law December 2018 in an effort to support and expand maternal mortality review committees (MMRCs) on a state level while allowing the Centers for Disease Control and Prevention (CDC) to further study disparities within maternal mortality. Although these efforts are a good first step to help reduce maternal mortality, more needs to be done to quell this growing epidemic.
We must now improve care access
One strategy to aid in decreasing maternal morbidity and mortality is to improve affordable access to medical care. Medicaid is the largest single payer of maternity care in the United States, covering 42.6% of births. Currently, in many states, Medicaid coverage only lasts until a woman is 60 days postpartum.2 Although 31 states, including the District of Columbia, have adopted Medicaid expansion programs to allow women to extend coverage beyond those 60 days, offering these programs is not a federal law. In the 19 remaining states with no extension options, the vast majority of women will lose their Medicaid coverage just after they are 2 months postpartum and will have no alternative health insurance coverage.2
Why does this coverage cutoff matter? Pregnancy-related deaths are defined as up to 12 months postpartum. A report reviewing 9 MMRCs found that 38% of pregnancy-related deaths occurred while a woman was pregnant, 45% of deaths occurred within 42 days of delivery, and 18% from 43 days to 1 year after delivery.3 Additionally, nearly half of women with Medicaid do not come to their 6-week postpartum visit (for a variety of reasons), missing a critical opportunity to address health concerns.2 Of the deaths that occurred in this later postpartum period, leading causes were cardiomyopathy (32%), mental health conditions (16%), and embolism (11%).3 Prevention and management of these conditions require regular follow-up with an ObGyn, as well as potentially from subspecialists in cardiology, psychiatry, hematology, and other subspecialties. Women not having access to affordable health care during the critical postpartum period greatly increases their risk of death or severe morbidity.
An important next step beyond the Preventing Maternal Deaths Act is to extend Medicaid coverage to 12 months postpartum for all women everywhere. MMRCs have concluded that extending coverage would ensure that “medical and behavioral health conditions [could be] managed and treated before becoming progressively severe.”3 This would presumably help decrease the risk of pregnancy-related death and address worsening morbidity. Additionally, the postpartum period is a well-established time of increased stress and can be an overwhelming and emotional time for many new mothers, especially for those with limited resources for childcare, transportation, stable housing, etc.6 Providing and ensuring ongoing medical care would substantially improve the lives and health of women and the health of their families.
We, as a country, need to make changes
Every step of the way, a woman faces challenges to safely and affordably access health care. Providing access to insurance coverage for 12 months postpartum can help to decrease our country’s rising maternal mortality and morbidity rates.
Take action
Congresswoman Robin Kelly (D-IL) and Senator Dick Durbin (D-IL) have introduced the MOMMA Act (H.R. 1897/S. 916) to help address the rising maternal mortality rate.
This Act would:
- Expand Medicaid coverage to 1 year postpartum.
- Work with the CDC to uniformly collect data to accurately assess maternal mortality and morbidity.
- Ensure the sharing of best practices of care across hospital systems.
- Focus on culturally-competent care to address implicit bias among health care workers.
- Support and expand the Alliance for Innovation on Maternal Health (AIM)—a data-driven initiative to implement safety protocols in hospitals across the country.
To call or contact your representative to co-sponsor this bill, click here. To review if your Congressperson is a co-sponsor, click here. To review if your Senator is a co-sponsor, click here.
As the rest of the industrialized world has seen a decline in maternal mortality, the United States has seen a substantial rise over the last 30 years (FIGURE).1 It is estimated that more than 60% of these pregnancy-related deaths are preventable. Additionally, substantial disparities exist, with African-American women 3 to 4 times more likely to die of pregnancy-related complications than white women.1
A good first step
The Preventing Maternal Deaths Act was passed by the 115th Congress and signed into law December 2018 in an effort to support and expand maternal mortality review committees (MMRCs) on a state level while allowing the Centers for Disease Control and Prevention (CDC) to further study disparities within maternal mortality. Although these efforts are a good first step to help reduce maternal mortality, more needs to be done to quell this growing epidemic.
We must now improve care access
One strategy to aid in decreasing maternal morbidity and mortality is to improve affordable access to medical care. Medicaid is the largest single payer of maternity care in the United States, covering 42.6% of births. Currently, in many states, Medicaid coverage only lasts until a woman is 60 days postpartum.2 Although 31 states, including the District of Columbia, have adopted Medicaid expansion programs to allow women to extend coverage beyond those 60 days, offering these programs is not a federal law. In the 19 remaining states with no extension options, the vast majority of women will lose their Medicaid coverage just after they are 2 months postpartum and will have no alternative health insurance coverage.2
Why does this coverage cutoff matter? Pregnancy-related deaths are defined as up to 12 months postpartum. A report reviewing 9 MMRCs found that 38% of pregnancy-related deaths occurred while a woman was pregnant, 45% of deaths occurred within 42 days of delivery, and 18% from 43 days to 1 year after delivery.3 Additionally, nearly half of women with Medicaid do not come to their 6-week postpartum visit (for a variety of reasons), missing a critical opportunity to address health concerns.2 Of the deaths that occurred in this later postpartum period, leading causes were cardiomyopathy (32%), mental health conditions (16%), and embolism (11%).3 Prevention and management of these conditions require regular follow-up with an ObGyn, as well as potentially from subspecialists in cardiology, psychiatry, hematology, and other subspecialties. Women not having access to affordable health care during the critical postpartum period greatly increases their risk of death or severe morbidity.
An important next step beyond the Preventing Maternal Deaths Act is to extend Medicaid coverage to 12 months postpartum for all women everywhere. MMRCs have concluded that extending coverage would ensure that “medical and behavioral health conditions [could be] managed and treated before becoming progressively severe.”3 This would presumably help decrease the risk of pregnancy-related death and address worsening morbidity. Additionally, the postpartum period is a well-established time of increased stress and can be an overwhelming and emotional time for many new mothers, especially for those with limited resources for childcare, transportation, stable housing, etc.6 Providing and ensuring ongoing medical care would substantially improve the lives and health of women and the health of their families.
We, as a country, need to make changes
Every step of the way, a woman faces challenges to safely and affordably access health care. Providing access to insurance coverage for 12 months postpartum can help to decrease our country’s rising maternal mortality and morbidity rates.
Take action
Congresswoman Robin Kelly (D-IL) and Senator Dick Durbin (D-IL) have introduced the MOMMA Act (H.R. 1897/S. 916) to help address the rising maternal mortality rate.
This Act would:
- Expand Medicaid coverage to 1 year postpartum.
- Work with the CDC to uniformly collect data to accurately assess maternal mortality and morbidity.
- Ensure the sharing of best practices of care across hospital systems.
- Focus on culturally-competent care to address implicit bias among health care workers.
- Support and expand the Alliance for Innovation on Maternal Health (AIM)—a data-driven initiative to implement safety protocols in hospitals across the country.
To call or contact your representative to co-sponsor this bill, click here. To review if your Congressperson is a co-sponsor, click here. To review if your Senator is a co-sponsor, click here.
- The Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System, Trends in Pregnancy-Related Deaths. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm. Accessed May 29, 2019.
- Stuebe A, Moore JE, Mittal P, et al. Extending medicaid coverage for postpartum moms. May 6, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190501.254675/full/. Accessed May 29, 2019.
- Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018. Color/Word_R17_G85_B204http://reviewtoaction.org/Report_from_Nine_MMRCs. Accessed May 29, 2019.
- MacDorman MF, Declercq E, Cabral H, et al. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447-455.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1-55.
- Vestal C. For addicted women, the year after childbirth is the deadliest. August 14, 2018. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2018/08/14/for-addicted-women-the-year-after-childbirth-is-the-deadliest. Accessed May 29, 2019.
- The Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System, Trends in Pregnancy-Related Deaths. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm. Accessed May 29, 2019.
- Stuebe A, Moore JE, Mittal P, et al. Extending medicaid coverage for postpartum moms. May 6, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190501.254675/full/. Accessed May 29, 2019.
- Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018. Color/Word_R17_G85_B204http://reviewtoaction.org/Report_from_Nine_MMRCs. Accessed May 29, 2019.
- MacDorman MF, Declercq E, Cabral H, et al. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447-455.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1-55.
- Vestal C. For addicted women, the year after childbirth is the deadliest. August 14, 2018. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2018/08/14/for-addicted-women-the-year-after-childbirth-is-the-deadliest. Accessed May 29, 2019.
Access to abortion care: Facts matter
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
Now is the time to be heard: October is Advocacy Month!
The American College of Obstetricians and Gynecologists (ACOG) and specifically the Junior Fellow College Advisory Council (JFCAC) are rolling out steps to help you make your voice heard. Starting October 1, head to acog.org/advocacy to check out the ACOG Physician Advocacy video to get inspired. (Or watch it here!) Whether you are a seasoned advocate or just getting started, ACOG and women across the country are counting on you!
Week 1 (October 1–7): Why I advocate
The focus of this week is on delving into topics that interest you, learning why advocacy is critically important, and developing your own message to advocate for women’s health.
- View advocacy videos here to understand what advocacy is and why it is so important.
- See ACOG’s 2018 list of legislative priorities here to find topics that inspire you.
Week 2 (October 8–14): Use your voice
Explore the multitude of platforms available today for amplifying your message. Learn to use social media smartly, get advice for how to write op-eds for local outlets, add your name to support current legislative efforts, and find out who your representatives are to schedule sit-down meetings.
- For tips on communicating with elected officials, click here.
- Connect with ACOG and your district on social media, and remember to use social media responsibly to advocate effectively. See this link for more information!
- Don’t forget to include #JFadvoMonth in your posts while highlighting your advocacy work on social media!
Continued to: Week 3 (October 15–19): Empower your patients
Week 3 (October 15–21): Empower your patients
As a physician, advocating for your patient extends into the clinic itself. Access toolkits, patient websites, handouts, and resources available through ACOG.
- Familiarize yourself with the Patient Page for videos, infographics, and FAQs that are useful resources for your patients.
- Toolkits for providers are available here—use these to enhance your practice and empower your patients!
Week 4 (October 22–28): Take it forward
Advocacy happens year-round. Be sure you are actively involved in ACOG’s efforts. Participate in calls to action and remember on November 6 to GET OUT THE VOTE!
- Participate in the annual Congressional Leadership Conference (March 10–12, 2019) in Washington, DC. Descend on Washington with hundreds of fellow ObGyns to advocate to Congress on important issues. For more information, click here.
- Donate to the Ob-GynPAC, ACOG’s political action committee dedicated to electing officials who support our specialty.
- Run for office! ACOG has resources to support you. Be on the lookout for opportunities to attend candidate workshops sponsored by the Ob-GynPAC!
Get active now!
We are at a critical moment for women’s health and the future of our specialty. Key issues nationally include advocating to Congress to move forward with bills in the Senate (S 1112) and House (HR 1318) to support efforts to reduce maternal mortality. (See this article for background information on these bills.)
To find your elected officials and take action now, click here and tell Congress to help prevent maternal mortality, defend patient protections, and improve access and quality of maternity care.
You can be an advocate for your patients and your profession. Your voice matters. Now is the time to be heard.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
The American College of Obstetricians and Gynecologists (ACOG) and specifically the Junior Fellow College Advisory Council (JFCAC) are rolling out steps to help you make your voice heard. Starting October 1, head to acog.org/advocacy to check out the ACOG Physician Advocacy video to get inspired. (Or watch it here!) Whether you are a seasoned advocate or just getting started, ACOG and women across the country are counting on you!
Week 1 (October 1–7): Why I advocate
The focus of this week is on delving into topics that interest you, learning why advocacy is critically important, and developing your own message to advocate for women’s health.
- View advocacy videos here to understand what advocacy is and why it is so important.
- See ACOG’s 2018 list of legislative priorities here to find topics that inspire you.
Week 2 (October 8–14): Use your voice
Explore the multitude of platforms available today for amplifying your message. Learn to use social media smartly, get advice for how to write op-eds for local outlets, add your name to support current legislative efforts, and find out who your representatives are to schedule sit-down meetings.
- For tips on communicating with elected officials, click here.
- Connect with ACOG and your district on social media, and remember to use social media responsibly to advocate effectively. See this link for more information!
- Don’t forget to include #JFadvoMonth in your posts while highlighting your advocacy work on social media!
Continued to: Week 3 (October 15–19): Empower your patients
Week 3 (October 15–21): Empower your patients
As a physician, advocating for your patient extends into the clinic itself. Access toolkits, patient websites, handouts, and resources available through ACOG.
- Familiarize yourself with the Patient Page for videos, infographics, and FAQs that are useful resources for your patients.
- Toolkits for providers are available here—use these to enhance your practice and empower your patients!
Week 4 (October 22–28): Take it forward
Advocacy happens year-round. Be sure you are actively involved in ACOG’s efforts. Participate in calls to action and remember on November 6 to GET OUT THE VOTE!
- Participate in the annual Congressional Leadership Conference (March 10–12, 2019) in Washington, DC. Descend on Washington with hundreds of fellow ObGyns to advocate to Congress on important issues. For more information, click here.
- Donate to the Ob-GynPAC, ACOG’s political action committee dedicated to electing officials who support our specialty.
- Run for office! ACOG has resources to support you. Be on the lookout for opportunities to attend candidate workshops sponsored by the Ob-GynPAC!
Get active now!
We are at a critical moment for women’s health and the future of our specialty. Key issues nationally include advocating to Congress to move forward with bills in the Senate (S 1112) and House (HR 1318) to support efforts to reduce maternal mortality. (See this article for background information on these bills.)
To find your elected officials and take action now, click here and tell Congress to help prevent maternal mortality, defend patient protections, and improve access and quality of maternity care.
You can be an advocate for your patients and your profession. Your voice matters. Now is the time to be heard.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
The American College of Obstetricians and Gynecologists (ACOG) and specifically the Junior Fellow College Advisory Council (JFCAC) are rolling out steps to help you make your voice heard. Starting October 1, head to acog.org/advocacy to check out the ACOG Physician Advocacy video to get inspired. (Or watch it here!) Whether you are a seasoned advocate or just getting started, ACOG and women across the country are counting on you!
Week 1 (October 1–7): Why I advocate
The focus of this week is on delving into topics that interest you, learning why advocacy is critically important, and developing your own message to advocate for women’s health.
- View advocacy videos here to understand what advocacy is and why it is so important.
- See ACOG’s 2018 list of legislative priorities here to find topics that inspire you.
Week 2 (October 8–14): Use your voice
Explore the multitude of platforms available today for amplifying your message. Learn to use social media smartly, get advice for how to write op-eds for local outlets, add your name to support current legislative efforts, and find out who your representatives are to schedule sit-down meetings.
- For tips on communicating with elected officials, click here.
- Connect with ACOG and your district on social media, and remember to use social media responsibly to advocate effectively. See this link for more information!
- Don’t forget to include #JFadvoMonth in your posts while highlighting your advocacy work on social media!
Continued to: Week 3 (October 15–19): Empower your patients
Week 3 (October 15–21): Empower your patients
As a physician, advocating for your patient extends into the clinic itself. Access toolkits, patient websites, handouts, and resources available through ACOG.
- Familiarize yourself with the Patient Page for videos, infographics, and FAQs that are useful resources for your patients.
- Toolkits for providers are available here—use these to enhance your practice and empower your patients!
Week 4 (October 22–28): Take it forward
Advocacy happens year-round. Be sure you are actively involved in ACOG’s efforts. Participate in calls to action and remember on November 6 to GET OUT THE VOTE!
- Participate in the annual Congressional Leadership Conference (March 10–12, 2019) in Washington, DC. Descend on Washington with hundreds of fellow ObGyns to advocate to Congress on important issues. For more information, click here.
- Donate to the Ob-GynPAC, ACOG’s political action committee dedicated to electing officials who support our specialty.
- Run for office! ACOG has resources to support you. Be on the lookout for opportunities to attend candidate workshops sponsored by the Ob-GynPAC!
Get active now!
We are at a critical moment for women’s health and the future of our specialty. Key issues nationally include advocating to Congress to move forward with bills in the Senate (S 1112) and House (HR 1318) to support efforts to reduce maternal mortality. (See this article for background information on these bills.)
To find your elected officials and take action now, click here and tell Congress to help prevent maternal mortality, defend patient protections, and improve access and quality of maternity care.
You can be an advocate for your patients and your profession. Your voice matters. Now is the time to be heard.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Title X and proposed changes: Take action now
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
The facts
Title X, a bill originally passed in 1970 under President Nixon, is the only federal grant program dedicated to providing family planning services as well as other preventive health care to primarily low-income patients. It is estimated that 70% of patients using Title X services are below the federal poverty level and more than 60% are uninsured or underinsured.1
In 2015 alone, Title X clinics served 3.8 million women, preventing 822,300 unintended pregnancies and 277,800 abortions.2 These clinics provide comprehensive family planning services including information, counseling, and referrals for abortion services. Title X clinics do not use the funding to provide abortion care, and no federal funding from Title X has ever been used to pay for abortions.

Proposed rule changes
The Trump Administration has proposed several new rules for Title X grant recipients.
Here are the main changes3:
- There must be a “financial and physical” separation between a clinic that is a Title X grant recipient and a facility where “abortion is a method of family planning.” This would prevent health centers that receive Title X funding from providing abortions at the same facility. This rule would predominantly affect health centers like Planned Parenthood. Although these clinics already have a financial separation from abortion care, there would not be a physical one in most situations and these clinics would lose Title X funding or be forced to stop providing abortion services.
- Providers who work at a clinic that receives Title X funding but provides abortions at a completely different facility may be ineligible for ongoing Title X grant money. In the new changes, “funds may not be used…to support the separate abortion business of Title X grant subrecipient.” The changes also propose to “protect Title X providers” from choosing between the health of their patients and their consciences. It plans to do this by removing the requirement to provide abortion counseling and referral and allows “non-directive” counseling.
- There would also be a requirement to encourage more parental involvement in minors’ decision making. While clinics already discuss parental involvement, the change would seek to increase the encouragement to young patients to involve parents. Most young patients do involve a parent or guardian in their care; however, many Title X clinics serve young patients who seek care confidentially. Patients seek confidential care due to a multitude of reasons, including history of abuse, lack of trust, and intimate partner violence.
- “A Title X project may not perform, promote, refer for, or support abortion as a method of family planning.” Although the rule does not prevent providers from discussing abortions, clinicians could offer little guidance if a patient opts for an abortion. Providers can give a list of “qualified, comprehensive health service providers” but may not disclose which, if any, of the providers perform abortions.
Take action
Title X provides important health care services to low-income, uninsured, and underinsured patients. These proposals put access to comprehensive health care for vulnerable populations at risk. Medical organizations including the American Medical Association and American College of Obstetricians and Gynecologists have made statements against the proposed changes to Title X. As ObGyns, we need to ensure our patients are fully informed and have access to all family planning and preventive health services.
Call or email your local representative and tell them you oppose the changes to Title X. Find your representatives here.
Follow ACOG’s Action Center on protecting Title X, which includes a flyer for your waiting room.
Send a message to the Health and Human Services Secretary. Submit a formal comment through July 31, 2018, on the Federal Registrar website expressing your thoughts with these proposed changes.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
- Title X: Helping ensure access to high-quality care. National family planning website. https://www.nationalfamilyplanning.org/document.doc?id=514. Accessed July 25, 2018.
- Publicly Funded Contraceptive Services at U.S. Clinics, 2015. Guttmacher website. https://www.guttmacher.org/article/2018/06/domestic-gag-rule-and-more-administrations-proposed-changes-title-x. Accessed July 25, 2018.
- Compliance with statutory program integrity requirements. Federal register website. https://www.federalregister.gov/documents/2018/06/01/2018-11673/compliance-with-statutory-program-integrity-requirements. Accessed July 25, 2018.
Supreme Court case NIFLA v Becerra: What you need to know
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
On March 20, 2018, the United States Supreme Court heard arguments in National Institute of Family and Life Advocates (NIFLA) v Becerra. The Court is expected to issue its decision in June and the results could shape legislation around the country. Here is what you need to know.
The background
There are more than 4,000 Crisis Pregnancy Centers (CPCs) around the country, vastly out numbering abortion clinics.1 The services offered and the make-up of the staff who work in CPCs can vary. CPCs can be licensed to provide medical services, including urine pregnancy tests and ultrasounds, and may have clinicians on staff. Alternatively, other CPCs may be volunteer-run and provide counseling as well as supplies for women, including diapers and baby formula. Within CPCs, however, women are often given misleading and medically inaccurate information about abortion and contraception and are not provided with appropriate or timely referrals if they seek abortion care.
To ensure women have access to comprehensive reproductive health services, California passed the Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act in 2015. This act requires licensed clinics — which may include some CPCs — to notify patients that they may access state-funded prenatal care, family planning, and abortion services through a county health department phone number. Additionally, facilities that provide pregnancy testing and ultrasounds are required to notify clients if they do not employ a licensed medical professional.
In response, NIFLA sued the state of California, alleging that the law violated their freedom of speech by forcing them to communicate about abortion with women who visited their centers.
The case
NIFLA argues that California is violating CPCs’ freedom of speech by requiring them to post statements about medications and medical procedures they strongly oppose. According to NIFLA, if California wants to promote state-funded options, they should publicize that information and not require the CPCs to post it.
The State of California enacted the law to ensure that California women have timely access to all available health care services, including contraception and abortion, and are made aware that the clinic they visit does not offer licensed medical care. Women may not know of their publicly funded options and, without this law, CPCs could withhold that information or provide misleading information, delaying or preventing women from accessing care.
Possible outcomes
If the Supreme Court strikes down California’s FACT Act as a violation of the First Amendment, CPCs in that state would not be required to provide information about free or low-cost prenatal care, contraception, and abortion services or post, if appropriate, that they were an unlicensed facility. However, such a ruling could call into question laws in 18 other states that require doctors to give women false information about possible side effects and complications of abortion during the consent process. This case could provide precedent for physicians to assert that such requirements violate their freedom of speech.
If the Supreme Court upholds California’s FACT Act, this would likely lead to similar laws around the country requiring CPCs to disclose the availability of affordable contraception and abortion services in their state and the lack of licensed medical providers.
For more information, check out https://www.supremecourt.gov/
Acknowledgement
Special thanks to Sara Needleman Kline, Esq, Chief Legal Officer, American College of Obstetricians and Gynecologists, for aid with this article.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.
- Dias E. The Abortion Battleground: Crisis Pregnancy Centers. Time Magazine. http://content.time.com/time/nation/article/0,8599,2008846,00.html. Published August 5, 2010. Accessed May 16, 2018.
Take action to prevent maternal mortality
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
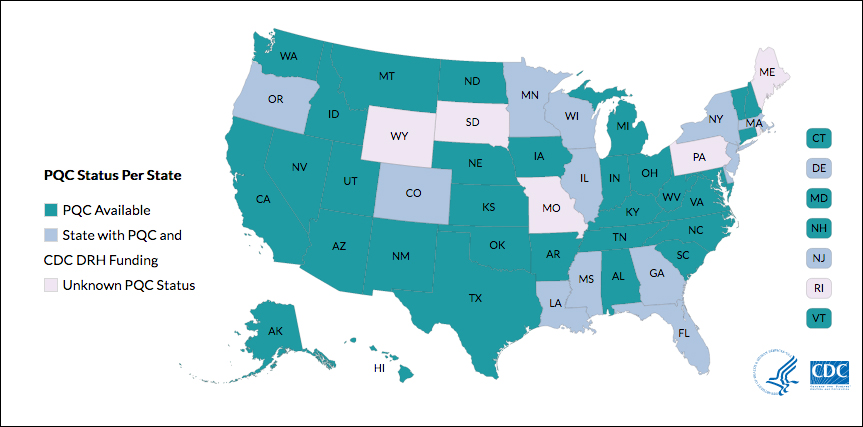
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
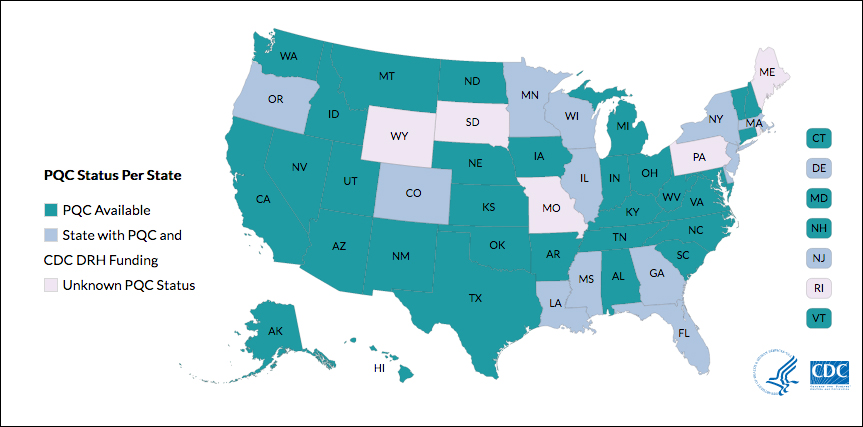
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
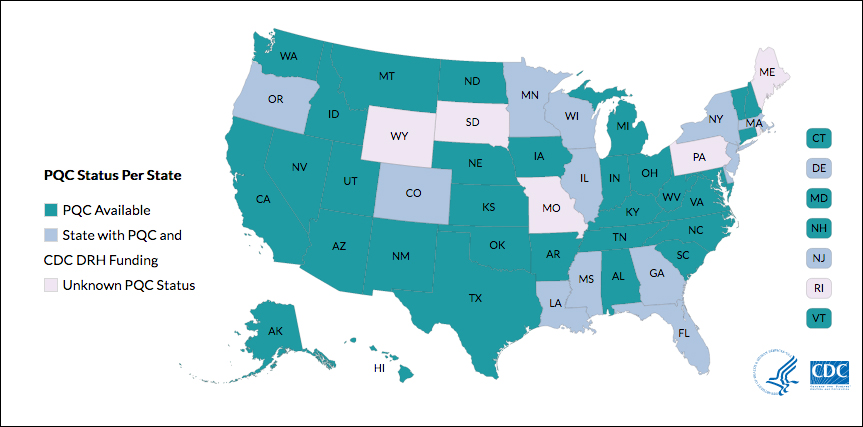
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.