User login
Hand hygiene linked to reduced ICU health care–associated infections
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
FROM CLINICAL MICROBIOLOGY AND INFECTION
Key clinical point: Hand hygiene was the key factor associated with a decrease in severe HAIs.
Major finding: A reduction in severe HAIs (aIRR 0.13) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56]) were observed.
Study details: A prospective database analysis of more nearly 65,000 hospitalized patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010.
Barriers loom for HCV care in young people who inject drugs
Young adults who inject drugs and are infected with hepatitis C virus “face unique barriers to HCV testing, counseling, and treatment,” according to Margie R. Skeer, ScD, of Tufts University, Boston, and her fellow researchers.
Dr. Skeer and her colleagues found five themes in 24 in-depth interviews with people aged 22-30 years who inject drugs and have HCV infection. At the time of the interviews, none of the patients had received the newer HCV treatment regimens (Drug Alcohol Depend. 2018 Sep 1;190:246-54).
These themes captured the knowledge of and experience of HCV along the continuum of care:
1. Deservingness of HCV treatment and stigma.
2. Dissatisfaction with provider interactions.
3. Perceived lack of referral to treatment and care continuity.
4. Disincentives around HCV treatment for PWID.
5. Perceived need for treatment.
The interviewees were largely uninformed about HCV prior to diagnosis and reported learning more about the virus after their diagnosis. They also tended to affirm the belief that they did not deserve treatment. They felt stigmatized by insurance companies and clinicians, thereby reducing their engagement in the care continuum. And, at the time, insurance companies enforced “sobriety” restrictions dictating the length of time patients had to be off drugs before qualifying for HCV treatment. In the words of one interviewee: “[Caregivers] have a big stigma when it comes to addicts. ... Their whole demeanor changes. They rush you, they slam things, they are very impatient with you, and it is very saddening to see.”
Interviewees reported no or incomplete referrals or being given pamphlets and flyers. They reported little follow-up as to whether they sought additional care, and experienced a lack of confidence from medical professionals that they could be counted on to adhere to an HCV treatment regimen.
Interviewees stated that injection drug use and HCV are inevitably linked, and that IV drug users will eventually contract HCV infections.
“Hep C’s no big deal, Hep C’s like the common cold for the junkie. ... It might take 5 years away from your, you know, life but, you know, we’re not even gonna live that long anyways, so who cares about it anyway,” remarked a 28-year old woman, who was not currently injecting drugs.
The study authors said there is an increased need to provide patient-oriented care for young injection drug users and described the potential benefits of some insurance companies reducing their sobriety and disease severity restrictions.
“Reducing stigma among healthcare professionals, which cuts across the different levels of the HCV care continuum, improving referral patterns and continuity of care, better informing people about their HCV status through patient-oriented testing and disclosure experiences, and reducing perceptions of personal responsibility for disease are crucial next steps to increasing treatment as prevention,” Dr. Skeer and her colleagues concluded.
The authors reported that they had no conflicts of interest.
AGA patient materials can help your patients better understand and manage living with hepatitis C. Learn more at patient.gastro.org.
Young adults who inject drugs and are infected with hepatitis C virus “face unique barriers to HCV testing, counseling, and treatment,” according to Margie R. Skeer, ScD, of Tufts University, Boston, and her fellow researchers.
Dr. Skeer and her colleagues found five themes in 24 in-depth interviews with people aged 22-30 years who inject drugs and have HCV infection. At the time of the interviews, none of the patients had received the newer HCV treatment regimens (Drug Alcohol Depend. 2018 Sep 1;190:246-54).
These themes captured the knowledge of and experience of HCV along the continuum of care:
1. Deservingness of HCV treatment and stigma.
2. Dissatisfaction with provider interactions.
3. Perceived lack of referral to treatment and care continuity.
4. Disincentives around HCV treatment for PWID.
5. Perceived need for treatment.
The interviewees were largely uninformed about HCV prior to diagnosis and reported learning more about the virus after their diagnosis. They also tended to affirm the belief that they did not deserve treatment. They felt stigmatized by insurance companies and clinicians, thereby reducing their engagement in the care continuum. And, at the time, insurance companies enforced “sobriety” restrictions dictating the length of time patients had to be off drugs before qualifying for HCV treatment. In the words of one interviewee: “[Caregivers] have a big stigma when it comes to addicts. ... Their whole demeanor changes. They rush you, they slam things, they are very impatient with you, and it is very saddening to see.”
Interviewees reported no or incomplete referrals or being given pamphlets and flyers. They reported little follow-up as to whether they sought additional care, and experienced a lack of confidence from medical professionals that they could be counted on to adhere to an HCV treatment regimen.
Interviewees stated that injection drug use and HCV are inevitably linked, and that IV drug users will eventually contract HCV infections.
“Hep C’s no big deal, Hep C’s like the common cold for the junkie. ... It might take 5 years away from your, you know, life but, you know, we’re not even gonna live that long anyways, so who cares about it anyway,” remarked a 28-year old woman, who was not currently injecting drugs.
The study authors said there is an increased need to provide patient-oriented care for young injection drug users and described the potential benefits of some insurance companies reducing their sobriety and disease severity restrictions.
“Reducing stigma among healthcare professionals, which cuts across the different levels of the HCV care continuum, improving referral patterns and continuity of care, better informing people about their HCV status through patient-oriented testing and disclosure experiences, and reducing perceptions of personal responsibility for disease are crucial next steps to increasing treatment as prevention,” Dr. Skeer and her colleagues concluded.
The authors reported that they had no conflicts of interest.
AGA patient materials can help your patients better understand and manage living with hepatitis C. Learn more at patient.gastro.org.
Young adults who inject drugs and are infected with hepatitis C virus “face unique barriers to HCV testing, counseling, and treatment,” according to Margie R. Skeer, ScD, of Tufts University, Boston, and her fellow researchers.
Dr. Skeer and her colleagues found five themes in 24 in-depth interviews with people aged 22-30 years who inject drugs and have HCV infection. At the time of the interviews, none of the patients had received the newer HCV treatment regimens (Drug Alcohol Depend. 2018 Sep 1;190:246-54).
These themes captured the knowledge of and experience of HCV along the continuum of care:
1. Deservingness of HCV treatment and stigma.
2. Dissatisfaction with provider interactions.
3. Perceived lack of referral to treatment and care continuity.
4. Disincentives around HCV treatment for PWID.
5. Perceived need for treatment.
The interviewees were largely uninformed about HCV prior to diagnosis and reported learning more about the virus after their diagnosis. They also tended to affirm the belief that they did not deserve treatment. They felt stigmatized by insurance companies and clinicians, thereby reducing their engagement in the care continuum. And, at the time, insurance companies enforced “sobriety” restrictions dictating the length of time patients had to be off drugs before qualifying for HCV treatment. In the words of one interviewee: “[Caregivers] have a big stigma when it comes to addicts. ... Their whole demeanor changes. They rush you, they slam things, they are very impatient with you, and it is very saddening to see.”
Interviewees reported no or incomplete referrals or being given pamphlets and flyers. They reported little follow-up as to whether they sought additional care, and experienced a lack of confidence from medical professionals that they could be counted on to adhere to an HCV treatment regimen.
Interviewees stated that injection drug use and HCV are inevitably linked, and that IV drug users will eventually contract HCV infections.
“Hep C’s no big deal, Hep C’s like the common cold for the junkie. ... It might take 5 years away from your, you know, life but, you know, we’re not even gonna live that long anyways, so who cares about it anyway,” remarked a 28-year old woman, who was not currently injecting drugs.
The study authors said there is an increased need to provide patient-oriented care for young injection drug users and described the potential benefits of some insurance companies reducing their sobriety and disease severity restrictions.
“Reducing stigma among healthcare professionals, which cuts across the different levels of the HCV care continuum, improving referral patterns and continuity of care, better informing people about their HCV status through patient-oriented testing and disclosure experiences, and reducing perceptions of personal responsibility for disease are crucial next steps to increasing treatment as prevention,” Dr. Skeer and her colleagues concluded.
The authors reported that they had no conflicts of interest.
AGA patient materials can help your patients better understand and manage living with hepatitis C. Learn more at patient.gastro.org.
FROM DRUG AND ALCOHOL DEPENDENCE
Fewer groin infections with closed incision negative pressure therapy after vascular surgery
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
Closed incision negative pressure therapy (ciNPT) was found to reduce surgical site infections (SSI) in vascular surgery, according to the results of a prospective, randomized, industry-sponsored trial of patients who underwent vascular surgery for peripheral artery disease (PAD) published online in the European Journal of Vascular and Endovascular Surgery.
The investigator-initiated Reduction of Groin Wound Infections After Vascular Surgery by Using an Incision Management System trial (NCT02395159) included 204 patients who underwent vascular surgery involving longitudinal groin incision to treat the lower extremity or the iliac arteries between July 2015 and May 2017 at two study centers.
The primary endpoint was the occurrence of SSI assessed by the Szilagyi classification (grades I-III). The mean patient age was nearly 67 years and 70% were men. In terms of PAD staging, 52% were stage 2B, 28% were stage 3, and 19% were stage 4. Among the patients, 45% had a previous groin incision and 42% had diabetes.
All patients underwent similar preoperative treatment: hair shaving and preparation with Poly Alcohol (Antiseptica, Pulheim, Germany) and Braunoderm (Braun, Melsungen, Germany). At 30 minutes preincision, patients received intravenous antibiotic treatment (1.5 g cefuroxime or 600 mg clindamycin, if allergic to penicillin). After closure, the incision and surrounding skin area was cleaned and dried using sterile gauze. In the control group, a sterile adhesive wound dressing was applied to the wound, which was changed daily. In the treatment group, ciNPT was applied under sterile conditions in the operating room using the Prevena device, which exerts a continuous negative pressure of 125 mm Hg on the closed incision during the time of application. The device was removed at 5-7 days postoperatively, and no further wound dressings were used in the treatment group unless an SSI occurred.
The control group experienced more frequent SSIs (33.3%) than the intervention group (13.2%) (P =.0015). This difference was based on an increased rate of Szilagyi grade I SSI in the control group (24.6% vs. 8.1%, P = .0012), according to Alexander Gombert, MD, of the University Hospital Aachen (Germany), and his colleagues. The absolute risk difference based on the Szilagyi classification was –20.1 per 100 (95% confidence interval, –31.9 to –8.2).
In addition, there was a statistically significantly lower rate of SSI when using ciNPT within the subgroups at greater risk of infection, compared with controls: PAD stage greater than or equal to 3 (P less than .001), body mass index greater than 25 kg/m2 (P less than .001), and previous groin incision (P = .016).
There were no statistical differences between the two groups in Szilagyi grade II and III SSIs (which occurred in 5.8% of all procedures).
No potentially device-related complications were observed in the trial and there were no failures of the device seen.
“The use of ciNPT rather than standard wound dressing after groin incision as access for vascular surgery was associated with a reduced rate of superficial SSI classified by Szilagyi, suggesting that ciNPT may be useful for reducing the SSI rate among high-risk patients,” the researchers concluded.
The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
SOURCE: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
FROM THE EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Closed incision negative pressure therapy lessened the incidence of groin infection after vascular surgery.
Major finding: The control group experienced more frequent surgical site infections (33.3%) than the intervention group (13.2%) (P =.0015).
Study details: A randomized, controlled trial of 204 patients with peripheral artery disease who underwent vascular surgery.
Disclosures: The trial was funded by Acelity. Dr. Gombert received travel grants from Acelity.
Source: Gombert A et al. Eur J Vasc Surg. 2018 Jul 2. doi: 10.1016/j.ejvs.2018.05.018.
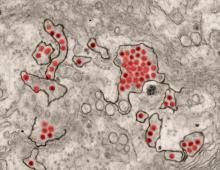
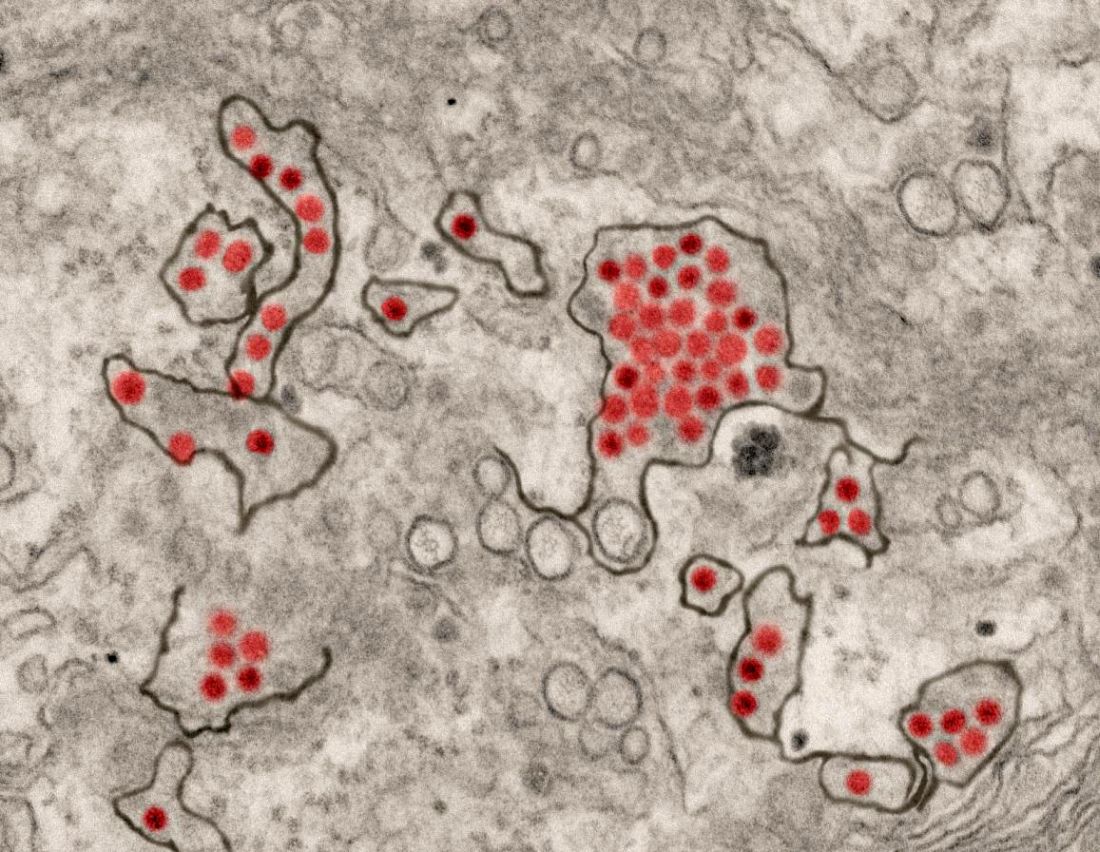
Model finds spontaneous HCV clearance higher than previous estimates
Up to 40% of hepatitis C virus (HCV)–infected individuals clear their infection spontaneously, based on the results of a new mathematical model of HCV transmission and clearance, according to a report published online in the International Journal of Infectious Diseases.
Houssein H. Ayoub, PhD, of Cornell University, New York, and his colleagues conducted a study on HCV clearance. Previous estimates using empirical data indicated that the HCV clearance rate was about 25% after and acute infection duration of 16.5 weeks, according to Dr. Ayoub and his colleagues.
They developed a model to describe HCV transmission and a virus clearance rate (fclearance), defined as the proportion of HCV-infected persons who spontaneously clear their infection after the acute stage. The rest of the infected population (1–fclearance) become chronically infected and positive for both HCV antibodies and HCV RNA.This was estimated by fitting the model to probability-based and nationally representative, population-based data from Egypt (2008 and 2015), and the U.S. National Health and Nutrition Examination Surveys (NHANES A and NHANES B) data. Their model showed that fclearance was related to the HCV viremic rate approximately as fclearance = 1.16 x (1–HCV viremic rate). The HCV viremic rate was defined as the proportion of individuals who were positive for HCV antibodies and HCV RNA out of all who were positive for HCV antibodies positive, regardless of RNA status, as measured in a cross-sectional survey.
Antibody prevalence in Egypt was estimated at 14.7% in 2008 and 10.0% in 2015, while the viremic rate was assessed as 67.1% and 70.2%, respectively. For the United States, the pooled antibody prevalence from the NHANES A data between 1999 and 2012 was an estimated 1.4% and the pooled viremic rate was estimated at around 74%. The NHANES B data used as the denominator for HCV viremic rate both individuals confirmed as HCV Ab positive and those with an undetermined HCV antibody status. (NHANES laboratory procedures can provide this added information because of their subsequent testing of undetermined HCV antibody results for HCV RNA positivity.) This change to the formula yielded a viremic rate of 64.6%.
They found that fclearance was an estimated at 39.9% and 33.5% for Egypt in 2008 and 2015, respectively, and 29.6% and 49.9% for NHANES A and NHANES B, respectively.
“Empirical measures from longitudinal cohort studies may have underestimated the ability of the host immune system to clear HCV infection. This finding may have also implications for our understanding of the biological determinants of HCV spontaneous clearance. It may hint that a strategy for HCV vaccine development could be a vaccine that does not necessarily prevent infection, but modulates immune response towards conditions that increase the capacity of the host immune system to clear HCV infection spontaneously,” the researchers concluded.
The study was funded by the Qatar National Research Fund and Cornell University. The authors reported no conflicts of interest.
SOURCE: Ayoub HH et al. Int J Infect Dis. 2018 Jul 18. doi: 10.1016/j.ijid.2018.07.013.
Up to 40% of hepatitis C virus (HCV)–infected individuals clear their infection spontaneously, based on the results of a new mathematical model of HCV transmission and clearance, according to a report published online in the International Journal of Infectious Diseases.
Houssein H. Ayoub, PhD, of Cornell University, New York, and his colleagues conducted a study on HCV clearance. Previous estimates using empirical data indicated that the HCV clearance rate was about 25% after and acute infection duration of 16.5 weeks, according to Dr. Ayoub and his colleagues.
They developed a model to describe HCV transmission and a virus clearance rate (fclearance), defined as the proportion of HCV-infected persons who spontaneously clear their infection after the acute stage. The rest of the infected population (1–fclearance) become chronically infected and positive for both HCV antibodies and HCV RNA.This was estimated by fitting the model to probability-based and nationally representative, population-based data from Egypt (2008 and 2015), and the U.S. National Health and Nutrition Examination Surveys (NHANES A and NHANES B) data. Their model showed that fclearance was related to the HCV viremic rate approximately as fclearance = 1.16 x (1–HCV viremic rate). The HCV viremic rate was defined as the proportion of individuals who were positive for HCV antibodies and HCV RNA out of all who were positive for HCV antibodies positive, regardless of RNA status, as measured in a cross-sectional survey.
Antibody prevalence in Egypt was estimated at 14.7% in 2008 and 10.0% in 2015, while the viremic rate was assessed as 67.1% and 70.2%, respectively. For the United States, the pooled antibody prevalence from the NHANES A data between 1999 and 2012 was an estimated 1.4% and the pooled viremic rate was estimated at around 74%. The NHANES B data used as the denominator for HCV viremic rate both individuals confirmed as HCV Ab positive and those with an undetermined HCV antibody status. (NHANES laboratory procedures can provide this added information because of their subsequent testing of undetermined HCV antibody results for HCV RNA positivity.) This change to the formula yielded a viremic rate of 64.6%.
They found that fclearance was an estimated at 39.9% and 33.5% for Egypt in 2008 and 2015, respectively, and 29.6% and 49.9% for NHANES A and NHANES B, respectively.
“Empirical measures from longitudinal cohort studies may have underestimated the ability of the host immune system to clear HCV infection. This finding may have also implications for our understanding of the biological determinants of HCV spontaneous clearance. It may hint that a strategy for HCV vaccine development could be a vaccine that does not necessarily prevent infection, but modulates immune response towards conditions that increase the capacity of the host immune system to clear HCV infection spontaneously,” the researchers concluded.
The study was funded by the Qatar National Research Fund and Cornell University. The authors reported no conflicts of interest.
SOURCE: Ayoub HH et al. Int J Infect Dis. 2018 Jul 18. doi: 10.1016/j.ijid.2018.07.013.
Up to 40% of hepatitis C virus (HCV)–infected individuals clear their infection spontaneously, based on the results of a new mathematical model of HCV transmission and clearance, according to a report published online in the International Journal of Infectious Diseases.
Houssein H. Ayoub, PhD, of Cornell University, New York, and his colleagues conducted a study on HCV clearance. Previous estimates using empirical data indicated that the HCV clearance rate was about 25% after and acute infection duration of 16.5 weeks, according to Dr. Ayoub and his colleagues.
They developed a model to describe HCV transmission and a virus clearance rate (fclearance), defined as the proportion of HCV-infected persons who spontaneously clear their infection after the acute stage. The rest of the infected population (1–fclearance) become chronically infected and positive for both HCV antibodies and HCV RNA.This was estimated by fitting the model to probability-based and nationally representative, population-based data from Egypt (2008 and 2015), and the U.S. National Health and Nutrition Examination Surveys (NHANES A and NHANES B) data. Their model showed that fclearance was related to the HCV viremic rate approximately as fclearance = 1.16 x (1–HCV viremic rate). The HCV viremic rate was defined as the proportion of individuals who were positive for HCV antibodies and HCV RNA out of all who were positive for HCV antibodies positive, regardless of RNA status, as measured in a cross-sectional survey.
Antibody prevalence in Egypt was estimated at 14.7% in 2008 and 10.0% in 2015, while the viremic rate was assessed as 67.1% and 70.2%, respectively. For the United States, the pooled antibody prevalence from the NHANES A data between 1999 and 2012 was an estimated 1.4% and the pooled viremic rate was estimated at around 74%. The NHANES B data used as the denominator for HCV viremic rate both individuals confirmed as HCV Ab positive and those with an undetermined HCV antibody status. (NHANES laboratory procedures can provide this added information because of their subsequent testing of undetermined HCV antibody results for HCV RNA positivity.) This change to the formula yielded a viremic rate of 64.6%.
They found that fclearance was an estimated at 39.9% and 33.5% for Egypt in 2008 and 2015, respectively, and 29.6% and 49.9% for NHANES A and NHANES B, respectively.
“Empirical measures from longitudinal cohort studies may have underestimated the ability of the host immune system to clear HCV infection. This finding may have also implications for our understanding of the biological determinants of HCV spontaneous clearance. It may hint that a strategy for HCV vaccine development could be a vaccine that does not necessarily prevent infection, but modulates immune response towards conditions that increase the capacity of the host immune system to clear HCV infection spontaneously,” the researchers concluded.
The study was funded by the Qatar National Research Fund and Cornell University. The authors reported no conflicts of interest.
SOURCE: Ayoub HH et al. Int J Infect Dis. 2018 Jul 18. doi: 10.1016/j.ijid.2018.07.013.
FROM THE INTERNATIONAL JOURNAL OF INFECTIOUS DISEASES
Key clinical point: The hepatitis C virus clearance rate was 39.9% and 33.5% for Egypt in 2008 and 2015, respectively, and 29.6% and 49.9% for two U.S. populations.
Major finding: A new model of HCV-infected persons indicates that up to 40% clear their infection spontaneously, higher than earlier estimates.
Study details: A mathematical model was developed to describe HCV transmission and clearance based on nationally representative population data for Egypt and the United States.
Disclosures: The study was funded by the Qatar National Research Fund and Cornell University. The authors reported no conflicts of interest.
Source: Ayoub HH et al. Int J Infect Dis. 2018 Jul 18. doi: 10.1016/j.ijid.2018.07.013.
Witnessed overdose, HCV infection associated with greater opioid overdose risk
With drug overdoses being the leading cause of accidental death in the United States, knowing the predictors of opioid overdose may help target treatment and prevention efforts to deal with this growing problem, according to Samantha Schiavon, MA, a graduate student in medical and clinical psychology, and her colleagues at the University of Alabama at Birmingham.
They performed a study that found a variety of factors associated with increased risk of opioid overdose, including witnessing an overdose (a friend or others), chronic hepatitis C virus (HCV) infection, and a higher frequency of distinct buprenorphine treatment episodes.
Data were acquired during Nov. 2015-July 2017 from an ongoing study to determine the impact of the distribution of naloxone kits to individuals at high risk for opioid overdose. All 247 participants included were considered at high risk of opioid overdose because they were recruited from sites providing opioid addiction treatment, including a residential drug treatment facility (43%), inpatient treatment following ED admittance (25%), and criminal justice supervision (32%). Of the participants, 57% were male, with a mean age of around 34 years; most were white (89%).
Participants were assessed using a self-reporting 30-item questionnaire regarding chronic medical conditions, STIs, past and current opioid misuse, nonfatal opioid overdose experiences, and frequency of every distinct opioid treatment episode including buprenorphine, methadone maintenance clinics, residential drug rehabilitation programs, and intensive outpatient treatment. All variables were answered on a 5-point scale ranging from 0 (never) to 4 (more than three times), according to the researchers.
Participants who witnessed a friend’s overdose (odds ratio, 4.21; 95% confidence interval, 1.99-8.89) showed the highest risk of personal overdose, while having witnessed others overdose at a higher frequency carried a lower increased risk (OR, 1.42; 95% CI, 1.11-1.82).
HCV infection was associated with a more than twofold increase in overdose risk (OR, 2.44; 95% CI, 1.20-4.97), likely because of the strong association between HCV and heroin injection drug use, according to the researchers. They added that this association may be an indicator of higher-risk injection behavior, including needle sharing. They also suggested that, given the current epidemiology of HCV infection, identifying HCV infections may benefit younger populations who may be at risk of an overdose from riskier injection practices or where injection drug risk is not yet known.
The researchers reported that a higher frequency of distinct buprenorphine treatment episodes also led to increased risk (OR, 1.55; 95% CI, 1.17-2.07), whereas a greater frequency of distinct methadone treatment episodes was related to decreased odds of experiencing a nonfatal overdose (OR, 0.67; 95% CI, 0.49-0.91) according to their report published in Addictive Behavior (2018;86:51-5).
In addition, those who experienced a past opioid overdose were more likely to have obtained methadone illicitly (65%; P less than or equal to .001) or have a friend who died from an overdose (90%; P = .001) compared with those who have not experienced an overdose, according to the researchers.
“The current study strongly contributes to our understanding of risk factors of experiencing an opioid overdose. The knowledge gained from this study may enable targeted treatment interventions to reduce preventable deaths from opioid overdose,” according to the researchers. In particular, they pointed out the increased risk of overdose with the use of illicitly obtained methadone and suggested that expanded access to medication-assisted treatments be made available to all patients. “Opioid antagonist medications such as naltrexone may be particularly helpful in preventing opioid overdose for patients leaving controlled environments such as hospital, drug treatment, and correctional facilities,” they concluded.
The researchers reported that they had no conflicts of interest.
SOURCE: Schiavon S et al. Addict Behav. 2018;86:51-5.
With drug overdoses being the leading cause of accidental death in the United States, knowing the predictors of opioid overdose may help target treatment and prevention efforts to deal with this growing problem, according to Samantha Schiavon, MA, a graduate student in medical and clinical psychology, and her colleagues at the University of Alabama at Birmingham.
They performed a study that found a variety of factors associated with increased risk of opioid overdose, including witnessing an overdose (a friend or others), chronic hepatitis C virus (HCV) infection, and a higher frequency of distinct buprenorphine treatment episodes.
Data were acquired during Nov. 2015-July 2017 from an ongoing study to determine the impact of the distribution of naloxone kits to individuals at high risk for opioid overdose. All 247 participants included were considered at high risk of opioid overdose because they were recruited from sites providing opioid addiction treatment, including a residential drug treatment facility (43%), inpatient treatment following ED admittance (25%), and criminal justice supervision (32%). Of the participants, 57% were male, with a mean age of around 34 years; most were white (89%).
Participants were assessed using a self-reporting 30-item questionnaire regarding chronic medical conditions, STIs, past and current opioid misuse, nonfatal opioid overdose experiences, and frequency of every distinct opioid treatment episode including buprenorphine, methadone maintenance clinics, residential drug rehabilitation programs, and intensive outpatient treatment. All variables were answered on a 5-point scale ranging from 0 (never) to 4 (more than three times), according to the researchers.
Participants who witnessed a friend’s overdose (odds ratio, 4.21; 95% confidence interval, 1.99-8.89) showed the highest risk of personal overdose, while having witnessed others overdose at a higher frequency carried a lower increased risk (OR, 1.42; 95% CI, 1.11-1.82).
HCV infection was associated with a more than twofold increase in overdose risk (OR, 2.44; 95% CI, 1.20-4.97), likely because of the strong association between HCV and heroin injection drug use, according to the researchers. They added that this association may be an indicator of higher-risk injection behavior, including needle sharing. They also suggested that, given the current epidemiology of HCV infection, identifying HCV infections may benefit younger populations who may be at risk of an overdose from riskier injection practices or where injection drug risk is not yet known.
The researchers reported that a higher frequency of distinct buprenorphine treatment episodes also led to increased risk (OR, 1.55; 95% CI, 1.17-2.07), whereas a greater frequency of distinct methadone treatment episodes was related to decreased odds of experiencing a nonfatal overdose (OR, 0.67; 95% CI, 0.49-0.91) according to their report published in Addictive Behavior (2018;86:51-5).
In addition, those who experienced a past opioid overdose were more likely to have obtained methadone illicitly (65%; P less than or equal to .001) or have a friend who died from an overdose (90%; P = .001) compared with those who have not experienced an overdose, according to the researchers.
“The current study strongly contributes to our understanding of risk factors of experiencing an opioid overdose. The knowledge gained from this study may enable targeted treatment interventions to reduce preventable deaths from opioid overdose,” according to the researchers. In particular, they pointed out the increased risk of overdose with the use of illicitly obtained methadone and suggested that expanded access to medication-assisted treatments be made available to all patients. “Opioid antagonist medications such as naltrexone may be particularly helpful in preventing opioid overdose for patients leaving controlled environments such as hospital, drug treatment, and correctional facilities,” they concluded.
The researchers reported that they had no conflicts of interest.
SOURCE: Schiavon S et al. Addict Behav. 2018;86:51-5.
With drug overdoses being the leading cause of accidental death in the United States, knowing the predictors of opioid overdose may help target treatment and prevention efforts to deal with this growing problem, according to Samantha Schiavon, MA, a graduate student in medical and clinical psychology, and her colleagues at the University of Alabama at Birmingham.
They performed a study that found a variety of factors associated with increased risk of opioid overdose, including witnessing an overdose (a friend or others), chronic hepatitis C virus (HCV) infection, and a higher frequency of distinct buprenorphine treatment episodes.
Data were acquired during Nov. 2015-July 2017 from an ongoing study to determine the impact of the distribution of naloxone kits to individuals at high risk for opioid overdose. All 247 participants included were considered at high risk of opioid overdose because they were recruited from sites providing opioid addiction treatment, including a residential drug treatment facility (43%), inpatient treatment following ED admittance (25%), and criminal justice supervision (32%). Of the participants, 57% were male, with a mean age of around 34 years; most were white (89%).
Participants were assessed using a self-reporting 30-item questionnaire regarding chronic medical conditions, STIs, past and current opioid misuse, nonfatal opioid overdose experiences, and frequency of every distinct opioid treatment episode including buprenorphine, methadone maintenance clinics, residential drug rehabilitation programs, and intensive outpatient treatment. All variables were answered on a 5-point scale ranging from 0 (never) to 4 (more than three times), according to the researchers.
Participants who witnessed a friend’s overdose (odds ratio, 4.21; 95% confidence interval, 1.99-8.89) showed the highest risk of personal overdose, while having witnessed others overdose at a higher frequency carried a lower increased risk (OR, 1.42; 95% CI, 1.11-1.82).
HCV infection was associated with a more than twofold increase in overdose risk (OR, 2.44; 95% CI, 1.20-4.97), likely because of the strong association between HCV and heroin injection drug use, according to the researchers. They added that this association may be an indicator of higher-risk injection behavior, including needle sharing. They also suggested that, given the current epidemiology of HCV infection, identifying HCV infections may benefit younger populations who may be at risk of an overdose from riskier injection practices or where injection drug risk is not yet known.
The researchers reported that a higher frequency of distinct buprenorphine treatment episodes also led to increased risk (OR, 1.55; 95% CI, 1.17-2.07), whereas a greater frequency of distinct methadone treatment episodes was related to decreased odds of experiencing a nonfatal overdose (OR, 0.67; 95% CI, 0.49-0.91) according to their report published in Addictive Behavior (2018;86:51-5).
In addition, those who experienced a past opioid overdose were more likely to have obtained methadone illicitly (65%; P less than or equal to .001) or have a friend who died from an overdose (90%; P = .001) compared with those who have not experienced an overdose, according to the researchers.
“The current study strongly contributes to our understanding of risk factors of experiencing an opioid overdose. The knowledge gained from this study may enable targeted treatment interventions to reduce preventable deaths from opioid overdose,” according to the researchers. In particular, they pointed out the increased risk of overdose with the use of illicitly obtained methadone and suggested that expanded access to medication-assisted treatments be made available to all patients. “Opioid antagonist medications such as naltrexone may be particularly helpful in preventing opioid overdose for patients leaving controlled environments such as hospital, drug treatment, and correctional facilities,” they concluded.
The researchers reported that they had no conflicts of interest.
SOURCE: Schiavon S et al. Addict Behav. 2018;86:51-5.
FROM ADDICTIVE BEHAVIORS
Key clinical point: The greatest increased risk of opioid overdose was associated with witnessing a friend’s overdose and chronic hepatitis C virus infection.
Major finding: Witnessing a friend’s overdose was associated with the highest risk of personal overdose (OR, 4.21).
Study details: 247 participants who were considered at high risk of opioid overdose and were recruited from sites providing opioid addiction treatment.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Schiavon S et al. Addict Behav. 2018;86:51-5.
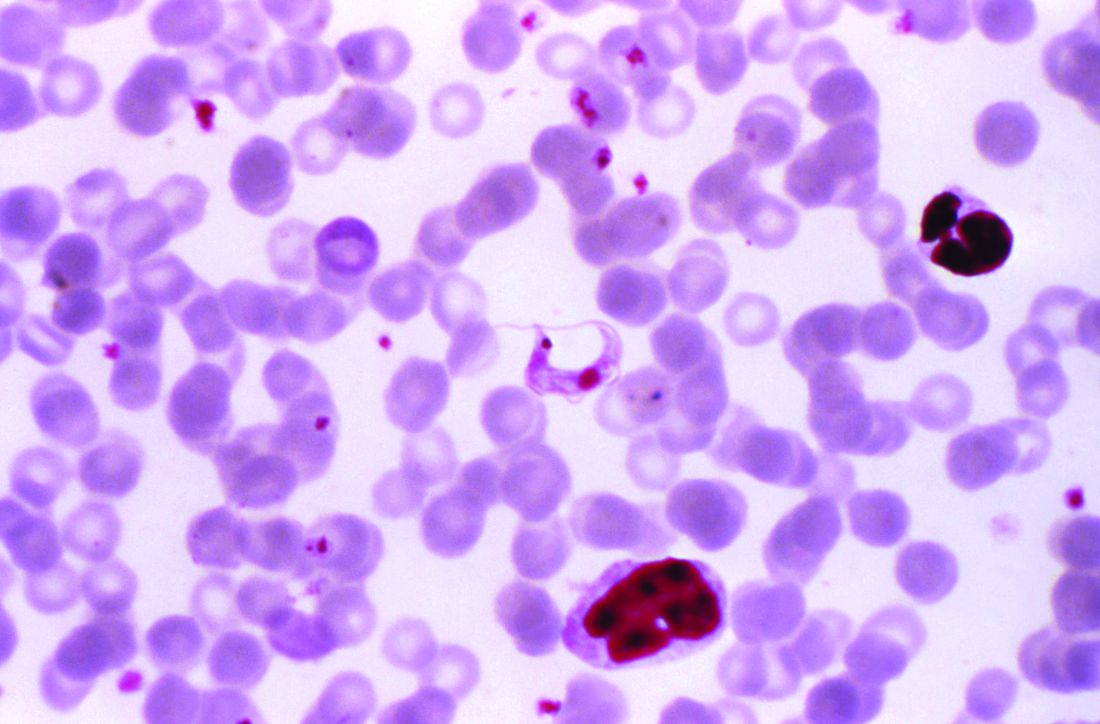
AHA: Chagas disease and its heart effects have come to the U.S.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
FROM CIRCULATION
Open AAA and peripheral bypass surgery patients among the highest users of post-acute care
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: The wide disparity among hospitals in their rates of postsurgery discharge to post-acute care (PAC) could be an area of focus for cost containment in Medicare spending.
Major finding: Rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals.
Study details: A database analysis of 3,487,365 National Inpatient Sample patients and 60,666 VA patients who had surgery during 2008-2011.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
Zika virus vaccine trial launches
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
A first-in-human trial of a live, attenuated Zika virus vaccine has begun, according to an announcement by the National Institutes of Health.
The vaccine, developed by scientists at the National Institute of Allergy and Infectious Diseases will be tested in 28 healthy, nonpregnant adults aged 18-50 years at two centers, the Johns Hopkins Bloomberg School of Public Health Center for Immunization Research in Baltimore, and the Vaccine Testing Center at the University of Vermont in Burlington.
The challenge virus in the vaccine is an attenuated genetic chimera consisting of a dengue virus 4 backbone that expresses Zika virus surface proteins designed to elicit an immune response. The virus was previously tested in rhesus macaque monkeys.
Study participants for the phase 1 trial, Evaluation of the Safety and Immunogenicity of the Live Attenuated Zika Vaccine rZIKV/D4Δ30-713 in Flavivirus-Naive Adults, (NCT03611946) will be assessed based on local and general adverse events to the vaccine and peak neutralizing antibody titer to Zika virus as measured up to 90 days after vaccination. The trial is expected to be reach primary completion by Dec. 31, 2018.
If the phase 1 trial is successful, the goal is to integrate the vaccine with a live, attenuated dengue vaccine candidate called TV003, which is designed to elicit antibodies against all four dengue virus serotypes. The TV003 experimental vaccine is currently under evaluation in a phase 3 clinical trial (NCT02406729) underway in Brazil. Both Zika and dengue viruses frequently are endemic in the same regions and a single vaccine against both diseases would be valued. Stephen Whitehead, PhD of NIAID’s Laboratory of Viral Diseases led the efforts to develop both experimental vaccines.
SOURCE: NIH, August 16, 2018. News Release.
Vascular training for general surgery residents continues downward trend
Operative experience in open arterial vascular surgery procedures for general surgery residents has significantly declined, according to the results of a study of the Accreditation Council for Graduate Medical Education (ACGME) national case log reports, which lists the mean numbers of operations performed.
“Because fundamental vascular surgery skills are necessary for operative general surgery, vascular surgery should remain an essential content area. However, programs cannot solely depend on operative experience to teach fundamental vascular surgery skills,” John R. Potts III, MD, FACS, and R. James Valentine, MD, FACS, stated in their report published online in Annals of Surgery.
The number of individuals completing ACGME-accredited general surgery and vascular surgery training each year of the study was obtained from public reports of the ACGME as well as the available summary national data regarding the reported operative experience of residents completing general surgery programs.
The researchers found that over 15 years (academic year 2001-2002 through AY 2016-2017), the total vascular operations performed by general surgery residents significantly declined as did the total open arterial vascular procedures, including those in seven of nine categories (P less than .0001).
The issue of adequate exposure to vascular procedures for general surgery residents is complex. “The number of individuals completing general surgery residency annually has increased by approximately 20% since AY 2001-2. During the same period, the number of open arterial operations reported by general surgery residents decreased by approximately 38%. Thus, the declining experience is clearly not simply a matter of distributing the same number of operations to a larger number of individuals,” the investigators reported.
The ACGME-designated “essential content areas” have increased in recent years for general surgery trainees to now encompass alimentary tract, abdomen, breast, head and neck, endocrine system, the surgical management of trauma, soft tissues, pediatric surgery, surgical critical care, surgical oncology, and vascular surgery. The essential content areas compete to varying degrees for the trainee’s time, potentially cutting into not just vascular cases but other areas as well. It is also the case that general surgery trainees are often in an institutional setting where they are competing with vascular surgery residents for the same pool of vascular surgery patients.
During those last 5 years, significant declines occurred in five categories: aneurysm, cerebrovascular disease, arteriovenous dialysis access, peripheral vascular disease, and extra-anatomic bypass, according to the authors.
“Knowledge of arterial anatomy, approaches, control, and repair are crucial to the practice of operative general surgery. In the face of declining experience for their resident as surgeon in open arterial operations, general surgery programs must augment resident education in the principles of vascular surgery through other means,” the authors concluded.
Portions of this study were presented at the2018 meeting of the American Surgical Association.
Dr. Potts and Dr. Valentine reported that they had no conflicts of interest.
SOURCE: Potts JR et al. Ann Surg. 2018 Jul 24. doi: 10.1097/SLA.0000000000002951.
In the role of discussant at the American Surgical Association meeting where this research was presented, K. Craig Kent, MD, a vascular surgeon and former president of the Society for Vascular Surgery, stated: “We don’t have enough open arterial cases to teach our general surgery residents. There is a problem on the other side, too, which is we don’t have enough open arterial cases to teach our vascular surgeons to be confident, open, vascular surgeons. What’s my solution? ... we need to share. We should take the opportunity whenever there’s a great arterial case to have everybody, vascular and general surgery trainees, participate,” he stated.
In the role of discussant at the American Surgical Association meeting where this research was presented, K. Craig Kent, MD, a vascular surgeon and former president of the Society for Vascular Surgery, stated: “We don’t have enough open arterial cases to teach our general surgery residents. There is a problem on the other side, too, which is we don’t have enough open arterial cases to teach our vascular surgeons to be confident, open, vascular surgeons. What’s my solution? ... we need to share. We should take the opportunity whenever there’s a great arterial case to have everybody, vascular and general surgery trainees, participate,” he stated.
In the role of discussant at the American Surgical Association meeting where this research was presented, K. Craig Kent, MD, a vascular surgeon and former president of the Society for Vascular Surgery, stated: “We don’t have enough open arterial cases to teach our general surgery residents. There is a problem on the other side, too, which is we don’t have enough open arterial cases to teach our vascular surgeons to be confident, open, vascular surgeons. What’s my solution? ... we need to share. We should take the opportunity whenever there’s a great arterial case to have everybody, vascular and general surgery trainees, participate,” he stated.
Operative experience in open arterial vascular surgery procedures for general surgery residents has significantly declined, according to the results of a study of the Accreditation Council for Graduate Medical Education (ACGME) national case log reports, which lists the mean numbers of operations performed.
“Because fundamental vascular surgery skills are necessary for operative general surgery, vascular surgery should remain an essential content area. However, programs cannot solely depend on operative experience to teach fundamental vascular surgery skills,” John R. Potts III, MD, FACS, and R. James Valentine, MD, FACS, stated in their report published online in Annals of Surgery.
The number of individuals completing ACGME-accredited general surgery and vascular surgery training each year of the study was obtained from public reports of the ACGME as well as the available summary national data regarding the reported operative experience of residents completing general surgery programs.
The researchers found that over 15 years (academic year 2001-2002 through AY 2016-2017), the total vascular operations performed by general surgery residents significantly declined as did the total open arterial vascular procedures, including those in seven of nine categories (P less than .0001).
The issue of adequate exposure to vascular procedures for general surgery residents is complex. “The number of individuals completing general surgery residency annually has increased by approximately 20% since AY 2001-2. During the same period, the number of open arterial operations reported by general surgery residents decreased by approximately 38%. Thus, the declining experience is clearly not simply a matter of distributing the same number of operations to a larger number of individuals,” the investigators reported.
The ACGME-designated “essential content areas” have increased in recent years for general surgery trainees to now encompass alimentary tract, abdomen, breast, head and neck, endocrine system, the surgical management of trauma, soft tissues, pediatric surgery, surgical critical care, surgical oncology, and vascular surgery. The essential content areas compete to varying degrees for the trainee’s time, potentially cutting into not just vascular cases but other areas as well. It is also the case that general surgery trainees are often in an institutional setting where they are competing with vascular surgery residents for the same pool of vascular surgery patients.
During those last 5 years, significant declines occurred in five categories: aneurysm, cerebrovascular disease, arteriovenous dialysis access, peripheral vascular disease, and extra-anatomic bypass, according to the authors.
“Knowledge of arterial anatomy, approaches, control, and repair are crucial to the practice of operative general surgery. In the face of declining experience for their resident as surgeon in open arterial operations, general surgery programs must augment resident education in the principles of vascular surgery through other means,” the authors concluded.
Portions of this study were presented at the2018 meeting of the American Surgical Association.
Dr. Potts and Dr. Valentine reported that they had no conflicts of interest.
SOURCE: Potts JR et al. Ann Surg. 2018 Jul 24. doi: 10.1097/SLA.0000000000002951.
Operative experience in open arterial vascular surgery procedures for general surgery residents has significantly declined, according to the results of a study of the Accreditation Council for Graduate Medical Education (ACGME) national case log reports, which lists the mean numbers of operations performed.
“Because fundamental vascular surgery skills are necessary for operative general surgery, vascular surgery should remain an essential content area. However, programs cannot solely depend on operative experience to teach fundamental vascular surgery skills,” John R. Potts III, MD, FACS, and R. James Valentine, MD, FACS, stated in their report published online in Annals of Surgery.
The number of individuals completing ACGME-accredited general surgery and vascular surgery training each year of the study was obtained from public reports of the ACGME as well as the available summary national data regarding the reported operative experience of residents completing general surgery programs.
The researchers found that over 15 years (academic year 2001-2002 through AY 2016-2017), the total vascular operations performed by general surgery residents significantly declined as did the total open arterial vascular procedures, including those in seven of nine categories (P less than .0001).
The issue of adequate exposure to vascular procedures for general surgery residents is complex. “The number of individuals completing general surgery residency annually has increased by approximately 20% since AY 2001-2. During the same period, the number of open arterial operations reported by general surgery residents decreased by approximately 38%. Thus, the declining experience is clearly not simply a matter of distributing the same number of operations to a larger number of individuals,” the investigators reported.
The ACGME-designated “essential content areas” have increased in recent years for general surgery trainees to now encompass alimentary tract, abdomen, breast, head and neck, endocrine system, the surgical management of trauma, soft tissues, pediatric surgery, surgical critical care, surgical oncology, and vascular surgery. The essential content areas compete to varying degrees for the trainee’s time, potentially cutting into not just vascular cases but other areas as well. It is also the case that general surgery trainees are often in an institutional setting where they are competing with vascular surgery residents for the same pool of vascular surgery patients.
During those last 5 years, significant declines occurred in five categories: aneurysm, cerebrovascular disease, arteriovenous dialysis access, peripheral vascular disease, and extra-anatomic bypass, according to the authors.
“Knowledge of arterial anatomy, approaches, control, and repair are crucial to the practice of operative general surgery. In the face of declining experience for their resident as surgeon in open arterial operations, general surgery programs must augment resident education in the principles of vascular surgery through other means,” the authors concluded.
Portions of this study were presented at the2018 meeting of the American Surgical Association.
Dr. Potts and Dr. Valentine reported that they had no conflicts of interest.
SOURCE: Potts JR et al. Ann Surg. 2018 Jul 24. doi: 10.1097/SLA.0000000000002951.
FROM ANNALS OF SURGERY
Key clinical point: General surgery residents may need more open vascular experience.
Major finding: The number of open arterial operations reported by general surgery residents has decreased by approximately 38% since academic year 2001-2002.
Study details: An analysis of 15 years of ACGME resident national case load reports.
Disclosures: Dr. Potts and Dr. Valentine reported that they had no conflicts of interest.
Source: Potts JR III et al. Ann Surg. 2018 Jul 24. doi: 10.1097/SLA.0000000000002951.
CDC supports Ebola response in DRC
The Centers for Disease Control and Prevention has been working with the Ministry of Health of the Democratic Republic of the Congo (DRC) on a new Ebola outbreak reported on Aug, 1, 2018, in North Kivu province.
“For the current outbreak, CDC has deployed experienced Ebola experts to DRC and the World Health Organization [WHO] to provide guidance on coordination of outbreak response, laboratory testing, disease contact tracing, infection control, and health communication,” according to a CDC press release.
The CDC’s online response also provides a Traveler’s Health notice of Watch Level 1 for the DRC, which advises standard precautions and avoiding infected individuals, but not an advisory against travel.
The Ebola virus associated with the current outbreak is Zaire ebolavirus, according to genetic testing by scientists in the DRC. This is the same species that caused an outbreak earlier this year in Equateur province in northwestern DRC, although differences between the genes of the viruses suggest the two outbreaks are not linked, according to the CDC media announcement.
As of Aug. 12, 2018, the following statistics were reported by the WHO on the outbreak:
- Confirmed cases: 30
- Probable cases: 27
- Total cases: 57
- Deaths: 41 (14 confirmed, 27 probable)
The outbreak is of particular concern because of the instability of the area, which hampers relief and quarantine efforts. The outbreak is in a part of the country identified by the U.S. State Department as a “restricted travel” zone due to armed conflict and violence targeting civilians, according to the CDC.
The Centers for Disease Control and Prevention has been working with the Ministry of Health of the Democratic Republic of the Congo (DRC) on a new Ebola outbreak reported on Aug, 1, 2018, in North Kivu province.
“For the current outbreak, CDC has deployed experienced Ebola experts to DRC and the World Health Organization [WHO] to provide guidance on coordination of outbreak response, laboratory testing, disease contact tracing, infection control, and health communication,” according to a CDC press release.
The CDC’s online response also provides a Traveler’s Health notice of Watch Level 1 for the DRC, which advises standard precautions and avoiding infected individuals, but not an advisory against travel.
The Ebola virus associated with the current outbreak is Zaire ebolavirus, according to genetic testing by scientists in the DRC. This is the same species that caused an outbreak earlier this year in Equateur province in northwestern DRC, although differences between the genes of the viruses suggest the two outbreaks are not linked, according to the CDC media announcement.
As of Aug. 12, 2018, the following statistics were reported by the WHO on the outbreak:
- Confirmed cases: 30
- Probable cases: 27
- Total cases: 57
- Deaths: 41 (14 confirmed, 27 probable)
The outbreak is of particular concern because of the instability of the area, which hampers relief and quarantine efforts. The outbreak is in a part of the country identified by the U.S. State Department as a “restricted travel” zone due to armed conflict and violence targeting civilians, according to the CDC.
The Centers for Disease Control and Prevention has been working with the Ministry of Health of the Democratic Republic of the Congo (DRC) on a new Ebola outbreak reported on Aug, 1, 2018, in North Kivu province.
“For the current outbreak, CDC has deployed experienced Ebola experts to DRC and the World Health Organization [WHO] to provide guidance on coordination of outbreak response, laboratory testing, disease contact tracing, infection control, and health communication,” according to a CDC press release.
The CDC’s online response also provides a Traveler’s Health notice of Watch Level 1 for the DRC, which advises standard precautions and avoiding infected individuals, but not an advisory against travel.
The Ebola virus associated with the current outbreak is Zaire ebolavirus, according to genetic testing by scientists in the DRC. This is the same species that caused an outbreak earlier this year in Equateur province in northwestern DRC, although differences between the genes of the viruses suggest the two outbreaks are not linked, according to the CDC media announcement.
As of Aug. 12, 2018, the following statistics were reported by the WHO on the outbreak:
- Confirmed cases: 30
- Probable cases: 27
- Total cases: 57
- Deaths: 41 (14 confirmed, 27 probable)
The outbreak is of particular concern because of the instability of the area, which hampers relief and quarantine efforts. The outbreak is in a part of the country identified by the U.S. State Department as a “restricted travel” zone due to armed conflict and violence targeting civilians, according to the CDC.