User login
Triple Therapy
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Antibiotics after drainage of uncomplicated skin abscesses
- Clopidogrel vs. combined aspirin-dipyridamole for acute ischemic stroke
- BNP-guided therapy in chronic heart failure outpatients
- Cognitive decline and dementia after hospitalization
- Clopidogrel delays up risks for DES implantation patients
- Clinical score identifies prolonged length of stay
- Time to therapy reduces mortality in sepsis patients
- PEEP associated with lower mortality for ARDS patients
Antibiotics Might Be Unnecessary after Drainage of Uncomplicated Skin Abscesses
Clinical question: Does trimethoprim/sulfamethoxazole (TMP/SMX) treatment after drainage of a skin abscess reduce treatment failure at seven days or development of new lesions at 30 days?
Background: Community ac-quired methicillin-resistant Staphylococcus aureus (MRSA) skin abscesses are increasing in frequency. The benefit of antibiotic treatment after incision and drainage is not clear, as there is a high cure rate without antibiotics.
Study design: Multicenter, double-blinded, randomized, placebo-controlled trial.
Setting: Four military EDs treating civilians and military patients.
Synopsis: The study enrolled a convenience sample of 220 patients, each of whom presented to EDs with uncomplicated skin abscesses from November 2007 to June 2009. Abscesses were drained in the ED, then patients were randomized to either placebo or to TMP/SMX (two DS tablets twice daily) for seven days. Re-evaluation for wound checks occurred at two days and seven days.
Treatment failure at seven days, defined as worsening infection, new lesions, or absence of clinical improvement, occurred in 26% of placebo patients and 17% of patients in the treatment arm, a nonsignificant difference (P=0.12). Fewer patients in the treatment arm had new lesions at 30 days (28% vs. 9%, P=0.02). MRSA was cultured from 53% of patients overall; all samples were sensitive to TMP/SMX.
The study was limited by the fact that only 69% of patients were evaluated at 30 days.
Bottom line: TMP/SMX treatment of uncomplicated skin abscess after drainage in EDs does not decrease treatment failure at seven days, but might decrease the development of new lesions.
Citation: Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection [published online ahead of print March 29, 2010]. Ann Emerg Med. doi:10.1016/j.annemerg med.2010.03.002.
Clopidogrel and Combined Aspirin-Dipyridamole Have Similar Safety and Efficacy Profiles for Acute Ischemic Stroke
Clinical question: What is the efficacy and safety of combined aspirin and extended-release dipyridamole (Asp/ER-DP) compared to clopidogrel in patients with acute ischemic stroke?
Background: Long-term antiplatelet therapy is effective at reducing recurrence after ischemic stroke. However, the relative safety and efficacy of Asp/ER-DP or clopidogrel is not known in patients with acute ischemic stroke.
Study design: Randomized, controlled trial.
Setting: A multicenter trial involving 695 sites in 35 countries.
Synopsis: This post-hoc subgroup analysis of the PRoFESS (Prevention Regimen for Effectively Avoiding Second Strokes) trial assessed the relative safety and efficacy of Asp/ER-DP versus clopidogrel administered within 72 hours of stroke onset in 1,360 patients. The primary endpoint was functional outcome at 30 days.
Secondary outcomes included symptomatic hemorrhagic transformation of the infarct, cerebral edema, recurrent stroke, myocardial infarction (MI), composite vascular events (combination of nonfatal stroke, nonfatal MI, and vascular death), death, cognition, bleeding, and serious adverse events studied at seven, 30, and 90 days.
Combined death or dependency did not differ between treatment groups. Nonsignificant trends to reduced recurrence and vascular events were present with Asp/ER-DP. Rates of death, major bleeding, and serious adverse events did not differ between treatment groups.
Bottom line: Either clopidogrel or combined aspirin and extended-release dipyridamole can be used to treat acute ischemic stroke, with similar outcomes and safety profiles.
Citation: Bath PM, Cotton D, Martin RH, et al. Effect of combined aspirin and extended-release dipyridamole versus clopidogrel on functional outcome and recurrence in acute, mild ischemic stroke: PRoFESS subgroup analysis. Stroke. 2010;41(4):732-738.
BNP-Guided Therapy Reduces All-Cause Mortality in Outpatients with Chronic Heart Failure
Clinical question: Is there a clinical benefit in using B-type natriuretic peptide (BNP) to guide adjustment of proven medications in chronic heart failure?
Background: BNP is secreted by the heart in response to increased volume. It has been shown to be useful in the diagnosis of decompensated heart failure, and it can be decreased by treatment with proven heart failure medications. It is unclear if this effect provides clinical benefit on mortality and hospitalization.
Study design: Meta-analysis of prospective randomized controlled trials.
Setting: Eight studies involving 1,726 patients, published internationally from 2005-2009.
Synopsis: Study sizes ranged from 41 to 499 patients, with three- to 24-month follow-up. Patients had New York Heart Association (NYHA) class II or greater heart failure, with ejection fractions <50%.
All-cause mortality was significantly lower in BNP-guided therapy compared with clinical-guided therapy (RR=0.76; 95% CI, 0.63-0.91; P=0.003), specifically in patients younger than 75 years old (RR=0.52; 95% CI, 0.33-0.82; P=0.005).
A proposed mechanism for this result was a statistically significant increase in adjustment of most heart failure medications for BNP-guided therapy compared with clinical-guided therapy (75% vs. 58%, P<0.001 in diuretics; 49.6% vs. 30.9%, P<0.001 in ACE inhibitors or Angiotensin II receptor blockers (ARBs); and 51.1% vs. 41.6%, P=0.02 in beta-blockers) and a higher percentage reaching target doses in the BNP-guided therapy group. However, there was no significant decrease in all-cause hospitalization or survival free of hospitalization.
The study limitations include: Hospitalization for heart failure was not meta-analyzed, the pooled data were weighted toward one study, and BNP-guided titration parameters varied across studies.
Bottom line: BNP-guided therapy reduces all-cause mortality in chronic heart failure patients younger than 75 years old, but not all-cause hospitalization or survival free of hospitalization.
Citation: Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: A meta-analysis. Arch Intern Med. 2010;170(6):507-514.
Hospitalization Is Associated with Cognitive Decline and Subsequent Risk for Dementia in the Elderly
Clinical question: Is critical illness in patients 65 and older associated with long-term cognitive impairment, and does it affect the incidence of dementia?
Background: There is literature suggesting that survivors of critical illness suffer long-term cognitive impairment, but premorbid measures of cognitive function have not been researched. No studies have evaluated the risk of incident dementia among this patient population.
Study design: Prospective cohort study.
Setting: Group Health Cooperative in Seattle.
Synopsis: This study analyzed data from 2,929 community-dwelling adults older than 65 without baseline dementia. From 1994 to 2007, the individuals were screened with the Cognitive Abilities Screening Instrument (CASI) at follow-up visits every two years. CASI scores lower than 86 (out of 100) led to an examination for dementia; the diagnosis of dementia was an outcome measure. Scores were adjusted for baseline cognitive scores, age, and other risk factors.
For patients following acute-care hospitalization, adjusted CASI scores were 1.01 points lower on average than for those not hospitalized. For patients following critical-illness hospitalization, scores were 2.14 points lower. The dementia rate was 14.6 cases per 1,000 person-years among patients not hospitalized, and 33.6 among those admitted for noncritical illness.
As suspected, hospitalization might be a marker for cognitive decline in the elderly after adjusting for premorbid CASI scores and comorbid illness. Some factors in acute illness—and moreso in critical illness—might be causally related to cognitive decline.
Bottom line: In elderly patients without dementia at baseline, hospitalization for acute care and critical illness increases the likelihood of cognitive decline compared with patients who were not hospitalized. Only noncritical-illness hospitalization was not associated with the development of dementia.
Citation: Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA. 2010;303(8): 763-770.
Increased Risk of Death and Myocardial Infarction in Patients Who Delay Filling Clopidogrel Prescription after Drug-Eluting Stent Implantation
Clinical question: Is there an increased risk of death or myocardial infarction (MI) in patients with recent drug-eluting stent (DES) implantation who delayed filling their clopidogrel prescription compared with those who filled their prescription on the day of hospital discharge?
Background: Filling an initial prescription of clopidogrel on the day of discharge is important after DES implantation, as prior studies suggest that lack of thienopyridine therapy is a risk factor for early stent thrombosis.
Study design: Retrospective cohort study.
Setting: Three large, integrated healthcare systems.
Synopsis: The cohort included 7,042 patients discharged after DES implantation. Filling of a clopidogrel prescription was based on pharmacy dispensing data. Primary analysis divided patients based on whether they filled the prescription on the day of discharge or any time after discharge. Secondary analysis further characterized delays as >1 day, >3 days, or >5 days after discharge.
One in 6 patients delayed filling the initial prescription. Patients with any degree of delay had significantly higher death and MI rates during follow-up (14.2% vs. 7.9%, P<0.001), as well as an increased risk of death/MI (hazard ratio 1.53; 95% CI, 1.25-1.87). Factors associated with a delay in filling clopidogrel included older age, prior MI, diabetes, renal dysfunction, prior revascularization, cardiogenic shock, in-hospital bleeding, and use of clopidogrel upon admission.
The study was limited in that data were based on pharmacy records, and that patients might have received medication at discharge or outside the healthcare system.
Bottom line: The delay in filling a clopidogrel prescription is associated with an increased risk of death and MI in patients with recent DES implantation.
Citation: Ho PM, Tsai TT, Maddox TM, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes. 2010;3(3):261-266.
Predicting Length of Stay after Stroke
Clinical question: Does a clinical score accurately predict prolonged length of stay after stroke?
Background: Stroke is a costly health problem, and length of stay is the most prominent factor contributing to the high costs. The factors leading to prolonged length of stay are varied, and there are no established tools to predict length of stay.
Study design: Prospective cohort study.
Setting: All 28 Israeli hospitals that admit stroke patients.
Synopsis: All patients admitted to Israeli hospitals during established two-month periods in 2004 (1,700 patients) and 2007 (1,648 patients) were included in the National Acute Stroke Israeli Survey (NASIS), and served as the derivation and validation cohort for development of a Prolonged Length of Stay (PLOS) score.
Using the 2004 data, investigators identified stroke severity using the National Institutes of Health Stroke Scale (NIHSS), history of congestive heart failure (CHF), history of atrial fibrillation, decreased level of consciousness on presentation, and intracerebral hemorrhage (as opposed to ischemic stroke) as predictors of prolonged length of stay. Four of these factors were expressed as dichotomous variables, whereas the stroke severity by NIHSS class was incorporated as a range; all were incorporated into a PLOS score.
Higher PLOS score correlated with longer length of stay. In the derivation cohort, 22% of patients with a PLOS score of 0 had a prolonged length of stay, whereas 85% of patients with PLOS scores of 6 or 7 had a prolonged length of stay. In the validation cohort, the corresponding figures were 19% and 72%.
Bottom line: Use of a simple score can predict risk of prolonged length of stay after stroke.
Citation: Koton S, Bornstein NM, Tsabari R, Tanne D, NASIS Investigators. Derivation and validation of the prolonged length of stay score in acute stroke patients. Neurology. 2010;74(19);1511-1516.
Earlier Administration of Appropriate Antimicrobials Decreases Mortality in Patients with Severe Sepsis and Septic Shock
Clinical question: Is the timing of antimicrobial administration an important determinant of survival in patients diagnosed with severe sepsis and septic shock?
Background: Severe sepsis and septic shock are associated with a 25% to 50% mortality rate. Early goal-directed therapy has been shown to increase survival in these patients. Antimicrobial treatment is a mainstay of this therapy, but the most effective timing of this treatment remains unclear.
Study design: Retrospective, single-center cohort study.
Setting: ED at an academic tertiary-care center.
Synopsis: Two hundred sixty-one patients in the ED in 2005-2006 presenting with severe sepsis or septic shock were enrolled in the hospital’s early goal-directed therapy (EGDT) algorithm, either at triage or later during their ED stay. Labs showed 56.7% of patients were culture-positive, with the most common sources being respiratory (30.6%), genitourinary (22.8%), and gastrointestinal (19.7%).
All patients received antibiotics and were stratified in one-hour intervals by the following categories: time from triage to antibiotics; time from qualification for EGDT to antibiotics; time from triage to appropriate antibiotics; and time from qualification for EGDT to appropriate antibiotics.
Total in-hospital mortality was 31% (35.1% for culture-positive patients vs. 25.7% for culture-negative patients, P=0.11). A significant decrease in mortality was only found when appropriate antibiotics were administered within one hour of triage, or within one hour of qualification for EGDT (OR=0.30; 95% CI, 0.11-0.83; P=0.02, and OR=0.50; 95% CI, 0.27-0.92; P=0.03, respectively).
Study limitations included the single-center site and small sample size.
Bottom line: In patients with severe sepsis and septic shock, initiating appropriate antimicrobial therapy within one hour of triage or entry into goal-directed therapy significantly reduces mortality.
Citation: Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045-1053.
Treatment with Higher Levels of Positive End-Expiratory Pressure Has Limited Affect on Hospital Survival
Clinical question: Is treatment with higher versus lower levels of positive end-expiratory pressure (PEEP) associated with improved hospital survival?
Background: In the management of patients with acute lung injury or acute respiratory distress syndrome (ARDS), a fundamental goal is to protect the lungs from ventilation-induced injury, but the optimal PEEP level has not been established.
Study design: Systematic review and meta-analysis.
Setting: N/A.
Synopsis: Three randomized-controlled trials eligible for this review included 2,299 critically ill adults with acute lung injury, as defined by the American-European Consensus Conference. The meta-analysis compared higher and lower PEEP levels with a mean difference of at least 3 cm H2O, incorporated a target tidal volume of less than 8 mL/kg of predicted body weight in both ventilation strategies, and provided patient follow-up until death or for at least 20 days.
This review demonstrated no statistically significant difference in hospital mortality between the groups. However, in patients with ARDS, higher levels of PEEP were associated with a relative reduction in mortality of 10%. This is supported by a recent cohort study in patients with acute lung injury or ARDS, which showed that the effect of PEEP on lung recruitment was associated with the proportion of potentially recruitable lung, as determined by computed tomography.
Since patients with ARDS have more pulmonary edema than those with acute lung injury without ARDS, the former have greater recruitability, and thus might benefit more from higher levels of PEEP.
Bottom line: Higher levels of PEEP might be associated with lower hospital mortality in patients with ARDS, but such a benefit is unlikely in patients with less severe lung injuries, and could actually be harmful.
Citation: Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865-873. TH
A Pain in the Bone
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
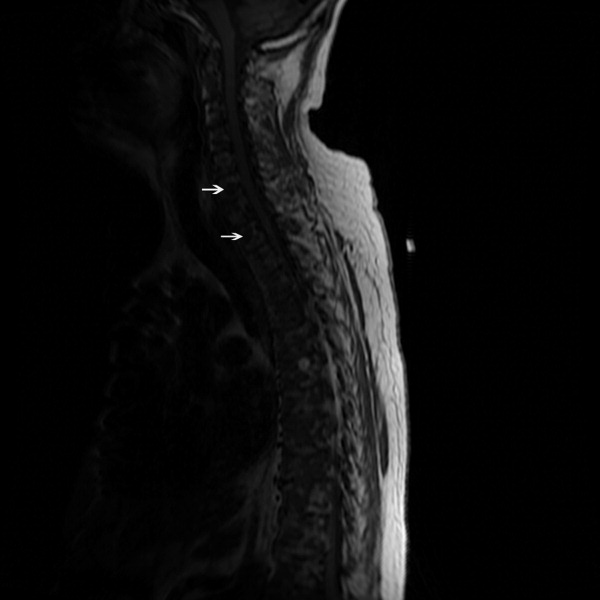
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

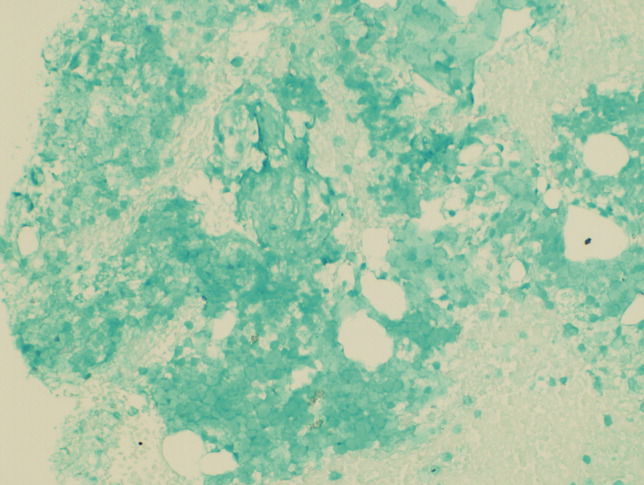
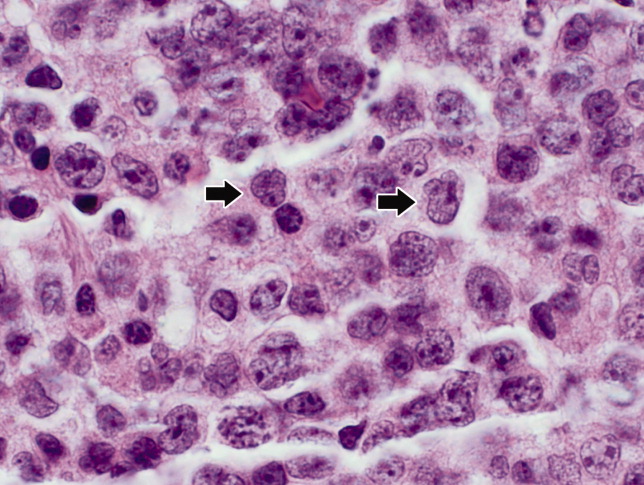
The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
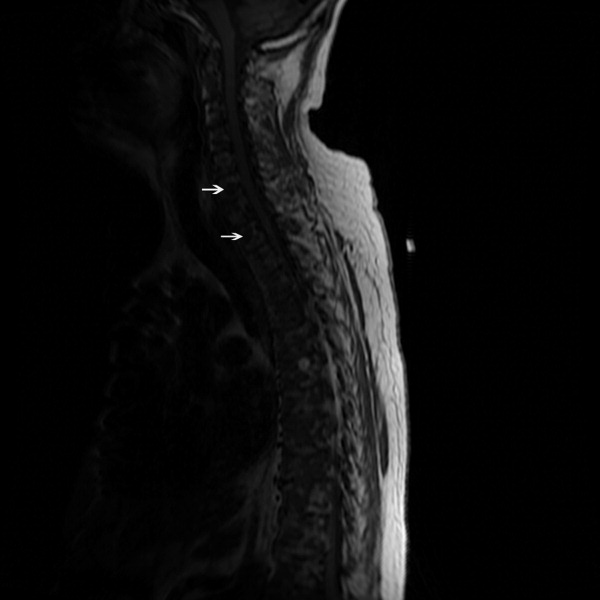
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

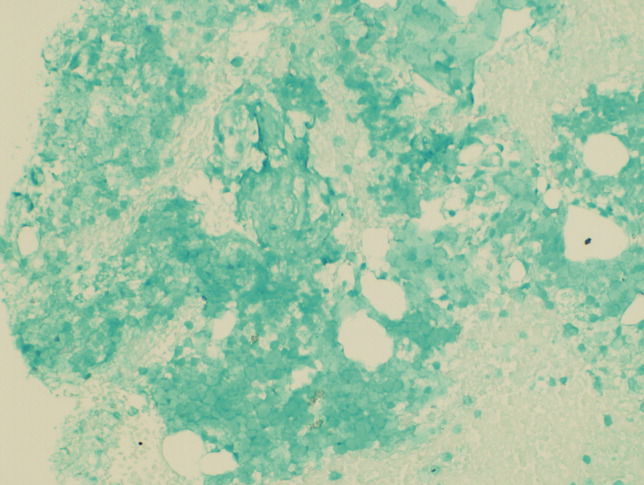
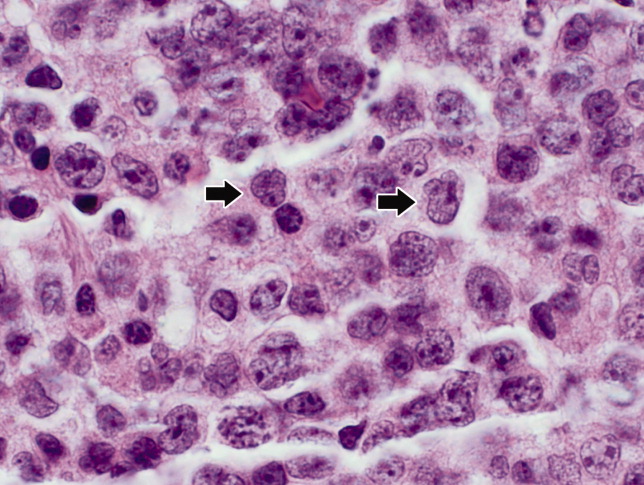
The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
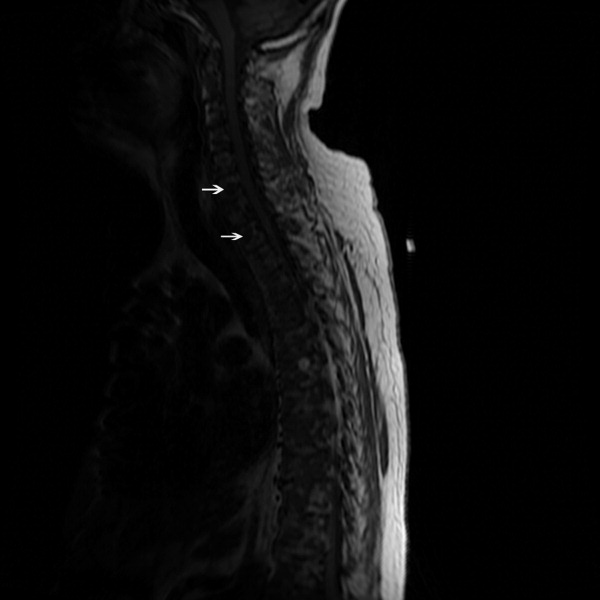
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
In the Literature
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH