User login
Updates in Perioperative Medicine
Given the rapid expansion of the field of perioperative medicine, clinicians need to remain apprised of the current evidence to ensure optimization of patient care. In this update, we review 10 key articles from the perioperative literature, with the goal of summarizing the most clinically important evidence over the past year. This summary of recent literature in perioperative medicine is derived from the Update in Perioperative Medicine sessions presented at the 10th Annual Perioperative Medicine Summit and the Society of General Internal Medicine 38th Annual Meeting. A systematic search strategy was used to identify pertinent articles, and the following were selected by the authors based on their relevance to the clinical practice of perioperative medicine.
PERIOPERATIVE CARDIOVASCULAR CARE
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;130:e278e333.
Background
The American College of Cardiology/American Heart Association (ACC/AHA) perioperative guideline provides recommendations for the evaluation and management of cardiovascular disease in patients undergoing noncardiac surgery.
Findings
The new guideline combines the evaluation of surgery‐ and patient‐specific risk in the algorithm for preoperative cardiovascular evaluation into a single step and recommends the use of 1 of 3 tools: the Revised Cardiac Risk Index (RCRI),[1] National Surgical Quality Improvement Program (NSQIP) Surgical Risk Calculator,[2] or the NSQIP‐derived myocardial infarction and cardiac arrest calculator.[3] Estimation of risk is also simplified by stratification into only 2 groups: low risk (risk of major adverse cardiac event 1%) and elevated risk (1% risk). Coronary evaluation can be considered for patients with elevated cardiac risk and poor functional capacity, but is advised only if the results would alter perioperative management. For example, a patient with very high risk who has evidence of ischemia on stress testing may choose to forego surgery. Preoperative coronary revascularization is only indicated for patients meeting criteria in the nonsurgical setting.
For patients with previous percutaneous coronary intervention, the ACC/AHA has not changed its recommendations to optimally delay surgery for at least 30 days after bare‐metal stenting and at least 1 year after drug‐eluting stent (DES) placement. However, in patients with a DES placed 6 to 12 months previously, surgery can be performed if the risks of surgical delay outweigh the risks of DES thrombosis. After any type of coronary stenting, dual antiplatelet therapy should be continued uninterrupted through the first 4 to 6 weeks and even later whenever feasible. If not possible, aspirin therapy should be maintained through surgery unless bleeding risk is too high.
The guideline recommends perioperative continuation of ‐blockers in patients taking them chronically. Preoperative initiation of ‐blocker therapy may be considered for patients with myocardial ischemia on stress testing or 3 RCRI factors and should be started far enough in advance to allow determination of patient's tolerance prior to surgery.
Cautions
Many recommendations are based on data from nonrandomized trials or expert opinion, and the data in areas such as perioperative ‐blockade continue to evolve.
Implications
The ACC/AHA guideline continues to be a critically valuable resource for hospitalists providing perioperative care to noncardiac surgery patients.
Wijeysundera DN, Duncan D, Nkonde‐Price C, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines.
J Am Coll Cardiol. 2014;64(22):24062425.
Background
Various clinical trials have reported conflicting results regarding the efficacy and safety of perioperative ‐blockers resulting in guideline committees changing their recommendations. Because of questions raised regarding the scientific integrity of the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography)‐I[4] and DECREASE‐IV[5] trials as well as the dosing of ‐blockers in POISE (PeriOperative Ischemic Evaluation) study,[6] this systematic review was performed in conjunction with the ACC/AHA guideline update[7] to evaluate the data with and without these trials.
Findings
Sixteen randomized control trials (RCTs) (n=12,043) and 1 cohort study (n=348) were included in the analysis. Perioperative ‐blockers were associated with a reduction in nonfatal myocardial infarction (MI) (relative risk [RR]: 0.69; 95% confidence interval [CI]: 0.58‐0.82; P0.001) but an increase in bradycardia (RR: 2.61; 95% CI: 2.18‐3.12), hypotension (RR: 1.47; 95% CI: 1.34‐1.6), and nonfatal strokes (RR: 1.76; 95% CI: 1.07‐2.91; P=0.02). The POISE trial was the only one demonstrating a statistically significant increase in stroke.
The major discrepancy between the DECREASE trials and the other RCTs was related to mortalitya reduction in both cardiovascular and all‐cause death in DECREASE but an increased risk of all‐cause death in the other trials.
Cautions
Because of its size, the POISE trial heavily influences the results, particularly for mortality and stroke. Including the DECREASE trials reduces the otherwise increased risk for death to a null effect. Exclusion of the POISE and DECREASE trials leaves few data to make conclusions about safety and efficacy of perioperative ‐blockade. Several cohort studies have found metoprolol to be associated with worse outcomes than with atenolol or bisoprolol (which were preferred by the European Society of Cardiology guidelines).[8]
Implications
Perioperative ‐blockade started within 1 day of noncardiac surgery was associated with fewer nonfatal MIs but at the cost of an increase in hypotension, bradycardia, and a possible increase in stroke and death. Long‐term ‐blockade should be continued perioperatively, whereas the decision to initiate a ‐blocker should be individualized. If starting a ‐blocker perioperatively, it should be done 2 days before surgery.
Botto F, Alonso‐Coello P, Chan MT, et al.; on behalf of The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Investigators. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30‐day outcomes. Anesthesiology. 2014;120(3):564578.
Background
Many patients sustain myocardial injury in the perioperative period as evidenced by troponin elevations, but most do not meet diagnostic criteria for MI. Myocardial injury after noncardiac surgery (MINS) is defined as prognostically relevant myocardial injury due to ischemia that occurs within 30 days after noncardiac surgery. This international, prospective cohort study of 15,065 patients 45 years old who underwent in‐patient noncardiac surgery determined diagnostic criteria, characteristics, predictors, and 30‐day outcomes of MINS.
Findings
The diagnostic criterion for MINS was a peak troponin T level 0.03 ng/mL judged to be due to an ischemic etiology. Twelve independent predictors of MINS were identified including age 75 years, known cardiovascular disease or risk factors, and surgical factors. MINS was an independent predictor of 30‐day mortality (adjusted hazard ratio [HR]: 3.87; 95% CI: 2.96‐5.08). Age >75 years, ST elevation, or new left bundle branch block, and anterior ischemic findings were independent predictors of 30‐day mortality among patients with MINS.
Cautions
Although screening high‐risk surgical patients without signs or symptoms of ischemia with postoperative troponins will increase the frequency of diagnosing MINS, evidence for an effective treatment has not yet been established. The ACC/AHA guidelines state that routine screening is of uncertain benefit for this reason.
Implications
Because MINS is common and carries a poor 30‐day prognosis, clinical trials are needed to determine when to obtain postoperative troponins and how to prevent and treat this complication.[9] Some observational data from POISE suggest that aspirin and statins can reduce the risk of 30‐day mortality in patients with postoperative MIs.
Devereaux PJ, Mrkobrada M, Sessler DI, et al. for the POISE‐2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):14941503.
Devereaux PJ, Sessler DI, Leslie K, et al. for the POISE‐2 Investigators. Clonidine in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):15041513.
Background
Medical risk reduction with aspirin and other agents in perioperative patients remains controversial. The POISE‐2 trial is a blinded RCT examining the effects of aspirin and clonidine on outcomes in >10,000 noncardiac surgery patients at risk of cardiovascular complications. The aspirin arm of the study included the initiation group and the continuation stratum, as well as placebo. Patients in the clonidine portion of the trial received 0.2 mg of clonidine or placebo daily for the same time periods.
Findings
The primary outcome was a composite of death or nonfatal MI within 30 days of surgery. Outcomes were similar in patients initiated or continued on aspirin. No difference was seen between aspirin or placebo in the primary outcome (7.0% vs 7.1%; HR: 0.86; 95% CI: 0.86‐1.15; P=0.92). There were no differences in rates of MI, venous thromboembolism, or stroke. Major bleeding rates were higher in aspirin versus placebo‐treated patients (4.6% vs 3.8%; HR: 1.23; 95% CI: 1.01‐1.49; P=0.04).
Clonidine did not alter the composite outcome of death or nonfatal MI (7.3% vs 6.8%; HR: 1.08; 95% CI: 0.93‐1.26; P=0.29). Clinically significant hypotension, bradycardia, and nonfatal cardiac arrest were more common in clonidine‐treated patients, although no difference was detected in stroke rates.
Cautions
Although patients in the trial had cardiovascular risk factors, 24% of patients had known coronary artery disease, and 5% had coronary stents. Conclusions based on this trial regarding perioperative management of antiplatelet therapy should not include patients with coronary artery stents.
Implications
Aspirin started before surgery and continued perioperatively did not decrease the rate of death or nonfatal MI but increased the risk of major bleeding. Perioperative management of aspirin needs to be undertaken in the context of cardiac and bleeding risks. Clonidine also did not improve outcomes and increased the risk of bradycardia and hypotension. Current guidelines recommend against using alpha‐2 agonists for prevention of perioperative cardiac events7; however, patients already on alpha‐2 agonists should not stop them abruptly.
PERIOPERATIVE PULMONARY CARE
Mutter TC, Chateau D, Moffatt M, et al. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121(4):707718.
Background
An increasing body of literature associates obstructive sleep apnea (OSA) with an increased risk of postoperative complications. Despite evidence of risk, potential benefits of preoperative diagnosis and treatment of OSA remain unclear.
Findings
Using databases to identify patients prescribed continuous positive airway pressure (CPAP) therapy, the study compared postoperative outcomes of patients who underwent surgery any time after polysomnography (PSG) and CPAP prescription (diagnosed OSA [DOSA]) and those who had surgery during the 5 years preceding their PSG (undiagnosed OSA [UOSA]). These patients were matched with patients who underwent the same procedure for the same indication and had no insurance claims for PSG or diagnosis of sleep‐disordered breathing.
After multivariate analysis, OSA of any type was associated with increased pulmonary complications (odds ratio [OR]: 2.08; 95% CI: 1.35‐2.19). However, no significant differences in respiratory outcomes were noted between DOSA patients (N=2640) and those with UOSA (N=1571). DOSA patients did have fewer cardiovascular complications than UOSA patients (OR: 0.34; 95% CI: 0.15‐0.77). Only severe OSA (apnea‐hypopnea index >30) was associated with increased pulmonary and cardiovascular complications.
Cautions
Although this study suggests an association between preoperative diagnosis and treatment of OSA and reduced cardiovascular complications, the results are not definitive due to the inability to control for all confounding variables in a retrospective study utilizing an administrative database.
Implications
OSA is an important risk factor for postoperative complications, and this study suggests that preoperative treatment with CPAP is associated with reduced risk of cardiovascular complications, particularly in patients with severe OSA. Future controlled trials should focus on the risk‐reduction potential of preoperative diagnosis and treatment of OSA.
Mazo V, Sabat S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219231.
Background
In 2010, Canet et al. published a novel risk index, the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) index, to provide a quantitative estimate of the risk of postoperative pulmonary complications (PPCs).[10]
In the current report, Mazo and colleagues studied the ARISCAT index in a broader sample to characterize its accuracy in predicting PPC risk. The ARISCAT index is derived from clinical risk factors: (1) age, (2) preoperative oxygen saturation, (3) respiratory infection in the prior month, (4) anemia, (5) surgical site, (6) duration of surgery, and (7) emergency surgery, with varying weights based on the strength of the association in a multivariable analysis. This score can be calculated via addition of these weighted risk factors, with a score>45 equal to high risk for PPC.
Findings
Examining 5099 patients from 63 European hospitals, the authors definition of PPC included respiratory failure, pulmonary infection, pleural effusion, atelectasis, pneumothorax, bronchospasm, and aspiration pneumonitis. PPC rates were as follows: low risk (3.39%), intermediate risk (12.98%), and high risk (38.01%). The positive likelihood ratio for PPC among the highest risk group was 7.12. The C statistic for fit was 0.80. Observed PPC rates were higher than predicted for the low (3.39% vs 0.87%) and intermediate (12.98% vs 7.82%) risk groups.
Cautions
The calibration slopes were less than ideal in all subsamples, with the Western European sample performing better than the other geographic areas; suggesting that the coefficients on the ARISCAT index may benefit from recalibration to match specific populations.
Implications
This is the first major pulmonary risk index that has been externally validated. Its use of readily available clinical information, simplicity, and accuracy in estimating PPC risk make it an important addition to the toolkit during a preoperative evaluation.
PERIOPERATIVE ATRIAL FIBRILLATION/ANTICOAGULATION
Gialdini G, Nearing K, Bhave P, et al. Perioperative atrial fibrillation and the long term risk of ischemic stroke. JAMA. 2014;312(6):616622.
Background
New‐onset atrial fibrillation (AF) is the most common perioperative arrhythmia.[11] However, little is known regarding the long‐term risks of ischemic stroke in patients who develop perioperative AF. This retrospective cohort study examined adults with no preexisting history of AF, hospitalized for surgery, and discharged free of cerebrovascular disease between 2007 and 2011 (n=1,729,360).
Findings
Of the eligible patients, 1.43% (95% CI: 1.41%‐1.45%) developed perioperative AF, and 0.81% (95% CI: 0.79%‐0.82%) had a stroke up to 1 year after discharge. Perioperative AF was associated with subsequent stroke after both cardiac (HR: 1.3; 95% CI: 1.1‐1.6) and noncardiac surgery (HR: 2; 95% CI: 1.7‐2.3). The association with stroke was stronger for perioperative AF after noncardiac versus cardiac surgery (P0.001 for interaction).
Cautions
This is a retrospective cohort study, using claims data to identify AF and stroke. Data on duration of the perioperative AF episodes or use of antithrombotic therapies were not available.
Implications
The association found between perioperative AF and long‐term risk of ischemic stroke may suggest that perioperative AF, especially after noncardiac surgery, should be treated aggressively in terms of thromboembolic risk; however, further data will be required to validate this association.
Van Diepen S, Youngson E, Ezekowitz J, McAlister F. Which risk score best predicts perioperative outcomes in nonvalvular atrial fibrillation patients undergoing noncardiac surgery? Am Heart J. 2014;168(1):6067.
Background
Patients with nonvalvular AF (NVAF) are at increased risk for adverse perioperative outcomes after noncardiac surgery.[12] The RCRI is commonly used to predict perioperative cardiovascular events for all patients, including those with NVAF, though AF is not part of this risk assessment. The goal of this retrospective cohort study was to examine the prognostic utility of already existing NVAF risk indices, including the CHADS2 (Congestive heart failure, Hypertension, Age 75 years, Diabetes mellitus, prior stroke or transient ischemic attack), CHA2DS2‐VASc (Congestive heart failure; Hypertension; Age 75 years; Diabetes mellitus; Stroke, TIA, or thromboembolism [TE]; Vascular disease; Age 65 to 74 years; Sex category [female]), and R2CHADS2 (Renal dysfunction, Congestive heart failure, Hypertension, Age, Diabetes, Stroke/TIA) for perioperative outcomes in patients undergoing noncardiac surgery.
Findings
A population dataset of NVAF patients (n=32,160) who underwent noncardiac surgery was examined, with outcome measures including 30‐day mortality, stroke, TIA, or systemic embolism. The incidence of the 30‐day composite outcome was 4.2% and the C indices were 0.65 for the RCRI, 0.67 for CHADS2, 0.67 for CHA2DS2‐VASc, and 0.68 for R2CHADS2. The Net Reclassification Index (NRI), a measure evaluating the improvement in prediction performance gained by adding a marker to a set of baseline predictors, was calculated. All NVAF scores performed better than the RCRI for predicting mortality risk (NRI: 12.3%, 8.4%, and 13.3% respectively, all P0.01).
Cautions
Patients in the highest risk category by RCRI appear to have an unadjusted higher 30‐day mortality risk (8%) than that predicted by the other 3 scores (5%, 5.6%, and 5%), indicating that these risk scores should not completely supplant the RCRI for risk stratification in this population. In addition, the overall improvement in predictive capacity of the CHADS2, CHA2DS2‐VASc, and R2CHADS2, although superior to the RCRI, is modest.
Implications
These findings indicate that the preoperative risk stratification for patients with NVAF can be improved by utilizing the CHADS2, CHA2DS2‐VASc, or R2CHADS2 scores when undergoing noncardiac surgery. For patients with NVAF identified as high risk for adverse outcomes, this assessment can be integrated into the preoperative discussion on the risks/benefits of surgery.
Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT‐AF). Circulation. 2015;131:488494
Background
Oral anticoagulation (OAC) significantly reduces the risk of stroke in patients with AF. Many AF patients on long‐term anticoagulation undergo procedures requiring temporary interruption of OAC. Although guidelines have been published on when and how to initiate bridging therapy, they are based on observational data. Thus, it remains unclear which patients should receive bridging anticoagulation.
Findings
This is a US registry of outpatients with AF with temporary interruptions of OAC for a procedure. Of 7372 patients treated with OAC, 2803 overall interruption events occurred in 2200 patients (30%). Bridging anticoagulants were used in 24% (n=665). Bleeding events were more common in bridged than nonbridged patients (5.0% vs 1.3%; adjusted OR: 3.84; P0.0001). The overall composite end point of myocardial infarction, stroke or systemic embolism, major bleeding, hospitalization, or death within 30 days was significantly higher in patients receiving bridging (13% vs 6.3%; adjusted OR: 1.94; P=0.0001). This statistically significant increase in the composite outcome, which includes cardiovascular events, is most likely in part secondary to inclusion of bleeding events. The recently published BRIDGE (Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery) trial did not find a statistically significant difference in cardiovascular events between bridged and nonbridged patients.[13]
Cautions
Although patients who were bridged appear to have had more comorbidities and a higher mean CHADS2 score than patients who were not bridged, it is difficult to determine which population of patients may be high risk enough to warrant bridging, as indicated by current American College of Chest Physicians guidelines, as this was not evaluated in this study
Implications
The use of bridging anticoagulation was significantly associated with higher overall bleeding and adverse event rates. The BRIDGE trial also found that forgoing bridging anticoagulation decreased the risk of major bleeding in patients with AF and was noninferior to bridging for the prevention of arterial TE.[13]
- , , , et al. Derivation and prospective evaluation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049.
- , , , et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842.
- , , , et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124:381–387.
- , , , et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high‐risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999;341(24):1789–1794.
- , , , et al; Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- POISE Study Group, , , , et al. Effects of extended‐release metoprolol succinate in patients undergoing non‐cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839–1847.
- , , , et al. American College of Cardiology; American Heart Association. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77–e137.
- , , , et al. 2014 ESC/ESA Guidelines on non‐cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non‐cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014;35(35):2383–431.
- , , , et al. The long‐term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053–1063.
- , , , et al. ARISCAT Group: Prediction of postoperative pulmonary complications in a population‐based surgical cohort. Anesthesiology. 2010;113:1338–1350.
- , . Noncardiac surgery: postoperative arrhythmias. Crit Care Med. 2000;28(10 suppl):N145–N150.
- , , , et al. Incidence, predictors, and outcomes associated with postoperative atrial fibrillation after major cardiac surgery. Am Heart J. 2012;164(6):918–924.
- , , , et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823–833.
Given the rapid expansion of the field of perioperative medicine, clinicians need to remain apprised of the current evidence to ensure optimization of patient care. In this update, we review 10 key articles from the perioperative literature, with the goal of summarizing the most clinically important evidence over the past year. This summary of recent literature in perioperative medicine is derived from the Update in Perioperative Medicine sessions presented at the 10th Annual Perioperative Medicine Summit and the Society of General Internal Medicine 38th Annual Meeting. A systematic search strategy was used to identify pertinent articles, and the following were selected by the authors based on their relevance to the clinical practice of perioperative medicine.
PERIOPERATIVE CARDIOVASCULAR CARE
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;130:e278e333.
Background
The American College of Cardiology/American Heart Association (ACC/AHA) perioperative guideline provides recommendations for the evaluation and management of cardiovascular disease in patients undergoing noncardiac surgery.
Findings
The new guideline combines the evaluation of surgery‐ and patient‐specific risk in the algorithm for preoperative cardiovascular evaluation into a single step and recommends the use of 1 of 3 tools: the Revised Cardiac Risk Index (RCRI),[1] National Surgical Quality Improvement Program (NSQIP) Surgical Risk Calculator,[2] or the NSQIP‐derived myocardial infarction and cardiac arrest calculator.[3] Estimation of risk is also simplified by stratification into only 2 groups: low risk (risk of major adverse cardiac event 1%) and elevated risk (1% risk). Coronary evaluation can be considered for patients with elevated cardiac risk and poor functional capacity, but is advised only if the results would alter perioperative management. For example, a patient with very high risk who has evidence of ischemia on stress testing may choose to forego surgery. Preoperative coronary revascularization is only indicated for patients meeting criteria in the nonsurgical setting.
For patients with previous percutaneous coronary intervention, the ACC/AHA has not changed its recommendations to optimally delay surgery for at least 30 days after bare‐metal stenting and at least 1 year after drug‐eluting stent (DES) placement. However, in patients with a DES placed 6 to 12 months previously, surgery can be performed if the risks of surgical delay outweigh the risks of DES thrombosis. After any type of coronary stenting, dual antiplatelet therapy should be continued uninterrupted through the first 4 to 6 weeks and even later whenever feasible. If not possible, aspirin therapy should be maintained through surgery unless bleeding risk is too high.
The guideline recommends perioperative continuation of ‐blockers in patients taking them chronically. Preoperative initiation of ‐blocker therapy may be considered for patients with myocardial ischemia on stress testing or 3 RCRI factors and should be started far enough in advance to allow determination of patient's tolerance prior to surgery.
Cautions
Many recommendations are based on data from nonrandomized trials or expert opinion, and the data in areas such as perioperative ‐blockade continue to evolve.
Implications
The ACC/AHA guideline continues to be a critically valuable resource for hospitalists providing perioperative care to noncardiac surgery patients.
Wijeysundera DN, Duncan D, Nkonde‐Price C, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines.
J Am Coll Cardiol. 2014;64(22):24062425.
Background
Various clinical trials have reported conflicting results regarding the efficacy and safety of perioperative ‐blockers resulting in guideline committees changing their recommendations. Because of questions raised regarding the scientific integrity of the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography)‐I[4] and DECREASE‐IV[5] trials as well as the dosing of ‐blockers in POISE (PeriOperative Ischemic Evaluation) study,[6] this systematic review was performed in conjunction with the ACC/AHA guideline update[7] to evaluate the data with and without these trials.
Findings
Sixteen randomized control trials (RCTs) (n=12,043) and 1 cohort study (n=348) were included in the analysis. Perioperative ‐blockers were associated with a reduction in nonfatal myocardial infarction (MI) (relative risk [RR]: 0.69; 95% confidence interval [CI]: 0.58‐0.82; P0.001) but an increase in bradycardia (RR: 2.61; 95% CI: 2.18‐3.12), hypotension (RR: 1.47; 95% CI: 1.34‐1.6), and nonfatal strokes (RR: 1.76; 95% CI: 1.07‐2.91; P=0.02). The POISE trial was the only one demonstrating a statistically significant increase in stroke.
The major discrepancy between the DECREASE trials and the other RCTs was related to mortalitya reduction in both cardiovascular and all‐cause death in DECREASE but an increased risk of all‐cause death in the other trials.
Cautions
Because of its size, the POISE trial heavily influences the results, particularly for mortality and stroke. Including the DECREASE trials reduces the otherwise increased risk for death to a null effect. Exclusion of the POISE and DECREASE trials leaves few data to make conclusions about safety and efficacy of perioperative ‐blockade. Several cohort studies have found metoprolol to be associated with worse outcomes than with atenolol or bisoprolol (which were preferred by the European Society of Cardiology guidelines).[8]
Implications
Perioperative ‐blockade started within 1 day of noncardiac surgery was associated with fewer nonfatal MIs but at the cost of an increase in hypotension, bradycardia, and a possible increase in stroke and death. Long‐term ‐blockade should be continued perioperatively, whereas the decision to initiate a ‐blocker should be individualized. If starting a ‐blocker perioperatively, it should be done 2 days before surgery.
Botto F, Alonso‐Coello P, Chan MT, et al.; on behalf of The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Investigators. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30‐day outcomes. Anesthesiology. 2014;120(3):564578.
Background
Many patients sustain myocardial injury in the perioperative period as evidenced by troponin elevations, but most do not meet diagnostic criteria for MI. Myocardial injury after noncardiac surgery (MINS) is defined as prognostically relevant myocardial injury due to ischemia that occurs within 30 days after noncardiac surgery. This international, prospective cohort study of 15,065 patients 45 years old who underwent in‐patient noncardiac surgery determined diagnostic criteria, characteristics, predictors, and 30‐day outcomes of MINS.
Findings
The diagnostic criterion for MINS was a peak troponin T level 0.03 ng/mL judged to be due to an ischemic etiology. Twelve independent predictors of MINS were identified including age 75 years, known cardiovascular disease or risk factors, and surgical factors. MINS was an independent predictor of 30‐day mortality (adjusted hazard ratio [HR]: 3.87; 95% CI: 2.96‐5.08). Age >75 years, ST elevation, or new left bundle branch block, and anterior ischemic findings were independent predictors of 30‐day mortality among patients with MINS.
Cautions
Although screening high‐risk surgical patients without signs or symptoms of ischemia with postoperative troponins will increase the frequency of diagnosing MINS, evidence for an effective treatment has not yet been established. The ACC/AHA guidelines state that routine screening is of uncertain benefit for this reason.
Implications
Because MINS is common and carries a poor 30‐day prognosis, clinical trials are needed to determine when to obtain postoperative troponins and how to prevent and treat this complication.[9] Some observational data from POISE suggest that aspirin and statins can reduce the risk of 30‐day mortality in patients with postoperative MIs.
Devereaux PJ, Mrkobrada M, Sessler DI, et al. for the POISE‐2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):14941503.
Devereaux PJ, Sessler DI, Leslie K, et al. for the POISE‐2 Investigators. Clonidine in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):15041513.
Background
Medical risk reduction with aspirin and other agents in perioperative patients remains controversial. The POISE‐2 trial is a blinded RCT examining the effects of aspirin and clonidine on outcomes in >10,000 noncardiac surgery patients at risk of cardiovascular complications. The aspirin arm of the study included the initiation group and the continuation stratum, as well as placebo. Patients in the clonidine portion of the trial received 0.2 mg of clonidine or placebo daily for the same time periods.
Findings
The primary outcome was a composite of death or nonfatal MI within 30 days of surgery. Outcomes were similar in patients initiated or continued on aspirin. No difference was seen between aspirin or placebo in the primary outcome (7.0% vs 7.1%; HR: 0.86; 95% CI: 0.86‐1.15; P=0.92). There were no differences in rates of MI, venous thromboembolism, or stroke. Major bleeding rates were higher in aspirin versus placebo‐treated patients (4.6% vs 3.8%; HR: 1.23; 95% CI: 1.01‐1.49; P=0.04).
Clonidine did not alter the composite outcome of death or nonfatal MI (7.3% vs 6.8%; HR: 1.08; 95% CI: 0.93‐1.26; P=0.29). Clinically significant hypotension, bradycardia, and nonfatal cardiac arrest were more common in clonidine‐treated patients, although no difference was detected in stroke rates.
Cautions
Although patients in the trial had cardiovascular risk factors, 24% of patients had known coronary artery disease, and 5% had coronary stents. Conclusions based on this trial regarding perioperative management of antiplatelet therapy should not include patients with coronary artery stents.
Implications
Aspirin started before surgery and continued perioperatively did not decrease the rate of death or nonfatal MI but increased the risk of major bleeding. Perioperative management of aspirin needs to be undertaken in the context of cardiac and bleeding risks. Clonidine also did not improve outcomes and increased the risk of bradycardia and hypotension. Current guidelines recommend against using alpha‐2 agonists for prevention of perioperative cardiac events7; however, patients already on alpha‐2 agonists should not stop them abruptly.
PERIOPERATIVE PULMONARY CARE
Mutter TC, Chateau D, Moffatt M, et al. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121(4):707718.
Background
An increasing body of literature associates obstructive sleep apnea (OSA) with an increased risk of postoperative complications. Despite evidence of risk, potential benefits of preoperative diagnosis and treatment of OSA remain unclear.
Findings
Using databases to identify patients prescribed continuous positive airway pressure (CPAP) therapy, the study compared postoperative outcomes of patients who underwent surgery any time after polysomnography (PSG) and CPAP prescription (diagnosed OSA [DOSA]) and those who had surgery during the 5 years preceding their PSG (undiagnosed OSA [UOSA]). These patients were matched with patients who underwent the same procedure for the same indication and had no insurance claims for PSG or diagnosis of sleep‐disordered breathing.
After multivariate analysis, OSA of any type was associated with increased pulmonary complications (odds ratio [OR]: 2.08; 95% CI: 1.35‐2.19). However, no significant differences in respiratory outcomes were noted between DOSA patients (N=2640) and those with UOSA (N=1571). DOSA patients did have fewer cardiovascular complications than UOSA patients (OR: 0.34; 95% CI: 0.15‐0.77). Only severe OSA (apnea‐hypopnea index >30) was associated with increased pulmonary and cardiovascular complications.
Cautions
Although this study suggests an association between preoperative diagnosis and treatment of OSA and reduced cardiovascular complications, the results are not definitive due to the inability to control for all confounding variables in a retrospective study utilizing an administrative database.
Implications
OSA is an important risk factor for postoperative complications, and this study suggests that preoperative treatment with CPAP is associated with reduced risk of cardiovascular complications, particularly in patients with severe OSA. Future controlled trials should focus on the risk‐reduction potential of preoperative diagnosis and treatment of OSA.
Mazo V, Sabat S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219231.
Background
In 2010, Canet et al. published a novel risk index, the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) index, to provide a quantitative estimate of the risk of postoperative pulmonary complications (PPCs).[10]
In the current report, Mazo and colleagues studied the ARISCAT index in a broader sample to characterize its accuracy in predicting PPC risk. The ARISCAT index is derived from clinical risk factors: (1) age, (2) preoperative oxygen saturation, (3) respiratory infection in the prior month, (4) anemia, (5) surgical site, (6) duration of surgery, and (7) emergency surgery, with varying weights based on the strength of the association in a multivariable analysis. This score can be calculated via addition of these weighted risk factors, with a score>45 equal to high risk for PPC.
Findings
Examining 5099 patients from 63 European hospitals, the authors definition of PPC included respiratory failure, pulmonary infection, pleural effusion, atelectasis, pneumothorax, bronchospasm, and aspiration pneumonitis. PPC rates were as follows: low risk (3.39%), intermediate risk (12.98%), and high risk (38.01%). The positive likelihood ratio for PPC among the highest risk group was 7.12. The C statistic for fit was 0.80. Observed PPC rates were higher than predicted for the low (3.39% vs 0.87%) and intermediate (12.98% vs 7.82%) risk groups.
Cautions
The calibration slopes were less than ideal in all subsamples, with the Western European sample performing better than the other geographic areas; suggesting that the coefficients on the ARISCAT index may benefit from recalibration to match specific populations.
Implications
This is the first major pulmonary risk index that has been externally validated. Its use of readily available clinical information, simplicity, and accuracy in estimating PPC risk make it an important addition to the toolkit during a preoperative evaluation.
PERIOPERATIVE ATRIAL FIBRILLATION/ANTICOAGULATION
Gialdini G, Nearing K, Bhave P, et al. Perioperative atrial fibrillation and the long term risk of ischemic stroke. JAMA. 2014;312(6):616622.
Background
New‐onset atrial fibrillation (AF) is the most common perioperative arrhythmia.[11] However, little is known regarding the long‐term risks of ischemic stroke in patients who develop perioperative AF. This retrospective cohort study examined adults with no preexisting history of AF, hospitalized for surgery, and discharged free of cerebrovascular disease between 2007 and 2011 (n=1,729,360).
Findings
Of the eligible patients, 1.43% (95% CI: 1.41%‐1.45%) developed perioperative AF, and 0.81% (95% CI: 0.79%‐0.82%) had a stroke up to 1 year after discharge. Perioperative AF was associated with subsequent stroke after both cardiac (HR: 1.3; 95% CI: 1.1‐1.6) and noncardiac surgery (HR: 2; 95% CI: 1.7‐2.3). The association with stroke was stronger for perioperative AF after noncardiac versus cardiac surgery (P0.001 for interaction).
Cautions
This is a retrospective cohort study, using claims data to identify AF and stroke. Data on duration of the perioperative AF episodes or use of antithrombotic therapies were not available.
Implications
The association found between perioperative AF and long‐term risk of ischemic stroke may suggest that perioperative AF, especially after noncardiac surgery, should be treated aggressively in terms of thromboembolic risk; however, further data will be required to validate this association.
Van Diepen S, Youngson E, Ezekowitz J, McAlister F. Which risk score best predicts perioperative outcomes in nonvalvular atrial fibrillation patients undergoing noncardiac surgery? Am Heart J. 2014;168(1):6067.
Background
Patients with nonvalvular AF (NVAF) are at increased risk for adverse perioperative outcomes after noncardiac surgery.[12] The RCRI is commonly used to predict perioperative cardiovascular events for all patients, including those with NVAF, though AF is not part of this risk assessment. The goal of this retrospective cohort study was to examine the prognostic utility of already existing NVAF risk indices, including the CHADS2 (Congestive heart failure, Hypertension, Age 75 years, Diabetes mellitus, prior stroke or transient ischemic attack), CHA2DS2‐VASc (Congestive heart failure; Hypertension; Age 75 years; Diabetes mellitus; Stroke, TIA, or thromboembolism [TE]; Vascular disease; Age 65 to 74 years; Sex category [female]), and R2CHADS2 (Renal dysfunction, Congestive heart failure, Hypertension, Age, Diabetes, Stroke/TIA) for perioperative outcomes in patients undergoing noncardiac surgery.
Findings
A population dataset of NVAF patients (n=32,160) who underwent noncardiac surgery was examined, with outcome measures including 30‐day mortality, stroke, TIA, or systemic embolism. The incidence of the 30‐day composite outcome was 4.2% and the C indices were 0.65 for the RCRI, 0.67 for CHADS2, 0.67 for CHA2DS2‐VASc, and 0.68 for R2CHADS2. The Net Reclassification Index (NRI), a measure evaluating the improvement in prediction performance gained by adding a marker to a set of baseline predictors, was calculated. All NVAF scores performed better than the RCRI for predicting mortality risk (NRI: 12.3%, 8.4%, and 13.3% respectively, all P0.01).
Cautions
Patients in the highest risk category by RCRI appear to have an unadjusted higher 30‐day mortality risk (8%) than that predicted by the other 3 scores (5%, 5.6%, and 5%), indicating that these risk scores should not completely supplant the RCRI for risk stratification in this population. In addition, the overall improvement in predictive capacity of the CHADS2, CHA2DS2‐VASc, and R2CHADS2, although superior to the RCRI, is modest.
Implications
These findings indicate that the preoperative risk stratification for patients with NVAF can be improved by utilizing the CHADS2, CHA2DS2‐VASc, or R2CHADS2 scores when undergoing noncardiac surgery. For patients with NVAF identified as high risk for adverse outcomes, this assessment can be integrated into the preoperative discussion on the risks/benefits of surgery.
Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT‐AF). Circulation. 2015;131:488494
Background
Oral anticoagulation (OAC) significantly reduces the risk of stroke in patients with AF. Many AF patients on long‐term anticoagulation undergo procedures requiring temporary interruption of OAC. Although guidelines have been published on when and how to initiate bridging therapy, they are based on observational data. Thus, it remains unclear which patients should receive bridging anticoagulation.
Findings
This is a US registry of outpatients with AF with temporary interruptions of OAC for a procedure. Of 7372 patients treated with OAC, 2803 overall interruption events occurred in 2200 patients (30%). Bridging anticoagulants were used in 24% (n=665). Bleeding events were more common in bridged than nonbridged patients (5.0% vs 1.3%; adjusted OR: 3.84; P0.0001). The overall composite end point of myocardial infarction, stroke or systemic embolism, major bleeding, hospitalization, or death within 30 days was significantly higher in patients receiving bridging (13% vs 6.3%; adjusted OR: 1.94; P=0.0001). This statistically significant increase in the composite outcome, which includes cardiovascular events, is most likely in part secondary to inclusion of bleeding events. The recently published BRIDGE (Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery) trial did not find a statistically significant difference in cardiovascular events between bridged and nonbridged patients.[13]
Cautions
Although patients who were bridged appear to have had more comorbidities and a higher mean CHADS2 score than patients who were not bridged, it is difficult to determine which population of patients may be high risk enough to warrant bridging, as indicated by current American College of Chest Physicians guidelines, as this was not evaluated in this study
Implications
The use of bridging anticoagulation was significantly associated with higher overall bleeding and adverse event rates. The BRIDGE trial also found that forgoing bridging anticoagulation decreased the risk of major bleeding in patients with AF and was noninferior to bridging for the prevention of arterial TE.[13]
Given the rapid expansion of the field of perioperative medicine, clinicians need to remain apprised of the current evidence to ensure optimization of patient care. In this update, we review 10 key articles from the perioperative literature, with the goal of summarizing the most clinically important evidence over the past year. This summary of recent literature in perioperative medicine is derived from the Update in Perioperative Medicine sessions presented at the 10th Annual Perioperative Medicine Summit and the Society of General Internal Medicine 38th Annual Meeting. A systematic search strategy was used to identify pertinent articles, and the following were selected by the authors based on their relevance to the clinical practice of perioperative medicine.
PERIOPERATIVE CARDIOVASCULAR CARE
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;130:e278e333.
Background
The American College of Cardiology/American Heart Association (ACC/AHA) perioperative guideline provides recommendations for the evaluation and management of cardiovascular disease in patients undergoing noncardiac surgery.
Findings
The new guideline combines the evaluation of surgery‐ and patient‐specific risk in the algorithm for preoperative cardiovascular evaluation into a single step and recommends the use of 1 of 3 tools: the Revised Cardiac Risk Index (RCRI),[1] National Surgical Quality Improvement Program (NSQIP) Surgical Risk Calculator,[2] or the NSQIP‐derived myocardial infarction and cardiac arrest calculator.[3] Estimation of risk is also simplified by stratification into only 2 groups: low risk (risk of major adverse cardiac event 1%) and elevated risk (1% risk). Coronary evaluation can be considered for patients with elevated cardiac risk and poor functional capacity, but is advised only if the results would alter perioperative management. For example, a patient with very high risk who has evidence of ischemia on stress testing may choose to forego surgery. Preoperative coronary revascularization is only indicated for patients meeting criteria in the nonsurgical setting.
For patients with previous percutaneous coronary intervention, the ACC/AHA has not changed its recommendations to optimally delay surgery for at least 30 days after bare‐metal stenting and at least 1 year after drug‐eluting stent (DES) placement. However, in patients with a DES placed 6 to 12 months previously, surgery can be performed if the risks of surgical delay outweigh the risks of DES thrombosis. After any type of coronary stenting, dual antiplatelet therapy should be continued uninterrupted through the first 4 to 6 weeks and even later whenever feasible. If not possible, aspirin therapy should be maintained through surgery unless bleeding risk is too high.
The guideline recommends perioperative continuation of ‐blockers in patients taking them chronically. Preoperative initiation of ‐blocker therapy may be considered for patients with myocardial ischemia on stress testing or 3 RCRI factors and should be started far enough in advance to allow determination of patient's tolerance prior to surgery.
Cautions
Many recommendations are based on data from nonrandomized trials or expert opinion, and the data in areas such as perioperative ‐blockade continue to evolve.
Implications
The ACC/AHA guideline continues to be a critically valuable resource for hospitalists providing perioperative care to noncardiac surgery patients.
Wijeysundera DN, Duncan D, Nkonde‐Price C, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines.
J Am Coll Cardiol. 2014;64(22):24062425.
Background
Various clinical trials have reported conflicting results regarding the efficacy and safety of perioperative ‐blockers resulting in guideline committees changing their recommendations. Because of questions raised regarding the scientific integrity of the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography)‐I[4] and DECREASE‐IV[5] trials as well as the dosing of ‐blockers in POISE (PeriOperative Ischemic Evaluation) study,[6] this systematic review was performed in conjunction with the ACC/AHA guideline update[7] to evaluate the data with and without these trials.
Findings
Sixteen randomized control trials (RCTs) (n=12,043) and 1 cohort study (n=348) were included in the analysis. Perioperative ‐blockers were associated with a reduction in nonfatal myocardial infarction (MI) (relative risk [RR]: 0.69; 95% confidence interval [CI]: 0.58‐0.82; P0.001) but an increase in bradycardia (RR: 2.61; 95% CI: 2.18‐3.12), hypotension (RR: 1.47; 95% CI: 1.34‐1.6), and nonfatal strokes (RR: 1.76; 95% CI: 1.07‐2.91; P=0.02). The POISE trial was the only one demonstrating a statistically significant increase in stroke.
The major discrepancy between the DECREASE trials and the other RCTs was related to mortalitya reduction in both cardiovascular and all‐cause death in DECREASE but an increased risk of all‐cause death in the other trials.
Cautions
Because of its size, the POISE trial heavily influences the results, particularly for mortality and stroke. Including the DECREASE trials reduces the otherwise increased risk for death to a null effect. Exclusion of the POISE and DECREASE trials leaves few data to make conclusions about safety and efficacy of perioperative ‐blockade. Several cohort studies have found metoprolol to be associated with worse outcomes than with atenolol or bisoprolol (which were preferred by the European Society of Cardiology guidelines).[8]
Implications
Perioperative ‐blockade started within 1 day of noncardiac surgery was associated with fewer nonfatal MIs but at the cost of an increase in hypotension, bradycardia, and a possible increase in stroke and death. Long‐term ‐blockade should be continued perioperatively, whereas the decision to initiate a ‐blocker should be individualized. If starting a ‐blocker perioperatively, it should be done 2 days before surgery.
Botto F, Alonso‐Coello P, Chan MT, et al.; on behalf of The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Investigators. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30‐day outcomes. Anesthesiology. 2014;120(3):564578.
Background
Many patients sustain myocardial injury in the perioperative period as evidenced by troponin elevations, but most do not meet diagnostic criteria for MI. Myocardial injury after noncardiac surgery (MINS) is defined as prognostically relevant myocardial injury due to ischemia that occurs within 30 days after noncardiac surgery. This international, prospective cohort study of 15,065 patients 45 years old who underwent in‐patient noncardiac surgery determined diagnostic criteria, characteristics, predictors, and 30‐day outcomes of MINS.
Findings
The diagnostic criterion for MINS was a peak troponin T level 0.03 ng/mL judged to be due to an ischemic etiology. Twelve independent predictors of MINS were identified including age 75 years, known cardiovascular disease or risk factors, and surgical factors. MINS was an independent predictor of 30‐day mortality (adjusted hazard ratio [HR]: 3.87; 95% CI: 2.96‐5.08). Age >75 years, ST elevation, or new left bundle branch block, and anterior ischemic findings were independent predictors of 30‐day mortality among patients with MINS.
Cautions
Although screening high‐risk surgical patients without signs or symptoms of ischemia with postoperative troponins will increase the frequency of diagnosing MINS, evidence for an effective treatment has not yet been established. The ACC/AHA guidelines state that routine screening is of uncertain benefit for this reason.
Implications
Because MINS is common and carries a poor 30‐day prognosis, clinical trials are needed to determine when to obtain postoperative troponins and how to prevent and treat this complication.[9] Some observational data from POISE suggest that aspirin and statins can reduce the risk of 30‐day mortality in patients with postoperative MIs.
Devereaux PJ, Mrkobrada M, Sessler DI, et al. for the POISE‐2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):14941503.
Devereaux PJ, Sessler DI, Leslie K, et al. for the POISE‐2 Investigators. Clonidine in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370(16):15041513.
Background
Medical risk reduction with aspirin and other agents in perioperative patients remains controversial. The POISE‐2 trial is a blinded RCT examining the effects of aspirin and clonidine on outcomes in >10,000 noncardiac surgery patients at risk of cardiovascular complications. The aspirin arm of the study included the initiation group and the continuation stratum, as well as placebo. Patients in the clonidine portion of the trial received 0.2 mg of clonidine or placebo daily for the same time periods.
Findings
The primary outcome was a composite of death or nonfatal MI within 30 days of surgery. Outcomes were similar in patients initiated or continued on aspirin. No difference was seen between aspirin or placebo in the primary outcome (7.0% vs 7.1%; HR: 0.86; 95% CI: 0.86‐1.15; P=0.92). There were no differences in rates of MI, venous thromboembolism, or stroke. Major bleeding rates were higher in aspirin versus placebo‐treated patients (4.6% vs 3.8%; HR: 1.23; 95% CI: 1.01‐1.49; P=0.04).
Clonidine did not alter the composite outcome of death or nonfatal MI (7.3% vs 6.8%; HR: 1.08; 95% CI: 0.93‐1.26; P=0.29). Clinically significant hypotension, bradycardia, and nonfatal cardiac arrest were more common in clonidine‐treated patients, although no difference was detected in stroke rates.
Cautions
Although patients in the trial had cardiovascular risk factors, 24% of patients had known coronary artery disease, and 5% had coronary stents. Conclusions based on this trial regarding perioperative management of antiplatelet therapy should not include patients with coronary artery stents.
Implications
Aspirin started before surgery and continued perioperatively did not decrease the rate of death or nonfatal MI but increased the risk of major bleeding. Perioperative management of aspirin needs to be undertaken in the context of cardiac and bleeding risks. Clonidine also did not improve outcomes and increased the risk of bradycardia and hypotension. Current guidelines recommend against using alpha‐2 agonists for prevention of perioperative cardiac events7; however, patients already on alpha‐2 agonists should not stop them abruptly.
PERIOPERATIVE PULMONARY CARE
Mutter TC, Chateau D, Moffatt M, et al. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121(4):707718.
Background
An increasing body of literature associates obstructive sleep apnea (OSA) with an increased risk of postoperative complications. Despite evidence of risk, potential benefits of preoperative diagnosis and treatment of OSA remain unclear.
Findings
Using databases to identify patients prescribed continuous positive airway pressure (CPAP) therapy, the study compared postoperative outcomes of patients who underwent surgery any time after polysomnography (PSG) and CPAP prescription (diagnosed OSA [DOSA]) and those who had surgery during the 5 years preceding their PSG (undiagnosed OSA [UOSA]). These patients were matched with patients who underwent the same procedure for the same indication and had no insurance claims for PSG or diagnosis of sleep‐disordered breathing.
After multivariate analysis, OSA of any type was associated with increased pulmonary complications (odds ratio [OR]: 2.08; 95% CI: 1.35‐2.19). However, no significant differences in respiratory outcomes were noted between DOSA patients (N=2640) and those with UOSA (N=1571). DOSA patients did have fewer cardiovascular complications than UOSA patients (OR: 0.34; 95% CI: 0.15‐0.77). Only severe OSA (apnea‐hypopnea index >30) was associated with increased pulmonary and cardiovascular complications.
Cautions
Although this study suggests an association between preoperative diagnosis and treatment of OSA and reduced cardiovascular complications, the results are not definitive due to the inability to control for all confounding variables in a retrospective study utilizing an administrative database.
Implications
OSA is an important risk factor for postoperative complications, and this study suggests that preoperative treatment with CPAP is associated with reduced risk of cardiovascular complications, particularly in patients with severe OSA. Future controlled trials should focus on the risk‐reduction potential of preoperative diagnosis and treatment of OSA.
Mazo V, Sabat S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219231.
Background
In 2010, Canet et al. published a novel risk index, the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) index, to provide a quantitative estimate of the risk of postoperative pulmonary complications (PPCs).[10]
In the current report, Mazo and colleagues studied the ARISCAT index in a broader sample to characterize its accuracy in predicting PPC risk. The ARISCAT index is derived from clinical risk factors: (1) age, (2) preoperative oxygen saturation, (3) respiratory infection in the prior month, (4) anemia, (5) surgical site, (6) duration of surgery, and (7) emergency surgery, with varying weights based on the strength of the association in a multivariable analysis. This score can be calculated via addition of these weighted risk factors, with a score>45 equal to high risk for PPC.
Findings
Examining 5099 patients from 63 European hospitals, the authors definition of PPC included respiratory failure, pulmonary infection, pleural effusion, atelectasis, pneumothorax, bronchospasm, and aspiration pneumonitis. PPC rates were as follows: low risk (3.39%), intermediate risk (12.98%), and high risk (38.01%). The positive likelihood ratio for PPC among the highest risk group was 7.12. The C statistic for fit was 0.80. Observed PPC rates were higher than predicted for the low (3.39% vs 0.87%) and intermediate (12.98% vs 7.82%) risk groups.
Cautions
The calibration slopes were less than ideal in all subsamples, with the Western European sample performing better than the other geographic areas; suggesting that the coefficients on the ARISCAT index may benefit from recalibration to match specific populations.
Implications
This is the first major pulmonary risk index that has been externally validated. Its use of readily available clinical information, simplicity, and accuracy in estimating PPC risk make it an important addition to the toolkit during a preoperative evaluation.
PERIOPERATIVE ATRIAL FIBRILLATION/ANTICOAGULATION
Gialdini G, Nearing K, Bhave P, et al. Perioperative atrial fibrillation and the long term risk of ischemic stroke. JAMA. 2014;312(6):616622.
Background
New‐onset atrial fibrillation (AF) is the most common perioperative arrhythmia.[11] However, little is known regarding the long‐term risks of ischemic stroke in patients who develop perioperative AF. This retrospective cohort study examined adults with no preexisting history of AF, hospitalized for surgery, and discharged free of cerebrovascular disease between 2007 and 2011 (n=1,729,360).
Findings
Of the eligible patients, 1.43% (95% CI: 1.41%‐1.45%) developed perioperative AF, and 0.81% (95% CI: 0.79%‐0.82%) had a stroke up to 1 year after discharge. Perioperative AF was associated with subsequent stroke after both cardiac (HR: 1.3; 95% CI: 1.1‐1.6) and noncardiac surgery (HR: 2; 95% CI: 1.7‐2.3). The association with stroke was stronger for perioperative AF after noncardiac versus cardiac surgery (P0.001 for interaction).
Cautions
This is a retrospective cohort study, using claims data to identify AF and stroke. Data on duration of the perioperative AF episodes or use of antithrombotic therapies were not available.
Implications
The association found between perioperative AF and long‐term risk of ischemic stroke may suggest that perioperative AF, especially after noncardiac surgery, should be treated aggressively in terms of thromboembolic risk; however, further data will be required to validate this association.
Van Diepen S, Youngson E, Ezekowitz J, McAlister F. Which risk score best predicts perioperative outcomes in nonvalvular atrial fibrillation patients undergoing noncardiac surgery? Am Heart J. 2014;168(1):6067.
Background
Patients with nonvalvular AF (NVAF) are at increased risk for adverse perioperative outcomes after noncardiac surgery.[12] The RCRI is commonly used to predict perioperative cardiovascular events for all patients, including those with NVAF, though AF is not part of this risk assessment. The goal of this retrospective cohort study was to examine the prognostic utility of already existing NVAF risk indices, including the CHADS2 (Congestive heart failure, Hypertension, Age 75 years, Diabetes mellitus, prior stroke or transient ischemic attack), CHA2DS2‐VASc (Congestive heart failure; Hypertension; Age 75 years; Diabetes mellitus; Stroke, TIA, or thromboembolism [TE]; Vascular disease; Age 65 to 74 years; Sex category [female]), and R2CHADS2 (Renal dysfunction, Congestive heart failure, Hypertension, Age, Diabetes, Stroke/TIA) for perioperative outcomes in patients undergoing noncardiac surgery.
Findings
A population dataset of NVAF patients (n=32,160) who underwent noncardiac surgery was examined, with outcome measures including 30‐day mortality, stroke, TIA, or systemic embolism. The incidence of the 30‐day composite outcome was 4.2% and the C indices were 0.65 for the RCRI, 0.67 for CHADS2, 0.67 for CHA2DS2‐VASc, and 0.68 for R2CHADS2. The Net Reclassification Index (NRI), a measure evaluating the improvement in prediction performance gained by adding a marker to a set of baseline predictors, was calculated. All NVAF scores performed better than the RCRI for predicting mortality risk (NRI: 12.3%, 8.4%, and 13.3% respectively, all P0.01).
Cautions
Patients in the highest risk category by RCRI appear to have an unadjusted higher 30‐day mortality risk (8%) than that predicted by the other 3 scores (5%, 5.6%, and 5%), indicating that these risk scores should not completely supplant the RCRI for risk stratification in this population. In addition, the overall improvement in predictive capacity of the CHADS2, CHA2DS2‐VASc, and R2CHADS2, although superior to the RCRI, is modest.
Implications
These findings indicate that the preoperative risk stratification for patients with NVAF can be improved by utilizing the CHADS2, CHA2DS2‐VASc, or R2CHADS2 scores when undergoing noncardiac surgery. For patients with NVAF identified as high risk for adverse outcomes, this assessment can be integrated into the preoperative discussion on the risks/benefits of surgery.
Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT‐AF). Circulation. 2015;131:488494
Background
Oral anticoagulation (OAC) significantly reduces the risk of stroke in patients with AF. Many AF patients on long‐term anticoagulation undergo procedures requiring temporary interruption of OAC. Although guidelines have been published on when and how to initiate bridging therapy, they are based on observational data. Thus, it remains unclear which patients should receive bridging anticoagulation.
Findings
This is a US registry of outpatients with AF with temporary interruptions of OAC for a procedure. Of 7372 patients treated with OAC, 2803 overall interruption events occurred in 2200 patients (30%). Bridging anticoagulants were used in 24% (n=665). Bleeding events were more common in bridged than nonbridged patients (5.0% vs 1.3%; adjusted OR: 3.84; P0.0001). The overall composite end point of myocardial infarction, stroke or systemic embolism, major bleeding, hospitalization, or death within 30 days was significantly higher in patients receiving bridging (13% vs 6.3%; adjusted OR: 1.94; P=0.0001). This statistically significant increase in the composite outcome, which includes cardiovascular events, is most likely in part secondary to inclusion of bleeding events. The recently published BRIDGE (Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery) trial did not find a statistically significant difference in cardiovascular events between bridged and nonbridged patients.[13]
Cautions
Although patients who were bridged appear to have had more comorbidities and a higher mean CHADS2 score than patients who were not bridged, it is difficult to determine which population of patients may be high risk enough to warrant bridging, as indicated by current American College of Chest Physicians guidelines, as this was not evaluated in this study
Implications
The use of bridging anticoagulation was significantly associated with higher overall bleeding and adverse event rates. The BRIDGE trial also found that forgoing bridging anticoagulation decreased the risk of major bleeding in patients with AF and was noninferior to bridging for the prevention of arterial TE.[13]
- , , , et al. Derivation and prospective evaluation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049.
- , , , et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842.
- , , , et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124:381–387.
- , , , et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high‐risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999;341(24):1789–1794.
- , , , et al; Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- POISE Study Group, , , , et al. Effects of extended‐release metoprolol succinate in patients undergoing non‐cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839–1847.
- , , , et al. American College of Cardiology; American Heart Association. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77–e137.
- , , , et al. 2014 ESC/ESA Guidelines on non‐cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non‐cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014;35(35):2383–431.
- , , , et al. The long‐term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053–1063.
- , , , et al. ARISCAT Group: Prediction of postoperative pulmonary complications in a population‐based surgical cohort. Anesthesiology. 2010;113:1338–1350.
- , . Noncardiac surgery: postoperative arrhythmias. Crit Care Med. 2000;28(10 suppl):N145–N150.
- , , , et al. Incidence, predictors, and outcomes associated with postoperative atrial fibrillation after major cardiac surgery. Am Heart J. 2012;164(6):918–924.
- , , , et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823–833.
- , , , et al. Derivation and prospective evaluation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049.
- , , , et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842.
- , , , et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124:381–387.
- , , , et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high‐risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999;341(24):1789–1794.
- , , , et al; Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- POISE Study Group, , , , et al. Effects of extended‐release metoprolol succinate in patients undergoing non‐cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839–1847.
- , , , et al. American College of Cardiology; American Heart Association. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77–e137.
- , , , et al. 2014 ESC/ESA Guidelines on non‐cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non‐cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014;35(35):2383–431.
- , , , et al. The long‐term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth Analg. 2014;119(5):1053–1063.
- , , , et al. ARISCAT Group: Prediction of postoperative pulmonary complications in a population‐based surgical cohort. Anesthesiology. 2010;113:1338–1350.
- , . Noncardiac surgery: postoperative arrhythmias. Crit Care Med. 2000;28(10 suppl):N145–N150.
- , , , et al. Incidence, predictors, and outcomes associated with postoperative atrial fibrillation after major cardiac surgery. Am Heart J. 2012;164(6):918–924.
- , , , et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823–833.
Triple Therapy
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
Dual antiplatelet therapy (DAPT) (aspirin plus a thienopyridine: clopidogrel or prasugrel) has become the standard treatment for patients with acute coronary syndromes (ACS) and after coronary stent placement (Table 1). Anticoagulant therapy with warfarin is indicated for stroke prevention in atrial fibrillation (AF), profound left ventricular dysfunction, and after mechanical heart valve replacement, as well as for treatment of deep venous thrombosis and pulmonary embolism (Table 2). It is estimated that 41% of the U.S. population over age 40 years is on some form of antiplatelet therapy,6 and 2.5 million patients, mostly elderly, are on long‐term warfarin therapy.7 More specifically, 5% of patients undergoing percutaneous coronary interventions (PCIs) also have an indication for warfarin.8 With widespread use of drug‐eluting stents (DES), the need for a longer duration of DAPT, and the increased age and complexity of hospitalized patients, the safety and challenges of triple therapy (combined DAPT and warfarin) have become more important to the practice of hospital medicine. Triple therapy may increase hospitalization rates, as the risk of major bleeding is four to five times higher than with DAPT.911 In contrast, DAPT is much less effective than warfarin alone in preventing embolic events in AF,12 and warfarin alone or in combination with aspirin (ASA) is inadequate therapy to prevent stent thrombosis. Even fewer data exist on the efficacy and safety of triple therapy in patients with mechanical valves or left ventricular dysfunction.
| Class Recommendations | Level of Evidence | |
|---|---|---|
| ||
| DAPT after PCI/stenting1 | ||
| ASA | ||
| Class I | ASA 325 mg/d after PCI for 1 mo (up to 6 mo depending on type of stent implanted) and then 7562 mg/d indefinitely | B |
| Class IIa | ASA 75‐325 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| In patients at risk of bleeding, a lower dose of 75‐162 mg/d is reasonable after stent implantation | C | |
| Thienopyridine | ||
| Class I | Clopidogrel 75 mg/d after BMS for at least 1 mo and ideally up to 12 mo unless increased risk of bleeding (at least 2 wk) | B |
| Clopidogrel 75 mg/d after DES for at least 12 mo if not at high risk for bleeding | B | |
| 2009 focus update2: Clopidogrel 75 mg daily or prasugrel 10 mg daily for at least 12 mo after BMS or DES for ACS | B | |
| Class IIa | Clopidogrel 75 mg/d indefinitely after brachytherapy unless risk of bleeding is significant | C |
| Class IIb | In patients with potential for lethal or catastrophic stent thrombosis, consider platelet aggregation studies and increase clopidogrel dose to 150 mg/d if 50% inhibition of platelet aggregation is seen | C |
| Continuation of clopidogrel 75 mg/day beyond 12 mo is reasonable after DES | C | |
| 2009 focus update2: consider continuation of clopidogrel or prasugrel beyond 15 mo after DES placement | C | |
| DAPT for UA/NSTEMI without stenting3 | ||
| ASA | ||
| Class I | Continue ASA (75 to 162 mg/d) indefinitely | A |
| Clopidogrel | ||
| Class 1 | Clopidogrel (75 mg/d) for at least 1 mo (A) and ideally for up to 1 y | B |
| Dipyridamole | ||
| Class III | Dipyridamole is not recommended because it has not been shown to be effective | A |
| |
| Condition | Risk (%) |
| Atrial fibrillation (without anticoagulation)4 | |
| Low‐risk atrial fibrillation (CHADS2 score 0) | 1.9 |
| Intermediate‐risk atrial fibrillation (CHADS2 score 1) | 2.8 |
| High‐risk atrial fibrillation (CHADS2 score 2‐6) | 418 |
| Mechanical heart valve5b | |
| Mechanical heart valve (without anticoagulation) | 8.6c |
| Mechanical heart valve (treated with ASA alone) | 7.5c |
| Mechanical heart valve (treated with warfarin) | 1.8c |
| Mechanical aortic valve (treated with warfarin) | 1.1c |
| Mechanical mitral valve (treated with warfarin) | 2.7c |
Hospitalists commonly care for patients on triple therapy; certain indications are appropriate and supported from the available literature while others lack evidence. Knowledge of existing practice guidelines and of supporting research studies leads to optimal management of these complicated patients, and minimizes excessive morbidity from bleeding complications or thromboembolic events such as strokes and stent thrombosis.
In the first part of this article, we present the evidence that supports current recommendations for DAPT or warfarin in specific medical conditions. We also address controversies and unanswered questions. The second part of this review focuses on the available data and provides guidance on the optimal care of patients on triple therapy.
Dual Antiplatelet Therapy Following Acute Coronary Syndromes
Table 3 summarizes key randomized trials of DAPT versus ASA alone in several clinical scenarios. The addition of clopidogrel to ASA in patients with nonST‐elevation ACS reduced the risk of adverse ischemic outcomes in the clopidogrel in unstable angina to prevent recurrent events (CURE) trial,15 as well as in its substudy, the PCI‐CURE (patients with ACS who have undergone stenting).17 In the main CURE study, the study groups diverged within the first 30 days after randomization and the benefit of DAPT persisted throughout the 12 months of the study period. DAPT is also superior to ASA in patients with ST‐elevation myocardial infarction (MI) (CLARITYTIMI 28 and COMMIT trials).13, 14 On the basis of these findings, DAPT has become the standard of care for patients with ACS. The American College of Cardiology (ACC)/American Heart Association (AHA)3 and the European Society of Cardiology18 recommend ASA treatment indefinitely for patients with ACS whether or not they underwent PCI. Clopidogrel is recommended for at least 12 months following ACS, especially for patients who receive a coronary stent.
| Trial | Endpoints | Results |
|---|---|---|
| ||
| ST elevation MI | ||
| CLARITY‐TIMI13 | Incidence of death, infarct‐related artery occlusion, or recurrent MI | 36% reduction (95% CI 2447); P .001 |
| COMMIT14 | Incidence of death, MI, or stroke | 9% reduction (95% CI 314); P .002 |
| ACS without ST elevation | ||
| CURE15 | Incidence of death, MI, or stroke | 20% reduction (RR 0.80 [0.720.90]); P .001 |
| Bare‐metal stent placement | ||
| CREDO16 | Incidence of death, MI, or stroke | 27% reduction (95% CI 3.944.4); P .02 |
| PCI‐CURE17 | Incidence of death, MI, or urgent TVR | 30% reduction (RR 0.70 [0.500.97]); P .03 |
Despite the proven efficacy of DAPT in ACS, about 15% of patients die or experience reinfarction within 30 days of diagnosis.19 The continued risk for thrombotic events could be due to delayed onset of platelet inhibition and to patient heterogeneity in responsiveness to therapy with ASA and/or clopidogrel.20 Consequently, the optimum dose for clopidogrel and ASA following ACS is uncertain. The CURRENT‐OASIS 7 trial evaluated the efficacy and safety of high‐dose clopidogrel (600‐mg loading dose, 150 mg once daily for 7 days, followed by 75 mg/d) versus standard‐dose clopidogrel (300‐mg loading dose, followed by 75 mg/d) and ASA (75‐100 mg versus 300‐325 mg/d) in patients with ACS who were treated medically, with or without stenting.21 In the overall study population as well as in patients who did not receive stenting, there was no significant difference in the combined rate of death from cardiovascular causes, MI, and stroke between patients receiving the high‐dose and the standard‐dose clopidogrel (4.2% vs 4.4%; P = .37) and high‐dose versus low‐dose ASA (4.2% vs 4.4%; P = .47). There were no significant differences in bleeding complications between the two clopidogrel treatment arms or between the high‐dose and low‐dose ASA groups.
The ACC/AHA guidelines recommend ASA, 75‐162 mg/d indefinitely after medical therapy without stenting (class I, level of evidence: A)3 and clopidogrel 75 mg/d for at least 1 month (class IA) and optimally for 1 year (class IB). Clopidogrel monotherapy is appropriate for patients with ACS who are unable to tolerate ASA due to either hypersensitivity or recent significant gastrointestinal bleeding.
As is the case after coronary stenting, interruption of DAPT soon after ACS may subject patients to high recurrence of cardiovascular events, although few data are available to support this observation. Interruption of DAPT due to bleeding complications or surgical procedures more than 1 month after ACS may be reasonable for a patient who did not receive a stent. Clinicians should restart DAPT after the surgical procedure once the bleeding risk becomes acceptable.
Dual Antiplatelet Therapy Following Coronary Stenting
Following Bare Metal Stents
Stent thrombosis occurs in approximately 20% of patients who receive bare metal stents (BMS) without DAPT22; the risk is highest in the first 30 days after implantation. The clinical presentation of stent thrombosis is often catastrophic: MI or sudden death occurs in over 60% of cases. DAPT reduces the incidence of stent thrombosis to a clinically acceptable level.22
In the ISAR trial of 517 patients treated with BMS for MI, suboptimal angioplasty, or other high‐risk clinical and anatomic features,23 patients were randomly assigned to treatment with ASA plus ticlopidine or ASA plus anticoagulation with heparin and warfarin. The primary endpoint of cardiac death, MI, coronary bypass surgery, or repeat angioplasty occurred in 1.5% of patients assigned to DAPT and 6.2% of those assigned to anticoagulant therapy (relative risk [RR], 0.25; 95% confidence interval [CI], 0.06‐0.77). The PCI‐CURE study evaluated patients who received BMS after ACS.17 The primary endpoint was a composite of cardiovascular death, MI, or urgent target‐vessel revascularization within 30 days of PCI. Long‐term administration of clopidogrel (8 months) conferred a lower rate of cardiovascular death, MI, or any revascularization (P = .03), with no significant difference in major bleeding between the groups (P = .64). In the CREDO trial,16 investigators evaluated 2116 patients undergoing PCI at 99 North American centers. Subjects received either a 300‐mg loading dose of clopidogrel or placebo 3‐24 hours before PCI. All patients then received clopidogrel 75 mg/d through day 28. For the following 12 months, patients in the loading dose group received clopidogrel, and those in the control group received placebo. All patients received ASA throughout the study. At 1 year, loading dose plus long‐term clopidogrel therapy conferred a 27% RR reduction (3% absolute risk reduction) in the combined endpoint of death, MI, or stroke (P = .02).
Based on these trials, the ACC and AHA recommend clopidogrel (75 mg/d) for a minimum of 1 month and optimally 12 months after BMS (class 1B).2 For patients at increased risk of bleeding, the ACC/AHA recommends a minimum of 2 weeks of clopidogrel. Although lifelong therapy with ASA is recommended, the optimal dose of ASA after BMS is unknown. However, on the basis of clinical trial protocols (no randomized data), guidelines recommend ASA 162 mg‐325 mg/d for at least 1 month, followed by indefinite use at a dose of 75‐162 mg. In patients for whom there is concern about bleeding, lower doses of ASA (75‐162 mg) are acceptable for the initial period after stent implantation.
Following Drug‐Eluting Stents
Drug‐eluting stents have become the standard percutaneous treatment for patients with symptomatic coronary artery disease. In 2005, a sampling of 140 US hospitals indicated that 94% of patients treated with a stent received at least one DES.24 Compared with BMS, restenosis and the need for revascularization are significantly less frequent. In contrast, unanticipated high rates of very late (>1 year) stent thrombosis have complicated DES.25 Because of the potentially lethal consequences of stent thrombosis, several authors have questioned the long‐term safety of DES2635 and examined the role of extended DAPT in reducing this delayed complication.27, 31, 36 Although the initial pivotal randomized trials of DES mandated clopidogrel use for only 3 months after sirolimus‐eluting stent and 6 months after paclitaxel‐eluting stent,37, 38 current guidelines recommend DAPT for at least 12 months after DES placement for patients who are not at high risk of bleeding.1
Although multiple studies have confirmed the benefit of DAPT, controversy remains regarding the extended use for more than 1 year. The only randomized trial that addressed this issue was nonblinded and underpowered.39 In this study of patients from two ongoing trials, the REAL‐LATE and ZEST‐LATE, extended duration DAPT (>12 months, median duration 19.2 months), did not reduce the incidence of MI and cardiac death.39 The rate of the primary endpoint was less than 25% of that expected (underpowered), and patients had already received clopidogrel for up to 24 months before enrollment.
The results from small, nonrandomized trials regarding this issue have been contradictory. Banerjee and colleagues studied 530 consecutive patients who underwent PCI (85% received a DES), were free of cardiovascular events for 6 months after PCI, and had follow‐up available for >12 months.26 In a multivariate analysis, clopidogrel use for 1 year was associated with lower mortality (hazard ratio [HR], 0.28; 95% CI, 0.140.59); this effect was independent of traditional cardiovascular risk factors, clinical presentation, and DES use. In a study at the Duke Heart Center40 among patients with DES (n = 528) who were event‐free at 12 months, continued clopidogrel use conferred lower rates of death (0% versus 3.5%; difference, 3.5%; 95% CI, 5.9% to 1.1%; P = .004) and death or MI (0% versus 4.5%; difference, 4.5%; 95% CI, 7.1% to 1.9%; P .001) at 24 months. In the TYCOON registry,35 patients with DES receiving clopidogrel for 2 years had a rate of stent thrombosis (0.4%) that was similar to those with BMS (0.7%) but significantly lower than patients with DES and 1‐year DAPT (2.9%).
In contrast, Roy and colleagues33 found that clopidogrel cessation at 12 months did not predict stent thrombosis, and Park and colleagues32 reported that clopidogrel continuation beyond 1 year did not appear to decrease stent thrombosis or clinical events after DES implantation. Similarly, Stone et al.34 performed a landmark analysis on the basis of the prospective, double‐blind TAXUS‐II SR, TAXUS‐IV, and TAXUS‐V trials. The authors found that thienopyridine use beyond 1 year after DES may reduce stent thrombosis over the subsequent 12‐month period, but did not reduce rates of death and MI at 2 and 5 years after either DES or BMS.
Current guidelines recommend ASA 162‐325 mg/d for at least 3‐6 months, followed by treatment indefinitely at a dose of 75‐162 mg daily. Clopidogrel, on the other hand, is given at 75 mg/d for at least 12 months.
Warfarin After Acute Coronary Syndromes
Warfarin with different international normalized ratio (INR) goals alone or in combination with ASA has been evaluated after ACS. In an early trial, patients with recent (mean interval 27 days) MI were treated with warfarin alone versus placebo.41 Warfarin conferred a relative risk reduction in mortality of 24% (95% CI, 4‐44%; P = .027) at the expense of major bleeding rates of 0.6%/y. In the ASPECT trial,42 moderate to high intensity anticoagulation after MI resulted in a 53% and 40% reduction in the relative risk of reinfarction (annual incidence 2.3% versus 5.1%) and cerebrovascular events (annual incidence 0.7% versus 1.2%), respectively. In the WARIS II43 and ASPECT‐244 trials, moderate intensity warfarin (INR 2.0‐2.5) in combination with low‐dose ASA, compared with ASA alone, reduced the composite occurrence of death or nonfatal reinfarction, as well as recurrent coronary occlusion after ST‐segment elevation MI. High‐intensity warfarin therapy alone (INR 3.0‐4.0 for ASPECT, 2.8‐4.2 for WARISII) reduced ischemic vascular events compared with ASA alone. Not unexpectedly, major bleeding episodes were more common among patients receiving warfarin.
No randomized trials have compared DAPT with warfarin plus ASA for patients with ACS who did not receive stents. The ACC/AHA guidelines recommend warfarin for secondary prevention following ACS (class IIb). High‐intensity warfarin alone (INR 2.5‐3.5) or moderate intensity (INR 2.0‐2.5) with low‐dose ASA (75‐81 mg/d) may be reasonable for patients at high ischemic and low bleeding risk who are intolerant of clopidogrel (level of evidence: B). Fixed dose warfarin is not recommended by the ACC/AHA primarily on the basis of the Coumadin Aspirin Reinfarction Study (CARS) results. This study of patients following MI was discontinued prematurely because of a lack of incremental benefit of reduced‐dose ASA (80 mg/d) combined with either 1 or 3 mg of warfarin daily when compared with 160 mg/d of ASA alone.
Triple Therapy for PCI and Atrial Fibrillation
AF is the most frequent indication (70%) for long‐term therapy with warfarin in patients scheduled for stent placement.10 Clinical trials have shown that warfarin alone is superior to ASA, clopidogrel, or DAPT for prevention of stroke in patients with AF.45, 46 Although warfarin is indispensable in these settings, DAPT is similarly necessary after stent implantation. As triple therapy increases the risk of bleeding, the management of patients with AF and who have received stents remains controversial. This situation is particularly problematic among patients who have received DES and may benefit from extended DAPT. No randomized trials exist to clarify the optimal treatment in these patients; and the feasibility of such studies is questionable. Small, mostly retrospective, studies (Table 4) provide limited guidance on this issue; most studies focus on bleeding events rather than the cardiovascular efficacy of triple therapy. Because of these limitations, cardiovascular societies give IIb recommendation for either triple therapy or the combination of warfarin and clopidogrel in this setting and the level of evidence is C.1, 59, 60
| Author | Year | Type | No. | Major Bleeding, % (range) | Thrombotic Events | Comments |
|---|---|---|---|---|---|---|
| ||||||
| Studies of one group (triple therapy group) | ||||||
| Orford et al.47 | 2004 | Obs | 66 | 4.5 (0.211.2) | N/A | Bleeding occurred only with suboptimal control of INR and/or pre‐existing GI disease. |
| Porter et al.48 | 2006 | Obs | 180 | 1.6 (0.04.2) | N/A | Bleeding rates were acceptable with short‐term TT after PCI. |
| Rubboli et al.49 | 2007 | Obs | 49 | 18 (4.436.9) | N/A | Most hemorrhages occurred during TT. |
| Rogacka et al.50 | 2008 | Obs | 127 | 4.7 | N/A | One‐half of bleeding episodes were lethal and 67% occurred within the first month. |
| Studies comparing triple therapy with dual antiplatelet therapy | ||||||
| Mattichak et al.51 | 2005 | Obs | 82 | 21 vs. 3.5 (P = .028)a | Reinfarction (29% vs. 9%, P = .15) | TT did not reduce reinfarction after stenting for MI but increased rates of GI bleeding and transfusions. |
| Khurram et al.11 | 2006 | Matched cohort | 214 | 6.6 vs. 0 (P = .03) | N/A | Higher bleeding rates for TT than DAPT. INR range or ASA dosage did not influence the bleeding risk. |
| DeEugenio et al.9 | 2007 | Matched cohort | 194 | OR 5.0 (1.417.8, P = .012) | N/A | ASA dose, age, sex, BMI, DM, hypertension, and procedural anticoagulant type or use did not influence risk of major bleeding. |
| Ruiz‐Nodar et al.52 | 2008 | Obs | 426 | 14.9 vs. 9.0 (P = .19) | Mortality: OR 3.43 (1.617.54, P = .002)b MACE: OR 4.9 (2.1711.1, P .01)b | TT was associated with a nonsignificant increase in major bleeding but lower all‐cause mortality and fewer MACE. |
| Sarafoff et al.53 | 2008 | Prosp | 515 | 1.4 vs. 3.1 (P = .34). | MACCE: OR 0.76 (0.481.21, P = .25) | No difference in MACCE or bleeding at 2 y. Stent thrombosis did not differ between groups. |
| Rossini et al.54 | 2008 | Prosp | 204 | 10.8 vs. 4.9 (P = .1) | MACE: 5.8% vs. 4.9% (P = .7) | INR was targeted to the lower range (2.0‐2.5). No significant difference in bleeding rates for TT versus DAPT at 18 mo. Less bleeding for patients whose INR was within target (4.9 versus 33%, P = .00019). No significant differences in MACE between groups. |
| Uchida et al.55 | 2010 | Obs | 575 | 18 vs. 2.7 (P .001) | MACE (P = .108) | No differences in MACE rates. More bleeding for patients on TT. |
| Studies comparing triple therapy versus dual antiplatelet therapy versus wararin and single antiplatelet agent | ||||||
| Karjalainen et al.10 | 2007 | Matched cohort | 239 | OR 3.3 (1.38.6, P = .014)c | MACE: OR 1.7 (1.0‐3.0, P = 0.05)c | This study compared patients on warfarin at baseline with those not on warfarinall undergoing stenting. Patients on warfarin at baseline were treated with a variety of strategies. Baseline warfarin use increased both major bleeding and MACE at 1 y. ASA plus warfarin was inadequate to prevent stent thrombosis, and premature warfarin cessation was associated with stroke. |
| Manzano‐Fernandez et al.56 | 2008 | Obs | 104 | EB (5.8 vs. 11.3, P = .33) LB (21.6 vs. 3.8, P = .006)d | MACE: 25.5% vs. 21.0% (P = .53)d | No difference in MACE rates between TT and non‐TT (WAA or DAPT). TT conferred higher late bleeding (>48 h). |
| Gao et al.57 | 2010 | Prosp | 622 | 2.9 vs. 1.8 vs. 2.5 (P = .725)e | MACCE: 8.8% vs. 20.1% vs. 14.9% (P = .010)e | Target INR was set as 1.8‐2.5. Lower stroke and MACCE rates for TT as compared with DAPT or WAA; no difference in bleeding. |
| Studies comparing triple therapy with warfarin and single antiplatelet agent | ||||||
| Nguyen et al.58 | 2007 | Obs | 800 | 5.9 vs. 46 (P = .46) | Death: 5.1% vs. 6.5% (P = .47) Stroke: 0.7% vs. 3.4% (P = .02) MI: 3.3% vs. 4.5% (P = .49) | TT and WAA lead to similar 6‐mo bleeding, death, and MI. Fewer strokes with TT (caveat: low event rate). |
In the largest study to date, Nguyen et al.58 evaluated 800 patients who underwent stenting for ACS and were discharged on warfarin plus single antiplatelet agent or triple therapy as part of the GRACE registry. At 6 months, triple therapy conferred a significant reduction in stroke (0.7% versus 3.4%, P = .02) but not in death or MI. There were no differences in in‐hospital major bleeding events between the two groups (5.9% versus 4.6%; P = .46). Similarly, Sarafoff et al.53 reported no significant differences in the combined endpoint (death, MI, stent thrombosis or stroke) or bleeding complications among patients who received triple therapy or DAPT at 2 years of follow‐up. In contrast, Ruiz‐Nodar et al.52 showed that triple therapy, compared with DAPT, at discharge reduced the incidence of death (17.8% versus 27.8%; adjusted HR = 3.43; 95% CI, 1.617.54; P = .002) and major adverse cardiac events (26.5% versus 38.7%; adjusted HR = 4.9; 95% CI, 2.1711.1; P = .01), without a substantial increase in major bleeding events.
The value of combination antiplatelet therapy to prevent stent thrombosis in these patients is clearer in the study reported by Karjalainen et al.10 This case‐control study of 239 patients receiving warfarin at baseline who underwent PCI evaluated a primary endpoint of death, MI, target‐vessel revascularization, or stent thrombosis and a secondary endpoint of major bleeding and stroke to 12 months of follow‐up. Forty‐eight percent of patients received triple therapy, whereas 15.5% were discharged on DAPT. The remaining patients received warfarin plus a single antiplatelet agent. Stent thrombosis occurred more frequently among patients receiving warfarin plus ASA (15.2%) than among those receiving triple therapy (1.9%). As expected, stroke was more frequent in patients treated with DAPT (8.8%) than among those receiving triple therapy (2.8%). Major bleeding was similar between groups. Therapy with warfarin was an independent predictor of both major bleeding and major cardiac events at 1 year. This observation illustrates that the outcome of PCI in patients on chronic warfarin therapy is unsatisfactory irrespective of the antithrombotic combinations used, highlighting the need for better strategies to treat these patients.
Choice of Therapy and Management of Patients Eligible for Triple Therapy
Current guidelines for PCI do not provide guidance for patients with an indication for triple therapy due to a paucity of published evidence. Several ongoing prospective trials aim to address the management of these patients (AFCAS, ISAR‐TRIPLE). Pending further study, clinicians should consider the embolic risk (CHADS2 score), target INR, type of stent, bleeding risk, and duration of treatment when determining the appropriate antiplatelet/anticoagulant combinations. The CHADS2 score (Table 2) stratifies the risk for stroke among patients with AF,4 while the Outpatient Bleeding Risk Index (OBRI) allows estimation of bleeding risk.12, 61 The OBRI considers age > 65 years, prior stroke, prior gastrointestinal bleeding, and any of four comorbidities (recent MI, anemia, diabetes, or renal insufficiency) in order to stratify patients into three risk groups.61 Patients with three to four risk factors have a high risk of bleeding (23% at 3 months and 48% at 12 months) whereas patients with no risk factors have only a 3% risk of bleeding at 12 months. Unfortunately, advanced age and prior stroke appear in both OBRI and CHADS.
For patients with AF who are at high risk for embolic stroke (>3% per year), we recommend triple therapy for the shortest time possible, followed by warfarin and ASA indefinitely. In case of BMS, it is acceptable to shorten triple therapy duration to 1 month. The optimal duration of triple therapy for patients with DES is uncertain; recommended durations range from 3 months to 1 year.62 If the potential consequences of stent thrombosis are high due to a large amount of myocardium at risk, an extended period of triple therapy might be justified. For patients whose stroke risk is lower (CHADS2 score of 0‐1), the risk for bleeding likely outweighs any benefit from stroke prevention. In this instance, it is reasonable to use DAPT with ASA and clopidogrel for 1 month after BMS and 12 months after DES, followed by ASA, with or without warfarin, indefinitely. In a recently published study, patients with AF and a CHADS2 score of 1 had a yearly stroke risk of 1.25% while taking DAPT63; the risk of major bleeding for triple therapy is 6.1% per year.64
For patients who have a high bleeding risk, BMS are the preferred stent type as the duration of triple therapy might be limited to 4 weeks. To our knowledge, no randomized study has evaluated the outcome of patients with BMS compared with DES who also have an indication for warfarin. Because studies have suggested that clopidogrel is more effective than aspirin in preventing stent thrombosis and in reducing death or MI after coronary stenting,40, 65 warfarin and single antiplatelet therapy with clopidogrel might be a reasonable treatment option in patients with high bleeding risk. The WOEST study (NCT00769938), currently recruiting participants, is the first randomized study specifically designed to test this hypothesis.
Since gastrointestinal bleeding accounts for approximately 30‐40% of hemorrhagic events in patients on combined ASA and anticoagulant therapy, an expert consensus document recommended concomitant treatment with proton pump inhibitors (PPIs) to reduce this risk.66 In contrast, the 2009 Focused Updates of the ACC/AHA/SCAI Guidelines did not recommend the use of PPIs with DAPT in the setting of ACS.2 This is because of studies that show inhibition of platelet activation,67 and potential clinical harm,68 when clopidogrel is combined with certain PPIs that inhibit the CYP2C19 enzyme. However, to date there are no convincing randomized clinical trial data documenting an important clinical drug‐drug interaction. The U.S. Food and Drug Administration (FDA) advises that physicians avoid the use of clopidogrel in patients with impaired CYP2C19 function due to known genetic variation or due to concomitant use of drugs that inhibit CYP2C19 activity. More specifically, the FDA recommends avoiding the use of omeprazole and esomeprazole in patients taking clopidogrel.69
In particular, elderly patients have an increased risk of bleeding while receiving triple therapy. In a study of patients over age 65, 2.5% were hospitalized for bleeding in the first year after PCI, and the use of triple therapy was the strongest predictor of bleeding (more than threefold increase).70 One in five patients suffered death or MI at 1 year after hospitalization for bleeding.70 The basis for poor outcomes after hospitalization for bleeding in this population is multifactorial and may be due to the location of bleeding, associated hypercoagulable state, potential adverse impact of blood transfusion, withdrawal of warfarin therapy in patients with AF and PCI, and the premature discontinuation of DAPT. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is common among the elderly and conferred a doubling of bleeding risk.70 Limiting the use of NSAID, the use of low‐dose ASA beyond 30 days after stent implantation, greater use of BMS, and maintaining INR at the lowest possible level (INR of 22.5) will reduce the risk for bleeding.57, 71
New Anticoagulants
Due to the high risk for bleeding with warfarin and the challenges inherent in INR monitoring, researchers have developed several novel anticoagulants whose advantages include fixed daily dosing and no need for monitoring. Dabigatran is a direct oral thrombin inhibitor that is already licensed in Europe and Canada for thromboprophylaxis after hip or knee surgery. It has also been studied in patients with AF. In the RE‐LY trial, patients with AF who received dabigatran 110 mg daily had rates of stroke and systemic embolism that were similar to those with warfarin, as well as lower rates of major hemorrhage.72 The randomized ReDEEM trial, reported at the AHA 2009 Scientific Sessions, was aimed at finding a dosage of dabigatran that achieves a good balance between clinical effectiveness and bleeding risk when combined with aspirin and clopidogrel after acute MI. Dosages ranging from 50 mg twice daily to 150 mg twice daily were all associated with 6‐month rates of bleeding lower than 2%. Hospitalists should view these encouraging results cautiously until the publication of ReDEEM trial results in a peer‐reviewed journal.
A variety of oral Xa antagonists are also being evaluated in patients with AF or ACS. These trials offer insight into triple therapy regimens that include ASA, clopidogrel, and an Xa antagonist. In a recent study of the oral Xa antagonist rivaroxaban, investigators stratified 3491 subjects with ACS according to whether they received concomitant ASA alone or ASA and clopidogrel.73 Subjects receiving ASA plus rivaroxaban had a modest increase in bleeding. Triple therapy, however, increased the composite bleeding rate from 3.5% in the DAPT group to approximately 6‐15% (low‐dose or high‐dose rivaroxaban, respectively). Rivaroxaban is currently under review by the FDA.
These novel agents might eventually replace warfarin for many or most indications for anticoagulation. It is imperative that future research compare the efficacy and risk of bleeding between triple therapy using these new agents and triple therapy with warfarin.
Conclusions
The management of patients on long‐term anticoagulation who require DAPT because of ACS or coronary stenting is challenging. DAPT may safely substitute for warfarin only for patients at low risk for a thromboembolic event (ie, low‐risk AF with low CHADS2 score). Clinicians should not interrupt warfarin in patients at higher risk (ie, intermediate to high‐risk AF, mechanical valves, or recent venous thromboembolism), even in the presence of DAPT. In these patients, triple therapy is the optimal approach following coronary stenting (and possibly during the initial period after ACS without stenting). As this approach confers a fivefold increase in bleeding complications compared with DAPT, careful monitoring of the INR, the addition of PPIs, and the exclusion of elderly patients who are at the highest risk for bleeding complications74 is recommended. The preferred duration of triple therapy after BMS in patients who require long‐term anticoagulation is 1 month, whereas the optimal duration after ACS or DES remains unresolved.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
- ,,, et al.2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee.Circulation2008;117:261–295.
- ,,, et al.2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.Circulation2009;120:2271–2306.
- ,,, et al.ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine.J Am Coll Cardiol2007;50:e1–e157.
- ,,, et al.Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin.Circulation2004;110:2287–2292.
- ,,.Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses.Circulation1994;89:635–641.
- ,,,,.Aspirin use among adults aged 40 and older in the United States: results of a national survey.Am J Prev Med2007;32:403–407.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th Edition).Chest2008;133:299S–339S.
- ,,, et al.Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry.Am Heart J2008;155:361–368.
- ,,, et al.Risk of major bleeding with concomitant dual antiplatelet therapy after percutaneous coronary intervention in patients receiving long‐term warfarin therapy.Pharmacotherapy2007;27:691–696.
- ,,, et al.Safety and efficacy of combined antiplatelet‐warfarin therapy after coronary stenting.Eur Heart J2007;28:726–732.
- ,,, et al.Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding.J Invasive Cardiol2006;18:162–164.
- ,,,,,.Development of a contemporary bleeding risk model for elderly warfarin recipients.Chest2006;130:1390–1396.
- ,,, et al.Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST‐segment elevation.N Engl J Med2005;352:1179–1189.
- ,,, et al.Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo‐controlled trial.Lancet2005;366:1607–1621.
- ,,,,,.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST‐segment elevation.N Engl J Med2001;345:494–502.
- ,,, et al.Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial.JAMA2002;288:2411–2420.
- ,,, et al.Effects of pretreatment with clopidogrel and aspirin followed by long‐term therapy in patients undergoing percutaneous coronary intervention: the PCI‐CURE study.Lancet2001;358:527–533.
- ,,, et al.Guidelines for the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes.Eur Heart J2007;28:1598–1660.
- .Burden of disease: medical and economic impact of acute coronary syndromes.Am J Manag Care2006;12:S430–S434.
- ,,,,,.Variability in platelet responsiveness to clopidogrel among 544 individuals.J Am Coll Cardiol2005;45:246–251.
- ,,, et al.Dose comparisons of clopidogrel and aspirin in acute coronary syndromes.N Engl J Med2010;363:930–942.
- ,,, et al.A clinical trial comparing three antithrombotic‐drug regimens after coronary‐artery stenting. Stent Anticoagulation Restenosis Study Investigators.N Engl J Med1998;339:1665–1671.
- ,,, et al.A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary‐artery stents.N Engl J Med1996;334:1084–1089.
- ,,.Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug‐eluting stents: report of the DEScover Registry.Circulation2006;114:2154–2162.
- ,,, et al.Safety and efficacy of sirolimus‐ and paclitaxel‐eluting coronary stents.N Engl J Med2007;356:998–1008.
- ,,, et al.Comparison of the impact of short (1 year) and long‐term (> or =1 year) clopidogrel use following percutaneous coronary intervention on mortality.Am J Cardiol2008;102:1159–1162.
- ,,.Stent thrombosis late after implantation of first‐generation drug‐eluting stents: a cause for concern.Circulation2007;115:1440–1455; discussion 55.
- ,,, et al.Early and late coronary stent thrombosis of sirolimus‐eluting and paclitaxel‐eluting stents in routine clinical practice: data from a large two‐institutional cohort study.Lancet2007;369:667–678.
- ,,, et al.Analysis of 14 trials comparing sirolimus‐eluting stents with bare‐metal stents.N Engl J Med2007;356:1030–1039.
- ,,,,,.Long‐term outcomes with drug‐eluting stents versus bare‐metal stents in Sweden.N Engl J Med2007;356:1009–1019.
- ,,,,,.Stent thrombosis in randomized clinical trials of drug‐eluting stents.N Engl J Med2007;356:1020–1029.
- ,,, et al.Stent thrombosis, clinical events, and influence of prolonged clopidogrel use after placement of drug‐eluting stent data from an observational cohort study of drug‐eluting versus bare‐metal stents.JACC Cardiovasc Interv2008;1:494–503.
- ,,, et al.Temporal relation between Clopidogrel cessation and stent thrombosis after drug‐eluting stent implantation.Am J Cardiol2009;103:801–805.
- ,,, et al.Effect of prolonged thienopyridine use after drug‐eluting stent implantation (from the TAXUS landmark trials data).Am J Cardiol2008;102:1017–1022.
- ,,, et al.Effectiveness of two‐year clopidogrel + aspirin in abolishing the risk of very late thrombosis after drug‐eluting stent implantation (from the TYCOON [two‐year ClOpidOgrel need] study).Am J Cardiol2009;104:1357–1361.
- ,,.Mortality in randomized controlled trials comparing drug‐eluting vs. bare metal stents in coronary artery disease: a meta‐analysis.Eur Heart J2006;27:2784–2814.
- ,,, et al.Sirolimus‐eluting stents versus standard stents in patients with stenosis in a native coronary artery.N Engl J Med2003;349:1315–1323.
- ,,, et al.A polymer‐based, paclitaxel‐eluting stent in patients with coronary artery disease.N Engl J Med2004;350:221–231.
- ,,, et al.Duration of dual antiplatelet therapy after implantation of drug‐eluting stents.N Engl J Med2010;362:1374–1382.
- ,,, et al.Clopidogrel use and long‐term clinical outcomes after drug‐eluting stent implantation.JAMA2007;297:159–168.
- ,,.The effect of warfarin on mortality and reinfarction after myocardial infarction.N Engl J Med1990;323:147–152.
- Effect of long‐term oral anticoagulant treatment on mortality and cardiovascular morbidity after myocardial infarction.Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group.Lancet1994;343:499–503.
- ,,,,.Warfarin, aspirin, or both after myocardial infarction.N Engl J Med2002;347:969–974.
- ,,,,.Aspirin and coumadin after acute coronary syndromes (the ASPECT‐2 study): a randomised controlled trial.Lancet2002;360:109–113.
- ,,, et al.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial.Lancet2006;367:1903–1912.
- ,,,.Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis.Ann Intern Med1999;131:492–501.
- ,,, et al.Safety and efficacy of aspirin, clopidogrel, and warfarin after coronary stent placement in patients with an indication for anticoagulation.Am Heart J2004;147:463–467.
- ,,,,,.Short‐term triple therapy with aspirin, warfarin, and a thienopyridine among patients undergoing percutaneous coronary intervention.Catheter Cardiovasc Interv2006;68:56–61.
- ,,,,.Periprocedural and medium‐term antithrombotic strategies in patients with an indication for long‐term anticoagulation undergoing coronary angiography and intervention.Coron Artery Dis2007;18:193–199.
- ,,, et al.Dual antiplatelet therapy after percutaneous coronary intervention with stent implantation in patients taking chronic oral anticoagulation.JACC Cardiovasc Interv2008;1:56–61.
- ,,,,,.Evaluation of safety of warfarin in combination with antiplatelet therapy for patients treated with coronary stents for acute myocardial infarction.J Interv Cardiol2005;18:163–166.
- ,,, et al.Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis.J Am Coll Cardiol2008;51:818–825.
- ,,, et al.Aspirin and clopidogrel with or without phenprocoumon after drug eluting coronary stent placement in patients on chronic oral anticoagulation.J Intern Med2008;264:472–480.
- ,,, et al.Long‐term outcomes in patients undergoing coronary stenting on dual oral antiplatelet treatment requiring oral anticoagulant therapy.Am J Cardiol2008;102:1618–1623.
- ,,,,.Impact of anticoagulant therapy with dual antiplatelet therapy on prognosis after treatment with drug‐eluting coronary stents.J Cardiol2010;55:362–369.
- ,,, et al.Increased major bleeding complications related to triple antithrombotic therapy usage in patients with atrial fibrillation undergoing percutaneous coronary artery stenting.Chest2008;134:559–567.
- ,,, et al.Comparison of different antithrombotic regimens for patients with atrial fibrillation undergoing drug‐eluting stent implantation.Circ J2010;74:701–708.
- ,,, et al.Combining warfarin and antiplatelet therapy after coronary stenting in the Global Registry of Acute Coronary Events: is it safe and effective to use just one antiplatelet agent?Eur Heart J2007;28:1717–1722.
- ,,, et al.2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2008;51:210–247.
- ,,, et al.Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology.Eur Heart J2005;26:804–847.
- ,,.Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin.Am J Med1998;105:91–99.
- ,,,.Coronary stents and chronic anticoagulation.Circulation2009;119:1682–1688.
- ,,, et al.Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE‐W).Stroke2008;39:1482–1486.
- ,,, et al.Early and late increased bleeding rates after angioplasty and stenting due to combined antiplatelet and anticoagulanttherapy.EuroIntervention2009;5:425–431.
- ,,, et al.Late clinical events after clopidogrel discontinuation may limit the benefit of drug‐eluting stents: an observational study of drug‐eluting versus bare‐metal stents.J Am Coll Cardiol2006;48:2584–2591.
- ,,, et al.ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents.Circulation2008;118:1894–1909.
- ,,, et al.Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double‐blind OCLA (Omeprazole CLopidogrel Aspirin) study.J Am Coll Cardiol2008;51:256–260.
- ,,, et al.Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome.JAMA2009;301:937–944.
- Follow‐Up to the January 26,2009, Early Communication about an Ongoing Safety Review of Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC). 11/17/2009. (Accessed at http://www.fda.gov/Drugs/DrugSafety/Postmarket DrugSafetyInformationforPatientsandProviders/DrugSafetyInformationfor HeathcareProfessionals/ucm190784.htm.)
- ,,, et al.Incidence, predictors, and prognostic implications of hospitalization for late bleeding after percutaneous coronary intervention for patients older than 65 years.Circ Cardiovasc Interv2010;3:140–147.
- ,,, et al.Antithrombotic therapy in patients treated with oral anticoagulation undergoing coronary artery stenting. An expert consensus document with focus on atrial fibrillation.Ann Med2008;40:428–436.
- ,,, et al.Dabigatran versus warfarin in patients with atrial fibrillation.N Engl J Med2009;361:1139–1151.
- ,,, et al.Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS‐TIMI 46): a randomised, double‐blind, phase II trial.Lancet2009;374:29–38.
- ,,,.Bleeding complications associated with combinations of aspirin, thienopyridine derivatives, and warfarin in elderly patients following acute myocardial infarction.Arch Intern Med2005;165:784–789.
A Pain in the Bone
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
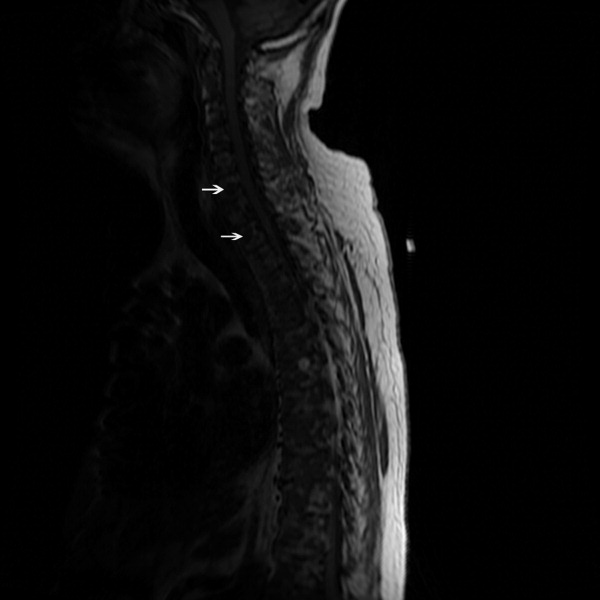
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

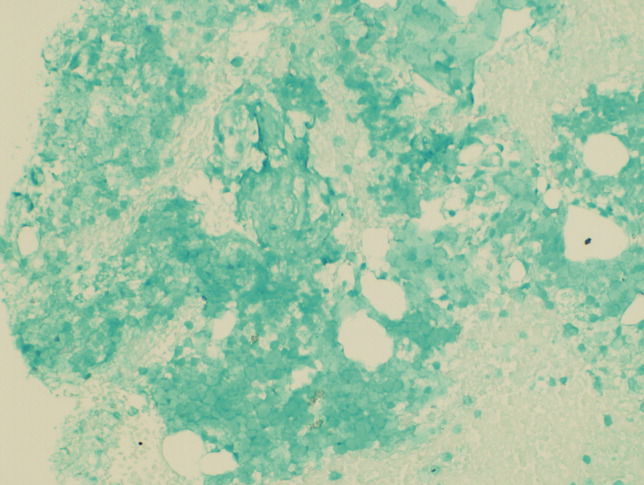
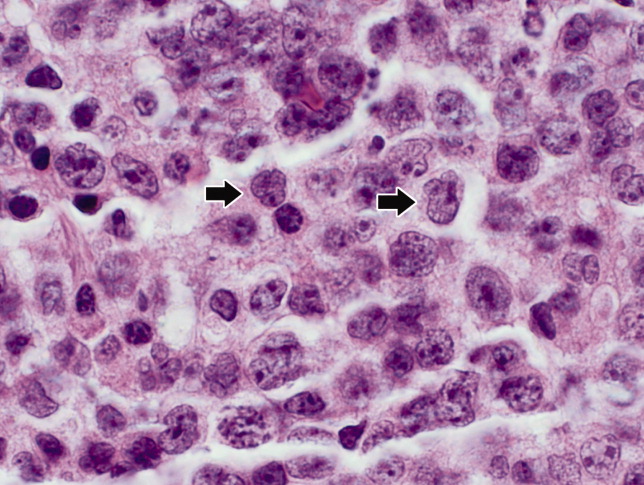
The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
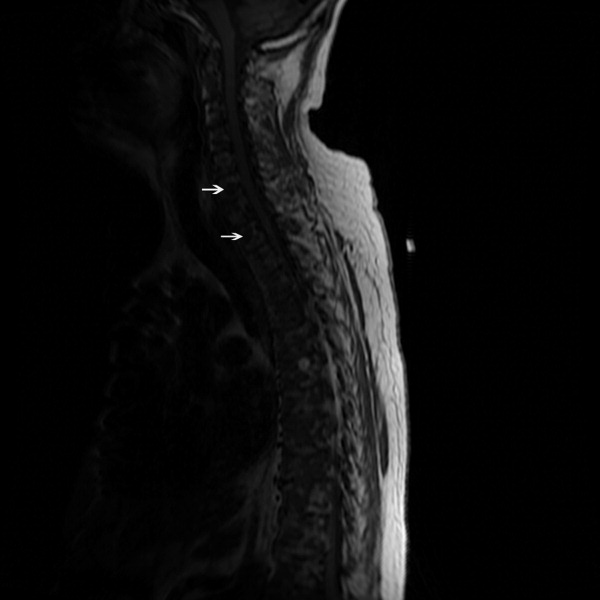
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

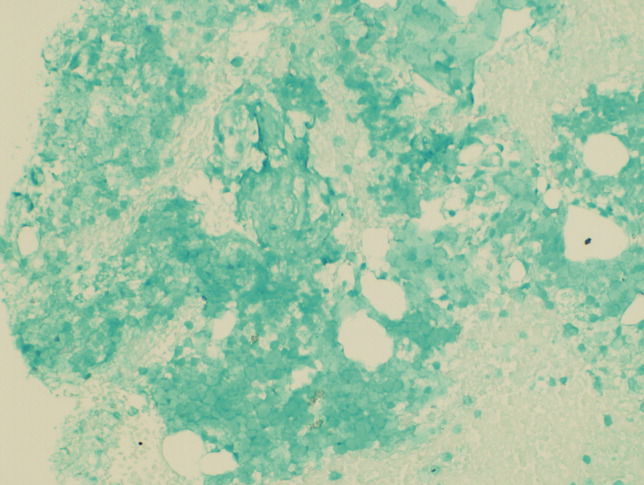
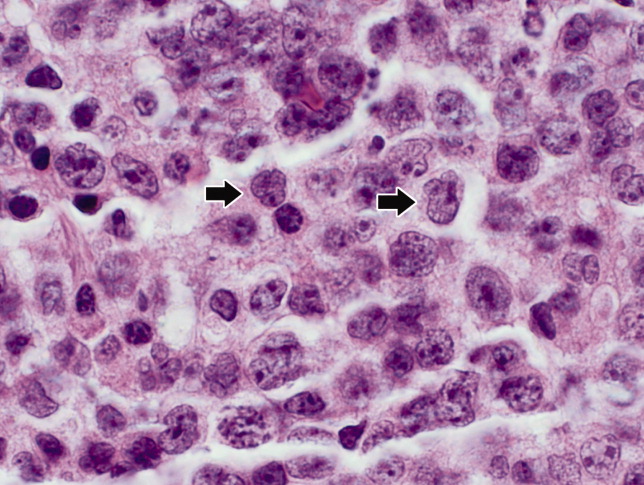
The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
A 71‐year‐old man presented to a hospital with a one week history of fatigue, polyuria, and polydipsia. He also reported pain in his back, hips, and ribs, in addition to frequent falls, intermittent confusion, constipation, and a weight loss of 10 pounds over the last 2 weeks. He denied cough, shortness of breath, chest pain, fever, night sweats, headache, and focal weakness.
Polyuria, which is often associated with polydipsia, can be arbitrarily defined as a urine output exceeding 3 L per day. After excluding osmotic diuresis due to uncontrolled diabetes mellitus, the 3 major causes of polyuria are primary polydipsia, central diabetes insipidus, and nephrogenic diabetes insipidus. Approximately 30% to 50% of cases of central diabetes insipidus are idiopathic; however, primary or secondary brain tumors or infiltrative diseases involving the hypothalamic‐pituitary region need to be considered in this 71‐year‐old man. The most common causes of nephrogenic diabetes insipidus in adults are chronic lithium ingestion, hypokalemia, and hypercalcemia. The patient describes symptoms that can result from severe hypercalcemia, including fatigue, confusion, constipation, polyuria, and polydipsia.
The patient's past medical history included long‐standing, insulin‐requiring type 2 diabetes with associated complications including coronary artery disease, transient ischemic attacks, proliferative retinopathy, peripheral diabetic neuropathy, and nephropathy. Seven years prior to presentation, he received a cadaveric renal transplant that was complicated by BK virus (polyomavirus) nephropathy and secondary hyperparathyroidism. Three years after his transplant surgery, he developed squamous cell carcinoma of the skin, which was treated with local surgical resection. Two years after that, he developed stage I laryngeal cancer of the glottis and received laser surgery, and since then he had been considered disease‐free. He also had a history of hypertension, hypercholesterolemia, osteoporosis, and depression. His medications included aspirin, amlodipine, metoprolol succinate, valsartan, furosemide, simvastatin, insulin, prednisone, sirolimus, and sulfamethoxazole/trimethoprim. He was a married psychiatrist. He denied tobacco use and reported occasional alcohol use.
The prolonged immunosuppressive therapy that is required following organ transplantation carries a markedly increased risk of the subsequent development of malignant tumors, including cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma. Primary brain lymphoma resulting in central diabetes insipidus would be unlikely in the absence of headache or focal weakness. An increased risk of lung cancer occurs in recipients of heart and lung transplants, and to a much lesser degree, recipients of kidney transplants. However, metastatic lung cancer is less likely in the absence of respiratory symptoms and smoking history (present in approximately 90% of all lung cancers). Nephrogenic diabetes insipidus, in its mild form, is relatively common in elderly patients with acute or chronic renal insufficiency because of a reduction in maximum urinary concentrating ability. On the other hand, this alone does not explain his remaining symptoms. The instinctive diagnosis in this case is tertiary hyperparathyroidism due to progression of untreated secondary hyperparathyroidism. This causes hypercalcemia, nephrogenic diabetes insipidus, and significant bone pain related to renal osteodystrophy.
On physical exam, the patient appeared chronically ill, but was in no acute distress. He weighed 197.6 pounds and his height was 70.5 inches. He was afebrile with a blood pressure of 146/82 mm Hg, a heart rate of 76 beats per minute, a respiratory rate of 12 breaths per minute, and an oxygen saturation of 97% while breathing room air. He had no generalized lymphadenopathy. Thyroid examination was unremarkable. Examination of the lungs, heart, abdomen, and lower extremities was normal. The rectal examination revealed no masses or prostate nodules; a test for fecal occult blood was negative. He had loss of sensation to light touch and vibration in the feet with absent Achilles deep tendon reflexes. He had a poorly healing surgical wound on his forehead at the site of his prior skin cancer, but no rash or other lesions. There was no joint swelling or erythema. There were tender points over the cervical, thoracic, and lumbar spine; on multiple ribs; and on the pelvic rims.
Perhaps of greatest importance is the lack of lymphadenopathy, organomegaly, or other findings suggestive of diffuse lymphoproliferative disease. His multifocal bone tenderness is concerning for renal osteodystrophy, multiple myeloma, or primary or metastatic bone disease. Cancers in men that metastasize to the bone usually originate from the prostate, lung, kidney, or thyroid gland. In any case, his physical examination did not reveal an enlarged, asymmetric, or nodular prostate or thyroid gland. I recommend a chest film to rule out primary lung malignancy and a basic laboratory evaluation to narrow down the differential diagnosis.
A complete blood count showed a normocytic anemia with a hemoglobin of 8.7 g/dL and a hematocrit of 25%. Other laboratory tests revealed the following values: sodium, 139 mmol/L; potassium, 4.1 mmol/L; blood urea nitrogen, 70 mg/dL; creatinine, 3.5 mg/dL (most recent value 2 months ago was 1.9 mg/dL); total calcium, 13.2 mg/dL (normal range, 8.5‐10.5 mg/dL); phosphate, 5.3 mg/dL; magnesium, 2.5 mg/dL; total bilirubin, 0.5 mg/dL; alkaline phosphatase, 130 U/L; aspartate aminotransferase, 28 U/L; alanine aminotransferase, 19 U/L; albumin, 3.5 g/dL; and lactate dehydrogenase (LDH), 1258 IU/L (normal range, 105‐333 IU/L). A chest radiograph was normal.
The most important laboratory findings are severe hypercalcemia, acute on chronic renal failure, and anemia. Hypercalcemia most commonly results from malignancy or hyperparathyroidism. Less frequently, hypercalcemia may result from sarcoidosis, vitamin D intoxication, or hyperthyroidism. The degree of hypercalcemia is useful diagnostically as hyperparathyroidism commonly results in mild hypercalcemia (serum calcium concentration often below 11 mg/dL). Values above 13 mg/dL are unusual in hyperparathyroidism and are most often due to malignancy. Malignancy is often evident clinically by the time it causes hypercalcemia, and patients with hypercalcemia of malignancy are more often symptomatic than those with hyperparathyroidism. Additionally, localized bone pain and weight loss do not result from hypercalcemia itself and their presence also raises concern for malignancy.
Nonmelanoma skin cancer is the most common cancer occurring after transplantation but does not cause hypercalcemia. Squamous cancers of the head and neck can rarely cause hypercalcemia due to secretion of parathyroid hormone‐related peptide; however, his early‐stage laryngeal cancer and the expected high likelihood of cure argue against this possibility. Osteolytic metastases account for approximately 20% of cases of hypercalcemia of malignancy (Table 1). Prostate cancer rarely results in hypercalcemia since bone metastases are predominantly osteoblastic, whereas metastatic non‐small‐cell lung cancer, thyroid cancer, and kidney cancer more commonly cause hypercalcemia due to osteolytic bone lesions. The total alkaline phosphatase has been traditionally used to assess the osteoblastic component of bone remodeling. Its normal level tends to predict a negative bone scan and supports the likelihood of lytic lesions. Posttransplantation lymphoproliferative disorders, which include a wide range of syndromes, can rarely result in hypercalcemia. I am also worried about the possibility of multiple myeloma as he has the classic triad of hypercalcemia, bone pain, and subacute kidney injury.
|
| Osteolytic metastases |
| Breast cancer |
| Multiple myeloma |
| Lymphoma |
| Leukemia |
| Humoral hypercalcemia (PTH‐related protein) |
| Squamous cell carcinomas |
| Renal carcinomas |
| Bladder carcinoma |
| Breast cancer |
| Ovarian carcinoma |
| Leukemia |
| Lymphoma |
| 1,25‐Dihydroxyvitamin D secretion |
| Lymphoma |
| Ovarian dysgerminomas |
| Ectopic PTH secretion (rare) |
| Ovarian carcinoma |
| Lung carcinomas |
| Neuroectodermal tumor |
| Thyroid papillary carcinoma |
| Rhabdomyosarcoma |
| Pancreatic cancer |
The first purpose of the laboratory evaluation is to differentiate parathyroid hormone (PTH)‐mediated hypercalcemia (primary and tertiary hyperparathyroidism) from non‐PTH‐mediated hypercalcemia (primarily malignancy, hyperthyroidism, vitamin D intoxication, and granulomatous disease). The production of vitamin D metabolites, PTH‐related protein, or hypercalcemia from osteolysis in these latter cases results in suppressed PTH levels.
In severe elevations of calcium, the initial goals of treatment are directed toward fluid resuscitation with normal saline and, unless contraindicated, the immediate institution of bisphosphonate therapy. A loop diuretic such as furosemide is often used, but a recent review concluded that there is little evidence to support its use in this setting.
The patient was admitted and treated with intravenous saline and furosemide. Additional laboratory evaluation revealed normal levels of prostate‐specific antigen and thyroid‐stimulating hormone. PTH was 44 pg/mL (the most recent value was 906 pg/mL eight years ago; normal range, 15‐65 pg/mL) and beta‐2 microglobulin (B2M) was 8 mg/L (normal range, 0.8‐2.2 mg/L).
The normal PTH level makes tertiary hyperparathyroidism unlikely and points toward non‐PTH‐related hypercalcemia. An elevated B2M level may occur in patients with chronic graft rejection, renal tubular dysfunction, dialysis‐related amyloidosis, multiple myeloma, or lymphoma. LDH is often elevated in patients with multiple myeloma and lymphoma, but this is not a specific finding. The next laboratory test would be measurement of PTH‐related protein and vitamin D metabolites, as these tests can differentiate between the causes of non‐PTH‐mediated hypercalcemia.
Serum concentrations of the vitamin D metabolites, 25‐hydroxyvitamin D (calcidiol) and 1,25‐dihydroxyvitamin D (calcitriol), were low‐normal. PTH‐related protein was not detected.
The marked elevation of serum LDH and B2M, the relatively suppressed PTH level, combined with undetectable PTH‐related protein suggest multiple myeloma or lymphoma as the likely cause of the patient's clinical presentation. The combination of hypercalcemia and multifocal bone pain makes multiple myeloma the leading diagnosis as hypercalcemia is uncommon in patients with lymphoma, especially at the time of initial clinical presentation.
I would proceed with serum and urine protein electrophoresis (SPEP and UPEP, respectively) and a skeletal survey. If these tests do not confirm the diagnosis of multiple myeloma, I would order a noncontrast computed tomography (CT) of the chest and abdomen and a magnetic resonance imaging (MRI) of the spine. In addition, I would like to monitor his response to the intravenous saline and furosemide.
Forty‐eight hours after presentation, repeat serum calcium and creatinine levels were 11.3 mg/dL and 2.9 mg/dL, respectively. He received salmon calcitonin 4 U/kg every 12 hours. Pamidronate was avoided because of his kidney disease. His confusion resolved. He received intravenous morphine intermittently to alleviate his bone pain.
The SPEP revealed a monoclonal immunoglobulin G (IgG) lambda (light chain) spike representing roughly 3% (200 mg/dL) of total protein. His serum Ig levels were normal. The UPEP was negative for monoclonal immunoglobulin and Bence‐Jones protein. The skeletal survey revealed marked osteopenia, and the bone scan was normal. An MRI of the spine showed multiple round lesions in the cervical, thoracic, and lumbar spine (Figure 1). A CT of the chest showed similar bone lesions in the ribs and pelvis. A CT of the abdomen and chest did not suggest any primary malignancy nor did it show thoracic or abdominal lymphadenopathy.
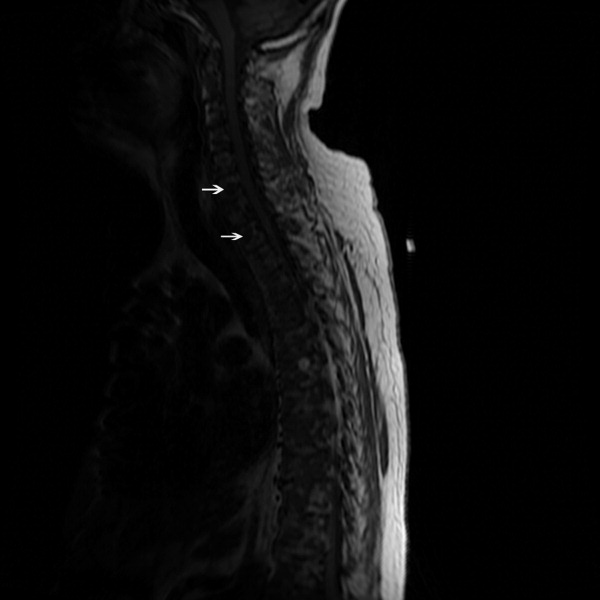
The lack of lymphadenopathy, splenomegaly, or a visceral mass by CT imaging and physical examination, along with the normal PSA level, exclude most common forms of non‐Hodgkin lymphoma and bone metastasis from solid tumors. In multiple myeloma, cytokines secreted by plasma cells suppress osteoblast activity; therefore, while discrete lytic bone lesions are apparent on skeletal survey, the bone scan is typically normal. The absence of lytic lesions, normal serum immunoglobulin levels, and unremarkable UPEP make multiple myeloma or light‐chain deposition disease a less likely diagnosis.
Typically, primary lymphoma of the bone produces increased uptake with bone scanning. However, because primary lymphoma of the bone is one of the least common primary skeletal malignancies and varies widely in appearance on imaging, confident diagnosis based on imaging alone usually is not possible.
Posttransplantation lymphoproliferative disorder (PTLD) refers to a syndrome that ranges from a self‐limited form of lymphoproliferation to an aggressive disseminated disease. Although the patient is at risk for PTLD, isolated bone involvement has only rarely been reported.
Primary lymphoma of the bone and PTLD are my leading diagnoses in this patient. At this point, I recommend a bone marrow biopsy and biopsy of an easily accessible representative bone lesion with special staining for Epstein‐Barr virus (EBV) (EBV‐encoded RNA [EBER] and latent membrane protein 1 [LMP1]). I expect this test to provide a definitive diagnosis. As 95% of PTLD cases are induced by infection with EBV, information regarding pretransplantation EBV status of the patient and the donor, current EBV status of the patient, and type and intensity of immunosuppression at the time of transplantation would be very helpful to determine their likelihood.
Seventy‐two hours after presentation, his serum calcium level normalized and most of his symptoms improved. Calcitonin was discontinued, and he was maintained on oral hydration. On hospital day number 5, he underwent CT‐guided bone biopsy of the L4 vertebral body, which showed large aggregates of atypical lymphoid cells (Figure 2). These cells were predominantly B‐cells interspersed with small reactive T‐cells. The cells did not express EBV LMP1 or EBER (Figure 3). On hospital day 7, he underwent a bone marrow biopsy, which revealed similar large atypical lymphoid cells that comprised the majority of marrow space (Figure 4). By immunohistochemistry, these cells brightly expressed the pan B cell marker, CD20, and coexpressed bcl‐2. EBER and LMP1 were also negative. A flow cytometry of the bone marrow demonstrated a lambda light chain restriction within the B lymphocytes.

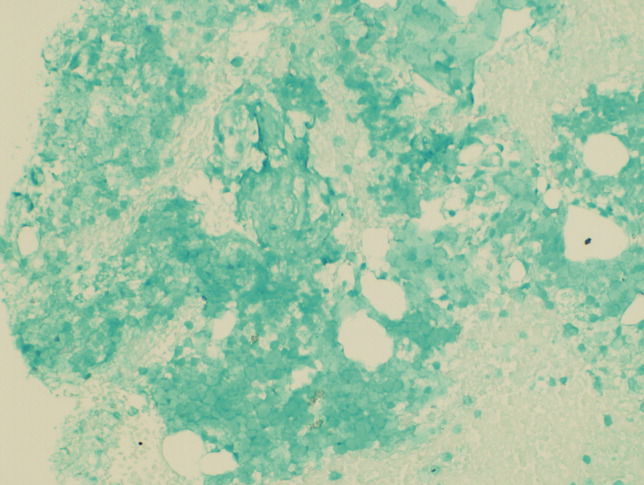
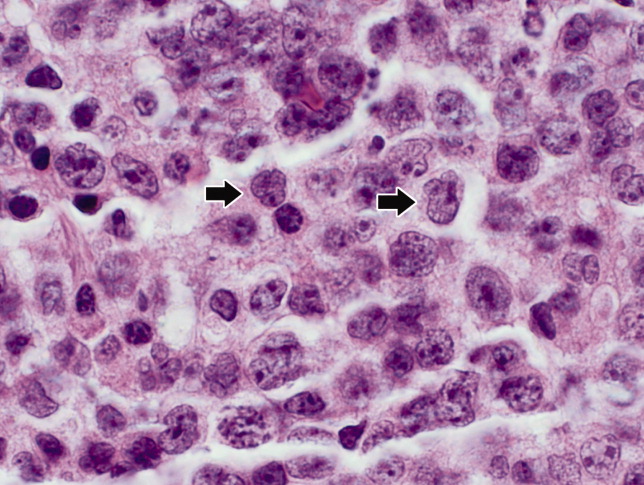
The medical records indicated that the patient had positive pretransplantation EBV serologies. He received a regimen based on sirolimus, mycophenolate mofetil, and prednisone, and did not receive high doses of induction or maintenance immunosuppressive therapy.
The biopsy results establish a diagnosis of diffuse large B‐cell lymphoma of the bone. PTLD is unlikely given his positive pretransplantation EBV status, the late onset of his disease (6 years after transplantation), the isolated bone involvement, and the negative EBER and LMP1 tests.
The patient was discharged and was readmitted 1 week later for induction chemotherapy with etoposide, vincristine, doxorubicin, cyclophosphamide, and prednisone [EPOCH]Rituxan (rituximab). Over the next several months, he received 6 cycles of chemotherapy, his hypercalcemia resolved, and his back pain improved.
Commentary
Hypercalcemia is among the most common causes of nephrogenic diabetes insipidus in adults.1 A urinary concentrating defect usually becomes clinically apparent if the plasma calcium concentration is persistently above 11 mg/dL.1 This defect is generally reversible with correction of the hypercalcemia but may persist in patients in whom interstitial nephritis has induced permanent medullary damage. The mechanism by which the concentrating defect occurs is incompletely understood but may be related to impairments in sodium chloride reabsorption in the thick ascending limb and in the ability of antidiuretic hormone to increase water permeability in the collecting tubules.1
Although hypercalcemia in otherwise healthy outpatients is usually due to primary hyperparathyroidism, malignancy is more often responsible for hypercalcemia in hospitalized patients.2 While the signs and symptoms of hypercalcemia are similar regardless of the cause, several clinical features may help distinguish the etiology of hypercalcemia. For instance, the presence of tachycardia, warm skin, thinning of the hair, stare and lid lag, and widened pulse pressure points toward hypercalcemia related to hyperthyroidism. In addition, risk factors and comorbidities guide the diagnostic process. For example, low‐level hypercalcemia in an asymptomatic postmenopausal woman with a normal physical examination suggests primary hyperparathyroidism. In contrast, hypercalcemia in a transplant patient raises concern of malignancy including PTLDs.3, 4
PTLDs are uncommon causes of hypercalcemia but are among the most serious and potentially fatal complications of chronic immunosuppression in transplant recipients.5 They occur in 1.9% of patients after kidney transplantation. The lymphoproliferative disorders occurring after transplantation have different characteristics from those that occur in the general population. Non‐Hodgkin lymphoma accounts for 65% of lymphomas in the general population, compared to 93% in transplant recipients.5, 6 The pathogenesis of PTLD appears to be related to B cell proliferation induced by infection with EBV in the setting of chronic immunosuppression.6 Therefore, there is an increased frequency of PTLD among transplant recipients who are EBV seronegative at the time of operation. These patients, who have no preoperative immunity to EBV, usually acquire the infection from the donor. The level of immunosuppression (intensity and type) influences PTLD rates as well. The disease typically occurs within 12 months after transplantation and in two‐thirds of cases involves extranodal sites. Among these sites, the gastrointestinal tract is involved in about 26% of cases and central nervous system in about 27%. Isolated bone involvement is exceedingly rare.5, 6
Primary lymphoma of the bone is another rare cause of hypercalcemia and accounts for less than 5% of all primary bone tumors.7 The majority of cases are of the non‐Hodgkin's type, characterized as diffuse large B‐cell lymphomas, with peak occurrence in the sixth to seventh decades of life.8 The classic imaging findings of primary lymphoma of the bone are a solitary metadiaphyseal lesion with a layered periosteal reaction on plain radiographs, and corresponding surrounding soft‐tissue mass on MRI.9 Less commonly, primary lymphoma of the bone can be multifocal with diffuse osseous involvement and variable radiographic appearances, as in this case. Most series have reported that the long bones are affected most frequently (especially the femur), although a large series showed equal numbers of cases presenting in the long bones and the spine.712
In order to diagnose primary lymphoma of the bone, it is necessary to exclude nodal or disseminated disease by physical examination and imaging. As plain films are often normal, bone scan or MRI of clinically affected areas is necessary to establish disease extent.9 Distinguishing primary bone lymphomas (PLB) from other bone tumors is important because PLB has a better response to therapy and a better prognosis.10, 11
Randomized trials addressing treatment options for primary lymphoma of bone are not available. Historically, PLB was treated with radiotherapy alone with good local control. However, the rate of distant relapses was relatively high. Currently, chemotherapy with or without radiation therapy is preferred; 5‐year survival is approximately 70% after combined therapy.10, 11
In this case, symptomatic hypercalcemia, a history of transplantation, marked elevation of both LDH and B2M, and a normal PTH level all pointed toward the correct diagnosis of malignancy. Low or normal levels of vitamin D metabolites and PTH‐related protein occur in 20% of patients with hypercalcemia caused by malignancy.13, 14 Diffuse osteopenia on skeletal survey is a prominent feature of renal osteodystrophy or osteoporosis related to chronic corticosteroid use. However, in a patient with diffuse osteopenia and hypercalcemia, clinicians must consider multiple myeloma and other lymphoproliferative disorders; the absence of osteoblastic or osteolytic lesions and a normal alkaline phosphatase do not rule out these diagnoses. When the results of serum and urine protein electrophoresis exclude multiple myeloma, the next investigation should be a bone biopsy to exclude PLB, an uncommon cause of anemia, hypercalcemia, and osteopenic, painful bones.
Key Points for Hospitalists
-
Normal total alkaline phosphatase does not exclude primary or metastatic bone malignancy. While a normal level tends to predict a negative bone scan, further diagnostic tests are needed to exclude bone malignancy if high clinical suspicion exists.
-
The degree of hypercalcemia is useful diagnostically; values above 13 mg/dL are most often due to malignancy.
-
Hypercalcemia in transplant patients deserves special attention due to an increased risk of malignancy, including squamous cancers of the lips and skin, lymphoproliferative disorders, and bronchogenic carcinoma.
-
While rare, consider primary lymphoma of the bone in patients with hypercalcemia and bone pain, along with the more common diagnoses of multiple myeloma and metastatic bone disease.
The approach to clinical conundrums by an expert clinician is revealed through presentation of an actual patient's case in an approach typical of morning report. Similar to patient care, sequential pieces of information are provided to the clinician who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring the patient and the discussant.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
- ,.Clinical Physiology of Acid‐Base and Electrolyte Disorders.5th ed.New York:McGraw‐Hill;2001:754–758.
- ,.Hypercalcemia: clinical manifestations, pathogenesis, diagnosis, and management. In: Favus MJ, ed.Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism.5th ed.Washington, DC:American Society for Bone and Mineral Research;2003:225–230.
- ,,, et al.Malignancy after renal transplantation: analysis of incidence and risk factors in 1700 patients followed during a 25‐year period.Transplant Proc.1997;29:831–833.
- ,.Malignancy‐associated hypercalcemia. In: DeGroot L, Jameson LJ, eds.Endocrinology.4th ed.Philadelphia, PA:Saunders;2001:1093–1100.
- ,.Diagnosis and management of posttransplant lymphoproliferative disorder in solid‐organ transplant recipients.Clin Infect Dis.2001;33(suppl 1):S38–S46.
- ,,, et al.Epstein‐Barr virus‐induced posttransplant lymphoproliferative disorders: ASTS/ASTP EBV‐PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting.Transplantation.1999;68:1517–1525.
- ,,, et al.Primary bone lymphoma: a new and detailed characterization of 28 patients in a single‐institution study.Jpn J Clin Oncol.2007;37(3):216–223.
- ,,, et al.Diffuse large B‐cell lymphoma of bone. An analysis of differentiation‐associated antigens with clinical correlation.Am J Surg Pathol.2003;27:1269–1277.
- ,,,,,.Primary bone lymphoma: radiographic‐MR imaging correlation.Radiographics.2003;23:1371–1383.
- ,,, et al.Primary bone lymphoma in 24 patients treated between 1955 and 1999.Clin Orthop.2002;397:271–280.
- ,,, et al.A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population‐based study of successively treated cohorts from the British Columbia Cancer Agency.Ann Oncol.2007;18:129.
- ,,, et al.Malignant lymphoma of bone.Cancer.1986;58:2646–2655.
- .Hypercalcemia in malignant lymphoma and leukemia.Ann N Y Acad Sci.1974;230:240–246.
- .Incidence and prognostic significance of hypercalcemia in B‐cell non‐Hodgkin's lymphoma. [Letter]J Clin Pathol.2002;55:637–638.
Postoperative pulmonary complications: An update on risk assessment and reduction
Although pulmonary complications are not as well studied as cardiac complications in the postoperative setting, they are just as common following noncardiac surgery and are even more costly. It is worthwhile to identify surgical patients most at risk of postoperative pulmonary complications and take measures known to mitigate risk. This paper discusses important risk factors to identify during a preoperative pulmonary evaluation and then focuses on recent advances in strategies for reducing postoperative pulmonary complications. Teaching questions are included throughout, along with the rationale behind their answers.
POSTOPERATIVE PULMONARY COMPLICATIONS: WHAT ARE WE TRYING TO PREVENT AND WHY?
The definition of postoperative pulmonary complications is more variable and less intuitive than that of cardiac complications. Cardiac complications—postoperative myocardial infarction, cardiac death, and pulmonary edema—are more consistently defined and measured in clinical trials. Studies of postoperative pulmonary complications often group together pneumonia, respiratory failure, atelectasis, bronchospasm, and exacerbation of chronic obstructive pulmonary disease (COPD), making it more difficult to individually evaluate risk factors for different outcomes.
There are several reasons why it is important to consider pulmonary risk when evaluating patients preoperatively:
Pulmonary complications are as common as cardiac complications following noncardiac surgery. For example, in a secondary analysis of the cohort of noncardiac surgical patients used to validate the Revised Cardiac Risk Index,1 Fleischmann et al found that the incidence of pulmonary complications (2.7%) was highly comparable to that of cardiac complications (2.5%).2
Respiratory failure is a marker of ill health and predicts further complications. Postoperative respiratory failure (often defined as the need for ventilation for more than 48 hours after surgery) is an extremely morbid event. Johnson et al compared the outcomes of patients with and without respiratory failure as a complication of surgery.3 Among patients with respiratory failure, 26% died within 30 days, 6% had a myocardial infarction, 35% developed pneumonia, 10% developed acute renal failure, and 3% developed a deep vein thrombosis or pulmonary embolism; in contrast, rates of each of these events were lower than 2% among patients without respiratory failure.
Pulmonary complications are expensive and require lengthy hospitalization. The National Surgical Quality Improvement Program (NSQIP) compared hospitalization costs and length of stay among patients with various postoperative complications.4 Among infectious, cardiovascular, venous thromboembolic, and pulmonary complications, pulmonary complications were by far the most costly and, along with venous thromboembolic complications, required the longest mean hospital stay.
For these reasons, identifying patients at risk for pulmonary complications and developing a strategy to reduce the risk is clearly worthwhile.
IDENTIFYING RISK FOR PULMONARY COMPLICATIONS
Question: Which of the following is the most important risk factor for postoperative pulmonary complications?
A. High-risk surgical site
B. General anesthesia
C. COPD
D. Obesity
The correct answer is A. Pulmonary complications differ from cardiac complications in an important way: procedure-related factors are more predictive of pulmonary complications than are patient-related factors. Even healthy patients undergoing high-risk surgery are at risk for pulmonary complications. As for the other answer choices, general anesthesia and COPD are risk factors but are not as important as surgical site, and obesity has not been shown to be a risk factor at all.
Take-home points from the 2006 ACP guideline
Patient-related risk factors. As noted in Table 1, the most important patient-related risk factors identified in the ACP guideline are increasing age and increasing American Society of Anesthesiologists (ASA) classification of comorbidity.
The effect of advanced age becomes particularly notable around age 60 years and escalates from there. This effect of age differs from that for cardiac complications, for which age drops out as a risk factor after adjustment for other diseases and risk factors. For pulmonary complications, in contrast, even older patients who are healthy are at increased risk.
The ASA classification is a general index of overall morbidity that ranges from class 1 (normal healthy patient) to class 5 (moribund patient who is not expected to survive without the operation).
Notably, COPD and smoking were only minor risk factors in the ACP analysis.
Procedure-related risk factors. Surgical site was found to be the most important of any of the patient- or procedure-related risk factors. The closer the incision is to the diaphragm, the greater the risk for pulmonary complications. Aortic, thoracic, and abdominal procedures carry the highest risk (Table 1), and among abdominal procedures, upper abdominal surgery (eg, cholecystectomy) is riskier than lower abdominal surgery (eg, gynecologic).
Other procedure-related risk factors identified were emergency surgery, surgery lasting more than 3 hours, use of general anesthesia, and multiple transfusions (Table 1).
Newly identified risk factors
Question: Which of the following has recently been identified as a risk factor for postoperative pulmonary complications?
A. Epidural anesthesia
B. Insulin-treated diabetes
C. Obstructive sleep apnea
D. Immobility
The correct answer is C. There is no evidence that epidural anesthesia or insulin-treated diabetes are risk factors. Immobility seems intuitively correct but has not emerged as a risk factor among high-quality studies in the literature.
Obstructive sleep apnea. The role of obstructive sleep apnea was unclear prior to publication of new data in the last couple of years. Hwang et al enrolled 172 patients who were soon to have elective surgery and had at least two of four clinical features of obstructive sleep apnea (snoring, daytime somnolence, witnessed apnea event, or crowded oropharynx).8 Patients underwent nocturnal oximetry before surgery and were divided into two groups based on number of desaturation episodes per hour. Patients with five or more desaturations had markedly higher rates of postoperative respiratory complications (8 complications among 98 patients) than did patients with fewer than five desaturations (1 complication among 74 patients). The presence of five or more desaturations was also associated with higher rates of cardiac, gastrointestinal, and bleeding complications. Though this was a small study, its results suggest a significant association between obstructive sleep apnea and pulmonary complications.
The issue of whether to screen patients for obstructive sleep apnea before major noncardiac surgery is still unresolved.
Pulmonary hypertension has also been identified as a risk factor in recent years with the publication of two studies that estimated its impact on morbidity and mortality after major noncardiac surgery.9,10 One of the studies, a retrospective database review, found a 28% incidence of respiratory failure among 145 surgical patients with pulmonary hypertension.9 In the other study, a prospective case-control trial, respiratory failure occurred in 21% of patients with pulmonary hypertension compared with only 3% of matched controls.10 In the case-control study, pulmonary hypertension was also associated with significantly elevated rates of heart failure and in-hospital death.
The results of these studies do not support preoperative screening for undiagnosed pulmonary hypertension, but they do underscore the need to recognize established pulmonary hypertension as an important risk factor for postoperative complications.
AN UPDATED INDEX FOR RESPIRATORY FAILURE
Several years ago, investigators from the Veterans Affairs Medical Centers developed a respiratory failure index using a design similar to those of well-established indices for cardiac risk.11 The same group also developed a separate risk index for pneumonia.12
This respiratory failure index was recently updated3 to reflect experience from private and academic hospitals, making the results more generally applicable. The researchers evaluated data from 180,000 patients undergoing major general or vascular surgery (defined according to the NSQIP) over a 3-year period. Respiratory failure was defined as requiring at least 48 hours of ventilation or unplanned reintubation.
Comparison and contrast with the ACP guideline
Question: How does the updated respiratory failure index differ most significantly from the 2006 ACP guideline?
A. New index places greater emphasis on ASA class
B. New index offers a simplified weighted point scheme
C. New index ranks low albumin as a less important risk factor
D. New index attributes low risk to cigarette use
The correct answer is C: low albumin is a minor risk factor in the respiratory failure index, whereas it was one of the single most important predictors in the ACP guideline. As for the other answer choices, the new index places about the same emphasis on ASA class and cigarette use as does the ACP guideline, and it does not offer a simplified approach, as it incorporates 28 different factors.
Overall, most risk factors were similar in the updated respiratory failure index and the ACP guideline, but the index differs in several important ways:
- The index assigns less risk to low albumin, functional dependence, and congestive heart failure
- The index assigns greater risk to orofacial surgery
- The index identifies several new risk factors—high-complexity surgery, preoperative sepsis, ascites, and hypernatremia (serum sodium > 145 mmol/L).
STRATEGIES FOR RISK REDUCTION
Postoperative CPAP: Good option when exercise ability is limited
Among the postoperative lung expansion modalities, continuous positive airway pressure (CPAP) is particularly useful for patients who are unable to perform deep breathing or incentive spirometry exercises. A recent systematic literature review identified nine randomized controlled trials of CPAP vs standard therapy in a total of 654 patients undergoing abdominal surgery.13 Meta-analysis of these studies showed that CPAP was associated with significant reductions in the risk of overall postoperative pulmonary complications (odds ratio [OR] = 0.66; 95% CI, 0.52–0.85), atelectasis (OR = 0.75; 95% CI, 0.58–0.97), and pneumonia (OR = 0.33; 95% CI, 0.14–0.75) relative to standard therapy.
Use nasogastric tubes selectively
Nasogastric tubes can be used either routinely following abdominal surgery or only in select patients—eg, those who have symptomatic abdominal distention or nausea. The difference is important since nasogastric tubes may potentially increase the risk of aspiration and thus lead to a pulmonary complication. Nelson et al conducted a meta-analysis of 24 studies that compared routine nasogastric tube use in abdominal surgery with selective use based on symptoms or abdominal distention.14 They found that routine use was associated with a significant increase in postoperative pulmonary complications (OR = 1.45; 95% CI, 1.08–1.93) relative to selective use, without achieving any of its intended goals.
Laparoscopic vs open surgery: Evidence begins to follow intuition
Intuitively, it seems that laparoscopic procedures should reduce risk for postoperative pulmonary complications compared with open surgical procedures, as they are associated with less postoperative pain, which should facilitate deep breathing and improve postoperative lung volumes. Nevertheless, evidence for whether laparoscopic surgery reduces the risk of pulmonary complications has been mixed until recently.
In 2008, however, Weller and Rosati published an analysis of a nationally representative database of 19,156 patients who underwent bariatric surgery in 2005.15 After adjusting for comorbidities, they found that the rate of postoperative pulmonary complications was nearly double if patients underwent open surgery as opposed to laparoscopic surgery (OR = 1.92; 95% CI, 1.54–2.38). Open surgery was also associated with significantly higher rates of sepsis, cardiovascular events, and reoperation compared with laparoscopic procedures. This study suggests that choosing laparoscopic procedures is another strategy that may reduce pulmonary complication rates, at least in the setting of bariatric surgery.
Postoperative thoracic epidural analgesia
Question: Thoracic epidural analgesia reduces rates of which of the following?
A. Pneumonia following abdominal aortic aneurysm repair
B. Pulmonary complications following coronary bypass surgery
C. Respiratory failure following abdominal surgery
D. All of the above
The correct answer is D. Thoracic epidural analgesia is another important strategy for reducing postoperative pulmonary complications, as demonstrated by a 2007 systematic literature review by Liu and Wu.16 Their analysis showed that rates of pneumonia, respiratory failure, and pulmonary complications overall were reduced by approximately one-third to more than one-half with the use of postoperative thoracic epidural analgesia in patients undergoing aortic aneurysm repair, coronary bypass surgery, and abdominal surgery.
Smoking cessation: The jury is still out
Whether preoperative cigarette cessation reduces pulmonary complication rates has been controversial over the past decade. Early reports showed that among patients who smoke, those who quit shortly before surgery actually had higher complication rates than patients who continued to smoke. The most reasonable explanation seems to be that many patients who stop smoking report increased coughing and sputum production for the first month or two. Selection bias also may have played a role in these findings.
More recently, two randomized trials studied the impact of perioperative smoking intervention programs involving counseling and nicotine replacement.17,18 Unfortunately, both studies primarily studied patients undergoing low-risk procedures and were insufficiently powered to show a difference in pulmonary complication rates. The question of whether smoking cessation is an effective strategy to reduce postoperative pulmonary risk remains unanswered.
Preoperative intensive lung expansion: A promising new intervention
While the effectiveness of postoperative lung expansion techniques is undisputed,7 preoperative lung expansion—also known as inspiratory muscle training—has only recently been investigated. Hulzebos et al randomized 279 patients undergoing coronary artery bypass graft surgery who were at high risk for developing pulmonary complications to either usual care or inspiratory muscle training.19 The latter intervention involved 20 minutes per day of incentive spirometry, active breathing, and forced expiration techniques for at least 2 weeks prior to surgery. Rates of high-grade postoperative pulmonary complications were cut in half (OR = 0.52; 95% CI, 0.30–0.92) and rates of pneumonia were reduced by 60% (OR = 0.40; 95% CI, 0.19–0.84) in patients who received inspiratory muscle training relative to the usual-care group.
In clinical practice, preoperative inspiratory muscle training can be done in a chest physical therapy outpatient setting or a pulmonary rehabilitation clinic in the hospital.
SUMMARY
There have been a number of significant recent developments in the perioperative management of pulmonary complications:
- Obstructive sleep apnea has been confirmed as a risk factor, and pulmonary hypertension has emerged as a novel risk factor.
- An updated respiratory failure index has emerged as a useful research tool to identify high-risk patients and to ensure uniform risk stratification in future research.
- Evidence has mounted for the effectiveness of several risk-reduction strategies, including the use of laparoscopic procedures for bariatric surgery; selective use of nasogastric tubes; postoperative thoracic epidural analgesia; and intensive preoperative inspiratory muscle training.
DISCUSSION
Question from the audience: I do preoperative evaluations in an orthopedic ambulatory surgery center. Our surgeons often tell me, “Just order preoperative pulmonary function tests,” or, “Get a blood gas.” How should I respond?
Dr. Smetana: This is an area of some controversy, but in general, spirometry does not add much to a preoperative risk assessment that is based on a history and physical exam. Usually if the spirometry is abnormal, it will not be a surprise after careful clinical assessment. Arterial blood gases have no role in routine preoperative assessment.
Question from the audience: A chest x-ray is often requested preoperatively, but is it a necessary study?
Dr. Smetana: The data for preoperative chest x-rays are fairly poor and don’t allow us to assess whether they accurately predict complication rates. Most studies on chest x-rays have looked at how they affect preoperative management—eg, whether they change the anesthesia or even the surgery—and have shown that preoperative management changes in only about 1% to 2% of cases. So the chest x-ray is a fairly low-yield test in this setting.
One could argue that a preoperative chest x-ray might provide a baseline for postoperative comparison, but actually it is not usually helpful in this regard. Having a baseline does not make it easier to correctly diagnose pneumonia postoperatively, for example. Abnormal chest x-rays correlate with higher risk, but most patients with abnormal films would be suspected of being at higher risk anyway based on findings from the clinical assessment.
Question from the audience: Many primary care doctors in my hospital screen patients for pulmonary hypertension, but this raises the question of what to do with any information gained. What do you tell patients? Anesthesiologists?
Dr. Smetana: I don’t recommend preoperative screening for pulmonary hypertension unless there is some specific clinical reason to look for it. We don’t know if the perioperative risks that I described for patients with diagnosed or symptomatic pulmonary hypertension would also apply to patients with unrecognized, asymptomatic pulmonary hypertension that happened to be identified by screening.
Patients with pulmonary hypertension are at very high risk, especially for respiratory failure. But we don’t have any risk-reduction strategies specific to these patients, although I would recommend applying the general risk-reduction strategies that I discussed.
Question from the audience: I saw a man at my high-risk preoperative clinic who scored normally on a 6-minute walk test but then was found sound asleep when I was ready to see him a little while later. I suspected he had undiagnosed sleep apnea, and therefore had an increased risk of postoperative pulmonary complications, but what evidence would I have to delay his surgery to diagnose the sleep apnea and stabilize him on CPAP?
Dr. Smetana: For a patient with clinically suspected but undiagnosed sleep apnea, we have some evidence that the diagnosis should be pursued before surgery is performed.8 If the surgery were elective, it would be appropriate to have the patient evaluated and, if obstructive sleep apnea were diagnosed, treated in the customary way with CPAP. For patients who are hospitalized after surgery, CPAP can be continued as soon as possible in the hospital.
I would not have made this recommendation a few years ago, but now the evidence is more compelling. However, at this point I would not recommend routine preoperative screening of all patients for sleep apnea. Ongoing research is looking at this question.
Follow-up question: How long should surgery be delayed to optimize the patient on CPAP?
Dr. Smetana: Risk for postoperative respiratory failure is reduced very quickly after initiating CPAP therapy. A week would probably be sufficient, but there are no good data to specifically address that question.
Question from the audience: What about patients with asthma who are undergoing surgery—which ones benefit from stress-level steroids and preoperative nebulizer therapy?
Dr. Smetana: Surprisingly, asthma—if well controlled—is not a risk factor for postoperative pulmonary complications. Patients within 80% of their predicted or personal best peak flow appear to have a risk similar to that of patients without asthma. For patients with uncontrolled or poorly controlled asthma, the general rule is the same as for patients with COPD: treat them the same as if they weren’t having surgery. If a patient with asthma has a clinical indication for corticosteroids based on his or her condition, give corticosteroids whether or not surgery is planned. Corticosteroids are safe and do not raise the risk of postoperative wound complications. But we have no evidence to support routine use of steroids for all patients with asthma simply because elective surgery is planned.
Follow-up question: Do you optimize poorly controlled patients with oral prednisone for several days preoperatively, or do you use a stress protocol?
Dr. Smetana: For a patient whom you would normally treat with an outpatient course of prednisone, you should do just that. For a patient with an exacerbation severe enough to require admission for intravenous steroids and inhaled nebulizer therapy, then you should use that strategy. If the surgery is elective, it should be delayed until the patient is at his or her personal best.
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999; 100:1043–1049.
- Fleischmann KE, Goldman L, Young B, et al. Association between cardiac and noncardiac complications in patients undergoing noncardiac surgery: outcomes and effects on length of stay. Am J Med 2003; 115:515–520.
- Johnson RG, Arozullah AM, Neumayer L, et al. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: results from the Patient Safety in Surgery Study. J Am Coll Surg 2007; 204:1188–1198.
- Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199:531–537.
- Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med 2006; 144:575–580.
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:581–595.
- Lawrence VA, Cornell JE, Smetana GW; American College of Physicians. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:596–608.
- Hwang D, Shakir N, Limann B, et al. Association of sleep-disordered breathing with postoperative complications. Chest 2008; 133:1128–1134.
- Ramakrishna G, Sprung J, Ravi BS, et al. Impact of pulmonary hypertension on the outcomes of noncardiac surgery: predictors of perioperative morbidity and mortality. J Am Coll Cardiol 2005; 45:1691–1699.
- Lai HC, Lai HC, Wang KY, Lee WL, Ting CT, Liu TJ. Severe pulmonary hypertension complicates postoperative outcome of noncardiac surgery. Br J Anaesth 2007; 99:184–190.
- Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 2000; 232:242–253.
- Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847–857.
- Ferreyra GP, Baussano I, Squadrone V, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg 2008; 247:617–626.
- Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 2007; Jul 18 (3):CD004929.
- Weller WE, Rosati C. Comparing outcomes of laparoscopic versus open bariatric surgery. Ann Surg 2008; 248:10–15.
- Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesth Analg 2007; 104:689–702.
- Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002; 359:114–117.
- Lindström D, Sadr Azodi O, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 2008; 248:739–745.
- Hulzebos EH, Helders PJ, Favié NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 2006; 296:1851–1857.
Although pulmonary complications are not as well studied as cardiac complications in the postoperative setting, they are just as common following noncardiac surgery and are even more costly. It is worthwhile to identify surgical patients most at risk of postoperative pulmonary complications and take measures known to mitigate risk. This paper discusses important risk factors to identify during a preoperative pulmonary evaluation and then focuses on recent advances in strategies for reducing postoperative pulmonary complications. Teaching questions are included throughout, along with the rationale behind their answers.
POSTOPERATIVE PULMONARY COMPLICATIONS: WHAT ARE WE TRYING TO PREVENT AND WHY?
The definition of postoperative pulmonary complications is more variable and less intuitive than that of cardiac complications. Cardiac complications—postoperative myocardial infarction, cardiac death, and pulmonary edema—are more consistently defined and measured in clinical trials. Studies of postoperative pulmonary complications often group together pneumonia, respiratory failure, atelectasis, bronchospasm, and exacerbation of chronic obstructive pulmonary disease (COPD), making it more difficult to individually evaluate risk factors for different outcomes.
There are several reasons why it is important to consider pulmonary risk when evaluating patients preoperatively:
Pulmonary complications are as common as cardiac complications following noncardiac surgery. For example, in a secondary analysis of the cohort of noncardiac surgical patients used to validate the Revised Cardiac Risk Index,1 Fleischmann et al found that the incidence of pulmonary complications (2.7%) was highly comparable to that of cardiac complications (2.5%).2
Respiratory failure is a marker of ill health and predicts further complications. Postoperative respiratory failure (often defined as the need for ventilation for more than 48 hours after surgery) is an extremely morbid event. Johnson et al compared the outcomes of patients with and without respiratory failure as a complication of surgery.3 Among patients with respiratory failure, 26% died within 30 days, 6% had a myocardial infarction, 35% developed pneumonia, 10% developed acute renal failure, and 3% developed a deep vein thrombosis or pulmonary embolism; in contrast, rates of each of these events were lower than 2% among patients without respiratory failure.
Pulmonary complications are expensive and require lengthy hospitalization. The National Surgical Quality Improvement Program (NSQIP) compared hospitalization costs and length of stay among patients with various postoperative complications.4 Among infectious, cardiovascular, venous thromboembolic, and pulmonary complications, pulmonary complications were by far the most costly and, along with venous thromboembolic complications, required the longest mean hospital stay.
For these reasons, identifying patients at risk for pulmonary complications and developing a strategy to reduce the risk is clearly worthwhile.
IDENTIFYING RISK FOR PULMONARY COMPLICATIONS
Question: Which of the following is the most important risk factor for postoperative pulmonary complications?
A. High-risk surgical site
B. General anesthesia
C. COPD
D. Obesity
The correct answer is A. Pulmonary complications differ from cardiac complications in an important way: procedure-related factors are more predictive of pulmonary complications than are patient-related factors. Even healthy patients undergoing high-risk surgery are at risk for pulmonary complications. As for the other answer choices, general anesthesia and COPD are risk factors but are not as important as surgical site, and obesity has not been shown to be a risk factor at all.
Take-home points from the 2006 ACP guideline
Patient-related risk factors. As noted in Table 1, the most important patient-related risk factors identified in the ACP guideline are increasing age and increasing American Society of Anesthesiologists (ASA) classification of comorbidity.
The effect of advanced age becomes particularly notable around age 60 years and escalates from there. This effect of age differs from that for cardiac complications, for which age drops out as a risk factor after adjustment for other diseases and risk factors. For pulmonary complications, in contrast, even older patients who are healthy are at increased risk.
The ASA classification is a general index of overall morbidity that ranges from class 1 (normal healthy patient) to class 5 (moribund patient who is not expected to survive without the operation).
Notably, COPD and smoking were only minor risk factors in the ACP analysis.
Procedure-related risk factors. Surgical site was found to be the most important of any of the patient- or procedure-related risk factors. The closer the incision is to the diaphragm, the greater the risk for pulmonary complications. Aortic, thoracic, and abdominal procedures carry the highest risk (Table 1), and among abdominal procedures, upper abdominal surgery (eg, cholecystectomy) is riskier than lower abdominal surgery (eg, gynecologic).
Other procedure-related risk factors identified were emergency surgery, surgery lasting more than 3 hours, use of general anesthesia, and multiple transfusions (Table 1).
Newly identified risk factors
Question: Which of the following has recently been identified as a risk factor for postoperative pulmonary complications?
A. Epidural anesthesia
B. Insulin-treated diabetes
C. Obstructive sleep apnea
D. Immobility
The correct answer is C. There is no evidence that epidural anesthesia or insulin-treated diabetes are risk factors. Immobility seems intuitively correct but has not emerged as a risk factor among high-quality studies in the literature.
Obstructive sleep apnea. The role of obstructive sleep apnea was unclear prior to publication of new data in the last couple of years. Hwang et al enrolled 172 patients who were soon to have elective surgery and had at least two of four clinical features of obstructive sleep apnea (snoring, daytime somnolence, witnessed apnea event, or crowded oropharynx).8 Patients underwent nocturnal oximetry before surgery and were divided into two groups based on number of desaturation episodes per hour. Patients with five or more desaturations had markedly higher rates of postoperative respiratory complications (8 complications among 98 patients) than did patients with fewer than five desaturations (1 complication among 74 patients). The presence of five or more desaturations was also associated with higher rates of cardiac, gastrointestinal, and bleeding complications. Though this was a small study, its results suggest a significant association between obstructive sleep apnea and pulmonary complications.
The issue of whether to screen patients for obstructive sleep apnea before major noncardiac surgery is still unresolved.
Pulmonary hypertension has also been identified as a risk factor in recent years with the publication of two studies that estimated its impact on morbidity and mortality after major noncardiac surgery.9,10 One of the studies, a retrospective database review, found a 28% incidence of respiratory failure among 145 surgical patients with pulmonary hypertension.9 In the other study, a prospective case-control trial, respiratory failure occurred in 21% of patients with pulmonary hypertension compared with only 3% of matched controls.10 In the case-control study, pulmonary hypertension was also associated with significantly elevated rates of heart failure and in-hospital death.
The results of these studies do not support preoperative screening for undiagnosed pulmonary hypertension, but they do underscore the need to recognize established pulmonary hypertension as an important risk factor for postoperative complications.
AN UPDATED INDEX FOR RESPIRATORY FAILURE
Several years ago, investigators from the Veterans Affairs Medical Centers developed a respiratory failure index using a design similar to those of well-established indices for cardiac risk.11 The same group also developed a separate risk index for pneumonia.12
This respiratory failure index was recently updated3 to reflect experience from private and academic hospitals, making the results more generally applicable. The researchers evaluated data from 180,000 patients undergoing major general or vascular surgery (defined according to the NSQIP) over a 3-year period. Respiratory failure was defined as requiring at least 48 hours of ventilation or unplanned reintubation.
Comparison and contrast with the ACP guideline
Question: How does the updated respiratory failure index differ most significantly from the 2006 ACP guideline?
A. New index places greater emphasis on ASA class
B. New index offers a simplified weighted point scheme
C. New index ranks low albumin as a less important risk factor
D. New index attributes low risk to cigarette use
The correct answer is C: low albumin is a minor risk factor in the respiratory failure index, whereas it was one of the single most important predictors in the ACP guideline. As for the other answer choices, the new index places about the same emphasis on ASA class and cigarette use as does the ACP guideline, and it does not offer a simplified approach, as it incorporates 28 different factors.
Overall, most risk factors were similar in the updated respiratory failure index and the ACP guideline, but the index differs in several important ways:
- The index assigns less risk to low albumin, functional dependence, and congestive heart failure
- The index assigns greater risk to orofacial surgery
- The index identifies several new risk factors—high-complexity surgery, preoperative sepsis, ascites, and hypernatremia (serum sodium > 145 mmol/L).
STRATEGIES FOR RISK REDUCTION
Postoperative CPAP: Good option when exercise ability is limited
Among the postoperative lung expansion modalities, continuous positive airway pressure (CPAP) is particularly useful for patients who are unable to perform deep breathing or incentive spirometry exercises. A recent systematic literature review identified nine randomized controlled trials of CPAP vs standard therapy in a total of 654 patients undergoing abdominal surgery.13 Meta-analysis of these studies showed that CPAP was associated with significant reductions in the risk of overall postoperative pulmonary complications (odds ratio [OR] = 0.66; 95% CI, 0.52–0.85), atelectasis (OR = 0.75; 95% CI, 0.58–0.97), and pneumonia (OR = 0.33; 95% CI, 0.14–0.75) relative to standard therapy.
Use nasogastric tubes selectively
Nasogastric tubes can be used either routinely following abdominal surgery or only in select patients—eg, those who have symptomatic abdominal distention or nausea. The difference is important since nasogastric tubes may potentially increase the risk of aspiration and thus lead to a pulmonary complication. Nelson et al conducted a meta-analysis of 24 studies that compared routine nasogastric tube use in abdominal surgery with selective use based on symptoms or abdominal distention.14 They found that routine use was associated with a significant increase in postoperative pulmonary complications (OR = 1.45; 95% CI, 1.08–1.93) relative to selective use, without achieving any of its intended goals.
Laparoscopic vs open surgery: Evidence begins to follow intuition
Intuitively, it seems that laparoscopic procedures should reduce risk for postoperative pulmonary complications compared with open surgical procedures, as they are associated with less postoperative pain, which should facilitate deep breathing and improve postoperative lung volumes. Nevertheless, evidence for whether laparoscopic surgery reduces the risk of pulmonary complications has been mixed until recently.
In 2008, however, Weller and Rosati published an analysis of a nationally representative database of 19,156 patients who underwent bariatric surgery in 2005.15 After adjusting for comorbidities, they found that the rate of postoperative pulmonary complications was nearly double if patients underwent open surgery as opposed to laparoscopic surgery (OR = 1.92; 95% CI, 1.54–2.38). Open surgery was also associated with significantly higher rates of sepsis, cardiovascular events, and reoperation compared with laparoscopic procedures. This study suggests that choosing laparoscopic procedures is another strategy that may reduce pulmonary complication rates, at least in the setting of bariatric surgery.
Postoperative thoracic epidural analgesia
Question: Thoracic epidural analgesia reduces rates of which of the following?
A. Pneumonia following abdominal aortic aneurysm repair
B. Pulmonary complications following coronary bypass surgery
C. Respiratory failure following abdominal surgery
D. All of the above
The correct answer is D. Thoracic epidural analgesia is another important strategy for reducing postoperative pulmonary complications, as demonstrated by a 2007 systematic literature review by Liu and Wu.16 Their analysis showed that rates of pneumonia, respiratory failure, and pulmonary complications overall were reduced by approximately one-third to more than one-half with the use of postoperative thoracic epidural analgesia in patients undergoing aortic aneurysm repair, coronary bypass surgery, and abdominal surgery.
Smoking cessation: The jury is still out
Whether preoperative cigarette cessation reduces pulmonary complication rates has been controversial over the past decade. Early reports showed that among patients who smoke, those who quit shortly before surgery actually had higher complication rates than patients who continued to smoke. The most reasonable explanation seems to be that many patients who stop smoking report increased coughing and sputum production for the first month or two. Selection bias also may have played a role in these findings.
More recently, two randomized trials studied the impact of perioperative smoking intervention programs involving counseling and nicotine replacement.17,18 Unfortunately, both studies primarily studied patients undergoing low-risk procedures and were insufficiently powered to show a difference in pulmonary complication rates. The question of whether smoking cessation is an effective strategy to reduce postoperative pulmonary risk remains unanswered.
Preoperative intensive lung expansion: A promising new intervention
While the effectiveness of postoperative lung expansion techniques is undisputed,7 preoperative lung expansion—also known as inspiratory muscle training—has only recently been investigated. Hulzebos et al randomized 279 patients undergoing coronary artery bypass graft surgery who were at high risk for developing pulmonary complications to either usual care or inspiratory muscle training.19 The latter intervention involved 20 minutes per day of incentive spirometry, active breathing, and forced expiration techniques for at least 2 weeks prior to surgery. Rates of high-grade postoperative pulmonary complications were cut in half (OR = 0.52; 95% CI, 0.30–0.92) and rates of pneumonia were reduced by 60% (OR = 0.40; 95% CI, 0.19–0.84) in patients who received inspiratory muscle training relative to the usual-care group.
In clinical practice, preoperative inspiratory muscle training can be done in a chest physical therapy outpatient setting or a pulmonary rehabilitation clinic in the hospital.
SUMMARY
There have been a number of significant recent developments in the perioperative management of pulmonary complications:
- Obstructive sleep apnea has been confirmed as a risk factor, and pulmonary hypertension has emerged as a novel risk factor.
- An updated respiratory failure index has emerged as a useful research tool to identify high-risk patients and to ensure uniform risk stratification in future research.
- Evidence has mounted for the effectiveness of several risk-reduction strategies, including the use of laparoscopic procedures for bariatric surgery; selective use of nasogastric tubes; postoperative thoracic epidural analgesia; and intensive preoperative inspiratory muscle training.
DISCUSSION
Question from the audience: I do preoperative evaluations in an orthopedic ambulatory surgery center. Our surgeons often tell me, “Just order preoperative pulmonary function tests,” or, “Get a blood gas.” How should I respond?
Dr. Smetana: This is an area of some controversy, but in general, spirometry does not add much to a preoperative risk assessment that is based on a history and physical exam. Usually if the spirometry is abnormal, it will not be a surprise after careful clinical assessment. Arterial blood gases have no role in routine preoperative assessment.
Question from the audience: A chest x-ray is often requested preoperatively, but is it a necessary study?
Dr. Smetana: The data for preoperative chest x-rays are fairly poor and don’t allow us to assess whether they accurately predict complication rates. Most studies on chest x-rays have looked at how they affect preoperative management—eg, whether they change the anesthesia or even the surgery—and have shown that preoperative management changes in only about 1% to 2% of cases. So the chest x-ray is a fairly low-yield test in this setting.
One could argue that a preoperative chest x-ray might provide a baseline for postoperative comparison, but actually it is not usually helpful in this regard. Having a baseline does not make it easier to correctly diagnose pneumonia postoperatively, for example. Abnormal chest x-rays correlate with higher risk, but most patients with abnormal films would be suspected of being at higher risk anyway based on findings from the clinical assessment.
Question from the audience: Many primary care doctors in my hospital screen patients for pulmonary hypertension, but this raises the question of what to do with any information gained. What do you tell patients? Anesthesiologists?
Dr. Smetana: I don’t recommend preoperative screening for pulmonary hypertension unless there is some specific clinical reason to look for it. We don’t know if the perioperative risks that I described for patients with diagnosed or symptomatic pulmonary hypertension would also apply to patients with unrecognized, asymptomatic pulmonary hypertension that happened to be identified by screening.
Patients with pulmonary hypertension are at very high risk, especially for respiratory failure. But we don’t have any risk-reduction strategies specific to these patients, although I would recommend applying the general risk-reduction strategies that I discussed.
Question from the audience: I saw a man at my high-risk preoperative clinic who scored normally on a 6-minute walk test but then was found sound asleep when I was ready to see him a little while later. I suspected he had undiagnosed sleep apnea, and therefore had an increased risk of postoperative pulmonary complications, but what evidence would I have to delay his surgery to diagnose the sleep apnea and stabilize him on CPAP?
Dr. Smetana: For a patient with clinically suspected but undiagnosed sleep apnea, we have some evidence that the diagnosis should be pursued before surgery is performed.8 If the surgery were elective, it would be appropriate to have the patient evaluated and, if obstructive sleep apnea were diagnosed, treated in the customary way with CPAP. For patients who are hospitalized after surgery, CPAP can be continued as soon as possible in the hospital.
I would not have made this recommendation a few years ago, but now the evidence is more compelling. However, at this point I would not recommend routine preoperative screening of all patients for sleep apnea. Ongoing research is looking at this question.
Follow-up question: How long should surgery be delayed to optimize the patient on CPAP?
Dr. Smetana: Risk for postoperative respiratory failure is reduced very quickly after initiating CPAP therapy. A week would probably be sufficient, but there are no good data to specifically address that question.
Question from the audience: What about patients with asthma who are undergoing surgery—which ones benefit from stress-level steroids and preoperative nebulizer therapy?
Dr. Smetana: Surprisingly, asthma—if well controlled—is not a risk factor for postoperative pulmonary complications. Patients within 80% of their predicted or personal best peak flow appear to have a risk similar to that of patients without asthma. For patients with uncontrolled or poorly controlled asthma, the general rule is the same as for patients with COPD: treat them the same as if they weren’t having surgery. If a patient with asthma has a clinical indication for corticosteroids based on his or her condition, give corticosteroids whether or not surgery is planned. Corticosteroids are safe and do not raise the risk of postoperative wound complications. But we have no evidence to support routine use of steroids for all patients with asthma simply because elective surgery is planned.
Follow-up question: Do you optimize poorly controlled patients with oral prednisone for several days preoperatively, or do you use a stress protocol?
Dr. Smetana: For a patient whom you would normally treat with an outpatient course of prednisone, you should do just that. For a patient with an exacerbation severe enough to require admission for intravenous steroids and inhaled nebulizer therapy, then you should use that strategy. If the surgery is elective, it should be delayed until the patient is at his or her personal best.
Although pulmonary complications are not as well studied as cardiac complications in the postoperative setting, they are just as common following noncardiac surgery and are even more costly. It is worthwhile to identify surgical patients most at risk of postoperative pulmonary complications and take measures known to mitigate risk. This paper discusses important risk factors to identify during a preoperative pulmonary evaluation and then focuses on recent advances in strategies for reducing postoperative pulmonary complications. Teaching questions are included throughout, along with the rationale behind their answers.
POSTOPERATIVE PULMONARY COMPLICATIONS: WHAT ARE WE TRYING TO PREVENT AND WHY?
The definition of postoperative pulmonary complications is more variable and less intuitive than that of cardiac complications. Cardiac complications—postoperative myocardial infarction, cardiac death, and pulmonary edema—are more consistently defined and measured in clinical trials. Studies of postoperative pulmonary complications often group together pneumonia, respiratory failure, atelectasis, bronchospasm, and exacerbation of chronic obstructive pulmonary disease (COPD), making it more difficult to individually evaluate risk factors for different outcomes.
There are several reasons why it is important to consider pulmonary risk when evaluating patients preoperatively:
Pulmonary complications are as common as cardiac complications following noncardiac surgery. For example, in a secondary analysis of the cohort of noncardiac surgical patients used to validate the Revised Cardiac Risk Index,1 Fleischmann et al found that the incidence of pulmonary complications (2.7%) was highly comparable to that of cardiac complications (2.5%).2
Respiratory failure is a marker of ill health and predicts further complications. Postoperative respiratory failure (often defined as the need for ventilation for more than 48 hours after surgery) is an extremely morbid event. Johnson et al compared the outcomes of patients with and without respiratory failure as a complication of surgery.3 Among patients with respiratory failure, 26% died within 30 days, 6% had a myocardial infarction, 35% developed pneumonia, 10% developed acute renal failure, and 3% developed a deep vein thrombosis or pulmonary embolism; in contrast, rates of each of these events were lower than 2% among patients without respiratory failure.
Pulmonary complications are expensive and require lengthy hospitalization. The National Surgical Quality Improvement Program (NSQIP) compared hospitalization costs and length of stay among patients with various postoperative complications.4 Among infectious, cardiovascular, venous thromboembolic, and pulmonary complications, pulmonary complications were by far the most costly and, along with venous thromboembolic complications, required the longest mean hospital stay.
For these reasons, identifying patients at risk for pulmonary complications and developing a strategy to reduce the risk is clearly worthwhile.
IDENTIFYING RISK FOR PULMONARY COMPLICATIONS
Question: Which of the following is the most important risk factor for postoperative pulmonary complications?
A. High-risk surgical site
B. General anesthesia
C. COPD
D. Obesity
The correct answer is A. Pulmonary complications differ from cardiac complications in an important way: procedure-related factors are more predictive of pulmonary complications than are patient-related factors. Even healthy patients undergoing high-risk surgery are at risk for pulmonary complications. As for the other answer choices, general anesthesia and COPD are risk factors but are not as important as surgical site, and obesity has not been shown to be a risk factor at all.
Take-home points from the 2006 ACP guideline
Patient-related risk factors. As noted in Table 1, the most important patient-related risk factors identified in the ACP guideline are increasing age and increasing American Society of Anesthesiologists (ASA) classification of comorbidity.
The effect of advanced age becomes particularly notable around age 60 years and escalates from there. This effect of age differs from that for cardiac complications, for which age drops out as a risk factor after adjustment for other diseases and risk factors. For pulmonary complications, in contrast, even older patients who are healthy are at increased risk.
The ASA classification is a general index of overall morbidity that ranges from class 1 (normal healthy patient) to class 5 (moribund patient who is not expected to survive without the operation).
Notably, COPD and smoking were only minor risk factors in the ACP analysis.
Procedure-related risk factors. Surgical site was found to be the most important of any of the patient- or procedure-related risk factors. The closer the incision is to the diaphragm, the greater the risk for pulmonary complications. Aortic, thoracic, and abdominal procedures carry the highest risk (Table 1), and among abdominal procedures, upper abdominal surgery (eg, cholecystectomy) is riskier than lower abdominal surgery (eg, gynecologic).
Other procedure-related risk factors identified were emergency surgery, surgery lasting more than 3 hours, use of general anesthesia, and multiple transfusions (Table 1).
Newly identified risk factors
Question: Which of the following has recently been identified as a risk factor for postoperative pulmonary complications?
A. Epidural anesthesia
B. Insulin-treated diabetes
C. Obstructive sleep apnea
D. Immobility
The correct answer is C. There is no evidence that epidural anesthesia or insulin-treated diabetes are risk factors. Immobility seems intuitively correct but has not emerged as a risk factor among high-quality studies in the literature.
Obstructive sleep apnea. The role of obstructive sleep apnea was unclear prior to publication of new data in the last couple of years. Hwang et al enrolled 172 patients who were soon to have elective surgery and had at least two of four clinical features of obstructive sleep apnea (snoring, daytime somnolence, witnessed apnea event, or crowded oropharynx).8 Patients underwent nocturnal oximetry before surgery and were divided into two groups based on number of desaturation episodes per hour. Patients with five or more desaturations had markedly higher rates of postoperative respiratory complications (8 complications among 98 patients) than did patients with fewer than five desaturations (1 complication among 74 patients). The presence of five or more desaturations was also associated with higher rates of cardiac, gastrointestinal, and bleeding complications. Though this was a small study, its results suggest a significant association between obstructive sleep apnea and pulmonary complications.
The issue of whether to screen patients for obstructive sleep apnea before major noncardiac surgery is still unresolved.
Pulmonary hypertension has also been identified as a risk factor in recent years with the publication of two studies that estimated its impact on morbidity and mortality after major noncardiac surgery.9,10 One of the studies, a retrospective database review, found a 28% incidence of respiratory failure among 145 surgical patients with pulmonary hypertension.9 In the other study, a prospective case-control trial, respiratory failure occurred in 21% of patients with pulmonary hypertension compared with only 3% of matched controls.10 In the case-control study, pulmonary hypertension was also associated with significantly elevated rates of heart failure and in-hospital death.
The results of these studies do not support preoperative screening for undiagnosed pulmonary hypertension, but they do underscore the need to recognize established pulmonary hypertension as an important risk factor for postoperative complications.
AN UPDATED INDEX FOR RESPIRATORY FAILURE
Several years ago, investigators from the Veterans Affairs Medical Centers developed a respiratory failure index using a design similar to those of well-established indices for cardiac risk.11 The same group also developed a separate risk index for pneumonia.12
This respiratory failure index was recently updated3 to reflect experience from private and academic hospitals, making the results more generally applicable. The researchers evaluated data from 180,000 patients undergoing major general or vascular surgery (defined according to the NSQIP) over a 3-year period. Respiratory failure was defined as requiring at least 48 hours of ventilation or unplanned reintubation.
Comparison and contrast with the ACP guideline
Question: How does the updated respiratory failure index differ most significantly from the 2006 ACP guideline?
A. New index places greater emphasis on ASA class
B. New index offers a simplified weighted point scheme
C. New index ranks low albumin as a less important risk factor
D. New index attributes low risk to cigarette use
The correct answer is C: low albumin is a minor risk factor in the respiratory failure index, whereas it was one of the single most important predictors in the ACP guideline. As for the other answer choices, the new index places about the same emphasis on ASA class and cigarette use as does the ACP guideline, and it does not offer a simplified approach, as it incorporates 28 different factors.
Overall, most risk factors were similar in the updated respiratory failure index and the ACP guideline, but the index differs in several important ways:
- The index assigns less risk to low albumin, functional dependence, and congestive heart failure
- The index assigns greater risk to orofacial surgery
- The index identifies several new risk factors—high-complexity surgery, preoperative sepsis, ascites, and hypernatremia (serum sodium > 145 mmol/L).
STRATEGIES FOR RISK REDUCTION
Postoperative CPAP: Good option when exercise ability is limited
Among the postoperative lung expansion modalities, continuous positive airway pressure (CPAP) is particularly useful for patients who are unable to perform deep breathing or incentive spirometry exercises. A recent systematic literature review identified nine randomized controlled trials of CPAP vs standard therapy in a total of 654 patients undergoing abdominal surgery.13 Meta-analysis of these studies showed that CPAP was associated with significant reductions in the risk of overall postoperative pulmonary complications (odds ratio [OR] = 0.66; 95% CI, 0.52–0.85), atelectasis (OR = 0.75; 95% CI, 0.58–0.97), and pneumonia (OR = 0.33; 95% CI, 0.14–0.75) relative to standard therapy.
Use nasogastric tubes selectively
Nasogastric tubes can be used either routinely following abdominal surgery or only in select patients—eg, those who have symptomatic abdominal distention or nausea. The difference is important since nasogastric tubes may potentially increase the risk of aspiration and thus lead to a pulmonary complication. Nelson et al conducted a meta-analysis of 24 studies that compared routine nasogastric tube use in abdominal surgery with selective use based on symptoms or abdominal distention.14 They found that routine use was associated with a significant increase in postoperative pulmonary complications (OR = 1.45; 95% CI, 1.08–1.93) relative to selective use, without achieving any of its intended goals.
Laparoscopic vs open surgery: Evidence begins to follow intuition
Intuitively, it seems that laparoscopic procedures should reduce risk for postoperative pulmonary complications compared with open surgical procedures, as they are associated with less postoperative pain, which should facilitate deep breathing and improve postoperative lung volumes. Nevertheless, evidence for whether laparoscopic surgery reduces the risk of pulmonary complications has been mixed until recently.
In 2008, however, Weller and Rosati published an analysis of a nationally representative database of 19,156 patients who underwent bariatric surgery in 2005.15 After adjusting for comorbidities, they found that the rate of postoperative pulmonary complications was nearly double if patients underwent open surgery as opposed to laparoscopic surgery (OR = 1.92; 95% CI, 1.54–2.38). Open surgery was also associated with significantly higher rates of sepsis, cardiovascular events, and reoperation compared with laparoscopic procedures. This study suggests that choosing laparoscopic procedures is another strategy that may reduce pulmonary complication rates, at least in the setting of bariatric surgery.
Postoperative thoracic epidural analgesia
Question: Thoracic epidural analgesia reduces rates of which of the following?
A. Pneumonia following abdominal aortic aneurysm repair
B. Pulmonary complications following coronary bypass surgery
C. Respiratory failure following abdominal surgery
D. All of the above
The correct answer is D. Thoracic epidural analgesia is another important strategy for reducing postoperative pulmonary complications, as demonstrated by a 2007 systematic literature review by Liu and Wu.16 Their analysis showed that rates of pneumonia, respiratory failure, and pulmonary complications overall were reduced by approximately one-third to more than one-half with the use of postoperative thoracic epidural analgesia in patients undergoing aortic aneurysm repair, coronary bypass surgery, and abdominal surgery.
Smoking cessation: The jury is still out
Whether preoperative cigarette cessation reduces pulmonary complication rates has been controversial over the past decade. Early reports showed that among patients who smoke, those who quit shortly before surgery actually had higher complication rates than patients who continued to smoke. The most reasonable explanation seems to be that many patients who stop smoking report increased coughing and sputum production for the first month or two. Selection bias also may have played a role in these findings.
More recently, two randomized trials studied the impact of perioperative smoking intervention programs involving counseling and nicotine replacement.17,18 Unfortunately, both studies primarily studied patients undergoing low-risk procedures and were insufficiently powered to show a difference in pulmonary complication rates. The question of whether smoking cessation is an effective strategy to reduce postoperative pulmonary risk remains unanswered.
Preoperative intensive lung expansion: A promising new intervention
While the effectiveness of postoperative lung expansion techniques is undisputed,7 preoperative lung expansion—also known as inspiratory muscle training—has only recently been investigated. Hulzebos et al randomized 279 patients undergoing coronary artery bypass graft surgery who were at high risk for developing pulmonary complications to either usual care or inspiratory muscle training.19 The latter intervention involved 20 minutes per day of incentive spirometry, active breathing, and forced expiration techniques for at least 2 weeks prior to surgery. Rates of high-grade postoperative pulmonary complications were cut in half (OR = 0.52; 95% CI, 0.30–0.92) and rates of pneumonia were reduced by 60% (OR = 0.40; 95% CI, 0.19–0.84) in patients who received inspiratory muscle training relative to the usual-care group.
In clinical practice, preoperative inspiratory muscle training can be done in a chest physical therapy outpatient setting or a pulmonary rehabilitation clinic in the hospital.
SUMMARY
There have been a number of significant recent developments in the perioperative management of pulmonary complications:
- Obstructive sleep apnea has been confirmed as a risk factor, and pulmonary hypertension has emerged as a novel risk factor.
- An updated respiratory failure index has emerged as a useful research tool to identify high-risk patients and to ensure uniform risk stratification in future research.
- Evidence has mounted for the effectiveness of several risk-reduction strategies, including the use of laparoscopic procedures for bariatric surgery; selective use of nasogastric tubes; postoperative thoracic epidural analgesia; and intensive preoperative inspiratory muscle training.
DISCUSSION
Question from the audience: I do preoperative evaluations in an orthopedic ambulatory surgery center. Our surgeons often tell me, “Just order preoperative pulmonary function tests,” or, “Get a blood gas.” How should I respond?
Dr. Smetana: This is an area of some controversy, but in general, spirometry does not add much to a preoperative risk assessment that is based on a history and physical exam. Usually if the spirometry is abnormal, it will not be a surprise after careful clinical assessment. Arterial blood gases have no role in routine preoperative assessment.
Question from the audience: A chest x-ray is often requested preoperatively, but is it a necessary study?
Dr. Smetana: The data for preoperative chest x-rays are fairly poor and don’t allow us to assess whether they accurately predict complication rates. Most studies on chest x-rays have looked at how they affect preoperative management—eg, whether they change the anesthesia or even the surgery—and have shown that preoperative management changes in only about 1% to 2% of cases. So the chest x-ray is a fairly low-yield test in this setting.
One could argue that a preoperative chest x-ray might provide a baseline for postoperative comparison, but actually it is not usually helpful in this regard. Having a baseline does not make it easier to correctly diagnose pneumonia postoperatively, for example. Abnormal chest x-rays correlate with higher risk, but most patients with abnormal films would be suspected of being at higher risk anyway based on findings from the clinical assessment.
Question from the audience: Many primary care doctors in my hospital screen patients for pulmonary hypertension, but this raises the question of what to do with any information gained. What do you tell patients? Anesthesiologists?
Dr. Smetana: I don’t recommend preoperative screening for pulmonary hypertension unless there is some specific clinical reason to look for it. We don’t know if the perioperative risks that I described for patients with diagnosed or symptomatic pulmonary hypertension would also apply to patients with unrecognized, asymptomatic pulmonary hypertension that happened to be identified by screening.
Patients with pulmonary hypertension are at very high risk, especially for respiratory failure. But we don’t have any risk-reduction strategies specific to these patients, although I would recommend applying the general risk-reduction strategies that I discussed.
Question from the audience: I saw a man at my high-risk preoperative clinic who scored normally on a 6-minute walk test but then was found sound asleep when I was ready to see him a little while later. I suspected he had undiagnosed sleep apnea, and therefore had an increased risk of postoperative pulmonary complications, but what evidence would I have to delay his surgery to diagnose the sleep apnea and stabilize him on CPAP?
Dr. Smetana: For a patient with clinically suspected but undiagnosed sleep apnea, we have some evidence that the diagnosis should be pursued before surgery is performed.8 If the surgery were elective, it would be appropriate to have the patient evaluated and, if obstructive sleep apnea were diagnosed, treated in the customary way with CPAP. For patients who are hospitalized after surgery, CPAP can be continued as soon as possible in the hospital.
I would not have made this recommendation a few years ago, but now the evidence is more compelling. However, at this point I would not recommend routine preoperative screening of all patients for sleep apnea. Ongoing research is looking at this question.
Follow-up question: How long should surgery be delayed to optimize the patient on CPAP?
Dr. Smetana: Risk for postoperative respiratory failure is reduced very quickly after initiating CPAP therapy. A week would probably be sufficient, but there are no good data to specifically address that question.
Question from the audience: What about patients with asthma who are undergoing surgery—which ones benefit from stress-level steroids and preoperative nebulizer therapy?
Dr. Smetana: Surprisingly, asthma—if well controlled—is not a risk factor for postoperative pulmonary complications. Patients within 80% of their predicted or personal best peak flow appear to have a risk similar to that of patients without asthma. For patients with uncontrolled or poorly controlled asthma, the general rule is the same as for patients with COPD: treat them the same as if they weren’t having surgery. If a patient with asthma has a clinical indication for corticosteroids based on his or her condition, give corticosteroids whether or not surgery is planned. Corticosteroids are safe and do not raise the risk of postoperative wound complications. But we have no evidence to support routine use of steroids for all patients with asthma simply because elective surgery is planned.
Follow-up question: Do you optimize poorly controlled patients with oral prednisone for several days preoperatively, or do you use a stress protocol?
Dr. Smetana: For a patient whom you would normally treat with an outpatient course of prednisone, you should do just that. For a patient with an exacerbation severe enough to require admission for intravenous steroids and inhaled nebulizer therapy, then you should use that strategy. If the surgery is elective, it should be delayed until the patient is at his or her personal best.
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999; 100:1043–1049.
- Fleischmann KE, Goldman L, Young B, et al. Association between cardiac and noncardiac complications in patients undergoing noncardiac surgery: outcomes and effects on length of stay. Am J Med 2003; 115:515–520.
- Johnson RG, Arozullah AM, Neumayer L, et al. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: results from the Patient Safety in Surgery Study. J Am Coll Surg 2007; 204:1188–1198.
- Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199:531–537.
- Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med 2006; 144:575–580.
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:581–595.
- Lawrence VA, Cornell JE, Smetana GW; American College of Physicians. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:596–608.
- Hwang D, Shakir N, Limann B, et al. Association of sleep-disordered breathing with postoperative complications. Chest 2008; 133:1128–1134.
- Ramakrishna G, Sprung J, Ravi BS, et al. Impact of pulmonary hypertension on the outcomes of noncardiac surgery: predictors of perioperative morbidity and mortality. J Am Coll Cardiol 2005; 45:1691–1699.
- Lai HC, Lai HC, Wang KY, Lee WL, Ting CT, Liu TJ. Severe pulmonary hypertension complicates postoperative outcome of noncardiac surgery. Br J Anaesth 2007; 99:184–190.
- Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 2000; 232:242–253.
- Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847–857.
- Ferreyra GP, Baussano I, Squadrone V, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg 2008; 247:617–626.
- Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 2007; Jul 18 (3):CD004929.
- Weller WE, Rosati C. Comparing outcomes of laparoscopic versus open bariatric surgery. Ann Surg 2008; 248:10–15.
- Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesth Analg 2007; 104:689–702.
- Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002; 359:114–117.
- Lindström D, Sadr Azodi O, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 2008; 248:739–745.
- Hulzebos EH, Helders PJ, Favié NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 2006; 296:1851–1857.
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999; 100:1043–1049.
- Fleischmann KE, Goldman L, Young B, et al. Association between cardiac and noncardiac complications in patients undergoing noncardiac surgery: outcomes and effects on length of stay. Am J Med 2003; 115:515–520.
- Johnson RG, Arozullah AM, Neumayer L, et al. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: results from the Patient Safety in Surgery Study. J Am Coll Surg 2007; 204:1188–1198.
- Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199:531–537.
- Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med 2006; 144:575–580.
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:581–595.
- Lawrence VA, Cornell JE, Smetana GW; American College of Physicians. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006; 144:596–608.
- Hwang D, Shakir N, Limann B, et al. Association of sleep-disordered breathing with postoperative complications. Chest 2008; 133:1128–1134.
- Ramakrishna G, Sprung J, Ravi BS, et al. Impact of pulmonary hypertension on the outcomes of noncardiac surgery: predictors of perioperative morbidity and mortality. J Am Coll Cardiol 2005; 45:1691–1699.
- Lai HC, Lai HC, Wang KY, Lee WL, Ting CT, Liu TJ. Severe pulmonary hypertension complicates postoperative outcome of noncardiac surgery. Br J Anaesth 2007; 99:184–190.
- Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 2000; 232:242–253.
- Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847–857.
- Ferreyra GP, Baussano I, Squadrone V, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg 2008; 247:617–626.
- Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 2007; Jul 18 (3):CD004929.
- Weller WE, Rosati C. Comparing outcomes of laparoscopic versus open bariatric surgery. Ann Surg 2008; 248:10–15.
- Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesth Analg 2007; 104:689–702.
- Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002; 359:114–117.
- Lindström D, Sadr Azodi O, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 2008; 248:739–745.
- Hulzebos EH, Helders PJ, Favié NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 2006; 296:1851–1857.
KEY POINTS
- Pulmonary complications are as common as cardiac complications following noncardiac surgery.
- Surgical site is the most important predictor of risk for postoperative pulmonary complications: aortic, thoracic, and upper abdominal surgeries are high-risk procedures, even in healthy patients.
- Obstructive sleep apnea and pulmonary hypertension have recently been identified as risk factors, but the limited available evidence does not support preoperative screening for these conditions in patients without symptoms.
- Postoperative continuous positive airway pressure therapy is effective for reducing pulmonary complications in patients who are unable to perform deep breathing or incentive spirometry exercises.
- The jury is out on whether smoking cessation shortly before surgery lowers risk for postoperative pulmonary complications.