User login
How and why it pays to genuinely praise a difficult patient
Transcend dread: 8 ways to transform your care of ‘difficult’ patients
In a psychiatric clinic, Dr. B treats Ms. D, a single 28-year-old, for depression. She has multiple pain and gastrointestinal complaints that have responded poorly to treatment, morbid obesity, chronic tiredness, irritability, and Cluster B personality traits. Ms. D is lonely, unemployed, and seems to be in perpetual crisis. She states “unless someone does something to make this better, I just might kill myself.” She blames Dr. B for failing to adequately treat her depression; he has tried many medications to no avail. In psychotherapy sessions, Ms. D complains instead of examining methods for improvement, and she does not complete psychotherapy homework. She is extremely passive in her approach to getting better.
Ms. D asks Dr. B fill out the necessary paperwork so she can qualify for disability. Dr. B informs her that he will not do so because he believes she is capable of employment and that receiving disability would make her less likely to improve. Ms. D and her parents file letters of complaint about Dr. B to the supervisor of the psychiatric clinic for lack of treatment efficacy and for not supporting her disability claim. Dr. B dreads seeing Ms. D on his appointment list, and realizes she repulses him.
Although “the difficult patient” is not a diagnosis or specific clinical entity, clinicians universally struggle with such patients and have an immediate sense of shared experience when describing the phenomenon. In primary care, O’Dowd1 aptly described this type of patient as the “heartsink” patient, meaning the practitioner often feels exasperation, defeat, or dislike when he or she sees the patient’s name on the schedule.
This article discusses the literature on this topic and provides strategies for dealing with difficult patients in psychiatric practice.
Patient characteristics
Most published reports of difficult patients involve descriptive case series or physician accounts, most often describing patients presenting in nonpsychiatric specialties, including family practice, emergency medicine, rheumatology, gastroenterology, plastic surgery, and dentistry, among others.2-7
In a survey of physicians in 4 primary care clinics, subjects rated 96 (15%) of 627 adult patients as “difficult.”8 Difficult patients were significantly more likely than others to have a mental disorder ( Table 1 ).8 They also had more functional impairment, higher health care utilization, and lower satisfaction with care.
A separate primary care clinic study found uncannily similar results—physicians rated 74 (15%) of 500 new walk-in patients as “difficult.”9 Compared with other patients, the difficult patients had:
- higher rates of psychiatric illness, somatization (>5 somatic complaints), and more severe symptoms
- poorer functional status, more unmet expectations, less satisfaction with care, and higher use of health services.
Fewer articles on difficult patients have been published in psychiatric literature, although some commonalities have emerged ( Box ).10-12 Often suffering from chronic conditions without well-defined treatment endpoints, difficult patients do worse clinically, have higher use of health services, and are less happy with their care than other patients.
Difficult patients challenge our competence as physicians and evoke personal distress. Physicians with less job satisfaction, less clinical experience, less training in counseling, and a poor attitude toward psychosocial problems are more likely to perceive a patient as difficult.13,14
Table 1
Common psychiatric disorders in difficult patients
| Multisomatoform disorder |
| Panic disorder |
| Dysthymia |
| Generalized anxiety disorder |
| Major depressive disorder |
| Alcohol abuse or dependence* |
| *Researchers categorized patients as having “probable” alcohol abuse or dependence but did not determine if they met DSM-IV-TR criteria for these disorders |
| Source: Reference 8 |
An Ovid Medline search of psychiatric literature for “difficult patients” found only 9 articles published from 1996 to 2008, and most were editorials or essays.10
Groves11 grouped difficult patients into 4 categories:
- dependent clingers
- entitled demanders
- manipulative help-rejecters
- self-destructive deniers.
For a description of the behaviors and personality traits associated with each of these 4 categories and strategies to address them, see “The nurse who worked the system,” Current Psychiatry, July 2009. Groves emphasized that a physician’s negative reactions evoked by such patients—once understood through introspection—may facilitate better understanding and psychological management in their care.
Hinshelwood12 wrote about the cognitive dissonance psychiatrists encounter when trying to balance the different responses evoked by patients with schizophrenia and severe personality disorders.
When confronted with a psychotic patient’s severely damaged reality testing, psychiatrists often depersonalize the patient in an effort to be “scientific.” Conversely, patients with severe personality disorders threaten the psychiatrist with their emotional instability. The psychiatrist loses the role of objective observer and instead becomes a “moral evaluator,” seeing the patient as “good” or “bad” instead of as a person in need of help.
Hinshelwood cautioned that patients such as this are difficult not because their treatment is complicated but because they challenge our identity as scientists and put us in personal difficulty.
Survival strategies for clinicians
Eight strategies can help improve your care of difficult patients ( Table 2 ).
Table 2
8 strategies for managing difficult patients
| 1. Acknowledge that the patient is difficult |
| 2. Develop empathy |
| 3. Seek out supervision/consultation |
| 4. Utilize a team approach |
| 5. Lower treatment goals |
| 6. Decompress the treatment timeline |
| 7. Use ‘plussing’ (positive comments and acknowledgements) |
| 8. Use imagery (visualize the patient as a character in an unfinished novel) |
2. Develop empathy. Empathy is identification with and understanding of why a person feels, thinks, and acts as he or she does. The best way to develop empathy for a difficult patient is to learn about him or her firsthand—directly from the patient, not from reading chart notes or from information passed among colleagues.
Learning about the patient firsthand means shifting from sign-and-symptom gathering to performing a genuine inquiry about how the person thinks or feels, including interests, loves, or background. Challenging clinical circumstances—such as seeing a patient in a busy emergency department or during a 15-minute medication check—can make this difficult. In some cases, however, the time needed to establish empathy can be surprisingly brief.
The more patients feel that the psychiatrist is “on their level,” the less likely they are to project internalized anguish or impulsively act on conflicted feelings.
3. Seek out supervision or consultation. You can gain new perspectives by taking a “step back” and looking at the case with a colleague. Seeking out consultation also allows you to decompress by “getting it off your chest.” Supervision often allows clinicians to develop:
- empathy toward a difficult patient
- increased energy and creativity in subsequent sessions.
If you cannot utilize a team to carry out treatment, this approach still may help you develop a treatment plan.
5. Lower treatment goals. The nature of difficult patients makes complete “cures” a rarity. A psychiatrist whose goal is to substantially help a patient may become chronically frustrated and feel inadequate in the face of a patient’s perpetual suffering. The clinician sometimes reacts by developing therapeutic nihilism and withdrawing energy from the case. The patient, of course, senses this and increases his or her general distress level, which intensifies the negative interaction.
By lowering goals—for example, aiming for stabilization rather than improvement—you can feel less like a failure and be more relaxed. A relaxed clinician is more tolerant and in a better position to help the patient. Other lowered goals might be to reduce harm from impulsive or dangerous behaviors instead of eliminating them or better coping with symptoms rather than symptom remission.
7. Use ‘plussing.’ Because we experience dread with difficult patients, clinicians often avoid, refrain from, or simply don’t see opportunities to use positive comments and acknowledgements (“plussing”) when they arise. Most patients (as well as clinicians) want to be liked, and small compliments—when genuinely and appropriately placed—sometimes can make a huge difference in patients’ willingness to cope or try new things.
This technique might allow you to see the humorous side of yourself as the hardworking, well-intentioned yet ineffectual psychiatrist. You don’t know how the story will unfold, but you can accept this as you would in any other unfinished novel.
CASE CONTINUED: A more effective approach
Dr. B realizes Ms. D is a difficult patient for him and takes the case into supervision. He is stunned when he is unable to answer several of his supervisor’s questions about Ms. D, including “What was her upbringing like?” and “What are her strengths or interests?” He realizes he knows little about Ms. D and becomes aware that he has focused most of their sessions on either fixing her immediate and never-ending crises or defending himself.
The supervisor points out that Dr. B’s lack of empathy for Ms. D keeps him from helping her—being anxious and defensive makes him less likely to be supportive or creative. Dr. B feels better after the supervision session. He experiences some catharsis and develops a plan to improve the situation.
Dr. B structures the next session to get to know Ms. D better. He mentally decompresses the treatment timeline and refocuses on the need to develop empathy instead of attempting to ameliorate symptoms. Dr. B begins by letting Ms. D know he wants to help her but doesn’t know much about her. She initially rejects his attempts at empathic communication, but with gentle persistence he learns about her upbringing and interests. Dr. B is able to genuinely compliment her on coping with previous traumas and begins to better understand her strengths. Over the next several weeks, Ms. D seems more able to accept supportive interventions and eventually begins a part-time job.
Related resources
- Colson DB. Difficult patients in extended psychiatric hospitalization: a research perspective on the patient, staff, and team. Psychiatry. 1990;53(4):369-382.
- Koekkoek B, van Meijel B, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57:795-802.
Dr. Battaglia reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. O’Dowd TC. Five years of heartsink patients in general practice. BMJ. 1988;297:528-530.
2. Smith HW. The difficult patient and doctor: origins and suggestions. Facial Plast Surg Clin North Am. 2008;16(2):177-178, vi.
3. Woods CD. The difficult patient: a psychodynamic perspective. J Calif Dent Assoc. 2007;35(3):186-191.
4. Müller-Lissner S. The difficult patient with constipation. Best Pract Res Clin Gastroenterol. 2007;21(3):473-484.
5. King K, Moss AH. The frequency and significance of the “difficult” patient: the nephrology community’s perceptions. Adv Chronic Kidney Dis. 2004;11(2):234-239.
6. Potter M, Gordon S, Hamer P. The difficult patient in private practice physiotherapy: a qualitative study. Aust J Physiother. 2003;49(1):53-61.
7. Fee C. Death of a difficult patient. Ann Emerg Med. 2001;37(3):354-355.
8. Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11(1):1-8.
9. Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159(10):1069-1075.
10. Ovid Medline [database online]. New York, NY: Ovid Technologies, Inc; 2009.
11. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
12. Hinshelwood RD. The difficult patient. The role of ‘scientific psychiatry’ in understanding patients with chronic schizophrenia or severe personality disorders. Br J Psychiatry. 1999;174:187-190.
13. Mathers N, Jones N, Hannay D. Heartsink patients: a study of their general practitioners. Br J Gen Pract. 1995;45(395):293-296.
14. Steinmetz D, Tabenkin H. The ‘difficult’ patient as perceived by family physicians. Fam Pract. 2001;18(5):495-500.
15. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
In a psychiatric clinic, Dr. B treats Ms. D, a single 28-year-old, for depression. She has multiple pain and gastrointestinal complaints that have responded poorly to treatment, morbid obesity, chronic tiredness, irritability, and Cluster B personality traits. Ms. D is lonely, unemployed, and seems to be in perpetual crisis. She states “unless someone does something to make this better, I just might kill myself.” She blames Dr. B for failing to adequately treat her depression; he has tried many medications to no avail. In psychotherapy sessions, Ms. D complains instead of examining methods for improvement, and she does not complete psychotherapy homework. She is extremely passive in her approach to getting better.
Ms. D asks Dr. B fill out the necessary paperwork so she can qualify for disability. Dr. B informs her that he will not do so because he believes she is capable of employment and that receiving disability would make her less likely to improve. Ms. D and her parents file letters of complaint about Dr. B to the supervisor of the psychiatric clinic for lack of treatment efficacy and for not supporting her disability claim. Dr. B dreads seeing Ms. D on his appointment list, and realizes she repulses him.
Although “the difficult patient” is not a diagnosis or specific clinical entity, clinicians universally struggle with such patients and have an immediate sense of shared experience when describing the phenomenon. In primary care, O’Dowd1 aptly described this type of patient as the “heartsink” patient, meaning the practitioner often feels exasperation, defeat, or dislike when he or she sees the patient’s name on the schedule.
This article discusses the literature on this topic and provides strategies for dealing with difficult patients in psychiatric practice.
Patient characteristics
Most published reports of difficult patients involve descriptive case series or physician accounts, most often describing patients presenting in nonpsychiatric specialties, including family practice, emergency medicine, rheumatology, gastroenterology, plastic surgery, and dentistry, among others.2-7
In a survey of physicians in 4 primary care clinics, subjects rated 96 (15%) of 627 adult patients as “difficult.”8 Difficult patients were significantly more likely than others to have a mental disorder ( Table 1 ).8 They also had more functional impairment, higher health care utilization, and lower satisfaction with care.
A separate primary care clinic study found uncannily similar results—physicians rated 74 (15%) of 500 new walk-in patients as “difficult.”9 Compared with other patients, the difficult patients had:
- higher rates of psychiatric illness, somatization (>5 somatic complaints), and more severe symptoms
- poorer functional status, more unmet expectations, less satisfaction with care, and higher use of health services.
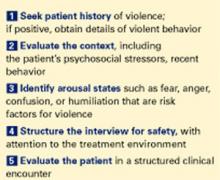
Fewer articles on difficult patients have been published in psychiatric literature, although some commonalities have emerged ( Box ).10-12 Often suffering from chronic conditions without well-defined treatment endpoints, difficult patients do worse clinically, have higher use of health services, and are less happy with their care than other patients.
Difficult patients challenge our competence as physicians and evoke personal distress. Physicians with less job satisfaction, less clinical experience, less training in counseling, and a poor attitude toward psychosocial problems are more likely to perceive a patient as difficult.13,14
Table 1
Common psychiatric disorders in difficult patients
| Multisomatoform disorder |
| Panic disorder |
| Dysthymia |
| Generalized anxiety disorder |
| Major depressive disorder |
| Alcohol abuse or dependence* |
| *Researchers categorized patients as having “probable” alcohol abuse or dependence but did not determine if they met DSM-IV-TR criteria for these disorders |
| Source: Reference 8 |
An Ovid Medline search of psychiatric literature for “difficult patients” found only 9 articles published from 1996 to 2008, and most were editorials or essays.10
Groves11 grouped difficult patients into 4 categories:
- dependent clingers
- entitled demanders
- manipulative help-rejecters
- self-destructive deniers.
For a description of the behaviors and personality traits associated with each of these 4 categories and strategies to address them, see “The nurse who worked the system,” Current Psychiatry, July 2009. Groves emphasized that a physician’s negative reactions evoked by such patients—once understood through introspection—may facilitate better understanding and psychological management in their care.
Hinshelwood12 wrote about the cognitive dissonance psychiatrists encounter when trying to balance the different responses evoked by patients with schizophrenia and severe personality disorders.
When confronted with a psychotic patient’s severely damaged reality testing, psychiatrists often depersonalize the patient in an effort to be “scientific.” Conversely, patients with severe personality disorders threaten the psychiatrist with their emotional instability. The psychiatrist loses the role of objective observer and instead becomes a “moral evaluator,” seeing the patient as “good” or “bad” instead of as a person in need of help.
Hinshelwood cautioned that patients such as this are difficult not because their treatment is complicated but because they challenge our identity as scientists and put us in personal difficulty.
Survival strategies for clinicians
Eight strategies can help improve your care of difficult patients ( Table 2 ).
Table 2
8 strategies for managing difficult patients
| 1. Acknowledge that the patient is difficult |
| 2. Develop empathy |
| 3. Seek out supervision/consultation |
| 4. Utilize a team approach |
| 5. Lower treatment goals |
| 6. Decompress the treatment timeline |
| 7. Use ‘plussing’ (positive comments and acknowledgements) |
| 8. Use imagery (visualize the patient as a character in an unfinished novel) |
2. Develop empathy. Empathy is identification with and understanding of why a person feels, thinks, and acts as he or she does. The best way to develop empathy for a difficult patient is to learn about him or her firsthand—directly from the patient, not from reading chart notes or from information passed among colleagues.
Learning about the patient firsthand means shifting from sign-and-symptom gathering to performing a genuine inquiry about how the person thinks or feels, including interests, loves, or background. Challenging clinical circumstances—such as seeing a patient in a busy emergency department or during a 15-minute medication check—can make this difficult. In some cases, however, the time needed to establish empathy can be surprisingly brief.
The more patients feel that the psychiatrist is “on their level,” the less likely they are to project internalized anguish or impulsively act on conflicted feelings.
3. Seek out supervision or consultation. You can gain new perspectives by taking a “step back” and looking at the case with a colleague. Seeking out consultation also allows you to decompress by “getting it off your chest.” Supervision often allows clinicians to develop:
- empathy toward a difficult patient
- increased energy and creativity in subsequent sessions.
If you cannot utilize a team to carry out treatment, this approach still may help you develop a treatment plan.
5. Lower treatment goals. The nature of difficult patients makes complete “cures” a rarity. A psychiatrist whose goal is to substantially help a patient may become chronically frustrated and feel inadequate in the face of a patient’s perpetual suffering. The clinician sometimes reacts by developing therapeutic nihilism and withdrawing energy from the case. The patient, of course, senses this and increases his or her general distress level, which intensifies the negative interaction.
By lowering goals—for example, aiming for stabilization rather than improvement—you can feel less like a failure and be more relaxed. A relaxed clinician is more tolerant and in a better position to help the patient. Other lowered goals might be to reduce harm from impulsive or dangerous behaviors instead of eliminating them or better coping with symptoms rather than symptom remission.
7. Use ‘plussing.’ Because we experience dread with difficult patients, clinicians often avoid, refrain from, or simply don’t see opportunities to use positive comments and acknowledgements (“plussing”) when they arise. Most patients (as well as clinicians) want to be liked, and small compliments—when genuinely and appropriately placed—sometimes can make a huge difference in patients’ willingness to cope or try new things.
This technique might allow you to see the humorous side of yourself as the hardworking, well-intentioned yet ineffectual psychiatrist. You don’t know how the story will unfold, but you can accept this as you would in any other unfinished novel.
CASE CONTINUED: A more effective approach
Dr. B realizes Ms. D is a difficult patient for him and takes the case into supervision. He is stunned when he is unable to answer several of his supervisor’s questions about Ms. D, including “What was her upbringing like?” and “What are her strengths or interests?” He realizes he knows little about Ms. D and becomes aware that he has focused most of their sessions on either fixing her immediate and never-ending crises or defending himself.
The supervisor points out that Dr. B’s lack of empathy for Ms. D keeps him from helping her—being anxious and defensive makes him less likely to be supportive or creative. Dr. B feels better after the supervision session. He experiences some catharsis and develops a plan to improve the situation.
Dr. B structures the next session to get to know Ms. D better. He mentally decompresses the treatment timeline and refocuses on the need to develop empathy instead of attempting to ameliorate symptoms. Dr. B begins by letting Ms. D know he wants to help her but doesn’t know much about her. She initially rejects his attempts at empathic communication, but with gentle persistence he learns about her upbringing and interests. Dr. B is able to genuinely compliment her on coping with previous traumas and begins to better understand her strengths. Over the next several weeks, Ms. D seems more able to accept supportive interventions and eventually begins a part-time job.
Related resources
- Colson DB. Difficult patients in extended psychiatric hospitalization: a research perspective on the patient, staff, and team. Psychiatry. 1990;53(4):369-382.
- Koekkoek B, van Meijel B, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57:795-802.
Dr. Battaglia reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
In a psychiatric clinic, Dr. B treats Ms. D, a single 28-year-old, for depression. She has multiple pain and gastrointestinal complaints that have responded poorly to treatment, morbid obesity, chronic tiredness, irritability, and Cluster B personality traits. Ms. D is lonely, unemployed, and seems to be in perpetual crisis. She states “unless someone does something to make this better, I just might kill myself.” She blames Dr. B for failing to adequately treat her depression; he has tried many medications to no avail. In psychotherapy sessions, Ms. D complains instead of examining methods for improvement, and she does not complete psychotherapy homework. She is extremely passive in her approach to getting better.
Ms. D asks Dr. B fill out the necessary paperwork so she can qualify for disability. Dr. B informs her that he will not do so because he believes she is capable of employment and that receiving disability would make her less likely to improve. Ms. D and her parents file letters of complaint about Dr. B to the supervisor of the psychiatric clinic for lack of treatment efficacy and for not supporting her disability claim. Dr. B dreads seeing Ms. D on his appointment list, and realizes she repulses him.
Although “the difficult patient” is not a diagnosis or specific clinical entity, clinicians universally struggle with such patients and have an immediate sense of shared experience when describing the phenomenon. In primary care, O’Dowd1 aptly described this type of patient as the “heartsink” patient, meaning the practitioner often feels exasperation, defeat, or dislike when he or she sees the patient’s name on the schedule.
This article discusses the literature on this topic and provides strategies for dealing with difficult patients in psychiatric practice.
Patient characteristics
Most published reports of difficult patients involve descriptive case series or physician accounts, most often describing patients presenting in nonpsychiatric specialties, including family practice, emergency medicine, rheumatology, gastroenterology, plastic surgery, and dentistry, among others.2-7
In a survey of physicians in 4 primary care clinics, subjects rated 96 (15%) of 627 adult patients as “difficult.”8 Difficult patients were significantly more likely than others to have a mental disorder ( Table 1 ).8 They also had more functional impairment, higher health care utilization, and lower satisfaction with care.
A separate primary care clinic study found uncannily similar results—physicians rated 74 (15%) of 500 new walk-in patients as “difficult.”9 Compared with other patients, the difficult patients had:
- higher rates of psychiatric illness, somatization (>5 somatic complaints), and more severe symptoms
- poorer functional status, more unmet expectations, less satisfaction with care, and higher use of health services.
Fewer articles on difficult patients have been published in psychiatric literature, although some commonalities have emerged ( Box ).10-12 Often suffering from chronic conditions without well-defined treatment endpoints, difficult patients do worse clinically, have higher use of health services, and are less happy with their care than other patients.
Difficult patients challenge our competence as physicians and evoke personal distress. Physicians with less job satisfaction, less clinical experience, less training in counseling, and a poor attitude toward psychosocial problems are more likely to perceive a patient as difficult.13,14
Table 1
Common psychiatric disorders in difficult patients
| Multisomatoform disorder |
| Panic disorder |
| Dysthymia |
| Generalized anxiety disorder |
| Major depressive disorder |
| Alcohol abuse or dependence* |
| *Researchers categorized patients as having “probable” alcohol abuse or dependence but did not determine if they met DSM-IV-TR criteria for these disorders |
| Source: Reference 8 |
An Ovid Medline search of psychiatric literature for “difficult patients” found only 9 articles published from 1996 to 2008, and most were editorials or essays.10
Groves11 grouped difficult patients into 4 categories:
- dependent clingers
- entitled demanders
- manipulative help-rejecters
- self-destructive deniers.
For a description of the behaviors and personality traits associated with each of these 4 categories and strategies to address them, see “The nurse who worked the system,” Current Psychiatry, July 2009. Groves emphasized that a physician’s negative reactions evoked by such patients—once understood through introspection—may facilitate better understanding and psychological management in their care.
Hinshelwood12 wrote about the cognitive dissonance psychiatrists encounter when trying to balance the different responses evoked by patients with schizophrenia and severe personality disorders.
When confronted with a psychotic patient’s severely damaged reality testing, psychiatrists often depersonalize the patient in an effort to be “scientific.” Conversely, patients with severe personality disorders threaten the psychiatrist with their emotional instability. The psychiatrist loses the role of objective observer and instead becomes a “moral evaluator,” seeing the patient as “good” or “bad” instead of as a person in need of help.
Hinshelwood cautioned that patients such as this are difficult not because their treatment is complicated but because they challenge our identity as scientists and put us in personal difficulty.
Survival strategies for clinicians
Eight strategies can help improve your care of difficult patients ( Table 2 ).
Table 2
8 strategies for managing difficult patients
| 1. Acknowledge that the patient is difficult |
| 2. Develop empathy |
| 3. Seek out supervision/consultation |
| 4. Utilize a team approach |
| 5. Lower treatment goals |
| 6. Decompress the treatment timeline |
| 7. Use ‘plussing’ (positive comments and acknowledgements) |
| 8. Use imagery (visualize the patient as a character in an unfinished novel) |
2. Develop empathy. Empathy is identification with and understanding of why a person feels, thinks, and acts as he or she does. The best way to develop empathy for a difficult patient is to learn about him or her firsthand—directly from the patient, not from reading chart notes or from information passed among colleagues.
Learning about the patient firsthand means shifting from sign-and-symptom gathering to performing a genuine inquiry about how the person thinks or feels, including interests, loves, or background. Challenging clinical circumstances—such as seeing a patient in a busy emergency department or during a 15-minute medication check—can make this difficult. In some cases, however, the time needed to establish empathy can be surprisingly brief.
The more patients feel that the psychiatrist is “on their level,” the less likely they are to project internalized anguish or impulsively act on conflicted feelings.
3. Seek out supervision or consultation. You can gain new perspectives by taking a “step back” and looking at the case with a colleague. Seeking out consultation also allows you to decompress by “getting it off your chest.” Supervision often allows clinicians to develop:
- empathy toward a difficult patient
- increased energy and creativity in subsequent sessions.
If you cannot utilize a team to carry out treatment, this approach still may help you develop a treatment plan.
5. Lower treatment goals. The nature of difficult patients makes complete “cures” a rarity. A psychiatrist whose goal is to substantially help a patient may become chronically frustrated and feel inadequate in the face of a patient’s perpetual suffering. The clinician sometimes reacts by developing therapeutic nihilism and withdrawing energy from the case. The patient, of course, senses this and increases his or her general distress level, which intensifies the negative interaction.
By lowering goals—for example, aiming for stabilization rather than improvement—you can feel less like a failure and be more relaxed. A relaxed clinician is more tolerant and in a better position to help the patient. Other lowered goals might be to reduce harm from impulsive or dangerous behaviors instead of eliminating them or better coping with symptoms rather than symptom remission.
7. Use ‘plussing.’ Because we experience dread with difficult patients, clinicians often avoid, refrain from, or simply don’t see opportunities to use positive comments and acknowledgements (“plussing”) when they arise. Most patients (as well as clinicians) want to be liked, and small compliments—when genuinely and appropriately placed—sometimes can make a huge difference in patients’ willingness to cope or try new things.
This technique might allow you to see the humorous side of yourself as the hardworking, well-intentioned yet ineffectual psychiatrist. You don’t know how the story will unfold, but you can accept this as you would in any other unfinished novel.
CASE CONTINUED: A more effective approach
Dr. B realizes Ms. D is a difficult patient for him and takes the case into supervision. He is stunned when he is unable to answer several of his supervisor’s questions about Ms. D, including “What was her upbringing like?” and “What are her strengths or interests?” He realizes he knows little about Ms. D and becomes aware that he has focused most of their sessions on either fixing her immediate and never-ending crises or defending himself.
The supervisor points out that Dr. B’s lack of empathy for Ms. D keeps him from helping her—being anxious and defensive makes him less likely to be supportive or creative. Dr. B feels better after the supervision session. He experiences some catharsis and develops a plan to improve the situation.
Dr. B structures the next session to get to know Ms. D better. He mentally decompresses the treatment timeline and refocuses on the need to develop empathy instead of attempting to ameliorate symptoms. Dr. B begins by letting Ms. D know he wants to help her but doesn’t know much about her. She initially rejects his attempts at empathic communication, but with gentle persistence he learns about her upbringing and interests. Dr. B is able to genuinely compliment her on coping with previous traumas and begins to better understand her strengths. Over the next several weeks, Ms. D seems more able to accept supportive interventions and eventually begins a part-time job.
Related resources
- Colson DB. Difficult patients in extended psychiatric hospitalization: a research perspective on the patient, staff, and team. Psychiatry. 1990;53(4):369-382.
- Koekkoek B, van Meijel B, Hutschemaekers G. “Difficult patients” in mental health care: a review. Psychiatr Serv. 2006;57:795-802.
Dr. Battaglia reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. O’Dowd TC. Five years of heartsink patients in general practice. BMJ. 1988;297:528-530.
2. Smith HW. The difficult patient and doctor: origins and suggestions. Facial Plast Surg Clin North Am. 2008;16(2):177-178, vi.
3. Woods CD. The difficult patient: a psychodynamic perspective. J Calif Dent Assoc. 2007;35(3):186-191.
4. Müller-Lissner S. The difficult patient with constipation. Best Pract Res Clin Gastroenterol. 2007;21(3):473-484.
5. King K, Moss AH. The frequency and significance of the “difficult” patient: the nephrology community’s perceptions. Adv Chronic Kidney Dis. 2004;11(2):234-239.
6. Potter M, Gordon S, Hamer P. The difficult patient in private practice physiotherapy: a qualitative study. Aust J Physiother. 2003;49(1):53-61.
7. Fee C. Death of a difficult patient. Ann Emerg Med. 2001;37(3):354-355.
8. Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11(1):1-8.
9. Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159(10):1069-1075.
10. Ovid Medline [database online]. New York, NY: Ovid Technologies, Inc; 2009.
11. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
12. Hinshelwood RD. The difficult patient. The role of ‘scientific psychiatry’ in understanding patients with chronic schizophrenia or severe personality disorders. Br J Psychiatry. 1999;174:187-190.
13. Mathers N, Jones N, Hannay D. Heartsink patients: a study of their general practitioners. Br J Gen Pract. 1995;45(395):293-296.
14. Steinmetz D, Tabenkin H. The ‘difficult’ patient as perceived by family physicians. Fam Pract. 2001;18(5):495-500.
15. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
1. O’Dowd TC. Five years of heartsink patients in general practice. BMJ. 1988;297:528-530.
2. Smith HW. The difficult patient and doctor: origins and suggestions. Facial Plast Surg Clin North Am. 2008;16(2):177-178, vi.
3. Woods CD. The difficult patient: a psychodynamic perspective. J Calif Dent Assoc. 2007;35(3):186-191.
4. Müller-Lissner S. The difficult patient with constipation. Best Pract Res Clin Gastroenterol. 2007;21(3):473-484.
5. King K, Moss AH. The frequency and significance of the “difficult” patient: the nephrology community’s perceptions. Adv Chronic Kidney Dis. 2004;11(2):234-239.
6. Potter M, Gordon S, Hamer P. The difficult patient in private practice physiotherapy: a qualitative study. Aust J Physiother. 2003;49(1):53-61.
7. Fee C. Death of a difficult patient. Ann Emerg Med. 2001;37(3):354-355.
8. Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11(1):1-8.
9. Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159(10):1069-1075.
10. Ovid Medline [database online]. New York, NY: Ovid Technologies, Inc; 2009.
11. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
12. Hinshelwood RD. The difficult patient. The role of ‘scientific psychiatry’ in understanding patients with chronic schizophrenia or severe personality disorders. Br J Psychiatry. 1999;174:187-190.
13. Mathers N, Jones N, Hannay D. Heartsink patients: a study of their general practitioners. Br J Gen Pract. 1995;45(395):293-296.
14. Steinmetz D, Tabenkin H. The ‘difficult’ patient as perceived by family physicians. Fam Pract. 2001;18(5):495-500.
15. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
5 keys to good results with supportive psychotherapy
Supportive psychotherapy began as a second-class treatment whose only operating principle was “being friendly” with the patient (Box).1 Critics called it “simple-minded”2 and sniffed, “if it is supportive, it is not therapy…if it is therapy, it is not supportive.”3
Since its lowly beginning, however, supportive psychotherapy has been proven highly effective, and clinicians have developed operating principles that distinguish it from expressive psychotherapy (Table 1).4
To help you make good use of supportive psychotherapy, this article describes its evolution and:
- evidence that demonstrates its effectiveness
- 5 key components for clinical practice
- how to use it when treating challenging patients.
Table 1
Differences between expressive and supportive psychotherapy
| Component | Expressive psychotherapy | Supportive psychotherapy |
|---|---|---|
| Treatment goal | Insight | Reduce Symptoms |
| Therapist style | Opaque | Conversational (“real”) |
| Transference | Examine | Nurture positive transference |
| Regression | Enhance | Minimize |
| Unconscious | Explore | Focus on conscious material |
| Defenses | Interpret | Reinforce mature defenses |
| Source: Reference 4 | ||
A proven treatment
Effective long-term therapy. Much research on supportive psychotherapy comes from studies in which supportive psychotherapy was included as a “treatment as usual” comparison. In an extensive longitudinal study, for example, the Meninger Psychotherapy Research Project examined 42 patients receiving psychoanalysis, psychodynamic psychotherapy, or supportive psychotherapy over 25 years.5
Despite the institutional expertise in psychoanalysis and expressive psychotherapy, patients in supportive psychotherapy did just as well as those receiving the other treatments. Researchers found that each therapy carried more supportive elements than was intended, and supportive elements accounted for many of the observed changes. They concluded that:
- thinking of change in terms of “structural” vs “behavioral” was not useful
- change did not occur in proportion to resolving unconscious conflict.
Early psychotherapy consisted of directive methods by which Charcot, Freud, and others “suggested” that patients rid themselves of symptoms while under hypnotic trance. Beneficial effects were sometimes immediate and dramatic but rarely lasted.
Dissatisfied with directive techniques, clinicians developed psychoanalytic principles and expressive psychotherapy, which emphasizes analyzing transference and uncovering unconscious thoughts, feelings, and motivations. Although expressive psychotherapy became popular, many patients—especially those with severe mental illness—were deemed unsuitable candidates or failed to improve.
These patients were relegated to supportive interventions, which initially were vaguely defined methods to reduce anxiety and provide encouragement. Therapists required little or no specialized training to provide supportive therapy and did not expect patients to make character (or structural) change. Surprisingly, many patients improved despite vague therapeutic guidelines.
Source: Reference 1
Therapists in the behavior therapy group used a manualized, highly structured treatment protocol that included in vivo desensitization and homework. Therapists who used supportive psychotherapy simply encouraged patients to ventilate their feelings and discuss problems. Supportive therapists were instructed to be nondirective and avoid confrontation unless the patient proposed it.
Improving personality disorders. Several studies examined a form of supportive psychotherapy that used a manualized, structured protocol for treating higher functioning patients who traditionally have been treated with expressive psychotherapy. The protocol used a conversation-based, dyadic style to improve self-esteem and adaptive skills through data-based praise, advice, education, appropriate reassurance, anticipatory guidance, clarification, and confrontation. Under these reproducible conditions, supportive psychotherapy showed good efficacy compared with dynamic therapies for patients with depressive, anxiety, and personality disorders.
A review of studies from 1986 to 1992 found that supportive psychotherapy was effective for a variety of psychiatric and medical conditions, including schizophrenia, bipolar disorder, depression, posttraumatic stress disorder, anxiety disorders, personality disorders, substance abuse, and stress associated with breast cancer and back pain.9
CASE STUDY: A negative experience
Mrs. S, a 32-year-old grant writer, is referred to a psychiatrist by an emergency department physician after she cut herself following an argument with her husband. She has chronic dysthymia, thoughts of harming herself, low self-esteem, and indecision about her marriage.
Mrs. S was not receiving mental health treatment because her first experience with a psychiatrist had a poor outcome: “He hardly ever said anything; in fact, sometimes I wondered if he was sleeping. I needed advice desperately, and I was hoping to get some help and direction for my life. Instead he answered every question with a question, and I ended up getting more confused. I felt guilty, like I wasn’t being a good patient because I couldn’t think for myself. I felt like he thought I was stupid. He gave me some antidepressants, but after a few months of feeling even worse I stopped going and vowed to never see a therapist again.”
5 key components
Although all psychotherapies have some elements of support, effective supportive psychotherapy has 5 key components (Table 2).
- asking directive questions
- allowing inflection in your voice
- making gestures
- discussing opinions.
Table 2
5 components of supportive psychotherapy
|
CASE CONTINUED: Learning to cope
Mrs. S’ new psychiatrist starts her on an antidepressant and once-weekly supportive psychotherapy. For the initial sessions, the psychiatrist helps Mrs. S explore options for her highly conflicted marriage and strategies for coping with panic symptoms.
Mrs. S develops a strong feeling of attachment to the psychiatrist, sometimes projecting anger onto him by declaring that he does not care enough. Instead of interpreting this transference, the psychiatrist uses it as an opportunity to explore coping options Mrs. S can try when she feels unloved or rejected.
Nurture positive transference. A positive relationship is essential for the therapeutic alliance. In most instances, a patient naturally develops good feelings toward the therapist over time as a result of repeated empathic interchange. In supportive psychotherapy, you may acknowledge these good feelings but do not interpret them for unconscious underpinnings.
Address transference only if it is negative. If the patient develops hostility or anger toward you, use techniques to improve the relationship, such as:
- acknowledging the validity of the patient’s angry feelings
- gaining an understanding of your role in the conflict and apologizing if sincere
- offering solutions to improve the conflict
- providing reassurance that working through the conflict will strengthen the therapeutic relationship.
Reduce anxiety. In supportive psychotherapy, the primary goal is to lessen the patient’s suffering. Although the patient often must talk about stressful or painful topics, you can help him or her do so in a tolerable manner. Focus on making it easier for the patient to talk.
Reducing anxiety means not only helping the patient talk about painful matters but also allowing him or her to avoid topics that are too uncomfortable to endure. You can always “earmark” areas of concern for later discussion. This modulation of anxiety is consistent with the object relations approach proposed by Kohut,10 in which emotional pain is addressed in “small, psychologically manageable portions.”
Enhance self-esteem. Virtually all patients in supportive psychotherapy suffer from low self-esteem, so it is beneficial to help them feel better about themselves. Take an active role by using positive comments and acknowledgements (“plussing”) as well as compliments when appropriate.
Most patients with low self-esteem have defects in the ability to nurture or forgive themselves (“self-soothe”). Work with patients to enhance this ability by:
- plussing where appropriate
- correcting negative self-distortions or self-reproach
- educating patients on how to both placate and reward themselves.
Strengthen coping mechanisms. In supportive psychotherapy the therapist acts as a coach, giving the patient suggestions on how to cope with difficult matters. As part of treatment, you might assign the patient homework and instruct him to practice specific coping strategies.
CASE CONTINUED: Feeling stronger
Eventually Mrs. S is able to talk in a limited fashion about childhood sexual abuse. With her psychiatrist’s encouragement, she begins to write about her feelings in a journal and exercising to help her “feel strong.” The psychiatrist often acknowledges her struggle and compliments her attempts at coping in healthy ways. After a year of supportive psychotherapy Mrs. S is better able to modulate her feelings and make decisions without feeling overwhelmed.
An option for challenging patients
Psychotic disorders. Although it may seem intuitive that psychotic conditions are a contraindication for psychotherapy, patients with schizophrenia and other psychotic disorders often benefit immensely from supportive psychotherapy. A supportive therapist’s guiding influence can help psychotic patients cope with fractured social and family life, struggles with independence, loneliness, frequent disturbances of reality, stigmatization from society, and difficulty with decision-making.
During a patient’s acute psychotic episodes, you can draw on the therapeutic relationship you have established, strongly advising the patient to accept treatment when he or she is paranoid and rejecting help. In such situations, you might say, “Joe, you know me. You know that in the past I have helped you get through some tough times. You are going to have to trust me that you need this medicine now, even if you don’t want to take it.”
Borderline personality disorder. Supportive psychotherapy’s emphasis on reducing anxiety and nurturing a therapeutic relationship makes it a good treatment for patients with borderline personality disorder. The focus on adaptive skills, self-esteem, and higher order defenses—such as repression, sublimation, rationalization, intellectualization, inhibition, displacement, and humor—is particularly suitable for self-injurious and suicidal patients.11
In addition, dialectical behavior therapy is congruent with supportive psychotherapy.12 I have found it useful to let patients know I am experienced and strong enough to undergo therapy with them and can live with the chaos of their lives. This often comforts patients with borderline personality disorder, as their internal state conveys a sense of destruction not only for them but anyone close to them. From a psychoanalytic perspective, conveying a sense of safety is a core healing component of supportive therapy.13
Substance abuse. A lack of treatment response and therapist burn-out are recurrent problems when treating patients with substance abuse.14 I have found it useful to “stretch” my treatment timeline—for example, by measuring change in years instead of months—so that I don’t continually feel unsuccessful. This allows me to focus not on the patient’s immediate sobriety but instead on the supportive relationship, especially on helping the patient address his or her sense of guilt and failure, which frequently underpins substance abuse.
Helping your patient to reframe his or her substance abuse as “bad choices” instead of the actions of a “bad person” is essential. Accompanying the patient to an Alcoholics Anonymous meeting—“I’ll go with you to the first one, after that it is up to you”—can be a powerful intervention with lasting benefits.
Related resources
- Werman DS. The practice of supportive psychotherapy. New York: Brunner/Mazel; 1984.
- Winston A, Rosenthal RN, Pinsker H. Introduction to supportive psychotherapy. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
- Pinsker H. A primer of supportive psychotherapy. Hillsdale, NJ. The Analytic Press; 1997.
- Imipramine • Tofranil
Dr. Battaglia is a consultant to Eli Lilly and Company.
1. Stewart RL. Psychoanalysis and psychoanalytic psychotherapy. In: Kaplan HI, Sadock BJ, eds. Comprehensive textbook of psychiatry/IV. Baltimore, MD: Williams & Wilkins; 1985:1331-65.
2. Sullivan PR. Learning theories and supportive psychotherapy. Am J Psychiatry 1971;128:763-6.
3. Crown S. Supportive psychotherapy: a contradiction in terms? Br J Psychiatry 1988;152:266-9.
4. Dewald P. Principles of supportive psychotherapy. Am J Psychother 1994;48(4):505-18.
5. Wallerstein RS. Psychoanalysis and psychotherapy: an historical perspective. Int J Psychoanal 1989;70:563-91.
6. Klein DF, Zitrin CM, Woerner MG, Ross DC. Treatment of phobias II. Behavior therapy and supportive psychotherapy: are there any specific ingredients? Arch Gen Psychiatry 1983;(40):139-45.
7. Hellerstein DJ, Rosenthal RN, Pinsker H, et al. A randomized prospective study comparing supportive and dynamic therapies. J Psychother Pract Res 1998;(7):261-71.
8. Rosenthal RN, Muran JC, Pinsker H, et al. Interpersonal change in brief supportive psychotherapy. J Psychother Pract Res 1999;(8):55-63.
9. Rockland LH. A review of supportive psychotherapy, 1986–1992. Hosp Community Psychiatry 1993;(44):1053-60.
10. Kohut H. The analysis of the self. New York: International Universities Press; 1971:229.
11. Aviram RB, Hellerstein DJ, Gerson J, Stanley B. Adapting supportive psychotherapy for individuals with borderline personality disorder who self-injure or attempt suicide. J Psychiatr Pract 2004;(10):145-55.
12. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: The Guilford Press; 1993.
13. Werman DS. On the mode of therapeutic action of psychoanalytic supportive psychotherapy. In: Rothstein A, ed. How does treatment help?: On the modes of therapeutic action of psychoanalytic psychotherapy. Madison, CT: International Universities Press; 1988:157–67.
14. Knudsen HK, Ducharme LJ, Roman PM. Counselor emotional exhaustion and turnover intention on therapeutic communities. J Subst Abuse Treat 2006;31(2):173-80.
Supportive psychotherapy began as a second-class treatment whose only operating principle was “being friendly” with the patient (Box).1 Critics called it “simple-minded”2 and sniffed, “if it is supportive, it is not therapy…if it is therapy, it is not supportive.”3
Since its lowly beginning, however, supportive psychotherapy has been proven highly effective, and clinicians have developed operating principles that distinguish it from expressive psychotherapy (Table 1).4
To help you make good use of supportive psychotherapy, this article describes its evolution and:
- evidence that demonstrates its effectiveness
- 5 key components for clinical practice
- how to use it when treating challenging patients.
Table 1
Differences between expressive and supportive psychotherapy
| Component | Expressive psychotherapy | Supportive psychotherapy |
|---|---|---|
| Treatment goal | Insight | Reduce Symptoms |
| Therapist style | Opaque | Conversational (“real”) |
| Transference | Examine | Nurture positive transference |
| Regression | Enhance | Minimize |
| Unconscious | Explore | Focus on conscious material |
| Defenses | Interpret | Reinforce mature defenses |
| Source: Reference 4 | ||
A proven treatment
Effective long-term therapy. Much research on supportive psychotherapy comes from studies in which supportive psychotherapy was included as a “treatment as usual” comparison. In an extensive longitudinal study, for example, the Meninger Psychotherapy Research Project examined 42 patients receiving psychoanalysis, psychodynamic psychotherapy, or supportive psychotherapy over 25 years.5
Despite the institutional expertise in psychoanalysis and expressive psychotherapy, patients in supportive psychotherapy did just as well as those receiving the other treatments. Researchers found that each therapy carried more supportive elements than was intended, and supportive elements accounted for many of the observed changes. They concluded that:
- thinking of change in terms of “structural” vs “behavioral” was not useful
- change did not occur in proportion to resolving unconscious conflict.
Early psychotherapy consisted of directive methods by which Charcot, Freud, and others “suggested” that patients rid themselves of symptoms while under hypnotic trance. Beneficial effects were sometimes immediate and dramatic but rarely lasted.
Dissatisfied with directive techniques, clinicians developed psychoanalytic principles and expressive psychotherapy, which emphasizes analyzing transference and uncovering unconscious thoughts, feelings, and motivations. Although expressive psychotherapy became popular, many patients—especially those with severe mental illness—were deemed unsuitable candidates or failed to improve.
These patients were relegated to supportive interventions, which initially were vaguely defined methods to reduce anxiety and provide encouragement. Therapists required little or no specialized training to provide supportive therapy and did not expect patients to make character (or structural) change. Surprisingly, many patients improved despite vague therapeutic guidelines.
Source: Reference 1
Therapists in the behavior therapy group used a manualized, highly structured treatment protocol that included in vivo desensitization and homework. Therapists who used supportive psychotherapy simply encouraged patients to ventilate their feelings and discuss problems. Supportive therapists were instructed to be nondirective and avoid confrontation unless the patient proposed it.
Improving personality disorders. Several studies examined a form of supportive psychotherapy that used a manualized, structured protocol for treating higher functioning patients who traditionally have been treated with expressive psychotherapy. The protocol used a conversation-based, dyadic style to improve self-esteem and adaptive skills through data-based praise, advice, education, appropriate reassurance, anticipatory guidance, clarification, and confrontation. Under these reproducible conditions, supportive psychotherapy showed good efficacy compared with dynamic therapies for patients with depressive, anxiety, and personality disorders.
A review of studies from 1986 to 1992 found that supportive psychotherapy was effective for a variety of psychiatric and medical conditions, including schizophrenia, bipolar disorder, depression, posttraumatic stress disorder, anxiety disorders, personality disorders, substance abuse, and stress associated with breast cancer and back pain.9
CASE STUDY: A negative experience
Mrs. S, a 32-year-old grant writer, is referred to a psychiatrist by an emergency department physician after she cut herself following an argument with her husband. She has chronic dysthymia, thoughts of harming herself, low self-esteem, and indecision about her marriage.
Mrs. S was not receiving mental health treatment because her first experience with a psychiatrist had a poor outcome: “He hardly ever said anything; in fact, sometimes I wondered if he was sleeping. I needed advice desperately, and I was hoping to get some help and direction for my life. Instead he answered every question with a question, and I ended up getting more confused. I felt guilty, like I wasn’t being a good patient because I couldn’t think for myself. I felt like he thought I was stupid. He gave me some antidepressants, but after a few months of feeling even worse I stopped going and vowed to never see a therapist again.”
5 key components
Although all psychotherapies have some elements of support, effective supportive psychotherapy has 5 key components (Table 2).
- asking directive questions
- allowing inflection in your voice
- making gestures
- discussing opinions.
Table 2
5 components of supportive psychotherapy
|
CASE CONTINUED: Learning to cope
Mrs. S’ new psychiatrist starts her on an antidepressant and once-weekly supportive psychotherapy. For the initial sessions, the psychiatrist helps Mrs. S explore options for her highly conflicted marriage and strategies for coping with panic symptoms.
Mrs. S develops a strong feeling of attachment to the psychiatrist, sometimes projecting anger onto him by declaring that he does not care enough. Instead of interpreting this transference, the psychiatrist uses it as an opportunity to explore coping options Mrs. S can try when she feels unloved or rejected.
Nurture positive transference. A positive relationship is essential for the therapeutic alliance. In most instances, a patient naturally develops good feelings toward the therapist over time as a result of repeated empathic interchange. In supportive psychotherapy, you may acknowledge these good feelings but do not interpret them for unconscious underpinnings.
Address transference only if it is negative. If the patient develops hostility or anger toward you, use techniques to improve the relationship, such as:
- acknowledging the validity of the patient’s angry feelings
- gaining an understanding of your role in the conflict and apologizing if sincere
- offering solutions to improve the conflict
- providing reassurance that working through the conflict will strengthen the therapeutic relationship.
Reduce anxiety. In supportive psychotherapy, the primary goal is to lessen the patient’s suffering. Although the patient often must talk about stressful or painful topics, you can help him or her do so in a tolerable manner. Focus on making it easier for the patient to talk.
Reducing anxiety means not only helping the patient talk about painful matters but also allowing him or her to avoid topics that are too uncomfortable to endure. You can always “earmark” areas of concern for later discussion. This modulation of anxiety is consistent with the object relations approach proposed by Kohut,10 in which emotional pain is addressed in “small, psychologically manageable portions.”
Enhance self-esteem. Virtually all patients in supportive psychotherapy suffer from low self-esteem, so it is beneficial to help them feel better about themselves. Take an active role by using positive comments and acknowledgements (“plussing”) as well as compliments when appropriate.
Most patients with low self-esteem have defects in the ability to nurture or forgive themselves (“self-soothe”). Work with patients to enhance this ability by:
- plussing where appropriate
- correcting negative self-distortions or self-reproach
- educating patients on how to both placate and reward themselves.
Strengthen coping mechanisms. In supportive psychotherapy the therapist acts as a coach, giving the patient suggestions on how to cope with difficult matters. As part of treatment, you might assign the patient homework and instruct him to practice specific coping strategies.
CASE CONTINUED: Feeling stronger
Eventually Mrs. S is able to talk in a limited fashion about childhood sexual abuse. With her psychiatrist’s encouragement, she begins to write about her feelings in a journal and exercising to help her “feel strong.” The psychiatrist often acknowledges her struggle and compliments her attempts at coping in healthy ways. After a year of supportive psychotherapy Mrs. S is better able to modulate her feelings and make decisions without feeling overwhelmed.
An option for challenging patients
Psychotic disorders. Although it may seem intuitive that psychotic conditions are a contraindication for psychotherapy, patients with schizophrenia and other psychotic disorders often benefit immensely from supportive psychotherapy. A supportive therapist’s guiding influence can help psychotic patients cope with fractured social and family life, struggles with independence, loneliness, frequent disturbances of reality, stigmatization from society, and difficulty with decision-making.
During a patient’s acute psychotic episodes, you can draw on the therapeutic relationship you have established, strongly advising the patient to accept treatment when he or she is paranoid and rejecting help. In such situations, you might say, “Joe, you know me. You know that in the past I have helped you get through some tough times. You are going to have to trust me that you need this medicine now, even if you don’t want to take it.”
Borderline personality disorder. Supportive psychotherapy’s emphasis on reducing anxiety and nurturing a therapeutic relationship makes it a good treatment for patients with borderline personality disorder. The focus on adaptive skills, self-esteem, and higher order defenses—such as repression, sublimation, rationalization, intellectualization, inhibition, displacement, and humor—is particularly suitable for self-injurious and suicidal patients.11
In addition, dialectical behavior therapy is congruent with supportive psychotherapy.12 I have found it useful to let patients know I am experienced and strong enough to undergo therapy with them and can live with the chaos of their lives. This often comforts patients with borderline personality disorder, as their internal state conveys a sense of destruction not only for them but anyone close to them. From a psychoanalytic perspective, conveying a sense of safety is a core healing component of supportive therapy.13
Substance abuse. A lack of treatment response and therapist burn-out are recurrent problems when treating patients with substance abuse.14 I have found it useful to “stretch” my treatment timeline—for example, by measuring change in years instead of months—so that I don’t continually feel unsuccessful. This allows me to focus not on the patient’s immediate sobriety but instead on the supportive relationship, especially on helping the patient address his or her sense of guilt and failure, which frequently underpins substance abuse.
Helping your patient to reframe his or her substance abuse as “bad choices” instead of the actions of a “bad person” is essential. Accompanying the patient to an Alcoholics Anonymous meeting—“I’ll go with you to the first one, after that it is up to you”—can be a powerful intervention with lasting benefits.
Related resources
- Werman DS. The practice of supportive psychotherapy. New York: Brunner/Mazel; 1984.
- Winston A, Rosenthal RN, Pinsker H. Introduction to supportive psychotherapy. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
- Pinsker H. A primer of supportive psychotherapy. Hillsdale, NJ. The Analytic Press; 1997.
- Imipramine • Tofranil
Dr. Battaglia is a consultant to Eli Lilly and Company.
Supportive psychotherapy began as a second-class treatment whose only operating principle was “being friendly” with the patient (Box).1 Critics called it “simple-minded”2 and sniffed, “if it is supportive, it is not therapy…if it is therapy, it is not supportive.”3
Since its lowly beginning, however, supportive psychotherapy has been proven highly effective, and clinicians have developed operating principles that distinguish it from expressive psychotherapy (Table 1).4
To help you make good use of supportive psychotherapy, this article describes its evolution and:
- evidence that demonstrates its effectiveness
- 5 key components for clinical practice
- how to use it when treating challenging patients.
Table 1
Differences between expressive and supportive psychotherapy
| Component | Expressive psychotherapy | Supportive psychotherapy |
|---|---|---|
| Treatment goal | Insight | Reduce Symptoms |
| Therapist style | Opaque | Conversational (“real”) |
| Transference | Examine | Nurture positive transference |
| Regression | Enhance | Minimize |
| Unconscious | Explore | Focus on conscious material |
| Defenses | Interpret | Reinforce mature defenses |
| Source: Reference 4 | ||
A proven treatment
Effective long-term therapy. Much research on supportive psychotherapy comes from studies in which supportive psychotherapy was included as a “treatment as usual” comparison. In an extensive longitudinal study, for example, the Meninger Psychotherapy Research Project examined 42 patients receiving psychoanalysis, psychodynamic psychotherapy, or supportive psychotherapy over 25 years.5
Despite the institutional expertise in psychoanalysis and expressive psychotherapy, patients in supportive psychotherapy did just as well as those receiving the other treatments. Researchers found that each therapy carried more supportive elements than was intended, and supportive elements accounted for many of the observed changes. They concluded that:
- thinking of change in terms of “structural” vs “behavioral” was not useful
- change did not occur in proportion to resolving unconscious conflict.
Early psychotherapy consisted of directive methods by which Charcot, Freud, and others “suggested” that patients rid themselves of symptoms while under hypnotic trance. Beneficial effects were sometimes immediate and dramatic but rarely lasted.
Dissatisfied with directive techniques, clinicians developed psychoanalytic principles and expressive psychotherapy, which emphasizes analyzing transference and uncovering unconscious thoughts, feelings, and motivations. Although expressive psychotherapy became popular, many patients—especially those with severe mental illness—were deemed unsuitable candidates or failed to improve.
These patients were relegated to supportive interventions, which initially were vaguely defined methods to reduce anxiety and provide encouragement. Therapists required little or no specialized training to provide supportive therapy and did not expect patients to make character (or structural) change. Surprisingly, many patients improved despite vague therapeutic guidelines.
Source: Reference 1
Therapists in the behavior therapy group used a manualized, highly structured treatment protocol that included in vivo desensitization and homework. Therapists who used supportive psychotherapy simply encouraged patients to ventilate their feelings and discuss problems. Supportive therapists were instructed to be nondirective and avoid confrontation unless the patient proposed it.
Improving personality disorders. Several studies examined a form of supportive psychotherapy that used a manualized, structured protocol for treating higher functioning patients who traditionally have been treated with expressive psychotherapy. The protocol used a conversation-based, dyadic style to improve self-esteem and adaptive skills through data-based praise, advice, education, appropriate reassurance, anticipatory guidance, clarification, and confrontation. Under these reproducible conditions, supportive psychotherapy showed good efficacy compared with dynamic therapies for patients with depressive, anxiety, and personality disorders.
A review of studies from 1986 to 1992 found that supportive psychotherapy was effective for a variety of psychiatric and medical conditions, including schizophrenia, bipolar disorder, depression, posttraumatic stress disorder, anxiety disorders, personality disorders, substance abuse, and stress associated with breast cancer and back pain.9
CASE STUDY: A negative experience
Mrs. S, a 32-year-old grant writer, is referred to a psychiatrist by an emergency department physician after she cut herself following an argument with her husband. She has chronic dysthymia, thoughts of harming herself, low self-esteem, and indecision about her marriage.
Mrs. S was not receiving mental health treatment because her first experience with a psychiatrist had a poor outcome: “He hardly ever said anything; in fact, sometimes I wondered if he was sleeping. I needed advice desperately, and I was hoping to get some help and direction for my life. Instead he answered every question with a question, and I ended up getting more confused. I felt guilty, like I wasn’t being a good patient because I couldn’t think for myself. I felt like he thought I was stupid. He gave me some antidepressants, but after a few months of feeling even worse I stopped going and vowed to never see a therapist again.”
5 key components
Although all psychotherapies have some elements of support, effective supportive psychotherapy has 5 key components (Table 2).
- asking directive questions
- allowing inflection in your voice
- making gestures
- discussing opinions.
Table 2
5 components of supportive psychotherapy
|
CASE CONTINUED: Learning to cope
Mrs. S’ new psychiatrist starts her on an antidepressant and once-weekly supportive psychotherapy. For the initial sessions, the psychiatrist helps Mrs. S explore options for her highly conflicted marriage and strategies for coping with panic symptoms.
Mrs. S develops a strong feeling of attachment to the psychiatrist, sometimes projecting anger onto him by declaring that he does not care enough. Instead of interpreting this transference, the psychiatrist uses it as an opportunity to explore coping options Mrs. S can try when she feels unloved or rejected.
Nurture positive transference. A positive relationship is essential for the therapeutic alliance. In most instances, a patient naturally develops good feelings toward the therapist over time as a result of repeated empathic interchange. In supportive psychotherapy, you may acknowledge these good feelings but do not interpret them for unconscious underpinnings.
Address transference only if it is negative. If the patient develops hostility or anger toward you, use techniques to improve the relationship, such as:
- acknowledging the validity of the patient’s angry feelings
- gaining an understanding of your role in the conflict and apologizing if sincere
- offering solutions to improve the conflict
- providing reassurance that working through the conflict will strengthen the therapeutic relationship.
Reduce anxiety. In supportive psychotherapy, the primary goal is to lessen the patient’s suffering. Although the patient often must talk about stressful or painful topics, you can help him or her do so in a tolerable manner. Focus on making it easier for the patient to talk.
Reducing anxiety means not only helping the patient talk about painful matters but also allowing him or her to avoid topics that are too uncomfortable to endure. You can always “earmark” areas of concern for later discussion. This modulation of anxiety is consistent with the object relations approach proposed by Kohut,10 in which emotional pain is addressed in “small, psychologically manageable portions.”
Enhance self-esteem. Virtually all patients in supportive psychotherapy suffer from low self-esteem, so it is beneficial to help them feel better about themselves. Take an active role by using positive comments and acknowledgements (“plussing”) as well as compliments when appropriate.
Most patients with low self-esteem have defects in the ability to nurture or forgive themselves (“self-soothe”). Work with patients to enhance this ability by:
- plussing where appropriate
- correcting negative self-distortions or self-reproach
- educating patients on how to both placate and reward themselves.
Strengthen coping mechanisms. In supportive psychotherapy the therapist acts as a coach, giving the patient suggestions on how to cope with difficult matters. As part of treatment, you might assign the patient homework and instruct him to practice specific coping strategies.
CASE CONTINUED: Feeling stronger
Eventually Mrs. S is able to talk in a limited fashion about childhood sexual abuse. With her psychiatrist’s encouragement, she begins to write about her feelings in a journal and exercising to help her “feel strong.” The psychiatrist often acknowledges her struggle and compliments her attempts at coping in healthy ways. After a year of supportive psychotherapy Mrs. S is better able to modulate her feelings and make decisions without feeling overwhelmed.
An option for challenging patients
Psychotic disorders. Although it may seem intuitive that psychotic conditions are a contraindication for psychotherapy, patients with schizophrenia and other psychotic disorders often benefit immensely from supportive psychotherapy. A supportive therapist’s guiding influence can help psychotic patients cope with fractured social and family life, struggles with independence, loneliness, frequent disturbances of reality, stigmatization from society, and difficulty with decision-making.
During a patient’s acute psychotic episodes, you can draw on the therapeutic relationship you have established, strongly advising the patient to accept treatment when he or she is paranoid and rejecting help. In such situations, you might say, “Joe, you know me. You know that in the past I have helped you get through some tough times. You are going to have to trust me that you need this medicine now, even if you don’t want to take it.”
Borderline personality disorder. Supportive psychotherapy’s emphasis on reducing anxiety and nurturing a therapeutic relationship makes it a good treatment for patients with borderline personality disorder. The focus on adaptive skills, self-esteem, and higher order defenses—such as repression, sublimation, rationalization, intellectualization, inhibition, displacement, and humor—is particularly suitable for self-injurious and suicidal patients.11
In addition, dialectical behavior therapy is congruent with supportive psychotherapy.12 I have found it useful to let patients know I am experienced and strong enough to undergo therapy with them and can live with the chaos of their lives. This often comforts patients with borderline personality disorder, as their internal state conveys a sense of destruction not only for them but anyone close to them. From a psychoanalytic perspective, conveying a sense of safety is a core healing component of supportive therapy.13
Substance abuse. A lack of treatment response and therapist burn-out are recurrent problems when treating patients with substance abuse.14 I have found it useful to “stretch” my treatment timeline—for example, by measuring change in years instead of months—so that I don’t continually feel unsuccessful. This allows me to focus not on the patient’s immediate sobriety but instead on the supportive relationship, especially on helping the patient address his or her sense of guilt and failure, which frequently underpins substance abuse.
Helping your patient to reframe his or her substance abuse as “bad choices” instead of the actions of a “bad person” is essential. Accompanying the patient to an Alcoholics Anonymous meeting—“I’ll go with you to the first one, after that it is up to you”—can be a powerful intervention with lasting benefits.
Related resources
- Werman DS. The practice of supportive psychotherapy. New York: Brunner/Mazel; 1984.
- Winston A, Rosenthal RN, Pinsker H. Introduction to supportive psychotherapy. Arlington, VA: American Psychiatric Publishing, Inc; 2004.
- Pinsker H. A primer of supportive psychotherapy. Hillsdale, NJ. The Analytic Press; 1997.
- Imipramine • Tofranil
Dr. Battaglia is a consultant to Eli Lilly and Company.
1. Stewart RL. Psychoanalysis and psychoanalytic psychotherapy. In: Kaplan HI, Sadock BJ, eds. Comprehensive textbook of psychiatry/IV. Baltimore, MD: Williams & Wilkins; 1985:1331-65.
2. Sullivan PR. Learning theories and supportive psychotherapy. Am J Psychiatry 1971;128:763-6.
3. Crown S. Supportive psychotherapy: a contradiction in terms? Br J Psychiatry 1988;152:266-9.
4. Dewald P. Principles of supportive psychotherapy. Am J Psychother 1994;48(4):505-18.
5. Wallerstein RS. Psychoanalysis and psychotherapy: an historical perspective. Int J Psychoanal 1989;70:563-91.
6. Klein DF, Zitrin CM, Woerner MG, Ross DC. Treatment of phobias II. Behavior therapy and supportive psychotherapy: are there any specific ingredients? Arch Gen Psychiatry 1983;(40):139-45.
7. Hellerstein DJ, Rosenthal RN, Pinsker H, et al. A randomized prospective study comparing supportive and dynamic therapies. J Psychother Pract Res 1998;(7):261-71.
8. Rosenthal RN, Muran JC, Pinsker H, et al. Interpersonal change in brief supportive psychotherapy. J Psychother Pract Res 1999;(8):55-63.
9. Rockland LH. A review of supportive psychotherapy, 1986–1992. Hosp Community Psychiatry 1993;(44):1053-60.
10. Kohut H. The analysis of the self. New York: International Universities Press; 1971:229.
11. Aviram RB, Hellerstein DJ, Gerson J, Stanley B. Adapting supportive psychotherapy for individuals with borderline personality disorder who self-injure or attempt suicide. J Psychiatr Pract 2004;(10):145-55.
12. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: The Guilford Press; 1993.
13. Werman DS. On the mode of therapeutic action of psychoanalytic supportive psychotherapy. In: Rothstein A, ed. How does treatment help?: On the modes of therapeutic action of psychoanalytic psychotherapy. Madison, CT: International Universities Press; 1988:157–67.
14. Knudsen HK, Ducharme LJ, Roman PM. Counselor emotional exhaustion and turnover intention on therapeutic communities. J Subst Abuse Treat 2006;31(2):173-80.
1. Stewart RL. Psychoanalysis and psychoanalytic psychotherapy. In: Kaplan HI, Sadock BJ, eds. Comprehensive textbook of psychiatry/IV. Baltimore, MD: Williams & Wilkins; 1985:1331-65.
2. Sullivan PR. Learning theories and supportive psychotherapy. Am J Psychiatry 1971;128:763-6.
3. Crown S. Supportive psychotherapy: a contradiction in terms? Br J Psychiatry 1988;152:266-9.
4. Dewald P. Principles of supportive psychotherapy. Am J Psychother 1994;48(4):505-18.
5. Wallerstein RS. Psychoanalysis and psychotherapy: an historical perspective. Int J Psychoanal 1989;70:563-91.
6. Klein DF, Zitrin CM, Woerner MG, Ross DC. Treatment of phobias II. Behavior therapy and supportive psychotherapy: are there any specific ingredients? Arch Gen Psychiatry 1983;(40):139-45.
7. Hellerstein DJ, Rosenthal RN, Pinsker H, et al. A randomized prospective study comparing supportive and dynamic therapies. J Psychother Pract Res 1998;(7):261-71.
8. Rosenthal RN, Muran JC, Pinsker H, et al. Interpersonal change in brief supportive psychotherapy. J Psychother Pract Res 1999;(8):55-63.
9. Rockland LH. A review of supportive psychotherapy, 1986–1992. Hosp Community Psychiatry 1993;(44):1053-60.
10. Kohut H. The analysis of the self. New York: International Universities Press; 1971:229.
11. Aviram RB, Hellerstein DJ, Gerson J, Stanley B. Adapting supportive psychotherapy for individuals with borderline personality disorder who self-injure or attempt suicide. J Psychiatr Pract 2004;(10):145-55.
12. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: The Guilford Press; 1993.
13. Werman DS. On the mode of therapeutic action of psychoanalytic supportive psychotherapy. In: Rothstein A, ed. How does treatment help?: On the modes of therapeutic action of psychoanalytic psychotherapy. Madison, CT: International Universities Press; 1988:157–67.
14. Knudsen HK, Ducharme LJ, Roman PM. Counselor emotional exhaustion and turnover intention on therapeutic communities. J Subst Abuse Treat 2006;31(2):173-80.
Is this patient dangerous?
Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Box) to quickly assess and respond to risk of violence in a psychiatric patient.
1 Seek patient history of violence; if positive, obtain details of violent behavior
2 Evaluate the context, including the patient’s psychosocial stressors, recent behavior
3 Identify arousal states such as fear, anger, confusion, or humiliation that are risk factors for violence
4 Structure the interview for safety, with attention to the treatment environment
5 Evaluate the patient in a structured clinical encounter
Step 1: Seek Patient History
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Table 1
Will this patient become violent?
Questions to consider before a clinical encounter
| Long-term behavior What violent acts has this patient committed? Were conditions similar with each episode? Any unprovoked acts? Was violence associated with alcohol or drug use? How has the patient behaved with health care providers in the hospital? In outpatient settings? |
| Immediate situation What are the patient’s immediate stressors? Did he or she arrive with family or in police custody? How did the patient behave while en route? |
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the Context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
Table 2
Risk factors for violence among psychiatric patients*
|
| *As identified in the literature |
Step 3: Identify Arousal States
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be businesslike with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Step 4: Structure the Interview for Safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face-to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: The Clinical Encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
For every violent act that requires staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org.
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv 2000;51: 1288-92.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S, ed. Manual of psychiatric emergencies. Boston: Little, Brown and Co.; 1988:23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.
Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Box) to quickly assess and respond to risk of violence in a psychiatric patient.
1 Seek patient history of violence; if positive, obtain details of violent behavior
2 Evaluate the context, including the patient’s psychosocial stressors, recent behavior
3 Identify arousal states such as fear, anger, confusion, or humiliation that are risk factors for violence
4 Structure the interview for safety, with attention to the treatment environment
5 Evaluate the patient in a structured clinical encounter
Step 1: Seek Patient History
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Table 1
Will this patient become violent?
Questions to consider before a clinical encounter
| Long-term behavior What violent acts has this patient committed? Were conditions similar with each episode? Any unprovoked acts? Was violence associated with alcohol or drug use? How has the patient behaved with health care providers in the hospital? In outpatient settings? |
| Immediate situation What are the patient’s immediate stressors? Did he or she arrive with family or in police custody? How did the patient behave while en route? |
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the Context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
Table 2
Risk factors for violence among psychiatric patients*
|
| *As identified in the literature |
Step 3: Identify Arousal States
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be businesslike with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Step 4: Structure the Interview for Safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face-to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: The Clinical Encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
For every violent act that requires staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org.
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv 2000;51: 1288-92.
Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Box) to quickly assess and respond to risk of violence in a psychiatric patient.
1 Seek patient history of violence; if positive, obtain details of violent behavior
2 Evaluate the context, including the patient’s psychosocial stressors, recent behavior
3 Identify arousal states such as fear, anger, confusion, or humiliation that are risk factors for violence
4 Structure the interview for safety, with attention to the treatment environment
5 Evaluate the patient in a structured clinical encounter
Step 1: Seek Patient History
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Table 1
Will this patient become violent?
Questions to consider before a clinical encounter
| Long-term behavior What violent acts has this patient committed? Were conditions similar with each episode? Any unprovoked acts? Was violence associated with alcohol or drug use? How has the patient behaved with health care providers in the hospital? In outpatient settings? |
| Immediate situation What are the patient’s immediate stressors? Did he or she arrive with family or in police custody? How did the patient behave while en route? |
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the Context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
Table 2
Risk factors for violence among psychiatric patients*
|
| *As identified in the literature |
Step 3: Identify Arousal States
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be businesslike with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Step 4: Structure the Interview for Safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face-to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: The Clinical Encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
For every violent act that requires staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org.
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv 2000;51: 1288-92.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S, ed. Manual of psychiatric emergencies. Boston: Little, Brown and Co.; 1988:23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S, ed. Manual of psychiatric emergencies. Boston: Little, Brown and Co.; 1988:23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.
Intramuscular olanzapine: Treating acute agitation in psychosis and bipolar mania
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
Is this patient dangerous? 5 steps to assess risk for violence
“Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Figure 1). to quickly assess and respond to risk of violence in a psychiatric patient.
Step 1: Seek patient history
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Figure 5 steps to assess and reduce the risk of patient violence
Past violence is the most powerful predictor of future violence, according to published studies. Higher frequency of aggressive episodes, greater degree of aggressive injury, and lack of apparent provocation in past episodes all increase the violence risk.3
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Demographic variables associated with higher violence rates include ages 15 to 24, nonwhite race, male gender, poverty, and low educational level. Other variables include history of abuse, victimization, family violence, limited employment skills, and “rootlessness,” such as poor family network and frequent moves or job changes.10
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
In other words, environmental stresses can be acute and destabilizing or part of the patient’s chronic life picture and serve in homeostatic functioning.
Step 3: Identify arousal states
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be business-like with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Table 1
Will this patient become violent? Questions to consider before a clinical encounter
Long-term behavior
|
Immediate situation
|
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Table 2
Risk factors for violence among psychiatric patients*
|
| * As identified in the literature. |
Step 4: Structure the interview for safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Cramped and overcrowded conditions on a psychiatric ward have been associated with higher rates of patient violence.2 In one case of context-specific violence, a veteran with known institutional transference issues toward the government attacked providers in a VA hospital on several occasions but did not exhibit this behavior in other, non-VA medical settings.
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face—to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: Tthe clinical encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
Visible, high numbers of confident-appearing—but not confrontational—staff or security may dissuade the patient from acting out. Then, most often, force will not be needed. If force is needed to control a violent patient, make sure the staff’s response is strong and overwhelming.
For every violent act requiring staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatric Services 2000;51:1288-92.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S (ed). Manual of psychiatric emergencies. Boston: Little, Brown and Co., 1988;23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.
“Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Figure 1). to quickly assess and respond to risk of violence in a psychiatric patient.
Step 1: Seek patient history
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Figure 5 steps to assess and reduce the risk of patient violence
Past violence is the most powerful predictor of future violence, according to published studies. Higher frequency of aggressive episodes, greater degree of aggressive injury, and lack of apparent provocation in past episodes all increase the violence risk.3
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Demographic variables associated with higher violence rates include ages 15 to 24, nonwhite race, male gender, poverty, and low educational level. Other variables include history of abuse, victimization, family violence, limited employment skills, and “rootlessness,” such as poor family network and frequent moves or job changes.10
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
In other words, environmental stresses can be acute and destabilizing or part of the patient’s chronic life picture and serve in homeostatic functioning.
Step 3: Identify arousal states
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be business-like with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Table 1
Will this patient become violent? Questions to consider before a clinical encounter
Long-term behavior
|
Immediate situation
|
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Table 2
Risk factors for violence among psychiatric patients*
|
| * As identified in the literature. |
Step 4: Structure the interview for safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Cramped and overcrowded conditions on a psychiatric ward have been associated with higher rates of patient violence.2 In one case of context-specific violence, a veteran with known institutional transference issues toward the government attacked providers in a VA hospital on several occasions but did not exhibit this behavior in other, non-VA medical settings.
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face—to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: Tthe clinical encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
Visible, high numbers of confident-appearing—but not confrontational—staff or security may dissuade the patient from acting out. Then, most often, force will not be needed. If force is needed to control a violent patient, make sure the staff’s response is strong and overwhelming.
For every violent act requiring staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatric Services 2000;51:1288-92.
“Will this patient turn violent?” Psychiatrists face this tough question every day. Although predicting a complex behavior such as violence is nearly impossible, we can prepare for dangerous behavior and improve our safety by:
- knowing the risk factors for patient violence
- assessing individuals for violence potential before clinical encounters
- controlling situations to reduce injury risk.
In one study, more than 50% of psychiatrists and 75% of mental health nurses reported an act or threat of violence from patients within the past year.1 To help you avoid becoming a statistic, this article provides a 5-step procedure (Figure 1). to quickly assess and respond to risk of violence in a psychiatric patient.
Step 1: Seek patient history
A careful review of past events and those immediately preceding the clinical encounter is the best tool for assessing potential for violence. The more you can learn from the patient chart and other sources before you see the patient, the better (Table 1). Valuable clues can be obtained from interviews with family members, outpatient providers, police officers, and others who have had pertinent social contact with the patient.
Figure 5 steps to assess and reduce the risk of patient violence
Past violence is the most powerful predictor of future violence, according to published studies. Higher frequency of aggressive episodes, greater degree of aggressive injury, and lack of apparent provocation in past episodes all increase the violence risk.3
A minority of patients account for most aggressive acts in clinical encounters. One study showed that recidivists committed 53% of all violent behaviors in a health care setting.4 A patient’s history of violence should be flagged in the chart and verbally passed on to staff to alert providers of increased risk.
However, not having a violent history does not guarantee that a patient will not become dangerous during a clinical encounter. All patients with a violent past had an initial violent episode, and that first time can occur in a practice setting.
Psychotic states by themselves appear to increase the risk of violence, although the literature is mixed.5,6 Clearly, however, psychotic states associated with arousal or agitation do predispose patients to violence, especially if the psychosis involves active paranoid delusions or hallucinations associated with negative affect (anger, sadness, anxiety).7
Increased rates of violence have also been reported in psychiatric patients with:
- acute manic states associated with arousal or agitation8
- nonspecific neurologic abnormalities such as abnormal EEGs, localizing neurologic signs, or “soft signs” (impaired face-hand test, graphesthesia, stereognosis).9
Demographic variables associated with higher violence rates include ages 15 to 24, nonwhite race, male gender, poverty, and low educational level. Other variables include history of abuse, victimization, family violence, limited employment skills, and “rootlessness,” such as poor family network and frequent moves or job changes.10
Psychiatric diagnoses associated with increased risk of violence include schizophrenia, bipolar mania, alcohol and other substance abuse, and personality disorders.11-13 In clinical practice, however, I find psychiatric diagnoses less useful in predicting violence than the patient’s arousal state and the other risk factors discussed above.
Step 2: Evaluate the context
In addition to evidence-supported risk factors (Table 2), context—or the broader situation in which a patient is embedded at the time of psychiatric evaluation—plays a prominent role in potentially violent situations. For example, if “divorce” is listed as a presenting factor:
- Is the patient recently divorced, or did it occur years ago?
- Does he hate all women or just his ex-wife?
- Was she having an affair, and did he just learn about this?
In other words, environmental stresses can be acute and destabilizing or part of the patient’s chronic life picture and serve in homeostatic functioning.
Step 3: Identify arousal states
Patients rarely commit violent acts when their anxiety and moods are well controlled. They are more likely to become aggressive in high arousal states.
Fear is probably an element of most situations where patients act out violently. Because the fearful patient may not exhibit easily interpreted danger signals, however, you may unwittingly provoke an assault by violating his or her personal space. A fearful, paranoid patient requires a greater-than-usual “intimate zone,” although this need for increased space may not be obvious.
Minimize provocation by explaining your actions and behaviors in advance (such as, “I would like to enter the room, sit down, and talk with you for about 20 minutes”). Be business-like with paranoid patients. Avoid exuding warmth, as they may view attempts at warmth as having sinister intent.
Clinicians are sometimes injured when trying to prevent a fearful, paranoid patient from fleeing. To avoid injury, don’t stand between the patient and the door. Let the patient escape from the immediate situation, and enlist security or police in further intervention attempts.
Anger is easy to recognize by signs of mounting tension. Loud voice, inappropriate staring, banging objects, clenched fists, agitated pacing, and verbal threats are common in the angry patient before a violent episode. Although this seems self-evident, it is surprising how many violent acts occur when these signs are obvious and noted by staff, yet no de-escalation measures are taken.
A patient’s verbal threats can actually help the clinician. This “red flag” alerts staff to focus on de-escalation techniques and prepare for a violent situation.
Confusion can be an underlying risk factor in patients with delirium or nonspecific organic brain syndrome. These patients may strike out unexpectedly when health care personnel are attempting to do routine procedures, and clinicians are sometimes caught off-guard when operating in a care-giving rather than defensive mode.
Table 1
Will this patient become violent? Questions to consider before a clinical encounter
Long-term behavior
|
Immediate situation
|
Clinicians can often avoid arousing confused patients by using orienting techniques and explaining their actions. For example, a nurse might say, “Hello Mr. X, I am a nurse and you are in this hospital for treatment of your illness. I will need to use this machine to check your blood pressure.”
Humiliation. Men in particular can react aggressively to loss of self-esteem and feelings of powerlessness. Take note if a man has been humiliated in front of family before being brought for evaluation; for example, was he removed by police in an emergency detention situation? This patient may need to act out violently to restore his sense of self.
Staff can lessen a patient’s potential to act on humiliation by using a therapeutic, esteem-building interview technique. For example, address the patient as “Mr.” instead of by first name, and highlight his strengths or accomplishments early in the interview.
Table 2
Risk factors for violence among psychiatric patients*
|
| * As identified in the literature. |
Step 4: Structure the interview for safety
The time you take before an interview to learn about a patient’s violence history, context, and arousal state is time well-spent and more patient-specific than past diagnoses. This information allows you to prepare for a safe intervention.
Interview environment. The physical and social environment where you interview the patient may contribute to violence potential.
- Is the patient being interviewed in a cramped room or an open hallway?
- Is the evaluation unit overcrowded?
- Are security personnel visible?
- Is the examiner of the same race or ethnic background as the patient?
Cramped and overcrowded conditions on a psychiatric ward have been associated with higher rates of patient violence.2 In one case of context-specific violence, a veteran with known institutional transference issues toward the government attacked providers in a VA hospital on several occasions but did not exhibit this behavior in other, non-VA medical settings.
Take control of the interview and treatment situation. Use the physical space and personnel as you would any other intervention tool—to increase safety and decrease potential for violent behavior. For example, some patients do better when interviewed in a small, private setting. Other interviews must be conducted in a triage area while police escorts hold the patient and handcuffs remain on.
Ideally, you and the patient should have equal access to the door if you conduct the psychiatric interview in an enclosed room. With high-risk patients, arrange your seating at a 90-degree angle—rather than face-to-face—to limit sustained, confrontational eye contact. Sit at greater than an arm swing or leg kick away from the patient, and require him or her to remain seated during the interview (or you will promptly leave).
In the outpatient practice, terminate the interview or evaluation session if a patient in a negative affective arousal state does not allow verbal redirection. Before you make any movement to exit, however, announce, “I am leaving the room now.”
Trust your intuition. I do not enter a closed, private space with a patient unless I feel safe. If I feel afraid, I take that as a valuable warning that further safety measures are necessary.
Use restraints as needed. When patients with a history of violence are brought to the hospital in high arousal states, I let them remain in restraint with security present during the initial interview. If the patient cannot have a back-and-forth conversation with me, I keep the security force present until I believe my verbal interactions have a substantial effect.
Patients must be responsive to talking interventions before restraint, security, or other environmental safety measures are removed. Some patients do not reach this point until after tranquilizing medications are given.
Step 5: Tthe clinical encounter
When discussing how to assess the likelihood of patient violence during a clinical encounter, a psychiatric colleague once commented, “Risk factors make you worry more; nothing makes you worry less.”
In other words, keep your guard up. Let clinical judgment take precedence over statistics when you are evaluating any patient. Statistics represent frequencies or averages; they may or may not apply to any one individual.
Techniques for assessing and treating violent patients are beyond the scope of this article, but at the very least:
- obtain training in safety/treatment protocols for violent patients
- ensure that your hospital/clinic has procedures in place to improve safety and to handle violent situations.
Visible, high numbers of confident-appearing—but not confrontational—staff or security may dissuade the patient from acting out. Then, most often, force will not be needed. If force is needed to control a violent patient, make sure the staff’s response is strong and overwhelming.
For every violent act requiring staff intervention, automatically schedule a debriefing session for those involved to assess the incident and allow them to express their feelings.
Related resources
- American Association for Emergency Psychiatry. www.emergencypsychiatry.org
- Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci 1999;11:307-14.
- McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatric Services 2000;51:1288-92.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S (ed). Manual of psychiatric emergencies. Boston: Little, Brown and Co., 1988;23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.
1. Nolan P, Dallender J, Soares J, et al. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs 1999;30:934-41.
2. Blomhoff S, Seim S, Friis S. Can prediction of violence among psychiatric inpatients be improved? Hosp Community Psychiatry 1990;41:771-5.
3. Convit A, Isay D, Otis D, et al. Characteristics of repeatedly assaultive psychiatric inpatients. Hosp Community Psychiatry 1990;41:1112-5.
4. Taylor P. Motives for offending among violent and psychotic men. Br J Psychiatry 1985;147:491-8.
5. Junginger J, Parks-Levy J, McGuire L. Delusions and symptom-consistent violence. Psychiatr Serv 1998;49:218-20.
6. Cheung P, Schweitzer I, Crowley K, et al. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res 1997;26:181-90.
7. Binder R, McNiel D. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
8. Convit A, Jaeger J, Pin Lin S, et al. Predicting assaultiveness in psychiatric inpatients: A pilot study. Hosp Community Psychiatry 1988;39:429-34.
9. Hyman S. The violent patient. In: Hyman S (ed). Manual of psychiatric emergencies. Boston: Little, Brown and Co., 1988;23-31.
10. Swartz M, Swanson J, Hiday V, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry 1998;155:226-31.
11. Owen C, Tarantello C, Jones M, et al. Repetitively violent patients in psychiatric units. Psychiatr Serv 1998;49:1458-61.
12. Citrome L, Volavka J. Clinical management of persistent aggressive behavior in schizophrenia, part I. Definitions, epidemiology, assessment and acute treatment. Essen Psychopharmacol 2002;5:1-16.
13. Abeyasinghe R, Jayasekera R. Violence in a general hospital psychiatry unit for men. Ceylon Med J 2003;48(2):45-7.