User login
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
In the Literature
Repeat Testing for C. Diff?
By Jeff Glasheen, MD
Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006 Apr;119(4):356.e7-356.e8
Clostridium difficile is a common complication of antibiotic and chemotherapeutic use, especially in hospitalized patients. Yet most nosocomial diarrhea is not caused by C. difficile. Most antibiotics can cause loose stools through changes in the gastrointestinal flora that result in inadequate digestion and absorption of carbohydrates and a resultant osmotic diarrhea. Further, antibiotics such as erythromycin and amoxicillin/clavulanate may result in diarrhea via increases in GI tract motility. While osmotic and motility causes of diarrhea tend to improve with antibiotic discontinuation, C. difficile-associated diarrhea is associated with significant morbidity that often continues until adequately treated.
Thus having a test that differentiates between C. difficile and non-clostridial diarrhea is essential. The most commonly used test is the enzyme immunoassay (EIA) that detects toxins A and B. The sensitivity and specificity of this test has been reported to range between 50%-90% and 70%-95%, respectively. The authors of this paper evaluated the utility of repeat EIA testing in patients with a one negative test in the setting of nosocomial diarrhea associated with antibiotic use.
The authors reviewed 474 sequential EIA tests for C. difficile in 396 patients over a 10-month period at a large university-affiliated community hospital with an EIA sensitivity and specificity of 80%-90% and 80%-95%, respectively. Tests were considered to be “repeat” if they occurred within seven days of the original negative test. Of the 78 repeat tests (16.5% of all tests), only one was positive, resulting in a 0.8% conversion rate. At an institutional cost of $128 per test the total cost of EIA testing over the 10-month period was $60,672. The cost of repeat testing alone was $9,984. The authors conclude that there is limited value—and high cost—in repeat EIA testing and that alternative sources of diarrhea should be sought or we should repeat EIA testing in patients with continued nosocomial diarrhea and a negative EIA test.
While prior studies have shown incremental benefit of retesting for C. difficile with the EIA assay, this study’s authors conclude that repeat “C. difficile testing is not clinically justified and is economically wasteful.” Unfortunately, the authors did not utilize a strong enough research design to defend this statement. From the data presented, all we can conclude is that repeat testing with an EIA assay did not add significant value to the diagnostic workup. The lack of a negative gold standard test, such as the cytotoxin assay or follow up outcomes, such as resolution of diarrhea, leaves the reader pondering if the repeat EIA assays were negative because the patients did not have C. difficile or because the test was not sensitive enough to detect the toxin. The reported sensitivity for the EIA assay used was 80-90%, meaning that 10%-20% of patients with C. difficile disease would have had a false negative test. While a second negative test would lower the likelihood of true disease, it would not lower it enough in a patient with a high pre-test probability of disease to sufficiently rule out the disease such that further testing is indicated.
Additionally, while we can extrapolate that the EIA test was of little utility to the patients studied here, no patient-specific data is presented. Thus it is difficult to determine if our patient population is represented in the study. More knowledge about the patients would allow the reader to use published prediction rules to better delineate how likely it was that this cohort was at high risk for having toxin-mediated diarrhea. Perhaps a more reasonable approach to this clinical conundrum would be to send the repeat stool test for a cytotoxin assay or to treat the patient empirically in situations where either the likelihood of disease or the disease burden is high.
Stroke after MI
By Ethan Cumbler, MD
Witt BJ, Ballman KV, Brown RD Jr, et al. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006 Apr;119(4):354.e1-9.
Stroke and myocardial infarction (MI) share many of the risk factors leading to atherosclerosis, including hypertension, hyperlipidemia, diabetes, tobacco abuse, and age. Logically, patients at risk for one event would also be at risk for the other, yet this interaction appears to be more complex. The study by Witt, et al., aims to elucidate the rate of in-hospital stroke in patients initially admitted with an MI.
The authors analyzed 22 observational studies of myocardial infarction that recorded the incidence of cerebrovascular accidents after acute MI. Clinical trials were excluded from the analysis in order to provide representation of an unselected population. Of the trials reviewed, 11 were included in the analysis of in-hospital strokes, three for the 30-day time point, and two for the one-year time point. The other trials used different time points and were not included in the analysis. The patients had a mean age ranging between 59 and 72.7 years, and all had a predominance of males. The rate of in-hospital stroke was 11.1 events per 1,000 hospitalizations. This incidence rose to 12.2/1,000 at 30 days and 21.4/1,000 at one year.
Plausible hypotheses for why the rate of cerebrovascular accident would be particularly high in the post-MI period include the potential for localized wall motion dysmotility or low flow leading to intracardiac thrombosis, event-related arrhythmia, or procedure-related embolic events. The studies from which this meta-analysis was derived were not designed in such a way for a causal relationship to be identified. However, age, diabetes, hypertension, prior stroke, anterior location of MI, atrial fibrillation, heart failure, and nonwhite race were all found to have an association with increased risk for stroke. Interestingly, angina on presentation was associated with an apparent decreased risk, theorized to potentially be due to ischemic preconditioning.
While this study shares the usual limitations of meta-analyses of observational studies, the authors have done an excellent summation of the data available including both English and non-English language articles in the analysis. Notably, the review included studies spanning more than 25 years and, thus, included data from studies done in the era prior to modern therapy for cardiac ischemia including potent antiplatelet and statin therapy. The three studies with in-hospital time points started in the 1990s had a lower average rate of stroke, which may reflect the effect of more potent anti-platelet agents used in today’s therapy for acute coronary syndromes.
The implication for the hospitalist is to recognize that patients admitted for MI are at high risk for stroke during the index hospitalization. A low threshold for suspicion of a cerebrovascular event needs to be maintained for post-MI patients with new neurologic symptoms. Future studies will be needed to address the risk/benefit of anticoagulation in high-risk patients for stroke following a myocardial infarction.
Predicting PE in the ED Using Revised Geneva Score
By Jeffrey Carter, MD
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006 Feb 7;144(3):165-171.
Introduction: Pulmonary embolism remains a common life-threatening disorder with imperfect diagnostic modalities and strategies. Much of the current literature focuses on the development and validation of clinical probability assessments that identify low-risk patients who can be safely managed without invasive testing or lung scanning.
Two common scoring systems include the Geneva and Wells criteria, which employ a combination of historical information, clinical and laboratory data to stratify patients into three risk groups.1,2 It has recently been shown that a single negative D-dimer test safely excludes patients with suspected VTE in a large cohort, with a three-month follow-up rate of VTE of 0%.3 Criticism of current clinical probability assessment strategies include the inclusion of subjective criteria or the need for blood gas values.1,2 In this paper, the authors sought to derive and validate a scoring system based on readily available objective clinical data.
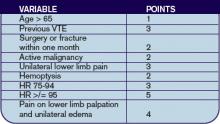
Methods: The cohort evaluated in this study consists of the same 965 patients used to prospectively evaluate an emergency department diagnostic strategy of VTE.3 Patients presenting to the emergency ward with complaints of chest pain or shortness of breath were evaluated with a standard diagnostic workup that included a checklist of demographic and historical information, signs and symptoms possibly consistent with VTE, ABG, chest X-ray, and EKG results, as well as the likelihood of another diagnosis. However, the goal was to create a scoring system based on readily available objective data, so ABG, chest X-ray and electrocardiogram results were not evaluated as possible components of the score. Clinical variables associated with pulmonary embolism were evaluated for statistical significance in both a univariate and multivariate model. These variables were then validated both internally and with an external cohort.
Results: The incidence of VTE was 23% (222/965). Ten clinical variables were found to be statistically significantly associated with VTE; these comprise the Revised Geneva Score.
Clinical probability is based on points: 0-3 is low probability; 4-10 is intermediate probability, and >10 is high probability. Low, intermediate, and high clinical probabilities had respective rates of VTE of 8%, 28%, and 74%. These percentages were found in the validation cohort and were similar to those in the derivation cohort.
Discussion: This study focuses on the derivation and validation of a clinical scoring system that can provide a numerical estimate of likelihood of VTE. The diagnostic strategy by which VTE is confirmed or excluded is from derivation cohort and is published elsewhere.3 In that study patients classified as no VTE and not treated had a 90-day risk of VTE of 1%. The nine-point revised Geneva score does indeed provide an accurate assessment of risk of VTE, and can thus help guide clinical decision-making. However it is not clear that the revised Geneva score will help decrease invasive diagnostic tests. In the low-risk group, 8% is too great a risk of a life-threatening illness to forego further diagnostic evaluation. Coupled with a negative ELISA D-dimer, exclusion of these patients is safe, but these patients cannot be safely excluded without risk stratification.3
References
- Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83:416-420.
- Wicki J, Perneger TV, Junof AF, et al. Assessing clinical probability of pulmonary embolism in the emergency ward: a simple score. Arch Intern Med. 2001 Jan 8;161(1):92-97.
- Perrier A, Roy PM, Aujesky D, et al. Diagnosing pulmonary embolism in outpatients with clinical assessment, D-dimer measurement, venous ultrasound and helical computed tomography: a multicenter management study. Am J Med. 2004 Mar 1;116(5):291-299.
LMWH for Inpatient Palliative Care
By Jeanie Youngwerth, MD
Noble SI, Nelson A, Turner C, et al. Acceptability of low molecular weight heparin thromboprophylaxis for patients receiving palliative care: qualitative study. BMJ. 2006 Mar 11:332(7541);577-580.ePub 2006 Feb 3.
Venous thromboembolism is a major risk factor for patients with malignancy. VTE may reduce survival time in patients receiving palliative care, with one in seven inpatients with cancer dying from pulmonary embolism. The American College of Chest Physicians recommend low molecular weight heparin (LMWH) in hospitalized patients with cancer as level 1A evidence in their 2004 consensus statement on VTE. There are no thromboprophylaxis guidelines in the United Kingdom. Many physicians view daily injections of LMWH as unnecessary distress for palliative care patients. This study focused on what inpatients with advanced cancer receiving palliative care thought about the effect of thromboprophylaxis on overall quality of life.
This was a qualitative study of 28 inpatients receiving palliative care who had advanced metastatic cancer and who were in a regional cancer center in Wales. The patients had received LMWH for at least five consecutive days. The patients were audiotaped and then had semi-structured interviews transcribed regarding cancer treatments they had received. These interviews covered the patients’ insight into prognosis, their understanding of thromboprophylaxis, their beliefs concerning the effects of thromboprophylaxis on overall quality of life, and the negative aspects of heparin treatment.
The main outcome measures were recurring themes of the effect of thromboprophylaxis on overall quality of life. Major themes identified were insight into prognosis, knowledge and understanding of thromboprophylaxis, acceptability of heparin thromboprophylaxis, reassurance, and optimism. Minor themes identified were bruising, negative impact of antiembolic stockings, and anger at paternalistic views toward terminally ill patients.
Most patients showed clear insight into the nature of their condition and understood heparin prophylaxis for VTE. Many patients identified immobility and surgery as VTE risk factors, with little understanding of cancer as a risk factor. All knew that VTE could cause death, but none were aware of the common symptoms. All patients found LMWH thromboprophylaxis acceptable. Patients believed taking measures to prevent symptoms might improve their quality of life and felt that the medical team had not given up on them.
The only negative experiences of LMWH thromboprophylaxis was bruising. All of the patients who wore antiembolic stockings during previous admissions found them uncomfortable. Patients expressed their need to be involved in decision-making, particularly with respect to withdrawal or non-administration of treatment.
This small, qualitative study showed that, contrary to many physicians’ beliefs, patients in palliative care units believe that LMWH injections are acceptable as thromboprophylaxis, but antiembolic stockings are not. The effect of daily injections had little or no effect on the quality of life, with many patients having positive feelings that things were being done to prevent new problems from occurring.
This study was limited by the small sample size, the qualitative nature that could introduce interpretation bias, and the fact that only patients using LMWH were included. Additionally, the United Kingdom has aggressively educated the public on the risks of VTE associated with long flights such that baseline knowledge may differ in other parts of the world. Resource utilization, including drug costs and length of stay, as well as effect on mortality were not studied.
The implications for hospitalists are that many inpatients with advanced cancer receiving palliative care may find LMWH thromboprophylaxis acceptable therapy, and that discussions with the patient regarding this option should be explored together.
Cost Analysis: Intensive Glycemic Control in Critically Ill Adults
By Whitney Woodmansee, MD
Krinsley JS, Jones, RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644-650.
Several studies have demonstrated improved outcomes and decreased mortality in ICU patients treated with intensive control of blood glucose levels. This study sought to identify the costs associated with intensive glycemic control in the ICU.
An ICU patient database was analyzed for cost data related to intensive glycemic control. A baseline group of 800 consecutive ICU patients admitted prior to initiation (baseline) of an intensive glucose management (blood glucose levels between 80-140 mg/dl protocol were compared with a treatment group of 800 consecutive patients admitted after initiation of the protocol). Previously reported outcomes of these patients demonstrated significant improvement in mortality with tight glycemic control. Costs related to ICU and non-ICU length of stay; duration of mechanical ventilation; and all laboratory, pharmacy, and radiology services were analyzed between groups. Resource utilization was determined by assessing charges from the database and adjusting for inflation and applying Medicare cost, charge ratios for each category, and fiscal year. Costs associated with the intensive glycemic control protocol were determined. Unfortunately, only cost estimates for insulin and associated disposable supplies for each group were available for analysis.
Baseline and treatment populations did not differ significantly regarding demographics such as age, gender, race, admitting diagnosis, diabetes prevalence, or APACHE II scores. There were fewer patients in the treatment group that required mechanical ventilation during their ICU stay (40.6% versus 33.6%). Intensive glucose management was associated with a 13.9% reduction in total ICU days and duration of mechanical ventilation (median of two days decreased to 1.7 days p=0.045). There was a $1,580 adjusted cost savings per patient in the intensive treatment group compared with the baseline group (p<0.001). This reduction in cost was primarily driven by a decrease in laboratory and radiology costs in the ventilated patients. There were nonsignificant cost reductions in the unventilated patients.
Intensive control of hyperglycemia in the hospitalized ICU patient appears to be associated with reduction of morbidity and mortality. This suggests that tight glycemic control also leads to reductions in overall patient care costs—particularly in the ventilated ICU patient. Although not a randomized control trial, database analysis of costs and resource utilization demonstrated an overall cost savings in the treatment group (after initiation of an intensive glycemic control protocol) compared with the baseline group (before protocol initiation). One caveat is that the authors used estimates when determining the costs associated with the implementation of the intensive glucose management protocol. Nevertheless, intensive glycemic control was associated with an overall reduction in patient costs related to decreased ICU days and mechanical ventilation as well as resource utilization in a patient population already shown to have improved mortality. These results, if confirmed, suggest that tight glycemic control in the ICU is cost effective and should become standard medical practice. TH
Repeat Testing for C. Diff?
By Jeff Glasheen, MD
Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006 Apr;119(4):356.e7-356.e8
Clostridium difficile is a common complication of antibiotic and chemotherapeutic use, especially in hospitalized patients. Yet most nosocomial diarrhea is not caused by C. difficile. Most antibiotics can cause loose stools through changes in the gastrointestinal flora that result in inadequate digestion and absorption of carbohydrates and a resultant osmotic diarrhea. Further, antibiotics such as erythromycin and amoxicillin/clavulanate may result in diarrhea via increases in GI tract motility. While osmotic and motility causes of diarrhea tend to improve with antibiotic discontinuation, C. difficile-associated diarrhea is associated with significant morbidity that often continues until adequately treated.
Thus having a test that differentiates between C. difficile and non-clostridial diarrhea is essential. The most commonly used test is the enzyme immunoassay (EIA) that detects toxins A and B. The sensitivity and specificity of this test has been reported to range between 50%-90% and 70%-95%, respectively. The authors of this paper evaluated the utility of repeat EIA testing in patients with a one negative test in the setting of nosocomial diarrhea associated with antibiotic use.
The authors reviewed 474 sequential EIA tests for C. difficile in 396 patients over a 10-month period at a large university-affiliated community hospital with an EIA sensitivity and specificity of 80%-90% and 80%-95%, respectively. Tests were considered to be “repeat” if they occurred within seven days of the original negative test. Of the 78 repeat tests (16.5% of all tests), only one was positive, resulting in a 0.8% conversion rate. At an institutional cost of $128 per test the total cost of EIA testing over the 10-month period was $60,672. The cost of repeat testing alone was $9,984. The authors conclude that there is limited value—and high cost—in repeat EIA testing and that alternative sources of diarrhea should be sought or we should repeat EIA testing in patients with continued nosocomial diarrhea and a negative EIA test.
While prior studies have shown incremental benefit of retesting for C. difficile with the EIA assay, this study’s authors conclude that repeat “C. difficile testing is not clinically justified and is economically wasteful.” Unfortunately, the authors did not utilize a strong enough research design to defend this statement. From the data presented, all we can conclude is that repeat testing with an EIA assay did not add significant value to the diagnostic workup. The lack of a negative gold standard test, such as the cytotoxin assay or follow up outcomes, such as resolution of diarrhea, leaves the reader pondering if the repeat EIA assays were negative because the patients did not have C. difficile or because the test was not sensitive enough to detect the toxin. The reported sensitivity for the EIA assay used was 80-90%, meaning that 10%-20% of patients with C. difficile disease would have had a false negative test. While a second negative test would lower the likelihood of true disease, it would not lower it enough in a patient with a high pre-test probability of disease to sufficiently rule out the disease such that further testing is indicated.
Additionally, while we can extrapolate that the EIA test was of little utility to the patients studied here, no patient-specific data is presented. Thus it is difficult to determine if our patient population is represented in the study. More knowledge about the patients would allow the reader to use published prediction rules to better delineate how likely it was that this cohort was at high risk for having toxin-mediated diarrhea. Perhaps a more reasonable approach to this clinical conundrum would be to send the repeat stool test for a cytotoxin assay or to treat the patient empirically in situations where either the likelihood of disease or the disease burden is high.
Stroke after MI
By Ethan Cumbler, MD
Witt BJ, Ballman KV, Brown RD Jr, et al. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006 Apr;119(4):354.e1-9.
Stroke and myocardial infarction (MI) share many of the risk factors leading to atherosclerosis, including hypertension, hyperlipidemia, diabetes, tobacco abuse, and age. Logically, patients at risk for one event would also be at risk for the other, yet this interaction appears to be more complex. The study by Witt, et al., aims to elucidate the rate of in-hospital stroke in patients initially admitted with an MI.
The authors analyzed 22 observational studies of myocardial infarction that recorded the incidence of cerebrovascular accidents after acute MI. Clinical trials were excluded from the analysis in order to provide representation of an unselected population. Of the trials reviewed, 11 were included in the analysis of in-hospital strokes, three for the 30-day time point, and two for the one-year time point. The other trials used different time points and were not included in the analysis. The patients had a mean age ranging between 59 and 72.7 years, and all had a predominance of males. The rate of in-hospital stroke was 11.1 events per 1,000 hospitalizations. This incidence rose to 12.2/1,000 at 30 days and 21.4/1,000 at one year.
Plausible hypotheses for why the rate of cerebrovascular accident would be particularly high in the post-MI period include the potential for localized wall motion dysmotility or low flow leading to intracardiac thrombosis, event-related arrhythmia, or procedure-related embolic events. The studies from which this meta-analysis was derived were not designed in such a way for a causal relationship to be identified. However, age, diabetes, hypertension, prior stroke, anterior location of MI, atrial fibrillation, heart failure, and nonwhite race were all found to have an association with increased risk for stroke. Interestingly, angina on presentation was associated with an apparent decreased risk, theorized to potentially be due to ischemic preconditioning.
While this study shares the usual limitations of meta-analyses of observational studies, the authors have done an excellent summation of the data available including both English and non-English language articles in the analysis. Notably, the review included studies spanning more than 25 years and, thus, included data from studies done in the era prior to modern therapy for cardiac ischemia including potent antiplatelet and statin therapy. The three studies with in-hospital time points started in the 1990s had a lower average rate of stroke, which may reflect the effect of more potent anti-platelet agents used in today’s therapy for acute coronary syndromes.
The implication for the hospitalist is to recognize that patients admitted for MI are at high risk for stroke during the index hospitalization. A low threshold for suspicion of a cerebrovascular event needs to be maintained for post-MI patients with new neurologic symptoms. Future studies will be needed to address the risk/benefit of anticoagulation in high-risk patients for stroke following a myocardial infarction.
Predicting PE in the ED Using Revised Geneva Score
By Jeffrey Carter, MD
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006 Feb 7;144(3):165-171.
Introduction: Pulmonary embolism remains a common life-threatening disorder with imperfect diagnostic modalities and strategies. Much of the current literature focuses on the development and validation of clinical probability assessments that identify low-risk patients who can be safely managed without invasive testing or lung scanning.
Two common scoring systems include the Geneva and Wells criteria, which employ a combination of historical information, clinical and laboratory data to stratify patients into three risk groups.1,2 It has recently been shown that a single negative D-dimer test safely excludes patients with suspected VTE in a large cohort, with a three-month follow-up rate of VTE of 0%.3 Criticism of current clinical probability assessment strategies include the inclusion of subjective criteria or the need for blood gas values.1,2 In this paper, the authors sought to derive and validate a scoring system based on readily available objective clinical data.
Methods: The cohort evaluated in this study consists of the same 965 patients used to prospectively evaluate an emergency department diagnostic strategy of VTE.3 Patients presenting to the emergency ward with complaints of chest pain or shortness of breath were evaluated with a standard diagnostic workup that included a checklist of demographic and historical information, signs and symptoms possibly consistent with VTE, ABG, chest X-ray, and EKG results, as well as the likelihood of another diagnosis. However, the goal was to create a scoring system based on readily available objective data, so ABG, chest X-ray and electrocardiogram results were not evaluated as possible components of the score. Clinical variables associated with pulmonary embolism were evaluated for statistical significance in both a univariate and multivariate model. These variables were then validated both internally and with an external cohort.
Results: The incidence of VTE was 23% (222/965). Ten clinical variables were found to be statistically significantly associated with VTE; these comprise the Revised Geneva Score.
Clinical probability is based on points: 0-3 is low probability; 4-10 is intermediate probability, and >10 is high probability. Low, intermediate, and high clinical probabilities had respective rates of VTE of 8%, 28%, and 74%. These percentages were found in the validation cohort and were similar to those in the derivation cohort.
Discussion: This study focuses on the derivation and validation of a clinical scoring system that can provide a numerical estimate of likelihood of VTE. The diagnostic strategy by which VTE is confirmed or excluded is from derivation cohort and is published elsewhere.3 In that study patients classified as no VTE and not treated had a 90-day risk of VTE of 1%. The nine-point revised Geneva score does indeed provide an accurate assessment of risk of VTE, and can thus help guide clinical decision-making. However it is not clear that the revised Geneva score will help decrease invasive diagnostic tests. In the low-risk group, 8% is too great a risk of a life-threatening illness to forego further diagnostic evaluation. Coupled with a negative ELISA D-dimer, exclusion of these patients is safe, but these patients cannot be safely excluded without risk stratification.3
References
- Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83:416-420.
- Wicki J, Perneger TV, Junof AF, et al. Assessing clinical probability of pulmonary embolism in the emergency ward: a simple score. Arch Intern Med. 2001 Jan 8;161(1):92-97.
- Perrier A, Roy PM, Aujesky D, et al. Diagnosing pulmonary embolism in outpatients with clinical assessment, D-dimer measurement, venous ultrasound and helical computed tomography: a multicenter management study. Am J Med. 2004 Mar 1;116(5):291-299.
LMWH for Inpatient Palliative Care
By Jeanie Youngwerth, MD
Noble SI, Nelson A, Turner C, et al. Acceptability of low molecular weight heparin thromboprophylaxis for patients receiving palliative care: qualitative study. BMJ. 2006 Mar 11:332(7541);577-580.ePub 2006 Feb 3.
Venous thromboembolism is a major risk factor for patients with malignancy. VTE may reduce survival time in patients receiving palliative care, with one in seven inpatients with cancer dying from pulmonary embolism. The American College of Chest Physicians recommend low molecular weight heparin (LMWH) in hospitalized patients with cancer as level 1A evidence in their 2004 consensus statement on VTE. There are no thromboprophylaxis guidelines in the United Kingdom. Many physicians view daily injections of LMWH as unnecessary distress for palliative care patients. This study focused on what inpatients with advanced cancer receiving palliative care thought about the effect of thromboprophylaxis on overall quality of life.
This was a qualitative study of 28 inpatients receiving palliative care who had advanced metastatic cancer and who were in a regional cancer center in Wales. The patients had received LMWH for at least five consecutive days. The patients were audiotaped and then had semi-structured interviews transcribed regarding cancer treatments they had received. These interviews covered the patients’ insight into prognosis, their understanding of thromboprophylaxis, their beliefs concerning the effects of thromboprophylaxis on overall quality of life, and the negative aspects of heparin treatment.
The main outcome measures were recurring themes of the effect of thromboprophylaxis on overall quality of life. Major themes identified were insight into prognosis, knowledge and understanding of thromboprophylaxis, acceptability of heparin thromboprophylaxis, reassurance, and optimism. Minor themes identified were bruising, negative impact of antiembolic stockings, and anger at paternalistic views toward terminally ill patients.
Most patients showed clear insight into the nature of their condition and understood heparin prophylaxis for VTE. Many patients identified immobility and surgery as VTE risk factors, with little understanding of cancer as a risk factor. All knew that VTE could cause death, but none were aware of the common symptoms. All patients found LMWH thromboprophylaxis acceptable. Patients believed taking measures to prevent symptoms might improve their quality of life and felt that the medical team had not given up on them.
The only negative experiences of LMWH thromboprophylaxis was bruising. All of the patients who wore antiembolic stockings during previous admissions found them uncomfortable. Patients expressed their need to be involved in decision-making, particularly with respect to withdrawal or non-administration of treatment.
This small, qualitative study showed that, contrary to many physicians’ beliefs, patients in palliative care units believe that LMWH injections are acceptable as thromboprophylaxis, but antiembolic stockings are not. The effect of daily injections had little or no effect on the quality of life, with many patients having positive feelings that things were being done to prevent new problems from occurring.
This study was limited by the small sample size, the qualitative nature that could introduce interpretation bias, and the fact that only patients using LMWH were included. Additionally, the United Kingdom has aggressively educated the public on the risks of VTE associated with long flights such that baseline knowledge may differ in other parts of the world. Resource utilization, including drug costs and length of stay, as well as effect on mortality were not studied.
The implications for hospitalists are that many inpatients with advanced cancer receiving palliative care may find LMWH thromboprophylaxis acceptable therapy, and that discussions with the patient regarding this option should be explored together.
Cost Analysis: Intensive Glycemic Control in Critically Ill Adults
By Whitney Woodmansee, MD
Krinsley JS, Jones, RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644-650.
Several studies have demonstrated improved outcomes and decreased mortality in ICU patients treated with intensive control of blood glucose levels. This study sought to identify the costs associated with intensive glycemic control in the ICU.
An ICU patient database was analyzed for cost data related to intensive glycemic control. A baseline group of 800 consecutive ICU patients admitted prior to initiation (baseline) of an intensive glucose management (blood glucose levels between 80-140 mg/dl protocol were compared with a treatment group of 800 consecutive patients admitted after initiation of the protocol). Previously reported outcomes of these patients demonstrated significant improvement in mortality with tight glycemic control. Costs related to ICU and non-ICU length of stay; duration of mechanical ventilation; and all laboratory, pharmacy, and radiology services were analyzed between groups. Resource utilization was determined by assessing charges from the database and adjusting for inflation and applying Medicare cost, charge ratios for each category, and fiscal year. Costs associated with the intensive glycemic control protocol were determined. Unfortunately, only cost estimates for insulin and associated disposable supplies for each group were available for analysis.
Baseline and treatment populations did not differ significantly regarding demographics such as age, gender, race, admitting diagnosis, diabetes prevalence, or APACHE II scores. There were fewer patients in the treatment group that required mechanical ventilation during their ICU stay (40.6% versus 33.6%). Intensive glucose management was associated with a 13.9% reduction in total ICU days and duration of mechanical ventilation (median of two days decreased to 1.7 days p=0.045). There was a $1,580 adjusted cost savings per patient in the intensive treatment group compared with the baseline group (p<0.001). This reduction in cost was primarily driven by a decrease in laboratory and radiology costs in the ventilated patients. There were nonsignificant cost reductions in the unventilated patients.
Intensive control of hyperglycemia in the hospitalized ICU patient appears to be associated with reduction of morbidity and mortality. This suggests that tight glycemic control also leads to reductions in overall patient care costs—particularly in the ventilated ICU patient. Although not a randomized control trial, database analysis of costs and resource utilization demonstrated an overall cost savings in the treatment group (after initiation of an intensive glycemic control protocol) compared with the baseline group (before protocol initiation). One caveat is that the authors used estimates when determining the costs associated with the implementation of the intensive glucose management protocol. Nevertheless, intensive glycemic control was associated with an overall reduction in patient costs related to decreased ICU days and mechanical ventilation as well as resource utilization in a patient population already shown to have improved mortality. These results, if confirmed, suggest that tight glycemic control in the ICU is cost effective and should become standard medical practice. TH
Repeat Testing for C. Diff?
By Jeff Glasheen, MD
Mohan SS, McDermott BP, Parchuri S, et al. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006 Apr;119(4):356.e7-356.e8
Clostridium difficile is a common complication of antibiotic and chemotherapeutic use, especially in hospitalized patients. Yet most nosocomial diarrhea is not caused by C. difficile. Most antibiotics can cause loose stools through changes in the gastrointestinal flora that result in inadequate digestion and absorption of carbohydrates and a resultant osmotic diarrhea. Further, antibiotics such as erythromycin and amoxicillin/clavulanate may result in diarrhea via increases in GI tract motility. While osmotic and motility causes of diarrhea tend to improve with antibiotic discontinuation, C. difficile-associated diarrhea is associated with significant morbidity that often continues until adequately treated.
Thus having a test that differentiates between C. difficile and non-clostridial diarrhea is essential. The most commonly used test is the enzyme immunoassay (EIA) that detects toxins A and B. The sensitivity and specificity of this test has been reported to range between 50%-90% and 70%-95%, respectively. The authors of this paper evaluated the utility of repeat EIA testing in patients with a one negative test in the setting of nosocomial diarrhea associated with antibiotic use.
The authors reviewed 474 sequential EIA tests for C. difficile in 396 patients over a 10-month period at a large university-affiliated community hospital with an EIA sensitivity and specificity of 80%-90% and 80%-95%, respectively. Tests were considered to be “repeat” if they occurred within seven days of the original negative test. Of the 78 repeat tests (16.5% of all tests), only one was positive, resulting in a 0.8% conversion rate. At an institutional cost of $128 per test the total cost of EIA testing over the 10-month period was $60,672. The cost of repeat testing alone was $9,984. The authors conclude that there is limited value—and high cost—in repeat EIA testing and that alternative sources of diarrhea should be sought or we should repeat EIA testing in patients with continued nosocomial diarrhea and a negative EIA test.
While prior studies have shown incremental benefit of retesting for C. difficile with the EIA assay, this study’s authors conclude that repeat “C. difficile testing is not clinically justified and is economically wasteful.” Unfortunately, the authors did not utilize a strong enough research design to defend this statement. From the data presented, all we can conclude is that repeat testing with an EIA assay did not add significant value to the diagnostic workup. The lack of a negative gold standard test, such as the cytotoxin assay or follow up outcomes, such as resolution of diarrhea, leaves the reader pondering if the repeat EIA assays were negative because the patients did not have C. difficile or because the test was not sensitive enough to detect the toxin. The reported sensitivity for the EIA assay used was 80-90%, meaning that 10%-20% of patients with C. difficile disease would have had a false negative test. While a second negative test would lower the likelihood of true disease, it would not lower it enough in a patient with a high pre-test probability of disease to sufficiently rule out the disease such that further testing is indicated.
Additionally, while we can extrapolate that the EIA test was of little utility to the patients studied here, no patient-specific data is presented. Thus it is difficult to determine if our patient population is represented in the study. More knowledge about the patients would allow the reader to use published prediction rules to better delineate how likely it was that this cohort was at high risk for having toxin-mediated diarrhea. Perhaps a more reasonable approach to this clinical conundrum would be to send the repeat stool test for a cytotoxin assay or to treat the patient empirically in situations where either the likelihood of disease or the disease burden is high.
Stroke after MI
By Ethan Cumbler, MD
Witt BJ, Ballman KV, Brown RD Jr, et al. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006 Apr;119(4):354.e1-9.
Stroke and myocardial infarction (MI) share many of the risk factors leading to atherosclerosis, including hypertension, hyperlipidemia, diabetes, tobacco abuse, and age. Logically, patients at risk for one event would also be at risk for the other, yet this interaction appears to be more complex. The study by Witt, et al., aims to elucidate the rate of in-hospital stroke in patients initially admitted with an MI.
The authors analyzed 22 observational studies of myocardial infarction that recorded the incidence of cerebrovascular accidents after acute MI. Clinical trials were excluded from the analysis in order to provide representation of an unselected population. Of the trials reviewed, 11 were included in the analysis of in-hospital strokes, three for the 30-day time point, and two for the one-year time point. The other trials used different time points and were not included in the analysis. The patients had a mean age ranging between 59 and 72.7 years, and all had a predominance of males. The rate of in-hospital stroke was 11.1 events per 1,000 hospitalizations. This incidence rose to 12.2/1,000 at 30 days and 21.4/1,000 at one year.
Plausible hypotheses for why the rate of cerebrovascular accident would be particularly high in the post-MI period include the potential for localized wall motion dysmotility or low flow leading to intracardiac thrombosis, event-related arrhythmia, or procedure-related embolic events. The studies from which this meta-analysis was derived were not designed in such a way for a causal relationship to be identified. However, age, diabetes, hypertension, prior stroke, anterior location of MI, atrial fibrillation, heart failure, and nonwhite race were all found to have an association with increased risk for stroke. Interestingly, angina on presentation was associated with an apparent decreased risk, theorized to potentially be due to ischemic preconditioning.
While this study shares the usual limitations of meta-analyses of observational studies, the authors have done an excellent summation of the data available including both English and non-English language articles in the analysis. Notably, the review included studies spanning more than 25 years and, thus, included data from studies done in the era prior to modern therapy for cardiac ischemia including potent antiplatelet and statin therapy. The three studies with in-hospital time points started in the 1990s had a lower average rate of stroke, which may reflect the effect of more potent anti-platelet agents used in today’s therapy for acute coronary syndromes.
The implication for the hospitalist is to recognize that patients admitted for MI are at high risk for stroke during the index hospitalization. A low threshold for suspicion of a cerebrovascular event needs to be maintained for post-MI patients with new neurologic symptoms. Future studies will be needed to address the risk/benefit of anticoagulation in high-risk patients for stroke following a myocardial infarction.
Predicting PE in the ED Using Revised Geneva Score
By Jeffrey Carter, MD
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006 Feb 7;144(3):165-171.
Introduction: Pulmonary embolism remains a common life-threatening disorder with imperfect diagnostic modalities and strategies. Much of the current literature focuses on the development and validation of clinical probability assessments that identify low-risk patients who can be safely managed without invasive testing or lung scanning.
Two common scoring systems include the Geneva and Wells criteria, which employ a combination of historical information, clinical and laboratory data to stratify patients into three risk groups.1,2 It has recently been shown that a single negative D-dimer test safely excludes patients with suspected VTE in a large cohort, with a three-month follow-up rate of VTE of 0%.3 Criticism of current clinical probability assessment strategies include the inclusion of subjective criteria or the need for blood gas values.1,2 In this paper, the authors sought to derive and validate a scoring system based on readily available objective clinical data.
Methods: The cohort evaluated in this study consists of the same 965 patients used to prospectively evaluate an emergency department diagnostic strategy of VTE.3 Patients presenting to the emergency ward with complaints of chest pain or shortness of breath were evaluated with a standard diagnostic workup that included a checklist of demographic and historical information, signs and symptoms possibly consistent with VTE, ABG, chest X-ray, and EKG results, as well as the likelihood of another diagnosis. However, the goal was to create a scoring system based on readily available objective data, so ABG, chest X-ray and electrocardiogram results were not evaluated as possible components of the score. Clinical variables associated with pulmonary embolism were evaluated for statistical significance in both a univariate and multivariate model. These variables were then validated both internally and with an external cohort.
Results: The incidence of VTE was 23% (222/965). Ten clinical variables were found to be statistically significantly associated with VTE; these comprise the Revised Geneva Score.
Clinical probability is based on points: 0-3 is low probability; 4-10 is intermediate probability, and >10 is high probability. Low, intermediate, and high clinical probabilities had respective rates of VTE of 8%, 28%, and 74%. These percentages were found in the validation cohort and were similar to those in the derivation cohort.
Discussion: This study focuses on the derivation and validation of a clinical scoring system that can provide a numerical estimate of likelihood of VTE. The diagnostic strategy by which VTE is confirmed or excluded is from derivation cohort and is published elsewhere.3 In that study patients classified as no VTE and not treated had a 90-day risk of VTE of 1%. The nine-point revised Geneva score does indeed provide an accurate assessment of risk of VTE, and can thus help guide clinical decision-making. However it is not clear that the revised Geneva score will help decrease invasive diagnostic tests. In the low-risk group, 8% is too great a risk of a life-threatening illness to forego further diagnostic evaluation. Coupled with a negative ELISA D-dimer, exclusion of these patients is safe, but these patients cannot be safely excluded without risk stratification.3
References
- Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83:416-420.
- Wicki J, Perneger TV, Junof AF, et al. Assessing clinical probability of pulmonary embolism in the emergency ward: a simple score. Arch Intern Med. 2001 Jan 8;161(1):92-97.
- Perrier A, Roy PM, Aujesky D, et al. Diagnosing pulmonary embolism in outpatients with clinical assessment, D-dimer measurement, venous ultrasound and helical computed tomography: a multicenter management study. Am J Med. 2004 Mar 1;116(5):291-299.
LMWH for Inpatient Palliative Care
By Jeanie Youngwerth, MD
Noble SI, Nelson A, Turner C, et al. Acceptability of low molecular weight heparin thromboprophylaxis for patients receiving palliative care: qualitative study. BMJ. 2006 Mar 11:332(7541);577-580.ePub 2006 Feb 3.
Venous thromboembolism is a major risk factor for patients with malignancy. VTE may reduce survival time in patients receiving palliative care, with one in seven inpatients with cancer dying from pulmonary embolism. The American College of Chest Physicians recommend low molecular weight heparin (LMWH) in hospitalized patients with cancer as level 1A evidence in their 2004 consensus statement on VTE. There are no thromboprophylaxis guidelines in the United Kingdom. Many physicians view daily injections of LMWH as unnecessary distress for palliative care patients. This study focused on what inpatients with advanced cancer receiving palliative care thought about the effect of thromboprophylaxis on overall quality of life.
This was a qualitative study of 28 inpatients receiving palliative care who had advanced metastatic cancer and who were in a regional cancer center in Wales. The patients had received LMWH for at least five consecutive days. The patients were audiotaped and then had semi-structured interviews transcribed regarding cancer treatments they had received. These interviews covered the patients’ insight into prognosis, their understanding of thromboprophylaxis, their beliefs concerning the effects of thromboprophylaxis on overall quality of life, and the negative aspects of heparin treatment.
The main outcome measures were recurring themes of the effect of thromboprophylaxis on overall quality of life. Major themes identified were insight into prognosis, knowledge and understanding of thromboprophylaxis, acceptability of heparin thromboprophylaxis, reassurance, and optimism. Minor themes identified were bruising, negative impact of antiembolic stockings, and anger at paternalistic views toward terminally ill patients.
Most patients showed clear insight into the nature of their condition and understood heparin prophylaxis for VTE. Many patients identified immobility and surgery as VTE risk factors, with little understanding of cancer as a risk factor. All knew that VTE could cause death, but none were aware of the common symptoms. All patients found LMWH thromboprophylaxis acceptable. Patients believed taking measures to prevent symptoms might improve their quality of life and felt that the medical team had not given up on them.
The only negative experiences of LMWH thromboprophylaxis was bruising. All of the patients who wore antiembolic stockings during previous admissions found them uncomfortable. Patients expressed their need to be involved in decision-making, particularly with respect to withdrawal or non-administration of treatment.
This small, qualitative study showed that, contrary to many physicians’ beliefs, patients in palliative care units believe that LMWH injections are acceptable as thromboprophylaxis, but antiembolic stockings are not. The effect of daily injections had little or no effect on the quality of life, with many patients having positive feelings that things were being done to prevent new problems from occurring.
This study was limited by the small sample size, the qualitative nature that could introduce interpretation bias, and the fact that only patients using LMWH were included. Additionally, the United Kingdom has aggressively educated the public on the risks of VTE associated with long flights such that baseline knowledge may differ in other parts of the world. Resource utilization, including drug costs and length of stay, as well as effect on mortality were not studied.
The implications for hospitalists are that many inpatients with advanced cancer receiving palliative care may find LMWH thromboprophylaxis acceptable therapy, and that discussions with the patient regarding this option should be explored together.
Cost Analysis: Intensive Glycemic Control in Critically Ill Adults
By Whitney Woodmansee, MD
Krinsley JS, Jones, RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644-650.
Several studies have demonstrated improved outcomes and decreased mortality in ICU patients treated with intensive control of blood glucose levels. This study sought to identify the costs associated with intensive glycemic control in the ICU.
An ICU patient database was analyzed for cost data related to intensive glycemic control. A baseline group of 800 consecutive ICU patients admitted prior to initiation (baseline) of an intensive glucose management (blood glucose levels between 80-140 mg/dl protocol were compared with a treatment group of 800 consecutive patients admitted after initiation of the protocol). Previously reported outcomes of these patients demonstrated significant improvement in mortality with tight glycemic control. Costs related to ICU and non-ICU length of stay; duration of mechanical ventilation; and all laboratory, pharmacy, and radiology services were analyzed between groups. Resource utilization was determined by assessing charges from the database and adjusting for inflation and applying Medicare cost, charge ratios for each category, and fiscal year. Costs associated with the intensive glycemic control protocol were determined. Unfortunately, only cost estimates for insulin and associated disposable supplies for each group were available for analysis.
Baseline and treatment populations did not differ significantly regarding demographics such as age, gender, race, admitting diagnosis, diabetes prevalence, or APACHE II scores. There were fewer patients in the treatment group that required mechanical ventilation during their ICU stay (40.6% versus 33.6%). Intensive glucose management was associated with a 13.9% reduction in total ICU days and duration of mechanical ventilation (median of two days decreased to 1.7 days p=0.045). There was a $1,580 adjusted cost savings per patient in the intensive treatment group compared with the baseline group (p<0.001). This reduction in cost was primarily driven by a decrease in laboratory and radiology costs in the ventilated patients. There were nonsignificant cost reductions in the unventilated patients.
Intensive control of hyperglycemia in the hospitalized ICU patient appears to be associated with reduction of morbidity and mortality. This suggests that tight glycemic control also leads to reductions in overall patient care costs—particularly in the ventilated ICU patient. Although not a randomized control trial, database analysis of costs and resource utilization demonstrated an overall cost savings in the treatment group (after initiation of an intensive glycemic control protocol) compared with the baseline group (before protocol initiation). One caveat is that the authors used estimates when determining the costs associated with the implementation of the intensive glucose management protocol. Nevertheless, intensive glycemic control was associated with an overall reduction in patient costs related to decreased ICU days and mechanical ventilation as well as resource utilization in a patient population already shown to have improved mortality. These results, if confirmed, suggest that tight glycemic control in the ICU is cost effective and should become standard medical practice. TH